Computational Modeling of Endometrial Dynamics: From Digital Twins to Clinical Translation
This article provides a comprehensive overview of the rapidly evolving field of computational modeling of the endometrium, a critical frontier in women's health research.
Computational Modeling of Endometrial Dynamics: From Digital Twins to Clinical Translation
Abstract
This article provides a comprehensive overview of the rapidly evolving field of computational modeling of the endometrium, a critical frontier in women's health research. We explore the foundational mathematical principles, from phenomenological models capturing hormonal regulation to sophisticated quantitative systems pharmacology (QSP) frameworks. The review details the application of diverse methodologies, including machine learning for diagnostic prediction, spatial eco-structural models of the tumor microenvironment, and agent-based simulations. We critically examine the challenges of model validation and optimization, highlighting the synergistic role of 3D organoids as biological validation platforms and the use of AI for refining model parameters. Finally, we present a comparative analysis of model types—from fractional calculus for capturing treatment memory effects to optimal control theory for designing personalized therapy regimens. This synthesis is tailored for researchers, scientists, and drug development professionals seeking to leverage computational power to decode endometrial biology, accelerate therapeutic discovery, and pave the way for personalized medicine in conditions like endometriosis, endometrial cancer, and infertility.
Decoding the Endometrium: Foundational Principles and Mathematical Frameworks
Biological Foundations of Endometrial Dynamics
The human endometrium, the inner lining of the uterus, exhibits remarkable regenerative capacity, undergoing more than 400 cycles of growth, differentiation, and shedding throughout a woman's reproductive life [1]. This dynamic tissue is exquisitely responsive to systemic hormonal cues, primarily 17β-estradiol (E2) and progesterone (P4), which orchestrate precise morphological and physiological changes across the menstrual cycle [2]. The endometrium consists of two distinct layers: the stratum functionalis (functional layer) that undergoes cyclic changes and is shed during menstruation, and the stratum basalis (basal layer) that remains and facilitates regeneration [1] [2].
Endometrial regeneration involves complex interactions between multiple cell types, including luminal and glandular epithelial cells, stromal cells, vascular endothelium, and immune cells, all embedded within a dynamically remodeling extracellular matrix (ECM) [1]. Recent 3D imaging has revealed that endometrial glands in the basalis layer form a unique rhizome-like network that expands horizontally along the myometrium, with glands vertically emanating into the functionalis layer [1]. This sophisticated architecture supports the endometrium's exceptional regenerative capability, characterized by repeated shedding and subsequent regeneration without scarring [3].
The menstrual cycle progresses through three distinct phases driven by hormonal fluctuations:
- Menstrual phase: Shedding of the functionalis layer when no embryo implants
- Proliferative phase: Estrogen-driven regeneration and growth of the functionalis
- Secretory phase: Progesterone-mediated differentiation to support embryo implantation [2]
These cyclic transformations make the endometrium one of the most dynamically regenerative tissues in the human body, yet this complexity also renders it susceptible to various pathologies when regulatory mechanisms fail.
Endometrial Pathologies and Clinical Challenges
Dysregulation of endometrial dynamics underlies several prevalent diseases that affect millions of women worldwide, often with limited treatment options. The major endometrial pathologies include:
Table 1: Major Endometrial Pathologies and Their Characteristics
| Disease | Key Pathological Feature | Clinical Challenges |
|---|---|---|
| Asherman Syndrome | Intrauterine adhesions and scarring following endometrial damage [1] | Infertility, menstrual disturbances, poor response to hormone therapy [4] |
| Thin Endometrium | Inadequate endometrial growth with thickness typically <7mm [4] | Failed embryo implantation, low success rates in assisted reproduction [4] |
| Endometriosis | Presence of endometrial-like tissue outside the uterine cavity [1] | Chronic pain, infertility, inflammation, and altered hormone response [1] |
| Adenomyosis | Endometrial tissue misplaced within the myometrium [1] | Heavy menstrual bleeding, pain, and altered hormone response [1] |
| Endometrial Cancer | Malignant proliferation of endometrial cells, often linked to hormonal imbalances [1] | Hyperproliferation, progression from endometrial hyperplasia [1] |
The etiology of thin endometrium exemplifies the multifactorial nature of endometrial disorders, with proposed causes including Asherman's syndrome, previous intrauterine surgery, pelvic radiation, genetic factors, impaired uterine blood flow, infections, certain medications, and dysfunctional estrogen signaling [4]. A recent single-cell RNA sequencing study further suggested that cellular senescence in stroma and epithelium combined with collagen overdeposition around blood vessels contributes to endometrial thinness [4].
Conventional treatments for endometrial disorders, including hormonal therapies, growth factors, and vasoactive substances, have demonstrated limited and inconsistent efficacy [4]. This therapeutic challenge underscores the critical need for more sophisticated research models that can accurately capture endometrial complexity and enable the development of more effective interventions.
Experimental Models for Studying Endometrial Dynamics
Traditional Research Models and Their Limitations
Endometrial research has historically relied on various model systems, each with distinct advantages and limitations for studying tissue dynamics:
Table 2: Comparison of Endometrial Research Models
| Model System | Advantages | Limitations |
|---|---|---|
| Animal Models (rodents, primates) [1] | Replicate entire lesion with all cell types; enable study of regeneration and systemic effects [1] | Costly; significant physiological variations between species; cannot exactly reproduce human disease [1] |
| Tissue Explants [1] | Preserve 3D tissue structure; retain all native cell types and physical interactions [1] | Reduced viability after 24 hours; limited ability to manipulate specific cell types [1] |
| 2D Cell Cultures [1] | Simple, inexpensive; enable high-throughput compound testing [1] | Cannot reproduce tissue architecture or cell-ECM interactions; lack physiological relevance [1] |
| Co-culture Models [1] | Include multiple cell types; study paracrine or direct cell interactions [1] | Do not necessarily replicate tissue structure; extended culture difficult [1] |
While these traditional approaches have yielded valuable insights, their limitations have impeded progress in understanding endometrial disease mechanisms and developing effective treatments. The field has particularly struggled with models that adequately recapitulate the dynamic hormonal responses, complex cell-cell interactions, and 3D tissue architecture characteristic of human endometrium.
Advanced Bioengineering Approaches
Recent advances in bioengineering have generated more sophisticated models that better mimic the endometrial microenvironment:
Endometrial Organoids: These 3D self-organizing structures derived from primary endometrial cells replicate key aspects of endometrial physiology, including epithelial cell polarity, hormone responsiveness, and gene expression profiles of eutopic and ectopic endometrium [1]. They can be established from menstrual flow non-invasively and are amenable to long-term expansion, biobanking, and drug testing [1] [3]. However, current endometriosis organoids typically contain only one cell type and do not fully reproduce interactions between endometrial cells and their microenvironment [1].
Microfluidic Systems: These platforms enable precise control over the cellular microenvironment and can replicate uterine peristaltic movement through controlled fluid flow and shear stresses [1]. They allow for the integration of multiple cell types and environmental factors, though current systems often lack circulation of culture medium and may be limited to endometrial cells only [1].
Bioengineered Scaffolds: Natural and synthetic hydrogel-based scaffolds simulate the physical and biomechanical properties of the native endometrium, maintaining the survival of transplanted stem cells and facilitating endometrial repair [3]. These materials show promise for supporting endometrial regeneration and improving reproductive outcomes.
Computational Modeling Approaches
Mathematical Modeling of Menstrual Cycle Dynamics
Phenomenological-based mathematical models represent a powerful approach for simulating the dynamic changes in endometrial tissue throughout the menstrual cycle. These models connect physiological phenomena with quantitative accuracy, allowing researchers to simulate multiple menstrual cycles and test hypotheses about regulatory mechanisms [2].
A recently developed phenomenological-based model predicts volume changes in the functional layer of the endometrium across menstrual cycle phases by considering changes in endometrial tissue, blood flow through spiral arteries, shedding of endometrial cells, and menstrual blood flow [2]. The model uses estrogen and progesterone dynamics as input variables, with hormone levels taken from a pre-existing validated model [2]. Key aspects of this modeling approach include:
- Tissue Dynamics: Modeling the growth and regression of endometrial tissue in response to hormonal signals
- Vascular Changes: Simulating the development and regression of spiral arteries that supply the functionalis layer
- Shedding Mechanisms: Representing the process of tissue breakdown and menstruation
- Feedback Loops: Incorporating regulatory interactions between hormones, tissue growth, and vascular development
This model successfully simulated endometrial volume and thickness changes that align with experimental data from the literature, providing valuable insights into the interactions between ovarian hormones and endometrial dynamics [2].
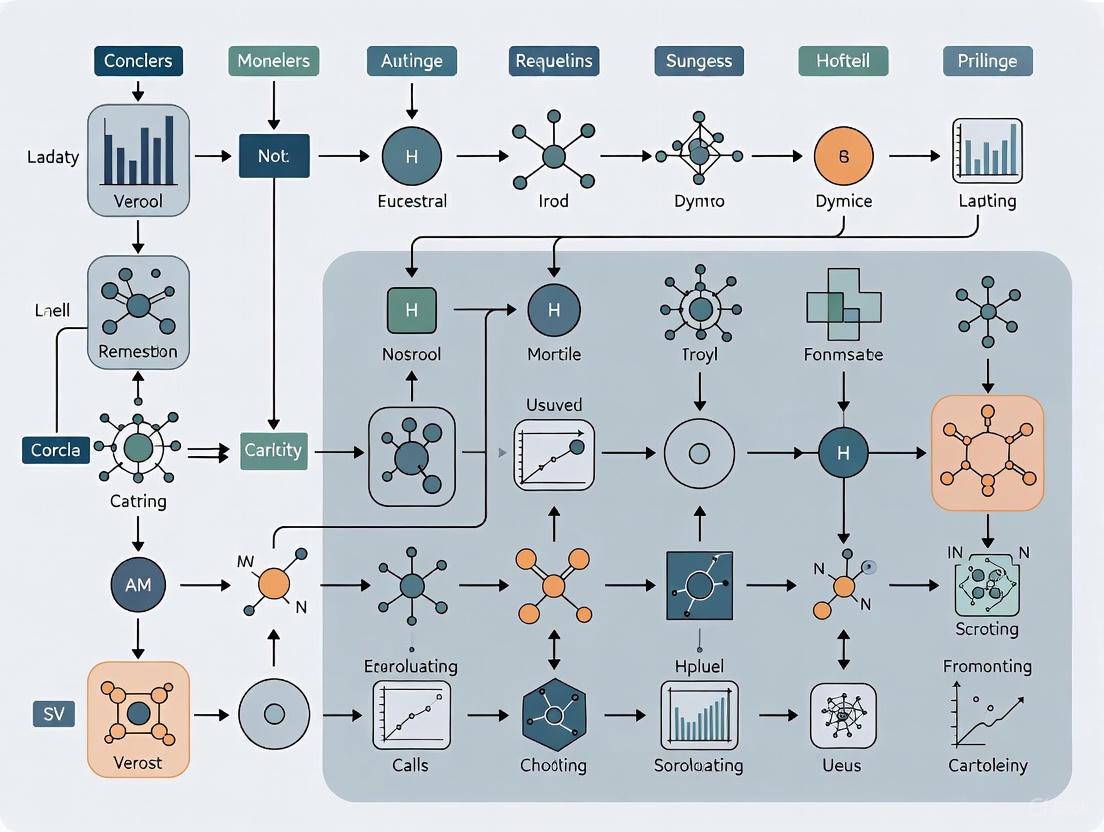
Diagram Title: Menstrual Cycle Computational Model Structure
Comparative Analysis of Computational Modeling Algorithms
In other domains of biological research, comparative studies of computational modeling algorithms have demonstrated the importance of selecting appropriate methods for specific research questions. A recent study comparing protein or peptide modeling algorithms revealed that different approaches have complementary strengths depending on the properties of the target molecule [5].
For hydrophobic peptides, AlphaFold and Threading approaches complemented each other, while for hydrophilic peptides, PEP-FOLD and Homology Modeling showed complementary strengths [5]. PEP-FOLD provided both compact structures and stable dynamics for most peptides, while AlphaFold generated compact structures for most targets [5]. These findings highlight that an integrated approach combining multiple algorithms may yield superior results compared to relying on a single method—a principle that likely applies to endometrial modeling as well.
Molecular dynamics (MD) simulations have emerged as particularly valuable for studying structural stability and intramolecular interactions over time. In the peptide modeling study, researchers performed 40 simulations (100 ns each) to determine the stability of structures predicted by different algorithms [5]. Similar approaches could be adapted to study the dynamics of endometrial proteins and signaling molecules involved in menstrual cycle regulation.
Experimental Protocols for Endometrial Research
Protocol: Establishing and Maintaining Endometrial Organoids
Purpose: To create 3D in vitro models that closely mimic endometrial architecture and function for disease modeling and drug testing [1].
Materials:
- Human endometrial tissue samples or menstrual flow collection
- Advanced DMEM/F-12 culture medium
- Essential growth factors (EGF, Noggin, R-spondin)
- Matrigel or other ECM scaffold
- Hormone supplements (estradiol, progesterone)
- Digestion enzymes (collagenase, dispase)
Procedure:
- Tissue Processing: Mechanically mince endometrial tissue samples and digest with collagenase/dispase solution (2 mg/mL) at 37°C for 60-90 minutes [1].
- Cell Isolation: Sequential filtration through 100μm and 40μm strainers to isolate epithelial fragments. Centrifuge at 800×g for 5 minutes.
- Matrix Embedding: Resuspend cell pellets in ice-cold Matrigel and plate as droplets in pre-warmed culture plates. Polymerize at 37°C for 30 minutes.
- Organoid Culture: Overlay with complete culture medium containing required growth factors and hormones. Culture at 37°C with 5% CO₂.
- Medium Refreshment: Change culture medium every 2-3 days, monitoring organoid formation and growth.
- Passaging: For maintenance, dissociate organoids with TrypLE every 7-14 days and replate in fresh Matrigel.
Applications: Disease modeling, drug screening, host-pathogen interaction studies, and personalized medicine approaches [1].
Protocol: Implementing a Phenomenological-Based Mathematical Model
Purpose: To develop a dynamic model predicting endometrial volume changes during the menstrual cycle in response to ovarian hormones [2].
Materials:
- Computational environment (MATLAB, Python, or similar)
- Experimental data for validation (endometrial volume/thickness measurements)
- Hormonal concentration data (estrogen, progesterone)
- Parameter estimation algorithms
Procedure:
- System Definition: Identify key system components—endometrial tissue volume, spiral artery length, menstrual blood flow [2].
- Equation Formulation: Develop differential equations representing growth, regression, and shedding processes based on physiological principles.
- Parameter Estimation: Use literature data and optimization algorithms to estimate model parameters that minimize difference between simulations and experimental data [2].
- Hormonal Inputs: Integrate pre-validated models of estrogen and progesterone dynamics as system inputs [2].
- Model Validation: Compare simulation outputs with independent experimental data for endometrial volume, thickness, and menstrual blood flow [2].
- Sensitivity Analysis: Identify parameters with greatest influence on system behavior to guide future experimental measurements.
Applications: Testing hypotheses about regulatory mechanisms, predicting pathological conditions, and simulating interventional strategies [2].
Research Reagent Solutions for Endometrial Studies
Table 3: Essential Research Reagents for Endometrial Dynamics Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Cell Culture Media [1] | Advanced DMEM/F-12, organoid culture media | Support growth and maintenance of endometrial cells and organoids |
| Growth Factors [1] [4] | EGF, Noggin, R-spondin, G-CSF | Promote cell proliferation and differentiation in 2D and 3D culture systems |
| Enzymatic Dissociation [1] | Collagenase, Dispase, TrypLE | Tissue processing and organoid passaging |
| Extracellular Matrices [1] [3] | Matrigel, synthetic hydrogels, HA-based scaffolds | Provide 3D support structure for organoids and tissue engineering |
| Hormonal Supplements [1] [2] | 17β-estradiol, progesterone, selective receptor modulators | Study hormone response and mimic menstrual cycle phases |
| Stem Cell Markers [4] | CD133+, mesenchymal stem cell markers | Isolation and characterization of regenerative cell populations |
| Computational Tools [5] [2] | MATLAB, Python, molecular dynamics software | Implement mathematical models and analyze complex datasets |
Diagram Title: Integrated Endometrial Research Workflow
Future Perspectives and Integrative Approaches
The future of endometrial research lies in developing increasingly sophisticated integrated approaches that combine advanced experimental models with computational methods. Organoid technology, microfluidic systems, and bioengineered scaffolds continue to evolve toward more faithfully recapitulating the native endometrial microenvironment [1] [3]. Similarly, computational models are incorporating more biological detail, including immune cell interactions, spatial organization, and multi-scale regulatory networks.
Emerging therapeutic strategies for endometrial disorders highlight the potential of these integrated approaches. Platelet-rich plasma (PRP) therapy, rich in growth factors and cytokines, has shown promise in improving endometrial thickness and receptivity in clinical studies, though standardized protocols are still needed [4]. Stem cell therapies using bone-marrow-derived stem cells (BMDSCs) and adipose-derived stem cells (ADSCs) have demonstrated ability to restore endometrial function and improve reproductive outcomes in pilot trials [4]. These interventions represent a new frontier in treating conditions like thin endometrium and Asherman's syndrome that have historically proven challenging to manage.
Computational modeling will play an increasingly critical role in optimizing these therapies by predicting treatment outcomes, personalizing intervention strategies, and reducing the need for extensive trial-and-error experimentation. As mathematical models incorporate more biological complexity and are validated against data from advanced experimental systems, they will accelerate the translation of basic research findings into clinical applications, ultimately improving diagnostic and therapeutic approaches for endometrial disorders.
The human endometrium exhibits a remarkable capacity for cyclical regeneration, undergoing monthly phases of growth, differentiation, and shedding in response to ovarian hormone fluctuations. Phenomenological-based modeling has emerged as a powerful computational framework for simulating these dynamic processes by integrating mathematical formalism with physiological understanding. Unlike purely data-driven approaches, phenomenological models maintain a direct connection to underlying biological mechanisms while achieving quantitative accuracy in predicting system behavior [2]. This approach enables researchers to move beyond statistical correlations to capture the causal relationships governing endometrial dynamics.
Within the broader context of computational modeling of endometrial dynamics, phenomenological-based models fill a critical niche between overly simplistic statistical regressions and prohibitively complex mechanistic descriptions. They incorporate key physiological phenomena—including hormonal regulation, tissue growth, vascular changes, and menstrual shedding—into a mathematically tractable framework that can be validated against experimental data [2]. This balance of biological interpretability and computational efficiency makes these models particularly valuable for both basic research and pharmaceutical development, allowing researchers to simulate intervention outcomes and generate testable hypotheses about endometrial function and dysfunction.
Biological Foundation: Endometrial Dynamics and Hormonal Regulation
Endometrial Compartments and Menstrual Cycle Phases
The endometrium consists of two primary layers: the stratum basalis (basal layer) and stratum functionalis (functional layer). The basalis remains relatively stable throughout the menstrual cycle, providing progenitor cells for monthly regeneration. In contrast, the functionalis—comprising approximately two-thirds of the endometrial thickness—undergoes dramatic cyclic changes in response to ovarian hormones [2]. This compartmentalization is fundamental to menstrual function, as the functional layer is selectively shed during menstruation while the basal layer is preserved to support subsequent regeneration [6].
The endometrial cycle progresses through three distinct phases regulated by systemic concentrations of 17β-estradiol (E2) and progesterone (P4):
- Proliferative Phase: Characterized by estrogen-driven regeneration and growth of the functional layer following menstruation.
- Secretory Phase: Initiated after ovulation, marked by progesterone-induced differentiation and vascular development to support potential implantation.
- Menstrual Phase: Triggered by progesterone withdrawal in the absence of pregnancy, involving tissue breakdown and shedding of the functionalis [2].
Hormonal Regulation and Key Physiological Processes
Ovarian sex steroids directly regulate endometrial transformations through receptor-mediated signaling pathways. Estrogen promotes endometrial proliferation and growth, while progesterone induces secretory differentiation and stabilizes the endometrium. The precise coordination of these hormonal signals ensures proper timing of endometrial receptivity and, in the absence of pregnancy, controlled tissue breakdown [2].
Critical processes incorporated into phenomenological models include:
- Endometrial Tissue Dynamics: Volume changes in the functional layer across cycle phases.
- Vascular Changes: Blood flow modulation through spiral arteries and associated angiogenesis.
- Menstrual Shedding: Controlled breakdown and removal of endometrial tissue.
- Cellular Turnover: Balance between proliferation, differentiation, and apoptosis [2].
Table 1: Key Hormonal Regulators of Endometrial Dynamics
| Hormone | Primary Source | Major Endometrial Actions | Phase of Dominance |
|---|---|---|---|
| 17β-Estradiol (E2) | Ovarian Follicles | Stimulates proliferation & growth | Proliferative Phase |
| Progesterone (P4) | Corpus Luteum | Promotes differentiation & secretory activity | Secretory Phase |
| Gonadotropins (FSH/LH) | Anterior Pituitary | Regulate ovarian steroid production | Throughout Cycle |
Model Development: Mathematical Framework and Implementation
Core Mathematical Structure and State Variables
Phenomenological-based models of endometrial dynamics employ ordinary differential equations to describe the temporal evolution of key state variables in response to hormonal inputs. The core model structure typically tracks multiple interacting components:
- Functional Layer Volume (V_f): Represents the changing volume of the endometrial functionalis throughout the menstrual cycle.
- Spiral Artery Length (L_s): Captures the development and regression of the endometrial vasculature.
- Menstrual Blood Flow (F_m): Quantifies the extent of menstrual fluid loss during shedding.
- Hormonal Inputs (E2, P4): Model inputs derived from validated endocrine models of the ovarian cycle [2].
The general mathematical formulation follows a phenomenological-based semi-physical modeling approach, where differential equations are derived from understanding the underlying physiological phenomena rather than purely first principles or empirical fitting. This ensures parameters maintain biological interpretability while achieving quantitative accuracy [2].
Model Equations and Parameter Estimation
The system dynamics are described through coupled differential equations that capture the dominant phenomena governing endometrial behavior. For the functional layer volume, the rate of change can be expressed as:
dVf/dt = kg·f(E2) - kd·g(P4withdrawal) - ks·h(inflammatoryfactors)
Where:
- k_g represents the growth rate constant stimulated by estrogen
- k_d denotes the degradation rate following progesterone withdrawal
- k_s captures the shedding rate during menstruation
- f, g, h are phenomenological functions describing hormonal and inflammatory effects
Parameter estimation utilizes experimental data from multiple sources, including:
- Endometrial volume and thickness measurements from medical imaging
- Menstrual blood loss quantification
- Histological dating of endometrial biopsies
- Hormone concentration profiles from serum assays [2]
Table 2: Key Parameters in Endometrial Phenomenological Models
| Parameter | Biological Interpretation | Estimation Method | Typical Range |
|---|---|---|---|
| k_g | Estrogen-driven growth rate constant | Fit to proliferative phase volume data | 0.1-0.3 dayâ»Â¹ |
| k_d | Progesterone withdrawal degradation constant | Fit to secretory phase regression | 0.05-0.15 dayâ»Â¹ |
| k_s | Menstrual shedding rate constant | Fit to menstrual blood flow measurements | 0.2-0.5 dayâ»Â¹ |
| Ï„ | Hormonal effect time delay | Estimated from histologic dating | 1-3 days |
| E2â‚…â‚€ | Estrogen half-saturation constant | Derived from receptor binding studies | 50-150 pg/mL |
Experimental Protocols for Model Validation
Endometrial Tissue Collection and Processing
Purpose: To obtain quantitative data on endometrial cellular composition and structure for model parameterization and validation.
Materials Required:
- Endometrial biopsy catheter or curette
- Transport medium (Advanced DMEM/F12 with antibiotics)
- Collagenase IV or Liberase digestion enzymes
- Phosphate-buffered saline (PBS)
- Tissue culture plates with Matrigel matrix
- Organoid culture medium supplements (B27, N2, growth factors) [7] [8]
Procedure:
- Obtain endometrial biopsies from consenting participants at specific cycle phases (confirmed by LH surge dating or histology).
- Immediately place tissue samples in cold transport medium and process within 2 hours.
- Mechanically mince tissue followed by enzymatic digestion at 37°C for 60-90 minutes.
- Filter through 100μm strainers to isolate epithelial glands from stromal components.
- Embed digested tissue in Matrigel droplets and overlay with organoid culture medium.
- Culture organoids for 7-14 days, monitoring structural development and hormonal responses [8].
- Analyze organoid morphology, hormone receptor expression, and response to hormonal manipulations.
Validation Metrics:
- Epithelial-to-stromal ratio quantification across cycle phases
- Hormone receptor expression patterns (ER-α, PR)
- Response to estradiol and progesterone exposure
- Secretory product analysis (glycodelin, MMPs) [9] [8]
Hormonal Manipulation and Menstruation Induction Protocol
Purpose: To experimentally validate model predictions regarding hormonal control of menstrual shedding using murine models.
Materials Required:
- Transgenic mouse models with chemogenetic actuators
- Clozapine-N-oxide (CNO) or other chemogenetic ligands
- Hormone pellets (estradiol, progesterone)
- Tissue fixation and processing reagents
- Single-cell RNA sequencing reagents [6]
Procedure:
- Implement hormonal priming in transgenic mice using estradiol and progesterone pellets over 21 days.
- Induce progesterone withdrawal through pellet removal to simulate luteal regression.
- Activate premenstrual differentiation pathways using chemogenetic tools (CNO administration).
- Monitor tissue responses through timed tissue collection at 0, 6, 12, 24, and 48 hours post-induction.
- Process tissues for histology, immunohistochemistry, and single-cell spatial transcriptomics.
- Quantify extent of shedding, immune cell infiltration, and vascular changes.
- Compare transcriptional profiles to human endometrial data to validate model relevance [6].
Validation Metrics:
- Percentage of endometrial area shed
- Spatial patterns of fibroblast differentiation
- Immune cell recruitment dynamics
- Vascular permeability and breakdown
- Correlation with human menstrual transcriptomes
Applications in Reproductive Medicine and Drug Development
Modeling Endometrial Responses to Pharmaceutical Interventions
Phenomenological models provide valuable platforms for simulating endometrial responses to therapeutic agents, including hormonal contraceptives, selective receptor modulators, and novel targeted therapies. By incorporating drug-specific parameters (receptor binding affinity, pharmacokinetic profiles, dose-response relationships), these models can predict:
- Endometrial thickness changes during treatment cycles
- Breakthrough bleeding incidence and patterns
- Impact on menstrual cycle regularity
- Tissue-specific versus systemic effects [2] [10]
For endocrine disorders such as polycystic ovary syndrome (PCOS) and endometriosis, customized model variants can incorporate pathological features including androgen sensitivity, inflammatory signaling, and progesterone resistance. This allows in silico testing of treatment strategies before clinical implementation [11] [10].
Integration with Advanced Experimental Systems
The combination of phenomenological modeling with emerging experimental platforms creates powerful synergies for basic research and translational applications:
Organoid Co-culture Systems: Endometrial organoids replicate glandular physiology and hormonal responsiveness in three-dimensional culture. When integrated with computational models, they provide quantitative data on epithelial-stromal interactions, hormone response dynamics, and pharmacological perturbations. Recent advances enable organoid derivation from various patient populations, including those with infertility, endometriosis, or endometrial cancer, facilitating personalized medicine approaches [7] [8].
Artificial Intelligence-Enhanced Histology: Deep learning algorithms can automatically segment endometrial tissue compartments, quantifying epithelial and stromal areas with accuracy exceeding 92%. This high-throughput quantification provides robust data for model parameterization and validation across normal and pathological conditions [9].
Figure 1: Iterative Framework for Model Development and Validation
Table 3: Essential Research Reagents for Endometrial Dynamics Studies
| Reagent/Category | Specific Examples | Research Application | Key References |
|---|---|---|---|
| Organoid Culture Components | Matrigel, B27 supplement, N2 supplement, Noggin, R-spondin-1 | 3D modeling of endometrial gland physiology | [7] [8] |
| Growth Factors & Cytokines | FGF10, HGF, EGF, A83-01 (TGF-β inhibitor) | Maintenance and differentiation of endometrial epithelia | [7] [8] |
| Hormonal Reagents | 17β-estradiol, progesterone, RU486 (mifepristone) | Manipulation of endocrine signaling pathways | [2] [6] |
| Molecular Analysis Tools | Single-cell RNA sequencing reagents, spatial transcriptomics platforms | Characterization of cellular heterogeneity and differentiation states | [6] |
| Computational Tools | MATLAB with ode45/fde12 solvers, Python with SciPy, R with deSolve | Numerical simulation of differential equation models | [2] [12] |
Figure 2: Core Hormonal Signaling Pathways Regulating Endometrial Dynamics
Future Directions and Implementation Considerations
The continued development of phenomenological-based models for endometrial dynamics will benefit from integration with emerging technologies and computational approaches. Promising directions include:
Multi-scale Model Integration: Linking endometrial tissue-level models with cellular-level processes (receptor signaling, gene regulation) and organ-level interactions (hypothalamic-pituitary-ovarian axis) will create more comprehensive representations of reproductive physiology. Reduced-order modeling techniques can help manage complexity while maintaining predictive capability [11].
Personalized Medicine Applications: Incorporating patient-specific parameters (hormone profiles, endometrial thickness measurements, genetic variants) can generate individualized model predictions for clinical decision support in infertility treatment and menstrual disorder management.
Advanced Computational Frameworks: Fractional calculus approaches using Caputo derivatives can capture memory effects and non-local interactions in biological systems, potentially improving representation of hysteresis in hormonal responses [12]. Optimal control theory frameworks can leverage these models to design personalized treatment protocols that optimize therapeutic outcomes while minimizing side effects [12].
Figure 3: Personalized Medicine Pipeline Using Endometrial Models
For researchers implementing these approaches, we recommend beginning with established model frameworks [2] and adapting them to specific research questions through iterative refinement with experimental data. The protocols and resources outlined herein provide a foundation for generating quantitative validation datasets, while the computational tools enable simulation of endometrial dynamics under various physiological and experimental conditions.
The hypothalamic-pituitary-ovarian (HPO) axis is a central regulatory system that controls reproductive function through complex hormonal interactions. Computational modeling of this axis provides a powerful framework for integrating multi-scale biological data, from gene expression to systemic hormone dynamics, to understand both normal reproductive physiology and pathological states. Within endometrial dynamics research, these models are invaluable for investigating disorders such as endometriosis and infertility, and for simulating the effects of pharmacological interventions. The integration of transcriptomic data with mathematical modeling allows researchers to move beyond associative observations to construct mechanistic, predictive models of HPO axis function [13] [14].
Key Quantitative Data from HPO Axis Transcriptomics
Transcriptomic analyses across HPO axis tissues have revealed dynamic gene expression patterns throughout developmental stages and in response to physiological challenges. The following tables summarize key quantitative findings from recent studies.
