Machine Learning in Biomarker Discovery: From Data to Clinical Impact
This article provides a comprehensive overview of machine learning (ML) applications in biomarker discovery for researchers, scientists, and drug development professionals.
Machine Learning in Biomarker Discovery: From Data to Clinical Impact
Abstract
This article provides a comprehensive overview of machine learning (ML) applications in biomarker discovery for researchers, scientists, and drug development professionals. It explores the foundational need for ML in analyzing complex omics data, details practical methodological approaches and successful applications, addresses critical challenges like overfitting and data quality, and examines rigorous validation frameworks. By synthesizing current methodologies and real-world case studies, this guide aims to bridge the gap between computational innovation and robust, clinically translatable biomarker development.
The New Frontier: Why Machine Learning is Revolutionizing Biomarker Research
The rapid evolution of high-throughput technologies has generated an unprecedented deluge of biological data, creating both opportunities and challenges for biomarker discovery. Multi-omics strategies, which integrate genomics, transcriptomics, proteomics, metabolomics, and epigenomics, have revolutionized our approach to understanding complex diseases like cancer [1]. This integrative approach provides a comprehensive view of molecular networks that govern cellular life, enabling the identification of robust biomarkers for diagnosis, prognosis, and therapeutic decision-making in personalized oncology [1]. The inherent complexity of biological systems means that single-omics approaches often fail to capture the complete picture of disease mechanisms, making multi-omics integration not merely advantageous but essential for meaningful biological inference [1] [2].
The transition from single-omics to multi-omics analysis represents a paradigm shift in biomedical research. Where traditional methods focused on single genes or proteins, multi-omics integration can reveal complex interactions and emergent properties that remain invisible when examining molecular layers in isolation [2]. This holistic perspective is particularly crucial for biomarker discovery, as biomarkers identified through multi-omics strategies demonstrate greater clinical utility and reliability compared to those derived from single-omics approaches [1]. The challenge now lies in developing sophisticated computational frameworks capable of navigating this high-dimensional landscape to extract biologically and clinically meaningful insights.
Analytical Frameworks and Computational Strategies
Multi-Omics Integration Approaches
The integration of diverse omics datasets requires sophisticated computational strategies that can be broadly categorized into three main paradigms: early, intermediate, and late integration [3]. Each approach offers distinct advantages and limitations, making them suitable for different research contexts and questions.
Early integration involves combining raw data from different omics layers at the beginning of the analytical pipeline. This strategy can capture complex correlations and relationships between different molecular layers but may introduce significant noise and computational challenges [3]. Intermediate integration processes each omics dataset separately initially, then combines them at the feature selection, extraction, or model development stage. This balanced approach maintains the unique characteristics of each data type while enabling the identification of cross-omics patterns [3]. Late integration, also known as vertical integration, analyzes each omics dataset independently and combines the results at the final interpretation stage. This method preserves dataset-specific signals but may miss important inter-omics relationships [3].
The selection of an appropriate integration strategy depends on multiple factors, including research objectives, data characteristics, computational resources, and the specific biological questions under investigation. A comprehensive understanding of the strengths and limitations of each approach is fundamental to effective multi-omics data analysis [3].
Machine Learning and Deep Learning Applications
Machine learning (ML) and deep learning (DL) have emerged as powerful tools for multi-omics integration, capable of identifying complex, non-linear patterns within high-dimensional datasets that traditional statistical methods often miss [1] [2]. These approaches have demonstrated particular utility in biomarker discovery, where they can integrate diverse data types including genomics, transcriptomics, proteomics, metabolomics, imaging, and clinical records [2].
Deep learning architectures, such as those implemented in tools like Flexynesis, provide flexible frameworks for bulk multi-omics data integration [4]. Flexynesis streamlines data processing, feature selection, and hyperparameter tuning while supporting multiple task types including regression, classification, and survival modeling [4]. This flexibility is especially valuable in precision oncology, where accurate decision-making depends on integrating multimodal molecular information [4]. The toolkit's modular design allows researchers to choose from various deep learning architectures or classical machine learning methods through a standardized interface, making advanced computational approaches more accessible to users with varying levels of computational expertise [4].
Beyond conventional ML/DL approaches, genetic programming has shown promise for optimizing multi-omics integration and feature selection. This evolutionary algorithm-based approach can identify robust biomarkers and improve predictive accuracy in survival analysis, as demonstrated in breast cancer research where it achieved a concordance index (C-index) of 67.94 on test data [3]. Similarly, adaptive integration frameworks like MOGLAM and MoAGL-SA employ dynamic graph convolutional networks with feature selection to generate high-quality omic-specific embeddings and identify important biomarkers [3].
Table 1: Performance Metrics of Selected Multi-Omics Integration Methods
| Method | Cancer Type | Application | Performance | Reference |
|---|---|---|---|---|
| DeepMO | Breast Cancer | Subtype Classification | 78.2% Accuracy | [3] |
| DeepProg | Liver/Breast Cancer | Survival Prediction | C-index: 0.68-0.80 | [3] |
| Adaptive Multi-omics Framework | Breast Cancer | Survival Analysis | C-index: 67.94 (Test) | [3] |
| SeekInCare | Multiple Cancers | Early Detection | 60.0% Sensitivity, 98.3% Specificity | [5] |
| MOFA+ | Pan-Cancer | Latent Factor Modeling | N/A (Interpretability Focus) | [3] |
Experimental Protocols and Workflows
Protocol: Multi-Omics Biomarker Discovery Pipeline
This protocol outlines a comprehensive workflow for biomarker discovery from multi-omics data, incorporating quality control, integration, and validation steps essential for generating clinically relevant findings.
Materials and Reagents:
- Multi-omics datasets (e.g., from TCGA, CPTAC, CCLE)
- High-performance computing infrastructure
- Bioinformatics software packages (e.g., Flexynesis, MOFA+)
- Statistical analysis environment (R, Python)
Procedure:
Data Acquisition and Curation
Quality Control and Preprocessing
- Perform platform-specific quality assessment for each omics dataset
- Apply normalization procedures to address technical variability
- Handle missing values using appropriate imputation methods
- Filter low-quality samples and features with minimal expression/variance
Data Integration and Feature Selection
- Select integration strategy (early, intermediate, or late) based on research question
- Implement dimensionality reduction techniques (PCA, UMAP, autoencoders)
- Apply feature selection algorithms to identify informative molecular features
- Utilize genetic programming or ML-based methods for optimized feature selection [3]
Predictive Model Development
- Partition data into training, validation, and test sets (e.g., 70/15/15 split)
- Train ML/DL models using appropriate architectures (e.g., fully connected networks, graph convolutional networks)
- Optimize hyperparameters through cross-validation
- Regularize models to prevent overfitting
Biomarker Validation and Interpretation
- Evaluate model performance on independent test sets using relevant metrics (AUC, C-index)
- Assess clinical utility through survival analysis or treatment response prediction
- Perform biological interpretation via pathway enrichment and network analysis
- Validate findings in external cohorts when available
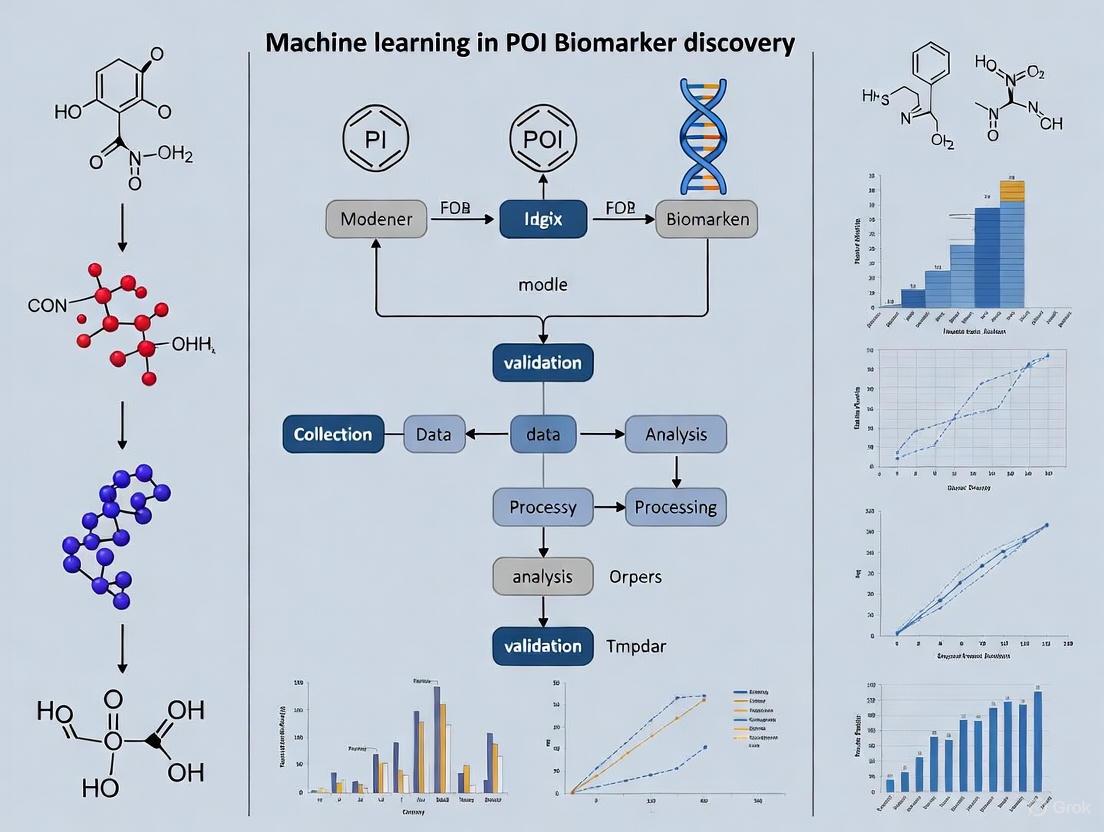
Workflow Visualization
Multi-Omics Biomarker Discovery Workflow: This diagram illustrates the comprehensive pipeline for biomarker discovery from multi-omics data, highlighting key stages from data collection to clinical application and the three primary integration strategies.
Applications in Precision Oncology
Clinically Validated Multi-Omics Biomarkers
Multi-omics approaches have yielded numerous clinically actionable biomarkers that are transforming precision oncology. These biomarkers operate at different molecular levels and have been validated through large-scale studies and clinical trials.
The tumor mutational burden (TMB), validated in the KEYNOTE-158 trial, has received FDA approval as a predictive biomarker for pembrolizumab treatment across various solid tumors [1]. Similarly, transcriptomic signatures such as Oncotype DX (21-gene) and MammaPrint (70-gene) have demonstrated utility in tailoring adjuvant chemotherapy decisions for breast cancer patients, as evidenced by the TAILORx and MINDACT trials [1]. Proteomic analyses through initiatives like the Clinical Proteomic Tumor Analysis Consortium (CPTAC) have identified functional subtypes and druggable vulnerabilities in ovarian and breast cancers that were missed by genomic analyses alone [1].
Epigenomic markers also show significant clinical promise. MGMT promoter methylation status serves as a established predictive biomarker for temozolomide response in glioblastoma patients [1]. Furthermore, DNA methylation-based multi-cancer early detection assays, such as the Galleri test, are currently under clinical evaluation and represent the next frontier in cancer screening [1].
Table 2: Clinically Validated Multi-Omics Biomarkers in Oncology
| Biomarker | Omics Layer | Cancer Type | Clinical Application | Level of Evidence |
|---|---|---|---|---|
| TMB | Genomics | Multiple Solid Tumors | Immunotherapy Response | FDA-Approved (KEYNOTE-158) |
| Oncotype DX | Transcriptomics | Breast Cancer | Chemotherapy Decision | TAILORx Trial |
| MammaPrint | Transcriptomics | Breast Cancer | Chemotherapy Decision | MINDACT Trial |
| MGMT Methylation | Epigenomics | Glioblastoma | Temozolomide Response | Standard of Care |
| 2-HG | Metabolomics | Glioma | Diagnosis & Mechanistic | Clinical Validation |
| SeekInCare | Multi-Omics | 27 Cancer Types | Early Detection | Retrospective & Prospective Studies [5] |
Blood-Based Multi-Omics Early Detection
Blood-based multi-omics tests represent a promising approach for non-invasive cancer early detection. The SeekInCare test exemplifies this strategy, incorporating multiple genomic and epigenetic hallmarks including copy number aberration, fragment size, end motif, and oncogenic virus detection via shallow whole-genome sequencing of cell-free DNA, combined with seven protein tumor markers from a single blood draw [5].
This multi-omics approach addresses cancer heterogeneity by targeting multiple biological hallmarks simultaneously, overcoming limitations of single-analyte tests. In retrospective validation involving 617 patients with cancer and 580 individuals without cancer across 27 cancer types, SeekInCare achieved 60.0% sensitivity at 98.3% specificity, with an area under the curve of 0.899 [5]. The test demonstrated increasing sensitivity with disease progression: 37.7% at stage I, 50.4% at stage II, 66.7% at stage III, and 78.1% at stage IV [5]. Prospective evaluation in 1,203 individuals receiving the test as a laboratory-developed test further confirmed its performance with 70.0% sensitivity at 95.2% specificity [5].
The Scientist's Toolkit: Essential Research Solutions
Successful navigation of high-dimensional omics landscapes requires specialized computational tools and resources. The following table details essential solutions for multi-omics biomarker discovery research.
Table 3: Essential Research Solutions for Multi-Omics Biomarker Discovery
| Tool/Resource | Type | Primary Function | Application in Biomarker Discovery |
|---|---|---|---|
| Flexynesis | Deep Learning Toolkit | Bulk multi-omics integration | Drug response prediction, cancer subtype classification, survival modeling [4] |
| TCGA | Data Repository | Curated multi-omics data | Provides validated datasets for model training and validation [1] |
| CPTAC | Data Repository | Proteogenomic data | Correlates genomic alterations with protein expression [1] |
| MOFA+ | Statistical Tool | Bayesian group factor analysis | Identifies latent factors across omics datasets; interpretable integration [3] |
| DriverDBv4 | Database | Multi-omics driver characterization | Integrates genomic, epigenomic, transcriptomic, and proteomic data [1] |
| Genetic Programming | Algorithm | Adaptive feature selection | Optimizes multi-omics integration and identifies robust biomarker panels [3] |
| SeekInCare | Analytical Method | Blood-based multi-omics analysis | Multi-cancer early detection using combined genomic and proteomic markers [5] |
| Tunaxanthin | Tunaxanthin, CAS:12738-95-3, MF:C40H56O2, MW:568.9 g/mol | Chemical Reagent | Bench Chemicals |
| Sinocrassoside C1 | Sinocrassoside C1, MF:C27H30O16, MW:610.5 g/mol | Chemical Reagent | Bench Chemicals |
Advanced Integration Methodologies
Comparative Analysis of Integration Techniques
The selection of an appropriate integration methodology significantly impacts biomarker discovery outcomes. Different computational approaches offer varying strengths in handling data complexity, scalability, and interpretability.
Deep learning methods excel at capturing non-linear relationships and complex interactions between molecular layers. Tools like Flexynesis provide architectures for both single-task and multi-task learning, enabling simultaneous prediction of multiple clinical endpoints such as drug response, cancer subtype, and survival probability [4]. This multi-task approach is particularly valuable in clinical settings where multiple outcome variables may have missing values for some samples [4].
In contrast, classical machine learning methods like Random Forest, Support Vector Machines, and XGBoost sometimes outperform deep learning approaches, especially with limited sample sizes [4]. These methods often provide greater interpretability through feature importance metrics, facilitating biological validation of discovered biomarkers.
Statistical approaches like MOFA+ employ Bayesian group factor analysis to learn shared low-dimensional representations across omics datasets [3]. These models infer latent factors that capture key sources of variability while using sparsity-promoting priors to distinguish shared from modality-specific signals. This explicit modeling of factor structure typically requires less training data than neural networks and offers enhanced interpretability by linking latent factors to specific molecular features [3].
Cross-Omics Relationship Visualization
Multi-Omics Integration Modalities: This diagram illustrates the three primary computational approaches for multi-omics data integration and their pathways to clinical application in biomarker discovery.
The navigation of high-dimensional omics landscapes represents both a formidable challenge and unprecedented opportunity in biomarker discovery. As multi-omics technologies continue to evolve, generating increasingly complex and voluminous datasets, the development of sophisticated computational frameworks becomes increasingly critical. The integration of machine learning and deep learning approaches with multi-omics data has demonstrated significant potential for identifying robust, clinically actionable biomarkers across diverse cancer types and other complex diseases. Future advancements will likely focus on refining integration methodologies, improving model interpretability, and establishing standardized validation frameworks to ensure the translation of computational discoveries into clinically useful tools that enhance patient care and outcomes.
The pursuit of biomarkers—measurable indicators of biological processes, pathological states, or therapeutic responses—faces unprecedented challenges in the era of high-dimensional biology [6]. Conventional statistical methods, including t-tests and ANOVA, which long served as the backbone of biomedical research, are increasingly inadequate for analyzing complex omics datasets [7]. These traditional approaches assume specific data distributions (e.g., normality), struggle with the scale of millions of molecular features, and cannot capture nonlinear relationships inherent in biological systems [7] [8]. The limitations of these methods become critically apparent in biomarker discovery for precision medicine, where researchers must integrate genomic, transcriptomic, proteomic, metabolomic, and clinical data to identify reproducible signatures [8]. This analytical gap has catalyzed the adoption of machine learning (ML) approaches capable of handling data complexity, heterogeneity, and volume that defy conventional parametric methods [7] [9].
Table 1: Comparison Between Traditional Statistical and Machine Learning Approaches
| Analytical Characteristic | Traditional Statistics | Machine Learning Approaches |
|---|---|---|
| Data distribution assumptions | Requires normality assumption | Distribution-free; handles diverse data types |
| Multiple testing correction | Struggles with extreme dimensionality | Embedded regularization and feature selection |
| Nonlinear relationships | Limited capture of complex interactions | Models complex, nonlinear patterns |
| Handling missing data | Often requires complete cases | Multiple imputation and robust handling |
| Integration of multi-omics data | Limited capacity for data fusion | Specialized architectures for multimodal data |
| Model interpretability | High inherent interpretability | Requires explainable AI (XAI) techniques |
Key Limitations of Conventional Statistical Methods
Dimensionality and Multiple Testing Challenges
Conventional statistical methods encounter fundamental limitations when applied to omics-scale data where the number of features (p) vastly exceeds the number of samples (n) [7]. In genome-wide association studies or transcriptomic analyses, researchers must test millions of hypotheses simultaneously, creating a massive multiple testing burden that dramatically reduces statistical power after correction [8]. This p>>n problem renders traditional univariate analyses ineffective for identifying subtle but biologically meaningful signals amidst overwhelming dimensionality [7]. Furthermore, biological heterogeneity introduces additional complexity that conventional methods struggle to accommodate, as they cannot efficiently model the intricate interactions between genetic, environmental, and lifestyle factors that collectively influence disease risk and treatment response [9].
Distributional and Complexity Constraints
Parametric statistical tests rely on assumptions that are frequently violated in omics data [7]. Gene expression data often exhibits skewness, kurtosis, and outliers that violate normality assumptions, while natural biological processes like gene duplication and selection create complex distributions that defy simple parametric description [7]. Additionally, conventional methods cannot adequately capture the nonlinear relationships and higher-order interactions that characterize complex biological systems, potentially missing critical biomarkers that operate in coordinated networks rather than isolation [8]. The limitations extend beyond analytical considerations to practical implementation, as large omics datasets with potentially millions of features present computational challenges that exceed the capabilities of many conventional statistical packages [7].
Machine Learning Approaches in Biomarker Discovery
Supervised Learning for Predictive Biomarker Identification
Supervised machine learning approaches train models on labeled datasets to classify disease status or predict clinical outcomes based on input features [10] [8]. These methods have demonstrated particular utility in biomarker discovery, where they can integrate diverse data types to identify patterns associated with specific phenotypes. Common supervised algorithms include support vector machines (SVMs), which identify optimal hyperplanes for separating classes in high-dimensional spaces; random forests, ensemble methods that aggregate multiple decision trees for robust classification; and gradient boosting algorithms (XGBoost, LightGBM) that iteratively correct previous prediction errors [8] [11]. These approaches have successfully identified diagnostic, prognostic, and predictive biomarkers across oncology, infectious diseases, neurological disorders, and autoimmune conditions [8].
Unsupervised Learning for Novel Disease Endotyping
Unsupervised learning methods explore unlabeled datasets to discover inherent structures or novel subgroupings without predefined outcomes [7] [8]. These approaches are invaluable for endotyping—classifying diseases based on underlying biological mechanisms rather than purely clinical symptoms [7]. Techniques include clustering methods (k-means, hierarchical clustering) that group patients with similar molecular profiles, and dimensionality reduction approaches (PCA, t-SNE, UMAP) that project high-dimensional data into lower-dimensional spaces for visualization and pattern recognition [7]. The concept of disease endotyping was first defined in asthma, where transcriptomics revealed immune/inflammatory endotypes with direct implications for targeted treatment strategies [7]. Unsupervised learning often serves as the initial step in bioinformatics pipelines, enabling quality control, outlier detection, and hypothesis generation before applying supervised approaches [7].
Experimental Protocol: ML-Driven Biomarker Discovery for Large-Artery Atherosclerosis
Study Design and Sample Preparation
This protocol outlines a machine learning workflow for biomarker discovery in large-artery atherosclerosis (LAA), adapted from a published study [11]. The study employs a case-control design with ischemic stroke patients exhibiting extracranial LAA (≥50% diameter stenosis) and normal controls (<50% stenosis confirmed by angiography). Participants are excluded for systemic diseases, cancer, or acute illness at recruitment. Blood samples are collected in sodium citrate tubes and processed within one hour of collection (centrifugation at 3000 rpm for 10 minutes at 4°C). Plasma aliquots are stored at -80°C until metabolomic analysis. The targeted metabolomics approach uses the Absolute IDQ p180 kit (Biocrates Life Sciences) to quantify 194 endogenous metabolites across multiple compound classes, with analysis performed on a Waters Acquity Xevo TQ-S instrument [11].
Table 2: Key Research Reagent Solutions for Metabolomic Biomarker Discovery
| Research Reagent | Manufacturer/Catalog | Function in Experimental Protocol |
|---|---|---|
| Absolute IDQ p180 kit | Biocrates Life Sciences | Targeted quantification of 194 metabolites from multiple compound classes |
| Sodium citrate blood collection tubes | Various suppliers | Preservation of blood samples for plasma metabolomics |
| Waters Acquity Xevo TQ-S | Waters Corporation | Liquid chromatography-tandem mass spectrometry system for metabolite quantification |
| Biocrates MetIDQ software | Biocrates Life Sciences | Data processing and metabolite level determination |
| Pandas Python package | Python Software Foundation | Data preprocessing, manipulation, and analysis |
| scikit-learn Python package | Python Software Foundation | Machine learning algorithms and model implementation |
Data Preprocessing and Machine Learning Workflow
The analytical workflow begins with data preprocessing, including missing data imputation (mean imputation), label encoding for categorical variables, and dataset splitting (80% for training/validation, 20% for external testing) [11]. Three feature sets are evaluated: clinical factors alone, metabolites alone, and combined clinical factors with metabolites. Six machine learning models are implemented and compared: logistic regression (LR), support vector machines (SVM), decision trees, random forests (RF), extreme gradient boosting (XGBoost), and gradient boosting [11]. Feature selection employs recursive feature elimination with cross-validation to identify the most predictive biomarkers. Models are trained with tenfold cross-validation on the training set, with hyperparameter optimization, before final evaluation on the held-out test set. Performance metrics include area under the receiver operating characteristic curve (AUC), accuracy, sensitivity, and specificity [11].
Results and Biomarker Interpretation
In the referenced LAA study, the logistic regression model achieved the best prediction performance with an AUC of 0.92 when incorporating 62 features in the external validation set [11]. The model identified LAA as being predicted by clinical risk factors (body mass index, smoking, medications for diabetes, hypertension, and hyperlipidemia) and metabolites involved in aminoacyl-tRNA biosynthesis and lipid metabolism [11]. Importantly, 27 features were consistently selected across five different models, and when used in the logistic regression model alone, achieved an AUC of 0.93, suggesting their robustness as candidate biomarkers [11]. This demonstrates the effectiveness of combining multiple machine learning algorithms with rigorous feature selection for identifying reproducible biomarker signatures with strong predictive power for complex diseases.
Advanced Applications: AI-Assisted Sensor Systems and Multi-Omics Integration
AI-Enhanced Wearable Sensors for Biomarker Monitoring
Emerging technologies combine wearable biosensors with machine learning for continuous biomarker monitoring. Recent research demonstrates an artificial intelligence-assisted wearable microfluidic colorimetric sensor system (AI-WMCS) for rapid, non-invasive detection of key biomarkers in human tears, including vitamin C, H+ (pH), Ca2+, and proteins [12]. The system comprises a flexible microfluidic patch that collects tears and facilitates colorimetric reactions, coupled with a deep learning neural network-based cloud server data analysis system embedded in a smartphone [12]. A multichannel convolutional recurrent neural network (CNN-GRU) corrects errors caused by varying pH and color temperature, achieving determination coefficients (R²) as high as 0.998 for predicting pH and 0.994 for other biomarkers [12]. This integration of physical sensing technology with machine learning enables accurate, simultaneous detection of multiple biomarkers using minimal sample volume (~20 μL), demonstrating the potential for continuous health monitoring.
Multi-Omics Integration for Comprehensive Biological Insight
Machine learning enables the integration of diverse data types, moving beyond single-omics approaches to multi-omics integration [8]. This comprehensive approach combines genomics, transcriptomics, proteomics, metabolomics, imaging data, and clinical records to provide holistic molecular profiles [8] [9]. Deep learning architectures, particularly convolutional neural networks (CNNs) and recurrent neural networks (RNNs), are well-suited for these complex biomedical data integration tasks [8]. CNNs excel at identifying spatial patterns in imaging data such as histopathology, while RNNs capture temporal dependencies in longitudinal biomarker measurements [8]. The integration of multi-omics data has been shown to improve early Alzheimer's disease diagnosis specificity by 32%, providing a crucial intervention window [9]. This approach facilitates the identification of intricate patterns and interactions among various molecular features that were previously unrecognized using conventional analytical methods.
Implementation Challenges and Future Directions
Critical Implementation Considerations
Despite their promise, machine learning approaches face several challenges in biomarker discovery. Model interpretability remains a significant hurdle, as many advanced algorithms function as "black boxes," making it difficult to elucidate the biological rationale behind specific predictions [8]. This lack of transparency poses practical barriers to clinical adoption, where trust in predictive models is essential [8]. Additionally, rigorous external validation using independent cohorts is necessary to ensure reproducibility and clinical reliability [8]. Data quality issues, including limited sample sizes, noise, batch effects, and biological heterogeneity, can severely impact model performance, leading to overfitting and reduced generalizability [8]. Ethical and regulatory considerations also influence deployment, as biomarkers used for patient stratification or therapeutic decisions must comply with rigorous FDA standards [8].
Emerging Solutions and Methodological Advances
Several emerging approaches address these implementation challenges. Explainable AI (XAI) techniques provide explanations for predictions that can be explored mechanistically before proceeding to validation studies [7]. The rise of explainable AI improves opportunities for true discovery by enhancing model interpretability [7]. Transfer learning approaches leverage knowledge from related domains to improve performance with limited data, while semi-supervised learning effectively utilizes both labeled and unlabeled data [10]. For regulatory compliance, researchers are developing frameworks that maintain model performance while ensuring transparency and fairness [9]. Future directions include expanding biomarker discovery to rare diseases, incorporating dynamic health indicators, strengthening integrative multi-omics approaches, conducting longitudinal cohort studies, and leveraging edge computing solutions for low-resource settings [9]. These advances promise to enhance personalized treatment strategies and improve patient outcomes through more precise biomarker-driven medicine.
The field of biomarker discovery is undergoing a fundamental transformation, moving from correlation-based observations to causation-driven mechanistic insights. Biomarkers, defined as measurable indicators of biological processes, pathological states, or responses to therapeutic interventions, are critical components of precision medicine [8]. They facilitate accurate diagnosis, effective risk stratification, continuous disease monitoring, and personalized treatment decisions, particularly for complex diseases such as cancer, severe asthma, and chronic obstructive pulmonary disease (COPD) [8] [13] [14]. Traditional biomarker discovery approaches have predominantly focused on single molecular features, such as individual genes or proteins identified through genome-wide association studies. However, these conventional methodologies face significant challenges, including limited reproducibility, high false-positive rates, inadequate predictive accuracy, and an inherent inability to capture the multifaceted biological networks that underpin disease mechanisms [8].
