Unraveling the Idiopathic Puzzle: Key Challenges and Emerging Solutions in POI Genetic Diagnosis
Premature Ovarian Insufficiency (POI) presents a significant diagnostic challenge, with a substantial proportion of cases historically classified as idiopathic.
Unraveling the Idiopathic Puzzle: Key Challenges and Emerging Solutions in POI Genetic Diagnosis
Abstract
Premature Ovarian Insufficiency (POI) presents a significant diagnostic challenge, with a substantial proportion of cases historically classified as idiopathic. This article synthesizes current research to address the complexities of genetic diagnosis in idiopathic POI. It explores the evolving etiological landscape, where improved diagnostics have reduced idiopathic cases but revealed a multifaceted genetic architecture involving chromosomal abnormalities, single-gene mutations, and oligogenic contributions. We evaluate advanced methodologies like next-generation sequencing (NGS) and array-CGH that now identify genetic anomalies in over 50% of previously idiopathic cases. The content further addresses critical interpretation pitfalls, such as variants of uncertain significance (VUS), and discusses validation strategies and comparative genomic approaches. Aimed at researchers and drug development professionals, this review outlines a path toward refined diagnostic frameworks and personalized therapeutic interventions by dissecting these core challenges.
The Shifting Etiological Landscape and Genetic Complexity of Idiopathic POI
Premature Ovarian Insufficiency (POI) represents a significant challenge in reproductive medicine, characterized by the loss of ovarian function before age 40. For decades, the majority of POI cases were classified as idiopathic due to diagnostic limitations, creating a substantial knowledge gap for researchers and clinicians. Recent epidemiological shifts reveal a dramatic transformation in this etiological distribution. Where once idiopathic cases dominated, advanced diagnostics and changing medical practices have substantially increased the proportion of identifiable causes. This paradigm shift from unknown to known etiologies fundamentally alters research approaches, enabling more targeted investigations into genetic architecture, pathogenic mechanisms, and potential therapeutic interventions. Understanding this transition is crucial for developing effective diagnostic strategies and addressing the remaining challenges in idiopathic POI.
Contemporary studies demonstrate a remarkable reduction in idiopathic cases. A 2025 comparative analysis revealed that idiopathic POI decreased from 72.1% in a historical cohort (1978-2003) to 36.9% in a contemporary cohort (2017-2024), while iatrogenic causes increased more than fourfold from 7.6% to 34.2% [1]. This redistribution reflects both improved diagnostic capabilities and the success of oncological treatments that unfortunately result in gonadal damage. The current prevalence of POI etiologies now stands at genetic (9.9%), autoimmune (18.9%), iatrogenic (34.2%), and idiopathic (36.9%) [1]. These findings underscore the critical need to reevaluate research priorities and methodological approaches to address the remaining idiopathic cases and their diagnostic challenges.
Table 1: Changing Prevalence of POI Etiologies Over Time
| Etiology | Historical Cohort (1978-2003) | Contemporary Cohort (2017-2024) | Change |
|---|---|---|---|
| Idiopathic | 72.1% | 36.9% | -35.2% |
| Iatrogenic | 7.6% | 34.2% | +26.6% |
| Autoimmune | 8.7% | 18.9% | +10.2% |
| Genetic | 11.6% | 9.9% | -1.7% |
Current Etiological Distribution of POI
Established Etiological Categories
The contemporary classification of POI encompasses several well-defined etiological categories, each with distinct pathogenic mechanisms and clinical implications. Iatrogenic POI has emerged as the leading identifiable cause, accounting for approximately one-third of all cases. This category primarily results from gonadotoxic cancer treatments, including chemotherapy and radiotherapy, with alkylating agents like cyclophosphamide and platinum-based drugs like cisplatin representing the most damaging to ovarian reserve [1] [2]. The rising prevalence reflects improved long-term survival for cancer patients, particularly childhood cancer survivors among whom POI prevalence reaches 18.6% [1]. Surgical interventions involving ovarian resection also contribute to this category, with laparoscopic ovarian cystectomy identified as a significant risk factor [2].
Autoimmune etiologies constitute the second largest identifiable category, implicated in approximately 18.9% of contemporary POI cases [1]. The pathogenesis involves lymphocytic infiltration targeting steroidogenic cells, leading to progressive follicular depletion. Multiple autoimmune conditions associate with POI, including Hashimoto's thyroiditis, Addison's disease, systemic lupus erythematosus, and rheumatoid arthritis [1] [2]. The detection of steroidogenic cell autoantibodies, particularly against 21-hydroxylase, supports an autoimmune mechanism. Hashimoto's thyroiditis demonstrates a particularly strong association, conferring an 89% higher risk of amenorrhea and a 2.4-fold increased risk of infertility due to ovarian failure [1].
Genetic causes represent a more complex and evolving etiological category. While accounting for 9.9% of contemporary cases [1], the understanding of genetic contributions has undergone significant revision. Chromosomal abnormalities, particularly X-chromosome anomalies like Turner syndrome (45,X and mosaic variants) and fragile X premutations (FMR1 gene with 55-200 CGG repeats), remain the most established genetic causes [1]. Turner syndrome affects approximately 1 in 2000-2500 live-born females, with over 80% experiencing absent spontaneous menstruation or developing POI [2]. Beyond chromosomal abnormalities, mutations in numerous autosomal genes involved in meiosis, DNA repair, and folliculogenesis have been implicated, though their penetrance and pathogenicity require careful interpretation [3].
Table 2: Current Prevalence and Characteristics of Major POI Etiologies
| Etiology | Prevalence | Key Examples | Primary Pathogenic Mechanisms |
|---|---|---|---|
| Iatrogenic | 34.2% | Chemotherapy, Radiotherapy, Ovarian Surgery | Direct follicular damage, DNA damage in oocytes, oxidative stress, vascular and stromal damage |
| Autoimmune | 18.9% | Autoimmune oophoritis, Hashimoto's thyroiditis, Addison's disease | Lymphocytic infiltration of steroidogenic cells, antibody-mediated destruction of follicular components |
| Genetic | 9.9% | Turner syndrome, FMR1 premutation, autosomal gene mutations | Chromosomal abnormalities, single gene mutations affecting folliculogenesis, meiosis, or DNA repair |
| Idiopathic | 36.9% | Unknown | Presumed genetic or environmental factors not yet identified |
Environmental and Other Factors
Beyond the major categories, environmental factors represent an increasingly recognized contributor to POI pathogenesis. Environmental toxicants (ETs) encompass atmospheric particulate matter, endocrine-disrupting chemicals (EDCs), pesticides, microplastics, heavy metals, and cigarette smoke [2]. These compounds can promote ovarian damage through multiple pathways, including oxidative stress, DNA damage, epigenetic modifications, and accelerated follicular atresia. Epidemiological studies have identified smoking as a significant risk factor, with up to a 2.75-fold elevated risk of POI among smokers [1]. The global increase in environmental pollution underscores the potential growing impact of these factors on ovarian function.
Additional etiological factors include infectious agents and metabolic disorders. While rare, viral infections including mumps, HIV, and recently SARS-CoV-2 have been associated with POI onset [1] [2]. The mechanisms may involve direct viral damage to ovarian tissue or inflammatory-mediated follicular destruction. Classic galactosemia, a rare autosomal recessive metabolic disorder caused by deficiency of galactose-1-phosphate uridyltransferase (GALT), represents another established cause, though not all affected individuals develop POI [1]. The toxic accumulation of galactose metabolites in the ovaries is thought to underlie the pathogenic process, though the precise mechanism remains incompletely understood.