Table 1: Differentially Expressed Genes (DEGs) in HPO Axis Tissues Across Developmental Stages [13]
| Tissue | Comparison (Weeks) | Number of DEGs | Key Biological Processes |
|---|---|---|---|
| Hypothalamus | 15w vs 20w vs 30w vs 68w | 381 | Tissue development, regulation of reproductive hormone biosynthesis |
| Pituitary | 15w vs 20w vs 30w vs 68w | 622 | Regulation of reproductive hormone secretion |
| Ovary | 15w vs 20w vs 30w vs 68w | 1,090 | Ovarian development and function |
| Ovary | 30w vs 15w | 867 | High ovulation capacity-related processes |
Table 2: Hormone and Follicle Changes in Response to Energy Availability [15]
| Parameter | Control Group | Energy-Deprived Group | Re-fed Group |
|---|---|---|---|
| Egg laying rate | Baseline | Significantly decreased | Recovered |
| Ovarian index | Baseline | Significantly decreased | Recovered |
| Small yellow follicles (SYF) | Baseline | Significantly decreased | Recovered |
| Normal hierarchical follicles (NHIE) | Baseline | Significantly decreased | Recovered |
| Estradiol (Eâ‚‚) | Baseline | Decreased | Recovered |
| Luteinizing hormone (LH) | Baseline | Decreased | Recovered |
| Follicle-stimulating hormone (FSH) | Baseline | Increased (contrasting pattern) | Returned to baseline |
Experimental Protocols
Protocol 1: HPO Axis Transcriptomic Profiling and Analysis
Purpose: To characterize gene expression patterns across hypothalamic-pituitary-ovarian tissues at different developmental stages or experimental conditions.
Materials:
- Hy-line brown laying hens (15, 20, 30, and 68 weeks of age) or equivalent model organism
- Trizol RNA extraction reagent
- Illumina Hiseq 2500 platform or equivalent sequencing system
- Primer Script RT reagent Kit for qRT-PCR validation
- Nano Photometer spectrophotometer, Qubit RNA Assay Kit, Agilent Bioanalyzer 2100 system
Procedure:
- Tissue Collection: Euthanize subjects and immediately extract hypothalamus, pituitary, and ovarian tissues (excluding follicles >2mm diameter). Flash-freeze in liquid nitrogen and store at -80°C.
- RNA Isolation: Isolate total RNA using Trizol reagent. Assess RNA quality using spectrophotometry (Qubit Fluorometer) and integrity (Agilent Bioanalyzer).
- Library Preparation and Sequencing: Prepare cDNA libraries and sequence using Illumina platform to generate 125bp paired-end reads.
- Quality Control: Process raw reads to remove adapters, poly-N sequences, and low-quality reads using Perl scripts. Calculate Q20, Q30, and GC content of clean data.
- Differential Expression Analysis: Calculate FPKMs using StringTie. Identify DEGs using edgeR package with thresholds of adjusted p < 0.05, |log fold change| ≥ 1, and FPKM > 1 in at least one group.
- Functional Annotation: Perform GO enrichment analysis using GOseq R package (p < 0.01) and KEGG pathway analysis using KOBAS software (p < 0.05).
- Network Analysis: Construct protein-protein interaction networks using STRING database (confidence score ≥ 0.7) and visualize with Cytoscape.
- Validation: Validate RNA-seq results using qRT-PCR with appropriate statistical analysis [13].
Protocol 2: Computational Modeling of HPO Axis Dynamics
Purpose: To develop mathematical models that simulate HPO axis hormone dynamics and their perturbation in pathological states or therapeutic interventions.
Materials:
- Transcriptomic datasets from HPO axis tissues
- Hormone measurement data (Eâ‚‚, Pâ‚„, LH, FSH, GnRH)
- Mathematical modeling software (MATLAB, R, Python with appropriate libraries)
- Clinical or experimental data for model validation
Procedure:
- Model Selection: Choose appropriate modeling framework based on research question:
Data Integration: Incorporate transcriptomic data on key regulatory genes (e.g., GnRHR, CGA, steroidogenic enzymes) and hormone measurements.
Model Parameterization: Estimate parameters using experimental data. For ion channel models, conduct sensitivity analysis to identify key parameters (e.g., K⺠current conductances and time constants) [16].
Model Implementation:
- Implement differential equations representing hormone synthesis, secretion, and feedback loops
- Incorporate spatial relationships (e.g., hypothalamus-pituitary-ovary communication)
- Include temporal dynamics (pulsatile secretion, menstrual cycle variations)
Model Validation: Compare model predictions with independent experimental data not used in parameter estimation.
Simulation Experiments: Use validated model to simulate:
Sensitivity Analysis: Identify key model parameters and potential intervention targets through global sensitivity analysis [16] [14].
Signaling Pathways and Experimental Workflows
HPO Axis Regulatory Network
HPO Modeling Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for HPO Axis Studies
| Reagent/Category | Function | Specific Examples |
|---|---|---|
| RNA Extraction Kits | Isolation of high-quality RNA from HPO tissues | Trizol RNA extraction reagent |
| Sequencing Platforms | Transcriptome profiling | Illumina Hiseq 2500 platform |
| qRT-PCR Reagents | Validation of RNA-seq results | Primer Script RT reagent Kit |
| Hormone Assay Kits | Quantification of reproductive hormones | Estradiol (Eâ‚‚), progesterone (Pâ‚„), LH, FSH assays |
| Cell Culture Systems | In vitro models of HPO axis components | Primary pituitary cells, ovarian granulosa cells |
| Mathematical Software | Computational modeling and simulation | MATLAB, R, Python with specialized libraries |
| Bioinformatics Tools | Analysis of transcriptomic data | edgeR, GOseq, KOBAS, STRING database |
| Visualization Tools | Network and pathway visualization | Cytoscape, Graphviz |
| Niridazole | Niridazole, CAS:61-57-4, MF:C6H6N4O3S, MW:214.20 g/mol | Chemical Reagent |
| Pongamol | Pongamol HPLC|CAS 484-33-3|Research Chemical |
Key Regulatory Genes and Ion Channels in HPO Function
Analysis of HPO axis transcriptomes has identified critical genes and signaling components that enable computational modeling of axis dynamics:
Steroidogenic Pathway Genes: PGR, HSD3B2, CYP17A1, CYP11A1, CYP21A2, STS, and CYP19A1 represent core components of steroid hormone biosynthesis identified through PPI network analysis [13].
Novel Regulatory Factors: ROCK2, TBP, GTF2H2, GTF2B, DHCR24, DHCR7, FDFT1, LSS, SQLE, MSMO1, CYP51A1, and PANK3 represent newly identified regulatory genes that expand our understanding of HPO axis control mechanisms [13].
Ion Channels in Uterine Excitability: KCNQ and hERG potassium channels contribute to the malleability of uterine action potentials, enabling the transition between plateau-like and long-lasting bursting-type APs as critical for parturition timing [16].
Energy-Responsive Genes: Energy deprivation downregulates genes related to energy and appetite-regulated neurotransmitter receptors and neuropeptides in the hypothalamus, subsequently inhibiting GnRH secretion and downstream pituitary-ovarian function [15].
Applications in Endometrial Dynamics Research
Computational models of the HPO axis provide critical insights for endometrial dynamics research, particularly in understanding and treating endometriosis. Three primary modeling approaches have been employed:
Regression and Machine Learning Models: These data-driven approaches enable non-surgical diagnosis of endometriosis by identifying associations between patient symptoms, characteristics, and medical history with disease presence, though they lack mechanistic insight [14].
Pharmacokinetic-Pharmacodynamic (PK-PD) Models: These mechanism-based models predict therapy delivery and effects on ovarian function, incorporating patient attributes, drug properties, and endogenous molecules that affect treatment response [14].
Quantitative Systems Pharmacology (QSP) Models: These comprehensive models incorporate detailed biological mechanisms, including synthesis, transport, and interactions between components throughout the HPO axis, enabling prediction of system-wide responses to hormonal therapies and other interventions [14].
The integration of HPO axis transcriptomics with these computational approaches provides a powerful framework for advancing our understanding of endometrial dynamics in both health and disease states.
Computational modeling has emerged as a powerful methodology for understanding the complex dynamics of endometrial tissues, which undergo vast changes each month during a person's reproductive years to prepare for potential pregnancy. Diseases of the endometrium, including endometriosis, adenomyosis, endometrial cancer, and Asherman syndrome, affect a significant portion of the population, yet efficient treatments remain limited due to the complexity of these conditions [1]. The endometrium consists of multiple cell types—including luminal epithelial cells, glandular epithelial cells, stromal cells, and immune cells—whose proportions and interactions change throughout the menstrual cycle in response to ovarian sex hormones [1]. This biological complexity necessitates sophisticated computational approaches that can capture spatial and temporal dynamics, cell-cell interactions, and hormonal regulation.
The field employs three primary computational frameworks—Ordinary Differential Equations (ODEs), Partial Differential Equations (PDEs), and Agent-Based Models (ABMs)—each offering distinct advantages for different research questions. ODEs model system-wide changes over time, PDEs incorporate spatial dynamics, and ABMs simulate individual cell behaviors and interactions. These approaches are not mutually exclusive; hybrid models that combine elements from multiple frameworks often provide the most comprehensive insights into endometrial function and dysfunction. As research progresses, these computational methods are increasingly integrated with experimental data from novel model systems, including endometrial organoids and microfluidic devices, creating a more robust framework for understanding endometrial diseases and developing targeted therapies [1].
Theoretical Foundations of Computational Frameworks
Ordinary Differential Equations (ODEs)
2.1.1 Fundamental Principles and Applications Ordinary Differential Equations (ODEs) are mathematical equations that describe the evolution of a system over time through functions of one independent variable and their derivatives. In the context of endometrial research, ODEs typically model population dynamics of different cell types or concentration changes of hormones and signaling molecules. These models are particularly valuable for capturing the temporal aspects of the menstrual cycle, where hormone levels (estrogen, progesterone) fluctuate in a regular pattern, driving cellular changes in the endometrial tissue [14]. The core strength of ODE modeling lies in its ability to provide a system-level perspective on dynamics that are homogeneous across space, making it ideal for understanding overall trends and equilibrium states in biological systems.
ODE models in endometrial research often take the form of compartmental models, where different biological states (e.g., proliferative, secretory, menstrual phases) are represented as distinct compartments with transition rates between them. These models can incorporate the effects of hormonal therapies by modifying transition parameters or adding terms that represent drug interactions. For instance, pharmacokinetic-pharmacodynamic (PK-PD) models use ODEs to predict how drugs are absorbed, distributed, metabolized, and excreted in the body, and how they subsequently affect endometrial tissue [14]. This approach has been valuable for optimizing hormonal therapies for endometriosis and other estrogen-associated conditions while minimizing adverse events.
2.1.2 Mathematical Formulation A typical system of ODEs for modeling endometrial dynamics might take the form:
dx/dt = f(x, t, θ)
where x represents a vector of state variables (e.g., concentrations of hormones, numbers of specific cell types), t represents time, and θ represents parameters that govern the system dynamics (e.g., rate constants, production rates, degradation rates). For example, a simple model of estrogen (E) and progesterone (P) interactions might be represented as:
dE/dt = αE - βE · E - γEP · E · P dP/dt = αP - βP · P - γPE · P · E
where α terms represent production rates, β terms represent degradation rates, and γ terms represent interaction coefficients between the hormones.
Partial Differential Equations (PDEs)
2.2.1 Spatial Dynamics in Endometrial Modeling Partial Differential Equations (PDEs) extend the concept of ODEs by incorporating spatial dimensions, making them particularly valuable for modeling how endometrial properties vary not only over time but also across physical space. While ODEs assume well-mixed, homogeneous systems, PDEs can capture heterogeneities in cell distribution, nutrient gradients, and hormone diffusion that are characteristic of real endometrial tissue [17]. This spatial component is crucial for understanding phenomena such as the formation of endometrial lesions in endometriosis, the invasion of endometrial tissue into the myometrium in adenomyosis, and the spatial progression of endometrial cancer.
PDE models of endometrial dynamics typically involve reaction-diffusion equations, where "reaction" terms represent local interactions and transformations (similar to ODE terms), while "diffusion" terms represent the spatial movement or spreading of substances or cells. For instance, a PDE might model how inflammatory cytokines diffuse through endometrial tissue, creating spatial gradients that influence immune cell recruitment and activation. Similarly, PDEs can capture the spatial dynamics of angiogenesis—the formation of new blood vessels—which is critical for both normal endometrial regeneration and pathological processes in endometrial diseases [18].
2.2.2 Mathematical Framework A general reaction-diffusion equation for modeling spatial dynamics in the endometrium might take the form:
∂u/∂t = D · ∇²u + f(u, x, t)
where u(x,t) represents the concentration of a substance or density of cells at position x and time t, D is the diffusion coefficient, ∇² is the Laplace operator representing diffusion, and f(u,x,t) represents local reactions or interactions. For modeling multiple interacting species (e.g., different cell types, hormones, nutrients), a system of coupled PDEs would be used:
∂ui/∂t = Di · ∇²ui + fi(u1, u2, ..., u_n, x, t)
where i = 1,...,n for n different species.
Agent-Based Models (ABMs)
2.3.1 Individual-Based Modeling of Cellular Behavior Agent-Based Models (ABMs) represent a fundamentally different approach from equation-based models, focusing on the behaviors and interactions of individual entities (agents) rather than population-level averages. In the context of endometrial research, agents typically represent individual cells (epithelial cells, stromal cells, immune cells) or cellular components that collectively give rise to tissue-level phenomena [19]. Each agent follows a set of rules that dictate its behavior, such as proliferation, differentiation, migration, or death, often in response to local environmental cues or interactions with neighboring agents. This "bottom-up" approach is particularly powerful for capturing emergent phenomena—system-level behaviors that arise from numerous local interactions but cannot be easily predicted from individual agent rules alone.
ABMs are exceptionally well-suited for modeling the heterogeneity inherent in endometrial systems, where individual cells may have different genetic profiles, receptor expressions, or behavioral tendencies. For example, in endometriosis, ABMs can simulate how individual endometrial cells with varying capacities for invasion and survival might establish lesions in ectopic locations [1]. Similarly, ABMs can capture the complex feedback between different cell types in the endometrial microenvironment, such as the paracrine signaling between epithelial and stromal cells that is crucial for normal endometrial function and often disrupted in disease states.
2.3.2 Formal Agent-Based Modeling Structure A typical ABM for endometrial dynamics can be formally described by:
ABM = (A, E, R, S)
where:
- A = {a1, a2, ..., a_n} represents the set of agents (cells)
- E represents the environment (tissue structure, chemical gradients)
- R = {r1, r2, ..., r_m} represents the behavioral rules for agents
- S represents the scheduling scheme for agent activation
Each agent ai has a state si that might include its cell type, position, age, receptor expression, and other relevant attributes. The behavioral rules R determine how agents update their states based on their current state, the states of neighboring agents, and environmental conditions. For example, a simple rule for an endometrial stromal cell might be:
IF (estrogenlevel > threshold) AND (spaceavailable) THEN probabilityofdivision = 0.1 END IF
Comparative Analysis of Computational Frameworks
Table 1: Comparative Characteristics of ODE, PDE, and ABM Frameworks
| Characteristic | ODE Models | PDE Models | Agent-Based Models |
|---|---|---|---|
| Representation Scale | Population-level, homogeneous | Population-level, spatially continuous | Individual-level, discrete |
| Spatial Resolution | None (well-mixed assumption) | Continuous space | Discrete space (lattice or continuous) |
| Mathematical Foundation | Systems of differential equations | Partial differential equations | Rule-based computational algorithms |
| Computational Demand | Generally low | Moderate to high | High to very high |
| Handling of Heterogeneity | Limited (requires population subdivisions) | Through continuous spatial variation | Natural handling of individual variation |
| Emergent Behavior Capture | Limited | Moderate through pattern formation | Strong (key feature of methodology) |
| Typical Applications in Endometrial Research | Hormone dynamics, pharmacokinetics | Tumor shape, invasion patterns, gradient formation | Cell-cell interactions, lesion formation, tissue organization |
| Data Requirements | Aggregate time-series data | Spatiotemporal data | Individual behavior and interaction data |
| Implementation Complexity | Low to moderate | Moderate to high | High (programming intensive) |
| Analytical Tractability | High (analytical solutions sometimes possible) | Moderate (analytical solutions rare) | Low (primarily computational) |
Table 2: Applications of Computational Frameworks to Specific Endometrial Diseases
| Endometrial Disease | ODE Applications | PDE Applications | ABM Applications |
|---|---|---|---|
| Endometriosis | Hormone therapy response, inflammatory cytokine dynamics | Spatial spread of lesions, diffusion of inflammatory mediators | Cell migration and adhesion in ectopic sites, immune cell interactions |
| Adenomyosis | Hormonal regulation of invasion | Pattern of myometrial invasion | Epithelial-stromal interactions in invasion process |
| Endometrial Cancer | Tumor growth kinetics, drug pharmacodynamics | Tumor shape evolution, angiogenesis patterns | Heterogeneous cell populations, clonal evolution, drug resistance emergence |
| Asherman Syndrome | Regeneration dynamics post-injury | Spatial pattern of fibrosis | Stem cell recruitment and differentiation during repair |
The choice between ODE, PDE, and ABM frameworks depends heavily on the specific research question, available data, and computational resources. ODE models offer mathematical elegance and computational efficiency for system-level questions where spatial heterogeneity can be reasonably neglected. They are particularly valuable for modeling hormonal regulation throughout the menstrual cycle and predicting patient responses to hormonal therapies [14]. The formalized nature of ODEs makes them amenable to mathematical analysis techniques such as stability analysis and bifurcation theory, which can provide deep insights into system dynamics.
PDE models bridge the gap between ODEs and ABMs by incorporating spatial dynamics while maintaining a continuous mathematical framework. They are ideal for investigating phenomena where spatial patterns and gradients play crucial roles, such as the formation of endometrial tissue boundaries, the invasion of endometrial cells into adjacent tissues, and the spatial distribution of drug delivery [17]. However, PDEs become computationally challenging for complex geometries and multiple interacting species, often requiring sophisticated numerical methods for solution.
ABMs excel at capturing the heterogeneity, adaptive behaviors, and emergent phenomena that characterize complex biological systems like the endometrium. Their strength lies in representing individual cells with distinct properties and behaviors, allowing for natural modeling of cellular decision-making processes, cell-cell interactions, and the evolution of population heterogeneity [19] [20]. This makes ABMs particularly valuable for studying the initiation and progression of endometrial diseases, where the interactions between different cell types and microenvironments drive pathological processes. The primary limitations of ABMs are their computational demands—especially for large numbers of agents—and the challenge of deriving general analytical insights from computational simulations.
Integrated Protocols for Endometrial Research
Protocol 1: Developing an ODE Model for Menstrual Cycle Regulation
Objective: To create a quantitative ODE model that captures the hormonal interactions regulating the menstrual cycle and predict how perturbations in these interactions contribute to endometrial diseases.
Background: The menstrual cycle is governed by complex feedback interactions between hormones from the hypothalamus, pituitary, and ovaries, which in turn regulate the endometrial cycle. Dysregulation of this system underpins many endometrial disorders, making mathematical modeling a valuable tool for understanding both normal and pathological states [14].
Materials and Reagents:
- Hormone concentration data: Time-series measurements of LH, FSH, estrogen, and progesterone
- Parameter estimation software: Packages such as MONOLIX, NONMEM, or MATLAB's parameter estimation tools
- ODE solver: Computational software with numerical ODE solving capabilities (MATLAB, R, Python with SciPy)
- Validation data: Clinical outcomes or experimental data not used in model development
Procedure:
- System Definition and Schematic Development
- Identify key system components: hypothalamic (GnRH), pituitary (LH, FSH), ovarian (estrogen, progesterone), and endometrial response elements
- Develop a conceptual diagram of interactions, noting stimulatory and inhibitory relationships
- Define system boundaries and time scale (typically one complete menstrual cycle)
Mathematical Formulation
- Translate conceptual diagram into a system of ODEs
- For each hormone, create a differential equation with production and clearance terms
- Incorporate feedback interactions using Hill functions or other nonlinear terms
- Example equation for estrogen dynamics: dE/dt = kLH·LH·(1 - E/KE) - δE·E - kP·P·E
Parameter Estimation
- Compile experimental data for hormone levels throughout the cycle
- Use maximum likelihood estimation or Bayesian methods to estimate unknown parameters
- Perform identifiability analysis to determine which parameters can be reliably estimated from available data
Model Validation
- Compare model predictions to clinical observations not used in parameter estimation
- Test model's ability to predict responses to interventions (e.g., hormone administration)
- Assess qualitative behaviors (e.g., emergence of periodic oscillations)
Experimental Applications
- Simulate hormonal perturbations corresponding to specific endometrial diseases
- Predict outcomes of therapeutic interventions
- Identify potential therapeutic targets through sensitivity analysis
Troubleshooting Tips:
- If model fails to exhibit cyclical behavior, review feedback loop structure and parameter ranges
- If parameter estimates have high uncertainty, consider structural identifiability analysis and additional data requirements
- If model validation fails, reassess model structure rather than just adjusting parameters
Protocol 2: Implementing an ABM for Endometriosis Lesion Development
Objective: To develop an agent-based model that simulates the establishment and growth of endometrial lesions in ectopic locations, capturing key cellular behaviors and interactions.
Background: Endometriosis involves the growth of endometrial-like tissue outside the uterus, with complex interactions between endometrial cells, immune cells, and the local microenvironment. ABMs are ideal for capturing the heterogeneity and spatial organization of these processes [1].
Materials and Reagents:
- Cellular behavior data: Measurements of endometrial cell migration, adhesion, proliferation, and apoptosis rates
- Interaction data: Information on paracrine signaling between endometrial, immune, and stromal cells
- ABM platform: Specialized software such as NetLogo, Repast, or custom code in Python/Java
- Visualization tools: Capabilities for visualizing agent distributions and behaviors over time
Procedure:
- Agent Definition and Classification
- Define agent types: endometrial epithelial cells, stromal cells, immune cells (macrophages, T-cells)
- Specify agent attributes: position, cell type, state (migratory/proliferative/apoptotic), receptor expression, secretion profiles
- Establish initial conditions: number and distribution of each agent type
Rule Specification
- Develop behavioral rules for each agent type based on experimental evidence
- Example rule for endometrial cell migration: IF (chemokinegradient > threshold) AND (notincontactwithstromalcells) THEN movetowardhigher_concentration END IF
- Implement rules for cell division, death, and differentiation
- Define rules for secretion of and response to signaling molecules
Environment Setup
- Create spatial environment representing peritoneal cavity or other ectopic site
- Initialize chemical fields for relevant signaling molecules (cytokines, growth factors)
- Set up boundary conditions and spatial constraints
Model Execution and Data Collection
- Implement scheduling algorithm for agent activation (synchronous vs. asynchronous)
- Run simulations for sufficient time to observe lesion development
- Collect quantitative data on lesion size, cellular composition, spatial organization
Model Validation and Analysis
- Compare simulation results with histological observations of endometriosis lesions
- Perform sensitivity analysis to identify most influential parameters
- Test model predictions through targeted experiments
Troubleshooting Tips:
- If simulation results lack biological realism, review and refine agent behavioral rules
- If computational demands are excessive, consider implementing more efficient spatial data structures
- If results are overly sensitive to small parameter changes, examine parameter ranges and model stability
Protocol 3: Hybrid PDE-ABM Approach for Endometrial Cancer Invasion
Objective: To develop a hybrid model that combines PDEs for diffusive signaling molecules with ABMs for individual cancer cells, capturing both the biochemical microenvironment and cellular heterogeneity in endometrial cancer invasion.
Background: Endometrial cancer progression involves both the dynamics of individual cancer cells with heterogeneous properties and the spatial distribution of signaling molecules in the tumor microenvironment. A hybrid approach leverages the strengths of both modeling paradigms to capture these multi-scale processes [18].
Materials and Reagents:
- Cellular imaging data: Time-lapse microscopy of cancer cell migration and proliferation
- Biochemical assay data: Measurements of growth factor and cytokine diffusion and degradation
- Computational framework: Hybrid modeling environment such as Chaste, PhysiCell, or custom MATLAB/Python code
- High-performance computing resources: For computationally intensive multi-scale simulations
Procedure:
- Model Scope and Scale Definition
- Define the spatial domain (e.g., tissue section with tumor-normal boundary)
- Specify time scale relevant to invasion process (days to weeks)
- Identify key processes to model at each scale:
- Cellular scale: division, migration, death
- Molecular scale: growth factor diffusion, degradation, cellular uptake
PDE Component Implementation
- Formulate reaction-diffusion equations for key signaling molecules (e.g., EGF, TGF-β)
- Implement numerical solver for PDEs (finite difference or finite element method)
- Set initial conditions and boundary conditions for chemical fields
ABM Component Implementation
- Define cancer cell agents with attributes: position, cell cycle status, receptor expression
- Implement behavioral rules that depend on local chemical concentrations
- Example: probabilityofdivision = f([GF], oxygen_tension)
Coupling Methodology
- Establish how ABM agents influence PDE fields (e.g., cells consume nutrients, produce signals)
- Implement how PDE solutions influence agent behaviors (e.g., chemotaxis along gradients)
- Ensure temporal synchronization between ABM and PDE components
Simulation, Analysis, and Experimental Integration
- Execute coupled simulations with appropriate numerical parameters
- Quantify invasion metrics: invasion depth, tumor shape, spatial heterogeneity
- Compare predictions with experimental models of endometrial cancer invasion
- Use model to test hypothetical treatment strategies targeting specific pathways
Troubleshooting Tips:
- If numerical instabilities occur, check time step sizes and spatial discretization
- If coupling between scales produces unrealistic behaviors, verify consistency of units and parameter magnitudes
- If computational demands limit exploration, consider simplifying less critical model aspects while preserving core dynamics
Essential Research Reagents and Computational Tools
Table 3: Key Research Reagents and Computational Tools for Endometrial Modeling
| Category | Specific Reagent/Tool | Function/Application | Example Use in Endometrial Research |
|---|---|---|---|
| Biological Models | Endometrial organoids | 3D in vitro culture systems that mimic endometrial architecture and function | Studying gland formation, hormone response, disease modeling [1] |
| Primary endometrial cells | Epithelial and stromal cells isolated from endometrial tissue | Investigating cell-type-specific behaviors in controlled environments | |
| Microfluidic systems | Devices for culturing cells under controlled fluid flow and mechanical stimuli | Modeling menstrual shedding, embryo implantation, drug transport [1] | |
| Computational Frameworks | AgentTorch | Framework for large-scale agent-based modeling | Creating population-scale simulations of endometrial disease spread [21] |
| Universal Differential Equations (UDEs) | Hybrid framework combining mechanistic models with machine learning | Enhancing traditional models with data-driven components for improved prediction [22] | |
| MATLAB, Python with SciPy | General-purpose platforms for numerical computation and ODE/PDE solving | Implementing custom models of endometrial dynamics | |
| Data Sources | Clinical hormone measurements | Time-series data on hormone levels throughout menstrual cycle | Parameterizing and validating ODE models of menstrual cycle regulation [14] |
| Histopathological images | Spatial data on tissue architecture and cellular distribution | Parameterizing and validating spatial models (PDEs, ABMs) | |
| 'Omics datasets | Transcriptomic, proteomic, and genomic data from endometrial samples | Informing model structure and parameter ranges based on molecular profiles |
Visualizing Computational Framework Integration
Computational Framework Integration
The diagram illustrates how different computational frameworks integrate to model endometrial biological systems. ODE, PDE, and ABM approaches each capture distinct aspects of endometrial dynamics, which can be combined in hybrid models to generate predictions and insights. These model outputs then undergo experimental validation, which in turn refines our understanding of the biological system and improves the computational models.
Framework Selection Workflow
This workflow diagram guides researchers in selecting appropriate computational frameworks based on their specific research questions. Temporal dynamics questions typically suit ODE approaches, spatial pattern questions align with PDE frameworks, cellular heterogeneity questions benefit from ABM approaches, and multi-scale questions often require hybrid methodologies. Example applications illustrate how each framework addresses specific endometrial research challenges.
The field of computational modeling in endometrial research is rapidly evolving, with several emerging trends likely to shape future investigations. Universal Differential Equations (UDEs) represent a promising framework that combines mechanistic models with machine learning, offering a balance between interpretability and predictive power [22]. This approach is particularly valuable for leveraging the growing availability of large-scale endometrial datasets while maintaining connection to biological mechanisms. Similarly, multi-scale modeling approaches that integrate molecular, cellular, tissue, and organism-level processes will provide more comprehensive understanding of endometrial diseases across biological scales.
The integration of high-resolution experimental data with computational models is another critical direction. Advanced imaging techniques, single-cell omics technologies, and detailed temporal monitoring of endometrial responses are generating rich datasets that can inform and validate increasingly sophisticated models. For instance, organoid technology and microfluidic systems provide unprecedented opportunities for generating quantitative data on endometrial cell behaviors under controlled conditions [1]. These experimental advances enable the development of more biologically grounded computational models that can make accurate predictions about endometrial function and therapeutic responses.
In conclusion, ODE, PDE, and ABM frameworks each offer distinct strengths for investigating different aspects of endometrial dynamics. ODEs provide efficient modeling of temporal processes like hormonal regulation, PDEs capture essential spatial dynamics of tissue organization and invasion, and ABMs excel at representing cellular heterogeneity and emergent behaviors. The integration of these approaches into hybrid models, combined with high-quality experimental data and emerging computational techniques, promises to advance our understanding of endometrial biology and accelerate the development of improved diagnostics and therapies for endometrial diseases. As these computational approaches become more accessible and widely adopted, they will play an increasingly central role in endometrial research, ultimately contributing to better health outcomes for people affected by endometrial conditions.
The human endometrium represents a paradigm of dynamic tissue remodeling, undergoing approximately 400-500 cycles of growth, differentiation, and shedding throughout a woman's reproductive life [23]. This remarkable regenerative capacity, driven by estrogen and progesterone fluctuations, necessitates sophisticated research approaches that bridge molecular mechanisms with tissue-level phenomena. Computational modeling integrated with advanced experimental systems now enables researchers to decode the complex hormonal signaling, cellular hierarchy, and spatial relationships that govern endometrial function in both physiological and pathological contexts [23] [24].
The endometrial regenerative program is orchestrated by tissue-resident stem/progenitor cells, primarily located within the basalis layer [23]. These cells demonstrate self-renewal and multilineage differentiation capabilities that sustain epithelial and stromal homeostasis after menstruation, parturition, or injury. Emerging evidence indicates that dysregulation of these endometrial stem/progenitor cells contributes to various clinical disorders including menstrual abnormalities, infertility, recurrent pregnancy loss, endometriosis, and endometrial cancer [23]. This application note outlines integrated computational and experimental protocols for investigating endometrial dynamics across biological scales, with particular emphasis on hormone-responsive mechanisms, cell-cell communication networks, and translational applications in reproductive medicine.
Computational Modeling of Endometrial Cell Population Dynamics
Theoretical Foundation and Model Specification
Computational models employing ordinary differential equations (ODEs) provide powerful tools for quantifying how endometrial epithelial and stromal cell populations respond to hormonal and cytokine stimuli. These models simulate temporal changes in cell proliferation and death rates based on specific microenvironmental conditions [24].
Protocol: ODE-Based Modeling of Hormone-Driven Cell Proliferation
- Objective: To simulate the dynamics of endometrial epithelial organoid size and stromal cell density in response to hormone and cytokine exposure.
- Model Inputs: Experimentally measured rates of epithelial organoid formation and stromal cell proliferation across multiple hormone/cytokine conditions.
- Model Calibration: Parameter estimation using previously published experimental datasets from 3D co-culture platforms containing primary human endometrial epithelial organoids and endometrial stromal cells.
- Implementation:
- Formulate ODEs describing population changes for each cell type
- Incorporate terms for hormone- and cytokine-dependent proliferation
- Include cell death/apoptosis terms influenced by microenvironmental factors
- Calibrate using experimental data from mono- and co-culture systems
- Validation: Compare simulated cell densities with experimental measurements across different donor samples and culture conditions.