The integration of machine learning (ML) and deep learning (DL) with multi-omics technologies represents a paradigm shift in biomarker research. These advanced computational techniques can analyze large, complex biological datasets—including genomics, transcriptomics, proteomics, metabolomics, imaging data, and clinical records—to identify reliable and clinically useful biomarkers [8]. This approach has enabled the emergence of endotype-based classification, which categorizes disease subtypes based on shared molecular mechanisms rather than solely clinical symptoms [14]. The distinction between phenotypes and endotypes is crucial: while phenotypes represent observable clinical characteristics, endotypes reflect the underlying biological or molecular mechanisms that give rise to these observable traits [14]. For instance, in severe asthma, the "frequent exacerbator" phenotype may result from distinct endotypes such as eosinophilic inflammation or infection-dominated mechanisms, each with different therapeutic implications [13].
This Application Note outlines standardized protocols for biomarker discovery and validation, with particular emphasis on causal machine learning approaches that bridge the gap from correlation to causation, ultimately enabling more precise patient stratification and targeted therapeutic interventions.
Biomarker Classification and Clinical Applications
Biomarkers can be broadly categorized based on their clinical applications and biological characteristics. Understanding these classifications is essential for appropriate biomarker selection, validation, and clinical implementation.
Table 1: Biomarker Types and Their Clinical Applications
| Biomarker Type | Definition | Clinical Utility | Representative Examples |
|---|---|---|---|
| Diagnostic | Identifies disease presence or subtype | Disease detection and classification | MicroRNA patterns in colorectal cancer [15] |
| Prognostic | Forecasts disease progression or recurrence | Patient risk stratification | T cell exhaustion markers in cancer immunotherapy [16] |
| Predictive | Estimates treatment efficacy | Therapy selection | PD-L1 expression for immune checkpoint inhibitor response [17] |
| Pharmacodynamic | Measures biological response to treatment | Treatment monitoring and dose optimization | Blood eosinophil counts in COPD for inhaled corticosteroid guidance [14] |
| Functional | Reflects underlying biological mechanisms | Endotype identification and targeted therapy | Biosynthetic gene clusters for antibiotic discovery [8] |
The clinical implementation of biomarkers spans diverse therapeutic areas. In oncology, biomarkers guide immunotherapy approaches, with immune checkpoint inhibitors (ICIs) targeting the PD-1/PD-L1 axis having revolutionized non-small cell lung cancer (NSCLC) treatment [17]. Similarly, in respiratory medicine, biomarkers such as blood eosinophil counts and serum C-reactive protein are progressively being implemented for patient stratification and guidance of targeted therapies for conditions like severe asthma and COPD [13] [14]. The emerging framework of "treatable traits" enhances personalized management by addressing modifiable factors beyond conventional diagnostic boundaries, including comorbidities, psychosocial determinants, and exacerbation triggers [14].
The Correlation Problem in Traditional Biomarker Discovery
Conventional biomarker discovery approaches predominantly rely on correlation-based analyses, which present significant limitations for clinical translation. A systematic review of 90 studies on immune checkpoint inhibitors revealed that despite employing ML or deep learning techniques, none incorporated causal inference [18]. This fundamental methodological flaw has profound implications for the reliability and clinical applicability of identified biomarkers.
Key Limitations of Correlation-Based Approaches
- Confounding Factors: Traditional models often fail to account for key confounding variables. In studies on the gut microbiome and immune checkpoint inhibitors, only 4 out of 27 studies conducted cross-validation, and crucial confounders such as antibiotic use and dietary differences were inadequately controlled [18].
- Immortal Time Bias: Correlation-based analyses can produce dramatically misleading results. For instance, in studying immune-related adverse events (irAEs) and survival, traditional Cox regression yielded a hazard ratio (HR) of 0.37, suggesting a protective effect of irAEs. However, causal ML using target trial emulation revealed a true HR of 1.02—completely overturning the conventional belief [18].
- Spurious Radiomic Associations: Deep learning models based on CT radiomics for predicting ICI responses reported an AUC of ~0.71, but the captured signals largely reflected confounders such as tumor burden and treatment line rather than true drug sensitivity [18].
Statistical Concerns in Biomarker Validation
Biomarker validation must discern associations that occur by chance from those reflecting true biological relationships. Several statistical issues commonly undermine validation studies:
- Within-Subject Correlation: When multiple observations are collected from the same subject, correlated results can inflate type I error rates and produce spurious findings. For example, in a study of microRNA expression in colorectal cancer, 36 miRNAs appeared significantly differentially expressed in unadjusted analyses, but none remained significant after adjustment for within-patient correlation [15].
- Multiplicity: The probability of false discovery increases with each additional test conducted. Biomarker validation studies are particularly sensitive to false positives because the list of potential markers is characteristically extensive [15].
- Selection Bias: Retrospective biomarker studies often suffer from selection bias inherent to observational studies, potentially skewing results and limiting generalizability [15].
Causal Machine Learning: From Correlation to Causation
Causal machine learning represents a paradigm shift in biomarker discovery, integrating causal inference with predictive modeling to distinguish genuine causal relationships from spurious correlations.
Advanced Causal ML Methodologies
Table 2: Causal Machine Learning Approaches for Biomarker Discovery
| Method | Mechanism | Advantages | Application Context |
|---|---|---|---|
| Targeted-BEHRT | Combines transformer architecture with doubly robust estimation | Infers long-term treatment effects from longitudinal data | Temporal treatment response modeling [18] |
| CIMLA | Causal inference using Markov logic networks | Exceptional robustness to confounding in gene regulatory networks | Tumor immune regulation analysis [18] |
| CURE | Leverages large-scale pretraining for treatment effect estimation | ~4% AUC and ~7% precision-recall improvement over traditional methods | Immunotherapy response prediction [18] |
| Causal-stonet | Handles multimodal and incomplete datasets | Effective for big-data immunology research with missing data | Multi-omics integration [18] |
| LiNGAM-based Models | Linear non-Gaussian acyclic model for causal discovery | Directly identifies causative factors (84.84% accuracy with logistic regression) | Mechanistic biomarker identification [18] |
Experimental Protocol: Causal Biomarker Validation Pipeline
Protocol 1: Integrated Workflow for Causal Biomarker Discovery and Validation
Objective: To establish a standardized pipeline for identifying and validating causal biomarkers using multi-omics data and causal machine learning approaches.
Materials:
- Multi-omics data (genomics, transcriptomics, proteomics, metabolomics)
- Clinical data and electronic health records
- High-performance computing infrastructure
- Causal ML software packages (CausalML, DoWhy, EconML)
Procedure:
Study Design and Causal Diagram Specification
- Define precise scientific objectives and scope
- Establish explicit subject inclusion/exclusion criteria
- Specify causal diagrams (Directed Acyclic Graphs) mapping hypothesized relationships between biomarkers, clinical variables, and outcomes
- Identify potential confounders, mediators, and colliders
Data Quality Control and Preprocessing
- Apply data type-specific quality metrics (fastQC for NGS data, arrayQualityMetrics for microarray data, pseudoQC for proteomics data) [19]
- Implement variance-stabilizing transformations for omics data
- Address batch effects using ComBat or similar methods
- Handle missing data through appropriate imputation techniques
Causal Feature Selection
- Apply doubly robust feature selection methods
- Implement causal forest algorithms for heterogeneous treatment effect estimation
- Use propensity score matching for observational data balancing
- Conduct sensitivity analyses for unmeasured confounding
Model Training and Validation
- Partition data into discovery (60%), validation (20%), and test (20%) sets
- Train multiple causal models (Targeted-BEHRT, CIMLA, CURE)
- Implement cross-validation with strict separation between training and validation sets
- Assess model performance using AUC, precision-recall, and causal effect sizes
Biological Validation and Mechanism Elucidation
- Perform experimental validation using perturbation studies (CRISPR, siRNA)
- Conduct pathway enrichment analysis for identified biomarker sets
- Validate in independent cohorts with diverse demographic characteristics
- Assess clinical utility through decision curve analysis
Expected Outcomes: Identification of causally-validated biomarkers with established biological mechanisms and demonstrated clinical utility for patient stratification and treatment selection.
Visualization of Key Workflows and Signaling Pathways
The following diagrams illustrate critical workflows and signaling pathways in causal biomarker discovery, generated using Graphviz DOT language with adherence to the specified color and formatting guidelines.
Diagram 1: Causal Biomarker Discovery Workflow. This diagram outlines the comprehensive pipeline from data collection through clinical implementation of causally-validated biomarkers.
Diagram 2: T-cell Signaling and Checkpoint Inhibition. This diagram illustrates the mechanistic pathway of T-cell exhaustion and immune checkpoint inhibitor function, relevant for predictive biomarkers in cancer immunotherapy.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of causal biomarker discovery requires carefully selected research tools and platforms that enable robust data generation and analysis.
Table 3: Essential Research Reagents and Platforms for Causal Biomarker Discovery
| Category | Specific Tools/Platforms | Function | Key Considerations |
|---|---|---|---|
| Multi-omics Platforms | RNA-seq, LC-MS/MS, NMR spectroscopy | Comprehensive molecular profiling | Platform compatibility, batch effect control [8] [19] |
| Single-cell Technologies | 10X Genomics, CITE-seq, ATAC-seq | Cellular heterogeneity resolution | Sample processing standardization, cell viability [19] |
| Causal ML Software | CausalML, DoWhy, EconML | Causal inference implementation | Algorithmic transparency, validation requirements [18] |
| Data Quality Control | fastQC, arrayQualityMetrics, pseudoQC | Data quality assessment and assurance | Platform-specific metrics, outlier detection [19] |
| Experimental Validation | CRISPR-Cas9, siRNA, organoid models | Functional validation of causal relationships | Physiological relevance, scalability [8] [18] |
| 19-Oxocinobufagin | 19-Oxocinobufagin, MF:C26H32O7, MW:456.5 g/mol | Chemical Reagent | Bench Chemicals |
| Secologanic acid | Secologanic acid, MF:C16H22O10, MW:374.34 g/mol | Chemical Reagent | Bench Chemicals |
Standardized Protocols for Biomarker Validation
Protocol for Multi-omics Data Integration
Objective: To integrate diverse omics datasets for comprehensive biomarker discovery while accounting for technical and biological variability.
Procedure:
Data Normalization
- Apply variance-stabilizing transformation to RNA-seq data
- Perform quantile normalization for proteomics data
- Use probabilistic quotient normalization for metabolomics data
Multi-omics Integration
- Implement early integration using sparse canonical correlation analysis
- Apply intermediate integration via multimodal neural networks
- Conduct late integration through stacked generalization
Causal Network Construction
- Build causal networks using LiNGAM-based approaches
- Validate edge directions through perturbation data
- Annotate networks with functional genomic information
Quality Control Metrics: Assess integration success through cross-omics consistency checks and biological coherence evaluation.
Protocol for Clinical Biomarker Validation
Objective: To validate putative biomarkers in independent clinical cohorts using causal inference approaches.
Procedure:
Cohort Selection
- Define inclusion/exclusion criteria a priori
- Match cases and controls for potential confounders
- Ensure adequate sample size through power calculations
Measurement Standardization
- Establish standard operating procedures for biomarker quantification
- Implement blinding procedures to prevent measurement bias
- Include quality control samples in each batch
Causal Effect Estimation
- Apply propensity score methods for treatment effect estimation
- Use instrumental variable analysis when appropriate
- Conduct sensitivity analyses for unmeasured confounding
Clinical Utility Assessment
- Evaluate reclassification metrics (NRI, IDI)
- Perform decision curve analysis
- Assess cost-effectiveness where applicable
The transition from correlation to causation represents a fundamental evolution in biomarker discovery. By integrating causal machine learning with multi-omics technologies and rigorous validation frameworks, researchers can identify biomarkers with genuine biological mechanisms and enhanced clinical utility. The implementation of standardized protocols, such as those outlined in this Application Note, will accelerate the discovery of causal biomarkers and their translation into clinical practice.
Future directions in causal biomarker discovery include the development of perturbation cell atlases, federated causal learning frameworks that preserve data privacy, and dynamic biomarker monitoring systems that adapt to disease progression and treatment responses. These advancements, coupled with ongoing improvements in causal inference methodologies, promise to transform precision medicine by enabling truly mechanistic patient stratification and targeted therapeutic interventions.
As the field progresses, emphasis must remain on rigorous validation, biological plausibility, and clinical relevance to ensure that causal biomarkers fulfill their promise of improving patient outcomes across diverse disease contexts.
The advent of large-scale public genomic data repositories has revolutionized the field of biomedical research, providing an unprecedented resource for machine learning (ML)-driven biomarker discovery. For researchers focused on protein and immunology (POI) biomarkers, resources like The Cancer Genome Atlas (TCGA), the Encyclopedia of DNA Elements (ENCODE), and the Genome Aggregation Database (gnomAD) offer complementary data types that can be integrated to uncover novel diagnostic, prognostic, and therapeutic targets. These repositories provide systematically generated, multi-omics data at a scale that enables the training of robust ML models capable of identifying subtle patterns indicative of disease states, treatment responses, and biological mechanisms. This article provides detailed application notes and protocols for effectively leveraging these resources within the context of ML-powered POI biomarker research, facilitating their use by scientists and drug development professionals.
A strategic understanding of the scope, content, and strengths of each repository is fundamental to designing effective biomarker discovery pipelines. The following table summarizes the core characteristics and quantitative data available from each resource.
Table 1: Core Characteristics of Major Public Genomic Data Repositories
| Repository | Primary Focus | Key Data Types | Data Volume (as of 2024/2025) | Primary Applications in Biomarker Discovery |
|---|---|---|---|---|
| TCGA [20] [21] | Cancer Genomics | RNA-seq, WGS, WES, DNA methylation, CNVs, clinical data | >20,000 cases across 33 cancer types; Multi-modal data per patient | Pan-cancer biomarker identification, prognostic model development, cancer subtype classification |
| ENCODE [22] [23] | Functional Genomics | ChIP-seq, ATAC-seq, RNA-seq, Hi-C, CRISPR screens | ~106,000 released datasets; >23,000 functional genomics experiments [22] | Defining regulatory elements, understanding gene regulation mechanisms, prioritizing non-coding variants |
| gnomAD [24] [25] | Population Genetics & Variation | Allele frequencies, constraint metrics, variant co-occurrence, haplotype data | v4: 807,162 individuals; v3.1: 76,156 whole genomes [24] [25] | Filtering benign variants, assessing population-specific allele frequency, estimating genetic prevalence |
Experimental Protocols and Data Access
Protocol 1: Downloading and Preprocessing Multi-omics Data from TCGA
This protocol outlines a streamlined pipeline for downloading TCGA data and reorganizing it for patient-level, multi-omics analysis, which is crucial for building integrated ML models for biomarker discovery.
I. Prerequisites and Setup
- Software Installation: Create a Conda environment with the required packages (Python 3.11.8, Snakemake 7.32.4, pandas, gdc-client) using the provided
TCGADownloadHelper_env.yamlfile [20]. - Folder Structure: Establish a local analysis directory with subfolders:
sample_sheets/manifests,sample_sheets/sample_sheets_prior, andsample_sheets/clinical_data[20].
II. Data Selection and Download
- Access the GDC Data Portal: Navigate to the GDC Data Portal.
- Build a Cart: Use the faceted search to select files of interest (e.g., RNA-seq counts, WES VCFs, clinical data) for a specific cohort (e.g., TCGA-LUAD, TCGA-COAD) [20].
- Export Metadata: Download the
manifest fileandsample sheetfrom the cart, saving them in themanifestsandsample_sheets_priorfolders, respectively. Export the clinical metadata to theclinical_datafolder. - Download Raw Data: Use the GDC Data Transfer Tool with the manifest file to download the selected files. For restricted data, use an NIH access token [20].
III. Data Reorganization and Preprocessing
- Execute Renaming Pipeline: Run the
TCGADownloadHelperSnakemake pipeline or Jupyter Notebook to map the opaque GDC file names to human-readable Case IDs using the sample sheet [20]. - Integrate Clinical Data: Merge the reorganized molecular data files with the clinical metadata using the Case ID as the key.
- Data Formatting for ML: Convert the processed data into a matrix format (e.g., features × samples) suitable for ML input. Perform standard preprocessing steps such as log-transformation for RNA-seq counts, imputation of missing values, and normalization.
Protocol 2: Interrogating Functional Elements with ENCODE Data
This protocol describes how to access and utilize ENCODE data to inform on the potential functional impact of genomic regions identified in biomarker studies.
I. Portal Navigation and Data Selection
- Access the ENCODE Portal: Navigate to https://www.encodeproject.org [22] [23].
- Faceted Search: Use the search interface with predefined facets (e.g.,
Assay type,Biosample,Target of assay) to find relevant datasets. For POI research, key assays include Histone ChIP-seq (H3K27ac for enhancers), ATAC-seq (accessibility), and RNA-seq [22]. - Review Uniform Processing Pipelines: Prioritize datasets that have been processed through ENCODE's uniform pipelines to ensure consistency and quality [22]. Check the File Association Graph on experiment pages for quality metrics [22].
II. Data Access and Visualization
- File Download: Add selected files to the cart. Use the cart's enhanced interface to filter by file properties (e.g.,
file type=bigWigfor coverage tracks) and download via the browser or programmatically using the REST API [22] [23]. - Genome Browser Visualization: Visualize
bigWigorBEDfiles directly in the integrated Valis Genome Browser or the Encyclopaedia Browser to see annotations in a genomic context [22].
III. Integration with Biomarker Lists
- Overlap Analysis: Cross-reference a list of genomic coordinates from your biomarker study (e.g., non-coding variants, differentially accessible regions) with ENCODE annotations to predict functional relevance (e.g., whether a variant falls in an active enhancer in a relevant cell type).
Protocol 3: Annotating and Filtering Variants with gnomAD
This protocol is essential for assessing the population frequency and constraint of genetic variants, a critical step in prioritizing pathogenic biomarkers.
I. Browser-Based Variant Interrogation
- Access the gnomAD Browser: Navigate to https://gnomad.broadinstitute.org.
- Gene-Centric Query: Enter a gene symbol (e.g.,
APOL1) to view a constraint metric summary (pLoF and missense Z-scores) and a table of all variants within the gene [24]. - Variant-Specific Query: Search for a specific variant (e.g.,
17-7043011-C-T) to view its allele frequency across global populations and sub-populations [25]. - Utilize Advanced Features:
- Local Ancestry Inference (LAI): For admixed populations (African/African American, Admixed American), check the "Local Ancestry" tab on the variant page to view ancestry-specific frequencies (LAI-AFR, LAI-EUR, LAI-AMR), which can reveal masked high-frequency alleles [25].
- Variant Co-occurrence: On gene pages for v2 data, check the variant co-occurrence table to see if pairs of rare variants are observed in trans, which can aid in interpreting recessive conditions [24].
II. Programmatic Data Access for ML
- Download Bulk Data: Access the complete VCF files or Hail Tables for gnomAD data from the downloads page [26].
- Annotate Variant Lists: Integrate gnomAD allele frequencies and constraint metrics into your variant annotation pipeline using tools like
bcftoolsor Hail. Filter out common variants (e.g., AF > 0.1%) in any population as likely benign.
Integration for Machine Learning Biomarker Discovery
The power of these repositories is magnified when their data is integrated into a unified ML workflow for POI biomarker discovery.
Workflow Diagram: Integrated ML Pipeline for Biomarker Discovery
The following diagram illustrates the logical flow of data from the repositories into a cohesive machine learning pipeline.
Application Note: A Case Study in Colon Adenocarcinoma
Recent research exemplifies the power of integrating TCGA data with ML for biomarker discovery. A 2025 study identified a taurine metabolism-related gene signature for prognostic stratification in colon adenocarcinoma (COAD) using TCGA data [27]. The workflow involved:
- Data Sourcing: RNA-seq and clinical data for the TCGA-COAD cohort were sourced from the GDC portal [27].
- Unsupervised Clustering: Non-negative Matrix Factorization (NMF) was applied to genes with prognostic significance, identifying two distinct molecular subtypes (C1 and C2) associated with taurine metabolism [27].
- Differential Analysis & Functional Enrichment: Analysis of 199 differentially expressed genes (DEGs) between clusters revealed enrichment in extracellular matrix organization and immune activity, suggesting distinct tumor microenvironments [27].
- Predictive Model Building: Using LASSO and multivariate Cox regression, a prognostic model based on nine key genes (
LEP,SERPINA1,ENO2,HSPA1A,GSR,GABRD,TERT,NOTCH3, andMYB) was constructed. The model demonstrated predictive efficacy with AUCs of 0.698, 0.699, and 0.73 for 1-, 3-, and 5-year survival, respectively [27].
This end-to-end analysis demonstrates a reproducible blueprint for using TCGA to derive a clinically actionable biomarker signature.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key computational tools and resources essential for executing the protocols described in this article.
Table 2: Essential Research Reagent Solutions for Genomic Data Analysis
| Tool/Resource Name | Type | Primary Function | Application in Workflow |
|---|---|---|---|
| TCGADownloadHelper [20] | Pipeline (Snakemake/Jupyter) | Simplifies TCGA data download and file renaming | Protocol 1: Automates the mapping of GDC file IDs to human-readable Case IDs, crucial for multi-modal data integration. |
| GDC Data Transfer Tool [20] | Command-line Tool | Bulk download of data from the GDC Portal | Protocol 1: Enables efficient, reliable download of large TCGA datasets specified by a manifest file. |
| ENCODE REST API [23] | Application Programming Interface | Programmatic access to ENCODE metadata and files | Protocol 2: Allows for automated, scripted querying and retrieval of ENCODE data, facilitating reproducible analysis. |
| Valis/Encyclopaedia Browser [22] | Genome Browser | Visualization of genomic data tracks | Protocol 2: Provides an intuitive visual context for ENCODE functional genomics data within the genome. |
| gnomAD Browser [24] | Web Application | Interactive exploration of gnomAD data | Protocol 3: Enables rapid, user-friendly lookup of variant frequencies, constraint scores, and local ancestry data. |
| Hail [26] | Library/Framework (for Python) | Scalable genomic data analysis | Protocol 3: Used for large-scale handling and analysis of gnomAD VCFs or Hail Tables for population-scale analysis. |
| 23-Hydroxylongispinogenin | 23-Hydroxylongispinogenin, CAS:42483-24-9, MF:C30H50O4, MW:474.7 g/mol | Chemical Reagent | Bench Chemicals |
| Astragaloside VI | Astragaloside VI, MF:C47H78O19, MW:947.1 g/mol | Chemical Reagent | Bench Chemicals |
The strategic integration of TCGA, ENCODE, and gnomAD provides a formidable foundation for machine learning-driven biomarker discovery. TCGA offers the disease-specific, multi-omics, and clinical context; ENCODE provides the functional genomic annotation to interpret findings mechanistically; and gnomAD delivers the population genetics framework to prioritize rare, potentially pathogenic variants. By following the detailed protocols and workflows outlined in this article, researchers can systematically navigate these complex resources, extract biologically and clinically relevant signals, and build robust models to identify the next generation of protein and immunology biomarkers. The continuous updates and increasing scale of these repositories promise to further enhance their utility in the years to come.
The ML Toolbox: Practical Algorithms and Real-World Applications in Biomarker Development
The discovery of robust and reproducible biomarkers has been revolutionized by sensitive omics platforms that enable measurement of biological molecules at an unprecedented scale [7]. Machine learning (ML) has emerged as a critical tool for analyzing these complex datasets, moving beyond traditional statistical methods that struggle with the scale, multiple testing, and non-linear relationships inherent in high-dimensional biological data [7]. Biomarkers—measurable indicators of biological processes, pathological states, or responses to therapeutic interventions—are crucial for disease diagnosis, prognosis, personalized treatment decisions, and monitoring treatment efficacy in precision medicine [8] [28]. The choice between supervised and unsupervised learning approaches represents a fundamental decision point in biomarker discovery pipelines, with significant implications for study design, analytical methodology, and clinical applicability.
Core Concepts: Supervised vs. Unsupervised Learning
Fundamental Differences and Applications
The primary distinction between supervised and unsupervised learning lies in the use of labeled datasets [29]. Supervised learning uses labeled input and output data to train algorithms for classifying data or predicting outcomes, while unsupervised learning algorithms analyze and cluster unlabeled data sets without human intervention to discover hidden patterns [29].
| Characteristic | Supervised Learning | Unsupervised Learning |
|---|---|---|
| Data Requirements | Labeled datasets with known outcomes [29] | Unlabeled datasets without predefined outcomes [29] |
| Primary Goals | Predict outcomes for new data; classification and regression [29] | Discover inherent structures; clustering, association, dimensionality reduction [29] |
| Common Algorithms | Logistic Regression, Support Vector Machines, Random Forest, XGBoost [8] [11] | K-means clustering, Principal Component Analysis, hierarchical clustering [8] [30] |
| Model Complexity | Relatively simple; calculated using programs like R or Python [29] | Computationally complex; requires powerful tools for large unclassified data [29] |
| Key Applications in Biomarker Research | Disease classification, outcome prediction, treatment response [11] | Patient stratification, disease subtyping, novel biomarker identification [31] [30] |
| Output Validation | Direct accuracy measurement against known labels [29] | Requires human intervention to validate output variables [29] |
Experimental Workflows and Signaling Pathways
The methodological pipeline for biomarker discovery differs significantly between supervised and unsupervised approaches, impacting everything from initial study design to final validation.
Supervised Learning Approaches in Biomarker Discovery
Methodological Framework and Protocols
Supervised learning involves training a model on a labeled dataset where both input data (e.g., gene expression or proteomic measurements) and output data (e.g., disease diagnosis or prognosis) are known [7]. The goal is to learn a mapping from inputs to outputs so the model can make predictions on new, unseen data [7]. This approach is particularly valuable when researchers have well-defined clinical outcomes or diagnostic categories.
Experimental Protocol: Supervised Biomarker Signature Development
Study Design and Cohort Selection
- Precisely define primary and secondary biomedical outcomes
- Establish clear subject inclusion/exclusion criteria
- Perform sample size determination and power analysis
- Implement sample selection and matching methods for confounder matching between cases and controls [19]
Data Collection and Preprocessing
- Collect multimodal data (genomics, transcriptomics, proteomics, metabolomics, clinical variables)
- Apply data type-specific quality control metrics (e.g., fastQC for NGS data, arrayQualityMetrics for microarray data) [19]
- Handle missing values (removal or imputation for features with <30% missing values)
- Remove features with zero or small variance
- Apply appropriate transformations (e.g., Box-Cox, variance stabilizing transformations) [19]
Feature Selection and Model Training
- Apply feature selection methods (LASSO, recursive feature elimination) to identify informative biomarkers [11]
- Split data into training/validation (80%) and testing (20%) sets [11]
- Implement multiple algorithms (Logistic Regression, SVM, Random Forest, XGBoost) with cross-validation [11]
- Tune hyperparameters using grid search or Bayesian optimization
Model Validation and Biomarker Confirmation
Case Study: Predicting Large-Artery Atherosclerosis
A study on large-artery atherosclerosis (LAA) demonstrated the effective application of supervised learning for biomarker discovery [11]. Researchers integrated clinical factors and metabolite profiles using six machine learning models, with logistic regression exhibiting the best prediction performance (AUC=0.92 in external validation) [11]. The study identified that combining clinical risk factors (body mass index, smoking, medications for diabetes, hypertension, hyperlipidemia) with metabolites involved in aminoacyl-tRNA biosynthesis and lipid metabolism provided the most stable predictive model [11]. Notably, 27 features were present across five different models, and using only these shared features in the logistic regression model achieved an AUC of 0.93, highlighting their importance as candidate biomarkers [11].
Unsupervised Learning Approaches in Biomarker Discovery
Methodological Framework and Protocols
Unsupervised learning involves training a model on an unlabeled dataset to uncover patterns or relationships without any prior knowledge or assumptions about the output [7]. This approach is particularly valuable for exploring complex, multimodal datasets without predefined categories or for identifying novel disease subtypes.
