Signaling Pathway Inhibitors in Cancer Therapy: A Comparative Analysis of Efficacy, Mechanisms, and Clinical Applications
This article provides a comprehensive comparative analysis of signaling pathway inhibitors for researchers, scientists, and drug development professionals.
Signaling Pathway Inhibitors in Cancer Therapy: A Comparative Analysis of Efficacy, Mechanisms, and Clinical Applications
Abstract
This article provides a comprehensive comparative analysis of signaling pathway inhibitors for researchers, scientists, and drug development professionals. It explores the foundational science behind major targeted pathways, including BTK, PI3K/Akt/mTOR, JAK/STAT, and MAPK, examining their roles in oncogenesis and therapeutic targeting. The content delves into methodological approaches for inhibitor development, from single-target agents to emerging multi-target strategies, and addresses critical challenges including drug resistance, toxicity management, and biomarker-driven patient stratification. Through systematic comparison of inhibitor classes, clinical trial data, and validation frameworks, this review synthesizes key insights to guide future research directions and clinical translation of targeted cancer therapies.
Cellular Signaling Pathways in Oncogenesis: From Basic Mechanisms to Therapeutic Targets
Dysregulation of intracellular signaling pathways is a hallmark of cancer, driving uncontrolled cell proliferation, survival, and metastasis. Four key pathways—BTK, PI3K/Akt/mTOR, JAK/STAT, and MAPK—represent critical therapeutic targets in oncology drug development. These pathways function as central communication networks that transduce extracellular signals into cellular responses, regulating fundamental processes including growth, differentiation, and apoptosis. Oncogenic activation of these pathways occurs through various mechanisms including gain-of-function mutations, gene amplifications, and epigenetic alterations. Understanding the comparative architecture, regulatory mechanisms, and therapeutic targeting of these pathways provides crucial insights for developing more effective cancer treatments and overcoming drug resistance.
The development of targeted inhibitors against these pathways has revolutionized cancer therapy, moving treatment beyond traditional chemotherapy toward precision medicine approaches. Small molecule inhibitors targeting key nodes within these signaling networks have demonstrated significant clinical efficacy across diverse hematological malignancies and solid tumors. This review provides a comprehensive comparative analysis of BTK, PI3K/Akt/mTOR, JAK/STAT, and MAPK pathway inhibitors, focusing on their mechanisms of action, clinical applications, and experimental evaluation methodologies to inform research and drug development efforts.
BTK Signaling Pathway and Inhibitors
Pathway Biology and Clinical Significance
Bruton's tyrosine kinase (BTK) is a non-receptor tyrosine kinase belonging to the Tec family of kinases that plays an essential role in B-cell receptor (BCR) signaling, development, and differentiation [1] [2]. Following BCR stimulation, BTK becomes phosphorylated and activates downstream signaling cascades that promote B-cell proliferation, survival, and metabolic adaptation [2]. The crucial role of BTK in normal B-cell development is highlighted by X-linked agammaglobulinemia (XLA), a primary immunodeficiency disorder caused by mutations in the BTK gene that result in almost no production of mature B cells and premature cell death [1] [2].
In malignant B-cells, BTK mediates proliferative and pro-survival signals through impaired adhesion properties and interaction with the tumor microenvironment [2]. This central role in B-cell malignancies has made BTK an attractive therapeutic target, particularly for chronic lymphocytic leukemia (CLL), mantle cell lymphoma (MCL), and Waldenström macroglobulinemia [1]. BTK inhibitors have dramatically changed the treatment landscape for these malignancies, demonstrating significant improvement in progression-free survival and overall survival compared with traditionally used chemoimmunotherapy [1].
Key BTK Inhibitors and Clinical Applications
Ibrutinib, the first-in-class BTK inhibitor, received FDA approval in 2013 for MCL and subsequently in 2014 for CLL, revolutionizing treatment for B-cell malignancies [1] [2]. Ibrutinib covalently and irreversibly binds to the cysteine-481 (C481) residue in the ATP-binding domain of BTK, blocking its ability to phosphorylate substrates and suppressing downstream survival signaling [1]. The RESONATE phase III trial established ibrutinib's efficacy in relapsed/refractory CLL, demonstrating significantly improved progression-free survival (HR = 0.22) and overall survival (HR = 0.43) compared to ofatumumab [1]. Long-term follow-up data confirmed durable responses, with 5-year PFS rates of 70% in previously untreated older CLL patients [1].
Next-generation BTK inhibitors including acalabrutinib and zanubrutinib were developed with enhanced selectivity for BTK to minimize off-target effects associated with ibrutinib [1] [2]. These agents show similar efficacy to ibrutinib but with improved safety profiles, particularly regarding cardiovascular toxicities [2]. Acalabrutinib received FDA approval in 2017 for MCL and later for CLL, while zanubrutinib was approved in 2019 for MCL [1]. Emerging non-covalent BTK inhibitors such as pirtobrutinib represent a promising approach to overcome resistance mediated by C481 mutations through reversible binding at alternative sites [1].
Table 1: Clinically Approved BTK Inhibitors in Oncology
| Inhibitor | Year Approved | Primary Indications | Key Clinical Trial Data | Major Adverse Effects |
|---|---|---|---|---|
| Ibrutinib | 2013 (MCL), 2014 (CLL) | CLL, SLL, MCL, WM, MZL, cGVHD | RESONATE: PFS HR=0.22 vs ofatumumab; 5-year PFS 70% in frontline CLL | Atrial fibrillation, bleeding, rash, diarrhea, infections |
| Acalabrutinib | 2017 | CLL, SLL, MCL | ELEVATE-TN: Superior PFS vs chlorambucil+obinutuzumab | Headache, diarrhea, musculoskeletal pain |
| Zanubrutinib | 2019 | MCL, WM | ASPEN: Similar overall response to ibrutinib in WM with improved safety | Neutropenia, upper respiratory infections |
| Tirabrutinib | 2020 (Japan) | Primary CNS lymphoma | - | Rash, neutropenia, lymphopenia |
Resistance Mechanisms and Novel Approaches
Despite the efficacy of BTK inhibitors, approximately 60% of patients treated long-term with covalent BTK inhibitors develop resistance [2]. The most common mechanism involves a cysteine-to-serine substitution at position 481 (C481S) in BTK, which prevents covalent binding of irreversible inhibitors [2]. Additional resistance mechanisms include mutations in downstream signaling molecules such as PLCγ2 and activation of alternative survival pathways [1]. To address these resistance mechanisms, non-covalent BTK inhibitors such as fenebrutinib and ARQ 531 are under investigation and have demonstrated efficacy against C481 mutant clones [2].
Current research focuses on combination therapies that target multiple pathways simultaneously. Clinical trials are exploring BTK inhibitors combined with anti-CD20 monoclonal antibodies (e.g., rituximab, obinutuzumab) or BCL2 inhibitors (e.g., venetoclax) to enhance therapeutic efficacy and potentially achieve treatment-free remission [1] [2]. The synergistic effect of these combinations may address the heterogeneity of B-cell malignancies and reduce the emergence of resistant subclones.
PI3K/Akt/mTOR Signaling Pathway and Inhibitors
Pathway Architecture and Oncogenic Activation
The PI3K/Akt/mTOR (PAM) signaling pathway represents a highly conserved signal transduction network that regulates cell survival, growth, proliferation, and metabolism in response to extracellular stimuli [3]. Growth factor binding to receptor tyrosine kinases (RTKs) or G-protein coupled receptors (GPCRs) initiates the canonical pathway, leading to activation of class I PI3K which phosphorylates phosphatidylinositol 4,5-bisphosphate (PIP2) to generate phosphatidylinositol 3,4,5-trisphosphate (PIP3) [4] [3]. PIP3 serves as a docking site for Akt and PDK1, leading to Akt phosphorylation and activation. Activated Akt then modulates numerous downstream substrates including mTOR, a master regulator of cell growth and metabolism [3].
The PAM pathway is the most frequently activated signaling pathway in human cancer, with aberrations occurring in approximately 50% of tumors [3]. Oncogenic activation occurs through multiple mechanisms including RTK overactivation, PI3K catalytic subunit (PIK3CA) mutations or amplification, loss of the tumor suppressor PTEN (which dephosphorylates PIP3), and Akt gain-of-function mutations [4] [3]. PIK3CA is the most commonly mutated oncogene across tumor lineages, with hotspot mutations E545K and H1047R driving constitutive pathway activation [3]. The central role of PAM signaling in cancer has made it a prime target for therapeutic intervention.
Table 2: PI3K/Akt/mTOR Pathway Inhibitors and Their Applications
| Inhibitor Class | Target Specificity | Representative Agents | Key Indications | Major Resistance Mechanisms |
|---|---|---|---|---|
| Pan-PI3K inhibitors | All class I PI3K isoforms | Buparlisib, Copanlisib | Breast cancer, lymphoma | RTK feedback activation, PIK3CA mutations |
| Isoform-selective PI3K inhibitors | Specific PI3K isoforms | Alpelisib (p110α), Idelalisib (p110δ) | PIK3CA-mutated breast cancer, CLL | AKT reactivation, additional PIK3CA mutations |
| AKT inhibitors | All AKT isoforms | Ipatasertib, Capivasertib | AKT1-mutated cancers, TNBC | Upstream RTK activation, mTOR feedback |
| mTORC1 inhibitors | mTORC1 complex | Everolimus, Temsirolimus | RCC, breast cancer, NET | mTORC2-mediated AKT activation |
| Dual PI3K/mTOR inhibitors | PI3K and mTORC1/2 | Dactolisib, Voxtalisib | Various solid tumors | Compensatory pathway activation |
Therapeutic Targeting and Clinical Applications
PI3K pathway inhibitors are categorized based on their specific molecular targets along the signaling cascade [4]. First-generation inhibitors include rapamycin analogs (rapalogs) such as everolimus and temsirolimus that specifically target mTORC1 [4] [3]. These agents demonstrated clinical efficacy in renal cell carcinoma, neuroendocrine tumors, and hormone receptor-positive breast cancer but have limited activity in other malignancies due to feedback activation of upstream signaling [3]. More recent development has focused on ATP-competitive inhibitors that target both mTORC1 and mTORC2, pan-PI3K inhibitors that inhibit all four class I PI3K isoforms, and isoform-selective PI3K inhibitors [4].
Isoform-selective inhibitors offer the potential for targeted therapy with reduced toxicity. Idelalisib, a p110δ inhibitor, received approval for relapsed CLL and indolent non-Hodgkin lymphoma, exploiting the predominantly hematopoietic expression of p110δ [3]. Alpelisib, a p110α-specific inhibitor, is approved for PIK3CA-mutated, hormone receptor-positive breast cancer in combination with endocrine therapy [3]. AKT inhibitors such as capivasertib and ipatasertib have shown promise in clinical trials, particularly in tumors with AKT alterations and triple-negative breast cancer [3].
Experimental Approaches for PI3K Pathway Inhibition
Research continues to address the challenges of therapeutic resistance and toxicity associated with PAM pathway inhibition. Combination strategies targeting parallel or compensatory pathways are under active investigation, including PI3K inhibitors with MEK inhibitors, CDK4/6 inhibitors, or endocrine therapies [3]. Novel therapeutic approaches include PROteolysis TArgeting Chimeras (PROTACs) that degrade target proteins, and adaptive dosing schedules to manage toxicities while maintaining efficacy [3].
The central role of PI3K signaling in immunology has also prompted investigation of PI3K inhibitors in immuno-oncology combinations. Preclinical models demonstrate that PI3Kδ and PI3Kγ inhibition can enhance antitumor immunity by modulating regulatory T cells and myeloid-derived suppressor cells, respectively [3]. Clinical trials are evaluating these combinations to overcome resistance to immune checkpoint inhibitors.
JAK/STAT Signaling Pathway and Inhibitors
Pathway Components and Regulatory Mechanisms
The Janus kinase/signal transducer and activator of transcription (JAK/STAT) pathway serves as a primary signaling cascade for numerous cytokines, interferons, growth factors, and hormones [5]. This pathway consists of three main components: ligand-receptor complexes, JAK kinases (JAK1, JAK2, JAK3, TYK2), and STAT transcription factors (STAT1-6) [6] [5]. Upon ligand binding, receptor-associated JAKs undergo trans-phosphorylation and subsequently phosphorylate STAT proteins. Phosphorylated STATs dimerize and translocate to the nucleus where they regulate transcription of target genes involved in proliferation, inflammation, and immune response [5].
The JAK family proteins contain seven homology domains (JH1-JH7), with JH1 representing the kinase domain and JH2 serving as a pseudokinase domain that regulates kinase activity [6] [5]. JAK3 is primarily expressed in hematopoietic cells and requires the common gamma chain (γc) for signaling, while other JAK family members are more widely expressed [5]. STAT proteins contain SH2 domains that facilitate their recruitment to phosphorylated receptor motifs and mediate dimerization [5]. The JAK/STAT pathway is tightly regulated by multiple mechanisms including suppressor of cytokine signaling (SOCS) proteins, protein inhibitors of activated STATs (PIAS), and protein tyrosine phosphatases [5].
JAK Inhibitors in Clinical Practice
JAK inhibitors are classified into first-generation non-selective inhibitors and second-generation more selective agents [6]. First-generation inhibitors such as tofacitinib and baricitinib inhibit multiple JAK family members and are approved for autoimmune diseases including rheumatoid arthritis, psoriasis, and atopic dermatitis [6] [7]. Second-generation inhibitors including filgotinib (JAK1-selective) and upadacitinib (JAK1-selective) offer improved specificity to minimize off-target effects [6].
In oncology, ruxolitinib (a JAK1/JAK2 inhibitor) is approved for myelofibrosis and polycythemia vera, representing the primary application of JAK inhibitors in hematologic malignancies [6] [5]. Ruxolitinib demonstrates efficacy in reducing splenomegaly and constitutional symptoms in myeloproliferative neoplasms, particularly those driven by the JAK2V617F mutation [6]. Fedratinib, a more selective JAK2 inhibitor, is also approved for myelofibrosis [6]. The development of JAK inhibitors for solid tumors has been more challenging due to pathway complexity and toxicities.
Classification and Binding Mechanisms
JAK inhibitors can be categorized based on their binding mechanisms as reversible (competitive) or irreversible (covalent) inhibitors [6]. Reversible inhibitors include type I inhibitors that bind to the active kinase conformation and compete with ATP, and type II inhibitors that bind to the inactive conformation [6]. Most clinically approved JAK inhibitors are type I ATP-competitive inhibitors. Irreversible JAK inhibitors typically target the unique cysteine residue (Cys909) in JAK3 and form covalent bonds, enhancing selectivity [6]. Ritlecitinib represents an example of an irreversible JAK3 inhibitor currently in clinical development [6].
JAK inhibitors are further characterized by their kinase inhibition profiles, which determine their therapeutic applications and safety considerations. The relative inhibition of different JAK isoforms influences both efficacy and toxicity profiles, with JAK1 inhibition primarily mediating anti-inflammatory effects, JAK2 inhibition associated with hematologic toxicities, and JAK3 inhibition providing more specific immunomodulation [6] [5].
MAPK Signaling Pathway and Inhibitors
Cascade Architecture and Oncogenic Roles
The mitogen-activated protein kinase (MAPK) pathways represent ubiquitous intracellular signaling networks that regulate diverse cellular processes including proliferation, differentiation, apoptosis, and stress responses [8]. Four major MAPK family members have been characterized: extracellular signal-regulated kinases 1 and 2 (ERK1/2), c-Jun N-terminal kinases (JNK), p38 MAP kinases, and ERK5 [8] [9]. Each MAPK is activated through a three-tiered kinase cascade consisting of MAPK kinase kinases (MAP3Ks) that phosphorylate and activate MAPK kinases (MAP2Ks), which in turn phosphorylate and activate the MAPKs [8].
The ERK1/2 pathway (Ras-Raf-MEK-ERK) is the most extensively studied MAPK cascade and is frequently activated in cancer through mutations in upstream regulators including Ras (KRAS, NRAS) and Raf (BRAF) [8] [9]. This pathway transduces signals from growth factor receptors to regulate gene expression and cell cycle progression. The JNK and p38 pathways primarily respond to cellular stress and inflammatory cytokines, while ERK5 integrates signals from growth factors and stress stimuli [8]. Constitutive activation of MAPK pathways, particularly ERK1/2, has been implicated in the initiation and progression of various cancers, making these pathways attractive therapeutic targets [8].
Targeted Inhibitors in Clinical Use
The development of MAPK pathway inhibitors has progressed significantly, with multiple agents receiving FDA approval [8] [9]. BRAF inhibitors such as vemurafenib, dabrafenib, and encorafenib are approved for BRAF-mutant melanoma, often in combination with MEK inhibitors to enhance efficacy and prevent resistance [9]. MEK inhibitors (trametinib, cobimetinib, binimetinib) target the downstream kinases MEK1/2 and are used in combination with BRAF inhibitors for BRAF-mutant melanoma and as monotherapy in other malignancies [8] [9].
p38 MAPK inhibitors including SB203580 and BIRB-796 were developed primarily for inflammatory diseases rather than oncology applications [8] [9]. Similarly, JNK inhibitors have faced challenges in clinical development due to toxicity concerns and limited efficacy [8]. The ERK1/2 pathway inhibitors targeting receptor tyrosine kinases upstream of MAPK signaling include gefitinib and erlotinib (EGFR inhibitors), sunitinib (PDGFR, VEGFR, c-Kit inhibitor), and sorafenib (multi-kinase inhibitor) [8].
Table 3: Clinically Utilized MAPK Pathway Inhibitors
| Therapeutic Target | Inhibitor | Primary Indications | Key Limitations |
|---|---|---|---|
| BRAF | Vemurafenib, Dabrafenib, Encorafenib | BRAF-mutant melanoma | Resistance development, paradoxical activation in wild-type BRAF |
| MEK1/2 | Trametinib, Cobimetinib, Binimetinib | BRAF-mutant melanoma (with BRAF inhibitors), NSCLC | Ocular toxicities, skin rash, diarrhea |
| EGFR | Gefitinib, Erlotinib | EGFR-mutant NSCLC | Resistance mutations (T790M, C797S) |
| Multi-targeted RTK | Sorafenib, Sunitinib | RCC, HCC, GIST | Broad toxicity profile, off-target effects |
| p38 | SB203580, BIRB-796 | Inflammatory diseases (investigational) | Limited efficacy in clinical trials |
Research Tools and Experimental Applications
MAPK pathway inhibitors serve as valuable research tools for elucidating pathway functions and validating therapeutic targets [8]. Selective inhibitors including U0126 and PD0325901 (MEK1/2 inhibitors), SB203580 (p38 inhibitor), and SP600125 (JNK inhibitor) have been extensively used to dissect the contributions of specific MAPK pathways to cellular responses [8]. These compounds enable researchers to establish causal relationships between pathway activation and biological outcomes through pharmacological inhibition.
Methodologies for evaluating MAPK pathway inhibition typically involve immunoblotting with phosphorylation-state-specific antibodies to quantify changes in pathway activation [8]. Standard experimental protocols include serum starvation followed by stimulation with growth factors or cytokines in the presence or absence of inhibitors, with subsequent analysis of phosphorylated MAPK substrates [8]. These approaches allow researchers to assess inhibitor potency, specificity, and duration of action in cellular models.
Comparative Analysis of Pathway Inhibitors
Therapeutic Targeting Strategies Across Pathways
The four signaling pathways discussed employ distinct therapeutic targeting strategies based on their molecular architectures and regulatory mechanisms. BTK inhibitors primarily utilize irreversible covalent binding to achieve sustained target inhibition, leveraging the unique cysteine residue (C481) in BTK's active site [1] [2]. This approach provides prolonged pharmacodynamic effects despite rapid plasma clearance. In contrast, most PI3K/Akt/mTOR, JAK/STAT, and MAPK pathway inhibitors function through reversible, competitive inhibition at ATP-binding sites [6] [4] [3]. The conservation of ATP-binding pockets across kinase families presents challenges for achieving selectivity, which has been addressed through structural biology-guided drug design.
The development of isoform-selective inhibitors represents an important advancement for minimizing off-target toxicities, particularly for the PI3K and JAK families where different isoforms serve distinct physiological functions [6] [3]. Alternative targeting strategies include allosteric inhibitors that bind outside the ATP pocket (e.g., MEK inhibitors), dual inhibitors that simultaneously target multiple pathway components (e.g., PI3K/mTOR inhibitors), and covalent irreversible inhibitors beyond BTK targeting (e.g., JAK3 covalent inhibitors) [6] [8] [4].
Resistance Mechanisms and Combination Approaches
Therapeutic resistance remains a significant challenge across all pathway inhibitors and develops through both shared and pathway-specific mechanisms. Common resistance mechanisms include on-target mutations that impair drug binding (e.g., BTK C481S, EGFR T790M), activation of alternative signaling pathways that bypass inhibition, and feedback loops that reactivate the targeted pathway [1] [2] [3]. The mutation profile varies by pathway, with kinase domain mutations predominating for BTK, EGFR, and ALK inhibitors, while PI3K pathway resistance frequently involves PTEN loss or Akt activation [2] [3].
Combination therapies represent the primary strategy to overcome or prevent resistance. Rational combination approaches include vertical pathway inhibition (targeting multiple nodes within the same pathway), horizontal pathway inhibition (targeting parallel pathways), and integration with non-kinase targeted therapies [1] [3]. Clinical successes include BRAF+MEK inhibitor combinations in melanoma, BTK+BCL2 inhibitor combinations in CLL, and PI3K inhibitor+endocrine therapy in breast cancer [1] [3]. The optimal combination strategies continue to be refined through preclinical models and biomarker-driven clinical trials.
Research Methodologies and Experimental Design
Standardized Assessment of Inhibitor Efficacy
Robust evaluation of signaling pathway inhibitors requires integrated methodological approaches spanning biochemical, cellular, and in vivo models. Standard assessment includes in vitro kinase assays to determine inhibitor potency (IC50 values) and selectivity across kinase panels [8] [9]. Cellular models then evaluate target engagement through immunoblotting of phosphorylated substrates, complemented by functional assays measuring proliferation, apoptosis, and cell cycle distribution [8].
For immune cell-targeting inhibitors such as BTK and JAK inhibitors, additional functional assays evaluate effects on primary immune cells including B-cell receptor signaling (for BTK inhibitors) or cytokine responses (for JAK inhibitors) [2] [5]. In vivo evaluation typically employs xenograft models for oncology applications and genetically engineered mouse models that recapitulate human diseases [1] [5]. These preclinical models help establish pharmacodynamic biomarkers that can be translated to clinical studies for assessing target inhibition.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Signaling Pathway Studies
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| Phospho-specific antibodies | p-BTK (Y223), p-AKT (S473), p-STAT3 (Y705), p-ERK1/2 (T202/Y204) | Western blot, immunofluorescence, flow cytometry | Validation of specificity, optimization of conditions |
| Selective inhibitors | Ibrutinib (BTK), Alpelisib (PI3Kα), Ruxolitinib (JAK1/2), Trametinib (MEK1/2) | Pathway validation, combination studies | Off-target effects, concentration optimization |
| Recombinant cytokines/growth factors | IL-6, IL-4, B-cell activating factor, EGF | Pathway stimulation assays | Concentration response, timing of stimulation |
| Kinase assay systems | ADP-Glo, mobility shift assays, radioactive filtration assays | Biochemical kinase inhibition profiling | ATP concentration optimization, enzyme linearity |
| Cell line models | Mino, JeKo-1 (MCL), Rec-1 (MCL), Ba/F3 engineered lines | Proliferation, apoptosis, signaling studies | Authentication, mycoplasma testing |
| HMG-CoA Reductase-IN-1 | HMG-CoA Reductase-IN-1, MF:C27H29N3O7, MW:507.5 g/mol | Chemical Reagent | Bench Chemicals |
| Nlrp3-IN-30 | Nlrp3-IN-30, MF:C19H17F3N4O2, MW:390.4 g/mol | Chemical Reagent | Bench Chemicals |
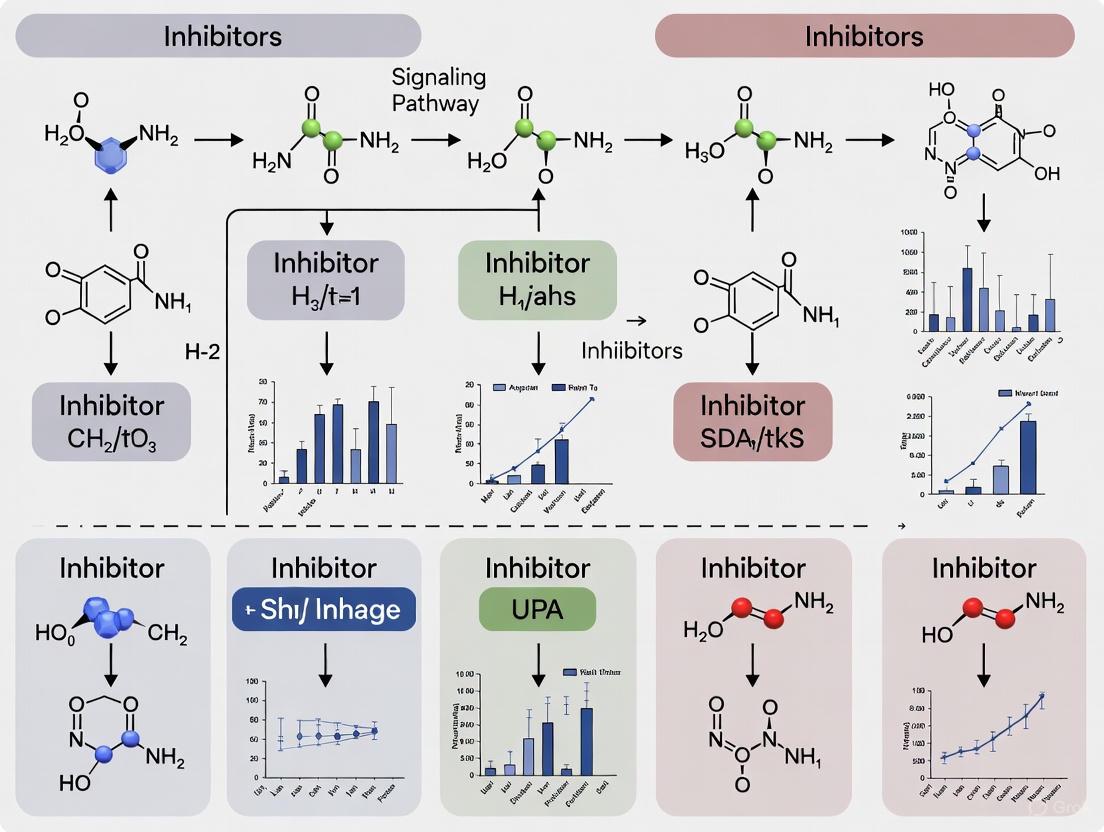
Visualizing Signaling Networks and Experimental Approaches
The following diagrams illustrate key signaling pathways and experimental methodologies discussed in this review, created using DOT visualization language.
Diagram 1: BTK Signaling Pathway and Inhibitor Mechanism
Diagram 2: PI3K/Akt/mTOR Signaling Pathway and Inhibition Points
Diagram 3: Experimental Workflow for Pathway Inhibition Studies
The comparative analysis of BTK, PI3K/Akt/mTOR, JAK/STAT, and MAPK signaling pathway inhibitors reveals both shared principles and distinct challenges in targeted cancer therapy. While each pathway possesses unique biological functions and therapeutic applications, common themes emerge including the importance of selectivity for minimizing toxicities, the inevitability of resistance mechanisms, and the necessity of rational combination approaches. The continued refinement of these targeted agents depends on deeper understanding of pathway biology, resistance mechanisms, and predictive biomarkers.
Future directions in signaling pathway inhibition include the development of novel therapeutic modalities such as PROTACs that degrade target proteins rather than simply inhibiting them, allosteric inhibitors with improved selectivity profiles, and fourth-generation inhibitors capable of overcoming resistance mutations [2] [3]. Additionally, the integration of pathway inhibitors with immunotherapy represents a promising frontier, particularly for modulating the tumor microenvironment. As our understanding of signaling network complexity grows, so too will our ability to develop more effective, durable, and personalized cancer therapies targeting these fundamental regulatory pathways.
Cancer pathogenesis is driven by a complex interplay of molecular dysregulation mechanisms that enable uncontrolled cell proliferation, evasion of cell death, and metastatic potential. The transition from normal cellular homeostasis to malignant transformation involves three fundamental categories of alterations: genetic mutations that directly change DNA sequence and protein function, gene amplifications that lead to oncogene overexpression, and epigenetic modifications that alter gene expression without changing the underlying DNA sequence [10] [11]. These mechanisms collectively hijack normal signaling pathways, creating dependencies that can be therapeutically targeted.
The landscape of targeted cancer therapy has evolved substantially from conventional cytotoxic agents to precision medicines that specifically target these molecular vulnerabilities. This evolution began with the recognition that cancers derived from different tissues often share common driver pathways, and that tumors from the same tissue of origin may harbor distinct molecular alterations requiring different therapeutic approaches [10]. The contemporary paradigm of precision medicine leverages detailed molecular profiling to match patients with targeted therapies based on the specific dysregulation mechanisms present in their tumors, moving beyond histology-based classification to mechanism-driven treatment selection [10].
Comparative Analysis of Dysregulation Mechanisms
Genetic Mutations: Direct Alterations of DNA Sequence
Genetic mutations constitute the most fundamental mechanism of oncogenic transformation, directly altering DNA sequence and consequently protein structure and function. These mutations can range from single nucleotide substitutions to large-scale chromosomal rearrangements, with varying impacts on oncogenic signaling. Gain-of-function mutations in proto-oncogenes (e.g., BRAF V600E) and loss-of-function mutations in tumor suppressor genes (e.g., TP53) represent two major categories of driver mutations in cancer [10].
The clinical success of mutation-targeted therapies is exemplified by inhibitors targeting the BCR-ABL fusion protein in chronic myelogenous leukemia (imatinib), BRAF V600E mutations in melanoma (vemurafenib), and EGFR mutations in non-small cell lung cancer (lazertinib) [10] [7]. These therapies demonstrate the principle of oncogene addiction, whereby cancer cells become dependent on a single activated oncogenic pathway or protein, creating a therapeutic window that can be exploited with targeted agents [10].
Gene Amplifications: Quantitative Increases in Oncogenic Signaling
Gene amplification represents another fundamental mechanism of oncogenic activation, leading to increased copy number and consequent overexpression of oncogenes. This quantitative increase in gene dosage results in enhanced oncogenic signaling without necessarily altering the protein structure itself. A paradigmatic example is HER2/neu (ERBB2) amplification in breast cancer, where increased gene copy number leads to overexpression of the HER2 receptor tyrosine kinase, driving proliferative signaling through multiple downstream pathways [10] [12].
The development of HER2-targeted therapies including trastuzumab, ado-trastuzumab emtansine (T-DM1), and trastuzumab deruxtecan (T-DXd) has fundamentally transformed the prognosis for HER2-positive breast cancer patients [12]. These therapies demonstrate that quantitative overexpression of oncogenes represents a clinically actionable vulnerability, with antibody-drug conjugates like T-DXd showing particular promise in managing HER2-positive breast cancer brain metastases due to their enhanced CNS penetration [12].
Epigenetic Modifications: Reversible Regulation of Gene Expression
Epigenetic modifications constitute a third major category of oncogenic dysregulation, involving heritable changes in gene expression that do not alter the underlying DNA sequence. The five principal mechanisms of epigenetic regulation include DNA modification, histone modification, RNA modification, chromatin remodeling, and non-coding RNA regulation [13]. These mechanisms function as an integrated regulatory system that controls chromatin state and accessibility, with enzymes categorized as "writers," "erasers," "readers," and "remodelers" based on their functions [13].
Cancer cells frequently exhibit widespread epigenetic alterations including global DNA hypomethylation with localized hypermethylation of tumor suppressor gene promoters, aberrant histone modification patterns, and dysregulated expression of non-coding RNAs [13] [11]. These changes can silence tumor suppressor genes or activate oncogenes, contributing fundamentally to malignant transformation. The reversibility of epigenetic modifications makes them particularly attractive therapeutic targets, as evidenced by FDA-approved agents targeting DNA methyltransferases (azacytidine, decitabine) and histone deacetylases (vorinostat, romidepsin) [13] [10].
Table 1: Comparative Features of Major Dysregulation Mechanisms in Cancer
| Dysregulation Mechanism | Molecular Basis | Key Examples | Therapeutic Approaches |
|---|---|---|---|
| Genetic Mutations | Alteration of DNA sequence leading to functional protein changes | BRAF V600E, TP53, IDH1/2, KRAS | Kinase inhibitors, PARP inhibitors (synthetic lethality) |
| Gene Amplifications | Increased gene copy number leading to protein overexpression | HER2/neu, MYC, EGFR | Monoclonal antibodies, antibody-drug conjugates, tyrosine kinase inhibitors |
| Epigenetic Modifications | Reversible changes to chromatin structure and accessibility | DNMT3A, EZH2, TET2 | DNMT inhibitors, HDAC inhibitors, EZH2 inhibitors |
Experimental Models and Methodologies for Studying Dysregulation Mechanisms
In Vitro Models for Inhibitor Screening and Validation
In vitro cancer models provide controlled systems for initial evaluation of therapeutic agents targeting specific dysregulation mechanisms. Cell line models enable detailed investigation of inhibitor effects on molecular pathways, with standardized protocols for assessing target engagement, pathway modulation, and cellular responses. The comparative analysis of CK2 inhibitors CX-4945 and SGC-CK2-2 exemplifies a rigorous in vitro approach for evaluating inhibitor specificity and efficacy [14].
Experimental Protocol: Kinase Inhibitor Profiling in Cancer Cell Lines
Cell Culture Conditions: Maintain human cancer cell lines (e.g., HeLa cervical cancer, MDA-MB-231 breast cancer) in appropriate media supplemented with 10% fetal bovine serum at 37°C in 5% CO₂ [14].
Inhibitor Treatment: Prepare serial dilutions of kinase inhibitors (e.g., CX-4945, SGC-CK2-2) in DMSO, with final concentrations typically ranging from 0.5-20 μM based on preliminary dose-finding studies. Include DMSO-only controls for normalization [14].
Treatment Duration: Expose cells to inhibitors for 24 hours to assess acute effects on signaling pathways, or for extended periods (72-96 hours) to evaluate effects on cell viability and proliferation [14].
Target Engagement Assessment: Harvest cells and prepare protein lysates for Western blot analysis using phosphospecific antibodies against known substrate phosphorylation sites (e.g., pS129-Akt, pS13-Cdc37 for CK2 inhibition) [14].
Validation of Specificity: Utilize phosphoantibodies recognizing consensus motif sequences (e.g., pS/pT-D-X-E for CK2 substrates) to evaluate global inhibition of target kinase activity and detect potential off-target effects [14].
Functional Assays: Assess cell viability using MTT, MTS, or CellTiter-Glo assays following 72-hour inhibitor treatment to correlate pathway inhibition with functional consequences [14].
This experimental approach enables systematic comparison of inhibitor potency (IC50 determination) and specificity across multiple cell line models, providing critical data for lead optimization and mechanism of action studies.
In Vivo Models for Therapeutic Efficacy Assessment
In vivo models provide essential preclinical data on the pharmacokinetics, biodistribution, and therapeutic efficacy of targeted agents in physiologically relevant contexts. These models capture the complexity of tumor microenvironment interactions, drug metabolism, and host toxicity that cannot be fully recapitulated in vitro.
Experimental Protocol: Patient-Derived Xenograft (PDX) Therapeutic Studies
Model Establishment: Implant patient-derived tumor fragments or cell suspensions subcutaneously into immunocompromised mice (e.g., NSG mice) to establish PDX models that maintain the molecular characteristics of original tumors [10].
Treatment Initiation: Randomize mice into treatment groups when tumors reach approximately 100-200 mm³, ensuring balanced group assignment based on initial tumor volume [15].
Dosing Regimens: Administer therapeutic agents via appropriate routes (oral gavage for small molecules, intraperitoneal or intravenous injection for biologics) at established maximum tolerated doses or clinically relevant concentrations [15].
Efficacy Monitoring: Measure tumor dimensions 2-3 times weekly using calipers, calculating volume using the formula: V = (length × width²)/2. Monitor body weight as an indicator of treatment toxicity [15].
Endpoint Analysis: Harvest tumors at study endpoint for molecular profiling (Western blot, IHC, RNA-seq) to confirm target modulation and identify potential resistance mechanisms [15].
PDX models have become the gold standard for preclinical therapeutic evaluation due to their preservation of tumor heterogeneity and predictive value for clinical response [10].
Signaling Pathways Commonly Dysregulated in Cancer
Multiple signaling pathways are frequently dysregulated in cancer through mutations, amplifications, or epigenetic mechanisms. Understanding these pathways is essential for developing effective targeted therapies and combination strategies.
Diagram 1: Key Oncogenic Signaling Pathways. This diagram illustrates major signaling pathways frequently dysregulated in cancer through mutations, amplifications, or epigenetic alterations, highlighting potential therapeutic targeting opportunities.
Comparative Efficacy of Therapeutic Approaches Targeting Different Dysregulation Mechanisms
Therapeutic approaches vary significantly based on the specific dysregulation mechanism being targeted. The tables below summarize comparative efficacy data for agents targeting different categories of molecular alterations.
Table 2: Comparative Efficacy of Agents Targeting Genetic Mutations and Amplifications
| Therapeutic Class | Specific Agent | Molecular Target | Cancer Type | Efficacy Metrics | Clinical Context |
|---|---|---|---|---|---|
| Tyrosine Kinase Inhibitors | Lazertinib | EGFR mutation | NSCLC | PFS: 20.6 months | Third-generation EGFR TKI [7] |
| BRAF Inhibitors | Vemurafenib | BRAF V600E | Melanoma | Response Rate: 48% | Single-agent therapy [10] |
| Antibody-Drug Conjugates | Trastuzumab Deruxtecan (T-DXd) | HER2 amplification | Breast Cancer (BCBM) | CNS Progression: HR 0.17 (vs. physician's choice) | HER2-positive with brain metastases [12] |
| CK2 Inhibitors | CX-4945 | CK2 kinase | Various cancers | pS129-Akt IC50: 0.7-0.9 μM | In vitro potency [14] |
| CK2 Inhibitors | SGC-CK2-2 | CK2 kinase | Various cancers | pS129-Akt IC50: 1.3-2.2 μM | Improved specificity, reduced potency [14] |
Table 3: Comparative Efficacy of Agents Targeting Epigenetic Modifications
| Therapeutic Class | Specific Agent | Molecular Target | Cancer Type | Efficacy Metrics | Clinical Context |
|---|---|---|---|---|---|
| DNMT Inhibitors | Azacytidine | DNA methyltransferases | MDS, AML | Overall Response: ~15-20% | Hematologic malignancies [10] |
| HDAC Inhibitors | Vorinostat | Histone deacetylases | CTCL | Response Rate: ~30% | Cutaneous T-cell lymphoma [10] |
| EZH2 Inhibitors | Tazemetostat | EZH2 | Lymphoma | Response Rate: 69% (EZH2 mutant) | Relapsed/refractory lymphoma [10] |
| IDH Inhibitors | AG-120 (Ivosidenib) | IDH1 mutation | AML | Complete Response: 30.4% | IDH1-mutant AML [10] |
Table 4: Comparative Efficacy of Androgen Receptor Pathway Inhibitors in Prostate Cancer
| Therapeutic Agent | Molecular Target | Patient Population | 2-Year PFS to mCRPC | PSA ≤0.2 ng/mL (12 weeks) | Time to PSA Nadir (months) |
|---|---|---|---|---|---|
| Abiraterone acetate | Androgen synthesis | mHSPC (n=94) | 74.1% | 25.5% | 12.2 |
| Apalutamide | Androgen receptor | mHSPC (n=91) | 81.4% | 44.0% | 7.2 |
| Enzalutamide | Androgen receptor | mHSPC (n=34) | 85.6% | 55.9% | 7.5 |
Data adapted from real-world comparative effectiveness study of ARPIs in metastatic hormone-sensitive prostate cancer (mHSPC) [16]
Advanced Research Tools and Computational Approaches
Modern cancer research utilizes sophisticated computational approaches to identify synergistic drug combinations and optimize therapeutic strategies. Artificial intelligence and multi-omics integration have transformed drug discovery by enabling prediction of drug interactions and patient-specific therapeutic responses [17].
Diagram 2: Computational Framework for Drug Combination Prediction. This workflow illustrates the integration of multi-omics data through AI approaches to predict synergistic drug combinations and identify predictive biomarkers.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 5: Essential Research Tools for Investigating Dysregulation Mechanisms
| Research Tool Category | Specific Examples | Primary Applications | Key Features |
|---|---|---|---|
| Kinase Inhibitors | CX-4945 (Silmitasertib), SGC-CK2-2 | Target validation, signaling pathway analysis | CX-4945: Broad kinase inhibition; SGC-CK2-2: Enhanced specificity [14] |
| Epigenetic Modulators | Azacytidine, Vorinostat, Tazemetostat | Epigenetic mechanism studies, combination therapy | DNMT inhibition, HDAC inhibition, EZH2 inhibition [13] [10] |
| Phosphospecific Antibodies | pS129-Akt, pS13-Cdc37, pS/pT-D-X-E motif | Target engagement assessment, pathway modulation | Validation in knockout cells, motif-specific recognition [14] |
| Computational Platforms | DeepSynergy, AuDNNsynergy, DrugComboRanker | Drug combination prediction, multi-omics integration | Deep learning architectures, network analysis capabilities [17] |
| Cell Line Models | HeLa, MDA-MB-231, Patient-derived organoids | High-throughput screening, mechanism studies | Well-characterized genetic backgrounds, disease representation [14] |
| Akt-IN-21 | Akt-IN-21, MF:C26H34N2O4, MW:438.6 g/mol | Chemical Reagent | Bench Chemicals |
| Gli1-IN-1 | Gli1-IN-1|GLI1 Inhibitor|For Research Use | Gli1-IN-1 is a potent GLI1 inhibitor for cancer research. It targets Hedgehog signaling. This product is for Research Use Only. Not for human or veterinary use. | Bench Chemicals |
The comparative analysis of dysregulation mechanisms in cancer reveals an increasingly sophisticated understanding of oncogenic processes and their therapeutic vulnerabilities. Genetic mutations, amplifications, and epigenetic alterations represent distinct but interconnected mechanisms that can be selectively targeted with specific therapeutic classes. The emerging paradigm in oncology emphasizes mechanism-driven therapy selection based on the specific molecular alterations present in individual tumors, rather than histology alone.
Future progress in cancer therapeutics will likely involve rational combination strategies that simultaneously target multiple dysregulation mechanisms, such as combining epigenetic modifiers with kinase inhibitors or immunotherapy agents. The integration of computational approaches with experimental validation will accelerate the identification of synergistic drug combinations and biomarkers of response. As our understanding of cancer dysregulation mechanisms deepens, so too will our ability to develop precisely targeted, effective therapeutic strategies that improve outcomes for cancer patients across diverse malignancy types.
Growth factor receptors are membrane-bound enzyme-linked receptors that play a pivotal role in cellular signaling, regulating critical processes including proliferation, differentiation, metabolism, and apoptosis [18]. The majority of these receptors are receptor tyrosine kinases (RTKs), which undergo ligand-induced activation and initiate downstream signaling cascades [19] [18]. Understanding the structure-function relationships of these receptors and their effectors is fundamental to developing targeted cancer therapies, as dysregulated signaling drives tumor progression, angiogenesis, and metastasis [20] [19] [21]. This guide provides a comparative analysis of major growth factor receptor families, their structural features, and the efficacy of therapeutic inhibitors, framing this within ongoing research on signaling pathway inhibition.
Structural Classification and Activation Mechanisms
Growth factor receptors share a common molecular organization but exhibit distinct structural features that define their activation mechanisms and functional roles [22].
Common Structural Domains
All RTKs contain three fundamental domains: an extracellular ligand-binding domain, a single transmembrane domain, and a cytoplasmic tyrosine kinase domain [18]. Ligand binding to the extracellular domain induces receptor dimerization or oligomerization, facilitating trans-autophosphorylation of tyrosine residues within the cytoplasmic domain [19] [18]. This phosphorylation stabilizes the active receptor conformation and creates docking sites for intracellular signaling proteins, initiating downstream signal transduction [19].
Classification of Receptor Tyrosine Kinases
Based on primary amino acid sequences and molecular organization, RTKs are classified into distinct families [22]. The ErbB family (Class I), including the epidermal growth factor receptor (EGFR/ErbB1) and HER2/ErbB2, plays crucial roles in epithelial cell growth [23]. The insulin and IGF-1 receptors (Class II) are critical for metabolic signaling, while platelet-derived growth factor receptors (PDGFR) and colony stimulating factor-1 receptor (CSF-1R) belong to Class III [22]. The vascular endothelial growth factor receptors (VEGFRs) constitute a separate class (Type IV) primarily regulating vasculogenesis and angiogenesis [20].
Figure 1: General activation mechanism of receptor tyrosine kinases. Growth factor binding induces receptor dimerization, leading to trans-autophosphorylation and downstream signaling cascade initiation.