Table 1: Key Parameters for Endometrial Cell Population Modeling
| Parameter | Description | Units | Estimation Method |
|---|---|---|---|
| Ïmax | Maximum proliferation rate | dayâ»Â¹ | Curve fitting to experimental data |
| KH | Hormone concentration for half-maximal effect | nM | Dose-response experiments |
| δ | Basal cell death rate | dayâ»Â¹ | Time-course measurements |
| αi,j | Cell-cell interaction coefficient | - | Co-culture vs mono-culture comparison |
| D | Molecular diffusion coefficient | μm²/s | Fluorescence recovery after photobleaching (FRAP) |
Spatial Modeling of Molecular Diffusion
Beyond population-level dynamics, partial differential equation (PDE)-based models simulate the spatial distribution and diffusion of signaling molecules within 3D endometrial cultures, accounting for cellular uptake and degradation processes.
Protocol: PDE-Based Diffusion Modeling
- Objective: To simulate molecular gradient formation and spatial heterogeneity in 3D endometrial culture systems.
- Model Inputs: Cell density predictions from ODE models; physical dimensions of 3D culture system; molecular properties of cytokines/hormones.
- Implementation:
- Formulate diffusion equations with uptake terms proportional to local cell density
- Set boundary conditions reflecting culture system geometry
- Solve numerically using finite element methods
- Application: Identify culture conditions where molecular gradients may create heterogeneous microenvironments affecting experimental outcomes.
Computational modeling workflow integrating cell population and spatial diffusion models.
Experimental Systems for Model Validation
3D Endometrial Organoid Culture and Analysis
Three-dimensional organoid cultures replicate endometrial architecture and function more accurately than traditional 2D systems, providing essential experimental platforms for validating computational predictions [23] [7].
Protocol: Establishment of Endometrial Cancer Organoids in Peptide Hydrogels
- Objective: To generate patient-derived endometrial cancer organoids that retain key tumor characteristics for drug screening and disease modeling.
- Materials:
- RFC self-assembling peptide (Ac-Arg-Leu-Asp-Ile-Lys-Val-Glu-Phe-Cys-Arg-Leu-Asp-Ile-Lys-Val-Glu-Phe-Cys-CONHâ‚‚) at 10 mg/mL stock concentration
- Advanced DMEM/F12 culture medium
- Growth factor supplements (B27, N2, EGF, FGF10, FGF2, R-spondin 1, Noggin)
- Small molecule inhibitors (A83-01, SB202190, Y-27632)
- Primary endometrial cancer tissue or cell lines
- Methods:
- Prepare RFC hydrogel by mixing 0.6 mL of 10 mg/mL RFC stock with 0.4 mL PBS to achieve 6 mg/mL final concentration
- Allow mixture to stabilize for 5 minutes at room temperature
- Embed dissociated endometrial cells in hydrogel at appropriate density
- Overlay with complete endometrial organoid culture medium
- Culture at 37°C with 5% CO₂, refreshing medium every 2-3 days
- Passage organoids every 7-14 days based on growth rate
- Validation: Confirm retention of tumor characteristics including proliferative activity, gene expression profiles, and drug resistance patterns [7].
Table 2: Research Reagent Solutions for Endometrial Organoid Culture
| Reagent Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Basal Medium | Advanced DMEM/F12 with HEPES and L-Glutamine | Nutrient support | Provides stable pH environment for 3D culture |
| Supplements | B27, N2, N-Acetylcysteine, Nicotinamide | Enhanced cell viability | Critical for stem cell maintenance |
| Growth Factors | EGF, FGF10, FGF2, R-spondin 1, Noggin | Proliferation and differentiation signaling | Concentrations must be optimized for endometrial tissue |
| Small Molecules | A83-01 (TGF-β inhibitor), SB202190 (p38 MAPK inhibitor), Y-27632 (ROCK inhibitor) | Pathway modulation | Y-27632 especially important during passaging |
| Scaffold Matrix | RFC self-assembling peptide | 3D structural support | Concentration affects mechanical properties |
Spatial Profiling of Endometrial Tumor Microenvironment
Understanding cellular spatial relationships within the endometrial tumor microenvironment enables more accurate computational model development and provides insights into disease mechanisms [25].
Protocol: Imaging Mass Cytometry for Spatial Eco-Structural Analysis
- Objective: To quantify frequency, spatial distribution, and intercellular crosstalk of immune and stromal cell populations in endometrial cancer specimens at single-cell resolution.
- Materials:
- Formalin-fixed, paraffin-embedded (FFPE) endometrial tissue sections (4 μm thickness)
- Metal-conjugated antibodies (MaxPar X8 Antibody Labelling Kit)
- Antibody panel targeting: lymphocytes (CD3, CD4, CD8, CD45, CD20), epithelial cells (E-cadherin, pancytokeratin), myeloid cells (CD11c, CD163), endothelial cells (CD31), stromal cells, cytokines, and immune checkpoints
- Imaging mass cytometry system (Fluidigm Hyperion)
- Methods:
- Section FFPE tissues using precision microtome (HistoCore MULTICUT system)
- Perform antigen retrieval with sodium citrate buffer (100°C, 30 minutes)
- Block with SuperBlock (30 minutes, room temperature)
- Incubate with metal-conjugated antibody cocktail overnight at 4°C
- Label nuclei with Intercalator-Ir
- Acquire data using imaging mass cytometry
- Process images using TissueNet algorithm for cell segmentation
- Analyze data with Rphenograph for cell clustering and spatial relationship mapping
- Key Applications: Identification of CD90+CD105+ endothelial cells as key regulators of macrophage polarization and T-cell infiltration dynamics in endometrial cancer [25].
Imaging Mass Cytometry workflow for spatial analysis of endometrial tumor microenvironment.
Integrated Workflow: From Single Cells to Tissue-Level Predictions
The true power of computational modeling emerges when combined with sophisticated experimental systems that validate and refine model predictions across biological scales.
Protocol: Multi-Scale Integration for Drug Response Prediction
- Objective: To predict patient-specific responses to endometrial cancer therapeutics using integrated computational and organoid screening approaches.
- Workflow:
- Establish patient-derived organoids in RFC hydrogels as described in Section 3.1
- Treat organoids with therapeutic agents (e.g., carboplatin, doxorubicin)
- Quantify dose-response relationships and resistance patterns
- Incorporate response data into computational models of cell proliferation and death
- Calibrate model parameters to reflect patient-specific drug sensitivity
- Generate predictions for alternative treatment regimens or drug combinations
- Validation: Compare model predictions with experimental outcomes for untested conditions; refine models based on discrepancies.
Table 3: Quantitative Drug Response Profiling in Endometrial Cancer Organoids
| Therapeutic Agent | Mechanism of Action | Reported Efficacy in Organoids | Key Resistance Observations |
|---|---|---|---|
| Carboplatin | DNA cross-linking | Variable response across patients | Retention of high proliferative activity in resistant organoids [7] |
| Doxorubicin | Topoisomerase inhibition and DNA intercalation | Strongest efficacy among tested therapeutics; significant reduction in organoid viability [7] | - |
| Targeted Therapies | Pathway-specific inhibition | Dependent on molecular subtype | Association with specific genetic alterations |
The integration of computational modeling with advanced experimental systems creates a powerful framework for bridging cellular processes to tissue-level phenomena in endometrial biology. The protocols outlined herein enable researchers to quantify hormonal response dynamics, map spatial relationships within the tumor microenvironment, and predict therapeutic efficacy with greater accuracy. As these approaches continue to evolve, they will undoubtedly accelerate the development of personalized treatment strategies for endometrial disorders and enhance our fundamental understanding of endometrial tissue dynamics across biological scales.
Future methodological developments will likely focus on incorporating multi-omics data into predictive models, establishing more complex multi-cellular systems that better recapitulate tissue-level organization, and creating closed-loop experimental-computational platforms that continuously refine model parameters based on experimental outcomes. These advances will further strengthen the bridge between molecular mechanisms and clinical manifestations in endometrial research.
From Code to Clinic: Methodological Approaches and Their Applications
Application Note: Machine Learning for Endometriosis Screening
Background and Rationale
Endometriosis—a systemic and chronic condition characterized by endometrial-like tissue outside the uterus—affects approximately 190 million women worldwide yet faces significant diagnostic delays. The current diagnostic gold standard, laparoscopic surgery, is invasive, costly, and carries surgical risks. This application note details a machine learning approach for non-invasive endometriosis screening using patient-reported symptoms and clinical data, representing a paradigm shift in clinical practice that could reduce diagnostic delays and empower patients [26].
Quantitative Performance Metrics
Table 1: Performance metrics of machine learning algorithms for endometriosis diagnosis
| Algorithm | Sensitivity | Specificity | F1-Score | AUC | Validation AUC |
|---|---|---|---|---|---|
| Logistic Regression (LR) | 0.82-1.00 | 0.00-0.80 | 0.00-0.88 | 0.50-0.89 | 0.91-0.95 |
| Random Forest (RF) | 0.82-1.00 | 0.00-0.80 | 0.00-0.88 | 0.50-0.89 | 0.91-0.95 |
| Decision Tree (DT) | 0.82-1.00 | 0.00-0.80 | 0.00-0.88 | 0.50-0.89 | 0.91-0.95 |
| eXtreme Gradient Boosting (XGB) | 0.82-1.00 | 0.00-0.80 | 0.00-0.88 | 0.50-0.89 | 0.91-0.95 |
| Voting Classifier | 0.82-1.00 | 0.00-0.80 | 0.00-0.88 | 0.50-0.89 | 0.91-0.95 |
Performance metrics are reported as ranges across different validation approaches and parameter optimizations. The models demonstrated particularly strong performance in validation studies, with AUC values ranging from 0.91 to 0.95, sensitivity from 0.91 to 0.95, specificity from 0.66 to 0.92, and F1-score from 0.77 to 0.92 [26].
Key Clinical and Symptom Features
The model was trained on 16 essential clinical and patient-based symptom features identified through expert consultation and Chi-square feature selection. These features encompass demographic characteristics, symptom history patterns, and clinical indicators that collectively provide a comprehensive picture of endometriosis risk factors [26].
Protocol: MLA Implementation for Endometriosis Screening
Data Collection and Preprocessing
Patient Recruitment and Consent: Collect pseudonymized data from patients with symptoms suggestive of endometriosis. Obtain informed consent in accordance with data protection regulations (e.g., GDPR) and approval from relevant ethics committees [26].
Feature Extraction: Extract three data types—numerical, categorical, and text—covering diagnosis, symptoms, imaging findings, medical treatments, fertility history, surgical treatments, and follow-up data. The training dataset should include approximately 8,000 patient records with 500 initial features, refined to 16 key features through expert consultation and statistical selection [26].
Data Labeling: Define cases as patients with confirmed endometriosis diagnosis based on previous treatment, clinical examination confirming deep endometriosis, or sonography/MRI detecting ovarian, peritoneal, or deep endometriosis. Controls should include patients with at least one suggestive symptom but without diagnostic confirmation [26].
Model Training and Validation
Algorithm Selection: Implement multiple machine learning algorithms including Logistic Regression (LR), Decision Tree (DT), Random Forest (RF), eXtreme Gradient Boosting (XGB), and hard/soft Voting Classifier [26].
Training Protocol:
- Split data into training (80%) and validation (20%) sets
- Apply 10-fold cross-validation
- Optimize hyperparameters using grid search
- Evaluate using sensitivity, specificity, F1-score, and AUC metrics
- Perform statistical validation on independent cohorts [26]
Validation Framework: Employ external validation using prospective cohorts (e.g., ENDOmiARN study with laparoscopic confirmation). Validation cohorts should include approximately 100 patient records with surgical confirmation of diagnosis [26].
Application Note: Gradient Boosting for Endometrial Receptivity Prediction
Background and Rationale
Defective endometrial receptivity (DER) causes approximately one-third of infertility and implantation failures, frustrating patients and clinicians alike. Current assessment methods, including transvaginal ultrasound (TVUS) and endometrial receptivity array (ERA), face limitations in accuracy or practicality. This application note describes a gradient boosting machine learning approach that leverages macrophage-endometrium interaction modules to predict endometrial receptivity status with superior accuracy compared to conventional methods [27].
Performance Comparison with Existing Methods
Table 2: Performance comparison of receptivity assessment methods
| Assessment Method | AUC | Sensitivity | Specificity | Cost-Benefit Ratio |
|---|---|---|---|---|
| XGBoost Model | 0.998 (0.994-1.00) | N/A | N/A | Superior |
| Random Forest | Lower than XGBoost | N/A | N/A | Intermediate |
| Regression Model | Lower than XGBoost | N/A | N/A | Intermediate |
| Transvaginal Ultrasound | N/A | 99% | 3% | Poor |
| Endometrial Receptivity Array | N/A | N/A | N/A | Intermediate |
The XGBoost algorithm demonstrated exceptional performance with AUCs of 0.998 (95% CI 0.994-1) in the primary dataset (GSE58144) and 0.993 (95% CI 0.979-1) in the validation dataset (GSE165004), significantly outperforming both random forest and regression models. The model also showed superiority to ultrasonography (endometrial thickness measurement) with a better cost-benefit ratio in the target population [27].
Biological Basis: Macrophage-Endometrium Interactions
Altered levels of macrophage (Mϕ) infiltration critically influence embryo implantation. Three key modules—manifested as macrophage-endometrium interactions—were enriched in immunoreactivity, decidualization, and signaling functions and pathways. Hub genes within these modules exerted significant reproductive prognostic effects, providing the biological foundation for the model's predictive capability [27].
Protocol: XGBoost Implementation for Endometrial Receptivity Assessment
Dataset Curation and Preprocessing
Data Source Selection: Utilize gene expression datasets from public repositories (e.g., GEO datasets GSE58144, GSE71835, GSE92324, GSE165004). The pooled analysis should include approximately 218 subjects (107 DER patients and 110 controls) for immune infiltration analysis [27].
Module Selection: Construct macrophage-endometrium interaction modules using weighted gene co-expression network analysis (WGCNA) in GSE58144. Identify differentially expressed genes using GSE19834 dataset, which includes telomerase-immortalized human endometrial stromal cell line (THESC) co-cultured with macrophages under four conditions: vehicle-treated control, estradiol + progesterone, control + macrophage-conditioned medium, and estradiol + progesterone + macrophage-conditioned medium [27].
Data Processing: Pre-process and normalize microarray datasets using Biobase and limma packages in R (version 3.6.2) based on raw data from the Agilent platform after conversion to log scale [27].
Model Development and Clinical Validation
Algorithm Comparison: Implement and compare three machine learning approaches: XGBoost (gradient boosting tree-structured model), random forests, and traditional regression algorithms [27].
Clinical Validation: Collect endometrial biopsy samples from eligible patients undergoing hysteroscopy. Inclusion criteria should comprise: (1) patients aged <45 years; (2) normal sex hormone levels; (3) absence of endometriosis, fibroids, pelvic inflammatory disease, or other medical comorbidities; (4) samples obtained in the mid-secretory phase. The control group (n=15) should have successful clinical pregnancies, while the DER group (n=25) should experience failed pregnancies during follow-up after procedures [27].
Validation Protocol: Compare model predictions with both surgical/clinical outcomes and existing assessment methods including endometrial thickness measurement via ultrasonography [27].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research reagents and computational tools
| Category | Item | Function/Application | Specifications/Alternatives |
|---|---|---|---|
| Data Sources | Ziwig Health Platform | Provides pseudonymized patient data for model training | 8,000 records, 500 features, patient consent managed per GDPR [26] |
| Data Sources | GEO Datasets | Gene expression data for receptivity modeling | GSE58144, GSE71835, GSE92324, GSE165004 for immune infiltration; GSE19834 for macrophage-stromal interaction [27] |
| Computational Tools | R Statistical Software | Data preprocessing and normalization | Version 3.6.2, with Biobase and limma packages for microarray analysis [27] |
| Computational Tools | XGBoost Library | Gradient boosting algorithm implementation | Handles tree-structured data, superior for genetic module-based prediction [27] |
| Computational Tools | Scikit-learn | Traditional ML algorithms | Provides LR, RF, DT, and Voting Classifier implementations [26] |
| Clinical Validation | Endometrial Biopsy Samples | Model validation against clinical outcomes | 40 samples (15 controls, 25 DER), collected in mid-secretory phase [27] |
| Analytical Methods | Weighted Gene Co-expression Network Analysis (WGCNA) | Construction of macrophage-endometrium interaction modules | Identifies co-expressed gene sets correlated with clinical traits [27] |
| Analytical Methods | Chi-Square Test | Feature selection for clinical predictors | Identifies top significant features given dependent variable [26] |
| PD-321852 | PD-321852, MF:C24H19Cl2N3O3, MW:468.3 g/mol | Chemical Reagent | Bench Chemicals |
| RM-65 | RM-65 Sheep Pox Virus Strain|Research Use Only | Research-grade RM-65 strain for ovine vaccine development. For Research Use Only. Not for human or veterinary therapeutic use. | Bench Chemicals |
Mathematical Modeling Extension: Optimal Control for Endometrial Cancer
Background and Framework
Beyond diagnostic applications, mathematical modeling provides powerful tools for understanding endometrial dynamics and treatment optimization. Recent research has developed both ordinary differential equation (ODE) and fractional differential equation (FDE) models to investigate endometrial cancer progression and treatment response under dostarlimab (immunotherapy) and chemotherapy [12].
Model Formulation and Implementation
The mathematical framework employs nonlinear ODEs and extends to FDEs with Caputo derivatives to capture memory effects. The model analyzes five key variables: tumor cells (T), activated CD8+ T-cells (A), immunosuppressive cells (C), dostarlimab concentration (D), and chemotherapeutic agent concentration (U) [12].
Numerical Implementation: Simulations are carried out in MATLAB, employing the ode45 solver for ODE systems and the fde12 solver for FDE systems. Results indicate that dostarlimab monotherapy surpasses chemotherapy alone, while combined therapy achieves the greatest reduction in cancer cells and strongest activation of CD8+ T-cells [12].
Comparative Outcomes: The ODE model provides faster tumor reduction and higher immune activation, whereas the FDE model achieves lower overall therapeutic cost by balancing tumor reduction with reduced drug usage, highlighting the potential of optimal control strategies for improving treatment outcomes in endometrial cancer management [12].
Mechanism-based pharmacokinetic-pharmacodynamic (PK-PD) and Quantitative Systems Pharmacology (QSP) modeling represent advanced computational approaches that have evolved from empirical descriptive disciplines into mechanistic sciences applicable across all drug discovery and development stages. These models incorporate specific mathematical expressions to characterize biological processes on the causal path between drug administration and observed effect, distinguishing them from traditional empirical models through their improved extrapolation and predictive capabilities [28] [29] [30].
In the context of endometrial dynamics research, these modeling frameworks offer powerful tools to understand complex uterine physiology and pathology. The endometrium undergoes dramatic monthly cycles of tissue growth, differentiation, and degeneration regulated by intricate hormonal signaling and cellular communication networks. Mechanism-based modeling enables researchers to quantitatively simulate these dynamic processes, investigate disruptions in conditions like endometriosis and polycystic ovary syndrome (PCOS), and predict how pharmacological interventions might restore normal function [14].
The fundamental principle underlying mechanism-based PK-PD modeling is the explicit separation of drug-specific properties from biological system-specific properties. This separation creates models with enhanced translational potential, as drug-specific parameters can often be scaled across species while system-specific parameters account for physiological and pathophysiological differences [29]. For endometrial research, this means models developed using preclinical data can be adapted to human physiology by incorporating human-specific parameters related to menstrual cycle dynamics, hormone receptor expression, and tissue composition.
Table 1: Key Characteristics of Modeling Approaches in Endometrial Research
| Model Type | Mechanistic Detail | Primary Applications | Endometrial Research Examples |
|---|---|---|---|
| Empirical PK-PD | Low | Descriptive exposure-response relationships | Simple hormone concentration-effect relationships |
| Mechanism-Based PK-PD | Medium | Target site distribution, receptor binding, signal transduction | Biophase distribution of hormonal therapies to endometrial tissue |
| QSP | High | System-level interactions, network biology, disease processes | Menstrual cycle modeling, endometriosis lesion development |
Foundational Concepts and Model Types
Basic Pharmacodynamic Relationships
The Hill equation, also known as the Emax model, represents a fundamental pharmacodynamic relationship where drug effects (E) are directly proportional to receptor occupancy. This model assumes plasma drug concentrations are in rapid equilibrium with the effect site and describes the concentration-effect relationship using several key parameters [28]:
Where E0 represents the baseline effect (if applicable), Emax denotes the maximum possible effect, Cp is the plasma drug concentration, and EC50 is the drug concentration producing half-maximal effect. The full sigmoid Emax model incorporates a curve-fitting parameter γ (gamma) to describe the steepness of the concentration-effect relationship [28]:
In endometrial research, these relationships can describe how hormonal therapies like progestins or GnRH agonists affect biomarkers of endometrial response. For instance, the effect of a progesterone receptor modulator on endometrial epithelial proliferation could be characterized using such models, with EC50 values reflecting drug potency and Emax values indicating maximal anti-proliferative effects.
Biophase Distribution and Hysteresis
Many drugs exhibit a temporal disconnect between plasma concentrations and pharmacological effects, a phenomenon known as hysteresis. For endometrial targets, distribution from systemic circulation to uterine tissue often represents a rate-limiting step. The "biophase" concept addresses this delay through a hypothetical effect compartment linked to the plasma compartment [28] [29].
The rate of change of drug concentrations at the biophase (Ce) is defined as:
Where keo represents the first-order rate constant for drug elimination from the effect compartment. This model successfully captures the delayed effects observed with many hormonal therapies in endometrial tissue, where clinical responses lag behind plasma drug concentrations [28].
Indirect Response Models
Many drug effects in endometrial biology occur through indirect mechanisms where the drug alters the production or elimination rate of an endogenous mediator rather than directly eliciting the response. Indirect response models capture these dynamics using differential equations that describe the turnover of response biomarkers [28].
For example, the effect of a GnRH antagonist on luteinizing hormone (LH) levels could be modeled as:
Where R represents the response (LH concentration), kin and kout are the zero-order production and first-order elimination rate constants, Imax is the maximal inhibition, C is drug concentration, and IC50 is the concentration producing half-maximal inhibition. Such models are particularly relevant for endometrial research where hormones regulate complex cellular processes through cascades of intermediate signals [28].
Table 2: Quantitative Parameters for Common Endometrial Pharmacodynamic Models
| Parameter | Symbol | Units | Typical Range | Biological Interpretation |
|---|---|---|---|---|
| Baseline Effect | E0 | Effect units | Variable | Pre-treatment endometrial thickness or histology score |
| Maximal Effect | Emax | Effect units | 0-100% | Maximum possible change in endometrial characteristic |
| Potency | EC50 | Concentration | nM-μM | Drug concentration for half-maximal effect |
| Hill Coefficient | γ | Dimensionless | 0.5-5 | Steepness of concentration-response relationship |
| Biophase Rate Constant | keo | time-1 | 0.01-1 h-1 | Rate of equilibration between plasma and endometrial tissue |
Experimental Protocols for Endometrial PK-PD Modeling
Protocol: Developing a Mechanism-Based PK-PD Model for Hormonal Therapies
Objective: To develop and qualify a mechanism-based PK-PD model for a novel progesterone receptor modulator (PRM) effect on endometrial epithelial proliferation.
Materials and Reagents:
- Test compound (PRM) and vehicle
- Ovariectomized female rats (n=8 per group) with hormonal priming
- 17β-estradiol pellets (0.1 mg, 21-day release)
- Progesterone solution for subcutaneous injection
- Ki-67 immunohistochemistry kit for proliferation markers
- LC-MS/MS equipment for drug concentration quantification
- Software for nonlinear mixed-effects modeling (e.g., NONMEM, Monolix)
Experimental Design:
- Animal Preparation: Ovariectomize 64 female Sprague-Dawley rats (200-225g) and allow 7 days recovery. implant 17β-estradiol pellets subcutaneously to establish estrogen background.
- Dosing: Randomize animals into 8 groups (n=8): vehicle control, progesterone reference (10 mg/kg), and 6 PRM dose levels (0.1, 0.3, 1, 3, 10, 30 mg/kg). Administer treatments orally once daily for 14 days.
- Sample Collection: On day 14, collect blood at 0.5, 1, 2, 4, 8, 12, and 24h post-dose for PK analysis (4 animals/timepoint). Euthanize animals 6h post-dose and collect uterine horns for PD analysis.
- Endpoint Quantification:
- Process plasma samples using protein precipitation and analyze PRM concentrations by LC-MS/MS.
- Fix uterine tissues in 10% neutral buffered formalin, embed in paraffin, section at 5μm, and perform Ki-67 immunohistochemistry.
- Quantify epithelial proliferation as percentage of Ki-67 positive nuclei in luminal and glandular epithelium (count ≥500 cells/animal).
Model Development:
- PK Model: Fit PRM concentration-time data using standard nonlinear regression techniques. A one-compartment model with first-order absorption and elimination is typically appropriate:
PD Model: Develop an indirect response model where PRM inhibits the production rate of epithelial proliferation:
Biophase Distribution: Link PK and PD components using an effect compartment:
Model Qualification: Evaluate model performance using diagnostic plots (observed vs. predicted, residuals vs. time/predictions), visual predictive checks, and precision of parameter estimates.
Expected Outcomes: A qualified mechanism-based PK-PD model that accurately predicts the time course of PRM effects on endometrial proliferation, with estimated IC50 values informing human dose projections and keo values characterizing endometrial tissue distribution.
Protocol: QSP Modeling of Menstrual Cycle Dynamics
Objective: To develop a QSP model of human menstrual cycle regulation and simulate intervention effects on endometrial dynamics.
Materials and Computational Tools:
- Literature data on hormone concentrations (GnRH, LH, FSH, estradiol, progesterone)
- Endometrial histology data across cycle phases
- Parameter estimation algorithms (e.g., maximum likelihood, Bayesian estimation)
- Ordinary differential equation solver (e.g., MATLAB, R)
- QSP platform (e.g., Certara IQ) [31]
Model Structure Development:
- Hypothalamic-Pituitary-Ovarian (HPO) Axis:
- Develop differential equations for GnRH pulsatility from hypothalamus
- Model gonadotrope responses in pituitary (LH, FSH synthesis and release)
- Simulate ovarian follicle development, steroidogenesis, and corpus luteum function
Endometrial Component:
- Incorporate estradiol and progesterone effects on endometrial proliferation and differentiation
- Include cellular composition changes (epithelial, stromal, vascular)
- Model molecular markers (receptors, growth factors, enzymes)
Intervention Modules:
- Add modules for hormonal contraceptives, GnRH modulators, or novel therapeutics
- Incorporate drug-specific PK parameters and mechanism of action
Model Calibration:
- Parameter Estimation: Use literature data from healthy menstrual cycles to estimate system-specific parameters
- Sensitivity Analysis: Identify most influential parameters using local (OAT) and global (SOBOL, Morris) methods
- Validation: Compare model predictions to independent clinical datasets not used for calibration
Simulation Experiments:
- Simulate endometriosis conditions by modifying inflammatory mediators and hormone sensitivity parameters
- Test different dosing regimens for hormonal therapies and predict effects on endometrial biomarkers
- Identify optimal intervention timing within the menstrual cycle for maximal efficacy
Expected Outcomes: A validated QSP platform for simulating menstrual cycle dynamics and pharmacological perturbations, enabling virtual trials of endometrial therapies and personalized dosing strategies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Endometrial PK-PD and QSP Modeling
| Tool Category | Specific Examples | Function in Modeling Pipeline | Application Notes |
|---|---|---|---|
| In Vivo Models | Ovariectomized rats with hormonal priming; NHP menstrual cycle models | Generate preclinical PK-PD data for model development | Rodent models offer throughput; NHP models provide translational relevance to human menstrual cycle |
| Biomarker Assays | Ki-67 IHC (proliferation); ER/PR immunohistochemistry; cytokine multiplex panels | Quantify drug effects on endometrial cellular responses | Digital pathology and AI-based segmentation improve quantification accuracy [9] |
| Analytical Systems | LC-MS/MS for drug quantification; ELISA for protein biomarkers; RNA-seq for transcriptomics | Generate concentration and response data for model input | Method validation following FDA bioanalytical guidelines ensures data quality |
| Computational Platforms | NONMEM; Monolix; MATLAB/SimBiology; Certara IQ; Phoenix Cloud | Implement, qualify, and simulate mathematical models | Cloud-based platforms enhance collaboration and computational scalability [31] |
| Data Resources | Clinical trial databases; literature compendiums; -omics datasets | Inform model structure and parameterization | Systematic literature reviews ensure comprehensive data incorporation |
Signaling Pathways and Workflow Visualization
QSP Model Development Workflow
The following diagram illustrates the iterative process for developing and qualifying QSP models of endometrial dynamics:
Endometrial Hormonal Signaling Network
This diagram depicts key signaling pathways regulating endometrial function that are incorporated into QSP models:
Biomarker Classification in Mechanism-Based Modeling
A critical advancement in mechanism-based modeling has been the development of a novel biomarker classification system that distinguishes seven types of biomarkers based on their position along the causal path between drug administration and clinical effect [30]. This framework is particularly valuable in endometrial research where multiple biomarker types can be measured.
Table 4: Biomarker Classification for Endometrial Research Applications
| Biomarker Type | Definition | Endometrial Research Examples |
|---|---|---|
| Type 0: Genotype/Phenotype | Genetic or phenotypic determinants of drug response | CYP3A5 metabolizer status affecting progestin clearance |
| Type 1: Drug Concentration | Concentration of drug or metabolite | Plasma or endometrial tissue concentrations of GnRH analogs |
| Type 2: Target Occupancy | Drug binding to molecular target | Progesterone receptor occupancy by PRMs |
| Type 3: Target Activation | Post-receptor signaling events | Phosphorylated STAT3 in endometrial stromal cells |
| Type 4: Physiological Measures | Integrated physiological responses | Uterine artery blood flow, endometrial thickness |
| Type 5: Pathophysiological Measures | Disease-specific parameters | Endometriosis lesion size, inflammatory cytokine levels |
| Type 6: Clinical Ratings | Clinical assessment scales | Menstrual pain scores, bleeding patterns |
This classification system guides model development by identifying which biomarker types to incorporate at different model levels. For example, a comprehensive QSP model of endometriosis might include Type 1 biomarkers (drug concentrations), Type 3 biomarkers (IL-6, TNF-α signaling), Type 4 biomarkers (endometrial cellular composition), and Type 6 biomarkers (pain scores) [14] [30]. The explicit representation of different biomarker types enhances model transparency and facilitates cross-species translation.
Applications in Endometrial Research and Therapeutics
Mechanism-based PK-PD and QSP modeling have demonstrated significant value across multiple applications in endometrial research, particularly for understanding endometriosis pathophysiology and optimizing treatment strategies.
Endometriosis Therapeutic Optimization
Endometriosis involves complex interactions between immune dysfunction, hormone dysregulation, and aberrant vascular development [14]. QSP models can integrate these multifaceted mechanisms to simulate disease progression and treatment response. For instance, models have been developed to predict the effects of hormonal therapies including oral contraceptives, progestins, and GnRH analogs on endometriosis lesion regression and symptom control.
These models typically incorporate:
- Hormone receptor dynamics in eutopic and ectopic endometrial tissue
- Inflammatory mediators (cytokines, chemokines, prostaglandins)
- Angiogenic factors supporting lesion vascularization
- Pain signaling pathways and their modulation
A recent application involved modeling the delivery and effects of anastrozole and levonorgestrel from an intravaginal ring for endometriosis treatment [14]. The model simulated drug release, systemic distribution, tissue penetration, and pharmacological effects on lesion regression, demonstrating how QSP approaches can inform product development and dosing regimen selection.