Experimental Protocol: Unsupervised Biomarker Discovery
Data Collection and Multimodal Integration
- Collect diverse data modalities (metabolome, microbiome, genetics, advanced imaging, clinical data) [31]
- Perform data transformation to address non-Gaussian distributions (e.g., rank-based inverse normal transformation) [31]
- Correct for covariates (age, sex, ancestry) using multiple linear regression [31]
Cross-Modality Association Network Construction
Module Identification and Biomarker Extraction
Patient Stratification and Clinical Validation
Case Study: Novel Signatures from Multimodal Data
A comprehensive study analyzing 1385 data features from 1253 individuals demonstrated the power of unsupervised learning for identifying novel biomarker signatures [31]. Researchers utilized a combination of unsupervised machine learning methods including cross-modality associations, network analysis, and patient stratification. The approach identified cardiometabolic biomarkers beyond standard clinical measures, with stratification based on these signatures identifying distinct subsets of individuals with similar health statuses [31]. Notably, subset membership was a better predictor for diabetes than established clinical biomarkers such as glucose, insulin resistance, and body mass index [31]. Specific novel biomarkers identified included 1-stearoyl-2-dihomo-linolenoyl-GPC and 1-(1-enyl-palmitoyl)-2-oleoyl-GPC for diabetes, and cinnamoylglycine as a potential biomarker for both gut microbiome health and lean mass percentage [31].
Integrated and Advanced Approaches
Hybrid Methodologies and Causal Inference
Advanced biomarker discovery increasingly integrates both supervised and unsupervised approaches with causal inference methods to enhance biomarker validation and biological interpretation.
Addressing Bias and Enhancing Generalizability
An important consideration in biomarker discovery is addressing potential biases in machine learning algorithms. Recent research has highlighted sex-based bias in ML models, showing that stratifying data according to sex improves prediction accuracy for clinical biomarkers including triglycerides, BMI, waist circumference, and systolic blood pressure [28]. For predictions within 10% error, the top performing models for waist circumference, albuminuria, BMI, blood glucose and systolic blood pressure showed males scoring higher than females, highlighting the importance of considering biological sex in biomarker discovery pipelines [28].
The Scientist's Toolkit: Essential Research Reagents and Solutions
| Category | Specific Tools/Reagents | Function in Biomarker Discovery |
|---|---|---|
| Omics Profiling Platforms | Absolute IDQ p180 kit (Biocrates) [11] | Targeted metabolomics analysis quantifying 194 endogenous metabolites from 5 compound classes |
| Biobanking Supplies | Sodium citrate tubes, polypropylene tubes [11] | Standardized blood collection and plasma storage at -80°C for reproducible metabolomic measurements |
| Quality Control Software | fastQC/FQC [19], arrayQualityMetrics [19], pseudoQC, MeTaQuaC, Normalyzer [19] | Data type-specific quality metrics for NGS, microarray, proteomics, and metabolomics data |
| Data Processing Tools | Pandas, NumPy, scikit-learn [11] | Python-based data preprocessing, feature selection, and machine learning implementation |
| Visualization Packages | Matplotlib, Seaborn [11] | Creation of publication-quality figures including PCA plots, t-SNE visualizations, and correlation matrices |
| Statistical Analysis Tools | SciPy, TableOne [11] | Statistical testing and cohort characterization for clinical and biomarker data |
| Network Analysis Software | Graphical Lasso implementation [31] | Construction of sparse Markov networks for identifying key biomarkers within functional modules |
| Validation Resources | Independent longitudinal cohorts [31] | Confirmation of biomarker stability and predictive performance over time |
| 1,1,1,1-Kestohexaose | 1,1,1,1-Kestohexaose, MF:C36H62O31, MW:990.9 g/mol | Chemical Reagent |
| Chrysogine | 2-(1-Hydroxyethyl)-4(3H)-quinazolinone | High-purity 2-(1-Hydroxyethyl)-4(3H)-quinazolinone for research. Explore its applications in medicinal chemistry and drug discovery. For Research Use Only. Not for human use. |
The choice between supervised and unsupervised learning in biomarker discovery depends on multiple factors including research objectives, data characteristics, and available clinical annotations. Supervised learning approaches are ideal when researchers have well-defined clinical endpoints or diagnostic categories and aim to develop predictive models for classification or outcome prediction [29] [11]. In contrast, unsupervised methods are particularly valuable for exploratory analysis of complex multimodal datasets, identification of novel disease subtypes or endotypes, and discovery of previously unrecognized biomarker patterns [31] [30].
Emerging trends in the field include the integration of both approaches in hybrid pipelines, where unsupervised learning identifies novel patient subgroups or biomarker patterns that subsequently inform supervised model development [32]. Additionally, the incorporation of causal inference methods like Mendelian randomization strengthens the biological validation of discovered biomarkers [32]. As multimodal data collection becomes increasingly comprehensive and complex, the strategic selection and integration of machine learning approaches will continue to drive advances in biomarker discovery, ultimately enhancing personalized medicine through improved diagnosis, prognosis, and treatment selection.
Application Notes
In the field of machine learning-driven biomarker discovery, the selection of an appropriate algorithm is critical for identifying robust, biologically relevant signatures from high-dimensional data. This document outlines the practical application, performance, and protocols for four core algorithms: Logistic Regression (LR), Random Forest (RF), eXtreme Gradient Boosting (XGBoost), and Support Vector Machine (SVM). These algorithms facilitate the transition from vast omics datasets to a concise set of potential biomarkers for diagnostic, prognostic, or predictive purposes.
The comparative performance of these algorithms, as evidenced by recent research, is summarized in the table below.
Table 1: Comparative Performance of Core Algorithms in Biomarker Discovery
| Algorithm | Reported AUC | Key Strengths | Common Feature Selection Methods | Exemplary Application Context |
|---|---|---|---|---|
| Logistic Regression (LR) | 0.92–0.93 [11] | Highly interpretable, provides odds ratios, less prone to overfitting with regularization. | Recursive Feature Elimination (RFE), Bagged Logistic Regression (BLESS) [33] | Predicting Large-Artery Atherosclerosis (LAA) from clinical and metabolomic data [11]. |
| Random Forest (RF) | 0.809–0.91 [11] [34] | Robust to outliers and non-linear data, intrinsic variable importance ranking. | Boruta, Permutation Importance, Recursive Feature Elimination (RFE) [34] | Classifying carotid artery plaques; stable biomarker identification framework [11] [34]. |
| XGBoost | >0.90 [35] | High accuracy, handles missing data, effective for complex interactions. | Embedded feature importance, Multi-objective Evolutionary Algorithms (e.g., MEvA-X) [36] | Ovarian cancer diagnosis; precision nutrition and weight loss prediction [36] [35]. |
| Support Vector Machine (SVM) | 0.98 (Accuracy) [37] | Effective in high-dimensional spaces, versatile kernels for non-linear separation. | RFE (SVM-RFE), Network-constrained regularization (CNet-SVM) [37] [38] | Identifying racial disparity biomarkers in Triple-Negative Breast Cancer (TNBC) [37]. |
Experimental Protocols
Protocol 1: Biomarker Discovery Using Logistic Regression with RFE
Application: This protocol is ideal for creating interpretable models where understanding the specific contribution of each biomarker is crucial. It has been successfully used to predict Large-Artery Atherosclerosis (LAA) by integrating clinical factors and metabolite profiles [11].
- Step 1: Data Preprocessing. Handle missing values using mean imputation. Encode categorical variables (e.g., smoking status, medication use) as dummy variables. Split the dataset into training/validation (80%) and external testing (20%) sets [11].
- Step 2: Feature Selection with RFE. Use Recursive Feature Elimination with Cross-Validation (RFECV) on the training set. The LR model is trained, and the least important features are pruned iteratively. Cross-validation determines the optimal number of features.
- Step 3: Model Training. Train a final Logistic Regression model on the entire training set using the optimal features identified in Step 2. Use regularization (e.g., L1 or L2) to enhance model generalization.
- Step 4: Model Evaluation. Validate the model on the held-out external test set. Evaluate performance using Area Under the ROC Curve (AUC), with an AUC >0.9 indicating an excellent diagnostic biomarker [39]. Calculate sensitivity, specificity, and accuracy.
Protocol 2: Stable Biomarker Identification with Random Forest and Boruta
Application: This protocol is suited for discovering stable and robust biomarkers from high-dimensional omics data (transcriptomics, metabolomics) where complex, non-linear relationships are suspected. A power analysis framework can be integrated for future study design [34].
- Step 1: Nested Cross-Validation Setup. Implement a nested cross-validation to ensure unbiased performance estimation and feature selection. The outer loop is for testing (e.g., 75:25 split), and the inner loop is for hyperparameter tuning and feature selection on the training fold [34].
- Step 2: Stable Feature Selection with Boruta. Within the inner loop, run the Boruta algorithm for multiple iterations (e.g., 100). Boruta creates "shadow" features by shuffling real data and compares their importance to real features to decide significance. Features selected in >90% of iterations are considered high-stringency (HS) stable biomarkers [34].
- Step 3: Model Training and Power Analysis. Train a final Random Forest model using the stable features. The out-of-bag (OOB) error is used for internal validation. Use the identified stable features and their effect sizes to perform a power analysis for estimating sample sizes required for future validation studies [34].
Protocol 3: Advanced Biomarker Optimization with XGBoost and Evolutionary Algorithms
Application: This protocol is designed for highly complex datasets with severe class imbalance and a very low samples-to-features ratio. It is effective for finding a small set of non-redundant biomarkers while optimizing multiple, conflicting objectives (e.g., high accuracy and model simplicity) [36].
- Step 1: Data Preparation and Imbalance Handling. Prepare the dataset (e.g., gene expression, clinical questionnaires). Address class imbalance using techniques such as SMOTE or assigning higher weights to the minority class during model training.
- Step 2: Multi-Objective Evolutionary Optimization. Employ a framework like MEvA-X, which combines a multiobjective Evolutionary Algorithm (EA) with XGBoost. The EA simultaneously optimizes XGBoost's hyperparameters and performs feature selection. It evolves a population of models towards a "Pareto frontier" that balances objectives like AUC and the number of features [36].
- Step 3: Solution Selection and Validation. From the set of Pareto-optimal solutions, select one or multiple models based on the desired trade-off between performance and complexity. Validate the chosen model(s) on a hold-out test set, reporting metrics like AUC and balanced accuracy.
Protocol 4: Network-Constrained Biomarker Discovery with SVM-RFE
Application: This protocol goes beyond identifying individual biomarkers to discover functionally connected sub-networks of biomarkers. It is particularly powerful for elucidating the synergistic role of genes in complex diseases like cancer [38].
- Step 1: Integration of Prior Biological Knowledge. Collect a prior gene interaction network from databases like STRING or BioGRID. Integrate this network with the gene expression dataset.
- Step 2: Network-Constrained Feature Elimination. Implement the Connected Network-constrained SVM (CNet-SVM). The SVM optimization includes a penalty term that encourages the selection of features that are connected in the prior network. The Recursive Feature Elimination (RFE) process is guided by this constraint, progressively eliminating genes that are isolated from the main connected component [38].
- Step 3: Validation of Network Biomarkers. Validate the classification performance of the selected connected biomarker network on independent data. Perform functional enrichment analysis (e.g., GO, KEGG) on the biomarker network to confirm its biological relevance to the disease pathology.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Materials for Biomarker Discovery
| Reagent/Material | Function in Research | Specific Example |
|---|---|---|
| Targeted Metabolomics Kit (Absolute IDQ p180) | Quantifies 194 endogenous metabolites from 5 compound classes (e.g., amino acids, lipids) in plasma/serum for biomarker discovery [11]. | Used to identify metabolites involved in aminoacyl-tRNA biosynthesis and lipid metabolism as predictors for Large-Artery Atherosclerosis [11]. |
| RNA Sequencing (RNA-seq) Data | Provides a comprehensive profile of the whole transcriptome to identify differentially expressed genes (DEGs) as potential biomarkers [37]. | Used with SVM-RFE to identify 24 genes that classify racial disparities in Triple-Negative Breast Cancer with 98% accuracy [37]. |
| Gene Interaction Network Databases | Provide prior biological knowledge on protein-protein interactions for network-constrained biomarker discovery [38]. | Databases like STRING or MalaCards are used in CNet-SVM to ensure selected biomarker genes form a connected functional network [38]. |
| PLINK Software | A whole-genome association analysis toolset used for rigorous quality control (QC) of genomic data before analysis [33]. | Used for QC of GWAS data, including filtering SNPs for missingness, minor allele frequency, and Hardy-Weinberg equilibrium [33]. |
| Clinical Data (e.g., CA-125, HE4) | Established clinical biomarkers used as covariates or to enhance model performance when combined with novel omics data [35]. | Integrated into ML models (e.g., XGBoost) to improve the diagnosis of ovarian cancer, achieving AUCs >0.90 [35]. |
| Buxifoliadine H | Buxifoliadine H, CAS:263007-72-3, MF:C16H15NO6, MW:317.297 | Chemical Reagent |
| Bletilol B | Bletilol B, MF:C27H26O7, MW:462.5 g/mol | Chemical Reagent |
Within the paradigm of precision medicine, the discovery of robust biomarkers is critical for early disease detection, accurate prognosis, and personalized treatment strategies. Large-artery atherosclerosis (LAA) is a leading cause of ischemic stroke, characterized by the formation of atherosclerotic plaques in major arteries [11]. Current diagnostic standards, including ultrasound, computed tomography, and magnetic resonance angiography, are often costly, time-consuming, and require specialized expertise, highlighting an urgent clinical need for more accessible diagnostic methods [11]. This case study explores the integration of clinical data and plasma metabolomic profiles with machine learning (ML) to identify biomarker signatures for LAA prediction. We detail the experimental workflow, analytical protocols, and key findings, providing a framework for ML-driven biomarker discovery in cardiovascular disease.
The application of machine learning to integrated clinical and metabolomic data has yielded highly predictive models for LAA. The core findings and performance metrics are summarized below.
Table 1: Performance of Machine Learning Models in Predicting LAA
| Model | Input Features | Validation Set | AUC | Key Strengths |
|---|---|---|---|---|
| Logistic Regression (LR) | 62 Clinical + Metabolomic Features | External | 0.92 [11] | Best overall performance; high interpretability |
| Logistic Regression (LR) | 27 Shared Features | External | 0.93 [11] | High reliability using cross-model features |
| Random Forest (RF) | Clinical + Metabolomic Features | Internal | 0.914 [11] | Robustness against overfitting |
| Support Vector Machine (SVM) | Clinical + Metabolomic Features | Internal | N/R | Effective for high-dimensional data [11] |
Table 2: Identified Biomarker Panels for Atherosclerosis
| Biomarker Category | Specific Biomarkers | Associated Biological Pathways | Clinical Significance |
|---|---|---|---|
| Clinical Risk Factors | Body Mass Index (BMI), Smoking Status, Medications for diabetes/hypertension/hyperlipidemia [11] | N/A | Confirms established risk profiles; provides model stability [11] |
| Metabolites (LAA) | Aminoacyl-tRNA biosynthesis intermediates, Lipid metabolism intermediates [11] | Aminoacyl-tRNA biosynthesis, Lipid Metabolism [11] | Reflects underlying metabolic dysfunction in LAA |
| Metabolites (Coronary AS) | Cholesteryl sulphate, TMAO, ADMA, LPC18:2, Tryptophan, Azelaic acid [40] | Cholesterol metabolism, Gut microbiome-derived metabolism [40] | Panel for diagnosing and assessing severity of coronary atherosclerosis [40] |
| Proteomic (AIS from LAA) | RNASE4, HBA1, ATF6B [41] | Cholesterol metabolism, Complement/coagulation cascades [41] | 3-protein panel for differentiating acute stroke from stable atherosclerosis [41] |
Experimental Protocols
Participant Recruitment and Sample Collection
Objective: To recruit a well-characterized cohort of LAA patients and matched healthy controls.
- Inclusion Criteria (LAA Patients): ischemic stroke patients with extracranial LAA exhibiting ≥50% diameter stenosis confirmed by cerebral angiography; stable neurological condition during blood collection [11].
- Inclusion Criteria (Healthy Controls): no history of stroke or coronary artery disease; no acute illness [11].
- Exclusion Criteria: systemic diseases (e.g., lupus, cirrhosis), cancer, recent use of probiotics or antibiotics [11] [40].
- Sample Collection: Venous blood is drawn into sodium citrate tubes and processed within one hour. Centrifugation is performed at 3,000 rpm for 10 minutes at 4°C to isolate plasma. Aliquots are stored at -80°C until analysis [11].
Metabolomic Profiling Using LC-MS
Objective: To quantitatively profile endogenous metabolites in plasma samples.
- Technology: Targeted metabolomics using the Absolute IDQ p180 kit (Biocrates Life Sciences AG), quantifying 194 metabolites from multiple compound classes [11].
- Instrumentation: Waters Acquity Xevo TQ-S mass spectrometer coupled with UPLC [11].
- Data Processing: Metabolite concentration data is extracted using Biocrates MetIDQ software [11]. Data preprocessing includes handling missing values via mean imputation and scaling [11].
Machine Learning Workflow for Biomarker Discovery
Objective: To build and validate predictive models for LAA using integrated clinical and metabolomic data.
- Data Splitting: The dataset is split into 80% for model training/validation (using tenfold cross-validation) and 20% as an external test set [11].
- Feature Selection: Recursive Feature Elimination with Cross-Validation (RFECV) is applied to identify the most predictive features and reduce overfitting [11].
- Model Training: Six candidate ML algorithms are trained and compared [11]:
- Logistic Regression (LR): A linear model providing high interpretability.
- Support Vector Machine (SVM): Effective in high-dimensional spaces.
- Random Forest (RF): An ensemble of decision trees, robust against noise.
- XGBoost: A gradient boosting algorithm with high predictive accuracy.
- Model Validation: Model performance is rigorously assessed on the held-out external validation set using the Area Under the Receiver Operating Characteristic Curve (AUC) [11].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Platforms
| Item | Function/Application | Specific Example/Kit |
|---|---|---|
| Targeted Metabolomics Kit | Simultaneous quantification of predefined metabolites | Absolute IDQ p180 Kit (Biocrates) [11] |
| Liquid Chromatography System | Separation of complex metabolite mixtures prior to detection | Ultra-Performance Liquid Chromatography (UPLC) system [11] |
| Mass Spectrometer | High-sensitivity detection and quantification of metabolites | Triple Quadrupole Mass Spectrometer (e.g., Waters Xevo TQ-S) [11] |
| Data Processing Software | Raw data processing, peak integration, and metabolite quantification | Biocrates MetIDQ software [11] |
| Machine Learning Libraries | Open-source programming tools for model development and evaluation | Scikit-learn, XGBoost, Pandas, NumPy in Python [11] |
| Gentiournoside D | Gentiournoside D, MF:C23H28O13, MW:512.5 g/mol | Chemical Reagent |
| Clematichinenoside C | Clematichinenoside C, MF:C70H114O34, MW:1499.6 g/mol | Chemical Reagent |
Analytical and Computational Pathways
The journey from raw data to a validated biomarker panel involves a sophisticated analytical pipeline. The following diagram illustrates the logical flow and key decision points in the computational analysis, from multi-omics data integration through feature selection and model optimization to final validation.
This case study demonstrates that integrating clinical and metabolomic data within a machine learning framework is a powerful strategy for discovering diagnostic biomarkers for complex diseases like Large-Artery Atherosclerosis. The high predictive accuracy (AUC > 0.92) achieved by models, particularly logistic regression, underscores the clinical potential of this approach. The identified biomarkers, rooted in pathways like aminoacyl-tRNA biosynthesis and lipid metabolism, provide not only a diagnostic signature but also biological insights into LAA pathology. This end-to-end protocol—from rigorous sample collection and metabolomic profiling to robust machine learning validation—offers a replicable blueprint for biomarker discovery that can be adapted to other disease contexts within precision medicine.
The discovery of prognostic and predictive biomarkers is a cornerstone of precision oncology, essential for accurate diagnosis, patient stratification, and treatment selection. Traditional biomarker discovery methods, which often focus on single molecular features, face significant challenges including limited reproducibility, high false-positive rates, and an inability to capture the complex, interconnected nature of disease biology [8]. Advanced computational architectures—including deep learning, contrastive learning, and network-based approaches—are overcoming these limitations by extracting meaningful patterns from high-dimensional, multi-modal data. These methods leverage intricate relationships within biological systems, leading to more robust and clinically actionable biomarkers [42] [43]. This article provides application notes and detailed protocols for implementing these state-of-the-art architectures in biomarker discovery research.
The table below summarizes the core architectures, key advantages, and documented performance of the advanced frameworks discussed in this article.
Table 1: Comparison of Advanced Architectures for Biomarker Discovery
| Architecture/ Framework | Core Methodology | Key Advantages | Reported Performance |
|---|---|---|---|
| Expression Graph Network Framework (EGNF) [42] | Graph Neural Networks (GCNs, GATs) on biologically-informed networks. | Captures complex sample-feature relationships; superior interpretability. | Perfect separation of normal/tumor samples; superior accuracy in disease progression classification. |
| Flexynesis [4] | Deep learning for bulk multi-omics integration. | High modularity & transparency; supports single & multi-task learning. | AUC=0.981 for MSI status classification; high accuracy in drug response prediction & survival modeling. |
| MarkerPredict [44] | Random Forest & XGBoost on network & protein disorder features. | High interpretability; integrates protein structure & network topology. | LOOCV accuracy of 0.7–0.96; identified 2084 potential predictive biomarkers. |
| CLEF [45] | Contrastive learning integrating Protein Language Models (PLMs) & biological features. | Enhances PLMs with experimental data; superior cross-modality representation. | Outperformed state-of-the-art models in predicting T3SEs, T4SEs, and T6SEs. |
| PRoBeNet [46] | Network medicine leveraging the human interactome. | Robust performance with limited data; reduces feature dimensionality. | Significantly outperformed models using all genes or randomly selected genes. |
Detailed Architectures and Application Protocols
Network-Based Approaches: The Expression Graph Network Framework (EGNF)
Principle: The EGNF moves beyond traditional models that treat genes as independent entities. It constructs dynamic, patient-specific graphs where nodes represent clusters of samples with similar gene expression patterns, and edges represent shared samples between these clusters. This structure inherently captures the interconnected nature of biological pathways [42].
Protocol: Implementing EGNF for Biomarker Discovery
Input Data Preparation:
- Data: Processed RNA-Seq count data from paired or unpaired study designs (e.g., tumor vs. normal, pre- vs. post-treatment).
- Split: Divide the dataset, using 80% for training and 20% for hold-out validation.
Differential Expression & Network Construction:
- Perform differential expression analysis on the training set using a tool like DESeq2 to identify significant genes [42].
- For each significant gene, perform one-dimensional hierarchical clustering on its expression values across samples.
- Node Creation: Define the extreme clusters (e.g., samples with the highest and lowest expression) from the clustering as nodes in the graph.
- Edge Creation: Establish connections (edges) between nodes from different genes if they share a significant number of samples.
Graph-Based Feature Selection:
- Prune the network to identify the most salient biomarkers using multiple criteria:
- Node Degree: Prioritize genes whose nodes have high connectivity.
- Community Structure: Identify genes that frequently co-occur within densely connected network communities.
- Biological Pathways: Overlap selected gene modules with known biological pathways (e.g., from KEGG, Reactome) to ensure relevance.
- Prune the network to identify the most salient biomarkers using multiple criteria:
Model Training and Prediction with GNNs:
- Build a final prediction network using the selected features.
- Train a Graph Neural Network (e.g., a Graph Convolutional Network or Graph Attention Network) on this network.
- For a new sample, generate a sample-specific subgraph and use the trained GNN to predict its class (e.g., tumor vs. normal) [42].
Figure 1: EGNF combines hierarchical clustering with graph neural networks to identify biomarkers from complex biological relationships.
Deep Learning for Multi-Omics Integration: The Flexynesis Framework
Principle: Flexynesis addresses the challenge of integrating disparate but interconnected molecular data types (e.g., transcriptomics, genomics, epigenomics). It uses deep learning to model the non-linear relationships between these omics layers, which are often missed by linear models [4].
Protocol: Multi-Omics Classification with Flexynesis
Tool Installation and Data Setup:
- Install Flexynesis via Bioconda, PyPi, or use it on the Galaxy server (
usegalaxy.eu) for enhanced accessibility [4]. - Input Data: Prepare your omics data (e.g., gene expression, methylation) as separate tab-delimited files, with samples as rows and features as columns. Normalize and log-transform data as required.
- Target Variable: Prepare a label file (e.g., MSI-High vs. MSI-Stable) corresponding to the samples.
- Install Flexynesis via Bioconda, PyPi, or use it on the Galaxy server (
Model Configuration:
- Choose a deep learning architecture (e.g., fully connected encoder) for the task.
- For a classification task (e.g., microsatellite instability status), attach a supervised multi-layer perceptron (MLP) head to the encoder.
- Flexynesis automates key steps like data processing, feature selection, and hyperparameter tuning, making it accessible to users without deep learning expertise.
Model Training and Validation:
- Execute the training process, using a standard 70/30 or 80/20 train-test split.
- The tool will output performance metrics like Area Under the Curve (AUC). For example, a model using only gene expression data achieved an AUC of 0.981 for MSI status classification, demonstrating the power of this approach [4].
Contrastive Learning for Enhanced Representation: The CLEF Model
Principle: Contrastive learning is a self-supervised technique that learns powerful data representations by pulling "similar" data points (positive pairs) closer and pushing "dissimilar" ones (negative pairs) apart in the feature space. The CLEF model applies this to biomarker discovery by integrating generic Protein Language Model (PLM) embeddings with specific biological features (e.g., from structural data or functional annotations), creating a richer, cross-modality representation [45].
Protocol: Contrastive Pre-training with CLEF for Effector Prediction
Data Preparation and Feature Extraction:
- Sequence Input: Compile amino acid sequences of proteins of interest.
- PLM Embedding: Generate base protein representations using a pre-trained model like ESM2 [45].
- Biological Modality: Encode supplementary biological information. This could be:
- Secretion Embedding: Features from a specialized effector classifier.
- 3Di Features: Structural information derived from tools like Foldseek.
- Annotation Text: Gene Ontology terms encoded via BioBERT.
Contrastive Pre-training:
- Input pairs of (PLM representation, Biological feature vector) for each protein into the CLEF model.
- CLEF uses a dual-encoder architecture and the InfoNCE loss function to learn a unified, cross-modality representation in a shared latent space. This step forces the model to align the information from the generic PLM with the specific biological context.
Classifier Fine-tuning:
- After pre-training, use the generated cross-modality representations as input features for a simpler classifier (e.g., a shallow neural network).
- Fine-tune this classifier on a smaller, labeled dataset (e.g., known effectors vs. non-effectors) to create the final predictive model [45].
Figure 2: CLEF uses contrastive learning to integrate protein language models with biological features for improved biomarker prediction.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools and Databases
| Category | Tool / Database | Primary Function | Application in Biomarker Discovery |
|---|---|---|---|
| Deep Learning Frameworks | PyTorch Geometric [42] | Library for Graph Neural Networks (GNNs). | Building and training models on graph-structured biological data (e.g., EGNF). |
| Graph Databases | Neo4j with GDS Library [42] | Graph database management and analytics. | Storing biological networks and performing network-based feature selection. |
| Multi-Omics Platforms | Flexynesis [4] | Deep learning toolkit for bulk multi-omics. | Integrating transcriptomic, genomic, and epigenomic data for classification and survival modeling. |
| Protein Language Models | ESM2 [45] | Pre-trained deep learning model on protein sequences. | Generating foundational protein representations for downstream prediction tasks. |
| Structural Feature Tools | Foldseek / ProstT5 [45] | Protein structural alignment and encoding. | Converting 3D protein structure into feature vectors for integration (e.g., in CLEF). |
| Biomarker Databases | CIViCmine [44] | Text-mined repository of cancer biomarkers. | Providing evidence-based positive/negative training sets for machine learning models. |
| Interaction Networks | SIGNOR, ReactomeFI [44] | Curated protein-protein interaction and signaling networks. | Providing the scaffold for network-based algorithms (e.g., PRoBeNet, MarkerPredict). |
| Saikosaponin H | Saikosaponin H, MF:C48H78O17, MW:927.1 g/mol | Chemical Reagent | Bench Chemicals |
The integration of deep learning, contrastive learning, and network-based frameworks represents a paradigm shift in biomarker discovery. By moving beyond single-analyte approaches and embracing the complexity of biological systems, these advanced architectures enable the identification of robust, interpretable, and clinically relevant biomarkers. The detailed protocols and tools outlined herein provide researchers and drug development professionals with a practical roadmap for implementing these powerful methods, ultimately accelerating the development of personalized cancer therapies and improving patient outcomes. As the field evolves, a focus on rigorous validation, model interpretability, and accessibility will be crucial for translating these computational advances into clinical practice [47] [8].
