Hormonal Control of Endometrial Gene Expression: From Molecular Mechanisms to Clinical Translation
This comprehensive review synthesizes current knowledge on how ovarian steroid hormones estradiol and progesterone orchestrate dynamic gene expression programs in the human endometrium throughout the menstrual cycle.
Hormonal Control of Endometrial Gene Expression: From Molecular Mechanisms to Clinical Translation
Abstract
This comprehensive review synthesizes current knowledge on how ovarian steroid hormones estradiol and progesterone orchestrate dynamic gene expression programs in the human endometrium throughout the menstrual cycle. We explore foundational transcriptomic and epigenetic mechanisms, advanced organoid and single-cell methodologies for studying endometrial biology, challenges in biomarker discovery and personalized medicine applications, and validation approaches through genetic mapping and clinical testing. By integrating insights from recent single-cell RNA sequencing, epigenetic analyses, and endometrial receptivity studies, this article provides researchers and drug development professionals with a multifaceted understanding of endometrial gene regulation and its implications for treating infertility and endometrial disorders.
Cyclical Transcriptomes and Epigenetic Landscapes: How Hormones Shape Endometrial Gene Expression
Estradiol and Progesterone Signaling Networks in Endometrial Tissue Remodeling
The endometrium, the inner lining of the uterus, undergoes dramatic cyclical remodeling throughout the menstrual cycle in preparation for embryo implantation. This dynamic process is primarily orchestrated by the ovarian steroid hormones estradiol (E2) and progesterone (P4), which coordinate complex transcriptional and cellular programs via their respective nuclear receptors [1] [2]. Estrogen dominates the proliferative phase, stimulating endometrial growth and regeneration, while progesterone during the secretory phase promotes glandular secretion and stromal differentiation—a process known as decidualization [2] [3]. The synchronized actions of these hormones ensure the brief period of endometrial receptivity known as the window of implantation (WOI), typically occurring on cycle days 20-24 in humans [4] [2]. Disruption of these precisely coordinated signaling networks underpins various endometrial pathologies, including endometriosis, implantation failure, and endometrial cancer [1] [3]. This review synthesizes current understanding of E2 and P4 signaling mechanisms governing endometrial gene expression and tissue remodeling, providing a foundational context for research on hormonal control of endometrial function.
Molecular Mechanisms of Hormone Receptor Signaling
Estrogen Receptor Signaling Pathways
Estrogen exerts its biological effects primarily through two nuclear receptors, estrogen receptor alpha (ERα) and beta (ERβ), which are expressed in multiple endometrial cell types including epithelial, stromal, and vascular cells [1]. Both receptors share a common domain structure comprising an N-terminal transcriptional activation function (AF-1) domain, a central DNA-binding domain (DBD), a hinge region, and a C-terminal ligand-binding domain (LBD) that contains the ligand-dependent activation function (AF-2) region [1]. Despite structural similarities, ERα and ERβ demonstrate distinct transcriptional activities and functional roles in the endometrium, with ERα predominantly mediating proliferative responses while ERβ may counterbalance ERα activity [1].
Estrogen signaling occurs through multiple mechanistic pathways. In the classical genomic pathway, ligand-bound ER dimers bind directly to estrogen response elements (EREs) in target gene promoters, recruiting co-regulator complexes to modulate transcription [1]. In non-classical pathways, ERs can tether to other transcription factors such as AP-1 and SP-1 without directly binding DNA. Additionally, membrane-associated receptors including G-protein coupled estrogen receptor (GPER) initiate rapid non-genomic signaling by activating secondary messengers and kinase cascades [1]. The expression patterns of these receptors are dynamically regulated throughout the menstrual cycle, with ERα notably downregulated during the implantation window in a progesterone-dependent manner, a change critical for establishing endometrial receptivity [4].
Progesterone Receptor Signaling and Antagonistic Functions
Progesterone signals through two main nuclear receptor isoforms, PRA and PRB, which are transcribed from the same gene but under different promoters [2]. PRB contains an additional 164 N-terminal amino acids and generally functions as a stronger transcriptional activator, while PRA often acts as a dominant-negative repressor of PRB activity [2]. In the human endometrium, both isoforms are expressed during the proliferative phase, but PRA becomes dominant in the early secretory phase, with PRB levels rising again during the mid-secretory phase [2].
Progesterone receptor signaling similarly involves genomic mechanisms where ligand-activated PR complexes bind progesterone response elements (PREs) to regulate target gene transcription [2]. The functional impact of progesterone signaling is highly context-dependent, with P4 generally opposing estrogen-driven proliferation by downregulating ER expression and promoting endometrial differentiation [2] [3]. This antagonistic relationship is crucial for the transition from the proliferative to secretory phase, with aberrant PR signaling or expression linked to impaired decidualization and endometrial receptivity defects [3].
Table 1: Estrogen and Progesterone Receptors in the Endometrium
| Receptor Type | Isoforms | Main Functions in Endometrium | Expression Patterns |
|---|---|---|---|
| Estrogen Receptor (ER) | ERα | Mediates epithelial proliferation, regulates implantation-related genes | High in proliferative phase, downregulated in secretory phase |
| ERβ | May counterbalance ERα activity, anti-proliferative effects | Expressed throughout cycle, function less defined | |
| Membrane Estrogen Receptor | GPER | Rapid non-genomic signaling, activates MAPK/PI3K pathways | Expressed in epithelium and stroma |
| Progesterone Receptor (PR) | PRA | Dominant-negative regulator of PRB, important for secretory changes | Dominant in early secretory phase |
| PRB | Strong transcriptional activator, promotes decidualization | Higher in mid-secretory phase |
Quantitative Analysis of Receptor Dynamics
Temporal Expression Patterns During the Menstrual Cycle
Advanced molecular techniques have enabled precise quantification of steroid hormone receptor dynamics throughout endometrial development. A 2020 study investigating endometrial samples from oocyte donors revealed statistically significant variations in both ERα and PR-B expression between day 0 (oocyte retrieval) and day 5 (implantation window) of the cycle [4]. Wilcoxon signed-rank test analysis demonstrated dramatic reductions in both receptors during this critical period, with P-values of P=0.0001 for ER nodal and stromal percentages, and P=0.0001 and P=0.035 for PR nodal and stromal percentages, respectively [4]. These quantitative findings confirm the progesterone-mediated downregulation of steroid receptors essential for acquisition of endometrial receptivity.
Further analysis revealed age-associated differences in ERα expression patterns, with patients under 30 years exhibiting 100% nodal staining on day 0 compared to 90% in women over 30 (P=0.014) [4]. This finding suggests potential molecular mechanisms underlying age-related declines in endometrial receptivity and highlights the importance of considering patient age in both research and clinical applications.
Hormonal Regulation of Receptor Expression
Experimental models have provided additional insights into hormonal cross-talk regulating receptor expression. Chromatin immunoprecipitation (ChIP) studies using endometrial cell lines (HEC1A, RL95-2) demonstrated that each steroid hormone receptor targets distinct gene groups, with estrogen treatment resulting in ER binding to 137 target genes in non-receptive HEC1A cells compared to only 35 in receptive RL95-2 cells [2]. Conversely, progesterone treatment generated PR binding to 83 targets in RL95-2 cells versus merely 7 in HEC1A cells, highlighting the cell-type and differentiation state specificity of hormonal signaling [2].
Table 2: Quantitative Changes in Steroid Hormone Receptors During the Implantation Window
| Receptor | Location | Day 0 Expression | Day 5 Expression | Statistical Significance |
|---|---|---|---|---|
| ERα | Nodal | 100% (<30y), 90% (>30y) | Significantly reduced | P=0.0001 |
| Stromal | High | Significantly reduced | P=0.0001 | |
| PR-B | Nodal | High | Significantly reduced | P=0.0001 |
| Stromal | High | Significantly reduced | P=0.035 |
Genomic and Non-Genomic Signaling Networks
Transcriptional Regulation of Endometrial Genes
Estradiol and progesterone coordinate endometrial remodeling through extensive transcriptional networks targeting genes involved in cell adhesion, extracellular matrix organization, immune modulation, and cellular differentiation. Research investigating 382 genes differentially expressed during the implantation window identified direct regulation by steroid hormone receptors through promoter binding [2]. Notably, progesterone signaling through PR isoforms activates genes critical for decidualization, including those encoding extracellular matrix components, growth factors, and immunomodulators [2] [3].
Recent single-cell RNA sequencing analyses have further refined understanding of cell-type-specific transcriptional responses to hormonal signaling. In stromal fibroblasts, progesterone signaling activates genes associated with cytoskeletal remodeling and differentiation, while in epithelial cells it represses pro-inflammatory pathways [3]. Serum response factor (SRF) has been identified as a key transcription factor interacting with hormonal signaling, particularly in regulating cytoskeletal genes during decidualization and suppressing epithelial inflammation [3]. Dysregulation of these transcriptional networks, as observed in endometriosis patients with decreased endometrial SRF expression, contributes to impaired decidualization and infertility [3].
Integrated Signaling in Endometrial Remodeling
The genomic and non-genomic signaling pathways of estradiol and progesterone converge to coordinate the complex process of endometrial remodeling. Estrogen signaling through both nuclear ER and membrane GPER activates growth factor pathways including EGFR, MAPK, and PI3K/AKT, which promote cellular proliferation and survival during the regenerative and proliferative phases [1]. Progesterone signaling subsequently dampens estrogen-driven proliferation while activating differentiation programs through both genomic mechanisms and rapid non-genomic signaling involving secondary messengers.
A critical aspect of this integrated signaling is the regulation of endometrial receptivity markers, including integrins, selectins, and cadherins [4]. Progesterone drives increased expression of integrin αvβ3 in epithelial cells, facilitating embryo attachment, while estrogen regulates E-cadherin expression important for epithelial integrity [4]. The dynamic interplay between these signaling networks ensures proper timing of the implantation window, with dysregulation leading to displaced WOI and implantation failure [5].
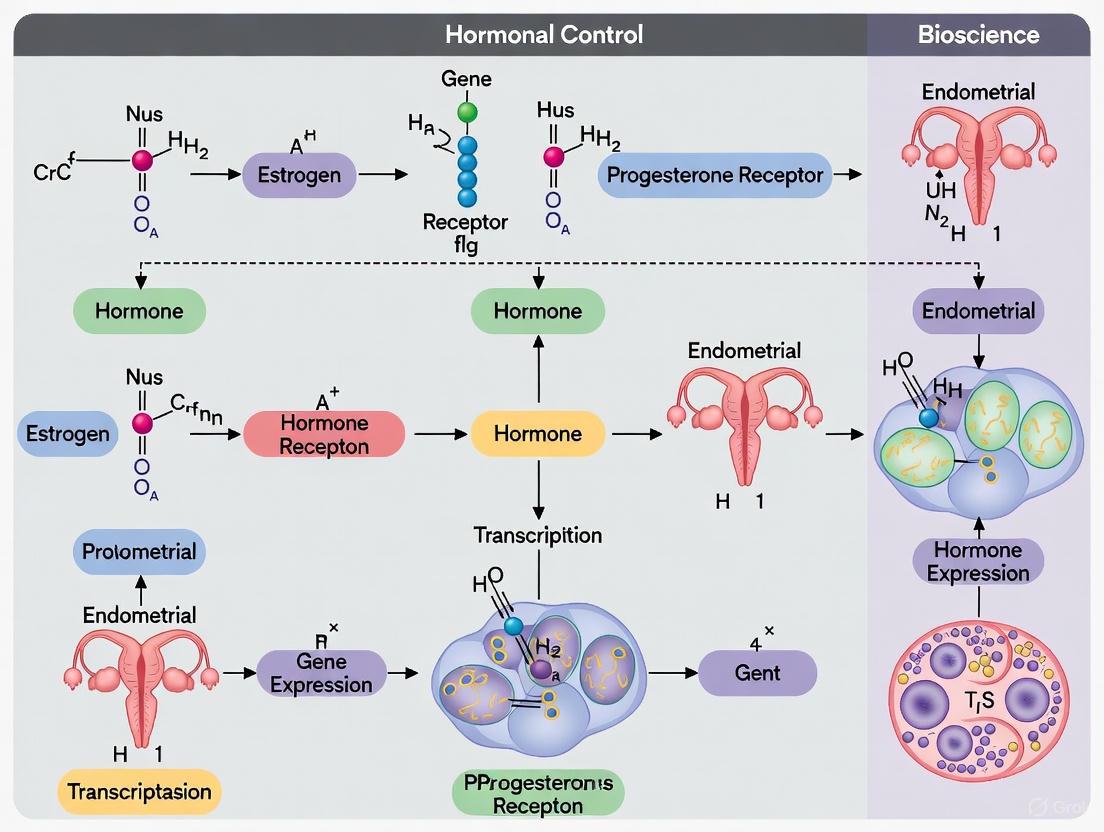
Diagram 1: Estradiol and Progesterone Signaling Networks in Endometrial Cells. This diagram illustrates the complex interplay between genomic and non-genomic signaling pathways activated by E2 and P4 in endometrial cells, highlighting the cross-regulation between receptor systems.
Experimental Models and Methodologies
In Vitro Models for Studying Endometrial Signaling
Various experimental systems have been developed to investigate E2 and P4 signaling in endometrial tissue. Immortalized human endometrial cell lines including HEC1A and RL95-2 provide reproducible models for studying hormone responsiveness, with RL95-2 cells particularly valuable as a model of receptive endometrium due to their enhanced adhesiveness for embryonic cells [2]. Primary endometrial stromal cells (HESCs) maintain critical in vivo characteristics including decidualization capacity in response to hormonal stimulation, making them essential for functional studies [3].
Recent advances in organoid technology have revolutionized endometrial research by enabling long-term expansion of primary epithelial cells that retain tissue-specific functions and hormone responsiveness [6]. Endometrial organoids recapitulate glandular architecture and express appropriate steroid hormone receptors, allowing investigation of epithelial-specific responses in a physiologically relevant context [6]. Microfluidic systems further enhance these models by incorporating mechanical stimuli including uterine peristaltic movement, enabling more accurate simulation of the endometrial microenvironment [6].
Key Methodological Approaches
Chromatin immunoprecipitation (ChIP) followed by quantitative PCR has been instrumental for identifying direct transcriptional targets of steroid hormone receptors. The standard protocol involves formaldehyde cross-linking of DNA-protein complexes, immunoprecipitation with receptor-specific antibodies (e.g., ERα, ERβ, PR), and quantification of bound genomic sequences [2]. This approach has identified hundreds of ER and PR binding sites in endometrial cells, revealing the extensive genomic networks regulated by these receptors.
For functional validation, RNA interference techniques (siRNA/shRNA) effectively knock down receptor expression in primary HESCs, enabling investigation of downstream consequences on decidualization, cytoskeletal organization, and cell viability [3]. Combined with transcriptomic analyses (RNA-seq), this approach has demonstrated that SRF deficiency in stromal cells disrupts actin cytoskeleton organization and blunts decidualization markers including IGFBP1 and PRL [3].
Immunohistochemistry remains essential for spatial localization of receptors and signaling components in endometrial tissue sections. Quantitative image analysis using software such as ImageJ enables precise measurement of staining intensity and distribution across epithelial and stromal compartments [4] [7]. This technique has demonstrated dynamic changes in ERα and PR expression patterns throughout the menstrual cycle and in pathological conditions.
Table 3: Essential Research Reagents for Endometrial Hormone Signaling Studies
| Reagent/Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Cell Models | RL95-2 cell line | Receptive endometrium model | Studies of embryo-endometrial dialogue |
| Primary HESCs | Decidualization studies | Stromal fibroblast differentiation | |
| Endometrial organoids | Epithelial function studies | 3D modeling of glandular physiology | |
| Antibodies | Anti-ERα (Clone 4f11) | IHC, ChIP | Detection and localization of ERα |
| Anti-PR (clone 16+SAN27) | IHC, Western blot | Progesterone receptor identification | |
| Anti-SRF | IHC, Functional studies | Transcription factor analysis | |
| Chemical Reagents | 4-hydroxytamoxifen | CreER lineage tracing | Genetic cell fate mapping |
| Estradiol + MPA + cAMP | Decidualization induction | In vitro stromal differentiation | |
| G-1 and G-15 | GPER studies | Specific GPER agonism/antagonism |
Technical Protocols for Key Experiments
Chromatin Immunoprecipitation (ChIP) for Steroid Receptor Genomic Binding
The following protocol adapted from Saare et al. (2009) details the procedure for identifying genomic targets of ER and PR in endometrial cell lines [2]:
Cell Culture and Hormone Treatment:
- Culture HEC1A or RL95-2 cells in appropriate media (McCoy 5A for HEC1A, DMEM/F12 for RL95-2) with 10% fetal bovine serum.
- 48 hours before experiments, switch to phenol-red free media with dextran-coated charcoal-treated FBS to eliminate hormone effects.
- Treat cells with 10 nM estradiol (E2) or progesterone (P4) for 45 minutes for ChIP experiments or 3-12 hours for mRNA analysis.
Cross-linking and Cell Lysis:
- Add 1% formaldehyde directly to culture media for 15 minutes at room temperature to cross-link DNA-protein complexes.
- Quench cross-linking with 125 mM glycine for 5 minutes.
- Wash cells twice with ice-cold PBS, harvest by scraping, and pellet by centrifugation.
Chromatin Preparation and Immunoprecipitation:
- Resuspend cell pellets in SDS lysis buffer and incubate on ice for 10 minutes.
- Sonicate chromatin to fragment DNA to 200-1000 bp fragments using a Vibra-Cell ultrasonic processor.
- Dilute lysate 10-fold in ChIP dilution buffer and pre-clear with protein A/G beads for 2 hours at 4°C.
- Incubate supernatant with 2-5 μg of specific antibodies (ERα: D-12, sc-8005; ERβ: H-150, sc-8974; PR: AB-52, sc-810) overnight at 4°C with rotation.
- Precipitate immune complexes with GammaBind Plus Sepharose beads for 2 hours.
- Wash beads sequentially with low salt, high salt, LiCl immune complex wash buffers, and TE buffer.
DNA Recovery and Analysis:
- Elute chromatin from beads with elution buffer (1% SDS, 0.1 M NaHCO3).
- Reverse cross-links by adding 5 M NaCl and incubating at 65°C overnight.
- Treat samples with Proteinase K, purify DNA using silica membrane columns.
- Analyze precipitated DNA by quantitative PCR with primers designed for regions of interest.
Endometrial Stromal Cell Decidualization Protocol
This protocol for in vitro decidualization of human endometrial stromal cells (HESCs) is adapted from recent publications [3]:
Primary HESC Isolation and Culture:
- Obtain endometrial biopsies or collect menstrual effluent by centrifugation at 800 × g for 10 minutes.
- Digest minced tissue with 0.2% collagenase type IA in DMEM/F12 for 60-90 minutes at 37°C with gentle agitation.
- Filter cell suspension through 40 μm and 20 μm sieves sequentially to separate glandular epithelial cells from stromal cells.
- Culture stromal cells in DMEM/F12 medium supplemented with 10% charcoal-stripped FBS, 1% penicillin-streptomycin, and 1% amphotericin B at 37°C in 5% CO2.
Decidualization Induction:
- At 80-90% confluence, switch to decidualization medium consisting of phenol-red free DMEM/F12 with 2% charcoal-stripped FBS, 1 μM medroxyprogesterone acetate (MPA), 0.5 mM 8-bromo-cAMP, and 10 nM 17β-estradiol.
- Refresh decidualization medium every 2-3 days for 6-12 days depending on experimental requirements.
Decidualization Validation:
- Monitor morphological changes from fibroblastic to rounded, epithelioid appearance.
- Measure established decidualization markers by RT-qPCR or ELISA: prolactin (PRL) and insulin-like growth factor binding protein 1 (IGFBP1).
- Assess cytoskeletal reorganization by phalloidin staining for F-actin.
Diagram 2: Chromatin Immunoprecipitation Experimental Workflow. This flowchart outlines the key steps in ChIP methodology for identifying genomic binding sites of steroid hormone receptors in endometrial cells.
Pathophysiological Implications and Therapeutic Applications
Clinical Implications of Signaling Disruption
Dysregulation of E2 and P4 signaling networks contributes significantly to various endometrial disorders. In endometriosis, aberrant estrogen signaling with concomitant progesterone resistance creates a inflammatory microenvironment characterized by defective decidualization and impaired endometrial receptivity [8] [3]. Single-cell RNA sequencing of endometriosis patient tissues has revealed decreased expression of critical transcription factors including SRF in both epithelial and stromal compartments, associated with cytoskeletal disorganization and blunted decidualization response [3].
Recurrent implantation failure (RIF) represents another condition with disrupted hormonal signaling, often featuring displaced window of implantation (WOI) [5]. Molecular diagnostic approaches including endometrial receptivity analysis (ERA) have identified significant correlations between patient age, number of previous failed embryo transfer cycles, and displaced WOI incidence [5]. Clinical studies demonstrate that personalized embryo transfer (pET) guided by ERA improves pregnancy rates in RIF patients from 49.3% to 62.7% and live birth rates from 40.4% to 52.5% [5].
In polycystic ovary syndrome (PCOS), metabolic disturbances including hyperinsulinemia synergize with hormonal imbalances to disrupt endometrial function [9]. Insulin resistance alters PI3K/AKT/MAPK signaling pathways, while chronic inflammation and hyperandrogenism interfere with normal estrogen and progesterone receptor signaling, resulting in impaired decidualization and increased pregnancy complications [9].
Therapeutic Targeting of Hormone Signaling Pathways
Understanding endometrial E2 and P4 signaling networks has enabled development of targeted therapeutic approaches. Selective estrogen receptor modulators (SERMs) including tamoxifen and raloxifene, and selective estrogen receptor downregulators (SERDs) such as fulvestrant, provide tools for manipulating estrogen signaling in endometrial pathologies [1]. For progesterone signaling, selective progesterone receptor modulators (SPRMs) offer potential for managing conditions including endometriosis and endometrial hyperplasia.
Emerging computational approaches including quantitative systems pharmacology (QSP) models integrate knowledge of hormonal signaling networks to predict treatment responses and optimize therapeutic strategies for endometrial disorders [8]. These models synthesize data on drug pharmacokinetics, receptor binding dynamics, and downstream signaling pathways to simulate patient-specific responses to hormonal manipulations [8].
Novel therapeutic strategies targeting the inflammatory components of endometrial disorders are also under development. Based on findings that SRF deficiency promotes endometrial inflammation and fibrosis, interventions aimed at restoring SRF expression or activity represent promising avenues for treating endometriosis-related infertility [3].
The signaling networks activated by estradiol and progesterone in endometrial tissue represent a sophisticated regulatory system that coordinates cyclical tissue remodeling, endometrial receptivity, and embryo implantation. The integration of genomic and non-genomic signaling pathways, combined with complex cross-talk between receptor systems, enables precise temporal and spatial control of endometrial function. Disruption of these networks underlies significant endometrial pathologies including endometriosis, implantation failure, and endometrial cancer.
Future research directions should focus on elucidating the single-cell resolution dynamics of hormonal signaling throughout the menstrual cycle, particularly during critical transitions such as the implantation window. Advanced organoid and microfluidic systems that better recapitulate the endometrial microenvironment will enable more physiologically relevant investigation of hormonal regulation. Additionally, computational modeling approaches integrating multi-omics data will provide unprecedented insights into the systems-level control of endometrial function by steroid hormones.
The continued refinement of our understanding of estradiol and progesterone signaling networks in the endometrium will undoubtedly yield novel diagnostic and therapeutic strategies for endometrial disorders, ultimately improving reproductive outcomes and women's health.
Single-Cell RNA Sequencing Reveals Phase-Specific Transcriptional Programs
The human endometrium undergoes profound, cyclic remodeling throughout a woman's reproductive life, characterized by sequential phases of proliferation, secretion, and shedding. This dynamic tissue transformation is exquisitely controlled by ovarian hormones—estrogen and progesterone—which regulate complex transcriptional programs to prepare the endometrium for embryo implantation. Understanding the hormonal control of endometrial gene expression at cellular resolution provides critical insights into reproductive success and the pathogenesis of gynecological diseases.
Single-cell RNA sequencing (scRNA-seq) has emerged as a transformative technology that enables researchers to decipher cellular heterogeneity and characterize phase-specific transcriptional programs within complex tissues. Unlike bulk RNA sequencing, which averages gene expression across cell populations, scRNA-seq reveals the unique transcriptomic signatures of individual cells, allowing for the identification of rare cell types, transitional states, and nuanced responses to hormonal cues [10]. This technical guide explores how scRNA-seq is illuminating the molecular mechanisms underlying endometrial physiology and pathology, with particular emphasis on hormonal regulation across the menstrual cycle.
scRNA-seq Technology: Principles and Workflows
Fundamental Technological Principles
Single-cell RNA sequencing technology has revolutionized transcriptomics by enabling researchers to profile gene expression at unprecedented resolution. The core principle involves isolating individual cells, converting their RNA into complementary DNA (cDNA), amplifying these transcripts, and preparing sequencing libraries that preserve cell-of-origin information through genetic barcoding [10]. Since its conceptual breakthrough in 2009, scRNA-seq has evolved rapidly, with throughput increasing from a few cells to hundreds of thousands of cells per experiment while costs have decreased dramatically [10].
The experimental workflow consists of several critical steps: (1) single-cell isolation and capture, (2) cell lysis, (3) reverse transcription (converting RNA to cDNA), (4) cDNA amplification, and (5) library preparation [10]. Among these, single-cell capture, reverse transcription, and cDNA amplification present the most significant technical challenges. Current high-throughput methods utilize microfluidic-microwell, droplet-based, or in situ barcoding approaches to process thousands of cells simultaneously [10].
A key innovation in scRNA-seq is the incorporation of unique molecular identifiers (UMIs), which tag each mRNA molecule during reverse transcription. UMIs enable accurate quantification by correcting for PCR amplification biases, thereby enhancing the quantitative nature of scRNA-seq data [10]. The choice between full-length transcript protocols (e.g., Smart-seq2) and 3'-end counting methods (e.g., 10x Genomics) depends on the specific research questions, with the former providing more complete transcript information and the latter enabling higher throughput [11] [10].
Experimental Design Considerations
Designing a robust scRNA-seq experiment requires careful consideration of multiple factors to ensure biologically meaningful results:
Sample Type Selection: Researchers must decide whether to sequence whole cells or nuclei. Single-nucleus RNA sequencing (snRNA-seq) is particularly valuable for tissues difficult to dissociate (e.g., brain, fibrous tissues) or when working with frozen clinical samples, as it minimizes artificial stress responses induced by tissue dissociation [10] [12]. For endometrial studies, snRNA-seq enables the use of valuable biobanked specimens collected throughout the menstrual cycle.
Replication Strategy: Both technical and biological replicates are essential. Technical replicates (processing the same sample multiple times) measure protocol variability, while biological replicates (different subjects under identical conditions) capture inherent biological variability and ensure reproducibility [12]. For menstrual cycle studies, biological replicates across different phases and multiple donors are crucial.
Fresh vs. Fixed Samples: While fresh samples ideally capture native transcriptional states, fixation permits sample storage and batched processing, which is particularly valuable for clinical samples obtained at unpredictable times or large-scale time-course experiments [12]. Fixed samples minimize batch effects in studies examining multiple menstrual cycle phases.
Cell Throughput and Sequencing Depth: There is an inherent trade-off between the number of cells sequenced, sequencing depth per cell, and the number of samples included. For cell-type-specific expression quantitative trait locus (ct-eQTL) mapping, sequencing more samples with lower coverage per cell increases statistical power more than deep sequencing of fewer samples [13]. This design principle is particularly relevant for population-scale studies of endometrial gene regulation.
Table 1: Key Decisions in scRNA-seq Experimental Design
| Design Factor | Options | Considerations | Endometrial Research Application |
|---|---|---|---|
| Sample Type | Whole cells vs. Nuclei | Nuclei preferable for difficult-to-dissociate tissues or frozen samples; whole cells capture cytoplasmic transcripts | Endometrial biopsies processed immediately (cells) vs. archived frozen samples (nuclei) |
| Replication | Technical vs. Biological | Technical replicates assess protocol noise; biological replicates capture donor variability | Multiple donors per menstrual phase account for interpersonal variation |
| Sample Processing | Fresh vs. Fixed | Fresh: optimal transcriptome preservation; Fixed: enables batching, clinical logistics | Fixed samples allow pooling across multiple cycle phases for direct comparison |
| Sequencing Strategy | High depth (fewer cells) vs. Low depth (more cells) | Low coverage with more cells increases power for population studies | Optimal for detecting rare cell populations in endometrial tissue across cycle phases |
Analysis of Phase-Specific Transcriptional Programs in the Endometrium
scRNA-seq Unravels Menstrual Cycle Dynamics
The application of scRNA-seq to endometrial tissue has revealed remarkable cellular heterogeneity and precise transcriptional changes across the menstrual cycle. A comprehensive analysis of 59,770 cells from normal endometrium identified 13 distinct cell clusters, with specific populations exhibiting phase-dependent expansion and regression [14]. Perivascular CD9+SUSD2+ cells emerged as putative progenitor cells with functions enriched in ossification, stem cell development, and wound healing—processes critical to cyclic endometrial regeneration [14].
Histological analysis demonstrated a significant perivascular expression pattern of CD9+SUSD2+ cells that varied across menstrual cycle phases, with higher abundance during the proliferative phase compared to the secretory phase [14]. This pattern aligns with the estrogen-driven regenerative program that dominates the proliferative phase, preparing the endometrium for potential implantation.
RNA velocity analysis, which predicts future cell states based on spliced and unspliced mRNA ratios, has established trajectory relationships between cell populations across the menstrual cycle [14]. This computational approach can delineate the developmental pathways through which progenitor cells differentiate into specialized endometrial cell types in response to hormonal cues.
Hormonal Regulation of Endometrial Cell Populations
scRNA-seq has enabled unprecedented resolution in mapping hormonal responses across different endometrial cell types. In the proliferative phase, estrogen signaling drives the expansion of epithelial and stromal compartments, with distinct transcriptional programs evident in each cell lineage [14]. During the secretory phase, progesterone signaling activates gene networks that support endometrial receptivity, including those involved in decidualization, nutrient transport, and immunomodulation.
A notable discovery from scRNA-seq is the identification of specialized epithelial subpopulations with unique hormone responsiveness. In adenomyosis patients, researchers identified a distinct "ECM-high epithelial cell" subpopulation that co-expressed both epithelial (EPCAM) and fibroblast (DCN) markers [15]. This hybrid cell population expanded in pathological states and exhibited altered hormonal response patterns, particularly to prolactin signaling [15].
Fibroblast subclusters also demonstrate phase-specific functional specialization. In the normal endometrium, fibroblasts differentiate into decidual stromal cells (ds1 and ds2) and pre-decidual stromal cells (Pre-ds) during the secretory phase, each with distinct transcriptional profiles [15]. The Pre-ds subcluster is characterized by proliferation-related genes (MKI67, TOP2A, CENPF, CDK1, CCNB1), while ds1 and ds2 cells exhibit differentiated phenotypes with unique signaling activities [15].
Table 2: Phase-Specific Endometrial Cell Populations and Their Transcriptional Programs
| Cell Type | Proliferative Phase Signature | Secretory Phase Signature | Putative Function |
|---|---|---|---|
| CD9+SUSD2+ Perivascular Cells | High abundance; enriched in stem cell development, wound healing | Reduced abundance | Progenitor function, tissue regeneration |
| Epithelial Subpopulations | Proliferation-associated genes; estrogen-responsive genes | Secretory programs; implantation factors | Lumen formation, glandular secretion, embryo attachment |
| Decidual Stromal Cells (ds1) | Low abundance | High DKK1, WNT4; decreased TGFβ and IGF signaling | Differentiated state, stromal remodeling |
| Decidual Stromal Cells (ds2) | Low abundance | High EGR1, IER2, TXNIP; stress response genes | Environmental sensing, stress adaptation |
| Endothelial Cells | Moderate angiogenic activity | Enhanced VEGF signaling, particularly CapECs | Vascular support, nutrient delivery |
Signaling Pathways in Endometrial Homeostasis and Pathology
Cell-Cell Communication Networks
CellChat analysis of scRNA-seq data has revealed intricate cell-cell communication networks that shift across the menstrual cycle. In the normal proliferative phase, signaling pathways that promote cellular proliferation and vascular development dominate, while secretory phase communications emphasize immune modulation and tissue stabilization [14].
In thin endometrium (TE), a condition associated with infertility, these communication networks become disrupted. scRNA-seq of proliferative phase endometrium from TE patients and controls revealed "TE-associated shifts in cell function, manifesting as increased fibrosis and attenuated cell cycle and adipogenic differentiation" [14]. Specifically, collagen signaling pathways showed abnormal over-activation around perivascular CD9+SUSD2+ cells, indicating a disrupted response to endometrial repair in TE, particularly in remodeling of the extracellular matrix [14].