Structural Basis of Activation
The conformational transition from inactive to active states is a fundamental aspect of receptor function. For EGFR, biophysical studies in live cells demonstrate that in quiescent cells with low receptor expression (<50,000/cell), receptors exist predominantly as monomers [23]. Ligand binding rapidly induces dimer formation, which then associates with clathrin-coated pits for internalization [23]. In contrast, the orphan receptor ErbB2 exists preformed in aggregates of three to eight molecules and larger clusters, even in the absence of ligand [23]. This pre-association may facilitate rapid signaling upon heterodimerization with other ErbB family members.
Comparative Analysis of Major Growth Factor Receptor Families
Vascular Endothelial Growth Factor Receptors (VEGFRs)
The VEGF-VEGFR system is a critical regulator of vasculogenesis and angiogenesis, with profound implications for tumor biology [20] [24].
Structural Features and Ligand Diversity
VEGF-A, the predominant pro-angiogenic factor, exists in multiple isoforms (VEGF-A121, VEGF-A145, VEGF-A165, VEGF-A189, VEGF-A206) generated through alternative splicing [20] [24]. These isoforms differ in their heparin-binding affinity and extracellular matrix (ECM) retention capabilities due to variations in their C-terminal domains [24]. For example, VEGF-A121 is freely diffusible, while VEGF-A189 and VEGF-A206 tightly bind heparan sulfate proteoglycans, creating steep concentration gradients that guide patterned vascular growth [24]. VEGF-A165, the most abundant isoform, contains both receptor-binding and heparin-binding domains, enabling balanced distribution and signaling [24].
VEGFRs comprise three main members: VEGFR1 (Flt1), VEGFR2 (KDR/Flk1), and VEGFR3 (Flt4) [20]. VEGFR1 binds VEGF-A, VEGF-B, and PIGF with very high affinity (Kd ~2-10 pM for VEGF-A) but exhibits weak kinase activity, potentially functioning as a decoy receptor [20]. VEGFR2 serves as the primary mitogenic signal transducer for VEGF-A (Kd ~1-10 nM) and is essential for physiological and pathological angiogenesis [20] [24]. VEGFR3 primarily regulates lymphangiogenesis and binds VEGF-C and VEGF-D [20].
Downstream Effectors and Functional Outcomes
VEGFR2 activation initiates multiple signaling pathways including PLCγ-PKC-MAPK (promoting proliferation), PI3K-Akt (enhancing survival), and FAK-paxillin (regulating migration) [20]. In pathological conditions like cancer, excessive VEGF signaling promotes tumor angiogenesis, creating immature, leaky vessels that facilitate nutrient delivery and metastasis [20] [21].
Epidermal Growth Factor Receptors (EGFR/ErbB Family)
The ErbB receptor family consists of four members: EGFR (ErbB1), HER2 (ErbB2), HER3 (ErbB3), and HER4 (ErbB4) [23].
Activation and Signaling Mechanisms
EGFR activation involves ligand-induced conformational changes that promote dimerization [23]. In living cells studied at physiological temperatures, unliganded EGFR exists primarily as monomers at low expression levels, with dimerization occurring predominantly after EGF binding [23]. This contrasts with HER2, which forms pre-existing aggregates and clusters that may facilitate signaling [23]. ErbB receptors form homo- and heterodimers with distinct signaling properties, with the HER2-HER3 heterodimer being particularly potent in activating oncogenic signaling [23].
Downstream Signaling Pathways
Activated EGFR initiates multiple signaling cascades including:
- RAS-RAF-MAPK pathway: Regulates gene expression and cellular proliferation
- PI3K-AKT-mTOR pathway: Promotes cell survival and metabolism
- JAK-STAT pathway: Influences gene transcription and immune responses [18]
Dysregulation of these pathways through EGFR overexpression or activating mutations drives uncontrolled cell growth in multiple cancers, including non-small cell lung cancer (NSCLC) [19].
Other Significant Growth Factor Receptors
Platelet-Derived Growth Factor Receptors (PDGFR)
PDGFRs belong to Class III RTKs and play crucial roles in connective tissue development and wound healing [22]. PDGFR activation stimulates pathways similar to other RTKs, including MAPK and PI3K-Akt, promoting cell proliferation, survival, and migration [25].
Fibroblast Growth Factor Receptors (FGFR)
The FGFR family (FGFR1-4) regulates embryonic development, cell growth, differentiation, and angiogenesis [18]. FGFR signaling involves complex interactions with heparan sulfate proteoglycans that modulate receptor-ligand binding and activation.
Therapeutic Targeting: Comparative Efficacy of Signaling Pathway Inhibitors
Targeted therapies against growth factor receptors primarily include monoclonal antibodies and small molecule tyrosine kinase inhibitors (TKIs) [19]. These agents have revolutionized cancer treatment but exhibit distinct efficacy and safety profiles.
Tyrosine Kinase Inhibitors (TKIs)
TKIs are small molecules that inhibit the enzymatic activity of the target protein [19]. They are categorized based on their mechanism of action: ATP-competitive inhibitors (binding the active kinase conformation), inhibitors recognizing inactive conformations, allosteric inhibitors (binding outside the ATP pocket), and covalent inhibitors (forming irreversible bonds) [19].
Table 1: Classification and Properties of Tyrosine Kinase Inhibitors
| Category | Mechanism of Action | Example Drugs | Key Characteristics |
|---|---|---|---|
| ATP-competitive inhibitors | Bind active conformation of ATP-binding site | Gefitinib, Erlotinib | Reversible binding; specificity varies |
| Inactive conformation binders | Recognize and stabilize inactive kinase conformation | Imatinib | Make activation energetically unfavorable |
| Allosteric inhibitors | Bind outside ATP site, modifying 3D structure | - | Disrupt ATP interaction; high specificity |
| Covalent inhibitors | Form irreversible covalent bonds with kinase | Osimertinib, Afatinib | Prolonged inhibition; potential resistance issues |
Comparative Clinical Efficacy in EGFR-Mutant NSCLC
Recent studies directly compare the efficacy of different TKI-based strategies in resectable EGFR-mutant NSCLC:
Table 2: Comparative Efficacy of Neoadjuvant EGFR-TKI Regimens in Resectable NSCLC
| Parameter | EGFR-TKI Monotherapy (N=20) | EGFR-TKI + Chemotherapy (N=30) | Statistical Significance |
|---|---|---|---|
| Pathological Complete Response (pCR) | 5.0% (1/20) | 20.0% (6/30) | P=0.22 |
| Major Pathological Response (MPR) | 35.0% (7/20) | 36.7% (11/30) | Not significant |
| 3-Year Recurrence-Free Survival (RFS) | 46.7% | 53.4% | P=0.42 |
| RO Resection Rate | 95% | 96.7% | Not significant |
| Grade ≥3 Adverse Events | 0% | 6% (2/30) | - |
This real-world multicenter retrospective study demonstrated that while combination therapy yielded a higher pCR rate (20.0% vs. 5.0%), the MPR rates and long-term RFS were comparable between groups [26] [27]. The combination therapy group experienced higher toxicity, with 6% of patients reporting grade ≥3 adverse events compared to none in the monotherapy group [26]. These findings suggest that while combination strategies may enhance pathological responses, the optimal regimen must balance efficacy with toxicity, considering individual patient and tumor characteristics [27].
Resistance Mechanisms to Targeted Therapies
Despite initial efficacy, acquired resistance often limits long-term benefits of TKI therapy [19]. Major resistance mechanisms include:
- Target modifications: Point mutations (e.g., T790M in EGFR), amplifications, or deletions altering drug binding [19]
- Bypass signaling: Activation of alternative RTKs or downstream effectors that circumvent inhibited targets [19]
- Phenotypic changes: Epithelial-mesenchymal transition, enhanced stemness, and metabolic reprogramming [21]
- Tumor microenvironment interactions: Recruitment of pro-angiogenic bone marrow-derived cells and alternative angiogenesis models like vascular mimicry [21]
Overcoming resistance requires combination therapies targeting parallel pathways and sequential treatment strategies based on molecular profiling at progression [19].
Experimental Methodologies for Evaluating Inhibitor Efficacy
Clinical Trial Design and Endpoints
The comparative study of EGFR-TKI regimens followed rigorous methodological standards [26] [27]. Key elements included:
- Study Population: Patients with pathologically confirmed NSCLC, clinical stage II-III, confirmed EGFR mutations, and receipt of at least 4 weeks of neoadjuvant targeted therapy before planned resection [27]
- Staging Methods: Comprehensive evaluation using enhanced chest CT, PET/CT, and brain MRI within 30 days pre-treatment [27]
- Response Assessment: Imaging evaluation using RECIST 1.1 criteria and pathological assessment of tumor regression according to International Association for the Study of Lung Cancer (IASLC) criteria [27]
- Pathological Evaluation: Continuous sectioning of all lesions with tumor bed calculation based on areas of tumor, necrosis, and fibrosis, evaluated by at least two experienced pathologists at each center [27]
Assessment of Treatment Efficacy
Primary endpoints included major pathological response (MPR), defined as ≤10% viable tumor in resected specimens [26]. Secondary endpoints encompassed pathological complete response (pCR), perioperative adverse events, and long-term survival outcomes including recurrence-free survival (RFS) [26] [27]. Surgical outcomes such as R0 resection rate (complete microscopic resection) and the proportion of minimally invasive procedures were also evaluated [26].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents for Growth Factor Receptor Studies
| Reagent/Material | Function/Application | Examples/Specifics |
|---|---|---|
| Tyrosine Kinase Inhibitors | Inhibit enzymatic activity of target kinases | Osimertinib, Gefitinib, Erlotinib (EGFR); Sunitinib, Sorafenib (VEGFR) |
| Monoclonal Antibodies | Block ligand-receptor interaction or induce receptor internalization | Bevacizumab (VEGF-A); Cetuximab, Panitumumab (EGFR); Trastuzumab (HER2) |
| Receptor Ligands | Activate receptors for signaling studies | VEGF-A isoforms (121, 165, 189); EGF; PDGF |
| Phospho-Specific Antibodies | Detect activated/phosphorylated receptors and signaling proteins | Anti-phospho-EGFR; Anti-phospho-Akt; Anti-phospho-ERK |
| Live Cell Imaging Tools | Study receptor dynamics in real-time | GFP-tagged receptors; Quantum dot conjugates; Fluorescence Correlation Spectroscopy |
| Proteolytic Enzymes | Process growth factor precursors to mature forms | Furin; ADAMTS3 (for VEGF-C processing) |
| Signal Transduction Assays | Measure pathway activation | MAPK pathway reporters; PI3K activity assays; AKT phosphorylation panels |
| MeOSuc-AAPF-CMK | MeOSuc-AAPF-CMK, MF:C26H35ClN4O7, MW:551.0 g/mol | Chemical Reagent |
| Lacutoclax | Lacutoclax (LP-108)|BCL-2 Inhibitor|RUO | Lacutoclax is a selective BCL-2 inhibitor for cancer research. This product is for Research Use Only (RUO). Not for human use. |
Figure 2: Key growth factor signaling pathways and therapeutic inhibition points. The diagram illustrates VEGF/VEGFR and EGFR signaling cascades with major downstream effectors, showing points of intervention by monoclonal antibodies and tyrosine kinase inhibitors.
The structure-function relationships of growth factor receptors and their downstream effectors reveal sophisticated signaling mechanisms that are precisely regulated in health but frequently dysregulated in disease. Comparative studies of therapeutic inhibitors demonstrate that targeting specificity, resistance mechanisms, and combination approaches significantly influence clinical outcomes. While TKI-based therapies have transformed cancer treatment, emerging challenges including therapeutic resistance and adverse effects necessitate continued research into novel targeting strategies. Future directions include developing allosteric inhibitors, covalent TKIs with improved specificity, and rational combination therapies that address compensatory pathways. The integration of structural biology, live-cell imaging, and clinical translation will further advance targeted therapeutic interventions in precision oncology.
Pathway Cross-talk and Compensatory Mechanisms in Tumor Survival
Targeted therapies against specific oncogenic signaling pathways often achieve limited long-term success in oncology due to the remarkable adaptability of cancer cells. This review examines the fundamental mechanisms by which tumors evade pathway inhibition through cross-talk and compensatory signaling, with a focus on combination strategies designed to overcome therapeutic resistance. We analyze experimental data from preclinical and clinical studies targeting key oncogenic pathways, including KRAS, MEK, and receptor tyrosine kinases, providing a comparative assessment of monotherapy versus combination approaches. The synthesized evidence underscores that co-inhibition of primary and compensatory pathways represents a promising strategy to enhance therapeutic efficacy and overcome adaptive resistance in multiple cancer types.
Cancer cells exploit the inherent redundancy and interconnectivity of signaling networks to survive therapeutic insult. When a primary oncogenic driver is targeted, tumors frequently activate alternative or parallel pathways to maintain proliferation and survival signals. This adaptive resistance occurs through multiple mechanisms, including feedback loop activation, bypass signaling, and pathway rewiring. The clinical manifestation of these phenomena is often an initial response followed by disease progression, as observed with many targeted therapies. Understanding these dynamic network interactions is crucial for designing effective long-term treatment strategies that preempt or overcome resistance.
Key Compensatory Mechanisms and Experimental Evidence
KRAS-MEK-ERK Pathway and RTK Feedback
The KRAS-RAF-MEK-ERK signaling cascade represents a critical oncogenic pathway with well-documented compensatory mechanisms. MEK inhibitors initially suppress ERK phosphorylation and cell proliferation in KRAS-mutant cancers, but this inhibition triggers rapid adaptive resistance through multiple feedback loops.
Experimental Protocol: Researchers treated multiple KRAS-mutant NSCLC cell lines (A549-G12S, H460-Q61H, SK-LU-1-G12D, SW900-G12V) with the MEK inhibitor trametinib for varying durations (3-10 days). Cell proliferation was assessed via MTT assay, apoptosis by flow cytometry with YO-PRO-1/PI staining, cell cycle distribution by propidium iodide staining, and invasion capacity through Transwell assays. Signaling changes were monitored via Western blotting for phosphorylated ERK and AKT. Transcriptomic analysis identified upregulated pathways following sustained MEK inhibition [28].
Table 1: Adaptive Resistance to MEK Inhibition in KRAS-Mutant NSCLC Models
| Cell Line | KRAS Mutation | Short-term Effect (3 days) | ERK Rebound | AKT Activation | Resistance Timeline |
|---|---|---|---|---|---|
| A549 | G12S | Growth inhibition | Yes | Yes | 5-10 days |
| H460 | Q61H | Growth inhibition | Yes | Yes | 5-10 days |
| SK-LU-1 | G12D | Growth inhibition | Yes | Yes | 5-10 days |
| SW900 | G12V | Growth inhibition | Yes | Yes | 5-10 days |
| H23 | G12C | Growth inhibition | Moderate | No | >10 days |
Transcriptomic analysis revealed that prolonged trametinib treatment (10 days) significantly upregulated genes in the PI3K-AKT signaling pathway and angiogenesis-related pathways, indicating broad activation of compensatory survival signals. This feedback activation was mediated through multiple receptor tyrosine kinases (RTKs), creating a biological rationale for combined MEK and RTK inhibition [28].
Clinical Validation of Combination Therapy
The mechanistic understanding of RTK-mediated compensation led to a clinical trial (NCT04967079) evaluating trametinib (MEK inhibitor) plus anlotinib (pan-RTK inhibitor) in advanced non-G12C KRAS-mutant NSCLC patients.
Experimental Protocol: This phase I study enrolled 33 patients with advanced KRAS-mutant NSCLC. Phase Ia (13 patients) established the recommended phase 2 dose (RP2D) through a 3+3 dose escalation design. Phase Ib (20 patients) further evaluated efficacy and safety at the RP2D. Patients received trametinib (2mg) plus anlotinib (8mg) orally once daily in 21-day cycles. Primary endpoints included objective response rate (ORR) and progression-free survival (PFS). Secondary endpoints included disease control rate (DCR), overall survival (OS), and safety profile. Response assessment followed RECIST 1.1 criteria with CT scans every 6 weeks [28].
Table 2: Clinical Outcomes of MEK/RTK Co-inhibition in KRAS-Mutant NSCLC
| Parameter | Phase Ia (n=13) | Phase Ib (n=20) | Combined (n=33) |
|---|---|---|---|
| Objective Response Rate | 69.2% | 65.0% | 66.7% |
| Disease Control Rate | 92.0% | 100.0% | 97.0% |
| Median PFS (months) | 6.9 | 11.5 | 9.2 |
| Median OS (months) | Not reached | 15.5 | Not reached |
| Adverse Events ≥G3 | 23% | 35% | 30% |
The combination therapy demonstrated significantly improved outcomes compared to historical controls of MEK inhibitor monotherapy, which typically shows ORRs of 10-20% in KRAS-mutant NSCLC. The clinical validation of this combination approach effectively demonstrates that preemptive targeting of compensatory mechanisms can enhance therapeutic efficacy [28].
Metabolic Reprogramming as a Compensatory Survival Mechanism
EGFR/Akt-Driven Warburg Effect in Colorectal Cancer
Beyond direct signaling pathway cross-talk, cancer cells employ metabolic reprogramming as a compensatory survival mechanism. In colorectal cancer (CRC), EGFR/Akt signaling promotes the Warburg effect (aerobic glycolysis) through upregulation of hexokinase II (HKII), creating dual pro-survival advantages.
Experimental Protocol: Investigations into the EGFR/Akt/HKII axis involved treating CRC cell lines with xanthohumol, a natural compound that inhibits EGFR phosphorylation. Subsequent Western blot analyses demonstrated downstream Akt and HKII inhibition. Glycolytic rate was measured via extracellular acidification rate, and apoptosis was assessed by Annexin V staining and cytochrome c release. HKII overexpression rescue experiments confirmed the specific role of this metabolic enzyme in compensatory survival [29].
Table 3: Metabolic Adaptations as Compensatory Survival Mechanisms
| Cancer Type | Primary Pathway | Metabolic Adaptation | Key Enzymes/Transporters | Functional Outcome |
|---|---|---|---|---|
| Colorectal Cancer | EGFR/Akt | Aerobic glycolysis | Hexokinase II (HKII) | Enhanced ATP production, apoptosis resistance |
| Various Cancers | Angiogenesis inhibition | Altered energy metabolism | ABCG2 transporter | Chemotherapy efflux, resistance |
| SDH-mutated Cancers | Succinate accumulation | Pseudohypoxia signaling | SUCNR1 receptor | Angiogenesis, invasion, metastasis |
The mitochondrial binding of HKII not only enhances glycolytic flux but also inhibits apoptosis by closing mitochondrial permeability transition pores and preventing cytochrome c release. This dual function represents a sophisticated compensatory mechanism that links metabolic reprogramming with apoptotic resistance [29].
Succinate Receptor Signaling in Tumor Microenvironment
Metabolite sensing through G-protein coupled receptors (GPCRs) represents another dimension of compensatory signaling. The succinate receptor SUCNR1 (GPR91) activates in response to accumulated succinate, particularly in tumors with succinate dehydrogenase (SDH) mutations.
Experimental Protocol: Studies evaluating SUCNR1 signaling employed succinate stimulation in SDH-mutated cancer cells, followed by Western blot analysis of PI3K-Akt-HIF-1α pathway activation. Invasion and migration were assessed via Boyden chamber assays. Macrophage polarization was evaluated through flow cytometry analysis of surface markers and cytokine secretion profiles after succinate exposure [30].
SUCNR1 activation drives tumor progression through multiple mechanisms: directly promoting cancer cell invasion via PI3K-Akt-HIF-1α signaling, inducing angiogenesis through ERK1/2-STAT3-VEGF activation in gastric cancer, and polarizing tumor-associated macrophages toward an M2 phenotype that secretes pro-migratory cytokines like IL-6. This exemplifies how metabolic byproducts can activate compensatory signaling pathways that support tumor survival under stress conditions [30].
Research Reagent Solutions for Investigating Compensatory Mechanisms
Table 4: Essential Research Tools for Studying Pathway Cross-talk
| Research Reagent | Specific Example | Research Application | Key Findings Enabled |
|---|---|---|---|
| MEK Inhibitors | Trametinib | Blockade of KRAS downstream signaling | Identified RTK feedback activation |
| Pan-RTK Inhibitors | Anlotinib | Multi-target RTK inhibition | Demonstrated efficacy of MEK/RTK co-inhibition |
| MERTK Inhibitors | UNC2025 | Selective MERTK tyrosine kinase inhibition | Suppressed pro-survival signaling in leukemia |
| Metabolic Inhibitors | Xanthohumol | Natural compound targeting EGFR/Akt/HKII axis | Established link between signaling and metabolic reprogramming |
| GPCR Agonists/Antagonists | Succinate (SUCNR1 agonist) | SUCNR1 pathway activation | Revealed metabolite sensing in tumor microenvironment |
Visualizing Signaling Pathways and Compensatory Mechanisms
KRAS-MEK-ERK Pathway and RTK Feedback
Metabolic Reprogramming Cross-talk
Discussion and Clinical Implications
The compiled evidence demonstrates that cancer cells employ diverse compensatory mechanisms when confronted with targeted pathway inhibition. These include vertical feedback within the same pathway (ERK rebound after MEK inhibition), horizontal activation of parallel pathways (PI3K-AKT activation following MEK inhibition), and metabolic reprogramming (Warburg effect enhancement through EGFR/Akt/HKII). Successful therapeutic strategies must therefore anticipate and preempt these adaptive responses through rational combination therapies.
The clinical data supporting MEK/RTK co-inhibition in KRAS-mutant NSCLC provides a paradigm for targeting pathway cross-talk, demonstrating significantly improved response rates and progression-free survival compared to historical monotherapy outcomes. Similarly, targeting both signaling and metabolic adaptations, as seen in colorectal cancer models, represents a promising approach for overcoming therapeutic resistance.
Future research directions should focus on identifying predictive biomarkers for specific compensatory mechanisms, allowing personalized combination therapy selection. Additionally, temporal sequencing of targeted therapies to anticipate and intercept resistance evolution may further enhance durable response rates. The continued elucidation of cancer pathway interconnectivity will undoubtedly reveal new therapeutic vulnerabilities and combination strategies to improve patient outcomes.
The evolution of cancer therapy represents a fundamental shift from broad cytotoxic approaches to highly specific molecular interventions. Traditional chemotherapy, characterized by its non-selective mechanism of action on rapidly dividing cells, often resulted in significant toxicity to healthy tissues and variable efficacy. The contemporary era of precision medicine is founded on directly targeting specific molecular alterations that drive cancer pathogenesis, enabled by sophisticated diagnostic technologies that guide therapeutic decision-making [31].
This transition began with early observations of the immune system's role in tumor regression, dating back to the 1700s with documented cases of tumor suppression following erysipelas infections. William Coley's development of Coley's toxins in the late 19th century represented one of the first systematic attempts to harness the immune system against cancer [31]. The modern targeted therapy revolution accelerated with several key developments: the discovery of monoclonal antibodies in 1975, the introduction of imatinib for chronic myeloid leukemia (CML) targeting BCR-ABL1, and the clinical success of trastuzumab for HER2-positive breast cancer [31]. These milestones established that targeting specific oncogenic drivers could produce dramatic clinical responses with improved therapeutic indices compared to conventional chemotherapy.
The Diagnostic Foundation: Technological Enablers of Precision Medicine
The advancement of targeted therapies is inextricably linked to parallel innovations in molecular diagnostics that enable identification of specific therapeutic targets. Accurate detection of genetic alterations, expression patterns, and protein biomarkers is essential for appropriate patient stratification and treatment selection.
Comparative Performance of Molecular Detection Technologies
Table 1: Performance Comparison of PCR-Based Diagnostic Technologies
| Technology | Detection Principle | Quantification Method | Optimal Use Case | Sensitivity in Low Target Scenarios | Tolerance to Inhibitors |
|---|---|---|---|---|---|
| Traditional PCR | Endpoint amplification | Semi-quantitative (gel electrophoresis) | Target detection in high-concentration samples | Low | Low |
| RT-qPCR | Fluorescence detection during amplification | Relative quantification (Ct values vs. standard curve) | Viral load monitoring, gene expression analysis | Moderate | Moderate |
| Digital Droplet PCR (ddPCR) | Partitioning and endpoint detection | Absolute quantification (Poisson statistics) | Minimal residual disease, low viral load detection, sequence variants | High | High |
| RT-LAMP | Isothermal amplification with multiple primers | Visual color change or turbidity | Point-of-care testing, resource-limited settings | Variable | High |
Recent technological comparisons reveal distinct performance characteristics across detection platforms. For SARS-CoV-2 detection, RT-qPCR using the CDC protocol demonstrated high accuracy as a diagnostic standard, while RT-LAMP showed lower sensitivity but offered advantages in procedural simplicity [32]. In tuberculosis diagnostics, ddPCR exhibited superior discriminant capacity for extrapulmonary tuberculosis compared to qPCR, with area under the ROC curve values of 0.97 versus 0.94 respectively [33].
For minimal residual disease (MRD) monitoring in chronic myeloid leukemia, ddPCR provides absolute quantification of BCR-ABL1 transcripts with reduced variability compared to RT-qPCR. However, this comes with a tradeoff: ddPCR demonstrated a lower proportion of deep molecular responses and required a cutoff of three BCR-ABL1 copies per duplicate to maintain a low false-positive rate (4%) [34]. In acute leukemia diagnostics, RT-qPCR has demonstrated higher sensitivity compared to Nested-PCR for detecting fusion transcripts like RUNX1::RUNX1T1, CBFB::MYH11, and BCR::ABL1 at diagnosis [35].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Research Reagents for Targeted Therapy Development
| Reagent Category | Specific Examples | Research Application | Functional Role |
|---|---|---|---|
| Reverse Transcriptase Kits | High-Capacity cDNA Reverse Transcription Kit | cDNA synthesis from RNA templates | Enables RNA biomarker analysis and expression studies |
| PCR Master Mixes | Platinum SuperFi II PCR Master Mix, GoTaq Probe qPCR System | Amplification of target sequences with high fidelity | Provides optimized buffer conditions and polymerase for specific PCR applications |
| DNA Polymerases | Pfu polymerase, Taq polymerase | PCR amplification with varying fidelity requirements | Pfu offers proofreading (3'→5' exonuclease) for high-fidelity amplification |
| RNA Extraction Kits | QIAmp Viral RNA Kit, TRIzol Reagent | Nucleic acid isolation from clinical samples | Provides high-purity RNA for downstream molecular applications |
| Fluorescent Probes | Hydrolysis probes (TaqMan), DNA binding dyes (SYBR Green) | Real-time detection of amplification products | Enables quantification and detection of specific targets in qPCR and ddPCR |
| Digital PCR Reagents | Droplet generation oil, supermixes | Partitioning and amplification for absolute quantification | Facilitates digital PCR workflow for highly sensitive detection |
| Ala-Ala-Pro-pNA | Ala-Ala-Pro-pNA, MF:C17H23N5O5, MW:377.4 g/mol | Chemical Reagent | Bench Chemicals |
| Dyrk2-IN-1 | Dyrk2-IN-1, MF:C29H31FN8O2S, MW:574.7 g/mol | Chemical Reagent | Bench Chemicals |
Key Signaling Pathways and Their Inhibitors
Targeted therapies function through precise intervention in dysregulated signaling networks that govern cellular proliferation, survival, and death. The following diagram illustrates major pathways currently targeted in precision oncology:
The EGFR signaling pathway represents one of the most successfully targeted oncogenic drivers, particularly in non-small cell lung cancer (NSCLC). Current first-line approaches for EGFR-mutant NSCLC include osimertinib as a single agent, osimertinib plus chemotherapy, or amivantamab (a bispecific antibody) plus lazertinib [36]. Resistance mechanisms remain a challenge, spurring development of next-generation agents like SYS6010, a novel EGFR-targeting antibody-drug conjugate showing promise in tumors resistant to available treatments [36].
The KRAS pathway, once considered "undruggable," has witnessed remarkable progress with the development of G12C-specific inhibitors (sotorasib, adagrasib). Research is now advancing beyond G12C to target other KRAS mutations, including G12D inhibitors (zoldonrasib/RMC-9805) and pan-KRAS inhibitors (AMG410) that target all KRAS mutation types while sparing wild-type KRAS signaling [36].
Experimental Workflows for Therapeutic Assessment
The development and evaluation of targeted therapies requires standardized methodologies to assess both compound efficacy and accompanying diagnostic approaches. The following diagram outlines a representative workflow for evaluating signaling pathway inhibitors:
Protocol: RT-ddPCR for Low-Abundance Transcript Detection
The accurate quantification of low-abundance targets is essential for monitoring minimal residual disease and assessing targeted therapy response. The following protocol is adapted from SARS-CoV-2 research but demonstrates principles applicable to oncology biomarkers [37]:
Sample Preparation:
- Obtain RNA from patient samples (blood, tissue, or other relevant biospecimens) using commercial extraction kits (e.g., QIAmp Viral RNA Kit)
- Quantify RNA using spectrophotometry (NanoDrop2000) and standardize concentration to 20 ng/μL
- Assess RNA quality using 260/280 nm ratio; samples with ratios between 1.8-2.0 are considered high purity
Reverse Transcription:
- Perform cDNA synthesis using High-Capacity cDNA Reverse Transcription Kit
- Use 20 μL RNA template per reaction
- Conduct reverse transcription in a thermal cycler with the following conditions: 10 minutes at 25°C, 120 minutes at 37°C, 5 minutes at 85°C
Droplet Digital PCR:
- Prepare reaction mix containing:
- 10 μL ddPCR Supermix
- 1 μL multiplexed primer/probe sets (targeting genes of interest and reference genes)
- 5 μL cDNA template
- Nuclease-free water to 20 μL final volume
- Generate droplets using droplet generator
- Transfer droplets to a 96-well PCR plate and seal
- Perform PCR amplification with the following conditions:
- 95°C for 10 minutes (enzyme activation)
- 40 cycles of: 94°C for 30 seconds (denaturation) and 60°C for 60 seconds (annealing/extension)
- 98°C for 10 minutes (enzyme deactivation)
- Read plate on droplet reader and analyze using Poisson statistics for absolute quantification
This protocol's key advantage is its ability to detect sequence mismatches through differential fluorescence amplitude, providing insights into tumor evolution and heterogeneity [37].
Protocol: Circulating Tumor DNA Analysis for Therapy Monitoring
Liquid biopsy approaches using circulating tumor DNA (ctDNA) have transformed monitoring of targeted therapy response and resistance emergence:
Sample Collection and Processing:
- Collect peripheral blood (typically 10-20 mL) in cell-stabilizing tubes
- Process within 4-6 hours of collection to prevent nucleic acid degradation
- Centrifuge at 5000 rpm for 5 minutes to separate plasma component
- Aliquot plasma and store at -80°C until analysis
ctDNA Extraction and Analysis:
- Extract ctDNA from 2-4 mL plasma using commercial circulating nucleic acid kits
- Quantify total cell-free DNA using fluorometry
- Analyze specific mutations using either:
- RT-qPCR: For known hotspot mutations with established assays
- Next-generation sequencing: For broader mutation profiling
- For RT-qPCR analysis:
- Use 5-20 ng ctDNA per reaction
- Apply probe-based detection with mutation-specific fluorescent probes
- Run in triplicate to ensure reproducibility
- For ddPCR analysis:
- Partition samples into approximately 20,000 droplets
- Use target-specific probes with different fluorophores for mutant and wild-type sequences
- Calculate mutant allele frequency based on positive droplet counts
Clinical Interpretation:
- Pre-surgery ctDNA levels predict recurrence patterns and overall outcomes
- Post-surgery ctDNA detection indicates minimal residual disease and need for adjuvant therapy
- Rising ctDNA during monitoring suggests emerging resistance to targeted therapy
- Specific mutation patterns in ctDNA can guide subsequent targeted therapy selection
Recent studies demonstrate that pre-surgery ctDNA levels in early-stage NSCLC predict recurrence locations (lung, distant non-brain, or brain) and identify patients requiring more aggressive treatment approaches [36].
Clinical Impact and Future Directions
The translation of targeted therapies from laboratory discovery to clinical application has produced substantial improvements in patient outcomes across multiple cancer types. In advanced breast cancer, survival times have increased progressively from 27.5 months (2011-2013) to 34.3 months (2020-2022), with particularly dramatic improvements in HER2-positive subtypes (increasing from 42 to 53.1 months) [38]. These gains directly correspond with the introduction of targeted agents including CDK4/6 inhibitors for HR+ disease, HER2-directed therapies, and recently, antibody-drug conjugates and PARP inhibitors for TNBC [38].
The future trajectory of targeted therapy development includes several promising areas. First, pan-KRAS inhibitors that target multiple KRAS mutation types while sparing wild-type KRAS signaling represent a significant advancement beyond current G12C-specific agents [36]. Second, radioligand therapies that deliver radiation specifically to cancer cells expressing surface targets (e.g., DLL3 in small cell lung cancer) combine precision targeting with potent cytotoxic effects [36]. Third, artificial intelligence approaches are accelerating drug discovery, with researchers now able to screen over one million compounds to identify promising candidates for preventing progression and metastasis of early-stage lung adenocarcinoma [36].
The ongoing challenge of therapeutic resistance continues to drive innovation in both therapeutic compounds and diagnostic approaches. Detection of mesenchymal circulating tumor cells in ALK fusion-positive lung cancer patients experiencing progression on ALK inhibitors illustrates how sophisticated monitoring techniques can predict treatment failure before radiographic progression [36]. Similarly, blood tests measuring SCLC tumor DNA fraction and immunosuppressive cell populations show promise in predicting responses to immunotherapy in small cell lung cancer [36].
As targeted therapies continue to evolve, the integration of advanced diagnostic technologies with therapeutic development will remain essential for realizing the full potential of precision oncology across diverse cancer types and patient populations.
Development Strategies and Therapeutic Applications of Pathway Inhibitors
Protein kinases represent one of the most important drug target families in the 21st century due to their frequent dysregulation in inflammatory diseases and cancer [7]. Since the landmark approval of imatinib in 2001, the development of small molecule kinase inhibitors has expanded dramatically, with the FDA recently approving the 100th small-molecule kinase inhibitor [39]. These inhibitors function by targeting the ATP-binding pocket or allosteric sites on kinases, preventing the phosphorylation and activation of downstream signaling pathways that drive disease progression [40]. The systematic classification of these inhibitors into Types I-VI based on their binding modes and mechanisms provides a crucial framework for understanding their therapeutic applications and guiding future drug design efforts [41] [40].
Targeted small molecule inhibitors offer significant advantages over traditional chemotherapy, including improved efficacy and safety profiles due to their specific action on molecular targets [40]. As of December 2020, 89 small-molecule targeted antitumor drugs had been approved by the US FDA and China's NMPA, with the number continuing to grow [40]. This article provides a comprehensive comparison of Type I-VI inhibitor classification, binding mechanisms, experimental characterization methods, and applications in targeted cancer therapy, with a specific focus on their implementation in drug discovery workflows.
Type I-VI Inhibitor Classification and Binding Mechanisms
Structural Classification Framework
The Roskoski classification system categorizes small molecule protein kinase inhibitors into six primary types (I-VI) based on their binding mode to the target enzyme [41] [40]. This classification system has become one of the most widely used methods for characterizing kinase inhibitors and provides critical insights into their mechanism of action, selectivity, and potential therapeutic applications.
Table 1: Classification of Small Molecule Protein Kinase Inhibitors
| Type | Binding Site | Kinase Conformation | Binding Reversibility | Key Structural Features |
|---|---|---|---|---|
| Type I | ATP-binding pocket | Active (DFG-Asp in, αC-helix in) | Reversible | Binds hinge region; occupies adenine binding pocket |
| Type I½ | ATP-binding pocket | DFG-Asp in inactive | Reversible | Extends into back cleft; long residence time |
| Type II | ATP-binding pocket | DFG-Asp out inactive | Reversible | Occupies adjacent hydrophobic pocket |
| Type III | Allosteric site adjacent to ATP pocket | N/A | Reversible | Does not compete with ATP binding |
| Type IV | Allosteric site outside cleft | N/A | Reversible | Binds distant from ATP pocket |
| Type V | Two different regions | N/A | Reversible | Bivalent inhibitors |
| Type VI | Covalent binding to kinase | Various | Irreversible | Forms covalent bond with nucleophilic residues |
Detailed Binding Mechanisms
Type I inhibitors represent the largest class of kinase inhibitors and target the active conformation of the kinase. They bind to the ATP-binding pocket when the activation loop adopts a DFG-Asp in conformation and the αC-helix is positioned inward [41]. These inhibitors typically form hydrogen bonds with the hinge region connecting the small and large lobes of the enzyme and occupy part of the adenine binding pocket [40]. Approximately 75 of the 85 FDA-approved small molecule protein kinase inhibitors are prescribed for neoplasms, with the remaining seven (including abrocitinib, baricitinib, and tofacitinib) used for inflammatory diseases [7].
Type I½ and Type II inhibitors both target inactive kinase conformations but with distinct structural differences. Type I½ inhibitors bind to a DFG-Asp in inactive kinase conformation with the αC-helix out, while Type II inhibitors bind to a DFG-Asp out inactive conformation [40]. Both types occupy the adenine binding pocket and form hinge region hydrogen bonds. These inhibitors are further divided into A and B subtypes based on their extension into the back cleft. Type A inhibitors extend past the gatekeeper residue into the back cleft and typically have long residence times (minutes to hours), while Type B inhibitors fail to extend into the back cleft and exhibit shorter residence times (seconds to minutes) [41].
Type III and Type IV inhibitors are allosteric in nature and do not compete directly with ATP binding. Type III inhibitors bind to a site adjacent to the ATP-binding pocket in the cleft between the small and large kinase lobes, while Type IV inhibitors bind outside of this cleft entirely [40]. These allosteric inhibitors often demonstrate improved selectivity due to the lower conservation of allosteric sites compared to the highly conserved ATP-binding pocket across the kinome.
Type V inhibitors are bivalent molecules that span two distinct regions of the kinase domain, while Type VI inhibitors form covalent bonds with their target enzymes, typically through reactive functional groups that target nucleophilic cysteine residues [40]. The covalent binding mechanism of Type VI inhibitors can provide prolonged target engagement and potentially overcome certain resistance mechanisms.
Diagram 1: Small Molecule Inhibitor Classification Framework
Experimental Characterization Methods
Structural Biology Approaches
X-ray Crystallography remains the gold standard for determining the binding modes of small molecule inhibitors to their target kinases. This method provides atomic-resolution structures of drug-enzyme complexes, enabling precise classification of inhibitor types based on kinase conformation and binding site location [41]. The X-ray crystal structures of 21 out of 27 FDA-approved small molecule inhibitors bound to their target protein kinases have been determined, providing crucial structural information for the classification system [41]. The methodology involves co-crystallizing the kinase domain with the inhibitor, collecting diffraction data, and solving the structure through molecular replacement or other phasing methods.
Crystallography Protocol:
- Express and purify the kinase domain of interest
- Co-crystallize with inhibitor using vapor diffusion or microbatch methods
- Optimize crystal growth conditions through screening additives and precipitants
- Collect X-ray diffraction data at synchrotron facilities
- Solve structure using molecular replacement with known kinase structures as templates
- Refine structure with iterative model building and computational refinement
- Analyze binding interactions and conformational changes induced by inhibitor
Computational and Biophysical Methods
Molecular Dynamics (MD) Simulations provide dynamic information about inhibitor binding mechanisms and conformational changes that cannot be captured by static crystal structures. Recent advances integrate MD with deep learning approaches to identify significant functional domains and binding selectivity [42]. For bromodomain inhibitors like those targeting BRD4 and BRD9, MD simulations have revealed that flexible loops (ZA-loop and BC-loop) significantly contribute to inhibitor binding selectivity [42].
MD Simulation Workflow:
- Build simulation system from crystal structure with explicit solvation
- Parameterize inhibitors using appropriate force fields
- Equilibrate system with gradual heating and pressure coupling
- Production run for 100ns-1μs depending on system size and research question
- Analyze trajectories for root-mean-square deviation, binding pocket volumes, and interaction persistence
- Perform binding free energy calculations using MM-GBSA or related methods
- Apply deep learning to identify key conformational features from trajectories
Binding Free Energy Calculations using methods like MM-GBSA (Molecular Mechanics with Generalized Born and Surface Area solvation) provide quantitative assessment of inhibitor binding affinity and identify key residues contributing to binding. For BRD4 and BRD9 inhibitors, these calculations have verified that van der Waals interactions are the primary forces responsible for inhibitor binding, with binding ability of H1B, JQ1 and TVU to BRD9 being stronger than to BRD4 [42].
Diagram 2: Experimental Characterization Workflow for Inhibitor Design
Research Reagent Solutions
Table 2: Essential Research Reagents for Kinase Inhibitor Characterization
| Reagent/Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| Kinase Expression Systems | Baculovirus (Sf9 cells), E. coli | Recombinant kinase production | Tagged constructs for purification |
| Crystallization Screens | Commercial sparse matrix screens | Crystal formation optimization | 96-condition initial screening |
| MD Simulation Software | AMBER, GROMACS, CHARMM | Molecular dynamics simulations | Force field parameterization |
| Binding Assay Kits | FP, TR-FRET, mobility shift | High-throughput inhibitor screening | Miniaturized format (384-well) |
| Covalent Probe Reagents | Iodoacetamide-fluorophore | Cysteine reactivity profiling | Type VI inhibitor characterization |
| Selectivity Panels | Kinase profiling services | Off-target activity assessment | Broad kinome coverage (200+ kinases) |
Comparative Analysis of Inhibitor Classes in Clinical Applications
CDK4/6 Inhibitors in Breast Cancer
CDK4/6 inhibitors represent a clinically significant class of small molecule inhibitors that have transformed the treatment landscape for HR+/HER2- advanced or metastatic breast cancer [43] [44]. These inhibitors target the cyclin D-CDK4/6 complex, preventing phosphorylation of the retinoblastoma (RB) protein and arresting cell cycle progression at the G1 phase [44]. First-line CDK4/6 inhibitors combined with endocrine therapy have demonstrated superior outcomes compared to endocrine therapy alone, with significant improvements in progression-free survival (PFS) and overall survival (OS) [43].
Table 3: Clinical Performance of CDK4/6 Inhibitors in Advanced Breast Cancer
| CDK4/6 Inhibitor | Combination Therapy | Median PFS (months) | Median OS (months) | Objective Response Rate | Severe Adverse Events Risk |
|---|---|---|---|---|---|
| Abemaciclib + AI | Aromatase Inhibitors | 27.0 | 59.6 | Superior ORR (RR=1.39) | Increased SAEs (RR=1.54) |
| Ribociclib + AI | Aromatase Inhibitors | - | - | - | - |
| Palbociclib + AI | Aromatase Inhibitors | - | - | - | - |
| Endocrine Therapy Alone | - | 14.4 | 50.0 | Reference | Reference |
Network meta-analysis of 24 studies involving 15,602 patients revealed that abemaciclib plus aromatase inhibitors (AI) represents one of the most effective combination therapies in terms of PFS, showing significant differences relative to palbociclib plus fulvestrant (HR = 2.01), abemaciclib plus fulvestrant (HR = 2.68), and ribociclib plus fulvestrant (HR = 2.75) [44]. The superior performance of specific CDK4/6 inhibitor combinations highlights the importance of molecular features in determining therapeutic outcomes.
BRD4 and BRD9 Inhibitors in Epigenetic Regulation
Bromodomain inhibitors targeting BRD4 and BRD9 represent an emerging class of epigenetic therapeutics with applications in cancer, inflammatory diseases, and other disorders [42] [45]. BRD4, a member of the bromodomain and extra-terminal (BET) family, recognizes acetylated lysine residues on histones and regulates gene transcription, with abnormalities leading to disorders of gene expression that play key roles in tumor development [42] [45]. Structural studies reveal that despite large sequence variations, all BRD proteins share a common topology with a left-handed bundle of four alpha helices connected by functional loop regions (ZA and BC loops) responsible for substrate specificity [42].
Comparative studies of BRD4 and BRD9 inhibitors using molecular dynamics simulations and binding free energy calculations have provided insights into their binding selectivity. The binding ability of inhibitors H1B, JQ1, and TVU to BRD9 is stronger than to BRD4, with van der Waals interactions identified as the primary forces responsible for inhibitor binding [42]. These findings have important implications for the development of selective inhibitors targeting specific BRD family members, which could potentially improve therapeutic efficacy while reducing off-target effects.
The classification of small molecule inhibitors into Types I-VI provides a valuable framework for understanding their mechanisms of action and guiding rational drug design. Each inhibitor type offers distinct advantages: Type I and II inhibitors targeting the ATP-binding pocket often demonstrate high potency, while Type III and IV allosteric inhibitors can provide improved selectivity. Type V bivalent inhibitors engage multiple binding sites, and Type VI covalent inhibitors offer prolonged target engagement. The choice of inhibitor type depends on the specific therapeutic context, considering factors such as target structure, resistance mechanisms, and desired pharmacokinetic properties.