The staggering molecular heterogeneity of complex diseases like cancer demands innovative approaches beyond traditional single-omics methods [48]. Multi-omics integration represents a paradigm shift in precision medicine, combining diverse molecular data layers—genomics, transcriptomics, proteomics, and metabolomics—to construct comprehensive molecular portraits of disease states [2]. This approach is particularly transformative in machine learning-driven biomarker discovery, where the integration of orthogonal molecular and phenotypic data enables researchers to recover system-level signals that are often missed by single-modality studies [48]. Where single-omics analyses provide limited snapshots, integrated multi-omics reveals a more complete picture of biological processes, disease mechanisms, and potential therapeutic targets [49].
The critical importance of multi-omics integration stems from the biological continuum that connects genetic blueprints to functional phenotypes. Genomics identifies DNA-level alterations including single-nucleotide variants (SNVs), copy number variations (CNVs), and structural rearrangements that drive disease initiation [48]. Transcriptomics reveals gene expression dynamics through RNA sequencing (RNA-seq), quantifying mRNA isoforms, non-coding RNAs, and fusion transcripts that reflect active transcriptional programs [48]. Proteomics catalogs the functional effectors of cellular processes, identifying post-translational modifications, protein-protein interactions, and signaling pathway activities that directly influence therapeutic responses [48]. Metabolomics profiles small-molecule metabolites, the biochemical endpoints of cellular processes, exposing metabolic reprogramming in diseases such as cancer [48]. Each layer provides orthogonal yet interconnected biological insights, collectively constructing a comprehensive molecular atlas of health and disease [48].
Machine learning and artificial intelligence serve as the essential scaffold bridging multi-omics data to clinically actionable biomarkers [2] [48]. Unlike traditional statistical methods, AI excels at identifying non-linear patterns across high-dimensional spaces, making it uniquely suited for multi-omics integration [48]. These approaches have demonstrated particular effectiveness in addressing the limitations of traditional biomarker discovery methods, including limited reproducibility, inability to integrate multiple data streams, high false-positive rates, and inadequate predictive accuracy [2]. By analyzing large, complex multi-omics datasets, machine learning methods can identify more reliable and clinically useful biomarkers for diagnostic, prognostic, and predictive applications across various disease areas, including oncology, infectious diseases, neurological disorders, and autoimmune conditions [2].
Multi-Omics Integration Strategies and Computational Frameworks
Classification of Integration Approaches
The integration of multi-omics data employs distinct computational strategies, each with specific strengths and applications in biomarker discovery. These approaches can be categorized based on when and how the integration occurs during the analytical workflow, with the choice of method heavily influenced by whether the data modalities are matched (profiled from the same cell or sample) or unmatched (profiled from different cells or samples) [50].
Table 1: Multi-Omics Integration Strategies and Their Characteristics
| Integration Type | Description | Typical Applications | Examples Tools |
|---|---|---|---|
| Early Integration (Data-Level) | Raw or preprocessed data from multiple omics are combined before analysis | Horizontal integration of the same omic across multiple datasets | Simple data concatenation |
| Intermediate Integration (Feature-Level) | Joint dimensionality reduction or latent space learning | Matched multi-omics from same samples; vertical integration | MOFA+, SNF, SCHEMA, Seurat v4 |
| Late Integration (Prediction-Level) | Separate models trained on each modality with subsequent combination of predictions | Unmatched data from different cells/samples; diagonal integration | Ensemble methods, late fusion models |
| Mosaic Integration | Integration when datasets have various combinations of omics with sufficient overlap | Complex experimental designs with partial modality overlap | COBOLT, MultiVI, StabMap |
Early integration, also known as data-level fusion, involves combining raw or preprocessed data from multiple omics layers into a single feature matrix before applying analytical algorithms [51]. While conceptually straightforward, this approach often faces challenges due to the high dimensionality and heterogeneity of the data, which can lead to the "curse of dimensionality" where the number of features vastly exceeds the number of samples [48] [51]. This approach may be suitable for horizontal integration of the same omic across multiple datasets but is less effective for true multi-omics integration [50].
Intermediate integration methods process multiple omics datasets simultaneously using joint dimensionality reduction techniques or latent space learning [52]. These approaches include similarity network fusion, matrix factorization, and neural network-based methods that create a unified representation of the data while preserving inter-modality relationships [53]. This strategy is particularly powerful for matched multi-omics data from the same samples (vertical integration), where the cell or sample itself serves as an anchor for integration [50]. Techniques like Similarity Network Fusion (SNF) compute a sample similarity network for each data type and fuse them into a single network that captures shared information across omics layers [53].
Late integration, also known as prediction-level fusion, involves building separate models for each data modality and subsequently combining their predictions [51]. This approach demonstrates particular strength in handling unmatched data from different cells or samples (diagonal integration) and situations with highly heterogeneous data types [50] [51]. Late fusion models have been shown to consistently outperform single-modality approaches in cancer survival prediction tasks using TCGA data, offering higher accuracy and robustness [51]. The advantage of this method lies in its resistance to overfitting, ease of addressing data heterogeneity, and ability to naturally weight each modality based on its informativeness without being affected by highly imbalanced dimensionalities across modalities [51].
Mosaic integration has emerged as an alternative approach for complex experimental designs where datasets have various combinations of omics that create sufficient overlap [50]. For example, if one sample was assessed for transcriptomics and proteomics, another for transcriptomics and epigenomics, and a third for proteomics and epigenomics, there is enough commonality between these samples to integrate the data using specialized tools like COBOLT, MultiVI, or StabMap [50].
Machine Learning and AI-Driven Integration Methods
Artificial intelligence, particularly machine learning and deep learning, has revolutionized multi-omics integration by enabling scalable, non-linear analysis of disparate omics layers [48]. These methods have proven effective in biomarker discovery by integrating diverse and high-volume data types to identify more reliable and clinically useful biomarkers [2].
Matrix factorization methods like MOFA+ (Multi-Omics Factor Analysis) use statistical techniques to identify latent factors that represent shared sources of variation across multiple omics datasets [50] [2]. These methods decompose the original high-dimensional data matrices into lower-dimensional representations that capture the essential biological signals while reducing noise [2].
Neural network-based approaches, including variational autoencoders (scMVAE), deep canonical correlation analysis (DCCA), and transformer models, use deep learning architectures to learn complex, non-linear relationships between different omics modalities [50] [48]. These methods can model intricate biological patterns that linear methods might miss and have shown particular promise in integrating transcriptomics, proteomics, and metabolomics data [48].
Network-based methods leverage graph theory and biological networks to integrate multi-omics data. Similarity Network Fusion (SNF) constructs sample similarity networks for each omics layer and iteratively fuses them into a single network that represents shared information across all data types [53]. The Integrative Network Fusion (INF) framework extends this approach by combining SNF with machine learning classifiers to extract compact, predictive biomarker signatures from multi-modal oncogenomics data [53].
Graph neural networks (GNNs) represent a cutting-edge approach that models biological networks, such as protein-protein interaction networks, perturbed by disease-associated alterations [48]. These methods can prioritize druggable hubs in complex diseases and have shown utility even in rare cancers where sample sizes are limited [48].
Table 2: AI and Machine Learning Methods for Multi-Omics Integration
| Method Category | Key Algorithms | Strengths | Limitations |
|---|---|---|---|
| Matrix Factorization | MOFA+, iNMF | Interpretable factors, handles missing data | Assumes linear relationships, may miss complex interactions |
| Variational Autoencoders | scMVAE, totalVI | Captures non-linear patterns, generative capability | Computationally intensive, requires large samples |
| Network-Based Methods | SNF, INF, Graph Neural Networks | Incorporates biological priors, models relationships | Network quality dependent on prior knowledge |
| Ensemble Methods | Random Forest, Gradient Boosting | Handles heterogeneous data, robust performance | Less interpretable, complex to tune |
| Transformers | Multi-modal transformers | Captures cross-modal attention, state-of-the-art performance | Extremely computationally demanding, data hungry |
Experimental Protocols for Multi-Omics Biomarker Discovery
Study Design and Data Collection Framework
Robust multi-omics biomarker discovery begins with meticulous study design and data collection. The initial critical step involves formulating precise biological questions that will guide the entire research project [49]. For biomarker discovery, questions might focus on characterizing disease subtypes, identifying diagnostic or prognostic biomarkers, predicting treatment response, or understanding regulatory processes underlying disease mechanisms [54]. The specificity of the research question significantly influences choices of omics technologies, dataset curation strategies, and analytical methods [49].
Omic technology selection should be guided by the biological question and considerations of each technology's advantages and limitations [49]. Transcriptomics data, with amplifiable transcripts that are easier to quantify, may be optimal for pathway enrichment analysis [49]. Proteomics datasets generated by mass spectrometry may carry biases toward highly expressed proteins, causing inter-experiment variations [49]. Metabolomics faces challenges in high-throughput compound annotation, making metabolomic profiles sparser and more ambiguous than transcriptomics [49]. Genomic variants from GWAS cannot always be mapped to genes as they may reside in both coding and noncoding regions [49].
Experimental design considerations must address data compatibility across datasets [49]. Researchers should ensure studies examine the same population of interest, as discrepancies can arise when comparing disease tissue against "adjacent normal tissue" versus "healthy control" from "peripheral blood" [49]. Careful attention to research backgrounds and experimental designs of each omics dataset is essential, including examination of metadata such as gender, age, treatment, time, location, and other factors to ensure input data compatibility for multi-omics integration [49].
Data quality assessment should prioritize quality over quantity [49]. Researchers should evaluate how data were collected and preprocessed, what tools were used, and whether studies underwent rigorous peer review [49]. Assessment should include compliance with best practices for data collection, processing, annotation, and adherence to common standards and formats for data representation and sharing [49]. Potential biases in experimental design, such as gender skew, should be identified, and technology-specific quality metrics should be examined [49].
Data Preprocessing and Harmonization Protocol
Comprehensive data standardization and harmonization are essential for reliable multi-omics integration [49]. This protocol outlines a standardized workflow for preparing multi-omics data for integration and analysis.
Step 1: Data Format Standardization Different studies and technologies generate data in diverse formats, units, and ontologies [49]. Researchers must:
- Convert all data to consistent formats (e.g., raw count matrices for sequencing data)
- Map identifiers to standard ontologies and nomenclature (e.g., HUGO gene names, UniProt IDs)
- Document all version information for databases and reference genomes
Step 2: Quality Control and Filtering Implement technology-specific quality control measures:
- For transcriptomics: Filter genes based on expression thresholds, assess ribosomal and mitochondrial content
- For proteomics: Apply intensity thresholds, filter based on missingness patterns
- For metabolomics: Remove contaminants, assess signal-to-noise ratios
- Record all filtering criteria and their justification
Step 3: Normalization and Batch Correction Address technical variability across datasets:
- Apply appropriate normalization methods for each data type (e.g., DESeq2 for RNA-seq, quantile normalization for proteomics) [48]
- Implement batch correction algorithms (e.g., ComBat, limma) to remove non-biological technical variation [48]
- Validate normalization effectiveness using PCA and other visualization techniques
Step 4: Missing Data Imputation Handle missing values using informed strategies:
- Assess patterns of missingness (missing completely at random, at random, or not at random)
- Apply appropriate imputation methods (e.g., k-nearest neighbors, matrix factorization, deep learning-based reconstruction) [48]
- Document imputation methods and proportion of imputed values
Step 5: Data Transformation and Scaling Prepare data for integration:
- Transform data to comparable scales using z-scores, rank-based methods, or log transformations
- Consider using ranking systems to alleviate batch effects [49]
- Ensure transformations maintain biological interpretability
Multi-Omics Integration and Biomarker Discovery Workflow
The following workflow implements the Integrative Network Fusion (INF) approach, which effectively combines multiple omics layers for biomarker discovery [53].
Step 1: Data Input and Preprocessing
- Input: Collect matched multi-omics datasets (e.g., gene expression, protein expression, metabolomics) from the same patient samples [53]
- Implementation: Follow the preprocessing protocol outlined in Section 3.2
- Output: Quality-controlled, normalized datasets ready for integration
Step 2: Parallel Integration Approaches Execute two integration approaches in parallel:
Approach A: Early Integration via Feature Juxtaposition
- Combine preprocessed omics datasets by simple concatenation (juxtaposition) of features [53]
- Train a machine learning classifier (e.g., Random Forest or linear SVM) on the juxtaposed data
- Rank features by their importance scores (e.g., ANOVA F-value for SVM) [53]
Approach B: Intermediate Integration via Similarity Network Fusion
- For each omics layer, construct a sample similarity network using appropriate distance metrics [53]
- Apply Similarity Network Fusion (SNF) to iteratively fuse the networks into a single combined network [53]
- Compute feature rankings (rSNF) based on contributions to the fused network structure [53]
Step 3: Feature Selection and Model Training
- Identify the intersection of top-ranked features from both juxtaposition and rSNF approaches [53]
- Train a final model (e.g., Random Forest) on the selected feature subset [53]
- Implement rigorous cross-validation (e.g., 10x5-fold) to avoid overfitting and ensure reproducibility [53]
Step 4: Biomarker Validation and Interpretation
- Validate selected biomarkers on independent test datasets
- Perform biological interpretation through pathway enrichment analysis, network analysis, and literature mining
- Assess clinical relevance through association with clinical outcomes
Research Reagent Solutions and Computational Tools
Table 3: Essential Research Reagents and Computational Tools for Multi-Omics Integration
| Category | Item | Function/Application | Examples/Alternatives |
|---|---|---|---|
| Omics Technologies | RNA-seq kits | Transcriptome profiling | Illumina, PacBio |
| Mass spectrometry systems | Proteome and metabolome quantification | LC-MS, GC-MS platforms | |
| SNP arrays | Genomic variant profiling | Affymetrix, Illumina arrays | |
| Computational Tools | MOFA+ | Factor analysis for multi-omics integration | Available as R/Bioconductor package |
| Seurat v4 | Weighted nearest-neighbor multi-omics integration | Supports mRNA, protein, chromatin accessibility | |
| Similarity Network Fusion | Network-based multi-omics integration | Python and R implementations | |
| SCHEMA | Metric learning-based integration | Handles chromatin accessibility, mRNA, proteins | |
| Cobolt | Multimodal variational autoencoder | Python implementation | |
| Data Resources | TCGA | Multi-omics cancer datasets | https://portal.gdc.cancer.gov/ |
| GEO | Functional genomics data repository | https://www.ncbi.nlm.nih.gov/geo/ | |
| MetaboLights | Metabolomics datasets | https://www.ebi.ac.uk/metabolights/ |
Applications in Precision Oncology and Biomarker Discovery
Multi-omics integration has demonstrated particular success in precision oncology, where it enables improved disease subtyping, prognosis, and treatment selection [55]. The Integrative Network Fusion (INF) framework has been successfully applied to TCGA datasets, achieving Matthews Correlation Coefficient values of 0.83 for predicting estrogen receptor status in breast cancer and 0.38 for overall survival prediction in kidney renal clear cell carcinoma, with significantly reduced feature set sizes (56 vs. 1801 features for BRCA-ER) [53]. These compact biomarker signatures maintain predictive power while enhancing biological interpretability and clinical translatability [53].
In breast cancer, multi-omics approaches have identified distinct molecular subtypes with differential treatment responses and survival outcomes [53]. Integration of genomics, transcriptomics, proteomics, and metabolomics has revealed regulatory networks and pathway alterations that drive cancer progression and therapeutic resistance [55]. Similar approaches in lung cancer, acute myeloid leukemia, and renal cell carcinoma have yielded prognostic biomarkers that outperform single-omics alternatives [53] [51].
The application of AI-driven multi-omics integration has enabled novel approaches in predictive biomarker discovery. Machine learning models integrating transcripts, proteins, metabolites, and clinical factors have consistently outperformed single-modality approaches in survival prediction across multiple cancer types [51]. These models successfully manage challenges like high dimensionality, small sample sizes, and data heterogeneity through sophisticated fusion strategies and rigorous validation frameworks [51].
Emerging technologies like single-cell multi-omics and spatial transcriptomics are further expanding the possibilities for biomarker discovery [55] [48]. These approaches allow researchers to resolve cellular heterogeneity and map molecular interactions within tissue architecture, providing unprecedented resolution for understanding tumor microenvironments and cellular ecosystems [55]. As these technologies mature, they promise to reveal novel biomarker signatures with improved sensitivity and specificity for early detection, monitoring, and therapeutic targeting.
Challenges and Future Directions
Despite significant advances, multi-omics integration faces several persistent challenges that require methodological innovations and community standards. Data heterogeneity remains a fundamental obstacle, with different omics layers exhibiting distinct data scales, noise ratios, and preprocessing requirements [50]. The "curse of dimensionality" presents statistical challenges when the number of features vastly exceeds sample sizes, increasing the risk of overfitting and spurious discoveries [48] [51]. Missing data, batch effects, and platform-specific technical variations further complicate integration and interpretation [48].
Methodological challenges include the development of approaches that effectively model non-linear relationships across omics layers while maintaining biological interpretability [2]. Many deep learning methods function as "black boxes," limiting their clinical translation where interpretability is essential for physician adoption and regulatory approval [2] [48]. Explainable AI (XAI) techniques like SHapley Additive exPlanations (SHAP) are emerging to address this limitation by clarifying how specific genomic variants or molecular features contribute to predictive models [48].
Future directions in multi-omics integration include the development of foundation models pretrained on millions of omics profiles, enabling transfer learning for rare diseases with limited samples [48]. Federated learning approaches will facilitate privacy-preserving collaboration across institutions by training models on decentralized data without sharing sensitive patient information [48]. Dynamic, longitudinal multi-omics profiling will capture temporal changes in molecular signatures during disease progression and treatment, moving beyond static snapshots to cinematic views of biological processes [48].
As the field advances, rigorous validation, model interpretability, and regulatory compliance will be essential for clinical implementation [2]. Multi-omics biomarker discovery must adhere to standards like the FDA's Biomarker Qualification Program to ensure reliability and reproducibility across diverse patient populations [2]. Through continued methodological innovation and collaborative science, multi-omics integration promises to transform precision medicine from reactive population-based approaches to proactive, individualized care [48].
Navigating Pitfalls: Strategies to Overcome Data, Model, and Generalization Challenges
In the field of machine learning-based biomarker discovery, overfitting represents the most significant barrier to developing clinically applicable models. Overfitting occurs when a model learns not only the underlying signal in the training data but also the random noise and idiosyncrasies, resulting in poor performance when applied to new, unseen datasets [7]. This challenge is particularly acute in biomarker research due to the high-dimensional nature of omics data (e.g., genomics, transcriptomics, proteomics, metabolomics) where the number of features (p) vastly exceeds the number of samples (n), creating the so-called "p >> n problem" [19] [56].
The consequences of overfitting are not merely theoretical; they directly impact translational potential. Overfit models generate false discoveries that fail to validate in independent patient cohorts, wasting valuable research resources and delaying clinical implementation [7] [47]. The complexity of biological systems, combined with technical noise, batch effects, and biological heterogeneity, creates an environment where overfitting can easily go undetected without rigorous validation strategies [19]. Thus, conquering overfitting is not a peripheral concern but a central requirement for advancing precision medicine through reliable biomarker discovery.
Foundational Principles for Preventing Overfitting
Strategic Study Design and Data Quality Assurance
Robust biomarker discovery begins with strategic study design that anticipates and mitigates overfitting risks before computational analysis commences. A meticulously planned study establishes the foundation for generalizable models by addressing critical constraints at the design phase.
- Clear Objective Definition: Precisely define primary and secondary biomedical outcomes, subject inclusion/exclusion criteria, and experimental conditions to avoid ambiguous endpoints that complicate model evaluation [19] [56].
- Adequate Sample Size Planning: Employ statistical power analysis and sample size determination methods to ensure sufficient samples relative to feature dimensionality, despite the high costs of omics data generation [19].
- Comprehensive Blocking Design: Strategically arrange samples across measurement batches to control for technical variability, ensuring biological signals can be distinguished from batch effects [19].
- Prospective Validation Planning: Allocate samples for independent validation at the study inception, either through splitting cohorts or planning external validation studies [11].
Data quality assurance forms the second pillar of overfitting prevention. Technical artifacts and poor-quality data can create spurious patterns that models readily overfit. Implement rigorous quality control pipelines using established software packages: fastQC/FQC for next-generation sequencing data, arrayQualityMetrics for microarray data, and MeTaQuaC/Normalyzer for proteomics and metabolomics data [19] [56]. Quality checks should be applied both before and after preprocessing to ensure data transformations do not introduce artificial patterns. Additionally, clinical data curation must include range validation, unit standardization, and format harmonization using common standards like OMOP, CDISC, and ICD10/11 [19].
Data Partitioning and Validation Frameworks
Appropriate data partitioning provides the critical framework for detecting overfitting during model development. A structured approach to data separation ensures honest assessment of model generalizability.
- Training-Validation-Test Split: Implement a three-way data split, reserving a substantial portion (typically 20%) as a completely held-out test set that is used only once for final model evaluation [11].
- Cross-Validation Implementation: Apply k-fold cross-validation (typically k=10) within the training set for hyperparameter tuning and model selection, ensuring that validation occurs on different data partitions than those used for training [11] [57].
- External Validation Mandate: Whenever possible, validate final models on completely independent cohorts from different institutions or studies, which provides the most rigorous assessment of generalizability [7] [11].
A critical pitfall to avoid is data leakage, where information from the test set inadvertently influences the training process. This can occur through improper preprocessing, feature selection, or imputation that uses the entire dataset before splitting. To prevent leakage, all steps including normalization, feature selection, and missing value imputation must be performed separately within each cross-validation fold and the training set only [47].
The following workflow illustrates a robust experimental design that incorporates these protective measures:
Technical Approaches to Combat Overfitting
Regularization Techniques for Feature Selection
Regularization methods represent one of the most powerful approaches for preventing overfitting by constraining model complexity. These techniques apply mathematical penalties during training to discourage over-reliance on any single feature, thereby promoting simpler, more generalizable models.
Table 1: Regularization Techniques for Biomarker Discovery
| Technique | Mechanism | Advantages | Ideal Applications |
|---|---|---|---|
| LASSO (L1 Regularization) | Adds absolute value of coefficients to loss function | Performs feature selection by driving coefficients to zero | High-dimensional omics data with many irrelevant features [11] [57] [58] |
| Ridge (L2 Regularization) | Adds squared magnitude of coefficients to loss function | Shrinks coefficients without eliminating them; handles correlated features | When all features may be relevant but require stabilization [58] |
| Elastic Net | Combines L1 and L2 regularization | Balances feature selection with handling of correlated variables | Proteomics and metabolomics data with highly correlated features [11] |
| Bio-Primed LASSO | Incorporates biological knowledge into L1 penalty | Prioritizes biologically plausible features; enhances interpretability | Integration with protein-protein interaction networks or pathway databases [57] |
Recent innovations like bio-primed regularization extend conventional LASSO by incorporating biological prior knowledge into the feature selection process. This approach uses biological evidence scores (e.g., from protein-protein interaction databases like STRING DB) to influence the regularization penalty, ensuring that statistically significant features with biological relevance receive preference [57]. In application to MYC dependency prediction, bio-primed LASSO identified coherent biological processes and biomarkers like STAT5A and NCBP2 that were missed by standard approaches, demonstrating improved biological interpretability without sacrificing predictive performance [57].
The following diagram illustrates the bio-primed LASSO workflow:
Data Augmentation and Multi-Omics Integration
In domains with limited sample sizes, such as clinical proteomics and transcriptomics, data augmentation creates artificially expanded training sets through label-preserving transformations. For omics data, this includes:
- Adding Gaussian Noise: Introducing small, random variations to expression values that mimic technical variability while preserving biological signal.
- Sample Mixing: Creating synthetic samples through weighted averages of existing samples, similar to MixUp techniques in computer vision.
- Bootstrapping: Generating new datasets through random sampling with replacement to assess model stability and variance.
While data augmentation cannot create fundamentally new biological information, it helps models learn more robust patterns invariant to technical noise [47].
Multi-omics integration provides a powerful alternative to artificial data augmentation by combining complementary data modalities to create a more comprehensive representation of the biological system. Three primary integration strategies have emerged:
- Early Integration: Combining raw features from multiple omics layers before model training, typically using dimensionality reduction techniques like Canonical Correlation Analysis (CCA) [19] [56].
- Intermediate Integration: Joining data sources during model training using architectures like multiple kernel learning or multimodal neural networks [19] [8].
- Late Integration: Training separate models on each data type and combining predictions through stacking or super learning [19] [56].
In predicting large-artery atherosclerosis, integration of clinical risk factors with metabolite profiles provided stability against dataset shifts and improved model robustness, demonstrating the protective effect of multimodal integration against overfitting [11].
Experimental Protocols for Robust Biomarker Discovery
Protocol: Regularized Biomarker Discovery with Bio-Primed LASSO
This protocol outlines the steps for implementing bio-primed LASSO regression to identify robust biomarkers while controlling overfitting.
I. Preprocessing and Data Preparation
- Quality Control: Perform data type-specific quality checks using appropriate packages (e.g., Normalyzer for proteomics, fastQC for sequencing) [19].
- Missing Value Imputation: Apply appropriate imputation (mean/median for low missingness, k-nearest neighbors for high missingness) separately to training and test sets [19].
- Normalization: Standardize features to zero mean and unit variance using parameters derived from the training set only [19].
- Data Splitting: Reserve 20% of samples as a held-out test set before any analysis [11].
II. Biological Prior Integration
- Evidence Scoring: Calculate biological evidence scores (Φ) for each feature using relevant databases (e.g., STRING DB for protein-protein interactions, KEGG for pathways) [57].
- Score Transformation: Convert evidence scores to penalty modifiers that reduce regularization strength for biologically supported features [57].
III. Model Training and Validation
- Cross-Validation Setup: Implement 10-fold cross-validation on the training set [57].
- Hyperparameter Optimization: Simultaneously optimize λ (regularization strength) and Φ (biological influence) through grid search across cross-validation folds [57].
- Feature Selection: Fit final model with optimal parameters to entire training set and extract features with non-zero coefficients [57].
- Performance Assessment: Evaluate final model on held-out test set using AUC, accuracy, and other relevant metrics [11].
Protocol: Multi-Omics Integration with Intermediate Fusion
This protocol describes intermediate integration of multiple omics datasets to enhance biological insight and reduce overfitting through complementary data sources.
I. Data Preparation and Normalization
- Platform-Specific Processing: Normalize each omics dataset according to platform-specific requirements (e.g., RMA for microarrays, TPM for RNA-seq) [19] [8].
- Batch Effect Correction: Apply ComBat or similar methods to remove technical batch effects within each data modality [19].
- Identifier Mapping: Map features to common identifiers (e.g., Gene Symbols, UniProt IDs) across omics layers [8].
II. Intermediate Integration Modeling
- Kernel Selection: Construct appropriate similarity kernels for each data type (e.g., linear kernel for clinical data, Gaussian kernel for expression data) [19] [56].
- Multiple Kernel Learning: Implement multiple kernel learning with uniform kernel combination or optimized weighting [19].
- Model Training: Train support vector machine or other kernel-based methods on the combined kernel representation [19] [56].
III. Validation and Interpretation
- Ablation Studies: Assess contribution of each data modality through leave-one-out experiments [19].
- Comparative Analysis: Benchmark against clinical-only models to demonstrate added value of omics data [19] [56].