Menstrual Cycle Modulation
Several mechanism-based models have been developed to simulate normal menstrual cycle dynamics and predict how pharmacological interventions alter cycle characteristics [14]. These models typically incorporate the hypothalamic-pituitary-ovarian axis with feedback loops, endometrial response components, and intervention modules for hormonal therapies.
Such models have been applied to:
- Optimize dosing regimens for ovulation induction
- Predict endometrial responses to hormonal contraceptives
- Design hormone replacement protocols
- Understand cycle disruptions in polycystic ovary syndrome (PCOS)
These applications demonstrate how mechanism-based modeling moves beyond descriptive dose-response relationships to provide systems-level insights into therapeutic effects on endometrial function.
Future Directions and Implementation Considerations
The field of mechanism-based modeling continues to evolve with several emerging trends particularly relevant to endometrial research. First, there is growing integration of artificial intelligence and machine learning with traditional mechanistic modeling [31] [9]. For example, deep-learning AI models can now rapidly and accurately segment endometrial histology images to quantify epithelial and stromal composition [9], generating high-quality data for model calibration.
Second, QSP modeling is increasingly applied to novel therapeutic modalities including gene therapies, cell therapies, and targeted protein degraders [32]. As these advanced modalities enter development for endometrial disorders, mechanism-based models will be essential for predicting their pharmacokinetics and pharmacodynamics.
Third, there is movement toward more collaborative and scalable modeling infrastructure. Cloud-based platforms like Certara IQ enable research teams to work collaboratively on QSP models with version control and reproducible workflows [31]. This facilitates model sharing across institutions and accelerates community model development for endometrial disorders.
For successful implementation of these approaches in endometrial research, we recommend:
- Early engagement of modeling expertise during research program planning
- Strategic investment in quantitative biomarker assays spanning the classification hierarchy
- Development of specialized endometrial tissue sampling protocols for PK-PD studies
- Establishment of cross-disciplinary teams integrating clinical, laboratory, and computational expertise
- Adoption of fit-for-purpose modeling approaches matched to specific research questions
As these modeling approaches become more accessible and widely adopted, they promise to transform endometrial research by enabling more predictive integration of preclinical findings, optimizing clinical trial designs, and ultimately personalizing therapies for endometrial disorders.
Endometrial cancer (EC) is the most common gynecological malignancy in developed countries, with its incidence steadily increasing due to factors such as rising obesity rates, type 2 diabetes, and an aging population [33]. While early-stage diagnoses are common, prognosis for advanced or recurrent disease remains poor, with a 5-year survival rate of approximately 20% for metastatic disease [33]. Traditional therapeutic strategies have primarily relied on aggressive histological types and molecular subtypes, but these approaches often fail to account for the spatial heterogeneity of the local tumor microenvironment (TME), leading to biased predictions of treatment response [34].
The emergence of spatial ecostructural modeling represents a paradigm shift in EC research, enabling high-resolution mapping of tumor-immune-stromal interaction networks. This approach integrates single-cell spatial multiomics data to delineate the biological characteristics of local functional units based on molecular labeling, adequately reflecting spatially adaptive changes during treatment or metastasis [34]. By moving beyond bulk tissue analysis, researchers can now visualize and quantify the complex cellular ecosystems that govern cancer progression and therapeutic resistance, opening new avenues for personalized therapeutic strategies.
Molecular Classification of Endometrial Cancer: The Foundation for Spatial Analysis
The updated FIGO 2023 staging system for endometrial cancer incorporates molecular factors alongside traditional clinicopathological parameters, enabling more accurate risk stratification [33] [35]. This integration reflects the impact of genomic studies, particularly The Cancer Genome Atlas (TCGA), which has redefined the biological understanding of EC into four distinct molecular subtypes:
- POLE ultramutated: Characterized by mutations in the DNA polymerase epsilon gene, typically associated with favorable prognosis.
- Mismatch repair deficient (dMMR) or microsatellite instability-high (MSI-H): Exhibits defects in DNA mismatch repair pathways.
- p53-mutated (or serous-like): Features TP53 mutations and represents an aggressive subtype with immunosuppressive TME.
- No specific molecular profile (NSMP): Also known as copy-number low, often displays an immune-desert phenotype [33] [36].
This molecular classification provides the essential framework for spatial ecostructural modeling, as each subtype demonstrates distinct cellular compositions and spatial organizations within the TME that significantly influence clinical outcomes and treatment responses.
Table 1: Molecular Subtypes of Endometrial Cancer and Their Microenvironmental Characteristics
| Molecular Subtype | Key Genetic Features | TME Characteristics | Clinical Implications |
|---|---|---|---|
| POLE ultramutated | POLE mutations, high mutation burden | High immune infiltration, favorable anti-tumor immunity | Excellent prognosis, potential for immunotherapy |
| dMMR/MSI-H | MMR gene defects, high mutation burden | High immune cell infiltration, responsive to immunotherapy | Strong response to immune checkpoint inhibitors |
| p53-mutated | TP53 mutations, copy-number alterations | Immunosuppressive TME with Tregs, M2 macrophages | poorest survival, resistance to immunotherapy |
| NSMP | Low mutation burden, no specific drivers | Immune-desert phenotype, minimal immune infiltration | Variable outcomes, often intermediate prognosis |
Key Components of the Endometrial Cancer Microenvironment
The endometrial cancer TME is a complex ecosystem comprising malignant cells and various non-malignant components that collectively influence tumor behavior and therapeutic response. Spatial ecostructural modeling has identified several critical cellular populations that drive EC progression:
Immunomodulatory Components
- CD90+ CD105+ Endothelial Cells: Single-cell resolution analysis has identified these specialized endothelial cells as key regulators of macrophage polarization and T-cell infiltration dynamics. They constitute a critical immunomodulatory component within the TME, demonstrating significant enrichment in macrophage differentiation pathways and serving as key mediators of intercellular signaling networks [34].
- Tumor-Associated Macrophages (TAMs): Particularly in p53-mutated EC, TAMs often polarize toward an M2 phenotype, secreting immunosuppressive cytokines that promote tumor progression and correlate with poor survival outcomes [36].
- T lymphocytes: Spatial distribution of CD8+ cytotoxic T cells and CD4+ helper T cells significantly influences immune surveillance capacity. The presence of dysfunctional (CD8+PD-1+) or terminally exhausted (CD8+PD-1+TOX+) T cells predicts treatment response and progression-free survival [36].
Stromal Components
- Cancer-Associated Fibroblasts (CAFs): These cells secrete cytokines such as TGF-β and IL-6, which suppress immune responses and restrict immune cell infiltration, contributing to the immunosuppressive niche [36].
- Tumor-Associated Neutrophils: The N2 neutrophil subtype promotes tumor growth and impairs cytotoxic T cell activity, further enhancing immunosuppression within the TME [36].
Table 2: Quantitative Cellular Analysis of Endometrial Cancer Microenvironment by Molecular Subtype
| Cell Type | p53-mutated | NSMP | dMMR/MSI-H | Functional Role in TME |
|---|---|---|---|---|
| CD90+ CD105+ Endothelial Cells | Enriched [34] | Moderate | Low | Regulate macrophage polarization & T-cell infiltration |
| M2 Macrophages | High [36] | Moderate | Low | Immunosuppression, tissue remodeling |
| CD8+ PD-1+ T cells | High (dysfunctional) [36] | Low | High (functional) | Exhausted anti-tumor immunity |
| Cancer-Associated Fibroblasts | High [36] | Variable | Low | ECM remodeling, cytokine secretion |
| Regulatory T Cells (Tregs) | Elevated [36] | Low | Moderate | Immune suppression, tolerance |
Computational Framework for Spatial Ecostructural Modeling
Agent-Based Modeling (ABM) Architecture
Spatial ecostructural modeling of the endometrial cancer TME primarily utilizes agent-based models, which are computational frameworks that simulate the actions and interactions of autonomous cells within a spatial context. ABMs excel at capturing emergent behaviors that arise from individual cell-cell interactions governed by local cues [37].
The core architecture of an ABM for EC TME includes:
- Agent Definitions: Each cell type (cancer cells, immune cells, stromal cells) is represented as a distinct agent with specific behavioral rules.
- Spatial Grid: A two-dimensional or three-dimensional lattice representing the physical tissue space.
- Interaction Rules: Predetermined rules governing how different agents interact based on proximity and molecular signatures.
- Temporal Dynamics: The model progresses through discrete time steps, simulating disease progression or treatment response [38] [37].
Model Initialization with Spatial Imaging Data
A critical advancement in spatial ecostructural modeling is the initialization of computational models with patient-derived imaging data. Imaging Mass Cytometry (IMC) has emerged as a particularly powerful technology for this purpose, enabling simultaneous detection of 40+ markers at single-cell resolution while preserving spatial information [34] [38].
Figure 1: Workflow for Spatial Ecostructural Modeling in Endometrial Cancer
Experimental Protocols for Spatial Analysis of EC TME
Imaging Mass Cytometry Protocol
Objective: To quantify the frequency, spatial distribution, and intercellular crosstalk of distinct immune and stromal cell populations in endometrial cancer tissues at single-cell resolution.
Materials and Reagents:
- Fresh or frozen endometrial cancer tissue specimens
- Metal-conjugated antibodies (40+ marker panel)
- Imaging Mass Cytometry instrument (Fluidigm/Hyperion)
- Laser ablation system
- Time-of-flight mass spectrometer
- Maximum-Ionosphere software for data acquisition
Methodology:
- Tissue Preparation: Section formalin-fixed paraffin-embedded (FFPE) tissues at 4-5μm thickness and mount on specialized IMC slides.
- Antibody Staining: Incubate tissue sections with a predefined panel of metal-tagged antibodies targeting:
- Epithelial markers (pan-cytokeratin, E-cadherin)
- Immune cell markers (CD45, CD3, CD4, CD8, CD68, CD163)
- Stromal markers (CD90, CD105, α-SMA)
- Functional markers (PD-1, PD-L1, Ki-67)
- Endometrial-specific markers (ER, PR)
- Laser Ablation: Utilize UV laser to ablate predefined regions of interest at 1μm resolution.
- Mass Cytometry: Transport ablated material to inductively coupled plasma time-of-flight mass spectrometer for simultaneous metal tag detection.
- Data Processing: Convert raw data files into multidimensional images using specialized software (e.g., MCD Viewer).
- Cell Segmentation: Apply machine learning-based algorithms (CellProfiler, Ilastik) to identify individual cell boundaries and extract single-cell expression data.
- Spatial Analysis: Quantify cell-cell interactions, neighborhood compositions, and spatial distribution patterns using computational tools (histoCAT, SpatialDM).
Validation: Confirm key findings using flow cytometry on dissociated tissue samples, with particular focus on validating CD90+ CD105+ endothelial cell populations and their association with T-cell infiltration dynamics [34].
Machine Learning-Based Spatial Phenotyping Protocol
Objective: To construct molecular subtype-specific signatures and develop accurate recurrence prediction models for high-risk endometrial cancer.
Materials and Software:
- Spatial transcriptomics data (10X Genomics Visium)
- Single-cell RNA sequencing data
- Python/R programming environments
- Scikit-learn, TensorFlow, or PyTorch frameworks
- Spatial analysis packages (Squidpy, Giotto)
Methodology:
- Feature Extraction: From spatial data, extract quantitative features including:
- Cell type abundances and densities
- Neighborhood composition patterns
- Cell-cell interaction frequencies
- Spatial autocorrelation metrics
- Dimensionality Reduction: Apply uniform manifold approximation and projection (UMAP) or t-distributed stochastic neighbor embedding (t-SNE) to visualize high-dimensional spatial data.
- Classifier Training: Implement random forest or support vector machine algorithms to associate spatial patterns with molecular subtypes.
- Recurrence Model Development: Train neural networks to integrate spatial features with clinical parameters for recurrence risk stratification.
- Model Validation: Use cross-validation and independent cohort testing to evaluate predictive accuracy [34].
Research Reagent Solutions for Spatial TME Analysis
Table 3: Essential Research Reagents for Spatial Ecostructural Modeling
| Reagent Category | Specific Examples | Research Application | Function in Experimental Protocol |
|---|---|---|---|
| Metal-labeled Antibodies | CD90-¹â¶â´Dy, CD105-¹â¶âµHo, CD45-¹â´Â¹Pr | Imaging Mass Cytometry | Cell phenotype identification at single-cell resolution |
| RNA Capture Oligos | 10X Visium Spatial Barcodes | Spatial Transcriptomics | Location-specific gene expression profiling |
| Cell Segmentation Reagents | Nuclear stains (Ir-191/193 intercalator), Membrane markers | Image Analysis | Delineation of individual cell boundaries |
| Tissue Dissociation Kits | Collagenase IV, DNAse I, Trypsin-EDTA | Single-cell RNA sequencing | Tissue digestion for cell suspension preparation |
| Computational Tools | CellProfiler, Ilastik, histoCAT, Squidpy | Spatial Data Analysis | Image analysis, cell typing, and interaction mapping |
Signaling Networks in Endometrial Cancer TME
Spatial ecostructural modeling has revealed complex signaling networks within the endometrial cancer TME, with CD90+ CD105+ endothelial cells emerging as central regulators. These specialized endothelial cells demonstrate significant enrichment in macrophage differentiation pathways and serve as key mediators of intercellular crosstalk [34].
Figure 2: Key Signaling Networks in Endometrial Cancer TME
The diagram illustrates how CD90+ CD105+ endothelial cells coordinate immunosuppressive signaling through multiple pathways. These cells secrete CSF1, promoting M2 macrophage polarization, which in turn releases TGF-β that directly inhibits T-cell function. Simultaneously, VEGF signaling drives abnormal angiogenesis, creating a physical barrier to immune cell infiltration. The spatial organization of these interactions creates specialized niches within the TME that foster immune evasion and tumor progression [34] [36].
Clinical Translation and Therapeutic Implications
Predictive Modeling for Treatment Response
Spatial ecostructural models have demonstrated high predictive accuracy for both molecular subtyping and recurrence risk stratification in patients with endometrial carcinoma [34]. Computational models integrating functional molecular signatures with cell-cell interaction profiles can simulate response to various treatment modalities, including:
- Immunotherapy: Models predict that tumors with higher CD4+ T cell and, to a lesser extent, macrophage counts respond more favorably to immune checkpoint inhibitors [38].
- Combination Therapies: Agent-based models initialized with patient-specific spatial data can effectively predict response to combination treatments, with oncolytic viruses showing particular promise as drivers of treatment efficacy in certain TME contexts [38].
- Recurrence Risk: Machine learning algorithms trained on spatial features can identify patients at high risk of recurrence, enabling personalized adjuvant therapy strategies [34].
Integration with Current Treatment Guidelines
Recent clinical guidelines from the Spanish Society of Medical Oncology (SEOM) and the Polish Society of Gynecological Oncology emphasize the importance of molecular classification in treatment decisions [33] [35]. Spatial ecostructural modeling enhances this approach by adding spatial context to molecular subtyping:
- For dMMR/MSI-H tumors, which typically show high immune infiltration, immunotherapy combinations with dostarlimab or pembrolizumab plus chemotherapy represent the new standard of care [33] [35].
- For p53-mutated tumors with immunosuppressive TME, spatial models can identify resistance mechanisms and guide combination strategies to overcome immune exclusion.
- For NSMP tumors with immune-desert phenotypes, spatial analysis might identify rare immunogenic niches that could be targeted with localized therapies.
The future clinical implementation of spatial ecostructural models promises to transform endometrial cancer management through truly personalized treatment strategies based on each patient's unique tumor ecosystem.
This document provides a detailed protocol for applying deep learning (DL) models to segment epithelial and stromal compartments in endometrial histopathological images. Accurate segmentation of these regions is a critical prerequisite for advanced analytical tasks in computational modeling of endometrial dynamics, including the evaluation of tumor infiltrating lymphocytes (TILs), assessment of glandular morphology, and analysis of spatial cellular interactions. The methodologies outlined herein leverage state-of-the-art convolutional neural networks (CNNs) and vision transformers (ViTs) to achieve robust, high-fidelity segmentation, enabling researchers to quantitatively interrogate tissue microstructure and its implications in endometrial health and disease.
The endometrial lining is a highly dynamic tissue that undergoes cyclical regeneration, a process driven by complex epithelial-stromal interactions [23]. In pathological contexts, such as endometrial cancer (EC), the precise architectural relationship between the epithelial glandular structures and the surrounding stroma is a critical determinant of diagnostic grading, molecular classification, and clinical outcome [39]. Traditional histological assessment of these compartments is susceptible to inter-observer variability and is inherently qualitative [39].
AI-powered segmentation addresses these limitations by providing an objective, scalable, and quantitative framework for tissue phenotyping. This protocol describes the implementation of a hybrid deep learning framework to automate this process, facilitating reproducible analysis of the epithelial-stromal interface—a key region of interest for understanding immune cell infiltration and tumor microenvironment in endometrial cancer [40].
Quantitative Performance of Deep Learning Models in Gynecologic Pathology
Deep learning models have demonstrated exceptional performance in various image analysis tasks within gynecologic pathology. The following table summarizes the quantitative results from recent key studies, providing benchmarks for model selection and expectation management.
Table 1: Performance Metrics of Deep Learning Models in Gynecologic Pathology Applications
| Study Focus | Model Architecture(s) | Key Performance Metric(s) | Dataset(s) Used |
|---|---|---|---|
| Endometrial Cancer Grading [39] | EndoNet (CNN + Vision Transformer) | Internal Test: F1-score: 0.91, AUC: 0.95External Test (TCGA): F1-score: 0.86, AUC: 0.86 | 929 internal WSIs; 100 TCGA WSIs |
| Gastric Cancer Classification [41] | Hybrid CNN-Transformer | Accuracy: 99.2%, F1-score: 0.991, AUC: 0.996 | GasHisSDB, TCGA-STAD, NCT-CRC-HE-100K |
| Endometriosis Lesion Classification [42] | Inception V3 (with 5-fold cross-validation) | Accuracy: 0.93 | Gynecologic Laparoscopy Endometriosis Dataset (GLENDA) |
| Endometrial Cancer Diagnosis [43] | Merged DL & Clinical Model (ResNet-50, etc.) | AUC: 0.892 (External Validation) | 1,443 multimodal ultrasound images from 611 patients |
Experimental Protocols
Protocol 1: Whole Slide Image Preprocessing and Patch Extraction
This protocol outlines the critical first steps for preparing large, gigapixel Whole Slide Images (WSIs) for deep learning model training.
I. Materials and Reagents
- Whole Slide Image Scanners (e.g., Aperio AT2/CS2 from Leica Biosystems)
- High-performance computing workstation with substantial GPU memory (≥ 11 GB recommended)
- Software: Python libraries (OpenSlide, OpenCV, NumPy)
II. Methodology
- WSI Acquisition: Digitize Hematoxylin and Eosin (H&E)-stained endometrial tissue sections using a slide scanner at 40x magnification (0.25 μm/pixel) [39].
- Quality Control: Manually review WSIs to exclude those with excessive artifacts, out-of-focus regions, or folding tissue.
- Stain Normalization: Apply color normalization techniques, such as color deconvolution [44], to separate the haematoxylin and eosin channels. This minimizes staining variability across different scanners and laboratory protocols [41].
- Downscaling (Optional): For computational efficiency during initial processing, downscale WSIs from 40x to 10x magnification (1 μm/pixel) using anti-aliasing interpolation [39].
- Patch Extraction: Tile the WSI into smaller, manageable image patches (e.g., 256x256 or 512x512 pixels). This is necessary due to memory constraints when processing gigapixel images [41] [44].
- Data Augmentation: Apply real-time augmentation to the patches during model training to increase dataset diversity and reduce overfitting. Techniques include:
Protocol 2: Training a Hybrid CNN-Transformer for Segmentation
This protocol describes the procedure for training a robust segmentation model that combines local feature extraction (CNN) with global contextual understanding (Transformer).
I. Materials and Reagents
- Annotated dataset of endometrial image patches with corresponding epithelial/stromal masks.
- Software: Python deep learning frameworks (PyTorch, TensorFlow).
II. Methodology
- Model Architecture:
- CNN Backbone: Utilize a pre-trained network like ResNet-50 or EfficientNet-B0 as a feature extractor. These models excel at capturing local spatial features like edges, textures, and nuclear morphology [43] [44].
- Transformer Encoder: Feed the feature maps from the CNN into a Transformer encoder. The self-attention mechanism in the Transformer captures global contextual relationships between different regions of the patch, which is crucial for understanding tissue architecture [41] [39].
- Transfer Learning: Initialize the CNN backbone with weights pre-trained on a large natural image dataset (e.g., ImageNet). Freeze the initial layers and fine-tune the later layers on the histopathology dataset to adapt the learned features [43].
- Model Training:
- Loss Function: Use a combined loss function, such as a weighted sum of Dice Loss and Cross-Entropy Loss, to handle class imbalance between epithelial, stromal, and background pixels.
- Optimizer: Employ the Adam optimizer with a learning rate of 3e-5 and L2 regularization (weight decay of 0.01) to prevent overfitting [43].
- Validation: Implement five-fold cross-validation to ensure model generalizability and mitigate overfitting [41] [42].
Protocol 3: Spatial Analysis of the Epithelial-Stromal Interface
After segmentation, this protocol uses the results to perform advanced spatial analysis on a critical tissue compartment.
I. Materials and Reagents
- Segmented epithelial and stromal masks from Protocol 2.
- Multiplex immunofluorescence (mIF) images (if available) for immune cell phenotyping [40].
- Spatial analysis software (e.g., CytoMAP, QuPath).
II. Methodology
- Define a Three-Compartment Model: Based on the segmentation output, partition the tissue into three distinct regions: the epithelial region, the stromal region, and the epithelial-stromal interface (a defined zone, e.g., 50 μm, surrounding the epithelial boundary) [40].
- Neighborhood Clustering Analysis: Apply algorithms like supervised neighborhood clustering in CytoMAP to objectively identify and map these compartments based on cellular composition and density [40].
- Lymphocyte Quantification: Within each compartment, quantify the density of specific immune cells, such as CD8+ T cells or CD8+ TIM3+ exhausted T cells, either from H&E images or registered mIF images.
- Statistical Comparison: Perform statistical tests to compare immune cell densities and spatial distributions across the three compartments. Studies have shown that the interface region often holds the highest density of CD8+ T cells, surpassing both the epithelial and stromal regions [40].
Workflow and Signaling Visualization
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents, Tools, and Datasets for AI-Powered Histological Analysis
| Item Name | Type/Category | Primary Function in Protocol |
|---|---|---|
| Aperio AT2/CS2 Scanners [39] | Hardware | High-resolution digitization of H&E-stained glass slides to create Whole Slide Images (WSIs). |
| Hematoxylin & Eosin (H&E) Stain | Laboratory Reagent | Standard histological staining for visualizing tissue morphology, nuclei, and cytoplasm. |
| CytoMAP [40] | Software Tool | Supervised neighborhood clustering analysis for defining tissue compartments and quantifying spatial relationships. |
| The Cancer Genome Atlas (TCGA) [39] | Public Dataset | Source of WSIs for external validation of model generalizability and performance. |
| ResNet-50 / EfficientNet-B0 [43] [44] | Deep Learning Model | Pre-trained CNN backbones for efficient feature extraction from image patches. |
| Anti-CD8 / Anti-TIM3 Antibodies [40] | Laboratory Reagent (mIF) | Antibodies for multiplex immunofluorescence, enabling phenotypic identification of specific immune cell subsets (e.g., exhausted T-cells) for spatial analysis. |
In silico clinical trials (ISCTs), which use computer simulations to evaluate the safety and efficacy of medical interventions, are transforming drug development for complex gynecological diseases. For endometrial cancer (EC) and endometriosis, conditions characterized by molecular heterogeneity and therapeutic challenges, ISCTs offer a pathway to personalized medicine by integrating multi-scale data, from single-cell transcriptomics to population-level clinical outcomes. These computational approaches enable the head-to-head comparison of therapies, the identification of novel drug targets, and the optimization of treatment protocols in a cost-effective and time-efficient manner, thereby accelerating translational research from bench to bedside [45].
This document details application notes and protocols for employing ISCTs within the broader context of computational modeling of endometrial dynamics. It provides a structured framework for researchers and drug development professionals to design, implement, and validate in silico studies for EC and endometriosis, leveraging the latest advancements in quantitative systems pharmacology, network pharmacology, and machine learning.
Computational Framework for Endometrial Conditions
The foundation of a robust ISCT is a multi-scale computational framework that integrates diverse data types and mathematical approaches to model disease pathophysiology and drug effects. The core components of this framework are outlined below.
Table 1: Multi-Scale Modeling Components for Endometrial Conditions
| Modeling Scale | Core Components | Application in Endometrial Research | Key Outputs |
|---|---|---|---|
| Molecular & Cellular | Network Pharmacology, Molecular Docking, Gene Regulatory Networks | Identifies bioactive compounds (e.g., ferulic acid) and core targets (e.g., EGFR, TP53) in EC; maps signaling pathways (e.g., PI3K/AKT) [46]. | Drug-target interactions, pathway activities, signaling network maps. |
| Tissue & Microenvironment | Fractional Calculus (FDEs), Ordinary Differential Equations (ODEs) | Models tumor-immune cell interactions (CD8+ T-cells, cancer cells) in EC; simulates endometriosis lesion proliferation and inflammation [12]. | Tumor volume dynamics, immune cell activation levels, lesion size. |
| Organ & System | Physiologically Based Pharmacokinetic (PBPK) Models | Predicts drug concentration-time profiles in different physiological compartments for drugs like dostarlimab [45]. | Drug bioavailability, tissue distribution, clearance rates. |
| Population | Virtual Population (vPOP) Generation, Quantitative Systems Pharmacology (QSP) | Creates in silico cohorts of EC patients or women with endometriosis with varying molecular subtypes, demographics, and comorbidities [45]. | Simulated clinical trial outcomes, prediction of treatment responders/non-responders. |
Application Notes & Protocols
Protocol 1: Network Pharmacology for Natural Product Evaluation in Endometrial Cancer
Objective: To systematically predict the efficacy and mechanism of action of a natural product, such as Angelica sinensis (AS), in treating endometrial cancer. Background: Network pharmacology allows for the holistic identification of multi-component, multi-target therapeutic interactions, which is particularly suited for studying complex traditional Chinese medicine formulas [46].
Procedure:
- Bioactive Ingredient Screening: Compile a comprehensive list of the natural product's chemical constituents from literature and chemical databases. Filter for drug-likeness using criteria like oral bioavailability.
- Target Prediction: Input the screened ingredients into a target prediction tool (e.g., Swiss Target Prediction) to identify putative protein targets. Standardize target names to official gene symbols.
- Disease Target Collection:
- Obtain EC-related genes from public databases (e.g., GeneCards with a relevance score >10).
- Analyze high-throughput genomic datasets (e.g., from GEO, such as GSE115810) to identify differentially expressed genes in EC versus healthy endometrium.
- Network Construction and Analysis:
- Intersect the drug target genes and disease target genes to obtain potential therapeutic targets.
- Construct a Protein-Protein Interaction (PPI) network using STRINGdb and import it into Cytoscape. Identify core targets based on network topology (e.g., degree ≥ 50). Core targets in EC include EGFR, TP53, CTNNB1, CCND1, and HRAS [46].
- Build a Herb-Ingredient-Target-Disease network to visualize the complex relationships.
- Enrichment Analysis & Molecular Docking:
- Perform Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway enrichment analysis on the core targets using the DAVID database. The PI3K/AKT signaling pathway is frequently implicated [46].
- Validate the binding affinity of key bioactive ingredients (e.g., ferulic acid and caffeic acid from AS) to the core targets through molecular docking simulations.
Protocol 2: Optimal Control Therapy with Immunotherapy and Chemotherapy
Objective: To design an optimal treatment schedule for combined dostarlimab (immunotherapy) and chemotherapy in endometrial cancer using a fractional-order optimal control problem (FOCP). Background: Fractional calculus incorporates memory effects into biological systems, providing a more accurate description of tumor growth and treatment response than classical integer-order models [12].
Procedure:
- Mathematical Model Formulation: Develop a system of fractional differential equations (FDEs) using the Caputo derivative. The model should compartmentalize the following variables:
- Tumor Cells ((\overline{\mathbb{T}})): Logistic growth term, killed by immune cells and therapy.
- Activated CD8+ T-cells ((\overline{\mathbb{A}})): Activated by tumor cells and cytokine signaling, inhibited by dostarlimab blockage of PD-1/PD-L1.
- Immunosuppressive Cells ((\overline{\mathbb{C}})): Representing Tregs or MDSCs that inhibit effector T-cells.
- Dostarlimab Concentration ((\overline{\mathbb{D}})): Administered via control input (\chi{\overline{\mathbb{D}}}).
- Chemotherapy Drug Concentration ((\overline{\mathbb{U}})): Administered via control input (\chi{\overline{\mathbb{U}}}) [12].
- Establish Well-Posedness: Prove the existence and uniqueness of the solution for the FDE system using fixed-point theorems (e.g., Banach fixed-point theorem).
- Formulate the Optimal Control Problem:
- Objective Functional (J): Define a cost functional to be minimized. This typically balances tumor cell reduction with the cost of treatment (e.g., drug dosage and side effects): ( J(u{\mathbb{D}}, u{\mathbb{U}}) = \int{0}^{tf} \left[ A \overline{\mathbb{T}}(t) + B u{\mathbb{D}}^2(t) + C u{\mathbb{U}}^2(t) \right] dt ) where ( u{\mathbb{D}} ) and ( u{\mathbb{U}} ) are the control inputs for dostarlimab and chemotherapy, and A, B, C are weight coefficients.
- Apply Pontryagin's Maximum Principle: Derive the necessary conditions for optimality, resulting in a system of FDEs for the state and adjoint variables.
- Numerical Simulation:
- Implement the forward-backward sweep method with a fractional-order numerical solver (e.g.,
fde12in MATLAB). - Simulate and compare monotherapies (dostarlimab-only, chemo-only) versus combined therapy. The FOCP model is expected to show that combined therapy achieves the greatest tumor reduction, potentially at a lower overall therapeutic cost than the ODE model [12].
- Implement the forward-backward sweep method with a fractional-order numerical solver (e.g.,
Protocol 3: Systems Pharmacology Drug Repurposing for Endometriosis
Objective: To repurpose approved drugs or nutraceuticals for endometriosis by building a systems pharmacology model of the disease. Background: This approach leverages existing knowledge to discover new therapies by analyzing the network-based relationship between disease genes and drug targets [47].
Procedure:
- Disease Network Construction:
- Compile endometriosis progression-related and infertility-related genes from OMIM, DisGeNET, and transcriptomic studies.
- Construct a protein-protein interaction (PPI) network using these genes. Statistically validate the overlap between progression and infertility subnetworks (e.g., p-value = 1.9 × 10â»Â¹Â¹) [47].
- In Silico Drug Screening:
- Create a library of approved drugs and their targets from databases like DrugBank.
- For each drug, calculate its molecular efficacy by measuring the number of endometriosis-related genes it targets, compared to a random expectation (e.g., p-value = 0.01). Prioritize drugs with superior efficacy to current treatments.
- Safety Profiling and Prioritization: Cross-reference candidate drugs with clinical side-effect databases to prioritize those with the safest profiles (e.g., zinc, copper, resveratrol) [47].
- In Vitro Validation:
- Treat endometriotic epithelial cells (e.g., 12Z cell line) with the top candidates.
- Assay for key phenotypes: cell proliferation (CCK-8 assay), migration (wound healing/transwell assay), and expression of endometriosis biomarkers (e.g., ERβ, IL-6, VEGF) via qPCR or ELISA. Effective candidates like zinc and copper should show significant suppression of these phenotypes [47].