Future directions in small molecule inhibitor design include the development of compounds with enhanced selectivity profiles, strategies to overcome resistance mutations, and the exploration of novel target classes beyond kinases. Protein degradation approaches such as PROTACs (proteolysis-targeting chimeras) represent an emerging modality that extends the capabilities of traditional inhibitory mechanisms [45]. Additionally, the integration of computational methods like molecular dynamics simulations with deep learning approaches shows promise for accelerating inhibitor discovery and optimization [42]. As structural biology techniques advance and our understanding of signaling pathways deepens, the rational design of small molecule inhibitors will continue to evolve, providing new therapeutic options for cancer and other diseases driven by dysregulated signaling pathways.
The paradigm of drug discovery has traditionally been dominated by the "one target–one drug" hypothesis, a concept rooted in the lock-and-key model proposed over a century ago [46]. This approach aims to minimize undesirable effects by selectively modulating a single biological target [46]. However, the multifactorial nature of complex diseases such as cancer, neurodegenerative disorders, and chronic inflammatory conditions often renders single-target interventions inadequate for effective treatment [46] [47]. Consequently, multi-target strategies have emerged as a promising alternative, designed to interact with multiple biological targets simultaneously through different mechanisms [46]. This review objectively compares the therapeutic advantages and limitations of single-target and multi-target approaches, providing a structured analysis for researchers, scientists, and drug development professionals engaged in the comparative effectiveness of signaling pathway inhibitors.
Conceptual Foundations and Definitions
Single-Target Approaches
Single-target drugs, also known as monotherapies, are designed to combat diseases by selectively attacking specific genes, proteins, or receptors responsible for pathological processes [48]. This strategy is based on the assumption that disease symptoms or progression can be mitigated by precisely activating or inhibiting a single biological target [46]. A prominent example is imatinib, which targets the BCR-ABL fusion protein in chronic myeloid leukemia [49].
Multi-Target Approaches
Multi-target drugs are molecules that incorporate pharmacophore groups for two or more biological targets within a single structure, enabling simultaneous interaction with multiple molecular targets [46]. This approach encompasses several strategies:
- Multi-Target Directed Ligands (MTDLs): Single chemical entities designed to modulate multiple targets simultaneously [48].
- Combination Therapy: Administration of two or more drugs with different mechanisms of action [48].
- Polypharmacology: The inherent ability of a single drug to interact with multiple biological targets, whether by design or serendipity [46].
MTDLs are further developed through framework combination approaches, including fused, merged, or linked pharmacophores from active molecules [48].
Comparative Analysis of Therapeutic Profiles
Table 1: Comparative analysis of single-target versus multi-target therapeutic approaches
| Parameter | Single-Target Approach | Multi-Target Approach |
|---|---|---|
| Efficacy in Complex Diseases | Often insufficient for multigenic diseases (e.g., Alzheimer's, cancer, diabetes) [46] | Enhanced efficacy through simultaneous pathway modulation; addresses disease heterogeneity [46] [48] |
| Resistance Development | Higher susceptibility due to single-point mutations or pathway reactivation [46] [48] | Reduced likelihood through complementary mechanisms; overcomes clonal heterogeneity [46] [48] |
| Toxicity Profile | Targeted side effects; generally predictable [48] | Potentially reduced toxicity through lower dosages; risk of off-target effects [46] [50] [48] |
| Therapeutic Specificity | High specificity for intended target [49] | Balanced selectivity across multiple targets; potentially broader physiological impact [46] [50] |
| Development Complexity | Straightforward target validation and optimization [46] | Complex design and optimization; requires balancing multiple pharmacophores [46] [50] |
| Clinical Validation | Established regulatory pathways [46] | Extensive preclinical and clinical validation needed; higher development costs [46] [50] |
| Applicable Diseases | Ideal for molecularly defined subtypes; infectious diseases [46] | Complex, multifactorial conditions (neurodegenerative diseases, cancer, metabolic disorders) [46] [47] |
Table 2: Clinical performance metrics in oncology applications
| Therapeutic Class | Objective Response Rate (ORR) | Progression-Free Survival (PFS) | Overall Survival (OS) | Grade 3+ Adverse Events |
|---|---|---|---|---|
| TACE + MTT + PD-(L)1 (Combination) | ORR=1.29 (95% CI: 0.64–2.60; p=0.479) [51] | HR=0.68 (p=0.131) [51] | HR=0.86 (p=0.674) [51] | 52% (p<0.0001) [51] |
| MTT + PD-(L)1 (Systemic) | Reference [51] | Reference [51] | Reference [51] | 15% (p<0.0001) [51] |
| FGFR Inhibitors | Varies by alteration type: amplifications (53.7-66%), mutations (26-38.8%), rearrangements/fusions (5.6-8%) [52] | Varies by specific inhibitor and cancer type [52] | Varies by specific inhibitor and cancer type [52] | Class-specific toxicities (e.g., hyperphosphatemia, ocular disorders) [52] |
| SIK2/PARP-1 Co-inhibition | Preclinical evidence of enhanced efficacy in HR-proficient tumors [53] | Potential improvement through dual synthetic lethality [53] | Theoretical improvement via metabolic reprogramming and immune modulation [53] | Not yet quantified (preclinical stage) [53] |
Experimental Models and Methodologies
Biochemical Kinase Profiling
Comprehensive kinase profiling employs panels of biochemical kinase assays (e.g., 255 wild-type kinases) to determine inhibitor selectivity [54]. Compounds are tested at concentration ranges (typically 1 μmol/L) with ATP levels near the KM,ATP for each kinase. Inhibition is measured via mobility shift assays (MSA), immobilized metal ion affinity particle (IMAP) assays, or enzyme-linked immunosorbent assays (ELISA) for specific kinases like MEK1/2 [54]. IC50 values are determined using duplicate 10-point dilution series, with data analysis employing 4-parameter logistic curve fitting and F-test validation for curve quality [54].
Cancer Cell Line Viability Assays
Cell panel profiling utilizes extensive cancer cell line collections (e.g., 134 lines) to assess compound efficacy [54]. Cells are seeded in optimized densities in 384-well plates, followed by 24-hour incubation before compound addition. Inhibitor stock solutions in DMSO are diluted in √10-fold steps to create 9-point dilution series, further diluted in HEPES buffer, and added to cells (final DMSO concentration 0.4% v/v). Following 72-hour incubation, viability is assessed via ATP quantification using luminescence-based assays. IC50 values are calculated similarly to kinase assays, with biphasic curves indicating potential dual mechanisms of action [54].
Biomarker Identification and Validation
Genomic and transcriptomic data from responsive cell lines are correlated with sensitivity profiles to identify predictive biomarkers [54]. For example, the uncommon EGFR p.G719S mutation was identified as a common response marker for EGFR inhibitors through comparative profiling of gefitinib, dacomitinib, and osimertinib [54]. Similarly, FGFR alterations predict sensitivity to FGFR inhibitors regardless of their specific clinical indications [54].
Signaling Pathways and Mechanisms
Key Oncogenic Signaling Pathways
The following diagram illustrates central cancer-associated signaling pathways and their intersections, highlighting potential multi-target intervention points:
Diagram 1: Central oncogenic signaling pathways and their interactions, highlighting potential multi-target intervention points.
Multi-Target Inhibitor Mechanisms
The diagram below illustrates the conceptual framework for multi-target drug design strategies, showing how single-target pharmacophores are combined:
Diagram 2: Multi-target drug design strategies framework.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential research reagents and technologies for inhibitor profiling
| Reagent/Technology | Function/Application | Example Use Cases |
|---|---|---|
| Biochemical Kinase Assay Panels | High-throughput screening of inhibitor activity against multiple kinases | Selectivity profiling across 255+ kinase assays [54] |
| Cancer Cell Line Panels | Assessment of compound efficacy in diverse genetic backgrounds | Viability assays across 134+ cancer cell lines [54] |
| Mobility Shift Assays (MSA) | Measure kinase activity through electrophoretic mobility changes | Kinase inhibition profiling at KM,ATP concentrations [54] |
| IMAP Assays | Fluorescence polarization-based kinase activity measurement | Alternative to MSA for specific kinase families [54] |
| ATP-based Viability Assays | Quantify cell viability through intracellular ATP levels | High-throughput compound screening in cell models [54] |
| 3D Cell Culture Systems | More physiologically relevant disease modeling | Automated platforms (e.g., MO:BOT) for organoid culture [55] |
| Multi-omics Integration Platforms | Combine genomic, transcriptomic, and proteomic data | Biomarker identification and validation [55] |
| AI-Assisted Drug Design Tools | Predict multi-target interactions and optimize lead compounds | Virtual screening and molecular docking studies [47] [50] |
| Hsd17B13-IN-16 | Hsd17B13-IN-16|HSD17B13 Inhibitor For Research | Hsd17B13-IN-16 is a research compound targeting HSD17B13 for liver disease studies. This product is For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| Tubulin inhibitor 43 | Tubulin inhibitor 43, MF:C20H21NO6, MW:371.4 g/mol | Chemical Reagent |
The comparative analysis of single-target and multi-target approaches reveals a nuanced therapeutic landscape where each strategy offers distinct advantages depending on the disease context. Single-target therapies provide precision and well-characterized safety profiles for molecularly defined conditions, while multi-target approaches demonstrate superior efficacy for complex, multifactorial diseases through simultaneous pathway modulation. The emerging integration of comprehensive profiling methodologies—combining biochemical kinase assays, cancer cell line panels, and multi-omics data—enables more informed therapeutic choices and targeted development strategies. As drug discovery evolves, the strategic application of both paradigms, guided by robust experimental data and mechanistic understanding, will maximize therapeutic outcomes across diverse disease contexts.
Bruton's tyrosine kinase (BTK) inhibitors have revolutionized the treatment landscape for B-cell malignancies, representing one of the most significant advances in targeted cancer therapy over the past decade. As a critical component of the B-cell receptor (BCR) signaling pathway, BTK plays a fundamental role in the proliferation, survival, and migration of malignant B cells [56]. The development of therapeutic agents targeting BTK has evolved through multiple generations, each addressing limitations of its predecessors while maintaining potent pathway inhibition.
The first-generation BTK inhibitor ibrutinib demonstrated unprecedented efficacy in chronic lymphocytic leukemia (CLL) and other B-cell malignancies, leading to its rapid regulatory approval and clinical adoption [57]. Subsequent second-generation inhibitors including acalabrutinib and zanubrutinib were designed with improved kinase selectivity to mitigate off-target toxicities while preserving efficacy [58]. Most recently, third-generation non-covalent inhibitors and novel therapeutic modalities like BTK degraders have emerged to address resistance mechanisms that limit earlier agents [59].
This review provides a comprehensive comparison of BTK inhibitors, focusing on their relative efficacy, safety profiles, resistance mechanisms, and appropriate clinical applications. We synthesize evidence from key clinical trials, long-term follow-up data, and network meta-analyses to inform researchers, scientists, and drug development professionals about the current state and future directions of BTK-targeted therapeutics.
The BTK Signaling Pathway and Therapeutic Targeting
Bruton's tyrosine kinase is a cytoplasmic non-receptor tyrosine kinase belonging to the Tec family of kinases. It is expressed in most hematopoietic cells except T cells and plasma cells, with particularly important functions in B-lymphocyte development, differentiation, and signaling [56]. Following B-cell receptor activation, BTK is phosphorylated by upstream Src-family kinases, leading to its activation and subsequent phosphorylation of phospholipase C gamma 2 (PLCG2). This initiates downstream signaling cascades including NF-κB, ERK, and AKT pathways that promote B-cell survival and proliferation [56].
In malignant B cells, this tonic BCR signaling becomes dysregulated, creating dependency on BTK-mediated survival signals. BTK inhibitors exploit this dependency by binding to the kinase domain of BTK, preventing autophosphorylation and subsequent activation of downstream signaling pathways [59]. The resulting disruption of these critical survival signals induces apoptosis and inhibits proliferation and migration of malignant B cells.
The diagram below illustrates the BTK signaling pathway and mechanism of action for different classes of BTK inhibitors:
Figure 1: BTK Signaling Pathway and Inhibitor Mechanisms. This diagram illustrates the B-cell receptor signaling cascade through BTK and PLCG2 to downstream survival pathways, alongside the mechanisms of different BTK inhibitor classes.
Comparative Efficacy of BTK Inhibitors
Clinical Trial Data and Direct Comparisons
The efficacy profiles of BTK inhibitors have been established through pivotal clinical trials across various B-cell malignancies, with the most extensive data available for CLL/SLL. First-generation ibrutinib demonstrated groundbreaking efficacy in the RESONATE-2 trial, which showed a median progression-free survival (PFS) of 8.9 years compared to just 1.3 years with chlorambucil in treatment-naïve CLL/SLL patients after nearly a decade of follow-up [60]. The 9-year overall survival (OS) rate was 68% for all patients in the ibrutinib arm, with particularly impressive results in high-risk genomic subgroups including unmutated IGHV, del(11q), TP53 mutation, or complex karyotype [60].
Second-generation BTK inhibitors were developed primarily to improve the safety profile of ibrutinib while maintaining comparable efficacy. In the ELEVATE-RR trial, acalabrutinib demonstrated non-inferior efficacy to ibrutinib in relapsed/refractory CLL with a median PFS of 38.4 months in both arms, but with significantly reduced rates of atrial fibrillation (5.8% vs 13.3%) and other adverse events [58]. Similarly, the ALPINE trial showed superior overall response rates with zanubrutinib compared to ibrutinib (80.4% vs 72.9%) in relapsed/refractory CLL, along with more favorable cardiac safety [61].
A recent network meta-analysis specifically focused on high-risk relapsed/refractory CLL populations provides the most comprehensive efficacy comparison to date. This analysis found zanubrutinib to be the most efficacious treatment, with significantly reduced risk of progression or death compared with ibrutinib (HR, 0.49; 95% CrI, 0.31-0.78) and acalabrutinib (HR, 0.55; 95% CrI, 0.32-0.94) [62]. Differences in overall survival demonstrated a numerical trend favoring zanubrutinib compared with ibrutinib (HR, 0.59; 95% CrI, 0.31-1.11) and acalabrutinib (HR, 0.72; 95% CrI, 0.35-1.50) [62].
Table 1: Key Efficacy Outcomes from Pivotal BTK Inhibitor Clinical Trials in CLL/SLL
| Trial | Phase | Patient Population | Treatment Arms | Median PFS | ORR | Key Efficacy Findings |
|---|---|---|---|---|---|---|
| RESONATE-2 [60] | 3 | Treatment-naïve CLL/SLL | Ibrutinib vs Chlorambucil | 8.9 years vs 1.3 years | 86% vs 35% | 9-year OS rate: 68% with ibrutinib; High-risk subgroup median PFS: 8.4 years |
| ALPINE [62] [61] | 3 | R/R CLL/SLL | Zanubrutinib vs Ibrutinib | Not reported | 80.4% vs 72.9% | Superior ORR with zanubrutinib (P=0.03); PFS benefit in high-risk patients (HR 0.49) |
| ELEVATE-RR [58] | 3 | R/R CLL with high-risk features | Acalabrutinib vs Ibrutinib | 38.4 mo vs 38.4 mo | 81% vs 77% | Non-inferior PFS; Reduced atrial fibrillation with acalabrutinib (5.8% vs 13.3%) |
| SEQUOIA [61] | 3 | Treatment-naïve CLL/SLL | Zanubrutinib vs BR | 6-year PFS: 74% | Not reported | Sustained PFS superiority vs chemoimmunotherapy; 6-year OS: 84% (88% COVID-adjusted) |
| CAPTIVATE [63] | 2 | Treatment-naïve CLL/SLL | Ibrutinib + Venetoclax (FD) | 5.5-year PFS: 66% | 97% | MRD status at EOT predictive of long-term PFS; 5.5-year OS: 97% |
Efficacy in High-Risk Genetic Subgroups
Patients with high-risk genetic features such as del(17p), TP53 mutations, and unmutated IGHV status have historically experienced poor outcomes with chemoimmunotherapy. BTK inhibitors have substantially improved outcomes for these difficult-to-treat populations. In the RESONATE-2 trial, the median PFS for patients with at least one high-risk genomic feature was 8.4 years with ibrutinib versus 0.7 years with chlorambucil [60]. The 9-year PFS rate for these high-risk patients on ibrutinib was 47%, demonstrating the ability of BTK inhibition to overcome the poor prognosis typically associated with these genetic alterations [60].
The network meta-analysis by Shadman et al. specifically examined high-risk relapsed/refractory CLL populations defined by the presence of del(17p) and/or TP53 mutations. In this analysis, zanubrutinib demonstrated superior efficacy not only compared to ibrutinib and acalabrutinib, but also to chemoimmunotherapy regimens including bendamustine + rituximab and idelalisib + rituximab (HR, 0.12; 95% CrI, 0.05-0.26) [62]. These findings position zanubrutinib as a particularly compelling option for patients with high-risk genetic features, though all BTK inhibitors show improved activity in these populations compared to pre-BTK inhibitor era treatments.
Safety and Tolerability Profiles
The safety and tolerability profiles of BTK inhibitors represent a key differentiator between agents, particularly as treatment durations extend with the continuous dosing approach used for most covalent BTK inhibitors. Ibrutinib is associated with characteristic adverse events including diarrhea (52%), fatigue (41%), cough (39%), and nausea (32%) based on long-term follow-up from the RESONATE-2 trial [60]. More concerning are the cardiovascular toxicities, with atrial fibrillation occurring in approximately 9% of patients in the relapsed/refractory setting based on a 10-year follow-up study [57], and hypertension occurring in 30.9% of patients (grade 3 or higher) [57].
Second-generation BTK inhibitors were specifically designed to improve kinome selectivity and reduce off-target toxicities. This development strategy has yielded measurable clinical benefits, with acalabrutinib demonstrating significantly lower rates of atrial fibrillation (5.8% vs 13.3%) and bleeding events compared to ibrutinib in the ELEVATE-RR trial [58]. Similarly, zanubrutinib has shown improved cardiac safety compared to ibrutinib, with lower rates of atrial fibrillation and other cardiovascular events [58] [61].
The management of adverse events is crucial for maintaining patients on long-term BTK inhibitor therapy. In the RESONATE-2 trial, 25% of patients required a dose reduction due to adverse events, with improvements seen in 88% of these patients [60]. This demonstrates that active dose management strategies can effectively mitigate adverse events and allow patients to remain on treatment, highlighting the importance of close monitoring and proactive management of toxicities.
Table 2: Comparative Safety Profiles of BTK Inhibitors
| Adverse Event | Ibrutinib | Acalabrutinib | Zanubrutinib |
|---|---|---|---|
| Any Grade Atrial Fibrillation | 9-13.3% [57] [58] | 5.8% [58] | Lower than ibrutinib [58] |
| Grade ≥3 Hypertension | 30.9% [57] | Lower than ibrutinib [58] | Not specified |
| Any Grade Diarrhea | 52% [60] | Lower than ibrutinib [58] | Not specified |
| Grade ≥3 Neutropenia | 53.9% [57] | Not specified | Not specified |
| Grade ≥3 Pneumonia | 26.3% [57] | Not specified | Not specified |
| Any Grade Bleeding | Higher than acalabrutinib [58] | Lower than ibrutinib [58] | Not specified |
| Treatment Discontinuation Due to AEs | 33% [60] | Not specified | Not specified |
Resistance Mechanisms and Next-Generation Approaches
Genetic Resistance to Covalent BTK Inhibitors
Despite the efficacy of covalent BTK inhibitors, resistance mechanisms eventually emerge in a significant proportion of patients, particularly in the relapsed/refractory setting. The most common on-target resistance mechanism involves acquired mutations in BTK, primarily at the Cys481 residue that is covalently bound by these inhibitors [56]. The BTK Cys481Ser mutation converts the covalent interaction to a reversible non-covalent interaction, allowing ATP to compete with the inhibitor due to its short plasma half-life, thereby re-establishing enzyme activity and downstream signaling [56].
Additional BTK mutations include kinase-impaired variants (e.g., Leu528Trp, Cys481Arg, Val416Leu) that disrupt normal BTK kinase function but induce scaffolding neofunction involving novel interactions with other intracellular signaling kinases to re-establish downstream signaling [56]. Gatekeeper mutations at the Thr474 codon (most commonly Thr474Ile) disrupt hydrogen networks critical for inhibitor binding and are observed more frequently in patients with disease resistant to acalabrutinib, typically in conjunction with Cys481Ser variants [56].
Beyond BTK mutations, resistance can also occur through mutations in PLCG2, the direct downstream target of BTK. Numerous missense variants (e.g., Arg665, Ser707, Leu845, Met1141) result in hypermorphic PLCG2 function through constitutive activation and hyper-sensitivity to upstream signaling [56]. These PLCG2 variants are rarely seen alone but rather more frequently observed in conjunction with BTK variants [56].
The diagram below illustrates the primary resistance mechanisms to BTK-directed therapies:
Figure 2: BTK Inhibitor Resistance Mechanisms. This diagram categorizes the primary genetic and non-genetic resistance mechanisms to BTK-directed therapies, including on-target BTK mutations, downstream PLCG2 mutations, alternative pathway activation, and tumor microenvironment-mediated protection.
Next-Generation BTK-Targeted Therapeutics
Several innovative approaches are being developed to overcome resistance to covalent BTK inhibitors. Third-generation non-covalent BTK inhibitors such as pirtobrutinib bind reversibly to BTK and retain activity against Cys481-mutated BTK [59]. However, some newly identified non-Cys481 resistance mutations show co-resistance to both covalent and non-covalent inhibitors, highlighting the need for continued therapeutic innovation [59].
Novel therapeutic modalities include BTK degraders such as BGB-16673, which utilize proteolysis-targeting chimera (PROTAC) technology to induce targeted degradation of BTK protein rather than merely inhibiting its kinase activity [61]. Early results from the Phase 1 CaDAnCe-101 study demonstrate promising efficacy and safety of BGB-16673 in patients with relapsed/refractory CLL/SLL and Waldenström macroglobulinemia [61]. Other emerging approaches include dual-binding inhibitors that engage multiple sites on BTK, and allosteric inhibitors that employ alternative mechanisms of action [59].
Combination strategies represent another important approach to enhance efficacy and prevent resistance development. The CAPTIVATE study investigated fixed-duration ibrutinib plus venetoclax in treatment-naïve CLL/SLL, demonstrating durable efficacy with 5.5-year PFS and OS rates of 66% and 97%, respectively [63]. These combinations leverage synergistic mechanisms of action by simultaneously targeting BCR signaling (via BTK inhibition) and apoptotic pathways (via BCL2 inhibition).
Experimental Methodologies in BTK Inhibitor Research
Key Assays and Technical Approaches
Research into BTK inhibitors employs a range of specialized methodologies to evaluate efficacy, resistance mechanisms, and therapeutic applications. Key experimental approaches include:
Genetic Sequencing for Resistance Mutations: Detection of BTK (Cys481, Thr474, Leu528, etc.) and PLCG2 (Arg665, Ser707, Leu845, etc.) mutations in patients progressing on BTK inhibitor therapy using next-generation sequencing approaches. This typically involves deep sequencing of circulating tumor DNA or cellular DNA from blood or tissue samples, with attention to cancer cell fraction (CCF) which can range from 10-80% depending on clinical context and specific BTKi [56].
Kinase Selectivity Profiling: Assessment of off-target kinase inhibition using kinase activity assays such as kinase binding assays, ATP competition assays, and cellular phosphorylation assays. Second-generation BTK inhibitors demonstrate improved selectivity profiles compared to ibrutinib, which explains their more favorable safety profiles [58] [59].
Minimal Residual Disease (MRD) Assessment: Highly sensitive flow cytometry (10^-4 sensitivity) or next-generation sequencing (10^-5-10^-6 sensitivity) to detect residual CLL cells following treatment. In the CAPTIVATE study, MRD status at the end of treatment was predictive of long-term PFS regardless of IGHV mutation status [63].
Patient-Derived Xenograft Models: Immunodeficient mouse models engrafted with primary CLL cells from patients, including those with BTK resistance mutations, to evaluate efficacy of novel BTK inhibitors and combination therapies [56].
Biochemical Binding Assays: Surface plasmon resonance and crystallography studies to characterize binding kinetics and structural interactions between BTK inhibitors and their target, providing insights into mechanisms of action and resistance [59].
Research Reagent Solutions
Table 3: Essential Research Reagents for BTK Inhibitor Studies
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| BTK Inhibitors | Ibrutinib, Acalabrutinib, Zanubrutinib, Pirtobrutinib | In vitro and in vivo efficacy studies; combination therapy screening; resistance mechanism investigations |
| BTK Degraders | BGB-16673 [61] | Novel mechanism of action studies; overcoming resistance models; protein homeostasis research |
| Antibodies for Phospho-BTK | Anti-pY223-BTK, Anti-pY551-BTK | Assessment of target engagement; downstream pathway modulation; pharmacodynamic studies |
| BCL2 Inhibitors | Venetoclax, Sonrotoclax [61] | Combination therapy studies; synergistic mechanism investigations; apoptosis pathway research |
| PLCG2 Mutant Plasmids | PLCG2 R665W, S707Y, L845F, M1141K | Functional characterization of resistance mutations; signaling pathway bypass studies |
| BTK Mutant Cell Lines | BTK C481S, T474I, L528W | Resistance mechanism studies; inhibitor screening; signaling adaptation investigations |
The development of BTK inhibitors has transformed the treatment paradigm for B-cell malignancies, particularly CLL/SLL, with multiple generations of agents offering progressively improved therapeutic profiles. Ibrutinib established the proof-of-concept for BTK inhibition with unprecedented efficacy in high-risk patients, while second-generation inhibitors zanubrutinib and acalabrutinib have demonstrated improved safety profiles and potentially enhanced efficacy in direct comparisons.
The evolving understanding of resistance mechanisms has driven development of innovative approaches including non-covalent inhibitors, BTK degraders, and rational combination strategies. Future directions will likely focus on molecularly-guided sequencing of therapies, MRD-driven treatment duration, and continued development of novel therapeutic modalities to address remaining challenges in BTK inhibitor therapy.
For researchers and drug development professionals, these advances highlight the importance of continued investigation into BTK biology, resistance mechanisms, and combination approaches to further improve outcomes for patients with B-cell malignancies.
The Phosphatidylinositol-3-kinase (PI3K)/AKT/mammalian target of rapamycin (MTOR) pathway represents one of the most frequently dysregulated signaling networks in human cancers, serving as a critical regulator of cellular growth, proliferation, survival, and metabolism [64] [65]. This pathway functions as a central hub that integrates signals from growth factors, nutrients, and cellular energy status to control anabolic processes and cell cycle progression. Under normal physiological conditions, the PI3K pathway is tightly regulated, but in cancer, its constitutive activation drives tumor development and progression through multiple mechanisms, including PIK3CA mutations, PTEN loss, and AKT amplifications [66] [65]. The high prevalence of PI3K pathway alterations across diverse cancer types, occurring in approximately 70% of breast cancers and 80% of endometrial cancers, has made it a compelling target for therapeutic intervention [66] [67].
The class I PI3K enzymes, particularly class IA, are most directly implicated in tumorigenesis and consist of heterodimeric proteins with a p110 catalytic subunit (p110α, p110β, p110δ) and a p85 regulatory subunit [64] [65]. These enzymes are activated by receptor tyrosine kinases (RTKs) and G-protein-coupled receptors, initiating a signaling cascade that converts phosphatidylinositol (3,4)-biphosphate (PIP2) to phosphatidylinositol (3,4,5)-triphosphate (PIP3) at the plasma membrane [64]. This lipid second messenger then recruits 3-phosphoinositide-dependent kinase 1 (PDK1) and AKT to the membrane, where AKT undergoes phosphorylation and activation. Once activated, AKT regulates numerous downstream substrates, including the mTOR complexes, which exist as two distinct multi-protein assemblies: mTORC1 and mTORC2 [64]. mTORC1 primarily controls protein synthesis, ribosome biogenesis, and metabolism, while mTORC2 regulates cytoskeletal organization and fully activates AKT through phosphorylation at Ser473 [64] [68].
The development of PI3K pathway inhibitors represents a cornerstone of targeted cancer therapy, with three principal pharmacological classes emerging: pan-class PI3K inhibitors, isoform-specific PI3K inhibitors, and dual PI3K/mTOR inhibitors [64] [65] [68]. Each class offers distinct therapeutic advantages and faces unique challenges regarding efficacy, toxicity, and resistance mechanisms. Understanding the comparative effectiveness of these inhibitor classes is essential for optimizing their clinical application and developing next-generation agents that can overcome current limitations in cancer treatment.
Classification and Mechanisms of PI3K Pathway Inhibitors
Pan-Class I PI3K Inhibitors
Pan-class I PI3K inhibitors represent the broadest-spectrum agents in this drug class, designed to target all four catalytic isoforms (p110α, p110β, p110δ, and p110γ) of class I PI3K enzymes [64] [65]. These inhibitors compete with ATP for binding to the kinase domain of p110 catalytic subunits, thereby blocking the conversion of PIP2 to PIP3 and subsequent downstream signaling [64]. The therapeutic rationale for pan-inhibition stems from the potential to completely abrogate PI3K signaling regardless of which isoform is driving pathway activation, while also preventing compensatory signaling through alternative isoforms [64] [68]. However, this comprehensive targeting approach also increases the risk of toxicity, as it affects both tumor cells and normal tissues that depend on specific PI3K isoforms for physiological functions [65].
Clinically approved and investigational pan-PI3K inhibitors include copanlisib, buparlisib, pictilisib, and sonolisib [64]. Copanlisib (BAY 80-6946) demonstrates preferential activity against PI3Kα and PI3Kδ isoforms and has shown efficacy in clinical trials involving patients with solid tumors harboring PIK3CA mutations [64]. Buparlisib (BKM120) has been extensively studied in breast cancer, where phase III trials demonstrated significantly prolonged progression-free survival when combined with fulvestrant in hormone receptor-positive, HER2-negative breast cancer patients, though treatment was associated with significant adverse effects including elevated liver enzymes, hyperglycemia, and hypertension [67]. Pictilisib (GDC-0941) has shown preclinical efficacy in impairing cell migration and tumor growth in medulloblastoma models and inducing apoptosis in PTEN-deficient ovarian cancer cells, though clinical trials in breast cancer revealed significant toxicity without corresponding progression-free survival benefits [64] [67].
Isoform-Specific PI3K Inhibitors
Isoform-specific PI3K inhibitors represent a more targeted approach designed to inhibit individual PI3K isoforms, thereby maximizing therapeutic efficacy against specific cancer types while minimizing off-target toxicities [64] [65]. The predominant isoforms targeted therapeutically include PI3Kα, PI3Kβ, PI3Kδ, and PI3Kγ, with each playing distinct roles in different cancer contexts [69]. PI3Kα inhibitors are particularly relevant for solid tumors, as PIK3CA (encoding p110α) is among the most frequently mutated oncogenes in cancers such as breast, endometrial, and colorectal cancer [66]. PI3Kδ and PI3Kγ inhibitors are more commonly employed in hematological malignancies due to their predominant expression in leukocytes and role in immune cell signaling [65].
Prominent isoform-specific inhibitors include alpelisib (PI3Kα-specific), taselisib (PI3Kα-specific), INK1117 (PI3Kα-specific), AZD8186 (PI3Kβ-specific), and GDC-0032 (PI3Kα-specific) [69] [67]. Alpelisib (BYL719) received FDA approval for use in combination with fulvestrant for HR-positive, HER2-negative breast cancer harboring PIK3CA mutations based on its ability to extend progression-free survival [67] [65]. Clinical trials demonstrated that alpelisib combined with fulvestrant showed relatively good activity with low toxicity compared to other agents in its class [67]. Taselisib, another α-specific inhibitor, showed positive antitumor effects when combined with fulvestrant in clinical trials, highlighting the importance of combination targeted therapies [67]. The development of mutant-specific PI3Kα inhibitors such as RLY-2608 and STX-478 represents a further refinement of this approach, designed to spare wild-type PI3Kα and potentially reduce treatment-induced hyperglycemia, though they still face limitations related to pathway feedback reactivation and resistance via mutations in PTEN/AKT [66].
Dual PI3K/mTOR Inhibitors
Dual PI3K/mTOR inhibitors constitute a strategically distinct class that simultaneously targets both PI3K catalytic activity and mTOR kinase function within a single molecule [68]. These agents are designed to address a key limitation of single-node inhibition: pathway reactivation through feedback mechanisms and parallel signaling nodes [66] [68]. By concurrently blocking upstream PI3K signaling and downstream mTOR effectors, these inhibitors achieve more comprehensive pathway suppression and theoretically reduce the likelihood of resistance development [68]. The structural basis for this dual targeting capability lies in the high degree of similarity between the kinase domains of PI3K and mTOR, allowing certain small molecules to effectively interact with both enzymes [68].
Notable dual inhibitors include gedatolisib, LY3023414, dactolisib, PI-103, GSK1059615, and voxtalisib [64] [67] [68]. Gedatolisib has shown promising efficacy signals in clinical trials and is currently under investigation in multiple cancer types [66] [67]. LY3023414 demonstrated potent inhibition of cell proliferation in PIK3CA-mutant colorectal cancer cells and reduced the growth of PIK3CA-mutant colon tumors in vivo [64]. PI-103, an early-generation dual inhibitor, exhibited potent activity against class IA PI3K enzymes and mTOR but suffered from unfavorable pharmacokinetics that limited its clinical development [68]. GSK1059615 is a pyridinylquinoline derivative that functions as both a pan-PI3K reversible inhibitor and a pan-mTOR inhibitor with subnanomolar IC50 values for PI3Kα and PI3Kβ, demonstrating potent activity against gastric cancer cells in preclinical models by blocking the entire PI3K-Akt-mTOR cascade and inducing apoptosis [68].
Table 1: Comparative Characteristics of Major PI3K Pathway Inhibitor Classes
| Parameter | Pan-PI3K Inhibitors | Isoform-Specific Inhibitors | Dual PI3K/mTOR Inhibitors |
|---|---|---|---|
| Molecular Targets | All class I PI3K isoforms (α, β, δ, γ) | Specific PI3K isoforms (typically α, δ, or β) | PI3K isoforms + mTORC1/mTORC2 |
| Key Examples | Copanlisib, Buparlisib, Pictilisib | Alpelisib, Taselisib, INK1117, AZD8186 | Gedatolisib, LY3023414, GSK1059615 |
| Mechanism | ATP-competitive inhibition of p110 catalytic subunits | Selective ATP-competitive inhibition of specific p110 isoforms | Concurrent ATP-competitive inhibition of PI3K and mTOR kinase domains |
| Primary Applications | Solid tumors, hematologic malignancies | Solid tumors (PI3Kα inhibitors), hematologic cancers (PI3Kδ inhibitors) | Advanced solid tumors, treatment-resistant cancers |
| Advantages | Broad pathway suppression, prevents isoform compensation | Reduced toxicity, better therapeutic index | Comprehensive pathway blockade, reduced feedback activation |
| Limitations | Higher toxicity, narrower therapeutic window | Potential for resistance via alternative isoforms | Overlapping toxicities, complex pharmacokinetics |
| Resistance Mechanisms | PTEN loss, AKT mutations, RTK upregulation | Bypass signaling, additional pathway mutations | PIM kinase activation, metabolic adaptations |
Comparative Effectiveness Analysis
Preclinical and Clinical Efficacy Data
Direct comparisons between inhibitor classes reveal distinct efficacy profiles and limitations for each approach. Single-node inhibitors (SNIs), including isoform-specific PI3K inhibitors and selective mTORC1 inhibitors, typically demonstrate modest therapeutic benefits as monotherapies due to several compensatory mechanisms that maintain pathway activity [66]. These limitations include pathway feedback reactivation, the presence of co-occurring pathway mutations beyond the targeted node, and systemic perturbations in glucose homeostasis that lead to hyperinsulinemia and pathway reactivation [66]. For instance, treatment with approved SNIs like alpelisib (PI3Kα-specific), everolimus (mTORC1 inhibitor), and capivasertib (AKT inhibitor) effectively decreases S6 phosphorylation but shows limited ability to prevent 4E-BP1 phosphorylation, allowing pro-growth signaling to persist [66].
In contrast, multi-node inhibition strategies, particularly those combining PI3K and mTOR targeting, demonstrate superior pathway suppression. Research in endometrial and breast cancer models shows that the combination of serabelisib (PI3Kα inhibitor) and sapanisertib (mTORC1/mTORC2 inhibitor) more effectively suppresses PI3K/AKT/mTOR pathway signaling than single-node inhibitors, with dramatically improved inhibition of both S6 and 4E-BP1 phosphorylation [66]. This combination approach remained highly effective even in cell lines with 2-3 PI3K/AKT/mTOR pathway mutations, including those with PTEN loss [66]. In xenograft models, the triplet combination of sapanisertib, serabelisib, and paclitaxel combined with an insulin-suppressing diet achieved complete inhibition of tumor growth and even tumor regression [66]. Clinical data support these findings, with a Phase 1b trial reporting an objective response rate of nearly 50% in patients with advanced, treatment-refractory breast, endometrial, and ovarian cancers receiving the sapanisertib/serabelisib/paclitaxel combination [66].
Table 2: Experimental Efficacy Data for Selected PI3K Pathway Inhibitors
| Inhibitor | Class | Molecular Targets | IC50 Values | Cancer Models | Key Outcomes |
|---|---|---|---|---|---|
| Copanlisib | Pan-PI3K | PI3Kα, PI3Kδ | N/A | Colorectal cancer, lymphomas | Increased apoptosis, decreased cell growth, reduced p-AKT [64] |
| Alpelisib | Isoform-specific | PI3Kα | N/A | HR+ HER2- breast cancer | Improved PFS with fulvestrant, manageable toxicity [67] |
| Taselisib | Isoform-specific | PI3Kα | N/A | Breast cancer, lymphomas | Positive antitumor effects with fulvestrant [67] |
| GSK1059615 | Dual PI3K/mTOR | PI3Kα, PI3Kβ, PI3Kγ, PI3Kδ, mTOR | 0.4, 0.6, 5, 2, 12 nM | Gastric cancer | Blocked PI3K-Akt-mTOR cascade, induced apoptosis [68] |
| PI-103 | Dual PI3K/mTOR | PI3Kα, PI3Kγ, mTOR | 8.4, 86, 5.7 nM | Oral squamous cell carcinoma | Radiosensitization in PTEN-mutated cells [68] |
| LY3023414 | Dual PI3K/mTOR | PI3K, mTOR | N/A | Colorectal cancer | Decreased cell proliferation, reduced tumor growth in vivo [64] |
Resistance Mechanisms and Toxicity Profiles
Each inhibitor class faces distinct resistance challenges that limit their long-term efficacy. For pan-PI3K inhibitors, resistance frequently emerges through PTEN loss, AKT mutations, and receptor tyrosine kinase upregulation that reactivates downstream signaling despite PI3K blockade [65]. Isoform-specific inhibitors face additional challenges from bypass signaling through non-targeted isoforms and the development of additional pathway mutations that maintain pathway activity [66] [65]. For instance, treatment with PI3Kα inhibitors like alpelisib or inavolisib can lead to loss of PTEN and subsequent AKT activation in breast cancer patients, as well as further mutations in PI3Kα itself at progression [66]. Dual PI3K/mTOR inhibitors, while overcoming some resistance mechanisms, still face challenges from PIM kinase activation and metabolic adaptations that sustain cell survival despite comprehensive pathway inhibition [66].
Toxicity profiles also vary significantly between classes. Pan-PI3K inhibitors are associated with hyperglycemia, liver dysfunction, lymphocytopenia, and hypertension due to their broad effects on PI3K signaling across multiple tissues [64] [67]. Isoform-specific inhibitors generally exhibit more favorable toxicity profiles, though PI3Kα inhibitors still cause hyperglycemia and gastrointestinal toxicities, while PI3Kδ inhibitors can cause hepatotoxicity and inflammatory conditions [66] [67]. Dual PI3K/mTOR inhibitors typically produce overlapping toxicities from both target classes, including metabolic disturbances, stomatitis, rash, and fatigue [68]. A common challenge for many PI3K pathway inhibitors is treatment-induced hyperglycemia and hyperinsulinemia, which occur as "on-target, off-tumor" effects where blockade of PI3K/AKT/GLUT4 signaling prevents glucose uptake by peripheral tissues [66]. This resulting elevation of systemic insulin directly promotes treatment resistance, though recent strategies using insulin-suppressing diets have shown promise in mitigating this effect and improving antitumor efficacy in preclinical models [66].
Experimental Methodologies for Inhibitor Evaluation
Standardized Protocols for Pathway Inhibition Assessment
Rigorous evaluation of PI3K pathway inhibitors requires standardized methodologies that quantitatively assess both pathway suppression and functional consequences across multiple dimensions. For in vitro studies, recommended protocols include treating cancer cell lines harboring relevant PI3K pathway mutations with clinically relevant drug concentrations that reflect free-drug exposures in patients (representing Caverage, Cmaximum, and intermediate concentrations) [66]. Western blot analysis should evaluate phosphorylation status of key pathway markers including p-AKT (Ser473), p-S6, and p-4E-BP1 at specified timepoints (typically 2-24 hours post-treatment) to assess pathway inhibition dynamics [66]. Functional assays should include CCK-8 proliferation assays conducted over 72-96 hours, apoptosis measurement via Annexin V/PI staining and flow cytometry at 24-48 hours, and cell cycle analysis using PI staining to determine G1/S phase distribution changes [70] [68].
For in vivo evaluation, xenograft models using patient-derived xenografts (PDXs) or genetically engineered mouse models (GEMMs) with documented PI3K pathway alterations provide the most clinically relevant systems [66]. Animals should be randomized to treatment groups when tumors reach 150-200mm³, with inhibitors administered at doses achieving plasma concentrations equivalent to human therapeutic exposures [66]. Tumor measurements should be recorded 2-3 times weekly, and studies should incorporate an insulin-suppressing diet when evaluating PI3K/AKT-targeting agents to mitigate compensatory hyperinsulinemia that confounds treatment efficacy [66]. Endpoint analyses should include immunohistochemical assessment of pathway markers (p-AKT, p-S6, Ki67) and comparison of tumor growth rates between treatment groups, with tumor regression defined as >50% reduction from baseline volume [66].
Meta-analytical approaches synthesizing data from multiple inhibitor studies have identified p-AKT and p-mTOR as the most reliable pharmacodynamic markers for assessing PI3K pathway inhibition, as these consistently reflect functional changes across diverse experimental systems [70]. These molecular endpoints show strong correlation with downstream functional effects including reduced proliferation (standardized mean difference -5.1 SD), decreased IL-6 secretion (-11.1 SD), and increased apoptosis (+2.7 SD) based on pooled analysis of in vitro data [70].
Assessment of Combination Therapies
Given the limitations of monotherapy approaches, standardized protocols for evaluating rational combination strategies are essential. For PI3K pathway inhibitors, promising combination partners include CDK4/6 inhibitors (palbociclib), hormone therapies (fulvestrant, elacestrant), chemotherapies (paclitaxel, carboplatin), and MEK inhibitors [66] [67]. Experimental designs should include appropriate synergy assessment using combination index calculations based on the Chou-Talalay method, with simultaneous and sequential dosing schedules to identify optimal administration sequences [66] [71].
In ovarian cancer models, combination approaches targeting both MAPK and PI3K/mTOR pathways have demonstrated particular promise, with the experimental drug rigosertib (MAPK inhibitor) combined with PI3K/mTOR inhibitors showing enhanced efficacy compared to single-agent treatment [71]. This dual pathway blockade strategy effectively overcomes resistance mechanisms that typically emerge with single-pathway inhibition [71]. Similar approaches have shown success in breast and endometrial cancer models, where the combination of serabelisib and sapanisertib effectively combined with multiple therapeutic classes including palbociclib, fulvestrant, elacestrant, selinexor, carboplatin, and paclitaxel [66].
Table 3: Essential Research Reagents for PI3K Pathway Inhibitor Studies
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Cell Line Models | MCF-7 (breast), T47D (breast), HEC-1A (endometrial), OVCAR-3 (ovarian), AGS (gastric) | In vitro efficacy screening, mechanism studies | Representative models with defined PI3K pathway alterations (PIK3CA mutations, PTEN loss) |
| Primary Cells | RA-FLS (rheumatoid arthritis), HFLS-RA, MH7A | Pathway biology, inhibitor effects in non-cancer systems | Study PI3K pathway in inflammatory disease contexts [70] |
| Phospho-Specific Antibodies | p-AKT (Ser473), p-S6 (Ser235/236), p-4E-BP1 (Thr37/46) | Western blot, IHC, flow cytometry | Assessment of pathway inhibition status, pharmacodynamic marker evaluation |
| Viability/Proliferation Assays | CCK-8, MTT, CellTiter-Glo | High-throughput screening, dose-response studies | Quantification of cell proliferation and metabolic activity |
| Apoptosis Detection Kits | Annexin V/PI staining, caspase-3/7 activity assays | Mechanism of action studies | Differentiation between cytostatic and cytotoxic effects |
| Animal Models | PDX models with PIK3CA mutations, PTEN-null GEMMs | In vivo efficacy, toxicity studies | Preclinical assessment of therapeutic efficacy in physiologically relevant systems |
Future Directions and Clinical Translation
The development of PI3K pathway inhibitors continues to evolve with several promising strategies emerging to address current limitations. Next-generation mutant-specific PI3Kα inhibitors such as RLY-2608 and STX-478 represent a significant advance in targeting precision, designed to selectively inhibit mutant PI3Kα while sparing the wild-type enzyme to reduce treatment-related hyperglycemia [66]. However, these agents still face challenges from pathway feedback reactivation and resistance via mutations in PTEN/AKT, highlighting the continued need for rational combination approaches [66]. PROTAC (Proteolysis Targeting Chimera) technology is being applied to develop degrader molecules that target PI3K pathway components for ubiquitination and proteasomal degradation, potentially offering advantages over traditional catalytic inhibitors through more complete target elimination and potentially reduced resistance [65].