- Biological Validation: Conduct pathway enrichment analysis on selected features and validate key findings through experimental methods [57].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Research Reagent Solutions for Robust Biomarker Discovery
| Reagent/Resource | Function | Application Notes |
|---|---|---|
| Absolute IDQ p180 Kit | Targeted metabolomics quantification of 194 metabolites | Used in atherosclerosis biomarker discovery; provides standardized metabolite measurements [11] |
| CRISPR-Cas9 Screening Libraries | Genome-wide functional genomic screens | Generates gene dependency data for biomarker validation; essential for causal inference [57] |
| STRING Database | Protein-protein interaction network resource | Provides biological evidence scores for bio-primed regularization approaches [57] |
| DepMap Portal | Cancer dependency map resource | Offers omics models with core and related feature sets for comparative biomarker discovery [57] |
| Biocrates MetIDQ Software | Metabolomics data analysis pipeline | Processes targeted metabolomics data from mass spectrometry instruments [11] |
Conquering overfitting in biomarker discovery requires a comprehensive strategy that integrates careful study design, appropriate technical methods, and rigorous validation. Regularization techniques, particularly biologically-informed approaches like bio-primed LASSO, provide powerful constraint mechanisms that balance model complexity with predictive performance. When combined with multi-omics integration and proper data partitioning, these methods enable the discovery of robust, clinically-relevant biomarkers that generalize beyond training datasets. As machine learning continues to transform precision medicine, maintaining diligence against overfitting will remain essential for translating computational findings into genuine clinical advancements.
In machine learning (ML)-driven biomarker discovery, data quality is not merely a preliminary step but the foundational element that determines the success or failure of translational research. The high-dimensional, multi-omics data essential for precision medicine presents unique challenges in data management and quality control. Batch effects, missing data, and a lack of standardization represent critical bottlenecks that can compromise the identification of robust, clinically applicable biomarkers [8] [59]. Without rigorous protocols to address these issues, even the most sophisticated ML algorithms produce models that fail to generalize beyond their original dataset, leading to irreproducible findings and costly dead ends in drug development.
The integration of ML into biomarker discovery represents a paradigm shift from traditional statistical approaches. ML excels at identifying complex, nonlinear patterns within large, multi-omics datasets—including genomics, transcriptomics, proteomics, metabolomics, and clinical records [8]. However, these algorithms are profoundly sensitive to the quality of their input data. Technical artifacts can be easily learned as false signals, a phenomenon known as overfitting, which ultimately reduces the clinical translatability of discovered biomarkers [7]. Therefore, establishing a rigorous data quality framework is imperative for distinguishing true biological signals from technical noise and for building ML models that are both predictive and clinically trustworthy.
Understanding Data Quality Challenges
The Pervasive Problem of Missing Data
Missing data is a ubiquitous problem in molecular epidemiology studies, with one analysis finding that 95% of studies either had missing data on a key variable or used data availability as an inclusion criterion [60]. When unaddressed, this issue introduces significant bias and reduces the statistical power of ML models. The nature of the "missingness" is critical, as the optimal handling strategy depends on the underlying mechanism.
- Missing Completely at Random (MCAR): The probability of data being missing is unrelated to both observed and unobserved data. An example is a sample measurement lost due to an instrumentation malfunction [60].
- Missing at Random (MAR): The probability of missingness may depend on observed data but not on unobserved data. For instance, subjects with advanced-stage cancer might be more likely to have missing genotyping data, but this missingness is unrelated to their actual, unobserved genotype [60].
- Not Missing at Random (NMAR): The missingness is related to the unobserved value itself. A classic example is a tumor size that is measured less frequently when it is smaller [60].
Despite the prevalence of missing data, the most common approach—complete-case (CC) analysis, which excludes any sample with a missing value—is statistically valid only under the strict and rarely met MCAR assumption. When data are MAR or NMAR, CC analysis yields biased and inefficient estimates, jeopardizing the validity of the biomarker study [60].
Batch Effects: A Primary Source of Technical Variance
Batch effects are notorious technical variations introduced when experiments are conducted across different times, locations, platforms, or reagent lots [59]. These non-biological signals can be so profound that they obscure true biological differences and lead to both false-positive and false-negative findings [59] [7]. In one documented case, a simple change in experimental solution caused a shift in calculated patient risk, leading to an incorrect treatment decision [59]. The challenge is compounded in large-scale, multi-center studies, which are essential for robust biomarker discovery but inherently prone to batch effects.
The impact of batch effects is heavily influenced by the study design, particularly the relationship between batch and biological factors:
- Balanced Design: Samples from different biological groups are evenly distributed across batches. This is the ideal scenario, as many batch-effect correction algorithms can perform effectively [59].
- Confounded Design: Biological groups are completely confounded with batch (e.g., all controls in one batch and all cases in another). This is a common reality in longitudinal studies and poses a severe challenge, as it becomes nearly impossible to distinguish biological signal from technical noise [59].
The Critical Lack of Data Standards
The drug discovery process, particularly in its early stages, is characterized by a lack of standardized experimental and data reporting protocols. This occurs in academic and research environments where work is exploratory but results in alarmingly low reproducibility—an estimated 80-90% of published biomedical literature is considered irreproducible [61]. This "reproducibility crisis" wastes immense resources and increases the risk of failure in later, regulated development phases.
The absence of standards manifests in three key areas:
- Experimental Standards: Lack of agreed-upon protocols for assay validation and characterization, as seen in the slow adoption of microphysiological systems (MPS) [61].
- Information Standards: Inconsistent data syntax, semantics, and content make it difficult to combine and mine datasets from different institutions [61].
- Dissemination Standards: Failure to adhere to FAIR principles (Findable, Accessible, Interoperable, Reusable) when publishing data, which limits its utility for the broader research community and for ML applications [61].
Protocols for Ensuring Data Quality
Protocol 1: Handling Missing Data in Biomarker Studies
A systematic protocol for handling missing data is essential for preserving statistical power and minimizing bias.
Step 1: Quantification and Pattern Analysis Determine the proportion of missing values for each variable and sample. Use visualization tools like heatmaps to identify patterns of missingness. Samples with an exceptionally high proportion of missing values (e.g., >60% in metabolomics) should be investigated for quality issues and potentially excluded [62].
Step 2: Mechanism Identification Perform an analysis to compare the characteristics of samples with complete data against those with missing data. If missingness is related to observed variables (e.g., disease stage), the data can be treated as MAR [60].
Step 3: Application of Imputation Methods Select and apply an imputation method appropriate for the data type and mechanism of missingness. The table below summarizes common methods.
Table 1: Methods for Handling Missing Data in Omics Studies
| Method | Principle | Best Suited For | Advantages/Limitations |
|---|---|---|---|
| Complete-Case Analysis [60] | Exclusion of samples with any missing data. | Only when data is MCAR. | Advantage: Simple.Limitation: Major loss of power and bias if not MCAR. |
| Mean/Median Imputation [62] | Replaces missing values with the variable's mean or median. | Simple, quick fix for low proportions of missing data. | Advantage: Simple, preserves sample size.Limitation: Distorts distribution and underestimates variance. |
| K-Nearest Neighbors (KNN) [62] | Uses the average value from the k most similar samples (neighbors) to impute. | Multivariate datasets with complex correlations. | Advantage: Robust; utilizes data structure.Limitation: Computationally intensive for large k. |
| Random Forest [62] | Uses an ensemble of decision trees to predict missing values iteratively. | Complex, non-linear data relationships. | Advantage: Handles non-linearity well; high accuracy.Limitation: Computationally demanding. |
| Multiple Imputation (MI) [60] | Creates multiple plausible datasets with imputed values, analyzes them separately, and pools results. | MAR data, particularly for covariates in statistical models. | Advantage: Accounts for uncertainty in the imputation; statistically sound.Limitation: Complex to implement and interpret. |
- Step 4: Validation After imputation, perform sensitivity analyses to assess the impact of the chosen method on downstream analysis, such as the list of candidate biomarkers identified.
Protocol 2: Batch Effect Detection and Correction
This protocol outlines a stepwise approach to diagnose and correct for batch effects, which is critical for integrating multi-batch datasets.
Step 1: Pre-Correction Visualization and Diagnosis Generate Principal Component Analysis (PCA) plots or t-SNE plots colored by batch and by biological group. A strong clustering of samples by batch, rather than by biology, is a clear indicator of batch effects [59] [7]. Quantitative metrics like the Signal-to-Noise Ratio (SNR) can also be calculated to measure batch separation [59].
Step 2: Selection of a Correction Algorithm Choose a Batch Effect Correction Algorithm (BECA) based on the study design (balanced vs. confounded) and data type. The performance of various algorithms was objectively assessed using multi-omics reference materials from the Quartet Project [59]. The following table summarizes key findings.
Table 2: Performance Comparison of Batch Effect Correction Algorithms
| Algorithm | Principle | Optimal Scenario | Performance Notes |
|---|---|---|---|
| Ratio-Based (e.g., Ratio-G) [59] | Scales feature values in study samples relative to a concurrently profiled reference material. | All scenarios, especially confounded. | Much more effective and broadly applicable than other methods in confounded designs [59]. |
| ComBat [59] | Empirical Bayes framework to adjust for batch effects. | Balanced designs. | Performs well in balanced scenarios but struggles when batch and biology are confounded [59]. |
| Harmony [59] | Dimensionality reduction and iterative clustering to integrate datasets. | Balanced single-cell RNA-seq data. | Shows promise but performance for other omics types in confounded scenarios is less effective than ratio-based methods [59]. |
| Per-Batch Mean-Centering (BMC) [59] | Centers the data for each feature within each batch to a mean of zero. | Balanced designs. | A simple method that works only in ideally balanced experiments [59]. |
| SVA/RUVseq [59] | Estimates surrogate variables or factors of unwanted variation. | Balanced designs with unknown sources of variation. | Can be effective but performance is inconsistent and often inferior to ratio-based methods in challenging scenarios [59]. |
Step 3: Implementation of Ratio-Based Correction Given its superior performance in confounded designs, the ratio-based method is recommended for widespread use. The procedure is as follows:
- Reference Material Selection: Integrate a well-characterized reference material (e.g., a commercial reference or a pooled sample) into the experimental design of every batch [59].
- Data Transformation: For each feature (e.g., gene expression) in each sample, calculate a ratio value:
Ratio_sample = Absolute_value_sample / Absolute_value_reference. This transforms the data from an absolute to a relative scale [59]. - Data Integration: Use the ratio-scaled data for all downstream analyses and ML model training.
Step 4: Post-Correction Validation Repeat the visualization from Step 1 (e.g., PCA plots). A successful correction will show samples clustering primarily by biological group, with minimal batch-associated clustering. The reliability of identifying differentially expressed features (DEFs) should also increase post-correction [59].
Protocol 3: Implementing Data Standards and Quality Frameworks
Adopting a structured Data Quality Framework (DQF) ensures data integrity throughout its lifecycle, which is crucial for regulatory compliance and scientific integrity [63].
Step 1: Adherence to Regulatory and FAIR Principles Familiarize your team with required data standards, such as those in the FDA Data Standards Catalog and the EMA's Data Quality Framework [64] [63]. Plan data management from the outset to ensure all data is Findable, Accessible, Interoperable, and Reusable (FAIR) [61].
Step 2: Establish Data Quality Dimensions Implement checks for key data quality dimensions throughout the project:
Step 3: Predefine Experimental and Analytical Pipelines Prior to initiating experiments, document and validate all standard operating procedures (SOPs) for sample processing, data generation, and primary analysis. This minimizes introduction of technical variability and facilitates replication [61].
Step 4: Continuous Monitoring and Auditing Implement a system for regular review of data processes to identify and correct quality issues promptly. Use feedback from these audits to refine and enhance data quality practices continuously [63].
The Scientist's Toolkit
Research Reagent Solutions
Table 3: Essential Materials and Reagents for High-Quality Biomarker Research
| Item | Function in Data Quality | Example/Note |
|---|---|---|
| Multi-Omics Reference Materials [59] | Serves as a technical calibrator for batch effect correction, enabling the ratio-based method. | Quartet Project reference materials (DNA, RNA, protein, metabolite) from four cell lines [59]. |
| Internal Standards [62] | Spiked into samples for metabolomics/proteomics to correct for instrument variability and aid in missing data imputation. | Stable isotope-labeled compounds. |
| Quality Control (QC) Samples [62] | Pooled samples run repeatedly to monitor instrument stability and data quality over time. | Used to filter out analytes with high variability (e.g., >50% missing in QC) [62]. |
| Standardized Assay Kits | Reduces protocol variability across labs and operators, improving data consistency. | Kits from reputable manufacturers with validated SOPs. |
| Electronic Lab Notebook (ELN) | Ensures data integrity, traceability, and adherence to FAIR principles from the point of generation. | ELN systems that are 21 CFR Part 11 compliant. |
Workflow Visualization
Batch Effect Correction Decision Workflow
The path to clinically viable, ML-discovered biomarkers is paved with high-quality data. Proactively addressing the trifecta of missing data, batch effects, and a lack of standardization is not an optional preprocessing step but a non-negotiable prerequisite for success. By integrating robust reference materials into experimental designs, employing statistically sound methods for data imputation and correction, and adhering to evolving regulatory and FAIR data standards, researchers can build a foundation of trust in their data. This, in turn, enables the development of machine learning models that generalize beyond a single cohort, ultimately accelerating the discovery of reliable biomarkers that can improve patient outcomes in precision medicine.
The application of machine learning (ML) in biomarker discovery represents a paradigm shift in precision medicine, yet it introduces a critical tension: the trade-off between model complexity and interpretability. As ML models become more sophisticated to decipher complex biological systems, their "black box" nature often obscures the mechanistic insights necessary for scientific validation and clinical adoption [8] [65]. This interpretability dilemma is particularly acute in biomarker research, where identifying reproducible, mechanistically grounded biomarkers is essential for understanding disease pathways and developing targeted therapies [65].
Explainable AI (XAI) has emerged as a solution to this challenge, providing tools and methods to make complex ML models more transparent and interpretable [66]. For researchers and drug development professionals, balancing predictive power with explainability is not merely a technical consideration but a fundamental requirement for building trust, ensuring reproducibility, and translating computational findings into biologically and clinically actionable insights [8] [43]. This balance is crucial for advancing personalized treatment strategies and improving patient outcomes across various disease areas, including oncology, neurodegenerative disorders, and infectious diseases [8].
XAI Fundamentals in Biomarker Research
Core Concepts and Terminology
In biomarker discovery, explainability refers to the ability to understand and interpret how a machine learning model arrives at its predictions, particularly in identifying biologically relevant features. This contrasts with opaque "black box" models where the reasoning behind predictions is not readily accessible to human researchers [65]. The rise of XAI aims to improve the opportunity for true discovery by providing explanations for predictions that can be explored mechanistically before proceeding to costly and time-consuming validation studies [65].
Several XAI techniques have been successfully applied in biomarker research. SHapley Additive exPlanations (SHAP) is a game theory-based approach that quantifies the contribution of each feature to individual predictions, providing both local and global interpretability [66]. Permutation Feature Importance measures the decrease in model performance when a single feature value is randomly shuffled, indicating which features the model relies on most for accurate predictions [66]. Partial Dependence Plots (PDPs) visualize the relationship between a feature and the predicted outcome while marginalizing the effects of other features, helping researchers understand how changes in biomarker levels influence model predictions [67].
The Scientific Imperative for Explainability
Beyond technical considerations, the drive for explainability in biomarker discovery is rooted in fundamental scientific principles. Explainable models facilitate the distinction between correlation and causation—a critical challenge in biomedical research [65]. For instance, while C-reactive protein (CRP) serves as a well-established inflammatory biomarker correlated with cardiovascular disease risk, the exact nature of this relationship required extensive temporal studies to establish that elevated CRP levels preceded disease onset rather than merely resulting from it [65].
Furthermore, XAI supports the identification of disease endotypes—subgroups of patients who share common underlying biological mechanisms despite similar clinical manifestations [65]. By revealing the distinct molecular signatures driving different endotypes, explainable ML models enable more precise patient stratification and targeted therapeutic development, advancing the goals of personalized medicine [65].
Application Notes: XAI Framework for Biomarker Discovery
Case Study: Integrating Biological Age and Frailty Prediction
A recent study demonstrates a practical framework for combining ML predictors with XAI techniques to identify aging biomarkers [66]. Researchers utilized data from the China Health and Retirement Longitudinal Study (CHARLS), including 9,702 participants in the baseline wave and 9,455 in the validation wave, with 16 blood-based biomarkers predicting biological age and frailty status [66].
Table 1: Model Performance Comparison in Aging Biomarker Study
| Model | Biological Age Prediction (MAE) | Frailty Status Prediction (Accuracy) | Key Biomarkers Identified |
|---|---|---|---|
| CatBoost | Best Performance | Competitive Performance | Cystatin C, HbA1c |
| Gradient Boosting | Competitive Performance | Best Performance | Cystatin C |
| Random Forest | Lower Performance | Lower Performance | Varied |
| XGBoost | Moderate Performance | Moderate Performance | Varied |
The study employed four tree-based ML algorithms with hyperparameter optimization via grid search and tenfold cross-validation [66]. For the frailty status predictor, which exhibited class imbalance (14.8% frail), the Synthetic Minority Over-sampling Technique (SMOTE) was applied to generate synthetic samples of frail subjects, resulting in a balanced dataset (n=8,267 per class) [66]. While traditional feature importance methods identified cystatin C and glycated hemoglobin (HbA1c) as major contributors to their respective models, subsequent SHAP analysis demonstrated that only cystatin C consistently emerged as a primary contributor across both models [66]. This finding highlights how XAI techniques can reveal consistent biomarker signatures that might be obscured by model-specific artifacts.
Experimental Protocol: XAI-Driven Biomarker Workflow
Protocol Title: Explainable AI Pipeline for Reproducible Biomarker Discovery
Objective: To establish a standardized protocol for identifying and validating ML-derived biomarkers using XAI techniques, ensuring biological interpretability and clinical relevance.
Materials and Reagents:
- Biological Samples: Based on study design (e.g., blood, tissue, CSF)
- Omics Profiling Platform: DNA/RNA sequencing, proteomics, or metabolomics platform
- Computational Environment: Python/R environment with ML libraries
Procedure:
Data Preparation and Preprocessing
- Collect and clean biomarker datasets, addressing missing values through appropriate imputation methods
- Normalize data using min-max scaling or z-score standardization to ensure comparability across features
- Partition data into training (80%), validation (10%), and test sets (10%) using stratified sampling to maintain class distribution
Model Training and Optimization
- Select multiple ML algorithms (e.g., Random Forest, Gradient Boosting, SVM) to assess robustness across models
- Implement hyperparameter tuning via grid search or Bayesian optimization with cross-validation
- Train models using appropriate techniques for imbalanced data (e.g., SMOTE, class weighting)
Explainable AI Analysis
- Apply SHAP analysis to quantify feature importance across the entire dataset and for individual predictions
- Generate permutation feature importance scores to validate SHAP findings
- Create partial dependence plots to visualize relationship between key biomarkers and predicted outcomes
Biological Validation and Interpretation
- Compare XAI-derived biomarkers with known biological pathways and prior literature
- Conduct hierarchical clustering of samples based on SHAP values to identify potential patient subgroups
- Perform pathway enrichment analysis on top-ranked biomarkers to assess biological plausibility
Troubleshooting Tips:
- If SHAP values show high variance across folds, increase cross-validation iterations or simplify model complexity
- When feature importance conflicts across XAI methods, prioritize consistent signals and investigate dataset artifacts
- If biomarkers lack biological plausibility, incorporate domain knowledge constraints or multi-omics integration
Table 2: Essential Research Reagents and Computational Tools for XAI Biomarker Discovery
| Category | Item | Function/Application | Example Sources/Platforms |
|---|---|---|---|
| Omics Technologies | RNA-seq Platforms | Transcriptomic biomarker discovery | Illumina, PacBio |
| Mass Spectrometry | Proteomic and metabolomic profiling | LC-MS/MS, GC-MS | |
| Methylation Arrays | Epigenetic biomarker identification | Illumina EPIC Array | |
| ML Frameworks | Tree-Based Algorithms | Handling non-linear relationships in biomarker data | Scikit-learn, XGBoost |
| Deep Learning Architectures | Complex pattern recognition in high-dimensional data | TensorFlow, PyTorch | |
| Explainability Libraries | Model interpretation and feature importance | SHAP, LIME, Eli5 | |
| Data Resources | Biobanks | Large-scale biomarker datasets | CHARLS, UK Biobank |
| Public Repositories | Access to multi-omics datasets | TCGA, GEO, ArrayExpress |
Visualization Framework: XAI Workflows in Biomarker Discovery
Comparative XAI Analysis Framework
Integrated Analytical Workflow for Biomarker Discovery
Technical Considerations and Implementation Challenges
Addressing Data Quality and Model Selection
The effectiveness of XAI in biomarker discovery is fundamentally constrained by data quality and appropriate model selection. ML approaches require large volumes of high-quality data, with an estimated 80% of ML efforts dedicated to data processing and cleaning [68]. Key considerations include:
Data Heterogeneity Management: Biomarker data often originates from diverse sources including genomics, transcriptomics, proteomics, metabolomics, imaging, and clinical records [8] [9]. This multi-modal integration presents significant challenges in data standardization, batch effect correction, and normalization. Establishing standardized governance protocols is essential for ensuring data consistency and model reproducibility [9].
Model Generalizability: A critical challenge in ML-based biomarker discovery is the tendency of models to overfit to specific datasets, limiting their applicability to broader populations [65]. This is particularly problematic in biomedical contexts where sample sizes may be limited and biological heterogeneity is substantial. Techniques to enhance generalizability include:
- Implementing rigorous external validation using independent cohorts
- Applying regularization methods (e.g., LASSO, Ridge regression) to prevent overfitting
- Utilizing ensemble methods that combine multiple models to improve robustness [8] [65]
Multi-Omics Integration: The complexity of biological systems often necessitates integrating multiple data modalities to identify meaningful biomarker signatures. XAI techniques must be adapted to handle these high-dimensional, heterogeneous datasets while maintaining interpretability. Network-based approaches that incorporate prior biological knowledge can help constrain the solution space to biologically plausible mechanisms [8] [69].
Validation and Clinical Translation
For AI-derived biomarkers to achieve clinical utility, they must undergo rigorous validation and demonstrate clear practical benefits:
Analytical Validation: Ensures that the biomarker test accurately and reliably measures the intended biomarkers across different laboratories and populations. This includes establishing sensitivity, specificity, precision, and reproducibility under defined conditions [43].
Clinical Validation: Establishes that the biomarker reliably predicts clinically meaningful endpoints, such as disease progression, treatment response, or survival outcomes [9]. This requires validation in independent, well-characterized patient cohorts that represent the intended-use population.
Regulatory Considerations: Biomarkers intended for clinical use must comply with regulatory standards set by agencies such as the FDA. The dynamic nature of ML-driven biomarker discovery, where models may continuously evolve with new data, presents particular challenges for regulatory frameworks that typically require fixed protocols [8].
Future Directions and Emerging Applications
The integration of XAI in biomarker discovery continues to evolve, with several promising directions emerging:
Dynamic Biomarker Monitoring: The proliferation of wearable devices and continuous monitoring technologies enables the development of dynamic biomarkers that capture physiological fluctuations and trends over time [9]. XAI methods will be essential for interpreting these complex temporal patterns and establishing their clinical relevance.
Functional Biomarker Discovery: Beyond conventional diagnostic and prognostic biomarkers, AI approaches are expanding to include functional biomarkers such as biosynthetic gene clusters (BGCs), which encode enzymatic machinery for producing specialized metabolites with therapeutic potential [8]. XAI can help elucidate the functional implications of these complex molecular systems.
Multi-Modal Data Fusion: Advanced XAI approaches are being developed to integrate diverse data types, including histopathological images, radiomics, genomics, and clinical records [43] [67]. These integrated models can capture complementary information across biological scales, potentially revealing more comprehensive biomarker signatures.
Privacy-Preserving XAI: As biomarker data becomes increasingly sensitive, methods for implementing XAI while protecting patient privacy are gaining importance. Techniques such as federated learning, differential privacy, and synthetic data generation enable model explanation without compromising individual data security [43].
The continued advancement of XAI in biomarker discovery will require close collaboration between computational scientists, biologists, and clinicians to ensure that models are not only predictive but also biologically interpretable and clinically actionable.
In the evolving field of machine learning-based biomarker discovery, the identification of robust, reproducible biomarker panels from high-dimensional biological data remains a significant challenge. This is particularly true for complex, heterogeneous conditions like premature ovarian insufficiency (POI), where the genetic etiology is not fully understood and diagnostic biomarkers are critically needed [70]. The central thesis of this research context is that sophisticated feature selection methodologies are not merely preprocessing steps but are fundamental to building clinically translatable models. Without rigorous feature selection, models are prone to overfitting, yield less interpretable results, and have diminished clinical utility due to the curse of dimensionality inherent in omics data [71] [47].
Recursive Feature Elimination (RFE) has emerged as a powerful wrapper technique that excels in this context by recursively constructing models and eliminating the least important features to find optimal feature subsets [72] [73]. This protocol details the application of RFE and complementary methods within a structured framework designed to identify robust biomarker panels, using POI biomarker discovery as a primary use case but applicable across diverse disease contexts.
Theoretical Foundations of Recursive Feature Elimination
The RFE Algorithm: Core Principles
Recursive Feature Elimination operates on a straightforward yet effective backward elimination principle. The algorithm starts with all available features and iteratively performs the following steps [72] [73]:
- Initial Model Fit: Train a model using the entire set of features.
- Feature Importance Ranking: Compute the importance of each feature based on model-specific criteria (e.g., Gini importance for Random Forests, coefficients for linear models).
- Feature Elimination: Remove the least important feature(s).
- Iteration: Repeat steps 1-3 until a predefined number of features remains or a performance threshold is met.
This process generates a ranking of features and identifies candidate subsets of varying sizes with their corresponding model performance metrics [74]. The ranking is critical because it helps researchers understand not just which features are selected, but their relative importance to the predictive model.
RFE Variants and Enhancement Strategies
Basic RFE can be enhanced through several strategic variations:
RFE with Cross-Validation (RFE-CV): Integrating cross-validation, as implemented in scikit-learn's
RFECV, automatically tunes the number of features selected and provides a more robust estimate of model performance [75]. This helps mitigate the instability that can arise from single train-test splits.Random Forest RFE (RF-RFE): Coupling RFE with Random Forest models is particularly effective for biological data. Random Forests naturally handle high-dimensional data and provide robust feature importance measures, making them well-suited for the RFE process [74]. Studies have demonstrated that RF-RFE can achieve high classification accuracy with fewer features [74].
Decision Variants for Optimal Subset Selection: A critical challenge in RFE is automatically determining the optimal feature subset without prior knowledge. Research has explored various decision variants beyond simply selecting the subset with the highest accuracy (HA) or using a preset number of features (PreNum) [74]. These include statistical measures of performance plateaus and voting strategies across cross-validation folds.
Table 1: Common Decision Variants for Determining the Optimal Feature Subset in RFE
| Variant | Description | Advantages | Limitations |
|---|---|---|---|
| Highest Accuracy (HA) | Selects the subset with the maximum classification accuracy [74] | Simple to implement and interpret | May select more features than necessary if accuracy plateaus |
| PreSet Number (PreNum) | Selects a predefined number of top-ranked features [74] | Useful when prior knowledge exists | Requires domain expertise; can be subjective |
| Performance Plateau | Selects the smallest subset where performance is within a specified margin (e.g., 1-2%) of the maximum [74] | Balances model simplicity and performance | Margin definition can be arbitrary |
| Voting Strategy | Combines subsets selected across different cross-validation folds [74] | Increases stability and robustness | More computationally intensive |
Integrated Experimental Protocol for Biomarker Discovery
This section provides a detailed, step-by-step protocol for identifying robust biomarker panels, integrating RFE with other bioinformatics and machine learning techniques. The workflow is summarized in the diagram below.
Sample Preparation and Data Generation
Objective: To generate high-quality transcriptomic profiles from patient samples.
Detailed Protocol:
Patient Cohort Selection:
- Recruit cases and controls with matched age and BMI. For POI studies, diagnostic criteria include age < 40 years, at least 4 months of oligo/amenorrhea, and serum basal FSH > 25 IU/L on two occasions >4 weeks apart [70].
- Exclusion Criteria: History of ovarian surgery, other endocrine diseases, or recent hormone therapy (e.g., within 3 months) [70].
- Collect relevant clinical data (e.g., AMH, FSH, LH, E2, AFC, age, BMI).
Sample Collection and RNA Extraction:
- Collect peripheral blood (e.g., 2.5 ml) in PAXgene Blood RNA tubes during days 2-4 of the menstrual cycle after a 12-hour fast [70].
- Extract total RNA using a matching kit (e.g., PAXgene Blood Kit). Assess RNA quality using metrics such as concentration (>40 ng/µL), OD260/280 ratio (1.7-2.5), and RNA Integrity Number (RIN ≥ 7) [70].