Experimental Workflow & Visualization
The following diagram illustrates the integrated workflow for developing and validating an in silico clinical trial for endometrial pathologies, synthesizing the protocols above.
Integrated ISCT Workflow for Endometrial Research
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational and Experimental Reagents for Endometrial ISCTs
| Category | Reagent / Tool / Model | Function / Application | Example Use Case |
|---|---|---|---|
| Computational Tools & Databases | Swiss Target Prediction [46] | Predicts biological targets of small molecules. | Identifying potential protein targets for compounds like ferulic acid. |
| STRINGdb [46] | Database of known and predicted protein-protein interactions. | Constructing PPI networks for endometrial cancer core targets. | |
| GEO Database (e.g., GSE115810) [46] | Public repository of functional genomics datasets. | Identifying differentially expressed genes in endometrial cancer. | |
MATLAB with fde12/ode45 solvers [12] |
Numerical computing environment for solving ODEs and FDEs. | Implementing and simulating optimal control models for therapy. | |
| Cell Lines & Experimental Models | 12Z Endometriotic Epithelial Cell Line [47] | A widely used human cell model for endometriosis. | Validating anti-proliferative and anti-migratory effects of repurposed drugs (e.g., zinc). |
| Primary Cells from Deep Endometriosis [48] | Patient-derived cells maintaining in vivo characteristics. | Testing the effects of EGCG on lesion fibrosis and survival. | |
| Biomarkers & Assays | PD-L1 IHC Assay [49] | Immunohistochemistry to detect PD-L1 protein expression. | Stratifying EC patients for immunotherapy response. |
| MSI/MMR Testing [49] | Detects microsatellite instability/mismatch repair deficiency. | Identifying EC patients (MMRd subtype) most likely to respond to ICIs. | |
| ELISA for IL-6, VEGF [47] | Quantifies protein levels of inflammatory/angiogenic factors. | Measuring biomarker modulation in treated endometriotic cells. | |
| Key Biologics & Compounds | Dostarlimab [12] [49] | Anti-PD-1 immune checkpoint inhibitor. | Modeling and testing immunotherapy in MMRd endometrial cancer. |
| Epigallocatechin Gallate (EGCG) [48] | Green tea catechin with anti-inflammatory/anti-fibrotic properties. | Investigating a non-hormonal treatment for endometriosis. | |
| Zinc and Copper (as nutraceuticals) [47] | Essential metals with predicted anti-endometriotic activity. | Repurposing for multi-target therapy in endometriosis. |
The protocols and application notes detailed herein provide a concrete roadmap for leveraging in silico clinical trials in endometrial cancer and endometriosis research. By integrating computational modeling with targeted experimental validation, researchers can de-risk the drug development process, uncover novel therapeutic synergies, and ultimately contribute to the advancement of personalized, effective treatments for these complex gynecological conditions. The future of this field lies in the continued refinement of multi-scale models, the incorporation of real-world data, and the close collaboration between computational scientists, clinicians, and experimental biologists.
Enhancing Predictive Power: Model Calibration, Optimization, and Integration
The management of endometrial cancer (EC), the most common gynecologic malignancy in the United States with an estimated 69,120 new cases in 2025, faces significant challenges due to disease heterogeneity and therapeutic resistance [50]. Optimal control theory (OCT) provides a rigorous mathematical framework for designing personalized therapeutic regimens that systematically navigate the complex balance between treatment efficacy and toxicity [51]. By formulating cancer treatment as a dynamical system optimization problem, OCT enables the in silico evaluation of numerous dosing, timing, and drug combination strategies that would be prohibitively expensive or unethical to test in clinical trials [51]. This approach is particularly valuable for endometrial cancer, where obesity-driven activation of the PI3K/AKT pathway and frequent progesterone receptor loss create a complex therapeutic landscape requiring sophisticated intervention strategies [50].
The integration of OCT with computational models of endometrial cancer dynamics represents a paradigm shift from population-based to patient-specific treatment optimization. Where traditional clinical trials determine dosing for an "average" patient, OCT leverages patient-specific data to create individualized regimens that account for unique tumor biology, metabolic factors, and drug pharmacokinetics [51]. This application note details the theoretical frameworks, experimental protocols, and implementation strategies for applying OCT to combination therapy development in endometrial cancer, with particular emphasis on clinically relevant considerations for translational research.
Methodological Frameworks for Optimal Control
Mathematical Formulations of Optimal Control Problems
Optimal control applications in endometrial cancer therapy employ both classical ordinary differential equation (ODE) and fractional-order (FDE) frameworks to model tumor dynamics and treatment response. The Caputo fractional derivative formulation effectively captures memory effects and hereditary properties in biological systems, providing enhanced representation of non-local interactions in tumor-immune dynamics [12]. A recently developed EC model incorporates dostarlimab immunotherapy and chemotherapy through the following FDE system [12]:
For heterogeneous cell populations, a general ODE framework models multiple cell types treated with multiple interacting drugs. The dynamics of cell population vector ( x \in R^n ) under drug concentration vector ( u \in R^m ) are described by linear growth rates with spontaneous cell-type conversion and drug-mediated effects [52]. This formulation captures three key phenomena: cell proliferation and death, spontaneous cell-type conversion, and genuine pharmacodynamic drug-drug interactions affecting multiple cell populations simultaneously [52].
Network Controllability Approaches
Beyond traditional OCT, network controllability theory identifies synergistic regulator pairs as candidate targets for combination therapy. The OptiCon algorithm identifies Optimal Control Nodes (OCNs) that exert maximal control over deregulated pathways while minimizing control over unperturbed genes to reduce side effects [53]. The algorithm defines a synergy score combining mutation enrichment and functional crosstalk between OCN-regulated subnetworks, enabling de novo identification of combination targets beyond existing drug targets [53].
Table 1: Key Parameters in Endometrial Cancer Optimal Control Models
| Parameter Class | Specific Parameters | Biological Interpretation | Estimated Values |
|---|---|---|---|
| Tumor Growth | μâ‚áµ…, νâ‚áµ… | Tumor growth rate and carrying capacity | Model-dependent |
| Immune Activation | γâ‚áµ…, γ₂ᵅ | CD8+ T-cell activation and tumor killing rates | Model-dependent |
| Drug Effects | ZT, ZA, ωT, ωA | Chemotherapy maximal kill rate and steepness | Model-dependent |
| Fractional Order | α | Memory effect intensity (0<α≤1) | 0.85-0.95 [12] |
Experimental Protocols for Model Calibration and Validation
In Vitro Combination Screening Protocol
Purpose: To quantitatively measure drug interaction effects for parameterizing combination therapy models in endometrial cancer.
Materials:
- EC cell lines: ECC1, KLE, Ishikawa H, Hec50 [50]
- Drugs: CUDC-907 (dual PI3K/HDAC inhibitor), BKM120 (PI3K inhibitor), LBH589 (HDAC inhibitor), medroxyprogesterone acetate (MPA) [50]
- Assay kits: WST-1 Cell Proliferation Colorimetric Assay Kit (TaKaRa MK400), resazurin assay (Sigma #7017) [50]
Procedure:
- Cell Seeding: Plate cells at 10,000 cells per well in 96-well plates and incubate for 24 hours to reach approximately 30% confluency [50].
- Drug Treatment: Prepare serial dilutions of single agents and combinations:
- PI3K inhibitors: 0.1 nM to 1 μM
- HDAC inhibitors: 0.1 nM to 100 nM
- Progestins: 1 μM to 20 μM
- Incubation: Treat cells for 72 hours under standard culture conditions.
- Viability Assessment:
- Add WST-1 reagent and incubate for 1-4 hours
- Measure absorbance at 440 nm using a plate reader
- Alternatively, use resazurin fluorescence for synergy studies
- Synergy Analysis: Upload dose-response data to SynergyFinder (https://synergyfinder.fimm.fi) to calculate combination indices and identify synergistic ratios [50].
Data Analysis:
- Calculate ICâ‚…â‚€ values using nonlinear regression
- Determine combination indices (CI) using the Chou-Talalay method
- Fit parameters for ODE models using maximum likelihood estimation
In Vivo Validation Protocol
Purpose: To validate optimized combination regimens in preclinical models of endometrial cancer.
Materials:
- Animal model: Immunocompromised mice with endometrial cancer xenografts
- Diet conditions: High-fat diet, normal chow, and fasting cohorts to model metabolic influences [50]
- Drugs: CUDC-907 formulated in 30% Captisol according to Curis guidelines [50]
- Assessment tools: Western blot reagents, ELISA kits for IGF-1 measurement [50]
Procedure:
- Xenograft Establishment: Subcutaneously inject 5×10ⶠEC cells into flanks of female immunocompromised mice.
- Treatment Initiation: Begin dosing when tumors reach 100-150 mm³, randomize mice into treatment groups (n=8-10).
- Dosing Regimens:
- Apply OCT-optimized schedules for single and combination therapies
- Include progestin combination arms to assess resensitization
- Monitor body weight and clinical signs three times weekly
- Endpoint Measurements:
- Measure tumor dimensions 2-3 times weekly using calipers
- Collect serum for IGF-1 ELISA at sacrifice
- Harvest tumors for Western blot analysis of p-AKT, p-rS6, PR expression
Data Analysis:
- Calculate tumor growth inhibition (TGI%) for each regimen
- Compare observed efficacy to OCT predictions
- Analyze correlation between IGF-1 reduction and treatment response
Implementation and Workflow Integration
Computational Implementation Framework
Successful implementation of OCT for endometrial cancer therapy requires integration of multiple computational tools and biological data sources. The following workflow outlines the key steps from data collection to regimen optimization:
For numerical solutions of ODE systems, MATLAB's ode45 solver provides efficient integration, while the fde12 solver handles fractional-order systems [12]. Optimization algorithms include genetic algorithms and particle swarm optimization for parameter estimation and control optimization [54]. Clinical translation incorporates adaptive model predictive control to adjust regimens based on patient response data [51].
Research Reagent Solutions
Table 2: Essential Research Reagents for Endometrial Cancer Therapy Optimization
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| EC Cell Models | ECC1, Ishikawa H, KLE, Hec50 | In vitro screening | Represent molecular heterogeneity [50] |
| Targeted Inhibitors | CUDC-907, BKM120, LBH589 | Pathway targeting | Dual PI3K/HDAC inhibition; isoform selectivity [50] |
| Hormonal Agents | Medroxyprogesterone acetate | Progestin resensitization | PR agonist activity [50] |
| Immunotherapies | Dostarlimab (anti-PD-1) | Immune activation | Checkpoint blockade [12] |
| Assay Systems | WST-1, resazurin | Viability assessment | Colorimetric/fluorometric readouts [50] |
| Animal Models | Xenograft mice on high-fat diet | Metabolic context | Models obesity-driven EC [50] |
Discussion and Future Directions
The integration of optimal control theory with endometrial cancer biology represents a transformative approach for addressing therapeutic complexity. Numerical simulations comparing ODE and FDE frameworks reveal distinct advantages: while ODE models provide faster predicted tumor reduction, FDE models achieve comparable efficacy with lower overall therapeutic cost by balancing tumor reduction with reduced drug usage [12]. For clinical translation, OCT must incorporate practical considerations including drug administration routes, toxicity management, and patient-specific pharmacokinetic variations [51].
Future development should focus on multiscale models that integrate intracellular signaling networks with tissue-level tumor-immune interactions. The combination of network controllability analysis [53] with pharmacological OCT provides a powerful framework for identifying novel target combinations and optimizing their modulation. As quantitative imaging and liquid biopsy technologies advance, real-time adaptive optimal control will enable truly personalized endometrial cancer therapy that dynamically adjusts to evolving tumor biology and treatment response.
Fractional calculus (FC) has transitioned from a mathematical concept to a vital tool for modeling complex biological systems. Unlike integer-order derivatives, fractional-order derivatives, particularly the Caputo derivative, are defined by integrals that capture non-local effects and system history. This "memory effect" makes FC exceptionally suitable for modeling biological processes where the current state depends on past interactions, such as tumor growth, immune response, and drug pharmacokinetics [12] [55]. In the context of endometrial dynamics, this capability allows researchers to create more accurate representations of disease progression and therapeutic interventions than traditional models permit.
The application of FC provides significant advantages for modeling endometrial cancer treatment. It enables the capture of hereditary properties and long-range temporal dependencies inherent in biological systems, often lost in conventional ordinary differential equation (ODE) approaches. Recent research has demonstrated that fractional-order models (FDEs) can achieve comparable therapeutic efficacy to ODE models while potentially reducing overall drug usage and associated toxicity, offering a more balanced approach to treatment optimization [12].
Mathematical Framework for Endometrial Cancer Treatment
Fractional-Order Model Formulation
A fractional-order mathematical model for endometrial cancer treatment incorporating dostarlimab immunotherapy and chemotherapy has been developed using the Caputo derivative operator. The model consists of a system of nonlinear fractional differential equations that capture the dynamics between tumor cells, activated CD8+ T-cells, circulating lymphocytes, dostarlimab concentration, and chemotherapy drug levels [12].
The system is defined by the following equations:
[ \begin{cases} {}^{C}{\mathscr{D}}{0+}^{\alpha} \overline{\mathbb{T}} (\hat{\theta}) = \mu1^{\alpha} \overline{\mathbb{T}} (\hat{\theta})(1-\nu1^{\alpha} \overline{\mathbb{T}} (\hat{\theta})) - \gamma1^{\alpha} \overline{\mathbb{T}} (\hat{\theta}) \overline{\mathbb{A}}(\hat{\theta}) - \delta^{\alpha} \overline{\mathbb{T}}(\hat{\theta}) + \epsilon1^{\alpha} \overline{\mathbb{A}}(\hat{\theta}) - \mathbb{Z}{\overline{\mathbb{T}}} \left( 1 - e^{-\omega{\overline{\mathbb{T}}}\overline{\mathbb{U}}(\hat{\theta})} \right) \overline{\mathbb{T}}(\hat{\theta}), \ {}^{C}{\mathscr{D}}{0+}^{\alpha}\overline{\mathbb{A}}(\hat{\theta}) = \eta^{\alpha} \overline{\mathbb{C}}(\hat{\theta})+\gamma2^{\alpha} \overline{\mathbb{T}}(\hat{\theta}) \overline{\mathbb{A}}(\hat{\theta}) - \frac{\rho1^{\alpha} \overline{\mathbb{A}}(\hat{\theta}) \overline{\mathbb{D}}(\hat{\theta})}{\varsigma1^{\alpha}+\overline{\mathbb{D}}(\hat{\theta})} - p^{\alpha} \overline{\mathbb{A}}(\hat{\theta})\overline{\mathbb{C}}(\hat{\theta}) - \epsilon2^{\alpha} \overline{\mathbb{A}}(\hat{\theta}) - \mathbb{Z}{\overline{\mathbb{A}}} \left( 1 - e^{-\omega{\overline{\mathbb{A}}} \overline{\mathbb{U}}(\hat{\theta})} \right) \overline{\mathbb{A}}(\hat{\theta}), \ {}^{C}{\mathscr{D}}{0+}^{\alpha}\overline{\mathbb{C}}(\hat{\theta}) = \mu2^{\alpha} \overline{\mathbb{C}}(\hat{\theta}) \left( 1-\nu2^{\alpha} \overline{\mathbb{C}}(\hat{\theta}) \right) - \frac{\rho2^{\alpha} \overline{\mathbb{A}}(\hat{\theta}) \overline{\mathbb{C}}(\hat{\theta})}{\varsigma2^{\alpha}+\overline{\mathbb{C}}(\hat{\theta})} - \left( \mathbb{Z}{\overline{\mathbb{C}}} +\mathbb{Z}{\overline{\mathbb{C}\mathbb{D}}}\overline{\mathbb{D}}(\hat{\theta}) \right) \left( 1-e^{-\omega{\overline{\mathbb{C}}}\overline{\mathbb{U}}(\hat{\theta})} \right) \overline{\mathbb{C}}(\hat{\theta}) - \zeta^{\alpha}\overline{\mathbb{D}}(\hat{\theta})\overline{\mathbb{C}}(\hat{\theta}), \ {}^{C}{\mathscr{D}}{0+}^{\alpha}\overline{\mathbb{D}}(\hat{\theta}) = \chi{\overline{\mathbb{D}}}(\hat{\theta}) - \Lambda1^{\alpha} \overline{\mathbb{D}}(\hat{\theta}) - \frac{\rho3^{\alpha} \overline{\mathbb{C}}( \hat{\theta}) \overline{\mathbb{D}}( \hat{\theta})}{\varsigma3^{\alpha}+\overline{\mathbb{D}}(\hat{\theta})}, \ {}^{C}{\mathscr{D}}{0+}^{\alpha}\overline{\mathbb{U}}(\hat{\theta}) = \chi{\overline{\mathbb{U}}}(\hat{\theta}) - \Lambda2^{\alpha} \overline{\mathbb{U}}(\hat{\theta}), \end{cases} ]
where (^{C}{\mathscr{D}}_{0+}^{\alpha}) denotes the Caputo fractional derivative of order (\alpha) [12].
Table 1: State Variables in the Endometrial Cancer Treatment Model
| Variable | Biological Interpretation |
|---|---|
| (\overline{\mathbb{T}}) | Population of endometrial tumor cells |
| (\overline{\mathbb{A}}) | Concentration of activated CD8+ T-cells |
| (\overline{\mathbb{C}}) | Concentration of circulating lymphocytes |
| (\overline{\mathbb{D}}) | Dostarlimab concentration |
| (\overline{\mathbb{U}}) | Chemotherapy drug concentration |
Model Parameterization
The fractional-order model requires careful parameter estimation to ensure biological relevance. Key parameters include growth rates, interaction coefficients, and drug efficacy parameters, each raised to the power of α (the fractional order) to maintain dimensional consistency.
Table 2: Key Parameters in the Fractional-Order Endometrial Cancer Model
| Parameter | Biological Interpretation | Estimation Method |
|---|---|---|
| (\mu1^{\alpha}), (\mu2^{\alpha}) | Fractional growth rates of tumor cells and lymphocytes | Literature-derived, curve fitting |
| (\gamma1^{\alpha}), (\gamma2^{\alpha}) | Fractional interaction coefficients between tumor and immune cells | Experimental data fitting |
| (\delta^{\alpha}) | Fractional natural death rate of tumor cells | In vitro studies |
| (\mathbb{Z}{\overline{\mathbb{T}}}), (\mathbb{Z}{\overline{\mathbb{A}}}), (\mathbb{Z}_{\overline{\mathbb{C}}}) | Fractional drug efficacy parameters | Clinical trial data, pharmacokinetic studies |
| (\Lambda1^{\alpha}), (\Lambda2^{\alpha}) | Fractional clearance rates for dostarlimab and chemotherapy | Pharmacokinetic studies |
Experimental Protocols and Implementation
Numerical Implementation Protocol
Protocol 1: Implementing Fractional-Order Model Simulations
Objective: To numerically solve the fractional-order differential equation system for endometrial cancer treatment dynamics.
Materials and Software:
- MATLAB R2020a or newer
- FDE12 solver for fractional differential equations
- ODE45 solver for classical ODE comparisons
- Standard computing hardware (8+ GB RAM recommended)
Procedure:
- System Initialization: Define initial conditions for all state variables based on clinically observed values in endometrial cancer patients.
- Parameter Assignment: Assign values to all fractional parameters, ensuring dimensional consistency with the chosen fractional order α.
- Solver Configuration:
- For FDE systems: Configure FDE12 solver with absolute and relative error tolerances of 1×10â»â¶
- For ODE comparisons: Use ODE45 solver with identical error tolerances
- Simulation Execution: Run simulations for a sufficient time horizon (typically 60-90 days) to observe treatment dynamics
- Control Implementation: Implement optimal control strategies using Pontryagin's Maximum Principle for fractional systems [12] [56]
Validation Steps:
- Verify solution existence and uniqueness via Banach fixed-point theorem
- Perform stability analysis using Routh-Hurwitz criteria for fractional systems
- Compare results with clinical data where available
Optimal Control Framework Protocol
Protocol 2: Fractional Optimal Control for Treatment Optimization
Objective: To develop optimal treatment strategies that minimize tumor burden while reducing drug toxicity using fractional optimal control theory.
Theoretical Framework:
- Control Variables: Define administration schedules for dostarlimab ((\chi{\overline{\mathbb{D}}}(\hat{\theta}))) and chemotherapy ((\chi{\overline{\mathbb{U}}}(\hat{\theta}))) as control variables
- Objective Functional: Formulate a cost functional that balances tumor reduction with treatment toxicity: [ J(\chi{\overline{\mathbb{D}}}, \chi{\overline{\mathbb{U}}}) = \int{0}^{tf} \left[ A\overline{\mathbb{T}}(\hat{\theta}) + B\chi{\overline{\mathbb{D}}}^2(\hat{\theta}) + C\chi{\overline{\mathbb{U}}}^2(\hat{\theta}) \right] d\hat{\theta} ] where A, B, C are weight parameters prioritizing treatment goals [12]
- Hamiltonian Formulation: Apply Pontryagin's Maximum Principle for fractional systems to derive necessary optimality conditions
- Adjoint System: Solve the fractional adjoint system backward in time
- Optimality Conditions: Derive optimal control characterizations from the Hamiltonian minimization condition [56]
Implementation Steps:
- Solve state system forward with initial control guesses
- Solve adjoint system backward in time
- Update controls using optimality conditions
- Iterate until convergence of the objective functional
Signaling Pathways and Therapeutic Mechanisms
Figure 1: Endometrial Cancer Signaling and Treatment Pathways
Research Reagent Solutions
Table 3: Essential Research Reagents for Endometrial Cancer Modeling
| Reagent/Resource | Function in Research | Application Context |
|---|---|---|
| Dostarlimab | PD-1 immune checkpoint inhibitor | Immunotherapy agent in endometrial cancer treatment [12] |
| Carboplatin/Paclitaxel | Chemotherapy drugs | Standard chemotherapy for endometrial cancer [12] |
| CD8+ T-cell markers (CD8, CD3, granzyme B) | Immune cell identification | Quantifying activated T-cell populations |
| Caputo derivative framework | Mathematical operator | Capturing memory effects in biological systems [12] [55] |
| FDE12 solver | Numerical computation | Solving fractional differential equations in MATLAB [12] |
| Primary endometrial cell cultures | In vitro modeling | Studying tumor-immune interactions |
| Cytokine assay kits | Immune response measurement | Quantifying inflammatory mediators in tumor microenvironment |
Computational Workflow for Fractional Modeling
Figure 2: Fractional-Order Modeling Workflow
Results Interpretation and Clinical Implications
Comparative Treatment Efficacy
Research findings demonstrate that fractional-order models provide distinct advantages in treatment optimization for endometrial cancer. Simulation results indicate that dostarlimab monotherapy shows greater efficacy than chemotherapy alone, while combined therapy achieves the most significant reduction in cancer cell populations and strongest activation of CD8+ T-cells [12].
A critical insight from fractional modeling is the difference in therapeutic dynamics between ODE and FDE frameworks. While ODE models typically predict faster tumor reduction and higher immune activation, FDE models achieve comparable long-term outcomes with lower overall therapeutic cost by balancing tumor reduction with reduced drug usage [12]. This suggests that fractional-order models may better capture the complex, memory-dependent nature of biological systems, leading to more realistic and potentially more sustainable treatment regimens.
Memory Effects in Treatment Response
The memory effect captured by fractional derivatives manifests clinically in several important ways:
- Hysteresis in drug response: Delayed effects between drug administration and observed therapeutic outcomes
- Cumulative immune activation: Progressive enhancement of immune response through repeated antigen exposure
- Long-term treatment efficacy: Sustained effects beyond the treatment period due to immunological memory
These effects are mathematically represented through the non-local nature of fractional derivatives, where the current rate of change depends on the entire history of the system rather than just its immediate past [12] [55].
Fractional calculus provides a powerful mathematical framework for modeling endometrial cancer dynamics and treatment response. By effectively capturing memory effects and hereditary properties of biological systems, fractional-order models offer enhanced predictive capability compared to traditional integer-order approaches. The application of fractional optimal control theory enables the design of treatment strategies that balance therapeutic efficacy with toxicity considerations.
Future research directions should include:
- Development of patient-specific fractional models incorporating individual hormonal profiles
- Integration of multi-scale modeling approaches connecting molecular pathways to organ-level dynamics
- Clinical validation of fractional-optimized treatment schedules through prospective studies
- Expansion of fractional modeling to other gynecological conditions and cancer types
As computational modeling continues to evolve, fractional calculus stands to play an increasingly important role in personalized medicine and treatment optimization for endometrial disorders and cancers.
The inherent complexity and heterogeneity of the human endometrium, a dynamic tissue that undergoes constant remodeling, present substantial challenges for both basic research and drug development [57]. Traditional two-dimensional (2D) cell cultures fail to capture the architectural integrity, cellular heterogeneity, and essential microenvironmental cues of in vivo tissue, limiting their translational relevance [58]. Similarly, common laboratory animal models are inadequate for studying human endometrial dynamics as they do not naturally undergo a menstrual cycle comparable to that of humans [57].
Within the context of computational modeling of endometrial dynamics, this gap between conventional models and human physiology creates a critical bottleneck. Computational models require high-quality, quantitative biological data for parameterization and validation. Without experimental systems that faithfully recapitulate human physiology, the predictive power of these in silico models remains limited.
The emergence of three-dimensional (3D) organoid technology has revolutionized this landscape. These self-organizing miniature structures closely mimic the cellular composition, hormonal responsiveness, and functional characteristics of the native endometrium [8]. This application note details protocols and analytical frameworks for leveraging endometrial organoids and assembloids to generate quantitative parameters for computational models and validate their predictions, thereby establishing a synergistic loop between in vitro and in silico methodologies.
Quantitative Characterization of Endometrial Organoids
The utility of 3D organoids in parameterizing computational models hinges on their ability to accurately replicate key anatomical and functional aspects of the native endometrium. The table below summarizes the core characteristics of endometrial organoids that are quantifiable for model parameterization.
Table 1: Key Parameterization Metrics from Endometrial Organoids
| Parameter Category | Specific Measurable Metric | Significance for Computational Modeling | Experimental Measurement Method |
|---|---|---|---|
| Architectural & Morphological | Gland-like structure formation, Apicobasal polarity [8] | Informs structural and spatial constraints in models of tissue organization. | Immunofluorescence (E-cadherin, PanCK), Confocal microscopy |
| Cellular Composition & Identity | Presence of progenitor (LRIG1, SOX9), secretory (PAEP, MUC1), and ciliated (FOXJ1) cells [8] | Defines cellular agent types and their proportions in agent-based models. | Single-cell RNA sequencing, Flow cytometry, PCR |
| Hormonal Response Dynamics | Upregulation of receptivity markers (HSPA9, DPP4, LIF) in response to estrogen/progesterone [8] | Provides kinetic parameters for modeling hormonal regulation and the window of implantation. | ELISA, qPCR, Luminex assays on apical secretions |
| Functional Secretory Profile | Apical secretion of DPP4, HSPA9; Basal secretion of cystatin C, miR-92a-3p [8] | Quantifies paracrine and autocrine signaling gradients within the tissue microenvironment. | Mass spectrometry, Western blot, miRNA sequencing |
| Invasion & Migration Capacity | Migration radius, Number of cell projections, Invasion distribution [59] | Critical for modeling trophoblast invasion during embryo implantation. | Deep learning analysis of time-lapse imaging (ImplantoMetrics) |
Protocol: Establishing a Functional Endometrial Assembloi*d for Dynamic Studies
For investigating complex processes like embryo implantation or cancer invasion, simple epithelial organoids are insufficient. The following protocol details the creation of a multi-compartment endometrial assembloid that mimics the architecture of endometrial tissue and recapitulates all three phases of the menstrual cycle [57].
Materials and Reagents
Table 2: Research Reagent Solutions for Endometrial Assembloid Culture*
| Reagent / Material | Function / Purpose | Example / Specification |
|---|---|---|
| Immortalized HESC cell line [59] | Forms the stromal compartment of the endometrium. | Telomerase-pretreated human endometrial stromal cell line. |
| HEC-1-A cell line [59] | Forms the epithelial barrier layer of the endometrium. | Human endometrial adenocarcinoma cell line with epithelial properties. |
| Sw.71 Trophoblast cell line [59] | Generates blastocyst-like spheroids (BLS) for invasion studies. | Telomerase-immortalized first-trimester trophoblast cell line. |
| Matrigel / BME | Simulates the human endometrial extracellular matrix (ECM); provides 3D scaffolding [59] [8]. | Basement membrane extract, growth factor-reduced. |
| Advanced DMEM/F12 Medium | Base nutrient medium for organoid culture [8]. | Supplied with GlutaMAX and HEPES. |
| Growth Factor Cocktail | Promotes cell proliferation, survival, and self-renewal [8]. | Includes FGF10, HGF, EGF, R-spondin-1 (RSPO1). |
| Signaling Pathway Inhibitors | Inhibits differentiation and promotes stemness [8]. | Noggin (BMP inhibitor), A83-01 (TGF-β inhibitor). |
| ROCK Inhibitor (Y-27632) | Enhances cell survival after dissociation and plating, reducing anoikis [8]. | Final concentration 10 µM. |
| Hormonal Additives | To induce and study specific phases of the menstrual cycle (e.g., decidualization) [57]. | Estradiol, Progesterone, cAMP. |
Step-by-Step Workflow
Diagram 1: Endometrial assembloid experimental workflow.
Day 1: Stromal Layer Seeding
- Plate Human Endometrial Stromal Cells (HESCs): Seed immortalized HESCs in a pre-warmed cell culture plate (e.g., 96-well). These cells represent the stromal compartment.
- Culture Conditions: Maintain in appropriate stromal cell medium at 37°C with 5% CO₂.
Day 2: Matrix and Epithelial Layer Addition
- Overlay with Matrigel: Gently cover the HESC layer with a thin layer of Matrigel (or similar ECM). Incubate at 37°C for 30-45 minutes to allow solidification.
- Seed Epithelial Cells: After solidification, add the HEC-1-A cell suspension on top of the Matrigel layer. This forms the epithelial barrier.
In Parallel: Prepare Blastocyst-Like Spheroids (BLS)
- Harvest Trophoblast Cells: Culture GFP-labeled Sw.71 trophoblast cells.
- Form Spheroids: Seed the trophoblast cells into ultra-low attachment plates to encourage 3D spherical aggregation over two days.
Day 4: Assembloi*d Integration and Initiation of Experiment
- Transfer BLS: Carefully transfer a single BLS onto the center of the pre-formed HESC/Matrigel/HEC-1-A assembloid.
- Apply Interventions: Add the drug, hormone, or other chemical of interest to the culture medium.
- Begin Imaging: Place the plate in a live-cell imager (e.g., Cytation 7 or similar). Capture images at regular intervals (e.g., every 8-12 hours) for up to six days [59].
Protocol: Quantitative Analysis of Invasion Dynamics Using Deep Learning
Manual quantification of invasion metrics is time-consuming and subjective. This protocol leverages the ImplantoMetrics tool to automate the extraction of quantitative parameters from imaging data [59].
Image Acquisition and Preprocessing
- Acquire Time-Lapse Data: Use fluorescence microscopy to capture images of the GFP-labeled BLS at consistent intervals.
- Export Image Stacks: Compile images into a standardized format (e.g., TIFF stack) for analysis, ensuring consistent naming conventions.
Automated Analysis with ImplantoMetrics
- Install Plugin: Install the ImplantoMetrics plugin in Fiji (ImageJ).
- Run Analysis: Open the image stack and execute the ImplantoMetrics pipeline. The underlying Convolutional Neural Network (CNN), based on the Xception architecture, automatically extracts key parameters [59].