The clinical pipeline continues to expand with numerous agents in advanced development. The PI3K inhibitors market has grown rapidly, reaching $1.38 billion in 2024 and projected to grow to $2.55 billion by 2029 at a compound annual growth rate of 13.2%, reflecting continued investment and innovation in this therapeutic area [72]. Major trends driving this growth include shifting focus toward dual and pan-isoform PI3K inhibitors, developing improved safety profiles, increasing use of combination therapies, and expanding applications beyond oncology into autoimmune diseases and neurological disorders [72]. Clinical trials are increasingly exploring PI3K inhibitors in combination with immunotherapies, particularly in triple-negative breast cancer where agents like eganelisib are being evaluated for their immunomodulatory and anticancer effects [67].
The accumulating clinical experience with PI3K pathway inhibitors underscores the importance of patient selection biomarkers and pharmacodynamic monitoring to optimize therapeutic outcomes. PIK3CA mutation status remains the primary biomarker for PI3Kα inhibitor use in breast cancer, while PTEN loss may predict sensitivity to broader pathway inhibition [66] [67]. Monitoring p-AKT and p-S6 in paired tumor biopsies or in platelet-rich plasma represents a promising approach for confirming target engagement and guiding dose optimization [70]. As the field advances, the integration of comprehensive pathway assessment with rational combination strategies will be essential to fully realize the therapeutic potential of PI3K pathway inhibition in cancer treatment.
The Janus kinase/Signal Transducer and Activator of Transcription (JAK-STAT) signaling pathway serves as a crucial communication node in cellular function, transducing signals from more than 50 cytokines and growth factors [5]. This evolutionarily conserved pathway regulates vital processes including hematopoiesis, immune fitness, inflammation, and apoptosis [73] [5]. Dysregulation of JAK-STAT signaling is implicated in various autoimmune diseases, hematological disorders, and cancers, making it an attractive therapeutic target for drug development [73] [74]. The discovery of JAK inhibitors represents a significant advancement in targeted therapy, offering oral treatment options for numerous immune-mediated inflammatory diseases (IMIDs) and myeloproliferative neoplasms [6] [75]. This review comprehensively examines the mechanistic foundations, comparative effectiveness, and clinical applications of JAK-STAT inhibitors, providing researchers and drug development professionals with critical insights for future therapeutic innovation.
The JAK-STAT Signaling Pathway: Molecular Mechanisms
Pathway Components and Activation Dynamics
The JAK-STAT pathway comprises three main components: tyrosine kinase-associated receptors, Janus kinases (JAKs), and Signal Transducers and Activators of Transcription (STATs) [73]. Four JAK family members (JAK1, JAK2, JAK3, and TYK2) and seven STAT family members (STAT1, STAT2, STAT3, STAT4, STAT5a, STAT5b, and STAT6) form the core signaling machinery [73] [5]. JAKs are non-receptor tyrosine kinases characterized by seven homologous JAK homology (JH) domains, with the C-terminal JH1 domain representing the catalytically active kinase domain and JH2 functioning as a critical regulatory pseudokinase domain [73] [6]. The FERM domain (formed by JH4-JH7) mediates receptor binding, while the SH2 domain facilitates STAT recruitment [73].
STAT proteins contain several functional domains arranged from N- to C-terminus: a unique N-terminal domain facilitating protein-protein interactions, a coiled-coil domain involved in nuclear import/export, a DNA-binding domain, a linker domain, an SH2 domain critical for dimerization, and a transcription activation domain [73]. Pathway activation initiates when extracellular cytokines or growth factors bind to their cognate receptors, inducing receptor dimerization and consequent trans-phosphorylation of associated JAKs [5]. The activated JAKs then phosphorylate tyrosine residues on cytokine receptors, creating docking sites for STAT proteins via their SH2 domains [73]. Following recruitment, JAKs phosphorylate STATs on conserved tyrosine residues, prompting STAT dimerization and subsequent nuclear translocation [73] [5]. Within the nucleus, STAT dimers bind specific promoter sequences to regulate transcription of target genes involved in inflammation, immunity, and cellular proliferation [73].
Visualizing the JAK-STAT Signaling Cascade
Figure 1: The JAK-STAT Signaling Pathway Activation Cascade. This diagram illustrates the sequential process from cytokine-receptor binding to gene transcription regulation.
JAK Inhibitor Classification and Mechanisms of Action
Structural and Functional Diversity of JAK Inhibitors
JAK inhibitors are categorized based on selectivity and binding mode. First-generation inhibitors (e.g., tofacitinib, baricitinib) act as broad-spectrum, non-selective JAK inhibitors, while second-generation agents (e.g., filgotinib, upadacitinib) demonstrate enhanced selectivity for specific JAK family members [6] [76]. From a mechanistic perspective, JAK inhibitors are classified as reversible (competitive) or irreversible (covalent) based on their binding interactions with JAK enzymes [6].
Reversible inhibitors constitute the majority of clinically approved JAK inhibitors and are further subdivided into:
Type I inhibitors: These compounds bind to the active conformation of the JAK kinase domain, competing with ATP for the catalytic binding site [6]. Their ability to target multiple kinases stems from the highly conserved structure of the ATP-binding pocket across JAK family members [6]. Examples include filgotinib (JAK1-selective), fedratinib (JAK2-selective), and tofacitinib (multi-JAK inhibitor) [6].
Type II inhibitors: These agents target the inactive conformation of the kinase domain, also binding to the ATP-binding site but stabilizing different conformational states [6]. Representative examples include NVP-BBT594 and NVP-CHZ868, which primarily inhibit JAK2 [6].
Allosteric inhibitors: This class binds to sites distinct from the ATP-binding pocket, enabling unique inhibition mechanisms [6]. Deucravacitinib (BMS-986165), a selective TYK2 inhibitor, exemplifies this approach by employing allosteric inhibition [6].
Irreversible JAK inhibitors represent a novel therapeutic strategy characterized by covalent binding to the unique Cys909 residue in JAK3 [6]. These compounds incorporate covalent-bond forming groups (e.g., acrylamide, α-cyanoacrylamide) that permanently modify the target cysteine, conferring exceptional selectivity for JAK3 over other JAK family members [6]. Ritlecitinib represents the most advanced clinical candidate in this category, currently undergoing evaluation in human trials [6].
Research Reagent Solutions for JAK-STAT Investigations
Table 1: Essential Research Tools for JAK-STAT Pathway Investigation
| Research Tool | Specific Examples | Research Application | Key Characteristics |
|---|---|---|---|
| JAK-Selective Inhibitors | Filgotinib (JAK1), Fedratinib (JAK2), Ritlecitinib (JAK3 covalent), Deucravacitinib (TYK2 allosteric) | Target validation, mechanism studies, dose-response relationships | Varying selectivity profiles; reversible/irreversible mechanisms; different conformational binding preferences |
| Cytokine Stimulation Agents | Interferons (IFN-α, IFN-γ), Interleukins (IL-4, IL-6, IL-13), Colony-stimulating factors (GM-CSF) | Pathway activation, signaling studies, inhibitor validation | Activate specific receptor complexes; recruit different JAK/STAT combinations; physiological relevance |
| Biomarker Assays | Phospho-STAT antibodies, TARC/CCL17 ELISA, Eosinophil count, Total IgE quantification | Treatment response monitoring, pathway activity assessment, patient stratification | Correlate with disease activity; reflect specific cytokine pathway engagement; predictive value |
| Cell-Based Reporter Systems | STAT-responsive luciferase constructs, JAK-overexpressing cell lines, Primary immune cells | High-throughput screening, mechanism of action studies, signaling dynamics | Enable real-time monitoring; permit genetic manipulation; provide physiological context |
Comparative Efficacy Across Disease States
Autoimmune and Inflammatory Disorders
JAK inhibitors have demonstrated significant clinical efficacy across multiple immune-mediated inflammatory diseases (IMIDs), with varying performance characteristics based on their selectivity profiles and target diseases [75] [76]. In rheumatoid arthritis (RA), multiple JAK inhibitors (tofacitinib, baricitinib, upadacitinib, filgotinib) have shown superiority over placebo and, in some studies, over methotrexate and TNF-α inhibitors in phase 3 clinical trials [75]. The efficacy extends to psoriatic arthritis, axial spondyloarthritis, and inflammatory bowel disease, where JAK inhibition improves both articular and extra-articular disease manifestations [75].
Recent investigations in giant cell arteritis (GCA) highlight the therapeutic potential of JAK inhibition. A phase 3 trial demonstrated that 15 mg upadacitinib daily with a 26-week glucocorticoid taper resulted in 46% of patients achieving sustained remission at week 52 compared to 29% in the placebo arm with a 52-week taper [75]. This finding led to FDA approval of upadacitinib for GCA treatment in adults [75].
In atopic dermatitis (AD), JAK1 inhibitors (abrocitinib, upadacitinib) demonstrate distinct efficacy profiles compared to biologic agents. A retrospective real-world study comparing JAK1 inhibitors with anti-IL-13 antibodies (lebrikizumab, tralokinumab) found that while both approaches achieved similar EASI 75 (75% improvement in Eczema Area and Severity Index) responses, JAK1 inhibitors provided significantly superior antipruritic effects, with higher odds of achieving PP-NRS 4 (≥4-point improvement in Peak Pruritus Numerical Rating Scale; OR=9.36, p=0.0063) and PP-NRS 0/1 (complete itch resolution; OR=34.61, p<0.0001) [77]. This enhanced antipruritic activity likely stems from inhibition of IL-31 signaling, a key pruritogenic cytokine [77].
Oncological Applications
The JAK-STAT pathway plays dual roles in oncology, contributing to both inflammatory-driven tumorigenesis and hematological malignancies [73] [6]. Constitutive JAK-STAT activation occurs in various human malignancies, promoting tumor cell survival, proliferation, and immune evasion [73]. Oncogenic JAK and STAT mutations are prevalent in solid tumors, leukemia, and lymphoma [73].
JAK2 inhibition represents a cornerstone therapy for myeloproliferative neoplasms, particularly those driven by the JAK2V617F mutation [6]. Ruxolitinib, a JAK1/JAK2 inhibitor, has received approval for myelofibrosis and polycythemia vera [6]. Fedratinib and pacritinib provide additional JAK2-targeting options with distinct safety profiles [6]. Beyond direct antitumor effects, JAK inhibitors are being investigated for combination with immunotherapy, where they may modulate the tumor microenvironment and overcome resistance to immune checkpoint inhibitors [75].
Table 2: Comparative Efficacy of JAK Inhibitors Across Autoimmune Diseases
| JAK Inhibitor | Primary Selectivity | Key Approved Indications | Efficacy Highlights | Biomarkers of Response |
|---|---|---|---|---|
| Tofacitinib | Pan-JAK | RA, PsA, UC | Superior to placebo & methotrexate in RA; higher MACE risk in high-risk RA patients vs TNFi [78] [75] | N/A |
| Baricitinib | JAK1/JAK2 | RA, AD | Rapid & significant efficacy in RA & AD; superior to TNFi in some RA populations [75] | N/A |
| Upadacitinib | JAK1 | RA, PsA, AS, AD, UC, GCA | 46% sustained remission in GCA vs 29% placebo; superior to adalimumab in PsA [75] | N/A |
| Filgotinib | JAK1 | RA, UC | Effective in RA & UC with favorable safety profile; lower VTE risk than some other JAKi [78] [75] | N/A |
| Abrocitinib | JAK1 | AD | Superior antipruritic effect vs anti-IL-13; rapid itch improvement [77] | Eosinophil count reduction (R=0.525, p=0.0009) [77] |
| Anti-IL-13 Agents | IL-13 (Biologic) | AD | Effective skin improvement; slower pruritus relief vs JAK1i [77] | TARC reduction (R=0.677, p<0.0001) [77] |
Abbreviations: RA (rheumatoid arthritis), PsA (psoriatic arthritis), UC (ulcerative colitis), AD (atopic dermatitis), AS (ankylosing spondylitis), GCA (giant cell arteritis), TNFi (TNF inhibitor), MACE (major adverse cardiovascular events), VTE (venous thromboembolism), TARC (thymus and activation-regulated chemokine)
Safety Profile Comparisons
Cardiovascular and Malignancy Risk Assessments
Safety considerations for JAK inhibitors were significantly influenced by the ORAL Surveillance trial, which compared tofacitinib with TNF antagonists in rheumatoid arthritis patients aged ≥50 years with ≥1 cardiovascular risk factor [78] [75]. This study demonstrated increased risks of major adverse cardiovascular events (3.4% vs 2.5%; HR=1.33), venous thromboembolism, cancer, and mortality with tofacitinib [78] [75]. These findings prompted regulatory restrictions requiring JAK inhibitor use only after TNF antagonist failure across all indications [78].
However, recent comprehensive meta-analyses incorporating 42 head-to-head comparative effectiveness studies (n=813,881 patients) challenge the broad generalization of these safety concerns [78]. This analysis revealed no meaningful differences in serious infections (IR 3.79 vs 3.03 per 100 person-years; pooled HR 1.05, 95% CI 0.97-1.13), malignant neoplasms (IR 1.00 vs 0.94 per 100 person-years; pooled HR 1.02, 95% CI 0.90-1.16), or major adverse cardiovascular events (IR 0.72 vs 0.66 per 100 person-years; pooled HR 0.91, 95% CI 0.80-1.04) between JAK inhibitors and TNF antagonists [78]. JAK inhibitor use was associated with a modestly elevated venous thromboembolism risk (IR 0.57 vs 0.52 per 100 person-years; pooled HR 1.26, 95% CI 1.03-1.54) [78].
Real-world evidence from the "JAK-pot" study, analyzing data from 13 registries encompassing 53,169 treatment initiations, found no significantly higher overall cancer risk in RA patients treated with JAK inhibitors versus biologic DMARDs [79]. Crude incidence rates for non-NMSC cancer were 2.2, 2.9, and 3.1 per 1000 patient-years for TNF inhibitors, JAK inhibitors, and bDMARDs with other mechanisms of action, respectively, with no statistically significant differences after adjustment [79]. However, a German RABBIT register analysis identified a small but significant overall increase in malignancy risk for JAK inhibitors versus bDMARDs (HR 1.40, 95% CI 1.09-1.80), particularly in treatment episodes exceeding 16 months and in specific patient subgroups (age ≥60 years, ≥3 prior csDMARDs, high disease activity) [80].
Dermatological and Infection Risks
Keratinocyte cancer risk represents a particularly relevant concern with JAK inhibitor therapy. Swedish registry data (n=21,121) demonstrated significantly higher rates of first keratinocyte cancer with JAK inhibitors versus TNF inhibitors (HR 1.72), primarily driven by basal cell carcinoma [79]. Among patients with prior keratinocyte cancer history, JAK inhibitors substantially increased the risk of second cancer diagnosis compared to TNF inhibitors (HR 2.76) [79]. These findings underscore the importance of regular dermatological surveillance in JAK inhibitor-treated patients.
Infection risks necessitate careful patient management, with herpes zoster reactivation representing a class-effect concern [75]. Clinical decision-making should incorporate pre-treatment vaccination strategies and consider specific patient factors including age, tuberculosis risk, and concomitant immunosuppressive therapies [75].
Table 3: Comparative Safety Profiles of JAK Inhibitors Versus TNF Antagonists
| Safety Outcome | JAK Inhibitor Incidence Rate (per 100 person-years) | TNF Antagonist Incidence Rate (per 100 person-years) | Pooled Hazard Ratio [95% CI] | Heterogeneity (I²) |
|---|---|---|---|---|
| Serious Infections | 3.79 [2.85-5.05] | 3.03 [2.32-3.95] | 1.05 [0.97-1.13] | Minimal to moderate |
| Malignant Neoplasms | 1.00 [0.77-1.31] | 0.94 [0.72-1.22] | 1.02 [0.90-1.16] | Minimal to moderate |
| Major Adverse Cardiovascular Events | 0.72 [0.56-0.92] | 0.66 [0.49-0.89] | 0.91 [0.80-1.04] | Minimal to moderate |
| Venous Thromboembolism | 0.57 [0.40-0.82] | 0.52 [0.37-0.73] | 1.26 [1.03-1.54] | Minimal to moderate |
Data derived from meta-analysis of 42 head-to-head comparative effectiveness studies (n=813,881 patients) [78]
Experimental Protocols and Methodologies
Comparative Effectiveness Study Design
Robust evaluation of JAK inhibitor efficacy and safety requires well-designed comparative studies. The recent comprehensive meta-analysis employed systematic literature search of Ovid Medline, Ovid EMBASE, and Web of Science databases from inception to June 25, 2025, identifying head-to-head comparative effectiveness studies in adults with immune-mediated inflammatory diseases (rheumatoid arthritis, inflammatory bowel disease, psoriasis/psoriatic arthritis, or spondyloarthropathy) treated with either JAK inhibitors or TNF antagonists [78]. The protocol excluded randomized clinical trials (to focus on real-world evidence), noncomparative observational studies, studies not reporting outcomes of interest, and studies with sample sizes <500 [78].
Statistical analyses incorporated random-effects meta-analysis models to obtain incidence rates and hazard ratios for safety outcomes, adjusting for key confounding variables [78]. Heterogeneity was quantified using I² statistics, with prespecified subgroup analyses by study location, IMID type, JAK inhibitor type, age group, and outcome subtype [78]. Meta-regression examined study-level factors including age, sex distribution, study recruitment midpoint, concomitant immunosuppressive use, and major comorbidities [78].
Biomarker Correlation Methodology
Retrospective cohort analyses in atopic dermatitis have elucidated biomarker relationships with treatment response [77]. Standardized assessment includes Eczema Area and Severity Index (EASI) and Peak Pruritus Numerical Rating Scale (PP-NRS) measurements at baseline and 3-month intervals [77]. Parallel biomarker evaluation encompasses peripheral blood eosinophil counts, serum TARC (thymus and activation-regulated chemokine) levels, and total immunoglobulin E quantification [77].
Statistical approaches employ multivariate logistic regression adjusted for confounding variables (treatment group, age, sex, bio-naïve status, history of systemic therapy, baseline scores) to identify factors associated with clinical outcomes [77]. Linear regression analyses determine correlations between EASI or PP-NRS improvement rates and biomarker improvement rates, with correlation coefficients (R) and corresponding p-values quantifying relationship strength [77]. In JAK1 inhibitor-treated patients, eosinophil count reduction strongly correlates with EASI improvement (univariate: R=0.525, p=0.0009; adjusted: β=0.567, p=0.0004), while anti-IL-13 antibody response associates with TARC reduction (univariate: R=0.677, p<0.0001; adjusted: β=0.661, p<0.0001) [77].
JAK-STAT pathway inhibitors represent a transformative therapeutic class with demonstrated efficacy across diverse autoimmune disorders and hematological malignancies. The evolving understanding of their safety profiles, particularly from recent large-scale comparative effectiveness research, enables more nuanced risk-benefit assessments in specific patient populations. Future research directions should prioritize long-term safety monitoring, particularly for cardiovascular and malignancy outcomes, and further elucidate the clinical implications of selectivity differences between JAK inhibitors. Biomarker-driven treatment selection promises enhanced precision medicine approaches, while novel therapeutic strategies including allosteric inhibition and covalent JAK3 targeting may expand the therapeutic arsenal. Combination therapies with emerging drug classes, such as the potential cardiovascular protection offered by GLP-1 receptor agonists in JAK inhibitor-treated patients, represent promising avenues for optimizing patient outcomes [79]. As the JAK inhibitor landscape continues to evolve, these targeted therapies will undoubtedly maintain their crucial role in the management of immune-mediated inflammatory diseases and hematological malignancies.
The complexity of cancer biology, characterized by tumor heterogeneity and dynamic adaptability, presents a fundamental challenge to monotherapeutic approaches. Single-agent therapies often achieve initial success but ultimately falter against the relentless capacity of cancer cells to develop evasion mechanisms. Combination therapies represent a strategic paradigm shift in oncology, designed to enhance therapeutic efficacy while simultaneously counteracting resistance. The rationale for this approach is rooted in the ability to target multiple pathological pathways simultaneously, creating a synergistic therapeutic effect that surpasses the sum of individual drug actions. This multifaceted strategy not only improves tumor cell killing but also addresses the diverse mechanisms of resistance that inevitably emerge during treatment [81] [82].
The transition from monotherapy to combination regimens represents a fundamental advancement in cancer treatment philosophy. By leveraging complementary mechanisms of action, these approaches can produce synergistic effects where the combined efficacy exceeds the additive effects of each agent alone. Furthermore, combination therapies can potentially allow for dose reduction of individual components, thereby mitigating dose-limiting toxicities while maintaining or even enhancing therapeutic outcomes. This is particularly valuable in oncology, where the therapeutic window is often narrow and quality of life considerations are paramount [81]. The strategic integration of different drug classes—including targeted therapies, immunotherapies, chemotherapies, and emerging modalities—creates a comprehensive assault on cancer cells that is more difficult to evade through singular resistance mechanisms.
Molecular Mechanisms of Therapeutic Resistance
Signaling Pathway Adaptations in Targeted Therapy Resistance
Resistance to molecularly targeted agents frequently arises through compensatory signaling activation and genetic evolution of tumor cells. In Chronic Myeloid Leukemia (CML), for instance, tyrosine kinase inhibitors (TKIs) targeting BCR::ABL1 oncogenic activity have revolutionized treatment, yet resistance remains a significant clinical challenge. The molecular underpinnings of TKI resistance involve both BCR::ABL1-dependent and independent mechanisms, including mutations within the kinase domain that impair drug binding and activation of alternative survival pathways that bypass BCR::ABL1 inhibition [83] [84].
Key signaling pathways implicated in TKI resistance include PI3K/AKT, MAPK, JAK/STAT, and SRC/AKT pathways. These pathways form interconnected networks that promote cell survival, proliferation, and metabolic adaptation despite continued therapeutic pressure. The PI3K/AKT pathway, in particular, serves as a critical hub for multiple resistance mechanisms, transmitting anti-apoptotic signals and enhancing protein synthesis that supports tumor cell persistence. Similarly, MAPK pathway reactivation provides sustained proliferative signals independent of the primary drug target, while JAK/STAT activation creates inflammatory and survival signals that counteract therapeutic inhibition [83] [84]. Understanding these interconnected resistance networks is essential for designing effective combination strategies that preemptively block escape routes.
Tumor Microenvironment and Immune Evasion Mechanisms
The tumor microenvironment (TME) constitutes a sophisticated ecosystem that actively contributes to therapeutic resistance through multiple interconnected mechanisms. Cancer cells employ immune checkpoint regulation, metabolic reprogramming, and recruitment of immunosuppressive cells to create an environment hostile to anti-tumor immunity. Key immune checkpoints such as PD-1/PD-L1 and CTLA-4 function as molecular brakes on T-cell activation, with tumor cells frequently overexpressing these ligands to inhibit effector immune responses [85] [86].
Beyond checkpoint molecules, the TME employs metabolic strategies to suppress immune function. Tumor cells often exhibit aerobic glycolysis, resulting in accumulation of lactic acid that creates an acidic environment detrimental to T-cell function and proliferation. This acidic milieu directly impairs T-cell activation, reduces production of critical cytokines like IL-2 and IFN-γ, and promotes differentiation of immunosuppressive cell populations. Additionally, metabolic byproducts such as ammonia induce a unique form of T-cell death through mitochondrial damage and lysosomal dysfunction, further diminishing anti-tumor immunity [85].
The TME also actively recruits and expands regulatory immune cells including myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs). These populations secrete immunosuppressive cytokines like TGF-β and IL-10, which directly inhibit effector T-cell and NK-cell function while reinforcing the immunosuppressive niche. MDSCs additionally deplete essential amino acids like arginine through arginase production, creating nutrient deprivation that limits T-cell proliferation and function [85]. This multifaceted immunosuppressive network presents a formidable barrier to effective anti-tumor immunity and necessitates combination approaches that simultaneously target multiple components of the resistance machinery.
Strategic Rationales for Combination Therapy Design
Vertical and Horizontal Pathway Inhibition
Combination strategies can be conceptually categorized into vertical and horizontal inhibition approaches. Vertical pathway inhibition involves targeting multiple nodes within the same signaling cascade to create more complete pathway suppression and prevent bypass through upstream/downstream signaling adaptations. This approach is particularly valuable in oncogene-addicted cancers where persistent pathway activation drives tumor survival. For example, in BRAF-mutant melanoma, combined inhibition of BRAF and its downstream effector MEK has demonstrated superior efficacy compared to BRAF inhibition alone, delaying the emergence of resistance while reducing cutaneous toxicity [87].
Horizontal pathway inhibition employs a different logic, targeting parallel or complementary pathways that collectively sustain tumor growth and survival. This strategy acknowledges the network biology of cancer signaling, where functional redundancy and cross-talk between pathways create robustness against single-point interventions. By concurrently disrupting multiple independent pathways essential for tumor maintenance, horizontal combinations reduce the probability of resistance emergence since cancer cells must simultaneously evolve bypass mechanisms across multiple systems. Examples include combining targeted therapies with immunomodulatory agents or simultaneously inhibiting growth factor signaling and apoptotic pathways [81] [82].
Immunotherapy Integration Strategies
The integration of immunotherapeutic agents with other treatment modalities represents a particularly promising combination approach. Immune checkpoint inhibitors (ICIs) have demonstrated remarkable efficacy in certain cancer types, but primary and acquired resistance remain common challenges. Combination strategies that modulate the TME to enhance ICI efficacy include pairing ICIs with anti-angiogenic agents, targeted therapies, and chemotherapy [85] [86] [88].
The rationale for ICI combination approaches centers on converting "cold" immunologically ignorant or excluded tumors into "hot" inflamed microenvironments permissive to immune-mediated destruction. Targeted therapies can enhance tumor immunogenicity by inducing immunogenic cell death, releasing tumor antigens, and modulating immunosuppressive factors. Similarly, anti-angiogenic agents can normalize tumor vasculature, improving T-cell infiltration while reducing immunosuppressive cell populations. Chemotherapeutic agents can selectively deplete immunosuppressive cells like Tregs and MDSCs while simultaneously creating immunogenic tumor cell death that primes anti-tumor immune responses [85] [86] [88].
Comparative Analysis of Combination Therapy Approaches
Table 1: Comparison of Combination Therapy Strategies Across Cancer Types
| Cancer Type | Combination Approach | Molecular Target/Pathway | Reported Efficacy | Resistance Mechanisms Addressed |
|---|---|---|---|---|
| CML | Dasatinib + PI3K inhibitor | BCR::ABL1 + PI3K/AKT | Preclinical synergy | Kinase domain mutations, alternative pathway activation |
| KRAS G12C-mutant NSCLC | Olomorasib + chemoimmunotherapy | KRAS G12C + PD-L1/chemotherapy | 61% ORR, 90% DCR [89] | Primary immunotherapy resistance, compensatory signaling |
| Metastatic colorectal cancer | Zanzalintinib + atezolizumab | VEGFR/MET/TAM + PD-L1 | Median OS: 10.9 vs 9.4 months [88] | Immunosuppressive TME, multiple growth pathways |
| Triple-negative breast cancer | PARPi + AhR antagonist | DNA repair + AhR/STING pathway | Preclinical synergy [82] | BRCA-independent resistance, immunosuppressive signaling |
| Ovarian cancer (BRCA2-mut) | PARPi + ATR/CHK1 inhibitor | DNA repair + DDR | Enhanced olaparib efficacy [82] | Homologous recombination restoration |
| HNSCC | Radiation + anti-PD-L1 | DNA damage + PD-L1 | Synergy in immunogenic and less immunogenic models [82] | Radioresistance, immune exclusion |
Table 2: Key Clinical Trial Results of Combination Therapies
| Trial/Study | Phase | Patient Population | Intervention | Control | Primary Outcome |
|---|---|---|---|---|---|
| SUNRAY-01 (Integrated analysis) [89] | I/III | Advanced KRAS G12C-mutant NSCLC (n=77) | Olomorasib + chemoimmunotherapy | Historical | ORR: 61%, DCR: 90% |
| STELLAR-303 [88] | III | Metastatic colorectal cancer (n=901) | Zanzalintinib + atezolizumab | Regorafenib | Median OS: 10.9 vs 9.4 months (HR 0.80) |
| La Monica et al. [82] | Preclinical | Osimertinib-resistant NSCLC | Osimertinib + PDMP | Osimertinib alone | Resensitization to osimertinib |
| Rykkelid et al. [82] | Preclinical | HNSCC mouse models | X-ray/proton radiotherapy + anti-PD-L1 | Radiation alone | Synergistic tumor control |
Experimental Models and Methodologies for Combination Therapy Development
Preclinical Screening and Validation Platforms
The development of effective combination therapies relies on sophisticated experimental systems that recapitulate the complexity of human tumors. High-throughput drug screening platforms utilizing genetically characterized cancer cell lines enable systematic evaluation of thousands of drug combinations, identifying synergistic interactions that can be further validated in more complex models [81] [87]. The OncoDrug+ database represents a valuable resource in this context, integrating drug combination data with biomarker information and cancer type specifications to facilitate evidence-based combination therapy selection [87].
Advanced cellular models including patient-derived organoids and 3D culture systems provide more physiologically relevant contexts for evaluating drug combinations, preserving critical aspects of tumor architecture and cellular heterogeneity. These systems bridge the gap between conventional cell line models and in vivo testing, offering improved predictive value for clinical efficacy. For investigating immune-targeting combinations, co-culture systems incorporating immune cells with tumor cells or organoids enable assessment of immunomodulatory effects and T-cell mediated killing [81].
In Vivo and Translational Models
Patient-derived xenograft (PDX) models represent a cornerstone of combination therapy development, maintaining the histological characteristics, genetic landscape, and therapeutic response patterns of original patient tumors. These immunocompromised models are particularly valuable for studying targeted therapy combinations, though their utility for immuno-oncology combinations is limited by the absence of a functional immune system. Humanized mouse models with reconstituted human immune systems address this limitation, enabling evaluation of immunotherapeutic combinations in the context of human immune cell interactions [87].
Genetic engineering approaches have produced sophisticated genetically engineered mouse models (GEMMs) that recapitulate the spontaneous development of tumors within intact immune systems, providing powerful platforms for studying combination immunotherapies and tumor-host interactions. These models capture the complex dynamics of the TME and enable investigation of how combination therapies modulate immune cell populations, cytokine networks, and stromal components over time [81].
Methodology for High-Throughput Combination Screening
A standardized protocol for high-throughput combination screening involves several critical steps:
Cell Line Selection and Characterization: Select appropriately characterized cancer cell lines representing specific molecular subtypes. Perform baseline genomic, transcriptomic, and proteomic characterization to identify potential biomarkers.
Drug Library Preparation: Prepare compound libraries in DMSO at 1000× final concentration. Include single agents and combination matrices with systematic variation of concentration ratios.
Automated Liquid Handling: Use robotic systems to dispense cells and compounds into 384-well or 1536-well plates. Include appropriate controls (vehicle, positive cytotoxicity, etc.).
Viability Assessment: After 72-120 hours of incubation, measure cell viability using ATP-based (CellTiter-Glo) or resazurin reduction assays. Include complementary assays for apoptosis, cell cycle, and other phenotypic endpoints.
Synergy Analysis: Calculate combination effects using multiple reference models including Bliss independence, Loewe additivity, Zero Interaction Potency (ZIP), and HSA models. Apply statistical thresholds to identify significant synergistic interactions.
Validation and Mechanistic Studies: Confirm synergistic combinations in secondary assays and investigate mechanisms of action through transcriptomic, proteomic, and functional genomic approaches [87].
Signaling Pathways in Therapeutic Resistance and Combination Targeting
The complexity of signaling networks underlying therapeutic resistance necessitates visual representation to comprehend the interconnected nature of these pathways and their therapeutic targeting. The following diagram illustrates key resistance mechanisms and potential combination strategies:
Signaling Pathways in Resistance and Combination Therapy. This diagram illustrates key resistance mechanisms across different therapeutic classes and corresponding combination strategies designed to overcome these resistance pathways. TKI resistance involves multiple bypass signaling pathways, immune evasion employs immunosuppressive mechanisms, and DNA repair resistance utilizes pathway restoration. Combination therapies (yellow nodes) target multiple resistance mechanisms simultaneously.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Tools for Combination Therapy Development
| Tool Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Drug Combination Databases | OncoDrug+, DCDB, DrugCombDB [87] | Evidence-based combination prioritization | Biomarker associations, clinical trial data, synergy scores |
| High-Throughput Screening Platforms | ALMANAC, AZ-DREAM [87] | Systematic combination screening | Standardized synergy metrics, dose-response matrices |
| Predictive Algorithms | REFLECT, OncoTreat [87] | Computational prediction of effective combinations | Multi-omics integration, patient stratification |
| Preclinical Models | Patient-derived organoids, PDX models [81] [87] | Therapeutic validation | Tumor heterogeneity preservation, clinical correlation |
| Immune Monitoring Tools | Multiplex immunofluorescence, CyTOF, scRNA-seq [82] [85] | TME and immune response analysis | Single-cell resolution, spatial context, deep phenotyping |
| Pathway Analysis Platforms | Phospho-proteomics, RNA-seq [83] [84] | Mechanism of action studies | Signaling network mapping, adaptive response identification |
| Antibacterial agent 149 | Antibacterial agent 149, MF:C21H18N4O2, MW:358.4 g/mol | Chemical Reagent | Bench Chemicals |
The strategic implementation of combination therapies represents the forefront of cancer therapeutics development, addressing the fundamental challenges of tumor heterogeneity and adaptive resistance. The rational design of these regimens—informed by comprehensive understanding of resistance mechanisms, sophisticated preclinical models, and robust biomarker strategies—holds immense promise for improving patient outcomes across diverse malignancies. Future advances will increasingly rely on multi-omics profiling, functional precision medicine approaches, and computational prediction tools to identify optimal combination therapies tailored to individual patient tumors.
The continued evolution of combination therapy development will require close integration of translational research and clinical validation. As our understanding of resistance mechanisms deepens and novel therapeutic modalities emerge, the combinatorial landscape will expand exponentially, necessitating sophisticated prioritization frameworks and innovative clinical trial designs. The ultimate goal remains the development of rationally designed, biomarker-driven combination regimens that deliver durable responses and improved quality of life for cancer patients through simultaneous targeting of multiple oncogenic dependencies and resistance pathways.
The paradigm of clinical research has shifted fundamentally from traditional "one-size-fits-all" approaches to precision medicine strategies that account for significant heterogeneity among individuals with the same disease [90]. This evolution has been driven by advancements in our understanding of molecular phenotypes in diseases and attempts to target these specific characteristics [90]. Biomarker-driven clinical trials represent a cornerstone of this transformation, enabling researchers to identify patient subgroups most likely to benefit from targeted therapies [91]. The completion of the Human Genome Project and the maturation of next-generation sequencing technologies have been pivotal in fueling this movement toward personalized medicine [90].
In contemporary drug development, biomarkers serve critical functions in patient selection, serving as prognostic or predictive indicators, and as pharmacodynamic endpoints [92]. The strategic implementation of biomarker-driven approaches allows for more efficient clinical development by enriching trial populations for potential responders, thereby optimizing resource allocation and enhancing the probability of trial success [93]. This comprehensive guide examines the key design strategies, experimental methodologies, and practical considerations for implementing effective biomarker-driven clinical trials, with a specific focus on patient stratification approaches.
Core Biomarker-Driven Trial Designs
Fundamental Design Frameworks
Biomarker-driven clinical trials employ several distinct design architectures, each with specific applications and strategic considerations. The choice among these designs depends on the maturity of biomarker evidence, the mechanistic relationship between the biomarker and therapeutic intervention, and the overall development objectives [91] [92].
Table 1: Core Biomarker-Driven Clinical Trial Designs
| Design Type | Key Characteristics | Best Use Cases | Advantages | Limitations |
|---|---|---|---|---|
| Enrichment Design | Enrolls and randomizes only biomarker-positive participants [91] [92] | Strong mechanistic rationale linking therapy to biomarker [92] | Efficient signal detection; reduces sample size [91] | Narrower regulatory label; no information on biomarker-negative patients [92] |
| Stratified Randomization | Enrolls all patients; randomizes within biomarker (+/-) subgroups [92] | Prognostic biomarkers to isolate treatment effect [92] | Avoids bias; enables comparison across subgroups [92] | Requires larger sample size; complex logistics [91] |
| All-Comers Design | Enrolls both biomarker + and - without stratification; retrospective analysis [92] | Hypothesis generation for future studies [92] | Captures broader population; real-world evidence [92] | Risk of diluted effects if only subgroup responds [92] |
| Basket Trial | Tests single therapy across multiple diseases sharing common biomarker [90] [91] | Tumor-agnostic therapies with strong predictive biomarkers [92] | Operational efficiency; evaluates pan-cancer biomarker utility [90] | Statistical complexity; heterogeneous responses across cancer types [91] |
| Umbrella Trial | Evaluates multiple targeted therapies for a single disease with different biomarkers [90] | Specific disease with multiple molecular subtypes [90] | Efficiently matches therapies to biomarker subgroups [90] | Complex operational logistics; multiple companion diagnostics [90] |
| Platform Trial | Continuously evaluates multiple interventions for a disease; adaptive design [90] | Rapid evaluation of multiple therapeutic approaches [90] | Adaptable; can add/drop arms; efficient resource use [90] | Statistical complexity; operational challenges [90] |
Design Selection Considerations
Choosing the appropriate trial design requires careful consideration of multiple factors. Enrichment designs are most appropriate when there is strong preliminary evidence that treatment benefit is likely confined to the biomarker-positive population [91]. This approach was successfully employed for therapies targeting EGFR mutations in non-small cell lung cancer [92]. Conversely, all-comers designs with retrospective biomarker analysis are valuable in early development when the biomarker's predictive utility is uncertain [92].
The emergence of master protocol frameworks, including basket, umbrella, and platform trials, represents a significant innovation in biomarker-driven research [90] [91]. These designs provide infrastructure for evaluating multiple hypotheses simultaneously under a single overarching protocol, enhancing operational efficiency and standardization [90]. Platform trials specifically introduce adaptability by allowing interventions to be added or dropped based on accumulating data, creating a more dynamic and efficient evaluation system [90].
Comparative Effectiveness of Signaling Pathway Inhibitors: A Case Study on CK2 Inhibition
Experimental Methodology for CK2 Inhibitor Evaluation
The comparative assessment of protein kinase CK2 inhibitors provides an illustrative case study for evaluating signaling pathway inhibitors with different specificity profiles. The following experimental protocol outlines a standardized approach for comparing inhibitor efficacy and specificity:
Cell Culture and Treatment:
- Maintain human cancer cell lines (e.g., HeLa, MDA-MB-231) in appropriate media with 10% fetal bovine serum and penicillin/streptomycin at 37°C in 5% CO₂ [14].
- Plate cells at 70% confluence and allow to adhere for 24 hours prior to treatment.
- Prepare inhibitor stock solutions in DMSO and dilute to working concentrations in culture media, maintaining DMSO concentration below 0.1% in all treatments [14].
- Treat cells with increasing concentrations of CX-4945 (0-20 µM) and SGC-CK2-2 (0-40 µM) for 24 hours [14].
Western Blot Analysis:
- Lyse cells in RIPA buffer containing protease and phosphatase inhibitors.
- Separate proteins (20-30 μg per lane) by SDS-PAGE and transfer to PVDF membranes.
- Block membranes with 5% BSA in TBST for 1 hour at room temperature.
- Incubate with primary antibodies overnight at 4°C against: p-S129 Akt (1:1000), p-S13 Cdc37 (1:1000), and CK2 phospho-substrate antibody (recognizing pS/pT within CK2 consensus motifs) [14].
- Use β-actin or GAPDH as loading controls.
- Incubate with HRP-conjugated secondary antibodies (1:5000) for 1 hour at room temperature.
- Visualize using enhanced chemiluminescence substrate and quantify band intensity using densitometry software [14].
Cell Viability and Death Assays:
- Assess cell viability using MTT assay after 48-72 hours of inhibitor treatment.
- Measure apoptosis via Annexin V/propidium iodide staining and flow cytometry.
- Perform colony formation assays to evaluate long-term proliferative potential following inhibitor treatment [14].
Quantitative Comparison of CK2 Inhibitors
The comparative analysis of CK-2 inhibitors CX-4945 and SGC-CK2-2 reveals important differences in their inhibitory profiles and cellular effects, highlighting the significance of inhibitor specificity in targeting signaling pathways.
Table 2: Comparative Efficacy of CK2 Inhibitors in Cancer Cell Lines
| Parameter | CX-4945 | SGC-CK2-2 | Biological Significance |
|---|---|---|---|
| CK2α NanoBRET IC₅₀ | Not reported | 920 nM [14] | SGC-CK2-2 shows reduced potency but improved specificity |
| p-S129 Akt IC₅₀ (HeLa) | 0.7 µM [14] | 2.2 µM [14] | Differential sensitivity of CK2 substrates to inhibition |
| p-S13 Cdc37 IC₅₀ (HeLa) | 3 µM [14] | 9 µM [14] | Substrate-specific variation in inhibitor sensitivity |
| p-S129 Akt IC₅₀ (MDA-MB-231) | 0.9 µM [14] | 1.3 µM [14] | Cell line-dependent variability in inhibitor response |
| p-S13 Cdc37 IC₅₀ (MDA-MB-231) | 4.4 µM [14] | 20.4 µM [14] | Tissue-specific factors influencing inhibitor efficacy |
| Kinase Selectivity | Limited; inhibits multiple kinases beyond CK2 [14] | Exceptional; selective for CK2α/CK2α' with 200-fold margin over HIPK2 [14] | Critical for attributing observed phenotypes to CK2 inhibition |
| Antiproliferative Effects | Significant reduction in cell viability [14] | Minimal impact on proliferation [14] | Suggests off-target effects may contribute to CX-4945 cytotoxicity |
Signaling Pathway Diagram: CK2 Inhibition Mechanism
Multi-Omics Approaches for Enhanced Patient Stratification
Comprehensive Biomarker Discovery and Validation
Tumor heterogeneity remains a significant challenge in clinical trials, driving the need for sophisticated stratification approaches that capture the complexity of disease biology [94]. Multi-omics technologies provide powerful tools for addressing this challenge by delivering a comprehensive view of tumor biology through distinct but complementary data layers:
Genomics examines the full genetic landscape, identifying mutations, structural variations, and copy number variations that drive tumor initiation and progression through whole genome and whole exome sequencing [94].
Transcriptomics analyzes gene expression patterns using techniques like RNA sequencing, single-cell RNA sequencing, and spatial transcriptomics to provide snapshots of pathway activity and regulatory networks within the tissue architecture [94].
Proteomics investigates the functional state of cells by profiling proteins, including post-translational modifications, interactions, and subcellular localization through mass spectrometry and immunofluorescence-based methods [94].
Spatial Biology preserves tissue architecture to reveal how cells interact and how immune cells infiltrate tumors through spatial transcriptomics, spatial proteomics, multiplex immunohistochemistry, and mass spectrometry imaging [94].
The integration of these multi-omics data layers enables researchers to identify distinct patient subgroups based on molecular and immune profiles, facilitating precise patient selection in clinical trials [94]. This approach improves the detection of true treatment effects and supports the development of personalized therapeutic strategies.
Experimental Workflow for Multi-Omics Patient Stratification
Essential Research Reagent Solutions
The successful implementation of biomarker-driven clinical trials requires a comprehensive suite of specialized research reagents and platforms. The following table outlines essential materials and their applications in biomarker discovery and validation:
Table 3: Essential Research Reagents for Biomarker-Driven Trials
| Reagent Category | Specific Examples | Primary Applications | Key Considerations |
|---|---|---|---|
| CK2 Inhibitors | CX-4945 (Silmitasertib), SGC-CK2-2, SGC-CK2-1 [14] | Kinase signaling studies; specificity profiling | Varying selectivity profiles (CX-4945 has off-target effects; SGC-CK2-2 more specific) [14] |
| Phospho-Specific Antibodies | p-S129 Akt, p-S13 Cdc37, CK2 consensus motif antibody [14] | Monitoring CK2 inhibition; pathway activity assessment | Differential sensitivity of phospho-epitopes to inhibition [14] |
| Multi-Omics Platforms | Whole genome/exome sequencing; RNA-seq; mass spectrometry; spatial transcriptomics [94] | Comprehensive biomarker discovery; patient stratification | Integration challenges; require specialized bioinformatics [94] |
| Preclinical Models | Patient-derived xenografts (PDX); patient-derived organoids (PDO) [94] | Biomarker validation; therapeutic efficacy assessment | Preserve tumor heterogeneity; predictive of clinical response [94] |
| Cell Lines | HeLa (cervical cancer); MDA-MB-231 (breast cancer) [14] | Initial drug screening; mechanism of action studies | Variable responses across cell lines [14] |
| Analytical Tools | IntegrAO; NMFProfiler; graph neural networks [94] | Multi-omics data integration; patient classification | Handle incomplete datasets; identify biologically relevant signatures [94] |
Regulatory and Practical Implementation Considerations
Regulatory Expectations and Compliance
Regulatory agencies have established clear expectations for biomarker-driven clinical trials, emphasizing rigorous analytical validation and pre-specified analysis plans [92]. The FDA has issued guidance documents describing recommendations for basket and umbrella trials, providing support for these innovative designs [90]. Key regulatory considerations include:
- Pre-specification and Error Control: When biomarkers drive eligibility or endpoints, agencies expect rigorous analysis plans with justified sample sizes and controlled type I error rates [92].