Library Preparation and Sequencing:
- Construct a cDNA library from qualified RNA samples.
- Perform sequencing using an appropriate platform (e.g., Oxford Nanopore Technology PromethION for long-read sequencing or Illumina for short-read) [70].
- Process raw data: align reads to a reference genome (e.g., using Minimap2 for ONT data), filter for identity and coverage, and obtain a final non-redundant sequence set for downstream analysis [70].
Bioinformatics Preprocessing and Differential Analysis
Objective: To process raw sequencing data and identify initial candidate genes.
Detailed Protocol:
Quantify Gene Expression: Calculate expression values (e.g., Counts Per Million - CPM). The formula is:
CPM = (R / T) * 1,000,000, where R is the number of reads aligned to a transcript and T is the total aligned fragments [70].Identify Differentially Expressed Genes (DEGs):
Functional and Pathway Enrichment Analysis:
- Perform Gene Set Enrichment Analysis (GSEA) using reference gene sets (e.g., C2.KEGG, Hallmark) to identify pathways enriched in the POI group [70]. A normalized enrichment score (NES) with |NES| > 1 and p < 0.05 indicates significant enrichment.
- Conduct functional annotation of DEGs using Gene Ontology (GO) and KEGG pathway databases [70].
- Identify core genes that are major contributors to the enrichment scores in significant pathways [70].
Protein-Protein Interaction (PPI) Network Construction:
- Input the core genes/DEGs into the STRING database to build a PPI network.
- Import the network into Cytoscape software and use algorithms (e.g., CytoHubba) to identify top hub genes based on connectivity [70].
Machine Learning-Based Feature Selection
Objective: To refine the candidate gene set and identify a minimal, optimal biomarker panel.
Detailed Protocol:
Data Preparation for Modeling:
Implementing Random Forest and Boruta for Feature Filtering:
- Rationale: The Boruta algorithm is a robust wrapper method that uses a Random Forest classifier to identify features that are significantly relevant compared to random shadow features [70].
- Implementation: Use the
Borutapackage in R or Python. Run the algorithm with the training data, using the hub genes and other candidates as input features. - Features confirmed as significant by the Boruta algorithm are carried forward [70].
Recursive Feature Elimination with Cross-Validation:
- Implementation in R using
caret:- Set up control parameters for RFE using
rfeControl, specifying the algorithm (e.g.,rfFuncsfor Random Forest) and resampling method (e.g., repeated 10-fold cross-validation with 5 repeats) [73]. - Use the
rfefunction with the training data, specifying a range of feature subset sizes to evaluate (e.g.,sizes = 1:13) [73]. - The output will recommend an optimal number of features and provide a ranked list.
- Set up control parameters for RFE using
- Implementation in Python using
scikit-learn:- Use the
RFECVclass for RFE with cross-validation [75]. - Specify the estimator (e.g.,
LogisticRegression()), scoring strategy (e.g.,scoring="accuracy"), and cross-validation strategy (e.g.,StratifiedKFold(5)) [75]. - After fitting the model (
rfecv.fit(X, y)), then_features_attribute gives the optimal number of features [75].
- Use the
- Decision Variant: Apply an appropriate decision variant (see Table 1) to automatically select the final feature subset. A voting strategy across folds or selecting a subset from a performance plateau can be more robust than simply selecting the highest accuracy subset [74].
- Implementation in R using
Experimental Validation
Objective: To technically validate the expression of identified biomarkers in an independent sample set.
Detailed Protocol:
- Independent Sample Collection: Recollect a new set of patient and control peripheral blood samples (e.g., 20 POI, 20 control) [70].
- qRT-PCR Assay:
- Extract monocytes using lymphocyte isolation liquid and total RNA with TRIzol reagent.
- Synthesize first-strand cDNA.
- Perform qRT-PCR with candidate gene primers and a reference gene (e.g., GAPDH).
- Calculate relative expression levels using the 2^(-ΔΔCt) method [70].
- Statistical Analysis: Compare expression levels between groups using Student's t-test or Mann-Whitney U test. Assess correlation with clinical parameters using Pearson correlation coefficient [70].
Table 2: Key Research Reagent Solutions for Biomarker Discovery Workflows
| Item/Category | Specific Examples | Function/Purpose |
|---|---|---|
| RNA Stabilization & Extraction | PAXgene Blood RNA Tube (BD); PAXgene Blood Kit; TRIzol Reagent (Invitrogen) | Maintains RNA integrity in whole blood; isolates total RNA from monocytes/cells [70] |
| cDNA Synthesis & qPCR | SweScript All-in-One cDNA Kit (Servicebio); SYBR Green qPCR Master Mix (ServiceBio) | Reverse transcribes RNA to cDNA; enables quantitative PCR amplification and detection [70] |
| Bioinformatics Analysis Tools | DESeq2, EdgeR, Limma R package; GATK, STAR, HISAT2; STRING; Cytoscape | Differential expression analysis; genomic alignment and variant calling; PPI network analysis and visualization [71] [70] |
| Machine Learning Frameworks | caret R package; scikit-learn (Python); Boruta R/Package; randomForest R package |
Provides unified interface for model training and RFE; implements core ML algorithms and RFE; performs robust feature selection [73] [70] |
| Data Repositories & Platforms | Gene Expression Omnibus (GEO); cBioPortal; The Cancer Genome Atlas (TCGA) | Public repository for functional genomics data; integrative exploration of cancer genomics datasets [71] [76] |
Anticipated Results and Interpretation
A successful execution of this protocol using POI patient data is expected to yield a panel of 3-8 validated biomarker genes. For example, one study identified seven candidate genes (COX5A, UQCRFS1, LCK, RPS2, EIF5A, etc.), five of which showed consistent expression via qRT-PCR, indicating their potential as biomarkers [70]. The RFE process should clearly show a performance peak or plateau at the optimal number of features, similar to the finding that 8 features provided the highest accuracy in a heart disease prediction model [73].
The functional enrichment analysis (GSEA) should reveal biologically relevant pathways. In the POI context, this might include the inhibition of the PI3K-AKT pathway, oxidative phosphorylation, and DNA damage repair pathways, along with the activation of inflammatory and apoptotic pathways [70]. This provides crucial mechanistic insight beyond a simple list of biomarkers.
The final logical relationship between the selected biomarker panel, the enriched biological pathways, and the clinical phenotype is encapsulated in the following diagram.
Troubleshooting and Best Practices
- Addressing Overfitting: The primary pitfall in biomarker discovery is overfitting, especially with small sample sizes and high-dimensional data. Mitigation strategies include the use of cross-validation at every stage (as in RFE-CV), independent validation on hold-out test sets, and finally, experimental validation in a new patient cohort [47] [75].
- Ensuring Model Interpretability: While complex models like deep learning can be powerful, they often offer limited interpretability. For biomarker discovery, simpler, more interpretable models (e.g., Random Forests, Logistic Regression) are often preferable, as they allow researchers to understand the contribution of each feature and generate testable biological hypotheses [47].
- Handling Data Complexity: For truly integrative models, employ multi-omics data fusion techniques. Cloud-based platforms (e.g., Galaxy, DNAnexus) and standardized bioinformatics pipelines are essential for managing the scale and complexity of data from genomics, transcriptomics, proteomics, and metabolomics [71].
The application of machine learning (ML) in biomarker discovery for predicting patient outcomes and drug efficacy represents a paradigm shift in precision medicine. However, the generalizability and clinical utility of these models are critically dependent on the representativeness of the underlying training data [9]. Bias—systematic errors that lead to unfair or inaccurate predictions for specific subpopulations—can be introduced throughout the ML lifecycle, potentially exacerbating healthcare disparities and undermining the validity of research findings [77] [78]. In biomarker research, where models aim to identify molecular, genetic, or digital indicators of biological processes or therapeutic responses, biased models risk misdirecting drug development efforts and failing vulnerable patient groups [9]. This Application Note provides a structured framework and practical protocols for identifying, assessing, and mitigating bias to ensure the development of generalizable ML models in biomarker discovery.
Background: The Bias Challenge in Biomarker Research
Biomarker-driven predictive models rely on multi-modal data, including genomics, proteomics, transcriptomics, and digital biomarkers from wearable devices [9]. The complexity and high dimensionality of these data create numerous avenues for bias. A systematic evaluation of healthcare AI models revealed that 50% demonstrated a high risk of bias, often stemming from absent sociodemographic data, imbalanced datasets, or weak algorithm design [77]. Furthermore, a review of neuroimaging-based AI models for psychiatric diagnosis found that 83% were rated at high risk of bias, with 97.5% including only subjects from high-income regions [77]. Such biases can lead to models that perform well for the average population but fail for underrepresented groups, ultimately compromising their translational value in drug development [79].
Quantifying the Bias Problem: Key Evidence
Table 1: Documented Prevalence and Impact of Bias in Healthcare AI
| Study Focus | Findings on Bias & Representativeness | Implication for Biomarker Research |
|---|---|---|
| General Healthcare AI Models [77] | 50% of 48 evaluated studies showed high risk of bias (ROB); only 20% had low ROB. | Highlights pervasive quality issues in model development that can affect biomarker discovery. |
| Neuroimaging AI for Psychiatry [77] | 83% of 555 models had high ROB; 97.5% used data solely from high-income regions. | Indicates severe geographic and demographic skew in foundational data for biomarker development. |
| Racial Bias in Clinical ML [78] | 67% of evaluated models exhibited racial bias; fairness metrics and mitigation strategies were inconsistently applied. | Underscores the need for standardized fairness evaluation and mitigation protocols in biomarker studies. |
A Framework for Mitigation: The ACAR Lifecycle Approach
Mitigating bias requires a systematic, lifecycle-oriented approach. The ACAR framework (Awareness, Conceptualization, Application, Reporting) provides a structured pathway for integrating fairness considerations from model conception to deployment [80].
Diagram 1: The ACAR Framework for mitigating algorithmic bias across the machine learning lifecycle, from initial awareness to post-deployment monitoring [80].
Awareness and Conceptualization
The initial phases involve identifying potential sources of bias and defining fairness goals. This includes specifying protected subgroups (e.g., by race, ethnicity, sex, age, socioeconomic status) and selecting appropriate fairness metrics aligned with the clinical context of the biomarker [78] [80].
Application and Reporting
The application phase involves implementing technical mitigation strategies, while reporting ensures transparency and accountability. Post-deployment monitoring is crucial to detect performance degradation or domain shift when the model encounters real-world data that differs from the training set [79] [77].
Experimental Protocols for Bias Assessment and Mitigation
Protocol 1: Representative Data Collection and Sampling
Objective: To assemble a dataset that accurately reflects the demographic, clinical, and genetic diversity of the target population for the biomarker.
- Define Target Population: Precisely specify the target population for the biomarker, including relevant demographic, clinical, genomic, and geographic characteristics [81].
- Sampling Method Selection: Prioritize probability sampling methods (e.g., stratified random sampling) to ensure all segments of the target population have a known, non-zero chance of selection, thereby enhancing representativeness [81].
- Sample Size Estimation: Calculate the minimum required sample size using power analysis to ensure the study is adequately powered to detect meaningful effects across predefined subgroups [81].
- Data Transparency Reporting: Document and report the demographic and baseline characteristics of the collected dataset, including distributions of age, race, ethnicity, sex, and clinical severity, using standardized reporting checklists like PROBAST (Prediction model Risk Of Bias Assessment Tool) [79].
Protocol 2: Preprocessing and Model Development Mitigation
Objective: To identify and mitigate biases present in the data and during model training.
- Bias Auditing: Prior to model training, conduct a thorough audit of the dataset. Calculate metrics such as Disparate Impact (ratio of positive outcome rates between groups) and Accuracy across subgroups to identify imbalances [78].
- Preprocessing Techniques:
- Oversampling: For underrepresented groups in the training data, use techniques like SMOTE (Synthetic Minority Over-sampling Technique) to synthetically balance class distributions [79].
- Reweighting: Assign differential weights to instances from different subgroups during model training to compensate for underrepresentation [78].
- In-processing Mitigation: During model training, employ fairness-aware algorithms. Adversarial De-biasing is a prominent technique where the primary model is trained to perform its task (e.g., predict a biomarker) while an adversarial model simultaneously tries to predict the protected attribute (e.g., race) from the primary model's predictions. This forces the primary model to learn features that are informative for the task but not for the protected attribute [79].
Protocol 3: Model Evaluation and Fairness Validation
Objective: To rigorously evaluate model performance and fairness on an independent, held-out test set that includes diverse subgroups.
- Subgroup Performance Analysis: Evaluate model performance not just overall, but separately for all predefined subgroups. Key metrics to report include sensitivity, specificity, and area under the receiver operating characteristic curve (AUROC) for each group [79] [78].
- Fairness Metric Calculation: Quantify algorithmic fairness using a suite of metrics. No single metric is sufficient; a combination must be used based on the clinical context [78].
- Equal Opportunity Difference: Measures the difference in true positive rates (sensitivity) between groups. An ideal value is 0.
- Average Odds Difference: Measures the average of the differences in true positive rates and false positive rates between groups. An ideal value is 0.
- Calibration: Assesses whether the predicted probabilities of an outcome reflect the true underlying probabilities for all subgroups. A model is well-calibrated if, for example, among patients assigned a risk score of 80%, 80 out of 100 actually have the outcome, regardless of their subgroup [78].
Table 2: Key Fairness Metrics for Model Evaluation in Biomarker Research
| Metric | Definition | Ideal Value | Clinical Interpretation |
|---|---|---|---|
| Equal Opportunity Difference [78] | Difference in True Positive Rates (Sensitivity) between groups. | 0 | The model is equally sensitive to the condition in all groups. |
| Average Odds Difference [78] | Average of (TPR difference + FPR difference) between groups. | 0 | The model's balance of sensitivity and specificity is similar across groups. |
| Disparate Impact [78] | Ratio of the rate of favorable outcomes for an unprivileged group to a privileged group. | 1 | The probability of a beneficial prediction is equal across groups. |
| Calibration [78] | Agreement between predicted probabilities and actual observed outcomes across groups. | Well-calibrated | A predicted risk score of X% means the same thing for every patient, regardless of subgroup. |
Protocol 4: Post-Deployment Monitoring and Continual Learning
Objective: To ensure model performance remains robust and unbiased in a dynamic clinical environment.
- Performance Monitoring: Implement continuous monitoring of the model's real-world performance, tracking key performance and fairness metrics discussed in Protocol 3 [79].
- Domain Shift Detection: Actively monitor the sociodemographic and clinical characteristics of incoming patient data. Compare these distributions to the training data to detect "domain shift," where the model is applied to a population different from the one it was trained on [79].
- Model Updating: Establish a protocol for model updating and retraining using Continual Learning approaches. This allows the model to integrate new, post-deployment data while retaining previously learned knowledge, thereby adapting to evolving patient populations and clinical practices without catastrophic forgetting [79].
Diagram 2: The sequential experimental workflow for ensuring representative data and mitigating bias, highlighting the critical feedback loop for continuous model improvement.
Table 3: Key Research Reagent Solutions for Bias-Resistant Biomarker Research
| Tool / Resource | Type | Primary Function in Bias Mitigation |
|---|---|---|
| PROBAST / PROBAST-AI [79] [80] | Reporting Checklist | Provides a structured tool for assessing the risk of bias and applicability of predictive model studies. |
| SHAP / LIME [79] | Explainability Tool | Enhances model transparency by explaining individual predictions, helping to identify if the model relies on spurious or biased correlates. |
| Adversarial De-biasing [79] | Algorithm | An in-processing mitigation technique that removes dependency on protected attributes from model representations. |
| ACAR Framework [80] | Conceptual Framework | Guides researchers through the stages of Awareness, Conceptualization, Application, and Reporting to embed fairness in the research lifecycle. |
| Stratified Sampling [81] | Methodology | A probability sampling technique that ensures adequate representation of key subgroups in the study population. |
| Fairness Metrics (e.g., Equalized Odds) [78] | Analytical Metric | Quantitative measures used to evaluate and validate the fairness of a model across protected subgroups. |
Ensuring representative data and mitigating bias is not a one-time check but a continuous, integral part of the ML lifecycle in biomarker discovery. By adopting the structured protocols and frameworks outlined in this Application Note—from rigorous sampling and preprocessing to comprehensive fairness evaluation and post-deployment monitoring—researchers and drug development professionals can significantly enhance the generalizability, reliability, and equity of their predictive models. This systematic commitment to fairness is foundational for building trustworthy AI tools that can successfully translate from the research environment to broad clinical application, ultimately ensuring that biomarker-driven innovations benefit all patient populations equitably.
From Model to Clinic: Validation Frameworks and Comparative Performance Analysis
In machine learning-based biomarker discovery, robust validation is not merely a final step but a fundamental component that underpins the development of clinically relevant and trustworthy models. The inherent complexity of biological data, often characterized by high dimensionality and small sample sizes, makes models particularly susceptible to overfitting and optimistic performance estimates [82] [8]. Within the specific context of precision medicine, where biomarkers are critical for diagnosis, prognosis, and personalized treatment strategies, a rigorous validation framework is essential to ensure that identified patterns are generalizable and reproducible [8]. This document outlines established validation paradigms—hold-out sets, cross-validation, and external validation—detailing their application, comparative advantages, and implementation protocols specifically for biomarker discovery research.
Core Validation Concepts and Their Importance in Biomarker Research
Validation techniques are designed to estimate the performance of a predictive model on unseen data, providing a safeguard against the aforementioned overfitting. The choice of validation strategy directly impacts the reliability and clinical translatability of a biomarker signature [83].
- Internal Validation assesses model performance using data derived from the same population or study that generated the training data. Its primary purpose is to provide a realistic estimate of model performance during development and to guide model selection. Key techniques include the hold-out method and cross-validation [82] [84].
- External Validation evaluates the model on a completely independent dataset, often collected from a different institution, population, or using alternative protocols [82] [83]. This is the gold standard for demonstrating that a biomarker model can generalize beyond its development context and is a critical step toward clinical application [83].
- Overfitting occurs when a model learns not only the underlying signal in the training data but also the statistical noise. This results in a model that performs exceptionally well on its training data but fails to generalize to new, unseen samples [85]. Techniques like cross-validation are designed to detect and mitigate this risk.
Hold-Out Validation
The hold-out method is the simplest form of validation, involving a single split of the dataset into two distinct subsets: a training set and a test (or hold-out) set [86] [87].
Table 1: Characteristics of the Hold-Out Method
| Aspect | Description |
|---|---|
| Core Principle | Single random partition of the dataset into a training set and a test set. |
| Typical Split Ratio | 70-80% for training; 20-30% for testing [87]. |
| Key Advantage | Computationally efficient and straightforward to implement. |
| Major Disadvantage | Performance estimate can have high variance, depending on a single, potentially unlucky, data split. The hold-out set reduces the amount of data available for training [82] [86]. |
| Ideal Use Case | Very large datasets where a single, large test set is representative of the overall data distribution. |
Cross-Validation (CV)
Cross-validation provides a more robust estimate of model performance by using multiple data splits. The most common form is k-Fold Cross-Validation [85] [86].
Table 2: Comparison of Common Cross-Validation Techniques
| Technique | Procedure | Advantages | Disadvantages | Suitability for Biomarker Data |
|---|---|---|---|---|
| k-Fold CV | Data partitioned into k folds. Model trained on k-1 folds and validated on the remaining fold; process repeated k times [85] [87]. | More reliable performance estimate than hold-out; all data used for training and validation. | Higher computational cost; performance can vary with different random splits. | General purpose; good for most small to medium-sized datasets [82]. |
| Stratified k-Fold CV | Ensures each fold has approximately the same proportion of target classes as the complete dataset [87]. | Prevents skewed performance estimates in imbalanced datasets. | Slightly more complex implementation. | Highly recommended for classification in biomarker studies, where class imbalance (e.g., case vs. control) is common [84]. |
| Leave-One-Out CV (LOOCV) | A special case of k-fold where k equals the number of samples (n). Each sample is used once as a test set [86] [87]. | Virtually unbiased estimate; uses maximum data for training. | Computationally very expensive for large n; high variance in estimate [87]. | Small, very costly-to-obtain datasets (n < 50). |
| Repeated k-Fold CV | k-Fold CV is repeated multiple times with different random partitions [87]. | More stable and reliable performance estimate. | Further increases computational cost. | When a highly robust internal performance estimate is needed. |
| Nested CV | Uses an outer k-fold loop for performance estimation and an inner k-fold loop for hyperparameter tuning [84]. | Provides an almost unbiased estimate of the true error of a model tuned via CV; prevents data leakage. | Very computationally intensive. | Essential for model selection and hyperparameter tuning when no separate external validation set is available [84]. |
External Validation
External validation involves testing a final model, developed on the entire initial dataset, on a completely independent cohort of patients [82] [83]. This is a critical step for verifying that a biomarker signature is not specific to the idiosyncrasies of the original study population (e.g., specific demographics, sample collection protocols, or assay platforms). A significant drop in performance upon external validation indicates limited generalizability and is a major hurdle for clinical adoption [83]. The independent dataset should be plausibly related but collected from a different clinical center, or at a different time, or should exhibit known and relevant variations in patient characteristics (e.g., different cancer stages, comorbidities) or technical measurements (e.g., different PET reconstruction parameters as simulated in [82]).
Quantitative Comparison of Validation Methods
Simulation studies provide empirical evidence for the relative performance of different validation paradigms. The table below summarizes findings from a study that simulated data from diffuse large B-cell lymphoma patients to compare validation approaches [82].
Table 3: Simulation-Based Comparison of Validation Method Performance
| Validation Method | Reported AUC (Mean ± SD)* | Key Observations from Simulation | Interpretation for Biomarker Research |
|---|---|---|---|
| 5-Fold Cross-Validation | 0.71 ± 0.06 | Stable performance estimate with moderate uncertainty. | Preferred internal method for small datasets; provides a good balance between bias and variance [82]. |
| Hold-Out (n=100 test set) | 0.70 ± 0.07 | Comparable mean performance to CV, but with higher uncertainty. | Using a single holdout set in small datasets is not advisable due to large uncertainty in the performance estimate [82]. |
| Bootstrapping | 0.67 ± 0.02 | Lower mean AUC and smaller standard deviation. | Can provide a less optimistic, stable estimate. |
| External Validation (n=100) | Similar to hold-out | Performance precision increases with the size of the external test set. | A single small external dataset suffers from large uncertainty; larger independent cohorts are needed for conclusive validation [82]. |
*Area Under the Curve (AUC) is a common metric for model discrimination, where 1.0 is perfect and 0.5 is random. SD = Standard Deviation.
Practical Experimental Protocols
Protocol 1: Implementing Stratified k-Fold Cross-Validation for a Binary Biomarker Classifier
This protocol is designed for a typical scenario in biomarker discovery: building a classifier to predict a binary outcome (e.g., responder vs. non-responder) from high-dimensional molecular data.
1. Objective: To obtain a robust internal performance estimate for a candidate biomarker model while accounting for potential class imbalance. 2. Materials:
- Dataset with
nsamples (rows) andpfeatures (columns), plus a corresponding outcome vectory(binary labels). - A machine learning environment (e.g., Python with scikit-learn).
3. Procedure:
a. Data Preprocessing: Standardize the feature matrix (e.g., using
StandardScaler). Critical: Fit the scaler on the training folds and transform the test fold in each split to avoid data leakage. [85] b. Model & CV Setup: Choose an algorithm (e.g., Logistic Regression with L1 penalty, Support Vector Machine). InitializeStratifiedKFoldwithn_splits=5or10. c. Cross-Validation Loop: For each split in theStratifiedKFold: i. Split data into training and test folds, preserving the class distribution. ii. Preprocess the data as described in (a). iii. Train the model on the training folds. iv. Predict on the test fold and calculate performance metrics (e.g., AUC, accuracy, precision, recall). d. Performance Calculation: Aggregate the metrics from all folds. Report the mean and standard deviation (e.g., AUC = 0.92 ± 0.03). 4. Output: A robust estimate of the model's generalization performance on data from a similar population.
Protocol 2: Designing an External Validation Study for a Prognostic Biomarker Signature
This protocol outlines the steps for the crucial process of externally validating a previously developed model.
1. Objective: To assess the generalizability and clinical transportability of a locked-down biomarker model in an independent patient cohort. 2. Materials:
- The finalized predictive model (trained on the full development dataset).
- An independent dataset, collected prospectively or from a different institution. The dataset must contain the same features and outcome definition. 3. Procedure: a. Cohort Definition: Define the external validation cohort based on the intended use of the biomarker. Clearly document inclusion/exclusion criteria and patient characteristics. b. Data Harmonization: Map variables in the external dataset to those required by the model. Account for potential technical batch effects (e.g., using ComBat) or differences in measurement platforms [82]. c. Model Application: Apply the locked model (no retraining) to the external dataset to generate predictions. d. Performance Assessment: i. Discrimination: Calculate the AUC or C-index. ii. Calibration: Assess the agreement between predicted probabilities and observed outcomes using a calibration plot and slope. A slope < 1 indicates overfitting, while >1 indicates underfitting [82]. e. Clinical Utility: If possible, evaluate the model's impact on decision-making, for example, by assessing net benefit using decision curve analysis. 4. Output: An unbiased assessment of the model's performance in a new population, which is critical for judging its readiness for clinical use [83].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Computational Tools for Biomarker Validation
| Tool / Reagent | Function in Validation | Example / Note |
|---|---|---|
| scikit-learn (Python) | Provides implementations for all major validation methods (e.g., KFold, StratifiedKFold, train_test_split), metrics, and ML algorithms [85] [11]. |
The cross_val_score and cross_validate functions streamline the CV process [85]. |
R caret / tidymodels |
Comprehensive suites for machine learning and validation in R, offering similar functionality to scikit-learn. | Facilitates reproducible model training and validation workflows. |
| Pipelines (sklearn) | Encapsulates preprocessing and model training steps to ensure they are correctly applied within each CV fold, preventing data leakage [85]. | make_pipeline(StandardScaler(), SVM(C=1)) |
| Biocrates Absolute IDQ p180 Kit | A targeted metabolomics kit used to quantify metabolites from plasma/serum, generating data for biomarker discovery and validation [11]. | Used in a study to discover metabolites predictive of large-artery atherosclerosis, validated via ML [11]. |
| Electronic Health Record (EHR) Data | A source of real-world clinical data for model development and, crucially, for external validation [84] [83]. | Requires careful handling of irregular sampling, missingness, and subject-wise splitting to avoid biased results [84]. |
| Radiomics Software (e.g., PyRadiomics) | Extracts quantitative features from medical images, which serve as high-dimensional input for predictive models requiring robust validation [82] [83]. | Used in studies validating radiomic signatures for cancer prognosis [82]. |
The journey from a promising machine learning model to a clinically useful biomarker requires a rigorous, multi-faceted validation strategy. Internal validation techniques, particularly stratified and nested cross-validation, are indispensable for reliable model development and selection, especially when dealing with the high-dimensional, small-sample-size datasets typical in biomarker research. However, internal validation alone is insufficient. External validation on independent, well-characterized cohorts remains the definitive test of a model's generalizability and is a non-negotiable step toward clinical translation. By systematically applying the protocols and considerations outlined in this document, researchers can enhance the robustness, credibility, and ultimately, the clinical impact of their biomarker discoveries.
Within the field of machine learning (ML) for biomarker discovery, the rigorous benchmarking of model performance is not merely a technical formality but the foundation of translational credibility. The selection and interpretation of key performance metrics—primarily the Area Under the Receiver Operating Characteristic Curve (AUC), Accuracy, and F1-Score—are critical for validating the potential of predictive biomarkers in clinical and research settings [47] [35]. These metrics provide a quantitative framework for assessing a model's ability to distinguish between health and disease, predict disease progression, or stratify risk, thereby guiding decisions on which models warrant further investment and validation. This document provides detailed application notes and protocols for the calculation, interpretation, and contextualization of these metrics, framed within the specific requirements of predictive biomarker (POI) research for researchers, scientists, and drug development professionals. The integration of explainability frameworks, such as SHapley Additive exPlanations (SHAP), further enriches this process by ensuring that high-performing models are also biologically interpretable, linking model predictions to underlying pathophysiology [88] [89].
Performance Metrics in Biomarker Research: Definition and Protocol
A deep understanding of each metric's calculation and strategic implication is essential for accurate model benchmarking. The following section delineates the experimental protocols for their derivation and their contextual significance.
