Decoding the Uncertain: A Comprehensive Guide to VUS Interpretation in Premature Ovarian Insufficiency for Researchers and Drug Developers
This article provides a comprehensive resource for researchers and drug development professionals tackling the challenge of Variants of Uncertain Significance (VUS) in Premature Ovarian Insufficiency (POI).
Decoding the Uncertain: A Comprehensive Guide to VUS Interpretation in Premature Ovarian Insufficiency for Researchers and Drug Developers
Abstract
This article provides a comprehensive resource for researchers and drug development professionals tackling the challenge of Variants of Uncertain Significance (VUS) in Premature Ovarian Insufficiency (POI). It covers the foundational genetic landscape of POI, detailing the over 90 associated genes and the high prevalence of VUS findings. The content explores established and emerging methodologies for VUS interpretation, including ACMG/AMP guidelines, functional assays, and advanced computational tools. It addresses critical troubleshooting strategies to optimize classification and minimize clinical ambiguity, and finally, outlines rigorous frameworks for the clinical and functional validation of POI-associated VUS, emphasizing their potential in therapeutic target discovery.
The Genetic Landscape of POI and the Scale of the VUS Challenge
Defining POI and the Critical Role of Genetic Etiology
FAQs on POI and Genetic Research
1. What is Premature Ovarian Insufficiency (POI) and how is it diagnosed?
Premature Ovarian Insufficiency (POI) is a clinical condition characterized by the loss of ovarian function before the age of 40 [1] [2]. It is diagnosed based on the following criteria, which align with guidelines from the European Society of Human Reproduction and Embryology (ESHRE) [3] [4]:
- Oligomenorrhea or amenorrhea for at least 4 months.
- Elevated follicle-stimulating hormone (FSH) level (>25 IU/L) on two occasions, more than 4 weeks apart [5] [2].
It is crucial to exclude other causes, such as chromosomal abnormalities, autoimmune diseases, or iatrogenic causes like chemotherapy and radiation [1] [3]. POI is distinct from menopause because ovarian function can be intermittent, and spontaneous ovulation and pregnancy, though rare, are still possible [1] [6].
2. Why is understanding genetic etiology critical in POI research?
A genetic etiology is a major contributing factor in a significant proportion of POI cases. Understanding it is vital for several reasons:
- High Prevalence of Unknown Etiology: In approximately 90% of diagnosed spontaneous POI cases, the underlying cause is unknown [1] [7]. Genetic research aims to solve these idiopathic cases.
- Establishing a Molecular Diagnosis: Identifying a pathogenic variant provides a definitive diagnosis for patients and families, ending a long and uncertain diagnostic odyssey [3].
- Informing Clinical Management: A genetic diagnosis can help assess associated health risks (e.g., for Fragile X premutation or Turner syndrome), guide reproductive planning, and enable cascade testing for relatives [3] [8].
- Elucidating Pathogenic Mechanisms: Discovering novel genes and variants expands our understanding of the fundamental biological processes governing ovarian development and function, including gonadogenesis, meiosis, and folliculogenesis [3].
3. What is a Variant of Uncertain Significance (VUS) and how should it be interpreted?
A Variant of Uncertain Significance (VUS) is a genetic variant for which there is currently insufficient evidence to classify it as either pathogenic or benign [9] [8] [10]. Interpretation guidelines are as follows:
- Not Clinically Actionable: A VUS should not be used for clinical decision-making regarding patient management or reproductive choices [9] [8] [10]. Clinical decisions must be based on personal and family history.
- A Spectrum of Suspicion: The VUS category is heterogeneous. Variants can be subjectively categorized on a "temperature" scale from "ice cold" (more likely benign) to "hot" (more likely pathogenic) based on available evidence [9] [10].
- Dynamic Classification: The classification of a VUS can change over time as more evidence accumulates from population databases, functional studies, and published case reports [9] [8]. Most VUSs are eventually reclassified as benign [9].
4. What experimental approaches can help clarify the role of a VUS in POI?
When a VUS is identified in a candidate gene, several experimental strategies can be employed to gather additional evidence:
- Family Segregation Studies: Testing parents and other affected or unaffected family members to see if the variant co-segregates with the disease phenotype. A de novo (new) variant in an affected child or inheritance from an affected parent can support pathogenicity [9] [8] [10].
- Functional Studies (In Vitro or In Vivo): Performing experiments to assess the biological impact of the variant on protein function, such as enzyme activity, protein expression, or subcellular localization. Providing functional evidence (PS3 code per ACMG guidelines) is a powerful method to upgrade a VUS to "Likely Pathogenic" [3] [8].
- Review of Updated Population Data: Periodically re-checking the variant's frequency in large, diverse population databases like gnomAD. A high frequency in healthy populations argues against pathogenicity [9].
- Consultation with a Genetics Professional: An abbreviated or e-consult with a clinical geneticist or molecular geneticist can help triage VUSs and determine the most appropriate next steps [9].
Genetic Landscape of POI: Key Data
Table 1: Summary of Genetic Findings from a Large-Scale POI WES Study (n=1,030) [3]
| Genetic Finding | Number of Cases | Contribution to Cohort | Notes |
|---|---|---|---|
| P/LP in Known Genes | 193 | 18.7% | Spanning 59 known POI-causative genes |
| Monoallelic Variants | 155 | 15.0% | Single heterozygous P/LP variants |
| Biallelic Variants | 24 | 2.3% | P/LP variants in both copies of a gene |
| Multiple Variants (Multi-het) | 14 | 1.4% | P/LP variants in different genes in one individual |
| Primary Amenorrhea (PA) | |||
| 31 / 120 | 25.8% | Higher frequency of biallelic/multi-het variants | |
| Secondary Amenorrhea (SA) | |||
| 162 / 910 | 17.8% | Mostly monoallelic variants |
Table 2: Categorization of Genes Implicated in POI Pathogenesis [1] [3]
| Functional Category | Example Genes | Primary Role in Ovarian Function |
|---|---|---|
| Meiosis & DNA Repair | HFM1, MSH4, SPIDR, MCM8, MCM9, BRCA2 |
Homologous recombination, DNA double-strand break repair, meiotic progression |
| Folliculogenesis & Ovulation | GDF9, BMP15, NR5A1, FOXL2 |
Follicle development, growth, and maturation; steroidogenesis |
| Gonadogenesis | NR5A1 |
Early ovarian development and formation |
| Metabolic & Mitochondrial | EIF2B2, POLG, ACAD9 |
Cellular energy production, metabolism, and overall oocyte health |
| Autoimmune Regulation | AIRE |
Immune system tolerance, prevention of autoimmune oophoritis |
| Chromosomal & Syndromic | FMR1 (premutation) |
RNA toxicity leading to accelerated follicle depletion |
Essential Experimental Protocols for Genetic POI Research
Whole-Exome Sequencing (WES) for Variant Discovery
Objective: To identify rare coding variants associated with POI in a hypothesis-free manner [3] [4].
Methodology:
- Sample Preparation: Extract genomic DNA from peripheral blood of well-phenotyped POI patients and select controls. Ensure informed consent and IRB approval [4].
- Library Preparation & Enrichment: Fragment DNA and prepare sequencing libraries using a kit (e.g., Agilent SureSelect). Hybridize and capture the exonic regions [4].
- Sequencing: Perform high-throughput sequencing on a platform such as Illumina HiSeq2000 to achieve sufficient coverage (e.g., >50x) [4].
- Bioinformatic Analysis:
- Variant Calling: Map sequence reads to a reference genome (e.g., GRCh38) and call variants (SNVs, indels).
- Variant Filtering: Filter against population frequency databases (e.g., gnomAD, 1000 Genomes) to remove common variants (MAF > 0.01). Prioritize rare, protein-altering variants (nonsense, frameshift, splice-site, missense) [3] [4].
- Variant Annotation & Prioritization: Use tools like CADD and PolyPhen-2 to predict pathogenicity. Cross-reference with known POI gene panels and perform case-control burden analysis to identify genes with a significant excess of LoF variants [3].
Functional Validation of a VUS via Segregation Analysis
Objective: To determine if a VUS co-segregates with the POI phenotype within a family, providing evidence for or against its pathogenicity [9] [8].
Methodology:
- Family Member Recruitment: Identify and recruit available first- and second-degree relatives of the proband, including both affected and unaffected individuals.
- Genotyping: Perform Sanger sequencing or targeted genotyping for the specific VUS in all recruited family members.
- Segregation Analysis:
- For an Autosomal Dominant Model: The variant should be present in all affected family members and absent in unaffected ones. Penetrance may be incomplete.
- For an Autosomal Recessive Model: The proband should have biallelic variants. Parents are typically heterozygous carriers.
- De novo status, where the variant is present in the proband but absent in both parents, provides strong evidence for pathogenicity [9] [8] [10].
- Interpretation: Consistent co-segregation supports a upgrade of the VUS to "Likely Pathogenic," while finding the variant in a clearly unaffected adult relative makes pathogenicity less likely [9].
Research Reagent Solutions
Table 3: Essential Materials for Genetic POI Research
| Reagent / Material | Function / Application | Example / Note |
|---|---|---|
| Agilent SureSelect Kit | Target enrichment for whole-exome sequencing | Captures exonic regions from genomic DNA libraries [4] |
| Illumina Sequencing Platform | High-throughput DNA sequencing | Platforms like HiSeq2000 generate short-read sequence data [4] |
| Sanger Sequencing Reagents | Validation and segregation studies | Confirms variants identified by NGS in proband and family members [4] |
| gnomAD Database | Population frequency filtering | Critical for filtering out common polymorphisms [3] [4] |
| CADD & PolyPhen-2 | In silico pathogenicity prediction | Computational tools to prioritize damaging missense variants [3] [4] |
| ACMG/AMP Guidelines | Variant classification framework | Standardized criteria for classifying variants as P, LP, VUS, LB, or B [9] [3] |
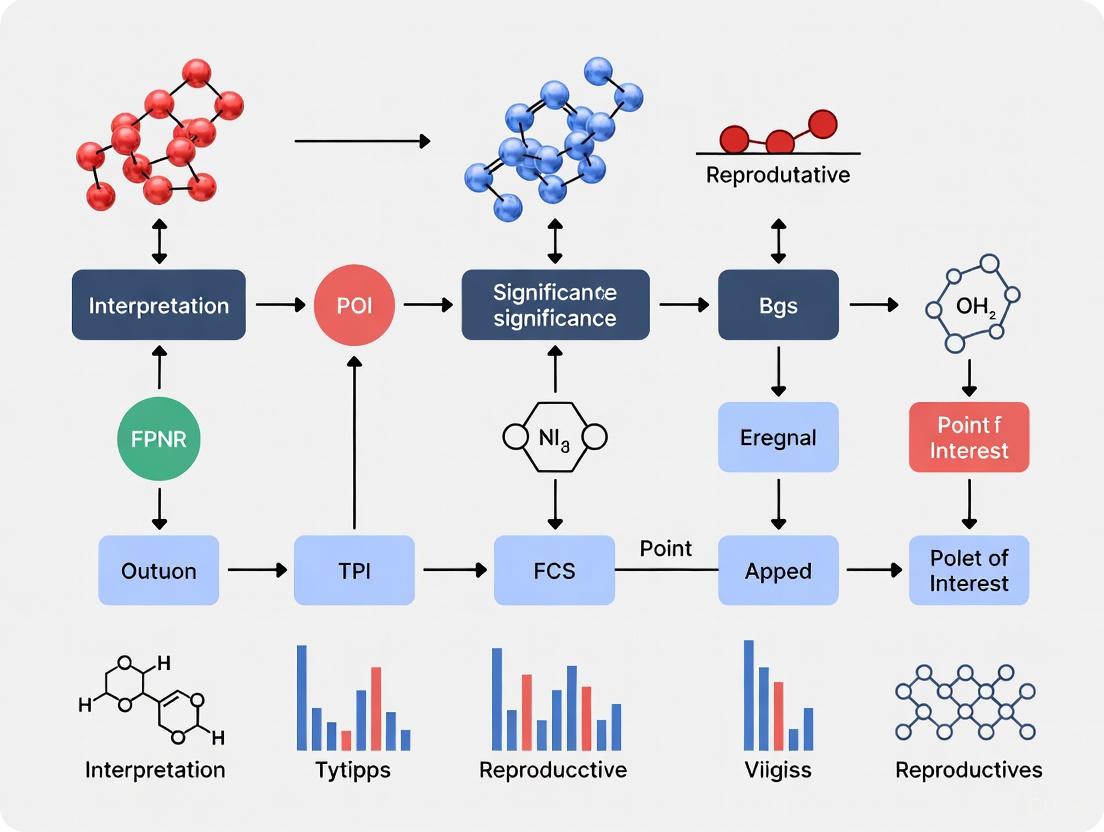
Workflow Diagram: From Patient to VUS Interpretation
The diagram below outlines the logical workflow for genetic analysis and VUS interpretation in POI research.
FAQs: Genetic Architecture of POI
Q1: What is the estimated genetic contribution to Premature Ovarian Insufficiency (POI)? Genetic factors play a pivotal role in POI, contributing to approximately 20-25% of diagnosed cases [11]. A large-scale whole-exome sequencing study of 1,030 patients identified pathogenic or likely pathogenic variants in known POI-causative genes in 18.7% of cases, with an additional 4.8% attributed to novel candidate genes, bringing the total genetic contribution to 23.5% [12]. The genetic contribution is significantly higher in patients with primary amenorrhea (25.8%) compared to those with secondary amenorrhea (17.8%) [12].
Q2: How are POI-associated genes functionally categorized? POI-associated genes can be systematically classified based on their biological roles in ovarian development and function. The main categories and their representative genes are summarized in the table below [11] [12] [13]:
Table: Functional Classification of POI-Associated Genes
| Functional Category | Biological Process | Key Representative Genes |
|---|---|---|
| Meiosis & DNA Repair | Homologous recombination, DNA damage repair, meiotic nuclear division | HFM1, SPIDR, BRCA2, MCM8, MCM9, MSH4, SHOC1, SLX4 |
| Ovarian & Follicular Development | Gonadogenesis, folliculogenesis, follicle activation | NOBOX, FIGLA, NR5A1, BMP15, GDF9, FOXL2 |
| Metabolic Pathways | Glycosylation, galactose metabolism | GALT, PMM2 |
| Mitochondrial Function | Mitochondrial metabolism, oxidative phosphorylation | AARS2, CLPP, POLG, TWNK, HADHB, CPT1A |
| Autoimmune Regulation | Immune tolerance, endocrine autoimmunity | AIRE |
| Chromosomal & Syndromic | X-chromosome related, syndromic forms | FMR1 (premutation), Turner Syndrome (45,X) |
Q3: What is the role of mitochondrial genes in POI pathogenesis? Mitochondrial dysfunction is a significant contributor to POI, affecting multiple aspects of ovarian function. Mitochondrial genes play crucial roles in meeting the energy demands of oogenesis and follicle maturation and are also involved in follicular atresia [14]. Key mechanisms include:
- Impaired Mitochondrial Dynamics: Deletion of mitochondrial fusion gene
Mfn2in oocytes leads to impaired oocyte maturation and follicle development, while targeted deletion of the fission geneDrp1reduces oocyte quality [14]. - Metabolic Dysregulation: Recent bioinformatic studies identified 119 mitochondria-related differentially expressed genes (MitoDEGs) in POI, including
Hadhb,Cpt1a,Mrpl12, andMrps7, which were validated in POI models and human granulosa cells [14]. - Oxidative Stress & Apoptosis: Mitochondrial dysfunction contributes to changes in metabolic pathways, triggering inflammatory responses, disrupting reactive oxygen species (ROS) homeostasis, and inducing cell apoptosis, ultimately leading to POI development [14].
Troubleshooting Genetic Experiments in POI Research
Challenge: Interpreting Variants of Uncertain Significance (VUS) in POI Genes
Problem: A VUS is identified in a known POI gene during genetic testing, and its clinical significance cannot be determined.
Solution: Implement a multi-step validation protocol to assess VUS pathogenicity.
Table: Research Reagent Solutions for VUS Interpretation
| Research Reagent | Specific Function/Application | Example Use Case in POI |
|---|---|---|
| Agilent SureSelect Human All Exon V6 kit [15] | Whole exome sequencing library construction | Comprehensive variant detection in POI patient cohort |
| SurePrint G3 Human CGH Microarray 4×180 K [16] | Copy Number Variation (CNV) identification | Detection of chromosomal structural abnormalities |
| Custom Capture Design (163 genes) [16] | Targeted NGS of ovarian function-related genes | Focused screening of known and candidate POI genes |
| AlphaFold-predicted model & DynaMut2 [15] | Protein structure prediction and stability analysis | Assessing structural impact of CHEK1 A26G variant |
| DESeq2 R Package [15] | Differential gene expression analysis from RNA-Seq | Identifying mis-regulated pathways in mutant cells |
| rMATS software [15] | Alternative splicing event analysis | Detecting aberrant splicing due to genetic variants |
Experimental Protocol: Functional Validation of VUS
Step 1: Computational Pathogenicity Prediction
- Utilize in silico tools (MutationTaster, PANTHER, PolyPhen-2) for initial pathogenicity assessment [15].
- Perform protein structural analysis using AlphaFold-predicted models and stability change prediction with DynaMut2 (e.g., ΔΔG value of -0.98 kcal/mol for CHEK1 A26G suggests destabilizing effect) [15].
Step 2: In Vitro Functional Studies
- Clone the wild-type and mutant (VUS) allele into mammalian expression vectors with appropriate tags (e.g., HA tags for detection) [15].
- Transfert constructs into suitable cell lines (e.g., 293FT cells for high transfection efficiency) and confirm protein expression and localization via immunofluorescence and Western blotting [15].
- Compare protein expression levels between wild-type and mutant (relative to GAPDH) to assess stability effects [15].
Step 3: Transcriptomic Analysis
- Perform RNA sequencing on cells expressing wild-type versus mutant protein.
- Identify differentially expressed genes (DEGs) using DESeq2 package (p-value <0.05, FDR <0.05) [15].
- Analyze alternative splicing events using rMATS software (FDR <0.05, inclusion-level difference >5%) [15].
- Conduct pathway enrichment analysis (e.g., GO, KEGG) to identify affected biological processes.
VUS Interpretation Workflow
Challenge: Low Diagnostic Yield in POI Genetic Testing
Problem: Despite comprehensive testing, a significant proportion of POI cases (approximately 70-80%) remain without a definitive genetic diagnosis.
Solution: Implement a multi-modal genetic testing approach.
Experimental Protocol: Comprehensive Genetic Screening for POI
Step 1: Chromosomal and FMR1 Analysis
- Perform standard karyotyping to identify X-chromosome abnormalities (e.g., Turner Syndrome, Trisomy X) which account for 4-12% of POI cases [11] [16].
- Conduct FMR1 premutation testing for CGG repeat expansions, a common genetic cause of POI [16].
Step 2: Copy Number Variation (CNV) Analysis
- Utilize array Comparative Genomic Hybridization (aCGH) with platforms such as SurePrint G3 Human CGH Microarray 4×180K [16].
- Analyze CNVs with minimum resolution of 60 kb along the genome, focusing on known POI critical regions (Xq13.1-Xq21.33 and Xq24-Xq27) [11] [16].
Step 3: Next-Generation Sequencing
- Employ whole-exome sequencing (WES) using capture kits (e.g., Agilent SureSelect) for comprehensive variant detection [12] [15].
- Alternatively, use targeted NGS panels covering known and candidate POI genes (e.g., 163-gene custom capture design) [16].
- Implement rigorous variant filtering: exclude common variants (MAF >0.01 in gnomAD or control databases), focus on loss-of-function and predicted damaging missense variants [12].
Step 4: Data Integration and Analysis
- Integrate findings from multiple genetic tests to identify compound heterozygous or oligogenic contributions.
- Correlate genetic findings with clinical presentation (primary vs. secondary amenorrhea), as genetic contribution differs significantly between these groups [12].
Advanced Research Methodologies
Integrative Bioinformatics Approach for Mitochondrial-Immune Interactions
Background: Mitochondrial dysfunction and immune dysregulation are interconnected in POI pathogenesis, but their interplay remains poorly understood [14].
Experimental Protocol: Identifying Mitochondrial-Related Gene Signatures
Step 1: Data Acquisition and Preprocessing
- Obtain transcriptomic data from public repositories (NCBI GEO: GSE128240, GSE233743, GSE39501) [14].
- Preprocess expression values using R package "limma" [14].
- Analyze single-cell RNA sequencing data (e.g., GSE200612) to elucidate cell-type specific expression [14].
Step 2: Identification of Mitochondria-Related Differentially Expressed Genes (MitoDEGs)
- Identify DEGs between normal and POI ovarian tissues (p <0.05, |logFC| >1) using "limma" package [14].
- Cross-reference DEGs with mitochondrial gene catalog (MitoCarta 3.0, 1140 genes) to identify MitoDEGs [14].
- Perform functional enrichment analysis (GSEA, GO, KEGG) using "clusterProfiler" package [14].
Step 3: Protein-Protein Interaction and Hub Gene Identification
- Construct PPI networks using STRING database [14].
- Identify hub genes using CytoHubba and MCODE plugins in Cytoscape [14].
- Validate hub genes (e.g.,
Hadhb,Cpt1a,Mrpl12,Mrps7) in POI models and human granulosa cells using RT-qPCR and Western blot [14].
Step 4: Immune Infiltration and Correlation Analysis
- Analyze immune cell infiltration using bioinformatic tools (e.g., Rank-In) [14].
- Perform correlation analysis between hub-MitoDEGs and immune-related genes/cells [14].
- Identify potential therapeutic agents using cMap database [14].
Mitochondrial Bioinformatic Analysis Pipeline
Research Recommendations and Future Directions
Enhancing VUS Interpretation: Develop POI-specific functional assays to characterize VUS in genes involved in key biological processes like meiosis (HFM1, MCM8, MCM9), mitochondrial function (TWNK, CPT1A), and folliculogenesis (NOBOX, FIGLA) [11] [12] [15].
Exploring Oligogenic Inheritance: Investigate potential oligogenic contributions to POI, where combinations of variants in multiple genes may collectively contribute to the phenotype, potentially explaining cases where single-gene variants show incomplete penetrance [13].
Standardizing Genetic Testing Protocols: Establish consensus guidelines for comprehensive POI genetic testing that includes chromosomal analysis, FMR1 testing, CNV detection, and next-generation sequencing to maximize diagnostic yield [16] [12].
Integrating Multi-Omics Data: Combine genomic data with transcriptomic, epigenomic, and proteomic profiles to identify novel regulatory mechanisms and biomarkers for POI, particularly focusing on mitochondrial-immune interactions [14].
Definition and Core Concepts
What is a Variant of Uncertain Significance (VUS)?
A Variant of Uncertain Significance (VUS) is a genetic variant that has been identified through genetic testing but whose significance to the function or health of an organism is not known [17]. In clinical practice, the term "variant" is favored over "mutation" as it describes an allele without inherently connoting pathogenicity [17].
The interpretation of DNA variants is fundamental to personalized medicine, enabling precise diagnosis and treatment selection [18]. The American College of Medical Genetics and Genomics (ACMG), the Association for Molecular Pathology (AMP), and the College of American Pathologists (CAP) have established a standardized five-tier system for classifying variants [19] [17]:
- Pathogenic (P): Well-documented to cause disease, meeting stringent criteria such as evidence from well-established functional studies or identification in multiple unrelated individuals with the disease [17].
- Likely Pathogenic (LP): Strong evidence of being disease-causing but lacking definitive proof, indicating greater than 90% certainty of being pathogenic [19] [17].
- Variant of Uncertain Significance (VUS): Unknown or conflicting clinical significance; insufficient evidence to determine if the variant is disease-causing [19] [17].
- Likely Benign (LB): Unlikely to be causative of disease, with more than 90% certainty that the variant is not causative for a disease [17].
- Benign (B): Not disease-causing, usually observed at high frequencies in population databases with strong evidence against pathogenic effect [17].
Figure 1: Variant Classification Workflow Following ACMG/AMP Guidelines
Current Landscape and Quantitative Data
The Burden of VUS in Clinical Practice
Variants of Uncertain Significance represent a significant challenge in genomic medicine. More than 70% of all unique variants in the ClinVar database are labeled as VUS [20]. The rate of VUS identification has grown over time with the increased adoption of genetic testing [20].