The Shifting Diagnostic Paradigm: Implications for Research
Advancements in Diagnostic Capabilities
The substantial reduction in idiopathic POI cases reflects significant advancements in diagnostic methodologies and their integration into clinical practice. Genetic testing has evolved from chromosomal analysis to include targeted genetic panels and whole exome sequencing (WES), expanding the repertoire of identifiable genetic causes. Recent studies have identified more than 75 genes associated with POI, primarily involved in meiosis and DNA repair mechanisms [1]. The 2024 evidence-based guideline from ESHRE/ASRM provides updated recommendations for genetic evaluation, including FMR1 premutation testing for all women with POI and consideration of chromosome microarray analysis [4].
Immunological assessment has similarly advanced, with improved antibody detection methodologies enhancing the identification of autoimmune etiologies. The detection of steroidogenic cell autoantibodies, particularly against 21-hydroxylase, supports an autoimmune mechanism for POI [1]. Additionally, the association between thyroid autoantibodies (TgAb, TPOAb) and increased POI risk, even in women with normal thyroid function, has expanded the diagnostic considerations [1]. These diagnostic refinements have been complemented by enhanced hormonal profiling, including the strategic use of anti-Müllerian hormone (AMH) testing and refined FSH measurement protocols that now require only one elevated FSH level >25 IU/L for diagnosis according to recent guidelines [4].
The integration of multi-omics approaches represents the next frontier in POI diagnostics. Genomic, transcriptomic, proteomic, and epigenomic analyses offer unprecedented insights into the complex pathogenic networks underlying POI. Epigenetic modifications, including DNA methylation patterns, histone modifications, and non-coding RNA expression, have emerged as significant contributors to POI pathogenesis [2]. Studies have demonstrated distinct epigenetic features in ovarian granular cells from women with diminished ovarian reserve, including increased DNA methylation variability [2]. These advanced molecular profiling techniques continue to unravel the complexity of POI and further reduce the idiopathic category.
Persistent Challenges in Genetic Diagnosis
Despite these advancements, significant challenges persist in genetic diagnosis, particularly regarding variant interpretation and penetrance. Groundbreaking research published in Nature Medicine has fundamentally challenged conventional thinking about genetic causes of POI [3] [5]. In the largest study to date, analyzing genetic data from 104,733 women in UK Biobank, researchers found that 98% of women carrying variations previously considered pathogenic for POI in fact experienced menopause over age 40, ruling out POI diagnosis [3] [5]. This suggests that many variants previously reported as causative may have low penetrance or represent benign population polymorphisms.
The oligogenic model of POI inheritance has gained support, proposing that the condition may result from combinations of variants in multiple genes rather than single-gene defects [3] [6]. This complex genetic architecture complicates diagnostic interpretation and genetic counseling. The traditional monogenic framework fails to capture this complexity, potentially leading to misinterpretation of genetic testing results. As Professor Anna Murray of the University of Exeter notes, "It now seems likely that premature menopause is caused by a combination of variants in many genes, as well as non-genetic factors" [3]. This paradigm shift necessitates more nuanced approaches to genetic analysis in POI research.
Functional validation remains a critical step in establishing pathogenicity, yet implementation challenges persist. The 2023 UK Biobank study identified genetic drivers with more subtle effects on reproductive longevity, including variations in TWNK and SOHLH2 genes associated with menopause up to three years earlier than the general population [3] [5]. However, confirming the functional consequences of these and other variants requires sophisticated experimental models and substantial resources. These limitations contribute to the continued classification of cases as idiopathic despite identified genetic variants, highlighting the gap between variant detection and pathogenicity determination.
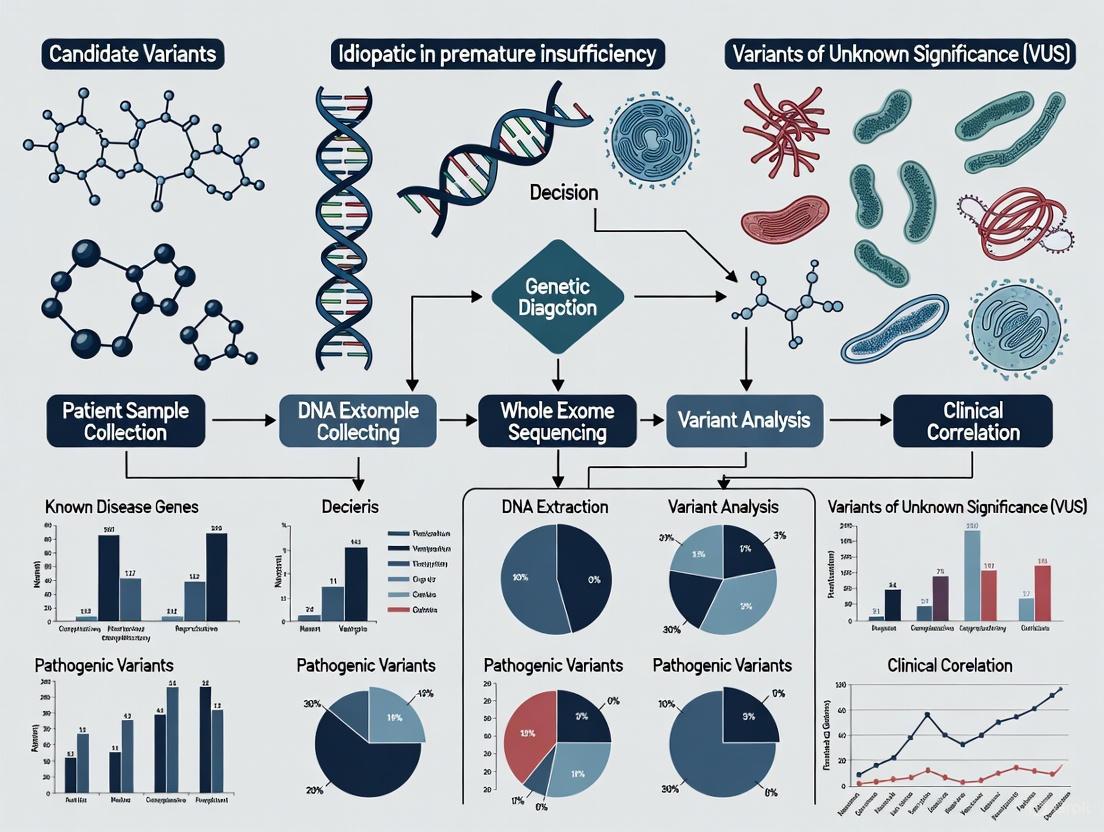
Diagram 1: Contemporary POI Etiological Classification Framework. This diagram illustrates the current classification system for POI etiologies, highlighting the multifactorial nature of the condition and the relationship between identifiable and idiopathic causes.
Technical Support: Methodologies for Etiological Investigation
Experimental Protocols for Genetic Analysis
Protocol 1: Whole Exome Sequencing and Variant Filtering for POI Research
Purpose: To identify potential pathogenic genetic variants in patients with idiopathic POI.
Methodology:
- DNA Extraction: Isolate genomic DNA from peripheral blood using standardized extraction kits (e.g., QIAamp DNA Blood Maxi Kit).
- Library Preparation: Prepare sequencing libraries using exome capture kits (e.g., Illumina Nextera Flex for Enrichment) targeting >99% of coding regions.
- Sequencing: Perform sequencing on appropriate platforms (e.g., Illumina NovaSeq 6000) with minimum 100x coverage.