- Assay Validation: Comprehensive analytical and clinical validation is required before pivotal studies, with companion diagnostics needing to meet stringent regulatory standards [92].
- Risk-Benefit Assessment: Enrichment designs can accelerate approval for well-defined populations but may narrow regulatory labels, while all-comers designs enable broader claims but risk diluted effects [92].
The European IVDR (In Vitro Diagnostic Regulation) has introduced additional complexity for biomarker and diagnostic development, creating challenges for companies working to synchronize drug launches with companion diagnostics across multiple jurisdictions [95]. Successful navigation of these regulatory landscapes requires early engagement with regulatory authorities and careful planning of biomarker assay development.
Practical Challenges and Solutions
The implementation of biomarker-driven trials presents several practical challenges that require strategic solutions:
Operational Complexity: Master protocols, including basket, umbrella, and platform trials, enjoy substantial infrastructure advantages but face unique operational challenges [91]. Centralized biomarker testing laboratories with standardized procedures can help mitigate these challenges by ensuring consistent assay performance across sites [93].
Statistical Considerations: Adaptive design elements play a crucial role in virtually all biomarker-driven trials, allowing for prospectively planned modifications based on accumulating data [91]. These include group sequential designs for early efficacy or futility stopping, sample size adaptation, and treatment arm selection [91].
Biomarker Assay Development: Choosing the appropriate assay is often the difference between success and failure [92]. Sponsors must evaluate whether tissue or liquid biopsy best matches the clinical question, ensure assay cut-points align with biomarker-drug response, and confirm sample integrity can be maintained, especially when transitioning to a companion diagnostic [92].
The future of biomarker-driven clinical trials will increasingly incorporate innovative technologies such as liquid biopsy, AI-assisted analysis, and adaptive protocols, transforming these tools from optional enhancements to essential components for trial success [92]. By integrating these technologies early, designing with methodological rigor, and engaging regulators proactively, researchers can maximize the impact of biomarker-driven strategies in drug development.
Addressing Clinical Challenges: Resistance, Toxicity, and Optimization Strategies
Targeted therapies against receptor tyrosine kinases (RTKs) have revolutionized the treatment of molecularly defined cancers, yet acquired resistance invariably develops, typically within 1 to 2 years, limiting their long-term efficacy [96] [97]. This resistance manifests through two primary mechanistic categories: (i) on-target mutations that directly alter the drug binding site and (ii) off-target bypass signaling that reactivates critical survival pathways through alternative receptors [96] [98]. Understanding the interplay and relative prevalence of these mechanisms is fundamental to designing next-generation therapeutic strategies that can overcome or prevent resistance.
The clinical paradigm of oncogene addiction, wherein cancers rely heavily on a single oncogenic protein or pathway for survival, provides the foundation for targeted therapy. In such cases, inhibition of the driver oncogene leads to substantial tumor regression [96]. Notable examples include non-small cell lung cancers (NSCLC) with activating mutations in the epidermal growth factor receptor (EGFR) or translocations in the anaplastic lymphoma kinase (ALK) gene [97]. Despite initial profound responses to corresponding tyrosine kinase inhibitors (TKIs), resistant clones eventually emerge and lead to disease progression, representing a central challenge in precision oncology [99].
On-target Resistance Mutations
Definition and Prevalence
On-target resistance refers to genetic alterations within the target kinase itself that impede drug binding while often preserving or enhancing the kinase's catalytic activity. These are typically secondary mutations that arise after treatment pressure and are distinct from the primary driver mutations [97]. The prevalence of these mutations is substantial; for example, the T790M mutation in EGFR is detected in more than 50% of EGFR-mutant lung cancers with acquired resistance to first-generation TKIs like gefitinib or erlotinib [96]. Similarly, resistance mutations in ALK are observed in approximately one-third of cancers with acquired resistance to the ALK inhibitor crizotinib [96].
Common On-target Mutations and Their Structural Impact
Table 1: Characterized On-target Resistance Mutations in Kinase Inhibitor Therapy
| Target Kinase | Resistance Mutation | Inhibitors Affected | Structural/Functional Consequence |
|---|---|---|---|
| EGFR | T790M (Gatekeeper) | Gefitinib, Erlotinib (1st Gen) | Increases ATP affinity, steric hindrance [97]. |
| EGFR | C797S | Osimertinib (3rd Gen) | Abrogates covalent binding to C797 residue [97]. |
| ALK | Multiple (e.g., L1196M, G1202R) | Crizotinib | Various steric interference and altered ATP affinity [96]. |
| MET | Y1230H | PHA-665752, PF-2341066 | Destabilizes autoinhibitory conformation, disrupts aromatic stacking with inhibitor [98]. |
The T790M "gatekeeper" mutation in EGFR involves a substitution of threonine with methionine at position 790 in the kinase domain. This mutation sterically hinders drug binding and increases the affinity of the kinase for ATP, reducing the inhibitory efficacy of ATP-competitive first-generation TKIs [96] [97]. In response, third-generation EGFR TKIs like osimertinib were designed to covalently bind to the C797 residue and are effective against T790M-positive cells. However, a subsequent C797S mutation prevents this covalent bonding, conferring resistance to osimertinib [97].
Beyond EGFR, analogous mutations occur in other targeted kinases. In MET-addicted cancers, the Y1230H mutation in the activation loop destabilizes the autoinhibitory conformation of the MET kinase and disrupts a critical aromatic stacking interaction with the inhibitor, leading to resistance to MET TKIs like PHA-665752 and PF-2341066 (crizotinib) [98].
Bypass Signaling Resistance Mechanisms
The Bypass Track Concept
Bypass track signaling represents a parallel resistance paradigm where tumor cells activate alternative RTKs to maintain pro-survival and proliferative signaling pathways despite sustained inhibition of the original oncogenic target [96]. This process is analogous to a cardiac bypass graft, where an alternative route circumvents a blocked artery. The bypass RTK reactivates key downstream pathways—primarily the PI3K-AKT and MEK-ERK cascades—effectively making the cancer cell no longer dependent on (or "addicted" to) the initially targeted kinase [96] [98].
Key Bypass RTKs and Their Ligands
Table 2: Documented Bypass Resistance Mechanisms in EGFR- and ALK-Mutant Cancers
| Oncogenic Driver | Bypass RTK | Mechanism of Activation | Key Downstream Pathway Sustained |
|---|---|---|---|
| EGFR | MET | Gene amplification or HGF ligand overexpression [96]. | PI3K/AKT & MEK/ERK [96]. |
| EGFR | HER2 (ErbB2) | Gene amplification [96]. | Not Specified |
| EGFR | AXL | Increased expression of AXL and its ligand GAS6 [96]. | Not Specified |
| EGFR | IGF1R | Loss of IGFBP3/4, increasing ligand availability [96]. | PI3K/AKT [96]. |
| EGFR | FGFR1 | FGF2-FGFR1 autocrine loop [96]. | Not Specified |
| MET | EGFR | Increased expression of TGF-α ligand [98]. | MEK/ERK [98]. |
Multiple RTKs have been implicated in mediating bypass resistance. In EGFR-mutant NSCLC, amplification of the MET gene is a well-established mechanism of resistance to gefitinib and erlotinib [96]. MET activation, either through genomic amplification or by its ligand hepatocyte growth factor (HGF), is sufficient to reactivate both PI3K/AKT and MEK/ERK signaling in the presence of effective EGFR blockade [96]. Similarly, activation of the EGFR pathway can drive resistance in MET-addicted cancers. In a resistant gastric carcinoma model, cells exhibited a marked increase in the expression of the EGFR ligand transforming growth factor α (TGFα), which sustained ERK signaling and promoted survival despite MET inhibition [98].
The following diagram illustrates the core concept of the bypass resistance mechanism, where an alternative RTK reactivates the critical downstream signaling pathways that were suppressed by the targeted therapy.
Experimental Models for Deciphering Resistance
In Vitro Resistance Modeling
A common experimental approach involves generating drug-resistant cell lines by continuously exposing a sensitive cell line to increasing concentrations of a TKI over several months [98]. For instance, the MET-addicted gastric carcinoma cell line SNU638 was cultured with the MET inhibitor PHA-665752 until clones emerged capable of proliferating in high (1 µM) drug concentrations [98]. Subsequent analysis of these resistant subclones can reveal the specific resistance mechanism(s) that evolved.
Protocol: Generating TKI-Resistant Cell Lines
- Culture Conditions: Maintain parental sensitive cells (e.g., SNU638, PC9) in appropriate media with 10% fetal bovine serum.
- Drug Exposure: Initiate treatment with a low concentration of the TKI (e.g., 10-50 nM) that inhibits growth by ~50% (IC50).
- Dose Escalation: Gradually increase the TKI concentration (e.g., in 2-fold steps) each time the cells resume robust growth. This process may take 6-9 months.
- Clonal Selection: Isplicate single-cell derived clones from the resistant population to assess heterogeneity.
- Validation: Confirm resistance by comparing the half-maximal inhibitory concentration (IC50) of the resistant clones to the parental line via cell viability assays (e.g., MTT, CellTiter-Glo) [98].
Analytical Techniques for Mechanism Identification
Once resistant models are established, multiple techniques are employed to pinpoint the resistance mechanism.
- Phospho-RTK Arrays: This tool allows for the simultaneous assessment of the phosphorylation status (activation) of dozens of RTKs. It can reveal the activation of a bypass RTK, such as maintained EGFR phosphorylation in MET-inhibited resistant cells [98].
- Genetic Analysis: DNA sequencing (e.g., Sanger, NGS) of the targeted kinase's coding region can identify secondary resistance mutations (e.g., EGFR T790M, MET Y1230H). RNA sequencing can uncover splice variants and expression changes in ligands or receptors [97] [98].
- Immunoblotting: Western blot analysis is used to monitor the activation state of downstream signaling pathways (e.g., pAKT, pERK, pS6) in the presence of the TKI, confirming whether the pathway has been reactivated in resistant cells [98].
The workflow below summarizes the key steps in modeling and analyzing acquired resistance.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Studying Resistance Mechanisms
| Reagent / Tool | Function/Application | Example Use Case |
|---|---|---|
| Tyrosine Kinase Inhibitors (TKIs) | Selective inhibition of target kinases to model therapeutic pressure and select for resistant clones. | PHA-665752 (MET inhibitor) for inducing resistance in SNU638 cells [98]. |
| Phospho-RTK Array Kit | Simultaneously screen for the activation of multiple receptor tyrosine kinases from cell lysates. | Identifying EGFR as an activated bypass RTK in MET-TKI resistant clones [98]. |
| Lentiviral shRNA/SgRNA Systems | Genetically knock down or knock out genes of interest to validate their functional role in resistance. | Validating that ERBB3 knockdown re-sensitizes cells to MET inhibition [98]. |
| Recombinant Growth Factors | Activate specific RTK pathways to test if ligand stimulation is sufficient to induce resistance. | Demonstrating that exogenous TGF-α confers resistance to MET inhibitors [98]. |
| Cellular Barcoding | Track the clonal dynamics and evolution of tumor cell populations under drug treatment. | Investigating the behavior of drug-tolerant persister cells upon EGFR-TKI treatment [97]. |
The relentless emergence of acquired resistance, driven by both on-target mutations and bypass signaling, underscores the remarkable adaptability of cancer cells under therapeutic pressure. A critical insight from research is that multiple resistance mechanisms can arise simultaneously within a single cancer, presenting daunting challenges for durable treatment [98]. Overcoming this requires a multi-pronged strategy.
The most direct approach is the development of next-generation inhibitors capable of binding the mutated target, such as osimertinib for EGFR T790M [97]. For bypass-mediated resistance, rational combination therapies that co-target the original oncogene and the bypass RTK are essential. For example, combined EGFR and MET inhibition can overcome MET-driven resistance in EGFR-mutant NSCLC, while combined MET and EGFR inhibition can overcome TGFα-driven resistance in MET-addicted gastric cancer [96] [98]. Future success will depend on continued molecular profiling of resistant tumors and the development of innovative therapeutic modalities, such as protolysis-targeting chimeras (PROTACs) and antibody-drug conjugates (ADCs), to outmaneuver the evolving defenses of cancer [100] [99].
NF-κB Pathway Activation as a Common Resistance Mechanism Across Inhibitor Classes
The nuclear factor-kappa B (NF-κB) signaling pathway represents a critical transcriptional hub that integrates diverse cellular signals to regulate genes controlling inflammation, cell survival, proliferation, and immune responses [101]. Beyond its established physiological roles, NF-κB activation has emerged as a powerful adaptive resistance mechanism that cancer cells and the tumor microenvironment (TME) utilize to evade targeted therapies, chemotherapeutics, and immunotherapies [102]. This pathway serves as a molecular escape route that is activated across multiple inhibitor classes, significantly limiting their clinical efficacy. Understanding how different therapeutic agents inadvertently activate NF-κB and developing strategies to counteract this resistance represents a frontier in improving cancer treatment outcomes. This review synthesizes evidence from recent studies demonstrating NF-κB-mediated resistance to JAK, MEK, and other targeted inhibitors, providing comparative experimental data and methodologies for investigating this convergent resistance mechanism.
NF-κB Signaling Fundamentals and Activation Mechanisms
The NF-κB transcription factor family consists of five members: RelA (p65), RelB, c-Rel, NF-κB1 (p50), and NF-κB2 (p52), which form various homo- and heterodimers regulated through two primary signaling cascades [101] [103]. In the canonical pathway, proinflammatory stimuli such as cytokines (TNF-α, IL-1β), pathogen-associated molecular patterns (PAMPs), and damage-associated molecular patterns (DAMPs) activate the IκB kinase (IKK) complex, leading to phosphorylation and degradation of IκB inhibitors and nuclear translocation of primarily p65:p50 dimers [101]. The non-canonical pathway, activated by specific TNF receptor family members, involves NF-κB-inducing kinase (NIK)-mediated processing of p100 to p52 and nuclear translocation of p52:RelB dimers [101]. Both pathways ultimately result in transcriptional activation of genes promoting cell survival, proliferation, and inflammation [101].
Table 1: Core Components of the NF-κB Signaling Pathway
| Component | Function | Role in Resistance |
|---|---|---|
| p65 (RelA) | Transcriptional transactivation subunit | Primary effector; phosphorylated at multiple regulatory sites |
| p50 | DNA-binding subunit | Forms heterodimer with p65; lacks transactivation domain |
| IκB proteins | Cytoplasmic sequestration of NF-κB | Degradation releases NF-κB for nuclear translocation |
| IKK complex | Phosphorylates IκB proteins | Signaling integration point for multiple resistance pathways |
| NEMO/IKKγ | Regulatory subunit of IKK complex | Essential for canonical NF-κB activation |
NF-κB activity is precisely regulated through post-translational modifications (PTMs), including phosphorylation, acetylation, ubiquitination, and methylation [104]. These modifications fine-tune NF-κB's transcriptional specificity, nuclear localization, and protein interactions, enabling context-dependent responses to therapeutic challenges [104]. For instance, phosphorylation of p65 at serine 536 enhances nuclear translocation and transcriptional activity, while acetylation at different lysine residues can either promote or suppress target gene expression [103] [104].
Diagram 1: NF-κB Activation Pathways in Therapeutic Resistance. Multiple inhibitor classes activate canonical and non-canonical NF-κB signaling, leading to expression of pro-survival genes and therapy resistance.
Comparative Analysis of NF-κB-Mediated Resistance Across Inhibitor Classes
JAK/STAT Inhibitors and NF-κB Compensation
JAK inhibitors represent a promising therapeutic class for hematological malignancies and inflammatory diseases, but their efficacy in solid tumors has been limited by compensatory mechanisms. Recent research demonstrates that JAK inhibition in tumor-associated macrophages (TAMs) leads to NF-κB activation, which subsequently upregulates a subset of tumor-promoting genes associated with therapeutic resistance [105]. This compensatory activation creates a molecular bypass that sustains tumor survival despite effective JAK/STAT pathway suppression.
Table 2: NF-κB-Mediated Resistance to JAK Inhibitors
| JAK Inhibitor | Experimental System | NF-κB Activation Readout | Resistance Outcome |
|---|---|---|---|
| Ruxolitinib (JAK1/2) | Bone marrow-derived macrophages + conditioned media from 4T1/HC11 tumor cells | Increased phospho-p65 (Ser536), nuclear p65 translocation | Upregulation of tumor-promoting genes; reduced efficacy in mammary tumor models |
| Ruxolitinib + IKK-16 | Mouse mammary tumor models (Balb/c) | Suppressed NF-κB activation | Improved survival over single-agent treatment; enhanced tumor growth reduction |
| Solcitinib (JAK1) | Human breast cancer cell lines + macrophage coculture | p65 phosphorylation within 15 minutes | Macrophage-mediated protection of tumor cells from JAK inhibition |
| NVP-BSK085 (JAK2) | Tumor-macrophage coculture systems | Rapid NF-κB pathway activation | Sustained tumor cell viability despite JAK2 pathway inhibition |
Mechanistically, JAK inhibition in TAMs triggers rapid phosphorylation of p65 at serine 536 and promotes its nuclear translocation within 15 minutes of treatment [105]. This activation is sufficient to induce transcription of pro-survival and inflammatory genes that compensate for suppressed JAK/STAT signaling. The functional consequence is demonstrated by studies showing that combining the JAK inhibitor ruxolitinib with the IKK inhibitor IKK-16 significantly improves survival outcomes compared to either agent alone in mammary tumor models [105].
MEK Inhibition and NF-κB-Driven Survival Pathways
In rectal cancer models, MEK inhibitors have been identified as potent enhancers of radiation response, yet their efficacy as single agents is limited by adaptive resistance mechanisms [106]. Research using patient-derived rectal cancer organoids demonstrates that MEK inhibition suppresses radiation-induced activation of RAS-MAPK signaling but concurrently modulates DNA damage response pathways [106]. Specifically, MEK inhibitors downregulate RAD51, a key homologous recombination protein, creating a therapeutic vulnerability that can be exploited with combination approaches.
The intersection between MEK inhibition and NF-κB activation involves cross-talk between the RAS-MAPK and NF-κB signaling networks. While not explicitly detailed in the available literature, this cross-talk potentially occurs through shared upstream regulators or parallel survival pathway activation. Combined MEK and PARP inhibition enhances radiosensitivity in rectal cancer models, suggesting that NF-κB activation may represent a complementary resistance mechanism to these targeted approaches [106].
PI3K/Akt Pathway Inhibitors and NF-κB Activation
The PI3K/Akt pathway frequently cooperates with NF-κB signaling to promote oncogenic transformation and therapeutic resistance. Akt stimulates the transactivation potential of the RelA/p65 subunit through IκB kinase activity and p38 mitogen-activated protein kinase signaling [107]. This regulation occurs via phosphorylation of p65 at serines 529 and 536, sites known to enhance transcriptional activity [107].
In Akt-transformed chicken embryonic fibroblasts, NF-κB-driven transcription is significantly elevated, and degradation of IκB protein is enhanced [108]. Introduction of a super-repressor of NF-κB (IκBSR) effectively interferes with PI3K- and Akt-induced oncogenic transformation, demonstrating the essential role of NF-κB in this process [108]. The molecular mechanism involves Akt-mediated phosphorylation of IKKα on threonine 23, which serves as a prerequisite for subsequent phosphorylation of p65 at serine 534 by IKKα and IKKβ [108]. This dual regulation of both IκB degradation and p65 phosphorylation illustrates how oncogenic signaling pathways directly co-opt NF-κB to maintain transformation.
Cross-Pathway Integration and Compensatory Activation
The recurrent theme across inhibitor classes is that targeted pathway inhibition creates selective pressure for cancer cells to activate alternative survival signaling, with NF-κB serving as a preferred escape route due to its central role in regulating anti-apoptotic genes. This compensatory activation can occur through multiple mechanisms:
- Direct pathway cross-talk: Shared regulatory nodes between targeted pathways and NF-κB signaling, such as Akt-mediated IKK phosphorylation [108] [107]
- Transcriptional reprogramming: Inhibitor-induced changes in the TME that activate NF-κB in stromal cells, particularly macrophages [105]
- Feedback loop activation: Relief of negative regulation on NF-κB components following pathway inhibition
- Post-translational modification: Altered phosphorylation, acetylation, or ubiquitination patterns that enhance NF-κB activity despite upstream inhibition [104]
Experimental Models and Methodologies for Investigating NF-κB Resistance
In Vitro Models and Coculture Systems
The investigation of NF-κB-mediated resistance requires sophisticated experimental models that recapitulate tumor-stroma interactions. Bone marrow-derived macrophages (BMDMs) cocultured with tumor cells provide a robust system for studying paracrine signaling-mediated resistance [105]. The standard methodology involves:
- Macrophage generation: Isolate bone marrow from mouse femurs and tibias, differentiate in M-CSF containing media (10-20 ng/mL) for 7 days to generate BMDMs [105]
- Serum starvation: Deprive BMDMs of serum for 2 hours to downregulate baseline pathway activation
- Conditioned media treatment: Treat BMDMs with tumor cell-conditioned media in the presence or absence of inhibitors (e.g., 0.5 μM ruxolitinib) for 15 minutes to assess rapid phosphorylation events or 4 hours for transcriptional analyses [105]
- Coculture experiments: Plate tumor cells in the bottom of culture plates with macrophages in 0.4 μm hanging inserts to allow soluble factor exchange without direct cell contact [105]
NF-κB Activation Assessment Techniques
Multiple complementary approaches are required to comprehensively evaluate NF-κB activation in resistance models:
Nuclear fractionation and immunoblotting: Using commercial kits (e.g., NE-PER Nuclear and Cytoplasmic Extraction Kit), separate nuclear and cytoplasmic proteins 15 minutes after treatment to assess p65 nuclear translocation [105]. Immunoblot analysis with phospho-specific p65 antibodies (e.g., anti-phospho-p65 Ser536) provides quantitative data on pathway activation.
Luciferase reporter assays: Transfect cells with NF-κB promoter reporters containing multiple κB binding sites (e.g., (TGGGGACTTTCCGC)5) to quantify transcriptional activity [108]. Normalize firefly luciferase activity to Renilla luciferase controls for accurate quantification.
Gene expression profiling: RNA sequencing or RT-PCR analyses 4 hours after treatment to identify NF-κB target genes upregulated in response to inhibitor treatment [105]. Focus on known NF-κB-regulated survival genes (Bcl-2, Bcl-XL, c-IAP1/2, c-FLIP) and inflammatory mediators.
In Vivo Validation Models
Transgenic mouse models and tumor xenografts provide essential platforms for validating NF-κB's role in therapeutic resistance:
- Mammary tumor models: Implant tumor cells (e.g., 4T1) in syngeneic Balb/c mice and treat with JAK inhibitors (ruxolitinib), NF-κB pathway inhibitors (IKK-16), or combinations to assess tumor growth and survival [105]
- Rectal cancer xenografts: Establish patient-derived xenografts or cell line-derived xenografts in immunocompromised mice to evaluate MEK/PARP inhibitor combinations with radiation [106]
- Metastasis models: Utilize experimental metastasis assays to evaluate the impact of NF-κB inhibition on distant organ colonization following primary tumor treatment
Research Reagent Solutions for NF-κB Resistance Studies
Table 3: Essential Research Reagents for Investigating NF-κB-Mediated Resistance
| Reagent Category | Specific Examples | Research Application | Experimental Considerations |
|---|---|---|---|
| NF-κB Pathway Inhibitors | IKK-16 (IKKβ inhibitor), BAY-11-7082 (IκB phosphorylation inhibitor), JSH-23 (nuclear translocation inhibitor) | Block specific nodes in NF-κB signaling cascade | Variable selectivity profiles; off-target effects at higher concentrations |
| JAK/STAT Inhibitors | Ruxolitinib (JAK1/2), Solcitinib (JAK1), NVP-BSK085 (JAK2) | Target oncogenic JAK/STAT signaling | Context-dependent effects on tumor vs. stromal cells; compensatory NF-κB activation |
| Phospho-Specific Antibodies | Anti-phospho-p65 (Ser536, Ser529), anti-phospho-IκBα | Detect activated NF-κB pathway components | Time-sensitive detection (15-30 min post-stimulation optimal) |
| Nuclear Fractionation Kits | NE-PER Nuclear and Cytoplasmic Extraction Kit | Assess NF-κB nuclear translocation | Rapid processing required to preserve protein modifications |
| Reporter Systems | NF-κB luciferase reporters (κB-binding site multimers) | Quantify NF-κB transcriptional activity | Normalization to constitutive controls essential for accuracy |
| Animal Models | Syngeneic tumor models (4T1 in Balb/c), patient-derived xenografts | In vivo validation of resistance mechanisms | Strain-specific immune responses influence NF-κB activation |
Strategic Approaches to Overcome NF-κB-Mediated Resistance
The consistent emergence of NF-κB activation as a resistance mechanism across therapeutic classes highlights the need for rational combination strategies. Several approaches show promise in preclinical models:
Vertical pathway targeting: Combining upstream targeted agents with NF-κB pathway inhibitors addresses compensatory activation while maintaining primary pathway suppression. For example, JAK inhibition combined with IKKβ blockade prevents macrophage-mediated resistance in mammary tumor models [105].
Horizontal pathway targeting: Simultaneously targeting multiple parallel survival pathways prevents compensatory signaling. The combination of MEK and PARP inhibitors in rectal cancer models represents this approach, where suppression of both MAPK signaling and DNA repair creates synthetic lethality [106].
Sequential therapy: Timing interventions to target resistance mechanisms as they emerge, rather than concurrently, may mitigate toxicity while maintaining efficacy. This approach requires careful monitoring of NF-κB activation dynamics during treatment.
Post-translational modification targeting: Developing agents that specifically modulate NF-κB PTMs (e.g., p65 phosphorylation, acetylation) could enable more precise disruption of resistance mechanisms without completely abrogating NF-κB's physiological functions [104].
Diagram 2: Strategic Framework to Overcome NF-κB-Mediated Therapeutic Resistance. Multiple inhibitor classes induce NF-κB activation through distinct cellular mechanisms, requiring integrated approaches to overcome resistance.
NF-κB pathway activation represents a convergent resistance mechanism that significantly limits the efficacy of diverse therapeutic classes, including JAK, MEK, and PI3K/Akt inhibitors. The consistent emergence of this pathway across contexts highlights its fundamental role in maintaining tumor cell survival under therapeutic pressure. Current evidence demonstrates that rational combination strategies targeting both primary oncogenic pathways and NF-κB signaling can overcome this resistance in preclinical models.
Future research directions should focus on several key areas: First, developing more precise methods to monitor NF-κB activation dynamics in patients receiving targeted therapies to identify resistance emergence before clinical progression. Second, creating more selective NF-κB modulators that disrupt resistance-associated functions while preserving physiological immune responses. Third, exploring the interplay between NF-κB and other resistance mechanisms, such as immune checkpoint upregulation and metabolic adaptation. Finally, advancing clinical trials that strategically combine pathway-specific inhibitors with NF-κB-targeted approaches based on robust predictive biomarkers.
As our understanding of NF-κB's role in therapeutic resistance continues to evolve, so too will opportunities to develop more durable and effective cancer treatments that preempt or counteract this adaptive survival mechanism.
Targeted therapies against specific signaling pathways have revolutionized cancer treatment. However, their clinical application is often limited by characteristic adverse effect profiles arising from both on-target and off-target mechanisms. Understanding the pathophysiology, incidence, and management strategies for these toxicities is crucial for optimizing patient outcomes in clinical practice and drug development. This guide provides a comparative analysis of toxicity profiles and mitigation strategies across major classes of signaling pathway inhibitors, synthesizing evidence from recent clinical studies and trials to inform researchers and drug development professionals.
Toxicity Profiles of Major Pathway Inhibitor Classes
Androgen Receptor Pathway Inhibitors (ARPIs)
Androgen receptor pathway inhibitors, including abiraterone acetate, apalutamide, and enzalutamide, represent a cornerstone in the treatment of metastatic hormone-sensitive prostate cancer (mHSPC). While demonstrating comparable efficacy in terms of progression-free survival, these agents exhibit distinct toxicity profiles and pharmacokinetic characteristics that may influence clinical selection [16].
Table 1: Comparative Efficacy and Safety of Androgen Receptor Pathway Inhibitors in mHSPC
| Parameter | Abiraterone Acetate | Apalutamide | Enzalutamide |
|---|---|---|---|
| 2-year PFS to mCRPC | 74.1% | 81.4% | 85.6% |
| PSA ≤0.2 ng/mL within 12 weeks | 25.5% | 44.0% | 55.9% |
| Median time to PSA nadir | 12.2 months | 7.2 months | 7.5 months |
| PSA reduction ≥90% within 12 weeks | 87.2% | 94.5% | 97.1% |
| Common adverse events | Hypertension, hypokalemia, hepatotoxicity | Rash, hypothyroidism, fatigue | Fatigue, hypertension, musculoskeletal pain |
In a real-world multicenter retrospective study with 219 patients, the apalutamide and enzalutamide groups demonstrated superior early PSA response kinetics compared to abiraterone acetate, achieving higher rates of PSA decline to ≤0.2 ng/mL within 12 weeks (44.0% and 55.9% vs. 25.5%, respectively) and significantly shorter median time to PSA nadir (7.2 and 7.5 months vs. 12.2 months; p<0.001) [16]. Importantly, this study identified early PSA response as an independent prognostic factor for improved progression-free survival regardless of ARPI selection, highlighting the importance of early toxicity management to maintain treatment intensity [16].
Tyrosine Kinase Inhibitors (TKIs)
Tyrosine kinase inhibitors represent a broad class of targeted therapies with diverse toxicity profiles dependent on their specificity and target kinases. The adverse effects of TKIs range from manageable constitutional symptoms to life-threatening cardiotoxicity requiring careful monitoring and intervention [25].
Table 2: Comparative Toxicity Profiles of Selected Tyrosine Kinase Inhibitors
| TKI Class | Representative Agents | Common Adverse Effects | Serious Adverse Effects | Management Strategies |
|---|---|---|---|---|
| VEGFR Inhibitors | Sunitinib, Sorafenib | Fatigue, diarrhea, hand-foot syndrome, hypertension | Left ventricular dysfunction, heart failure, thyroid dysfunction | Regular ECG and echocardiogram monitoring, antihypertensives, dose modification |
| EGFR Inhibitors | Erlotinib, Gefitinib | Acneiform rash, diarrhea, mucositis | Interstitial lung disease, hepatotoxicity | Topical corticosteroids/antibiotics, antidiarrheals, drug interruption for severe toxicity |
| BCR-ABL Inhibitors | Imatinib, Nilotinib | Peripheral edema, nausea, muscle cramps | QT prolongation, hepatotoxicity, myelosuppression | Electrolyte monitoring, dose reduction, EKG monitoring |
| BTK Inhibitors | Ibrutinib, Acalabrutinib | Diarrhea, bleeding, arrhythmias | Atrial fibrillation, hemorrhage, infections | Cardiac monitoring, anticoagulation management |
The cardiovascular toxicity of TKIs deserves particular emphasis, with HER2-targeted therapies, vascular endothelial growth factor inhibitors (VEGFIs), and BCR-ABL TKIs associated with the highest relative risk for high-grade cardiotoxicity [25]. A meta-analysis of clinical trials in 10,647 patients with various malignancies treated with TKIs (axitinib, pazopanib, sorafenib, sunitinib, and vandetanib) showed a combined incidence of asymptomatic left ventricular dysfunction of 2.4% [25]. The mechanisms underlying TKI-induced cardiovascular damage include inhibition of VEGF signaling leading to reduced myocardial capillary density (rarefaction), impaired neuregulin-HER pathway signaling critical for cardiomyocyte survival, and mitochondrial dysfunction through activation of various cell death pathways including ferroptosis and pyroptosis [25].
Immune Checkpoint Inhibitors (ICIs)
Immune checkpoint inhibitors targeting CTLA-4, PD-1, and PD-L1 have transformed oncology but are associated with immune-related adverse events (irAEs) resulting from unleashed immune responses against normal tissues. The toxicity profiles differ between ICI classes and combination regimens, requiring specialized management approaches [109] [110].
In patients with nervous system cancers, the top five reported irAEs include seizure, confused state, encephalopathy, muscular weakness, and gait disturbance [109]. Older patients demonstrate greater susceptibility to these neurological irAEs, with significant differences in time-to-onset between age groups [109]. The molecular mechanisms underlying irAEs involve inflammatory responses, secretion of inflammatory mediators, and aberrant activation of pathologic pathways in normal tissues [109].
Emerging strategies to mitigate ICI toxicities focus on targeting specific molecular pathways involved in irAE pathogenesis without compromising antitumor efficacy. Key modifiable pathways include cytokine signaling (IL-6, IL-17, IL-4, IFN-γ, IL-1β, TNF-α), integrin-mediated interactions (integrin subunits α4 and β7), and microbiome-related factors [110]. Notably, cytokine-blocking antibodies such as anti-IL-6R have demonstrated potential to curtail irAEs while potentially enhancing ICI efficacy for certain malignancies [110].
Selective RET Inhibitors
The selective RET inhibitors selpercatinib and pralsetinib have demonstrated improved toxicity profiles compared to multi-kinase inhibitors, with treatment discontinuation rates due to emerging toxicities of approximately 4%-7% for pralsetinib and 2%-5% for selpercatinib in clinical trials [111]. The most common adverse events for both agents include fatigue, hypertension, constipation, and diarrhea, occurring in more than 25% of patients [111].
Table 3: Laboratory Abnormalities with Selective RET Inhibitors
| Laboratory Parameter | Selpercatinib | Pralsetinib |
|---|---|---|
| Grade 3-4 Lymphopenia | Common | Common |
| Increased ALT/AST | Common | Common |
| Hyponatremia | Common | Common |
| Hypocalcemia | Common | Common |
| Neutropenia | Less common | Common |
| Anemia | Less common | Common |
| Thrombocytopenia | Rare | Common |
| Increased Alkaline Phosphatase | Rare | Common |
The pathophysiology of RET inhibitor toxicities involves both inhibition of endogenous RET receptors, which play roles in bone marrow niches and parasympathetic neurons of the gastrointestinal system, and off-target effects on non-RET receptors [111]. For instance, hypersensitivity reactions and QT interval prolongation with selpercatinib and pneumonitis with pralsetinib may result from non-RET receptor inhibition [111].
Mitigation Strategies and Management Approaches
General Principles for Toxicity Management
Effective management of targeted therapy toxicities requires a systematic approach including prophylactic measures, early detection, prompt intervention, and appropriate dose modifications. The overarching goal is to maintain therapeutic efficacy while minimizing treatment interruptions and preserving quality of life [111] [25].
For most targeted therapies, milder toxicities (Grade 1-2) can be managed with supportive care without treatment modification. Moderate toxicities (Grade 2-3) often require temporary treatment interruption and symptomatic management until resolution to Grade ≤1, followed by dose reduction upon resumption. Severe or life-threatening toxicities (Grade 4) typically necessitate permanent discontinuation [111].
Specific Management Protocols
Hepatotoxicity Management
Regular monitoring of ALT and AST every 2 weeks for the first 3 months, then monthly thereafter, is recommended for agents with hepatotoxicity risk [111]. For Grade ≥3 events, the drug should be withheld and liver function tests monitored weekly until toxicity decreases to Grade 1. Upon resolution, treatment can be resumed at a reduced dose (by 1 dose level for pralsetinib and 2 dose levels for selpercatinib) with gradual escalation to the original dose if tolerated [111]. Permanent discontinuation is recommended if Grade ≥3 hepatotoxicity recurs [111].
Cardiovascular Toxicity Management
Baseline cardiovascular risk assessment is essential before initiating TKIs with known cardiovascular toxicity profiles [25]. For patients receiving VEGF inhibitors, blood pressure should be monitored regularly, and antihypertensive therapy initiated or adjusted for blood pressure >140/90 mmHg [25]. Asymptomatic left ventricular dysfunction typically warrants consultation with a cardiologist and consideration of ACE inhibitors or beta-blockers, while symptomatic heart failure may require treatment interruption or discontinuation [25].
Skin Toxicity Management
For localized Grade 1 or 2 cutaneous toxicities, topical steroids (e.g., hydrocortisone 2.5% cream) and/or topical antibiotics (e.g., clindamycin 1% gel) are recommended [111]. Oral antihistamines can be added for pruritus. For generalized and mildly symptomatic Grade 2 rash, oral doxycycline (100 mg twice daily) or minocycline (100 mg twice daily) in addition to topical therapy is effective [111]. Generalized and severe Grade ≥3 rash requires systemic steroids and treatment withholding until toxicity improves to Grade ≤1, with reassessment after 2 weeks of supportive treatment and resumption at a reduced dose level [111].
Hypersensitivity Reactions
Management of hypersensitivity reactions involves immediate drug withholding and administration of steroids (e.g., prednisone 1 mg/kg) [111]. After symptom resolution, treatment can be resumed at a third dose level with gradual weekly escalation until the original dose is restored [111]. Steroids should be continued until the target dose is achieved and then gradually tapered if symptoms remain controlled. Permanent discontinuation is recommended if hypersensitivity recurs [111].
Experimental Models and Research Methodologies
Preclinical Toxicity Assessment Models
Preclinical assessment of signaling pathway inhibitor toxicities employs a range of in vitro and in vivo models. Primary human cardiomyocytes and endothelial cells are utilized to assess cardiotoxicity potential, measuring parameters such as mitochondrial membrane potential, reactive oxygen species production, and apoptosis activation [25]. Mouse models with humanized immune systems provide platforms for evaluating immune-related adverse events, particularly for immunotherapies [110].
The PI3K/AKT/mTOR signaling pathway, frequently dysregulated in cancer, also serves as an important model for understanding on-target toxicities. Genetically engineered mouse models with tissue-specific PIK3CA mutations or PTEN deletion recapitulate toxicity patterns observed in patients and enable mechanistic studies of adverse event pathogenesis [3].
Clinical Trial Designs for Toxicity Assessment
The multicenter retrospective cohort study design provides real-world evidence on toxicity profiles across different patient populations. The ARPI study analyzed 219 patients with mHSPC who received first-line ARPIs combined with androgen deprivation therapy, evaluating progression-free survival and PSA response within 12 weeks [16]. Statistical analysis included Kaplan-Meier survival estimates, log-rank tests for comparisons, and multivariate Cox proportional hazards models to identify factors independently associated with outcomes [16].
Network meta-analyses of randomized controlled trials enable indirect comparisons of toxicity profiles across multiple agents. The hepatocellular carcinoma systematic review and network meta-analysis included 18 RCTs involving 6,910 patients, synthesizing data on grade ≥3 adverse events and treatment discontinuation due to toxicities [112]. Bayesian random-effects models were employed with treatments ranked according to the surface under the cumulative ranking curve (SUCRA) values [112].
Signaling Pathways and Toxicity Mechanisms
Figure 1: Signaling Pathways and Associated Toxicities. This diagram illustrates the core signaling pathway (yellow-blue) and how inhibition of specific therapeutic targets (red) leads to characteristic adverse effects (gray).
The PI3K/AKT/mTOR (PAM) signaling pathway represents a central signaling network frequently targeted in cancer therapy and exemplifies the challenge of on-target toxicities [3]. This pathway is highly conserved in eukaryotic cells and promotes cell survival, growth, and proliferation in response to external stimuli [3]. Dysregulation of this pathway occurs in approximately 50% of tumors, making it the most commonly activated pathway in human cancer [3].
Inhibition of receptor tyrosine kinases (RTKs) upstream of PI3K can lead to toxicities through both on-target and off-target effects. For example, VEGF inhibitors cause cardiovascular toxicities through rarefaction of the myocardial capillary network, leading to myocardial hypoperfusion and impaired contractility [25]. Similarly, inhibition of the neuregulin-HER pathway by anti-HER2 TKIs disrupts cardioprotective signaling, contributing to left ventricular dysfunction [25].
The pathophysiology of adverse events varies by drug class. Immune-related adverse events from checkpoint inhibitors result from unleashed immune responses against normal tissues, with specific T-cell subsets and cytokine signaling (IL-6, IL-17, IFN-γ) playing central roles [110]. RET inhibitor toxicities stem from inhibition of endogenous RET receptors crucial for bone marrow niches and gastrointestinal parasympathetic neurons [111].
Research Reagent Solutions
Table 4: Essential Research Reagents for Toxicity Studies
| Reagent/Category | Specific Examples | Research Applications |
|---|---|---|
| Cell-Based Assays | Primary human cardiomyocytes, Hepatocytes, iPSC-derived cells | In vitro toxicity screening, mechanistic studies |
| Animal Models | Humanized immune system mice, Tissue-specific knockout mice | Preclinical toxicity assessment, irAE modeling |
| Cytokine Detection | IL-6, IL-17, IFN-γ ELISA kits, Multiplex immunoassays | irAE biomarker identification, inflammatory monitoring |
| Signal Transduction | Phospho-specific antibodies for AKT, mTOR, RET | Pathway inhibition assessment, target engagement |
| Toxicity Biomarkers | Troponin, NT-proBNP, ALT/AST assays | Cardiotoxicity and hepatotoxicity monitoring |
| Immunohistochemistry | PD-L1, CD3, CD8 antibodies | Tissue-based toxicity evaluation, immune cell infiltration |
The management of adverse effects from signaling pathway inhibitors requires a deep understanding of their mechanisms, incidence patterns, and evidence-based mitigation strategies. While significant progress has been made in toxicity management, several challenges remain, including predicting individual patient susceptibility, managing cross-toxicities in combination therapies, and developing targeted approaches that dissociate antitumor efficacy from adverse effects. Future research directions should focus on predictive biomarker development, personalized toxicity risk assessment, and novel therapeutic strategies that selectively target oncogenic signaling while sparing normal physiological functions.
Optimizing Dosing Schedules and Administration Routes for Improved Tolerability
The therapeutic landscape for numerous complex diseases, particularly in oncology and dermatology, has been revolutionized by the advent of targeted therapies, including signaling pathway inhibitors. These advanced systemic therapies (ASTs) offer enhanced precision over conventional treatments by interfering with specific molecular pathways driving disease pathogenesis [113]. However, their clinical success is not determined by efficacy alone; optimal dosing schedules and administration routes play a pivotal role in determining real-world tolerability, treatment persistence, and ultimately, patient outcomes. The comparative effectiveness of these inhibitors is intrinsically linked to their pharmacokinetic and pharmacodynamic properties, which are influenced by their formulation and dosing regimens [113] [16].
This guide provides a systematic comparison of different classes of signaling pathway inhibitors, focusing on how their dosing schedules and administration routes impact tolerability profiles. By synthesizing data from recent real-world studies, clinical trials, and meta-analyses, we aim to offer drug development professionals and researchers an objective framework for evaluating these critical parameters in the context of treatment optimization and future drug design.
Comparative Analysis of Dosing and Tolerability Across Inhibitor Classes
JAK Inhibitors in Inflammatory Dermatoses
Janus kinase (JAK) inhibitors represent a prominent class of oral small molecule inhibitors used in immune-mediated inflammatory diseases. Their administration route and dosing frequency significantly influence their efficacy and safety profiles.
Table 1: Comparative Dosing and Tolerability of JAK Inhibitors in Dermatologic Conditions
| Drug Name | Indication | Administration Route | Dosing Schedule | Notable Tolerability Concerns |
|---|---|---|---|---|
| Upadacitinib | Atopic Dermatitis [114] | Oral | Once daily [114] | Infections, acne [113] |
| Baricitinib | Alopecia Areata [115] | Oral | Once daily [115] | - |
| Abrocitinib | Atopic Dermatitis [114] | Oral | Once daily [114] | - |
| Ritlecitinib | Alopecia Areata [115] | Oral | Once daily (50 mg) [115] | Favorable safety profile in high-dose groups [115] |
| Deuruxolitinib | Alopecia Areata [115] | Oral | Once daily (8 mg, 12 mg) [115] | Higher likelihood of adverse events [115] |
| Brepocitinib | Alopecia Areata [115] | Oral | Once daily (30 mg) [115] | - |
| Delgocitinib | Atopic Dermatitis [114] | Topical Ointment | - | Reduced systemic exposure |
| Ruxolitinib | Alopecia Areata [115] | Topical Cream | - | Reduced systemic exposure |
The oral administration route common to most JAK inhibitors offers convenience and systemic exposure suitable for moderate-to-severe disease. However, this is associated with a higher frequency of systemic adverse events, including infections and acneiform eruptions, as observed in real-world studies [113]. In contrast, topical formulations like delgocitinib ointment and ruxolitinib cream provide a valuable alternative for localized disease, minimizing systemic exposure and associated adverse events, though their efficacy in severe cases may be limited [115].