Table 1: VUS Reclassification Rates Across Studies
| Study Focus | Sample Size | Reclassification Rate | Key Findings |
|---|---|---|---|
| Multicenter Cancer Study [21] | 2,715 individuals with 3,261 VUS | 8.1% overall | 11.3% of reclassified VUS resulted in clinically actionable findings; 4.6% subsequently changed clinical management |
| Tumor Suppressor Genes [22] | 128 unique VUS | 31.4% reclassified as likely pathogenic using new ClinGen criteria | Highest reclassification rate in STK11 (88.9%) |
| Multi-Institutional Real-World Evidence [23] | VUS across 20 hereditary cancer and cardiovascular genes | 32% of VUS carriers | 99.7% reclassified to Benign/Likely Benign; 0.3% to Pathogenic/Likely Pathogenic |
Racial and ethnic disparities exist in VUS reclassification. A multicenter study found that compared to their prevalence in the overall sample, reclassification rates for Black individuals were higher (13.6% vs. 19.0%), whereas the rates for Asian individuals were lower (6.3% vs. 3.5%) [21].
The two-year prevalence of VUS reclassification remained steady between 2014 and 2019, suggesting consistent reinterpretation efforts over time [21].
Methodologies and Experimental Approaches
Variant Reclassification Frameworks
Several advanced methodologies have been developed to improve VUS reinterpretation:
Real-World Evidence (RWE) Approach A novel RWE approach integrates de-identified, longitudinal clinical data with variant carriers and non-carriers identified from exome or genome sequence data across large-scale clinicogenomic datasets [23]. This method enables rigorous variant-specific case-control analyses from population data by:
- Compiling phenotypes for established gene-level disease associations from longitudinal medical records
- Applying statistically robust case-control analyses
- Systematically applying RWE to all variants, including previously identified VUS in clinically relevant genes
New ClinGen PP1/PP4 Criteria Recent Clinical Genome Resource (ClinGen) guidance focuses on cosegregation (PP1) and phenotype-specificity criteria (PP4) based on the observation that phenotype specificity could provide a greater level of pathogenicity evidence [22]. This point-based system assigns:
- Pathogenic evidence: 1 (supporting), 2 (moderate), 4 (strong), and 8 (very strong) points
- Benign evidence: -1 (supporting), -2 (moderate), and -4 (strong) points
- Classification thresholds: ≥10 (pathogenic), 6–9 (likely pathogenic), 0–5 (VUS), -1 to -6 (likely benign), ≤-6 (benign)
Figure 2: Advanced VUS Reclassification Methodologies
Non-Coding Variant Interpretation
Most clinical genetic testing has traditionally focused on protein-coding regions, but non-coding variants play an increasingly recognized role in penetrant disease [24]. Key considerations for non-coding variants include:
- Defining candidate regulatory elements: promoters, enhancers, repressors, splice regions, untranslated regions (UTRs)
- Understanding mechanisms: effects on splicing, transcription, translation, RNA processing and stability, chromatin interactions
- Adapting ACMG/AMP guidelines for non-coding contexts, as current guidelines primarily address protein-coding variants [24]
Non-coding region variants are significantly under-ascertained in clinical variant databases because these regions are often excluded from capture regions or removed during bioinformatic processing [24].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for VUS Interpretation Research
| Resource Category | Specific Tools/Databases | Primary Function |
|---|---|---|
| Variant Databases | ClinVar, dbSNP, dbVar, gnomAD | Repository for clinically significant variants and population frequencies |
| In Silico Predictors | REVEL, SpliceAI, CADD, SIFT, GERP | Computational prediction of variant impact using AI and statistical methods |
| Automated Interpretation Tools | PathoMAN, VIP-HL | Automate evaluation of ACMG/AMP guideline criteria by integrating diverse data sources |
| Functional Assays | Multiplexed functional assays [20] | High-throughput experimental assessment of variant impact |
| Clinico-Genomic Datasets | Helix Research Network, UK Biobank, All of Us | Large-scale datasets linking genomic and clinical data for RWE approaches |
| Stipuleanoside R2 | Stipuleanoside R2, CAS:96627-72-4, MF:C53H84O23, MW:1089.2 g/mol | Chemical Reagent |
| D-Biotinol | D-Biotinol, CAS:53906-36-8, MF:C10H18N2O2S, MW:230.33 g/mol | Chemical Reagent |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q: What should I do when a VUS is identified in a patient with a strong personal and family history of disease?
A: First, ensure comprehensive phenotyping and detailed family history collection. Consider implementing the new ClinGen PP1/PP4 criteria, which assign higher weight to phenotype specificity [22]. For genes with high locus homogeneity (where only one gene explains the phenotype), this approach can assign up to five points solely from phenotype specificity criteria. Additionally, explore functional assays to gather additional evidence of pathogenicity [20].
Q: How can we reduce the high rate of VUS in clinical testing?
A: Implement systematic approaches including:
- Leverage large-scale real-world evidence: Integrating RWE from clinicogenomic datasets is projected to resolve over 50% of VUS carriers once longitudinal databases are available for approximately 3 million individuals [23].
- Apply updated classification criteria: Use disease-specific guidelines like the new ClinGen PP1/PP4 criteria, which significantly improve reclassification rates for tumor suppressor genes [22].
- Utilize automated interpretation tools: These can help standardize variant assessment, though expert oversight remains crucial, particularly for VUS interpretation [18].
Q: What are the best practices for handling VUS in non-coding regions?
A: For non-coding variants:
- Define regulatory elements relevant to your gene of interest, including promoters, enhancers, and untranslated regions [24].
- Use specialized prediction tools for non-coding variant impact assessment.
- Consider experimental validation of regulatory function when possible.
- Consult emerging guidelines for adapting ACMG/AMP criteria to non-coding regions [24].
Q: How reliable are automated variant interpretation tools for VUS classification?
A: Automated tools demonstrate high accuracy for clearly pathogenic/benign variants but show significant limitations with VUS [18]. While these tools enhance efficiency by automating evidence collection and criteria evaluation, expert oversight is still needed in clinical contexts, particularly for VUS interpretation [18]. Tools vary in their automation approaches, data sources, and criteria implementation, so careful selection and validation are essential.
Q: What is the typical timeframe for VUS reclassification, and how can we facilitate this process?
A: Reclassification timeframes vary significantly. One study found the two-year prevalence of VUS reclassification remained steady between 2014 and 2019 [21]. To facilitate reclassification:
- Participate in data sharing initiatives such as ClinVar to contribute to community knowledge [20].
- Establish laboratory protocols for periodic variant reassessment (e.g., every three years) [22].
- Implement systems to efficiently return reinterpreted genetic test results to patients and providers [21].
- Utilize updated classification criteria as they become available to maximize current knowledge application [22].
Table 1: Reported Prevalence of VUS and Pathogenic Variants in POI Cohort Studies
| Study Cohort Size | Total Cases with P/LP/VUS | Pathogenic/Likely Pathogenic (P/LP) Variants | Variants of Uncertain Significance (VUS) | Key Findings | Citation |
|---|---|---|---|---|---|
| 28 patients | 16/28 (57.1%) | 9/28 (32.1%) causal SNVs/CNVs | 7/28 (25.0%) | First study combining array-CGH and NGS in same POI cohort. | [16] |
| 68 Turkish patients | 4/68 (5.9%) | 1 likely pathogenic variant | 3 VUS in NOBOX, GDF9, STAG3 | First genetic epidemiology study in Türkiye with a 26-gene panel. | [25] |
| 1,030 patients | 193/1030 (18.7%) with P/LP | 195 P/LP variants in 59 genes | 75 VUS functionally evaluated (55 confirmed deleterious) | Large-scale WES study; 38 VUS were upgraded to LP after functional assays. | [26] |
| 500 Chinese patients | 72/500 (14.4%) with P/LP | 61 P/LP variants in 19 genes | Not explicitly quantified | 58/61 (95.1%) of the identified P/LP variants were novel. | [27] |
| 151 Belgian patients | 2/151 (1.3%) with NOBOX variants | 1 pathogenic variant | 1 VUS in NOBOX (c.259C>A) | Highlights discordance between ACMG classification and in vitro functional data. | [28] |
Experimental Protocols for VUS Interpretation
Protocol: Comprehensive Genetic Screening Workflow for POI
Objective: To identify and classify genetic variants, including VUS, in patients with idiopathic Premature Ovarian Insufficiency.
Materials:
- DNA extracted from patient peripheral blood samples.
- Array-CGH platform (e.g., Agilent SurePrint G3 Human CGH Microarray 4x180 K).
- Next-Generation Sequencing platform (e.g., Illumina NextSeq 550).
- Custom-designed gene panels or whole-exome capture kits.
- Bioinformatics analysis software (e.g., Alissa Align&Call, CytoGenomics).
Procedure:
- Patient Selection & DNA Extraction: Select patients meeting diagnostic criteria for POI (amenorrhea for >4 months before age 40 and elevated FSH >25 IU/L). Exclude other known causes (karyotype abnormalities, FMR1 premutation, autoimmune, or iatrogenic causes). Extract high-quality DNA [16].
- Copy Number Variation (CNV) Analysis:
- Perform array-CGH following manufacturer's protocols.
- Use bioinformatics software to identify CNVs with a minimum resolution of 60 kb.
- Annotate identified CNVs using databases like DECIPHER and ClinGen [16].
- Sequencing Analysis (Targeted Panel or WES):
- Variant Filtering and Annotation:
- Variant Classification:
- Functional Validation (For VUS Upgrade):
- For a subset of VUS, particularly in key biological pathways, proceed with functional assays.
- Example: For VUS in the FSHR gene, use cell culture models transfected with wild-type and mutant plasmids. Assess cell surface expression of the receptor and measure downstream signaling (e.g., cAMP production) in response to FSH stimulation [29].
Figure 1: Genetic Screening and VUS Interpretation Workflow for POI.
Protocol: Functional Assay for VUS in the FSHR Gene
Objective: To determine the functional impact of a VUS in the Follicle-Stimulating Hormone Receptor (FSHR) gene on receptor expression and signaling.
Materials:
- Plasmids containing the common (wild-type) FSHR allele and plasmids with the VUS.
- Cell line suitable for transfection (e.g., HEK293).
- FSH hormone.
- Antibodies for FSHR detection (for surface expression).
- cAMP assay kit (e.g., competitive ELISA or HTRF).
Procedure:
- Cell Transfection: Transfect cells with separate plasmids: wild-type FSHR, each VUS individually, both VUS together (in trans), and an empty vector control [29].
- Cell Surface Expression Analysis:
- Measure the cell surface expression of FSHR using a technique like flow cytometry or immunofluorescence with FSHR-specific antibodies.
- Compare the expression level of the VUS-containing receptors to the wild-type receptor. A marked reduction (e.g., up to 93% as reported) supports a deleterious effect [29].
- cAMP Production Assay:
- Stimulate transfected cells with a saturating concentration of FSH.
- Lyse cells and measure intracellular cAMP production using a commercial assay kit.
- Compare cAMP production in cells expressing VUS to those expressing the wild-type receptor. A significant reduction (e.g., ~50%) indicates impaired downstream signal transduction [29].
FAQs & Troubleshooting Guide
FAQ 1: A significant number of VUS in our POI cohort are in the NOBOX gene, but in silico tools and ACMG criteria classify them as benign or VUS, despite literature suggesting a role in POI. How should we proceed?
- Problem: Discordance between population frequency-based ACMG classification and biological evidence for POI-specific genes.
- Solution:
- Consider Gene-Specific Caveats: Be aware that ACMG criteria like BS1 (allele frequency greater than expected for disorder) and BS2 (observed in a healthy adult) can be problematic for POI. The condition has a prevalence of 1-3.7%, and pathogenic variants can be carried asymptomatically by male relatives, skewing population database frequencies [28].
- Prioritize Functional Evidence: Proceed with functional studies, as was done for NOBOX variants showing nuclear localization impairment and dominant-negative effects, even for some ACMG-classified "benign" variants [28].
- Investigate Oligogenic Models: Consider that the phenotypic expression of a VUS in NOBOX might depend on the presence of variants in other genes (oligogenic inheritance) [28] [27].
FAQ 2: Our diagnostic pipeline has identified a VUS. What are the established pathways for gathering additional evidence to re-classify it?
- Problem: Lack of evidence to resolve a VUS.
- Solution:
- Segregation Analysis: Test first-degree relatives, particularly affected and unaffected females, to see if the variant co-segregates with the POI phenotype. This can provide strong evidence (ACMG codes PP1/BS4) [16] [27].
- Functional Assays: As detailed in Protocol 2.2, perform in vitro experiments to demonstrate a deleterious impact on protein function (e.g., reduced cell surface expression, impaired signaling, altered transcriptional activity). This provides PS3 evidence [29] [26].
- Look for Biallelic or Oligogenic Hits: In recessive disorders, finding a second pathogenic variant in trans (on the other allele) can clarify the pathogenicity of the first VUS. Also, search for potential additional VUS in interacting genes that might have a cumulative effect [27].
FAQ 3: We are designing a genetic study for POI. What is the relative merit of a targeted gene panel versus Whole Exome Sequencing (WES)?
- Problem: Uncertainty in selecting the optimal sequencing strategy.
- Solution:
- Targeted Panels are simpler, more cost-effective, and allow for deep coverage of known POI-associated genes. They are ideal for focused diagnostic screening [29] [25].
- WES is more comprehensive and allows for the discovery of novel candidate genes and oligogenic interactions. It is the preferred tool for research aiming to expand the genetic landscape of POI [26] [30]. The decision should align with the primary goal of the study: routine diagnosis or novel gene discovery.
Key Signaling Pathways & Genetic Networks
Table 2: Key Biological Processes and Associated POI Genes Frequently Harboring VUS
| Biological Process | Description | Example Genes | Challenges with VUS Interpretation |
|---|---|---|---|
| Meiosis & DNA Repair | Ensures accurate chromosome segregation and genomic integrity in germ cells. | MSH4, MSH5, HFM1, SPIDR, STAG3 | Functional assays are complex; variants may not show overt phenotypes in somatic cells. |
| Folliculogenesis | Regulates the development and activation of ovarian follicles. | NOBOX, FIGLA, GDF9, BMP15 | Genes are ovary-specific, limiting functional study options; strong candidate but often VUS. |
| Hormone Signaling & Receptors | Mediates communication between the pituitary and the ovary. | FSHR, BMPR1A/B, ESR2 | In vitro assays (see Protocol 2.2) are well-established but resource-intensive. |
| Metabolic & Mitochondrial | Provides energy and supports fundamental cellular functions in the oocyte. | PMM2, TWNK, EIF2B2 | Can cause syndromic or isolated POI; phenotype can be variable, complicating classification. |
Figure 2: Genetic Network of POI showing VUS Hotspots.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for POI Genetic Research and VUS Functional Analysis
Premature Ovarian Insufficiency (POI) is a clinically heterogeneous condition characterized by the loss of ovarian function before age 40, presenting with menstrual disturbances and elevated Follicle-Stimulating Hormone (FSH) levels [31]. The diagnostic landscape has evolved, with recent guidelines indicating that only one elevated FSH measurement (>25 IU/L) is now required for diagnosis, replacing the previous requirement for two separate measurements [5].
Historically, the majority of POI cases were classified as idiopathic due to limited diagnostic capabilities. However, contemporary research reveals a significant shift in this etiological distribution. A comparative analysis of historical (1978-2003) and contemporary (2017-2024) cohorts demonstrates a dramatic reduction in idiopathic cases from 72.1% to 36.9%, coupled with a more than fourfold increase in identifiable iatrogenic causes (from 7.6% to 34.2%) and a doubling of autoimmune cases [31]. This transformation reflects advances in diagnostic precision and changes in patient populations, including improved survival rates for conditions requiring gonadotoxic treatments.
Table: Comparative Analysis of POI Etiology Over Time
| Etiological Category | Historical Cohort (1978-2003) | Contemporary Cohort (2017-2024) | Change |
|---|---|---|---|
| Genetic | 11.6% | 9.9% | Stable |
| Autoimmune | 8.7% | 18.9% | 2.2x increase |
| Iatrogenic | 7.6% | 34.2% | 4.5x increase |
| Idiopathic | 72.1% | 36.9% | 49% decrease |
Understanding Variants of Uncertain Significance (VUS) in POI Research
The Fundamental Nature of VUS
Variants of Uncertain Significance represent genetic changes whose association with disease risk is currently unknown. The American College of Medical Genetics and Genomics (ACMG/AMP) defines VUS as variants that "do not fulfill criteria using either pathogenic or benign evidence sets, or the evidence for benign and pathogenic is conflicting" [32]. In the context of POI research, VUS present a significant interpretive challenge that reflects the natural biological heterogeneity of human populations.
Current data from ClinVar indicates that VUS constitute the largest single category of genetic variants (44.6% of all germline variation records), outnumbering both pathogenic and benign variants combined [32]. This distribution underscores that VUS are not an intermediate category between pathogenic and benign variants, but rather represent variants with insufficient or conflicting evidence for classification. The persistence of VUS arises from multiple biological factors including differential penetrance, modifier genes, allele dosage effects, and environmental influences [32].
VUS and POI Heterogeneity
The clinical heterogeneity of POI mirrors the biological complexity of VUS interpretation. POI presents across a spectrum of severity, age of onset, and associated health implications, making straightforward genotype-phenotype correlations challenging. This heterogeneity means that the same genetic variant may manifest differently across individuals due to:
- Penetrance Variation: Some carriers of a POI-associated variant may experience complete ovarian failure while others maintain partial function
- Modifier Genes: Genetic background influences phenotypic expression
- Environmental Interactions: Factors like chemical exposures can modify genetic risk
- Allele Dosage Effects: Haploinsufficiency and gene dosage sensitivity vary by gene
Frequently Asked Questions: VUS Troubleshooting in POI Research
Q1: We've identified a VUS in a POI patient with no family history. How should we proceed with interpretation?
Begin by implementing a network-based gene association approach. Tools like VariantClassifier utilize biological evidence-based networks including protein-protein interaction, co-expression, co-localization, genetic interaction, and common pathways networks to contextualize your VUS [33]. The methodology involves:
- Extract known POI-associated variants and genes from ClinVar
- Map your VUS onto gene-association networks
- Select an informative subnetwork by identifying neighboring nodes of the variant gene
- Extract variants from large-scale data for all genes in the subnetwork
- Apply polygenic risk models to detect groups of synergistically acting variants [33] This approach significantly improves risk prediction accuracy by moving beyond single-variant analysis to consider variant synergies.
Q2: What functional evidence is most valuable for VUS reclassification in POI?
Prioritize evidence that demonstrates biological impact on ovarian function. Key experimental approaches include:
- Protein Degradation Assays: Utilize Targeted Protein Degradation tools to assess the functional impact of VUS. Heterobifunctional small molecule degraders can help determine if the variant affects protein stability or function [34]
- Hormone Response Testing: Evaluate the variant's impact on folliculogenesis and steroidogenesis pathways
- Family Segregation Studies: When possible, track variant inheritance patterns in affected and unaffected relatives
- Population Frequency Analysis: Compare variant frequency in POI cohorts versus control populations
Q3: How can we distinguish between pathogenic variants and VUS in genes with low penetrance for POI?
Low-penetrance genes require a quantitative framework for interpretation. Implement the following strategy:
- Calculate a synergy score using network-based methods that consider variant pairs and groups rather than individual variants in isolation [33]
- Incorporate protective variant analysis alongside pro-disease variants to create a more complete genetic risk profile
- Use polygenic risk scoring that aggregates the effects of multiple variants falling below traditional significance thresholds
- Apply functional validation using induced proximity platforms to assess the biological consequences of specific variants [34]
Q4: Our team found conflicting interpretations of the same VUS in different databases. How should we resolve this?
Conflicting interpretations reflect genuine biological heterogeneity rather than simply database errors. Resolution requires:
- Evidence Weighting: Prioritize functional evidence over computational predictions
- Cohort Specificity: Consider the ethnic and clinical characteristics of the populations in which the variant was observed
- Methodological Review: Evaluate the testing methodologies and classification criteria used by different submitters
- Expert Consultation: Refer to gene-specific variant interpretation committees when available, such as the International Society for Gastrointestinal Hereditary Tumours (InSiGHT) model [32]
Experimental Protocols for VUS Investigation in POI
Network-Based VUS Prioritization Workflow
The VarClass methodology provides a systematic approach for prioritizing VUS through network-based gene association [33].
Table: VarClass Pipeline Components
| Step | Process | Tools/Resources | Key Output |
|---|---|---|---|
| 1. Input Generation | Extract known disease-associated variants | ClinVar database | Curated list of POI-related genes/variants |
| 2. Network Construction | Build biological evidence-based networks | GeneMANIA | Five network types: PPI, co-expression, co-localization, genetic interaction, pathways |
| 3. VUS Mapping | Place VUS onto constructed networks | Custom scripts | Network positioning of VUS relative to known genes |
| 4. Subnetwork Selection | Identify neighboring nodes of VUS gene | Network analysis tools | Informative subnetwork of biologically related genes |
| 5. Variant Extraction | Extract variants for all subnetwork genes | WES/WGS data | Expanded variant set for risk modeling |
| 6. Risk Modeling | Develop polygenic risk prediction models | Machine learning algorithms | Two models: with and without VUS under investigation |
| 7. Significance Assessment | Evaluate VUS impact on model performance | ROC analysis, IDI measures | Quantitative significance score for VUS |
Protocol Details:
- Begin by querying ClinVar for established POI-associated genes and variants to create a reference set [33]
- Construct comprehensive gene-association networks using GeneMANIA, incorporating multiple evidence types: physical interactions, genetic interactions, pathway sharing, and co-expression [33]
- Map your VUS of interest onto these networks based on their gene locations
- Extract the local subnetwork comprising direct neighbors and connecting nodes of the VUS gene
- Compile all variants within this subnetwork from your cohort data
- Develop two polygenic risk models: Model 1 includes all subnetwork variants; Model 2 excludes the specific VUS under investigation
- Compare model performance using Receiver Operating Characteristic curves and Integrated Discrimination Improvement metrics to quantify the VUS contribution to risk prediction [33]
Targeted Protein Degradation for Functional Validation
VUS Functional Degradation Workflow
Experimental Procedure:
- PROTAC Design: Select appropriate heterobifunctional degraders based on your target protein. Bio-Techne offers various degraders including PROTAC molecules, molecular glues, and TAG degraders [34]
- Cell Line Selection: Choose appropriate ovarian cell lines or create patient-derived induced pluripotent stem cells (iPSCs) differentiated into ovarian cell types
- Treatment Conditions: Apply degraders at varying concentrations (typically nM to μM range) and time points (hours to days)
- Ternary Complex Validation: Confirm induced proximity using co-immunoprecipitation or proximity-based assays
- Ubiquitination Assay: Detect ubiquitin conjugation to target protein using ubiquitination-specific antibodies or mass spectrometry
- Degradation Monitoring: Measure target protein levels over time via Western blot or Simple Western assays
- Functional Assessment: Evaluate downstream phenotypic consequences including hormone production, folliculogenesis markers, and apoptosis assays
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table: Key Research Reagents for POI VUS Investigation
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Targeted Protein Degraders | PROTAC molecules, dTAG/aTAG degraders, Molecular glues [34] | Functional validation of VUS impact | Catalytic mode of action, target previously "undruggable" proteins, reversible effects |
| Ubiquitin-Proteasome System Components | E3 Ubiquitin Ligases (VHL, CRBN, SKP2), Cullin-Rbx complexes, Ubiquitination assay kits [34] | Mechanistic studies of VUS effects | Highly active enzymes, neddylated cullins available, compatibility with various substrates |
| Network Analysis Tools | VariantClassifier, GeneMANIA, GEMINI [33] | VUS prioritization and interpretation | Integration of multiple biological networks, synergy detection, handles VUS from WES/WGS |
| POI-Specific Assays | Hormone response assays, folliculogenesis markers, meiotic recombination tests | Functional characterization of ovarian impact | POI-relevant cellular contexts, measures key pathological processes |
| Custom Degrader Services | PROTAC panel builders, degrader building blocks, custom E3 ligase development [34] | Tailored solutions for novel VUS | Target-specific degrader design, access to novel E3 ligase ligands, custom chemistry |
| Huzhangoside D | Huzhangoside D | High-purity Huzhangoside D, a natural saponin for cancer research. For Research Use Only. Not for human consumption. | Bench Chemicals |
| Rutarensin | Rutarensin, CAS:119179-04-3, MF:C31H30O16, MW:658.6 g/mol | Chemical Reagent | Bench Chemicals |
Advanced Analytical Framework for VUS Interpretation
VUS Interpretation Decision Pathway
The evolving etiological spectrum of POI, with its marked shift from idiopathic to identifiable causes, underscores the critical importance of sophisticated VUS interpretation frameworks. The integration of network-based prioritization, functional validation through targeted protein degradation, and clinical correlation creates a powerful pipeline for transforming VUS into clinically actionable findings. As the field advances, this multidisciplinary approach will continue to reduce the proportion of idiopathic POI cases while providing deeper insights into ovarian biology and the complex genetic architecture underlying Premature Ovarian Insufficiency.