- Bioinformatic Analysis:
- Align sequences to reference genome (GRCh38) using BWA-MEM or similar aligner
- Perform variant calling with GATK Best Practices workflow
- Annotate variants using ANNOVAR with population databases (gnomAD, 1000 Genomes), prediction tools (SIFT, PolyPhen-2), and disease databases (ClinVar, HGMD)
- Variant Filtering:
- Remove variants with allele frequency >0.1% in population databases
- Retain protein-altering variants (missense, nonsense, splice-site, indels)
- Prioritize genes with known POI associations and genes in related biological pathways
- Validation: Confirm prioritized variants by Sanger sequencing
- Segregation Analysis: Test available family members to assess co-segregation with phenotype
Troubleshooting Notes:
- For variants of uncertain significance, perform in silico structural modeling and consult gene constraint metrics (pLI scores)
- Consider oligogenic inheritance by analyzing potential compound heterozygosity or combinations of variants in interacting genes
- Be aware of technical limitations in detecting repeat expansions or complex structural variations
Protocol 2: Functional Validation of POI-Associated Genetic Variants
Purpose: To establish pathogenicity of identified genetic variants through experimental assessment.
Methodology:
- Plasmid Construction: Generate expression vectors containing wild-type and mutant cDNA sequences of the gene of interest.
- Cell Culture: Utilize appropriate cell lines (e.g., HEK293T, COV434, or patient-derived fibroblasts) maintained under standard conditions.
- Transfection: Introduce expression vectors using lipid-based transfection reagents (e.g., Lipofectamine 3000).
- Functional Assays (selection based on gene function):
- Protein Expression: Assess by Western blot and immunofluorescence
- Localization: Determine subcellular localization using confocal microscopy with organelle-specific markers
- Protein-Protein Interactions: Evaluate by co-immunoprecipitation or yeast two-hybrid systems
- Enzymatic Activity: Measure using appropriate substrate conversion assays
- Gene Expression Analysis: Quantify mRNA levels by RT-qPCR and assess alternative splicing by RT-PCR
- CRISPR/Cas9 Modeling: Generate isogenic cell lines with introduced variants using CRISPR/Cas9 gene editing for phenotypic comparison
Troubleshooting Notes:
- Include multiple biological replicates and appropriate positive/negative controls
- For missense variants, compare to known pathogenic and benign variants in the same protein
- Consider protein stability and degradation pathways when interpreting expression results
Research Reagent Solutions
Table 3: Essential Research Reagents for POI Etiological Investigation
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Genetic Analysis Tools | Whole exome sequencing kits, Sanger sequencing reagents, CRISPR/Cas9 components | Identification and validation of genetic variants | Prioritize kits with high coverage uniformity; validate CRISPR edits thoroughly |
| Immunoassay Reagents | ELISA kits for anti-ovarian antibodies, 21-hydroxylase antibodies, inflammatory cytokines | Detection of autoimmune markers | Use standardized controls; confirm specificity with blocking experiments |
| Cell Culture Models | Primary granulosa cells, ovarian cortical tissue, established cell lines (COV434, KGN) | In vitro modeling of ovarian function | Optimize culture conditions for primary cells; authenticate cell lines regularly |
| Molecular Biology Reagents | RNA extraction kits, cDNA synthesis kits, qPCR primers/probes, Western blot reagents | Gene expression and protein analysis | Include multiple reference genes for qPCR; validate antibodies for specific applications |
| Animal Models | Transgenic mice, xenograft models, chemotherapeutic injury models | In vivo pathophysiological studies | Consider species differences in ovarian physiology; monitor estrous cycles |
| Histopathology Tools | Tissue fixation/embedding supplies, immunohistochemistry reagents, multiplex fluorescence kits | Ovarian tissue analysis | Optimize antigen retrieval; use appropriate positive controls for staining |
FAQs: Addressing Key Challenges in POI Etiology Research
Q1: What proportion of POI cases remain truly idiopathic with current diagnostic capabilities?
Recent comprehensive studies indicate that approximately 36.9% of POI cases remain classified as idiopathic after thorough evaluation [1]. This represents a substantial decrease from historical rates of 72.1%, reflecting significant advances in diagnostic methodologies. However, the term "idiopathic" continues to evolve as new genetic, autoimmune, and environmental factors are identified. Research suggests that many idiopathic cases likely represent complex genetic etiologies with oligogenic inheritance patterns or gene-environment interactions that current technologies cannot fully characterize [3] [6].
Q2: How has our understanding of genetic contributions to POI changed recently?
Groundbreaking research from 2023 has fundamentally altered our understanding of genetic contributions to POI. The largest study to date, analyzing data from over 100,000 women, found that 98% of women carrying genetic variants previously considered pathogenic for POI actually experienced menopause after age 40 [3] [5]. This indicates that many reported "causative" variants have low penetrance and that POI likely results from combinations of variants in multiple genes rather than single-gene defects. This shift toward an oligogenic model complicates genetic diagnosis but more accurately reflects the complex inheritance of most POI cases.
Q3: What are the most significant methodological challenges in POI etiological research?
Key methodological challenges include: (1) Variant interpretation difficulties - distinguishing truly pathogenic variants from low-penetrance alleles or benign polymorphisms; (2) Oligogenic complexity - identifying and validating combinations of variants that collectively contribute to disease risk; (3) Functional validation bottlenecks - the time and resource-intensive nature of experimentally confirming variant pathogenicity; (4) Model system limitations - the lack of ideal in vitro systems that fully recapitulate human ovarian physiology; and (5) Ethical constraints - limitations on experimental manipulation of human ovarian tissue [3] [2] [6].
Q4: Which environmental factors have the strongest evidence for contributing to POI?
Epidemiological and experimental studies have identified several environmental factors with substantial evidence for POI contribution: (1) Cigarette smoking - associated with up to 2.75-fold increased risk in a dose-dependent manner [1]; (2) Endocrine-disrupting chemicals - including phthalates, bisphenol A (BPA and analogs), and pesticides that promote oxidative stress and follicular atresia [1] [2]; (3) Chemotherapeutic agents - particularly alkylating compounds like cyclophosphamide and platinum-based drugs like cisplatin [1]; and (4) Atmospheric particulate matter - associated with increased DNA damage and oxidative stress in ovarian tissue [2].
Q5: What diagnostic approach is recommended for maximizing etiological identification?
The 2024 evidence-based guideline from ESHRE/ASRM recommends: (1) Comprehensive history - including family history, exposures, and autoimmune symptoms; (2) Genetic testing - FMR1 premutation screening for all patients and chromosomal analysis for those with primary amenorrhea; (3) Autoimmune evaluation - assessment for associated conditions and relevant autoantibodies; (4) Hormonal profiling - including FSH (>25 IU/L on one measurement now sufficient for diagnosis) and AMH where uncertainty exists [4]. A systematic, stepwise approach incorporating these elements maximizes etiological identification while remaining cost-effective.
Diagram 2: Comprehensive Diagnostic Workflow for POI Etiology. This diagram outlines a systematic approach to etiological investigation in POI, illustrating the sequential evaluation process and the point at which idiopathic classification is appropriate after comprehensive assessment.
The landscape of POI etiology has transformed dramatically, with identifiable causes now representing the majority of cases. This shift from idiopathic to identifiable reflects substantial progress in diagnostic capabilities and etiological understanding. However, significant challenges remain, particularly in deciphering the complex genetic architecture underlying remaining idiopathic cases. The recognition that POI likely results from oligogenic combinations rather than single-gene defects necessitates more sophisticated analytical approaches that consider variant combinations, gene-gene interactions, and gene-environment interplay.