- Extract Quantitative Data: The tool outputs a data file containing the following metrics for each time point:
- Spheroid Radius: The core radius of the BLS.
- Migration/Invasion Radius: The distance the trophoblast cells have migrated outwards.
- Number of Cell Projections: Count of lamellipodial and filopodial protrusions.
- Total Area: Combined area of the spheroid core and its projections.
- Distribution of Migration: A measure of how evenly distributed the invasion is around the spheroid.
- Circularity: A shape descriptor (a value of 1.0 indicates a perfect circle).
- Calculate Invasion Factor: ImplantoMetrics integrates these parameters to compute a single, quantitative "Invasion Factor" (ranging from 0 to 1), which assesses the probability of successful invasion [59].
Table 3: Parameters Extracted by ImplantoMetrics for Model Validation
| Parameter | Description | Role in Computational Model Validation |
|---|---|---|
| Migration Radius | Radial distance of outward cell migration. | Validates the spatial expansion dynamics predicted by the model. |
| Number of Projections | Count of cellular protrusions, indicating active invasion. | Serves as a metric for model-predicted cellular activity and polarization. |
| Invasion Distribution | Measure of the uniformity of invasion around the spheroid. | Tests if the model correctly simulates homogeneous vs. directed invasion. |
| Circularity | Shape descriptor (4π×Area/Perimeter²). | Validates predictions about the stability of the spheroid structure over time. |
| Invasion Factor | Composite score (0-1) of invasion success. | Provides a single quantitative benchmark for overall model accuracy. |
Diagram 2: Deep learning-based analysis of spheroid invasion.
Integrating Organoid Data with Computational Frameworks
The quantitative data generated from the above protocols feed directly into computational models, creating a synergistic cycle. A prime example is the "Organoid plus and minus" framework, which combines technological augmentation with culture system refinement to improve screening accuracy and physiological relevance [58]. Furthermore, AI models like PharmaFormer demonstrate how transfer learning can be used to predict clinical drug responses by initially pre-training on abundant 2D cell line data and then fine-tuning with limited, but highly physiologically relevant, organoid pharmacogenomic data [60].
In this paradigm, the parameterized computational model can be used to run in silico simulations to predict outcomes under novel conditions (e.g., a new drug combination or genetic mutation). These predictions are then tested experimentally using the assembloid platform. The resulting experimental data serves to validate and iteratively refine the computational model, enhancing its predictive power for the next cycle of research. This closed-loop synergy between advanced in vitro models and in silico tools dramatically accelerates discovery and translation in endometrial research.
In the field of computational modeling of endometrial dynamics, the development of robust machine learning (ML) models is paramount for achieving reliable diagnostics and predictive outcomes. Model overfitting represents a fundamental challenge, occurring when a model learns the training data too well, including its noise and random fluctuations, but fails to generalize to unseen data [61] [62]. This is particularly critical in endometrial cancer research, where models must perform accurately across diverse patient populations and clinical settings. The consequences of overfitting include reduced predictive power on real-world clinical data, limited applicability across different healthcare institutions, and potentially flawed clinical decision-making [61].
The balance between bias and variance is crucial for model generalizability. High-bias models, which are overly simplistic, can miss relevant patterns in endometrial tissue analysis, while high-variance models capture noise specific to training data, leading to poor performance on new patient data [61]. In endometrial cancer detection, where models are increasingly used for diagnosing and staging from histopathological images and MRI scans, overfitting can significantly impact patient outcomes by reducing the model's clinical utility and reliability [63] [64]. Understanding and mitigating overfitting is therefore essential for advancing computational research in endometrial dynamics and ensuring translational success from research to clinical practice.
Quantitative Assessment of Model Performance and Overfitting
Evaluating model performance requires careful analysis of metrics across training and testing datasets to identify potential overfitting. The table below summarizes key performance metrics and their implications for model generalizability in endometrial cancer research contexts:
Table 1: Performance Metrics for Model Assessment and Overfitting Detection
| Model Type | Training Accuracy | Test Accuracy | AUC | Implied Status | Clinical Research Implication |
|---|---|---|---|---|---|
| Overfit Model | 99.9% | 45% | Significantly higher on training | Overfit | Poor generalizability; unsuitable for clinical use |
| Appropriately Fit Model | 99.9% | 95% | Comparable between datasets | Healthy | Good generalizability potential |
| Underfit Model | 87% | 87% | Consistently moderate | Underfit | Missed patterns; requires model optimization |
| Tuned Model | High | Slightly lower | Maintains performance on perturbed data | Robust | Clinically applicable; reliable predictions |
Performance disparities between training and testing phases provide crucial indicators of overfitting. A significant drop in test accuracy compared to training accuracy, such as from 99.9% to 45%, clearly indicates overfitting [65]. In endometrial cancer research, where models like DCS-NET achieve up to 90.8% accuracy in staging early endometrial cancer, maintaining this performance on unseen clinical data is essential for clinical adoption [63]. The AUC (Area Under the Curve) metric is particularly valuable for binary classification tasks common in cancer detection, where an AUC significantly higher on training data than test data suggests overfitting [61]. For regression problems in endometrial dynamics, such as predicting treatment responses, R-squared values that are very high on training data but much lower on test data may indicate overfitting [61].
Experimental Protocols for Assessing Model Robustness
Robustness Testing via Data Perturbation
Assessing model robustness involves testing performance under various conditions, including scenarios the model may not have encountered during training [61]. The following protocol provides a systematic approach for evaluating model robustness in endometrial cancer research:
Protocol 1: Model Robustness Assessment via Data Perturbation
Objective: Evaluate model performance stability when subjected to small variations in input data, simulating real-world clinical variations.
Materials and Setup:
- Trained model for endometrial analysis (e.g., classification or detection model)
- Hold-out test dataset with known ground truth labels
- Computational environment for perturbation (Python with PiML toolkit or similar)
- Performance metrics (AUC, accuracy, F1-score)
Procedure:
- Step 1: Establish baseline performance metrics on unperturbed test data
- Step 2: Apply perturbation to test data using either raw or quantile methods:
- Step 3: Calculate model outputs f̂(x+△x) on perturbed data
- Step 4: Evaluate performance metrics Score(y, f̂(x+△x)) on perturbed data
- Step 5: Repeat steps 2-4 for multiple iterations (recommended: 10 times) for all test samples
- Step 6: Compare performance degradation across perturbation sizes
Interpretation: Models showing significant performance decline (e.g., AUC drop from 0.77 to 0.72 at perturbation size 0.1) indicate sensitivity to input variations and poor robustness [61].
Cross-Validation Protocol for Endometrial Data
Cross-validation provides a robust methodology for assessing model generalizability, particularly important with limited endometrial cancer datasets:
Protocol 2: k-Fold Cross-Validation for Endometrial Models
Objective: Assess model performance across different data splits to ensure generalizability beyond specific training samples.
Materials:
- Endometrial dataset (e.g., histopathological images, MRI scans, clinical data)
- ML model architecture (e.g., CNN, logistic regression, ensemble method)
- Computational resources for multiple training runs
Procedure:
- Step 1: Randomize dataset and partition into k subsets (folds), typically k=5 or k=10
- Step 2: For each fold i (i=1 to k):
- Use fold i as validation set
- Use remaining k-1 folds as training set
- Train model on training set
- Evaluate performance on validation set
- Record performance metrics (accuracy, AUC, precision, recall)
- Step 3: Calculate mean and standard deviation of performance metrics across all folds
- Step 4: Analyze variance in performance across folds - high variance suggests sensitivity to specific data partitions
Clinical Consideration: For endometrial cancer applications with class imbalance (e.g., rare cancer subtypes), implement stratified cross-validation to maintain class distribution in each fold.
Mitigation Strategies for Overfitting in Endometrial Research
Technical Approaches to Reduce Overfitting
Several technical strategies effectively mitigate overfitting in computational models for endometrial research:
Table 2: Overfitting Mitigation Techniques and Their Applications
| Mitigation Technique | Implementation Method | Mechanism of Action | Endometrial Research Application |
|---|---|---|---|
| Regularization | L1 (Lasso), L2 (Ridge), ElasticNet | Adds penalty terms to loss function to discourage complex models | Prevents overfitting on high-dimensional omics data from endometrial tissues |
| Cross-Validation | k-Fold, Stratified k-Fold | Assesses performance across multiple data splits | Validates models on limited endometrial cancer datasets |
| Data Augmentation | Random transformations, synthetic data generation | Increases effective dataset size and diversity | Expands limited histopathological image datasets [64] |
| Ensemble Methods | Random Forest, Model averaging | Combines predictions from multiple models | Improves robustness in endometrial cancer classification |
| Early Stopping | Monitoring validation performance | Halts training when validation performance plateaus | Prevents overtraining in deep learning models for MRI analysis [63] |
| Feature Selection | Recursive Feature Elimination, correlation analysis | Reduces dimensionality by selecting relevant features | Identifies key biomarkers in endometrial cancer detection |
| Dropout | Randomly deactivating neurons during training | Prevents co-adaptation of neurons | Regularizes neural networks for cytology analysis [66] |
Data-Centric Strategies for Enhanced Generalizability
Data quality and quantity fundamentally impact model generalizability in endometrial research:
Increasing Training Data Volume
- Collect larger, more diverse endometrial cancer datasets across multiple institutions
- Apply data augmentation techniques to histopathological images (rotations, flips, color variations) [64]
- Utilize transfer learning from related domains when endometrial-specific data is limited
Addressing Data Imbalance
- Implement class weighting to make minority classes (e.g., rare endometrial subtypes) more "important" during training [65]
- Apply sampling techniques (upsampling minority classes, downsampling majority classes)
- Use performance metrics robust to imbalance (AUC_weighted, F1-score) rather than accuracy alone [65]
Preventing Target Leakage
- Ensure no data from the future is available during training for temporal predictions
- Validate that features used during training will be available in clinical deployment scenarios
- Conduct thorough domain expert review to identify potential leakage sources
Case Study: Robustness in Endometrial Cancer Detection Models
Recent advances in endometrial cancer detection provide illustrative examples of overfitting mitigation in practice. The DCS-NET framework for uterine ROI detection and automatic staging of early endometrial cancer in MRI implements several robustness strategies, achieving 90.8% accuracy through a multi-task approach that incorporates region-focused analysis to improve staging accuracy by 5% compared to direct classification [63]. This architecture demonstrates how domain-specific structural insights (uterine region localization prior to classification) can enhance generalizability.
The ECgMLP model for endometrial cancer diagnosis from histopathological images achieves 99.26% accuracy through advanced preprocessing techniques including normalization, Non-Local Means denoising, and alpha-beta enhancement, combined with effective segmentation using Otsu thresholding and watershed approaches [64]. This comprehensive preprocessing pipeline reduces reliance on spurious patterns in raw data, enhancing model robustness.
In cytology support models, YOLOv5x architectures achieve malignant mAP of 0.798 in endometrial cancer detection, with Grad-CAM visualizations providing interpretability into model decision-making [66]. The integration of explainable AI techniques builds trust in model predictions and helps identify potential overfitting to irrelevant visual features.
Essential Research Reagent Solutions for Endometrial Computational Modeling
Table 3: Research Reagent Solutions for Endometrial Computational Modeling
| Reagent/Tool | Function | Application Example | Implementation Considerations |
|---|---|---|---|
| PiML Toolkit | Model diagnostics and robustness testing | Measuring AUC gaps between train/test data; perturbation testing [61] | Open-source Python package; supports multiple ML frameworks |
| YOLOv5/x | Object detection for region localization | Uterine ROI detection in MRI scans [63] | Pretrained models available; requires domain-specific fine-tuning |
| ResNet34 | Deep learning classification | Endometrial cancer staging from cropped uterine regions [63] | Transfer learning from ImageNet; architecture modifications for medical images |
| Grad-CAM | Model interpretability and visualization | Understanding focus areas in cytology images [66] | Requires specific model architectures; integration with visualization pipelines |
| AutoML Platforms | Automated hyperparameter tuning and regularization | Preventing overfitting through optimized model configuration [65] | Azure ML, Google AutoML; computational resource requirements |
| Data Augmentation Pipelines | Generating synthetic training data | Increasing histopathological image diversity [64] | Domain-specific transformations; preservation of pathological features |
| Cross-Validation Frameworks | Robust performance estimation | k-Fold validation for limited endometrial datasets [62] | Stratified variants for imbalanced data; computational overhead management |
Achieving robust, generalizable machine learning models in endometrial computational research requires systematic approaches to identify and mitigate overfitting. Through rigorous assessment protocols including perturbation testing and cross-validation, combined with strategic implementation of regularization, data augmentation, and architectural optimizations, researchers can develop models that maintain performance in clinical settings. The continuing integration of domain knowledge from endometrial pathology with advanced machine learning techniques promises to enhance model reliability and accelerate the translation of computational research into improved patient care outcomes.
High-Performance Computing and Algorithmic Advances for Complex Model Simulation
Recent advances in high-performance computing and machine learning algorithms are revolutionizing computational modeling in biomedical research. The development of deep active optimization pipelines and sophisticated mathematical frameworks now enables researchers to simulate complex biological systems with unprecedented accuracy and efficiency. Within endometrial cancer research, these computational approaches provide powerful tools for modeling tumor dynamics, predicting treatment responses, and optimizing therapeutic strategies. This article presents application notes and experimental protocols for implementing these cutting-edge computational techniques, specifically focusing on their integration into endometrial cancer research workflows. We demonstrate how deep neural surrogate models, fractional calculus implementations, and optimal control theory can be combined to create predictive models that account for the complex, high-dimensional nature of cancer-immune interactions and treatment responses.
The computational modeling of endometrial dynamics represents a significant challenge due to the complex, nonlinear interactions between tumor cells, immune components, and therapeutic interventions. Traditional modeling approaches often fail to capture the high-dimensional parameter spaces and multi-scale dynamics inherent in biological systems. The emergence of deep active optimization frameworks and fractional calculus-based models has created new opportunities for developing more accurate and computationally efficient simulations of endometrial cancer progression and treatment response.
Recent algorithmic advances have demonstrated remarkable capabilities in handling complex systems with up to 2,000 dimensions while requiring significantly fewer data points than conventional methods [67]. These developments are particularly valuable in endometrial cancer research, where limited data availability and system complexity present substantial obstacles to model development. Furthermore, the integration of optimal control theory with biological modeling enables researchers to in silico evaluate single and combination therapies, potentially accelerating the development of personalized treatment strategies [12].
This article provides detailed application notes and experimental protocols for implementing these advanced computational techniques in endometrial cancer research. We present structured methodologies, performance benchmarks, and practical implementation guidelines to enable researchers to leverage these powerful approaches in their investigations of endometrial dynamics.
Computational Frameworks and Algorithmic Advances
Deep Active Optimization with Neural-Surrogate-Guided Tree Exploration
The DANTE (Deep Active Optimization with Neural-Surrogate-Guided Tree Exploration) pipeline represents a significant advancement in optimization methodologies for complex systems with limited data availability. This approach combines deep neural networks with tree search algorithms to efficiently navigate high-dimensional search spaces while minimizing the number of required experimental samples [67].
Table 1: Key Components of the DANTE Framework
| Component | Function | Advantage |
|---|---|---|
| Deep Neural Surrogate | Approximates complex system behavior | Handles high-dimensional, nonlinear systems |
| Tree Exploration | Navigates solution space efficiently | Balances exploration-exploitation tradeoffs |
| Conditional Selection | Determines when to expand search nodes | Prevents value deterioration in search process |
| Local Backpropagation | Updates node values selectively | Enables escape from local optima |
| Data-Driven UCB | Guides exploration based on visitation counts | Uses frequentist approach to uncertainty |
The DANTE framework operates through an iterative process that begins with a relatively small initial dataset (typically 100-200 points) and proceeds through cycles of model training, candidate selection, and experimental validation. This approach has demonstrated superior performance across diverse problem domains, identifying optimal solutions in 80-100% of test cases while using as few as 500 data points in problems ranging from 20 to 2,000 dimensions [67].
Fractional Calculus Models for Endometrial Cancer Dynamics
Fractional differential equations (FDEs) provide a powerful mathematical framework for modeling endometrial cancer dynamics by incorporating memory effects and hereditary properties of biological systems. Recent work has established FDE-based models that capture the complex interactions between tumor cells (Ŧ), activated CD8+ T-cells (Å), circulating lymphocytes (Ć), dostarlimab concentration (Ď), and chemotherapy drugs (Ù) [12].
The fractional-order model extends traditional ordinary differential equations through the Caputo derivative, enabling more accurate representation of the non-local temporal dependencies characteristic of biological systems. Numerical implementation utilizes the fde12 solver in MATLAB, which provides efficient computation of fractional differential equations through discretization and approximation techniques.
Table 2: Performance Comparison: Ordinary vs. Fractional Differential Equation Models for Endometrial Cancer Treatment
| Parameter | ODE Model | FDE Model |
|---|---|---|
| Tumor Reduction Rate | Faster initial reduction | More gradual, sustained reduction |
| Immune Activation | Higher CD8+ T-cell activation | Balanced immune response |
| Therapeutic Cost | Higher overall drug usage | 20-30% lower therapeutic cost |
| Memory Effects | Not captured | Explicitly incorporated |
| Computational Demand | Lower (ode45 solver) | Higher (fde12 solver) |
The FDE framework demonstrates particular advantages in balancing treatment efficacy with cost minimization, achieving comparable tumor reduction with 20-30% lower therapeutic cost compared to conventional ODE models [12].
Application to Endometrial Cancer Research
Spatial Ecostructural Modeling of Tumor Microenvironment
Advanced computational approaches are enabling high-resolution mapping of the endometrial tumor microenvironment through spatial ecostructural modeling. This methodology integrates imaging mass cytometry with machine learning-based spatial phenotyping to characterize cellular distributions and interaction networks within tumor tissues [34].
Single-cell resolution analysis of endometrial cancer cases across molecular subtypes has identified CD90+ CD105+ endothelial cells as key regulators of macrophage polarization and T-cell infiltration dynamics. Computational models integrating functional molecular signatures with cell-cell interaction profiles demonstrate high predictive accuracy for both molecular subtyping and recurrence risk stratification [34].
The experimental workflow involves:
- Tissue processing and staining with metal-conjugated antibodies
- Imaging mass cytometry data acquisition at single-cell resolution
- Cell segmentation and feature extraction using automated pipelines
- Spatial relationship mapping through graph-based approaches
- Machine learning classification of tumor subtypes and recurrence risk
This approach has revealed novel insights into tumor heterogeneity and identified potential targets for personalized therapeutic strategies in endometrial cancer management.
Multi-Modal Imaging Data Integration
The computational analysis of multi-modal imaging data represents another significant application of advanced algorithms in endometrial cancer research. Deep learning approaches, particularly hybrid models combining ResNet50 and Vision Transformer (ViT) architectures, have demonstrated remarkable accuracy in classifying endometrial cancer using both MRI and CT imaging data [68].
The ViTNet model achieves 90.24% accuracy with MRI images and 86.99% accuracy with CT images in endometrial cancer detection, enabling non-invasive diagnostic approaches that can complement traditional histological methods [68]. These models facilitate the extraction of quantitative features from medical images, creating non-invasive biomarkers that reflect underlying tumor biology.
Experimental Protocols and Implementation
Protocol: Implementing DANTE for Endometrial Cancer Model Optimization
Purpose: To optimize complex endometrial cancer models using limited experimental data through the DANTE framework.
Materials and Computational Requirements:
- Initial dataset (100-200 data points recommended)
- High-performance computing environment with GPU acceleration
- Python with PyTorch/TensorFlow for deep neural surrogate implementation
- Custom tree search implementation (Python/C++)
Procedure:
- Initial Data Collection:
- Gather initial dataset representing parameter combinations and corresponding outcomes
- Ensure coverage of parameter space through Latin hypercube sampling or similar design
Deep Neural Surrogate Training:
- Implement feedforward neural network with 5-10 hidden layers
- Use ReLU activation functions with batch normalization
- Train until convergence with early stopping prevention
Tree Search Configuration:
- Initialize root node with current best solution
- Set exploration parameters (c1=1.0, c2=1.0 recommended)
- Configure stopping criteria (iteration count or convergence threshold)
Iterative Optimization Cycle:
- Perform conditional selection to identify promising search regions
- Execute stochastic rollout to generate candidate solutions
- Apply local backpropagation to update node values
- Select top candidates for experimental validation
- Augment training dataset with new experimental results
- Retrain neural surrogate model
Validation and Analysis:
- Validate optimized solutions through independent experimental tests
- Analyze search trajectory to identify key parameter influences
- Document optimization performance metrics
Troubleshooting Tips:
- If convergence stalls, increase exploration parameters to escape local optima
- For high-dimensional problems (>500 dimensions), consider dimensionality reduction techniques
- Monitor surrogate model accuracy regularly to prevent error accumulation
Protocol: Fractional-Order Modeling of Endometrial Cancer Treatment Response
Purpose: To implement fractional-order mathematical models for simulating endometrial cancer progression and treatment response under dostarlimab and chemotherapy.
Materials and Computational Requirements:
- MATLAB with fde12 solver for fractional differential equations
- Clinical or experimental data for parameter estimation
- High-precision numerical computation environment
Procedure:
- Model Formulation:
- Define model variables: tumor cells (Ŧ), activated CD8+ T-cells (Å), circulating lymphocytes (Ć), dostarlimab (Ď), chemotherapy (Ù)
- Establish parameter values through literature review or experimental fitting
- Implement both ODE and FDE versions for comparative analysis
Numerical Implementation:
- Code ordinary differential equation system using ode45 solver
- Implement fractional differential equation system using fde12 solver
- Set appropriate initial conditions based on clinical scenarios
- Configure simulation time frame (typically 90-180 days)
Parameter Estimation:
- Apply maximum likelihood estimation to clinical data
- Use sensitivity analysis to identify most influential parameters
- Validate parameter sets through comparison with experimental results
Optimal Control Implementation:
- Define objective function balancing tumor reduction and treatment cost
- Implement Hamiltonian framework for optimal control determination
- Solve resulting optimization problem through numerical methods
Simulation and Analysis:
- Execute simulations for single and combination therapies
- Compare ODE and FDE model predictions
- Analyze tradeoffs between treatment efficacy and cost
- Perform sensitivity analysis on key parameters
Validation Methods:
- Compare model predictions with experimental animal studies
- Validate against clinical trial data when available
- Assess predictive accuracy through statistical measures (RMSE, AIC)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools and Biological Resources for Endometrial Cancer Modeling
| Resource | Type | Function | Implementation Notes |
|---|---|---|---|
| DANTE Framework | Algorithm | High-dimensional optimization | Custom implementation based on [67] |
| Fractional Calculus Model | Mathematical Framework | Captures memory effects in biological systems | MATLAB fde12 solver [12] |
| ViTNet Architecture | Deep Learning Model | Classifies endometrial cancer from medical images | Hybrid ResNet50-ViT implementation [68] |
| Imaging Mass Cytometry | Experimental Platform | Enables single-cell spatial analysis | Hyperion Imaging System [34] |
| Optimal Control Theory | Mathematical Framework | Optimizes treatment scheduling and dosing | Hamiltonian formulation with constraints [12] |
| CD90+ CD105+ Markers | Biological Reagents | Identifies key endothelial cell populations | Antibody conjugates for IMC [34] |
| Dostarlimab | Therapeutic Agent | PD-1 inhibitor for immunotherapy | Clinical-grade for validation studies [12] |
Visualizations
DANTE Optimization Workflow
Endometrial Cancer Treatment Response Model
Spatial Ecostructural Analysis Workflow
Benchmarking Success: Model Validation, Comparative Analysis, and Path to Translation
The shift towards personalized medicine in oncology and complex diseases like endometriosis has revealed the limitations of single-data-type analyses. Traditional approaches that analyze molecular data in isolation place a high burden on these nascent technologies to be informative alone, often underestimating the proven value of established clinical and histopathological information [69]. The true power of modern biomedical research lies in the integrative analysis of diverse data types, where clinical, histological, and molecular data are not merely sequenced but analyzed in concert to create predictive models greater than the sum of their parts [69]. This paradigm is particularly relevant in endometrial research, where conditions such as endometrial cancer and endometriosis involve complex interactions between cellular morphology, genetic drivers, and clinical manifestations.
This protocol outlines established frameworks for the systematic integration of multi-scale data, leveraging computational modeling to uncover biological insights inaccessible through independent analysis of individual data streams. We demonstrate through specific examples how integrated models achieve superior prognostic discrimination and biological understanding compared to single-modality approaches, providing a validated roadmap for researchers pursuing comprehensive computational modeling of endometrial dynamics.
Core Integration Framework and Data Types
The integrated data framework relies on systematic collection and alignment of complementary data types, each contributing unique biological insights. When combined, these data streams enable the construction of more robust and predictive computational models of disease pathogenesis and treatment response.
Table 1: Data Types for Integrated Analysis in Endometrial Research
| Data Category | Specific Data Elements | Research Applications | Considerations |
|---|---|---|---|
| Clinical Data | Patient age, BMI, symptoms (e.g., pain, infertility), medical history, tumor stage, response to therapy [14] [69]. | Patient stratification, model contextualization, evaluation of generalizability. | Quality and standardization of electronic health records; missing data. |
| Histopathological Data | Tissue morphology from H&E stains [70], immunohistochemistry (IHC) for protein expression (e.g., MMR, p53) [70], central pathology review findings [71]. | Tumor classification, identification of histological subtypes, correlation with molecular features. | Inter-observer variability [71]; requires expert annotation. |
| Molecular Data | Genomic (DNA sequencing) [72] [70], transcriptomic (RNA expression) [72], proteomic/phosphoproteomic profiles [69], methylation data. | Identification of causal drivers [72], pathway analysis, molecular subtyping, biomarker discovery. | Cost, technical noise, data dimensionality requiring feature selection. |
The critical importance of integration is demonstrated in ovarian cancer, where proteomics data assemblages that alone were uninformative (p = 0.245 for progression-free survival) became highly informative when combined with clinical information (p = 0.022) [69]. Similarly, in central nervous system germ cell tumors, integrated analysis of 190 cases revealed molecular heterogeneity and clinical associations, such as frequent MAPK pathway mutations in males and PI3K/mTOR pathway mutations in basal ganglia cases, which were not apparent from clinical data alone [71].
Computational Modeling Approaches
The selection of an appropriate computational modeling strategy depends on the research question, available data, and desired level of biological mechanism integration. The following approaches represent a spectrum from associative to highly mechanistic modeling.
Table 2: Computational Modeling Approaches for Integrated Data
| Modeling Approach | Key Characteristics | Representative Applications | Implementation Considerations |
|---|---|---|---|
| Regression & Machine Learning | Data-driven; identifies associations without presupposing causality [14]. | Developing non-surgical diagnostic tools for endometriosis from symptoms and clinical history [14]. | Requires careful feature selection to avoid overfitting; less interpretable than mechanistic models. |
| Mechanism-Based (QSP/PK-PD) | Incorporates causal relationships and interactions between components in space and time [14]. | Predicting effects of hormonal therapies on menstrual cycle dynamics and treatment outcomes [14]. | Requires extensive prior knowledge of system biology; more complex to parameterize and validate. |
| Monte Carlo Analysis | Quantifies the useful information content within a data assemblage by testing against randomized datasets [69]. | Assessing whether adding proteomic data to clinicopathological models genuinely improves prognostic discrimination [69]. | Computationally intensive; provides robust assessment of model value beyond standard performance metrics. |
Workflow for Integrated Model Development
The following diagram illustrates the logical workflow for developing and validating an integrated model, highlighting key decision points to ensure robust and interpretable results.
Experimental Protocols
Protocol 1: Monte Carlo Analysis for Assessing Data Assemblage Utility
This protocol evaluates whether adding new data types (e.g., molecular measures) to an existing model (e.g., clinical data) provides genuine prognostic value beyond what could occur by chance [69].
Materials
- Dataset: Clinical, histopathological, and molecular data with associated patient outcomes (e.g., survival, treatment response).
- Software: Statistical computing environment (R, Python) with survival analysis and resampling capabilities.
Procedure
- Model Fitting: Fit a Cox Proportional Hazards Regression (CPHR) model using the combined data assemblage (e.g., clinical + molecular data). Calculate the model's discriminative ability using the concordance index (c-index).
- Randomization: For 10,000 iterations, independently shuffle the values of the variables being tested (e.g., molecular data) across patients, breaking their relationship with the outcome but preserving their distribution.
- Null Distribution: For each randomized dataset, fit a new CPHR model and compute its c-index, building a null distribution of c-indices expected by chance.
- Significance Testing: Calculate a p-value as the proportion of randomized datasets with a c-index equal to or greater than the c-index from the actual model. A low p-value (e.g., < 0.05) indicates the tested data assemblage contains significant prognostic information.
Interpretation A significant result confirms that the integrated data provides more predictive power than either dataset alone. This method is particularly valuable for identifying when apparently good model performance is actually due to overfitting rather than true information content [69].
Protocol 2: Developing an AI-Driven Framework for Endometrial Feature Measurement
This protocol details the development of an AI framework for automated endometrial thickness (ET) measurement in transvaginal ultrasound (TVUS), demonstrating the integration of imaging data with clinical annotation [73].
Materials
- Imaging Data: A large dataset of TVUS images (e.g., 9,850 images from 5,110 cases) with expert annotations for endometrial boundaries.
- Computational Resources: GPU-enabled workstation for deep learning model training.
- Software: Deep learning frameworks (e.g., PyTorch, TensorFlow) and image processing libraries.
Procedure
- Data Curation: Retrospectively and prospectively collect TVUS images with annotations from sonographers of varying experience levels. Include diverse endometrial echogenic patterns (triple-line, intermediate isoechogenic, homogeneous hyperechogenic) [73].
- Model Architecture:
- Implement a uterine corpus segmentation model.
- Implement a separate endometrial segmentation model.
- Develop a maximum interior tangent circle (MITC) search algorithm to identify the optimal ET measurement line [73].
- Training: Train the segmentation models using the annotated dataset. Use appropriate loss functions (e.g., Dice loss) for segmentation tasks.
- Validation: Perform internal validation on a held-out test set from the same institution. Conduct external validation on a prospectively collected cohort from a different time period or institution.
- Performance Assessment: Evaluate model performance using:
- Mean Absolute Error (MAE) between AI and expert measurements.
- Intraclass Correlation Coefficient (ICC) for agreement.
- Clinical Acceptability Rate: Percentage of measurements within a predefined error range (e.g., < ±2 mm) of expert sonographers [73].
Interpretation A robust AI framework should achieve performance comparable to an experienced sonographer (e.g., MAE ~1.0 mm, ICC > 0.9) and maintain high clinical acceptability rates in external validation, demonstrating its utility as a reproducible tool for quantitative endometrial assessment.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Resources for Integrated Endometrial Studies
| Resource Category | Specific Tool / Assay | Function in Research |
|---|---|---|
| Data Sources & Cohorts | The Cancer Genome Atlas (TCGA-UCEC) [72] [70] | Provides publicly available molecular data (genomics, transcriptomics) and matched histopathology images for endometrial carcinoma. |
| Clinical Proteomic Tumor Analysis Consortium (CPTAC) [70] | Supplies proteomic and phosphoproteomic data for cancer samples, complementing genomic resources. | |
| Institutional Biobanks with IRB-approved cohorts [70] | Enables validation of findings in independent, real-world patient populations with comprehensive clinical annotation. | |
| Molecular Assays | Mismatch Repair (MMR) Immunohistochemistry [70] | Determines MMR-deficient molecular subtype in endometrial cancer. |
| TP53 Sequencing [70] | Identifies p53 aberrant molecular subtype in endometrial cancer. | |
| POLE Sequencing [70] | Detects POLE pathogenic mutations for molecular subtyping. | |
| Computational Tools | STAMP (Solid-Tumour Associative Modelling in Pathology) Pipeline [70] | An open-source pipeline for preprocessing whole-slide images, feature extraction, and Multiple Instance Learning (MIL)-based prediction. |
| Foundation Model Encoders (e.g., UNI2, Virchow2) [70] | Pre-trained deep learning models that convert image tiles into numerical feature embeddings, ready for downstream analysis. | |
| MIL Aggregators (e.g., CLAM, TransMIL) [70] | Algorithms that aggregate tile-level features from a whole-slide image to make a single slide-level prediction, enabling weak supervision. |
Pathway and Workflow Visualization
Integrated Data Analysis Workflow for Molecular Subtyping
The following diagram details the specific workflow for applying an integrated computational approach to molecular subtyping of endometrial cancer from histopathology images, leveraging foundation models and multiple instance learning [70].