Biologics vs. JAK Inhibitors in Atopic Dermatitis
Direct comparisons between biologic agents and JAK inhibitors for atopic dermatitis (AD) reveal critical differences in response dynamics and persistence, which are indirectly influenced by their administration protocols.
Table 2: Biologics vs. JAK Inhibitors: Dosing, Response, and Tolerability
| Parameter | Biologics (e.g., Dupilumab, Tralokinumab) | JAK Inhibitors (e.g., Upadacitinib, Abrocitinib) |
|---|---|---|
| Administration Route | Subcutaneous injection [114] | Oral [114] |
| Typical Dosing Frequency | Every 1-4 weeks (varies by agent) [114] | Once or twice daily [114] |
| Onset of Action | Slower early response [113] | Faster early response [113] |
| Long-term Improvement | Greater absolute improvements from weeks 16-52 [113] | - |
| Treatment Persistence | Longer persistence over time [113] | - |
| Common Adverse Events | Ocular symptoms (e.g., conjunctivitis) [113] [114] | Infections, acne [113] |
The subcutaneous route for biologics entails less frequent dosing, which may contribute to longer treatment persistence as observed in real-world settings [113]. The oral route for JAK inhibitors facilitates faster onset of action but is associated with a distinct adverse event profile, including infections and acne [113]. This underscores the importance of tailoring the choice of inhibitor class not only to disease severity but also to patient preference regarding administration frequency and tolerance of specific adverse events.
Androgen Receptor Pathway Inhibitors in Prostate Cancer
In metastatic hormone-sensitive prostate cancer (mHSPC), androgen receptor pathway inhibitors (ARPIs) demonstrate how dosing schedules and treatment duration can vary and impact clinical outcomes.
Table 3: Dosing and Early Response of Androgen Receptor Pathway Inhibitors
| Drug Name | Standard Dose | Administration Route | Median Medication Duration (Months) | PSA ≤0.2 ng/mL within 12 Weeks |
|---|---|---|---|---|
| Abiraterone Acetate | 1000 mg daily (with prednisone) [16] | Oral [16] | 30.4 [16] | 25.5% [16] |
| Apalutamide | 240 mg daily [16] | Oral [16] | 13.7 [16] | 44.0% [16] |
| Enzalutamide | 160 mg daily [16] | Oral [16] | 14.1 [16] | 55.9% [16] |
All three ARPIs are administered orally and once daily, but real-world data shows significant differences in treatment duration and early response kinetics [16]. Abiraterone acetate was associated with a significantly longer median medication duration, potentially reflecting its use in different patient populations or its tolerability profile [16]. Conversely, apalutamide and enzalutamide achieved superior rates of early deep PSA response (PSA ≤0.2 ng/mL within 12 weeks), indicating potentially faster disease control [16]. This highlights that even within the same drug class and administration route, differences in molecular structure and pharmacokinetics can lead to variations in early response and treatment patterns.
Experimental Protocols for Assessing Dosing and Tolerability
Real-World Observational Study Protocol
Real-world evidence (RWE) studies are crucial for understanding how dosing and tolerability perform outside the strict constraints of randomized controlled trials (RCTs).
Protocol Title: Real-World Comparison of Dosing Schedules, Administration Routes, and Tolerability of Advanced Systemic Therapies.
Methodology Overview: An ambispective (retrospective and prospective), observational, multicenter cohort design [113].
Key Procedures:
- Cohort Identification: Identify patients from hospital electronic medical records (EMRs) who initiated AST within a defined period [113].
- Group Stratification: Divide patients into cohorts based on the inhibitor class (e.g., biologics vs. JAK inhibitors), specific agent, and dosing regimen [113].
- Data Collection:
- Baseline Data: Record demographic information, disease severity scores, and comorbidities to ensure cohort comparability [113] [16].
- Exposure Data: Document the specific drug, administration route, dosing schedule, and any dose modifications or interruptions [16].
- Outcome Data:
- Effectiveness: Collect clinical severity scores at predefined intervals (e.g., 16, 24, and 52 weeks) to assess response dynamics [113].
- Tolerability: Systematically record all adverse events (AEs), serious adverse events (SAEs), and their type (e.g., infections, ocular symptoms, acne) [113] [114] [115].
- Persistence: Calculate drug survival (time to treatment discontinuation) as a composite measure of both efficacy and tolerability [113].
- Statistical Analysis: Employ appropriate statistical models (e.g., Kaplan-Meier for drug survival, multivariate regression to adjust for confounders) to compare outcomes between groups [113] [16].
Network Meta-Analysis (NMA) Protocol
NMA provides indirect comparisons of different treatments across multiple RCTs, which is valuable when head-to-head trials are unavailable.
Protocol Title: Network Meta-Analysis of Dosing and Tolerability of Signaling Pathway Inhibitors.
Methodology Overview: A systematic review and frequentist or Bayesian NMA of RCTs [114] [115].
Key Procedures:
- Systematic Search: Conduct a comprehensive literature search of major electronic databases (e.g., PubMed, Embase, Cochrane Central) for RCTs involving the inhibitors of interest [114] [115].
- Eligibility Screening: Apply PICOS (Population, Intervention, Comparator, Outcomes, Study design) criteria to select relevant studies. Include only RCTs comparing different inhibitors or doses against a control or each other [116].
- Data Extraction: Extract data on study characteristics, patient demographics, interventions (including drug, dose, and administration route), and outcomes (both efficacy and safety endpoints) [114] [115].
- Outcome Measures:
- Statistical Synthesis and Ranking:
- Pool data using a network meta-analysis model.
- Rank treatments for each outcome using metrics like P-scores or SUCRA (Surface Under the Cumulative Ranking Curve) values. A higher SUCRA value indicates a better ranking for efficacy or a lower ranking for adverse events [115].
Signaling Pathways and Experimental Workflows
Key Signaling Pathways Targeted by Inhibitors
The following diagram illustrates the primary signaling pathways discussed in this guide, highlighting the molecular targets of different inhibitor classes.
Experimental Workflow for Comparative Effectiveness Research
This diagram outlines the core methodology for generating real-world evidence on dosing and tolerability, as described in the observational study protocol.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Tools for Pathway Inhibitor Research
| Research Tool | Primary Function | Application Context |
|---|---|---|
| Validated Clinical Severity Scores (e.g., EASI, SALT) | Quantify disease severity and treatment response in a standardized manner. | Essential for assessing efficacy outcomes in both clinical trials and real-world studies [113] [115]. |
| Adverse Event (AE) and Serious AE (SAE) Coding Systems (e.g., MedDRA) | Systematically categorize and report tolerability issues. | Critical for uniform safety reporting across studies to compare AE profiles of different inhibitors [113] [114]. |
| Electronic Medical Record (EMR) Data Extraction Frameworks | Facilitate structured, high-volume data collection from routine clinical practice. | Foundation for real-world evidence studies on dosing patterns, persistence, and comparative tolerability [113] [16]. |
Bayesian Network Meta-Analysis Software (e.g., R gemtc, JAGS) |
Enable indirect comparison of multiple treatments using integrated RCT data. | Used to rank different inhibitors and doses based on efficacy and safety when head-to-head trials are absent [115]. |
| Cox Proportional Hazards Models | Analyze time-to-event outcomes (e.g., treatment persistence, survival). | Key statistical tool for identifying factors influencing long-term tolerability and drug survival [16]. |
The optimization of dosing schedules and administration routes is a critical determinant in the successful clinical application of signaling pathway inhibitors. Evidence synthesized from recent studies indicates that these factors profoundly influence not only the kinetics of treatment response but also the distinct tolerability profiles that guide therapeutic personalization. The choice between a daily oral JAK inhibitor with rapid onset and a biweekly subcutaneous biologic with longer persistence exemplifies the complex risk-benefit analysis required in modern therapy [113]. Furthermore, even within the same class and administration route, variations in dosing and early response kinetics can signal differences in the therapeutic window [16].
Future research should prioritize head-to-head trials that directly compare dosing regimens and further develop topical or targeted delivery systems to maximize efficacy while minimizing systemic exposure. By systematically integrating real-world evidence and advanced statistical analyses, researchers and drug developers can continue to refine these parameters, ultimately leading to safer, more effective, and more tolerable targeted therapies for patients.
Blood-Brain Barrier Penetration and CNS Delivery Challenges
The blood-brain barrier (BBB) represents one of the most significant challenges in central nervous system (CNS) drug development, excluding more than 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics from entering the brain [117] [118]. This highly selective semi-permeable membrane maintains CNS homeostasis by protecting the brain from toxins and pathogens while regulating the transport of essential nutrients [117] [118]. For researchers developing signaling pathway inhibitors, the BBB presents a formidable obstacle that must be systematically addressed to achieve therapeutic relevance in CNS disorders. The global health crisis of neurodegenerative diseases is worsening with population aging, with projections indicating dementia cases will triple by 2050, creating an urgent need for effective CNS therapeutics [119]. Understanding BBB structure and function is therefore critical for designing effective drug delivery strategies for neurological disorders.
The BBB's protective function stems from its multicellular structure, which includes brain microvascular endothelial cells (BMECs) connected by tight junctions, surrounded by pericytes, and enveloped by astrocytic end-feet [120] [118] [121]. Unlike peripheral endothelial cells, BMECs exhibit specialized characteristics including minimal pinocytosis, absence of fenestrations, and elevated mitochondrial content to support energy-dependent transport processes [120] [118]. These features collectively contribute to the barrier's high transendothelial electrical resistance (TEER), which severely restricts paracellular diffusion [118] [121]. Additionally, ATP-binding cassette (ABC) transporters such as P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP) actively efflux xenobiotics back into the bloodstream, further limiting brain exposure to therapeutic compounds [121] [122].
Table: Key Cellular Components of the Blood-Brain Barrier
| Component | Function | Clinical Significance |
|---|---|---|
| Brain Microvascular Endothelial Cells (BMECs) | Form the core barrier through tight junctions; express transporters and receptors | Primary determinant of BBB permeability; target for drug delivery systems |
| Tight Junctions | Seal paracellular space via claudins, occludin, ZO-1 | Restrict paracellular diffusion of most therapeutics |
| Pericytes | Regulate BBB development, capillary blood flow, and clearance | Pericyte deficiency increases BBB permeability |
| Astrocytes | Form end-feet that cover BMECs; regulate transporter expression | Influence neurovascular coupling and barrier function |
| Basement Membrane | Provides structural support; anchors BBB cells | Altered composition affects BBB integrity in disease |
Comparative Analysis of BBB Penetration Strategies
Passive Diffusion and Physicochemical Optimization
The simplest approach to BBB penetration relies on passive diffusion of small, lipophilic molecules. This non-saturable process depends on molecular weight (<400-600 Da), lipophilicity (LogP>2), limited hydrogen bonding capacity (<6 bonds), and polar surface area (<60-70 Ų) [117] [118]. While increasing lipophilicity can enhance BBB penetration, this strategy often compromises specificity and increases peripheral toxicity due to accumulation in non-target tissues [118]. Furthermore, efflux transporters recognize and actively remove many lipophilic compounds, negating the benefits of this approach [118] [122]. For signaling pathway inhibitors, which typically target intracellular kinases, passive diffusion alone is often insufficient to achieve therapeutic concentrations in the CNS.
Active Transport Mechanisms
Receptor-mediated transcytosis (RMT) represents the most promising approach for targeted CNS delivery of biologics and nanoparticle systems [123] [119] [121]. This pathway hijacks endogenous receptor systems to shuttle therapeutics across the BBB. Key receptors exploited for RMT include transferrin receptor (TfR), insulin receptor (IR), low-density lipoprotein receptor-related proteins (LRP1/2), and lactoferrin receptor (LfR) [123] [121]. Antibodies, peptides, or endogenous ligands conjugated to drug carriers facilitate brain-specific delivery through these pathways. Similarly, carrier-mediated transport (CMT) utilizes nutrient transporters such as glucose transporter 1 (GLUT1) and L-type amino acid transporter 1 (LAT1) to transport structurally similar drugs [117] [118].
Adsorptive-mediated transcytosis (AMT) represents another active transport mechanism that relies on electrostatic interactions between cationic charges on therapeutics and the negatively charged glycocalyx of BMECs [117] [124]. While less specific than RMT, AMT can accommodate a wider range of cargo sizes and does not require specific receptor binding.
Table: Comparison of BBB Penetration Strategies for Signaling Pathway Inhibitors
| Strategy | Mechanism | Advantages | Limitations | Therapeutic Examples |
|---|---|---|---|---|
| Passive Diffusion | Concentration-driven movement of lipophilic molecules | Simple; non-saturable; no carrier required | Limited to small molecules; susceptibility to efflux | Crizotinib analogs [118] |
| Receptor-Mediated Transcytosis (RMT) | Ligand-receptor binding and vesicular transport | High specificity; suitable for biologics and nanoparticles | Potential receptor competition; immunogenicity | Transferrin-modified liposomes [123] |
| Carrier-Mediated Transport (CMT) | Exploitation of nutrient transporters | Efficient for small molecule analogs | Structural constraints; competition with endogenous substrates | LAT1-targeting prodrugs [117] |
| Adsorptive-Mediated Transcytosis (AMT) | Electrostatic interactions with cell surface | Broad applicability; no specific receptor needed | Lower specificity; potential cytotoxicity | Cationic cell-penetrating peptides [124] |
| Nanoparticle-Based Delivery | Multiple mechanisms depending on surface functionalization | Multifunctionality; controlled release | Complex manufacturing; potential toxicity concerns | Lactoferrin-functionalized NPs [123] [124] |
| Physical BBB Disruption | Temporary opening of tight junctions | Immediate access for various therapeutics | Invasive; risk of neurotoxicity | Focused ultrasound with microbubbles [119] |
Emerging and Alternative Approaches
Recent advances in nanotechnology have revolutionized CNS drug delivery through the development of multifunctional systems that combine targeting, therapeutic, and diagnostic capabilities [123] [124] [122]. Surface-functionalized nanoparticles can be engineered with specific ligands to engage RMT pathways while incorporating controlled release properties and stealth characteristics to evade immune recognition [124]. Physical disruption techniques such as focused ultrasound with microbubbles create temporary, reversible openings in the BBB under image guidance [119]. While this approach offers immediate access for therapeutics, it carries risks of neuroinflammation and requires specialized equipment. Alternative administration routes, particularly intranasal delivery, bypass the BBB entirely by utilizing olfactory and trigeminal nerve pathways to deliver drugs directly to the CNS [118] [122].
Experimental Models for Evaluating BBB Penetration
In Vitro BBB Models
Traditional two-dimensional (2D) in vitro models utilizing BMEC monolayers grown on transwell filters provide a cost-effective platform for initial permeability screening [121]. These systems generate quantifiable parameters such as transendothelial electrical resistance (TEER) and apparent permeability (Papp) coefficients, enabling high-throughput assessment of BBB penetration [121]. However, their simplified architecture fails to recapitulate the complex multicellular interactions, hemodynamic forces, and three-dimensional geometry of the neurovascular unit, limiting their predictive value [121].
Advanced three-dimensional (3D) in vitro models address these limitations through hydrogel-based systems, microfluidic organs-on-chips, spheroids, and organoids that better mimic the native BBB microenvironment [121]. These systems incorporate fluid shear stress, co-culture with pericytes and astrocytes, and relevant extracellular matrix composition to promote BBB phenotype expression [120] [121]. Microfluidic platforms specifically apply physiological shear stress (estimated at 1-2 Pa in human brain capillaries), which enhances tight junction formation and transporter expression [120]. While more complex and resource-intensive, these advanced models provide superior predictive capability for CNS penetration assessment.
In Vivo and Imaging Approaches
In vivo evaluation remains essential for comprehensive assessment of BBB penetration and distribution. Conventional methods involve measuring brain-to-plasma ratio (Kp) following systemic administration, with Kp > 0.3 generally indicating favorable brain exposure [125]. However, this approach fails to distinguish between vascularly sequestered and parenchymally distributed drug, potentially overestimating therapeutic relevance.
Advanced neuroimaging techniques provide non-invasive, spatially resolved assessment of BBB penetration and target engagement. Dynamic contrast-enhanced magnetic resonance imaging (DCE-MRI) quantifies BBB permeability through kinetic analysis of contrast agent distribution [125]. Translocator protein positron emission tomography (TSPO-PET) visualizes neuroinflammation, a key feature of BBB dysfunction in neurodegenerative diseases [125]. These methodologies enable longitudinal assessment in the same subject, reducing inter-individual variability and accelerating therapeutic development.
Table: Experimental Methods for Assessing BBB Penetration
| Method | Key Parameters | Applications | Advantages | Limitations |
|---|---|---|---|---|
| 2D Transwell Assay | TEER, Papp | High-throughput screening; mechanism studies | Cost-effective; reproducible | Limited physiological relevance |
| 3D Microfluidic Models | Permeability, receptor expression | Targeted delivery validation; disease modeling | Incorporates shear stress; multicellular | Technical complexity; low-throughput |
| In Vivo Brain Distribution | Kp (brain:plasma ratio) | Preliminary in vivo efficacy | Whole-system assessment | Doesn't distinguish vascular vs. parenchymal drug |
| DCE-MRI | Permeability surface area product | BBB integrity assessment; treatment monitoring | Non-invasive; spatially resolved | Indirect measurement; limited molecular specificity |
| TSPO-PET | Neuroinflammation; glial activation | Disease progression; therapeutic response | Molecular specificity; quantitative | Affected by TSPO polymorphism |
Research Reagent Solutions for BBB Studies
The following research reagents and materials represent essential tools for investigating BBB penetration and developing enhanced CNS delivery strategies:
Primary Human Brain Microvascular Endothelial Cells (HBMECs): Provide the most physiologically relevant in vitro BBB model when cultured under appropriate conditions [121]. Critical for establishing transwell permeability assays and more complex 3D models.
Tight Junction Markers (Claudin-5, Occludin, ZO-1 Antibodies): Essential for evaluating BBB integrity and assessing the impact of penetration enhancers or disease states on barrier function [118] [121]. Used in immunohistochemistry, Western blot, and live-cell imaging.
ABC Transporter Substrates and Inhibitors: Tools for evaluating efflux susceptibility, including P-gp substrates (digoxin, rhodamine 123) and inhibitors (verapamil, elacridar) [118] [122]. Critical for understanding contribution of active efflux to poor CNS exposure.
Receptor-Targeting Ligands: Transferrin, lactoferrin, angiopep-2, and RVG peptides for functionalizing nanocarriers to exploit RMT pathways [123] [121] [124]. Enable targeted delivery while maintaining BBB integrity.
TEER Measurement Systems: Electrode systems for quantifying transendothelial electrical resistance, a key indicator of tight junction integrity in BBB models [121]. Higher TEER values (>150 Ω×cm²) correlate with better barrier function.
BBB Penetration Screening Kits: Commercial systems (e.g., PAMPA-BBB) that predict passive permeability during early drug discovery [122]. Enable high-throughput screening of compound libraries.
Cytokines and Inflammatory Mediators: TNF-α, IL-1β, and IL-6 for modeling neuroinflammatory conditions that alter BBB permeability [125] [120]. Essential for disease-relevant barrier models.
Nanoparticle Formulation Components: Biocompatible polymers (PLGA, PLA), lipids, and surface modification reagents for constructing brain-targeted delivery systems [123] [124] [122].
The development of effective CNS therapeutics requires sophisticated strategies to overcome the formidable challenge of BBB penetration. For signaling pathway inhibitors, successful brain delivery necessitates careful consideration of molecular properties, transporter susceptibility, and potentially advanced delivery technologies. The comparative analysis presented herein demonstrates that no single approach universally solves the BBB challenge, but rather a tailored strategy based on the specific therapeutic candidate and target pathology is required.
Emerging technologies including multivalent nanocarriers, focused ultrasound, and intranasal delivery show significant promise for enhancing CNS exposure of therapeutics [119] [126] [122]. The integration of artificial intelligence and computational modeling approaches accelerates the rational design of BBB-penetrant therapeutics and delivery systems [123] [126]. Furthermore, advanced 3D in vitro models that better recapitulate the human BBB provide more predictive screening platforms while reducing animal studies [121].
For researchers focusing on signaling pathway inhibitors, the most promising path forward involves early integration of BBB penetration assessment in the drug discovery pipeline, application of targeted delivery strategies for problematic compounds, and utilization of physiologically relevant models that can accurately predict human CNS exposure. As our understanding of BBB biology and drug delivery mechanisms continues to advance, so too will our ability to develop effective therapeutics for neurodegenerative diseases, brain tumors, and other CNS disorders.
Pharmacokinetic (PK) optimization is a critical discipline in modern drug development, bridging the gap between in vitro pharmacological activity and in vivo therapeutic efficacy. The process focuses on enhancing key parameters including bioavailability and tissue distribution to ensure drugs reach their intended sites of action at sufficient concentrations and for adequate duration. For signaling pathway inhibitors, whose targets are often intracellular and tissue-specific, precise PK optimization is particularly crucial for translating mechanistic potency into clinical success. This guide compares current strategies and experimental approaches for optimizing these essential pharmacokinetic properties, providing researchers with a framework for evaluating and improving drug candidates.
Core Concepts in PK Optimization
Bioavailability refers to the fraction of an administered dose that reaches systemic circulation unchanged. It is influenced by factors such as solubility, permeability, and first-pass metabolism. Tissue distribution describes the reversible transfer of a drug from systemic circulation to various tissues and organs, determined by properties like lipophilicity, plasma protein binding, and active transport mechanisms. For signaling pathway inhibitors—whether targeting JAK-STAT, MAPK, PI3K, or other pathways—optimal tissue distribution is especially critical as it determines drug exposure at the precise cellular and molecular site of action [127].
The following diagram illustrates the key interrelationships between drug properties, optimization strategies, and the resulting pharmacokinetic profiles:
Comparative Analysis of Optimization Strategies
Structural Modification of Lead Compounds
Structural modification involves altering a compound's molecular structure to improve its pharmacokinetic properties while maintaining target affinity.
Case Study: JAK3 Inhibitors Researchers optimized the JAK3 inhibitor FM-381, which initially showed poor oral bioavailability (10.4%) and short elimination half-life (23 minutes). Through systematic structural modifications to stabilize metabolically vulnerable side groups, they developed derivatives with improved metabolic stability and tissue exposure. The most significant improvement came from conjugating the inhibitor to macrolide scaffolds, which enhanced distribution to immune cells and inflamed tissues—key target sites for JAK3 inhibitors [127].
Case Study: Matrine Derivatives The matrine derivative MASM demonstrated significantly improved bioavailability (44.50%) compared to its parent compound matrine (18.5%). Structural modifications also altered its tissue distribution profile, with highest concentrations found in liver, kidney, and spleen tissues—potentially advantageous for treating liver diseases and inflammation [128].
Formulation Technologies and Advanced Delivery Systems
Formulation strategies can dramatically improve bioavailability without altering the active compound's chemical structure.
Case Study: Sporoderm-Removed Ganoderma Lucidum Spores The sporoderm-removed Ganoderma lucidum spore powder (RGLSP) showed significantly enhanced bioavailability of triterpenoids compared to sporoderm-broken preparations. This formulation approach facilitated rapid absorption (Tmax: 0.25-2.33 h) and extensive distribution to major organs including liver, lung, spleen, kidney, and heart [129].
Case Study: Chitooligosaccharides (COS) Despite promising pharmacological activities, chitobiose and chitotriose exhibit extremely low oral bioavailability (0.32%-0.52%). Research continues to explore formulation strategies including nanoparticle systems and combination approaches to overcome the absorption barriers limiting their clinical translation [130].
Carrier-Mediated Tissue Targeting
Carrier systems can direct drugs to specific tissues or cell types, enhancing therapeutic efficacy while reducing systemic exposure.
Case Study: Inflammation-Targeted JAK3 Inhibitors Conjugation of JAK3 inhibitors to azalide macrolides (e.g., azithromycin) leveraged the natural tissue-targeting properties of these carriers. The resulting conjugates showed preferential accumulation in inflamed tissues and immune cells, with long tissue half-lives and high exposure to activated immune cells—the intended site of action for autoimmune disease treatments [127].
Table 1: Comparison of Pharmacokinetic Optimization Strategies
| Strategy | Mechanism of Action | Key Parameters Improved | Representative Examples | Experimental Evidence |
|---|---|---|---|---|
| Structural Modification | Altering molecular structure to enhance stability & permeability | Bioavailability, metabolic stability, tissue partitioning | MASM (Matrine derivative), JAK3 inhibitor derivatives | MASM bioavailability increased from 18.5% to 44.5% [128] |
| Formulation Technology | Overcoming physicochemical barriers to absorption | Solubility, dissolution rate, permeability | Sporoderm-removed Ganoderma spores, nanoparticle formulations | RGLSP triterpenoids achieved Tmax 0.25-2.33 h [129] |
| Carrier-Mediated Delivery | Exploiting natural distribution pathways of carrier molecules | Tissue-specific distribution, cellular uptake | Macrolide-conjugated JAK3 inhibitors | Enhanced distribution to inflamed tissue and immune cells [127] |
| Prodrug Approach | Chemical derivatives converted to active form after administration | Absorption, first-pass metabolism, targeting | 8-acetamino-isocorydine (AICD) | Absolute bioavailability of 76.5% achieved [131] |
Experimental Protocols for PK Optimization
Protocol for Tissue Distribution Studies Using LC-MS/MS
Objective: Quantify drug and metabolite concentrations in biological matrices to characterize tissue distribution profiles.
Materials:
- UPLC-MRM-MS system or validated LC-MS/MS method
- Quality control samples (LLOQ, LQC, MQC, HQC)
- Tissue homogenization equipment
- Isotope-labeled internal standards
- ACQUITY UPLC BEH amide column or equivalent [129] [132]
Method:
- Sample Collection: Administer test compound to animal models (typically rats or mice). At predetermined timepoints, euthanize animals and perfuse with saline via cardiac perfusion to remove blood from tissues.
- Tissue Processing: Precisely dissect target tissues (liver, kidney, spleen, lung, heart, brain regions). Weigh tissues and homogenize in PBS (0.1 M, pH 7.4) at 4°C using an automated tissue homogenizer. Prepare homogenates at 0.2 g/mL final concentration [132].
- Sample Preparation: Mix calibration standards, quality control samples, or test samples with appropriate internal standard working solution. Precipitate proteins and extract analytes using appropriate solvents (e.g., acetonitrile) [132].
- UPLC-MS/MS Analysis:
- Column: ACQUITY UPLC BEH amide (100 mm × 2.1 mm, 1.7 µm)
- Mobile Phase: Gradient of 0.1% ammoniacal aqueous solution and 0.1% ammonia in acetonitrile
- Flow Rate: 0.2 mL/min with 2 µL injection volume
- Detection: Positive ionization mode with t-SIM for quantification [130]
- Data Analysis: Calculate tissue concentrations using calibration curves with weighted linear regression. Apply appropriate pharmacokinetic models to determine distribution parameters.
Protocol for Bioavailability Assessment
Objective: Determine absolute bioavailability by comparing exposure after extravascular and intravenous administration.
Method:
- Study Design: Use crossover or parallel group design with at least two administration routes (typically oral and intravenous).
- Dosing and Sampling: Administer test compound orally and intravenously to separate animal groups. Collect serial blood samples at appropriate timepoints (e.g., 0, 0.083, 0.25, 0.5, 1, 2, 4, 6, 8, 12, 24, 36, 48, 72 h) into polypropylene tubes containing Kâ‚‚EDTA [132].
- Sample Processing: Centrifuge blood samples at 3000 × g for 20 min at 4°C. Collect plasma supernatant for analysis.
- Bioanalytical Quantification: Determine plasma concentrations using validated LC-MS/MS methods meeting FDA bioanalytical guidelines [129].
- Calculation: Calculate absolute bioavailability using the formula: F = (AUCₚₒ × Dᵢᵥ)/(AUCᵢᵥ × Dₚₒ) × 100%, where AUC is area under the concentration-time curve and D is dose.
Table 2: Key Pharmacokinetic Parameters and Their Significance in Optimization
| Parameter | Definition | Optimization Target | Experimental Measurement |
|---|---|---|---|
| Bioavailability (F) | Fraction of dose reaching systemic circulation | Maximize for oral drugs | Compare AUC after extravascular and IV administration [131] |
| Tmax | Time to reach maximum concentration | Optimal based on therapeutic goal | Direct observation from concentration-time profile [129] |
| Cmax | Maximum plasma concentration | Balance efficacy and toxicity | Direct observation from concentration-time profile [129] |
| AUC | Area under concentration-time curve | Maximize within therapeutic window | Linear/log trapezoidal method [129] |
| Volume of Distribution (Vd) | Apparent volume into which drug distributes | Tissue-specific targeting | Dose/AUC × elimination rate constant [132] |
| Elimination Half-life (t½) | Time for concentration to reduce by half | Optimal dosing frequency | 0.693/elimination rate constant [132] |
| Tissue-Plasma Ratio | Ratio of tissue to plasma concentration | Tissue targeting efficiency | Direct measurement in tissue and plasma at equilibrium [128] |
Advanced Methodologies in PK Optimization
Physiologically-Based Pharmacokinetic (PBPK) Modeling
PBPK modeling represents a powerful "bottom-up" approach that integrates drug-specific properties with organism-specific physiological parameters to predict pharmacokinetic profiles [133].
Application in Lead Optimization:
- Predicts human PK from preclinical data
- Mechanistically predicts drug-drug interactions (DDIs)
- Enables formulation simulation for oral and modified-release drugs
- Extends drug knowledge to pediatric and special populations via virtual simulations
Workflow:
- Model Construction: Define anatomical compartments representing tissues and organs
- Parameter Integration: Incorporate species-specific physiological parameters and drug-specific properties
- Model Calibration: Adjust using available in vivo PK data
- Validation: Employ independent datasets not used in model development
- Simulation: Predict concentration-time profiles under various dosing regimens [133]
In Silico Trials and AI-Driven Optimization
Computer simulations and virtual models are increasingly used to forecast drug effectiveness and pharmacokinetic parameters, reducing the need for extensive animal testing [134].
Advantages:
- Saving time and costs compared to traditional trials
- Increased personalization through modeling of genetic differences
- More accurate modeling leveraging AI and machine learning
- Enhanced sustainability and ethics by reducing animal testing [134]
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagents for Pharmacokinetic Studies
| Reagent/Solution | Function | Application Examples |
|---|---|---|
| UPLC-MRM-MS System | High-sensitivity quantification of analytes in biological matrices | Simultaneous quantification of 12 triterpenoids in rat plasma and tissues [129] |
| Stable Isotope-Labeled Standards | Internal standards for mass spectrometry quantification | Deuterium-labeled MASM for metabolite identification [128] |
| ACQUITY UPLC BEH Amide Column | Hydrophilic interaction chromatography for polar compounds | Separation of chitobiose and chitotriose in biological samples [130] |
| PBPK Software (Simcyp, GastroPlus) | Mechanistic modeling of drug disposition | Predicting human PK from preclinical data, DDI assessment [133] |
| Organ-on-a-Chip Technologies | Human-relevant models of disease for preclinical testing | Improving predictive power of preclinical testing [135] |
Pharmacokinetic optimization represents a critical frontier in the development of effective signaling pathway inhibitors. As evidenced by the comparative data presented, success requires integrated application of multiple strategies—from structural chemistry and formulation science to advanced modeling and targeted delivery approaches. The experimental protocols and methodologies outlined provide researchers with a framework for systematically evaluating and improving the bioavailability and tissue distribution of drug candidates. As the field advances, the integration of PBPK modeling, AI-driven approaches, and sophisticated tissue-targeting strategies will continue to enhance our ability to optimize pharmacokinetic profiles, ultimately accelerating the development of more effective and targeted therapies for complex diseases.
Comparative Efficacy Analysis and Validation Frameworks for Pathway Inhibitors
The development of targeted therapies has revolutionized cancer treatment, with inhibitors of key signaling pathways representing a cornerstone of modern oncology. The phosphoinositide 3-kinase (PI3K)/AKT/mammalian target of rapamycin (MTOR) pathway, the mitogen-activated protein kinase (MAPK) pathway, and the signal transducer and activator of transcription (STAT) pathway are among the most critically investigated signaling networks in cancer biology. Understanding the comparative efficacy of inhibitors targeting these pathways is essential for optimizing therapeutic strategies. This guide provides a systematic comparison of efficacy and safety profiles across different inhibitor classes based on recent clinical trial data and meta-analyses, offering evidence-based insights for researchers, scientists, and drug development professionals.
Quantitative Efficacy and Safety Profiles Across Inhibitor Classes
PI3K and AKT Inhibitors
Table 1: Efficacy and Safety of PI3K and AKT Inhibitors in Cancer Treatment
| Inhibitor | Target | Cancer Type | Efficacy Outcomes | Common Adverse Events |
|---|---|---|---|---|
| Capivasertib | AKT | Solid tumors (e.g., Breast Cancer) | Effective in PIK3CA-mutant cancers; Improved outcomes in breast cancer [136] | Hyperglycemia, hypertension, pneumonitis [136] |
| Ipatasertib | AKT | Solid tumors | Clinical benefit in specific cancer subtypes [136] | Similar class-related toxicity profile [136] |
| Idelalisib | PI3K (δ isoform) | Hematologic cancers (CLL) | Effective for chronic lymphocytic leukemia [136] | Immune-related toxicities, hepatotoxicity [136] |
| Alpelisib | PI3K (α isoform) | PIK3CA-mutant solid tumors | Approved for PIK3CA-mutant breast cancer [64] | Hyperglycemia, rash, gastrointestinal intolerance [64] |
| Copanlisib | Pan-PI3K (α/δ) | Solid tumors, Lymphoma | Activity in PIK3CA-mutant colorectal cancer models [64] | Hypertension, hyperglycemia [136] |
A 2024 systematic review and network meta-analysis encompassing 34 studies and 6,710 patients provided robust head-to-head comparisons of PI3K/AKT inhibitors [136]. The analysis revealed that AKT inhibitor capivasertib demonstrated optimal efficacy for solid tumors such as breast cancer, while PI3K inhibitor idelalisib showed superior outcomes for hematologic cancers like chronic lymphocytic leukemia (CLL). Importantly, the study highlighted that PI3K/AKT inhibitors are particularly effective in patients with specific genetic mutations (e.g., PIK3CA mutations), underscoring the importance of biomarker-driven patient selection [136].
Safety profiles emerged as a significant differentiator, with PI3K/AKT inhibitors demonstrating substantial toxicity concerns including hyperglycemia, hypertension, and severe pneumonitis. These adverse effects have limited their widespread use and necessitated careful risk-benefit assessment in clinical decision-making [136].
MEK Inhibitors in Erdheim-Chester Disease
Table 2: MEK Inhibitor Efficacy by Mutation Status in Erdheim-Chester Disease
| Mutation Status | Patient Count | Objective Response Rate | Stable Disease | Disease Progression |
|---|---|---|---|---|
| MAPK-ERK Pathway Mutations (BRAF, MAP2K1, KRAS, NRAS) | 64 | 61% (39 patients) | 30% (19 patients) | 9% (6 patients) |
| No Identifiable Mutations (Wild-Type) | 16 | 63% (10 patients) | 31% (5 patients) | 6% (1 patient) |
Recent real-world evidence from a multicenter cohort of 80 Erdheim-Chester disease (ECD) patients demonstrated that MEK inhibitors are effective regardless of MAPK-ERK pathway mutation status [137]. The study reported strikingly similar response rates between patients with identifiable mutations (61%) and those without (63%), supporting the use of MEK inhibitors as a reasonable therapeutic approach for ECD patients regardless of mutational status. This finding contrasts with BRAF inhibitors, which are predominantly effective only in patients harboring the BRAF V600E mutation [137].
Emerging STAT Inhibitors
The STAT inhibitor landscape represents an emerging field with promising therapeutic potential. Current pipeline analysis reveals that over 18 companies are developing 22 STAT inhibitor drugs at various stages of development [138]. Notable candidates include:
- TTI-101 (Tvardi Therapeutics): A small molecule STAT3 inhibitor currently in Phase II trials for breast cancer, idiopathic pulmonary fibrosis, and liver cancer [138]
- KT-621 (Kymera Therapeutics): An oral STAT6 degrader showing potential in atopic dermatitis [138]
- VVD-850 (Vividion Therapeutics): A STAT3 inhibitor under investigation for tumors [138]
These agents primarily target dysregulated STAT pathways, particularly STAT3 and STAT5, which play crucial roles in cancers and inflammatory conditions. The field is capitalizing on potential biomarkers and precision medicine approaches to optimize therapeutic development [138].
Experimental Protocols for Inhibitor Efficacy Assessment
Enzyme Inhibition Analysis Protocol
Detailed Methodology for Inhibition Constant (Kic and Kiu) Estimation:
IC50 Determination: Estimate half-maximal inhibitory concentration (IC50) using % control activity data across various inhibitor concentrations (IT) with a single substrate concentration (ST), typically at the KM value [139].
Experimental Design:
- Substrate concentrations: 0.2KM, KM, and 5KM
- Inhibitor concentrations: 0, 1/3 IC50, IC50, and 3IC50 [139]
Velocity Measurement: Measure initial velocity (V0) of product formation for each combination of substrate and inhibitor concentrations using standardized assay conditions [139].
Data Analysis: Fit the mixed inhibition model to the velocity data using the equation: V0 = (Vmax × ST) / [KM(1 + IT/Kic) + ST(1 + IT/Kiu)] where Vmax is maximal velocity, KM is Michaelis-Menten constant, Kic is competitive inhibition constant, and Kiu is uncompetitive inhibition constant [139].
Optimized Approach (50-BOA): Recent evidence suggests that incorporating the relationship between IC50 and inhibition constants allows precise estimation with a single inhibitor concentration greater than IC50, substantially reducing experimental requirements by >75% while maintaining accuracy [139].
Gene Expression Profiling for Efficacy Prediction
Advanced methodologies for predicting therapeutic efficacy utilize high-content statistical categorization of gene expression profiles:
Cell Culture and Treatment: Primary human neuronal precursor cells are cultured and differentiated, then treated with pharmaceutical compounds at clinically relevant concentrations for 24 hours [140].
RNA Processing: Extract total RNA from treated cells and prepare biotin-labeled cDNA using poly(T) primers [140].
Microarray Hybridization: Hybridize samples to oligonucleotide microarrays containing approximately 11,000 probes, followed by staining with fluorescent detection agents [140].
Data Acquisition and Analysis: Scan arrays and analyze images to quantify gene expression. Pre-filter data to include genes detectable at least 3× background after signal normalization [140].
Statistical Classification: Apply supervised classification algorithms (classification tree and random forest) to analyze microarray data and derive "efficacy profiles" of biomarker gene expression that correlate with drug mechanisms [140].
This approach has demonstrated 88.9% accuracy in classifying drugs into correct therapeutic categories based solely on gene expression signatures induced in vitro [140].
Signaling Pathway Diagrams
PI3K/AKT/MTOR Signaling Pathway
PI3K/AKT/mTOR Signaling Cascade. This pathway illustrates how extracellular signals activate PI3K, which converts PIP2 to PIP3, recruiting PDK1 and AKT to the membrane. AKT is fully activated through phosphorylation by PDK1 and mTORC2, subsequently activating mTORC1 to promote cell growth and survival. PTEN acts as a critical negative regulator by converting PIP3 back to PIP2 [64] [141].
Enzyme Inhibition Experimental Workflow
Enzyme Inhibition Analysis Workflow. This diagram outlines the optimized protocol for estimating inhibition constants. The traditional approach involves determining IC50 followed by multi-concentration testing. The 50-BOA (IC50-Based Optimal Approach) significantly reduces experimental requirements by using a single inhibitor concentration greater than IC50 while maintaining precision [139].
Research Reagent Solutions
Table 3: Essential Research Reagents for Inhibitor Efficacy Studies
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Cell-Based Assay Systems | Primary human neuronal precursor cells; Cancer cell lines (medulloblastoma, ovarian, colorectal) | Preclinical efficacy screening | Assess inhibitor effects on cell proliferation, apoptosis, migration [140] [64] |
| Gene Expression Profiling | CuraChip microarray (11,000 oligonucleotide probes); RNA extraction kits | Mechanism of action studies; Efficacy prediction | Generate gene expression signatures for drug classification [140] |
| PI3K Pathway Inhibitors | Pictilisib (GDC-0941); D-116883; Copanlisib; LY3023414 | Pathway validation; Combination therapy studies | Target PI3K isoforms in mutation-specific contexts [64] |
| Statistical Analysis Tools | "R" statistical software; Classification tree algorithms; Random forest models | Data analysis and efficacy prediction | Classify expression profiles; Predict therapeutic categories [140] |
| Specialized Assay Reagents | Trizol reagent; Biotin-labeling kits; Cy3-conjugated detection buffers | Microarray processing and detection | RNA isolation, cDNA labeling, and signal detection [140] |
The comparative analysis of inhibitor classes reveals distinct efficacy and safety profiles across different cancer types and molecular contexts. PI3K/AKT inhibitors demonstrate mutation-specific efficacy with capivasertib and idelalisib showing optimal performance in solid and hematologic malignancies, respectively. MEK inhibitors exhibit broad efficacy in Erdheim-Chester disease independent of mutation status. Emerging STAT inhibitors represent a promising new therapeutic avenue currently in clinical development. The optimization of enzyme inhibition protocols through approaches like 50-BOA significantly enhances experimental efficiency. These findings underscore the importance of biomarker-driven patient selection and pathway-specific targeting for maximizing therapeutic outcomes while managing toxicity profiles.
The validation of robust biomarkers is fundamental to the advancement of precision oncology, enabling the stratification of patients for targeted therapies. Among the most critical biomarkers in cancer signaling pathways are the loss of the tumor suppressor PTEN and activating mutations in the oncogene PIK3CA, both key regulators of the phosphatidylinositol 3-kinase (PI3K)/AKT/mTOR pathway [142]. This pathway is frequently dysregulated in human cancers and governs essential cellular processes including growth, survival, and metabolism [143]. The comparative effectiveness of signaling pathway inhibitors often hinges on the accurate detection of these molecular alterations. This guide provides a comparative analysis of the clinical performance, validation methodologies, and predictive value of PTEN loss and PIK3CA mutations, offering structured experimental data and protocols to inform research and clinical development.
Biomarker Performance and Clinical Validation Data
The clinical utility of a biomarker is determined by its analytical validity and its proven association with clinical outcomes. The following table summarizes key performance characteristics of PTEN loss and PIK3CA mutations across different cancer types, based on recent clinical studies.
Table 1: Clinical Validation Data for PTEN Loss and PIK3CA Mutations
| Biomarker | Cancer Type | Prevalence | Predictive Value for Adverse Pathology | Assay Method | Key Clinical Association |
|---|---|---|---|---|---|
| PTEN Loss | Prostate Cancer (Gleason 6) | 8% (13/158) [144] | 100% upgrading or NOCD at RP (5/5 with PTEN loss) [144] | IHC [145] | Strong predictor of upgrading and non-organ confined disease (NOCD) [144] |
| PTEN Loss | Prostate Cancer (Gleason 3+4=7) | 27% (70/260) [144] | Significantly more likely to have non-organ confined disease at prostatectomy [144] | IHC [144] | Associated with higher risk in intermediate-risk disease |
| PIK3CA Mutation | Advanced Colorectal Cancer | 19.2% (3,388/17,622 samples) [146] | Associated with advanced-stage disease and higher TMB [146] | ctDNA (NGS) [146] | Higher genomic instability, potential for immunotherapy |
| PIK3CA Mutation | Endometrial Carcinoma | Not Specified | Correlates with improved Overall Survival (OS) [147] | NGS (TCGA) [147] | Protective factor (HR <1), associated with activated immune state |
Abbreviations: NOCD: Non-Organ Confined Disease; RP: Radical Prostatectomy; IHC: Immunohistochemistry; ctDNA: Circulating Tumor DNA; NGS: Next-Generation Sequencing; TMB: Tumor Mutational Burden; HR: Hazard Ratio.
Experimental Protocols for Biomarker Assessment
Analytic Validation of PTEN by Immunohistochemistry (IHC)
Principle: A clinically-grade, automated IHC assay detects PTEN protein loss, which most commonly results from homozygous PTEN gene deletion [145].
Detailed Protocol:
- Sample Preparation: Formalin-fixed, paraffin-embedded (FFPE) tumor tissue sections are cut to a specified thickness (e.g., 4 µm).
- Staining Protocol: Sections are stained using a validated anti-PTEN antibody on an automated IHC platform. Appropriate positive and negative control tissues are included in each run.
- Interpretation and Scoring: PTEN expression is assessed by a pathologist. Intact PTEN expression is defined by the presence of cytoplasmic and nuclear staining in tumor cells. PTEN loss is defined when tumor cells show absent or markedly reduced staining compared to internal positive controls (e.g., stromal cells, benign glands) [145].
- Validation against FISH: The IHC assay is validated against Fluorescence In Situ Hybridization (FISH) for PTEN gene deletion. Performance characteristics are as follows:
- Specificity: 91% for absence of PTEN gene deletion (549/602 tumors with two PTEN gene copies by FISH showed intact PTEN by IHC).
- Sensitivity: 97% for homozygous PTEN deletion (65/67 tumors); 65% for hemizygous PTEN deletion (40/62 tumors) [145].