Prolactin Signaling in Endometrial Disorders
scRNA-seq has identified prolactin (PRL) signaling as a key pathway in endometrial pathology. In adenomyosis, a condition characterized by ectopic endometrial tissue in the myometrium, scRNA-seq revealed a distinct epithelial subcluster with enriched PRL receptor (PRLR) expression [15]. This ECM-high epithelial subcluster expanded with disease progression and exhibited exaggerated PRL signaling, which promoted cellular survival and proliferation, contributing to lesion formation [15].
Similarly, scRNA-seq identified a fibroblast subpopulation in adenomyosis patients characterized by strong expression of inflammation-related genes and heightened PRL signaling [15]. PRL treatment of these fibroblasts increased inflammatory cytokine production, establishing a link between hyperactivated PRL signaling and the stromal inflammation characteristic of adenomyosis [15]. These findings were validated in preclinical models, where transgenic overexpression of PRL or pituitary transplantation induced adenomyosis, while PRLR inhibition with the monoclonal antibody HMI-115 ameliorated disease manifestations [15].
Figure 1: Prolactin Signaling Pathway in Adenomyosis. Hyperactivated PRL-PRLR signaling through JAK-STAT pathway drives disease pathogenesis.
Technical Considerations for Endometrial scRNA-seq Studies
Sample Preparation and Quality Control
Proper sample preparation is critical for successful endometrial scRNA-seq studies. The ideal sample viability should be between 70% and 90%, with intact cell morphology and minimal debris [12]. To achieve this:
Temperature Control: Maintain cold conditions (4°C) during cell extraction to arrest metabolic functions and reduce stress response gene upregulation that can skew data [12]. Endometrial cells held at room temperature rapidly degrade, extruding cellular contents and forming clumps.
Minimize Debris: Filter samples to remove debris, use calcium- and magnesium-free media (e.g., HEPES or Hanks' buffered salt) to prevent aggregation, and optimize centrifugation speeds to avoid over-pelleting [12]. Aggregation should be maintained below 5% for optimal results.
Dissociation Method Selection: Choose enzymatic dissociation protocols specific to endometrial tissue. Commercial enzyme cocktails (e.g., from Miltenyi Biotec) or automated dissociators (gentleMACS Dissociator) can provide reproducible, high-quality single-cell suspensions [12].
For menstrual cycle studies, precise timing of sample collection relative to the luteinizing hormone (LH) surge is essential. Mid-luteal phase samples should be collected on LH days 7-9 for consistent transcriptional profiling [14]. Additionally, careful patient screening is necessary to exclude confounding conditions like endometriosis, leiomyoma, adenomyosis, or polycystic ovary syndrome unless these are the focus of investigation [14].
Computational Analysis Workflow
The computational analysis of endometrial scRNA-seq data typically follows a standardized workflow:
Quality Control and Filtering: Using tools like the Seurat R package, filter out cells with fewer than 1,000 detected genes and less than 10,000 transcripts to remove low-quality cells and debris [14].
Normalization and Variable Feature Selection: Normalize raw counts using the "LogNormalize" method with a scale factor of 10,000, then identify highly variable genes (3,000-4,800 features) for downstream analysis [14].
Dimensionality Reduction and Clustering: Perform principal component analysis (PCA) on highly variable genes, then construct shared nearest neighbor graphs using 20-30 principal components. Cell clustering is typically performed at resolution parameters between 0.5-1.0 [14].
Differential Expression and Pathway Analysis: Identify cluster-specific markers using differential expression testing, followed by Gene Ontology (GO) enrichment analysis to determine biological functions of identified clusters [14].
RNA Velocity and Trajectory Inference: Analyze cellular dynamics using scVelo package to predict developmental trajectories and state transitions across menstrual cycle phases [14].
Figure 2: scRNA-seq Workflow for Endometrial Research. Key steps from sample collection to biological validation.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Endometrial scRNA-seq Studies
| Reagent/Technology | Function | Application in Endometrial Research |
|---|---|---|
| Seurat R Package (v5.0.1+) | Single-cell data analysis | Quality control, normalization, clustering, and visualization of endometrial cell populations |
| scVelo Package | RNA velocity analysis | Prediction of cellular trajectories across menstrual cycle phases |
| Unique Molecular Identifiers (UMIs) | mRNA molecule barcoding | Accurate transcript quantification by correcting PCR amplification biases |
| 10x Genomics Chromium | High-throughput scRNA-seq | Processing thousands of endometrial cells simultaneously for comprehensive atlas generation |
| Smart-seq2 | Full-length scRNA-seq | Detailed characterization of transcript isoforms in specific endometrial cell types |
| CellChat R Package | Cell-cell communication analysis | Mapping signaling interactions between endometrial cell populations |
| ClusterProfiler (v4.12.2+) | Pathway enrichment analysis | Functional interpretation of phase-specific gene signatures |
| Fluorescence-Activated Cell Sorting | Cell isolation and enrichment | Separation of specific endometrial populations (e.g., CD9+SUSD2+ cells) for downstream analysis |
| gentleMACS Dissociator | Tissue dissociation | Generation of high-quality single-cell suspensions from endometrial biopsies |
| Mianserin | Mianserin, CAS:24219-97-4, MF:C18H20N2, MW:264.4 g/mol | Chemical Reagent |
| Phenelzine Sulfate | Phenelzine Sulfate|MAO Inhibitor|CAS 156-51-4 |
Single-cell RNA sequencing has fundamentally transformed our understanding of endometrial biology by revealing the phase-specific transcriptional programs underlying the remarkable cyclic regeneration of this tissue. Through the application of scRNA-seq, researchers have identified specialized cell populations, delineated their hormonal regulation, and uncovered pathogenic mechanisms in conditions like thin endometrium and adenomyosis.
The insights gained from these studies highlight the potential of scRNA-seq to advance reproductive medicine by identifying novel therapeutic targets and developing personalized treatment strategies for endometrial disorders. As the technology continues to evolve, with improvements in spatial transcriptomics, multi-omics integration, and computational analysis, we can anticipate even deeper understanding of the intricate hormonal control of endometrial gene expression and its role in reproductive success and disease.
The endometrium, the lining of the uterus, is a quintessential hormone-responsive tissue, undergoing cycles of proliferation, differentiation, and shedding in response to circulating estrogen and progesterone. These dramatic changes are facilitated by precisely orchestrated gene expression programs. Epigenetics—the study of heritable changes in gene function that do not involve changes to the underlying DNA sequence—provides a critical regulatory layer that interprets hormonal signals to control these transcriptional programs [16]. The dynamic and reversible nature of epigenetic mechanisms makes them particularly suited for mediating the cyclic changes in the endometrium. Dysregulation of these processes is increasingly implicated in the pathophysiology of hormone-driven reproductive disorders, including endometriosis, endometrial cancer, and infertility [17] [18]. This review details the core epigenetic mechanisms—DNA methylation, histone modifications, and non-coding RNAs (ncRNAs)—that govern hormonal responses in the endometrium, providing a technical guide for researchers and drug development professionals.
Core Epigenetic Mechanisms and Their Role in Hormone Response
DNA Methylation
DNA methylation involves the addition of a methyl group to the 5-carbon position of a cytosine residue, predominantly within CpG dinucleotides. This modification is catalyzed by DNA methyltransferases (DNMTs), with DNMT3A and DNMT3B establishing de novo methylation patterns and DNMT1 maintaining these patterns during DNA replication [19] [18]. In the context of hormone response, DNA methylation primarily functions to repress gene transcription by preventing transcription factor binding or recruiting proteins that promote chromatin compaction [18].
In the endometrium, global and gene-specific DNA methylation patterns fluctuate across the menstrual cycle, directly influenced by the changing estrogen and progesterone milieu. For instance, promoter hypermethylation can silence genes involved in immunological control and estrogen metabolism, thereby determining the cellular response to hormonal signals [17]. Aberrant DNA methylation is a hallmark of endometrial pathologies; in endometriosis, hypermethylation of genes like HOXA10 disrupts endometrial receptivity, while in endometrial cancer, distinct methylation signatures can predict prognosis and response to therapy [20] [17].
Histone Modifications
Histone modifications are post-translational alterations—including acetylation, methylation, and phosphorylation—to the N-terminal tails of histone proteins. These modifications influence chromatin structure by altering the electrostatic charge of histones or creating binding platforms for other proteins. Specific marks are associated with transcriptional activation or repression; for example, H3K27ac and H3K4me3 are robust markers of active promoters and enhancers, while H3K27me3 is linked to transcriptional silencing [21] [22].
During endometrial decidualization, a process driven by progesterone, genome-wide increases in H3K27ac and H3K4me3 are observed at the promoter regions of genes critical for insulin signaling and glucose uptake, facilitating their up-regulation [21]. This demonstrates how histone modifications directly mediate the transcriptional output of hormonal signaling. The balance between histone acetylation and deacetylation, governed by histone acetyltransferases (HATs) and deacetylases (HDACs), is particularly important for maintaining the open chromatin state required for the expression of hormone-responsive genes.
Non-Coding RNAs (ncRNAs)
Non-coding RNAs are functional RNA molecules that regulate gene expression at the transcriptional and post-transcriptional levels without being translated into proteins. The two most studied classes in the context of hormonal response are microRNAs (miRNAs) and long non-coding RNAs (lncRNAs). miRNAs typically bind to the 3' untranslated region (UTR) of target mRNAs, leading to their degradation or translational repression. lncRNAs employ diverse mechanisms, including chromatin modification, transcriptional interference, and serving as molecular "sponges" for miRNAs [23].
In the endometrium, specific ncRNAs are differentially expressed during the window of implantation, a period of peak progesterone response. For example, miR-30b, miR-30d, and miR-494 are involved in establishing endometrial receptivity by fine-tuning the expression of genes critical for embryo implantation [23]. In endometriosis, dysregulated ncRNA expression profiles contribute to disease progression by promoting inflammation, cellular proliferation, and hormone resistance [18]. The presence of stable ncRNAs in bodily fluids like endometrial fluid also highlights their potential as non-invasive biomarkers for endometrial function and disease [23].
Table 1: Key Epigenetic Modifications in Endometrial Hormone Response
| Mechanism | Key Enzymes/Effectors | Functional Outcome | Role in Endometrial Hormone Response |
|---|---|---|---|
| DNA Methylation | DNMT1, DNMT3A, DNMT3B, TET proteins | Transcriptional repression, genomic imprinting, X-chromosome inactivation | Cyclic, hormone-driven silencing of genes involved in receptivity and inflammation; aberrant patterns in endometriosis and cancer [19] [17] |
| Histone Modifications | HATs, HDACs, KMTs, KDMs | Altered chromatin accessibility (e.g., H3K27ac=active; H3K27me3=repressed) | Genome-wide H3K27ac/H3K4me3 increases during decidualization; mediates progesterone-driven gene expression [21] [22] |
| Non-Coding RNAs | miRNAs (e.g., miR-30b, miR-494), lncRNAs | Post-transcriptional regulation, chromatin remodeling, molecular decoys | Fine-tune gene expression for embryo implantation; dysregulated in endometriosis; potential diagnostic biomarkers [23] [18] |
Experimental Protocols for Epigenetic Analysis
Analyzing DNA Methylation
Bisulfite Sequencing is the gold-standard method for base-resolution mapping of 5-methylcytosine (5mC). The protocol relies on the selective deamination of unmethylated cytosines to uracils by sodium bisulfite treatment, while methylated cytosines remain unchanged [24].
- Workflow for Whole-Genome Bisulfite Sequencing (WGBS):
- DNA Extraction & Fragmentation: Isolate high-quality genomic DNA and fragment it by sonication or enzymatic digestion.
- Bisulfite Conversion: Treat DNA with sodium bisulfite. This converts unmethylated cytosines to uracils, while methylated cytosines are protected.
- Library Preparation & Amplification: Build a sequencing library from the converted DNA. During subsequent PCR amplification, uracils are amplified as thymines.
- High-Throughput Sequencing: Sequence the library on a platform such as Illumina.
- Bioinformatic Analysis: Map sequenced reads to a reference genome. The methylation level at each cytosine is calculated as the percentage of reads reporting a cytosine (vs. thymine) at that position [24].
For cost-effective analyses focused on CpG-rich regions, Reduced Representation Bisulfite Sequencing (RRBS) uses a restriction enzyme (e.g., MspI) to digest and size-select for genomic regions with high CpG density, reducing the required sequencing depth [24].
WGBS/RRBS Experimental Flow
Profiling Histone Modifications
Chromatin Immunoprecipitation followed by sequencing (ChIP-seq) is the primary method for genome-wide mapping of histone modifications and transcription factor binding sites [21] [22].
- Workflow for ChIP-seq:
- Cross-Linking: Treat cells with formaldehyde to covalently link proteins (including histones) to DNA.
- Chromatin Shearing: Use sonication or enzymatic digestion to break the cross-linked chromatin into small fragments (200–600 bp).
- Immunoprecipitation (IP): Incubate the chromatin with a highly specific antibody against the histone modification of interest (e.g., anti-H3K27ac). The antibody-enriched chromatin complexes are pulled down.
- Reverse Cross-Linking & Purification: Heat the IP sample to break the protein-DNA bonds and purify the immunoprecipitated DNA fragments.
- Library Preparation & Sequencing: Construct a sequencing library from the purified DNA and sequence it.
- Data Analysis: Map the sequenced reads to the reference genome and identify regions with significant enrichment (peaks) compared to a control input sample, indicating the locations of the specific histone mark [21].
Novel techniques like CUT&Tag and CUT&RUN offer advantages over ChIP-seq, including higher resolution, lower background noise, and compatibility with low cell numbers, making them suitable for clinical samples [22] [24].
Investigating Non-Coding RNAs
RNA Sequencing (RNA-seq) is a powerful, unbiased method for discovering and quantifying all ncRNAs expressed in a sample.
- Workflow for ncRNA RNA-seq:
- Total RNA Extraction: Isolate total RNA, preserving the small RNA fraction.
- Library Preparation: For miRNA analysis, this typically involves size-selection of small RNAs, followed by adapter ligation and reverse transcription. For lncRNA analysis, ribosomal RNA (rRNA) depletion is often performed to enrich for other RNA species.
- High-Throughput Sequencing: Sequence the libraries.
- Bioinformatic Analysis: Map reads to the genome, quantify expression levels, and identify differentially expressed known and novel ncRNAs. Target prediction algorithms and pathway analysis are then used to infer biological functions [23].
Table 2: Key Methodologies in Epigenetic Research
| Method | Target | Resolution | Key Advantage | Primary Limitation |
|---|---|---|---|---|
| WGBS [24] | 5-methylcytosine | Base-pair | Gold standard; comprehensive genome coverage | High cost; cannot distinguish 5mC from 5hmC |
| RRBS [24] | CpG-rich regions | Base-pair | Cost-effective; focused on regulatory regions | Incomplete genome coverage; sequence bias |
| ChIP-seq [21] [22] | Histone modifications, TFs | ~200 bp | Genome-wide binding/ modification profiles | Requires high-quality antibodies; high cell input |
| CUT&Tag [22] | Histone modifications, TFs | Single-cell | Low background; works with low cell numbers | Still a relatively new technique |
| RNA-seq [23] | ncRNAs (miRNA, lncRNA) | Single transcript | Discovery and quantification in one assay | Complex bioinformatics; high depth needed for rare transcripts |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Epigenetic Studies
| Reagent / Tool | Function | Example Application |
|---|---|---|
| Sodium Bisulfite [24] | Chemical conversion of unmethylated cytosine to uracil | Essential pre-treatment for BS-seq, WGBS, and RRBS to determine methylation status. |
| MspI Restriction Enzyme [24] | Cuts at CCGG sites regardless of methylation | Used in RRBS to digest and enrich for CpG-rich genomic regions. |
| Anti-H3K27ac Antibody [21] | Specifically binds to H3K27ac epitope | Immunoprecipitation step in ChIP-seq to pull down DNA associated with active enhancers and promoters. |
| Formaldehyde [22] | Reversible cross-linking of proteins to DNA | Fixation step in ChIP-seq to preserve in vivo protein-DNA interactions. |
| DNMT Inhibitors (e.g., Decitabine) [19] [22] | Inhibits DNA methyltransferases | Experimental tool to demethylate DNA and study the functional consequences of loss of methylation. |
| HDAC Inhibitors (e.g., Vorinostat) [19] [22] | Inhibits histone deacetylases | Experimental tool to increase global histone acetylation and study its effect on gene expression. |
| CRISPR/dCas9 Epigenetic Editors [19] | Targeted epigenetic modification | dCas9 fused to DNMT3A (for methylation) or p300 (for acetylation) allows precise editing of specific loci. |
| Phenglutarimid | Phenglutarimid, CAS:1156-05-4, MF:C17H24N2O2, MW:288.4 g/mol | Chemical Reagent |
| S3QEL-2 | S3QEL-2, MF:C19H25N5, MW:323.4 g/mol | Chemical Reagent |
Signaling Pathways and Conceptual Workflows
The following diagram integrates the core epigenetic mechanisms into a conceptual pathway of hormonal signaling in the endometrium, illustrating how estrogen and progesterone signals are transduced into epigenetic and transcriptional changes.
Hormonal Regulation via Epigenetics
The window of implantation (WOI) represents a critical, transient period of endometrial maturation during which the uterine lining becomes receptive to embryonic implantation. This period, generally occurring between days 19-21 of a typical 28-day menstrual cycle, is characterized by a specific molecular signature that enables the trophectoderm of the blastocyst to attach to endometrial epithelial cells and subsequently invade the endometrial stroma [25]. The clinical significance of accurately identifying the WOI is profound, as suboptimal endometrial receptivity and altered embryo-endometrial crosstalk account for approximately two-thirds of human implantation failures [26].
Molecular assessment of endometrial receptivity has revealed that a significant proportion of women undergoing assisted reproductive technology (ART) exhibit displaced WOI. Recent large-scale studies demonstrate that approximately 34.18% (771/2256) of subfertile patients show WOI displacement, with 25.0% presenting with pre-receptive endometrium and 9.2% with post-receptive endometrium at the expected receptivity timeframe [27]. The precision of embryo transfer timing relative to the WOI significantly impacts ART outcomes, with transfers deviating more than 12 hours from the optimal window showing substantially reduced pregnancy rates (23.08% vs 44.35%, p < 0.001) and approximately twofold increase in pregnancy loss [27]. These findings underscore the critical importance of precise WOI determination for successful embryo implantation and pregnancy establishment.
Molecular Biomarkers of Endometrial Receptivity
Transcriptomic Signatures
The molecular basis of endometrial receptivity is characterized by complex gene expression patterns that transform the endometrium into a receptive state. Transcriptomic analyses have identified specific gene signatures that reliably predict receptivity status across different patient populations and cycle types. Several molecular tests have been developed based on these signatures, each utilizing distinct biomarker panels and technological platforms.
Table 1: Comparative Analysis of Endometrial Receptivity Testing Platforms
| Test Name | Technology Platform | Biomarker Number | Reported Accuracy | Key Characteristics |
|---|---|---|---|---|
| ER Map [27] | High-throughput RT-qPCR | Not specified | Significant improvement in pregnancy rates (p<0.001) | Identifies WOI displacement in 34.18% of subfertile patients |
| rsERT [28] | RNA-Sequencing | 175 genes | 98.4% (cross-validation) | Improved pregnancy rates in RIF patients (50.0% vs 23.7%) |
| beREADY [29] | TAC-seq | 72 genes (57 biomarkers + 11 WOI genes + 4 housekeepers) | 98.8% (cross-validation) | Detected displaced WOI in 15.9% of RIF patients vs 1.8% in fertile women |
| ERA [30] | Microarray | 238 genes | Established clinical utility | One of the first clinical transcriptomic tests for receptivity |
The molecular signature of receptivity involves coordinated expression changes across multiple gene families. Key functional categories include:
- Morphogenesis Factors: Genes involved in tissue remodeling and structural preparation for implantation
- Immunomodulators: Factors that establish maternal immune tolerance to the semi-allogeneic embryo
- Cell Adhesion Molecules: Mediators of embryo-endometrial attachment and interaction
- Transcription Factors: Regulators that coordinate the receptivity network
- Metabolic Pathway Genes: Enzymes supporting the bioenergetic demands of implantation [27] [30]
Recent research has revealed that the WOI timeframe exhibits considerable individual variability, with receptive endometria detected as early as 2.5 days after progesterone administration (P4 + 2.5) and up to 8 days after progesterone (P4 + 8) in hormone replacement therapy (HRT) cycles [27]. This variability highlights the limitations of standardized progesterone protocols and supports the need for personalized receptivity assessment.
Beyond Gene-Level Expression: Splicing and Isoform Variations
Emerging evidence indicates that transcript isoform-level and RNA splicing variations provide an additional layer of regulation in endometrial receptivity that is not detectable through conventional gene-level expression analysis. A 2025 study integrating large endometrial transcriptomic datasets (n=206) identified significant RNA splicing and transcript isoform-level changes across the menstrual cycle and in endometriosis [31].
Notably, when comparing mid-proliferative (MP) and mid-secretory (MS) phases, transcript-level analyses revealed that 24.5% of genes with differential transcript usage (DTU) and 27.0% of genes with differential splicing (DS) would not have been detected by gene-level expression analysis alone [31]. These splicing-specific changes affect biologically meaningful pathways including hormone regulation and cell growth, providing new insights into the molecular complexity of endometrial receptivity.
In endometriosis cases, specific splicing alterations have been identified, including decreased exon 4-skipping in the ZNF217 gene (ΔPSI = -6.4%), which is involved in estrogen receptor α-mediated signal transduction [31]. This finding demonstrates how genetic regulation of splicing may contribute to endometriosis-related implantation failure, potentially opening new avenues for diagnostic and therapeutic interventions.
Methodological Approaches for Transcriptomic Analysis
Experimental Workflow for Endometrial Receptivity Assessment
The standard protocol for endometrial receptivity assessment involves a coordinated process from sample collection through computational analysis. The following diagram illustrates the integrated experimental and computational workflow for transcriptomic profiling of endometrial receptivity:
Sample Collection and Processing Protocols
Patient Selection and Endometrial Biopsy:
- Timing: Endometrial biopsies are typically performed during the mid-secretory phase (LH+7 in natural cycles or P+5 in hormone replacement cycles) [28]
- Validation: Timing should be corroborated with histological evaluation using Noyes' criteria and/or LH peak measurements [29] [32]
- Exclusion Criteria: Standard protocols exclude patients with endometrial pathologies (polyps, adhesions, endometritis), hydrosalpinx, endocrine disorders, or active infections [32]
RNA Extraction and Quality Control:
- Extraction Method: Use of commercial kits (e.g., Qiagen RNeasy Mini Kits) following manufacturer's protocol [32]
- Quality Assessment: RNA integrity evaluation using Agilent Bioanalyzer; concentration measurement via NanoDrop spectrophotometer [33]
- Inclusion Threshold: Samples must meet minimum RNA quality standards (e.g., RIN > 7) for reliable transcriptomic analysis
Sequencing and Computational Analysis
Library Preparation and Sequencing:
- rRNA Depletion: Ribosomal RNA removal from total RNA to enrich for mRNA transcripts
- Library Construction: Strand-specific library preparation using fragmented mRNA [33]
- Sequencing Platforms: Various platforms including BGISEQ, Illumina, or other high-throughput systems generating typically 6 Gb of data per sample [33]
Bioinformatic Processing:
- Quality Control: FastQC, Trim Galore, or Cutadapt for raw read quality assessment and adapter trimming
- Alignment and Quantification: STAR alignment to reference genome followed by gene-level quantification using StringTie and RSEM [33]
- Normalization: Expression level normalization using FPKM and TPM metrics for cross-sample comparison
Differential Expression Analysis:
- Statistical Methods: DESeq2 package in R for identifying differentially expressed genes (DEGs) with FDR < 0.05 and fold change > 1.5 [33]
- Enrichment Analysis: Gene Ontology (GO) enrichment using clusterProfiler package to identify biological processes associated with receptivity [33]
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Endometrial Receptivity Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| RNA Extraction Kits | Qiagen RNeasy Mini Kits, RNA-easy isolation reagent (Vazyme) | Total RNA isolation from endometrial tissue | Ensure RNA integrity (RIN >7) for reliable sequencing |
| Library Prep Kits | Strand-specific library preparation kits | Construction of sequencing libraries | rRNA depletion crucial for transcriptome coverage |
| Sequencing Platforms | BGISEQ, Illumina platforms | High-throughput transcriptome sequencing | Typically generate ~6 Gb data per sample [33] |
| Computational Tools | FastQC, Trim Galore, Cutadapt, STAR, DESeq2, clusterProfiler | Quality control, alignment, differential expression, and pathway analysis | R/Bioconductor environment standard for analysis |
| Reference Datasets | GEO datasets (GSE111974, GSE71331, GSE58144, GSE106602) [32] | Validation and meta-analysis | Enable cross-study validation and biomarker discovery |
| Sacubitril sodium | Sacubitril sodium, CAS:149690-05-1, MF:C24H28NNaO5, MW:433.5 g/mol | Chemical Reagent | Bench Chemicals |
| Scrip | Scrip, CAS:94162-23-9, MF:C54H77N13O9, MW:1052.3 g/mol | Chemical Reagent | Bench Chemicals |
Molecular Heterogeneity and Clinical Subtypes
Recurrent Implantation Failure Subtypes
Recent research has revealed that recurrent implantation failure (RIF) exhibits distinct molecular subtypes with different underlying pathophysiologies. A 2025 multi-omics study identified two biologically distinct endometrial subtypes of RIF:
- Immune-Driven Subtype (RIF-I): Characterized by enrichment of immune and inflammatory pathways (IL-17 and TNF signaling, p < 0.01) with increased infiltration of effector immune cells [32]
- Metabolic-Driven Subtype (RIF-M): Marked by dysregulation of oxidative phosphorylation, fatty acid metabolism, steroid hormone biosynthesis, and altered expression of the circadian clock gene PER1 [32]
These subtypes demonstrate the heterogeneous nature of RIF pathogenesis and highlight the potential for personalized therapeutic approaches. The MetaRIF classifier developed to distinguish these subtypes achieved high accuracy in independent validation cohorts (AUC: 0.94 and 0.85) [32].
Endometrial-Embryo Cross-Talk Mechanisms
Successful implantation requires sophisticated bi-directional communication between the endometrium and embryo during the WOI. The following diagram illustrates key molecular mechanisms governing this cross-talk:
Key molecular players in this cross-talk include:
- Cytokines and Growth Factors: LIF (Leukemia Inhibitory Factor) promotes decidualization, pinopod expression, and trophoblast differentiation [25]; HB-EGF (heparin-binding epidermal growth-like factor) triggers initial communication between blastocyst and endometrium [25]
- Adhesion Molecules: Integrins (particularly β3 integrin) and selectins facilitate strong connection between blastocyst and endometrium during adhesion [25]
- Extracellular Vesicles: Bi-directional exchange of extracellular vesicles between endometrial cells and embryo facilitates synchronous molecular programming [26]
- Imm Modulators: HLA-G expressed by invading trophoblasts modulates cytokine secretion to maintain local immunosuppressive state [25]
Current Challenges and Future Directions
Despite significant advances in understanding the molecular signature of endometrial receptivity, several challenges remain in translating these findings to clinical practice:
- Technical Standardization: Variability in sampling techniques, RNA processing methods, and computational pipelines across centers [26]
- Spatial Heterogeneity: Current sampling from single endometrial sites may not capture molecular patterns across potential implantation sites [26]
- Dynamic Monitoring: Static molecular assessments fail to capture the temporal dynamics of receptivity establishment [26]
- Clinical Validation: Need for larger randomized controlled trials to validate the efficacy of personalized embryo transfer based on molecular receptivity testing [28]
Future research directions focus on integrating multi-omics approaches (transcriptomics, proteomics, metabolomics) to develop more comprehensive receptivity signatures [30], utilizing single-cell and spatial transcriptomics to resolve cellular heterogeneity [33], and developing non-invasive diagnostic methods using uterine fluid or exosomal biomarkers [30]. Artificial intelligence-driven models show particular promise, with some machine learning approaches already achieving AUC > 0.9 in predicting receptivity status [30].
The continued elucidation of molecular mechanisms governing endometrial receptivity will enable more precise personalization of fertility treatments, potentially transforming outcomes for patients experiencing implantation failure and advancing the field of reproductive medicine.
Decidualization, the transformation of endometrial stromal cells (ESCs) into specialized decidual stromal cells (DSCs), represents a pivotal genomic reprogramming event essential for embryo implantation and the establishment of pregnancy. This process is a fundamental component of the hormonal control of endometrial gene expression, driven primarily by the postovulatory rise in progesterone levels and local cyclic AMP (cAMP) production [34] [35]. Occurring in species with invasive hemochorial placentae, decidualization enables the endometrium to acquire a receptive phenotype, preventing immunological rejection of the semi-allogeneic embryo and fostering its development [36] [37]. The profound genetic, epigenetic, and proteomic changes during this transition are orchestrated by a complex hormonal cascade, culminating in the brief window of implantation (WOI) [29]. Disruptions in this meticulously regulated process are implicated in significant reproductive disorders, including recurrent implantation failure (RIF), recurrent pregnancy loss, and endometriosis [36] [32] [35]. This review examines the molecular mechanisms, metabolic reprogramming, and experimental methodologies underlying decidualization, framing them within the broader context of hormonal regulation of endometrial gene expression.
Molecular Mechanisms and Genomic Reprogramming
Hormonal Signaling and Transcriptional Regulation
The initiation and progression of decidualization are governed by a well-defined hormonal sequence. Following ovulation, progesterone binding to its receptor (PGR) activates downstream signaling cascades, including the MAPK and PI3K/AKT pathways, which are critical for the expression of decidualization markers [34] [35]. Concurrently, local cAMP accumulation acts as a potent intracellular second messenger, synergizing with progesterone to drive the differentiation of fibroblast-like ESCs into rounded, secretory epithelioid DSCs [34] [37].
Key transcription factors, including HAND2, CEBPB, and EGR1, are upregulated during this process and execute the genomic reprogramming necessary for the decidual phenotype [35]. HAND2, a downstream effector of stromal progesterone signaling, is particularly crucial as it suppresses epithelial cell proliferation via fibroblast growth factors (FGFs), facilitating appropriate endometrial remodeling [35]. Recent research has highlighted the role of epigenetic regulators in this process. Menin, a subunit of the H3K4 methyltransferase complex, facilitates histone 3 lysine 4 trimethylation (H3K4me3) at promoters of genes essential for decidualization, such as SFRP2 and DKK1 (negative regulators of the WNT pathway) [35]. Reduced Menin expression in the endometrial stroma of RIF patients is associated with impaired decidualization and aberrant WNT signaling activation, underscoring the importance of epigenetic regulation in endometrial receptivity [35].
Oxidative Stress Resistance
Decidualizing stromal cells must tolerate high levels of reactive oxygen species (ROS) and inflammation associated with cellular reprogramming and deep placentation [36]. Successful decidualization involves the activation of robust antioxidant defense mechanisms. Key molecular players, including SLC40A1 and GPX4, coordinate iron balance and mitigate lipid peroxidation, thereby conferring cellular resilience to oxidative stress [36]. The resistance to oxidative stress is a hallmark of strong, progesterone-driven decidualization in certain eutherian mammals, creating a specialized maternal-fetal interface that supports pregnancy establishment [36].
Table 1: Key Molecular Regulators of Decidualization
| Regulator | Function | Mechanism of Action | Associated Reproductive Disorder |
|---|---|---|---|
| Menin (MEN1) | Epigenetic regulator | Catalyzes H3K4me3; represses WNT pathway via SFRP2/DKK1 | Recurrent Implantation Failure (RIF) [35] |
| HAND2 | Transcription factor | Suppresses epithelial proliferation via FGFs; stromal progesterone effector | Impaired endometrial receptivity [35] |
| SLC40A1 | Iron transporter | Coordinates iron balance to mitigate oxidative stress | Impaired decidualization [36] |
| GPX4 | Antioxidant enzyme | Reduces lipid peroxidation; confers oxidative stress resistance | Early pregnancy loss [36] |
| GLUT1 | Glucose transporter | Mediates glucose uptake; upregulated by progesterone/PI3K-AKT | Decidualization deficiency in hyperinsulinemia/PCOS [34] |
Metabolic Reprogramming in Decidualization
Glucose Metabolism and the Warburg Effect
Decidualization is an energy-intensive process accompanied by significant metabolic reprogramming [34] [37]. Differentiating stromal cells exhibit characteristics of the Warburg effect, preferentially producing lactate from glucose via glycolysis even under normoxic conditions, rather than through oxidative phosphorylation [34]. This shift to glycolysis provides rapidly available energy and biomass to meet the high demands of cellular differentiation and function.