This workflow has been validated to deliver accurate and generalizable molecular classification, with foundation model pipelines (e.g., UNI2 with CLAM) achieving a macro-AUC of 0.780 on an independent external cohort, significantly outperforming traditional CNN approaches [70].
The field of computational modeling in endometrial dynamics research is increasingly polarized between two distinct paradigms: mechanism-based models, grounded in established biological principles, and data-driven models, which identify patterns directly from complex datasets. Endometrial cancer (EC), the most common gynecologic cancer in high-income countries with rising incidence rates, presents a compelling case study for examining these approaches [74]. The endometrium presents unique modeling challenges due to its remarkable regenerative capacity and complex hormonal regulation [2]. This review provides a systematic comparison of these modeling paradigms, evaluates their applications in endometrial research, and offers practical protocols for their implementation, aiming to guide researchers in selecting appropriate methodologies for specific biological questions in endometrial dynamics.
Theoretical Foundations of Modeling Paradigms
Mechanism-Based Modeling Approaches
Mechanism-based models, also termed phenomenological or semi-physical models, are constructed from prior knowledge of biological systems and first principles. These models mathematically represent established physiological relationships, treating the system as a white box whose internal mechanisms are transparent and interpretable. For endometrial dynamics, mechanism-based models typically incorporate known relationships between ovarian sex steroids (estrogen and progesterone) and endometrial tissue responses [2].
A prime example is the phenomenological-based model of endometrial growth and shedding during the menstrual cycle, which predicts volume changes in the functional layer based on hormonal inputs [2]. This model couples physiological processes by incorporating blood flow through spiral arteries, endometrial cell shedding, and menstrual blood flow, with estrogen and progesterone dynamics serving as inputs derived from a previously validated model [2]. The key strength of such models lies in their interpretability; each parameter corresponds to a specific biological element or process, allowing researchers to make direct physiological inferences from simulation results.
Data-Driven Modeling Approaches
In contrast, data-driven models employ machine learning and deep learning techniques to discern complex patterns directly from observational data, often treating the system as a black box where internal mechanisms may remain opaque. These approaches have gained significant traction in endometrial research, particularly with the increasing availability of large-scale molecular and clinical datasets.
Convolutional Neural Networks (CNNs) and other deep learning architectures have demonstrated remarkable efficacy in image-based gynecological cancer diagnosis, analyzing complex visual patterns in medical imaging data [75]. More advanced implementations include multimodal deep learning frameworks that integrate physical metallurgical theory with machine learning, though similar approaches are emerging in biological contexts [76]. Data-driven models excel at identifying complex, non-linear relationships in high-dimensional data without requiring a priori knowledge of all underlying mechanisms.
Hybrid Modeling Frameworks
Recognizing the complementary strengths of both paradigms, researchers are increasingly developing hybrid frameworks that integrate mechanistic knowledge with data-driven methodologies. These dual-driven approaches leverage physical constraints from biological mechanisms while maintaining the flexibility to learn from complex datasets [76].
A notable example in endometrial research is the molecular staging model that uses global gene expression data to precisely determine endometrial cycle stage [77]. This model combines knowledge of endometrial biology with data-driven analysis of transcriptomic patterns, creating a more accurate temporal mapping than traditional histological dating methods. Such hybrid models represent a promising direction for computational endometrial research, potentially overcoming limitations inherent in either pure approach.
Application in Endometrial Dynamics Research
Endometrial Cycle Modeling
The menstrual cycle presents a compelling application domain for comparing modeling paradigms. Mechanism-based approaches have successfully simulated endometrial growth dynamics using differential equations that represent physiological responses to hormonal fluctuations. One such model quantitatively predicts endometrial volume changes throughout the cycle, incorporating spiral arteries length and menstrual blood flow based on estrogen and progesterone dynamics [2]. This model successfully replicates clinical observations, including the correlation between endometrial volume and thickness, and provides insights into menstrual disorders by modifying key parameters.
In parallel, data-driven approaches have leveraged transcriptomic data to develop precise molecular staging models. Researchers have created a method that assigns cycle stage based on global gene expression patterns from RNA sequencing data of endometrial samples [77]. This model revealed significant and synchronized daily expression changes in over 3,400 endometrial genes throughout the cycle, with the most dramatic changes occurring during the secretory phase [77]. The data-driven approach enabled identification of differentially expressed genes associated with age and ethnicity, offering insights beyond the capabilities of purely mechanistic models.
Endometrial Cancer Risk Prediction
Endometrial cancer risk stratification has been dominated by data-driven approaches, with several multivariable models developed to identify high-risk individuals for targeted prevention. A recent systematic review identified nine EC risk prediction models, predominantly based on epidemiological factors, with four incorporating polygenic risk scores and one using blood biomarkers [74] [78]. These models typically employ logistic regression or machine learning algorithms to estimate individual absolute risk of developing EC over specific timeframes.
Table 1: Performance Metrics of Endometrial Cancer Risk Prediction Models
| Model Type | Predictors Included | Discrimination (AUROC) | Calibration | Validation Status |
|---|---|---|---|---|
| Epidemiological Models | BMI, reproductive factors, hormone exposures | 0.64-0.77 | Variable, some with significant overestimation | Limited external validation |
| Polygenic Risk Score Models | SNPs + epidemiological factors | Moderate improvement over baseline | Not consistently reported | Limited external validation |
| Biomarker-Enhanced Models | Serum biomarkers + risk factors | Not fully quantified | Not fully quantified | Limited external validation |
Most existing models demonstrate moderate discrimination (AUROC ranging from 0.64 to 0.77), with varying calibration and limited external validation [74]. A significant limitation is the demographic homogeneity of development datasets, predominantly comprising postmenopausal women of White or European ancestry from Western countries, restricting generalizability to diverse populations [74] [78]. This represents a critical shortcoming given the disproportionate increase in EC incidence and mortality among non-White racial and ethnic groups [74].
Tumor Microenvironment and Molecular Subtyping
The emerging frontier in endometrial cancer modeling focuses on the tumor immune microenvironment (TIME) and molecular subtyping, areas where both modeling paradigms are contributing significant insights. Mechanism-based approaches have employed spatial ecostructural modeling to identify the key role of CD90+ CD105+ endothelial cells in tumor heterogeneity [34]. These models quantify the frequency, spatial distribution, and intercellular crosstalk of distinct immune and stromal cell populations using imaging mass cytometry data.
Simultaneously, data-driven approaches have leveraged machine learning-based spatial phenotyping to construct molecular subtype-specific signatures and recurrence prediction models for high-risk endometrial cancer [34]. The integration of single-cell spatial multiomics data has enabled high-resolution mapping of tumor-immune-stromal interaction networks, revealing novel targets for personalized therapeutic strategies [34].
Molecular classification of EC into four subtypes (POLE mutated, MSI-H/dMMR, CNL/p53wt, and CNH/p53abn) has fundamentally transformed prognostic stratification and therapeutic planning, particularly for immunotherapy applications [79]. This subtyping framework exemplifies how data-driven discoveries can inform mechanistic understanding of disease biology.
Comparative Analysis: Strengths and Limitations
Table 2: Strengths and Limitations of Modeling Paradigms in Endometrial Research
| Aspect | Mechanism-Based Models | Data-Driven Models |
|---|---|---|
| Interpretability | High - Parameters directly correspond to biological elements | Low to Moderate - "Black box" nature limits insight |
| Data Requirements | Low to Moderate - Can be developed with limited data | High - Require large, annotated datasets |
| Generalizability | Context-dependent - May fail outside established mechanisms | Limited by training data - Poor performance on underrepresented populations |
| Discovery Potential | Limited to hypothesized mechanisms | High - Can identify novel, unexpected patterns |
| Implementation Complexity | Moderate - Requires domain expertise | High - Requires specialized computational skills |
| Validation Approach | Comparison to known physiological behaviors | Statistical metrics (discrimination, calibration) |
The comparative analysis reveals complementary strengths and limitations. Mechanism-based models offer high interpretability and physiological relevance but may oversimplify complex biological systems [2]. Conversely, data-driven models excel at identifying complex patterns from high-dimensional data but suffer from limited interpretability and require extensive validation [74] [75]. The limitation is particularly evident in EC risk prediction, where models demonstrate moderate performance (AUROC 0.64-0.77) and insufficient validation for clinical implementation [74].
A critical challenge for both paradigms is ensuring equitable performance across diverse populations. Current EC risk models exhibit limited generalizability due to development in predominantly White/European cohorts [74] [78]. Similarly, molecular staging models have identified differential gene expression across ethnicities, highlighting the need for diverse representation in modeling cohorts [77].
Experimental Protocols
Protocol 1: Developing a Mechanism-Based Model of Endometrial Dynamics
Objective: To create a phenomenological-based model of endometrial growth and shedding during the menstrual cycle.
Materials and Reagents:
- Hormonal concentration data (estrogen, progesterone)
- Endometrial volume/thickness measurements (ultrasound/MRI)
- Mathematical modeling software (MATLAB, Python, R)
- Physiological parameters from literature
Procedure:
- System Definition: Define system boundaries and state variables (endometrial volume, spiral arteries length, menstrual blood flow).
- Equation Formulation: Develop differential equations representing endometrial tissue growth, vascular changes, and shedding processes.
- Parameter Estimation: Estimate parameters from experimental data using curve-fitting techniques.
- Model Validation: Compare simulation results against independent clinical data for endometrial volume, thickness, and menstrual blood flow.
- Sensitivity Analysis: Identify parameters with greatest influence on model outputs.
Validation Criteria: Quantitative assessment using experimental data of endometrial cycle dynamics; comparison of simulated vs. measured endometrial volume/thickness; prediction of multiple menstrual cycles.
Protocol 2: Implementing a Data-Driven EC Risk Prediction Model
Objective: To develop and validate a multivariate risk prediction model for endometrial cancer incidence.
Materials and Reagents:
- Epidemiological dataset (including BMI, reproductive history, hormone use)
- Genetic data (polygenic risk scores when applicable)
- Biomarker measurements (serum biomarkers when available)
- Statistical software with machine learning capabilities
Procedure:
- Cohort Definition: Establish inclusion/exclusion criteria (intact uterus, no prior cancer, age restrictions).
- Predictor Selection: Identify relevant risk factors through literature review and preliminary analysis.
- Model Training: Implement machine learning algorithms (logistic regression, random forests, neural networks) using appropriate validation techniques.
- Performance Assessment: Evaluate discrimination (AUROC/C-statistic) and calibration (E/O ratio, calibration plots).
- External Validation: Test model performance in independent datasets with different demographic characteristics.
Validation Criteria: Discrimination (AUROC >0.70); calibration (E/O ratio 0.8-1.2); successful external validation in diverse populations.
Implementation Framework
Research Reagent Solutions
Table 3: Essential Research Reagents and Computational Tools for Endometrial Modeling
| Reagent/Tool | Function | Application Examples |
|---|---|---|
| Imaging Mass Cytometry (IMC) | High-plex protein detection in tissue sections | Spatial analysis of tumor immune microenvironment [34] |
| RNA Sequencing | Genome-wide transcriptome profiling | Molecular staging model development [77] |
| Polygenic Risk Scores | Aggregated genetic susceptibility assessment | EC risk prediction models [74] |
| Mathematical Modeling Software | Numerical solution of differential equations | Mechanism-based model simulation [2] |
| Deep Learning Frameworks | Implementation of neural networks | Image-based EC diagnosis [75] |
Workflow Integration
The integration of modeling approaches requires systematic workflow design. The following diagram illustrates a proposed framework for combining mechanism-based and data-driven paradigms in endometrial research:
Research Modeling Workflow Integration
This integrated framework leverages the complementary strengths of both modeling paradigms, enabling robust and translatable research outcomes in endometrial dynamics.
The comparative analysis of modeling paradigms reveals distinct yet complementary roles for mechanism-based and data-driven approaches in endometrial dynamics research. Mechanism-based models provide physiological interpretability and theoretical foundation, while data-driven approaches offer powerful pattern recognition capabilities in complex datasets. The most promising path forward involves hybrid frameworks that integrate mechanistic constraints with data-driven flexibility, potentially overcoming the limitations of either approach alone. Future directions should prioritize improved demographic diversity in model development, incorporation of novel risk factors and biomarkers, and enhanced validation across heterogeneous populations. Such advances will be essential for realizing the potential of computational modeling to improve endometrial cancer prevention, early detection, and personalized treatment strategies.
Endometrial cancer (EC) is the most common gynecological malignancy in developed countries, and the management of its primary advanced or recurrent forms remains a significant clinical challenge [33]. While chemotherapy has long been the standard of care, many patients experience disease progression, creating an urgent need for more effective treatment strategies [80]. The recent introduction of immuno-oncology therapeutics, particularly the programmed death-1 (PD-1) receptor antagonist dostarlimab, has transformed the treatment landscape [80] [81].
Computational modeling provides a powerful framework for quantitatively analyzing complex biological systems and treatment responses. This case study investigates two mathematical approaches for modeling endometrial cancer dynamics under dostarlimab and chemotherapy treatment: classical integer-order ordinary differential equations (ODEs) and fractional differential equations (FDEs) utilizing the Caputo derivative [82] [12]. The FDE framework specifically incorporates memory effects and non-local interactions, which may more accurately capture the complex biological processes underlying tumor-immune interactions and drug responses [12].
Table 1: Clinical Context of Endometrial Cancer and Dostarlimab
| Aspect | Description | Clinical Significance |
|---|---|---|
| Epidemiology | Most common gynecological cancer in developed countries [33] | Significant healthcare burden with ~60,000 new US cases annually [80] |
| Treatment Challenge | Poor outcomes for advanced/recurrent disease [33] | 5-year survival ~20% for metastatic disease [33] |
| dMMR/MSI-H Status | Present in 20-29% of endometrial cancers [80] | Predictive biomarker for immunotherapy response [80] |
| Dostarlimab Mechanism | PD-1 blocking antibody [80] | Enhances immune system's anti-tumor activity [80] |
| Clinical Efficacy | 71% reduction in risk of progression/death in dMMR/MSI-H patients [80] | Practice-changing outcome from RUBY trial [80] [81] |
Background and Clinical Context
Endometrial Cancer and Current Treatment Landscape
Endometrial cancer incidence has steadily increased in recent decades, largely driven by rising rates of obesity, type 2 diabetes, and an aging population [33]. The disease is molecularly heterogeneous, with the mismatch repair deficient (dMMR) or microsatellite instability-high (MSI-H) subtype present in approximately 20-29% of cases [80]. This molecular classification has become crucial for treatment selection, particularly for immunotherapy approaches [33].
The standard first-line treatment for primary advanced or recurrent endometrial cancer has historically been platinum-based chemotherapy (carboplatin and paclitaxel) [33]. However, therapeutic options have recently evolved with advances in immunotherapy. Based on results from the phase III RUBY trial, the combination of dostarlimab with carboplatin-paclitaxel, followed by dostarlimab maintenance, has become a new standard of care for dMMR/MSI-H primary advanced or recurrent endometrial cancer [80] [33] [81].
Dostarlimab Mechanism and Clinical Efficacy
Dostarlimab (Jemperli) is a humanized monoclonal antibody that functions as a programmed death receptor-1 (PD-1)-blocking agent [80]. It binds to the PD-1 receptor and blocks its interaction with the ligands PD-L1 and PD-L2, thereby reversing T-cell suppression and enhancing the immune response against cancer cells [80].
Clinical efficacy data from the RUBY trial demonstrate that adding dostarlimab to standard chemotherapy significantly improves outcomes. In the dMMR/MSI-H population, the combination resulted in a 71% reduction in the risk of disease progression or death compared to chemotherapy alone [80]. Updated results show the median duration of response was significantly longer with dostarlimab - 10.6 months versus 6.2 months with placebo in the overall population [81]. The 24-month duration of response rates further underscored this benefit: 37.0% in the dostarlimab arm versus 14.3% in the placebo arm [81].
Mathematical Models
Model Formulation
The mathematical model for endometrial cancer treatment with dostarlimab and chemotherapy was developed using nonlinear ordinary differential equations and extended to fractional differential equations with Caputo derivatives to capture memory effects [82] [12]. The system dynamics involve multiple cellular compartments and their interactions.
The fractional-order model with Caputo derivative is expressed as [12]:
[ \begin{cases} ^{C}{}{\mathscr{D}}{0+}^{ \alpha } \overline{\mathbb{T}} ( \hat{\theta }) = \mu1^{\alpha} \overline{\mathbb{T}} ( \hat{\theta })(1-\nu1^{\alpha} \overline{\mathbb{T}} ( \hat{\theta })) - \gamma1^{\alpha} \overline{ \mathbb{T}} ( \hat{\theta }) \overline{ \mathbb{A}}(\hat{\theta }) - \delta^{\alpha} \overline{\mathbb{T}}(\hat{\theta }) + \epsilon1^{\alpha} \overline{\mathbb{A}}(\hat{\theta }) - \mathbb{Z}{\overline{\mathbb{T}}} \left( 1 - e^{-\omega{\overline{\mathbb{T}}}\overline{\mathbb{U}}(\hat{\theta })} \right) \overline{\mathbb{T}}(\hat{\theta }), \ ^{C}{}{\mathscr{D}}{0+}^{\alpha}\overline{\mathbb{A}}(\hat{\theta }) = \eta^{\alpha} \overline{\mathbb{C}}(\hat{\theta })+\gamma2^{\alpha} \overline{\mathbb{T}}(\hat{\theta }) \overline{\mathbb{A}}(\hat{\theta }) - \frac{\rho1^{\alpha} \overline{\mathbb{A}}(\hat{\theta }) \overline{\mathbb{D}}(\hat{\theta })}{\varsigma1^{\alpha}+\overline{\mathbb{D}}(\hat{\theta })}-p^{\alpha} \overline{\mathbb{A}}(\hat{\theta })\overline{\mathbb{C}}(\hat{\theta }) - \epsilon2^{\alpha} \overline{\mathbb{A}}(\hat{\theta }) - \mathbb{Z}{ \overline{\mathbb{A}}} \left( 1 - e^{-\omega{\overline{\mathbb{A}}} \overline{\mathbb{U}}(\hat{\theta })} \right) \overline{\mathbb{A}}(\hat{\theta }), \ ^{C}{}{\mathscr{D}}{0+}^{\alpha}\overline{\mathbb{C}}(\hat{\theta }) = \mu2^{\alpha} \overline{\mathbb{C}}(\hat{\theta }) \left( 1-\nu2^{\alpha} \overline{\mathbb{C}}(\hat{\theta }) \right) - \frac{\rho2^{\alpha} \overline{\mathbb{A}}(\hat{\theta }) \overline{\mathbb{C}}(\hat{\theta })}{\varsigma2^{\alpha}+\overline{\mathbb{C}}(\hat{\theta })} - \left( \mathbb{Z}{\overline{\mathbb{C}}} +\mathbb{Z}{\overline{\mathbb{C}\mathbb{D}}}\overline{\mathbb{D}}(\hat{\theta }) \right) \left( 1-e^{-\omega{\overline{\mathbb{C}}}\overline{\mathbb{U}}(\hat{\theta })} \right) \overline{\mathbb{C}}(\hat{\theta })- \zeta^{\alpha}\overline{\mathbb{D}}(\hat{\theta })\overline{\mathbb{C}}(\hat{\theta }), \ ^{C}{}{\mathscr{D}}{0+}^{\alpha}\overline{\mathbb{D}}(\hat{\theta }) = \chi{\overline{\mathbb{D}}}(\hat{\theta }) - \Lambda1^{\alpha} \overline{\mathbb{D}}(\hat{\theta }) - \frac{\rho3^{\alpha} \overline{\mathbb{C}}( \hat{\theta }) \overline{\mathbb{D}}( \hat{\theta })}{\varsigma3^{\alpha}+\overline{\mathbb{D}}(\hat{\theta })}, \ ^{C}{}{ \mathscr{D}}{0+}^{\alpha}\overline{\mathbb{U}}(\hat{\theta }) = \chi{\overline{\mathbb{U}}}(\hat{\theta }) - \Lambda2^{\alpha} \overline{\mathbb{U}}(\hat{\theta }), \end{cases} ]
Where the state variables are:
- (\overline{\mathbb{T}}): Tumor cell population
- (\overline{\mathbb{A}}): Activated CD8+ T-cells
- (\overline{\mathbb{C}}): Circulating lymphocytes
- (\overline{\mathbb{D}}): Dostarlimab concentration
- (\overline{\mathbb{U}}): Chemotherapy drug concentration
The classical ODE model represents a special case when the fractional order α = 1 [82].
Figure 1: Model Architecture and System Dynamics
Model Comparison Framework
The ODE and FDE models were compared under three treatment scenarios: dostarlimab monotherapy, chemotherapy alone, and combined therapy [82] [12]. The optimal control framework was formulated to minimize tumor burden while considering treatment costs and immune activation.
Table 2: Key Parameters in Mathematical Models
| Parameter | Biological Meaning | ODE Formulation | FDE Formulation |
|---|---|---|---|
| μ₠| Tumor growth rate | Classical derivative | Caputo fractional derivative |
| γ₠| T-cell killing rate of tumor cells | Instantaneous interactions | Memory-dependent interactions |
| Z({}_{\overline{\mathbb{T}}}) | Chemotherapy effect on tumor | First-order kinetics | Non-exponential decay patterns |
| Ïâ‚ | Dostarlimab effect on T-cells | Linear PD-1 blockade | History-dependent immune activation |
| Memory Effects | Not incorporated | Explicitly captured via fractional order α |
Results and Comparative Analysis
Treatment Efficacy Across Models
Numerical simulations implemented in MATLAB demonstrated distinct performance characteristics between the ODE and FDE approaches [82] [12]. The ode45 solver was employed for ODE systems, while the fde12 solver was used for FDE systems [12].
Table 3: Model Performance Comparison Across Treatment Modalities
| Treatment Modality | ODE Model Performance | FDE Model Performance | Clinical Correlation |
|---|---|---|---|
| Dostarlimab Monotherapy | More effective than chemotherapy alone [82] | Similar superiority pattern with memory effects [82] | 73.6% ORR in dMMR/MSI-H patients [81] |
| Chemotherapy Alone | Limited long-term control [82] | Reduced efficacy with historical dependence [82] | 61.5% ORR in dMMR/MSI-H patients [81] |
| Combined Therapy | Greatest tumor reduction & strongest CD8+ T-cell activation [82] | Significant tumor reduction with lower drug exposure [12] | 71% reduction in progression/death risk [80] |
| Tumor Reduction Dynamics | Faster initial tumor reduction [82] | More gradual reduction trajectory [12] | Median PFS 11.8 vs 7.9 months [81] |
| Immune Activation | Higher CD8+ T-cell activation [82] | Sustained activation with memory [12] | Durable responses observed in clinical trials [81] |
| Therapeutic Cost | Higher cumulative drug exposure [12] | Lower overall cost balanced efficacy [82] [12] | Toxicity management consideration [83] |
Clinical Validation and Correlations
The mathematical findings align with clinical observations from the RUBY trial. The combined therapy approach demonstrated superior efficacy, with the ODE model showing faster tumor reduction and the FDE model achieving comparable outcomes with reduced therapeutic exposure [82] [12]. Clinically, the dostarlimab-chemotherapy combination showed a 71% reduction in the risk of disease progression or death in the dMMR/MSI-H population [80].
The median duration of response data from clinical trials provides validation for the model predictions. In the overall population, the median DOR was 10.6 months with dostarlimab plus chemotherapy versus 6.2 months with chemotherapy alone [81]. The FDE model's ability to capture sustained responses aligns with the clinical observation that 30.7% of patients maintained response for at least 24 months with dostarlimab versus 12.0% with placebo [81].
Figure 2: Treatment Strategy Performance Across Models
Experimental Protocols
Numerical Implementation Protocol
Protocol Title: MATLAB Implementation of ODE and FDE Models for Endometrial Cancer Treatment Optimization
Objective: To numerically solve and compare the ODE and FDE formulations of endometrial cancer dynamics under dostarlimab and chemotherapy treatments.
Materials and Computational Tools:
- MATLAB R2020b or later
- Optimization Toolbox
- Parallel Computing Toolbox (optional, for parameter sweeps)
- ode45 solver for ODE systems [12]
- fde12 solver for FDE systems [12]
Procedure:
Parameter Initialization
- Set initial conditions for state variables: (\overline{\mathbb{T}}(0)), (\overline{\mathbb{A}}(0)), (\overline{\mathbb{C}}(0)), (\overline{\mathbb{D}}(0)), (\overline{\mathbb{U}}(0))
- Define model parameters: growth rates ((\mu1), (\mu2)), interaction terms ((\gamma1), (\gamma2)), drug efficacies ((\mathbb{Z}{\overline{\mathbb{T}}}), (\mathbb{Z}{\overline{\mathbb{A}}}))
- For FDE model: set fractional order α ∈ (0,1]
ODE Model Implementation
FDE Model Implementation
Optimal Control Framework
- Define cost functional: J(u) = ∫[Q·T(t) + R·u²(t)]dt
- Implement Pontryagin's Maximum Principle for ODE case
- Use fractional optimal control theory for FDE case
- Solve using forward-backward sweep algorithms
Treatment Scenario Simulation
- Run simulations for three scenarios: dostarlimab monotherapy, chemotherapy alone, combined therapy
- Compare tumor reduction, immune activation, and cost metrics
- Perform sensitivity analysis on key parameters
Validation and Calibration:
- Calibrate parameters using clinical data from RUBY trial [80] [81]
- Validate model predictions against reported response rates and survival outcomes
- Compare simulated CD8+ T-cell dynamics with immunophenotyping data
Model Analysis Protocol
Protocol Title: Stability and Sensitivity Analysis for Endometrial Cancer Treatment Models
Objective: To establish existence, uniqueness, and stability of solutions for both ODE and FDE formulations, and perform sensitivity analysis on key parameters.
Procedure:
Existence and Uniqueness Analysis
- Apply Banach fixed-point theorem to prove solution existence and uniqueness [12]
- Verify Lipschitz continuity conditions for right-hand side functions
- For FDE case: establish conditions for fractional-order system
Stability Analysis
- Compute equilibrium points of the system
- Perform linearization around equilibria
- Apply Routh-Hurwitz criteria for ODE local stability [12]
- Use Matignon's conditions for FDE stability analysis
Sensitivity Analysis
- Implement Latin Hypercube Sampling for parameter space exploration
- Calculate Partial Rank Correlation Coefficients (PRCC) for key outputs
- Identify most influential parameters for treatment optimization
Research Reagent Solutions
Table 4: Essential Research Materials and Computational Tools
| Reagent/Tool | Specifications | Application in Research | Source/Reference |
|---|---|---|---|
| MATLAB with Optimization Toolbox | Version R2020b or later | Numerical solution of ODE/FDE systems and optimal control [12] | MathWorks |
| ode45 Solver | Variable step Runge-Kutta (4,5) method | Solving classical ODE model for cancer dynamics [12] | MATLAB built-in |
| fde12 Solver | Fractional differential equations solver | Implementing Caputo derivative-based FDE model [12] | MATLAB Central |
| Dostarlimab (Jemperli) | 500mg IV every 3 weeks (initial), then 1000mg every 6 weeks [83] | Immunotherapy component in combined treatment [80] | GSK |
| Carboplatin-Paclitaxel | Standard chemotherapy regimen | Chemotherapy backbone in combined therapy [80] | Various manufacturers |
| Clinical Trial Data (RUBY) | NCT03981796, Phase III randomized | Model validation and parameter estimation [80] [81] | ClinicalTrials.gov |
| AlphaFold3 | Deep learning protein structure prediction | Peptide scaffold design for organoid cultures [7] | DeepMind |
Discussion
The comparative analysis of ODE and FDE models for endometrial cancer treatment with dostarlimab provides valuable insights for both computational modeling and clinical application. The ODE framework demonstrated advantages in simulating rapid initial tumor reduction and strong immune activation, aligning with clinical observations of early response in immunotherapy-treated patients [82] [81]. Conversely, the FDE model captured memory effects and non-local interactions that may better represent the biological reality of immune system memory and historical dependence of tumor growth dynamics [12].
The finding that combined therapy achieves the greatest reduction in cancer cells across both modeling frameworks strongly supports the current clinical approach of combining dostarlimab with chemotherapy [82] [80]. This convergence of mathematical prediction and clinical evidence reinforces the robustness of this treatment strategy. Additionally, the FDE model's suggestion that lower overall therapeutic cost can be achieved while maintaining efficacy presents an intriguing possibility for optimizing treatment schedules to minimize toxicity while preserving effectiveness [12].
From a clinical translation perspective, these modeling approaches offer potential for personalized treatment optimization. The ability to simulate different treatment scenarios and predict outcomes based on individual patient parameters could inform therapeutic decision-making, particularly for balancing efficacy and toxicity considerations [82] [12]. The demonstration that fractional-order models can capture memory effects suggests they may be particularly valuable for modeling the durable responses observed with immunotherapy, where immune memory plays a crucial role in long-term disease control [12] [81].
Future research directions should include integration of additional biological complexity, such as tumor heterogeneity and spatial considerations, as well as validation against larger clinical datasets. The combination of computational modeling with experimental approaches, such as organoid systems [7] [84], presents a promising path toward more predictive models that can ultimately improve patient outcomes in endometrial cancer.
Within computational modeling of endometrial dynamics, artificial intelligence (AI) has emerged as a transformative tool for enhancing diagnostic precision, prognostic stratification, and molecular classification. The validation of these AI models requires rigorous assessment of their performance against established clinical standards and expert pathologist interpretation. This Application Note provides a structured framework for the quantitative evaluation and experimental validation of AI models in endometrial cancer analysis, detailing key performance metrics, concordance methodologies, and essential research protocols to ensure robust, clinically relevant model performance.
Performance Metrics for AI Model Validation
A comprehensive validation strategy for AI models in endometrial analysis relies on multiple quantitative metrics to assess diagnostic accuracy, discriminatory power, and prognostic value. The following data, synthesized from recent studies, illustrates the performance benchmarks for various AI tasks.