Methodological Frameworks and Tools for VUS Interpretation in POI
Foundational Concepts of Variant Classification
What is the fundamental principle of the ACMG/AMP guidelines? The 2015 ACMG/AMP guidelines provide a standardized framework for interpreting sequence variants in genes associated with Mendelian disorders. The core outcome of this process is the classification of each variant into one of five categories based on the weight and combination of evidence applied: Pathogenic (P), Likely Pathogenic (LP), Variant of Uncertain Significance (VUS), Likely Benign (LB), or Benign (B) [35] [36]. These classifications use specific terminology to ensure consistency across clinical laboratories.
What defines a Variant of Uncertain Significance (VUS)? A VUS is a genomic variant for which there is insufficient or conflicting evidence to conclude whether it is disease-causing (pathogenic) or harmless (benign) [10]. This classification encompasses a wide range of probabilities of pathogenicity, from 10% to 90% [10]. It is critical to note that a VUS is not considered clinically actionable, and clinical management decisions, such as screening or cascade testing of family members, should not be based on this finding alone [10].
Why are gene-specific guideline specifications necessary? The original ACMG/AMP guidelines were designed to be broadly applicable across all Mendelian genes. However, the 2015 publication itself anticipated that "those working in specific disease groups should continue to develop more focused guidance" [36]. To address this, initiatives like the Clinical Genome Resource (ClinGen) have established Variant Curation Expert Panels (VCEPs). These expert panels create and publish detailed, gene-specific specifications for applying the ACMG/AMP criteria, which greatly improves classification consistency and accuracy for that gene-disease pair [37] [38]. For instance, a VCEP for the PALB2 gene advised against using 13 general codes, limited the use of six, and tailored nine others to create a final, optimized guideline [37].
A Step-by-Step Framework for VUS Interpretation in POI Research
The following workflow provides a structured approach for researchers interpreting variants in the context of Premature Ovarian Insufficiency (POI). It synthesizes the general ACMG/AMP criteria with the gene-specific specification process used by ClinGen VCEPs.
Step 1: Assemble Evidence for the Variant
Gather all available data for the variant, categorizing it into the following evidence types [39]:
- Population Data: Determine the variant's frequency in large population databases like gnomAD. A frequency significantly higher than the disease prevalence is strong evidence against pathogenicity [38].
- Computational and Predictive Data: Use in silico tools to predict the variant's impact on protein function (e.g., conservation, splice site effect).
- Functional Data: Review existing functional studies from the literature. "Well-established" assays that are analytically sound and reflect the biological environment can provide strong evidence [40].
- Case-Level and Clinical Data: Collect segregation data within families, information on de novo occurrence, and the patient's phenotype.
Step 2: Apply and Weight ACMG/AMP Criteria
Map the assembled evidence to the corresponding ACMG/AMP criteria. This is where gene-specific knowledge is critical.
- First, investigate if a ClinGen VCEP or other expert group has published specifications for your POI gene of interest. These specifications define how general criteria should be adapted (e.g., setting a gene-appropriate population frequency threshold for the BS1 criterion) [37] [38].
- Apply the criteria based on these customized rules. For example, the strength of functional evidence (PS3/BS3) can be modified to "Supporting" or "Moderate" based on the validation and performance of a specific assay [40].
Step 3: Combine Criteria for Classification
Follow the ACMG/AMP combining rules to reach a final classification. The table below outlines the general logic for pathogenic classifications. Note that the presence of conflicting evidence (e.g., a pathogenic criterion like PS1 and a benign criterion like BS1) will typically result in a VUS classification [41].
Step 4: Determine the Final Classification and Action
- If the variant classifies as Pathogenic or Likely Pathogenic, it can be considered a definitive finding for the purposes of your research, with the understanding that LP variants have a >90% certainty of being disease-causing [36].
- If the variant remains a VUS, it should be prioritized for further study to gather additional evidence, such as functional assays or segregation data from more family members [10].
Troubleshooting Common Scenarios (FAQs)
FAQ 1: We have a VUS with strong computational predictions of damage, but it is absent from population databases. Why is it not "Likely Pathogenic"?
This is a common scenario. Computational data (PP3) and absence from population databases (PM2) are typically considered supporting or moderate-level evidence. According to the ACMG/AMP combining rules, these evidence strengths alone are often insufficient to reach a Likely Pathogenic classification, which requires stronger evidence such as de novo occurrence (PS2) or well-established functional data (PS3) [35] [41]. The variant you describe is a classic "hot VUS" that is a high priority for gathering additional evidence, such as segregation or functional data, to enable reclassification [10].
FAQ 2: Our functional assay shows a damaging result for a VUS. When can we use this to upgrade the variant?
To use functional data as strong (PS3) evidence for pathogenicity, the assay must be "well-established." [40] This requires:
- Robust Validation: The assay should have been tested with a set of known pathogenic and benign control variants and demonstrated a high ability to distinguish between them.
- Biological Relevance: The assay should reflect the gene's biological function and the disease mechanism (e.g., loss-of-function, dominant negative).
- Technical Rigor: The experiment should include appropriate controls, replicates, and statistical analysis [40]. Without these parameters, the evidence strength may need to be downgraded to moderate (PS3Moderate) or supporting (PS3Supporting). ClinGen VCEPs often provide guidance on which specific assays for a gene meet this bar [40].
FAQ 3: How should we handle a VUS that is found in a patient with a compelling phenotype?
A compelling phenotype can be used as evidence (PP4), but it is usually a supporting-level criterion. Clinical management should be based on the personal and family history, not on the presence of the VUS [10] [41]. In a research context, you can:
- Perform Segregation Analysis: Test other affected and unaffected family members to see if the variant co-segregates with the disease.
- Seek Additional Evidence: Pursue functional studies or look for independent observations of the same variant in other cases.
- Leverage Team Expertise: Discuss the variant in a multi-disciplinary team setting where clinical, genetic, and functional data can be integrated to assess if the VUS can be reclassified [10].
Quantitative Framework for Evidence Integration
The ACMG/AMP guidelines are compatible with a Bayesian statistical framework, which allows for a quantitative interpretation of the evidence strength. The Sequence Variant Interpretation (SVI) working group of ClinGen has estimated the relative odds of pathogenicity for each evidence level [38]. This framework is useful for understanding the quantitative "weight" behind each criterion you apply.
Table 1: Bayesian Weights of ACMG/AMP Evidence Criteria
| Evidence Strength | Odds of Pathogenicity | Posterior Probability of Pathogenicity* |
|---|---|---|
| Supporting (P) | 2.08 : 1 | ~67.5% |
| Moderate (M) | 4.33 : 1 | ~81.2% |
| Strong (S) | 18.7 : 1 | ~94.9% |
| Very Strong (VS) | 350 : 1 | ~99.7% |
*Assuming a 0.1% prior probability of pathogenicity. Adapted from Tavtigian et al. (2018) as cited in [38].
Table 2: Example Combinations for Pathogenic Classifications
| Pathogenic Criteria Met | Combined Odds (Approx.) | Combined Probability (Approx.) | Final Classification |
|---|---|---|---|
| 1 Strong (S) + 1 Moderate (M) | 81 : 1 | ~98.8% | Likely Pathogenic |
| 1 Very Strong (VS) | 350 : 1 | ~99.7% | Pathogenic |
| 2 Strong (S) | 350 : 1 | ~99.7% | Pathogenic |
| 1 Strong (S) + 2 Moderate (M) | 350 : 1 | ~99.7% | Pathogenic |
Table 3: Essential Resources for VUS Interpretation
| Resource / Reagent | Function in VUS Analysis | Key Considerations |
|---|---|---|
| gnomAD Database | Provides population allele frequency data to assess variant rarity. | Use the filtering allele frequency (FAF) to control for population substructure. Be mindful of adult-onset diseases in this dataset [38]. |
| ClinVar Database | A public archive of reports on genomic variants and their relationship to phenotype. | Helps identify if a VUS has been seen and interpreted by other labs, though interpretations may conflict [37]. |
| ClinGen VCEP Specifications | Gene- and disease-specific rules for applying ACMG/AMP criteria. | Check the ClinGen website for approved specifications for your gene of interest; these override the general guidelines [37] [42]. |
| In Silico Prediction Tools | Computational programs (e.g., SIFT, PolyPhen-2) that predict the functional impact of a missense variant. | Results are considered supporting evidence (PP3 for damaging, BP4 for benign). Use a combination of tools for a more reliable prediction [35]. |
| Validated Functional Assays | Laboratory tests (e.g., in vitro, model organisms) that measure the biochemical consequence of a variant. | Must be "well-established" and validated with known controls to be used as strong (PS3/BS3) evidence [40]. |
Experimental Protocols for Key Evidence Types
Protocol: Validating a Functional Assay for PS3/BS3 Application Based on the analysis of multiple VCEPs, the following parameters are critical for developing a functional assay that can be used as strong evidence for variant classification [40]:
- Define Disease Mechanism: First, establish the expected molecular effect for pathogenic variants in your gene (e.g., loss-of-function, gain-of-function, dominant negative). The assay must directly measure this specific function.
- Establish a Reference Range: Test a set of at least 10-15 known pathogenic and 10-15 known benign variant controls in your assay. This is essential for validation.
- Set a Quantitative Threshold: Based on the control results, define a clear, statistical threshold that distinguishes pathogenic from benign variants. The assay should have a high sensitivity and specificity (>90% is ideal for strong-level evidence).
- Incorporate Experimental Controls: Each experimental run must include:
- Positive Control: A known pathogenic variant.
- Negative Control: A known benign variant or wild-type.
- Technical Replicates: Perform a minimum of three independent experimental replicates to ensure robustness and reproducibility.
- Document and Publish: Fully document the assay protocol, validation data, and results for the VUS. Publication in a peer-reviewed journal strengthens the evidence.
Protocol: Gathering Segregation Data for PP1 Application
- Identify Family Members: Recruit as many first- and second-degree relatives of the proband as possible, both affected and unaffected.
- Perform Genotyping: Genotype all recruited family members for the VUS.
- Statistical Analysis: Calculate a LOD score (logarithm of the odds) if the family structure is sufficiently large. As a rule of thumb, the PP1 criterion can be applied at a supporting strength if the variant is observed to co-segregate with disease in multiple affected family members. The strength can be upgraded to moderate or strong with a statistically significant LOD score [35].
Leveraging Population Genomics Databases (gnomAD, ClinVar) for Allele Frequency Analysis
Within Premature Ovarian Insufficiency (POI) research, a genetic diagnosis is achieved in only 20-25% of cases, leaving a significant portion of patients without a known etiology [16]. The analysis of genetic variants, particularly the interpretation of Variants of Uncertain Significance (VUS), is therefore a critical component of POI research. Population genomics databases are indispensable tools in this process, enabling researchers to distinguish rare, potentially pathogenic variants from common benign polymorphism.
This technical support center provides targeted guidance for leveraging the Genome Aggregation Database (gnomAD) and ClinVar to address common challenges in POI allele frequency analysis.
Frequently Asked Questions & Troubleshooting Guides
How do I filter variants based on population frequency in gnomAD?
A core task in POI research is filtering out variants that are too common in the general population to be responsible for a rare condition.
- Problem: A researcher needs to filter variants with a population frequency of less than 1% but is unsure which gnomAD field to use and how to interpret the values.
Solution:
- The
AF(Allele Frequency) field in gnomAD is expressed as a proportion, not a percentage [43]. A value of0.01corresponds to 1%. - For a strict filter against common variants, using the
popmax(maximum allele frequency across all specific populations) orAF_popmaxfield is recommended. This helps avoid missing a variant that is common in a specific population but rare globally [43]. - To select for variants with a frequency of <1%, you should filter where
AF_popmax < 0.01.
- The
Example Filtering Logic for a Rare Disease like POI:
Why does a variant have a high population frequency in gnomAD but is also listed as pathogenic in ClinVar?
Encountering a variant described as pathogenic in ClinVar that also has a high allele frequency in gnomAD is a common point of confusion.
- Problem: A putative pathogenic variant in a POI candidate gene (e.g., NOBOX, BMP15) is observed with a high frequency in gnomAD, which contradicts its supposed disease-causing role in a rare condition.
- Solution: This discrepancy is a major red flag and typically indicates one of the following issues [44] [45]:
- Misclassification in ClinVar: The variant's pathogenic classification may be erroneous. Older submissions might not have had access to large population data.
- Benign Founder Variant: The variant could be a benign founder variant that is common in a specific population.
- Reduced Penetrance: The variant might cause disease only in combination with other genetic or environmental factors.
- Troubleshooting Steps:
- Check ClinVar Submissions: On the ClinVar variant page, review the number of submitters and the review status. Conflicts between submitters or a single submitter without expert review (e.g., zero stars) lower confidence in the pathogenic call [46] [45].
- Investigate Population-Specific Frequency: In gnomAD, drill down into the frequency within specific ancestral populations. A variant rare globally but common in one population might be a founder variant.
- Re-evaluate Pathogenicity: Use the ACMG/AMP guidelines. A high population frequency is strong evidence against pathogenicity (BS1 criterion) and should prompt a re-classification of the variant.
How can I integrate gnomAD constraint metrics into my analysis of POI candidate genes?
Not all genes are equally tolerant to genetic variation. gomAD's constraint metrics help identify genes that are intolerant to loss-of-function or missense variation.
- Problem: A researcher identifies a rare missense variant in a novel gene in a POI patient and wants to assess the gene's overall relevance to disease.
- Solution: Use gnomAD's loss-of-function observed/expected (oe) constraint score and the missense Z-score.
- A low LoF oe score (significantly < 0.35) indicates that the gene has fewer loss-of-function variants than expected, suggesting purifying selection and that it is likely essential—a hallmark of disease-associated genes [44].
- A high missense Z-score indicates intolerance to missense variation.
- Application: A gene with a low LoF constraint score is a stronger candidate for harboring pathogenic variants contributing to POI. For example, if your novel gene has an LoF oe score of 0.1 (pLI = 1.0), this strengthens the case that the rare variant you found may be deleterious.
What is the best way to resolve conflicting interpretations in ClinVar for a VUS in a POI gene?
It is common to find VUS with conflicting interpretations of pathogenicity in ClinVar.
- Problem: A FIGLA variant is listed as a VUS in your internal analysis, and ClinVar shows two submissions: one as "Likely pathogenic" and another as "Uncertain significance."
- Solution:
- Examine the Evidence: On the ClinVar VCV page, expand each submission to see the submitter's name, the date of last evaluation, and the evidence cited [46].
- Prioritize Expert-Reviewed Submissions: Favor submissions from reputable labs or consortia that provide detailed evidence and have a high review status (e.g., multiple stars) [46].
- Cross-reference with Population Data: Check the variant's frequency in gnomAD. If it is completely absent or very rare (
AF_popmax < 0.0001), it remains a candidate. If it is common, it is likely benign. - Use Parsing Tools: Leverage pipelines that parse ClinVar data to flag "conflicted" variants systematically, defined as those with both pathogenic and benign assertions [45].
Database Comparison & Key Metrics
Table 1: Core Features of gnomAD and ClinVar for POI Research
| Feature | gnomAD | ClinVar |
|---|---|---|
| Primary Purpose | Catalog of population allele frequencies from control cohorts [44] | Archive of genotype-phenotype relationships and clinical interpretations [47] |
| Key Data Provided | Allele frequencies (global, per-population), constraint scores (pLI, missense Z), genotype quality metrics [44] | Pathogenicity assertions (Pathogenic, VUS, Benign), submitter information, review status, reported phenotypes [46] |
| Role in VUS Interpretation | Provides quantitative evidence to filter out common variants and assess gene intolerance [44] | Provides qualitative evidence from clinical testing and research, highlighting (in)consistency in interpretation [45] |
| Critical Field for POI | popmax AF (for filtering common variants); pLI (for gene-level candidacy) |
Review Status (to gauge confidence in an assertion); Conflicted flag (to identify discordance) [46] [45] |
Table 2: Essential gnomAD Metrics for Filtering in POI Research
| Metric | Description | Interpretation in POI Context |
|---|---|---|
| AF_popmax | The highest allele frequency observed in any specific population within gnomAD [43]. | Primary filter to remove common variants. Use AF_popmax < 0.01 (1%) for a rare disease like POI. |
| pLI | Probability of being loss-of-function intolerant. Range 0-1 [44]. | A high pLI (≥ 0.9) suggests the gene is sensitive to LoF variants, strengthening a candidate gene. |
| Filters | PASS vs. various failure codes (e.g., for sequencing artifacts) [48]. | Prioritize variants with a PASS filter status to avoid technical false positives. |
Experimental Protocol: Integrated Allele Frequency Workflow
This protocol outlines a standard methodology for leveraging gnomAD and ClinVar in the analysis of sequencing data from a POI cohort, as used in recent studies [16].
1. Input Data: VCF file from Next-Generation Sequencing (Whole Exome or Whole Genome) of POI patients [16].
2. Annotation: Annotate variants using a pipeline (e.g., VEP, SnpEff) that includes population frequency data from gnomAD and clinical interpretations from ClinVar.
3. Initial Filtering:
* Remove variants that do not have a PASS quality filter.
* Remove variants with a gnomAD AF_popmax > 0.01.
* Retain only exonic and splice-site variants.
4. Prioritization & Triage:
* Check remaining variants against ClinVar. Prioritize those with established Pathogenic/Likely Pathogenic interpretations.
* For variants not in ClinVar or listed as VUS, analyze the gene-level constraint in gnomAD. Prioritize variants in genes with high pLI scores.
* For VUS, manually review the evidence on the ClinVar VCV page, paying close attention to conflicted status and review stars [46] [45].
5. Validation: Confirm prioritized variants (especially indels and CNVs) using an orthogonal method such as Sanger sequencing or array-CGH [16].
Integrated gnomAD and ClinVar Analysis Workflow for POI VUS Interpretation
Table 3: Essential Resources for Population Genomics in POI Research
| Resource / Reagent | Function in Analysis | Specifications / Notes |
|---|---|---|
| gnomAD Browser | Primary interface for querying population allele frequencies and constraint scores [44]. | Use v2.1.1 for GRCh37 and v3.1.2 for GRCh38. Be mindful of sample overlap between versions [44]. |
| ClinVar VCV Page | Displays all data aggregated for a single variant, including submissions and review status [46]. | Critical for investigating conflicting interpretations and assessing the evidence behind a classification. |
| Custom Gene Panel | A targeted list of genes known or suspected to be involved in ovarian function [16]. | The 2025 POI study used a panel of 163 genes. Focuses analysis and increases depth of coverage. |
| ACMG/AMP Guidelines | A standardized framework for classifying variants based on evidence from population data, computational predictions, and functional data [49]. | Provides the criteria (e.g., PM2, BS1) for assigning Pathogenic, VUS, or Benign labels. |
| Variant Normalization Tool (e.g., vt normalize) | Standardizes variant representation to ensure consistent matching and annotation across databases [45]. | Prevents errors caused by non-minimal or left-aligned representations of complex variants. |
Frequently Asked Questions for POI Research
FAQ 1: Which in silico tools are most recommended for interpreting VUS in POI genes?
No single tool is perfect, and performance can vary. However, some tools consistently demonstrate high accuracy. For researchers beginning their analysis, a combination of the following tools is recommended:
- High-Performance Ensemble Tools: REVEL, BayesDel, and MutPred2 are meta-predictors that aggregate outputs from multiple other tools, often leading to more robust predictions [50] [51]. A 2025 study on CHD genes found BayesDel to be the most accurate score-based tool overall [51].
- Emerging AI-Based Tools: AlphaMissense shows significant promise. It is an AI model trained on human and primate variant population frequency databases and has been shown to outperform many established tools in initial validations [50] [51]. In a study on a CHEK1 VUS in POI, AlphaMissense provided a high pathogenicity score (0.754), which supported further investigation [15].
- Commonly Used Tools: SIFT, PolyPhen-2, and CADD are widely used and integrated into many analysis pipelines. A 2025 benchmark found SIFT to be the most sensitive tool for categorically classifying pathogenic variants in a specific gene family [51].
Table 1: Summary of Key In Silico Prediction Tools
| Tool Name | Type | Key Principle | Strengths in POI Research |
|---|---|---|---|
| REVEL [50] | Ensemble/Meta-predictor | Random forest classifier integrating scores from multiple tools (SIFT, PolyPhen-2, etc.) | High performance in benchmarking studies; useful for a broad range of variants. |
| AlphaMissense [50] [15] | AI/Deep Learning | Fine-tuned from AlphaFold; uses protein structure and evolutionary context. | High accuracy for rare variants; provides genome-wide predictions. |
| BayesDel [50] [51] | Ensemble/Meta-predictor | Native Bayes classifier trained on ClinVar and HGMD data (without allele frequency). | Identified as a top-performing tool for predicting pathogenicity in specific gene families. |
| MutPred2 [50] | Machine Learning | Deep neural network incorporating protein structural and functional data. | Provides hypotheses on molecular mechanisms of pathogenicity. |
| CADD [50] | Heuristic/Integration | Integrates diverse annotations but not trained on a specific disease variant set. | Widely used; can predict pathogenicity of variants not seen in training sets. |
| SIFT [51] | Sequence Homology-Based | Predicts effect based on sequence conservation across species. | High sensitivity; useful for initial filtering of deleterious variants. |
FAQ 2: I have conflicting predictions from different tools for my POI-related VUS. How should I proceed?
Conflicting predictions are common and highlight the need for a structured, multi-step approach.
- Consensus Check: Use a tool that generates a consensus from multiple predictors, such as REVEL or BayesDel [50]. A higher number of tools agreeing on a prediction increases confidence.
- Gene-Specific Validation: Be aware that tool performance can be gene-specific. A tool's overall high accuracy does not guarantee equal performance for all genes [50]. Consult the literature to see if validation has been performed for your gene of interest (e.g., a 2023 large-scale POI study identified genes where specific biological processes like meiosis are enriched) [26].
- Incorporate Structural Impact: Use tools that evaluate the variant's impact on protein structure. For example, in the case of a CHEK1 VUS (p.A26G), structural analysis with DynaMut2 predicted the variant would destabilize the protein (ΔΔG = -0.98 kcal/mol), supporting pathogenicity despite conflicting primary tool outputs [15].
- Proceed to Functional Assays: Computational evidence alone is often insufficient for a definitive classification. If the VUS remains uncertain, functional studies are the critical next step [15].
FAQ 3: What is an appropriate experimental workflow to validate a VUS identified in a POI patient?
A robust validation protocol integrates computational evidence with functional data. The following workflow is adapted from established methodologies in genetic research [16] [15] [26].
FAQ 4: How do I handle a VUS that might affect splicing?
- Use a Splice-Aware Tool: Always run a splicing-specific in silico tool such as SpliceAI [50]. This tool can predict whether a coding region variant may create a novel splice site.
- Follow Guideline Thresholds: The ClinGen Sequence Variant Interpretation Working Group recommends thresholds for SpliceAI. A score of >0.38 supports pathogenicity, while a score of <0.2 supports benignity [50].
- Experimental Splicing Assays: If a variant is predicted to affect splicing, the next step is to perform a functional assay, such as a mini-gene splicing assay, to confirm the prediction in a cellular context.
Troubleshooting Guides
Problem: Inconsistent or low-confidence predictions from in silico tools for a VUS in a known POI gene.
Solution:
- Step 1: Expand your toolset. Do not rely on a single tool. Include at least one high-performance ensemble tool (e.g., REVEL, BayesDel) and one of the newer AI-based tools (e.g., AlphaMissense) in your analysis [50] [51].
- Step 2: Perform gene-specific and structure-specific analysis.
- Check if your gene of interest has specific clinical guideline recommendations for in silico tools [50].
- Use a tool like MISCAST or perform a structural analysis using an AlphaFold2-predicted model to evaluate the impact of the variant on protein stability and structure, as demonstrated in the CHEK1 A26G study [50] [15].
- Step 3: Corroborate with population data. Ensure the variant is truly rare by checking its frequency in population databases like gnomAD. A high frequency would lean against pathogenicity.
- Step 4: If uncertainty remains, the evidence is likely insufficient for classification, and you should progress to functional assays [15].
Problem: Need to design a functional experiment to validate a VUS's impact on protein function.
Solution: Implement a multi-tiered experimental strategy as outlined in the workflow above and detailed below.
- Cell Culture & Transfection: Use a standard cell line like 293FT for high transfection efficiency. Clone the wild-type and mutant (VUS) gene constructs with tags (e.g., HA-tag) for detection [15].