Glucose uptake, mediated by glucose transporters (GLUTs), is the critical first step in this metabolic shift. Among the GLUT family members expressed in the human endometrium, GLUT1 (SLC2A1) is dynamically regulated during the menstrual cycle, showing significant upregulation in the mid-secretory phase that is further enhanced during decidualization [34]. Progesterone facilitates GLUT1 expression through PGR binding and downstream activation of IRS2, MAPK, and PI3K/AKT pathways [34]. Epigenetic modifications, such as histone H3 lysine-27 acetylation (H3K27ac), have also been implicated in GLUT1 upregulation [34]. Conversely, miR-140-5p downregulates GLUT1, leading to reduced glucose uptake, impaired decidualization, and increased apoptosis [34]. Other transporters, including GLUT3, GLUT4, GLUT8, and SGLT1, also contribute to glucose homeostasis in the endometrium, with dysregulation linked to reproductive pathologies such as PCOS and RIF [34].
Once inside the cell, glucose is metabolized through glycolysis, and key enzymes in this pathway are critically involved in decidualization:
- Hexokinase 2 (HK2): The first rate-limiting enzyme of glycolysis, HK2 expression is upregulated during decidualization, stimulating glucose uptake and lactate production. Its downregulation via miR-6887-3p suppresses glycolysis and impairs decidualization [34].
- Phosphofructokinase-1 (PFK1): This enzyme catalyzes the conversion of fructose-6-phosphate to fructose-1,6-bisphosphate (FBP). Steroid receptor coactivator-2 (SRC-2) accelerates glycolytic flux by inducing PFKFB3, which allosterically activates PFK1. FBP accumulation in DSCs promotes decidualization, trophoblast invasion, and maternal-fetal tolerance [34].
Table 2: Glucose Metabolism in Decidualization
| Metabolic Component | Role in Decidualization | Regulation |
|---|---|---|
| GLUT1 | Primary glucose uptake transporter; expression increases during decidualization | Upregulated by progesterone, PI3K/AKT, H3K27ac; downregulated by miR-140-5p [34] |
| HK2 | Commits glucose to glycolysis; increased activity supports Warburg effect | Downregulated by miR-6887-3p; knockdown impairs decidualization [34] |
| PFK1/PFKFB3 | Rate-limiting step glycolysis; FBP accumulation promotes implantation | Activated by SRC-2 via PFKFB3 induction [34] |
| Warburg Effect | Metabolic shift to glycolysis for rapid ATP and biomass production | Characterized by enhanced extracellular acidification rate (ECAR) [34] [37] |
Metabolic Heterogeneity and Alternative Energy Pathways
Beyond glucose metabolism, decidualization involves reprogramming of amino acid and sphingolipid metabolism [37]. Single-cell RNA sequencing (scRNA-seq) has revealed significant metabolic heterogeneity among decidual cells, with subpopulations exhibiting distinct metabolic activities correlating with differentiation maturity and cellular function [37]. For instance, decidual cells with high metabolic activity demonstrate greater cellular communication potential [37]. Lipids provide essential energy and raw materials for stromal-decidual transformation, and disruption of sphingolipid metabolism can lead to uterine vascular bed instability and impaired decidualization [37]. This metabolic heterogeneity underscores the complexity of energy management during endometrial reprogramming.
Experimental Models and Methodologies
In Vitro Decidualization Models
The gold standard for studying human decidualization in vitro involves isolating and differentiating primary human endometrial stromal cells (hESCs). The following protocol details a typical experimental setup for inducing and validating decidualization:
Protocol: In Vitro Decidualization of Primary hESCs
- Cell Culture: Primary hESCs are isolated from endometrial biopsies obtained during the proliferative phase of the menstrual cycle. Cells are cultured in DMEM/F-12 medium supplemented with 10% charcoal-striped fetal bovine serum (FBS) and 1% penicillin-streptomycin.
- Decidualization Induction: Upon reaching 70-80% confluence, cells are treated with a decidualization cocktail. A standard formulation includes:
- 1 μM Medroxyprogesterone acetate (MPA) or other progestin.
- 0.5 mM cAMP analog (e.g., 8-Br-cAMP).
- 10 nM Estradiol (E2). The medium containing the decidualization stimuli is replaced every 2-3 days for 6-12 days to achieve full differentiation [35].
- Functional Validation: Successful decidualization is confirmed by morphological and molecular markers:
- Morphological Change: Differentiating cells transition from elongated, fibroblastic shapes to larger, rounded epithelioid shapes with expanded cytoplasm. F-actin staining (e.g., with phalloidin) can visualize this cytoskeletal reorganization [35].
- Molecular Markers: The most widely used markers are the secreted products:
- Prolactin (PRL): Secreted levels measured by ELISA in the culture supernatant. A significant increase (often 10-100 fold) is observed in successfully decidualized cells [35].
- Insulin-like Growth Factor Binding Protein-1 (IGFBP-1): mRNA expression measured by qRT-PCR and/or protein levels by Western Blot or immunofluorescence [35].
- Proliferation Assay: Decidualization is associated with a switch from proliferation to differentiation. Assays like EdU incorporation or CCK-8 should show reduced proliferation in decidualized cells compared to undifferentiated controls [35].
Advanced Models and Omics Technologies
- Genetic Manipulation: Lentivirus-mediated knockdown (e.g., of MEN1) or overexpression is used to investigate gene function. Transfected cells are selected with antibiotics (e.g., puromycin) prior to decidualization induction [35].
- Assembloids: To study stromal-epithelial communication, researchers co-culture decidualizing stromal cells with endometrial epithelial organoids. These 3D models, or "assembloids," better recapitulate the tissue microenvironment and allow for the study of paracrine signaling, such as the HAND2-FGFs-FGFR axis [35].
- Single-Cell RNA Sequencing (scRNA-seq): This technology is instrumental in uncovering cellular heterogeneity and metabolic subpopulations within decidualizing stroma. Standard workflows involve cell isolation, library preparation (e.g., using 10x Genomics platform), sequencing, and bioinformatic analysis with packages like Seurat in R [37]. It allows for the identification of rare cell types and trajectory inference (pseudotime analysis) using tools like Monocle2 [37].
- Bulk RNA Sequencing: For comprehensive transcriptomic profiling, bulk RNA-seq of decidualized versus control hESCs is performed. Data analysis pipelines (e.g., alignment with STAR, quantification with RSEM, differential expression with DESeq2) identify differentially expressed genes and pathways [31] [35]. Specialized analyses for alternative splicing and transcript usage (e.g., DTE, DTU) can reveal additional layers of regulation not apparent in gene-level analyses [31].
Diagram 1: Experimental workflow for studying decidualization in vitro.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Decidualization Research
| Reagent/Catalog | Function in Experiment |
|---|---|
| Primary Human Endometrial Stromal Cells (hESCs) | The primary model system for in vitro decidualization studies. |
| Medroxyprogesterone Acetate (MPA) / Progesterone | Synthetic/natural progestin used to activate progesterone receptor signaling and initiate decidualization. |
| 8-Br-cAMP / cAMP | Cell-permeable cAMP analog used to mimic intracellular cAMP signaling, a critical inducer of decidualization. |
| Charcoal-stripped FBS | Serum with steroids removed via charcoal treatment, ensuring a defined hormonal background in cell culture media. |
| Anti-PRL / Anti-IGFBP1 Antibodies | For detecting classic decidualization marker proteins via ELISA, Western Blot, or Immunofluorescence. |
| Lentiviral shRNA Particles (e.g., targeting MEN1) | For stable knockdown of target genes to investigate their functional role in the decidualization process. |
| Seurat / Monocle2 R Packages | Standard bioinformatics software for the analysis of single-cell RNA-sequencing (scRNA-seq) data. |
| DESeq2 R Package | Statistical software for identifying differentially expressed genes from bulk RNA-sequencing data. |
| Revaprazan | Revaprazan, CAS:199463-33-7, MF:C22H23FN4, MW:362.4 g/mol |
| Ro 24-6392 | Ro 24-6392, CAS:131149-63-8, MF:C31H31FN8O8S2, MW:726.8 g/mol |
Clinical Implications and Future Directions
Decidualization in Reproductive Disorders
Dysregulated decidualization is a central factor in several infertility-related conditions. In Recurrent Implantation Failure (RIF), molecular profiling of endometrial tissue has revealed distinct subtypes, including an immune-driven subtype (RIF-I) enriched for inflammatory pathways and a metabolic-driven subtype (RIF-M) characterized by dysregulated oxidative phosphorylation and fatty acid metabolism [32]. This heterogeneity explains the variable response to empirical treatments and underscores the need for personalized diagnostic approaches.
In endometriosis, transcriptomic analyses focusing on the mid-secretory phase have identified splicing quantitative trait loci (sQTLs) and isoform-level changes in genes like ZNF217 and GREB1, which are not detectable through conventional gene-level expression analysis [31]. These alterations in RNA splicing may contribute to impaired decidualization and receptivity in affected women. Furthermore, thin endometrium (TE) is associated with immune-related transcriptomic alterations, including upregulation of cytotoxic genes (CORO1A, GNLY, GZMA) and altered immune cell infiltration, which may disrupt the endometrial microenvironment necessary for successful decidualization [33].
Diagnostic and Therapeutic Perspectives
Accurate assessment of endometrial receptivity remains a challenge. Molecular tests like the endometrial receptivity array (ERA) aim to personalize embryo transfer timing but do not address underlying impaired receptivity [29] [35]. Novel targeted gene expression profiling methods, such as the beREADY test using TAC-seq technology, show promise in detecting displaced WOI with high accuracy, particularly in RIF patients where displaced WOI is significantly more common than in fertile women [29]. Future therapeutic strategies may target specific molecular lesions identified in omics studies. For instance, CMap-based drug predictions suggest sirolimus (rapamycin) for the RIF-I subtype and prostaglandins for the RIF-M subtype [32]. Similarly, correcting Menin deficiency or modulating the WNT pathway could represent novel avenues for treating RIF [35].
Diagram 2: Menin-H3K4me3 regulation of WNT signaling in decidualization.
Decidualization represents a quintessential example of hormonally controlled genomic reprogramming, where progesterone and cAMP signaling drive a cascade of transcriptional, epigenetic, and metabolic changes to transform stromal cells into a receptive matrix for the embryo. The integration of advanced omics technologies has unveiled the remarkable complexity of this process, including significant metabolic reprogramming towards glycolysis, intricate epigenetic regulation, and previously unappreciated heterogeneity at the single-cell level. The molecular insights gained from studying decidualization not only elucidate fundamental biological principles of cellular differentiation and tissue remodeling but also provide critical pathogenetic insights into female infertility. As research continues to unravel the nuanced interplay between hormonal signals, metabolic status, and epigenetic landscapes in the endometrium, the promise of developing targeted, effective diagnostics and therapeutics for implantation disorders grows increasingly tangible.
Advanced Models and Diagnostic Tools: From Organoids to Clinical Biomarkers
Endometrial Organoids as Physiologically Relevant In Vitro Models
The human endometrium, the mucosal lining of the uterus, undergoes dynamic cyclical changes in response to ovarian hormones, making it exceptionally challenging to model in vitro [38]. Research into the hormonal control of endometrial gene expression has been hampered by the limitations of traditional two-dimensional cell culture systems, which fail to recapitulate the tissue's complex architecture and cellular heterogeneity. Endometrial organoids have emerged as revolutionary biomimetic systems that offer a physiologically relevant in vitro model to study the specific tissue or organ of origin [39] [38]. These self-organizing three-dimensional structures derived from primary tissue or non-invasive sources faithfully replicate the cellular, transcriptomic, and functional characteristics of the native endometrium, providing unprecedented opportunities to investigate hormonal regulation, embryo-endometrium interactions, and pathophysiology of endometrial disorders within a controlled laboratory setting.
Physiological Relevance of Endometrial Organoids
Faithful Recapitulation of Native Endometrium
Endometrial organoids closely mimic the in vivo endometrium at multiple biological levels. Transcriptomic analyses comparing organoids to primary tissue have demonstrated conservation of gene expression patterns specific to endometrial cell types, including markers of progenitor cells (LRIG1, PROM1, AXIN2, SOX9), epithelial lineage (EPCAM, KRT7, CDH1), gland development (FOXA2), and secretory activity (PAEP, MUC1) [40]. Single-cell RNA sequencing studies have further validated that organoids maintain the molecular signatures of different epithelial subpopulations found in vivo, including lumenal and glandular phenotypes [41].
Crucially, endometrial organoids retain functional hormone responsiveness, expressing receptors for estrogen (ESR1) and progesterone (PGR), and undergoing appropriate morphological and molecular changes when exposed to hormone treatments that simulate the menstrual cycle [38] [40]. When treated with sex steroids and early-pregnancy hormones such as prolactin (PRL), human placental lactogen (hPL), and human chorionic gonadotropin (hCG), organoids upregulate characteristic 'uterine milk' proteins including glycodelin (PAEP) and exhibit increased mucin expression (MUC1), mirroring the hypersecretory phenotype of early pregnancy [40].
Modeling Temporal Dynamics Across the Menstrual Cycle
The endometrium undergoes profound transcriptomic changes throughout the menstrual cycle, and organoids provide a unique platform to study these dynamic processes. Recent research has identified distinct phase-specific transcriptional patterns, with the most significant changes occurring during transitions between proliferative and secretory phases [31]. During the hormone-driven secretory phase, organoids demonstrate appropriate differentiation responses, including the development of ciliated cells and secretory activity, enabling researchers to model the window of implantation in vitro [41].
Table 1: Transcriptomic Changes in Endometrial Organoids During Hormonal Stimulation
| Gene/Pathway | Response to Hormonal Stimulation | Biological Significance |
|---|---|---|
| PAEP (Glycodelin) | Significant upregulation with progesterone, estrogen, cAMP, and pregnancy hormones [40] | Marker of secretory transformation and endometrial receptivity |
| MUC1 | Increased expression with hormone treatment [40] | Contributes to the formation of a receptive endometrial surface |
| Acetylated Tubulin | Increased expression indicating ciliogenesis [40] | Development of ciliated epithelial cells in response to hormonal cues |
| WNT Signaling | Downregulation promotes secretory lineage differentiation [41] | Pathway regulation determines epithelial cell fate decisions |
| NOTCH Signaling | Downregulation enhances ciliated cell differentiation [41] | Controls balance between secretory and ciliated lineages |
Establishing Endometrial Organoid Cultures
Source Materials and Derivation Protocols
Endometrial organoids can be established from various source materials, each with distinct advantages:
Traditional Biopsies: Endometrial tissue obtained via Pipelle biopsy or scratch biopsy provides a reliable source of glandular fragments for organoid derivation [40]. The protocol involves sequential enzymatic digestion (typically with trypsin and collagenase) to isolate epithelial fragments, which are then embedded in extracellular matrix scaffolds and cultured with specialized media containing growth factors and pathway modulators [42].
Menstrual Flow: A non-invasive alternative utilizing gland fragments recovered from menstrual flow collected in menstrual cups [40]. This approach achieves an 87% success rate in organoid derivation and produces organoids that are transcriptomically and functionally identical to those derived from paired biopsy samples from the same patient [40]. The method eliminates the need for invasive procedures, enabling longitudinal sampling and broader participation in research studies.
Culture Conditions and Extracellular Matrix Requirements
Successful long-term maintenance of endometrial organoids requires specific culture conditions. The base medium typically consists of Advanced DMEM/F12 supplemented with essential components including B27, N2, nicotinamide, and growth factors such as EGF, FGF-10, R-spondin1, Noggin, and Wnt3a [42]. The TGF-β receptor inhibitor A83-01 is often included to support epithelial growth [42].
The extracellular matrix scaffold is critical for three-dimensional growth. While Matrigel (commercially available as Cultrex) has been traditionally used, recent advances include fully synthetic polyethylene glycol (PEG)-based hydrogels functionalized with adhesion peptides such as GFOGER (collagen-derived) and PHSRN-K-RGD (fibronectin-derived) [43]. These defined synthetic matrices support both epithelial organoids and stromal co-cultures while enabling precise control over biophysical and biochemical properties [43].
Co-culture Systems for Stromal-Epithelial Crosstalk
The endometrium functions through intricate stromal-epithelial interactions, which can be modeled using advanced co-culture systems. A recently developed protocol enables the establishment of stromal and epithelial cells from the same biological source, allowing investigation of paracrine factors impacting epithelial development [42]. In these systems, stromal cells are expanded in 2D culture before being co-cultured with freshly isolated epithelial cells, enabling the study of hormone-mediated signaling in a more physiological context [42].
Fully synthetic hydrogel platforms have been developed to co-culture endometrial epithelial organoids with stromal cells, capturing healthy and disease states across a simulated menstrual cycle [43]. These systems have revealed dysregulation of epithelial proliferation mediated by stromal cells during inflammation, highlighting their utility for studying pathological mechanisms [43].
Applications in Hormonal Control Research
Studying Hormonal Regulation of Gene Expression
Endometrial organoids provide a controlled system to investigate how ovarian hormones regulate gene expression networks. Transcriptomic analyses of organoids have revealed that estrogen and progesterone regulate distinct sets of genes involved in cell proliferation, differentiation, and secretory function [38] [41]. Importantly, organoids enable researchers to dissect the specific contributions of epithelial versus stromal compartments to hormonal responses through compartment-specific analyses and co-culture experiments.
Recent studies utilizing organoids have identified a crucial role for WNT and NOTCH signaling pathways in mediating hormonal effects on epithelial differentiation [41]. Downregulation of WNT signaling promotes secretory lineage differentiation, while NOTCH pathway inhibition enhances ciliated cell differentiation, revealing the pathway regulation that determines epithelial cell fate decisions in response to hormonal cues [41].
Table 2: Key Signaling Pathways in Endometrial Organoid Hormonal Response
| Pathway | Role in Endometrial Biology | Experimental Manipulation | Effect on Organoid Differentiation |
|---|---|---|---|
| WNT Signaling | Regulates glandular proliferation and secretory differentiation [41] | Downregulation via inhibitors [41] | Increases secretory lineage differentiation efficiency [41] |
| NOTCH Signaling | Controls balance between ciliated and secretory cell fates [41] | Downregulation via inhibitors [41] | Enhances ciliated cell differentiation [41] |
| Estrogen Signaling | Drives proliferative phase changes via ESR1 [38] | 17-β-estradiol treatment [40] | Induces proliferation and P4-R expression [40] |
| Progesterone Signaling | Mediates secretory transformation via PGR [38] | Progesterone treatment [40] | Promotes secretory changes and downregulates P4-R [40] |
Modeling the Window of Implantation
Endometrial organoids have proven particularly valuable for studying the window of implantation (WOI), the brief period when the endometrium becomes receptive to embryo implantation. Organoid-based adhesion models have emerged as appropriate in vitro platforms that faithfully reproduce the receptive endometrium [39]. These models enable the study of molecular mechanisms underlying early embryo-endometrium interaction while bypassing ethical restrictions associated with human embryo research.
Transcriptomic profiling of organoids has identified biomarkers of endometrial receptivity, facilitating the development of clinical diagnostic tests such as the beREADY test, which utilizes targeted gene expression profiling of 68 endometrial receptivity genes to accurately determine WOI timing [29]. In clinical validation, this approach detected displaced WOI in 15.9% of women with recurrent implantation failure compared to only 1.8% of fertile women, highlighting the clinical relevance of molecular signatures identified using organoid models [29].
Disease Modeling and Drug Screening
Endometrial organoids provide powerful platforms for investigating the pathophysiology of endometrial disorders and screening potential therapeutics. Organoids derived from patients with conditions such as endometriosis, endometrial cancer, and thin endometrium retain disease-specific characteristics, enabling researchers to study molecular mechanisms underlying these conditions [33] [32].
For recurrent implantation failure (RIF), organoid studies have helped identify two distinct molecular subtypes: an immune-driven subtype (RIF-I) characterized by enriched immune and inflammatory pathways, and a metabolic-driven subtype (RIF-M) featuring dysregulation of oxidative phosphorylation and fatty acid metabolism [32]. This subtyping has enabled predictions of targeted therapeutic approaches, with sirolimus suggested for RIF-I and prostaglandins for RIF-M [32].
In thin endometrium, organoid models have revealed immune-related transcriptomic alterations, including upregulation of CORO1A, GNLY, and GZMA—genes functionally related to cytotoxic immune responses [33]. These findings suggest that immune dysregulation may play a more prominent role than previously recognized in this condition's pathogenesis [33].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Endometrial Organoid Culture
| Reagent Category | Specific Examples | Function in Organoid Culture |
|---|---|---|
| Base Medium | Advanced DMEM/F12 [42] | Nutrient foundation for organoid growth |
| Essential Supplements | B27 supplement, N2 supplement, Nicotinamide [42] | Provide essential growth factors and nutrients |
| Growth Factors | EGF, FGF-10, R-spondin1, Noggin, Wnt3a [42] | Maintain progenitor state and promote proliferation |
| Pathway Inhibitors | A83-01 (TGF-β receptor inhibitor) [42] | Supports epithelial growth by inhibiting differentiation |
| Enzymatic Dissociation | Trypsin, Collagenase V [42] | Tissue digestion and organoid passaging |
| Extracellular Matrix | Cultrex (Matrigel), Synthetic PEG hydrogels [42] [43] | 3D scaffold for organoid growth and differentiation |
| Hormonal Stimuli | Progesterone, Estrogen, cAMP, PRL, hPL, hCG [40] | Induce secretory differentiation and receptivity |
| Sakurasosaponin | Sakurasosaponin | High-purity Sakurasosaponin for lab research. Explore its potential in anticancer studies and other biological applications. For Research Use Only. |
| Sangivamycin | Sangivamycin | Sangivamycin is a potent nucleoside analog for research into cancer, COVID-19, and viral mechanisms. This product is For Research Use Only (RUO). |
Endometrial organoids represent a transformative in vitro model system that faithfully recapitulates the physiological characteristics of the native endometrium. Their ability to mimic in vivo transcriptomic profiles, hormone responsiveness, and functional differentiation makes them invaluable tools for investigating the hormonal control of endometrial gene expression. As research advances, organoid models will continue to refine our understanding of endometrial biology, enable personalized approaches to treating endometrial disorders, and provide platforms for developing novel therapeutics for conditions ranging from infertility to endometrial cancer. The integration of organoids with emerging technologies such as single-cell multi-omics, CRISPR-based screening, and microfluidic systems will further enhance their utility in reproductive research and clinical translation.
Single-Cell and Spatial Transcriptomics for Cell-Type-Specific Analysis
The human endometrium, the mucosal lining of the uterus, undergoes dramatic cyclic remodeling under precise hormonal control throughout a woman's reproductive life. This complex tissue consists of multiple interacting cell types—including epithelial, stromal, fibroblast, and immune cells—that must coordinate dynamically to establish endometrial receptivity for embryo implantation. Understanding the cell-type-specific gene expression programs governing these processes has been transformed by the advent of single-cell and spatial transcriptomic technologies. These approaches now enable researchers to decode the cellular heterogeneity and spatiotemporal organization of endometrial tissue with unprecedented resolution, revealing how hormonal signaling orchestrates cellular responses across the menstrual cycle and how these processes become dysregulated in reproductive disorders.
This technical guide provides an in-depth framework for applying single-cell and spatial transcriptomics to investigate hormonal control of endometrial gene expression. We present comprehensive datasets, detailed methodologies, signaling pathway diagrams, and essential research tools that empower researchers to explore endometrial biology at cellular resolution, with particular emphasis on technical considerations for drug development applications.
Quantitative Atlas of Endometrial Cellular Heterogeneity
Large-scale integration of single-cell and single-nucleus RNA sequencing datasets has established comprehensive reference atlases that quantitatively map the cellular composition of the human endometrium across the menstrual cycle and in pathological states. The recently developed Human Endometrial Cell Atlas (HECA) represents the most comprehensive resource to date, harmonizing data from 121 individuals and approximately 626,000 cells and nuclei [44].
Table 1: Major Cell Populations in the Human Endometrial Cell Atlas
| Cell Category | Specific Cell Types | Key Marker Genes | Hormonal Response Characteristics |
|---|---|---|---|
| Epithelial Cells | SOX9+ basalis (CDH2+) progenitor cells | SOX9, CDH2, AXIN2, ALDH1A1 | Resident in basalis; relatively hormone-independent |
| Functionalis glandular cells | Not specified in results | Highly responsive to estrogen and progesterone | |
| Luminal epithelial cells | Not specified in results | First point of contact for implantation | |
| Stromal/ Mesenchymal Cells | Decidualized stromal cells | Not specified in results | Specialized response to progesterone |
| Fibroblast basalis (C7+) | CXCL12 | Interacts with progenitor cells via CXCL12-CXCR4 | |
| Perivascular cells | CD9, SUSD2 | Putative progenitor function | |
| Immune Cells | Endometrial macrophages | Various | Implicated in endometriosis pathogenesis |
| CD45+ leukocytes | Various | Distinct functionalis vs. subluminal populations | |
| CD56+ leukocytes | Various | Natural killer cell populations |
The power of integrated single-cell atlases is further demonstrated by their ability to identify previously unrecognized cell populations. For instance, HECA revealed a SOX9+ basalis (CDH2+) epithelial population expressing established endometrial stem/progenitor markers that interacts with fibroblast populations via CXCL12-CXCR4 signaling [44]. This population was spatially mapped to basalis glands using spatial transcriptomics and single-molecule fluorescence in situ hybridization (smFISH), illustrating how multi-modal approaches validate and contextualize atlas findings.
Table 2: Technical Comparison of Endometrial Transcriptomic Studies
| Study | Technology | Sample Size | Key Findings | Relevance to Hormonal Control |
|---|---|---|---|---|
| HECA [44] | scRNA-seq + snRNA-seq + spatial | 121 individuals, ~626,000 cells/nuclei | Identified SOX9+ basalis progenitor population; stromal-immune dysregulation in endometriosis | Comprehensive mapping across menstrual cycle phases |
| RIF Spatial Atlas [45] | 10x Visium spatial transcriptomics | 8 samples (4 RIF, 4 controls) | 7 distinct cellular niches; 685 DEGs in luminal epithelium in RIF | Mid-luteal phase timing (LH+7) |
| Cell-type-specific RNA-seq [46] | FACS + RNA-seq | 16 women (paired LH+2 and LH+7) | 499 epithelial and 581 stromal genes up-regulated in receptivity | Direct comparison of pre-receptive vs. receptive phases |
| TE scRNA-seq [14] | scRNA-seq | 6 samples (3 TE, 3 normal) | Perivascular CD9+SUSD2+ cells as progenitors; dysfunctional collagen deposition | Proliferative phase defects in thin endometrium |
| RIF Regional Analysis [47] | Spatial transcriptomics | 16 women (8 RIF, 8 fertile) | Region-specific DEGs (685 luminal epithelium, 293 glandular epithelium) | WNT signaling and estradiol response pathways altered |
Experimental Framework for Endometrial Transcriptomics
Sample Collection and Processing Protocols
Patient Selection and Ethical Considerations Endometrial transcriptomic studies require careful patient characterization and ethical oversight. The research protocol should be approved by an institutional ethics committee, with written consent obtained from all participants [45]. Key inclusion criteria typically encompass: regular menstrual cycles (25-35 days), age ≤35 years, BMI <28 kg/m², absence of uterine pathologies (endometriosis, adenomyosis, leiomyoma), and no hormonal medication for ≥3 months prior to recruitment [45] [46]. For receptivity studies, participants should have proven fertility (at least one live birth) and normal ovarian function.
Menstrual Cycle Timing and Biopsy Collection Precise cycle phase determination is essential for interpreting hormonal responses. Methods combine menstrual history, urinary luteinizing hormone (LH) surge detection (LH+0), transvaginal ultrasound, and endometrial histology using Noyes' criteria [46]. Receptive-phase sampling typically occurs at LH+7/LH+8, while pre-receptive samples are collected at LH+2 [46]. Biopsies are obtained using a Pipelle catheter or hysteroscopic guidance from the uterine fundus/upper wall [45] [14].
Single-Cell/Nucleus Suspension Preparation For scRNA-seq: fresh tissue undergoes enzymatic digestion (collagenase-based protocols) followed by fluorescence-activated cell sorting (FACS) if specific populations are targeted [46]. For snRNA-seq: snap-frozen tissue is cryosectioned, with nuclei isolated using homogenization and density gradient centrifugation [44]. Quality control measures include RNA Integrity Number (RIN) >7 for spatial transcriptomics [45] and cell viability >80% for live cell protocols.
Single-Cell RNA Sequencing Workflow
The following diagram illustrates the comprehensive workflow for single-cell and spatial transcriptomic analysis of endometrial tissues:
Library Preparation and Sequencing The 10x Genomics platform is widely used for single-cell and spatial transcriptomics. For single-cell applications, the Chromium system generates barcoded droplets for 3'-end counting. For spatial transcriptomics, the Visium platform captures RNA directly from tissue sections on patterned arrays containing ~5,000 barcoded spots [45]. Sequencing is performed on Illumina platforms (NovaSeq 6000) with PE150 configuration, targeting sequencing saturation >90% and Q30 scores >90% for all read types [45].
Computational Analysis Pipeline
Quality Control and Preprocessing Raw sequencing data is processed through Space Ranger (spatial) or Cell Ranger (single-cell) pipelines aligned to the human reference genome (GRCh38) [45]. The Seurat R package (v4.3.0+) is used for downstream analysis [45] [14]. Quality thresholds typically exclude cells with <500-1,000 genes or >10,000 transcripts, and mitochondrial gene percentage >20% [45] [14]. Spatial data spots with <500 genes or >20% mitochondrial genes are also filtered out [45].
Data Integration and Clustering Batch effects across samples are corrected using Harmony integration [45] [14]. Highly variable genes are selected (typically 3,000-4,800 features) for principal component analysis. Shared nearest neighbor graph construction uses top principal components (typically 30 PCs), followed by clustering at resolution 0.6-0.7 [45] [14]. Cell types are annotated using canonical markers from reference datasets.
Differential Expression and Pathway Analysis Differentially expressed genes (DEGs) between conditions are identified using Seurat's FindAllMarkers or FindMarkers functions. Gene Ontology (GO) enrichment analysis is performed with clusterProfiler (v4.12.2+) [14]. Cell-cell communication networks are inferred using tools like CellChat to map ligand-receptor interactions across cell populations [44] [14].
Spatial Deconvolution The conditional autoregressive-based deconvolution (CARD) package estimates cell type proportions within spatial transcriptomics spots by integrating single-cell reference data [45]. This enables mapping of cell-type-specific expression patterns within tissue architecture.
Signaling Pathways in Endometrial Cell Communication
Key Signaling Pathways in Endometrial Organization
Single-cell and spatial transcriptomic analyses have revealed intricate signaling networks that coordinate cellular responses to hormonal cues in the endometrium. The following diagram illustrates the principal signaling pathways governing cellular organization and communication in the endometrial microenvironment:
Pathway-Specific Molecular Mechanisms
TGF-β Signaling in Functionalis Coordination In the functionalis layer, intricate stromal-epithelial coordination occurs via transforming growth factor beta (TGFβ) signaling [44]. This pathway facilitates paracrine communication between decidualizing stromal cells and adjacent epithelial populations, synchronizing tissue remodeling in response to progesterone dominance during the secretory phase. Disruption of this signaling axis may contribute to impaired receptivity in conditions like recurrent implantation failure.
CXCL12-CXCR4 Axis in Basalis Niche Maintenance The basalis layer features specialized signaling between SOX9+ basalis epithelial cells and fibroblast populations through the CXCL12-CXCR4 chemokine axis [44]. Fibroblast basalis (C7+) cells express CXCL12, which interacts with CXCR4 receptors on SOX9+ epithelial cells, maintaining progenitor cell properties and supporting regenerative capacity after menstruation.
WNT Signaling in Endometriosis Pathogenesis In endometriosis, ectopic endometrial stromal cells exhibit WNT5A upregulation and aberrant activation of non-canonical WNT signaling [48]. This pathway mediates interactions between ectopic endometrial stromal cells and distinct ovarian stromal cell (OSC) populations, promoting lesion establishment and growth. Two distinct OSC types localize to different lesion zones, displaying gene expression profiles associated with fibrosis and inflammation, respectively [48].
Extracellular Matrix Dysregulation in Thin Endometrium In thin endometrium (TE), perivascular CD9+SUSD2+ cells show disrupted collagen deposition around blood vessels, indicating impaired extracellular matrix remodeling during endometrial repair [14]. This dysfunctional matrix organization likely contributes to the inadequate endometrial growth characteristic of TE, highlighting the importance of stem cell-microenvironment interactions in endometrial regeneration.