Key Metric Definitions and Calculations
Area Under the Receiver Operating Characteristic Curve (AUC-ROC)
- Experimental Protocol: The ROC curve is generated by plotting the True Positive Rate (TPR) against the False Positive Rate (FPR) at various probability threshold settings. The AUC is then calculated as the integral of this curve. In practice, this involves using functions such as
roc_curveandaucfrom libraries likescikit-learnin Python. The model's predicted probabilities for the test set are used as the input. - Context of Use: AUC is the preferred metric for evaluating a model's discriminative ability, independent of any specific classification threshold. It is particularly valuable in early-stage biomarker discovery where the optimal operational threshold is not yet known. An AUC above 0.9 is considered excellent, as demonstrated in a gastric cancer staging model [88], while an AUC of 0.891 for predicting interstitial lung disease in rheumatoid arthritis patients indicates strong performance [90].
- Experimental Protocol: The ROC curve is generated by plotting the True Positive Rate (TPR) against the False Positive Rate (FPR) at various probability threshold settings. The AUC is then calculated as the integral of this curve. In practice, this involves using functions such as
Accuracy
- Experimental Protocol: Accuracy is calculated as (True Positives + True Negatives) / Total Predictions. This is a standard metric provided by most ML model evaluation functions (e.g.,
accuracy_scoreinscikit-learn). It requires first applying a threshold (typically 0.5 for binary classification) to the model's output probabilities to generate class labels. - Context of Use: Accuracy provides a straightforward measure of overall correctness. However, its utility can be misleading in the presence of class imbalance, which is common in biomedical datasets. For instance, a study on osteoarthritis prediction reported an accuracy of 0.6245, which, while modest, must be interpreted in the context of the dataset's prevalence [89].
- Experimental Protocol: Accuracy is calculated as (True Positives + True Negatives) / Total Predictions. This is a standard metric provided by most ML model evaluation functions (e.g.,
F1-Score
- Experimental Protocol: The F1-score is the harmonic mean of Precision and Recall: F1 = 2 * (Precision * Recall) / (Precision + Recall). Precision is calculated as True Positives / (True Positives + False Positives), and Recall as True Positives / (True Positives + False Negatives). These are calculated after applying a classification threshold.
- Context of Use: The F1-score is the critical metric when there is an uneven class distribution and the cost of false positives and false negatives is high. It balances the competing demands of precision (avoiding false discoveries) and recall (identifying all true cases). In the ovarian cancer domain, models achieving high F1-scores are considered robust for diagnostic applications [35].
Structured Comparison of Metrics in Recent Studies
Table 1: Benchmarking Performance Metrics Across Recent Biomarker Discovery Studies
| Disease Context | ML Model | AUC | Accuracy | F1-Score | Primary Biomarkers |
|---|---|---|---|---|---|
| Gastric Cancer Staging [88] | CatBoost | 0.9499 | N/R | N/R | Uric Acid, APTT, Engineered Ratios |
| RA-ILD Prediction [90] | XGBoost | 0.891 | N/R | N/R | KL-6, IL-6, CYFRA21-1 |
| Osteoarthritis Prediction [89] | Gradient Boosting | N/R | 0.6245 | 0.6232 | Derived Blood/Urine Biomarkers |
| Ovarian Cancer Detection [35] | Ensemble Methods | > 0.90 | Up to 99.82% | N/R | CA-125, HE4, CRP, NLR |
Abbreviations: N/R = Not explicitly reported in the search results; RA-ILD = Rheumatoid Arthritis-Associated Interstitial Lung Disease.
Experimental Protocol for Model Benchmarking
A robust benchmarking workflow is essential for generating credible, reproducible performance metrics. The following protocol outlines the key stages from data preparation to final evaluation.
The following diagram illustrates the end-to-end experimental workflow for benchmarking a machine learning model in biomarker research.
Detailed Methodology
Data Preprocessing and Feature Engineering
- Data Imputation: Handle missing values using appropriate methods. The K-nearest neighbors (KNN) algorithm (e.g.,
KNNImputerwith k=5) is a robust choice for clinical laboratory data [88]. Exclude variables with a high percentage (>40%) of missing values. - Feature Engineering: Construct biologically informed ratio and composite features to enhance model performance. This is a critical step, as demonstrated in gastric cancer research where incorporating ratios (e.g., neutrophil-to-lymphocyte ratio, apolipoprotein ratios) significantly boosted the AUC from 0.802 to 0.981 [88].
- Class Imbalance Handling: Address class imbalance using techniques like the Synthetic Minority Over-sampling Technique combined with Edited Nearest Neighbors (SMOTEEN) [88].
- Data Splitting: Split the dataset into training (80%) and testing (20%) sets, ensuring stratification by the target variable to maintain class distribution [88] [90].
- Data Imputation: Handle missing values using appropriate methods. The K-nearest neighbors (KNN) algorithm (e.g.,
Model Training and Validation
- Algorithm Selection: Systematically evaluate a suite of supervised ML algorithms. Common high-performing algorithms in biomarker research include XGBoost, CatBoost, Random Forest, and Support Vector Machines [88] [90] [35].
- Hyperparameter Tuning: Optimize model hyperparameters using techniques like competitive random halving [44] or grid search coupled with cross-validation.
- Robust Validation: Employ 10-fold cross-validation on the training set to assess model stability. The final model performance must be reported on the held-out test set [88] [90]. For the highest rigor, perform 1000 bootstrap iterations on the test set to generate confidence intervals for performance metrics (e.g., 95% CI for AUC) [88].
Performance Evaluation and Interpretation
- Metric Calculation: Calculate AUC, Accuracy, Precision, Recall, and F1-score on the test set predictions.
- Explainability Analysis: Use SHapley Additive exPlanations (SHAP) to interpret the model. This identifies key predictive biomarkers (e.g., KL-6 in RA-ILD [90]) and verifies the biological plausibility of the model through interaction analysis [88] [89].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Platforms for Biomarker ML Research
| Item | Function/Application | Example Use Case |
|---|---|---|
| LUMIPULSE G1200 (Fujirebio) | Automated immunoassay system for quantifying protein biomarkers. | Measurement of KL-6, a key biomarker for predicting RA-ILD [90]. |
| Cobas e411 (Roche) | Electrochemiluminescence immunoassay analyzer. | Quantification of cytokines (e.g., IL-6) and cancer markers (e.g., CYFRA21-1) [90]. |
| Anti-MMR Antibodies (MLH1, MSH2, MSH6, PMS2) | Immunohistochemistry (IHC) reagents for assessing mismatch repair status. | Defining deficient MMR (dMMR) as a biomarker in gastric cancer studies [88]. |
| scikit-learn (Python Library) | Open-source library for machine learning, providing tools for preprocessing, model training, and evaluation. | Implementing SVM, LR, and data preprocessing steps like standardization and imputation [89] [90]. |
| XGBoost / CatBoost Libraries | Optimized gradient boosting libraries for building high-performance classification models. | Developing top-performing models for gastric cancer staging and RA-ILD prediction [88] [90]. |
| SHAP (Python Library) | A game theoretic approach to explain the output of any machine learning model. | Interpreting model predictions and identifying key biomarkers like uric acid and APTT in gastric cancer [88] [89]. |
Interpreting Metric Relationships and Trade-offs
Understanding the interplay between metrics is crucial for a holistic benchmark. The following diagram conceptualizes the relationship between the core metrics and the classification process.
Strategic Interpretation:
- AUC provides the overarching assessment of a model's separation power. It is an inherent property evaluated across all possible thresholds, making it the primary metric for initial biomarker screening [35].
- F1-Score and Accuracy are threshold-dependent. The F1-score becomes the metric of focus when the class distribution is imbalanced or when both false positives and false negatives carry significant cost. For example, in a screening context, a high recall (part of the F1-score) is often prioritized to minimize false negatives, even at the expense of more false positives [35].
- Researchers must align the choice of the primary metric with the clinical or research objective. A high AUC is necessary but not sufficient; the operational metric (F1 or Accuracy) must also be acceptable at a feasible probability threshold.
The rigorous benchmarking of machine learning models using AUC, Accuracy, and F1-score is a non-negotiable standard in biomarker discovery. As evidenced by recent research across gastric cancer, RA-ILD, and ovarian cancer, these metrics provide a multi-faceted view of model performance that, when combined with robust validation and explainability analysis, builds the foundation for translational success [88] [90] [35]. The protocols and frameworks detailed herein offer a structured pathway for researchers to generate credible, interpretable, and clinically relevant benchmarks, thereby accelerating the development of reliable predictive biomarkers in oncology and beyond.
Predictive biomarkers are indispensable to precision oncology, enabling the selection of targeted cancer therapies based on an individual's molecular profile [44]. The discovery of these biomarkers, however, remains challenging due to the complexity of cancer signaling networks and the limited scope of hypothesis-driven approaches [91]. MarkerPredict is a novel, computational framework designed to address this challenge by leveraging machine learning (ML), network topology, and protein structural features to systematically identify predictive biomarkers [44]. This case study details the framework's methodology, experimental validation, and implementation protocols, providing a resource for researchers in machine learning-based biomarker discovery.
The core innovation of MarkerPredict lies in its hypothesis-generating framework. It is founded on the observation that intrinsically disordered proteins (IDPs)—proteins lacking a fixed tertiary structure—are significantly enriched in key regulatory motifs within cancer signaling networks [44]. This integration of network motifs and protein disorder provides a mechanistic basis for discovering biomarkers that might be missed by conventional methods.
Materials and Methods
The MarkerPredict workflow integrates multiple data types and analysis steps to classify predictive biomarker potential. The following diagram illustrates the logical flow and relationships between the core components of the framework.
Signaling Network Curation
MarkerPredict operates on three signed protein-protein interaction networks to ensure comprehensive coverage:
- Human Cancer Signaling Network (CSN): A focused network of cancer-related pathways [44].
- SIGNOR: A repository of signaling relationships with activity states (e.g., activation, inhibition) [44].
- ReactomeFI: The Reactome Functional Interaction network, representing pathway-based relationships [44].
These networks provide the topological framework for identifying interactions between drug targets and their potential biomarkers. The networks vary in size and connectivity, contributing to the robustness of the findings [44].
Intrinsically Disordered Protein (IDP) Annotation
Protein disorder is defined using three complementary sources:
- DisProt: A curated database of experimentally determined IDPs [44].
- AlphaFold DB: Protein structure predictions where an average pLLDT score <50 indicates disorder [44].
- IUPred2.0: A computational tool that predicts disorder from amino acid sequence; an average score >0.5 indicates disorder [44].
The use of multiple definitions accounts for different types of evidence and increases confidence in the structural annotations.
Known Biomarker and Target Annotation
- CIViCmine: A text-mining database that annotates proteins with various biomarker types (predictive, prognostic, diagnostic) [44]. This is used to establish ground truth for model training.
- Oncotherapeutic Targets: A set of proteins that are known targets of approved or investigational cancer drugs [44].
Key Experimental Protocols
Protocol 1: Identification of Network Motifs and Target-Neighbor Pairs
Purpose: To identify tightly regulated, three-node subnetworks (triangles) containing both a drug target and a potential biomarker. Steps:
- Network Preprocessing: Load the three signaling networks (CSN, SIGNOR, ReactomeFI) using a network analysis library such as NetworkX.
- Motif Detection: Use the FANMOD software to identify all three-node motifs within each network [44].
- Triangle Selection: Filter the motifs to retain only fully connected three-node subgraphs ("triangles").
- Target and IDP Mapping: Annotate each node in the triangles using the provided lists of oncotherapeutic targets and IDPs (from DisProt, AlphaFold, and IUPred).
- Pair Generation: Extract all unique "target-neighbor pairs" from the triangles, where one node is a known target and another is its direct interaction partner (neighbor). These pairs form the candidate set for classification.
Protocol 2: Construction of Training Datasets
Purpose: To generate labeled data for supervised machine learning. Steps:
- Positive Controls (Class 1): A target-neighbor pair is assigned to the positive class if the neighbor protein is annotated in the CIViCmine database as a known predictive biomarker for drugs targeting its partner node [44]. The study identified 332 such positive pairs.
- Negative Controls (Class 0): The negative set is constructed from:
- Neighbor proteins that are not listed in the CIViCmine database at all.
- Randomly generated target-neighbor pairs that do not appear in the network motifs [44].
- The final training set consists of 880 target-interacting protein pairs in total [44].
Protocol 3: Feature Engineering and Model Training
Purpose: To train machine learning models that can distinguish true predictive biomarkers from non-biomarkers. Features: For each target-neighbor pair, features are derived from:
- Network Topology: The motif type and the structural role of the nodes within the network [44].
- Protein Properties: The disorder status of the neighbor protein from all three IDP sources [44].
Training Procedure:
- Model Selection: Implement two tree-based ensemble algorithms: Random Forest and XGBoost [44].
- Model Variants: Train separate models on each individual signaling network and on each individual IDP dataset, as well as on combined data. This results in 32 different models for a comprehensive analysis [44].
- Hyperparameter Tuning: Optimize model-specific parameters using competitive random halving search [44].
- Validation: Evaluate model performance using Leave-One-Out-Cross-Validation (LOOCV), k-fold cross-validation, and a 70:30 train-test split [44].
The Biomarker Probability Score (BPS)
To harmonize predictions across the 32 models, MarkerPredict defines a Biomarker Probability Score (BPS). The BPS is a normalized summative rank of the probability outputs from all models. This single score allows for the ranking of all target-neighbor pairs by their likelihood of being a valid predictive biomarker [44].
Performance of Machine Learning Models
The machine learning models powering MarkerPredict demonstrated high performance across multiple validation methods, indicating strong predictive capability.
Table 1: Performance Metrics of MarkerPredict Machine Learning Models during LOOCV [44]
| Model Type | Signaling Network | IDP Data Source | LOOCV Accuracy Range | AUC |
|---|---|---|---|---|
| XGBoost | Combined (All three) | Combined (All three) | 0.7 - 0.96 | High |
| Random Forest | Combined (All three) | Combined (All three) | Marginally underperformed XGBoost | High |
| All Models | CSN (Smallest network) | All | Less performant than other networks | Acceptable |
Classification Output and Biomarker Discovery
The application of MarkerPredict to the signaling networks led to the classification of a large number of potential predictive biomarkers.
Table 2: Summary of MarkerPredict Classification Output [44]
| Category | Number of Pairs | Description |
|---|---|---|
| Classified Target-Neighbor Pairs | 3,670 | Total pairs processed and scored by the framework. |
| Potential Predictive Biomarkers | 2,084 | Pairs with a high Biomarker Probability Score (BPS). |
| High-Confidence Biomarkers | 426 | Biomarkers classified positively by all four BPS calculations (individual and combined IDP data). |
The study highlighted the biomarker potential of LCK and ERK1 as specific examples from the high-confidence set [44].
The Scientist's Toolkit: Research Reagent Solutions
The following table details key software, data resources, and computational tools essential for implementing a framework like MarkerPredict.
Table 3: Essential Research Reagents and Computational Tools for ML-Based Biomarker Discovery
| Item Name | Type | Function in the Workflow | Source/Example |
|---|---|---|---|
| Signaling Networks | Data | Provides the topological framework for motif analysis. | CSN, SIGNOR, ReactomeFI [44] |
| IDP Databases & Tools | Data / Software | Annotates proteins with intrinsic structural disorder. | DisProt, IUPred2.0, AlphaFold DB [44] |
| Biomarker Database | Data | Provides ground-truth annotations for model training. | CIViCmine [44] |
| FANMOD | Software | Identifies recurring network motifs (e.g., triangles) in large networks. | FANMOD Tool [44] |
| Scikit-learn / XGBoost | Software | Provides machine learning algorithms for classification (Random Forest, XGBoost). | Python Libraries [44] |
Visualizing Key Signaling Pathways
MarkerPredict's analysis revealed that IDPs are enriched in specific network motifs, particularly three-node triangles, with drug targets. These motifs often represent core regulatory units within larger signaling pathways. The following diagram illustrates a generalized signaling pathway containing such a motif, highlighting the relationship between a target, a predictive biomarker, and a third regulatory protein.
Discussion and Future Perspectives
MarkerPredict establishes a robust, hypothesis-generating framework that integrates network science, protein biophysics, and machine learning for predictive biomarker discovery. The high performance of its models and the identification of over 2,000 potential biomarkers, including 426 high-confidence candidates, underscore its utility as a tool for accelerating precision oncology [44]. The framework is available on GitHub, providing the research community with a resource to prioritize biomarkers for experimental validation.
Future directions in the field will likely involve:
- Enhanced Generalizability: The application of ML frameworks like TrialTranslator to evaluate how trial results, and the biomarkers derived from them, translate to real-world patient populations with heterogeneous prognoses [92].
- Multi-Omics Integration: Combining genomic, proteomic, and transcriptomic data with network features to create more comprehensive biomarker profiles [91] [93].
- AI-Powered Discovery: Leveraging deep learning and contrastive learning to uncover complex, non-intuitive patterns in high-dimensional data beyond predefined network motifs [91] [94].
The convergence of these computational approaches promises to further refine the discovery and clinical application of predictive biomarkers, ultimately improving personalized cancer therapy.
The integration of machine learning into biomarker discovery has revolutionized precision medicine by enabling the identification of molecular, imaging, and metabolic signatures across diverse pathological conditions. This comparative analysis examines the performance of machine learning models in discovering and validating biomarkers for various diseases, including cancer, liver fibrosis, and hypoxic-ischemic encephalopathy. We evaluate analytical frameworks encompassing feature selection techniques, data normalization approaches, and validation methodologies that impact model efficacy and biomarker stability. By synthesizing findings from multiple studies, this analysis provides a standardized protocol for developing robust, clinically translatable biomarker signatures, addressing critical challenges in model generalization and performance verification across different biological contexts and data modalities.
Biomarker discovery represents a cornerstone of precision oncology and personalized medicine, enabling early disease detection, prognostic stratification, and prediction of therapeutic response. The emergence of high-throughput technologies has generated multidimensional datasets from genomic, metabolomic, and imaging platforms, creating unprecedented opportunities for biomarker identification through machine learning approaches [95]. However, the evaluation of model performance across different biomarker types and disease contexts presents significant methodological challenges, including data heterogeneity, feature redundancy, and cohort-specific biases that can compromise clinical translation [96] [97].
Machine learning frameworks have demonstrated remarkable utility in navigating the complexity of biological systems to identify biomarker signatures with diagnostic, prognostic, and predictive value. The comparative performance of these models varies substantially depending on the biomarker modality (e.g., genomic, metabolic, imaging), disease context, and analytical pipeline employed [44] [98]. Furthermore, the stability and biological interpretability of discovered biomarkers are influenced by pre-processing strategies, feature selection techniques, and validation approaches that collectively determine clinical utility [96] [97].
This application note provides a systematic evaluation of machine learning performance across diverse biomarker types and disease contexts, with emphasis on analytical protocols that enhance reproducibility and clinical applicability. Within the broader thesis of machine learning-driven biomarker discovery, we establish a standardized framework for model development, validation, and implementation across various biological domains and data modalities.
Biomarker Types and Analytical Challenges
Genomic Biomarkers
Genomic biomarkers encompass molecular signatures derived from gene expression, mutations, and epigenetic modifications that inform disease classification, prognosis, and therapeutic response. High-dimensional genomic data presents unique analytical challenges, including significant feature redundancy, technical noise, and biological heterogeneity that can obscure true biomarker signals [96]. Studies have employed various feature selection strategies to address these challenges, with multivariate approaches generally outperforming univariate methods in capturing biologically relevant gene interactions despite higher computational complexity [96].
Network-based analyses have emerged as powerful tools for contextualizing genomic biomarkers within biological pathways. For instance, MarkerPredict incorporates network motifs and protein disorder properties to identify predictive biomarkers for targeted cancer therapies, achieving leave-one-out cross-validation accuracy of 0.7-0.96 across 32 different models [44]. This approach leverages the observation that intrinsically disordered proteins are significantly enriched in network triangles and demonstrate strong biomarker potential, with more than 86% of identified disordered proteins functioning as prognostic biomarkers across three signaling networks [44].
Metabolic Biomarkers
Metabolomics provides a direct readout of cellular activity and physiological status by quantifying small molecule metabolites, offering unique insights into disease mechanisms and therapeutic responses [95]. Metabolomic data is characterized by high dimensionality, significant intercorrelation between features, and substantial technical variability introduced during sample preparation and analysis. These datasets typically exhibit right-skewed distributions, heteroscedasticity, and extensive missingness that require specialized pre-processing approaches [95].
The performance of classification models applied to metabolomic data is heavily influenced by normalization strategies that remove technical artifacts while preserving biological signals. Comparative studies have demonstrated that probabilistic quotient normalization (PQN), median ratio normalization (MRN), and variance stabilizing normalization (VSN) significantly enhance model performance, with VSN-normalized data achieving 86% sensitivity and 77% specificity in classifying hypoxic-ischemic encephalopathy using Orthogonal Partial Least Squares models [97]. These normalization methods outperform conventional approaches like total concentration normalization and autoscaling in mitigating cohort discrepancies while highlighting biologically relevant pathways such as fatty acid oxidation and purine metabolism [97].
Imaging Biomarkers
Quantitative imaging biomarkers derived from modalities such as high-definition microvasculature imaging (HDMI) provide non-invasive methods for characterizing tissue microstructure and function. In thyroid cancer detection, HDMI extracts morphological parameters of tumor microvessels—including tortuosity, vessel density, diameter, Murray's deviation, microvessel fractal dimension, bifurcation angle, number of branch points, and vessel segments—as potential biomarkers of malignancy [99]. These parameters capture the anarchical angiogenesis associated with cancer progression, offering complementary information to conventional imaging features.
The performance of imaging biomarker classification models varies significantly depending on the selected features and algorithm architecture. A support vector machine (SVM) model trained on six significant HDMI biomarkers achieved an AUC of 0.9005 (95% CI: 0.8279-0.9732) with sensitivity, specificity, and accuracy of 0.7778, 0.9474, and 0.8929, respectively, for discriminating benign from malignant thyroid nodules [99]. Model performance improved further (AUC: 0.9044) when incorporating clinical data including TI-RADS scores, age, and nodule size, demonstrating the value of multimodal integration for diagnostic classification [99].
Table 1: Performance Metrics of Machine Learning Models Across Biomarker Types and Diseases
| Disease Context | Biomarker Type | ML Algorithm | Performance Metrics | Key Biomarkers Identified |
|---|---|---|---|---|
| Thyroid Cancer | Imaging (HDMI) | Support Vector Machine | AUC: 0.9005; Sensitivity: 77.78%; Specificity: 94.74% | Vessel tortuosity, density, diameter, fractal dimension |
| Liver Fibrosis | Genomic (Ferroptosis-related) | Random Forest + SVM | AUC > 0.8; Experimental validation confirmed | ESR1, GSTZ1, IL1B, HSPB1, PTGS2 |
| Osteosarcoma Prognosis | Genomic (Metastasis-related) | LASSO-Cox Regression | Significant prognostic prediction (P < 0.05) | 15-gene signature including FKBP11 |
| Targeted Cancer Therapies | Genomic (Network-based) | Random Forest, XGBoost | LOOCV Accuracy: 0.7-0.96 | 426 high-confidence biomarkers across models |
| Hypoxic-Ischemic Encephalopathy | Metabolic | OPLS with VSN | Sensitivity: 86%; Specificity: 77% | Glycine, Alanine, Fatty Acid Oxidation markers |
Comparative Model Performance Across Diseases
Oncology Applications
Machine learning approaches have demonstrated exceptional utility in oncology for identifying biomarkers that predict disease progression, therapeutic response, and clinical outcomes. In osteosarcoma, a 15-gene prognostic signature constructed using LASSO-Cox regression effectively stratified patients into high-risk and low-risk groups, enabling prediction of metastatic potential and survival outcomes [100]. The identified signature genes were enriched in critical pathways including Wnt signaling, highlighting their functional relevance in cancer progression [100]. Similarly, in liver fibrosis, multiple machine learning methods including Weighted Gene Co-expression Network Analysis, Random Forest, and Support Vector Machines identified nine core ferroptosis-related genes, with experimental validation confirming ESR1 and GSTZ1 as protective biomarkers with diagnostic utility for both liver fibrosis and hepatocellular carcinoma [98].
The MarkerPredict framework exemplifies the power of integrating network biology with machine learning for predictive biomarker discovery in oncology. By incorporating topological information from signaling networks and protein annotations including intrinsic disorder, this approach classified 3,670 target-neighbor pairs and established a Biomarker Probability Score that identified 2,084 potential predictive biomarkers for targeted cancer therapeutics [44]. Notably, 426 biomarkers were consistently classified across all model configurations, demonstrating the robustness of this integrated approach [44].
Metabolic and Neurological Disorders
Metabolomic biomarker discovery presents distinct challenges and opportunities for machine learning applications. In hypoxic-ischemic encephalopathy, the performance of Orthogonal Partial Least Squares models varied significantly based on normalization methods, with VSN demonstrating superior sensitivity and specificity compared to other approaches [97]. Glycine consistently emerged as a top biomarker across six of seven normalization methods, confirming its biological relevance while highlighting the impact of pre-processing on biomarker prioritization [97].
The application of multiple validation methods is particularly critical for metabolomic studies, given the sensitivity of metabolic profiles to pre-analytical variables and technical artifacts. Studies incorporating leave-one-out cross-validation, k-fold cross-validation, and train-test splits provide more robust performance estimates, with reported AUC values exceeding 0.8 for well-optimized models [95] [97]. Additionally, the integration of clinical data with metabolic profiles consistently enhances model performance, reflecting the multifactorial nature of metabolic disorders.
Table 2: Methodological Considerations for Different Biomarker Types
| Biomarker Type | Recommended ML Algorithms | Critical Pre-processing Steps | Validation Strategies | Unique Challenges |
|---|---|---|---|---|
| Genomic | Random Forest, XGBoost, LASSO-Cox | Batch effect correction, normalization | LOOCV, bootstrap validation | High feature dimensionality, biological heterogeneity |
| Metabolic | OPLS, SVM, Random Forest | VSN, PQN, MRN normalization, missing value imputation | k-fold CV, external validation | Technical variability, right-skewed distribution |
| Imaging | SVM, CNN, Random Forest | Vessel enhancement filtering, morphological filtering | Hold-out validation, ROC analysis | Motion artifacts, inter-observer variability |
Experimental Protocols
Protocol 1: Genomic Biomarker Discovery Using Network-Based Machine Learning
Principle: This protocol integrates network topology features with protein characteristics to identify predictive biomarkers using tree-based machine learning algorithms, based on the MarkerPredict framework [44].
Materials:
- RNA sequencing or gene expression data
- Protein-protein interaction networks (CSN, SIGNOR, or ReactomeFI)
- Protein disorder predictions (DisProt, AlphaFold, IUPred)
- Biomarker annotation databases (CIViCmine)
Procedure:
- Data Preparation: Compile gene expression data from disease and control samples. Annotate proteins with intrinsic disorder predictions using multiple databases.
- Network Analysis: Map expression data onto signaling networks. Identify three-nodal motifs (triangles) using FANMOD software. Calculate topological features for all node pairs.
- Training Set Construction: Establish positive controls using literature-curated biomarker-target pairs. Create negative controls from non-biomarker pairs and random pairs.
- Model Training: Implement Random Forest and XGBoost algorithms with competitive random halving for hyperparameter optimization. Train separate models for different network and disorder databases.
- Biomarker Scoring: Calculate Biomarker Probability Score as normalized summative rank across all models. Apply threshold to identify high-confidence biomarkers.
- Validation: Perform leave-one-out cross-validation and independent test set validation. Evaluate using AUC, accuracy, and F1-score metrics.
Notes: Network selection significantly impacts results; use disease-relevant networks when available. The combined model integrating multiple networks and disorder databases generally outperforms individual approaches.
Protocol 2: Metabolic Biomarker Discovery with Variance Stabilizing Normalization
Principle: This protocol applies variance stabilizing normalization to metabolomic data before model construction to enhance biomarker stability and classification performance, adapted from [97].
Materials:
- Quantitative metabolomic data (LC-MS, GC-MS, or NMR platforms)
- VSN R package (vsn2)
- ropls package for OPLS models
- Quality control samples
Procedure:
- Data Pre-processing: Apply general pre-processing including peak alignment, integration, and compound identification. Filter metabolites with >50% missing values.
- Variance Stabilizing Normalization: Implement VSN using the vsn2 package with parameters optimized on the training dataset. Transform both training and test sets using the same parameters.