- Protein Expression Analysis:
- Protocol: Transfert cells with wild-type and mutant constructs. Perform Western blotting 48-72 hours post-transfection.
- Key Reagents: Anti-tag antibody (e.g., anti-HA) and a loading control antibody (e.g., anti-GAPDH).
- Expected Outcome: Altered protein expression levels or size, as seen with the CHEK1 A26G variant, can indicate instability [15].
- Transcriptome Analysis (RNA-seq):
- Protocol: Extract total RNA from cells expressing wild-type and mutant proteins. Prepare libraries and perform RNA sequencing.
- Data Analysis: Use tools like DESeq2 to identify differentially expressed genes (DEGs). Perform Gene Ontology (GO) enrichment analysis on the DEGs.
- Expected Outcome: The VUS may disrupt key biological pathways. For example, the CHEK1 A26G variant altered the expression of genes involved in metabolism and inflammation [15].
Research Reagent Solutions
Table 2: Essential Materials and Reagents for VUS Validation Experiments
| Item | Function/Description | Example from Literature |
|---|---|---|
| WES Kit | Identifies coding variants across the exome. | Agilent SureSelect Human All Exon V6 kit [15] [26]. |
| Array-CGH | Detects copy number variations (CNVs). | Agilent SurePrint G3 CGH Microarray [16]. |
| Custom NGS Panel | Targets a specific set of genes for sequencing. | Custom capture design of 163 genes involved in ovarian function [16]. |
| Expression Vector | For cloning and overexpressing gene variants in cells. | HA-tagged vector for CHEK1 [15]. |
| Cell Line | Model system for in vitro functional assays. | 293FT cells for transfection [15]. |
| RNA-Seq Service | For transcriptome-wide analysis of gene expression changes. | Commercial service (e.g., BerryGenomics) [15]. |
| Pathogenicity Tools | Computational prediction of variant impact. | REVEL, AlphaMissense, CADD, SIFT, PolyPhen-2 [50] [51] [15]. |
| Structural Analysis Tools | Predicts impact of mutation on protein stability. | DynaMut2, MISCAST, AlphaFold2-predicted models [50] [15]. |
Multiplexed Assays of Variant Effect (MAVEs) represent a transformative approach in genetics, enabling the simultaneous functional assessment of thousands of genetic variants in a single experiment [52]. For researchers investigating Premature Ovarian Insufficiency (POI), these high-throughput techniques are crucial for addressing the challenge of Variants of Uncertain Significance (VUS) – genetic changes whose impact on health is unknown [20]. With over 70% of unique variants in clinical databases classified as VUS, MAVEs provide a systematic pathway to decipher their biological consequences, moving beyond the limitations of traditional one-variant-at-a-time functional studies [20]. This technical support center provides essential guidance for implementing MAVE technologies to advance POI research and variant interpretation.
Essential MAVE Workflows and Signaling Pathways
Core MAVE Experimental Workflow
The following diagram illustrates the generalized workflow for MAVE experiments, from design to clinical application:
MAVE Clinical Validation Pathway
This pathway details the critical process for translating MAVE data into clinically actionable evidence:
Technical Support: Frequently Asked Questions
Experimental Design and Setup
Q: What factors should I consider when designing a MAVE for POI-associated genes? A successful MAVE design requires careful consideration of several factors: First, ensure the assay measures a phenotype relevant to the gene's function in ovarian biology. For POI genes, this might include protein function, signaling pathway activity, or cellular viability. Second, select appropriate saturation mutagenesis coverage – aim for deep coverage (typically >500x) to ensure robust statistical power. Third, include proper controls: synonymous variants as neutral controls, known pathogenic variants as positive controls, and nonsense variants for loss-of-function calibration [53].
Q: What positive controls are appropriate for POI-related MAVE experiments? Any tissue demonstrated to be positive for each marker via chromogenic IHC can serve as a positive control. Each target requires its own positive control, which may necessitate multiple control tissues. For optimal comparison, tissue sections should be as close to serial as possible [54].
Q: Can I use MAVEs for genes with long coding sequences? Yes, though this presents technical challenges. Functional verification of missense mutations in long genes requires sophisticated approaches. Consider implementing advanced technologies such as cell immortalization, induced pluripotent stem cells (iPSC), gene editing, transposon systems, and patch clamp technology to overcome these challenges [55].
Troubleshooting Experimental Issues
Q: When comparing SignalStar staining to chromogenic staining on serial sections, I observe more positive cells. How do I verify this excess staining is correct? During optimization, fluorescent staining often shows higher percent-positivity than chromogenic methods. To confirm specificity: verify correct subcellular localization and check for expected co-localization with other stains. For example, if all CD8+ cells are CD3+, any excess CD8+ staining compared to chromogenic is likely correct [54].
Q: How long after staining completion can I wait to image my slides? For Imaging Round 1, robust signal typically persists up to 8 hours post-staining completion. For Imaging Round 2, imaging should be performed as close to staining completion as possible but remains robust for up to 8 hours [54].
Q: Do I need to optimize kits and reagents for my specific tissue type? Yes, tissue-specific optimization is essential. While MAVE kits and reagents are optimized for fluorophore pairing and antibody order, tissues vary in quality and target expression levels. Increasing antibody concentration by 2-fold or decreasing by 0.5-fold can help achieve optimal signal for your specific tissue [54].
Data Analysis and Interpretation
Q: What quality control metrics are essential for MAVE data analysis? Robust QC should include: separation between synonymous and nonsense variant readouts (validates assay performance for loss-of-function), measurement of biological and technical replicate consistency, assessment of coverage depth across the variant library, and evaluation of known pathogenic vs. benign variant distributions [53].
Q: How do I determine appropriate thresholds for designating variant impact? Thresholds should be calibrated using the separation between positive and negative controls within your dataset. For loss-of-function genes, analyze the distribution of nonsense variants versus synonymous variants. Establish thresholds that maximize separation between these control groups while maintaining statistical confidence intervals [53].
Q: What computational resources are available for MAVE data analysis? Multiple open-source tools and resources are available through the Atlas of Variant Effects Alliance, including MaveDB (public repository for MAVE datasets), analysis pipelines for quality control, and statistical methods for interpretation. The Wellcome Connecting Science course also provides comprehensive computational training [52] [56].
Clinical Translation and Validation
Q: What are the requirements for clinical validation of MAVE data? Clinical validation requires adherence to the Brnich et al. methodology, which includes: quantifying concordance against variant truth sets (previously classified benign/pathogenic variants), producing assay-level evidence strength as a log likelihood ratio, demonstrating understanding of disease mechanism, and evaluating experimental methodology including replicates [53].
Q: Will clinical diagnosticians accept our internal MAVE validation? Survey data indicates only 35% of clinical scientists accept author-provided validation alone. 61% prefer awaiting validation by a trusted central body, and 72% would use MAVE data ahead of formal publication if reviewed and validated by such a body. Engaging with organizations like ClinGen SVI Functional Working Group, VCEPs, or CanVIG-UK early in the process is recommended [53].
Q: Where should we deposit our MAVE data for clinical use? Primary options include ClinVar (familiar to diagnosticians) and MaveDB (repository for MAVE data). While ClinVar has higher recognition in clinical communities, deposition in both ensures broad accessibility. CanVar-UK also hosts variant-level data from multiple MAVEs for cancer susceptibility genes [53].
Research Reagent Solutions for MAVE Experiments
Table: Essential Research Reagents for MAVE Implementation
| Reagent Category | Specific Examples | Function & Application | Validation Considerations |
|---|---|---|---|
| Antibody Panels | SignalStar Multiplex IHC kits | Target detection in FFPE tissues | Validate combinations through titration and fluorophore pairing; test on relevant tissues [54] |
| Secondary Detection | SignalStar Secondary Antibodies | Enable use of unconjugated primary antibodies | Can only be used in first round of imaging [54] |
| Signal Removal Reagents | SignalStar Fluorescence Removal Kit (#32722) | Remove fluorescent oligos between imaging rounds | Enables sequential staining without antibody stripping [54] |
| Antigen Retrieval | SignalStain EDTA Unmasking Solution | Antigen exposure in FFPE tissues | Follow optimized protocols; microwave methods may reduce signal [54] |
| Control Materials | Tissue known positive for target markers | Assay performance validation | Required for each target; use serial sections for optimal comparison [54] |
MAVE Clinical Implementation Survey Findings
Recent survey data from NHS clinical scientists reveals critical insights for implementing MAVE data in clinical practice:
Table: Clinical Scientist Perspectives on MAVE Data Implementation (n=46)
| Survey Question | Response Distribution | Clinical Implementation Implication |
|---|---|---|
| Acceptance of author-provided clinical validation | 35% would accept | Majority require additional validation beyond what assay developers provide |
| Preferred validation approach | 61% await central body validation20% attempt local validation | Centralized validation is strongly preferred for clinical adoption |
| Use of pre-publication MAVE data | 72% would use if validated by trusted central body | Formal publication less critical than robust central review |
| Trusted validation bodies | CanVIG-UK (median=5/5)VCEPs (median=5/5)ClinGen SVI (median=4/5) | Existing variant interpretation frameworks are trusted for MAVE validation [53] |
Advanced Methodologies for POI Research
Model Organism Approaches
Drosophila functional assays provide valuable tools for VUS classification in rare diseases. Key methodologies include: studying loss-of-function of orthologous fly genes, assessing human gene ability to rescue fly mutant phenotypes, determining effects of human protein overexpression, and testing functional consequences of rare variants by generating analogous fly mutants [57]. These approaches help classify variants into specific allelic categories (loss-of-function or gain-of-function) and can be leveraged to design effective MAVEs [57].
Specialized Functional Assays
Mini-gene splicing assays enable functional validation of splicing variants. For example, in studies of DEPDC5 gene variants in familial focal epilepsy, researchers used mini-gene assays to demonstrate that specific variants disrupt alternative splicing, revealing critical mechanisms in disease pathogenesis [55]. Similar approaches can be adapted for POI-associated genes to evaluate the impact of non-coding and splice-site VUS.
Metabolic marker analysis provides an alternative functional assessment approach. In methylmalonic acidemia research, scientists used mass spectrometry to show that patients with pathogenic mutations exhibited significantly higher levels of metabolic markers (C3, C3/C0, C3/C2) compared to non-carriers, offering a novel approach to VUS pathogenicity assessment [55]. This methodology could be adapted for POI research by identifying and measuring relevant endocrine biomarkers.
MAVE technologies represent a powerful toolkit for advancing POI research by systematically characterizing VUS and bridging the gap between variant discovery and clinical interpretation. Successful implementation requires robust experimental design, appropriate troubleshooting strategies, adherence to clinical validation standards, and engagement with trusted central bodies for review and endorsement. By leveraging these approaches and resources, researchers can significantly accelerate the interpretation of genetic variants in POI and ultimately improve diagnostic outcomes and personalized treatment strategies for affected individuals.
Frequently Asked Questions (FAQs)
FAQ 1: Why is a multi-omics approach necessary for resolving Variants of Uncertain Significance (VUS) when DNA sequencing alone is inconclusive?
DNA sequencing, such as whole exome or genome sequencing (WES/WGS), can identify a variant but often cannot determine its functional consequences on the cellular system [58]. A VUS is a genetic change whose impact on health is unclear, and they are disproportionately more common in individuals of non-European ancestry due to less reference data [59]. DNA-level information alone is often insufficient for interpretation [60].
A multi-omics approach is crucial because it moves beyond the static genomic blueprint to observe dynamic molecular activity.
- Transcriptomics (RNA-seq) can reveal if a variant causes aberrant splicing, alters gene expression levels, or leads to nonsense-mediated decay (NMD) of the RNA transcript [60].
- Proteomics can determine if changes at the RNA level subsequently affect the abundance or function of the resulting proteins [58] [61].
- Methylation Patterns (Epigenomics) can identify disease-specific epigenetic signatures, such as hypermethylation of a tumor suppressor gene's promoter, which can silence its expression and drive disease independently of the DNA sequence [58] [62].
By integrating these layers, you can gather functional evidence to reclassify a VUS as either likely pathogenic or benign [60].
FAQ 2: What are the most common technical challenges in integrating transcriptomic, proteomic, and methylation data, and how can they be overcome?
The primary challenge is the heterogeneity of the data. Each omics technology generates data with different structures, scales, noise profiles, and batch effects [63]. For instance, your RNA-seq data is count-based, methylation arrays produce beta-values, and proteomics data may be spectral counts or intensities.
The following table summarizes key challenges and their solutions:
| Challenge | Description | Recommended Solution |
|---|---|---|
| Lack of Pre-processing Standards | Each data type requires tailored normalization and batch effect correction [63]. | Standardize data into a sample-by-feature matrix. Use tools like ComBat for batch correction and platform-specific normalization (e.g., BMIQ for methylation arrays) [62] [64]. |
| Data Heterogeneity | Data types are not directly comparable due to different units and distributions [63]. | Preprocess data individually, then apply harmonization techniques to align them onto a common scale or in a shared latent space [64]. |
| Complex Data Interpretation | Translating integrated statistical findings into biological insight is difficult [63]. | Use pathway and network analysis on the multi-omics feature set. Prioritize features that are significant across multiple omics layers [65]. |
FAQ 3: Which computational integration methods are best suited for combining these omics data to classify VUS?
The choice of method depends on whether your analysis is supervised (using known patient outcomes to guide integration) or unsupervised (exploring the data without pre-defined labels).
Unsupervised Methods: These are ideal for discovering novel molecular subgroups or patterns without bias.
- MOFA (Multi-Omics Factor Analysis): A powerful tool that identifies the principal sources of variation (latent factors) across your multiple omics datasets. You can then investigate if any factors are strongly associated with the presence of the VUS [63].
- Similarity Network Fusion (SNF): Constructs sample-similarity networks for each omics data type and then fuses them into a single network. Patients with similar multi-omics profiles will cluster together, which can help correlate a VUS carrier's profile with known pathogenic or benign profiles [63].
Supervised Methods: These are used when you want to integrate data specifically to predict a known categorical outcome.
- DIABLO (Data Integration Analysis for Biomarker discovery using Latent cOmponents): This method is excellent for classification. It integrates your omics datasets to find a composite biomarker that best discriminates between, for example, "VUS pathogenic" and "VUS benign" groups, while also performing feature selection to identify the most important transcripts, proteins, and CpG sites [63].
The workflow for resolving a VUS using multi-omics data typically follows a structured path from data generation to functional interpretation, as visualized below:
Experimental Protocols for Key Multi-Omic Assays
Protocol 1: Transcriptome Sequencing (RNA-seq) for VUS Analysis
Objective: To identify the impact of a VUS on gene expression, splicing, and allelic imbalance.
Methodology:
- Sample Preparation: Extract high-quality total RNA from patient-derived cells or tissue (e.g., fibroblasts, PBMCs) using a kit that includes DNase I treatment. Assess RNA Integrity Number (RIN) > 8.0.
- Library Preparation: Use a stranded mRNA-seq library preparation kit to enrich for poly-adenylated RNA. This allows for the assessment of allele-specific expression.
- Sequencing: Perform sequencing on an Illumina platform to a minimum depth of 30-50 million paired-end reads (e.g., 2x150 bp) for robust splicing analysis [60].
- Bioinformatic Analysis:
- Alignment & Quantification: Align reads to the reference genome using a splice-aware aligner like STAR. Quantify gene-level counts with featureCounts and transcript-level abundance with Salmon or Kallisto [60].
- Splicing Analysis: Use rMATS or LeafCutter to detect aberrant splicing events, such as exon skipping or intron retention, caused by the VUS [60].
- Variant Effect Validation: Employ SpliceAI to computationally predict the impact of the VUS on splicing and then validate these predictions with your RNA-seq data [66].
Protocol 2: DNA Methylation Profiling Using Microarrays
Objective: To uncover epigenetic dysregulation associated with the VUS that may indicate a pathogenic gene silencing event.
Methodology:
- Sample Preparation: Perform bisulfite conversion on patient genomic DNA using a dedicated kit (e.g., EZ DNA Methylation Kit). This converts unmethylated cytosines to uracils, while methylated cytosines remain unchanged.
- Methylation Array Processing: Hybridize the bisulfite-converted DNA to an Illumina Infinium EPIC array, which Interrogates over 850,000 CpG sites across the genome [62].
- Data Preprocessing & Normalization:
- Differential Methylation Analysis: Identify differentially methylated positions (DMPs) or regions (DMRs) between VUS carriers and control groups using linear modeling in the limma package. Focus on DMRs in promoter and enhancer regions of genes relevant to the disease phenotype [62].
Protocol 3: Data Integration Using MOFA+
Objective: To identify coordinated sources of variation across transcriptomic, proteomic, and methylation datasets that are linked to the VUS.
Methodology:
- Data Input Preparation: Create three separate, sample-matched matrices:
- Transcriptomics: Normalized gene expression counts (e.g., TPM or variance-stabilized counts).
- Methylation: M-values or beta-values from the EPIC array.
- Proteomics: Normalized, imputed protein abundance data. Ensure the matrices are linked by a common sample identifier.
- Model Training: Use the MOFA2 R package to train the model. The algorithm will decompose the multi-omics data into a set of latent factors that capture the major axes of variation [63].
- Downstream Analysis:
- Factor Interpretation: Correlate the inferred factors with known sample covariates (e.g., VUS status, clinical severity). A factor strongly associated with VUS carrier status is of high interest.
- Feature Inspection: Examine the "weights" of the omics features (genes, proteins, CpG sites) that drive this factor. Overlap these top-weighted features with known pathogenic pathways [65] [63].
The path from data integration to biological insight and final VUS interpretation relies on synthesizing evidence from all omics layers, as shown in the following decision pathway:
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table catalogs key reagents and computational tools critical for executing the multi-omics workflows described in this guide.
| Category | Item/Reagent | Function & Application Note |
|---|---|---|
| Wet-Lab Reagents | DNase I Treatment Kit | Critical for RNA extraction to remove genomic DNA contamination prior to RNA-seq. |
| TruSeq Stranded mRNA Library Prep Kit | Prepares sequencing libraries from poly-A RNA for transcriptomic analysis on Illumina platforms. | |
| Infinium MethylationEPIC Kit | Industry-standard array for cost-effective, genome-wide DNA methylation profiling. | |
| EZ DNA Methylation Kit | Enables bisulfite conversion of DNA, a crucial step for methylation analysis. | |
| Bioinformatics Tools | STAR Aligner | Splice-aware aligner for accurately mapping RNA-seq reads to the reference genome [60]. |
| minfi R/Bioconductor Package | Comprehensive suite for preprocessing, normalization, and analysis of Illumina methylation arrays [62]. | |
| MOFA2 | Leading tool for unsupervised integration of multiple omics datasets to discover latent factors [63]. | |
| rMATS | Detects differential splicing events from RNA-seq data, crucial for assessing VUS impact [60]. | |
| SpliceAI | Deep learning model for predicting the impact of DNA sequence variants on pre-mRNA splicing; used for in silico prioritization [66]. | |
| Reference Databases | GTEx Portal | Provides context on normal tissue-specific gene expression, helping to assess if a VUS alters expression beyond normal ranges [60]. |
| ClinVar | Public archive of reports on genotype-phenotype relationships; used for comparing VUS with known pathogenic/benign variants. | |
| Precyasterone | Precyasterone, MF:C29H44O8, MW:520.7 g/mol | Chemical Reagent |
| Hapepunine | Hapepunine, MF:C28H47NO2, MW:429.7 g/mol | Chemical Reagent |
Troubleshooting VUS Interpretation and Strategies for Optimization
FAQs on Common Research Pitfalls
FAQ 1: What are the primary challenges in managing Variants of Uncertain Significance (VUS) in POI research, and what is their clinical impact? A significant challenge is the systematic gap in communicating updated variant classifications to patients and providers. A recent study found that at least 1.6% of variant classifications used in Electronic Health Records (EHRs) for clinical care were outdated compared to the current classifications in ClinVar. Furthermore, the study identified 26 instances where a testing laboratory had updated a variant's classification in ClinVar but never communicated this reclassification to the patient or the ordering provider [67] [68]. This failure in the communication loop creates a direct risk for clinical decision-making based on obsolete information. The burden of VUS is also not evenly distributed; reporting can vary by over 14-fold depending on the primary indication for genetic testing and 3-fold depending on a patient's self-reported race, highlighting critical disparities in genomic medicine [67].
FAQ 2: How can researchers mitigate the risk of evidence overlap and confounding when integrating data from randomized trials and observational studies for POI? Integrating causal inference methods is key to mitigating confounding and selection bias in observational data. A framework developed for comparative effectiveness research demonstrates the utility of using advanced statistical techniques—such as regression modeling, inverse probability of treatment weighting, and optimal full propensity matching—to adjust for non-randomization in observational data [69]. When these methods were applied, they produced essentially equivalent survival plots and similar comparative effectiveness conclusions, suggesting they can help reconcile differences between observational and RCT findings. Furthermore, combining individual-level data from registries with published study-level RCT results in a cumulative network meta-analysis can increase the precision of effect estimates (e.g., Hazard Ratios) and strengthen the credibility of conclusions [69].
FAQ 3: What are the consequences of poor participant recruitment planning in clinical trials, and how can they be avoided? Poor recruitment planning is a major source of waste in clinical research. An economic model showed that the financial consequences of overestimating recruitment rates are dramatic. Trials that required more sites or time extensions needed at least AUD $600,000 in additional funding (50% above budget), while incomplete trials cost over AUD $2 million more than planned (260% above budget) [70]. The core of the solution is to accurately assess recruitment rates during the trial planning phase. This involves realistically estimating the probabilities of patient eligibility and consent, which directly determine the recruitment rate per site and the variable cost of recruiting each participant [70].
FAQ 4: Beyond genetic causes, what other key etiological factors should be considered in POI research to avoid data gaps? While genetic factors account for about 20-25% of POI cases, researchers must consider a broader etiological landscape to avoid critical data gaps [71]. Key factors include:
- Iatrogenic Causes: Accounting for roughly 25% of cases, these include chemotherapy (e.g., alkylating agents like cyclophosphamide), radiotherapy, and pelvic surgeries that can impair ovarian blood supply or directly damage follicles [72] [71].
- Autoimmune Causes: Associated with approximately 4-30% of spontaneous POI cases. Common conditions include Hashimoto's thyroiditis, Addison's disease, and systemic lupus erythematosus [71].
- Environmental Toxicants (ETs): A growing area of concern, exposure to substances like atmospheric particulate matter, endocrine-disrupting chemicals (e.g., phthalates), pesticides, and heavy metals can contribute to POI through mechanisms such as oxidative stress and DNA damage in oocytes [71].
Troubleshooting Guides
Guide 1: Implementing a System for Tracking VUS Reclassifications
- Problem: Outdated VUS classifications in clinical and research datasets lead to "imprecision medicine."
- Protocol: Proactive VUS Management Workflow
- Centralized Aggregation: Create a local database, modeled on resources like the Brotman Baty Institute Clinical Variant Database (BBI-CVD), that links EHR data with genetic testing reports from multiple laboratories [67] [68].
- Scheduled Re-interrogation: Establish a protocol to re-check the classification of all VUS in your cohort against updated databases like ClinVar on a regular (e.g., annual) basis.
- Automated Flagging: Where possible, implement automated systems to flag discrepancies between local EHR classifications and the current consensus classification in ClinVar.
- Defined Communication Pathway: Move beyond a vague "shared responsibility" model. Create a formal Standard Operating Procedure (SOP) that clearly designates who is responsible for communicating a reclassification (e.g., the principal geneticist or study coordinator) and how it will be documented and delivered to the patient and their provider [68].
The following diagram illustrates this proactive workflow for managing VUS reclassifications:
Guide 2: Integrating Diverse Data Types to Address Evidence Gaps in POI
- Problem: POI has a heterogeneous etiology, and relying on a single data type (e.g., genetic only) leads to incomplete understanding.
- Protocol: Multi-Modal Data Integration Framework
- Systematic Data Collection: For a study cohort, systematically gather not only genetic data but also structured clinical history (e.g., autoimmune conditions, chemotherapy exposure), lifestyle questionnaires, and, where feasible, biospecimens for evaluating exposure to environmental toxicants [71].
- Apply Causal Inference Methods: When analyzing observational data from this cohort, use statistical methods to control for confounding. For example, apply Inverse Probability of Treatment Weighting (IPTW) to create a pseudo-population where the distribution of measured confounders (e.g., age, BMI) is balanced across exposure groups, allowing for a less biased estimate of the effect of a specific exposure on POI risk [69].
- Evidence Synthesis: Conduct a network meta-analysis that incorporates your own individual-level patient data (IPD) with published study-level data from both RCTs and observational studies. This synthesis allows for direct and indirect comparisons of factors associated with POI, strengthening the validity and credibility of the findings by increasing the precision of estimates [69].