Essential Research Reagent Solutions
Table 3: Essential Research Reagents for Endometrial Transcriptomics
| Reagent Category | Specific Product | Application | Technical Considerations |
|---|---|---|---|
| Tissue Dissociation | Collagenase-based digestion kits | Single-cell suspension preparation | Optimization required for endometrial tissue; affects cell type recovery |
| Cell Sorting | FACS antibodies (CD9, SUSD2) | Progenitor cell isolation | Enables cell-type-specific RNA-seq; preserves transcriptional states |
| Single-Cell Platform | 10x Genomics Chromium | scRNA-seq library preparation | Standardized workflow; 3'-end counting sufficient for cell typing |
| Spatial Transcriptomics | 10x Visium Spatial Kit | Spatial gene expression mapping | Requires fresh frozen tissue; RIN >7 essential for RNA quality |
| Sequencing | Illumina NovaSeq 6000 | High-throughput sequencing | PE150 configuration; target >90% sequencing saturation |
| Computational Tools | Seurat R package | scRNA-seq data analysis | Comprehensive toolkit for QC, integration, clustering, and DEG |
| Harmony algorithm | Batch effect correction | Essential for multi-sample integration preserving biology | |
| CARD package | Spatial deconvolution | Maps cell types to spatial locations using scRNA-seq reference | |
| CellChat | Cell-cell communication | Infers ligand-receptor interactions from scRNA-seq data | |
| Validation | smFISH probes | Spatial validation of markers | Confirms single-cell findings in tissue context |
| Immunofluorescence antibodies | Protein-level validation | Critical for translational confirmation of transcriptomic findings |
Single-cell and spatial transcriptomic technologies have fundamentally transformed our ability to investigate hormonal control of endometrial gene expression with cell-type-specific resolution. The integrated approaches outlined in this technical guide—combining single-cell RNA sequencing, spatial transcriptomics, computational deconvolution, and signaling pathway analysis—provide a powerful framework for decoding the complex cellular interactions that underpin endometrial function and dysfunction.
These methodologies have revealed previously unappreciated cellular heterogeneity, including SOX9+ basalis progenitor populations, distinct perivascular stem cells, and specialized stromal niches that maintain tissue homeostasis through precise signaling networks. The application of these technologies to reproductive disorders has identified key pathogenic mechanisms: WNT signaling dysregulation in endometriosis, collagen deposition defects in thin endometrium, and region-specific transcriptional alterations in recurrent implantation failure.
For drug development professionals, these insights offer new opportunities for targeted therapeutic strategies. The cell-type-specific signaling pathways and ligand-receptor interactions identified through these approaches represent promising targets for treating endometriosis, implantation failure, and other endometrial disorders with greater precision and fewer systemic effects. As these technologies continue to evolve, they will undoubtedly yield further insights into endometrial biology and empower the development of novel interventions for reproductive health conditions.
Endometrial Receptivity Arrays (ERA) and Molecular Diagnostics for Infertility
Endometrial receptivity is a critical, transient phase in the menstrual cycle when the endometrium acquires a functional status capable of supporting blastocyst implantation. This window of implantation (WOI) represents a hormonally coordinated process driven by complex gene expression changes that prepare the uterine environment for embryonic attachment. The molecular orchestration of this process involves precise transcriptional regulation mediated primarily by estrogen and progesterone signaling, which synchronizes endometrial cellular responses to create a receptive microenvironment [49].
The development of Endometrial Receptivity Array (ERA) technology represents a significant advancement in molecular diagnostics for infertility, enabling precise identification of the WOI through transcriptomic profiling. This approach has transformed the assessment of endometrial function from histopathological dating to quantitative molecular phenotyping, offering unprecedented insights into the hormonal control of endometrial gene expression [49]. For researchers and drug development professionals, understanding ERA methodology and applications provides critical foundations for developing targeted infertility interventions and refining personalized treatment approaches in assisted reproductive technologies (ART).
Hormonal Regulation of Endometrial Gene Expression
Molecular and Genetic Markers of Receptivity
The transition to a receptive endometrial state is characterized by distinct molecular changes mediated by hormonal signaling. During the WOI, which typically occurs between days 19-21 of a 28-day menstrual cycle, the endometrium exhibits a unique gene expression signature regulated by progesterone and estrogen activity [49]. Key molecular markers include:
Estrogen receptor-alpha (ER-α) and progesterone receptor (PR): These nuclear receptors mediate hormonal signaling essential for endometrial maturation. Their expression patterns shift during the WOI, with decreased stromal PR signaling facilitating decidualization [49].
Transcriptional regulators: Factors including COUP-TFII suppress inhibitory pathways while BCL6 immunoregulatory gene expression increases during receptivity. Aberrant BCL6 expression is associated with impaired receptivity in endometriosis and other inflammatory reproductive disorders [49].
Implantation markers: Genes including HOXA10, glycodelin, and specific integrins demonstrate cycle-dependent expression patterns directly regulated by hormonal signaling [50]. These molecular changes collectively create a favorable environment for embryo implantation through regulation of immune tolerance, vascular remodeling, and cellular adhesion pathways.
Table 1: Key Molecular Markers of Endometrial Receptivity and Their Hormonal Regulation
| Molecular Marker | Function in Endometrial Receptivity | Hormonal Regulation |
|---|---|---|
| ER-α and PR | Nuclear receptors mediating estrogen and progesterone signaling | Direct ligand activation by estrogen and progesterone |
| COUP-TFII | Transcription factor suppressing inhibitory pathways | Progesterone-dependent expression |
| BCL6 | Immunoregulatory gene | Upregulated by inflammatory cytokines; associated with progesterone resistance |
| HOXA10 | Homeobox transcription factor critical for implantation | Estrogen and progesterone-regulated expression |
| Glycodelin | Endometrial secretory protein modulating immune response | Progesterone-induced secretion during secretory phase |
| Integrins | Cell adhesion molecules facilitating embryonic attachment | Hormonally regulated expression during WOI |
Signaling Pathways in Endometrial Receptivity
The complex process of endometrial receptivity involves coordinated activity across multiple signaling pathways that respond to hormonal cues. The PI3K/AKT/MAPK pathway integrates insulin signaling with hormonal responses, while Wnt/β-catenin signaling interacts with progesterone receptor activity to regulate stromal cell decidualization [9]. In conditions associated with endometrial dysfunction such as polycystic ovary syndrome (PCOS), hyperinsulinemia and insulin resistance can disrupt these pathways through androgen-mediated shifts in WT1 transcription factor and altered Wnt/β-catenin activity [9]. Simultaneously, inflammatory cytokines including TNF-α and IL-6 interfere with normal estrogen, progesterone, and insulin receptor signaling, creating a suboptimal environment for implantation [9].
Diagram 1: Hormonal Control of Endometrial Receptivity Signaling Pathways
ERA Technology: Development and Technical Aspects
Evolution from Histological to Molecular Assessment
Traditional methods for assessing endometrial receptivity relied primarily on histological evaluation of endometrial tissue biopsies according to the Noyes criteria, which determined morphological changes during the menstrual cycle. These methods suffered from significant subjectivity, variability, and limited predictive value for implantation success [49]. The development of ERA addressed these limitations by introducing a quantitative molecular approach based on gene expression profiling.
The original ERA methodology utilized microarray technology to analyze the expression of approximately 248 genes associated with endometrial receptivity [49]. This molecular signature enabled objective classification of endometrial status into receptive, pre-receptive, or post-receptive phases, providing a personalized assessment of each patient's WOI. Subsequent technological advancements have introduced alternative platforms including targeted RNA sequencing and quantitative PCR-based approaches, further improving test accuracy and accessibility [29] [51].
Technical Methodology and Workflow
The standard ERA protocol involves obtaining an endometrial biopsy during the putative window of implantation, typically day 19-21 of a natural cycle or after 5-6 days of progesterone administration in a hormonally controlled cycle [49]. The tissue sample undergoes RNA extraction, followed by targeted analysis of receptivity-associated genes using microarray, next-generation sequencing, or qPCR platforms.
Recent methodological innovations include the beREADY assay, which employs Targeted Allele Counting by sequencing (TAC-seq) technology to analyze 72 genes (57 endometrial receptivity biomarkers, 11 additional WOI-relevant genes, and 4 housekeeping genes) [29]. This approach enables highly quantitative analysis of transcript abundance down to single-molecule level, providing superior sensitivity and dynamic range compared to earlier methodologies.
Table 2: Comparison of Molecular Diagnostic Platforms for Endometrial Receptivity Testing
| Platform/Test | Technology | Genes Analyzed | Reported Accuracy | Advantages |
|---|---|---|---|---|
| ERA (Igenomix) | Microarray | ~248 | Not specified | Established validation data; widespread clinical use |
| beREADY | TAC-seq | 72 | 98.2% validation accuracy | High sensitivity; quantitative measurement; scalable |
| ER Map (IGLS) | Not specified | Not specified | Not specified | Comprehensive diagnostic approach |
| WIN-Test (INSERM) | Not specified | Not specified | Not specified | Alternative methodology |
| rsERT (Yikon Genomics) | Not specified | Not specified | Not specified | Regional accessibility |
Diagram 2: Experimental Workflow for Endometrial Receptivity Testing
Clinical Validation and Performance Data
Analytical Validation Studies
The beREADY model development involved analysis of 63 endometrial biopsies spanning proliferative, early-secretory, mid-secretory, and late-secretory endometrial phases. Following exclusion of 11 samples with inconsistent histology and LH-day measurements, the remaining samples demonstrated clear clustering according to menstrual cycle phases, enabling precise receptivity class prediction [29]. The predictive model achieved 98.8% accuracy in cross-validation for classifying pre-receptive, receptive, and post-receptive stages.
Validation studies on 57 samples from healthy volunteers demonstrated that the test correctly identified all early-secretory phase samples as pre-receptive and all late-secretory samples as post-receptive. Among mid-secretory phase samples, which correspond to the expected WOI, 96.2% (25/26) were classified as receptive, with 23.1% (6/26) falling within the early-receptive transitional zone representing normal WOI variability [29]. Only one sample (1.8%) demonstrated displaced WOI in this fertile control group.
Clinical Performance in Patient Populations
ERA testing has demonstrated particular utility in populations with recurrent implantation failure (RIF). In a study of 44 women with RIF, displaced WOI was detected in 15.9% of cases, significantly higher than the 1.8% rate observed in fertile controls (p=0.012) [29]. Specifically, 6.8% showed pre-receptive profiles and 9.1% demonstrated post-receptive profiles, supporting the concept that WOI displacement contributes to implantation failure in a subset of RIF patients.
Notably, research examining PCOS patients found no significant differences in endometrial receptivity biomarker expression compared to healthy women across all menstrual cycle phases [29]. This suggests that endometrial receptivity dysfunction may not be a primary factor in PCOS-related infertility, despite systemic metabolic and endocrine disturbances characteristic of this condition [9].
Experimental Protocols and Research Applications
Protocol for Endometrial Receptivity Analysis Using TAC-Seq
Sample Collection and Preparation
- Perform endometrial biopsy using standard pipelle technique during putative WOI (LH+7 in natural cycles or after 5 days of progesterone administration in hormone replacement therapy cycles)
- Immediately stabilize tissue in RNAlater or similar RNA stabilization solution
- Store at -80°C until RNA extraction
- Extract total RNA using column-based purification methods with DNase treatment
- Assess RNA quality using Bioanalyzer or similar system (RIN >7.0 recommended)
Library Preparation and TAC-Seq
- Convert RNA to cDNA using reverse transcription with gene-specific primers
- Amplify target regions using multiplex PCR with barcoded primers for sample multiplexing
- Purify amplification products using solid-phase reversible immobilization (SPRI) beads
- Quantify library concentration using fluorometric methods
- Pool libraries at equimolar concentrations for sequencing
- Sequence on Illumina platform (minimum 100,000 reads per sample recommended)
Bioinformatic Analysis
- Demultiplex sequencing data using barcode information
- Align reads to reference transcriptome
- Calculate transcript abundance using unique molecular identifiers (UMIs) for digital counting
- Normalize expression data using housekeeping genes
- Apply computational classification model (beREADY or similar) for receptivity status determination
- Generate clinical report indicating receptive, pre-receptive, or post-receptive status
Protocol for Cross-Platform Validation of Molecular Diagnostics
For transferring ERA testing between qPCR platforms, specific validation protocols are required [51]:
- Perform equivalence testing using Bland-Altman and Deming regression analyses
- Establish platform-specific cutoff values through method comparison studies
- Evaluate cross-platform agreement using kappa statistics
- Assess precision through repeatability and reproducibility studies
- Validate analytical performance across intended quantification range
Research Reagent Solutions and Technical Tools
Table 3: Essential Research Reagents for Endometrial Receptivity Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| RNA Stabilization Reagents | RNAlater, PAXgene Tissue System | Preservation of endometrial tissue RNA integrity during storage and transport |
| RNA Extraction Kits | miRNeasy Mini Kit, Monarch Total RNA Miniprep Kit | High-quality total RNA isolation including small RNAs |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit | cDNA synthesis with consistent efficiency across samples |
| Target Amplification Systems | Multiplex PCR kits, AmpliSeq Transcriptome | Targeted amplification of endometrial receptivity gene panels |
| Sequencing Platforms | Illumina NextSeq, Ion Torrent | High-throughput sequencing of transcriptome libraries |
| Housekeeping Genes | GAPDH, ACTB, RPLP0, B2M | Reference genes for expression data normalization |
| Bioinformatic Tools | DESeq2, EdgeR, ClustVis | Differential expression analysis and data visualization |
Current Limitations and Future Directions
Despite advances in ERA technology, several challenges remain in molecular assessment of endometrial receptivity. Significant heterogeneity exists between transcriptomic studies, with limited overlap in identified biomarkers across different research groups [52]. This variability stems from differences in sample timing, processing methodologies, population selection, and data analysis pipelines, complicating identification of conserved pathways in endometrial receptivity.
Future directions include integration of multi-omics approaches combining transcriptomic, epigenomic, proteomic, and metabolomic data to comprehensively characterize the receptive endometrium [50]. Additionally, implementation of single-cell RNA sequencing will enable resolution of cellular heterogeneity within endometrial tissue and identification of cell-type-specific receptivity signatures [52]. Artificial intelligence applications may further enhance predictive accuracy through pattern recognition in complex molecular datasets [49].
The continued refinement of molecular diagnostics for endometrial receptivity holds significant promise for personalized embryo transfer in ART. By precisely identifying the individual WOI, these approaches may optimize implantation rates particularly in patients with previous implantation failure. However, broader implementation requires standardized protocols, rigorous validation across diverse patient populations, and consensus regarding clinical interpretation criteria.
Personalized Hormone Screening Platforms for IVF Treatment Optimization
Successful embryo implantation during in vitro fertilization (IVF) hinges on a precisely timed dialogue between the embryo and a receptive endometrium. This state of receptivity, known as the window of implantation (WOI), is predominantly orchestrated by ovarian hormones—estrogen and progesterone—which exert their effects by regulating complex gene expression networks within the endometrial tissue [29]. Disruptions in this hormonal control can lead to displaced WOI and is a key factor in conditions like recurrent implantation failure (RIF) and thin endometrium (TE) [29] [32] [33].
Personalized hormone screening platforms represent a paradigm shift in reproductive medicine. They move beyond traditional, population-averaged hormonal protocols to an approach that deciphers the individual's endometrial molecular response to hormonal cues. By analyzing the transcriptomic landscape of the endometrium, these platforms can identify a patient's unique receptivity signature, thereby enabling precise synchronization of embryo transfer with the WOI and paving the way for customized hormonal interventions [29].
This technical guide explores the scientific foundation, key methodologies, and emerging applications of these platforms within the context of hormonal control of endometrial gene expression, providing researchers and drug developers with the tools to advance this transformative field.
Hormonal Regulation of Endometrial Receptivity: A Transcriptomic Perspective
The endometrial tissue undergoes dynamic molecular changes across the menstrual cycle, driven by fluctuating hormone levels. Recent high-resolution transcriptomic studies reveal that this regulation is far more complex than previously understood, occurring not only at the gene expression level but also through alternative splicing and isoform-specific expression.
Gene-Level and Isoform-Level Dynamics
Research involving large endometrial transcriptomic datasets (n=206) has demonstrated that the most significant transcriptomic changes occur during the transition from the mid-proliferative (MP) to the early-secretory (ES) and mid-secretory (MS) phases [31]. While gene-level expression analysis (Differential Gene Expression, DGE) identifies broad changes, transcript-level analyses (Differential Transcript Expression, DTE; Differential Transcript Usage, DTU; and Differential Splicing, DS) uncover an additional layer of regulation. A comparative analysis between MP and MS phases revealed that 24.5% of genes with evidence of DTU and 27.0% with DS would have been missed by DGE analysis alone [31]. This indicates that hormone-driven alternative splicing and isoform selection are critical mechanisms in preparing the endometrium for implantation.
Genetic Regulation of Splicing in Endometriosis
The genetic basis for individual variation in endometrial response is increasingly being uncovered. Splicing Quantitative Trait Loci (sQTL) analysis, which identifies genetic variants that regulate RNA splicing, has been applied to the endometrium. One study identified 3,296 sQTLs in endometrial tissue, with the majority (67.5%) of these genetic effects on splicing not being discovered in a standard gene-level eQTL analysis [31]. Furthermore, by integrating sQTL data with endometriosis genome-wide association study (GWAS) data, two genes, GREB1 and WASHC3, were significantly linked to endometriosis risk through genetically regulated splicing events [31]. This establishes a direct molecular link between genetic variation, hormone-mediated splicing, and endometrial pathology.
Table 1: Transcriptomic Changes in the Human Endometrium Across the Menstrual Cycle
| Analysis Level | Number of Genes with Changes (MP vs. MS phase) | Genes Unique to This Level (Not in DGE) | Key Biological Insight |
|---|---|---|---|
| Gene-Level (DGE) | 11,912 | - | Baseline measure of gene expression magnitude. |
| Transcript-Level (DTE) | 11,930 | 1,536 (12.9%) | Reveals changes in specific transcript isoforms. |
| Transcript Usage (DTU) | 2,347 | 576 (24.5%) | Identifies shifts in the relative abundance of a gene's transcripts. |
| Splicing (DS) | 3,205 | 865 (27.0%) | Uncovers hormone-regulated alternative splicing events. |
Source: Adapted from [31]
Established Platforms and Analytical Methodologies
Several targeted molecular assays have been developed to translate transcriptomic findings into clinically actionable diagnostics for endometrial receptivity.
The beREADY Targeted Sequencing Model
The beREADY model is a quantitative PCR-based test for reliable WOI detection. Its methodology offers a robust framework for a personalized screening platform [29].
Workflow and Experimental Protocol:
- Sample Collection: An endometrial biopsy is performed during a mock cycle. Tissue is snap-frozen or stored in RNAlater.
- RNA Extraction: Total RNA is extracted using kits such as Qiagen RNeasy Mini Kits, with quality and concentration assessed (e.g., NanoDrop, Bioanalyzer).
- Library Prep & Sequencing: The TAC-seq (Targeted Allele Counting by sequencing) technology is used. This involves:
- Reverse transcription of mRNA into cDNA with molecular barcodes to enable digital counting and reduce amplification bias.
- Pooling and amplification of the barcoded cDNA.
- High-throughput sequencing on platforms like BGISEQ or Illumina.
- Computational Analysis: A pre-trained classifier model analyzes the expression profile of the 72-gene panel (57 receptivity biomarkers, 11 WOI-relevant genes, 4 housekeepers). The model outputs a quantitative prediction, classifying the endometrium as pre-receptive, receptive (including early- and late-receptive sub-states), or post-receptive.
Performance and Validation: In a validation cohort of 57 samples from fertile women, the beREADY model demonstrated an accuracy of 98.2%. It detected a displaced WOI in only 1.8% of these fertile controls, but in a significantly higher proportion (15.9%) of an RIF patient group (p=0.012) [29]. Crucially, the study found no significant difference in the expression of these receptivity biomarkers between healthy women and PCOS patients, suggesting the model's robustness across different patient etiologies [29].
Machine Learning for Prognostic Prediction
Artificial intelligence (AI) is being leveraged to move beyond receptivity status to predict live birth outcomes, directly informing IVF strategy. A recent study compared Machine Learning Center-Specific (MLCS) models against a national registry-based model (SART) across six US fertility centers [53].
The MLCS models, trained on local patient data, significantly improved the minimization of false positives and negatives and more appropriately assigned over 20% of patients to a higher live birth probability (LBP) category compared to the SART model [53]. This demonstrates the power of center-specific personalized modeling to improve prognostic counseling and cost-success transparency.
Emerging Research: Molecular Subtyping and Novel Targets
The application of transcriptomics is moving beyond receptivity dating to define distinct molecular pathologies of implantation failure, enabling truly personalized therapeutic interventions.
Molecular Subtyping of Recurrent Implantation Failure (RIF)
A landmark multi-dataset computational analysis identified two biologically distinct molecular subtypes of RIF rooted in endometrial dysfunction [32]:
- Immune-Driven Subtype (RIF-I): Characterized by enrichment of immune and inflammatory pathways (e.g., IL-17 and TNF signaling) and increased infiltration of effector immune cells.
- Metabolic-Driven Subtype (RIF-M): Marked by dysregulation of oxidative phosphorylation, fatty acid metabolism, and steroid hormone biosynthesis.
This subtyping has direct therapeutic implications. Using the Connectivity Map (CMap) database, researchers predicted sirolimus (an immunomodulator) as a candidate for RIF-I and prostaglandins for RIF-M [32]. A molecular classifier, MetaRIF, was developed to distinguish these subtypes with high accuracy (AUC up to 0.94) [32].
Immune Dysregulation in Thin Endometrium (TE)
Bulk and single-cell RNA sequencing of TE tissues has revealed 57 differentially expressed genes (DEGs) compared to healthy controls [33]. GO enrichment analysis implicated immune activation processes, including leukocyte degranulation and NK cell-mediated cytotoxicity. Significant upregulation of immune-related genes CORO1A, GNLY, and GZMA was validated in TE and associated with cytotoxic immune responses [33]. This provides a new mechanistic understanding of TE, positioning it as a condition of local immune dysregulation and offering potential new biomarker targets.
Table 2: Key Molecular Subtypes of Endometrial Dysfunction in Infertility
| Condition | Molecular Subtype | Defining Transcriptomic Features | Potential Targeted Intervention |
|---|---|---|---|
| Recurrent Implantation Failure (RIF) [32] | RIF-I (Immune-Driven) | ↑ IL-17/TNF signaling, ↑ effector immune cell infiltration | Sirolimus (Immunomodulation) |
| RIF-M (Metabolic-Driven) | Dysregulated oxidative phosphorylation, fatty acid metabolism, altered PER1 clock gene | Prostaglandins | |
| Thin Endometrium (TE) [33] | Immune-Associated Phenotype | ↑ CORO1A, GNLY, GZMA; ↑ NK cell cytotoxicity, leukocyte degranulation | Therapies to modulate local immune response |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Reagent Solutions for Endometrial Transcriptomic Research
| Reagent / Technology | Function in Research | Example Application in Literature |
|---|---|---|
| TAC-seq (Targeted Allele Counting by sequencing) [29] | Enables highly quantitative, digital counting of transcript molecules; reduces amplification bias. | Core technology for the beREADY endometrial receptivity test. |
| Qiagen RNeasy Mini Kits [32] [33] | Isolation of high-quality total RNA from endometrial biopsy tissue. | Used for RNA extraction in multiple transcriptomic studies. |
| DESeq2 R Package [33] | Statistical analysis for determining differentially expressed genes from RNA-seq data. | Used to identify DEGs in thin endometrium and other conditions. |
| Seurat R Package [33] | A comprehensive toolkit for single-cell RNA-seq data analysis, including normalization, clustering, and visualization. | Applied for analyzing cellular heterogeneity in endometrial tissues. |
| ConsensusClusterPlus R Package [32] | Implements consensus clustering for unsupervised class discovery; robustly identifies molecular subtypes. | Used to define RIF-I and RIF-M subtypes in RIF patients. |
| Connectivity Map (CMap) Database [32] | A repository of gene expression profiles from cell lines treated with bioactive small molecules; enables drug repurposing. | Used to predict sirolimus and prostaglandins as subtype-specific therapies for RIF. |
| Sannamycin G | Sannamycin G, CAS:73522-72-2, MF:C14H30N4O4, MW:318.41 g/mol | Chemical Reagent |
| Sarothralin G | Sarothralin G|CAS 130756-15-9|Antibacterial Compound | Sarothralin G is a potent antibacterial compound isolated fromHypericum japonicum. For Research Use Only. Not for human use. |
Personalized hormone screening platforms represent the vanguard of a new era in reproductive medicine. By defining the individual's endometrial response to hormonal signals at the transcriptomic level, these platforms transform IVF from a sequential, trial-and-error process into a targeted, precise intervention. The integration of machine learning for outcome prediction and the emergence of molecular subtyping for conditions like RIF and TE provide a robust foundation for developing novel, mechanism-based therapies.
The future of this field lies in the deeper integration of multi-omics data—including genetics, transcriptomics, and proteomics—to build even more comprehensive models of endometrial receptivity. Furthermore, validating subtype-specific therapies in clinical trials will be the critical next step in fulfilling the promise of personalized hormone screening to significantly improve live birth rates and reduce the physical and emotional burden of infertility.
Genetic Tool Development for Patient-Specific Therapy Selection
The paradigm of therapeutic development is shifting from a one-size-fits-all approach to highly individualized strategies. This is particularly relevant in the context of hormonal control of endometrial gene expression, where conditions like polycystic ovary syndrome (PCOS) and endometrial cancer (EC) exhibit significant patient-to-patient heterogeneity [9] [54]. Precision medicine utilizes population-wide data to categorize diseases and select treatments, whereas personalized medicine tailors interventions based on data from a single individual [55]. For researchers and drug development professionals, this entails leveraging advanced genetic tools—from single-cell omics to genome editing—to decipher complex endometrial pathophysiology and create patient-specific therapy selection frameworks. The ultimate goal is to move beyond symptomatic management and address the root molecular causes of disease, which often involve intricate interactions between hormonal signaling, metabolic disturbance, and genetic susceptibility [9] [56].
Core Technologies Enabling Patient-Specific Therapies
Genomic and Transcriptomic Profiling Tools
The foundation of patient-specific therapy selection rests on comprehensively characterizing the molecular landscape of a patient's disease. High-throughput genomic technologies are indispensable for this purpose.
- Single-Cell RNA Sequencing (scRNA-seq) and Single-Nuclei RNA Sequencing (snRNA-seq): These technologies resolve cellular heterogeneity within tissues by providing gene expression data for individual cells. A recent landmark study applied snRNA-seq to 247,791 endometrial nuclei from control and PCOS patients, revealing cell-type-specific disease signatures in epithelial subpopulations (e.g., SOX9+LGR5+ cells) and alterations in cellular composition that were previously obscured in bulk tissue analyses [54]. This level of resolution is critical for identifying rare cell populations driving disease pathology.
- Spatial Transcriptomics: This technique complements scRNA/snRNA-seq by preserving the spatial context of gene expression within a tissue section. It validated the location of specific epithelial and stromal subpopulations and their transcriptomic changes in the PCOS endometrium, linking molecular signatures to tissue microarchitecture [54].
- Genome-Wide CRISPR Screening: This powerful functional genomics tool uses a library of guide RNAs (gRNAs) to systematically knock out genes in a population of cells, which is then subjected to a selective pressure (e.g., drug treatment). Genes whose knockout confers a survival advantage are identified via next-generation sequencing of the resulting gRNAs. A genome-wide CRISPR screen in Ishikawa EC cells treated with medroxyprogesterone acetate (MPA) identified ADCK3 as a novel key regulator of progesterone response, a finding that would have been difficult to uncover through hypothesis-driven research alone [56].
Genome Editing and Targeted Therapeutic Modalities
Once key targets are identified, a suite of targeted genetic tools can be deployed to develop therapies.
- CRISPR-Cas9 Genome Editing: The CRISPR-Cas9 system can be programmed to induce DNA double-strand breaks at specific genomic loci, leading to gene knockout via frameshift mutations or enabling precise gene correction [56]. Its application is expanding from a research tool to a therapeutic platform.
- Individualized Genetic Therapies: This category includes antisense oligonucleotides (ASOs), siRNA, and mRNA therapies designed to target a genetic variant unique to a small number of individuals, sometimes just a single patient [57]. These modalities can modulate gene expression without permanently altering the DNA sequence.
Table 1: Key Genetic Technologies for Therapy Development
| Technology | Primary Function | Key Application in Endometrial Research |
|---|---|---|
| snRNA-seq | Cell-type-specific transcriptomic profiling | Identifying distinct epithelial stromal signatures in PCOS endometrium [54] |
| Spatial Transcriptomics | Gene expression analysis within tissue context | Validating spatial localization of disease-specific cell clusters [54] |
| Genome-Wide CRISPR Screening | Unbiased discovery of genes involved in a phenotype | Identifying ADCK3 as a regulator of progesterone response in EC [56] |
| ASOs/siRNA | Transient, targeted gene expression modulation | Developing N-of-1 therapies for ultra-rare mutations [57] |
Experimental Workflows and Protocols
Workflow for Single-Cell Endometrial Atlas Construction
Creating a cellular atlas of diseased endometrium is a critical first step in identifying therapeutic targets. The following workflow, derived from a recent study, details the process [54]:
- Patient Selection & Biopsy: Recruit cohorts (e.g., PCOS vs. controls), matched for factors like age and BMI. Obtain superficial endometrial biopsies during a specific menstrual phase (e.g., proliferative phase, days 6–8).
- Nuclei Isolation: Mechanically and enzymatically dissociate the tissue to release individual nuclei. Isolate nuclei using density gradient centrifugation.
- snRNA-seq Library Preparation & Sequencing: Use a platform (e.g., 10x Genomics) to barcode and capture nuclei. Prepare sequencing libraries following the manufacturer's protocol. Sequence the libraries on an appropriate platform (e.g., Illumina).
- Bioinformatic Analysis:
- Quality Control: Filter out low-quality nuclei based on metrics like unique molecular identifier (UMI) counts, number of genes detected, and mitochondrial gene percentage.
- Clustering and Cell Type Annotation: Perform dimensionality reduction (e.g., PCA, UMAP). Cluster cells based on gene expression patterns and annotate cell types using known markers (e.g., EPCAM for epithelial cells, IGF1 for stromal cells).
- Differential Expression Analysis: Compare gene expression between conditions (e.g., PCOS vs. control) within each cell type or subcluster to identify disease-specific signatures.
- Integration with Spatial Data: Overlay snRNA-seq findings onto spatial transcriptomics data to validate the anatomical location of identified cell states and signatures.
- Intervention and Re-sampling: In a sub-cohort, administer an intervention (e.g., 16-week metformin therapy or lifestyle management). Obtain a second biopsy and repeat the snRNA-seq workflow to assess transcriptomic recovery or changes.
Protocol for Genome-Wide CRISPR Knockout Screening
This protocol is used to discover genes that modulate response to a therapy, such as progesterone in endometrial carcinoma [56].
- Library Amplification and Lentivirus Production:
- Transform a high-complexity genome-wide CRISPR library (e.g., the Brunello library) into competent E. coli to amplify the plasmid DNA.
- In a biosafety level 2 facility, produce lentivirus by transfecting HEK293T cells with the library plasmid and packaging plasmids (e.g., pMD2.G, psPAX2) using a transfection reagent. Harvest the viral supernatant at 48 and 72 hours post-transfection.
- Cell Line Infection and Selection:
- Culture the target cell line (e.g., Ishikawa EC cells). Perform a test infection to determine the viral titer and multiplicity of infection (MOI).
- Infect a large number of cells (e.g., 2 × 10^7) at a low MOI (e.g., 0.3) to ensure most cells receive a single viral integrant. After 48 hours, select transduced cells with puromycin for 2 days.
- Selection Pressure and gDNA Isolation:
- Split the selected cells and treat one group with the therapeutic agent of interest (e.g., 40 µM MPA) and maintain another group as an untreated control. Culture for a predetermined period (e.g., 4 days treatment + 10 days recovery).
- Harvest cells from both treated and control groups. Isolate genomic DNA (gDNA) using a commercial maxi kit.
- gRNA Amplification and Sequencing:
- Amplify the integrated gRNA sequences from the gDNA via PCR using primers that add sequencing adapters.
- Purify the PCR products and sequence them on a high-throughput platform (e.g., Illumina NovaSeq).
- Bioinformatic Analysis:
- Align sequenced reads to the library reference to count the abundance of each gRNA in treated and control samples.
- Use specialized algorithms (e.g., MAGeCK) to identify gRNAs that are significantly enriched or depleted in the treated group compared to the control, indicating genes that confer resistance or sensitivity to the therapy.
Signaling Pathways and Molecular Mechanisms
The p53-ADCK3-ALOX15 Axis in Progesterone Sensitization
A genome-wide CRISPR screen identified ADCK3 as a critical regulator of progesterone sensitivity in endometrial cancer cells [56]. The molecular pathway linking p53 activation to ferroptosis sensitization can be summarized as follows:
- p53 Activation: The small molecule Nutlin-3A inhibits MDM2, leading to the stabilization and activation of the tumor suppressor p53.