- Model Construction: Build Orthogonal Partial Least Squares models using normalized training data with disease status as the dependent variable.
- Biomarker Identification: Extract metabolites with Variable Importance in Projection (VIP) scores >1.0 as potential biomarkers.
- Pathway Analysis: Conduct metabolic pathway enrichment analysis using identified biomarkers.
- Validation: Apply model to normalized test dataset. Calculate sensitivity, specificity, and AUC. Compare performance against alternative normalization methods.
Notes: VSN parameters must be determined exclusively from the training set to avoid overfitting. Performance should be benchmarked against PQN and MRN normalization for the specific dataset.
Protocol 3: Imaging Biomarker Extraction from Microvasculature Images
Principle: This protocol extracts quantitative morphological parameters from high-definition microvasculature images for classification of malignant and benign tumors, based on [99].
Materials:
- High frame rate ultrasound data
- Alpinion E-Cube 12R ultrasound scanner with L3-12H linear probe
- Custom MATLAB scripts for HDMI processing
- SVM implementation (e1071 R package)
Procedure:
- Data Acquisition: Acquire ultrasound data in longitudinal and transverse cross-sections during breath-hold. Maintain minimal probe pressure to avoid vessel compression.
- Image Processing: Apply clutter filtering, denoising, vessel enhancement filtering, and morphological filtering to extract microvessel structures.
- Vessel Segmentation: Implement vessel segmentation algorithms to generate binary vessel maps. Manually segment nodule boundaries using B-mode images.
- Parameter Extraction: Calculate twelve morphological parameters: vessel density, number of vessel segments, number of branch points, vessel diameter, tortuosity, Murray's deviation, microvessel fractal dimension, bifurcation angle, and derived parameters.
- Feature Selection: Apply Wilcoxon rank-sum test to identify parameters with significant differences between malignant and benign nodules (p < 0.01).
- Model Construction: Train Support Vector Machine classifier using significant parameters. Optimize kernel parameters through cross-validation.
- Multimodal Integration: Incorporate clinical data (TI-RADS, age, nodule size) to enhance model performance.
Notes: Longitudinal views typically provide more reliable data due to reduced out-of-plane motion. Multiple acquisitions per orientation improve reproducibility.
Visualization Framework
Biomarker Discovery and Validation Workflow
Diagram 1: Comprehensive Workflow for Biomarker Discovery
Network-Based Biomarker Identification
Diagram 2: Network-Based Biomarker Identification Process
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for Biomarker Discovery
| Category | Specific Resource | Application | Key Features |
|---|---|---|---|
| Data Resources | FerrDb Database | Ferroptosis-related gene annotation | Curated database of ferroptosis drivers, suppressors, markers |
| CIViCmine Database | Clinical interpretation of genomic variants | Text-mined biomarker-disease relationships with evidence levels | |
| DisProt Database | Intrinsically disordered protein annotation | Manually curated database of protein disorder regions | |
| Analytical Tools | VSN R Package | Metabolomic data normalization | Variance-stabilizing transformation for enhanced model performance |
| WGCNA R Package | Weighted gene co-expression network analysis | Systems biology approach for module-trait relationships | |
| FANMOD Software | Network motif identification | Efficient detection of overrepresented network patterns | |
| Experimental Platforms | Alpinion E-Cube 12R | High-definition microvasculature imaging | Plane wave imaging for microvessel resolution to ~300μm |
| Dual Luciferase Assay Kit | ceRNA network validation | Functional verification of miRNA-mRNA interactions | |
| Machine Learning Libraries | XGBoost | Gradient boosting framework | Tree-based algorithm with high predictive accuracy |
| randomForest R Package | Random Forest implementation | Ensemble method for feature selection and classification | |
| glmnet R Package | LASSO regression | Regularized regression for high-dimensional data |
This comparative analysis demonstrates that machine learning model performance in biomarker discovery is influenced by multiple factors including biomarker type, disease context, data pre-processing strategies, and algorithm selection. Genomic biomarkers benefit from network-based approaches that contextualize molecular signatures within biological pathways, while metabolomic biomarkers require sophisticated normalization methods like VSN to address technical variability. Imaging biomarkers derived from microvasculature morphology provide complementary diagnostic information when integrated with clinical data.
The consistent observation that multi-modal integration enhances model performance across diverse biomarker types highlights the importance of holistic analytical frameworks that capture the complexity of biological systems. Furthermore, rigorous validation using multiple methods is essential to ensure biomarker stability and clinical translatability. The protocols and methodologies outlined in this application note provide a standardized framework for advancing machine learning-powered biomarker discovery across therapeutic areas, ultimately enhancing precision medicine initiatives through robust, clinically actionable biomarker signatures.
The application of machine learning (ML) to biomarker discovery represents a paradigm shift in precision oncology, yet the translation of computational findings into clinically validated tools remains a significant challenge. Despite the proliferation of ML-based biomarker candidates, few navigate the complex pathway from discovery to regulatory approval and clinical implementation successfully. This transition requires not only algorithmic excellence but also rigorous validation, regulatory compliance, and seamless workflow integration—elements often overlooked in early research phases. The growing recognition that many late-stage failures originate from decisions made earlier in the pipeline underscores the critical need for integrated translational strategies that connect computational discovery with clinical application [101].
This protocol details a systematic framework for the clinical translation of ML-derived biomarkers, with particular emphasis on predictive oncology applications. We present a structured approach encompassing computational validation, analytical verification, clinical validation, regulatory strategy, and workflow integration. By addressing these interconnected components throughout the development lifecycle, researchers can significantly enhance the translational potential of their ML-based biomarker discoveries and accelerate their impact on patient care and drug development.
Regulatory Framework for AI/ML-Based Biomarkers
Foundational Regulatory Principles
The regulatory pathway for ML-based biomarkers requires adherence to established medical device and in vitro diagnostic frameworks, while accommodating the unique characteristics of adaptive algorithms. Regulatory approval hinges on demonstrating analytical validity, clinical validity, and clinical utility through rigorous evidence generation. The U.S. Food and Drug Administration (FDA) and other major regulatory bodies increasingly recognize that traditional review processes must evolve to address the rapid iteration cycles characteristic of AI/ML development [102].
The FDA's INFORMED (Information Exchange and Data Transformation) initiative serves as a blueprint for regulatory innovation, functioning as a multidisciplinary incubator for deploying advanced analytics across regulatory functions [102]. This initiative demonstrates the value of creating protected spaces for experimentation within regulatory agencies, highlighting the importance of multidisciplinary teams that integrate clinical, technical, and regulatory expertise. For ML-based biomarkers, this translates to regulatory expectations that include:
- Prospective validation in intended-use populations rather than reliance on retrospective benchmarking alone
- Demonstration of generalizability across diverse datasets and clinical settings
- Comprehensive documentation of model development, training data, and performance characteristics
- Analytical validation under realistic conditions reflecting clinical workflow variability
Clinical Evidence Requirements
Regulatory acceptance of ML-based biomarkers requires compelling clinical evidence that aligns with the claimed intended use. The evidence threshold correlates directly with the innovation level and claimed impact of the AI solution—more transformative claims demand more comprehensive validation [102]. For predictive biomarkers intended to guide therapeutic decisions, this typically necessitates prospective randomized controlled trials (RCTs) or well-designed observational studies that demonstrate statistically significant and clinically meaningful impact on patient outcomes [102].
Adaptive trial designs that allow for continuous model updates while preserving statistical rigor represent a viable approach for evaluating AI technologies in clinical settings. The validation framework must assess how AI systems perform when making forward-looking predictions rather than identifying patterns in historical data, addressing potential issues of data leakage or overfitting [102]. Beyond regulatory approval, commercial success depends on demonstrating value to payers and healthcare systems, requiring evidence of clinical utility, cost-effectiveness, and improvement over existing alternatives [102].
Integrated Workflow for ML-Based Biomarker Translation
End-to-End Translation Pipeline
Successful translation of ML-based biomarkers requires a coordinated, multi-stage process that connects computational discovery with clinical implementation. The following workflow integrates technological, regulatory, and operational considerations across the development continuum:
Figure 1: Integrated workflow for ML-based biomarker translation, connecting discovery with clinical implementation through iterative development with regulatory feedback.
Computational Validation & Model Optimization
The initial discovery phase requires rigorous computational validation to establish foundational evidence for biomarker candidates. This begins with comprehensive data acquisition from diverse biological sources, including multi-omics profiles, clinical records, and real-world data, followed by meticulous data preprocessing to address quality, batch effects, and heterogeneity [103] [104]. Feature extraction then identifies biologically relevant patterns using ML approaches optimized for high-dimensional data.
For model development, we advocate emphasizing interpretability and biological plausibility over mere algorithmic complexity. Studies demonstrate that complex deep learning architectures often offer negligible performance gains in typical clinical proteomics datasets while exacerbating interpretability challenges [47]. Instead, ensemble methods like Random Forest and XGBoost frequently provide optimal balance between performance and interpretability for biomarker discovery [44]. The MarkerPredict framework, which integrates network motifs and protein disorder information, exemplifies this approach—achieving leave-one-out-cross-validation accuracy of 0.7–0.96 across 32 different models while maintaining biological interpretability [44].
Model validation must address generalizability across diverse populations and robustness to technical variability. Performance metrics should extend beyond traditional accuracy measures to include clinical relevance indicators such as positive/negative predictive values in intended-use populations. Strict separation of training, validation, and test sets is essential, with external validation on completely independent datasets representing the target clinical population [47].
Table 1: Key Performance Metrics for Computational Validation of ML-Based Biomarkers
| Metric Category | Specific Metrics | Target Threshold | Clinical Significance |
|---|---|---|---|
| Discrimination | AUC-ROC, AUC-PR | >0.80 | Ability to distinguish patient subgroups |
| Calibration | Brier score, calibration slope | <0.10 | Agreement between predicted and observed outcomes |
| Clinical Utility | Net Benefit, Decision Curve Analysis | Superior to standard care | Improvement over current practice |
| Stability | Performance variance across sites | <15% degradation | Generalizability across settings |
Analytical Validation Protocols
Analytical validation establishes that the biomarker test accurately and reliably measures the intended analytes in the intended specimen types. For ML-based biomarkers, this requires demonstration of robustness across pre-analytical variables, reproducibility across operators and sites, and analytical specificity against potential interferents.
Protocol: Multi-Site Reprodubility Assessment
Purpose: To evaluate the analytical performance of an ML-based biomarker assay across multiple testing sites and operators.
Materials:
- Reference standard samples with known status (positive/negative)
- Standardized operating procedures for sample processing
- Participating testing sites (minimum 3 recommended)
- Data collection forms capturing pre-analytical variables
Procedure:
- Distribute blinded sample sets to participating sites (minimum 30 positive, 30 negative samples)
- Process samples according to standardized protocols
- Perform feature extraction using validated methods
- Apply ML algorithm to extracted features
- Collect results and pre-analytical variables for analysis
Acceptance Criteria:
- Inter-site concordance >90% for binary classifications
- Intra-class correlation coefficient >0.8 for continuous scores
- Minimal impact of pre-analytical variables on performance metrics
Statistical Analysis: Calculate concordance statistics, variance components, and multivariate analysis of pre-analytical factors affecting results.
Clinical Validation & Regulatory Submission
Clinical validation provides evidence that the biomarker accurately identifies the clinical condition or predicts the therapeutic response in the target population. For predictive biomarkers in oncology, this typically requires demonstration of clinical utility—showing that biomarker use leads to improved patient outcomes or provides information that meaningfully impacts clinical decision-making.
Protocol: Prospective Clinical Validation Study
Purpose: To evaluate the clinical validity and utility of an ML-based predictive biomarker for selecting cancer therapy.
Study Design: Prospective randomized controlled trial or registry study comparing biomarker-directed care versus standard approach.
Participants:
- Inclusion: Patients with the relevant cancer type eligible for the therapeutic choices being guided by the biomarker
- Exclusion: Conditions that would preclude evaluation of the primary endpoint
- Sample Size: Sufficient to detect clinically meaningful difference in primary endpoint with 80-90% power
Intervention:
- Experimental arm: Treatment selection based on ML-based biomarker results
- Control arm: Treatment selection based on standard criteria
Primary Endpoints:
- Progression-free survival (for predictive biomarkers)
- Overall response rate
- Other clinically relevant endpoints specific to the clinical context
Statistical Considerations:
- Pre-specified statistical analysis plan
- Intent-to-treat principle
- Adjustment for relevant covariates
- Predefined subgroup analyses
Regulatory submission requires comprehensive documentation including complete analytical validation data, clinical validation study results, assay specifications, and proposed labeling. The FDA's pre-submission process provides valuable opportunity for feedback on validation strategies and evidence requirements.
Implementation & Workflow Integration
Technology Integration Frameworks
Successful clinical implementation of ML-based biomarkers requires seamless integration into existing clinical and research workflows. The complexity of integrating multiple point solutions represents a significant barrier to adoption, making unified platforms that connect electronic data capture (EDC) systems, eCOA solutions, and clinical services increasingly essential [105].
Interoperability standards are critical for scalable implementation. Platforms should support RESTful APIs for real-time data exchange, FHIR standards for healthcare data integration, and OAuth 2.0 for secure authentication [105]. For decentralized clinical trial implementations, which are particularly relevant for biomarker validation studies, integrated platforms must accommodate remote patient monitoring, telemedicine visits, home health services, and direct-to-patient drug shipment while maintaining regulatory compliance [105].
Implementation success depends heavily on user-centered design that accommodates clinical workflow constraints. This includes intuitive interfaces for clinical staff, automated data flows between systems, and minimal disruption to established practices. Training requirements, change management, and ongoing technical support significantly influence adoption rates and should be addressed proactively in implementation planning.
Quality Management & Continuous Monitoring
Post-implementation monitoring is essential for maintaining biomarker performance in real-world settings. A robust quality management system should include regular performance reassessment, drift detection mechanisms, and processes for controlled updates based on accumulating real-world evidence.
For ML-based biomarkers specifically, continuous monitoring should track:
- Data drift: Changes in the distribution of input features over time
- Concept drift: Changes in the relationship between features and outcomes
- Performance degradation: Deterioration in key metrices compared to validation studies
- Clinical utility maintenance: Ongoing assessment of impact on patient outcomes
Documented procedures should govern the circumstances under which model retraining or refinement is warranted, with clear change control processes that may require regulatory notification or re-review depending on the magnitude of changes.
Essential Research Reagents & Computational Tools
Successful translation of ML-based biomarkers requires both wet-lab reagents and computational resources. The following table details key solutions essential for implementing the protocols described in this document:
Table 2: Essential Research Reagents & Computational Tools for ML-Based Biomarker Translation
| Category | Specific Solution | Function/Purpose | Implementation Notes |
|---|---|---|---|
| Spatial Biology | Visium HD (10x Genomics) | Spatial transcriptomics for biomarker localization within tissue architecture | Enables study of biomarker distribution patterns in tumor microenvironment [104] |
| Computational Framework | MarkerPredict (GitHub) | ML tool for predictive biomarker identification using network motifs and protein disorder | Random Forest/XGBoost models with Biomarker Probability Score output [44] |
| Multi-omic Integration | Tempus multimodal data library | Integrated analysis of DNA, RNA, and H&E data with clinical outcomes | Provides real-world evidence for biomarker validation [106] |
| Advanced Models | Patient-derived organoids | Functional validation of biomarker candidates in 3D culture systems | Recapitulates human tissue architecture for biomarker screening [104] |
| Data Standardization | Digital Biomarker Discovery Pipeline (DBDP) | Open-source toolkit for standardized biomarker development | Implements FAIR principles; Apache 2.0 License [103] |
| Clinical Trial Infrastructure | Castor EDC integrated platform | Unified system for clinical data capture, eConsent, and eCOA in validation studies | Supports decentralized trial elements with native integration [105] |
The successful translation of ML-based biomarkers from discovery to clinical application requires a meticulously planned and executed strategy that integrates computational science, regulatory science, and clinical implementation. By adopting the structured frameworks, validation protocols, and implementation strategies outlined in this document, researchers can significantly enhance the translational potential of their biomarker discoveries. The path to clinical translation demands rigorous validation, strategic regulatory planning, and seamless workflow integration—elements that transform promising computational findings into clinically impactful tools that advance precision medicine and improve patient care.
Conclusion
Machine learning has undeniably transformed the landscape of biomarker discovery, providing powerful tools to extract meaningful signals from complex, high-dimensional biological data. The successful application of ML hinges not on algorithmic complexity alone, but on a rigorous, principled approach that prioritizes data quality, model interpretability, and robust validation. Future progress will depend on the widespread adoption of standardized practices, enhanced multi-omics integration, and the development of more efficient methods for scenarios with limited data. By embracing these principles, researchers can accelerate the translation of computational discoveries into clinically validated biomarkers, ultimately paving the way for more precise diagnostics, effective therapeutics, and personalized medicine.
References
- 1. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 2. Machine learning enhances biomarker discovery: From multi [https://esmed.org/MRA/mra/article/view/6888]
- 3. Adaptive multi-omics integration framework for breast ... [https://www.nature.com/articles/s41598-025-22202-z]
- 4. Flexynesis: A deep learning toolkit for bulk multi-omics data ... [https://www.nature.com/articles/s41467-025-63688-5]
- 5. Clinical Validation of a Noninvasive Multi-Omics Method for ... [https://www.sciencedirect.com/science/article/pii/S1525157825001060]
- 6. Challenges in Biomarker Discovery: Combining Expert ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3548234/]
- 7. The benefits and pitfalls of machine learning for biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10558383/]
- 8. Machine Learning in Biomarker Discovery for Precision ... [https://esmed.org/machine-learning-in-biomarker-discovery-for-precision-medicine/]
- 9. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 10. Machine learning in point-of-care testing: innovations, ... [https://www.nature.com/articles/s41467-025-58527-6]
- 11. Machine learning approaches for biomarker discovery to ... [https://www.nature.com/articles/s41598-023-42338-0]
- 12. An artificial intelligence-assisted microfluidic colorimetric ... [https://www.nature.com/articles/s41528-024-00321-3]
- 13. Use of biomarkers to identify phenotypes and endotypes ... [https://pubmed.ncbi.nlm.nih.gov/30059792/]
- 14. Toward precision medicine in COPD: phenotypes, endotypes ... [https://respiratory-research.biomedcentral.com/articles/10.1186/s12931-025-03356-w]
- 15. Biomarker Validation: Common Data Analysis Concerns [https://pmc.ncbi.nlm.nih.gov/articles/PMC4122484/]
- 16. T cells in cancer: mechanistic insights and therapeutic advances [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00807-w]
- 17. Mechanistic insights into the immune biomarker of ... [https://pubmed.ncbi.nlm.nih.gov/40799452/]
- 18. Correlation does not equal causation: the imperative of ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1630781/full]
- 19. Ten quick tips for biomarker discovery and validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9371329/]
- 20. TCGADownloadHelper: simplifying TCGA data extraction ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1569290/full]
- 21. Updating TCGA glioma classification through integration of ... [https://www.nature.com/articles/s41597-025-05117-2]
- 22. Data navigation on the ENCODE portal [https://www.nature.com/articles/s41467-025-64343-9]
- 23. Access to ENCODE data [https://www.encodeproject.org/about/data-access/]
- 24. News | gnomAD browser - Broad Institute [https://gnomad.broadinstitute.org/news/]
- 25. Improved allele frequencies in gnomAD through local ... [https://www.nature.com/articles/s41467-025-63340-2]
- 26. Changelog | gnomAD browser [https://gnomad.broadinstitute.org/news/changelog/]
- 27. Bioinformatics analysis of TCGA data identifies a taurine ... [https://pubmed.ncbi.nlm.nih.gov/41220730/]
- 28. A supervised machine learning approach with feature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12219308/]
- 29. Supervised vs. Unsupervised Learning: What's the ... [https://www.ibm.com/think/topics/supervised-vs-unsupervised-learning]
- 30. An unsupervised learning approach for clustering joint ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11851129/]
- 31. An unsupervised learning approach to identify novel ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-019-0705-z]
- 32. Integrating supervised and unsupervised machine learning ... [https://www.sciencedirect.com/science/article/pii/S3050787125000277]
- 33. Frontiers | BLESS: bagged logistic regression for biomarker identification [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1336891/full]
- 34. A random forest based biomarker discovery and power ... [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-020-00826-6]
- 35. A Review on Biomarkerâ€Enhanced Machine Learning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421415/]
- 36. MEvA-X: a hybrid multiobjective evolutionary tool using an XGBoost ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10354005/]
- 37. Identifying Biomarkers Using Support Vector Machine to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10325814/]
- 38. Biomarker discovery from high-throughput data by ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417423006814]
- 39. Logistic regression and other statistical tools in diagnostic biomarker studies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11333519/]
- 40. Multiâ€omics analysis revealed biomarkers for coronary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12371206/]
- 41. High-throughput DeepPRM-Stellar proteomics coupled ... [https://pubs.rsc.org/en/content/articlelanding/2025/an/d5an00396b]
- 42. Expression graph network framework for biomarker discovery [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554635/]
- 43. AI-driven biomarker discovery: enhancing precision in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906928/]
- 44. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 45. Contrastive-learning of language embedding and ... [https://www.nature.com/articles/s41467-025-56526-1]
- 46. A Network-Based Framework to Discover Treatment ... [https://www.sciencedirect.com/science/article/pii/S1525157824001612]
- 47. A 2025 perspective on the role of machine learning for ... [https://pubmed.ncbi.nlm.nih.gov/40772544/]
- 48. AI-driven multi-omics integration in precision oncology [https://pmc.ncbi.nlm.nih.gov/articles/PMC12634751/]
- 49. 6 practices to begin with multi-omics data integration [https://www.pythiabio.com/post/6-practices-to-begin-with-multi-omics-data-integration]
- 50. A Guide to Multi-omics Integration Strategies [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 51. A machine learning approach for multimodal data fusion ... [https://www.nature.com/articles/s41698-025-00917-6]
- 52. Strategies for Comprehensive Multi-Omics Integrative Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11592251/]
- 53. Integrative Network Fusion: A Multi-Omics Approach in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7340129/]
- 54. A guide to multi-omics data collection and integration for ... [https://www.sciencedirect.com/science/article/pii/S200103702200544X]
- 55. Multi-omics strategies for biomarker discovery and ... [https://pubmed.ncbi.nlm.nih.gov/41269529/]
- 56. Ten quick tips for biomarker discovery and validation analyses ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1010357]
- 57. Bio-primed machine learning to enhance discovery of ... [https://www.nature.com/articles/s41698-025-00825-9]
- 58. Biomarker discovery using 1-norm regularization for ... [https://www.sciencedirect.com/science/article/abs/pii/S0925231212000811]
- 59. Correcting batch effects in large-scale multiomics studies using a reference-material-based ratio method | Genome Biology | Full Text [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-023-03047-z]
- 60. The Handling of Missing Data in Molecular Epidemiology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5508724/]
- 61. Data standards in drug discovery: A long way to go [https://www.sciencedirect.com/science/article/abs/pii/S1359644624000047]
- 62. Data Cleaning in Metabolomics Biomarker Research [https://www.metwarebio.com/data-cleaning-in-metabolomics-biomarker-research/]
- 63. Data Quality Frameworks guide for pharma & life sciences [https://www.ideagen.com/thought-leadership/blog/data-quality-frameworks-dqf-guide]
- 64. CDER Data Standards Program [https://www.fda.gov/drugs/electronic-regulatory-submission-and-review/cder-data-standards-program]
- 65. The benefits and pitfalls of machine learning for biomarker ... [https://link.springer.com/article/10.1007/s00441-023-03816-z]
- 66. Explainable machine learning framework for biomarker ... [https://www.nature.com/articles/s41598-025-98948-3]
- 67. Integration of machine learning in biomarker discovery for ... [https://www.sciencedirect.com/science/article/abs/pii/S0344033825002766]
- 68. Applications of machine learning in drug discovery and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6552674/]
- 69. Integrating artificial intelligence in drug discovery and early ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00758-2]
- 70. Exploring biomarkers of premature ovarian insufficiency ... [https://www.nature.com/articles/s41598-023-38754-x]
- 71. Current Bioinformatics Tools in Precision Oncology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238682/]
- 72. Recursive Feature Elimination: A Powerful Technique for ... [https://medium.com/the-modern-scientist/recursive-feature-elimination-a-powerful-technique-for-feature-selection-in-machine-learning-89b3c2f3c26a]
- 73. Recursive Feature Elimination Using R [https://towardsdatascience.com/effective-feature-selection-recursive-feature-elimination-using-r-148ff998e4f7/]
- 74. Decision Variants for the Automatic Determination of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6027449/]
- 75. Recursive feature elimination with cross-validation [https://scikit-learn.org/stable/auto_examples/feature_selection/plot_rfe_with_cross_validation.html]
- 76. Biomarker identification for rheumatoid arthritis with ... [https://www.sciencedirect.com/science/article/pii/S017129852500035X]
- 77. Bias recognition and mitigation strategies in artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897215/]
- 78. Evaluation and Mitigation of Racial Bias in Clinical Machine ... [https://medinform.jmir.org/2022/5/e36388/]
- 79. Mitigating bias in machine learning for medicine [https://www.nature.com/articles/s43856-021-00028-w]
- 80. Identifying and Mitigating Algorithmic Bias through a ... [https://arxiv.org/html/2510.14669v1]
- 81. Achieving a representative sample in health research [https://www.sciencedirect.com/science/article/abs/pii/S147159532400115X]
- 82. External validation: a simulation study to compare cross ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9464671/]
- 83. Externally validated and clinically useful machine learning ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02463-y]
- 84. Practical Considerations and Applied Examples of Cross ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11041453/]
- 85. 3.1. Cross-validation: evaluating estimator performance [https://scikit-learn.org/stable/modules/cross_validation.html]
- 86. Cross-validation (statistics) [https://en.wikipedia.org/wiki/Cross-validation_(statistics)]
- 87. Cross-Validation in Machine Learning: How to Do It Right [https://neptune.ai/blog/cross-validation-in-machine-learning-how-to-do-it-right]
- 88. Biomarker-based and interpretable machine learning ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559646/]
- 89. Evaluation of blood- and urine-derived biomarkers for ... [https://www.sciencedirect.com/science/article/abs/pii/S0169260725001968]
- 90. A multi-biomarker machine learning approach for early ... [https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-025-03855-y]
- 91. AI-Powered Biomarker Discovery: 7 ... [https://lifebit.ai/blog/ai-powered-biomarker-discovery-2/]
- 92. Evaluating generalizability of oncology trial results to real- ... [https://www.nature.com/articles/s41591-024-03352-5]
- 93. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 94. AI-driven predictive biomarker discovery with contrastive ... [https://www.sciencedirect.com/science/article/pii/S1535610825001308]
- 95. Statistical methods and resources for biomarker discovery ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05383-0]
- 96. A Comparative Analysis of Biomarker Selection Techniques [https://pmc.ncbi.nlm.nih.gov/articles/PMC3842054/]
- 97. A Comparative Analysis of Data Normalization Approaches ... [https://www.mdpi.com/2079-3197/12/7/137]
- 98. Machine Learning and Experimental Validation Identified ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11625426/]
- 99. Quantitative Biomarkers Derived from a Novel Contrast-Free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10046818/]
- 100. Machine learning and experimental validation to construct a ... [https://josr-online.biomedcentral.com/articles/10.1186/s13018-022-03386-w]
- 101. Integrating translational and clinical research to advance ... [https://www.ddw-online.com/how-integrating-translational-and-clinical-research-can-advance-drug-development-37444-202510/]
- 102. AI in Drug Development: Clinical Validation and ... [https://globalforum.diaglobal.org/issue/june-2025/ai-in-drug-development-clinical-validation-and-regulatory-innovation-are-dual-imperatives/]
- 103. Biomarker discovery pipeline: 3 Critical Steps 2025 [https://lifebit.ai/blog/biomarker-discovery-pipeline/]
- 104. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 105. Decentralized Clinical Trial Platforms in 2025 - Castor EDC [https://www.castoredc.com/insight-briefs/decentralized-clinical-trial-platforms-in-2025-a-practical-guide-for-clinical-operations/]
- 106. Biomarkers & Precision Medicine US 2025 [https://www.tempus.com/events/biomarkers-us-2025/?srsltid=AfmBOoodVMzLZA4SbhLFKUrv4oTT1YytSggOF3vIhc3mNWHof6HFguFW]