Future research directions should prioritize several key areas: (1) Multi-omics integration - combining genomic, transcriptomic, epigenomic, and proteomic data to construct comprehensive pathogenic networks; (2) Advanced functional models - developing more physiologically relevant in vitro systems, including organoid cultures and microfluidic platforms that better recapitulate ovarian microenvironments; (3) Environmental exposure mapping - systematically characterizing the exposome and its interactions with genetic susceptibility; and (4) Computational approaches - implementing artificial intelligence and machine learning to identify complex patterns across diverse data types. These approaches promise to further reduce the idiopathic category and enable truly personalized management strategies for women with POI.
The progressive elucidation of POI pathogenesis underscores the dynamic nature of etiological classification in complex disorders. As research methodologies continue to advance, the remaining idiopathic cases will inevitably yield their secrets, paving the way for improved diagnostics, targeted interventions, and ultimately better outcomes for affected women. The journey from idiopathic to identifiable represents both a remarkable achievement and an ongoing challenge for the research community.
Frequently Asked Questions (FAQs)
FAQ 1: What is the current understanding of the genetic contribution to idiopathic Premature Ovarian Insufficiency (POI)?
POI is a highly heterogeneous condition, and its genetic architecture is complex. While approximately 70% of POI cases were historically classified as idiopathic, advanced genetic techniques are now revealing underlying causes in a significant portion of these patients [7] [8]. Genetic factors are pivotal, contributing to approximately 20–25% of all POI cases with known causes [8]. A large-scale whole-exome sequencing study of 1,030 POI patients identified pathogenic or likely pathogenic variants in known POI-causative genes in 18.7% of cases. When novel candidate genes from association analyses were included, the genetic contribution rose to 23.5% of cases [9]. The genetic yield is even higher in specific subgroups; for instance, one study combining array-CGH and Next-Generation Sequencing (NGS) identified a genetic anomaly in 57.1% (16/28) of idiopathic POI patients [7].
Table 1: Genetic Diagnostic Yield in Recent POI Studies
| Study Description | Cohort Size | Overall Genetic Diagnostic Yield | Notes |
|---|---|---|---|
| Large-scale WES study [9] | 1,030 patients | 23.5% (242/1030) | Included known and novel candidate genes |
| Combined array-CGH & NGS panel [7] | 28 idiopathic patients | 57.1% (16/28) | 39.3% of patients had a family history of POI |
| Genetic contribution in POI [8] | N/A | 20-25% | Figure for all POI cases with a known cause |
FAQ 2: How do chromosomal abnormalities contribute to POI?
Chromosomal abnormalities are a well-established cause of POI, accounting for approximately 10-13% of cases [8] [1]. These abnormalities are more frequently observed in women with primary amenorrhea (21.4%) compared to those with secondary amenorrhea (10.6%) [1]. The most significant contributors are abnormalities of the X chromosome, as normal ovarian function requires two active copies of X-linked genes.
- X Chromosome Aneuploidies: Turner Syndrome (45, X) is a major cause, resulting from the complete or partial absence of an X chromosome and leading to accelerated follicular atresia [8] [1]. Trisomy X Syndrome (47, XXX) has also been associated with diminished ovarian reserve and an increased risk of POI [8].
- Structural Chromosomal Abnormalities: These include isochromosomes, deletions, and translocations, particularly within defined "critical regions" on the long arm (q) of the X chromosome (Xq13.1–q21.33 and Xq24–q27). X-autosomal translocations can also disrupt ovarian function through gene disruption, meiosis errors, or positional effects [8].
FAQ 3: What is the role of monogenic (single-gene) defects in POI?
Monogenic inheritance refers to traits or conditions caused by pathogenic variants in a single gene [10]. In POI, over 75 genes have been implicated, impacting processes critical for ovarian function [1]. These monogenic causes can present as either non-syndromic (isolated POI) or syndromic (POI as part of a broader clinical picture).
- Non-Syndromic POI: Genes involved include those critical for ovarian development, folliculogenesis, meiosis, and DNA repair. Examples include NOBOX, BMP15, GDF9, and FSHR [1] [9].
- Syndromic POI: Several genetic syndromes feature POI as a component. Examples include:
- Fragile X-associated POI (FXPOI): Caused by a premutation (55-200 CGG repeats) in the FMR1 gene [1].
- Galactosemia: An autosomal recessive disorder caused by mutations in the GALT gene, leading to toxic metabolite accumulation and POI in 80-90% of female patients [8] [1].
- Autoimmune Polyendocrine Syndrome Type 1 (APS-1): Caused by mutations in the AIRE gene [8].
- Ataxia-telangiectasia (AT): Caused by mutations in the ATM gene, which plays a crucial role in DNA damage repair [8].
Table 2: Examples of Key Monogenic Causes of POI
| Gene | Primary Functional Category | Phenotype | Prevalence / Note |
|---|---|---|---|
| FMR1 (premutation) | Gene regulation | FXPOI | Highest risk with 70-100 CGG repeats [1] |
| GALT | Metabolism | Galactosemia with POI | 80-90% of patients affected [1] |
| AIRE | Autoimmune regulation | APS-1 with POI | ~41% of APS-1 patients have POI [8] |
| NR5A1 | Gonadal development | Isolated or syndromic POI | One of the most frequently mutated genes in a large cohort (1.1%) [9] |
| EIF2B2 | Mitochondrial function | Isolated POI | Had the highest prevalence of pathogenic alleles in one study (0.8%) [9] |
FAQ 4: Is there evidence for oligogenic inheritance in POI?
Yes, emerging evidence strongly suggests that oligogenic inheritance—where a few genes interact to cause a disease—plays a significant role in POI [11] [12]. This complexity challenges the traditional monogenic view.
Research indicates that the cumulative effects of genetic defects influence the clinical severity of POI. A large WES study found that patients with primary amenorrhea had a substantially higher frequency of biallelic and multi-heterozygous (variants in different genes) pathogenic variants compared to those with secondary amenorrhea [9]. This suggests that the combined impact of variants in multiple genes can lead to a more severe phenotype. The post-genome era, with increased access to NGS, is allowing researchers to unravel these complex genetic mechanisms behind POI and other inherited disorders [11].
FAQ 5: What are the key experimental protocols for genetic analysis in POI research?
A comprehensive genetic workup for POI involves a combination of techniques to capture different types of variants.
- Karyotyping and Chromosomal Microarray (array-CGH): These are first-line tests to identify numerical and structural chromosomal abnormalities, including large deletions/duplications (copy number variations, or CNVs). Array-CGH can detect CNVs of a minimum of 60 kb [7].
- FMR1 CGG Repeat Analysis: This specific test is crucial for diagnosing FXPOI and should be performed, especially in patients with a family history of POI or intellectual disability [1].
- Next-Generation Sequencing (NGS): This is the cornerstone for identifying single nucleotide variations (SNVs) and small insertions/deletions (indels).
- Gene Panel Sequencing: Uses a custom capture design targeting known and suspected POI genes (e.g., 163 genes) [7].
- Whole Exome Sequencing (WES): Sequences all protein-coding genes and is effective for identifying novel candidate genes in research settings [9].
- Whole Genome Sequencing (WGS): Captures the entire genome, including non-coding regions, offering the most comprehensive analysis.