- Transcriptional Upregulation of ADCK3: Activated p53 binds to the promoter region of the ADCK3 gene, directly increasing its transcription.
- ALOX15 Activation and Ferroptosis: ADCK3, an atypical mitochondrial kinase, is required for the transcriptional upregulation of arachidonate 15-lipoxygenase (ALOX15). ALOX15 is a key enzyme in the oxidation of polyunsaturated fatty acids, leading to lipid peroxidation.
- Synergistic Cell Death: Treatment with MPA alone can induce cell death. However, when combined with Nutlin-3A, the potentiated p53-ADCK3-ALOX15 axis drives a robust ferroptotic cell death program, thereby sensitizing EC cells to progesterone therapy.
Endometrial Dysfunction in PCOS: A Convergent Pathway Model
PCOS endometrial dysfunction arises from the synergistic interplay of several core pathophysiological components, which create a deleterious molecular microenvironment [9].
- Hyperinsulinemia & Insulin Resistance: This disrupts key signaling pathways like PI3K/AKT and MAPK, and interacts with Wnt/β-catenin signaling, leading to altered cellular metabolism and growth.
- Chronic Low-Grade Inflammation: Upregulated inflammatory cytokines (e.g., TNF-α, IL-6, IL-8) interfere with normal estrogen, progesterone, and insulin receptor signaling.
- Sex Steroid Hormone Imbalance: Hyperandrogenism, along with estrogen/progesterone imbalance (e.g., unopposed estrogen, progesterone resistance), causes aberrant expression of key regulators like CYP19A1, COX-2/PGE2, and HOXA10.
- Molecular Consequences: The convergence of these disturbances leads to widespread epigenetic alterations, transcriptomic rewiring, and metabolomic shifts. This results in clinical manifestations such as abnormal uterine bleeding, impaired decidualization, subfertility, and an increased risk of endometrial cancer.
Table 2: Molecular Alterations in PCOS Endometrium and Potential Therapeutic Targets
| Pathophysiological Component | Key Molecular Alterations | Associated Clinical Manifestations | Potential Targeted Therapies |
|---|---|---|---|
| Insulin Resistance & Hyperinsulinemia | Altered PI3K/AKT/MAPK & Wnt/β-catenin signaling [9] | Menstrual irregularity, metabolic dysfunction | Metformin, PI3K/AKT pathway inhibitors |
| Chronic Low-Grade Inflammation | ↑ TNF-α, IL-6, IL-8, IL-18; disrupted hormone receptor signaling [9] | Implantation failure, miscarriage | Anti-cytokine therapies (e.g., anti-IL-6R) |
| Hyperandrogenism & Hormone Imbalance | ↓ ESR1 in epithelial subpopulations; ↑ PAEP, NEAT1 [54] | Impaired decidualization, reduced receptivity | Androgen receptor blockers, PR modulators |
| Altered Cell Composition | ↑ Epithelial cell proportion; ↓ Stromal/Lymphoid cells [54] | Altered endometrial function, cancer risk | Integrin inhibitors (identified via snRNA-seq) [54] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Genetic Tool Development and Analysis
| Reagent / Material | Function / Application | Example & Context |
|---|---|---|
| Brunello CRISPR Knockout Library | Genome-wide pooled gRNA library for loss-of-function screens | Used to identify ADCK3 as a mediator of MPA response in Ishikawa cells [56] |
| 10x Genomics Single-Cell Platform | Integrated system for generating barcoded scRNA-seq/snRNA-seq libraries | Used to profile 247,791 endometrial nuclei from PCOS and control patients [54] |
| Lentiviral Packaging Plasmids (psPAX2, pMD2.G) | Essential plasmids for producing third-generation lentivirus | Used for delivery of CRISPR libraries or individual gRNA constructs [56] |
| Medroxyprogesterone Acetate (MPA) | Synthetic progestin; selective pressure in CRISPR screen | Used to identify genes conferring progesterone resistance in EC [56] |
| Metformin | Insulin-sensitizing drug; intervention in PCOS studies | Partially restored PCOS-specific endometrial transcriptomic signatures post-treatment [54] |
| Nutlin-3A | Small-molecule MDM2 inhibitor; activates p53 pathway | Synergized with MPA to inhibit EC growth via p53-ADCK3 axis [56] |
| Antibodies for Cell Type Markers | Validation of cell identities via protein expression (IHC/WB) | EPCAM (epithelium), IGF1 (stroma) for annotating snRNA-seq clusters [54] |
| Ferroptosis Inhibitors (Liproxstatin-1, Ferrostatin-1) | Small molecules that inhibit ferroptosis; mechanistic validation | Used to confirm ADCK3 knockout confers resistance via suppressed ferroptosis [56] |
| SB-284851-BT | SB-284851-BT Inhibitor | SB-284851-BT is a potent small molecule inhibitor for research. It is For Research Use Only, not for diagnostic or therapeutic applications. |
Overcoming Heterogeneity: Technical Challenges and Pathological Disruptions
Addressing Menstrual Cycle Bias in Biomarker Discovery
Biomarker discovery in endometrial research is critically influenced by the dynamic physiological changes of the menstrual cycle. Failure to account for these cyclical variations introduces significant bias, compromising the validity and reproducibility of research findings. This technical guide examines the sources and impacts of menstrual cycle bias within the context of hormonal control of endometrial gene expression and provides rigorous methodological frameworks for its mitigation. By integrating precise phase verification methods, advanced normalization techniques, and appropriate statistical approaches, researchers can enhance the accuracy of biomarker identification and advance the development of diagnostics and therapeutics for women's health conditions.
The human endometrium undergoes profound molecular and cellular transformations across the menstrual cycle in response to fluctuating estrogen and progesterone levels. These regulated changes essential for reproductive function simultaneously present a substantial challenge for biomarker discovery, as cyclic variation can be misattributed to pathological states or treatment effects [58] [59]. Sex and gender biases have historically favored male participants in medical research, resulting in insufficient attention to female-specific physiological processes like the menstrual cycle [60]. This neglect has contributed to a health gap affecting diverse populations of women and perpetuated the underdiagnosis and misunderstanding of women's health conditions [60].
The endometrial cycle is traditionally divided into three main phases: menstrual, proliferative, and secretory, with the latter two further subdivided into early, mid, and late stages [58]. Each phase exhibits distinct transcriptional networks regulated by complex epigenetic mechanisms including DNA methylation, histone modifications, and non-coding RNAs [58]. During the proliferative phase, estrogen-driven expression of genes like ESR1 and IGF-1 promotes endometrial growth and regeneration [58]. Following ovulation, the secretory phase is characterized by progesterone-dominated signaling that activates genes necessary for decidualization and implantation, such as PGR, IHH, and HOXA10 [58] [59]. This cyclic transcriptional program results in significant expression variation for thousands of genes, creating substantial potential for confounding in study designs that fail to account for cycle phase [59].
Methodological Foundations: Accurate Cycle Phase Determination
The Pitfalls of Assumption and Estimation
A critical review of current practices reveals that many studies rely on assumed or estimated menstrual cycle phases based solely on calendar counting or participant self-report [61]. This approach constitutes a significant methodological flaw with potentially far-reaching consequences for research validity. Calendar-based methods typically define the pre-menstrual phase as "just prior to the onset of menstruation" and menstruation as a "clear-cut point" [61]. However, these assumptions fail to account for the substantial inter-individual variability in hormonal profiles and the high prevalence of subtle menstrual disturbances in reproductive-age women, including anovulatory and luteal phase deficient cycles [61].
Table 1: Limitations of Assumed versus Measured Cycle Phase Determination
| Aspect | Assumed/Estimated Phase | Directly Measured Phase |
|---|---|---|
| Ovulation Detection | Presumed based on cycle day | Confirmed via LH surge testing |
| Hormonal Validation | None | Progesterone measurement confirms luteal phase |
| Cycle Disturbance Detection | Undetectable | Identifies anovulatory/luteal deficient cycles |
| Phase Boundary Precision | Low (calendar-based) | High (hormone-based) |
| Data Validity | Questionable | Scientifically rigorous |
The distinction between eumenorrheic cycles (confirmed hormonal profiles with ovulation and adequate luteal phase) and naturally menstruating women (regular cycle length without hormonal confirmation) is crucial for appropriate participant characterization in research settings [61]. Research indicates that when cycles are assessed solely based on regular menstruation, subtle menstrual disturbances affecting up to 66% of exercising females may remain undetected despite presenting meaningfully different hormonal profiles [61].
Recommended Phase Verification Protocols
Direct hormonal measurements provide the definitive method for menstrual cycle phase determination in research contexts. The following protocols represent minimum standards for rigorous biomarker studies:
Ovulation Confirmation: Detect the luteinizing hormone (LH) surge in urine using commercially available ovulation predictor kits. The onset of the LH surge provides a precise reference point for identifying the peri-ovulatory period [61] [62].
Luteal Phase Verification: Measure serum or salivary progesterone levels during the mid-luteal phase (approximately 7 days post-ovulation). Progesterone concentrations ≥10 nmol/L in serum or corresponding salivary levels provide biochemical evidence of ovulation and adequate luteal function [61].
Cycle Phase Classification: Combine hormonal data with cycle tracking to define specific phases:
- Early Proliferative: Days 1-6 of cycle (following menstruation onset)
- Late Proliferative: Days 7-14 (pre-ovulation, rising estrogen)
- Ovulatory: 2 days before to 3 days after detected LH surge [62]
- Early Luteal: Days 1-5 post-ovulation
- Mid-Luteal: Days 6-10 post-ovulation (peak progesterone)
- Late Luteal: Days 11-14 post-ovulation (declining progesterone)
These direct measurement approaches eliminate guesswork and establish a biochemical foundation for accurate phase classification, significantly reducing a major source of bias in endometrial biomarker research.
Advanced Methodologies for Bias Mitigation
Normalization Strategies for Cyclic Variation
The substantial transcriptional changes across the menstrual cycle necessitate specialized normalization approaches in genomic studies. For RNA-seq experiments comparing expression profiles between cycle phases or conditions, standard normalization methods that assume consistent expression patterns are inadequate. The Scale Based Normalization (SCBN) method offers a robust solution by leveraging conserved orthologous genes and a hypothesis testing framework to determine optimal scaling factors [63].
The SCBN method operates on the principle of identifying a scaling factor that minimizes the deviation between empirical and nominal type I errors when testing for differential expression. The algorithm:
- Identifies conserved orthologous genes or stable reference genes
- Models read counts using a Poisson distribution with parameters accounting for gene length and sequencing depth
- Tests the hypothesis (H0: \lambda{gk1} = \frac{L{gk1}}{L{gk2}} \frac{N1}{N2} c \lambda{gk2}) for each gene (gk)
- Iteratively determines the scaling factor (c) that minimizes false positive rates
This approach specifically addresses the challenges of different gene lengths, unmapped genes, and varying sequencing depths between samples—critical considerations when comparing endometrial samples across menstrual cycle phases [63].
Machine Learning Approaches for Phase Classification
Wearable sensor technology combined with machine learning algorithms offers promising approaches for continuous, non-invasive cycle phase monitoring. Recent studies demonstrate that physiological signals including skin temperature, electrodermal activity (EDA), interbeat interval (IBI), and heart rate (HR) can accurately classify menstrual phases [62].
Table 2: Performance of Machine Learning Models in Menstrual Phase Classification
| Model Type | Number of Phases | Accuracy | AUC-ROC | Data Collection Method |
|---|---|---|---|---|
| Random Forest | 3 (Period, Ovulation, Luteal) | 87% | 0.96 | Wrist-worn device |
| Random Forest | 4 (Period, Follicular, Ovulation, Luteal) | 68% | 0.77 | Wrist-worn device |
| Hidden Markov Model | Ovulation Detection | 76.92% | N/A | In-ear temperature sensor |
| Radial Basis Function | 3 (Follicular, Ovulation, Luteal) | 95% | N/A | ECG/HRV features |
The optimal random forest model utilizing a fixed window technique and leave-last-cycle-out validation achieved 87% accuracy in three-phase classification, demonstrating the feasibility of automated phase tracking through multimodal physiological monitoring [62]. These approaches can significantly reduce participant burden while providing objective, continuous cycle phase data.
Innovative Biospecimen Collection Methods
Menstrual effluent (period blood) represents a novel, non-invasive biospecimen source for endometrial biomarker discovery. Traditionally dismissed as clinical waste, menstrual blood contains a unique mixture of endometrial tissue, circulating blood, and vaginal fluid that reflects the uterine microenvironment [64]. Several startups and research programs are now leveraging this biospecimen for diagnostic purposes:
NextGen Jane collects menstrual blood using specialized tampons that participants mail to a central laboratory for analysis of DNA, RNA, and proteins, with a focus on developing non-invasive diagnostics for endometriosis [64].
The Rose Project utilizes menstrual cups to collect intact cells for morphological analysis, identifying differences in cell quantity and shape in individuals with endometriosis versus controls [64].
Qvin has received FDA approval for a specialized menstrual pad that collects blood for HbA1c monitoring in diabetics, validating the utility of menstrual blood for systemic biomarker detection [64].
These collection methods enable repeated sampling at minimal cost and discomfort, facilitating longitudinal studies of endometrial biology without the need for invasive biopsy procedures.
Experimental Design and Statistical Considerations
Statistical Methods for Differential Expression Analysis
Identifying truly differentially expressed genes amid natural cyclic variation requires specialized statistical approaches. The t-test remains a fundamental method for comparing two conditions when replicated samples are available, but several modifications have been developed to address the challenges of genomic data [65]:
Regularized t-test: Combines gene-specific variance estimates with global average variance using a weighted average as the denominator, implemented in the Cyber T package [65].
Significance Analysis of Microarrays (SAM): Adds a small positive constant to the denominator of the gene-specific t-test, preventing genes with small fold changes but low variability from being selected as significant [65].
B statistic: A log posterior odds ratio of differential expression versus non-differential expression that allows for gene-specific variances while combining information across genes for greater stability [65].
The volcano plot provides an effective visualization tool, displaying the negative log10-transformed p-values from statistical tests against the log2 fold change. This allows simultaneous assessment of both statistical significance and magnitude of effect, helping researchers identify biologically meaningful changes amid cyclic variation [65].
Addressing Multiple Testing in Cyclic Data
The large number of hypotheses tested in genomic studies creates substantial risk of false positives without appropriate correction. Family-wise error rate (FWER) control methods, such as the Bonferroni correction, provide stringent protection against false discoveries but may be overly conservative for exploratory biomarker discovery [65]. As an alternative, false discovery rate (FDR) control methods like the Benjamini-Hochberg procedure offer a more balanced approach by limiting the proportion of false positives among significant results rather than guaranteeing no false positives [65].
For menstrual cycle studies, permutation-based approaches that shuffle cycle phase labels can generate empirical null distributions for hypothesis testing. These methods require sufficient replication—a minimum of about six replicates per condition is recommended to yield 924 distinct permutations for a two-sample comparison [65].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Menstrual Cycle Biomarker Studies
| Reagent/Technology | Primary Function | Application Notes |
|---|---|---|
| Urinary LH Detection Kits | Confirm ovulation timing | Identify LH surge for precise phase determination |
| Progesterone ELISA Kits | Verify luteal phase function | Serum/saliva measurements 7 days post-ovulation |
| RNA Stabilization Reagents | Preserve transcriptomic profiles | Critical for accurate gene expression studies |
| OvuSense/Vaginal Sensors | Continuous core temperature monitoring | 99% accuracy for ovulation detection [62] |
| E4/EmbracePlus Wristbands | Physiological signal acquisition | Capture HR, EDA, temperature, IBI for phase classification |
| Specialized Menstrual Collection | Non-invasive endometrial sampling | Tampons, cups, pads for menstrual effluent analysis |
| Single-Cell RNA-seq Kits | Cell-type specific expression profiling | Resolve distinct endometrial cell type responses |
Signaling Pathways and Experimental Workflows
Hormonal Regulation of Endometrial Gene Expression
Hormonal Regulation Pathway
The diagram illustrates the core pathway of hormonal control in the endometrium. During the proliferative phase, estrogen binds to estrogen receptor alpha (ESR1), driving epithelial proliferation and inducing expression of the progesterone receptor (PGR) [58] [59]. Following ovulation, progesterone binding to PGR promotes stromal differentiation and establishes endometrial receptivity through target genes including IHH, HOXA10, and FOXO1 [58] [59].
Comprehensive Experimental Workflow
Experimental Workflow for Cycle-Aware Biomarker Discovery
This workflow outlines a comprehensive approach for menstrual cycle-aware biomarker discovery. The process begins with carefully defined phase-specific research questions, followed by participant recruitment with strict inclusion criteria. The critical phase verification step employs direct hormonal measurements rather than calendar estimates. Multi-modal data collection incorporates transcriptomic, epigenomic, and physiological data from appropriate biospecimens. Analysis utilizes cycle-specific normalization methods and appropriate statistical corrections, with final validation in independent cohorts.
Addressing menstrual cycle bias requires a fundamental shift from assumption-based to measurement-based research methodologies. By implementing direct hormonal verification, employing appropriate normalization strategies, and leveraging emerging technologies like wearable sensors and menstrual blood analysis, researchers can significantly reduce cyclic confounding in biomarker studies. These rigorous approaches will accelerate the development of accurate diagnostics and effective therapeutics for endometriosis, endometrial cancer, infertility, and other women's health conditions that have historically suffered from research neglect. As the field advances, integration of single-cell technologies, multi-omics approaches, and machine learning algorithms will further refine our understanding of cyclic endometrial biology and its implications for health and disease.
Recurrent implantation failure (RIF) presents a significant challenge in assisted reproductive technology (ART), defined as the failure to achieve clinical pregnancy after multiple transfers of high-quality embryos. While initial research focused predominantly on embryonic factors, emerging evidence confirms that endometrial dysfunction constitutes a major contributor to RIF pathogenesis. The endometrium undergoes precise molecular transformations under hormonal control to achieve receptivity during the window of implantation (WOI). Disruptions in these carefully orchestrated gene expression patterns can lead to implantation failure despite the transfer of morphologically normal embryos.
Recent transcriptomic advances have revealed that RIF is not a monolithic condition but represents a heterogeneous disorder with distinct molecular subtypes. This review examines the emerging paradigm of RIF classification based on endometrial gene expression profiles, focusing specifically on immune and metabolic dysregulation as primary drivers of implantation failure. Understanding these subtypes provides a foundation for developing personalized diagnostic and therapeutic approaches that move beyond empirical treatments.
Molecular Landscape of Endometrial Receptivity
The human endometrium undergoes dynamic changes throughout the menstrual cycle under the influence of estrogen and progesterone. These hormonal fluctuations trigger complex gene expression networks that regulate endometrial maturation. During the window of implantation, the endometrium transitions to a receptive state characterized by specific molecular signatures essential for embryo attachment and invasion.
Transcriptomic studies have identified numerous genes and pathways critical for receptivity. A recent study developing the beREADY endometrial receptivity test analyzed 68 endometrial receptivity genes and found that 15.9% of RIF patients exhibited displaced WOI compared to only 1.8% of fertile women [29]. This molecular dyssynchrony represents one mechanism contributing to implantation failure. Beyond temporal displacement, fundamental pathological processes in the endometrium can be categorized into distinct molecular subtypes.
Table 1: Endometrial Receptivity Analysis in RIF Populations
| Study Group | Sample Size | Displaced WOI Rate | Pre-receptive | Post-receptive |
|---|---|---|---|---|
| RIF Patients | 44 | 15.9% | 6.8% | 9.1% |
| Fertile Women | 57 | 1.8% | 1.8% | 0% |
Molecular Subtyping of RIF: Immune vs Metabolic Dysregulation
Identification of Distinct Molecular Subtypes
Comprehensive computational analysis integrating publicly available endometrial transcriptomic datasets with prospectively collected samples has revealed two biologically distinct RIF subtypes. Using unsupervised clustering of endometrial tissue samples from RIF patients, researchers identified two reproducible subtypes: an immune-driven subtype (RIF-I) and a metabolic-driven subtype (RIF-M) [32] [66].
The analysis identified 1,776 robust differentially expressed genes (DEGs) between RIF and normal endometrial samples. Consensus clustering demonstrated that these DEGs consistently segregated into two distinct patterns across multiple validation cohorts. The RIF-I subtype showed enrichment in immune and inflammatory pathways, while the RIF-M subtype exhibited dysregulation in metabolic pathways [32].
Immune-Driven Subtype (RIF-I)
The RIF-I subtype is characterized by predominant dysregulation of immune responses and inflammatory pathways. Gene Set Enrichment Analysis (GSEA) revealed significant enrichment for IL-17 signaling, TNF signaling, and other pro-inflammatory pathways (p < 0.01) [32]. Immunohistochemical analysis demonstrated an increased T-bet/GATA3 expression ratio in RIF-I endometrium, indicating a shift toward Th1-type immune responses [32].
The RIF-I endometrium displays increased infiltration of effector immune cells, including uNK cells, macrophages, and T cells. These immune alterations create a hostile endometrial environment that impairs embryo implantation and trophoblast invasion. Single-cell RNA sequencing studies have further confirmed immune dysregulation in RIF, with altered proportions and function of various immune cell populations in the endometrial microenvironment [33] [67].
Metabolic-Driven Subtype (RIF-M)
The RIF-M subtype primarily exhibits disturbances in cellular metabolic processes. Pathway analysis revealed prominent dysregulation of oxidative phosphorylation, fatty acid metabolism, and steroid hormone biosynthesis [32]. Additionally, RIF-M endometrium showed altered expression of the circadian clock gene PER1, suggesting disruption of metabolic rhythms that may contribute to impaired receptivity.
The metabolic alterations in RIF-M likely affect energy production and cellular homeostasis in the endometrium, creating a suboptimal environment for embryo implantation. These findings highlight the importance of metabolic homeostasis for successful implantation, independent of immune function.
Table 2: Characteristics of RIF Molecular Subtypes
| Feature | RIF-I (Immune-Driven) | RIF-M (Metabolic-Driven) |
|---|---|---|
| Key Pathways | IL-17 signaling, TNF signaling, immune cell activation | Oxidative phosphorylation, fatty acid metabolism, steroid hormone biosynthesis |
| Characteristic Genes | Increased T-bet, inflammatory cytokines | Altered PER1, metabolic enzymes |
| Immune Profile | Increased effector immune cell infiltration | Minimal immune dysregulation |
| T-bet/GATA3 Ratio | Higher | Lower |
| Proposed Therapeutics | Sirolimus | Prostaglandins |
Experimental Methodologies for Subtype Identification
Sample Collection and Processing
Endometrial biopsy specimens should be collected during the mid-secretory phase (5-8 days after the luteinizing hormone peak) with precise cycle dating confirmed by histological evaluation using Noyes' criteria [32]. Participants must meet strict inclusion criteria: age between 18-38 years, BMI 18-25 kg/m², regular menstrual cycles (25-35 days), and absence of hormonal treatments for at least three months prior to biopsy.
Exclusion criteria include intrauterine pathologies, hydrosalpinx, polycystic ovary syndrome, endometriosis, adenomyosis, abnormal chromosomal karyotypes, antiphospholipid antibodies, active infections, endocrine disorders, and current use of hormonal contraception [32]. Tissue samples should be immediately frozen and stored at -80°C for RNA extraction.
Transcriptomic Analysis Pipeline
RNA Extraction and Library Preparation: Total RNA is isolated using Qiagen RNeasy Mini Kits following manufacturer's protocol. Transcriptome libraries are prepared using massively parallel single-cell RNA-seq methods (MARS-seq) [32]. For targeted approaches, the TAC-seq technology enables precise quantification of transcript abundances down to single-molecule resolution [29].
Data Integration and Normalization: Multi-platform data harmonization is performed using random-effects models to account for batch effects. The "sva" R package is recommended for correcting batch effects introduced by different datasets [68]. Normalization should be performed using FPKM and TPM metrics for cross-study comparisons.
Differential Expression Analysis: Differentially expressed genes between RIF and control samples are identified using MetaDE or DESeq2 with thresholds of adjusted p-value (FDR) < 0.05 and fold change > 1.5 [32] [33]. For subtype identification, unsupervised clustering is performed using ConsensusClusterPlus with Euclidean distance and Ward's linkage [32].
Pathway Analysis: Gene Set Enrichment Analysis (GSEA) is conducted to identify enriched biological pathways in each subtype. Single-gene GSEA can further elucidate the biological processes associated with specific diagnostic genes [68].
Validation Methods
Immunohistochemistry: Protein-level validation of subtype-associated genes is performed using IHC. For RIF subtyping, evaluation of T-bet and GATA3 expression provides confirmation of immune status [32].
Machine Learning Classification: The MetaRIF classifier was developed using the optimal F-score from 64 combinations of machine learning algorithms. This classifier accurately distinguishes subtypes in independent validation cohorts (AUC: 0.94 and 0.85) [32].
Single-Cell RNA Sequencing: Integration with publicly available scRNA-seq data enables validation at cellular resolution and identification of cell-type-specific expression patterns [33].
Experimental Workflow for RIF Molecular Subtyping
Diagnostic Biomarkers and Clinical Applications
Molecular Classifier Development
The MetaRIF classifier represents a significant advance in RIF diagnostics, outperforming previously published models with an AUC of 0.88 compared to 0.48-0.72 for other signatures [32]. This classifier enables stratification of RIF patients into immune and metabolic subtypes, facilitating personalized treatment approaches.
Beyond the MetaRIF classifier, research has identified specific diagnostic genes shared between RIF and related conditions like endometriosis. The EHF gene has been validated as a diagnostic biomarker with excellent accuracy for both conditions, highlighting shared pathological processes [68].
Immune Dysregulation Signatures
Comprehensive immune profiling reveals distinct alterations in RIF patients. These include dysregulation of both innate and adaptive immunity, with altered Th1/Th2 ratios, increased uNK cell numbers and cytotoxicity, and changes in macrophage polarization [67] [69]. Additionally, altered antibody production, including anti-phospholipid and anti-sperm antibodies, may contribute to implantation failure in some RIF patients [67].
In thin endometrium, a condition associated with RIF, immune-related gene signatures show upregulation of CORO1A, GNLY, and GZMA—genes functionally related to cytotoxic immune responses [33]. This suggests shared immune mechanisms across different endometrial pathologies associated with implantation failure.
Table 3: Immune Cell Alterations in RIF Endometrium
| Immune Cell Type | Alteration in RIF | Functional Consequences |
|---|---|---|
| uNK Cells | Increased number and cytotoxicity | Impaired trophoblast invasion, excessive inflammation |
| Macrophages | Altered polarization | Dysregulated tissue remodeling and vascular adaptation |
| T Cells | Th1/Th2 imbalance, Treg deficiency | Disrupted immune tolerance, inflammation |
| B Cells | Autoantibody production | Anti-embryonic immune responses |
Therapeutic Implications and Personalized Approaches
Subtype-Specific Treatment Strategies
The identification of molecular subtypes enables targeted therapeutic interventions based on underlying pathophysiology. Connectivity Map (CMap) analysis has predicted sirolimus (rapamycin) as a candidate treatment for RIF-I, targeting immune dysregulation, while prostaglandins may benefit RIF-M patients by addressing metabolic deficiencies [32].
Current immunomodulatory treatments for RIF include intravenous immunoglobulin (IVIG), tacrolimus, glucocorticoids, and granulocyte colony-stimulating factor (G-CSF) [70] [67]. However, recent multicenter randomized trials have challenged the efficacy of some interventions, particularly glucocorticoids, which did not improve live birth rates in RIF patients [70]. This underscores the importance of patient stratification—these treatments may benefit only the immune-dysregulated subset.
Hormonal Modulation of Endometrial Receptivity
Within the context of hormonal control of endometrial gene expression, therapeutic approaches can target the hormonal pathways that regulate implantation. Progesterone, in particular, plays a crucial role in modulating immune responses during the implantation window. The metabolic RIF-M subtype, with its dysregulated steroid hormone biosynthesis, may benefit from personalized hormonal supplementation protocols tailored to restore metabolic homeostasis.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for RIF Molecular Subtyping
| Reagent/Technology | Application | Specific Function |
|---|---|---|
| Qiagen RNeasy Mini Kits | RNA extraction | Isolation of high-quality total RNA from endometrial tissue |
| TAC-seq (Targeted Allele Counting) | Transcript quantification | Precise measurement of endometrial receptivity biomarkers at single-molecule resolution |
| ConsensusClusterPlus | Bioinformatics | Unsupervised clustering to identify molecular subtypes |
| MetaDE | Statistical analysis | Identification of differentially expressed genes across multiple datasets |
| Connectivity Map (CMap) | Drug discovery | Prediction of candidate therapeutic compounds based on gene expression signatures |
| CIBERSORT | Immune profiling | Deconvolution of immune cell populations from bulk RNA-seq data |
The classification of RIF into immune and metabolic subtypes represents a paradigm shift in understanding implantation failure. This framework acknowledges the biological heterogeneity of RIF and provides a roadmap for developing personalized diagnostic and therapeutic strategies. The development of validated molecular classifiers like MetaRIF represents a critical step toward clinical implementation of this subtyping approach.
Future research should focus on refining subtype definitions through integrated multi-omics approaches, including proteomic and metabolomic profiling. Additionally, longitudinal studies tracking subtype stability across cycles and large-scale clinical trials validating subtype-specific treatments are essential. Ultimately, these advances will enable true personalization of infertility treatment, moving beyond empirical approaches to target the specific molecular pathophysiology underlying each patient's implantation failure.
Hormonal Control to Personalized Treatment Pathway
PCOS-Associated Endometrial Dysfunction and Therapeutic Interventions
Polycystic ovary syndrome (PCOS) is the most common endocrine disorder affecting 11-13% of reproductive-aged women, creating an economic burden of approximately US$8 billion in 2020 [54] [71]. While traditionally recognized for its ovarian manifestations, research now establishes that PCOS significantly impacts endometrial function, contributing to subfertility, increased miscarriage rates, and elevated risk of endometrial cancer [54] [71]. This whitepaper examines the molecular mechanisms underlying PCOS-associated endometrial dysfunction within the broader context of hormonal control of endometrial gene expression, providing researchers and drug development professionals with current experimental approaches, quantitative findings, and promising therapeutic directions.
The endometrial dysfunction in PCOS manifests through multiple interconnected pathways including aberrant sex steroid hormone signaling, insulin resistance, chronic inflammation, and altered immune cell populations [9]. Recent single-cell transcriptomic analyses have revealed previously unappreciated cellular heterogeneity and cell-type-specific disease signatures in the PCOS endometrium [54]. Understanding these mechanisms is essential for developing targeted interventions that address the root causes of endometrial dysfunction rather than merely managing symptoms.
Molecular Mechanisms of Endometrial Dysfunction
Altered Cellular Composition and Gene Expression
Advanced single-nuclei RNA sequencing of 247,791 endometrial nuclei has demonstrated significant differences in cellular composition between PCOS and healthy endometria [54]. PCOS endometrium shows a higher proportion of epithelial cells and fewer stromal and lymphoid cells, indicating fundamental changes in tissue architecture that may impact function [54] [71].
Table 1: Endometrial Cellular Composition Changes in PCOS
| Cell Type | Change in PCOS | Functional Implications |
|---|---|---|
| Epithelial cells | Increased proportion | Disrupted endometrial growth patterns |
| Stromal cells | Decreased proportion | Impaired decidualization potential |
| Lymphoid cells | Decreased proportion | Altered immune environment |
| SOX9+ LGR5+ epithelial progenitors | Altered gene expression | Disrupted tissue regeneration |
Epithelial subpopulations in PCOS endometrium exhibit significant transcriptomic alterations, with the most differentially expressed genes observed in SOX9+LGR5+ (n=138), SOX9+ cycling (n=174), AR+ (n=257), and ciliated (n=259) subclusters [54]. Key changes include downregulation of SEMA3E (implicated in angiogenesis) and upregulation of PAEP (linked to recurrent pregnancy loss) and NEAT1 (associated with endometrial cancer and inflammation) [54].
Hormonal Signaling Disruption
PCOS endometrium exhibits profound dysregulation of hormonal signaling pathways, creating an environment hostile to embryo implantation and maintenance. Estrogen receptor-α (ESR1) is significantly downregulated in AR+, SOX9+LGR5+, and SOX9+ cycling epithelial subpopulations, while androgen receptor expression remains elevated [54]. This hormonal imbalance creates a state of "progesterone resistance" that impairs decidualization – the critical transformation of endometrial stromal cells necessary for successful embryo implantation [9].
The Wnt/β-catenin signaling pathway, crucial for endometrial proliferation and differentiation, is also disrupted in PCOS [9]. This pathway interacts with both insulin and androgen signaling, creating a complex network of dysregulation that contributes to endometrial dysfunction. Hyperandrogenism directly impacts endometrial gene expression through transcription factors such as Wilms tumor-1 (WT1), which regulates genes involved in cell development and survival [9].