The diagram below outlines this integrated approach to evidence generation:
Data Presentation
Table 1: Quantitative Insights into VUS and POI Etiology
| Data Category | Specific Finding | Quantitative Measure | Implication for Research |
|---|---|---|---|
| VUS Reporting Disparities | Variation by testing indication | >14-fold difference | Research cohorts must be well-phenotyped to avoid biased VUS interpretation [67]. |
| VUS Reporting Disparities | Variation by self-reported race | 3-fold difference | Highlights urgent need for diverse genetic databases to ensure equity [67]. |
| VUS Data Integrity | Outdated classifications in EHRs | 1.6% | Underscores the necessity of proactive variant re-evaluation protocols [67] [68]. |
| POI Etiology | Genetic causes | ~20-25% | Reinforces the importance of comprehensive genetic testing in idiopathic cases [71]. |
| POI Etiology | Iatrogenic causes | ~25% | Suggests study designs should carefully account for medical history [71]. |
| POI Etiology | Autoimmune causes | 4-30% | Indicates screening for autoimmune comorbidities is crucial in clinical workups [71]. |
Table 2: Essential Research Reagent Solutions for POI and VUS Studies
| Reagent / Solution | Primary Function in Research | Key Considerations |
|---|---|---|
| Multi-Gene Panels (POI-focused) | Identifies pathogenic variants and VUS in genes known to be associated with ovarian function (e.g., FMR1, BMP15) [72] [71]. | Should include genes involved in gonadogenesis, meiosis, follicular development, and DNA repair [71]. |
| ClinVar Database | Public archive used to report and interpret variants; critical for assessing the current classification of a VUS [67]. | Classifications can be updated; requires regular checking. Does not solve the "last mile" communication problem [67] [68]. |
| Electronic Health Record (EHR) | Source of rich phenotypic data needed to correlate genetic findings (like a VUS) with clinical presentation [67]. | Data is often unstructured. Linking EHRs to variant databases (BBI-CVD) facilitates cohort analysis [67]. |
| Validated Clinical Data Management Software | Pre-validated electronic data capture (EDC) systems designed to meet regulatory requirements (ISO 14155:2020) for clinical trials [73]. | Prefer systems with APIs (open systems) to allow seamless data transfer between EDC, CTMS, and other tools, reducing manual errors [73]. |
| Assays for Environmental Toxicants | Measures exposure to ETs (e.g., phthalates, heavy metals) that can contribute to POI pathogenesis via oxidative stress and DNA damage [71]. | Allows researchers to investigate the interaction between genetic susceptibility and environmental exposures. |
Experimental Protocols
Protocol 1: Validated Electronic Data Capture for Clinical Studies
- Objective: To ensure clinical data collection meets regulatory standards and minimizes errors, thereby addressing data integrity pitfalls.
- Methodology:
- System Selection: Invest in a purpose-built, pre-validated clinical data management solution instead of general-purpose tools like spreadsheets. The system must comply with standards such as ISO 14155:2020 (section 7.8.3), which requires validation of electronic systems for authenticity, accuracy, reliability, and consistent intended performance [73].
- Workflow Integration: Test the study design and data collection tools within the real-world clinical workflows of the sites involved. This involves consulting with end-users (e.g., clinical research coordinators) to ensure the protocol is feasible in their environment (e.g., confirming if tablets can be used in an operating theater) [73].
- Access Control Management: Implement and document strict user roles and permissions within the EDC system. Establish a Standard Operating Procedure (SOP) for promptly revoking system access when personnel leave the study or change roles [73].
Protocol 2: Analyzing DNA Damage in Ovarian Cells for POI Pathogenesis
- Objective: To investigate the contribution of DNA damage, a key pathological mechanism in POI, induced by factors like chemotherapeutic agents or environmental toxicants.
- Methodology:
- Model System Selection: Use appropriate in vitro (e.g., cultured ovarian granulosa cells) or in vivo (e.g., mouse model) systems.
- Induction of Damage: Treat the model system with a POI-relevant stressor. Examples from literature include:
- Detection of DNA Damage: Employ a standard assay to quantify DNA damage. The γ-H2AX immunofluorescence assay is a gold standard for identifying and counting DNA DSBs. Alternatively, comet assays can be used to measure general DNA strand breaks.
- Correlation with Outcome: Correlate the extent of DNA damage with markers of ovarian dysfunction, such as increased apoptosis of oocytes or granulosa cells, reduced hormone production, or accelerated depletion of the primordial follicle pool [71].
FAQ: What is ancestral bias in genomic datasets and why is it a critical issue in POI research?
Ancestral bias refers to the severe under-representation of non-European populations in genomic databases [74] [75]. This inequity limits our understanding of human disease and leads to disparities in precision medicine effectiveness across ethnic groups [74]. In Premature Ovarian Insufficiency (POI) research, this bias is particularly problematic because POI is a highly heterogeneous condition with significant genetic components [11] [26]. When databases lack diversity, researchers cannot adequately interpret Variants of Uncertain Significance (VUS) across different ancestral backgrounds, potentially missing disease-causing variants unique to underrepresented populations or misclassifying benign population-specific variants as pathogenic.
FAQ: How does ancestral bias specifically impact VUS interpretation in POI genetics?
The interpretation of VUS depends heavily on population frequency data. Variants that are rare in European populations but common in other ancestral groups may be incorrectly classified as pathogenic when found in underrepresented populations [74]. POI research has identified over 50 gene mutations associated with the condition, impacting processes including gonadal development, DNA replication/meiosis, DNA repair, and mitochondrial function [11]. However, these findings primarily stem from European-centric datasets, creating blind spots in our understanding of POI genetics across global populations.
Table: Global Representation in Genomic Databases
| Region/Ancestry | Representation in Genomic Databases | Impact on POI Research |
|---|---|---|
| European | Dramatically over-represented (95% in GWAS Catalog) [74] | Reference standard, but limited generalizability |
| African | Severely under-represented (~5% of transcriptomic data) [74] | Missed insights despite greater genetic diversity [74] |
| Middle Eastern/North African | Limited regional data aggregation [75] | Under-characterized POI variants in consanguineous populations [76] |
| Asian (Various) | Variable representation [75] | Population-specific variants potentially misclassified |
Technical Challenges & Methodological Solutions
Troubleshooting Guide: Addressing Ancestral Bias in Your POI Research
Problem: How can I improve VUS classification in POI patients from underrepresented ancestral backgrounds?
Solution: Implement computational methods that adjust for ancestral bias and incorporate diverse reference data.
Experimental Protocol: Utilizing PhyloFrame for Equitable Genomic Analysis
PhyloFrame is a machine learning method that corrects for ancestral bias by integrating functional interaction networks and population genomics data with transcriptomic training data [74] [77]. The methodology proceeds as follows:
Initial Disease Signature Generation: Use logistic regression with LASSO penalty to obtain an initial set of POI-relevant genes from available transcriptomic data [77].
Network Projection: Project the initial disease signature onto a functional interaction network, extending the network to include first and second neighbors of each signature gene [77].
Ancestral Diversity Filtering: Filter this new gene set using Enhanced Allele Frequency (EAF), a statistic that captures population-specific allelic enrichment in healthy tissue [74]. EAF identifies which individuals from a population are more likely to have a variant than individuals from all other ancestries.
Signature Expansion: From each ancestry, select a subset of genes with high EAF and gene expression variability in the training data to add to the PhyloFrame signature [77].
Model Retraining: Retrain the model with forced inclusion of these equitable genes, resulting in a disease signature that generalizes to all populations, even those not represented in the training data [77].
FAQ: What is the difference between race and genetic ancestry in POI research context?
Race is a social construct based on self-identification or social categorization, while genetic ancestry refers to the genetic heritage and composition of an individual [78]. A massive NIH study from 2025 demonstrated that self-reported racial categories differ markedly from people's genetic makeup [78]. For POI research, this distinction is critical because:
- Using race as a proxy for genetic ancestry can lead to inaccurate VUS interpretations
- Environmental and social factors associated with race may confound genetic associations
- Admixed individuals (with ancestry from multiple populations) cannot be sufficiently represented by single-ancestry medical models [74]
The NIH study recommends: "Biomedical research should adjust directly for ancestries estimated from genetic data rather than relying on self-identified race or ethnicity" [78].
Implementation Strategies & Research Reagents
Research Reagent Solutions for Diverse Genomic Studies
Table: Essential Resources for Ancestrally-Aware POI Research
| Resource Type | Specific Tool/Database | Function in POI/VUS Research |
|---|---|---|
| Equitable ML Tools | PhyloFrame [74] [77] | Creates ancestry-aware disease signatures that generalize across populations |
| Population Databases | gnomAD [26] [76] | Provides allele frequency across diverse populations for VUS interpretation |
| Variant Classification | ACMG/AMP Guidelines [29] [76] | Standardized framework for pathogenicity assessment |
| Functional Validation | Cell culture models (e.g., FSHR mutation studies) [29] | Experimental confirmation of variant impact on protein function |
| Data Diversity Frameworks | GA4GH Diversity in Datasets [79] | Policy framework promoting global diversity in genomic research |
Troubleshooting Guide: Implementing Diverse Recruitment Strategies
Problem: How can I improve diversity in my POI research cohort when working with limited resources?
Solution: Implement targeted strategies based on your region's genomic maturity level [75].
Protocol for High Maturity Regions (e.g., US, UK, EU):
- Establish community advisory boards including indigenous and minority representatives [75]
- Implement alternative recruitment methods (e.g., mobile blood collection units) [75]
- Provide clear "return on investment" to participants regarding data usage and benefits [75]
Protocol for Medium/Low Maturity Regions (e.g., Brazil, Uganda, Thailand):
- Focus on building local infrastructure and retaining local expertise [75]
- Develop education and training in bioinformatics and data interpretation [75]
- Address historical trust issues through transparent engagement [75]
Data Analysis & Interpretation Framework
FAQ: How do I properly contextualize POI genetic findings across diverse populations?
Solution: Implement a standardized framework for cross-ancestral genetic interpretation.
Experimental Protocol: Ancestrally-Aware VUS Classification for POI Genes
Variant Frequency Assessment: Check allele frequencies across diverse populations in gnomAD, emphasizing population-specific rather than aggregate frequencies [76].
Functional Domain Mapping: Determine if the variant occurs in a known functional domain of POI-associated genes (e.g., FSHR ligand-binding domain) [29].
Experimental Validation: Implement functional studies similar to FSHR mutation characterization:
Segregation Analysis: Confirm co-segregation with POI phenotype in families, noting inheritance patterns (e.g., biallelic FSHR mutations causing recessive POI) [29].
ACMG Classification Integration: Synthesize evidence using standardized ACMG/AMP guidelines, documenting population data as key evidence [26] [76].
Table: POI Genetic Findings Across Diverse Populations
| Genetic Aspect | European Populations | Underrepresented Populations | Implications for VUS Interpretation |
|---|---|---|---|
| Known POI Genes | 59 genes with P/LP variants [26] | Limited characterization in MENA region (79 variants in 25 genes) [76] | Potential novel genes undetected in European populations |
| Variant Spectrum | 18.7% of cases have P/LP variants [26] | 19 pathogenic/likely pathogenic variants identified in MENA region [76] | Different variant profiles may exist across populations |
| Phenotypic Correlation | Higher genetic contribution in primary (25.8%) vs secondary (17.8%) amenorrhea [26] | No clear phenotype-genotype association in MENA region [76] | Ancestry may influence phenotypic expression |
Troubleshooting Guide: Handling Incomplete or Biased Reference Data
Problem: How should I proceed when reference populations lack diversity for my POI gene of interest?
Solution: Implement a cautious interpretation framework with clear limitations statements.
Explicitly Acknowledge Data Gaps: Document the ancestral composition of reference databases used and note populations with insufficient representation.
Leverage Multiple Prediction Tools: Use concordance across different computational prediction algorithms when population frequency data is lacking [29].
Prioritize Functional Studies: For high-priority VUS in clinically suspected genetic POI cases, invest in functional validation rather than relying solely on computational predictions [29].
Report Ancestry-Specific Uncertainties: Clearly communicate to clinicians that VUS interpretations may have different confidence levels across ancestral backgrounds.
The progressive integration of these equitable approaches will enhance the precision and global applicability of POI genetic research, ultimately benefiting patients across all ancestral backgrounds through improved diagnosis and personalized management strategies.
FAQs: Understanding the SPCV4 Framework and VUS Subclassification
What is the SPCV4 framework and how does it differ from previous ACMG/AMP guidelines?
The SPCV4 (Standards and Guidelines for the Interpretation of Sequence Variants, version 4) framework represents a major overhaul of the 2015 ACMG/AMP variant classification guidelines. Key improvements include a Bayesian, points-based system that provides clearer rules to avoid double-counting evidence and introduces VUS subclasses (low, mid, high). This updated system is currently in pilot testing across 30 laboratories and addresses many limitations of the previous guidelines, particularly the overly broad VUS category that spanned an SA0% confidence range for pathogenicity [80] [81].
Why is VUS subclassification important in POI research and clinical diagnostics?
VUS subclassification is crucial because not all VUS have the same probability of being reclassified as pathogenic or benign. Research across four clinical laboratories reveals distinct reclassification patterns: VUS-low variants almost never progress to pathogenic, while VUS-high variants are most likely to be reclassified, with almost half ultimately becoming pathogenic. This distinction helps prioritize investigative resources and can inform clinical decision-making, even while acknowledging the inherent uncertainty [80] [82]. In POI research, where genetic heterogeneity is high, this allows researchers to focus on the most promising variants.
How should researchers handle different VUS subclasses in POI gene discovery?
The evidence level should guide the investment in follow-up investigations. VUS-high variants warrant prioritization for functional studies, segregation analysis in families, and deeper phenotyping. VUS-low variants generally require less urgent investment. Some laboratories have adopted reporting practices where VUS-low variants are not reported in certain contexts, such as healthy population screening, while VUS-high and VUS-mid are reported as a single VUS category, though practices vary by institution [81].
What constitutes evidence for assigning VUS subclasses?
The subclasses are defined by the strength and direction of available evidence [81]:
- VUS-high: Evidence suggests pathogenicity but falls short of "Likely Pathogenic."
- VUS-low: Evidence suggests a benign role but is insufficient for "Likely Benign."
- VUS-mid: Equivocal with conflicting evidence or no evidence at all.
What are the proven rates of VUS reclassification between subclasses?
Data aggregated from multiple clinical laboratories demonstrate distinct reclassification odds [82] [81]:
Table: VUS Reclassification Rates by Subclass
| VUS Subclass | Reclassification to Pathogenic/Likely Pathogenic | Reclassification to Benign/Likely Benign | Key Findings |
|---|---|---|---|
| VUS-low | Never observed | Variable | "VUS-low almost never moves to pathogenic" [80] |
| VUS-mid | Low to moderate | Low to moderate | Equivocal reclassification pattern |
| VUS-high | Highest rate (~50% in one dataset) | Low | "Almost half of those ultimately become pathogenic" [80] |
Experimental Protocols for VUS Resolution in POI
Protocol 1: Functional Validation of POI-Associated VUS Using In Vitro Assays
This protocol outlines a standard approach for generating functional evidence (ACMG/AMP PS3 code) to resolve VUS in novel POI candidate genes.
Materials and Reagents:
- Expression vectors
- Site-directed mutagenesis kit
- Cell line (e.g., 293FT)
- Transfection reagent
- Antibodies for Western Blot
- RNA extraction kit
- RNA-Seq library prep kit
Methodology:
- Variant Modeling: Introduce the candidate VUS into an appropriate expression vector containing the wild-type cDNA using site-directed mutagenesis [15].
- Cell Transfection: Transfect both wild-type and mutant constructs into a suitable cell line (e.g., 293FT) in parallel with an empty vector control.
- Protein Analysis: Perform Western blot analysis to assess whether the variant affects protein stability or expression levels. Quantify band intensity normalized to a loading control like GAPDH [15].
- Transcriptomic Analysis: Extract total RNA from transfected cells and perform RNA sequencing. Use tools like DESeq2 to identify differentially expressed genes. Analyze alternative splicing events using software like rMATS [15].
- Pathway Enrichment: Subject the list of differentially expressed genes to Gene Ontology (GO) analysis and pathway overrepresentation tests to determine affected biological processes.
Protocol 2: Clinical and Genetic Data Integration for VUS Interpretation
This protocol describes the collection of clinical and genetic data necessary to apply phenotype-specificity (PP4) evidence for VUS in a POI context.
Materials and Reagents:
- Patient phenotypic data
- Family history
- Hormonal assay results (FSH, AMH)
- Ultrasound data
- Genomic DNA
- WES or gene panel kit
Methodology:
- Deep Phenotyping: Systematically collect and record detailed patient information, including type of amenorrhea (primary or secondary), age at diagnosis, family history of POI, and hormone levels (FSH, AMH). Transvaginal ultrasound for antral follicle count is also recommended [16].
- Genetic Analysis: Perform targeted gene panel, whole-exome, or whole-genome sequencing. Focus on a curated list of known and candidate POI genes [16] [26].
- Variant Classification: Annotate and filter variants using population frequency databases (e.g., gnomAD). Classify variants according to ACMG/AMP guidelines and, if possible, assign VUS subclasses based on available evidence [16] [19].
- Phenotype-Genotype Correlation: Correlate the patient's specific phenotype with the known gene function and inheritance pattern. Strong phenotype-genotype correlation can provide moderate evidence (PP4) for pathogenicity [83].
Signaling Pathways and Experimental Workflows
VUS Resolution Workflow in POI Research
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Resources for VUS Investigation in POI
| Resource Category | Specific Tool / Database | Primary Function in VUS Resolution |
|---|---|---|
| Variant Databases | ClinVar [80] [83] | Public archive of variant interpretations and clinical significance |
| gnomAD [80] [83] | Assess allele frequency in general populations to filter common polymorphisms | |
| Computational Predictors | REVEL & AlphaMissense [80] | In silico prediction of variant deleteriousness using advanced algorithms |
| CADD [26] | Integrative score predicting variant pathogenicity | |
| Functional Assay Platforms | MAVE (Multiplex Assays of Variant Effect) [80] | Large-scale functional measurements for thousands of variants simultaneously |
| Mini-gene Splicing Assays [55] | In vitro method to determine if a variant disrupts normal mRNA splicing | |
| Data Sharing Networks | GeneMatcher / VariantMatcher [80] | Matchmaking platforms to find other researchers or clinicians with interest in the same gene or variant |
| GA4GH (Global Alliance) [80] | Develops frameworks and standards for responsible genomic data sharing | |
| Classification Tools | ACMG/AMP & SPCV4 Guidelines [80] [19] | Standardized evidence-based framework for variant pathogenicity classification |
| quadranoside III | Quadranoside III|C36H58O11|Research Compound |
Frequently Asked Questions
Q1: What are the core functions of ClinGen and ClinVar, and how do they differ?
A: ClinGen and ClinVar are complementary NIH-funded resources with distinct roles in genomic medicine. ClinGen is dedicated to building an authoritative central resource that defines the clinical relevance of genes and variants through expert curation. Its key goals are to aggregate relevant data, curate genes and variants through expert panels, disseminate resources, and continuously evaluate and improve its processes [84]. In contrast, ClinVar is a public archive that collects reports of variant associations with clinical phenotypes and assertions about clinical significance submitted by laboratories, researchers, and other groups [85]. ClinGen expert panels use ClinVar as a source of variant data and subsequently submit their standardized expert interpretations back to ClinVar, creating a critical partnership for improving genomic knowledge [86] [85].
Q2: What standard classification terms does ClinVar use for germline and somatic variants?
A: ClinVar uses standardized classification terms based on authoritative sources. For germline variants in Mendelian diseases, it uses the five ACMG/AMP recommended terms: Pathogenic, Likely Pathogenic, Uncertain Significance, Likely Benign, and Benign. Additionally, for low penetrance variants and risk alleles, ClinVar uses ClinGen-recommended terms including "Pathogenic, low penetrance," "Likely pathogenic, low penetrance," "Uncertain risk allele," "Likely risk allele," and "Established risk allele" [87]. For somatic variants, ClinVar supports two classification types: clinical impact (using AMP/ASCO/CAP tiered system: Tier I - Strong, Tier II - Potential, Tier III - Uncertain significance, Tier IV - Benign/likely benign) and oncogenicity (using ClinGen/CGC/VICC terms: Oncogenic, Likely Oncogenic, Uncertain Significance, Likely Benign, Benign) [87].
Table: Standard Variant Classification Terms in ClinVar
| Variant Type | Classification System | Standard Terms |
|---|---|---|
| Germline | ACMG/AMP | Pathogenic, Likely Pathogenic, Uncertain Significance, Likely Benign, Benign [87] |
| Germline (Low Penetrance) | ClinGen | Pathogenic/Likely Pathogenic (low penetrance), Uncertain/Likely/Established Risk Allele [87] |
| Somatic (Clinical Impact) | AMP/ASCO/CAP | Tier I (Strong), Tier II (Potential), Tier III (Uncertain Significance), Tier IV (Benign/Likely Benign) [87] |
| Somatic (Oncogenicity) | ClinGen/CGC/VICC | Oncogenic, Likely Oncogenic, Uncertain Significance, Likely Benign, Benign [87] |
Q3: How does the Matchmaker Exchange facilitate gene discovery for rare diseases?
A: The Matchmaker Exchange (MME) addresses the challenge of rare disease gene discovery through a federated network connecting databases of genotypes and phenotypes using a common API (Application Programming Interface) [88]. This platform enables researchers to find additional cases with similar genotypic and phenotypic profiles across multiple databases without needing to deposit data in each one separately. Unlike centralized databases, MME's federated approach allows each database to maintain autonomy over its data schema and control, while still participating in a global network. The core function is to help researchers identify additional unrelated cases with deleterious variants in the same gene and overlapping phenotypes, which can provide sufficient evidence to causally implicate a gene in disease [88].
Q4: What are common challenges when interpreting Variants of Uncertain Significance (VUS) in POI research?
A: Interpreting VUS presents several challenges, particularly for conditions like Primary Ovarian Insufficiency (POI). First, there is often insufficient evidence from functional assays, population frequency data, or segregation analysis. Second, restricted access to global data means critical evidence might be siloed in individual research or clinical databases. Third, limitations of automated interpretation tools - while these tools demonstrate high accuracy for clearly pathogenic/benign variants, they show significant limitations with VUS and still require expert oversight [18]. Additionally, there may be conflicting interpretations between different laboratories or resources, requiring expert resolution through efforts like ClinGen's Expert Panels [85].
Q5: What steps should I take if I find conflicting variant interpretations in ClinVar?
A: When encountering conflicting interpretations in ClinVar, first examine the review status of each submission. ClinVar aggregates classifications with precedence given to submissions with higher review status levels, with "practice guideline" (4 stars) being the highest [87]. Second, check if the variant has been reviewed by a ClinGen Expert Panel, as these assertions represent expert-curated consensus interpretations. Third, contribute your own evidence by submitting your variant classification with supporting evidence to ClinVar, which will help highlight the conflict and prompt expert review [87]. Finally, leage ClinGen's resolution efforts - ClinGen has specific processes where expert panels work with clinical laboratories to resolve differences in variant interpretation [85].
Troubleshooting Guides
Problem: Inconsistent automated interpretation results for a VUS Solution:
- Verify the input data quality and completeness, including precise variant representation and patient phenotype information using standardized ontologies like HPO [49].
- Utilize multiple interpretation tools and compare results rather than relying on a single tool [18].
- Supplement automated predictions with manual curation following ACMG/AMP guidelines and relevant ClinGen specifications [18] [86].
- Search for additional cases through Matchmaker Exchange to identify patients with similar genotype-phenotype combinations [88].
Problem: Unable to find matching cases for a candidate gene in rare disease research Solution:
- Ensure comprehensive phenotypic characterization using standardized ontologies (HPO) to improve matching accuracy [49] [88].
- Submit your case to multiple Matchmaker Exchange services through a single API connection, as different services may have different specialized databases [88].
- Verify that your candidate gene is correctly specified and that variant data includes necessary details (zygosity, inheritance pattern, variant type) [88].
- Participate in ClinGen's expert curation groups or utilize their Gene Curation Interface to assess the validity of gene-disease relationships [86].
Problem: Difficulty navigating between different genomic resources and platforms Solution:
- Utilize ClinGen's Allele Registry (CAR) to obtain unique variant identifiers that can be used across resources [86].
- Leverage the Data Exchange standards developed by ClinGen, which provide standardized data models and tools for genomic knowledge sharing [86].