Table 3: Key Methodologies for Genetic Diagnosis in POI
| Technique | Primary Use | Key Takeaway |
|---|---|---|
| Karyotype | Detect numerical and large structural chromosomal abnormalities. | Essential for diagnosing Turner Syndrome and other aneuploidies. |
| Array-CGH | Genome-wide detection of CNVs. | Identifies microdeletions/duplications below the resolution of karyotyping. |
| FMR1 Testing | Detect CGG triplet repeat premutation. | A specific test for a common genetic cause; not detected by NGS. |
| NGS (Panel/WES) | Identify SNVs/indels in single genes. | The most effective method for detecting monogenic causes. A combined approach with array-CGH increases diagnostic yield [7]. |
Experimental Protocol: Combined Array-CGH and Targeted NGS Panel Analysis [7]
- Sample Collection: Obtain peripheral blood samples from patients after informed consent. DNA is extracted using standardized kits (e.g., QIAsymphony DNA midi kits).
- Array-CGH:
- Platform: SurePrint G3 Human CGH Microarray 4 × 180 K.
- Procedure: Follow supplier's recommendations for hybridization.
- Bioinformatics Analysis: Use software like CytoGenomics v5.0 and Cartagenia Bench Lab CNV v5.1 to identify CNVs. Report CNVs with a minimum size of 60 kb.
- Targeted NGS:
- Capture Design: Use a custom SureSelect capture design targeting a panel of genes (e.g., 163 genes involved in ovarian function).
- Library Preparation & Sequencing: Use SureSelect XT-HS reagents on a system like Magnis, followed by sequencing on a platform like Illumina NextSeq 550.
- Bioinformatics Analysis: Perform using a pipeline such as Alissa Align&Call v1.1 and Alissa Interpret v5.3 for variant calling and annotation.
- Variant Interpretation:
- Filter against population databases (e.g., gnomAD) and variation databases (e.g., ClinVar, HGMD).
- Classify variants according to ACMG guidelines (Pathogenic, Likely Pathogenic, Variant of Uncertain Significance (VUS), Likely Benign, Benign).
- Correlate genotypes with clinical phenotypes using databases like OMIM and the literature.
The following workflow diagram illustrates the diagnostic genetic analysis for POI:
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Genetic Studies in POI
| Reagent / Tool | Function in Research | Example Product / Software |
|---|---|---|
| DNA Extraction Kit | Isolate high-quality genomic DNA from patient samples (e.g., blood). | QIAsymphony DNA midi kits (Qiagen) [7] |
| Array-CGH Platform | For genome-wide detection of copy number variations (CNVs). | SurePrint G3 Human CGH Microarray 4 × 180 K (Agilent) [7] |
| Array-CGH Analysis Software | To identify, visualize, and interpret CNVs from array data. | CytoGenomics v5.0, Cartagenia Bench Lab CNV v5.1 (Agilent) [7] |
| NGS Target Enrichment | To capture and sequence a specific panel of POI-related genes. | SureSelect XT-HS Custom Capture (Agilent) [7] |
| NGS Platform | To perform high-throughput sequencing of captured libraries. | Illumina NextSeq 550 [7] |
| NGS Analysis Pipeline | For alignment, variant calling, annotation, and interpretation. | Alissa Align&Call v1.1 & Alissa Interpret v5.3 [7] |
| Variant Annotation Databases | To filter variants and assess population frequency and pathogenicity. | gnomAD, ClinVar, HGMD [7] [9] |
| Tovopyrifolin C | Tovopyrifolin C | High-Purity Research Compound | Tovopyrifolin C for research. Investigate its bioactivity & mechanism. For Research Use Only. Not for human or veterinary use. |
| Patamostat | Patamostat | Potent Serine Protease Inhibitor | RUO | Patamostat is a potent serine protease inhibitor for research on thrombosis, inflammation, and pancreatitis. For Research Use Only. Not for human consumption. |
The following diagram summarizes the complex genetic architecture underlying POI:
FAQs: Navigating Autosomal Gene Analysis in Idiopathic POI
FAQ 1: A significant proportion of POI cases are classified as idiopathic. What is the emerging genetic understanding of these cases?
While historically over 70-90% of POI cases were considered idiopathic, recent advances in genetic testing have significantly reduced this percentage. It is now understood that a substantial genetic component underpins many of these cases, with current estimates of idiopathic forms standing between 39% and 67% [6] [13]. This shift is largely due to the identification of numerous autosomal genes associated with POI. The genetic architecture is highly heterogeneous, involving mutations in over 100 genes, and is not limited to X-chromosome defects [14] [8]. Furthermore, the inheritance patterns in idiopathic POI are now recognized to extend beyond simple monogenic inheritance to include digenic, oligogenic, and polygenic models, where variants in multiple genes collectively contribute to the phenotype [14].
FAQ 2: Which key biological processes, governed by autosomal genes, are most frequently disrupted in POI pathogenesis?
Autosomal genes implicated in POI are integral to a wide range of critical ovarian functions. The primary biological processes and some of the key genes involved are summarized in the table below [8] [14] [6]:
Table 1: Key Biological Processes and Associated Autosomal Genes in POI
| Biological Process | Description of Role in Ovarian Function | Key Associated Autosomal Genes |
|---|---|---|
| DNA Repair & Meiosis | Maintains genomic stability during homologous recombination and meiotic division in germ cells. | MCM8, MCM9, MSH4, MSH5, SYCE1, STAG3, FANCE [14] [15] [16] |
| Folliculogenesis | Regulates the development, growth, and maturation of follicles from primordial to antral stages. | BMP15, GDF9, NOBOX, FIGLA, FSHR [14] [13] [16] |
| Ovary Formation & Oogenesis | Controls gonadal differentiation, formation of the ovary, and early development of oocytes. | FOXL2, SOHLH1, LHX8 [14] [16] |
| Mitochondrial Function | Provides energy for oocyte maturation and follicular development; dysfunction can trigger apoptosis. | MRPS22, LRPPRC [8] |
FAQ 3: Our research is focusing on novel therapeutic targets. Which autosomal genes have recently been identified as promising candidates?
Recent genomic studies employing genome-wide association studies (GWAS) integrated with expression quantitative trait loci (eQTL) analysis have pinpointed several novel autosomal genes with strong causal evidence for POI. Two genes, in particular, stand out as promising druggable targets:
FANCE(FA Complementation Group E): This gene is part of the Fanconi anemia pathway, crucial for DNA repair through homologous recombination. Mendelian randomization and colocalization analyses have established a causal link betweenFANCEand a reduced risk of POI [15].RAB2A(Member RAS Oncogene Family): This gene is involved in autophagy regulation and intracellular vesicle trafficking. Similar analyses have identifiedRAB2Aas a significant factor conferring reduced POI risk, highlighting it as another potential therapeutic target [15].
The following diagram illustrates the logical workflow and key findings from this genomic approach to target identification:
FAQ 4: What are the common experimental challenges when validating novel autosomal gene variants in POI?
A major challenge is establishing a definitive causal relationship between a genetic variant and the POI phenotype. Linkage disequilibrium can lead to false positives, where a detected variant is merely linked to the true causal variant rather than being causative itself [15]. Furthermore, the high heterogeneity and proposed oligogenic nature of POI mean that a single variant may be insufficient to cause the disease, requiring investigation of multiple hits in different genes [6] [14]. To overcome these challenges, it is critical to employ colocalization analysis, a Bayesian method that tests whether two traits share the same causal variant. A high posterior probability for H4 (PP.H4 ≥ 0.8) provides strong evidence that the same variant influences both gene expression and POI risk, strengthening causal inference [15]. Functional validation in model systems remains an essential subsequent step.