Hormonal and Metabolic Disruption Pathways in PCOS Endometrium
Immune Dysregulation and Chronic Inflammation
Endometrial immune balance is critically disrupted in PCOS, with significant alterations in T-cell populations and inflammatory markers. Flow cytometry analyses reveal that Th1 cells decrease while Th2 cells increase significantly in PCOS endometrium, creating an imbalanced immune environment [72]. This Th1/Th2 imbalance may contribute to the increased miscarriage rates observed in women with PCOS.
Chronic low-grade inflammation is a hallmark of PCOS endometrium, characterized by upregulated inflammatory cytokines including IL-1, 2, 6, 8, 17, 18, and TNF-α [9]. Endometrial epithelial organoids (EEOs) derived from PCOS patients maintain this inflammatory signature in vitro, showing increased expression of genes such as Oncostatin M Receptor (OSMR) and Intercellular Adhesion Molecule 1 (ICAM1) [73]. This pro-inflammatory environment likely contributes to the impaired endometrial receptivity and increased risk of pregnancy complications.
Experimental Models and Methodologies
Single-Cell RNA Sequencing Approaches
The creation of a cellular atlas of PCOS endometrium requires sophisticated single-cell methodologies. The following workflow represents the experimental approach used in recent groundbreaking research [54]:
Single-Nuclei RNA Sequencing Workflow for PCOS Endometrium
This methodology enabled the analysis of 247,791 nuclei from 27 endometrial biopsies (5 controls, 12 PCOS cases at baseline, 7 after metformin treatment, and 3 after lifestyle intervention) [54]. Samples were processed using the 10x Genomics protocol, with stringent quality control applied before identification of seven main cell clusters based on established markers [54].
Endometrial Epithelial Organoid Models
The establishment of PCOS-derived endometrial epithelial organoids (EEOs) represents a significant advance for studying endometrial dysfunction [73]. These 3D models closely mimic in vivo pathophysiology and maintain disease-specific traits through multiple passages.
Table 2: Endometrial Epithelial Organoid Culture Protocol
| Step | Description | Key Components | Duration |
|---|---|---|---|
| Tissue collection | Endometrial biopsies from PCOS and controls | Proliferative phase sampling | N/A |
| Organoid establishment | Embedding in Matrigel with growth factors | EGF, Noggin, R-spondin, Wnt3a | 7-14 days |
| Hormonal exposure | Simulation of menstrual cycle phases | β-estradiol, progesterone, cAMP | 6 days |
| Androgen testing | Hyperandrogenism simulation | Dihydrotestosterone (DHT) | 6 days |
| Analysis | Transcriptomic and morphological assessment | RNA-seq, RT-qPCR, H&E staining | Varies |
PCOS EEOs demonstrate increased inflammation-related gene expression and reduced diameter compared to controls [73]. Overweight/obese PCOS EEOs show aberrant response to steroid exposure with reduced expression of receptivity-related genes (PAEP and LIF), providing insights into the molecular basis of endometrial dysfunction in different PCOS phenotypes [73].
Research Reagent Solutions
Table 3: Essential Research Reagents for PCOS Endometrial Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Antibodies for flow cytometry | CD4, CD8, Th1, Th2, Th17, Treg markers | Immune cell profiling [72] |
| Cell culture supplements | β-estradiol, progesterone, cAMP, DHT | Hormonal response assays [73] |
| Extracellular matrix | Matrigel | 3D organoid culture [73] |
| Sequencing reagents | 10x Genomics kits | Single-cell RNA sequencing [54] |
| Metabolic drugs | Metformin | Intervention studies [54] [71] |
Clinical Outcomes and Quantitative Data
Pregnancy and Perinatal Complications
Large-scale clinical studies demonstrate significantly worse reproductive outcomes in women with PCOS. A retrospective cohort study of 21,074 frozen embryo transfer (FET) cycles found markedly increased risks across multiple pregnancy complication categories [72]:
Table 4: Pregnancy and Perinatal Outcomes in PCOS vs Non-PCOS Patients
| Outcome Measure | PCOS Incidence | Non-PCOS Incidence | Significance |
|---|---|---|---|
| Miscarriage | Significantly increased | Reference | p<0.05 |
| Hypertensive disorders of pregnancy | Significantly increased | Reference | p<0.05 |
| Preterm birth | Significantly increased | Reference | p<0.05 |
| Fetal malformations | Significantly increased | Reference | p<0.05 |
These adverse outcomes were particularly pronounced in PCOS women with the hyperandrogenic phenotype, highlighting the importance of accounting for phenotypic heterogeneity in both research and clinical management [72].
Endometrial Receptivity Assessment
Targeted gene expression profiling of 68 endometrial receptivity genes revealed no significant differences between healthy women and PCOS patients when comparing the expression patterns of established receptivity biomarkers [29]. This suggests that the fundamental timing of the window of implantation may remain intact in PCOS, with dysfunction arising from other mechanisms such as inflammatory milieu or impaired decidualization.
However, in recurrent implantation failure (RIF) patients, molecular subtyping has identified distinct endometrial phenotypes including an immune-driven subtype (RIF-I) characterized by enriched IL-17 and TNF signaling pathways, and a metabolic-driven subtype (RIF-M) showing dysregulation of oxidative phosphorylation and fatty acid metabolism [32]. These subtypes may have relevance for PCOS-associated infertility and represent targets for personalized therapeutic approaches.
Therapeutic Interventions and Future Directions
Current Intervention Strategies
Despite strong biological rationales for multiple interventions, a systematic review identified that no specific strategy can currently be recommended for improving endometrial receptivity in PCOS patients based on robust clinical evidence [74]. The review identified 24 potential interventions but found limited confirmation from randomized controlled trials for any approach [74].
Metformin treatment for 16 weeks demonstrates promising effects in restoring endometrial health, with single-cell analyses showing extensive recovery of disease-specific gene expression signatures [54] [71]. Metformin administration normalizes gene expression in specific cell types, particularly epithelial and stromal cells, and reduces hyperandrogenism and insulin resistance [54]. Lifestyle interventions also show beneficial effects, though generally less pronounced than metformin [54].
Emerging Therapeutic Targets
Advanced transcriptomic analyses have identified potential therapeutic targets for PCOS-associated endometrial dysfunction. Integrin inhibitors represent promising candidates based on their role in cell adhesion and communication pathways disrupted in PCOS [54]. Similarly, the identification of an immune-driven endometrial subtype in RIF patients suggests potential application of immunomodulatory approaches such as sirolimus for selected PCOS patients [32].
The establishment of PCOS endometrial organoid models enables high-throughput screening of potential therapeutics in a system that maintains patient-specific disease characteristics [73]. These models allow for testing of candidate compounds targeting specific pathways identified in omics studies, potentially accelerating drug development for PCOS endometrial dysfunction.
PCOS-associated endometrial dysfunction arises from complex interactions between hormonal imbalances, metabolic disturbances, and inflammatory processes that disrupt normal endometrial gene expression and function. Recent advances in single-cell technologies and organoid models have provided unprecedented insights into the cellular and molecular basis of this dysfunction, revealing altered cellular composition, cell-type-specific gene expression signatures, and profound immune dysregulation.
While current evidence supports the potential of metformin and lifestyle interventions for restoring endometrial health in PCOS, more research is needed to develop targeted therapies addressing the specific molecular pathways identified in recent studies. The integration of multi-omics data, advanced experimental models, and clinical outcomes will enable researchers and drug development professionals to create more effective, personalized approaches for managing PCOS-associated endometrial dysfunction and improving reproductive outcomes for affected women.
Controlled Ovarian Stimulation Effects on Endometrial Receptivity Signatures
Controlled ovarian stimulation (COS), a cornerstone of assisted reproductive technology (ART), induces profound hormonal alterations that significantly impact endometrial receptivity. This whitepaper synthesizes current research on the molecular signatures of endometrial receptivity under COS regimens, framing the discussion within the broader context of hormonal control of endometrial gene expression. Evidence from transcriptomic, proteomic, and functional studies demonstrates that COS disrupts the delicate hormonal orchestration required for the window of implantation (WOI), leading to altered expression of key receptivity markers, displacement of the WOI, and compromised pregnancy outcomes. Understanding these mechanisms is critical for developing personalized approaches to endometrial preparation and improving ART success rates for researchers and drug development professionals.
Endometrial receptivity refers to a transient, well-defined period during the mid-secretory phase of the menstrual cycle when the endometrium acquires a functional status capable of supporting blastocyst implantation. This "window of implantation" (WOI) is characterized by a precise sequence of molecular and cellular events directed by the coordinated actions of estrogen and progesterone. Controlled ovarian stimulation (COS), essential for obtaining multiple oocytes in ART, introduces supraphysiologic steroid hormone levels that disrupt this delicate endocrine balance. A growing body of evidence indicates that the high estrogen and progesterone concentrations achieved during COS significantly alter the endometrial molecular landscape, leading to deferred or impaired receptivity that persists even at the time of embryo transfer. This whitepaper examines the specific effects of COS on endometrial receptivity signatures, exploring the underlying gene expression changes, disrupted biological pathways, and clinical implications within the framework of hormonal control of endometrial gene expression research.
Molecular Signature Alterations in COS Cycles
Transcriptomic Profiling Evidence
Comprehensive gene expression analyses reveal significant discrepancies between endometrial receptivity development in natural versus COS cycles.
Table 1: Key Transcriptomic Alterations in COS vs. Natural Cycles
| Transcriptomic Feature | Natural Cycle Profile | COS Cycle Profile | Functional Consequence |
|---|---|---|---|
| Global Gene Expression | Normal transition from pre-receptive to receptive phase [75] | Heterogeneous disruption; two distinct profiles identified: moderately altered (majority) and strongly altered (subgroup) [75] | Desynchronization of endometrial maturation |
| WOI Timing | Consistent timing relative to LH surge [76] | Displacement observed in 26-47% of RIF patients [76] [29] | Embryo-endometrium asynchrony |
| Specific Pathway Disruption | Intact TGFβ signaling, leukocyte transendothelial migration, and cell cycle pathways [75] | Defective activation of TGFβ signaling, leukocyte transendothelial migration, and cell cycle functions [75] | Impaired implantation signaling and immune dialogue |
| Cellular Senescence Marker | Normal p16 expression in young women with NOR [77] | Significantly elevated p16 expression in young women with DOR (P < 0.001) [77] | Premature endometrial aging |
Key Receptor and Marker Expression Dysregulation
Beyond transcriptomic shifts, COS significantly impacts the expression of specific endometrial receptivity biomarkers critical for embryo attachment and invasion:
- Integrin αvβ3 and Osteopontin: The integral combination of integrin αvβ3 with its ligand osteopontin serves as a key molecular marker of endometrial receptivity crucial for embryo implantation. Dysregulation of this system disrupts hormonal regulation and cytokine expression [78].
- HOXA10: This essential transcription factor regulates endometrial receptivity and embryo implantation by affecting integrin αvβ3 expression. HOXA10 imbalance under COS conditions can significantly impair implantation capacity [78].
- Leukemia Inhibitory Factor (LIF): A critical cytokine for implantation, LIF expression is significantly downregulated in high-androgen environments associated with PCOS patients undergoing COS. Experimental studies confirm that high testosterone doses directly suppress LIF expression in endometrial cells [79].
- Insulin-like Growth Factor Binding Protein 1 (IGFBP-1): This important implantation marker also shows significantly reduced expression in endometrial tissue from COS cycles with high androgen levels, further compromising receptivity [79].
Experimental Protocols for Assessing COS Impact
Comparative Endometrial Transcriptomic Profiling
Objective: To comprehensively analyze the global gene expression profile of human endometrial biopsies during the early-secretory and mid-secretory phases of natural and stimulated cycles in the same patients [75].
Patient Selection:
- Include 21 normal-responder patients (age 30.9 ± 3.3 years) with male infertility factor
- Exclude patients with endometriosis, uterine abnormalities, hydrosalpinx, or endometrial pathologies
- Obtain written informed consent and IRB approval
Sample Collection:
- During a natural cycle: Collect two endometrial biopsies at day 2 (LH+2) and day 7 (LH+7) after the LH peak
- During a subsequent COS cycle: Collect two biopsies at day 2 (hCG+2) and day 5 (hCG+5) after hCG administration
- Total: 84 endometrial samples (4 per patient)
- Immediately freeze samples at -80°C in RLT RNA extraction buffer
RNA Processing and Microarray Hybridization:
- Extract total RNA using micro RNeasy Kit
- Assess RNA quantity with Nanodrop ND-1000 spectrophotometer and integrity with Agilent 2100 Bioanalyzer
- Prepare labeled complementary RNA (cRNA) with two rounds of amplification from 100 ng total RNA
- Hybridize fragmented cRNA (12 μg) to Affymetrix HG-U133 Plus 2.0 arrays
- Process scanned GeneChip images using Affymetrix GCOS 1.4 software with MAS5.0 algorithm
Data Analysis:
- Use Significant Analysis of Microarrays (SAM) to identify genes with significant expression variations
- Perform unsupervised classification with principal component analysis (PCA) and hierarchical clustering
- Analyze selected gene lists (mean fold change > 2 and FDR < 5%) with Ingenuity Pathway Analysis and FatiGO+ software
- Identify altered biological pathways and networks
Targeted Gene Expression Profiling for WOI Detection
Objective: To apply a targeted sequencing approach for accurate endometrial receptivity testing and detection of WOI displacement in COS cycles [29].
TAC-seq (Targeted Allele Counting by Sequencing) Workflow:
- Panel Design: Develop a targeted gene panel covering 57 endometrial receptivity biomarkers, 11 additional WOI-relevant genes, and 4 housekeeper genes (72 total genes)
- Library Preparation: Use TAC-seq technology for biomolecule analysis down to single-molecule level
- Sequencing: Perform high-coverage sequencing on Illumina platform
- Computational Analysis: Apply beREADY classification model to sequence data
- Sample Classification: Categorize endometrium as pre-receptive, early-receptive, receptive, late-receptive, or post-receptive based on expression profiles
Validation:
- Validate classification accuracy using endometrial samples from healthy volunteers (26 ESE, 26 MSE, and 5 LSE phase samples)
- Apply to RIF patient population to detect WOI displacement prevalence
Signaling Pathways and Molecular Mechanisms
The molecular dialogue between the embryo and endometrium during the WOI involves complex signaling pathways that are significantly disrupted by COS protocols. The supraphysiologic hormone levels alter the expression of key receptors, cytokines, and growth factors, creating a suboptimal environment for implantation.
Hormonal Regulation and Receptor Signaling
COS induces profound changes in the hormonal milieu, with elevated estrogen levels in the early stimulation phase followed by rapidly increasing progesterone levels after ovulation trigger. This altered steroid environment directly impacts endometrial gene expression through nuclear estrogen and progesterone receptors. Research demonstrates that COS cycles are associated with:
- Premature progesterone receptor downregulation that disrupts the normal sequence of endometrial maturation [75]
- Altered estrogen receptor expression patterns that affect endometrial response to rising estrogen levels [50]
- Dysregulation of HOXA10 expression, a critical transcription factor that regulates multiple implantation-related genes [78]
These receptor-level changes create a cascade effect on downstream signaling pathways essential for receptivity.
Growth Factor and Cytokine Pathways
The impaired receptivity observed in COS cycles involves significant alterations in critical growth factor and cytokine pathways:
- TGF-β Signaling Pathway: Transcriptomic analyses consistently identify disrupted TGF-β signaling as a key feature of COS-altered endometrium. This pathway is essential for endometrial stromal cell decidualization and proper embryo-endometrial cross-talk [75].
- LIF Signaling: Leukemia inhibitory factor (LIF), a pleiotropic cytokine essential for implantation, shows significantly reduced expression in endometrial tissue from COS cycles, particularly in hyperandrogenic environments such as PCOS [79].
- IGF System: Insulin-like growth factor binding protein 1 (IGFBP-1), a major product of decidualized endometrial stromal cells, is downregulated in COS cycles with high androgen levels, compromising the endometrial response to embryonic signals [79].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Endometrial Receptivity Studies
| Research Tool | Specific Product Examples | Research Application |
|---|---|---|
| Endometrial Biopsy Collection | Pipelle de Cornier, Tao Brush | Obtain endometrial tissue samples for molecular analysis with minimal patient discomfort |
| RNA Stabilization Buffer | RLT Buffer (Qiagen) | Preserve RNA integrity immediately after tissue collection during multi-center studies |
| RNA Extraction Kits | RNeasy Micro Kit (Qiagen) | Isolve high-quality RNA from limited endometrial tissue samples |
| RNA Quality Assessment | Agilent 2100 Bioanalyzer | Evaluate RNA integrity number (RIN) to ensure sample quality before transcriptomic analysis |
| Microarray Platforms | Affymetrix HG-U133 Plus 2.0 Arrays | Comprehensive gene expression profiling with 54,675 probe sets |
| Targeted Sequencing | TAC-seq Custom Panels | Highly quantitative analysis of specific endometrial receptivity biomarker genes |
| Cell Culture Models | Ishikawa Cell Line | Study hormonal regulation of receptivity markers in vitro |
| Pathway Analysis Software | Ingenuity Pathway Analysis (IPA) | Identify biologically relevant networks and pathways from gene expression data |
| Immunohistochemistry Reagents | p16INK4a antibodies | Detect cellular senescence markers in endometrial tissue sections |
Clinical Implications and Future Directions
The molecular evidence demonstrating COS-induced alterations in endometrial receptivity signatures has significant clinical implications for ART practice. The recognition that COS creates a suboptimal endometrial environment has driven the widespread adoption of "freeze-all" strategies with subsequent frozen-thawed embryo transfer (FET) in natural or artificially prepared cycles. This approach allows the endometrium to recover from the supraphysiologic hormone levels of COS before embryo transfer.
Emerging strategies to overcome COS-induced receptivity issues include:
- Personalized Embryo Transfer (pET): Endometrial receptivity array (ERA) and similar transcriptomic-based tests identify the displaced WOI in approximately 25% of RIF patients, enabling personalized transfer timing that improves pregnancy rates from 65% with standard timing [76].
- Natural Cycle FET: Utilizing natural cycles for FET avoids further hormonal manipulation, potentially creating a more physiologic receptivity environment [75].
- Adjuvant Therapies: Platelet-rich plasma (PRP) containing growth factors shows promise for improving endometrial thickness and receptivity in patients with thin endometrium or recurrent implantation failure [80].
- Modulated COS Protocols: Developing milder stimulation protocols with reduced gonadotropin doses may minimize the detrimental effects on endometrial receptivity while maintaining adequate oocyte yield.
Future research directions should focus on developing less intrusive ovarian stimulation protocols, identifying predictive biomarkers for COS-induced receptivity compromise, and creating targeted interventions to restore normal molecular signatures in the endometrium after stimulation.
Controlled ovarian stimulation induces significant alterations in the molecular signatures of endometrial receptivity through multiple mechanisms, including transcriptomic profile disruptions, WOI displacement, and dysregulation of key receptivity markers. These changes are mediated by the supraphysiologic steroid hormone environment created by COS, which disrupts the normal hormonal control of endometrial gene expression. The comprehensive analysis of these effects through multi-omics approaches provides valuable insights for researchers and drug development professionals seeking to optimize ART outcomes. Future innovations in ovarian stimulation and endometrial preparation should prioritize the preservation of normal receptivity signatures alongside optimal oocyte yield, moving toward truly personalized approaches in reproductive medicine.
Computational Correction Methods for Cycle Phase Confounding
The dynamic nature of the human endometrium, driven by hormonal fluctuations across the menstrual cycle, presents a significant challenge for transcriptomic and other omics studies. The extensive molecular changes that occur can confound attempts to identify genuine biomarkers for endometrial disorders or receptivity. This technical guide outlines the sources of this confounding and details computational methods to correct for it, thereby enhancing the robustness and reproducibility of research into the hormonal control of endometrial gene expression.
The Challenge of Cycle Phase Confounding
The endometrium undergoes cyclical processes of repair, proliferation, differentiation, and shedding in response to circulating levels of estradiol (E2) and progesterone (P4) [81] [82]. This dynamism is reflected in widespread changes in gene expression. In fact, menstrual cycle timing is often the dominant source of variation in endometrial gene expression data, frequently captured in the first principal component in Principal Component Analysis (PCA) [82]. Failure to account for this major source of variation reduces statistical power and can introduce spurious signals, leading to poor reproducibility and a proliferation of false-positive biomarkers in case-control studies [82]. Systematic reviews have highlighted a concerning lack of consensus among studies investigating conditions like endometriosis and recurrent implantation failure (RIF), with very few overlapping differentially expressed genes identified across multiple studies [82].
Computational Correction Methodologies
Accurate Menstrual Cycle Dating and Phase Definition
The foundation of any correction method is the accurate temporal characterization of the endometrial sample.
- Traditional Histological Dating: The established method, based on the Noyes criteria, is subjective and lacks the precision required for high-resolution omics studies [82].
- Molecular Dating: A more robust approach involves using molecular profiles to estimate the temporal position of a sample within the cycle. This can be achieved by building a reference model of gene expression changes across a finely timed cycle and then projecting new samples onto this model to infer their "molecular time" [82].
Table 1: Key Hormonal and Molecular Changes Across the Menstrual Cycle Phases
| Phase | Approximate Cycle Days (28-day cycle) | Hormonal Profile | Key Molecular/Transcriptomic Features |
|---|---|---|---|
| Early Follicular | Days 1-7 | Low E2, Low P4 [81] | Tissue repair and initiation of proliferation [82]. |
| Late Follicular (Pre-ovulatory) | Days 8-14 | High, peaking E2, Low P4 [81] | Estrogen-driven proliferation and angiogenesis [82]. |
| Early-Mid Secretory (Luteal) | Days 15-23 | Moderate E2, High, peaking P4 [81] | Progesterone-driven differentiation and secretion; preparation for implantation. Rapid, discontinuous transcriptomic activation marks the window of implantation (e.g., PAEP, GPX3, CXCL14) [82]. |
| Late Secretory (Perimenstrual) | Days 24-28 | Rapidly falling E2 and P4 [81] | Tissue breakdown and inflammation triggered by hormone withdrawal [82]. |
Statistical Modeling Approaches to Account for Cycle Effects
Once cycle phase information is accurately determined, it must be incorporated into statistical models to isolate the biological signal of interest (e.g., disease state) from the variation due to the cycle.
- Covariate Adjustment: The most straightforward method is to include cycle phase or a continuous measure of molecular time as a covariate in linear models when performing differential expression analysis. This approach adjusts for the mean expression differences associated with the cycle [82].
- Advanced Regression Frameworks: For more complex study designs, mixed-effects models or generalized additive models (GAMs) can be employed. These are particularly useful for modeling non-linear gene expression changes across the cycle and for handling repeated measures [83].
- Bayesian Integrative Models: Advanced frameworks can integrate gene expression data with clinical variables to improve predictive power. For instance, one study using transcriptomic profiles from uterine fluid extracellular vesicles (UF-EVs) employed a Bayesian logistic regression model that integrated gene co-expression modules with clinical variables (e.g., vesicle size, history of previous miscarriages). This model achieved a high predictive accuracy for pregnancy outcome (AUC = 0.83), demonstrating the power of combining molecular and clinical data while accounting for confounding factors [84].
Leveraging Gene Co-expression Networks
Weighted Gene Co-expression Network Analysis (WGCNA) is a systems biology method used to cluster genes into modules based on highly correlated expression patterns across samples. These modules often correspond to specific biological functions.
- Application to Cycle Confounding: WGCNA can be used to identify a gene module highly correlated with menstrual cycle progression. The "eigengene" of this module (the first principal component of the module's expression matrix) can then be used as a powerful surrogate variable representing the global transcriptional state of the endometrium in relation to the cycle. This eigengene can be included in downstream models to regress out the effect of the cycle [84]. A study on UF-EVs successfully used WGCNA to cluster differentially expressed genes into functionally relevant modules involved in embryo implantation, which were then integrated into the Bayesian predictive model [84].
Detailed Experimental Protocol for a Cycle-Aware Transcriptomic Study
The following workflow provides a step-by-step guide for conducting an endometrial transcriptomic study that robustly accounts for menstrual cycle phase.
Protocol Steps:
Sample Collection & Preparation:
- Patient Cohort Identification: Recruit a well-characterized cohort, clearly defining case and control groups. Record detailed metadata, including age, BMI, and gynecological history [84] [82].
- Precise Cycle Phase Determination: This is critical. Use a combination of methods for highest accuracy:
- First day of last menstrual period: Track cycle length.
- Urinary luteinizing hormone (LH) surge detection: To pinpoint ovulation.
- Serum hormone measurement: Quantify E2 and P4 levels at the time of biopsy.
- Histological dating: Perform according to Noyes criteria.
- Endometrial Tissue Biopsy / Non-Invasive Sampling: Collect endometrial tissue biopsies via pipelle. As a less invasive alternative, collect uterine fluid (UF) for the isolation of extracellular vesicles (UF-EVs), whose transcriptomic profile has been shown to correlate strongly with paired endometrial tissue [84].
- RNA Extraction & Sequencing: Extract total RNA using standardized kits (e.g., Qiagen RNeasy). Assess RNA integrity (RIN > 7). Prepare libraries and sequence on an Illumina platform to a depth of at least 30 million paired-end reads per sample.
Data Preprocessing & Cycle Modeling:
- Raw Read Processing: Align sequencing reads to a reference genome (e.g., GRCh38) using a splice-aware aligner like STAR. Quantify gene-level counts using featureCounts.
- Cycle Phase Covariate Creation: Synthesize the data from step 1 to assign each sample a primary cycle phase or a continuous temporal variable.
- Molecular Time Estimation (Optional): For higher resolution, use a reference dataset to model gene expression as a continuous function of cycle time and project your samples onto this model to infer a "molecular date" [82].
Statistical Analysis & Correction:
- Differential Expression Analysis with Covariate Adjustment: Using a tool like DESeq2 or limma, model the read counts with a design formula that includes the condition of interest (e.g., disease status) and the cycle phase covariate (or molecular time).
- Example model in DESeq2:
~ Batch + Cycle_Phase + Condition
- Example model in DESeq2:
- Gene Co-expression Network Analysis (WGCNA): Perform WGCNA on variance-stabilized expression data to identify modules of co-expressed genes. Identify modules significantly associated with the cycle. Use the module eigengene as a more powerful covariate to correct for cycle effects.
- Functional Enrichment: Perform Gene Set Enrichment Analysis (GSEA) on the ranked list of genes from the corrected differential expression analysis to identify enriched biological processes (e.g., "adaptive immune response," "ion homeostasis") [84].
- Differential Expression Analysis with Covariate Adjustment: Using a tool like DESeq2 or limma, model the read counts with a design formula that includes the condition of interest (e.g., disease status) and the cycle phase covariate (or molecular time).
Validation & Interpretation:
- Independent Validation: Validate key findings in an independent patient cohort.
- Biological Interpretation: Focus on the genes and pathways that remain significant after cycle correction for downstream biological interpretation and candidate biomarker selection.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Computational Tools
| Item | Function/Application | Example/Note |
|---|---|---|
| Pipelle Endometrial Biopsy Catheter | Minimally invasive collection of endometrial tissue samples. | Standard of care for tissue acquisition. |
| RNA Stabilization Reagent (e.g., RNAlater) | Preserves RNA integrity in tissue samples immediately after collection. | Critical for preventing RNA degradation. |
| Total RNA Extraction Kit | Isolation of high-quality RNA from tissue or UF-EV samples. | Qiagen RNeasy Kit; assess RNA Quality (RIN). |
| UF-EV Isolation Reagents | Isolation of extracellular vesicles from uterine fluid aspirates. | Ultracentrifugation or commercial exosome isolation kits. |
| RNA-Sequencing Library Prep Kit | Preparation of sequencing libraries from total RNA. | Illumina TruSeq Stranded mRNA kit. |
| DESeq2 / limma (R/Bioconductor) | Statistical software for differential gene expression analysis. | Allows for inclusion of covariates in the model design. |
| WGCNA (R package) | Construction of weighted gene co-expression networks. | Identifies modules of co-expressed genes related to the cycle. |
| Bayesian Statistical Software (e.g., RStan) | Implementation of advanced Bayesian models for integrative prediction. | Used to combine molecular and clinical data [84]. |
| Urinary LH Test Kits | At-home detection of the LH surge to pinpoint ovulation. | Critical for accurate peri-ovulatory and luteal phase timing. |
The confounding effect of the menstrual cycle is a major, often overlooked, factor undermining reproducibility in endometrial transcriptomics. Moving beyond simple, inaccurate histological dating to incorporate precise cycle phase information—or preferably, molecular timing estimates—into statistical models is no longer optional for rigorous science. By adopting the computational correction methods outlined in this guide, including covariate adjustment, co-expression network analysis, and advanced Bayesian frameworks, researchers can significantly improve the reliability of their findings, accelerate the discovery of genuine biomarkers, and advance our understanding of endometrial biology and pathology.
Genetic Mapping and Clinical Validation: From eQTLs to Targeted Therapies
Endometrial Expression Quantitative Trait Loci (eQTLs) and Genetic Regulation
The endometrium, the inner lining of the uterus, undergoes dynamic, hormone-driven changes throughout the menstrual cycle to support implantation and pregnancy. Understanding the genetic regulation of these processes is fundamental to advancing reproductive medicine. Expression Quantitative Trait Loci (eQTL) mapping has emerged as a powerful technique to elucidate the genetic variants that influence gene expression levels. In the context of the endometrium, eQTL studies provide a crucial link between genetic predisposition and the molecular mechanisms governing endometrial function, offering insights into the pathophysiology of diseases such as endometriosis, endometrial cancer, and infertility [85]. This whitepaper details the core concepts, methodologies, and applications of endometrial eQTL research, framing it within the broader thesis of hormonal control of endometrial gene expression.
Core Concepts and Methodological Framework
Defining eQTLs in the Endometrial Context
An expression Quantitative Trait Locus (eQTL) is a genomic locus that explains a fraction of the genetic variance of a gene expression phenotype. In endometrial research, eQTLs are categorized based on their genomic position relative to the gene they regulate:
- cis-eQTLs: Located close (typically within 1 Mb) to the start site of the target gene. Their effects are often allele-specific and stable across cell types.
- trans-eQTLs: Located far from the target gene, often on a different chromosome. They typically affect multiple genes and can be highly tissue-specific.
- Co-regulatory eQTLs (creQTLs): A specialized class that influences the expression of a coordinated group of genes, often reflecting the action of upstream regulatory molecules like transcription factors or signaling proteins [86].
Hormonal status is a critical confounder in endometrial eQTL studies. The transcriptional landscape of the endometrium shifts dramatically across the menstrual cycle in response to estrogen and progesterone [85]. Therefore, precise documentation of the cycle stage (e.g., proliferative vs. secretory) during tissue sampling is essential for accurate eQTL identification, as an eQTL detectable in one hormonal milieu may not be active in another.
Standard Experimental Workflow and Protocols
A robust endometrial eQTL study follows a structured workflow, from sample collection to data integration. The key procedural steps are outlined below.
Diagram 1: Standard workflow for endometrial eQTL mapping studies.
Protocol 1: Endometrial Tissue Collection and Processing
- Objective: To obtain high-quality endometrial tissue with associated clinical and hormonal metadata.
- Materials: See the "Research Reagent Solutions" table for specific items.
- Procedure:
- Patient Selection & Consent: Recruit participants with documented menstrual cycle regularity and obtain informed consent. Exclude patients with current hormonal treatments, infections, or uterine pathologies unless they are the subject of study.
- Cycle Stage Determination: Record the cycle day and correlate with serum levels of luteinizing hormone (LH), estrogen, and progesterone. The LH surge is designated as day 0. Alternatively, histological dating of the tissue sample according to established criteria can be used.
- Tissue Biopsy: Perform an endometrial biopsy using a disposable pipelle or similar device under sterile conditions.
- Sample Processing:
- Molecular Analysis: Immediately snap-freeze a portion of the tissue in liquid nitrogen and store at -80°C for subsequent RNA and DNA extraction.
- Histology: Place another portion in formalin for paraffin-embedding and histological examination to confirm the cycle stage and absence of pathology.
- Data Annotation: Record all patient metadata, including age, BMI, parity, and precise cycle stage.
Protocol 2: High-Throughput Genotyping and RNA Sequencing
- Objective: To generate genotype and gene expression data from endometrial samples.
- Procedure:
- Nucleic Acid Extraction:
- Extract genomic DNA from frozen tissue or blood samples using a commercial kit. Assess DNA quality and quantity via spectrophotometry and gel electrophoresis.
- Extract total RNA from frozen endometrial tissue using a kit with a DNase digestion step. Assess RNA integrity using an instrument, accepting only samples with high integrity numbers.