Detection of PIK3CA Mutations by Circulating Tumor DNA (ctDNA) Analysis
Principle: This non-invasive "liquid biopsy" method sequences cell-free DNA from blood plasma to identify somatic mutations, such as those in PIK3CA, providing a comprehensive view of tumor heterogeneity [146].
Detailed Protocol:
- Sample Collection and Processing: Blood samples are collected from patients into specialized tubes that stabilize cell-free DNA. Plasma is separated through centrifugation.
- DNA Extraction and Sequencing: Cell-free DNA is extracted from plasma. Next-generation sequencing (NGS) is performed on a platform like the Guardant360 assay, which targets a panel of cancer-related genes (e.g., up to 83 genes).
- Bioinformatic Analysis: Sequencing data is processed through a bioinformatics pipeline to identify single nucleotide variants, insertions/deletions, and copy number alterations. PIK3CA mutations are called with high confidence.
- Data Interpretation: Mutations are reported, with a focus on frequent "hotspot" mutations in exons 9 (e.g., E545, E542) and 20 (e.g., H1047) [146]. Concurrent analysis of tumor mutational burden (TMB) and microsatellite instability (MSI) status can also be performed.
Signaling Pathways and Biomarker Interplay
The following diagram illustrates the PI3K/AKT/mTOR signaling pathway, highlighting the roles of PTEN and PIK3CA and the points of inhibition for targeted therapies.
The diagram shows how PIK3CA mutations constitutively activate PI3K, driving excessive downstream signaling [142]. Conversely, PTEN loss fails to dephosphorylate PIP3 back to PIP2, leading to accumulated PIP3 and persistent AKT/mTOR pathway activation [142]. Targeted inhibitors act at specific nodes to suppress this oncogenic signaling.
The Scientist's Toolkit: Essential Research Reagents
Successful biomarker research and validation rely on a suite of reliable reagents and tools. The following table details key solutions used in the featured experiments and the broader field.
Table 2: Research Reagent Solutions for Biomarker Analysis
| Research Reagent | Function / Application | Example Use in Context |
|---|---|---|
| Validated PTEN IHC Antibody | Detection of PTEN protein loss in FFPE tissue sections. | Analytic validation of PTEN as a prognostic biomarker in prostate cancer; scoring is correlated with FISH [145]. |
| ctDNA NGS Assay Kit | Isolation and sequencing of cell-free DNA from plasma to detect somatic mutations. | Profiling PIK3CA mutations in advanced colorectal cancer; enables TMB and MSI analysis [146]. |
| Pathway Activity Modeling Software | Machine learning-based analysis of transcriptomic data to compute pathway activity scores. | Used to predict drug response by simulating the effect of compounds on pathway signatures in patient samples [148]. |
| Functional Representation (FRoGS) | Deep learning model that projects gene signatures onto functional space rather than gene identity. | Enhances compound-target prediction by capturing weak pathway signals that gene-identity methods miss [149]. |
| Reverse-Phase Protein Array (RPPA) | High-throughput immunoassay to measure protein expression and phosphorylation levels. | Used to evaluate expression/activation of 195 proteins in HNSCC cell lines to identify biomarkers of response to PI3K pathway inhibitors [143]. |
The comparative data and methodologies presented herein underscore the validated utility of PTEN loss and PIK3CA mutations as critical biomarkers in oncology. PTEN loss, effectively detected by clinical-grade IHC, is a powerful prognostic indicator for adverse pathology in cancers like prostate cancer [144] [145]. PIK3CA mutations, detectable in tumor tissue or liquid biopsy, are prevalent across carcinomas and are associated with distinct clinical features, including potential for targeted therapy and an altered immune context [147] [146] [142]. The ongoing integration of advanced methodologies, such as functional representation of gene signatures and machine learning, promises to further refine predictive models [148] [149]. The choice of biomarker and detection platform must be guided by the clinical context, available tissue, and the specific therapeutic question, with both biomarkers offering robust tools for advancing personalized cancer treatment.
In the rigorous evaluation of new cancer therapies, particularly signaling pathway inhibitors, oncologists and researchers rely on specific efficacy endpoints to determine treatment benefit. Overall Survival (OS) represents the gold standard endpoint, defined as the time from randomization until death from any cause. Progression-Free Survival (PFS) measures the time from randomization until objective tumor progression or death, while Objective Response Rate (ORR) quantifies the proportion of patients with a predefined reduction in tumor burden. Duration of Response (DOR) has emerged as an increasingly important endpoint, measuring the time from initial response until documented tumor progression.
The relationship between these endpoints becomes particularly complex when evaluating targeted therapies and immuno-oncology agents, which may demonstrate different efficacy patterns compared to traditional chemotherapy. Understanding how these endpoints correlate across different cancer types and therapeutic mechanisms is essential for drug development, regulatory decision-making, and ultimately, improving patient outcomes through more effective treatment strategies.
Comparative Analysis of Endpoints Across Cancer Types and Therapies
Correlation Patterns Between Endpoints
Table 1: Correlation Between Efficacy Endpoints in Immuno-Oncology Trials Based on Meta-Analyses
| Analysis Scope | ORR-PFS Correlation | ORR-OS Correlation | PFS-OS Correlation | Key Findings |
|---|---|---|---|---|
| PD-1 Inhibitors across multiple solid tumors [150] | Significant (HR correlation) | Not significant for medians/gains | Protective effects greater for OS than PFS | Traditional PFS may not fully capture PD-1 inhibitor benefit |
| Immunotherapy regimens (68 trials) [151] | Moderate (R² = 0.503) | Weak (R² = 0.157) | Not reported | ORR predicts PFS better in first-line settings |
| Anti-PD-(L)1 monotherapy (17 trials) [151] | Stronger correlation | Weaker correlation | Not reported | ORR's predictive value declines in later treatment lines |
The relationship between conventional efficacy endpoints varies substantially across different therapeutic modalities. A meta-analysis of PD-1 inhibitors (nivolumab and pembrolizumab) in solid tumors revealed that while hazard ratios for PFS and OS were significantly correlated, there was no significant correlation between median PFS and median OS or between the gains in these medians [150]. This analysis found the protective effects of treatment were greater for OS than for PFS (pooled ratio of HRs: 1.18; 95% CI: 1.06-1.31; P = .002), suggesting that PFS alone may not adequately capture the full survival benefit of PD-1 inhibitors [150].
Across 55 immuno-oncology trials examining various combinations, the correlation between ORR and PFS was moderate (R² = 0.503), indicating ORR can serve as a useful predictor of short-term disease control. However, the correlation between ORR and OS was notably weaker (R² = 0.157), especially in trials evaluating combination therapies [151]. This suggests that ORR alone may not reliably predict long-term survival outcomes in the context of modern cancer therapeutics.
Endpoint Performance Across Cancer Types
Table 2: Efficacy Outcomes by Cancer Type and Therapeutic Approach
| Cancer Type | Therapeutic Approach | ORR | Median PFS | Median OS | Median DOR | Evidence Source |
|---|---|---|---|---|---|---|
| Extensive-Stage Small Cell Lung Cancer | Ifinatamab deruxtecan (2nd line) | 56.3% | 5.6 months | 12.0 months | 7.2 months | Phase 2 Trial [152] |
| Extensive-Stage Small Cell Lung Cancer | Ifinatamab deruxtecan (3rd line+) | 45.7% | 4.9 months | 10.3 months | 4.3 months | Phase 2 Trial [152] |
| PTEN-deficient tumors (preclinical) | ATR/mTOR dual inhibition | N/A | N/A | N/A | N/A | AI-discovered inhibitors [153] |
Recent advances in targeted therapies demonstrate how specific molecular targeting can yield substantial clinical benefits even in aggressive malignancies. For extensive-stage small cell lung cancer (ES-SCLC), the B7-H3 directed antibody-drug conjugate ifinatamab deruxtecan demonstrated a confirmed ORR of 48.2% in previously treated patients, with a median PFS of 4.9 months and median OS of 10.3 months [152]. Notably, in patients receiving this agent as second-line therapy, outcomes were more favorable with an ORR of 56.3%, median PFS of 5.6 months, and median OS of 12.0 months [152].
The line of therapy significantly influences endpoint relationships, with stronger ORR-PFS correlations observed in first-line settings compared to later lines of treatment [151]. This pattern underscores the evolving nature of tumor biology and treatment resistance over the course of the disease continuum, highlighting the need for contextual interpretation of efficacy endpoints based on the treatment setting.
Emerging Endpoints and Methodological Considerations
Duration of Response as an Alternative Endpoint
Recent evidence suggests that Duration of Response (DOR) may provide valuable insights beyond conventional endpoints, particularly for immuno-oncology agents. A simulated modeling study that resampled patients from completed phase 3 trials of immune checkpoint inhibitors found that restricted mean DOR difference correctly estimated a positive OS benefit more frequently than ORR or PFS tests across different sample sizes, significance levels, and censoring levels [154].
When both OS and PFS differed between treatment arms, the power rates for detecting this difference ranged from 79.2% to 98.7% for DOR, compared to 56.3% to 93.2% for PFS and 67.0% to 96.0% for ORR [154]. More notably, in scenarios where OS differed but PFS did not - a pattern sometimes observed with immunotherapies - the power rates were 24.0% to 76.0% for DOR versus only 3.0% to 19.0% for PFS and 10.5% to 38.0% for ORR [154]. These findings suggest that DOR may be a more sensitive predictor of OS benefit in randomized phase 2 trials, potentially facilitating more efficient drug development decisions.
Methodological Challenges in Endpoint Assessment
The assessment of efficacy endpoints in cancer clinical trials faces several methodological challenges:
Response criteria limitations: Traditional RECIST criteria may not adequately capture atypical response patterns associated with immunotherapies, such as pseudoprogression [151]. Modified criteria like iRECIST have been developed to address these limitations.
Crossover effects: In randomized trials, crossover of patients from control to experimental arms can confound OS analysis, potentially diminishing observed treatment effects [150].
Brain metastasis assessment: Conventional response assessment may underestimate activity in patients with central nervous system involvement. In an exploratory analysis of ifinatamab deruxtecan, an intracranial ORR of 46.2% was observed in patients with baseline brain metastases, highlighting the importance of specialized assessment methods [152].
Signaling Pathways and Therapeutic Targeting
Key Pathways in Cancer Progression and Treatment Resistance
The efficacy of cancer therapies is fundamentally linked to their interaction with critical signaling pathways that govern tumor growth, survival, and treatment resistance. Several key pathways have emerged as particularly important therapeutic targets:
The Wnt/β-catenin signaling pathway represents a highly conserved pathway implicated in cancer development through various biological processes including oncogenic transformation, cancer cell proliferation, stemness, metabolism, and immune regulation [155]. Notably, its activation plays a crucial role in drug resistance to chemotherapy, targeted therapy, and immunotherapy [155]. This pathway is regulated by three core protein families: Wnt ligands, frizzled (Fzd) receptors, and TCF/LEF transcription factors, with β-catenin serving as the key nuclear effector [155].
The PI3K/AKT/mTOR pathway represents another critical signaling axis, particularly in PTEN-deficient tumors. PTEN serves as one of the most frequently lost tumor-suppressor genes in human cancer and functions as a key brake on the PI3K/AKT/mTOR signaling pathway that governs cell growth, metabolism, and survival [153]. Its loss promotes unchecked proliferation, genomic instability, therapy resistance, and aggressive tumor progression [153]. PTEN deficiency is particularly prevalent in cancers with a high propensity for CNS spread, including ovarian, lung, breast, and melanoma, where tumor cells rely heavily on mTOR-driven growth and survival [153].
Targeting Resistance Pathways
Novel therapeutic approaches are increasingly focused on overcoming resistance mechanisms by simultaneously targeting multiple pathways. For instance, Rakovina Therapeutics has developed ATR/mTOR dual inhibitors designed to address PTEN-deficient tumors that rely heavily on both ATR-mediated DNA damage response and mTOR-driven survival signaling [153]. These AI-discovered compounds represent an innovative approach to targeting complementary resistance mechanisms, with preclinical data showing meaningful CNS penetration - a key limitation of current clinical ATR inhibitors [153].
Similarly, peptide inhibitors targeting oncogenic pathways like RAS and mTOR have gained attention as promising therapeutic alternatives due to their high selectivity in disrupting protein-protein interactions and ligand binding [156]. Key examples include KRpep-2D, cyclo-CRVLIR, P1_WT, and hSPAR, with some candidates demonstrating promising clinical potential in ongoing trials [156].
Experimental Design and Methodological Framework
Clinical Trial Design Considerations
The assessment of PFS, ORR, and OS requires rigorous clinical trial methodologies with specific design elements:
Blinded Independent Central Review (BICR): Modern trials increasingly implement BICR to minimize bias in progression assessments, particularly in open-label studies [152].
Staggered Accrual and Additional Censoring: Simulation studies incorporate these elements to mimic real-world trial conditions and ensure fair comparisons between different analysis methods [154].
Stratification Factors: Trials typically stratify randomization by key prognostic factors, such as prior lines of therapy, PD-L1 expression status, and presence of specific genetic alterations.
Crossover Provisions: Many contemporary trials allow crossover from control to experimental arms upon progression, which must be accounted for in OS analysis plans.
Statistical Analysis Methods
Table 3: Key Statistical Methods for Endpoint Analysis
| Method Category | Specific Methods | Application Context | Considerations |
|---|---|---|---|
| Time-to-Event Analysis | Kaplan-Meier estimator, Cox proportional hazards models | PFS, OS, DOR | Handles censored data, provides hazard ratios |
| Response Assessment | Logistic regression, RECIST v1.1, iRECIST | ORR, DCR | Accounts for atypical response patterns |
| Correlation Analysis | Pearson correlation, Linear regression on logarithmic scale | Endpoint relationships | Quantifies surrogate utility |
| Simulation Methods | Resampling from completed trials, Additional censoring | Method comparison, Trial design optimization | Models real-world conditions |
Advanced statistical methods are essential for proper evaluation of efficacy endpoints. The correlation between ORR, PFS, and OS is typically evaluated using linear regression models on a logarithmic scale, with calculation of the coefficient of determination (R²) and associated 95% confidence intervals [151]. For time-to-event endpoints, Cox proportional hazards regression models provide hazard ratios that quantify treatment effects, while logistic regression models estimate odds ratios for response endpoints [151].
Simulation approaches have become increasingly valuable for comparing endpoint performance. These methods typically involve resampling patients from completed randomized phase 3 trials and applying additional censoring to mimic staggered accrual, enabling fair comparisons between different analysis methods under controlled conditions [154].
Essential Research Reagents and Tools
Table 4: Key Research Reagents and Experimental Tools
| Reagent/Tool Category | Specific Examples | Primary Research Application | Key Function |
|---|---|---|---|
| Cell Line Models | PTEN-deficient tumor models, Patient-derived organoids | Therapeutic efficacy screening | Recapitulate tumor biology and therapy response |
| Animal Models | SCID mice, Xenograft models | In vivo efficacy assessment | Evaluate tumor growth inhibition and survival |
| Biochemical Assays | Enzymatic inhibition assays, Liver microsomal stability tests | Compound profiling | Assess potency, selectivity, and metabolic stability |
| AI/Computational Platforms | Enki generative AI platform, Deep-Docking platform | Drug discovery and optimization | Design novel compounds with specific properties |
| Genomic Tools | Single-cell RNA sequencing, Multiomics analysis | Mechanism of action studies | Characterize tumor heterogeneity and resistance |
Contemporary cancer therapeutic research relies on increasingly sophisticated research tools. Generative AI platforms like Enki enable the design of novel compounds with specific target profiles, such as CNS-penetrant ATR/mTOR dual inhibitors [153]. Single-cell RNA sequencing technologies have revealed nearly 400 genes with altered expression in dormant cancer cells within bone niches, providing insights into resistance mechanisms [157]. Multiomics analysis further illuminates the genetic and non-genetic mechanisms governing complex cancer phenotypes like dormancy and treatment resistance [157].
Advanced model systems including 3D organoid cultures and patient-derived xenografts better recapitulate the tumor microenvironment and therapeutic response patterns observed in clinical settings, bridging the gap between preclinical discovery and clinical application [158].
The relationship between progression-free survival, overall response rates, and overall survival varies substantially across cancer types and therapeutic modalities. While moderate correlation exists between ORR and PFS, the connection between these intermediate endpoints and overall survival is more variable, particularly in the context of immunotherapies and targeted agents. Emerging endpoints like duration of response show promise as potentially more sensitive predictors of OS benefit in early-phase trials.
The efficacy of signaling pathway inhibitors is fundamentally linked to their ability to overcome resistance mechanisms governed by pathways such as Wnt/β-catenin and PI3K/AKT/mTOR. Novel approaches including dual pathway inhibition and peptide-based therapeutics represent promising strategies for addressing these resistance mechanisms. As the field advances, continued refinement of efficacy endpoints and research methodologies will be essential for accelerating the development of more effective cancer therapies.
The therapeutic index (TI), defined as the ratio between the toxic dose and the therapeutic dose of a drug, serves as a critical measure in oncology drug development, quantifying the balance between efficacy and toxicity. For signaling pathway inhibitors, this balance is particularly crucial, as these targeted agents are designed to interfere with specific molecular pathways driving cancer progression. The evolution from conventional cytotoxic chemotherapy to targeted agents has reshaped the risk-benefit paradigm in cancer treatment, yet optimizing the TI remains a fundamental challenge in drug development [159].
The standard phase I clinical trial paradigm has traditionally focused primarily on establishing the maximum tolerated dose (MTD) based on toxicity endpoints. However, novel therapies—particularly molecularly targeted agents, vaccines, and immunotherapies—often challenge this approach, as they may demonstrate non-monotonic dose-efficacy relationships or limited toxicity that mandates novel designs to identify the biologically optimal dose (BOD) rather than simply the MTD [160]. This paradigm shift necessitates more sophisticated frameworks for TI assessment that simultaneously incorporate both efficacy and toxicity endpoints from early development through post-marketing surveillance.
Methodological Framework for TI Assessment
Clinical Trial Designs for Efficacy-Toxicity Trade-off Analysis
Advanced model-based trial designs have been developed to formally incorporate both efficacy and toxicity outcomes in dose-finding studies. The continual reassessment method (CRM) and its extensions represent a significant methodological advancement over traditional algorithm-based designs like the standard 3+3 design. These model-based adaptive designs allow for more efficient dose selection and have demonstrated better operating characteristics, including a higher proportion of patients treated at or near the optimal dose level [160].
The trivariate CRM (TriCRM) incorporates a trinary ordinal outcome variable encompassing (1) acceptable toxicity without efficacy, (2) acceptable toxicity with efficacy, and (3) severe toxicity. This approach utilizes either proportional odds models or continuation ratio models to estimate the probability of each outcome as a function of dose. For a single agent, the continuation ratio model is specified as:
Where ψ₀, ψâ‚, and ψ₂ represent the probabilities of the three outcomes, x is the dose, and β₠> 0 and β₂ > 0 ensure appropriate monotonicity constraints [160]. These models are estimated within a Bayesian framework with prior distributions reflecting clinical knowledge, updated sequentially as patient outcome data accumulate.
Meta-analytic Approach for Cross-Compound Comparison
A comprehensive meta-analysis of phase 3 randomized controlled trials (RCTs) in solid tumors provides a systematic approach for quantifying the efficacy-toxicity trade-offs across multiple therapeutic classes. This methodology involves:
- Systematic identification of all phase 3 RCTs evaluating new drugs in advanced breast, colorectal, lung, or prostate cancer completed between 2005-2016 (n=143 trials, 88,603 patients) [161]
- Efficacy quantification through extraction of hazard ratios (HRs) for progression-free survival (PFS) and overall survival (OS)
- Toxicity assessment via calculation of odds ratios (ORs) for treatment-related deaths, treatment discontinuation without progression, and grade 3/4 adverse events
- Pooled analysis using random-effects models to account between-study heterogeneity
- Sensitivity analyses to evaluate the impact of trial design elements (blinding, placebo control) on efficacy and toxicity estimates [161]
This methodology provides a robust framework for comparing the therapeutic indices across different drug classes within and across cancer types.
Comparative TI Analysis of Signaling Pathway Inhibitors
CDK4/6 Inhibitors in ER+/HER2- Breast Cancer
Table 1: Efficacy and Safety Profiles of FDA-Approved CDK4/6 Inhibitors
| Agent | PFS HR vs Control | Common Grade 3/4 AEs | Unique Safety Considerations | Therapeutic Index Determinants |
|---|---|---|---|---|
| Palbociclib | 0.80 (PALOMA-3) [162] | Neutropenia (66%), Leukopenia (43%) [162] | Higher neutropenia risk vs other CDK4/6 inhibitors [162] | Requires 7-day break in 28-day cycle; dose reduction for hematologic toxicity |
| Ribociclib | 0.80 (MONALEESA-7) [162] | Neutropenia (60%), Hepatotoxicity (9%) [162] | QT interval prolongation; hepatic and respiratory toxicity [162] | Monitoring ECG, liver function tests; contraindicated with QT-prolonging drugs |
| Abemaciclib | 0.80 (MONARCH-3) [162] | Diarrhea (19%), Neutropenia (22%) [162] | Superior blood-brain barrier penetration; continuous dosing [162] | Differentiated toxicity profile with lower hematologic but higher GI toxicity |
CDK4/6 inhibitors demonstrate a favorable therapeutic index in ER+/HER2- breast cancer, with all three approved agents showing similar efficacy (PFS HR ≈ 0.80) but distinct toxicity profiles. The TI optimization for this class involves toxicity-based differentiation rather than efficacy differentiation, with management strategies tailored to the specific toxicity profile of each agent [162].
Androgen Receptor Pathway Inhibitors in Metastatic Prostate Cancer
Table 2: Comparative Effectiveness and Safety of ARPIs in mHSPC
| Agent | 2-year PFS to mCRPC | PSA ≤0.2 ng/mL at 12 weeks | Time to PSA Nadir (months) | Common Grade 3/4 AEs |
|---|---|---|---|---|
| Abiraterone acetate | 74.1% [16] | 25.5% [16] | 12.2 [16] | Hypertension, hypokalemia, hepatotoxicity |
| Apalutamide | 81.4% [16] | 44.0% [16] | 7.2 [16] | Rash, hypothyroidism, fatigue |
| Enzalutamide | 85.6% [16] | 55.9% [16] | 7.5 [16] | Fatigue, hypertension, musculoskeletal pain |
Despite comparable long-term efficacy outcomes, ARPIs demonstrate significant differences in early response kinetics and toxicity profiles. The more rapid PSA responses observed with apalutamide and enzalutamide (median time to nadir ~7 months) versus abiraterone (12.2 months) may influence TI calculations when considering time to response as an efficacy metric [16]. The differential toxicity profiles allow for treatment selection based on individual patient comorbidities and toxicity tolerability.
JAK Inhibitors in Inflammatory and Oncologic Indications
Table 3: Therapeutic Index Considerations for JAK Inhibitors Across Indications
| JAK Inhibitor | Primary Indications | Efficacy Metrics | Class-wide Safety Concerns | Exposure-Response Relationships |
|---|---|---|---|---|
| Tofacitinib | Rheumatoid arthritis, Ulcerative colitis [7] | ACR20 response, Clinical remission | Herpes zoster reactivation, Thrombosis, Major adverse cardiac events [163] | Dose-dependent efficacy and toxicity [163] |
| Upadacitinib | Atopic dermatitis, Rheumatoid arthritis [164] | EASI-75, ACR20 | Increased risk of serious infections, Malignancy [163] | Concentration-dependent response; TDM potential [163] |
| Ruxolitinib | Myelofibrosis, GvHD [163] | Spleen volume reduction, GvHD response | Anemia, Thrombocytopenia, Neutropenia [163] | Higher exposure in GvHD vs myelofibrosis [163] |
JAK inhibitors present unique TI challenges due to their class-wide safety concerns and dose-dependent efficacy and toxicity. Therapeutic drug monitoring approaches are being investigated to optimize the TI through precise exposure control, particularly given the significant interindividual pharmacokinetic variability (20-50% CV) observed with these agents [163]. The concentration-efficacy relationship is well-established for most JAK inhibitors, while concentration-toxicity relationships require further characterization to define optimal therapeutic ranges.
Mechanistic Basis for Differential Therapeutic Indices
Signaling Pathway Architecture and Inhibitor Specificity
The therapeutic index of signaling pathway inhibitors is fundamentally determined by the biological context of their molecular targets. Differential TIs across drug classes can be understood through several mechanistic principles:
- Target Essentiality in Malignant vs Normal Cells: CDK4/6 inhibitors exploit the differential dependence of cancer cells on cyclin D-CDK4/6 for G1-S phase progression, providing a relatively wide TI due to reversible cytostasis rather than cytotoxicity [162]
- Pathway Breadth and Redundancy: JAK inhibitors target a broadly utilized signaling cascade with pleiotropic functions, resulting in multifaceted immunosuppression and corresponding infection risks [163]
- Oncogene Addiction: Tumors harboring FGFR alterations demonstrate exquisite sensitivity to FGFR inhibition, potentially enhancing the TI in biomarker-selected populations [165]
Diagram 1: Relationship between signaling pathway complexity and therapeutic index. Inhibitors targeting pathways with greater cancer cell specificity (e.g., receptor TKIs in biomarker-selected populations) generally demonstrate wider TIs than those affecting broad signaling networks.
Resistance Mechanisms and TI Evolution
The therapeutic index of targeted agents evolves with treatment duration due to emerging resistance mechanisms. For CDK4/6 inhibitors, resistance develops through RB1 loss, cyclin E amplification, and activation of alternative signaling pathways, ultimately diminishing the efficacy component of the TI over time [162]. Similarly, FGFR inhibitors face resistance via gatekeeper mutations, alternative pathway activation, and phenotypic transformation, which can alter both the efficacy and toxicity relationships [165].
Research Reagent Solutions for TI Assessment
Table 4: Essential Research Tools for Therapeutic Index Evaluation
| Research Tool Category | Specific Examples | Application in TI Assessment | Experimental Considerations |
|---|---|---|---|
| Cell Line Models | RB-proficient vs RB-deficient lines [162] | Differential sensitivity to CDK4/6 inhibition | Context-dependent vulnerability based on oncogene addiction |
| Pharmacokinetic Assays | LC-MS/MS for JAK inhibitor quantification [163] | Exposure-response relationship establishment | Matrix effects, protein binding, metabolic stability |
| Toxicity Screening Platforms | Hematopoietic progenitor cell assays [162] | Myelotoxicity prediction for kinase inhibitors | Species differences in sensitivity |
| Biomarker Detection Assays | FGFR FISH, RT-PCR for fusions [165] | Patient stratification for enriched efficacy | Detection threshold establishment for clinical utility |
| Pathway Activity Reporters | Phospho-STAT, phospho-RB immunoassays [160] | Target engagement and pathway modulation assessment | Temporal dynamics and feedback mechanisms |
The therapeutic index comparison of signaling pathway inhibitors reveals a complex interplay between molecular specificity, cellular context, and clinical application. CDK4/6 inhibitors demonstrate how agents with similar efficacy can be differentiated by toxicity profiles, while JAK inhibitors illustrate the challenges of balancing efficacy against class-wide safety concerns. ARPIs exemplify how similar molecular targets can yield differential therapeutic indices based on pharmacokinetic and pharmacodynamic properties.
Future directions in TI optimization will likely include:
- Therapeutic drug monitoring approaches for JAK and other inhibitors with significant pharmacokinetic variability and established exposure-response relationships [163]
- Biomarker-driven patient selection to enrich for populations most likely to benefit from specific targeted therapies [165]
- Novel clinical trial designs that formally incorporate efficacy-toxicity trade-offs into dose optimization [160]
- Combinatorial strategies that enhance efficacy while mitigating overlapping toxicities
The continued refinement of TI assessment methodologies will be essential for maximizing the clinical benefit of targeted anticancer therapies while minimizing their toxicity burdens.
Cost-Effectiveness Analysis and Healthcare Economic Considerations
The development and clinical application of signaling pathway inhibitors have revolutionized the treatment of numerous diseases, particularly in oncology. These targeted therapies, which include tyrosine kinase inhibitors (TKIs) and immune checkpoint inhibitors, specifically interfere with key molecular pathways driving disease progression. While these innovations represent significant clinical advances, their substantial costs necessitate rigorous cost-effectiveness analyses (CEA) to inform healthcare decision-making. This guide provides a structured framework for comparing the economic value of different signaling pathway inhibitors, focusing on methodology standardization, critical appraisal of existing studies, and integration of economic considerations with clinical efficacy data.
Economic evaluations in this field must balance multiple competing factors: clinical efficacy, toxicity profiles, acquisition costs, and broader healthcare system impacts. The fundamental metric in these analyses is the incremental cost-effectiveness ratio (ICER), which quantifies the additional cost per unit of health gain (typically per quality-adjusted life year or QALY) when comparing one intervention to another. These analyses help payers, clinicians, and health technology assessment bodies determine which treatments provide the best value for limited healthcare resources.
Methodological Framework for Cost-Effectiveness Analysis
Core Analytical Components
Conducting a robust cost-effectiveness analysis requires careful consideration of several methodological components that collectively determine the validity and generalizability of the results.
Model Structure Selection: Most economic evaluations of signaling pathway inhibitors utilize state-transition models, particularly Markov models or partitioned survival models, to simulate disease progression over time. These models typically incorporate three core health states: progression-free survival (PFS), progressive disease (PD), and death [166] [167]. The model structure should reflect the natural history of the disease and capture relevant clinical pathways.
Time Horizon Selection: The analysis should extend over a sufficient time horizon to capture all important differences in costs and outcomes between strategies. For chronic conditions and oncology, this often requires lifetime horizons (e.g., 10-50 years) or until all patients have reached death [168].
Perspective Determination: The analytical perspective (e.g., healthcare system, societal) determines which costs and consequences are included. The healthcare system perspective is most common in published analyses and typically includes direct medical costs (drug acquisition, administration, monitoring, adverse event management, and subsequent therapies) [167].
Discounting: Future costs and health outcomes are typically discounted at an annual rate of 3-5% to reflect time preference, consistent with health economic guidelines [166].
Data Integration and Modeling
Table 1: Key Data Inputs for Cost-Effectiveness Models of Signaling Pathway Inhibitors
| Data Category | Specific Parameters | Sources |
|---|---|---|
| Clinical Efficacy | Hazard ratios for overall survival and progression-free survival; response rates; duration of response | Randomized controlled trials; pooled meta-analyses |
| Safety Data | Incidence of adverse events; discontinuation rates due to toxicity | Clinical trials; long-term extension studies |
| Health-Related Quality of Life | Utility weights for health states; disutilities for adverse events | Published literature; prospective studies; mapping from clinical outcomes |
| Cost Data | Drug acquisition costs; administration costs; monitoring costs; adverse event management costs; subsequent therapy costs | National fee schedules; hospital accounting systems; published literature |
| Resource Use | Frequency of administration; monitoring intensity; management of complications | Clinical guidelines; expert opinion; retrospective studies |
Handling Uncertainty
Comprehensive uncertainty analysis is essential for establishing the robustness of cost-effectiveness results:
Deterministic Sensitivity Analysis: Evaluates the impact of varying key parameters individually over plausible ranges to identify which parameters have the greatest influence on results [166].
Probabilistic Sensitivity Analysis: Simultaneously varies all uncertain parameters according to their probability distributions to quantify the overall decision uncertainty and generate cost-effectiveness acceptability curves [166] [168].
Scenario Analysis: Assesses the impact of structural uncertainties, such as alternative model assumptions or treatment sequences [167].
Comparative Cost-Effectiveness of Signaling Pathway Inhibitors: Case Studies
Advanced Renal Cell Carcinoma
A recent comprehensive cost-effectiveness analysis compared first-line treatment regimens for advanced renal cell carcinoma (aRCC) in both the United States and China, providing insights into the economic value of different therapeutic strategies [166].
Table 2: Cost-Effectiveness Comparison of First-Line Treatments for Advanced Renal Cell Carcinoma
| Treatment Regimen | QALYs Gained | Total Costs (US) | Total Costs (China) | ICER vs. Sunitinib (US) | ICER vs. Sunitinib (China) |
|---|---|---|---|---|---|
| Nivolumab + Ipilimumab | 3.45 | $158,200 | $72,400 | Dominant* | Dominant* |
| Pembrolizumab + Axitinib | 3.12 | $162,700 | $79,100 | $42,300/QALY | $28,500/QALY |
| Sunitinib | 2.68 | $165,100 | $83,200 | Reference | Reference |
Note: *Dominant = more effective and less costly; QALY = quality-adjusted life year; ICER = incremental cost-effectiveness ratio [166]
The analysis demonstrated that Nivolumab plus Ipilimumab sequential Cabozantinib provided the optimal cost-effectiveness profile among the evaluated regimens in both the US and China, associated with both lower costs and higher QALYs compared to other options [166]. This favorable economic profile was consistent across different risk subgroups defined by the International mRCC Database Consortium (IMDC) criteria and the intent-to-treat population.
Gastrointestinal Stromal Tumors
A systematic review of cost-effectiveness analyses for tyrosine kinase inhibitors in gastrointestinal stromal tumors (GIST) identified 15 relevant studies published between 2005 and 2020 [167]. The evidence consistently demonstrated that:
- For advanced GIST, the sequence of imatinib followed by sunitinib represents a cost-effective treatment strategy [167].
- In the third-line setting, regorafenib was cost-effective compared with imatinib re-challenge therapy [167].
- For resectable GIST, 3-year adjuvant imatinib therapy constituted a cost-effective approach compared to shorter durations [167].
- Precision medicine-assisted imatinib treatment, guided by mutational analysis, was cost-effective compared to empirical treatment [167].
Despite variations in absolute costs and QALYs across different healthcare systems, there was remarkable consistency in the overall conclusions regarding the cost-effectiveness of specific therapeutic sequences in GIST.
Experimental Protocols for Generating Cost-Effectiveness Evidence
Model Development and Validation Protocol
The development of a robust cost-effectiveness model requires systematic approaches to ensure validity and relevance to clinical decision-making.
Model Structure Definition: Based on the comparative analysis of published models, initial development should specify the target population, treatment comparators, time horizon, and perspective [168]. For signaling pathway inhibitors, the model should reflect the treatment pathway, including subsequent therapy options after progression.
Data Identification and Synthesis: Comprehensive literature searches should identify relevant clinical efficacy data, preferably from randomized controlled trials or high-quality meta-analyses. Resource use and cost data should be obtained from national databases, fee schedules, or hospital accounting systems [167]. Utility weights for quality-of-life adjustment should be derived from prospective studies conducted alongside clinical trials or from systematic literature reviews.
Model Validation: The developed model should undergo both internal validation (verification of computational accuracy) and external validation (comparison of model predictions with real-world evidence or clinical trial data not used in model development) [168].
Clinical Efficacy Data Extraction Protocol
The accurate synthesis of clinical efficacy data forms the foundation of reliable cost-effectiveness analyses.
Systematic Literature Review: Comprehensive searches of PubMed/MEDLINE, Embase, Cochrane Library, and clinical trial registries should be conducted using predefined search strategies. Search terms should include the specific signaling pathway inhibitors, relevant disease states, and study design filters for randomized trials [167].
Data Extraction: Standardized extraction forms should capture details on study population characteristics, intervention and comparator regimens, outcome definitions, follow-up duration, and results for primary efficacy endpoints (overall survival, progression-free survival, response rates). Extraction should be performed independently by two reviewers with disagreements resolved through consensus [167].
Time-to-Event Data Reconstruction: When individual patient data are unavailable, digitization software can be used to reconstruct time-to-event data from published Kaplan-Meier curves. These data can then be used to fit parametric survival distributions (exponential, Weibull, Gompertz) to extrapolate outcomes beyond the trial period [166].
Visualization Approaches for Comparative Economic Evidence
Effective visualization of cost-effectiveness results enhances interpretability for diverse stakeholders.
Cost-Effectiveness Planes: The cost-effectiveness plane provides a visual representation of uncertainty in cost-effectiveness results, with the horizontal axis representing differences in effectiveness and the vertical axis representing differences in cost. Each quadrant has different policy implications [169].
Cost-Effectiveness Acceptability Curves: These curves display the probability that an intervention is cost-effective across a range of willingness-to-pay thresholds, helping decision-makers understand how the value proposition changes with different valuation of health benefits [169].
Comparative Tornado Diagrams: One-way sensitivity analyses can be visually represented using tornado diagrams, which display the magnitude of impact that each parameter has on the ICER, allowing prioritization of parameters for further research [166].
Table 3: Essential Methodological Resources and Analytical Tools for Cost-Effectiveness Analysis
| Resource Category | Specific Tools/Resources | Application in Economic Evaluation |
|---|---|---|
| Modeling Software | TreeAge Pro, R, Microsoft Excel with VBA | Development of decision-analytic models; implementation of sensitivity analyses |
| Reporting Guidelines | CHEERS (Consolidated Health Economic Evaluation Reporting Standards) | Ensuring comprehensive and transparent reporting of economic evaluations |
| Quality Assessment Tools | QHES (Quality of Health Economic Studies) instrument | Critical appraisal of published economic evaluations for systematic reviews |
| Clinical Data Sources | PubMed/Medline, Embase, Cochrane Central | Identification of clinical efficacy data for model parameterization |
| Cost Databases | Medicare Fee Schedules, WHO-CHOICE, National Health Service Reference Costs | Acquisition of country-specific cost data for economic models |
| Utility Weight Sources | EQ-5D valuation studies, MAUI valuation studies, published literature | Obtaining quality-of-life weights for QALY calculations |
Emerging Framework for Dynamic Cost-Effectiveness Assessment
The traditional approach to health technology assessment typically provides one-time evaluations of new interventions. However, the treatment landscape for many diseases evolves rapidly, with multiple competitors entering the market over time. This creates challenges for health systems that must prioritize among numerous options without clear signals about relative value [169].
A proposed framework for dynamic assessment includes three core considerations:
Proportionate Processes: Prioritizing topics for reassessment based on expected impact on patients and the health system, with flexibility in decision-making approaches [169].
Multiple Treatment Recommendations: Explicitly considering the costs and benefits of recommending multiple treatment options rather than a single cost-effective treatment, acknowledging legitimate reasons for diversity including heterogeneity in patient responses and preferences [169].
Value-Based Pricing with Confidential Discounts: Developing approaches to achieve value-based pricing when multiple manufacturers offer confidential discounts, potentially through approaches that focus on the maximum price consistent with cost-effectiveness for each product [169].
This evolving framework recognizes that cost-effectiveness analysis must adapt to dynamic therapeutic areas where multiple signaling pathway inhibitors compete within the same indication, with evidence, prices, and treatment pathways evolving over time.
Cost-effectiveness analysis provides an essential framework for evaluating the value of signaling pathway inhibitors amidst growing healthcare cost pressures. Standardized methodologies, comprehensive uncertainty analysis, and transparent reporting are crucial for generating credible evidence. The case studies in renal cell carcinoma and gastrointestinal stromal tumors demonstrate that while new targeted therapies often command premium prices, many provide reasonable value when considering their clinical benefits. As the therapeutic landscape continues to evolve with increasing numbers of signaling pathway inhibitors, dynamic assessment frameworks and sophisticated visualization approaches will become increasingly important for supporting healthcare decision-makers in optimizing resource allocation while ensuring patient access to innovative therapies.
FDA Approval Landscapes and Regulatory Considerations for Novel Inhibitors
The development and regulatory approval of novel inhibitors represent a cornerstone of modern targeted therapy, particularly in oncology and inflammatory diseases. The protein kinase family has emerged as one of the most significant drug targets of the 21st century due to its frequent deregulation in numerous diseases [7]. As of 2025, the U.S. Food and Drug Administration (FDA) has approved 85 small molecule protein kinase inhibitors, with approximately 75 of these drugs prescribed for neoplastic diseases and 7 for inflammatory conditions [7]. This guide provides a comprehensive comparison of recently approved inhibitors, examining their regulatory pathways, therapeutic applications, and supporting experimental data to inform researchers and drug development professionals about the current landscape and future directions.
2025 FDA Approval Landscape for Novel Inhibitors
The third quarter of 2025 demonstrated significant activity in the novel drug approval space, with the FDA's Center for Drug Evaluation and Research (CDER) approving 16 novel drugs in Q3 alone, matching the total approvals from the first half of the year [170]. These approvals encompassed a diverse range of therapeutic areas, with commercial projections for the Q3 cohort exceeding $16 billion by 2030 [170]. The following table summarizes key novel inhibitor approvals from 2025, highlighting their therapeutic targets and indications.
Table 1: Selected Novel Inhibitor Approvals by the FDA in 2025
| Drug Name | Active Ingredient | Approval Date | FDA-Approved Use | Therapeutic Target/Pathway |
|---|---|---|---|---|
| Hyrnuo | sevabertinib | 11/19/2025 | Locally advanced or metastatic non-squamous NSCLC with HER2 tyrosine kinase domain mutations [171] | HER2 tyrosine kinase |
| Redemplo | plozasiran | 11/18/2025 | Reduce triglycerides in adults with familial chylomicronemia syndrome [171] | Not specified (non-inhibitor) |
| Komzifti | ziftomenib | 11/13/2025 | Relapsed/refractory AML with NPM1 mutation [171] | Not specified |
| Lynkuet | elinzanetant | 10/24/2025 | Moderate-to-severe vasomotor symptoms due to menopause [171] | Not specified (non-inhibitor) |
| Rhapsido | remibrutinib | 9/30/2025 | Chronic spontaneous urticaria in adults with inadequate response to H1 antihistamines [171] | Bruton's tyrosine kinase (BTK) |
| Palsonify | paltusotine | 9/25/2025 | Acromegaly in adults with inadequate response to surgery [171] | Not specified |
| Inluriyo | imlunestrant | 9/25/2025 | ER-positive, HER2-negative, ER-1-mutated advanced or metastatic breast cancer [171] | Estrogen receptor antagonist |
| Forzinity | elamipretide | 9/19/2025 | Improve muscle strength in patients with Barth syndrome [171] | Not specified (non-inhibitor) |
| Wayrilz | rilzabrutinib | 8/29/2025 | Persistent or chronic immune thrombocytopenia [171] | Bruton's tyrosine kinase (BTK) |
| Dawnzera | donidalorsen | 8/21/2025 | Prevent attacks of hereditary angioedema [171] | Not specified (antisense oligonucleotide) |
| Brinsupri | brensocatib | 8/12/2025 | Non-cystic fibrosis bronchiectasis [171] | Dipeptidyl peptidase 1 (DPP-1) inhibitor |
| Hernexeos | zongertinib | 8/8/2025 | Unresectable or metastatic non-squamous NSCLC with HER2 mutations [171] | HER2 tyrosine kinase |
| Modeyso | dordaviprone | 8/6/2025 | Diffuse midline glioma with H3 K27M mutation [171] | Protease activator |
| Vizz | aceclidine | 7/31/2025 | Presbyopia [171] | Not specified (non-inhibitor) |
| Anzupgo | delgocitinib | 7/23/2025 | Moderate-to-severe chronic hand eczema [171] | JAK inhibitor |
| Ekterly | sebetralstat | 7/3/2025 | Acute attacks of hereditary angioedema [171] | Kallikrein inhibitor |
| Zegfrovy | sunvozertinib | 7/2/2025 | Locally advanced or metastatic NSCLC with EGFR exon 20 insertion mutations [171] | EGFR inhibitor |
| Lynozyfic | linvoseltamab-gcpt | 7/2/2025 | Relapsed/refractory multiple myeloma [171] | Bispecific BCMA-directed CD3 T-cell engager |
| Andembry | garadacimab-gxii | 6/16/2025 | Prevent attacks of hereditary angioedema [171] | Factor XIIa inhibitor |
| Ibtrozi | taletrectinib | 6/11/2025 | Locally advanced or metastatic ROS1-positive NSCLC [171] | ROS1 inhibitor |
| Emrelis | telisotuzumab vedotin-tllv | 5/14/2025 | Locally advanced/metastatic non-squamous NSCLC with c-Met overexpression [171] | c-Met inhibitor (antibody-drug conjugate) |
| Avmapki Fakzynja Co-Pack | avutometinib and defactinib | 5/8/2025 | KRAS-mutated recurrent low-grade serous ovarian cancer [171] | MEK inhibitor and FAK inhibitor |
| Imaavy | nipocalimab-aahu | 4/29/2025 | Generalized myasthenia gravis [171] | Not specified (FcRn blocker) |
| penpulimab-kcqx | penpulimab-kcqx | 4/23/2025 | Recurrent/metastatic non-keratinizing nasopharyngeal carcinoma [171] | PD-1 inhibitor |
| Vanrafia | atrasentan | 4/02/2025 | Reduce proteinuria in adults with primary IgA nephropathy [171] | Endothelin A receptor antagonist |
| Qfitlia | fitusiran | 3/28/2025 | Prevent/reduce bleeding episodes in hemophilia A or B [171] | Not specified (siRNA) |
| Blujepa | gepotidacin | 3/25/2025 | Uncomplicated urinary tract infections [171] | Not specified (bacterial topoisomerase inhibitor) |
| Romvimza | vimseltinib | 2/14/2025 | Symptomatic tenosynovial giant cell tumor [171] | CSF1R inhibitor |
| Gomekli | mirdametinib | 2/11/2025 | Neurofibromatosis type 1 with symptomatic plexiform neurofibromas [171] | MEK inhibitor |
| Journavx | suzetrigine | 1/30/2025 | Moderate to severe acute pain [171] | Not specified (non-inhibitor) |
| Grafapex | treosulfan | 1/21/2025 | Preparative regimen for allogeneic hematopoietic stem cell transplantation for AML and MDS [171] | Alkylating agent |
| Datroway | datopotamab deruxtecan-dlnk | 1/17/2025 | Unresectable/metastatic HR-positive, HER2-negative breast cancer [171] | TROP2-directed antibody-drug conjugate |
Regulatory Considerations and Global Landscape
Comparative Analysis of Regulatory Agencies
Significant disparities exist in the regulatory approval timelines and labeling requirements across major international regulatory agencies. A comprehensive study comparing approvals of small-molecule inhibitors across the FDA, European Medicines Agency (EMA), and Japanese Pharmaceuticals and Medical Devices Agency (PMDA) revealed that the FDA granted first approval for 85.5% of agents, followed by PMDA (12.7%) and EMA (1.8%) [172]. The median approval gap between the first and last agency approval was 25 months (range: 1-88 months), potentially creating substantial delays in therapy availability across different regions [172].