Troubleshooting Guides for Key Experiments
Guide 1: Troubleshooting Causal Gene Identification via SMR & HEIDI Tests
Objective: To identify genes whose expression levels have a putative causal effect on POI risk using Summary-data-based Mendelian Randomization (SMR).
Table 2: Troubleshooting the SMR and HEIDI Analysis Workflow
| Step | Protocol Detail | Common Issue | Solution |
|---|---|---|---|
| 1. Data Input | Use cis-eQTL data (e.g., from GTEx ovary tissue) and POI GWAS summary statistics. | Population stratification confounding results. | Ensure both datasets are from ancestrally matched cohorts (e.g., both of European descent) [15]. |
| 2. SMR Analysis | Run SMR software (v1.3.1) to test for gene-POI associations. | A significant SMR p-value (PSMR) is observed. | This indicates a genetic association, but it could be due to pleiotropy. Proceed to the HEIDI test [15]. |
| 3. HEIDI Test | Perform the heterogeneity test to rule out pleiotropy. | PHEIDI < 0.05. | Interpretation: The association is likely caused by linkage (pleiotropy), not causality. Action: Exclude the gene from the candidate list [15]. |
| 4. Result | Final candidate gene list. | PSMR < 0.05 AND PHEIDI > 0.05. | Interpretation: Supports a causal relationship between gene expression and POI. Action: Proceed to colocalization analysis for further validation [15]. |
Guide 2: Troubleshooting the Interpretation of Complex Inheritance Patterns
Objective: To correctly design studies and analyze data for POI cases that do not follow simple Mendelian inheritance.
Problem: A proband with a strong family history of POI undergoes targeted sequencing for a known autosomal gene (e.g.,
NOBOX) but no pathogenic variants are found.- Potential Cause: The POI in the family might be caused by a variant in a different gene, or follow a digenic/oligogenic inheritance pattern requiring mutations in two or more genes [14].
- Solution: Expand genetic testing from a single-gene approach to a larger panel of POI-associated genes or clinical exome sequencing. Analytical methods should be employed that can detect the combined effect of multiple medium-effect variants [6] [14].
Problem: A novel missense variant of uncertain significance (VUS) is identified in an autosomal POI gene (e.g.,
BMP15), but its functional impact is unknown.- Investigation Protocol:
- Computational Prediction: Use in silico tools (SIFT, PolyPhen-2) to predict variant deleteriousness.
- Family Segregation Analysis: Test for co-segregation of the variant with the POI phenotype across affected and unaffected family members.
- Functional Assay: For a gene like
BMP15, which regulates granulosa cell proliferation and oocyte maturation, an in vitro assay could involve creating the mutant construct, transfecting it into a granulosa cell line, and measuring its impact on SMAD phosphorylation via Western blot compared to wild-type [16] [8].
- Investigation Protocol:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Investigating Autosomal POI Genes
| Reagent / Material | Function / Application in POI Research |
|---|---|
| GWAS Summary Data (e.g., FinnGen R11) | Serves as the foundational dataset for identifying genetic variants associated with POI in large populations. Essential for MR studies [15]. |
| Cis-eQTL Datasets (GTEx V8, eQTLGen) | Provides data on how genetic variants affect gene expression in specific tissues like the ovary. Critical for linking GWAS hits to functional genes [15]. |
| SMR & HEIDI Test Software | A specialized software tool (e.g., SMR v1.3.1) used to perform Mendelian randomization and heterogeneity tests to infer causal genes from GWAS and eQTL data [15]. |
| Coloc R Package | A Bayesian statistical tool used for colocalization analysis to determine if two traits share a single causal genetic variant, thereby validating MR findings [15]. |
| Granulosa Cell Line (e.g., KGN, COV434) | An in vitro model for functional validation experiments, particularly for genes involved in folliculogenesis (e.g., BMP15, GDF9, FSHR) to study signaling pathways and steroidogenesis [16]. |
| 9-Fluorenol | 9H-Fluoren-9-ol | High Purity | Research Grade |
| Paliperidone-d4 | Paliperidone-d4 | Deuteration Grade >98% | RUO |
FAQ: Understanding Familial Risk and Heritability
What is the evidence for a genetic component in POI? Population-based studies provide strong evidence that POI has a significant genetic component. A large, multigenerational genealogical study demonstrated excess familial clustering of POI, with relatives of affected women having a significantly higher risk of the condition compared with matched controls [17]. Furthermore, twin studies indicate that the heritability estimate for age at natural menopause is approximately 0.52, suggesting genetic factors explain at least half of the interindividual variation [18].
How much does family history increase the risk of POI? The risk of POI is substantially higher among relatives of affected individuals, with the risk decreasing as the degree of relatedness becomes more distant [17] [6].
- First-degree relatives (mothers, sisters, daughters) have a 18.52-fold increased risk [17] [6].
- Second-degree relatives (aunts, grandmothers, nieces) have a 4.21-fold increased risk [17].
- Third-degree relatives (first cousins) have a 2.67-fold increased risk [17] [6].
An early menopause in a close family member is associated with a 6- to 8-fold increased risk of early or premature menopause [18].
What proportion of POI cases are considered familial? Studies have found that about 6.3% of identified POI cases have an affected relative when assessed via electronic medical records [17]. Other research indicates that up to 31% of patients with POI report a familial form of the condition, and first-degree relatives have an odds ratio of 4.6 for also having POI [6].
What are the common inherited causes of POI? The most well-defined genetic causes include [1] [18]:
- X-chromosome abnormalities: Turner syndrome (45,X and mosaic variants) is a common cause, particularly of primary amenorrhea.
- FMR1 premutations: A premutation (55-200 CGG repeats) in the FMR1 gene is the most common single-gene cause, accounting for POI in about 6% of women with a normal karyotype. This is known as Fragile X-associated Primary Ovarian Insufficiency (FXPOI) [1] [19].
- Autosomal gene mutations: Mutations in over 75 genes involved in ovarian development, meiosis, and DNA repair have been implicated, though many are rare [20].
Quantitative Data on POI Etiology and Risk
Table 1: Changing Etiological Spectrum of POI Over Time
| Etiology | Historical Cohort (1978-2003) | Contemporary Cohort (2017-2024) | Change |
|---|---|---|---|
| Idiopathic | 72.1% | 36.9% | Significant decrease (p<0.05) |
| Iatrogenic | 7.6% | 34.2% | >4-fold increase (p<0.05) |
| Autoimmune | 8.7% | 18.9% | >2-fold increase (p<0.05) |
| Genetic | 11.6% | 9.9% | Not statistically significant |
Data adapted from a comparative study of 283 patients from a single tertiary center [1].
Table 2: Familial Risk of POI
| Relationship to Proband | Relative Risk (RR) | 95% Confidence Interval |
|---|---|---|
| First-Degree Relatives | 18.52 | 10.12 – 31.07 |
| Second-Degree Relatives | 4.21 | 1.15 – 10.79 |
| Third-Degree Relatives | 2.65 | 1.14 – 5.21 |
Data from a population-level genealogical study of 396 cases [17] [6].
Experimental Protocols for Genetic Diagnosis
Protocol 1: First-Tier Genetic Testing for POI This protocol is recommended in clinical practice guidelines for the initial workup of a new POI diagnosis [4] [18].
Karyotype Analysis (High-Resolution)
- Objective: To identify numerical and structural chromosomal abnormalities, particularly X-chromosome anomalies like Turner syndrome and translocations.
- Methodology: Standard cytogenetic analysis of peripheral blood lymphocytes. A minimum of 20 metaphase cells should be analyzed, with resolution to at least 550 bands.