- Genotyping: Genotype DNA samples using a high-density SNP microarray. Perform stringent quality control: exclude samples with low call rates, gender mismatches, or outliers in identity-by-state analysis; exclude SNPs with low call rates, significant deviation from Hardy-Weinberg equilibrium, or low minor allele frequency.
- RNA Sequencing:
- Prepare libraries from high-quality total RNA. Use ribosomal RNA depletion to capture both poly-A and non-poly-A transcripts.
- Sequence the libraries on a high-throughput platform to a sufficient depth.
- Process raw sequencing reads: trim adapter sequences and low-quality bases, align cleaned reads to a reference genome, and quantify gene-level counts.
- Nucleic Acid Extraction:
Protocol 3: Computational eQTL Mapping
- Objective: To identify genetic variants associated with variation in gene expression.
- Software: Tools such as
Matrix eQTL,FastQTL, orSMR. - Procedure:
- Data Preprocessing:
- Genotype Data: Impute missing genotypes using a reference panel and convert to dosage format.
- Expression Data: Normalize raw count data to correct for library size and composition bias. Regress out technical covariates and hidden confounders. A common approach is to convert counts to a normal distribution.
- Covariate Selection: Include relevant covariates in the statistical model to increase power. These typically include:
- Genetic principal components to account for population stratification.
- Technical factors.
- Menstrual cycle stage (as a categorical or continuous variable) is a critical biological covariate for endometrial studies [85].
- Association Testing: For each gene-SNP pair, perform a linear regression where the normalized expression of the gene is the dependent variable, and the genotype dosage of the SNP is the independent variable, while adjusting for the selected covariates.
- For cis-eQTL analysis: Test SNPs within a defined window around the transcriptional start site of each gene.
- For trans-eQTL analysis: Test all SNPs against all genes, applying stringent multiple testing correction.
- Significance Thresholding: Correct for multiple hypothesis testing using methods like False Discovery Rate. A standard significance threshold is FDR < 0.05.
- Data Preprocessing:
Data Interpretation and Integration
Key Quantitative Findings from Endometrial eQTL Studies
The following table synthesizes key quantitative findings from published eQTL studies involving human endometrial tissue.
Table 1: Summary of Key Findings from Endometrial eQTL Studies
| Study Focus | Sample Size & Tissue | Key Quantitative Findings | Implications for Hormonal Control |
|---|---|---|---|
| Baseline Endometrial eQTL Mapping [85] | 229 endometrial samples | - 45,923 cis-eQTLs for 417 genes- 2,968 trans-eQTLs affecting 82 genes- 2,427 gene probes showed significant cycle stage effects | Directly demonstrates that mean expression levels of thousands of genes are under hormonal control across the menstrual cycle. |
| Co-regulatory eQTL (creQTL) in Endometrial Cancer [86] | Endometrial cancer study | Identified a creQTL upstream of STARD13 that co-regulates a group of 7 IFNβ-induced genes. | Suggests a genetic mechanism regulating signaling pathways (Rho-GTPase) that can be modulated by hormonal and inflammatory cues. |
| Integration with Endometriosis GWAS [87] | eQTLs from GTEx (Uterus, Ovary, etc.) | Endometriosis-risk variants were enriched for eQTLs in uterus and ovary, regulating genes like MICB, CLDN23, and GATA4. | Links genetic risk to tissue-specific dysregulation, potentially affecting hormonal response pathways and tissue remodeling. |
| Multi-omic SMR for Endometriosis [88] | SMR integrating eQTL, mQTL, pQTL, and GWAS | Identified 18 eQTL-associated genes and 7 pQTL-associated proteins with causal evidence for endometriosis. Highlights MAP3K5 and THRB. | Provides causal evidence for how genetic variation influences gene expression and protein abundance, interacting with the hormonal environment. |
Integration with Genome-Wide Association Studies (GWAS)
A primary application of eQTL data is to annotate the findings from GWAS. Many disease-associated variants from GWAS lie in non-coding regions, suggesting they likely influence disease risk by regulating gene expression rather than altering protein structure.
Colocalization analysis is a statistical method used to determine if the same genetic variant is responsible for both the eQTL signal and the GWAS signal. A high posterior probability for colocalization implies a shared causal variant, thereby nominating the eQTL target gene as a strong candidate for the GWAS association [88]. For instance, an endometriosis-risk variant might colocalize with an eQTL for a gene involved in estrogen signaling, providing a mechanistic hypothesis for the genetic association.
Mendelian Randomization (MR) takes this a step further by testing for a causal relationship between the genetically predicted expression of a gene and a disease outcome. In one study, MR was used with eQTLs from The Cancer Genome Atlas (TCGA) to identify causal genes for endometrial carcinoma prognosis, leading to an 8-gene prognostic model [89].
Advanced Multi-Omic Integration and Signaling Pathways
Beyond eQTLs: A Multi-Omic Framework
To fully capture the layers of genetic regulation, endometrial research is moving towards multi-omic integration. This involves combining eQTL data with other QTL types:
- Methylation QTLs (mQTLs): Identify variants that influence DNA methylation levels.
- Protein QTLs (pQTLs): Identify variants that influence the abundance of specific proteins.
The Summary-data-based Mendelian Randomization (SMR) method is frequently used for this integration, as it can test the causal effect of a molecular trait (e.g., gene expression, methylation) on a complex disease [88]. A multi-omic SMR analysis of endometriosis identified 196 CpG sites, 18 eQTL-associated genes, and 7 pQTL-associated proteins, revealing a complex causal network [88]. For example, it suggested that methylation at a specific CpG site downregulates MAP3K5 expression, thereby increasing endometriosis risk.
Key Signaling Pathways Highlighted by eQTL Studies
eQTL and multi-omic studies have highlighted several critical signaling pathways in endometrial physiology and pathology, many of which are directly modulated by steroid hormones.
Table 2: Key Signaling Pathways in Endometrial Biology and Disease
| Signaling Pathway | Core Components | Role in Endometrium | Hormonal & eQTL Linkage |
|---|---|---|---|
| Steroid Hormone Signaling | ESR1, ESR2, PGR | Regulates proliferation, differentiation, and receptivity. Adenomyosis and endometriosis feature estrogen overexpression and progesterone resistance [90]. | eQTLs can regulate the expression of hormone receptors (e.g., ESR1, PGR), modulating the tissue's response to hormonal stimuli [90] [91]. |
| GRB2-Related Signaling | GRB2, EGFR, ERK, AKT | Critical for implantation and decidualization. Loss of GRB2 in mouse models leads to progesterone resistance and infertility [91]. | Downregulation of GRB2 disrupts growth factor signaling, leading to impaired response to progesterone and estrogen, a pathway potentially influenced by genetic variation [91]. |
| Wnt/β-Catenin Signaling | WNT, β-catenin, TCF/LEF | Regulates cell proliferation, survival, and epithelial-mesenchymal transition (EMT). Aberrant activation is found in adenomyosis and endometriosis [90] [92]. | A study found ARG2 promotes adenomyosis by regulating the Wnt/β-catenin pathway, a process that could be under genetic control [90]. |
| TGF-β Signaling | TGF-β, Smads, SNAI, ZEB | A primary driver of EMT and fibrosis in endometriosis, facilitating invasion and lesion establishment [92]. | eQTLs could influence the expression of ligands, receptors, or transcription factors in this pathway, thereby affecting the invasive potential of endometrial cells. |
The following diagram illustrates the GRB2 signaling pathway, a key pathway implicated in endometrial receptivity and whose dysregulation leads to progesterone resistance.
Diagram 2: GRB2-mediated signaling pathway in endometrial receptivity.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Endometrial eQTL Studies
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| Endometrial Biopsy Pipelle | Minimally invasive collection of endometrial tissue. | Standardized sample acquisition for RNA and DNA extraction [85]. |
| RNA Stabilization Reagent | Preserves RNA integrity immediately upon tissue collection. | Prevents degradation of RNA during sample transport and storage, ensuring accurate expression profiling. |
| Ribosomal RNA Depletion Kit | Removes ribosomal RNA prior to RNA-seq, enriching for mRNA and non-coding RNAs. | Provides a more complete view of the transcriptome compared to poly-A selection alone [85]. |
| High-Density SNP Microarray | Genotyping of hundreds of thousands to millions of genetic variants. | Provides the genotype data required for eQTL association testing [89] [85]. |
| STAU1 Antibody & Assays | Detection and validation of a stable reference gene for endometrial studies. | STAU1 was identified as a superior reference gene for studying decidualization, crucial for normalizing RT-qPCR data [93]. |
| Primary Human Endometrial Stromal Cells (ESCs) | In vitro model for studying decidualization and hormone response. | Used to validate the functional impact of genetic variants or gene knockdowns (e.g., GRB2 attenuation) [91]. |
Technical Considerations and Future Directions
Critical Considerations for Endometrial eQTL Studies
- Cell Type Specificity: The endometrium is a complex tissue composed of epithelial, stromal, and immune cells. eQTL signals identified from bulk tissue represent an average across these cell types. Cell-type-specific eQTLs can be masked. Single-cell RNA sequencing combined with genotyping is a promising but costly approach to deconvolute these signals.
- Hormonal Dynamics: As emphasized throughout, the cyclic nature of the endometrium is a major source of expression variation. Future studies with large sample sizes across multiple cycle stages will be needed to discover cycle-stage-interaction eQTLs.
- Reference Gene Validation: For gene expression validation using RT-qPCR, the choice of reference gene is critical. Traditional genes like β-actin can be unstable. Studies have identified STAU1 as a more stable reference gene for endometrial decidualization studies [93].
Endometrial eQTL mapping provides a powerful genetic lens through which to view the hormonal control of gene expression. By identifying the genetic variants that drive transcriptional changes, researchers can move from statistical associations in GWAS to mechanistic understandings of disease etiology. The future of this field lies in the deeper integration of multi-omic data (eQTLs, mQTLs, pQTLs) from well-annotated, large cohorts, analyzed with sophisticated methods like SMR and colocalization. Furthermore, incorporating single-cell analyses and in vitro functional validation in models like primary endometrial stromal cells will be essential to translate genetic discoveries into actionable biological insights and novel therapeutic strategies for endometrial disorders.
Overlap Between Endometrial eQTLs and Disease Risk Loci
The endometrium, a dynamic tissue under precise hormonal control, undergoes extensive gene expression changes across the menstrual cycle. Genetic variants that regulate endometrial gene expression, known as expression quantitative trait loci (eQTLs), provide a mechanistic bridge between inherited risk variants and reproductive disease pathogenesis. This technical review synthesizes current research demonstrating how endometrial eQTLs colocalize with disease risk loci for endometriosis, polycystic ovarian syndrome, and endometrial cancer. We present comprehensive quantitative data, experimental methodologies for identifying these overlaps, and visual frameworks for understanding the functional consequences of genetically regulated transcription in endometrial biology and pathology.
The human endometrium undergoes dramatic molecular and cellular reprogramming throughout the menstrual cycle in response to fluctuating estrogen and progesterone levels. This hormonal regulation directs a complex transcriptional landscape that can be genetically modulated. Expression quantitative trait loci (eQTLs) represent genomic regions containing genetic variants that influence gene expression levels. Endometrial eQTLs demonstrate both shared regulation with other tissues and tissue-specific effects, potentially explaining susceptibility to various reproductive diseases [94]. The integration of eQTL data with genome-wide association studies (GWAS) has emerged as a powerful approach to identify functional genes and mechanisms underlying disease risk loci, moving beyond mere statistical associations to mechanistic understanding [95] [87].
Methodological Framework for Endometrial eQTL Mapping
Sample Collection and Processing
Table 1: Key Specifications for Endometrial eQTL Studies
| Component | Specifications | Notes |
|---|---|---|
| Sample Size | 206-229 individuals | Provides sufficient power for cis-eQTL detection [95] [94] |
| Tissue Source | Endometrial biopsies | Collected across menstrual cycle phases [95] |
| Cycle Staging | Histological confirmation (M, EP, MP, LP, ES, MS, LS) | Critical for controlling for cyclic transcriptional changes [95] [94] |
| RNA Processing | Microarray or RNA-seq | Different platforms require specific normalization approaches [95] [31] |
| Genotyping | Genome-wide SNP arrays | Followed by imputation to increase variant resolution [95] |
eQTL Identification Pipeline
The standard workflow for endometrial eQTL mapping involves several critical steps:
Transcriptome Quantification: Gene expression levels are quantified using microarray [95] or RNA-seq [31] [94] technologies. For RNA-seq data, this includes read alignment, transcript assembly, and expression quantification at gene or transcript level.
Quality Control and Normalization: Rigorous QC removes low-quality samples and normalizes expression data to account for technical covariates and batch effects. Cycle stage must be incorporated as a key covariate [95].
Genotype Processing: Genotype data undergoes imputation to increase marker density, followed by standard QC procedures including Hardy-Weinberg equilibrium, missingness, and relatedness checks.
Expression-genotype Association Testing: For cis-eQTL mapping, each gene is tested against genetic variants within a specified window (typically 1 Mb upstream and downstream of the gene body). The linear model accounts for relevant covariates including genetic principal components to control for population stratification [95] [94].
Multiple Testing Correction: Significant associations are determined using false discovery rate (FDR) control, with typical significance thresholds of FDR < 0.05 [94].
Figure 1: Endometrial eQTL Mapping Workflow. The process integrates genomic and transcriptomic data with critical clinical metadata like menstrual cycle stage.
Colocalization Analysis with GWAS Signals
To establish overlap between endometrial eQTLs and disease risk loci, several statistical approaches are employed:
Colocalization Analysis: Determines whether the same underlying genetic variant influences both gene expression and disease risk using methods such as COLOC or fastENLOC.
Transcriptome-Wide Association Study (TWAS): Predicts genetically regulated expression and tests for association between predicted expression and disease risk [94].
Summary-data-based Mendelian Randomization (SMR): Tests for pleiotropic association between a genetic variant with both expression levels and disease traits [94].
Quantitative Landscape of Endometrial eQTLs
Magnitude and Specificity of Genetic Effects
Table 2: Endometrial eQTL Magnitudes from Key Studies
| eQTL Category | Count | Number of Genes | Significance Threshold | Notes |
|---|---|---|---|---|
| cis-eQTLs | 45,923 | 417 | FDR < 0.05 | Within 1 Mb of gene [95] |
| cis-eQTLs | 444 (sentinel) | 444 | P < 2.57 × 10â»â¹ | Sentinel variants [94] |
| trans-eQTLs | 2,968 | 82 | FDR < 0.05 | Distant regulatory effects [95] |
| trans-eQTLs | 30 | 30 | P < 4.65 × 10â»Â¹Â³ | Highly significant trans effects [94] |
| sQTLs | 3,296 | >2,000 | FDR < 0.05 | Splicing QTLs [31] |
Endometrial eQTLs demonstrate both shared and tissue-specific regulation. Approximately 85% of endometrial eQTLs are shared with other tissues, while 15% may represent endometrium-specific regulatory effects [94]. The genetic control of endometrial gene expression extends beyond steady-state levels to include transcriptional silencing/activation across the menstrual cycle and alternative splicing [95] [31].
Hormonal Influence on Genetic Regulation
The hormonal fluctuations across the menstrual cycle significantly impact genetic regulation of endometrial gene expression:
Cycle Stage Effects: Significant effects of cycle stage on mean expression levels were observed for 2,427/15,262 probes expressed in most samples and 2,877/9,626 probes variably expressed across samples [95].
Dynamic Expression Patterns: The most pronounced transcriptional changes occur between proliferative and early-secretory phases, with 95 genes showing progressive expression changes across all cycle stages [95].
Pathway Enrichment: Genes with cycle-dependent expression are enriched in hallmark pathways including epithelial-mesenchymal transition, estrogen response (early and late), and KRAS signaling [95].
Disease-Relevant Endometrial eQTL Overlaps
Endometriosis
Endometriosis, affecting 6-10% of reproductive-aged women, demonstrates strong genetic links to endometrial eQTLs:
Table 3: Endometrial eQTLs Colocalizing with Endometriosis Risk Loci
| Gene | Chromosome | Function | eQTL Effect | Disease Association |
|---|---|---|---|---|
| LINC00339 | 1 | Long non-coding RNA | Expression-modifying | Endometriosis risk locus [95] |
| VEZT | 12 | Adherens junction protein | Expression-modifying | Endometriosis risk locus [95] |
| GREB1 | 2 | Estrogen-regulated gene | Splicing QTL | Endometriosis risk through splicing [31] |
| WASHC3 | Endosomal trafficking | Splicing QTL | Endometriosis risk through splicing [31] |
The TWAS analysis integrating endometrial eQTLs with endometriosis GWAS data identified significant associations at 39 genomic loci, including five known endometriosis risk regions [94]. Notably, sQTL analysis has revealed additional mechanisms, with the majority of genes with sQTLs (67.5%) not discovered in gene-level eQTL analyses [31].
Polycystic Ovary Syndrome (PCOS)
While fewer specific PCOS-related endometrial eQTLs have been characterized, several lines of evidence suggest overlapping genetic regulation:
Gene expression profiling of endometrial receptivity biomarkers revealed no significant differences between healthy women and PCOS patients, suggesting that PCOS status may not affect expression profiles of key endometrial receptivity genes [29].
Pathway analysis of endometrial eQTLs highlights potential target genes for PCOS, though specific genes require further characterization [95].
Endometrial Cancer
Recent large-scale GWAS meta-analyses have identified multiple risk loci for endometrial cancer, with emerging evidence for eQTL overlaps:
NAV3: A novel risk gene identified at 12q21.2, where downregulation in endometrial cell lines accelerated cell division and wound healing capacity, while overexpression reduced cell survival, suggesting tumor suppressor function [96].
PPARG and BPTF: Additional candidate genes supported by gene-based analyses of endometrial cancer risk loci [96].
Multi-tissue eQTL analysis reveals that endometriosis-associated variants regulate genes involved in hormonal response, tissue remodeling, and adhesion in reproductive tissues [87].
Advanced Analytical Techniques
Multi-tissue Integration Approaches
The integration of endometrial eQTL data with other tissue eQTL resources enables broader insights:
GTEx Project Cross-referencing: Comparing endometrial eQTLs with 42 tissues from the GTEx project reveals tissue-shared and endometrium-specific regulatory effects [87].
Functional Characterization: Endometriosis-associated variants demonstrate tissue-specific regulatory profiles, with immune and epithelial signaling genes predominating in non-reproductive tissues, while reproductive tissues show enrichment for hormonal response and tissue remodeling genes [87].
Beyond Conventional eQTLs: Splicing QTLs
Recent evidence highlights the importance of genetic regulation of RNA splicing in endometrium:
Splicing-Specific Effects: 67.5% of genes with sQTLs were not discovered in gene-level eQTL analysis, indicating splicing-specific genetic effects [31].
Endometriosis Associations: Integration of sQTLs with endometriosis GWAS identified two genes (GREB1 and WASHC3) significantly associated with endometriosis risk through genetically regulated splicing events [31].
Figure 2: From Risk Variant to Disease Mechanism. Integration of GWAS and QTL data bridges statistical associations with biological function.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Endometrial eQTL Studies
| Reagent/Resource | Function | Specifications | Reference |
|---|---|---|---|
| RNAlater | RNA stabilization | Tissue preservation for RNA extraction | [94] |
| iTRAQ Reagents | Quantitative proteomics | Protein quantification and comparison | [97] |
| TAC-seq Technology | Targeted transcriptomics | Sensitive detection of endometrial receptivity biomarkers | [29] |
| GTEx v8 Database | Multi-tissue eQTL reference | Comparison of endometrial with other tissue eQTLs | [87] |
| FUMA Software | Functional mapping | Functional annotation of GWAS and eQTL signals | [95] |
| COLOC/fastENLOC | Colocalization analysis | Statistical test for eQTL-GWAS colocalization | [94] |
The integration of endometrial eQTL maps with disease risk loci has substantially advanced our understanding of the genetic architecture underlying reproductive diseases. The overlap between endometrial eQTLs and risk loci for endometriosis, PCOS, and endometrial cancer provides mechanistic insights that bridge statistical genetic associations with biological function. Future research directions should include:
Larger Sample Sizes: Current studies of 200-300 samples remain underpowered for detecting tissue-specific and context-dependent eQTLs.
Single-cell Resolution: Bulk tissue eQTLs average across cell types; single-cell approaches will reveal cell-type-specific genetic regulation.
Dynamic eQTL Mapping: Characterizing how genetic effects on expression change across menstrual cycle phases and hormonal contexts.
Multi-omic Integration: Combining eQTLs with epigenetic, proteomic, and metabolomic data for comprehensive molecular understanding.
These advances will further elucidate the complex interplay between genetic variation, hormonal regulation, and endometrial function, ultimately informing diagnostic and therapeutic approaches for reproductive diseases.
Validation of Biomarker Panels Across Multiple Patient Cohorts
The validation of biomarker panels across multiple patient cohorts represents a critical step in translating discoveries from basic research into clinically applicable tools. Within the specific field of hormonal control of endometrial gene expression, this process is paramount for understanding endometrial receptivity, infertility, and related pathologies. The inherent biological complexity of the endometrium, a tissue undergoing profound, hormonally regulated changes throughout the menstrual cycle, presents unique challenges for biomarker development [98]. A biomarker signature identified in one cohort of patients may fail to replicate in another due to variations in sample timing, patient demographics, or analytical protocols. This whitepaper provides an in-depth technical guide to the methodologies and statistical considerations essential for robust cross-cohort validation of endometrial biomarker panels, framing them within the context of a dynamic hormonal environment.
The Critical Need for Cross-Cohort Validation in Endometrial Research
The primary challenge in endometrial biomarker discovery is the potent confounding effect of the menstrual cycle. Transcriptomic studies have demonstrated that endometrial gene expression fluctuates significantly across the proliferative, early-secretory, mid-secretory, and late-secretory phases [98] [29]. If not adequately controlled for, these hormonally driven changes can mask the more subtle expression differences associated with a pathological state, leading to both false positives and false negatives.
Evidence indicates that standard practices are often insufficient. A systematic review found that 31.43% of transcriptomic studies on endometrial pathologies did not register the menstrual cycle phase of the collected samples [98]. This oversight has tangible consequences; when the menstrual cycle bias was statistically removed from gene expression data, an average of 44.2% more genes were identified as differentially expressed in uterine disorders [98]. This demonstrates that menstrual cycle progression can obscure true molecular biomarkers, and validation across cohorts requires explicit correction for this major source of variation.
Furthermore, the lack of reproducibility between individual studies highlights the need for rigorous multi-cohort validation. Many reported biomarkers for conditions like endometriosis or recurrent implantation failure (RIF) show poor overlap between studies, often arising from low sample sizes, sample heterogeneity, and undetected confounding variables [98]. Cross-cohort validation is therefore not merely a final check but an integral part of the discovery process, ensuring that identified biomarker panels are generalizable and robust.
Methodological Frameworks for Cohort Harmonization
Before statistical validation can begin, data from multiple cohorts must be made comparable through harmonization. This process addresses differences in platforms, protocols, and sample characteristics.
Pre-Harmonization: Cohort and Sample Standardization
The most reliable foundation for validation is built upon prospective specimen collection from a well-defined target population that directly reflects the intended use of the biomarker [99]. Key considerations include:
- Patient Phenotyping: Detailed metadata is essential. This includes the menstrual cycle phase (confirmed by LH surge or histology), patient age, BMI, infertility diagnosis, and hormonal treatments [98] [29].
- Sample Collection Standardization: Using standardized protocols for tissue biopsy, RNA preservation, and storage across all participating collection sites minimizes pre-analytical variation.
- Randomization and Blinding: To avoid batch effects and bias, specimens from different clinical groups (e.g., case and control) should be randomly assigned to processing batches, sequencing runs, or microarray plates. The personnel generating the biomarker data should be blinded to the clinical outcomes [99].
Technical Harmonization Approaches
When cohorts have been profiled using different technical platforms, statistical harmonization is required.
- Z-score Normalization: This approach standardizes data from different platforms by re-scaling it to a common distribution with a mean of zero and a standard deviation of one. This method has been successfully applied to harmonize cerebrospinal fluid biomarkers and imaging data in Alzheimer's disease research, allowing data from heterogeneous sources to be combined and analyzed as a continuous quantitative trait [100]. The formula for a Z-score is: ( Z = \frac{X - \mu}{\sigma} ), where ( X ) is the raw value, ( \mu ) is the mean of the cohort, and ( \sigma ) is the standard deviation.
- Non-Parametric Imputation: For cognitive data with imperfect variable overlap, a non-parametric imputation approach has proven effective [101]. This method uses observed data patterns to predict missing neuropsychological variables for any individual, allowing for the creation of a complete dataset across cohorts. This approach is particularly useful when dealing with differing neuropsychological test batteries across studies.
- Batch Effect Correction: Linear models, such as those implemented in the
limmaR package, can remove unwanted technical variation (e.g., from different microarray slides) or biological variation (e.g., the menstrual cycle effect) while preserving the variation of interest (e.g., disease status) [98]. TheremoveBatchEffectfunction is a specific tool for this purpose.
Table 1: Comparison of Data Harmonization Methods
| Method | Principle | Best Use Case | Advantages | Limitations |
|---|---|---|---|---|
| Z-score Normalization | Standardizes data to a common scale (mean=0, SD=1) | Combining continuous data from different measurement units or scales | Simple, intuitive, maintains distribution shape | Assumes normal distribution; may not remove non-linear batch effects |
| Non-Parametric Imputation | Predicts missing data based on patterns in observed data | Cohorts with partially overlapping variables or test items | Maximizes use of all available data; handles complex missingness | Computational intensity; requires large, high-quality overlapping data |
| Linear Model Correction | Models and subtracts out known sources of variation | Removing batch effects or specific biological confounders (e.g., menstrual cycle) | Directly targets known confounders; highly customizable | Requires careful model specification to avoid removing signal of interest |
The following workflow diagram illustrates the sequential stages of a cross-cohort validation study, from initial cohort selection to the final validated signature.
Statistical and Analytical Considerations for Validation
Distinguishing Prognostic and Predictive Biomarkers
A fundamental statistical distinction must be made between the two primary types of biomarkers:
- Prognostic Biomarkers provide information about the overall disease outcome, regardless of therapy. They are identified through a main effect test of association between the biomarker and the outcome in a statistical model. In endometrial research, a biomarker for recurrent implantation failure (RIF) that indicates a lower probability of successful pregnancy regardless of treatment would be prognostic [99] [102].
- Predictive Biomarkers inform about the likely benefit from a specific treatment. They are identified through an interaction test between the treatment and the biomarker in a statistical model, ideally using data from a randomized clinical trial [99]. For example, a biomarker that identifies which women with displaced window of implantation (WOI) will benefit from personalized embryo transfer (pET) is predictive.
Performance Metrics and Validation
The validation of a biomarker panel requires assessing its performance against pre-specified metrics. The choice of metric depends on the biomarker's intended use (e.g., diagnostic, prognostic).
Table 2: Key Performance Metrics for Biomarker Validation
| Metric | Definition | Interpretation in Endometrial Context |
|---|---|---|
| Sensitivity | Proportion of true positives correctly identified | Ability to correctly identify women with endometrial receptivity dysfunction |
| Specificity | Proportion of true negatives correctly identified | Ability to correctly identify women with normal endometrial function |
| Positive Predictive Value (PPV) | Proportion of test-positive patients who have the disease | Probability that a woman with a positive test result truly has a receptive endometrium |
| Negative Predictive Value (NPV) | Proportion of test-negative patients who are truly disease-free | Probability that a woman with a negative test result truly has a non-receptive endometrium |
| Area Under the Curve (AUC) | Overall measure of how well the biomarker distinguishes between two groups | An AUC of 0.5 is no better than chance; 1.0 is perfect discrimination between receptive and non-receptive states |
| Calibration | How well the predicted probabilities of risk match the observed frequencies | Agreement between the model's predicted probability of pregnancy and the actual outcome rate |
It is critical to control for multiple comparisons when validating panels with many biomarkers, using measures like the False Discovery Rate (FDR) [99]. Furthermore, continuous biomarkers retain more information and provide better performance than pre-dichotomized versions; cut-offs for clinical decision-making should be established in later validation stages [99].
Experimental Protocols for Endometrial Biomarker Studies
Protocol 1: Correcting for Menstrual Cycle Bias in Transcriptomic Analysis
This protocol is essential for unmasking disease-related genes in endometrial studies [98].
- Sample Collection & RNA Extraction: Collect endometrial biopsies (e.g., using Pipelle catheter) during the target phase (e.g., mid-secretory for receptivity studies). Verify cycle phase by LH peak dating or histology (Noyes criteria). Extract total RNA using a standardized kit (e.g., Qiagen RNeasy).
- Gene Expression Profiling: Perform transcriptomic analysis using microarray (e.g., Affymetrix) or RNA-Seq (e.g., Illumina). For targeted panels, use highly quantitative methods like TAC-seq [29].
- Data Pre-processing: Normalize raw data (e.g., quantile normalization for microarrays; low-count filtering with
edgeRfor RNA-Seq). Annotate probesets to gene symbols. - Exploratory Analysis: Conduct a Principal Component Analysis (PCA) to visualize the primary sources of variation in the data. This often shows a strong separation of samples by menstrual cycle phase.
- Cycle Effect Correction: Using the
limmapackage in R, apply theremoveBatchEffectfunction, specifying the menstrual cycle phase as the "batch" to be removed. The design matrix should be defined to preserve the condition of interest (e.g., case vs. control). - Differential Expression Analysis: Perform case versus control differential expression analysis (e.g., using
limma) on the corrected data. Compare the results with an analysis performed on the uncorrected data to demonstrate the impact of bias removal.
Protocol 2: Developing and Validating a Multi-Cohort Gene Signature
This protocol outlines the steps for creating a signature like the Endometrial Failure Risk (EFR) signature [102].
Signature Discovery Cohort:
- Collect a well-phenotyped cohort of patients (e.g., women undergoing HRT cycles).
- Obtain endometrial biopsies in the mid-secretory phase and collect reproductive outcomes (e.g., live birth after single embryo transfer).
- Perform RNA sequencing and correct gene expression data for luteal phase timing variation.
- Use machine learning (e.g., random forest, LASSO regression) on the cycle-corrected data to identify a gene panel that stratifies patients into "poor" and "good" endometrial prognosis groups based on clinical outcomes.
Analytical Validation:
- Develop a quantitative predictor model (e.g., using logistic regression or a support vector machine) based on the expression of the gene panel.
- Train the model on a subset of the discovery cohort and tune hyperparameters via cross-validation (e.g., 5-fold). Assess initial accuracy, sensitivity, and specificity.
Independent Clinical Validation:
- Apply the trained model to one or more independent, external validation cohorts. These cohorts must be profiled using the same technology and harmonized as described in Section 3.
- Measure the model's performance (see Table 2) in predicting the clinical outcome in the new cohorts. For example, the EFR signature demonstrated a median accuracy of 0.92, sensitivity of 0.96, and specificity of 0.84 in its validation [102].
The pathway from biomarker discovery to clinical application involves rigorous analytical and clinical validation stages, as shown below.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Endometrial Biomarker Studies
| Reagent / Material | Function / Application | Example Kits / Platforms |
|---|---|---|
| Endometrial Biopsy Kit | Minimally invasive collection of endometrial tissue for RNA/protein analysis | Pipelle de Cornier, Tao Brush |
| RNA Stabilization & Extraction Kit | Preserves RNA integrity at collection and purifies high-quality RNA for transcriptomics | PAXgene Tissue System, Qiagen RNeasy, TRIzol |
| Gene Expression Profiling Platform | Genome-wide or targeted analysis of transcript abundance | Illumina RNA-Seq, Affymetrix Microarrays, Targeted TAC-seq |
| Immunohistochemistry Kits | Visualize and quantify protein-level biomarker expression (e.g., ER/PR) in tissue sections | Ventana BenchMark ULTRA system, DAB detection kits |
| Liquid Biopsy Assay Kits | Isolate and analyze biomarkers from biofluids (blood, uterine lavage) | Circulating tumor DNA (ctDNA) kits, Exosome isolation kits (e.g., from Qiagen, Thermo Fisher) |
| Statistical Software & Packages | Data harmonization, batch correction, and differential expression analysis | R/Bioconductor (limma, sva, edgeR), Python (scikit-learn, pandas) |
The future of biomarker validation lies in the integration of multi-omics data and advanced computational methods. Combining genomics, transcriptomics, proteomics, and metabolomics provides a more comprehensive view of endometrial biology and can lead to more robust biomarker panels [103] [104]. Artificial intelligence (AI) and machine learning are poised to revolutionize this field by systematically exploring these massive, high-dimensional datasets to find complex patterns that traditional methods miss [105] [104]. AI-powered platforms can integrate imaging, transcriptomic, and clinical data to identify meta-biomarkers, potentially reducing discovery timelines from years to months [105].