Table 2: Global Regulatory Comparison for Small-Molecule Inhibitor Approvals
| Regulatory Aspect | FDA | EMA | PMDA |
|---|---|---|---|
| First Approval Rate | 85.5% | 1.8% | 12.7% |
| Median Approval Gap | 25 months (range: 1-88) | ||
| Dosing Concordance | Fully concordant in 89% of cases | ||
| Pediatric Indications | Only 27% of approved drugs have pediatric indications |
Despite these timeline differences, there is strong alignment in adult dosing recommendations, with 89% (49 of 55) of inhibitors showing fully concordant dosing across all three agencies [172]. Only 4 drugs (7%) demonstrated partially concordant dosing, and 2 (4%) were non-concordant [172]. Regarding pediatric labeling, among the 55 drugs approved by all three agencies, only 15 (27%) included pediatric indications, with 7 of these (46.7%) approved across all three regions [172]. The study observed no complete divergence in pediatric dosing, though minimum age thresholds varied between agencies [172].
Accelerated Approval Pathways and Expanded Indications
The FDA has increasingly utilized accelerated approval pathways for novel inhibitors targeting rare or difficult-to-treat conditions. In Q3 2025, several oncology products received approval through these mechanisms:
- Dordaviprone (Modeyso) received accelerated approval as the first systemic therapy for H3 K27M-mutant diffuse midline glioma, an ultra-rare and aggressive brain tumor primarily affecting children and young adults [173].
- Pembrolizumab (Keytruda Qlex), a new subcutaneous formulation, was approved for multiple tumor types [173].
- Two products that previously received accelerated approval gained full FDA approval: lazertinib mesylate (Lazcluze) for NSCLC and pembrolizumab for Hodgkin lymphoma and primary mediastinal large B-cell lymphoma [173].
Additionally, the FDA expanded indications for several previously approved inhibitors:
- Roflumilast (Zoryve) was approved for atopic dermatitis in children aged 2-5 years, based on the INTEGUMENT study showing rapid skin clearance and safety [174].
- Upadacitinib, an oral selective JAK inhibitor, received label expansion for inflammatory bowel disease, supported by the U-ACHIEVE trial demonstrating durable remission and endoscopic response [174].
- Revumenib (Revuforj) was approved for relapsed/refractory NPM1-mutated AML, representing the first targeted oral therapy for this indication [174].
Comparative Effectiveness of Signaling Pathway Inhibitors
PI3K/AKT/mTOR Pathway Inhibitors
A recent systematic review and meta-analysis quantified the effects of PI3K/AKT/mTOR pathway inhibition in rheumatoid arthritis fibroblast-like synoviocytes (RA-FLSs) [70]. The analysis demonstrated that targeted blockade of this pathway markedly reduced proliferation (standardized mean difference [SMD] -5.1), IL-6 secretion (SMD -11.1), and IL-8 secretion (SMD -6.5), while significantly increasing apoptosis (SMD +2.7) [70]. Fourteen of seventeen outcome clusters showed large effects (|g| ≥ 0.8), with low-to-moderate heterogeneity (I² ≤ 35% in 11 clusters) [70]. The phosphorylation status of AKT (p-AKT) and mTOR (p-mTOR) consistently reflected functional changes and emerged as reliable pharmacodynamic markers for treatment response [70].
Figure 1: PI3K/AKT/mTOR Signaling Pathway and Inhibitor Mechanism: This diagram illustrates the PI3K/AKT/mTOR signaling cascade, showing how inhibitors target key nodes in the pathway. The biomarkers p-AKT and p-mTOR provide pharmacodynamic readouts of pathway inhibition [70].
MEK Inhibitors in MAPK Pathway-Driven Tumors
The developmental landscape for MEK inhibitors continues to evolve, with next-generation agents showing improved pharmacodynamic profiles. PAS-004, a macrocyclic oral MEK inhibitor, demonstrated promising results in a phase 1 trial (NCT06299839) for patients with MAPK pathway-driven advanced solid tumors with RAS, NF1, or RAF mutations [175]. In cohort 7 of the trial, PAS-004 administered in 37 mg capsules was deemed safe and well-tolerated, with no dose-limiting toxicities or treatment-related adverse events observed during the DLT period [175].
Pharmacodynamic assessment revealed that PAS-004 inhibited phosphorylated ERK (pERK) by 80% near Cmax at steady-state and maintained 60% pERK inhibition at Cmin (24 hours post-dose) [175]. The agent exhibited linear pharmacokinetics and dose-proportionality, with a favorable pharmacokinetic curve (Cmax/Cmin ratio <2) [175]. This sustained pathway suppression profile is particularly valuable for diseases requiring chronic dosing over extended periods [175].
Figure 2: MAPK Signaling Pathway and MEK Inhibitor Mechanism: The diagram shows the MAPK signaling cascade, frequently dysregulated in solid tumors. PAS-004, a novel MEK inhibitor, targets MEK to suppress phosphorylation of ERK, a key downstream effector [175].
Experimental Protocols and Methodologies
Systematic Review and Meta-Analysis Protocol
The quantitative synthesis of PI3K/AKT/mTOR inhibitor effects followed a rigorous systematic review protocol registered with PROSPERO (ID: CRD420251058185) in accordance with PRISMA 2020 guidelines [70]. The methodology encompassed:
- Search Strategy: Comprehensive searches of PubMed (MEDLINE), Europe PMC, and Cochrane Library up to May 18, 2025, using optimized search queries combining four thematic domains: pathology, cellular model, molecular targets, and intervention type [70].
- Inclusion Criteria: Original studies using human RA-FLSs (primary, immortalized, or commercial cell lines) evaluating pharmacological inhibitors of PI3K/AKT/mTOR pathway with defined control groups and quantitative assessment of relevant outcomes [70].
- Quality Assessment: Two independent reviewers extracted data and assessed study quality using SciRAP tool, with requirement of at least three biological replicates or samples from three independent donors [70].
- Statistical Synthesis: Standardized mean differences (Hedges g) were pooled using Sidik-Jonkman random-effects model with Hartung-Knapp confidence intervals. Heterogeneity (τ², I²) and 95% prediction intervals were calculated, with robustness tested via REML-HK, leave-one-out, and Baujat diagnostics [70].
Phase 1 Trial Design for Novel MEK Inhibitor
The clinical evaluation of PAS-004 followed a structured phase 1 trial design (NCT06299839) with the following key elements [175]:
- Study Population: Patients ≥18 years with histologically confirmed MAPK pathway-driven advanced solid tumors that were surgically unresectable and had failed standard therapy, with documented RAS, NF1, or RAF mutations.
- Dose Escalation: Sequential dose escalation across 8 cohorts (2 mg, 4 mg, 8 mg, 15 mg, 22 mg, 30 mg, 37 mg, and 45 mg) administered as once-daily oral capsules.
- Primary Endpoints: Assessment of dose-limiting toxicities, adverse events, discontinuations due to AEs, and hematology/clinical chemistry laboratory parameters.
- Pharmacodynamic Assessments: Evaluation of pERK inhibition in patient plasma at Cmax and Cmin to establish target engagement and pathway suppression.
- Exclusion Criteria: Prior antitumor treatment within 21 days or five half-lives, active CNS metastases, impaired cardiac function, or conditions affecting drug absorption.
Research Tools and Reagent Solutions
Advancements in inhibitor development have been facilitated by novel research tools that enable more comprehensive analysis of signaling pathways and inhibitor effects. The following table details essential research reagents and platforms referenced in the cited literature.
Table 3: Essential Research Reagent Solutions for Inhibitor Research
| Tool/Reagent | Type/Platform | Primary Function | Research Application |
|---|---|---|---|
| PTMNavigator | Web application integrated with ProteomicsDB | Interactive visualization of PTM data overlayed on pathway diagrams | Projects PTM perturbation datasets onto pathway diagrams to trace signaling cascades and identify pivotal PTMs [176] |
| PhosphoSitePlus | Database | Comprehensive repository of PTM sites with functional annotations | Annotates sites with functions and upstream/downstream regulators; provides kinase-substrate relationships [176] |
| PHONEMeS | Algorithm/Software | Mathematical optimization to extract interactions explaining phosphoproteomic observations | Creates data-driven pathways from phosphoproteomics datasets using prior knowledge networks [176] |
| Guardant360 CDx | Companion diagnostic assay | Liquid biopsy test for genomic alterations | Identifies breast cancer patients with ESR1 mutations eligible for imlunestrant treatment [173] |
| Oncomine Dx Express Test | Companion diagnostic test | Detection of genetic mutations in tumor tissue | Identifies EGFR exon 20 insertion mutations in NSCLC patients eligible for sunvozertinib treatment [173] |
| SciRAP | Quality assessment tool | Methodological quality evaluation for in vitro studies | Standardized quality assessment during systematic review of in vitro studies [70] |
Figure 3: Experimental Workflow for Inhibitor Research: This diagram outlines the key stages in inhibitor research, from experimental design through data interpretation. Essential research tools (green) integrate at specific stages to facilitate analysis [70] [176].
The landscape of FDA-approved novel inhibitors continues to expand rapidly, with 2025 witnessing significant approvals across therapeutic areas, particularly in oncology and inflammatory diseases. The comparative analysis reveals that while dosing recommendations show high concordance (89%) across major regulatory agencies, substantial approval timeline disparities persist, with the FDA leading in first approvals for 85.5% of small-molecule inhibitors [172]. Quantitative syntheses of inhibitor effects provide robust evidence for pathway engagement, with PI3K/AKT/mTOR inhibition demonstrating large effects on proliferation (SMD -5.1), cytokine secretion (SMD -11.1 for IL-6), and apoptosis (SMD +2.7) in RA-FLS models [70]. Next-generation inhibitors like PAS-004 show optimized pharmacodynamic profiles with sustained target engagement, highlighting ongoing innovation in drug development [175]. Emerging research tools, particularly PTMNavigator and comprehensive PTM databases, are enhancing our ability to visualize and interpret complex signaling pathway modulation, ultimately accelerating the development of more effective and targeted inhibitor therapies [176].
The field of oncology is witnessing a paradigm shift from conventional chemotherapy to sophisticated targeted therapies designed to interfere with specific molecular drivers of cancer growth. Among these, next-generation inhibitors represent a vanguard, overcoming historical challenges such as the "undruggability" of key oncoproteins and treatment resistance. This guide provides a comparative analysis of three major classes of next-generation inhibitors: direct RAS inhibitors, immune checkpoint and tyrosine kinase inhibitor (ICI-TKI) combinations, and selective estrogen receptor degraders (SERDs). By objectively comparing their mechanisms, clinical efficacy, and experimental data, this resource aims to inform research and development strategies for scientists and drug development professionals.
Comparative Analysis of Emerging Inhibitor Classes
The following section provides a structured, data-driven comparison of key emerging inhibitor classes, highlighting their distinct mechanisms, clinical performance, and developmental status.
Table 1: Comparative Overview of Next-Generation Inhibitor Classes
| Inhibitor Class | Prototypical Agents | Primary Mechanism of Action | Key Targeted Cancers | Notable Clinical Efficacy Data | Developmental Stage |
|---|---|---|---|---|---|
| Direct RAS Inhibitors | Daraxonrasib (RMC-6236) [177] | Pan-RAS(on) multiselective inhibitor; binds active-state RAS proteins, blocking downstream signaling [178] [177]. | Pancreatic ductal adenocarcinoma (PDAC), other RAS-mutant solid tumors [177]. | In KRAS-mutant PDAC: mPFS of 8.8 months, ORR of 36% (300 mg dose) [177]. | Phase III (H1 2026 readout expected) [177]. |
| ICI-TKI Combinations | Pembrolizumab + Lenvatinib [179] | TKI attacks tumor vasculature and proliferation; ICI reverses T-cell exhaustion, yielding synergistic effect [179]. | Advanced renal cell carcinoma (RCC), endometrial carcinoma, hepatocellular carcinoma (HCC) [179]. | Approved in RCC, endometrial cancer, and HCC; superior PFS and OS vs. sunitinib in RCC [179]. | Multiple regimens FDA-approved [179]. |
| Oral SERDs | Imlunestrant, Camizestrant [177] | Oral selective estrogen receptor degraders; bind to and degrade estrogen receptor, overcoming endocrine resistance [177]. | ER+/HER2- advanced breast cancer, particularly with ESR1 mutations [177]. | Camizestrant: 56% reduction in risk of progression in patients with ESR1 mutations [177]. | Phase III (pre-NDA; approval expected 2025/2026) [177]. |
Detailed Examination of Key Therapeutic Classes
Direct RAS Inhibitors: Conquering an "Undruggable" Target
The RAS signaling pathway, particularly through mutations in KRAS, NRAS, and HRAS, is a pivotal driver of oncogenesis [178]. For decades, RAS proteins were considered "undruggable" due to their smooth surface and lack of deep binding pockets [178]. Recent breakthroughs, however, have led to the development of covalent inhibitors targeting specific mutations like KRASG12C. The current frontier is the development of pan-RAS inhibitors like daraxonrasib, which target multiple RAS variants simultaneously [177].
- Mechanism of Action: Daraxonrasib is an oral, direct RAS(on) multiselective inhibitor. It is designed to target the active, GTP-bound "on" state of a wide spectrum of RAS proteins, making it potentially effective across various RAS mutations common in cancers like pancreatic ductal adenocarcinoma (PDAC) [177].
- Supporting Experimental Data: A phase I/II trial of daraxonrasib demonstrated meaningful antitumor activity in KRAS-mutant PDAC, showing a median progression-free survival (mPFS) of 8.8 months and an objective response rate (ORR) of 36% at the 300 mg dose [177]. This represents a significant improvement over the historical efficacy of chemotherapy alone in this aggressive cancer with poor prognosis.
ICI-TKI Combinations: Harnessing Synergistic Antitumor Effects
The combination of Immune Checkpoint Inhibitors (ICIs) and Tyrosine Kinase Inhibitors (TKIs) represents a rational therapeutic strategy to overcome the immunosuppressive tumor microenvironment and activate a robust antitumor immune response [179]. These combinations have gained significant therapeutic importance, with several now approved for advanced solid cancers.
- Mechanism of Action: TKIs target tumor vasculature (anti-angiogenesis) and proliferative signaling pathways, which can help to normalize the tumor vasculature and reduce immunosuppressive factors. ICIs, such as anti-PD-1/PD-L1 antibodies, block inhibitory signals on T-cells, thereby reinvigorating the anti-tumor immune response. The two drug classes together produce a complementary and often synergistic effect [179].
- Supporting Experimental Data: Clinical trials have led to the approval of combinations like nivolumab + cabozantinib, pembrolizumab + axitinib, and pembrolizumab + lenvatinib in advanced renal cell carcinoma (RCC), endometrial carcinoma, and hepatocellular carcinoma (HCC) [179]. These regimens have consistently demonstrated superior efficacy over previous standards of care, such as sunitinib, in terms of progression-free survival (PFS) and overall survival (OS) [179]. A key consideration is that these combinations often come with higher toxicities compared to monotherapies, necessitating careful management [179].
Oral SERDs: Advancing Endocrine Therapy
In hormone receptor-positive (HR+) breast cancer, resistance to traditional endocrine therapy is a major clinical challenge. A key mechanism of resistance is the acquisition of mutations in the ESR1 gene, which codes for the estrogen receptor [177]. Oral Selective Estrogen Receptor Degraders (SERDs) are a new class of agents designed to overcome this resistance.
- Mechanism of Action: Oral SERDs, such as imlunestrant and camizestrant, function by binding to the estrogen receptor and inducing its degradation, thereby depriving the cancer cell of this critical growth signal. Their oral administration is a significant advantage over the first-generation SERD, fulvestrant, which requires intramuscular injection [177].
- Supporting Experimental Data: In Phase III studies, these agents have shown significant promise. Camizestrant, for instance, demonstrated a 56% reduction in the risk of disease progression in patients with ESR1 mutations, a population that constitutes up to 50% of metastatic cases [177]. Lilly's imlunestrant reduced this risk by 38% in the same group [177]. These drugs are poised to establish a new endocrine backbone in HR+/HER2- breast cancer.
Experimental Protocols for Evaluating Inhibitor Efficacy
Robust and standardized experimental methodologies are critical for the objective comparison of inhibitor efficacy in both preclinical and clinical settings. The following protocols outline key approaches.
Clinical Trial Endpoints for Solid Tumors
This protocol describes the standard evaluation of inhibitor efficacy in human clinical trials for solid cancers, based on designs from large phase III studies [179] [177].
- Primary Objective: To determine the efficacy of a novel inhibitor or combination therapy compared to a standard of care.
- Key Endpoints:
- Overall Survival (OS): Defined as the time from randomization (or first treatment) to death from any cause. This is the gold standard endpoint for assessing clinical benefit [179].
- Progression-Free Survival (PFS): The time from randomization to first documented disease progression or death from any cause [179] [177]. Assessed via blinded independent central review using RECIST v1.1 criteria.
- Objective Response Rate (ORR): The proportion of patients with a reduction in tumor burden of a predefined amount, including both complete response (CR) and partial response (PR) [177].
- Patient Population: Patients with histologically confirmed advanced or metastatic cancer relevant to the drug's target (e.g., KRAS-mutant PDAC for daraxonrasib). Prior lines of therapy must be specified [177].
- Methodology:
- Randomization: Patients are randomly assigned to the experimental arm or the control arm (e.g., standard chemotherapy).
- Treatment Administration: The investigational inhibitor is administered per protocol-defined dosing schedule.
- Tumor Assessment: Tumor imaging (CT/MRI) is performed at baseline and at regular intervals (e.g., every 6-8 weeks). Responses are classified per RECIST v1.1 [179].
- Statistical Analysis: PFS and OS are analyzed using Kaplan-Meier methods and compared between arms with a log-rank test. ORR is compared using a chi-square or Fisher's exact test.
Predictive Biomarker Analysis Using Machine Learning
With the growing complexity of cancer therapeutics, machine learning models are being developed to predict patient response using routine clinical data [180].
- Primary Objective: To develop and validate a predictive model for response to immune checkpoint inhibitor (ICI) therapy using routine clinical and laboratory data.
- Data Collection:
- Input Features: Routinely available data collected within 30 days before first ICI infusion. This includes demographic data, clinical characteristics, and standardized measurements from laboratory blood tests (complete blood count, comprehensive metabolic panel) [180].
- Outcomes: The two primary outcomes are Overall Survival (OS) and Clinical Benefit, defined as complete response, partial response, or stable disease lasting ≥6 months per RECIST v1.1 [180].
- Methodology:
- Cohort Definition: Use a large, real-world cohort of ICI-treated patients across multiple cancer types (e.g., n=9,745 across 21 cancer types) [180].
- Model Training: Train an ensemble machine learning model (e.g., SCORPIO) on a training set to predict the target outcomes. Use five-fold cross-validation for hyperparameter tuning [180].
- Validation: Test the model on internal hold-out test sets and external validation sets from global phase 3 trials and independent health systems. Evaluate performance using time-dependent Area Under the Curve (AUC) and compare against standard biomarkers like TMB and PD-L1 [180].
Signaling Pathways and Inhibitor Mechanisms
The following diagrams, generated with Graphviz, illustrate the core signaling pathways and sites of action for the key inhibitor classes discussed in this guide.
RAS Signaling & Inhibition Pathway
ICI-TKI Synergistic Mechanism
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues key reagents and technologies that are foundational for research and development in the field of next-generation inhibitors.
Table 2: Essential Research Reagents and Platforms
| Reagent / Technology | Primary Function in R&D | Example Use Case |
|---|---|---|
| MSK-IMPACT Platform [180] | An FDA-authorized, large-panel, high-throughput DNA sequencing platform for targeted exon capture. | Used to determine Tumor Mutational Burden (TMB) and identify actionable mutations in clinical cohorts for biomarker discovery [180]. |
| SCORPIO Machine Learning Model [180] | A predictive algorithm that utilizes routine blood tests and clinical data to forecast patient response to immune checkpoint inhibitors. | Serves as a non-invasive predictive biomarker, outperforming TMB and PD-L1 in predicting overall survival and clinical benefit from ICI therapy [180]. |
| Flowfect Tx Platform (Kytopen) [181] | A continuous-flow, non-viral cell engineering system for high-viability transfection of primary immune cells. | Streamlines manufacturing of cell therapies, such as CAR-T cells, by enabling rapid, non-viral gene editing of billions of cells [181]. |
| TcBuster GMP Transposon System (Bio-Techne) [181] | A non-viral transposon system capable of delivering large, multigene cargos into cell genomes. | Used in conjunction with delivery platforms like Flowfect Tx for advanced immune cell therapy manufacturing, avoiding the use of viral vectors [181]. |
| DeepHRD AI Tool [182] | A deep-learning tool designed to detect homologous recombination deficiency (HRD) from standard biopsy slides. | Identifies patients likely to respond to PARP inhibitors and platinum-based chemotherapy, with higher accuracy and lower failure rates than genomic tests [182]. |
Conclusion
The comparative analysis of signaling pathway inhibitors reveals a rapidly evolving landscape where targeted therapies are fundamentally transforming cancer treatment. Key takeaways include the demonstrated superiority of multi-target approaches over single-target inhibitors for overcoming resistance, the critical importance of biomarker-driven patient stratification, and the necessity of addressing pathway cross-talk and compensatory mechanisms. The future of signaling pathway inhibition lies in developing smarter combination strategies, next-generation inhibitors with improved therapeutic windows, and sophisticated diagnostic tools for precise patient selection. As our understanding of signaling networks deepens, the integration of computational drug design, real-world evidence, and adaptive clinical trials will accelerate the development of more effective, personalized cancer therapies that ultimately improve patient outcomes across diverse malignancies.
References
- 1. Selecting the optimal BTK inhibitor therapy in CLL [https://pmc.ncbi.nlm.nih.gov/articles/PMC9373150/]
- 2. Comparative Analysis of BTK Inhibitors and Mechanisms ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.630942/full]
- 3. PI3K/AKT/mTOR signaling transduction pathway and targeted ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-023-01827-6]
- 4. a comparative review of PI3K/AKT/mTOR pathway inhibitors [https://pubmed.ncbi.nlm.nih.gov/24748656/]
- 5. The JAK/STAT signaling pathway: from bench to clinic [https://www.nature.com/articles/s41392-021-00791-1]
- 6. A Comprehensive Overview of Globally Approved JAK Inhibitors [https://pmc.ncbi.nlm.nih.gov/articles/PMC9146299/]
- 7. Properties of FDA-approved small molecule protein kinase ... [https://www.sciencedirect.com/science/article/pii/S1043661825001483]
- 8. Use of Inhibitors in the Study of MAP Kinases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3727897/]
- 9. Review Pharmacological inhibitors of MAPK pathways [https://www.sciencedirect.com/science/article/abs/pii/S0165614700018654]
- 10. Genetic Mutations and Epigenetic Modifications [https://pmc.ncbi.nlm.nih.gov/articles/PMC5480027/]
- 11. Crosstalk between metabolic and epigenetic modifications ... [https://www.sciencedirect.com/science/article/pii/S2589004224025847]
- 12. Comparative Efficacy of Tyrosine Kinase Inhibitors and ... [https://www.mdpi.com/2072-6694/14/14/3372]
- 13. Epigenetics-targeted drugs: current paradigms and future ... [https://www.nature.com/articles/s41392-024-02039-0]
- 14. Comparative Efficacy of CK2 Inhibitors CX-4945 and SGC- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562567/]
- 15. Hepatocellular carcinoma: signaling pathways and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11802921/]
- 16. Comparative effectiveness of androgen receptor pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599407/]
- 17. Computational frameworks transform antagonism to ... [https://www.nature.com/articles/s41746-025-01435-2]
- 18. Growth Factor Receptor - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/growth-factor-receptor]
- 19. Molecular mechanisms of acquired resistance to tyrosine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2864216/]
- 20. Structural Basis for Vascular Endothelial Growth Factor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7765180/]
- 21. Decoding tumor angiogenesis: pathways, mechanisms, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12007322/]
- 22. Structure-function relationships of growth factors and their ... [https://pubmed.ncbi.nlm.nih.gov/2557120/]
- 23. Structure-Function Relationships of ErbB RTKs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3970415/]
- 24. Vascular endothelial growth factor signaling in health and ... [https://www.nature.com/articles/s41392-025-02249-0]
- 25. Adverse effects of tyrosine kinase inhibitors in cancer ... [https://www.nature.com/articles/s41392-023-01469-6]
- 26. Comparative efficacy of epidermal growth factor receptor ... [https://pubmed.ncbi.nlm.nih.gov/40799446/]
- 27. Comparative efficacy of epidermal growth factor receptor ... [https://tlcr.amegroups.org/article/view/103452/html]
- 28. Coinhibition of the MEK/RTK pathway has high therapeutic ... [https://www.nature.com/articles/s41392-025-02382-w]
- 29. The Crosstalk Between Signaling Pathways and Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8650587/]
- 30. Signaling pathways in cancer metabolism: mechanisms ... [https://www.nature.com/articles/s41392-023-01442-3]
- 31. Advances in cancer immunotherapy: historical perspectives ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057291/]
- 32. Comparison of diagnostic performance of RT-qPCR, RT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10170900/]
- 33. Droplet digital PCR vs. quantitative real time ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1248842/full]
- 34. Comparison of Real-Time Quantitative PCR and Digital ... [https://www.sciencedirect.com/science/article/pii/S1525157819304039]
- 35. Nested-PCR vs. RT-qPCR: A Sensitivity Comparison in the ... [https://www.mdpi.com/2673-8856/4/3/19]
- 36. A Future of Unifying Cancer Science and Medicine [https://www.lungevity.org/blogs/future-of-unifying-cancer-science-and-medicine-highlights-from-aacr-2025]
- 37. Comparison of Reverse Transcription (RT)-Quantitative PCR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10100669/]
- 38. ABC8: Evolution of the overall survival of patients with ABC ... [https://www.oncology-central.com/abc8-evolution-of-the-overall-survival-of-patients-with-advanced-breast-cancer-from-the-past-decade/]
- 39. FDA approves 100th small-molecule kinase inhibitor [https://www.nature.com/articles/d41573-025-00188-7]
- 40. Small molecules in targeted cancer therapy [https://www.nature.com/articles/s41392-021-00572-w]
- 41. Classification of small molecule protein kinase inhibitors ... [https://pubmed.ncbi.nlm.nih.gov/26529477/]
- 42. Binding Mechanism of Inhibitors to BRD4 and BRD9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11054187/]
- 43. Comparative long-term outcomes of first-line CDK4/6 ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1600892/full]
- 44. Comparative efficacy and safety of CDK4/6 inhibitors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509362/]
- 45. Current landscape of BRD4 inhibitors: Selective targeting ... [https://www.sciencedirect.com/science/article/pii/S2211715625006538]
- 46. Recent Insights in Multiâ€Target Drugs in Pharmacology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479389/]
- 47. Editorial: Multi-target drug discovery and design for ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1633600/full]
- 48. Potentials and future perspectives of multi-target drugs in ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-024-01607-9]
- 49. Small molecule inhibitors targeting the cancers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9560750/]
- 50. What Makes a Smart Drug? Inside the Science of Multi- ... [https://www.news-medical.net/health/What-Makes-a-Smart-Drug-Inside-the-Science-of-Multi-Target-Therapeutics.aspx]
- 51. Comparative Effectiveness and Safety of Molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12278979/]
- 52. Targeting FGFR for cancer therapy - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11149307/]
- 53. Synergistic interplay and dual-target therapeutics [https://www.sciencedirect.com/science/article/abs/pii/S0045206825011241]
- 54. Comparative kinase and cancer cell panel profiling of ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.953013/full]
- 55. Inside ELRIG's Drug Discovery 2025 [https://www.drugtargetreview.com/article/190237/inside-elrigs-drug-discovery-2025/]
- 56. Resistance to targeted therapies in chronic lymphocytic ... [https://www.nature.com/articles/s41375-025-02662-y]
- 57. Ten-year follow-up of a phase II study of ibrutinib in relapsed [https://www.iwcll.org/work/biennial-meetings/iwcll-xxi-biennial-meeting-2025/2025-poster-gallery/ten-year-follow-up-of-a-phase-ii-study-of-ibrutinib-in-relapsed-refractory-chronic-lymphocytic-leukemia-cll-small-lymphocytic-lymphoma-sll/]
- 58. Second-Generation BTK Inhibitors Set the Stage for Future ... [https://www.onclive.com/view/second-generation-btk-inhibitors-set-the-stage-for-future-advances-in-cll-management]
- 59. BTK inhibitors and next-generation BTK-targeted ... [https://pubmed.ncbi.nlm.nih.gov/40335884/]
- 60. New 10-Year Data Show Ibrutinib's Lasting Efficacy in CLL ... [https://www.targetedonc.com/view/new-10-year-data-show-ibrutinib-s-lasting-efficacy-in-cll-sll]
- 61. BeOne Medicines Showcases Leadership in B-cell ... [https://www.businesswire.com/news/home/20251120303213/en/BeOne-Medicines-Showcases-Leadership-in-B-cell-Malignancies-at-ASH-2025]
- 62. Comparative efficacy of Bruton tyrosine kinase inhibitors in ... [https://pubmed.ncbi.nlm.nih.gov/40203277/]
- 63. Fixed-Duration Ibrutinib Plus Venetoclax Demonstrates ... [https://www.onclive.com/view/fixed-duration-ibrutinib-plus-venetoclax-demonstrates-long-term-efficacy-in-untreated-cll-sll]
- 64. The Precision-Guided Use of PI3K Pathway Inhibitors for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189650/]
- 65. Targeting PI3K family with small-molecule inhibitors in cancer ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02072-1]
- 66. Multi-node inhibition targeting mTORC1, mTORC2 and ... [https://www.nature.com/articles/s41416-025-03035-z]
- 67. Breast Cancer Treatments: Drugs Targeting the PI3K/AKT ... [https://www.mdpi.com/2075-1729/15/10/1583]
- 68. Recent Advances in Dual PI3K/mTOR Inhibitors for Tumour ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9124774/]
- 69. PI3K Inhibitors: Efficacy in Diverse Cancer Forms [https://www.sciencedirect.com/science/article/pii/S2468294225001649]
- 70. Pharmacological Inhibition of the PI3K/AKT/mTOR Pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388949/]
- 71. Targeting MAPK and PI3K/mTOR pathways halts ovarian ... [https://www.drugtargetreview.com/news/177726/targeting-mapk-and-pi3k-mtor-pathways-halts-ovarian-cancer-growth/]
- 72. PI3K Inhibitors Market Report 2025, Growth, Outlook 2034 [https://www.thebusinessresearchcompany.com/report/phosphoinositide-3-kinase-pi3k-inhibitors-global-market-report]
- 73. JAK-STAT Signaling in Autoimmunity and Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12080488/]
- 74. Small molecule drug discovery targeting the JAK-STAT ... [https://www.sciencedirect.com/science/article/pii/S1043661824001610]
- 75. JAK Inhibitors 101 [https://www.the-rheumatologist.org/article/jak-inhibitors-101/?singlepage=1]
- 76. JAK inhibitors (JAKi): Mechanisms of action and ... [https://www.sciencedirect.com/science/article/pii/S0248866324012517]
- 77. Comparative short-term efficacy of Janus kinase 1 ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1639932/full]
- 78. Comparative Safety of JAK Inhibitors vs TNF Antagonists in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423869/]
- 79. New data reveals insights into cancer and cardiovascular ... [https://www.news-medical.net/news/20250612/New-data-reveals-insights-into-cancer-and-cardiovascular-safety-of-JAK-inhibitors.aspx]
- 80. Comparative risk of incident malignancies in rheumatoid ... [https://www.sciencedirect.com/science/article/pii/S0003496725010246]
- 81. Combination Therapies in Cancer Treatment: Enhancing ... [https://www.frontiersin.org/research-topics/66212/combination-therapies-in-cancer-treatment-enhancing-efficacy-and-reducing-resistanceundefined]
- 82. Therapeutic resistance and combination therapy for cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289883/]
- 83. Mechanisms and signaling pathways of tyrosine kinase ... [https://pubmed.ncbi.nlm.nih.gov/40823259/]
- 84. Mechanisms and signaling pathways of tyrosine kinase ... [https://www.sciencedirect.com/science/article/pii/S2213048925000354]
- 85. Immune evasion in cancer: mechanisms and cutting-edge ... [https://www.nature.com/articles/s41392-025-02280-1]
- 86. Resistance mechanisms to immune checkpoint inhibitors [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02212-7]
- 87. A highly annotated drug combination resource for ... [https://www.nature.com/articles/s41597-025-05630-4]
- 88. ESMO 2025: Combination of immunotherapy and targeted ... [https://ecancer.org/en/news/27160-esmo-2025-combination-of-immunotherapy-and-targeted-therapy-improves-survival-for-patients-with-advanced-colorectal-cancer]
- 89. WCLC 2025: Combination therapy achieves durable ... [https://www.mdanderson.org/newsroom/research-newsroom/wclc-2025--combination-therapy-achieves-durable-response-in-adva.h00-159779601.html]
- 90. New clinical trial design in precision medicine [https://www.nature.com/articles/s41392-024-01760-0]
- 91. Biomarker-Driven Oncology Clinical Trials: Key Design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7446374/]
- 92. Biomarker-Driven Clinical Trials in Oncology [https://www.precisionformedicine.com/blog/biomarker-driven-clinical-trials-in-oncology-enrichment-stratification-all-comers-basket-when-to-use-what-and-why]
- 93. Biomarker Assay-Driven Clinical Trials [https://www.cerbaresearch.com/news/biomarker-assay-driven-clinical-trials/]
- 94. The Future of Clinical Trials: Incorporating 'Omics for ... [https://blog.crownbio.com/the-future-of-clinical-trials-incorporating-omics-for-enhanced-stratification]
- 95. Insights from Biomarkers & Precision Medicine 2025 [https://www.signifyresearch.net/insights/biomarkers-billions-and-breakthroughs-insights-from-biomarkers-precision-medicine-2025/]
- 96. Bypass Mechanisms of Resistance to Receptor Tyrosine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3876281/]
- 97. Mechanisms of Acquired Resistance and Tolerance to EGFR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9856371/]
- 98. Multiple Mutations and Bypass Mechanisms Can ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3208270/]
- 99. Acquired resistance to tyrosine kinase targeted therapy [https://www.sciencedirect.com/science/article/pii/S1368764624001341]
- 100. Cracking the EGFR code: Cancer biology, resistance ... [https://www.sciencedirect.com/science/article/pii/S0031699725074848]
- 101. NF-κB in inflammation and cancer [https://www.nature.com/articles/s41423-025-01310-w]
- 102. Inhibition of NF-κB signaling unveils novel strategies to ... [https://www.sciencedirect.com/science/article/pii/S1368764623001255]
- 103. Mechanisms of NF-κB p65 and strategies for therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6217131/]
- 104. Post-translational governance of NF-κB in cancer immunity [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479462/]
- 105. Targeting the NF-κB pathway enhances responsiveness of ... [https://www.nature.com/articles/s41598-023-32321-0]
- 106. Combined MEK and PARP inhibition enhances radiation ... [https://www.sciencedirect.com/science/article/pii/S266637912500357X]
- 107. Akt Stimulates the Transactivation Potential of the RelA/p65 ... [https://www.sciencedirect.com/science/article/pii/S0021925819670201]
- 108. Akt-mediated regulation of NFκB and the essentialness of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2767458/]
- 109. Toxicity profiles of immune checkpoint inhibitors in nervous ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11383843/]
- 110. Review Targeting molecular pathways to control immune ... [https://www.sciencedirect.com/science/article/pii/S1471490624002990]
- 111. Strategies for mitigating adverse events related to selective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10772460/]
- 112. Comparative efficacy and safety of second-line therapies ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1697949/full]
- 113. Comparative real-world effectiveness and safety of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12592040/]
- 114. Comparative efficacy and safety of dupilumab versus newly ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0319400]
- 115. Comparative efficacy and safety of JAK inhibitors in the ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1372810/full]
- 116. Comparative Efficacy of Immune Checkpoint Inhibitors and ... [https://www.mdpi.com/2076-393X/13/4/423]
- 117. Strategies for delivering drugs across the blood-brain ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 118. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 119. Overcoming the Blood–Brain Barrier: Advanced Strategies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388969/]
- 120. Mechanobiology of the blood-brain barrier during ... [https://www.nature.com/articles/s41467-025-61888-7]
- 121. 3D in vitro blood–brain barrier models: recent advances ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1637602/full]
- 122. Precision targeting of the CNS: recent progress in brain ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra03578c]
- 123. Advances in brain-targeted delivery strategies and natural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12107825/]
- 124. Surface-functionalized nanoparticles for targeted drug ... [https://www.sciencedirect.com/science/article/abs/pii/S0167732225011158]
- 125. Imaging brain inflammation and blood brain barrier ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629060/]
- 126. A new era in brain drug delivery: Integrating multivalency ... [https://www.sciencedirect.com/science/article/pii/S0169409X2500122X]
- 127. Pharmacokinetic Optimization of Small Molecule Janus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9380220/]
- 128. Pharmacokinetic, Tissue Distribution, Metabolite, and ... [https://www.mdpi.com/1420-3049/29/2/297]
- 129. Pharmacokinetic and tissue distribution analysis of ... [https://www.sciencedirect.com/science/article/abs/pii/S1570023225001801]
- 130. Pharmacokinetics, bioavailability and tissue distribution of ... [https://bioresourcesbioprocessing.springeropen.com/articles/10.1186/s40643-022-00500-y]
- 131. Study on pharmacokinetics and tissue distribution of the ... [https://www.sciencedirect.com/science/article/pii/S2211383515000568]
- 132. Pharmacokinetics and tissue distribution analysis of ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1582644/full]
- 133. Application of Physiologically-Based Pharmacokinetic (PBPK ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334468/]
- 134. Top Trends in the Pharmaceutical Industry [2025] [https://www.epicflow.com/blog/top-trends-in-the-pharmaceutical-industry-what-to-expect/]
- 135. Biopharma Trends 2025 [https://www.bcg.com/publications/2025/biopharma-trends]
- 136. The efficacy and safety of PI3K and AKT inhibitors for ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299924006411]
- 137. MEK inhibitors are effective in Erdheim–Chester disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12133560/]
- 138. STAT Inhibitors Pipeline Market Landscape Report 2025 [https://finance.yahoo.com/news/stat-inhibitors-pipeline-market-landscape-100100382.html]
- 139. Optimizing enzyme inhibition analysis: precise estimation ... [https://www.nature.com/articles/s41467-025-60468-z]
- 140. Prediction of clinical drug efficacy by classification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC170965/]
- 141. Targeting Tumorigenic Coactivators in the PI3K/AKT ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12571992/]
- 142. Predictive, preventive, and personalized medicine in breast ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04841-w]
- 143. A Comprehensive Evaluation of Biomarkers Predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4221385/]
- 144. (PDF) MP07-17 Clinical Validation of a Live-Cell Phenotypic... [https://www.academia.edu/144549154/MP07_17_Clinical_Validation_of_a_Live_Cell_Phenotypic_Biomarker_Based_Diagnostic_Assay_for_the_Prediction_of_Adverse_Pathology_in_Prostate_Cancer]
- 145. Analytic validation of a clinical-grade PTEN immunohistochemistry... [https://pubmed.ncbi.nlm.nih.gov/27174589/]
- 146. Comprehensive analysis of PIK3CA mutations in advanced ... [https://www.nature.com/articles/s41698-025-00975-w]
- 147. Unveiling PIK3CA mutation: a prognostic beacon in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605787/]
- 148. Using predictive machine learning models for drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8551267/]
- 149. Drug target prediction through deep learning functional ... [https://www.nature.com/articles/s41467-024-46089-y]
- 150. A Comparison of Response Patterns for Progression-Free ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6324401/]
- 151. The Relationship Between Response Rate and Survival ... [https://www.mdpi.com/2072-6694/17/3/495]
- 152. Ifinatamab Deruxtecan Demonstrated Clinically Meaningful ... [https://www.merck.com/news/ifinatamab-deruxtecan-demonstrated-clinically-meaningful-response-rates-in-patients-with-extensive-stage-small-cell-lung-cancer-in-ideate-lung01-phase-2-trial/]
- 153. Rakovina Therapeutics Showcases Compelling Preclinical ... [https://www.globenewswire.com/news-release/2025/11/24/3193233/0/en/Rakovina-Therapeutics-Showcases-Compelling-Preclinical-Data-on-AI-Discovered-CNS-Penetrant-ATR-mTOR-Inhibitors-at-the-2025-Society-for-Neuro-Oncology-Annual-Meeting.html]
- 154. Comparison of Duration of Response vs Conventional ... [https://pubmed.ncbi.nlm.nih.gov/34047794/]
- 155. Wnt/β-catenin mediated signaling pathways in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150590/]
- 156. Review article Peptide inhibitors: Breaking cancer code [https://www.sciencedirect.com/science/article/pii/S0223523425007263]
- 157. Cancer cell dormancy: An update to 2025 [https://bmrat.biomedpress.org/index.php/BMRAT/article/view/994]
- 158. Cancer stem cells: landscape, challenges and emerging ... [https://www.nature.com/articles/s41392-025-02360-2]
- 159. From toxicity assessment to adaptive safety care ... [https://www.sciencedirect.com/science/article/pii/S2059702925016655]
- 160. Model-based phase I designs incorporating toxicity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2931331/]
- 161. Efficacy, safety and tolerability of drugs studied in phase 3 ... [https://www.nature.com/articles/s41598-021-90403-3]
- 162. CDK4/6 Inhibitors and the Promise of Combination Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190213/]
- 163. Therapeutic Drug Monitoring for Precision Dosing of Janus ... [https://www.researchprotocols.org/2025/1/e70312]
- 164. Comparative real-world effectiveness and safety of ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1658843/full]
- 165. Targeting FGFR for cancer therapy [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-024-01558-1]
- 166. A cost-effectiveness comparison between immunotherapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536148/]
- 167. Cost-Effectiveness Analysis of Tyrosine Kinase Inhibitors in ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2021.768765/full]
- 168. Comparative analyses of published cost effectiveness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7105898/]
- 169. A Framework for Using Cost-effectiveness Analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12227514/]
- 170. FDA new drug approvals in Q3 2025 [https://www.nature.com/articles/d41573-025-00170-3]
- 171. Novel Drug Approvals for 2025 [https://www.fda.gov/drugs/novel-drug-approvals-fda/novel-drug-approvals-2025]
- 172. Global regulatory variability in small-molecule inhibitor ... [https://pubmed.ncbi.nlm.nih.gov/41045422/]
- 173. FDA and EMA Oncology Drug Approvals in Q3 2025 ... [https://www.aptitudehealth.com/oncology-news/fda-and-ema-oncology-drug-approvals-in-q3-2025-included-treatments-for-3-rare-brain-tumors/]
- 174. 5 Expanded FDA Approvals From October [https://www.ajmc.com/view/5-expanded-fda-approvals-from-october]
- 175. Cohort 7 of Novel MEK Inhibitor Trial Completed for MAPK ... [https://www.cancernetwork.com/view/cohort-7-of-novel-mek-inhibitor-trial-completed-for-mapk-pathway-driven-tumors]
- 176. PTMNavigator: interactive visualization of differentially ... [https://www.nature.com/articles/s41467-024-55533-y]
- 177. Pipeline Report 2025: Late-stage programs set to reshape ... [https://www.mmm-online.com/features/pipeline-report-2025-late-stage-programs-set-to-reshape-treatment/]
- 178. Evolution of direct RAS inhibitors: from undruggable target ... [https://pubmed.ncbi.nlm.nih.gov/40993828/]
- 179. and tyrosine kinase inhibitor combinations in advanced ... [https://www.sciencedirect.com/science/article/pii/S0305737224000458]
- 180. Prediction of checkpoint inhibitor immunotherapy efficacy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11922749/]
- 181. Next-Generation Therapeutics | May Round-Up 2025 [https://www.decibio.com/insights/next-generation-therapeutics-may-round-up-2025]
- 182. Top Oncology Innovations That Shaped the First Half of 2025 [https://binaytara.org/cancernews/article/top-oncology-innovations-that-shaped-the-first-half-of-2025]