- Clinical Value: Chromosomal abnormalities have a prevalence of 10-13% in POI and are more common in women with primary amenorrhea (21.4%) than secondary amenorrhea (10.6%) [1] [18].
FMR1 Gene Molecular Analysis
- Objective: To detect CGG trinucleotide repeat expansions in the FMR1 gene, identifying premutation carriers.
- Methodology: PCR and/or Southern blot analysis of DNA extracted from peripheral blood. The number of CGG repeats is quantified.
- Interpretation: Normal: <45 repeats; Intermediate/Gray Zone: 45-54; Premutation: 55-200; Full Mutation: >200. POI risk is highest with 70-100 repeats [1].
- Clinical Value: Offered to all women with POI and a normal karyotype, as 6% will carry a premutation. Crucial for genetic counseling due to the risk of having children with Fragile X syndrome [19].
Protocol 2: Advanced Genomic Investigation for Idiopathic POI This protocol is used in a research setting to identify novel genetic causes in cases where first-tier testing is uninformative.
Array Comparative Genomic Hybridization (array CGH)
- Objective: To detect submicroscopic chromosomal copy-number variations (CNVs) not visible on karyotype.
- Methodology: Hybridization of patient and reference DNA to a microarray platform containing thousands of genomic probes. Identifies deletions and duplications.
- Research Value: A study found a 2.5-fold enrichment for rare CNVs on the X chromosome comprising ovary-expressed genes in POI patients, supporting a polygenic etiology [18].
Next-Generation Sequencing (NGS)
- Objective: To identify pathogenic single-nucleotide variants (SNVs) and small insertions/deletions (indels) in POI-associated genes.
- Methodology:
- Targeted Gene Panels: NGS of a predefined set of genes known to be associated with ovarian function and POI.
- Whole Exome/Genome Sequencing (WES/WGS): Unbiased sequencing of all protein-coding genes or the entire genome to discover novel candidate genes.
- Bioinformatic Analysis: Pipeline includes alignment to a reference genome, variant calling, annotation, and filtering against population databases. Focus on rare, protein-altering variants.
- Research Value: In a recent study of 1030 POI patients, 23.5% had potentially pathogenic mutations identified via genetic testing, expanding the understanding of the genetic architecture of POI [20].
Signaling Pathways and Genetic Networks in POI
The following diagram illustrates the key biological processes and a subset of implicated genes in the pathogenesis of POI, highlighting its complex and polygenic nature.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for POI Genetic Research
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Oligonucleotide Primers | Amplification of specific genomic regions for Sanger sequencing or validation. | Targeted sequencing of known POI genes like FMR1 CGG repeats, BMP15, GDF9 [1]. |
| NGS Library Prep Kits | Preparation of fragmented DNA for high-throughput sequencing on platforms like Illumina. | Constructing libraries for whole exome sequencing or targeted gene panels in idiopathic POI cohorts [20]. |
| Array CGH Microarrays | Genome-wide screening for copy-number variations with high resolution. | Identifying novel microdeletions/duplications on the X chromosome and autosomes in POI patients [18]. |
| Cytogenetic Karyotyping Kits | Analysis of chromosomal number and structure in metaphase cells. | Diagnosing Turner syndrome (45,X) and other structural X-chromosome rearrangements [18] [19]. |
| Anti-Müllerian Hormone (AMH) ELISA | Quantifying serum AMH levels as a marker of ovarian reserve. | Used as a correlative biochemical marker in genetic studies to assess ovarian function status [21] [4]. |
| Cell Culture Media for Lymphocytes | Short-term culture of peripheral blood cells to obtain metaphase chromosomes for karyotyping. | Essential for the initial cytogenetic analysis in the POI diagnostic workflow [19]. |
| Picfeltarraenin IA | Picfeltarraenin IA | Autophagy Inducer For Research | Picfeltarraenin IA is a natural triterpenoid for cancer & autophagy research. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| Aristolactam A IIIa | Aristolactam A IIIa, MF:C16H11NO4, MW:281.26 g/mol | Chemical Reagent |
FAQs: Core Concepts and Genetic Challenges in POI Research
Q1: What is the fundamental clinical and genetic distinction between syndromic and non-syndromic POI?
A1: The primary distinction lies in the presence of extra-ovarian symptoms.
- Non-Syndromic POI: The ovarian dysfunction is an isolated finding. Patients typically present with secondary amenorrhea or oligomenorrhea before age 40 and elevated Follicle-Stimulating Hormone (FSH >25 IU/L), without other associated health issues pointing to a broader syndrome [4] [6].
- Syndromic POI: Ovarian insufficiency is one feature of a multi-system genetic disorder. Examples include Turner syndrome (associated with short stature and cardiac anomalies) and Fragile X premutation syndrome (which can also cause tremor/ataxia and intellectual disability in offspring) [1] [6].
Q2: What proportion of POI cases remain idiopathic, and why is this a major research challenge?
A2: Recent large-scale studies show the idiopathic fraction is shrinking but remains significant. A 2024 study found 36.9% of cases were idiopathic, a substantial decrease from historical cohorts where this figure was 72.1% [1]. This shift is largely due to improved genetic diagnostics. The challenge of idiopathic POI stems from its extreme genetic heterogeneity, the likely role of oligogenic inheritance (where variants in multiple genes act together), and the potential contribution of epigenetic factors and environmental toxicants not captured by standard genetic panels [22] [9] [6].
Q3: What are the key overlapping genetic pathways between syndromic and non-syndromic forms?
A3: Research reveals critical shared biological pathways, indicating common functional networks. The most prominent overlapping pathway is DNA repair and meiotic recombination [22] [9]. Genes in this pathway, such as MCM8, MCM9, SPIDR, HFM1, and several Fanconi Anemia genes (e.g., FANCA, FANCM), can cause both syndromic and non-syndromic POI. Other overlapping pathways include folliculogenesis (e.g., GDF9, BMP15), mitochondrial function, and transcriptional regulation [22] [9] [6].
Q4: How does establishing a genetic diagnosis impact patient management beyond fertility?
A4: A genetic diagnosis is critical for personalized medicine. In one large study, 37.4% of patients with a genetic diagnosis had variants in genes also associated with tumor/cancer susceptibility (e.g., BRCA2), necessitating lifelong monitoring [22]. Furthermore, in 8.5% of diagnosed cases, POI was the only initial symptom of a multi-organ genetic disease, guiding comprehensive health screening and management [22].
Q5: What is the recommended genetic testing workflow for a new POI patient?
A5: The 2024 international evidence-based guideline recommends a tiered approach [4]:
- First-line Tests: Karyotype and FMR1 premutation testing.
- Next-Step Diagnosis: If first-line tests are normal, proceed with Whole Exome Sequencing (WES) or a targeted Next-Generation Sequencing (NGS) panel covering known POI genes. WES is particularly effective for adolescents and those with a family history [23].
- Copy Number Variation (CNV) Analysis: This should be performed on WES or NGS data, as it can increase diagnostic yield [23].
Troubleshooting Guides for Genetic Diagnosis
Problem: Low Diagnostic Yield in a Well-Phenotyped POI Cohort
Potential Causes and Solutions:
- Cause 1: Inadequate Gene Coverage. Standard panels may miss newly discovered genes.
- Cause 2: Over-reliance on Monogenic Models. The etiology may involve variants in more than one gene.
- Solution: Investigate an oligogenic model. Look for potential digenic or polygenic interactions by analyzing variants in genes from the same biological pathway (e.g., two different DNA repair genes) [6].