Table 1: Performance Metrics for AI Models in Endometrial Cancer Diagnosis and Subtyping
| AI Model Task | Study/Source | Sensitivity (%) | Specificity (%) | AUC | Overall Accuracy (%) | Key Findings |
|---|---|---|---|---|---|---|
| EC Screening (Meta-Analysis) | JMIR Meta-Analysis [85] | 86 (95% CI: 79-90) | 92 (95% CI: 87-95) | - | - | Pooled results from 13 studies demonstrate high diagnostic accuracy. |
| Molecular Subtyping from H&E WSIs | Clinical-grade AI Model [86] | - | - | - | 90-92 (by subtype) | Achieved 92% accuracy for POLEmut and MMRd, 91% for p53abn, and 90% for NSMP. |
| Histological Grading (EndoNet) | Deep Learning for Gradining EC [87] | - | - | 0.95 (Internal) 0.86 (External) | - | Weighted F1 score of 0.91 (internal) and 0.86 (external test set). |
| Predicting Aggressive EC from MRI | Multiparametric MRI Model [88] | - | - | 0.925 (Test Cohort) | - | Combined clinical-DTL model further improved AUC to 0.950. |
Table 2: Advanced Performance and Prognostic Metrics
| Model Feature | Study/Source | Metric | Result/Value |
|---|---|---|---|
| Survival Prediction | Clinical-grade AI Model [86] | Correlation (R²) with observed survival | 0.9692 |
| Mean Absolute Error (MAE) | 123 days | ||
| Population-Specific Prognostication | Computational Image and Molecular Analysis [89] | C-Index for AA-specific model (M_AA) | 0.86 - 0.90 |
| C-Index for EA-specific model (M_EA) | 0.90 - 0.93 | ||
| Prognostic Value | Computational Image and Molecular Analysis [89] | Hazard Ratio (HR) for population-specific risk scores | Statistically significant (p < 0.05) in multivariable analysis |
Experimental Protocols for Validation
Protocol 1: Validation of WSI-Based Molecular Subtyping
This protocol outlines the procedure for validating an AI model designed to predict molecular subtypes of endometrial cancer directly from Hematoxylin and Eosin (H&E) stained Whole-Slide Images (WSIs) [86].
- Objective: To assess the accuracy and generalizability of a deep learning model in classifying endometrial cancer into four molecular subtypes: POLEmut, MMRd, p53abn, and NSMP, using H&E WSIs as input.
- Materials:
- WSI Dataset: Retrospectively collected H&E-stained WSIs from hysterectomy specimens, with confirmed molecular subtypes via gold-standard methods (Sanger sequencing and Immunohistochemistry).
- Computational Infrastructure: High-performance computing cluster with GPUs for deep learning model training and inference.
- Software: Python with deep learning libraries (e.g., PyTorch, TensorFlow), digital pathology image analysis tools.
- Methods:
- Data Curation and Preprocessing:
- Collect a minimum of 393 patients with ≥5 years of follow-up [86].
- Annotate molecular subtypes for each case using sequencing and IHC as a reference standard.
- Scan histology slides to generate WSIs at high magnification (e.g., 40x).
- Apply a pre-processing pipeline including super-resolution enhancement (e.g., SRResGAN) to improve image quality and transformer-based models (e.g., MedSAM) for automated segmentation of diagnostically relevant regions of interest (ROIs) [86].
- Model Training and Validation:
- Employ a convolutional neural network backbone (e.g., ResNet-101) for feature extraction and subtype classification [86].
- Partition the dataset at the patient level into training (80%) and test (20%) sets, ensuring balanced subtype distribution.
- Train the model to minimize cross-entropy loss using the annotated training set.
- Performance Assessment:
- Evaluate the model on the held-out test set and external validation cohorts from independent institutions.
- Calculate per-subtype accuracy, sensitivity, specificity, and area under the receiver operating characteristic curve (AUC).
- Assess survival correlation by comparing model-predicted risk strata with actual patient outcomes using correlation coefficients (R²) and Mean Absolute Error (MAE).
- Data Curation and Preprocessing:
- Validation and Concordance Measure:
- Model performance is validated against the molecular biology reference standard, not solely pathologist interpretation.
- Generalizability is confirmed through high performance on external test cohorts (e.g., N=35 and N=83) [86].
Protocol 2: Preoperative Prediction of Aggressive Histology via MRI
This protocol describes the development and validation of a Deep Transfer Learning (DTL) model using multiparametric Magnetic Resonance Imaging (MRI) to predict endometrial cancer aggressiveness preoperatively [88].
- Objective: To create a non-invasive tool for preoperatively distinguishing between aggressive and non-aggressive endometrial cancer histologies using multiparametric MRI.
- Materials:
- Patient Cohort: Retrospectively enrolled patients (e.g., n=207) with pathologically confirmed EC who underwent preoperative MRI [88].
- MRI Sequences: T2-weighted imaging (T2WI), diffusion-weighted imaging (DWI), apparent diffusion coefficient (ADC) maps, and contrast-enhanced T1-weighted imaging (CE-T1WI).
- Segmentation Software: ITK-SNAP software for manual tumor segmentation.
- DL Models: Pre-trained deep learning architectures (e.g., ResNet50, ResNet101, DenseNet121) for feature extraction.
- Methods:
- Data Acquisition and Annotation:
- Acquire preoperative MRI scans for all patients.
- Manually delineate the 3D region of interest (ROI) encompassing the entire tumor on all relevant slices, reviewed by a senior radiologist.
- Classify patients post-surgery into "aggressive" (e.g., high-grade endometrioid, serous, clear cell, carcinosarcoma) and "non-aggressive" (low-grade endometrioid) groups based on final histopathology [88].
- Model Development and Fusion:
- Split the dataset into training (70%) and test (30%) cohorts.
- For each MRI sequence, extract features using DTL models. Select the best-performing model (e.g., ResNet101).
- Apply decision-level fusion strategies (mean, maximum, minimum) to integrate predictions from the best-performing image sequences (e.g., T2WI, ADC, and CE-T1WI) [88].
- Construct a combined model by integrating significant clinical predictors (e.g., CA-125 levels, menopausal status) identified via logistic regression with the DTL features.
- Model Evaluation:
- Assess model performance using the Area Under the ROC Curve (AUC) in both training and test cohorts.
- Perform Decision Curve Analysis (DCA) to evaluate clinical utility.
- Assess model calibration using calibration curves.
- Data Acquisition and Annotation:
- Validation and Concordance Measure:
- The model's prediction is validated against the gold standard of postoperative histopathological diagnosis.
- Concordance is measured by the model's AUC, with a benchmark of >0.90 considered strong performance [88].
Visualization of Experimental Workflows
AI Validation Workflow for Endometrial Analysis
The following diagram illustrates the overarching workflow for developing and validating AI models in endometrial cancer analysis, integrating paths for both WSI and MRI-based approaches.
Pathologist Concordance Assessment Logic
The logical workflow for assessing concordance between AI model predictions and pathologist interpretations is critical for clinical validation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for AI Validation in Endometrial Analysis
| Item Name | Function/Application | Specifications/Examples |
|---|---|---|
| H&E-Stained Tissue Sections | Primary data source for WSI-based models; provides morphological context for AI pattern recognition. | Formalin-fixed, paraffin-embedded (FFPE) endometrial tissue blocks sectioned at 4-5 μm. |
| Whole-Slide Scanners | Digitizes glass slides to create high-resolution Whole-Slide Images (WSIs) for computational analysis. | Scanners from Philips, Leica, or 3DHistech; 40x magnification recommended. |
| Immunohistochemistry Kits | Gold-standard validation for molecular subtypes (e.g., MMRd, p53abn) and protein expression. | Automated IHC stainers; antibodies for p53, MLH1, PMS2, MSH2, MSH6. |
| Molecular Sequencing Assays | Gold-standard validation for genetic alterations (e.g., POLE mutations). | Sanger sequencing or Next-Generation Sequencing (NGS) panels. |
| Pre-trained Deep Learning Models | Backbone architectures for feature extraction and transfer learning, reducing data requirements. | ResNet-101, Vision Transformer (ViT), DenseNet [86] [88]. |
| Digital Pathology Analysis Software | Platform for WSI visualization, manual annotation, and integration with AI algorithms. | QuPath, HALO, Indica Labs, or custom Python-based platforms. |
| High-Performance Computing (HPC) | Infrastructure for training and running complex deep learning models on large image datasets. | GPU clusters (NVIDIA), cloud computing platforms (AWS, Google Cloud). |
Background
The integration of computational models into clinical practice is a cornerstone of modern personalized medicine, promising to transform vast, heterogeneous datasets into functional understanding and personalized treatment strategies [90]. These models support a mechanistic understanding of the factors that drive diseases, allowing for the design of tailored therapeutic interventions [90]. Within the specific context of endometrial cancer research, the limitations of current classification systems, which are based on aggressive histological types and molecular subtypes, are becoming apparent. Ignoring the spatial distribution of immune and stromal cells fails to account for the profound heterogeneity of the local tumour microenvironment, which can bias predictions of treatment response [34]. Precision medicine aims to delineate the biological characteristics of local functional units, a goal that requires computational tools capable of reflecting spatially adaptive changes during treatment or metastasis [34]. This document provides application notes and detailed protocols for employing these computational methods to advance clinical decision support, with a specific focus on endometrial cancer.
Application Notes: Key Computational Approaches
Computational-modeling approaches can be broadly categorized as either theory-driven mechanistic models or data-driven approaches, which often employ artificial intelligence (AI) and machine learning (ML) [90]. The choice of approach depends on the research question, the availability of prior structural knowledge, and the volume of data.
Mechanistic Models for Functional Understanding
Mechanistic models aim to functionally understand, examine, and predict the emergent properties of individual components of a biological system [90].
- Molecular Interaction Maps (MIMs): These are static network models that depict physical and causal interactions among biological species. They serve as a knowledge-base for pathways and regulatory modules. In endometrial cancer, MIMs can be used to visualize the activity level of established disease markers and regulators within signalling networks [90].
- Boolean Models (BM): As the simplest form of logic-based models, Boolean models describe nodes (e.g., genes, proteins) as being in an ON (1) or OFF (0) state. They do not require detailed kinetic data, making them suitable for large systems. In systems medicine, this approach is often applied for cancer research to model signalling pathways [90] [34].
- Quantitative and Pharmacokinetic Models: These include Ordinary Differential Equation (ODE)-based models that quantitatively analyse the behaviour of biochemical reactions over time. A key application is Pharmacokinetic (PK) and Physiologically-Based PK (PBPK) modelling, which describes drug concentration in plasma or tissues to estimate on-target and off-target drug exposure and predict effect strength [90]. These can be personalized to represent specific patient cohorts [90].
Data-Driven Models for Knowledge Discovery
Data-driven concepts, such as machine learning (ML) and deep learning (DL), are fundamentally based on large datasets and aim for knowledge discovery through multidimensional regression analysis without necessarily requiring prior functional understanding [90] [91].
- Deep Learning for Diagnostics: Studies have demonstrated the potential of deep learning to match or exceed dermatologist-level accuracy in skin cancer classification [91]. Transfer learning, which uses pre-trained deep learning models, has shown high accuracy in automatically detecting and classifying brain tumors from MRI data [91].
- Machine Learning for Risk Stratification: ML algorithms can be applied to small, imbalanced datasets, such as those for chronic kidney disease (CKD), to enable early prediction. Techniques like the synthetic minority oversampling technique (SMOTE) and dynamic classifier selection can improve model performance on limited data [91].
- Spatial Eco-Structural Modelling: The integration of single-cell spatial multiomics data with machine learning allows for high-resolution mapping of tumour-immune-stromal interaction networks. For example, in endometrial cancer, this approach has identified CD90+CD105+ endothelial cells as key regulators of macrophage polarization and T-cell infiltration, enabling the construction of accurate recurrence prediction models [34].
Table 1: Comparison of Primary Computational Modeling Approaches
| Model Type | Key Objective | Data Requirements | Example Applications in Endometrial Cancer |
|---|---|---|---|
| Molecular Interaction Maps | Visualize static network properties and pathway knowledge | Network topology, expression data | Visualization of signalling pathways and dysregulated networks [90] |
| Boolean Models | Simulate system dynamics using logical rules | Network topology, qualitative states | Modelling of key signalling pathways driving tumour progression [90] |
| Quantitative (ODE) Models | Analyse quantitative dynamics of biochemical reactions | Detailed kinetic parameters, concentration data | Personalised simulation of drug response and biomarker discovery [90] |
| Pharmacokinetic (PBPK) Models | Predict drug disposition in different tissues/organs | Physiological parameters, drug properties | Personalising chemotherapy dosing based on patient physiology [90] |
| Spatial ML Models | Identify spatial cell patterns and predict clinical outcomes | Imaging Mass Cytometry (IMC) data, clinical outcomes | Predicting disease recurrence based on tumour microenvironment spatial structure [34] |
| Deep Transfer Learning | Automate detection and classification from images | Labelled image datasets (e.g., histology, MRI) | Classification of tumour subtypes from histopathological images [91] |
Experimental Protocols
Protocol for Spatial Ecostructural Modelling of Endometrial Cancer
This protocol details the procedure for using single-cell spatial analysis to model the tumour microenvironment and predict disease recurrence, based on the work by Wu et al. [34].
Background
This protocol enables the high-resolution mapping of tumour-immune-stromal interaction networks in endometrial cancer. It integrates single-cell spatial multiomics data to identify key cellular regulators of the tumour microenvironment and construct predictive models for molecular subtyping and recurrence risk [34].
Key features
- Identifies spatial distribution of immune and stromal cells.
- Quantifies intercellular crosstalk and signalling networks.
- Validates functional role of key cell clusters via flow cytometry.
- Constructs machine learning-based predictive models for clinical outcomes.
Materials and reagents
Table 2: Research Reagent Solutions for Spatial Ecostructural Modelling
| Item | Function | Specifications / Example |
|---|---|---|
| Antibody Panel for IMC | To label specific protein targets on tissue sections for imaging. | Metal-tagged antibodies against CD90, CD105, immune cell markers (CD3, CD8, CD68), tumour markers [34]. |
| Endometrial Cancer Tissue Microarray (TMA) | A platform containing tissue cores from multiple patients and molecular subtypes for parallel analysis. | TMA with cores from 40 endometrial cancer cases across four molecular subtypes [34]. |
| Cell Line or Primary Cells | For in vitro validation of identified cell clusters' functional roles. | Primary endothelial cells for flow cytometry validation [34]. |
Equipment
- Mass Cytometer with Imaging Capability (e.g., Hyperion Imaging System)
- Flow Cytometer
- Standard cell culture equipment
Software and datasets
- IMC image processing software (e.g., MCD Viewer, histoCAT)
- Statistical analysis software (e.g., R, Python with relevant ML libraries)
- Single-cell analysis pipelines
Procedure
- Sample Preparation: Section the endometrial cancer TMA slices to a specified thickness (e.g., 4 µm).
- Staining: Stain the tissue sections with the predefined panel of metal-tagged antibodies according to established IMC protocols.
- Data Acquisition: Acquire high-resolution images of the stained tissues using the imaging mass cytometer, collecting data on the spatial distribution and abundance of all labelled targets.
- Cell Segmentation and Phenotyping: Use computational tools to segment individual cells in the images and assign a phenotypic identity based on the antibody staining patterns.
- Spatial Analysis: Quantify the frequency, spatial distribution (e.g., proximity analyses), and intercellular crosstalk of distinct immune and stromal cell populations.
- Correlation with Clinical Data: Systematically correlate the spatial ecosystem-level features with clinical features and outcomes, including treatment response and survival.
- Functional Validation (Flow Cytometry): Isolate relevant cell populations (e.g., CD90+CD105+ endothelial cells) and use flow cytometry to validate their functional role in tumour subtype specification and microenvironmental remodelling.
- Predictive Model Building: Employ machine learning-based spatial phenotyping to construct molecular subtype-specific signatures and a recurrence prediction model for high-risk endometrial cancer.
Data analysis
- Spatial Statistics: Apply spatial statistics to identify significant co-localization or exclusion of cell types.
- Network Analysis: Construct and analyse cell-cell interaction networks to identify key regulators.
- Machine Learning: Use classifiers (e.g., random forest, support vector machines) with nested cross-validation to build and validate predictive models for recurrence based on the spatial features.
Validation of protocol
Provide evidence of the protocol's robustness by referencing specific data, such as:
- The predictive accuracy of the recurrence model (e.g., AUC, sensitivity, specificity) as reported in the original study [34].
- Validation data from flow cytometry confirming the immunomodulatory role of identified key cell clusters (e.g., CD90+ clusters in macrophage polarization) [34].
Protocol for Developing a PBPK Model for Personalized Dosing
This protocol outlines the steps for developing and individualizing a Physiologically-Based Pharmacokinetic (PBPK) model to guide personalized drug dosing in specific patient cohorts [90].
Background
PBPK modelling aims to reproduce the physiology of an organism at a high level of detail, explicitly representing different organs with specific properties (volumes, blood-flow rates) [90]. This allows for the integration of diverse patient-specific information to simulate drug pharmacokinetics and pharmacodynamics, guiding tailored treatments.
Key features
- Represents human physiology at a high level of granularity.
- Can be individualized using patient-specific physiological parameters.
- Supports the assessment of drug efficacy and safety in specific cohorts.
Materials and reagents
- Drug-Specific Parameters: A comprehensive set of drug-specific parameters (e.g., lipophilicity, plasma protein binding, metabolic clearance pathways).
- Physiological Database: Access to a database of human physiological parameters (e.g., organ volumes, blood flow rates, enzyme abundances) for the target population.
Software and datasets
- PBPK modelling and simulation software (e.g., GastroPlus, Simcyp Simulator, PK-Sim).
- Clinical PK data for model verification.
Procedure
- Base Model Construction: Develop a base reference PBPK model that represents an average individual from the population of interest, incorporating mean values of physiological parameters.
- Drug Model Incorporation: Integrate the drug-specific parameters into the base physiological model.
- Model Verification: Verify the model by comparing its simulations against observed clinical PK data from the literature or average study population data.
- Cohort Specification: Specify the model to represent a specific cohort of patients (e.g., elderly, obese, or patients with renal impairment) by adjusting the relevant physiological parameters in the base model [90].
- Model Validation: Validate the individualized model by comparing its predictions against observed clinical data from the specific patient cohort, if available.
- Simulation and Dosing Regimen Optimization: Use the validated, individualized model to simulate drug exposure in the target cohort and explore different dosing regimens to optimize therapeutic outcomes.
Data analysis
- Perform model qualification and validation by assessing the goodness-of-fit between simulated and observed concentration-time profiles.
- Use visual predictive checks and other quantitative methods to evaluate model performance.
Validation of protocol
Validation can be achieved by:
- Demonstrating that the base model adequately recapitulates observed PK data in a general population.
- Providing evidence that the cohort-specific model accurately predicts drug exposure in the target patient group (e.g., the elderly [90]).
Data Presentation
The presentation of quantitative results must be clear and concise, enabling easy comparison and interpretation. Tables should be self-explanatory and include necessary details such as the number of observations (N) and measures of variance or performance where applicable [92] [93].
Table 3: Performance Metrics of Different Machine Learning Models for a Hypothetical Endometrial Cancer Classification Task
| Model Algorithm | Accuracy (%) | Precision (%) | Recall (%) | F1-Score (%) | N |
|---|---|---|---|---|---|
| Random Forest | 92.5 | 93.1 | 91.8 | 92.4 | 150 |
| Support Vector Machine | 89.3 | 90.5 | 87.9 | 89.2 | 150 |
| Decision Tree | 85.7 | 86.2 | 84.5 | 85.3 | 150 |
| InceptionResNetV2 (TL) | 95.8 | 96.2 | 95.5 | 95.8 | 150 |
Note: This table exemplifies the presentation of model performance metrics. The specific results are for illustrative purposes. TL = Transfer Learning [91].
Visualization
Workflow for Spatial Ecostructural Modelling and Analysis
This diagram outlines the key steps in the protocol for spatial ecostructural modelling of endometrial cancer, from sample preparation to clinical prediction.
Key Signalling Pathway in Endometrial Cancer Microenvironment
This diagram schematically represents a simplified key signalling interaction identified through spatial ecostructural modelling, such as the role of CD90+ endothelial cells in macrophage polarization.
Conclusion
The integration of computational modeling with experimental biology is ushering in a new era for endometrial research. Foundational phenomenological and QSP models have successfully decoded the complex hormonal dialogue governing endometrial dynamics, while sophisticated applications in machine learning and spatial modeling are revolutionizing diagnostics and our understanding of disease ecosystems. The field is now adeptly tackling optimization and validation challenges through fractional calculus, optimal control theory, and the critical synergy with 3D organoid technology. Looking forward, the convergence of high-fidelity biological data from multi-omics and advanced imaging with increasingly powerful in silico models promises the development of true 'digital twins' of the endometrium. Future research must focus on standardizing validation frameworks across institutions, improving model interoperability, and initiating prospective clinical trials to firmly establish computational modeling as an indispensable tool for personalized risk prediction, therapeutic optimization, and ultimately, improved patient outcomes in endometrial cancer, endometriosis, and infertility.
References
- 1. Strategies for modelling endometrial diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10052865/]
- 2. A phenomenological-based model of the endometrial ... [https://www.sciencedirect.com/science/article/abs/pii/S0022519321003416]
- 3. Bioengineering approaches for the endometrial research ... [https://www.sciencedirect.com/science/article/pii/S2590006424001042]
- 4. An Update on Experimental Therapeutic Strategies for Thin ... [https://www.mdpi.com/2673-396X/4/4/48]
- 5. A comparative study of computational modeling ... [https://www.nature.com/articles/s41598-025-16866-w]
- 6. Induction of menstruation in mice reveals the regulation of ... [https://labs.sciety.org/articles/by?article_doi=10.1101/2025.10.08.681007]
- 7. Predicted peptide scaffolds for drug screening in ... [https://www.nature.com/articles/s41598-025-21282-1]
- 8. Endometrial Organoids and Their Role in Modeling Human ... [https://www.mdpi.com/2073-4409/14/11/829]
- 9. Dynamic changes in AI-based analysis of endometrial ... [https://www.sciencedirect.com/science/article/pii/S2153353924000038]
- 10. Computational Models for Diagnosing and Treating ... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2021.699133/full]
- 11. Reduced model for female endocrine dynamics [https://www.sciencedirect.com/science/article/abs/pii/S0025556423000202]
- 12. Mathematical model of optimal control for endometrial ... [https://www.nature.com/articles/s41598-025-23149-x]
- 13. Novel Regulatory Factors in the Hypothalamic-Pituitary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7672196/]
- 14. Computational Models for Diagnosing and Treating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580807/]
- 15. Integrated transcriptomic hypothalamic-pituitary-ovarian ... [https://www.sciencedirect.com/science/article/pii/S2405654524001483]
- 16. Computational Modeling Reveals Key Contributions of KCNQ ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0114034]
- 17. Comparing partial differential equations and agent-based ... [https://www.sciencedirect.com/science/article/abs/pii/S0377042725006971]
- 18. Integrating Mathematical Models in Clinical Oncology [https://www.scientificarchives.com/article/integrating-mathematical-models-in-clinical-oncology-enhancing-therapeutic-strategies]
- 19. On-Line Guide for Newcomers to ABM (Axelrod and Tesfatsion) [https://faculty.sites.iastate.edu/tesfatsi/archive/tesfatsi/abmread.htm]
- 20. Equation-Based Modeling vs. Agent ... [https://www.mdpi.com/2227-7390/11/1/253]
- 21. New Paper at AAMAS 2025: Scaling LLM-Guided Agent ... [https://www.media.mit.edu/posts/new-paper-on-limits-of-agency-at-aamas-2025/]
- 22. Universal differential equations as a unifying modeling ... [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2025.1677930/full]
- 23. Unlocking the Secrets of the Endometrium: Stem Cells, Niches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561017/]
- 24. and cytokine-dependent proliferation of endometrial cells ... [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.1101/2025.10.18.682837]
- 25. Spatial ecostructural modelling of endometrial cancer ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00724-6]
- 26. Machine learning algorithms as new screening approach for patients with endometriosis | Scientific Reports [https://www.nature.com/articles/s41598-021-04637-2]
- 27. Gradient Boosting Machine Learning Model for Defective Endometrial Receptivity Prediction by Macrophage-Endometrium Interaction Modules - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9120433/]
- 28. Mechanism-Based Pharmacodynamic Modeling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3684160/]
- 29. Mechanism-based pharmacokinetic-pharmacodynamic ... [https://www.sciencedirect.com/science/article/abs/pii/S0165614708000497]
- 30. Mechanism-based pharmacokinetic-pharmacodynamic ... [https://pubmed.ncbi.nlm.nih.gov/16132354/]
- 31. ACoP 2025 Insights: Scaling the Future of QSP Modeling ... [https://www.certara.com/blog/acop-2025-insights-scaling-the-future-of-qsp-modeling-with-certara-iq/]
- 32. The Impact of QSP Modeling on the Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12625082/]
- 33. SEOM-GEICO clinical guidelines on endometrial cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12630260/]
- 34. of Spatial identifies the... ecostructural modelling endometrial cancer [https://pubmed.ncbi.nlm.nih.gov/41243106/]
- 35. Updated Guidelines for the Diagnosis and Treatment of ... [https://www.mdpi.com/1718-7729/32/6/340]
- 36. Frontiers | Single-Cell Technologies and Spatial Transcriptomics... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1636483/abstract]
- 37. Challenges and opportunities for the next generation of ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003269]
- 38. Spatial computational modelling illuminates the role of ... [https://www.nature.com/articles/s41540-024-00419-4]
- 39. Deep Learning for Grading Endometrial Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11373039/]
- 40. Neighborhood clustering analysis to define epithelial– ... [https://www.sciencedirect.com/science/article/pii/S2153353925000513]
- 41. An interpretable hybrid deep learning framework for gastric ... [https://www.nature.com/articles/s41598-025-15702-5]
- 42. Deep learning based detection of endometriosis lesions in ... [https://www.sciencedirect.com/science/article/pii/S266652122500033X]
- 43. Integrating deep learning and clinical characteristics for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1600242/full]
- 44. The current landscape of artificial intelligence in ... [https://link.springer.com/article/10.1007/s12672-025-02212-z]
- 45. Methods to Develop an in silico Clinical Trial [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2021.741170/full]
- 46. Efficacy and mechanisms of Angelica sinensis in treating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12103411/]
- 47. Systems Pharmacology Model Predicts Zinc and Copper ... [https://www.medrxiv.org/content/10.1101/2025.10.06.25337149v1]
- 48. Epigallocatechin Gallate as a Potential Therapeutic Agent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12251065/]
- 49. Biomarkers and immunotherapy in endometrial cancer [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1684549/full]
- 50. Dual PI3K and HDAC inhibitor, CUDC-907, effectively ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531805/full]
- 51. Optimal Control Theory for Personalized Therapeutic ... [https://www.mdpi.com/2077-0383/9/5/1314]
- 52. Optimal Control in Combination Therapy for Heterogeneous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521341/]
- 53. Optimal control nodes in disease-perturbed networks as ... [https://www.nature.com/articles/s41467-019-10215-y]
- 54. Using particle swarm optimization and genetic algorithms for ... [https://www.semanticscholar.org/paper/93917230f21ce8e7137fc3304b68f77c0eacfc0d]
- 55. Application of Fractional Calculus as an Interdisciplinary ... [https://www.mdpi.com/2504-3110/9/10/663]
- 56. Fractional-order mathematical modeling and optimal ... [https://www.sciencedirect.com/science/article/pii/S2090447925004435]
- 57. 3D map-guided modeling of functional endometrial tissue ... [https://pubmed.ncbi.nlm.nih.gov/40894553/]
- 58. Iteration of Tumor Organoids in Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566727/]
- 59. Multidimensional trophoblast invasion assessment by ... [https://www.nature.com/articles/s41540-025-00589-9]
- 60. PharmaFormer predicts clinical drug responses through ... [https://www.nature.com/articles/s41698-025-01082-6]
- 61. Model Diagnostics: Overfitting & Robustness | by PiML Tutorials [https://piml.medium.com/model-diagnostics-overfitting-and-robustness-46f26367c8ad]
- 62. How to Avoid Overfitting in Machine Learning? [https://www.geeksforgeeks.org/machine-learning/how-to-avoid-overfitting-in-machine-learning/]
- 63. DCS-NET: a multi-task model for uterine ROI detection and ... [https://www.nature.com/articles/s41598-025-25004-5]
- 64. ECgMLP: A novel gated MLP model for enhanced ... [https://www.sciencedirect.com/science/article/pii/S2666990025000059]
- 65. Prevent overfitting and imbalanced data with Automated ML [https://learn.microsoft.com/en-us/azure/machine-learning/concept-manage-ml-pitfalls?view=azureml-api-2]
- 66. Development and Clinical Application of a Deep Learning ... [https://www.medrxiv.org/content/10.1101/2025.05.21.25327411v1]
- 67. Deep active optimization for complex systems [https://www.nature.com/articles/s43588-025-00858-x]
- 68. A Comparative Study of MRI and CT in Endometrial Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596896/]
- 69. Novel Monte Carlo approach quantifies data assemblage utility and... [https://www.nature.com/articles/srep15563?error=cookies_not_supported&code=16417890-1602-4019-bd9f-f914ca025eca]
- 70. Real-World Benchmarking and Validation of Foundation ... [https://www.medrxiv.org/content/10.1101/2025.10.10.25337691v1.full-text]
- 71. , histopathological, and Integrated analysis of... clinical molecular data [https://pubmed.ncbi.nlm.nih.gov/31420671/]
- 72. Development and validation of a prognostic model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599766/]
- 73. Clinical Application of an AI-Driven Framework for Accurate ... [https://www.sciencedirect.com/science/article/abs/pii/S0301562925003151]
- 74. Insights and limitations of endometrial cancer risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628995/]
- 75. The Evolving Role of Deep Learning in Image-Based ... [https://www.sciencedirect.com/science/article/pii/S2590005625001687]
- 76. and Mechanism Dual- Data Multimodal Deep Learning... driven [http://ijmmm.ustb.edu.cn/article/doi/10.1007/s12613-025-3198-3?viewType=citedby-info]
- 77. A molecular staging model for accurately dating the ... [https://www.nature.com/articles/s41467-023-41979-z]
- 78. Insights and limitations of endometrial cancer risk ... [https://pubmed.ncbi.nlm.nih.gov/41257634/]
- 79. TIME for Endometrial Cancer: Advancements and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616419/]
- 80. Jemperli ( dostarlimab ) plus chemotherapy approved in the US... | GSK [https://www.gsk.com/en-gb/media/press-releases/jemperli-plus-chemotherapy-approved-in-us-for-new-indication/]
- 81. Shows Response in Dostarlimab | Targeted... Endometrial Cancer [https://www.targetedonc.com/view/dostarlimab-shows-response-in-endometrial-cancer]
- 82. Mathematical model of optimal control for endometrial with... cancer [https://pubmed.ncbi.nlm.nih.gov/41219298/]
- 83. FDA grants accelerated approval to dostarlimab -gxly for dMMR... | FDA [https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-dostarlimab-gxly-dmmr-endometrial-cancer]
- 84. Unlocking the Secrets of the Endometrium: Stem Cells, ... [https://www.mdpi.com/2227-9059/13/10/2435]
- 85. Diagnosis Test Accuracy of Artificial Intelligence for ... [https://www.jmir.org/2025/1/e66530]
- 86. Clinical-grade AI model for molecular subtyping of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597869/]
- 87. Deep Learning for Grading Endometrial Cancer [https://www.sciencedirect.com/science/article/pii/S0002944024002025]
- 88. Preoperative prediction of aggressive endometrial cancer ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1694223/full]
- 89. Computational image and molecular analysis reveal ... [https://www.nature.com/articles/s41698-025-00972-z]
- 90. Computational Models for Clinical Applications in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8879572/]
- 91. Exploring Computational Methods to Advance Clinical ... [https://www.mdpi.com/2076-3417/15/10/5636]
- 92. Presenting data in tables and charts - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4008059/]
- 93. Presenting the Results of Quantitative Analysis [https://pressbooks.ric.edu/socialdataanalysis/chapter/writing-about-quantitative-data/]