- Use the common API developed by the Global Alliance for Genomics and Health (GA4GH) that enables interoperability between platforms like ClinGen, ClinVar, and Matchmaker Exchange [88] [85].
Experimental Protocols & Workflows
Protocol 1: Comprehensive VUS Interpretation Pipeline for POI Research
Purpose: To systematically interpret Variants of Uncertain Significance in Primary Ovarian Insufficiency research using global data sharing resources.
Materials:
- Patient genomic data (WES or WGS recommended for rare disease analysis)
- Phenotypic data structured using Human Phenotype Ontology (HPO) terms
- Access to ClinVar for existing variant interpretations
- ClinGen Pathogenicity Calculator for ACMG/AMP guideline implementation
- Matchmaker Exchange API for identifying similar cases
- Population frequency databases (gnomAD, 1000 Genomes)
Procedure:
- Data Collection & Quality Assessment
- Collect comprehensive patient information including clinical history, family history, and genetic reports [83].
- Perform quality control on sequencing data, checking for coverage, alignment quality, and potential contamination [49].
- Annotate variants using standardized nomenclature (HGVS) and functional impact predictors [49].
Variant Prioritization & Filtering
- Filter variants based on population frequency (e.g., exclude variants with frequency >0.1% in gnomAD for rare disorders).
- Prioritize variants based on predicted functional impact and gene relevance to reproductive disorders.
- Identify candidate VUS through inheritance pattern analysis and phenotype match.
Evidence Collection & Integration
- Query ClinVar for existing interpretations and conflicting assertions [87] [85].
- Search ClinGen's Evidence Repository for structured variant-level evidence [86].
- Submit query to Matchmaker Exchange to identify cases with similar genotype-phenotype profiles [88].
- Collect functional evidence from literature and databases.
Classification & Interpretation
- Apply ACMG/AMP guidelines using ClinGen's Pathogenicity Calculator [86].
- Consider gene-specific guidelines from ClinGen's Expert Panels where available.
- Resolve conflicting evidence through weighted evaluation based on evidence strength.
Data Sharing & Collaboration
Protocol 2: Matchmaker Exchange Utilization for Gene-Disease Validation
Purpose: To utilize the Matchmaker Exchange platform for building evidence for novel gene-disease associations in POI research.
Materials:
- Candidate gene(s) with suspected but unproven association with POI
- Detailed phenotypic data using HPO terms
- Genomic variant data in standardized format
- Access to MME-compliant services (such as GeneMatcher, MyGene2, or DECIPHER)
- Institutional approval for data sharing
Procedure:
- Data Preparation
- Structure case data according to MME API specifications, including case ID, submitter information, candidate gene(s), and phenotypic features [88].
- Include additional optional fields to increase specificity: gender, age of onset, inheritance pattern, condition name (OMIM/Orphanet ID), zygosity, and variant type [88].
Service Selection & Data Submission
- Select appropriate MME service based on specialization and focus areas.
- Submit case data to initiating MME service, ensuring compliance with data sharing agreements and privacy requirements.
Federated Query Execution
- The initiating service automatically distributes queries to connected MME services through the standardized API [88].
- Each receiving service applies its own matching algorithms to identify similar cases based on genotypic and phenotypic profiles.
Match Analysis & Validation
- Review matches returned through the federated query system.
- Follow MME User Agreement requirements: no attempt to identify individual patients, obtain permission before publishing results, and acknowledge MME in publications [88].
- Contact submitters of matching cases to collaborate on further validation.
Evidence Integration & Interpretation
- Combine evidence from multiple matching cases to build case for gene-disease association.
- Submit validated gene-disease relationships to ClinGen for official curation and recognition [86].
Table: Matchmaker Exchange Service Requirements
| Requirement Category | Specific Requirements |
|---|---|
| Technical | Implement standardized MME API, establish minimum 2 point-to-point API connections to other services, successfully implement matching algorithms using test data [88] |
| Content | Contain content useful for matching, ability to flag/prioritize candidate genes, require users to deposit case data to undertake federated queries [88] |
| Administrative | Enable dual notification of data requester and prior data depositor, store queries for auditing and statistics, attest to database security requirements [88] |
| Community | Advance MME goals through active participation, define representative for MME steering committee [88] |
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Resources for Collaborative Variant Interpretation
| Resource | Type | Primary Function | Access Information |
|---|---|---|---|
| ClinGen Pathogenicity Calculator | Software Tool | Enables application of ACMG/AMP guidelines and similar standards for variant classification [86] | Available through ClinGen website |
| ClinGen Evidence Repository | Database | Provides access to variant-level evidence used by ClinGen Expert Panels in variant classification [86] | Publicly accessible online |
| ClinGen Allele Registry (CAR) | Registry Service | Provides unique variant identifiers programmatically via APIs to facilitate cross-database queries [86] | Available through ClinGen website |
| Matchmaker Exchange API | Programming Interface | Standardized protocol for exchanging genotypic and phenotypic information between rare disease databases [88] | Implemented by MME services (GeneMatcher, MyGene2, etc.) |
| Variant Curation Interface (VCI) | Curation Platform | Supports ClinGen's variant curation process combining clinical, genetic, population, and functional evidence with expert review [86] | Available to ClinGen curators and expert panels |
| ClinVar Submission Portal | Data Submission | Allows laboratories and researchers to submit variant interpretations to the public archive [87] | NCBI website |
| Human Phenotype Ontology (HPO) | Standardized Vocabulary | Provides standardized terms for describing phenotypic abnormalities to enable semantic similarity matching [49] | http://www.human-phenotype-ontology.org |
Operationalizing Segregation Analysis and Family Studies for Evidence Generation
FAQs: Addressing Common Challenges in VUS Interpretation for POI
FAQ 1: What is the first step after identifying a Variant of Uncertain Significance (VUS) in a POI patient? The initial step involves comprehensive validation and segregation analysis. Begin by confirming the variant using an orthogonal method, such as Sanger sequencing, to rule out next-generation sequencing (NGS) errors [29]. Subsequently, perform family segregation studies by testing the variant in available family members. This helps determine if the variant co-segregates with the POI phenotype, which provides critical evidence for pathogenicity assessment.
FAQ 2: How can I determine if a VUS is contributing to Premature Ovarian Insufficiency? A multi-line evidence approach is required. This includes:
- Computational Prediction: Utilize in silico tools to predict the variant's impact on protein function.
- Segregation Analysis: Assess if the variant tracks with the disease in the family.
- Functional Studies: Perform in vitro assays to test the biological impact of the variant, such as measuring cell surface expression or downstream signaling activity [29]. The American College of Medical Genetics (ACMG) guidelines integrate these evidence types for classification [89].
FAQ 3: What functional assays are most relevant for POI-related VUS in genes like FSHR? For genes involved in hormonal signaling, such as the Follicle-Stimulating Hormone Receptor (FSHR), key functional assays include:
- Cell Surface Expression Analysis: Transfect cells with plasmids carrying the mutant allele and use flow cytometry or immunoblotting to quantify receptor expression levels. Pathogenic variants often show a marked reduction (e.g., >90%) in cell surface expression [29].
- Signal Transduction Assays: Measure downstream second messengers like cyclic AMP (cAMP) production in response to FSH stimulation. A significant reduction (e.g., 50% lower) in cAMP production indicates impaired receptor functionality [29].
FAQ 4: A VUS was found in a known POI gene, but the patient's phenotype is atypical. How should I proceed? POI is clinically heterogeneous, and genotype-phenotype correlations can be variable. It is essential to:
- Thoroughly re-evaluate the patient's clinical history and family history.
- Consider the possibility of syndromic POI, where ovarian failure is one feature of a broader multi-organ condition [30].
- Explore expanded genetic testing, such as whole-exome sequencing, to investigate variants in other genes that may modify the phenotype or indicate a different diagnosis [26].
FAQ 5: What is the typical diagnostic yield of genetic testing in a POI cohort? The yield varies depending on the cohort and technology used. In large-scale studies, pathogenic and likely pathogenic variants in known POI-causative genes are identified in approximately 18.7% of cases [26]. The yield is higher in patients with primary amenorrhea (25.8%) compared to those with secondary amenorrhea (17.8%) [26]. An overall genetic contribution, including novel candidate genes, can account for up to 23.5% of POI cases [26].
Experimental Protocols for VUS Interpretation
Protocol 1: Familial Segregation Analysis
Objective: To determine if a genetic variant co-segregates with the POI phenotype within a family.
Materials:
- DNA samples from the proband and available family members (parents, siblings, and other affected or unaffected relatives).
- PCR primers flanking the genomic region of the VUS.
- Sanger sequencing reagents or targeted genotyping platform.
Methodology:
- Genotyping: Amplify and sequence the target region from each family member's DNA.
- Phenotype Correlation: Construct a family pedigree and document the POI status (e.g., primary vs. secondary amenorrhea, FSH levels) of each individual.
- Analysis: Analyze the inheritance pattern of the variant. Does it appear in all affected individuals? Is it absent in unaffected family members? For a recessive model, confirm that affected individuals carry biallelic variants [29] [26].
Troubleshooting:
- Incomplete Penetrance: The variant may not manifest in all carriers due to other genetic or environmental modifiers. A detailed family history is crucial.
- Small Family Size: Limited familial samples can reduce the power of segregation analysis. In such cases, functional evidence becomes more critical.
Protocol 2: Functional Characterization of a FSHR VUS
Objective: To assess the functional impact of a VUS in the FSHR gene on receptor expression and signaling.
Workflow Overview:
Materials:
- Plasmids: Plasmids containing the wild-type FSHR sequence, the VUS, and a vector control [29].
- Cell Line: A mammalian cell line suitable for transfection (e.g., HEK293).
- Reagents: FSH hormone, cAMP ELISA kit, antibodies for FSHR detection, transfection reagent.
Methodology:
- Cell Transfection: Transfect cells with equal amounts of the wild-type, mutant, and control plasmids.
- Cell Surface Expression:
- 24-48 hours post-transfection, harvest cells.
- 3a. Use an antibody against FSHR and analyze via flow cytometry. Compare the mean fluorescence intensity of mutant-transfected cells to wild-type controls. A >50% reduction is indicative of a damaging effect [29].
- cAMP Signaling Assay:
- 3b. Stimulate transfected cells with a saturating concentration of FSH.
- Lyse cells and measure intracellular cAMP production using a commercial ELISA kit.
- Normalize cAMP levels to protein concentration and compare the response of mutant FSHR to wild-type. A significant reduction confirms impaired signal transduction [29].
Quantitative Data in POI Genetic Studies
| Category | Number of Cases | Percentage of Cohort | Key Observations |
|---|---|---|---|
| Total with P/LP Variants | 193 | 18.7% | 195 pathogenic/likely pathogenic variants found |
| Monoallelic Variants | 155 | 15.0% | Single heterozygous P/LP variants |
| Biallelic Variants | 24 | 2.3% | Two P/LP variants in the same gene |
| Multiple Heterozygous Variants | 14 | 1.4% | P/LP variants in different genes |
| Primary Amenorrhea (PA) | 31 / 120 | 25.8% | Higher yield, more biallelic/multi-het variants |
| Secondary Amenorrhea (SA) | 162 / 910 | 17.8% | Lower yield compared to PA |
Table 2: Biological Pathways Implicated in POI from Genetic Studies
| Pathway | Example Genes | Proportion of Genetically Explained Cases [26] | Functional Role |
|---|---|---|---|
| Meiosis & DNA Repair | HFM1, SPIDR, BRCA2, MSH4 |
48.7% | Homologous recombination, DNA double-strand break repair |
| Mitochondrial Function | AARS2, POLG, CLPP |
22.3% | Cellular energy production, oxidative phosphorylation |
| Metabolic & Autoimmune | GALT, AIRE |
Included in above | Galactose metabolism, immune tolerance |
| Folliculogenesis | NR5A1, BMP15, GDF9 |
Not specified | Follicle development, growth, and ovulation |
Research Reagent Solutions
Table 3: Essential Reagents for POI Genetic and Functional Studies
| Reagent / Material | Function in Experiment | Specific Application in POI Research |
|---|---|---|
| Whole-Exome Sequencing Kits | Comprehensive identification of coding variants. | Unraveling the molecular etiology in large POI cohorts; identifying novel candidate genes [26]. |
| Custom Targeted Gene Panels | Focused sequencing of known POI-associated genes. | Cost-effective initial screening for established genes like NOBOX, FIGLA, and FSHR [89] [29]. |
| Sanger Sequencing Reagents | Orthogonal validation of NGS findings. | Confirming the presence of a VUS in the proband and for family segregation studies [29]. |
| Mammalian Expression Vectors | Cloning wild-type and mutant gene sequences. | Functional characterization of VUS via in vitro assays (e.g., for FSHR) [29]. |
| cAMP ELISA Kits | Quantifying intracellular cAMP levels. | Measuring downstream FSH receptor signaling activity in transfected cell models [29]. |
| FSH Hormone Preparations | Ligand for receptor activation in functional assays. | Stimulating FSHR in cell-based assays to test the functionality of mutant receptors [29]. |
| Antibodies against FSHR | Detecting receptor protein expression. | Assessing cell surface expression of wild-type vs. mutant FSHR using flow cytometry or Western blot [29]. |
Validation, Clinical Translation, and Comparative Analysis of POI VUS
Frequently Asked Questions
What are the minimum requirements for a functional assay to be considered "well-validated" for clinical variant interpretation?
According to ClinGen recommendations, a well-validated functional assay should demonstrate a clear link to the disease mechanism and undergo rigorous validation. This includes testing a sufficient number of known positive and negative control variants. A minimum of 11 total pathogenic and benign variant controls is recommended to achieve moderate-level evidence. The assay should show high sensitivity and specificity, with validation parameters including experimental design, replication, and appropriate statistical analysis [90].
How can I determine what strength of evidence (PS3/BS3) my functional data can support?
The ClinGen Sequence Variant Interpretation Working Group recommends a four-step framework:
- Define the disease mechanism
- Evaluate the applicability of general assay classes
- Evaluate the validity of specific assay instances
- Apply evidence to individual variant interpretation
The strength of evidence depends on how closely your assay reflects the biological environment and the quality of validation data. Patient-derived material generally provides the strongest evidence, while in vitro systems may require more extensive validation [90].
Our team found a rare missense variant in a POI patient. What experimental approaches can we use to functionally characterize it?
For missense variants in POI-related genes, consider these validated approaches:
- Cell surface expression assays (e.g., for FSHR variants, measure receptor expression via flow cytometry)
- Signal transduction assays (e.g., cAMP production in response to FSH stimulation)
- Patch clamp studies for ion channel genes (e.g., KCNH2 in other systems)
- Multiplex assays of variant effect (MAVEs) for comprehensive variant scanning
A study on FSHR mutations demonstrated 93% reduction in cell surface expression and approximately 50% reduction in cAMP production at saturating FSH concentrations, providing strong functional evidence for pathogenicity [29] [91].
Which pathogenicity prediction tools perform best on rare variants in POI genes?
Recent benchmarking shows that MetaRNN and ClinPred demonstrate the highest predictive power for rare variants. These methods incorporate conservation, multiple prediction scores, and allele frequency as features. Performance across most prediction methods tends to decline as allele frequency decreases, with specificity showing particularly large declines for very rare variants [92].
What quantitative benchmarks should I use to correlate functional data with pathogenicity predictions in POI research?
For POI-related transmembrane proteins like PSEN1, PSEN2, and APP, recent studies found:
- AlphaMissense showed moderate correlation with Aβ42/Aβ40 ratio (critical biomarker)
- Weaker correlations were observed for individual Aβ40 or Aβ42 levels across all tools
- ROC-AUC analysis demonstrated high performance for validated variants (AUC >0.8)
- Comparative benchmarks should include CADD, EVE, and ESM-1b alongside newer tools [93]
Experimental Protocols & Troubleshooting Guides
Protocol: Cell-Based FSHR Functional Characterization Assay
Based on: Sassi et al. evaluation of FSHR mutations in POI [29]
Materials Required:
- Plasmids containing wild-type FSHR and variant constructs
- Cell line suitable for transfection (e.g., HEK293)
- FSH for stimulation
- cAMP detection kit (ELISA or luminescence-based)
- Flow cytometry equipment for surface expression analysis
Methodology:
- Transfection: Transfect cells with plasmids containing common FSHR allele, each mutation, combined mutants, and vector control
- Surface Expression Analysis:
- 48 hours post-transfection, harvest cells
- Label with FSHR-specific antibody
- Analyze by flow cytometry
- Calculate percentage reduction compared to wild-type
- cAMP Production Assay:
- Stimulate transfected cells with saturating FSH concentration
- Measure intracellular cAMP production after specified time
- Compare to wild-type response
Expected Results & Interpretation: Pathogenic FSHR variants typically show >50% reduction in both surface expression and cAMP production compared to wild-type. The original study demonstrated 93% reduction in surface expression and approximately 50% reduction in cAMP production for pathogenic variants [29].
Troubleshooting:
- Low transfection efficiency: Optimize DNA:transfection reagent ratio
- High background in cAMP assay: Include vehicle-only controls and concentration gradient
- Variable surface expression: Ensure consistent cell passage number and viability
Protocol: Automated Patch Clamp for Ion Channel Variants
Based on: KCNH2 variant characterization in long QT syndrome [91]
Materials Required:
- Automated patch clamp system
- Cells expressing wild-type or variant ion channels
- Appropriate recording solutions
- Voltage protocols specific to channel function
Methodology:
- Prepare cells expressing variant and wild-type channels
- Establish whole-cell configuration
- Apply disease-relevant voltage protocols
- Analyze current density, activation, inactivation, and deactivation properties
- Calculate z-scores compared to wild-type
Interpretation: Severe loss-of-function variants typically show z-scores < -3. The referenced study reported z-scores of -5.16 and -3.97 for homozygous and heterozygous KCNH2 variants, respectively [91].
Protocol: Multiplex Assays of Variant Effect (MAVE)
Based on: Large-scale variant functional characterization principles [94]
Materials Required:
- Variant library synthesis capability
- Appropriate selection system
- High-throughput sequencing capability
- Bioinformatics pipeline for data analysis
Methodology:
- Design and synthesize variant library covering regions of interest
- Introduce library into model system
- Apply functional selection pressure
- Sequence pre- and post-selection populations
- Calculate enrichment scores for each variant
Applications in POI: MAVEs can be applied to POI genes to systematically assess thousands of variants simultaneously, creating comprehensive functional maps for variant interpretation [94].
Performance Benchmarks for Pathogenicity Prediction Tools
Table 1: Correlation of Computational Predictions with Functional Data in Alzheimer's Proteins
| Prediction Tool | Correlation with Aβ42/Aβ40 Ratio | Correlation with Aβ40 Levels | ROC-AUC for Validated Variants |
|---|---|---|---|
| AlphaMissense | Moderate correlation | Moderate correlation | >0.8 |
| CADD v1.7 | Weaker correlation | Weaker correlation | Lower than AM |
| EVE | Weaker correlation | Weaker correlation | Lower than AM |
| ESM-1B | Weaker correlation | Weaker correlation | Lower than AM |
Data adapted from benchmarking study of 114 VUS in APP, PSEN1, and PSEN2 [93].
Table 2: Performance of Selected Prediction Methods on Rare Variants
| Method | AF Handling in Training | Sensitivity on Rare Variants | Specificity on Rare Variants | Key Features |
|---|---|---|---|---|
| MetaRNN | Trained on rare variants | High | High | Conservation, multiple scores, AF |
| ClinPred | AF as feature | High | High | Conservation, multiple scores, AF |
| REVEL | Trained on rare variants | Moderate | Moderate | Ensemble method |
| CADD | AF as feature | Moderate | Lower than sensitivity | Multiple genomic features |
Based on performance assessment of 28 prediction methods on rare variants from ClinVar [92].
Research Reagent Solutions
Table 3: Essential Materials for POI Functional Studies
| Reagent/Resource | Function/Application | Example Use in POI Research |
|---|---|---|
| N2A mouse neuroblastoma cells (Psen1/Psen2 KO) | Cell-based assay system | Functional characterization of PSEN1/PSEN2 variants via Aβ42/Aβ40 measurement [93] |
| FSHR expression plasmids | Receptor function studies | Cell surface expression and cAMP signaling assays for FSHR variants [29] |
| Automated patch clamp systems | Ion channel characterization | High-throughput functional assessment of ion channel variants [91] |
| cAMP detection kits | Second messenger signaling | Quantifying G-protein coupled receptor activity (e.g., FSHR) [29] |
| Multiplex variant libraries | Large-scale functional screening | Simultaneous assessment of thousands of variants in POI genes [94] |
| AlphaMissense predictions | Computational pathogenicity assessment | Benchmarking against experimental data for variant interpretation [93] |
Experimental Workflows and Validation Frameworks
Functional Validation Workflow
Assay Selection Framework
Key Considerations for POI Research
Gene-Specific Validation: Different POI genes require tailored experimental approaches. For example:
- FSHR: Focus on cell surface expression and cAMP signaling
- Meiosis genes (HFM1, MSH4, etc.): Assess DNA repair efficiency or meiotic progression
- Mitochondrial genes (AARS2, HARS2, etc.): Measure oxidative phosphorylation or mitochondrial membrane potential
Phenotypic Correlation: POI presents with both primary (25.8% with pathogenic variants) and secondary amenorrhea (17.8% with pathogenic variants), with different genetic architectures. Functional validation should consider this phenotypic heterogeneity [26].
Statistical Rigor: Incorporate appropriate statistical analysis for functional data. Recent guidelines emphasize the importance of replicate experiments, appropriate controls, and quantitative analysis rather than qualitative assessments [90] [95].
The field continues to evolve with new technologies like MAVEs and improved computational predictions, enabling more systematic functional characterization of VUS in POI genes. Following established validation frameworks ensures that functional evidence meets clinical-grade standards for variant interpretation.
FAQ: Foundational Concepts and Definitions
Q1: What is the core clinical difference between primary and secondary amenorrhea?
- Primary Amenorrhea (PA) is defined as the failure to reach menarche by age 15 or the absence of menses 3 years after thelarche (breast development) [96] [97].
- Secondary Amenorrhea (SA) is the cessation of previously regular menses for 3 months or more, or of irregular menses for 6 months or more [96] [97].
Q2: How do the genetic diagnostic yields typically compare between PA and SA?
Genetic abnormalities are more frequently identified in PA. One large study of 320 patients found that while a normal karyotype was common in both groups, 66.9% of PA patients had a normal karyotype, meaning about one-third had an abnormal one. In contrast, 88.9% of SA patients had a normal karyotype, suggesting a lower prevalence of gross chromosomal abnormalities [98]. The most common genetic causes also differ, as outlined in the table below.
Q3: What is a Variant of Uncertain Significance (VUS) and how should it be handled in a research context?
A VUS is a genomic variant for which there is insufficient evidence to classify it as either pathogenic (disease-causing) or benign [59] [10]. It is not clinically actionable, and management decisions should not be based on its presence alone [10]. For researchers, a "hot" VUS (one nearly classified as likely pathogenic) warrants further investigation through methods such as segregation analysis in families, functional studies, and deep phenotyping to gather evidence for potential reclassification [10].
FAQ: Genetic Findings and Interpretation
Q4: What are the most common genetic etiologies for Primary Amenorrhea?
PA is often linked to chromosomal disorders and gonadal dysgenesis. Key examples include [96] [97]:
- Turner Syndrome (45,X): A frequent cause involving short stature and ovarian dysgenesis.
- Pure Gonadal Dysgenesis (46,XX or 46,XY): Such as Swyer syndrome, where patients have a female phenotype but non-functional gonads.
- Müllerian Anomalies: Conditions like Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome, which can sometimes have a genetic component.
Q5: Which genes are most implicated in Secondary Amenorrhea, particularly Premature Ovarian Insufficiency (POI)?
SA, especially when diagnosed as POI, is associated with a wider spectrum of specific gene mutations. A study focusing on idiopathic POI found a high diagnostic yield, with causal single nucleotide variations (SNVs) or copy number variations (CNVs) identified in 9 of 28 patients (32.1%) [16]. Commonly implicated genes include [98] [16]:
- FMR1 (Premutation): A leading genetic cause of POI.
- FIGLA, BMP15, GDF5: Genes involved in ovarian function and folliculogenesis.
- Numerous other genes involved in meiosis, DNA repair, and ovarian development.
Q6: How can a researcher approach a patient cohort with amenorrhea for genetic studies?
A combined cytogenetic and molecular approach is most effective. The following workflow visualizes a comprehensive diagnostic and research pipeline, adapted from current clinical studies [98] [16]:
Diagram Title: Comprehensive Genetic Research Workflow for Amenorrhea
Experimental Protocols for Key Methodologies
Protocol 1: Karyotyping and G-Banding for Cytogenetic Analysis
Purpose: To identify numerical and structural chromosomal abnormalities in patients with amenorrhea, a common finding in PA [98].