Furthermore, the use of liquid biopsies—analyzing biomarkers in blood, uterine lavage, or cervicovaginal fluid—is a promising non-invasive alternative to traditional tissue biopsies [103] [104]. As technologies for measuring circulating tumor DNA (ctDNA) and exosomes advance, these approaches will facilitate repeated sampling and real-time monitoring of endometrial status [103] [104].
In conclusion, the successful validation of biomarker panels across multiple cohorts is a demanding but achievable goal. It requires a meticulous approach that begins with robust cohort design and sample collection, incorporates rigorous statistical harmonization to control for major confounders like the menstrual cycle, and ends with stringent validation in independent populations. By adhering to these frameworks and leveraging emerging technologies, researchers can develop reliable biomarkers that truly refine diagnoses, predict outcomes, and pave the way for personalized treatments in endometrial health and disease.
Cross-Tissue Comparison of Hormone-Responsive Genetic Architecture
Within the broader thesis on the hormonal control of endometrial gene expression, this whitepaper investigates the principles governing hormone-responsive genetic architecture across diverse human tissues. The endometrium, a quintessential hormone-responsive tissue, undergoes cyclical remodeling directed by estradiol (E2) and progesterone (P4) [38]. However, a critical gap exists in understanding how these hormonal regulatory paradigms compare across the multi-tissue landscape. Recent population-scale transcriptomic datasets now enable systematic identification of genes whose expression exhibits switch-like ("on" or "off") patterns in response to hormonal and epigenetic influences [106]. This technical guide provides researchers and drug development professionals with methodologies and analytical frameworks for cross-tissue comparison, using endometrial hormone response as a foundational model to illuminate broader principles of genetic architecture.
Core Concepts and Definitions
Defining Hormone-Responsive Genetic Architecture
Hormone-responsive genetic architecture encompasses the genomic elements and regulatory mechanisms that dictate how genes respond to hormonal signals. In the context of cross-tissue analysis, this architecture manifests through several key phenomena:
- Switch-like gene expression: Bimodal expression patterns where genes are either "on" in some individuals and "off" in others, driven by hormonal or genetic variation [106]
- Tissue-specificity: Regulatory mechanisms that enable distinct hormonal responses across different tissues despite identical genetic background
- Epigenetic regulation: Chromatin modifications and DNA methylation changes that modulate hormone receptor binding and downstream signaling
- Transcriptomic dynamics: Gene expression changes across biological processes (e.g., menstrual cycle) that reflect underlying hormonal responsiveness [38]
Endometrial Context for Hormonal Regulation
The endometrium provides an ideal model system for studying hormone-responsive genetics due to its exquisite sensitivity to ovarian hormones. Each month, the endometrial tissue undergoes precisely timed morphological and molecular changes directed by E2 and P4 [38] [107]. During the proliferative phase, E2 stimulates tissue growth and thickening, while the secretory phase sees P4 promoting cellular differentiation into a receptive state capable of supporting embryo implantation [38]. This cyclical remodeling involves dramatic transcriptomic changes across epithelial, stromal, and immune cell populations, making the endometrium a prime exemplar of hormone-responsive genetic programming.
Methodological Framework
Experimental Design for Cross-Tissue Analysis
Comprehensive cross-tissue comparison requires standardized sampling, processing, and analytical approaches. The following experimental design leverages lessons from large-scale transcriptomic initiatives:
Table 1: Key Considerations for Cross-Tissue Experimental Design
| Design Element | Recommendation | Rationale |
|---|---|---|
| Tissue Selection | Include 20+ diverse tissues with hormone responsiveness | Enables identification of universal vs. tissue-specific patterns [106] |
| Sample Size | Minimum 30 individuals per tissue | Provides statistical power for bimodality detection [106] |
| Donor Characteristics | Stratify by age, sex, hormonal status | Controls for confounding variables in hormone response |
| Tissue Processing | Standardized RNA extraction and sequencing protocols | Minimizes technical batch effects across tissues |
| Metadata Collection | Detailed clinical, hormonal, and demographic data | Enables covariate adjustment and subgroup analysis |
Core Molecular Profiling Methods
Transcriptomic Sequencing: Bulk RNA-seq (≥50 million reads, paired-end) provides expression quantification across tissues. Single-cell RNA-seq (10X Genomics platform) enables cell-type resolution of hormone responses, particularly valuable in heterogeneous tissues like endometrium with its epithelial, stromal, endothelial and immune cell populations [38].
Epigenetic Profiling: ATAC-seq assays chromatin accessibility in hormone-responsive regions. Whole-genome bisulfite sequencing identifies methylation changes correlated with hormonal status.
Genetic Variant Calling: Whole-genome sequencing (30X coverage) identifies structural variants and single-nucleotide polymorphisms underlying expression variation.
Computational and Statistical Approaches
Identification of Switch-like Genes: Apply the dip test of unimodality to expression distributions across individuals for each gene-tissue pair, with p-value recalibration to control confounders and multiple hypothesis correction [106].
Tissue-Specificity Quantification: Calculate pairwise tissue-to-tissue correlation of expression levels for all tissue pairs, followed by principal component analysis to identify clusters of co-expressed genes [106].
Causal Inference: Employ Mendelian randomization to explore causal relationships between gene expression influenced by environmental factors like endocrine-disrupting chemicals and disease outcomes [108].
Network Analysis: Implement Weighted Gene Co-expression Network Analysis (WGCNA) to cluster correlated genes into modules associated with phenotypic traits [107].
Data Analysis and Interpretation
Classifying Hormone-Responsive Genes
Analysis of 27 tissues from 943 individuals reveals that hormone-responsive genes fall into distinct categories based on their expression patterns:
Table 2: Classification of Hormone-Responsive Gene Expression Patterns
| Gene Category | Prevalence | Regulatory Mechanism | Example Genes | Tissue Specificity |
|---|---|---|---|---|
| Universally Switch-like | 8.5% (40/473 genes) | Genetically controlled epigenetic silencing [106] | GPX1P1, FAM118A | All tissues |
| Tissue-Specific Switch-like | 85.3% (404/473 genes) | Hormone-driven epigenetic modification [106] | KRT17, SOX9 | Specific tissue subsets |
| Sex-Specific | 1.7% (8/473 genes) | Y-chromosome location or X-inactivation [106] | EIF1AY, XIST | All non-sex-specific tissues |
| Cycle-Phase Dependent | ~4.5% (est.) | Hormone receptor activation | ESR1, PGR, THBS1 [38] | Endometrium and reproductive tissues |
Endometrial Transcriptomic Dynamics
The endometrial epithelium exhibits precisely orchestrated transcriptomic changes across the menstrual cycle, driven by hormonal fluctuations:
Table 3: Endometrial Transcriptomic Changes During Menstrual Cycle Phases
| Cycle Phase | Hormonal Milieu | Key Upregulated Genes | Biological Processes |
|---|---|---|---|
| Menstrual/ Early Proliferative | Low P4, rising E2 | MMP7, MMP10, MMP11, PDGFRa [38] | Tissue breakdown, re-epithelialization, ECM remodeling |
| Proliferative | High E2 | ESR1, PGR, TIMP1, CADM1, THBS1 [38] | Tissue growth, angiogenesis, cellular proliferation |
| Secretory | High P4 | LIF, PAEP, HB-EGF, PRL, IGFBP1 [38] | Cellular differentiation, secretion, immunotolerance |
Signaling Pathways and Regulatory Networks
The following diagram illustrates the core transcriptional response to hormonal signaling in the endometrium and its cross-tissue regulation:
Hormonal Regulation of Gene Expression
Advanced Analytical Workflow
The comprehensive analysis of cross-tissue hormone-responsive genes requires an integrated workflow:
Cross-Tissue Analysis Workflow
Research Reagent Solutions
Table 4: Essential Research Reagents for Hormone-Responsive Genetic Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Reference Transcriptomes | GTEx dataset (27 tissues, 943 individuals) [106] | Baseline for cross-tissue expression comparison |
| Endometrial Organoids | Primary tissue-derived 3D cultures [38] | In vitro modeling of endometrial hormone response |
| Hormone Receptor Modulators | Selective estrogen receptor modulators, Progesterone antagonists | Experimental manipulation of hormonal signaling pathways |
| Single-Cell RNA-seq Kits | 10X Genomics Chromium Single Cell 3' Kit | Cell-type resolution transcriptomics in heterogeneous tissues |
| Epigenetic Profiling Kits | ATAC-seq kits, Bisulfite conversion kits | Mapping chromatin accessibility and DNA methylation patterns |
| Bioinformatics Tools | WGCNA R package [107], DESeq2, GENCODE annotations | Differential expression, co-expression network analysis |
Applications and Future Directions
Therapeutic Target Discovery
Cross-tissue analysis of hormone-responsive genes enables prioritization of therapeutic targets with optimal efficacy and safety profiles. Genes exhibiting tissue-specific switch-like behavior present particularly attractive targets, as their modulation may achieve therapeutic effects while minimizing off-target consequences. For example, endometrial-specific switch-like genes identified through comparison to 26 other tissues may offer targets for treating endometriosis or infertility with reduced systemic effects [106] [109].
Personalized Medicine Applications
The individual variation in hormone-responsive gene expression enables personalized approaches to reproductive medicine. Transcriptomic profiling of uterine fluid extracellular vesicles (UF-EVs) presents a non-invasive method for assessing endometrial receptivity, with Bayesian modeling of gene expression modules achieving predictive accuracy of 0.83 for pregnancy outcomes [107]. Similarly, identification of switch-like genes in vaginal epithelium associated with vaginal atrophy enables targeted interventions for individuals with the "off" state of protective genes [106].
Environmental Health Risk Assessment
Integrative causal inference approaches illuminate gene-environment interactions linking endocrine disruptors to female infertility. Mendelian randomization and colocalization analyses have identified five genes (SULT1B1, MASTL, TTC39C, ESR1, AKAP13) significantly associated with infertility risk, with interactions between these genes and endocrine-disrupting chemicals like BPA and TCDD revealing molecular mechanisms through which environmental exposures influence fertility [108]. These findings enable stratification of genetic susceptibility to environmental reproductive toxicants.
This technical guide establishes a comprehensive framework for cross-tissue comparison of hormone-responsive genetic architecture, anchored in endometrial biology but extensible to diverse tissue types. The methodologies, classifications, and analytical approaches detailed herein provide researchers and drug development professionals with robust tools for deciphering the complex interplay between hormonal signals, genetic variation, and tissue context in shaping gene expression patterns. As single-cell technologies advance and multi-omic datasets expand, these cross-tissue comparisons will increasingly illuminate the fundamental principles of hormonal gene regulation while accelerating development of targeted therapeutics for reproductive disorders and hormone-responsive diseases.
Clinical Validation of Molecular Classifiers for Endometrial Receptivity
The successful establishment of pregnancy relies on the precise synchronization of a viable embryo with a receptive endometrium, a transient state known as the window of implantation (WOI). This process is orchestrated by a complex network of ovarian steroid hormones—primarily estrogen and progesterone—that regulate endometrial gene expression to enable embryonic attachment and invasion. Dysregulation of this hormonally controlled transcriptional program is a significant cause of recurrent implantation failure (RIF), presenting a major challenge in assisted reproductive technology (ART).
Molecular classifiers for endometrial receptivity represent a paradigm shift from traditional histological dating to transcriptome-based profiling. These tools aim to objectively identify the WOI by analyzing the expression patterns of hormonally-regulated genes, thereby enabling personalized embryo transfer (pET) for women with implantation disorders. This whitepaper examines the clinical validation of these emerging molecular diagnostics, framing them within the broader context of hormonal control of endometrial gene expression. We evaluate their technical performance, clinical utility, and integration into drug development pipelines for novel therapeutics targeting endometrial dysfunction.
Current Landscape of Validated Molecular Classifiers
Established Transcriptomic Assays
Several molecular classifiers have transitioned from research to clinical application, employing distinct gene panels and analytical approaches to assess endometrial receptivity.
Table 1: Clinically Available Molecular Classifiers for Endometrial Receptivity
| Test Name | Technology Platform | Number of Genes | Reported Accuracy | Key Validated Clinical Applications |
|---|---|---|---|---|
| Endometrial Receptivity Array (ERA) | Microarray | 238 | Not explicitly stated in results | Identification of displaced WOI in RIF patients [29] [110] |
| beREADY | TAC-seq (Targeted Allele Counting by sequencing) | 72 | 98.8% cross-validation accuracy [29] | Detection of WOI shifts in RIF patients (15.9% vs 1.8% in fertile controls) [29] |
| ER Map | Not specified in results | Not specified in results | Not specified in results | Clinical application mentioned but performance metrics not detailed [29] |
| WIN-Test | Not specified in results | Not specified in results | Not specified in results | Clinical application mentioned but performance metrics not detailed [29] |
| rsERT test | Not specified in results | Not specified in results | Not specified in results | Clinical application mentioned but performance metrics not detailed [29] |
The clinical validation of these tests primarily focuses on their ability to identify displaced WOI in patients with recurrent implantation failure. The beREADY test demonstrated a significantly higher proportion of displaced WOI in RIF patients (15.9%) compared to fertile controls (1.8%, p=0.012) [29]. This suggests that molecular displacement of the WOI represents a genuine pathophysiological mechanism in a subset of RIF patients.
Novel Approaches and Emerging Biomarkers
Beyond established mRNA-based classifiers, emerging technologies are expanding the diagnostic arsenal for endometrial receptivity assessment:
miRNA-Based Profiling: The microRNA Receptivity Assay (MIRA) analyzes 89 microRNAs and shows 72% concordance with ERA (Kappa=0.50). Notably, patients with delayed miRNA expression relative to mRNA profiles ("Slow" group) had significantly lower pregnancy rates (54.5%) compared to those with synchronous or leading miRNA expression (81.9-94.1%, p=0.031) [110]. This suggests miRNA-mRNA asynchrony may represent a novel dysfunction mechanism.
Non-Invasive Liquid Biopsies: Transcriptomic analysis of extracellular vesicles from uterine fluid (UF-EVs) represents a promising non-invasive alternative to endometrial biopsy. A Bayesian logistic regression model integrating UF-EV gene expression modules with clinical variables achieved a predictive accuracy of 0.83 and F1-score of 0.80 for pregnancy outcome prediction [107].
Molecular Subtyping of RIF: Recent research has identified two biologically distinct endometrial subtypes in RIF patients: immune-driven (RIF-I) and metabolic-driven (RIF-M). A molecular classifier (MetaRIF) accurately distinguished these subtypes in independent validation cohorts (AUC: 0.94 and 0.85) and outperformed previously published models [111].
Experimental Protocols for Development and Validation
Sample Collection and Processing Standards
Robust clinical validation requires standardized protocols across multiple sites. Key methodological considerations include:
Timing and Verification: Endometrial biopsies should be timed according to the LH surge (e.g., LH+7 for mid-secretory phase) with precise dating corroborated by histological evaluation using Noyes' criteria [111]. Studies report exclusion of 11/63 samples due to inconsistency between histology and LH dating, highlighting the importance of rigorous timing verification [29].
Sample Processing: Tissues should be immediately cryopreserved at -80°C. RNA extraction using commercial kits (e.g., Qiagen RNeasy Mini Kits) with quality assessment via NanoDrop spectrophotometry and Agilent Bioanalyzer is standard [111] [33]. Ribosomal RNA depletion followed by strand-specific library construction enables comprehensive transcriptome analysis [33].
Analytical Workflows
Table 2: Key Analytical Methods for Molecular Classifier Development
| Method | Application | Technical Considerations |
|---|---|---|
| TAC-seq (Targeted Allele Counting by sequencing) | Highly quantitative analysis of targeted gene panels down to single-molecule level [29] | Enables precise cost-effective biomarker analysis with high dynamic range |
| RNA Sequencing (Bulk) | Differential expression analysis; identification of DEGs [111] [33] | Requires normalization (FPKM, TPM); DEG identification using DESeq2 with FDR <0.05 |
| Single-cell RNA Sequencing | Cellular heterogeneity analysis; mapping gene expression to specific cell types [33] | Quality control critical (exclude cells with low gene counts/high mitochondrial content); Seurat package standard for analysis |
| Weighted Gene Co-expression Network Analysis (WGCNA) | Identification of correlated gene modules associated with clinical traits [107] | Clusters genes into functionally relevant modules; module eigengenes represent overall expression patterns |
| Consensus Clustering | Unsupervised molecular subtyping [111] | Identifies reproducible subtypes (e.g., RIF-I and RIF-M); biological characteristics analyzed via GSEA |
The analytical pipeline for the beREADY test exemplifies a rigorous approach: after sample processing and sequencing, expression data undergoes a three-stage computational classification (pre-receptive, receptive, post-receptive) with transitionary classes (early-receptive, late-receptive) representing normal WOI variability [29]. Model performance is validated through cross-validation (98.8% accuracy) and independent validation cohorts [29].
Figure 1: Experimental Workflow for Molecular Classifier Development and Validation
Integration with Hormonal Regulation Pathways
Molecular classifiers must be interpreted within the context of hormonal control mechanisms that govern endometrial gene expression. Progesterone-driven signaling is particularly critical for establishing receptivity.
Figure 2: Hormonal Regulation of Endometrial Receptivity and Dysfunction Pathways
The molecular subtypes of RIF reflect distinct disruptions in hormonally-regulated pathways. The RIF-M subtype demonstrates dysregulation of oxidative phosphorylation, fatty acid metabolism, steroid hormone biosynthesis, and altered expression of the circadian clock gene PER1 [111]. In contrast, the RIF-I subtype shows enrichment for immune and inflammatory pathways (IL-17 and TNF signaling) with increased infiltration of effector immune cells [111]. These findings highlight how progesterone signaling coordinates diverse biological processes to establish receptivity, and how distinct dysfunction patterns require different therapeutic approaches.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Endometrial Receptivity Research
| Reagent/Kit | Manufacturer | Function/Application |
|---|---|---|
| Qiagen RNeasy Mini Kits | Qiagen | Total RNA isolation from endometrial tissues [111] |
| RNA-easy isolation reagent | Vazyme | Total RNA extraction; rRNA removal for mRNA enrichment [33] |
| TAC-seq (Targeted Allele Counting by sequencing) | Custom | Highly quantitative analysis of targeted gene panels [29] |
| DESeq2 package | R/Bioconductor | Differential expression analysis; identifies DEGs with FDR <0.05 [111] [33] |
| Seurat package | R | scRNA-seq data preprocessing, normalization, dimensionality reduction, and clustering [33] |
| ConsensusClusterPlus | R/Bioconductor | Unsupervised molecular subtyping; identifies reproducible subtypes [111] |
| clusterProfiler package | R/Bioconductor | Gene Ontology enrichment analysis of biological processes [33] |
Clinical Validation and Performance Metrics
Analytical Validation
Molecular classifiers must demonstrate robust analytical performance before clinical implementation:
Precision and Reproducibility: The beREADY test showed 98.2% accuracy in validation groups, with cross-validation accuracy of 98.8% [29]. The MetaRIF classifier for RIF subtyping achieved AUCs of 0.94 and 0.85 in independent validation cohorts, outperforming previous models [111].
Discriminatory Power: The asynchrony between miRNA and mRNA profiles demonstrates novel discriminatory capacity, with the "Slow" miRNA group showing significantly poorer pregnancy outcomes (54.5% vs 81.9-94.1%) [110].
Clinical Utility and Outcomes
The ultimate validation of molecular classifiers rests on their ability to improve clinical outcomes:
WOI Displacement Detection: Molecular profiling identifies WOI displacements in approximately 15.9% of RIF patients compared to 1.8% in fertile controls [29], providing a molecular diagnosis for a subset of previously unexplained implantation failure.
Predictive Value for Pregnancy Outcomes: UF-EV transcriptomic analysis combined with clinical variables achieved 0.83 accuracy for predicting pregnancy outcome [107], suggesting potential for non-invasive receptivity assessment.
Personalized Treatment Guidance: The identification of RIF subtypes (RIF-I and RIF-M) enables subtype-specific therapeutic approaches, with CMap-based drug predictions identifying sirolimus as a candidate for RIF-I and prostaglandins for RIF-M [111].
Molecular classifiers for endometrial receptivity represent a significant advancement in personalized reproductive medicine, moving beyond morphological assessment to hormonally-regulated transcriptomic profiling. Clinical validation studies demonstrate their ability to identify displaced WOI in RIF patients, classify molecular subtypes of endometrial dysfunction, and predict pregnancy outcomes with increasing accuracy.
Future developments will likely focus on non-invasive approaches using uterine fluid biomarkers, integration of multi-omics data (transcriptomics, proteomics, metabolomics), and artificial intelligence-driven models to further enhance predictive power. Additionally, connecting molecular classifications with targeted therapeutic interventions represents the next frontier for truly personalized management of implantation disorders. As these technologies evolve, they will continue to illuminate the complex hormonal control of endometrial gene expression while offering new hope for patients with previously unexplained implantation failure.
Conclusion
The hormonal control of endometrial gene expression represents a sophisticated interplay between cyclical transcriptional programs, epigenetic modifications, and genetic variation that collectively determine endometrial function and receptivity. Recent advances in single-cell technologies, organoid models, and molecular profiling have revolutionized our understanding of endometrial biology, revealing distinct pathological subtypes in conditions like recurrent implantation failure and PCOS. The development of validated diagnostic tools and personalized screening platforms marks a significant transition toward precision medicine in reproductive health. Future research must focus on integrating multi-omics data across diverse patient populations, developing targeted interventions for specific molecular subtypes of endometrial dysfunction, and translating these findings into improved clinical outcomes for infertility and endometrial disorders. The continued elucidation of endometrial gene regulatory networks will undoubtedly yield novel therapeutic targets and diagnostic strategies for the next generation of reproductive medicine.
References
- 1. Estrogen Receptor Function: Impact on the Human ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.827724/full]
- 2. Genes targeted by the estrogen and progesterone receptors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2805670/]
- 3. Serum response factor is essential for endometrial function ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595411/]
- 4. Endometrial changes in estrogen and progesterone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7579777/]
- 5. The study on the clinical efficacy of endometrial receptivity ... [https://www.nature.com/articles/s41598-025-91745-y]
- 6. Strategies for modelling endometrial diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10052865/]
- 7. Endometrial expression of estrogen and progesterone ... [https://www.sciencedirect.com/science/article/abs/pii/S0093691X17305782]
- 8. Computational Models for Diagnosing and Treating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580807/]
- 9. Molecular Impact of Metabolic and Endocrine Disturbance on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563804/]
- 10. Singleâ€cell RNA sequencing technologies and applications [https://pmc.ncbi.nlm.nih.gov/articles/PMC8964935/]
- 11. Experimental design for single-cell RNA sequencing [https://pubmed.ncbi.nlm.nih.gov/29126257/]
- 12. Getting Started with scRNA-seq: Experimental Design and ... [https://www.parsebiosciences.com/blog/getting-started-with-scrna-seq-experimental-design-and-sample-preparation/]
- 13. Optimized design of single-cell RNA sequencing ... [https://www.nature.com/articles/s41467-020-19365-w]
- 14. Single-cell RNA sequencing of endometrium uncovers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465366/]
- 15. Single-cell RNA sequencing identifies the prolactin ... [https://www.nature.com/articles/s41392-025-02339-z]
- 16. Genetic Regulation of Transcription in the Endometrium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9580733/]
- 17. Epigenetics' responsibility in endometriosis [https://www.sciencedirect.com/science/article/abs/pii/S0960076025001426]
- 18. Leveraging epigenetic aberrations in the pathogenesis of ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1597287/full]
- 19. Epigenetic Regulation of Aging and its Rejuvenation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12402629/]
- 20. The Prognosis Prediction Model for Endometrial Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12174473/]
- 21. Genome-Wide Analysis of Histone Modifications in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5414786/]
- 22. Epigenetic regulation in metabolic diseases: mechanisms ... [https://www.nature.com/articles/s41392-023-01333-7]
- 23. Non-Coding RNAs in Endometrial Physiopathology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6073439/]
- 24. From DNA Methylation and Histone Modifications to Non- ... [https://www.mdpi.com/2076-3417/15/18/9940]
- 25. Endometrial Receptivity - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK587449/]
- 26. Non-Invasive and Mechanism-Based Molecular ... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2022.863173/full]
- 27. The precise determination of the window of implantation ... [https://www.nature.com/articles/s41598-021-92955-w]
- 28. The role of transcriptomic biomarkers of endometrial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8082865/]
- 29. Targeted gene expression profiling for accurate ... [https://www.nature.com/articles/s41598-023-40991-z]
- 30. Advances in endometrial receptivity and embryo ... [https://www.sciencedirect.com/science/article/pii/S2950248925000355]
- 31. Regulation of RNA splicing in endometrial tissue and its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359188/]
- 32. Molecular subtype of recurrent implantation failure reveals ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06771-1]
- 33. Immune-related gene signatures of thin endometrium [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1626451/full]
- 34. Glucose metabolism and endometrium decidualization [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1546335/full]
- 35. Endometrial stromal Menin supports ... [https://www.nature.com/articles/s42003-025-08434-9]
- 36. Mechanisms Driving Resistance to Oxidative Stress During ... [https://pubmed.ncbi.nlm.nih.gov/40891509/]
- 37. Metabolic reprogramming and heterogeneity during the ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01763-y]
- 38. Organoids as powerful models of endometrium epithelium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12234953/]
- 39. Organoids as powerful models of endometrium epithelium ... [https://pubmed.ncbi.nlm.nih.gov/40622575/]
- 40. Menstrual flow as a non-invasive source of endometrial ... [https://www.nature.com/articles/s42003-021-02194-y]
- 41. Mapping the temporal and spatial dynamics of the human ... [https://www.nature.com/articles/s41588-021-00972-2]
- 42. Protocol for the establishment and characterization of an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10879800/]
- 43. Organoid co-culture model of the human endometrium in a ... [https://www.sciencedirect.com/science/article/pii/S2666634023002271]
- 44. An integrated single-cell reference atlas of the human ... [https://www.nature.com/articles/s41588-024-01873-w]
- 45. A spatial transcriptomics dataset of the endometrium from ... [https://www.nature.com/articles/s41597-025-05995-6]
- 46. Human endometrial cell-type-specific RNA sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9632455/]
- 47. Cell type and region-specific transcriptional changes in the ... [https://pubmed.ncbi.nlm.nih.gov/40063812/]
- 48. Single-cell and spatial transcriptomic profiling revealed ... [https://www.sciencedirect.com/science/article/pii/S2666979X24003665]
- 49. A Comprehensive Review of the Endometrial in... Receptivity Array [https://pmc.ncbi.nlm.nih.gov/articles/PMC11424594/]
- 50. Endometriosis-associated infertility: Multi-omics insights ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1613334/full]
- 51. Transferring a Quantitative Molecular Diagnostic Test to ... [https://www.sciencedirect.com/science/article/pii/S152515781730524X]
- 52. toward defining endometrial-based infertility - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10833067/]
- 53. Machine learning center-specific models show improved ... [https://www.nature.com/articles/s41467-025-58744-z]
- 54. Single-cell profiling of the human endometrium in ... [https://www.nature.com/articles/s41591-025-03592-z]
- 55. Enabling technologies for personalized and precision ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7924935/]
- 56. Genome-wide CRISPR screening reveals ADCK3 as a key ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10421920/]
- 57. A framework for N-of-1 trials of individualized gene ... [https://www.nature.com/articles/s41467-024-54077-5]
- 58. The role of epigenetic mechanisms in the regulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8146649/]
- 59. Genetic Regulation of Transcription in the Endometrium in ... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2021.795464/full]
- 60. Advances in biomonitoring technologies for women's health [https://pmc.ncbi.nlm.nih.gov/articles/PMC12475061/]
- 61. Why We Must Stop Assuming and Estimating Menstrual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12152053/]
- 62. Machine learning-based menstrual phase identification ... [https://www.nature.com/articles/s44294-025-00078-8]
- 63. A statistical normalization method and differential expression ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-019-2745-1]
- 64. 'A medical miracle': is period blood 'the most overlooked ... [https://www.theguardian.com/society/ng-interactive/2025/oct/27/menstrual-period-blood-testing-womens-health]
- 65. Statistical tests for differential expression in cDNA microarray ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC154570/]
- 66. Molecular subtype of recurrent implantation failure reveals ... [https://pubmed.ncbi.nlm.nih.gov/40660214/]
- 67. Innate and adaptive immune dysregulation in women with ... [https://www.sciencedirect.com/science/article/abs/pii/S0165037824000718]
- 68. Shared diagnostic biomarkers and underlying mechanisms ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1490746/full]
- 69. Recurrent implantation failure: A comprehensive summary ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.1061766/full]
- 70. Efficacy of glucocorticoids treatment in recurrent embryo ... [https://www.nature.com/articles/s41420-025-02753-w]
- 71. Cell atlas of the endometrium in women with PCOS may ... [https://news.ki.se/cell-atlas-of-the-endometrium-in-women-with-pcos-may-lead-to-better-treatment]
- 72. Enhancing understanding of endometrial function in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11900192/]
- 73. PCOS endometrium-derived epithelial organoids as a novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12314152/]
- 74. Review Pharmacological and non- ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648324005704]
- 75. Gene expression profile of human endometrial receptivity [https://pmc.ncbi.nlm.nih.gov/articles/PMC2871799/]
- 76. Endometrial transcriptome profiling of patients with ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1292723/full]
- 77. Clinical pregnancy outcomes in young women with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339334/]
- 78. Molecular and biological markers for assessing endometrial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12041708/]
- 79. High androgen level during controlled ovarian stimulation ... [https://www.nature.com/articles/s41598-024-74295-7]
- 80. Platelet-Rich Plasma in Reproductive Endocrinology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561688/]
- 81. How to study the menstrual cycle - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8363181/]
- 82. Improving Replication in Endometrial Omics [https://www.mdpi.com/1422-0067/26/2/857]
- 83. Learning exceptions to category rules varies across the ... [https://www.nature.com/articles/s41598-023-48628-x]
- 84. Endometrial receptivity profiled through transcriptomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12518540/]
- 85. Genetic regulation of disease risk and endometrial gene expression highlights potential target genes for endometriosis and polycystic ovarian syndrome - PubMed [https://pubmed.ncbi.nlm.nih.gov/30061686/]
- 86. Co-regulatory expression quantitative trait loci mapping: method and application to endometrial cancer - PubMed [https://pubmed.ncbi.nlm.nih.gov/21226949/]
- 87. Regulatory Effects of Endometriosis-Associated Genetic Variants [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385710/]
- 88. Multiomic insight into the involvement of cell aging related genes in the pathogenesis of endometriosis | Scientific Reports [https://www.nature.com/articles/s41598-025-96711-2]
- 89. Development and validation of a prognostic model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599766/]
- 90. Signaling pathways and advances in targeted therapy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635047/]
- 91. GRB2 regulation of essential signaling pathways in the ... [https://www.nature.com/articles/s41467-025-57173-2]
- 92. Insights into the Molecular Mechanisms and Signaling ... [https://www.mdpi.com/1422-0067/26/15/7460]
- 93. Selection and validation of reference genes for ... [https://www.sciencedirect.com/science/article/pii/S1642431X25000300]
- 94. Tissue specific regulation of transcription in endometrium and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7048713/]
- 95. Genetic regulation of disease risk and endometrial gene ... [https://www.nature.com/articles/s41598-018-29462-y]
- 96. GWAS meta-analysis identifies five susceptibility loci for ... [https://www.sciencedirect.com/science/article/pii/S2352396425002749]
- 97. Proteomic Analysis of Human Endometrial Tissues Reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7463404/]
- 98. Guidelines for biomarker discovery in endometrium [https://pmc.ncbi.nlm.nih.gov/articles/PMC8063681/]
- 99. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 100. Harmonization of CSF and imaging biomarkers in ... [https://www.sciencedirect.com/science/article/pii/S0969996123003893]
- 101. A robust harmonization approach for cognitive data from ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10369372/]
- 102. Predicting risk of endometrial failure: a biomarker signature ... [https://www.sciencedirect.com/science/article/pii/S0015028224001900]
- 103. Present progress in biomarker discovery of endometrial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12032760/]
- 104. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 105. AI-Powered Biomarker Discovery: 7 ... [https://lifebit.ai/blog/ai-powered-biomarker-discovery/]
- 106. Switch-like gene expression modulates disease risk [https://www.nature.com/articles/s41467-025-60513-x]
- 107. Endometrial receptivity profiled through transcriptomic ... [https://www.nature.com/articles/s41598-025-19633-z]
- 108. Integrative causal inference illuminates gene-environment ... [https://www.sciencedirect.com/science/article/pii/S0147651325010243]
- 109. Regulation of RNA splicing in endometrial tissue and its ... [https://www.sciencedirect.com/science/article/pii/S2589004225014683]
- 110. Asynchrony Between Endometrial miRNA- and mRNA- ... [https://www.mdpi.com/1422-0067/26/15/7349]
- 111. Molecular subtype of recurrent implantation failure reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257665/]