Methodology (as per [98]):
- Lymphocyte Culture: Set up duplicate cultures of peripheral blood samples in RPMI-1640 media supplemented with phytohemagglutinin (PHA) and antibiotics.
- Metaphase Arrest & Harvesting: Process and harvest cells using standard techniques to obtain metaphase chromosomes.
- Slide Preparation & G-Banding: Prepare metaphase slides and perform G-banding for visualization.
- Karyotype Analysis: Analyze at least 20 metaphases to rule out chromosomal abnormalities and 30 cells to rule out mosaicism using a computerized microscope and GenASIS software (or equivalent). A band resolution of 400-500 bphs is standard.
- Reporting: Report karyotypic conditions according to the International System for Human Cytogenetic Nomenclature (ISCN) 2020 guidelines.
Protocol 2: Chromosomal Microarray Analysis (CMA) for CNV Detection
Purpose: To detect sub-microscopic copy number variants (CNVs) such as microdeletions/duplications (<5 Mb) in patients with a normal karyotype [98].
Methodology (Adapted from [98] and [16]):
- DNA Extraction: Isolate genomic DNA from peripheral blood using a commercial kit (e.g., QIAgen Kit).
- Platform Selection:
- Option A (Affymetrix): Use the Affymetrix 750K microarray. Digest 50 ng of DNA with NspI, followed by adapter ligation, PCR, fragmentation, biotin labeling, and hybridization to probes [98].
- Option B (Agilent): Use oligonucleotide array-CGH (e.g., 4x180K). Follow manufacturer's protocol for labeling and hybridization [16].
- Data Analysis: Analyze fluorescence data using dedicated software (e.g., Chromosome Analysis Suite for Affymetrix or CytoGenomics for Agilent). CNVs are typically called at a minimum size of 60 kb [16].
- Interpretation: Analyze identified CNVs using databases like DECIPHER, ClinGen, and DGV to determine clinical significance.
Protocol 3: Next-Generation Sequencing (NGS) for Single Nucleotide Variants
Purpose: To identify pathogenic single nucleotide variations (SNVs) and small indels in genes known or suspected to be involved in ovarian function and amenorrhea [16].
Methodology (Adapted from [98] and [16]):
- Library Preparation: Use a target capture system (e.g., Agilent SureSelect) focused on a custom panel of ~150-163 genes associated with amenorrhea/POI or clinical exome.
- Sequencing: Perform sequencing on a platform such as Illumina NextSeq 550, aiming for a coverage of 80-100X, with variant analysis focused on regions covered at 20X or more.
- Bioinformatics Analysis:
- Alignment & Variant Calling: Use pipelines like GATK/Sentieon for alignment, deduplication, and variant calling.
- Annotation & Filtering: Annotate non-synonymous and splice site variants using population databases (e.g., gnomAD), mutation databases (e.g., ClinVar, HGMD), and disease databases (e.g., OMIM).
- Variant Classification: Classify variants according to ACMG/AMP guidelines as Benign, Likely Benign, VUS, Likely Pathogenic, or Pathogenic [10].
Comparative Data Tables
Table 1: Key Genotype-Phenotype Correlations in Amenorrhea
| Phenotype Category | Primary Amenorrhea (PA) | Secondary Amenorrhea (SA) / POI |
|---|---|---|
| Prevalence of Chromosomal Abnormalities | Higher (One study: ~33% of 266 PA patients had abnormal karyotype) [98]. | Lower (One study: ~11% of 54 SA patients had abnormal karyotype) [98]. |
| Common Karyotypic Findings | Turner Syndrome (45,X or mosaicism), Pure Gonadal Dysgenesis (46,XY; Swyer syndrome) [96] [97]. | Less frequently associated with gross karyotype anomalies; FMR1 premutation is a key exception [16] [5]. |
| Common Mutated Genes/Panels | Genes involved in gonadal development and sex determination (e.g., SRY, WT1, NR5A1) [98]. | Genes critical for ovarian function and maintenance (e.g., FMR1, FIGLA, BMP15, FOXL2) [98] [16]. |
| Typical Ovarian Phenotype | Gonadal dysgenesis, "streak" ovaries, absent follicular activity [98] [96]. | Primary Ovarian Insufficiency (POI); depletion of ovarian follicle pool before age 40 [16] [5]. |
| Associated Features | Often includes absent puberty, short stature (e.g., Turner syndrome), and Mullerian anomalies [96] [97]. | Post-pubertal onset; may include vasomotor symptoms (hot flashes) and other signs of estrogen deficiency [16] [5]. |
Table 2: Diagnostic Yield of Genetic Techniques in Idiopathic POI (A Subset of SA)
Data derived from a study of 28 idiopathic POI patients using combined array-CGH and NGS [16].
| Genetic Analysis Method | Pathogenic/Likely Pathogenic Findings | Variant of Uncertain Significance (VUS) | Total Diagnostic Yield* |
|---|---|---|---|
| Array-CGH (CNVs) | 1/28 (3.6%) - 15q25.2 deletion | 2/28 (7.1%) | 3/28 (10.7%) |
| NGS (SNVs/Indels) | 8/28 (28.6%) - e.g., FIGLA, TWNK | 7/28 (25.0%) | 15/28 (53.6%) |
| Combined Approach | 9/28 (32.1%) | 9/28 (32.1%) | 16/28 (57.1%) |
*Total Diagnostic Yield includes patients with either a pathogenic/likely pathogenic finding or a VUS.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Platforms for Genetic Amenorrhea Research
| Research Reagent / Platform | Function / Application | Example Use Case |
|---|---|---|
| RPMI-1640 Media with PHA | Stimulates T-lymphocyte proliferation for cell culture in karyotyping [98]. | Standard media for peripheral blood lymphocyte culture. |
| Affymetrix CytoScan 750K Array | High-resolution platform for genome-wide CNV and SNP analysis [98]. | Detecting microdeletions/duplications <5 Mb in patients with normal karyotypes [98]. |
| Agilent SureSelect XT-HS Target Enrichment | Prepares sequencing libraries for NGS by capturing specific genomic regions [16]. | Custom capture of a 163-gene panel related to ovarian function for sequencing [16]. |
| Illumina NextSeq 550 System | High-throughput sequencing platform for NGS [16]. | Sequencing targeted gene panels or exomes for variant discovery. |
| GATK / Sentieon Pipelines | Bioinformatics software for processing NGS data, including alignment and variant calling [98]. | Primary analysis of raw sequencing data to identify genetic variants. |
| Chromosome Analysis Suite (ChAS) | Software for visualizing and interpreting CNV data from Affymetrix microarrays [98]. | Analysis and clinical reporting of CMA results. |
Core Concepts: VUS in POI Research
What is a Variant of Uncertain Significance (VUS) in the context of POI?
A Variant of Uncertain Significance (VUS) is a genetic change identified through sequencing whose impact on health and disease is unknown. In Premature Ovarian Insufficiency (POI) research, these are typically missense mutations, small in-frame insertions/deletions, or variants near splice sites where the functional consequences are not yet understood [99]. The American College of Medical Genetics (ACMG) classifies variants into five categories: Pathogenic (P), Likely Pathogenic (LP), Variant of Uncertain Significance (VUS), Likely Benign (LB), and Benign (B) [83]. When a VUS is identified in a POI patient, it enters a "genetic limbo" where clinical interpretation and counseling become challenging until functional studies can resolve its significance [99].
Why is POI particularly challenging for genetic diagnosis?
POI affects approximately 1-3.7% of women under 40 and represents a highly heterogeneous condition with diverse etiologies [89] [26] [5]. Genetic factors account for an estimated 20-25% of cases, but known genes explain only a fraction of these [27]. The largest whole-exome sequencing study to date (1,030 patients) found that pathogenic variants in known POI genes explain only 18.7% of cases, underscoring the substantial knowledge gaps [26]. This genetic heterogeneity, combined with the challenge of classifying numerous VUS, makes POI a prime area for implementing systematic VUS interpretation pipelines.
Table 1: Genetic Contribution to POI in Recent Large-Scale Studies
| Study Cohort | Cohort Size | Genetic Diagnostic Yield | Key Findings |
|---|---|---|---|
| Chinese Han POI patients [27] | 500 | 14.4% (72/500) | 61 P/LP variants in 19 genes; 58 were novel |
| Multi-center cohort [26] | 1,030 | 23.5% (242/1030) | 195 P/LP variants in 59 known genes plus 20 novel candidate genes |
| MENA region systematic review [89] [76] | 1,080 | 19 P/LP variants identified | 79 variants across 25 genes reported in 10 MENA countries |
Troubleshooting Guides & FAQs
FAQ: How do I determine if a VUS is worth investigating further?
Answer: Prioritize VUS investigation based on these evidence streams:
- Gene-Disease Validity: Focus on genes with established POI associations. The most frequently mutated genes in large studies include NR5A1, MCM9, FOXL2, HFM1, and MSH4 [26] [27].
- Variant Characteristics: Favor protein-truncating variants (nonsense, frameshift, canonical splice-site) over missense variants, though the latter can be pathogenic.
- Inheritance Pattern: Assess if the variant fits the gene's known inheritance pattern (e.g., autosomal recessive for MSH4, MSH5; autosomal dominant for NR5A1, NOBOX) [89] [27].
- Family Segregation: Multiple affected family members with the same variant strengthen candidacy.
- Population Frequency: Rare variants (MAF < 0.01 in gnomAD) are more likely to be pathogenic than common polymorphisms [89].
FAQ: What is the gold standard approach for VUS reclassification?
Answer: A multi-step orthogonal validation strategy is recommended [29] [99]:
- Variant Validation: Confirm the variant using Sanger sequencing after initial NGS discovery
- Family Segregation Analysis: Perform haplotype analysis in pedigrees with multiple affected members
- Computational Prediction: Use multiple in silico tools to assess functional impact
- Functional Assays: Design experiments to test the molecular consequences
- Clinical Correlation: Integrate patient phenotype and family history data
Troubleshooting Guide: My functional assay results are inconclusive
Problem: After identifying a promising VUS and developing a functional assay, the results are ambiguous or contradictory.
Solution: Follow this systematic troubleshooting approach:
Verify Experimental Controls:
Assay Optimization:
- Systematically vary key parameters one at a time (e.g., plasmid concentration, incubation time, reagent concentrations)
- Ensure biological and technical replicates to assess consistency [100]
Confirm Reagent Integrity:
- Verify plasmid sequences through full-length sequencing
- Check cell line authentication and contamination status
- Confirm antibody specificity and optimal working concentrations [101]
Consider Alternative Assays:
- If a protein expression assay fails, consider switching to transcriptional reporter assays, protein-protein interaction studies, or subcellular localization experiments
- The FSHR VUS study used both cell surface expression and cAMP production assays to comprehensively assess impact [29]
Experimental Protocols
Protocol: In Silico Systems Biology Analysis for VUS Prioritization
Purpose: To computationally prioritize VUS for further functional studies using bioinformatics tools [99].
Workflow:
Materials:
- Hardware: Standard computational workstation
- Software: CADD, DANN, MetaSVM for variant effect prediction; NNSplice, SplicePort, SoftBerry for splicing impact; GERP++, PhyloP for evolutionary conservation
- Databases: gnomAD, 1000 Genomes, ClinVar, PubMed, LOVD, InSiGHT database [99] [27]
Procedure:
- Variant Annotation: Annotate each VUS with functional predictions using multiple algorithms
- Splicing Analysis: Analyze potential splice site disruption or creation using three independent tools
- Conservation Scoring: Calculate evolutionary conservation scores across species
- Population Filtering: Exclude variants with frequency >0.01 in control populations
- Literature Mining: Search for previous reports of the variant in public databases
- Integrated Scoring: Combine evidence to generate a priority score for experimental follow-up
Protocol: Functional Validation of FSHR VUS through Signaling Assays
Purpose: To experimentally characterize the functional impact of FSHR VUS on receptor function and signaling [29].
Workflow:
Materials:
- Expression Vectors: Plasmids containing wild-type FSHR, mutant FSHR constructs, empty vector control
- Cell Lines: HEK293 or similar mammalian cell line
- Reagents: FSH hormone, cAMP ELISA kit, transfection reagent, cell culture media
- Equipment: Flow cytometer, fluorescence microscope, plate reader [29]
Procedure:
- Construct Generation: Clone identified FSHR VUS into expression vectors using site-directed mutagenesis
- Cell Transfection: Transfect cells with wild-type FSHR, mutant FSHR, or vector control
- Surface Expression Analysis:
- 48 hours post-transfection, harvest cells
- Label with FSHR antibody and analyze by flow cytometry
- Calculate percentage reduction in cell surface expression compared to wild-type
- cAMP Signaling Assay:
- Serum-starve transfected cells for 4-6 hours
- Stimulate with saturating FSH concentration (100 ng/mL) for 30 minutes
- Measure intracellular cAMP production using ELISA
- Compare mutant response to wild-type control
- Data Interpretation: >50% reduction in either surface expression or cAMP production suggests pathogenic effect
Research Reagent Solutions
Table 2: Essential Research Reagents for POI VUS Functional Validation
| Reagent Category | Specific Examples | Application in POI Research |
|---|---|---|
| Sequencing Technologies | Whole exome sequencing, Targeted gene panels (28-295 genes) | Initial variant discovery; targeted screening of known POI genes [26] [27] |
| Computational Prediction Tools | CADD, DANN, MetaSVM, NNSplice, SplicePort, SoftBerry | In silico prioritization of VUS by predicting functional impact [99] [27] |
| Functional Assay Systems | Luciferase reporter assays, cAMP ELISA, Flow cytometry, Yeast two-hybrid | Experimental validation of molecular consequences [29] [27] |
| Cell Culture Models | HEK293, COV434, KGN cells, Primary granulosa cells | Heterologous expression systems and ovarian cell models [29] |
| Public Databases | ClinVar, gnomAD, LOVD, InSiGHT, 1000 Genomes | Variant frequency data and clinical interpretations [89] [99] |
Pathway to Clinical Translation
Case Study: Successful FSHR VUS Reclassification
A exemplary case involved a proband with severe POI and a family history showing affected siblings, suggesting Mendelian inheritance [29]. The investigation:
Initial Discovery: NGS sequencing of a 31-gene POI panel revealed two compound heterozygous variants in the FSHR gene: maternal c.646G>A (G216R) and paternal c.1313C>T (T438I)
Segregation Analysis: Sanger sequencing confirmed the variants segregated with disease in the family
Functional Characterization:
- Surface Expression: Mutant FSHR showed up to 93% reduction in cell surface expression
- Signaling Assay: cAMP production was approximately 50% lower in mutant receptors at saturating FSH concentrations
Reclassification: The combined evidence allowed reclassification from VUS to pathogenic, confirming FSH resistance as the disease mechanism [29]
Key Considerations for Clinical Translation
- Phenotype-Genotype Correlations: Primary amenorrhea cases show higher genetic diagnostic yield (25.8%) than secondary amenorrhea (17.8%) [26]
- Oligogenic Inheritance: Approximately 1.8% of POI cases may involve digenic or multigenic variants, often with more severe phenotypes [27]
- Population-Specific Variants: The p.R349G variant in FOXL2 was identified in 2.6% of Chinese Han POI patients but is extremely rare in control populations [27]
- Functional Domain Focus: Variants affecting key protein domains (e.g., FSHR extracellular hormone-binding domain) are more likely to be pathogenic
Premature Ovarian Insufficiency (POI) is a clinically heterogeneous disorder characterized by the loss of ovarian function before age 40, affecting approximately 1-3.7% of women [102] [26]. It represents a major cause of female infertility and is associated with significant long-term health sequelae, including osteoporosis, cardiovascular disease, and neurological complications [5] [2]. Despite extensive research, the etiology of a substantial proportion of POI cases remains unknown, with genetic factors believed to play a crucial role in a majority of idiopathic cases [102]. The extreme genetic heterogeneity of POI has presented substantial challenges for molecular diagnosis using traditional genetic approaches.
Whole-exome sequencing (WES) has emerged as a powerful tool for investigating the genetic architecture of complex disorders like POI. By enabling simultaneous analysis of the protein-coding regions of thousands of genes, WES provides an efficient approach for identifying pathogenic variants across numerous potential candidate genes without prior knowledge of specific genetic defects [103]. This technical support document examines the diagnostic yield of WES across diverse POI cohorts, explores methodological considerations for optimizing variant detection, and addresses common challenges in variant interpretation, with particular focus on variants of uncertain significance (VUS) within the context of POI research.
Quantitative Synthesis: Diagnostic Yields Across POI Cohorts
Table 1: Diagnostic Yields of WES Across Published POI Cohorts
| Study Cohort Size | Overall Diagnostic Yield (%) | Primary Amenorrhea (PA) Yield | Secondary Amenorrhea (SA) Yield | Key Contributor Genes |
|---|---|---|---|---|
| 1,030 patients [26] | 23.5% (242/1030) | 25.8% (31/120) | 17.8% (162/910) | NR5A1, MCM9, EIF2B2, HFM1, SPIDR, BRCA2 |
| 375 patients [102] | 29.3% (110/375) | Not specified | Not specified | DNA repair genes (37.4%), follicular growth genes (35.4%) |
| 24 patients [103] | 58.3% (14/24) | Included both PA and SA cases | Included both PA and SA cases | BNC1, HFM1, EIF2B2, FOXL2, MCM9, FANCA, ATM |
| 70 families [104] | ~50% (reported in 50% of families) | Not specified | Not specified | Broad array of pathogenic/likely pathogenic variants |
Table 2: Inheritance Patterns of Pathogenic Variants in POI (Based on 1,030-Patient Cohort) [26]
| Inheritance Pattern | Prevalence Among Diagnosed Cases | Clinical Implications |
|---|---|---|
| Monoallelic (Heterozygous) | 80.3% (155/193) | Often autosomal dominant inheritance; high penetrance variability |
| Biallelic | 12.4% (24/193) | Typically autosomal recessive inheritance; more severe phenotypes |
| Multiple Heterozygous (Multi-het) | 7.3% (14/193) | Oligogenic inheritance possible; modified disease expression |
The collective evidence demonstrates that WES provides a substantial diagnostic yield in POI, ranging from approximately 18% to 58% across studies [103] [102] [26]. This variability likely reflects differences in cohort characteristics, inclusion criteria, stringency of variant interpretation, and the proportion of patients with primary versus secondary amenorrhea. The largest cohort study to date (n=1,030) revealed a clear distinction in molecular diagnostic rate between primary amenorrhea (25.8%) and secondary amenorrhea (17.8%) cases, suggesting that more severe clinical presentations may have stronger genetic components [26]. Furthermore, this study identified that the majority of solved cases (80.3%) involved monoallelic variants, with biallelic and multiple heterozygous variants accounting for the remainder of diagnoses [26].
Gene enrichment analysis across studies indicates that biological pathways involving DNA repair/meiosis, folliculogenesis, mitochondrial function, and immune regulation constitute the principal mechanisms disrupted in genetic POI [102] [26]. The prominent role of DNA repair genes is particularly noteworthy, as these accounted for 37.4% of diagnosed cases in one cohort and represent a significant tumor susceptibility risk that necessitates appropriate clinical follow-up [102].
Experimental Protocols: Methodological Framework for WES in POI
Patient Recruitment and Diagnostic Criteria
Standardized diagnostic criteria are essential for cohort homogeneity in POI genetic studies. The European Society of Human Reproduction and Embryology (ESHRE) guidelines define POI as: (1) oligomenorrhea or amenorrhea for at least 4 months, and (2) elevated follicle-stimulating hormone (FSH) level >25 IU/L on two occasions >4 weeks apart, occurring before age 40 [26]. Exclusion criteria typically encompass chromosomal abnormalities, FMR1 premutations, and known non-genetic causes such as chemotherapy, radiotherapy, autoimmune diseases, or extensive ovarian surgery [102] [26]. Comprehensive clinical data collection should include menstrual history (primary amenorrhea (PA), secondary amenorrhea (SA), or spaniomenorrhea), pubertal development, family history, ultrasonography findings (ovarian volume, follicular count), and complete hormonal profiles (FSH, LH, estradiol, AMH, TSH) with relevant autoantibodies [102].
WES Laboratory Workflow
The technical workflow for WES in POI research involves:
- DNA Extraction: High-quality genomic DNA extraction from peripheral blood using standardized protocols
- Exome Capture: Utilization of commercial exome capture kits (e.g., IDT xGen Exome Research Panel, Agilent SureSelect) targeting ~35-60 Mb of coding regions
- Sequencing: High-throughput sequencing on platforms such as Illumina NovaSeq or HiSeq systems with minimum 100x mean coverage and >95% of target bases covered at 20x [26]
- Variant Calling: Bioinformatic processing including alignment to reference genome (GRCh37/hg19 or GRCh38/hg38), variant calling using GATK best practices, and quality control filtering [102] [26]
Variant Filtering and Prioritization Strategy
A systematic approach to variant prioritization is critical for diagnostic success:
- Frequency Filtering: Exclusion of common variants (minor allele frequency >0.01 in population databases such as gnomAD, 1000 Genomes, or ethnically-matched control cohorts) [103] [26]
- Impact Prediction: Prioritization of loss-of-function variants (nonsense, frameshift, canonical splice-site) and missense variants predicted deleterious by multiple algorithms (SIFT, PolyPhen-2, CADD, MutationTaster) [103] [26]
- Gene-Phenotype Correlation: Focus on known POI-associated genes and biologically plausible candidate genes involved in ovarian development, function, and related pathways [102]
- Segregation Analysis: Family studies when possible to confirm de novo inheritance or co-segregation with phenotype [102]
- ACMG/AMP Guidelines: Application of standardized pathogenicity classification criteria for variant interpretation [102] [26]
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for WES in POI Studies
| Reagent/Platform | Specific Examples | Application in POI Research |
|---|---|---|
| Exome Capture Kits | IDT xGen Exome Research Panel, Agilent SureSelect | Target enrichment of coding regions; impacts uniformity and coverage |
| Sequencing Platforms | Illumina NovaSeq 6000, Illumina HiSeq 4000 | High-throughput sequencing; impacts read length and quality |
| Variant Annotation | ANNOVAR, SnpEff, VEP | Functional consequence prediction of identified variants |
| Population Databases | gnomAD, 1000 Genomes, ESP6500 | Allele frequency filtering in control populations [103] [26] |
| Pathogenicity Predictors | SIFT, PolyPhen-2, CADD, MutationTaster | In silico assessment of variant deleteriousness [103] |
| ACMG Classification | InterVar, Varsome | Semi-automated application of ACMG/AMP guidelines [102] [26] |
| Orthogonal Validation | Sanger Sequencing, 10x Genomics Linked-Reads | Confirmation of variant presence and phasing [26] |
Troubleshooting Common Technical Challenges
FAQ: Addressing Variant of Uncertain Significance (VUS) Interpretation
Q: What strategies can improve resolution of VUS in POI research?
A: Multiple complementary approaches can enhance VUS classification:
- Functional Studies: Implement targeted functional assays to provide experimental evidence (PS3/BS3 criteria under ACMG guidelines). For example, in the largest POI WES study to date, 75 VUS from seven POI genes were experimentally validated, with 55 confirmed as deleterious, enabling 38 to be reclassified as likely pathogenic [26].
- Segregation Analysis: Perform family studies to determine if VUS co-segregates with phenotype across multiple affected relatives.
- Population Frequency Refinement: Utilize larger, ethnically-matched control cohorts to assess variant prevalence in specific populations.
- Computational Evidence Integration: Combine multiple in silico prediction tools with conservation scores and protein structure modeling.
- Phenotype Expansion: Consider whether genes with VUS have established roles in related phenotypes or biological pathways relevant to ovarian function.
Q: How can we mitigate technical artifacts and platform-specific discordances in WES?
A: Cross-platform validation is essential, as demonstrated by studies showing that a subset of variants passing quality filters in gnomAD still exhibit significant allele frequency differences between WES and whole-genome sequencing (WGS) data [105]. Specific recommendations include:
- Discordant Site Awareness: Consult curated lists of known discordant sites (e.g., from gnomAD) that show systematic differences between sequencing platforms [105].
- Orthogonal Validation: Employ alternative genotyping methods (Sanger sequencing, array-based genotyping) for putative pathogenic variants, particularly in regions with known technical challenges [105] [26].
- Platform-Specific Filters: Adjust quality thresholds based on sequencing platform characteristics and capture kit performance.
- Complex Region Annotation: Flag variants in low-complexity regions, segmental duplications, or high-identity pseudogenes that are prone to mapping errors [105].
FAQ: Optimizing Diagnostic Yield in POI Genetic Studies
Q: What factors significantly impact diagnostic yield in POI WES studies?
A: Key factors include:
- Phenotype Stratification: Primary amenorrhea cases show higher diagnostic rates (25.8%) compared to secondary amenorrhea (17.8%) [26]. Focus recruitment on patients with early-onset or syndromic presentations.
- Inclusion Criteria: Stringent application of diagnostic criteria with comprehensive exclusion of non-genetic etiologies improves cohort homogeneity.
- Variant Interpretation Framework: Implementation of consistent ACMG/AMP guidelines with multidisciplinary review (clinical geneticists, molecular biologists, bioinformaticians) enhances classification accuracy [102] [26].
- Gene Panel Composition: Regular updates to include newly discovered POI-associated genes increases diagnostic potential over time.
Q: How should we handle incidental findings or dual diagnoses in POI patients?
A: Approximately 7% of molecular diagnoses in adults reveal dual Mendelian conditions [106], and 8.5% of POI cases represent the only manifestation of a multi-organ genetic disorder [102]. Establish clear protocols for:
- Incidental Finding Management: Develop institutional policies for return of results, particularly for cancer predisposition genes (e.g., BRCA2) identified in 37.4% of solved cases in one cohort [102].
- Phenotype Reassessment: When a genetic diagnosis suggests a syndromic condition, conduct comprehensive clinical reassessment for previously unrecognized features.
- Multidisciplinary Consultation: Engage appropriate specialists based on gene functions and associated phenotypic spectra.
Pathway Analysis: Molecular Mechanisms in POI Pathogenesis
Integration of WES findings from multiple cohorts has elucidated several critical pathways disrupted in POI, revealing the molecular complexity underlying ovarian function. The major biological pathways implicated include DNA repair/meiosis, folliculogenesis, mitochondrial function, and immune regulation [102] [26]. The diagram below illustrates the key pathways and their interrelationships identified through WES studies in POI.
WES has demonstrated considerable utility in identifying the genetic etiology of POI, with diagnostic yields ranging from 18% to 58% across diverse cohorts. The technology has enabled discovery of novel POI-associated genes and illuminated key biological pathways underlying ovarian function. Future directions should focus on standardizing variant interpretation protocols, expanding functional validation capabilities, and implementing integrated multi-omics approaches to resolve cases remaining undiagnosed after WES. The progressive elucidation of POI genetics promises enhanced personalized management, including targeted therapeutic interventions and refined fertility prognostication for affected women.
FAQ: Foundations of VUS in POI Research
What is a Variant of Uncertain Significance (VUS) in the context of Premature Ovarian Insufficiency (POI)? A Variant of Uncertain Significance (VUS) is a genetic change whose impact on disease risk is not yet known. In POI research, it is a variant identified in a gene associated with ovarian function, but for which there is insufficient evidence to classify it as either disease-causing (pathogenic) or benign [19] [107]. The American College of Medical Genetics and Genomics (ACMG) recommends a five-tier system for variant classification: Benign, Likely Benign, Variant of Uncertain Significance (VUS), Likely Pathogenic, and Pathogenic [19] [83]. The VUS category is essential for acknowledging uncertainty and preventing premature conclusions that could lead to mismanagement.
Why is resolving VUS a critical challenge in POI genetics? POI is a genetically heterogeneous disorder, affecting about 1-3.5% of women under 40, with a significant portion of cases having an unknown genetic cause [16] [5]. Large-scale sequencing studies identify a VUS in a high proportion of patients. For instance, one study found that 39.3% of idiopathic POI patients carried a VUS or likely pathogenic variant [16]. Another major study identified pathogenic or likely pathogenic variants in 23.5% of 1,030 POI cases, implying a vast space for VUS resolution to further close the diagnostic gap [26]. The challenge is compounded because VUS results can complicate clinical decision-making, cause patient anxiety, and lead to unnecessary resource utilization until the uncertainty is resolved [107].
What is the typical fate of a VUS upon re-evaluation? Current data suggests that when a VUS is re-classified, the majority (approximately 85-90%) are downgraded to "Likely Benign" or "Benign." Only about 10-15% of re-classified VUS are upgraded to "Likely Pathogenic" or "Pathogenic" [107]. However, re-classification often occurs too slowly to benefit the patient in whom the VUS was first identified, highlighting the need for proactive and rapid functional validation strategies [107].
FAQ: Technical & Analytical Challenges
How are variants classified, and what evidence is needed to resolve a VUS? Variant classification follows standardized guidelines that weigh multiple types of evidence [19]. The table below summarizes key evidence types used to resolve a VUS.
| Evidence Type | Description | Role in VUS Resolution |
|---|---|---|
| Population Data | Frequency of the variant in general population databases (e.g., gnomAD). | A variant too common in the general population is unlikely to cause a rare disease like POI, supporting a benign classification [107] [83]. |
| Computational & Predictive Data | In silico tools predicting the impact of an amino acid change on protein function. | Provides supporting evidence; multiple algorithms predicting a deleterious effect can support pathogenicity [107] [83]. |
| Functional Data | Laboratory assays testing the biological impact of the variant (e.g., on protein stability, enzyme activity). | Provides strong evidence of a deleterious or non-deleterious effect and is often key for definitive re-classification [19] [107] [108]. |
| Segregation Data | Tracking whether the variant co-occurs with the disease in multiple family members. | Observing the variant in affected relatives supports pathogenicity, while its absence in affected individuals supports a benign classification [107]. |
| De Novo Data | Confirming the variant is new in the patient and not inherited from either parent. | A de novo occurrence in a relevant gene provides moderate evidence of pathogenicity [107]. |
Our research has identified a VUS in a non-coding region of a POI-associated gene. How should we proceed? Non-coding variants (e.g., in promoters, enhancers, introns) are a significant source of VUS in whole-genome sequencing data. Interpretation requires specialized approaches [24]. First, definitively link the non-coding region to its target gene using regulatory data (e.g., chromatin interaction maps like Hi-C). Then, assess the sequence for high conservation and overlap with known transcription factor binding sites. Functional validation is crucial and can involve reporter assays (to test impact on gene expression) and RNA sequencing (to detect aberrant splicing or expression levels) [24]. Non-coding variants are under-ascertained in clinical databases, making your functional data critically important for the community [24].
A base editing screen identified our VUS as a potential modulator of drug response. What are the functional classes of such variants? Functional studies can classify variants that modulate drug response into distinct categories, which have direct implications for therapy. The following diagram illustrates a generalized workflow for resolving a VUS and identifying its potential therapeutic class.
Advanced screens, such as CRISPR base editing, can prospectively identify and categorize variants into functional classes based on their behavior in the presence or absence of a drug [108]. The table below outlines these classes and their therapeutic implications.
| Functional Class | Proliferation Phenotype | Potential Therapeutic Implication |
|---|---|---|
| Canonical Drug Resistance | Advantage only with drug. | Develop next-generation inhibitors; combination therapies. |
| Drug Addiction Variant | Advantage with drug, deleterious without drug. | Intermittent dosing ("drug holidays") to selectively eliminate resistant clones [108]. |
| Driver Variant | Advantage with and without drug. | Requires broad-spectrum or multi-targeted therapeutic approaches. |
| Drug-Sensitizing Variant | Deleterious only with drug. | Ideal for combination therapy; the variant indicates a synthetic lethal interaction. |
Troubleshooting Guides
Problem: Inconclusive In Silico Predictions for a VUS
- Challenge: Different computational prediction tools (e.g., PolyPhen-2, SIFT, MutationTaster) provide conflicting results on the potential impact of a VUS [15].
- Investigation & Solution:
- Consensus Check: Use meta-predictors like REVEL or CADD that aggregate multiple algorithms. A high CADD score (e.g., >20-25) can support deleteriousness [26].
- Structural Analysis: Perform protein structure modeling with tools like AlphaFold. Analyze the variant's location in critical domains (e.g., kinase active site, DNA-binding domain). Tools like DynaMut2 can predict its effect on protein stability (ΔΔG) [15].
- Move to Functional Assays: Do not rely solely on computational data. Conflicting in silico results are a strong indicator that functional validation is required. For the CHEK1 A26G VUS in a POI patient, structural modeling predicted a destabilizing effect (ΔΔG -0.98 kcal/mol), which was then pursued through experimental validation [15].
Problem: Validating the Functional Impact of a Non-Coding VUS
- Challenge: A VUS is located in a putative enhancer region, and its effect on gene expression is unknown.
- Investigation & Solution:
- Define the Regulatory Element: Use epigenomic data (e.g., H3K27ac ChIP-seq from ovarian cell types) to confirm the region is a active enhancer in a relevant tissue.
- Functional Reporter Assay:
- Protocol: Clone the wild-type and mutant DNA sequence into a luciferase reporter plasmid (e.g., pGL4.23).
- Method: Transfect the constructs into an appropriate cell line (e.g., a granulosa cell line). Measure luciferase activity after 48 hours. A significant reduction in activity for the mutant sequence supports a damaging effect [24].
- CRISPR-Based Validation: Use CRISPR/Cas9 to introduce the VUS into a cell model and perform RNA-Seq to quantify changes in the expression of the putative target gene [24].
Problem: Translating a Resolved Pathogenic Variant into a Drug Target
- Challenge: A VUS in a DNA damage repair gene (e.g., CHEK1) has been re-classified as Likely Pathogenic through functional studies. How can this inform therapy?
- Investigation & Solution:
- Mechanistic Insight: Use the functional data to understand the variant's biochemical consequence. For example, the CHEK1 A26G variant was linked to altered expression of metabolism and inflammation-related genes via RNA sequencing [15].
- Identify Synthetic Lethality: Screen for drugs that are selectively toxic to cells carrying the variant. If the variant causes a defect in DNA repair, the cells may be hypersensitive to PARP inhibitors or other agents causing DNA damage.
- Explore Pathway-Targeted Therapies: The resolved variant pinpoints a specific pathway dysfunction (e.g., DNA damage response, metabolic reprogramming). This allows for the rational selection of targeted agents (e.g., AKT inhibitors, metabolic inhibitors) for pre-clinical testing in relevant cellular models.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and resources essential for VUS resolution experiments in POI research.
| Research Reagent / Solution | Function in VUS Resolution | Example Application in POI Research |
|---|---|---|
| CRISPR Base Editing Systems | Enables precise, single-nucleotide mutagenesis to install a specific VUS in a cell model for functional testing. | Prospectively screen for variants that confer resistance or sensitivity to drugs in cancer cell lines, modeling therapy response [108]. |
| Custom Capture NGS Panels | Targeted sequencing of a curated set of genes known or suspected to be involved in a specific pathology. | Idiopathic POI patients were screened using a custom panel of 163 genes related to ovarian function, increasing diagnostic yield [16]. |
| RNA Sequencing (RNA-Seq) | Reveals global changes in gene expression and alternative splicing patterns caused by a VUS. | CHEK1 A26G VUS overexpression altered the transcriptome, revealing mis-regulation of metabolic and inflammatory pathways [15]. |
| Luciferase Reporter Assays | Measures the functional impact of non-coding variants on transcriptional activity of promoters or enhancers. | Validating the effect of a non-coding VUS on the expression of a nearby POI-associated gene [24]. |
| Population Genomics Databases (gnomAD) | Provides allele frequency data to filter out common polymorphisms unlikely to cause rare disease. | A variant with a high frequency in gnomAD is typically classified as benign, aiding in VUS filtration [83] [26]. |
| Variant Classification Databases (ClinVar) | A public archive of reports of the relationships between variants and phenotypes, with supporting evidence. | Cross-referencing a novel VUS against previously classified variants in the community [83]. |
Conclusion
The resolution of VUS in POI represents a pivotal frontier in reproductive genetics, with direct implications for accurate diagnosis, personalized patient management, and the identification of novel therapeutic targets. A multidisciplinary approach that integrates evolving classification standards, advanced computational and functional methodologies, and global collaborative data sharing is essential to reduce the burden of uncertainty. Future efforts must prioritize the inclusion of diverse populations to ensure equitable advances. For researchers and drug developers, systematically resolved VUS are not merely reclassified variants but are potential beacons illuminating new pathways in ovarian biology, offering unprecedented opportunities for innovative therapeutic interventions in POI.
References
- 1. Primary Ovarian Insufficiency - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK589674/]
- 2. Evidence-based guideline: premature ovarian insufficiency [https://pmc.ncbi.nlm.nih.gov/articles/PMC11631070/]
- 3. Landscape of pathogenic mutations in premature ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9941050/]
- 4. Exome Sequencing to Identify Novel Variants Associated ... [https://www.mdpi.com/2227-9059/12/4/785]
- 5. Evidence-based guideline: Premature Ovarian Insufficiency [https://www.asrm.org/practice-guidance/practice-committee-documents/evidence-based-guideline-premature-ovarian-insufficiency--2024/]
- 6. Primary Ovarian Insufficiency: Causes, Symptoms & ... [https://my.clevelandclinic.org/health/diseases/17963-primary-ovarian-insufficiency]
- 7. Primary Ovarian Insufficiency | POI [https://medlineplus.gov/primaryovarianinsufficiency.html]
- 8. VUS – The Most Maligned Result in Genetic Testing [https://www.blueprintgenetics.com/resources/vus-the-most-maligned-result-in-genetic-testing/]
- 9. Understanding genetic variants of uncertain significance [https://pmc.ncbi.nlm.nih.gov/articles/PMC8900699/]
- 10. Variant of uncertain significance (VUS) — Knowledge Hub [https://www.genomicseducation.hee.nhs.uk/genotes/knowledge-hub/variant-of-uncertain-significance-vus/]
- 11. insights into the complexity of premature ovarian insufficiency... Genetic [https://pmc.ncbi.nlm.nih.gov/articles/PMC11295921/]
- 12. Landscape of pathogenic mutations in premature... | Nature Medicine [https://www.nature.com/articles/s41591-022-02194-3?error=cookies_not_supported&code=e9ac742f-ec44-442e-b04a-5601d382cdce]
- 13. Frontiers | Primary ovarian insufficiency: update on clinical and genetic ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1464803/full]
- 14. Integrative bioinformatics analysis for identifying the... [https://biomedcentral.eu/articles/10.1186/s12916-024-03675-7]
- 15. CHEK1 variant is a risk factor for premature ovarian ... [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-025-00774-1]
- 16. Genetics Investigation of Idiopathic Premature Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11942377/]
- 17. Variant of uncertain significance [https://en.wikipedia.org/wiki/Variant_of_uncertain_significance]
- 18. The promises and pitfalls of automated variant interpretation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12513165/]
- 19. Standards and Guidelines for the Interpretation of Sequence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4544753/]
- 20. Systematic gaps in reporting variants of uncertain ... [https://www.sciencedirect.com/science/article/pii/S1098360025001480]
- 21. A multicenter study of clinical impact of variant of uncertain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9939195/]
- 22. Reassessment of variants of uncertain significance in ... [https://www.nature.com/articles/s41431-025-01911-z]
- 23. From Uncertain to Actionable: Significant Reduction in ... [https://www.medrxiv.org/content/10.1101/2025.08.12.25333547v1]
- 24. Recommendations for clinical interpretation of variants found ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-022-01073-3]
- 25. Screening of Premature Ovarian Insufficiency-Associated ... [https://namikkemalmedj.com/articles/screening-of-premature-ovarian-insufficiency-associated-genes-in-turkish-patients/nkmj.galenos.2025.83435]
- 26. Landscape of pathogenic mutations in premature ovarian ... [https://www.nature.com/articles/s41591-022-02194-3]
- 27. Next-generation sequencing of 500 POI patients identified ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-023-01104-6]
- 28. Commentary on NOBOX Mutations in Premature Ovarian ... [https://www.scientificarchives.com/article/commentary-on-nobox-mutations-in-premature-ovarian-insufficiency]
- 29. Explaining the unexplained: new genetic mutations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8244336/]
- 30. Genetic landscape of a large cohort of Primary Ovarian ... [https://www.sciencedirect.com/science/article/pii/S2352396422004285]
- 31. Changing Etiological Spectrum of Premature Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12248835/]
- 32. There will always be variants of uncertain significance ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11616676/]
- 33. Selecting variants of unknown significance through ... [https://www.nature.com/articles/s41598-019-39796-w]
- 34. Targeted Protein Degradation (TPD) | Complete Solution [https://www.bio-techne.com/research-areas/targeted-protein-degradation]
- 35. Standards and guidelines for the interpretation of ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/25741868/]
- 36. Standards and guidelines for the interpretation of ... [https://www.nature.com/articles/gim201530]
- 37. Specifications of the ACMG/AMP variant curation guidelines ... [https://pubmed.ncbi.nlm.nih.gov/40967221/]
- 38. Overview of specifications to the ACMG/AMP variant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6885382/]
- 39. Understanding ACMG Guidelines: Standards for Genetic ... [https://3billion.io/blog/what-are-the-acmg-standards-and-guidelines-and-how-do-they-work]
- 40. Comparative analysis of functional assay evidence use by ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-019-0683-1]
- 41. Variants of Uncertain Significance: Should We Revisit How ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5999032/]
- 42. Sequence Variant Interpretation [https://clinicalgenome.org/working-groups/sequence-variant-interpretation/]
- 43. bioinformatics - gnomAD database allele frequency [https://stackoverflow.com/questions/70924497/gnomad-database-allele-frequency]
- 44. Variant interpretation using population databases [https://pmc.ncbi.nlm.nih.gov/articles/PMC9160216/]
- 45. ClinVar data parsing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5473414/]
- 46. The ClinVar VCV (variant) page - NCBI [https://www.ncbi.nlm.nih.gov/clinvar/docs/variation_report/]
- 47. ClinVar - NCBI - NIH [https://www.ncbi.nlm.nih.gov/clinvar/]
- 48. gnomAD [https://discuss.gnomad.broadinstitute.org/]
- 49. Best practices for the interpretation and reporting of clinical ... [https://www.nature.com/articles/s41525-022-00295-z]
- 50. The performance of in silico prediction tools for variant ... [https://www.medrxiv.org/content/10.1101/2025.07.29.25331316v1.full-text]
- 51. Assessing In Silico Tools for Accurate Pathogenicity ... [https://www.sciencedirect.com/science/article/pii/S0022283625004796]
- 52. MAVE Resources [https://www.varianteffect.org/resources/]
- 53. Validating data from Multiplex Assays of Variant Effect [https://pmc.ncbi.nlm.nih.gov/articles/PMC12256791/]
- 54. SignalStarâ„¢ Multiplex IHC Frequently Asked Questions [https://www.cellsignal.com/applications/signalstar-multiplex-ihc-faq?srsltid=AfmBOoq0ZkpuZDzl7MaCJ_e6ueoY2K4H91eeB00198nxMVfnd8aeMy05]
- 55. Editorial: Functional study of novel VUS (variant of ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1578736/full]
- 56. Multiplex assays of variant effects (MAVEs) [https://coursesandconferences.wellcomeconnectingscience.org/event/multiplex-assays-of-variant-effects-maves-approaches-analysis-and-interpretation-20251123/]
- 57. Functional assays in Drosophila facilitate classification of ... [https://pubmed.ncbi.nlm.nih.gov/40467338/]
- 58. Implementation of multi-omics in diagnosis of pediatric rare ... [https://www.nature.com/articles/s41390-024-03728-w]
- 59. Variant of Uncertain Significance (VUS) [https://www.genome.gov/genetics-glossary/Variant-of-Uncertain-Significance-VUS]
- 60. Transcriptome analysis provides critical answers to the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9560997/]
- 61. Navigating Challenges and Opportunities in Multi-Omics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11274472/]
- 62. From Biomarker Discovery to Precision Medicine Integration [https://www.cd-genomics.com/epigenetics/resource-methylation-databases-biomarkers-ai-precision-medicine.html]
- 63. Multi-Omics: Challenges and Solutions [https://bigomics.ch/blog/key-challenges-in-multi-omics-data-integration/]
- 64. Ten quick tips for avoiding pitfalls in multi-omics data ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1011224]
- 65. A guide to multi-omics data collection and integration for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9747357/]
- 66. Understanding variants of unknown significance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11299926/]
- 67. Systematic gaps in reporting variants of uncertain ... [https://pubmed.ncbi.nlm.nih.gov/40542645/]
- 68. 'Imprecision Medicine:' New Study Reveals Critical Gaps in ... [https://brotmanbaty.org/news/imprecision-medicine-new-study-reveals-critical-gaps-in-how-patients-are]
- 69. Integrating Analytical Methods to Improve Comparative ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK603795/]
- 70. An Economic Model for Estimating Trial Costs with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9931787/]
- 71. The risk factors, pathogenesis and treatment of premature ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01714-2]
- 72. Premature Ovarian Insufficiency - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10022589/]
- 73. The 5 most common clinical data pitfalls in 2025 (and how ... [https://www.greenlight.guru/blog/common-clinical-data-pitfalls]
- 74. Equitable machine learning counteracts ancestral bias in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11894161/]
- 75. Data and diversity in genomics: landscaping report - Wellcome [https://wellcome.org/insights/reports/data-and-diversity-genomics-landscaping-report]
- 76. The landscape of genetic variations in non-syndromic ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1289333/full]
- 77. AI tool adjusts for ancestral bias in genetic data [https://www.nature.com/articles/s41587-025-02651-7]
- 78. Study rethinks use of race in research at politically sensitive time [https://www.statnews.com/2025/06/05/nih-all-of-us-genetics-study-examines-nuanced-interplay-of-race-and-genetics/]
- 79. Diversity in Datasets [https://www.ga4gh.org/product/diversity-in-datasets-best-practices/]
- 80. Heidi Rehm on Tackling the Variant of Uncertain ... [https://www.insideprecisionmedicine.com/topics/molecular-dx/heidi-rehm-on-tackling-the-variant-of-uncertain-significance-crisis/]
- 81. Distinct rates of VUS reclassification are observed when ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11601763/]
- 82. Distinct rates of VUS reclassification are observed ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/40035215/?dopt=Abstract]
- 83. A Practical Guide to Clinical Variant Interpretation [https://www.euformatics.com/blog-post/a-practical-guide-to-clinical-variant-interpretation]
- 84. About Us - ClinGen | Clinical Genome Resource [https://clinicalgenome.org/about/]
- 85. Putting variants into practice: ClinGen, ClinVar, and the ... [https://www.broadinstitute.org/blog/putting-variants-practice-clingen-clinvar-and-challenge-interpreting-genetics-clinic]
- 86. The Clinical Genome (ClinGen) Resource [https://www.genome.gov/Funded-Programs-Projects/ClinGen-Clinical-Genome-Resource]
- 87. Representation of classifications in ClinVar - NCBI [https://www.ncbi.nlm.nih.gov/clinvar/docs/clinsig/]
- 88. The Matchmaker Exchange: A Platform for Rare Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4610002/]
- 89. The landscape of genetic variations in non-syndromic primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11082268/]
- 90. Recommendations for application of the functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6938631/]
- 91. Integration of validated functional evidence to support the ... [https://www.sciencedirect.com/science/article/pii/S2949774424010148]
- 92. Assessing the performance of 28 pathogenicity prediction ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11787-4]
- 93. Benchmarking AlphaMissense pathogenicity predictions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145806/]
- 94. Variant Interpretation: Functional Assays to the Rescue - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5590843/]
- 95. Consultation informs strategies for improving the use of ... [https://www.sciencedirect.com/science/article/pii/S0002929725001831]
- 96. Amenorrhea - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK482168/]
- 97. Amenorrhea: An Approach to Diagnosis and Management [https://www.aafp.org/pubs/afp/issues/2013/0601/p781.html]
- 98. Identification of genetic variants in patients with primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12199654/]
- 99. In Silico Systems Biology Analysis of Variants of Uncertain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5626617/]
- 100. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 101. How to be a Better Troubleshooter in Your Laboratory [https://www.goldbio.com/blogs/articles/how-to-be-a-better-troubleshooter?srsltid=AfmBOopaT55bmJ2LiqNvWmdQFsUSL_WBUO_bNK2i9dkQOjE5AOeQ8DTT]
- 102. Genetic landscape of a large cohort of Primary Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9475279/]
- 103. Whole-exome sequencing in patients with premature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7510158/]
- 104. Whole exome sequencing in a cohort of familial premature ... [https://www.sciencedirect.com/science/article/pii/S0015028221023165]
- 105. Discordant calls across genotype discovery approaches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10519400/]
- 106. Molecular diagnostic experience of whole-exome ... [https://www.sciencedirect.com/science/article/pii/S1098360021043975]
- 107. The challenge of genetic variants of uncertain clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10555957/]
- 108. Base editing screens define the genetic landscape of ... [https://www.nature.com/articles/s41588-024-01948-8]