- Cause 3: Variant Filtering Stringency. Overly strict filtering may discard pathogenic non-canonical variants.
- Solution: Manually review Variants of Unknown Significance (VUS) in known POI genes, especially non-canonical splice sites or deep intronic variants. Seek functional validation for top candidates [9].
Problem: Validating the Pathogenicity of a Novel Variant
Experimental Protocol: Functional Validation in a DNA Repair Gene
- Background: A novel missense variant is identified in a DNA repair gene (e.g., MCM8). In silico predictions are conflicting.
- Objective: To determine if the variant compromises DNA repair function.
- Materials:
- Patient-derived lymphocytes or engineered cell lines (e.g., HEK293, HeLa) with the variant.
- Control cell lines (isogenic wild-type).
- Mitomycin C (MMC), a DNA cross-linking agent.
- Immunofluorescence microscopy reagents (antibodies for γH2AX, RAD51).
- Comet assay kit.
- Methodology:
- Treat Cells: Expose patient and control cell lines to a low dose of MMC (e.g., 10-50 nM) for 24 hours. Include an untreated control.
- Assay DNA Damage:
- Comet Assay (Single-Cell Gel Electrophoresis): Perform under alkaline conditions to detect single and double-strand breaks. A significant increase in tail moment in variant cells indicates elevated basal and MMC-induced DNA damage.
- Immunofluorescence for DNA Repair Foci: Stain for γH2AX (a marker of DNA double-strand breaks) and RAD51 (a marker of homologous recombination). Quantify the number of foci per nucleus. Variant cells should show persistent γH2AX foci and reduced RAD51 foci post-treatment, indicating defective repair [22].
- Measure Chromosomal Instability: Perform metaphase spread analysis on lymphocytes after MMC exposure. A higher frequency of chromosomal gaps, breaks, and radial figures in patient cells confirms hypersensitivity to clastogenic agents and a defective DNA repair phenotype [22].
- Interpretation: The variant is classified as likely pathogenic if the cells show clear hypersensitivity to MMC, evidenced by increased DNA damage in the comet assay, impaired repair focus formation, and elevated chromosomal breakage.
Quantitative Data on POI Genetics
Table 1: Diagnostic Yields from Recent Genetic Studies in POI
| Study / Cohort Description | Cohort Size | Overall Genetic Diagnostic Yield | Key Genes and Pathways Identified |
|---|---|---|---|
| Large WES Cohort (Nature Med, 2023) [9] | 1,030 patients | 23.5% (242/1030) | Meiosis/HR genes (48.7%), Mitochondrial genes, Novel candidates (LGR4, KASH5, ZP3) |
| Targeted & WES Cohort (EBioMedicine, 2022) [22] | 375 patients & 70 families | 29.3% | DNA repair/meiosis (37.4%), Follicular growth (35.4%), Tumor susceptibility |
| Russian Adolescent Cohort (Front. Endocrinol., 2025) [23] | 63 patients (<18 yrs) | 23.8% (monogenic) | FMR1, STAG3, NOBOX, MCM8, CNVs in BNC1, CPEB1 |
| Etiology Shift Analysis (PMC, 2025) [1] | 111 patients (contemporary) | N/A (Etiology breakdown) | Iatrogenic (34.2%), Autoimmune (18.9%), Genetic (9.9%), Idiopathic (36.9%) |
Table 2: Overlapping Gene Families in Syndromic and Non-Syndromic POI
| Gene Family / Pathway | Syndromic POI Examples | Non-Syndromic POI Examples | Primary Ovarian Function |
|---|---|---|---|
| DNA Repair & Meiosis | BLM (Bloom syndrome), FANC genes (Fanconi anemia) [9] | MCM8, MCM9, HFM1, MSH4 [22] [9] | Meiotic recombination, DNA double-strand break repair, genomic integrity in oocytes |
| Transcription Regulation | NOBOX (associated with hearing loss) [6] | NOBOX, FIGLA [22] [6] | Regulation of oocyte-specific gene expression, folliculogenesis |
| Mitochondrial Function | TWNK (Perrault syndrome), POLG (SCAE, PEO) [9] | AARS2, HARS2, CLPP [9] | Oocyte energy production, apoptosis regulation |
| Folate Metabolism | MTHFR (associated with neural tube defects) [6] | MTHFR polymorphisms [6] | Follicular development and oocyte quality |
Visualization: Overlapping Genetic Networks
The following diagram illustrates the core genetic and cellular pathways overlapping in syndromic and non-syndromic POI, highlighting shared genes and the points where idiopathic forms present research challenges.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for POI Genetic Research
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Whole Exome Sequencing (WES) | Comprehensive analysis of the protein-coding genome to identify novel and rare variants. | Discovery of novel POI-associated genes (e.g., HELQ, KASH5) in large patient cohorts [9] [23]. |
| Custom Targeted NGS Panels | Focused, cost-effective sequencing of a curated set of known and candidate POI genes. | High-throughput diagnostic screening for established genes (e.g., panels covering 88+ POI genes) [22]. |
| Mitomycin C (MMC) | DNA cross-linking agent used to induce replication stress and DNA double-strand breaks. | Functional validation of DNA repair gene variants by assessing chromosomal breakage sensitivity in patient lymphocytes [22]. |
| Anti-γH2AX & Anti-RAD51 Antibodies | Immunofluorescence detection of DNA damage and homologous recombination repair foci. | Quantifying the efficiency of DNA repair in cells carrying a VUS in a meiosis-related gene [22]. |
| Copy Number Variation (CNV) Callers | Bioinformatics tools to detect exon-level deletions/duplications from NGS data. | Identifying pathogenic CNVs in genes like BNC1 and FSHR that are missed by SNV analysis [23]. |
| DL-Methionine-d4 | DL-Methionine-3,3,4,4-d4 (98%)|Stable Isotope | |
| GW4869 | GW4869, MF:C30H30Cl2N6O2, MW:577.5 g/mol | Chemical Reagent |
Advanced Genomic Technologies and Their Diagnostic Yield in Idiopathic POI
Array Comparative Genomic Hybridization (array-CGH) has established itself as a cornerstone technology for detecting copy number variants (CNVs) across the genome. This powerful molecular technique provides high-resolution detection of chromosomal deletions and duplications that underlie various genetic disorders. Within the specific research context of idiopathic Premature Ovarian Insufficiency (POI), defined as the loss of ovarian function before age 40 with a prevalence of 1-2% in women, array-CGH has proven particularly valuable for identifying genetic anomalies where standard karyotyping and FMR1 premutation testing yield no answers [7] [24]. Historically, the diagnosis of POI remained elusive in approximately 70% of cases, categorized as idiopathic because no specific cause could be identified [7]. The integration of array-CGH into genetic research workflows has significantly addressed this diagnostic gap by enabling genome-wide screening for submicroscopic CNVs that escape detection by conventional cytogenetic methods. This technical support document provides comprehensive guidance on optimizing array-CGH methodologies specifically for POI research, addressing common experimental challenges, and implementing robust troubleshooting protocols to enhance research outcomes in idiopathic POI genetic diagnosis.
Technical Foundations: How Array-CGH Works
Array-CGH functions on the principle of competitive hybridization between test and reference DNA samples to a microarray platform containing thousands of immobilized DNA probes. In standard implementation, patient DNA and reference DNA are labeled with different fluorescent dyes (typically Cy5 and Cy3, respectively) [25]. The labeled samples are mixed in equal quantities and hybridized to the array, where they competitively bind to complementary probe sequences. Following hybridization and washing, the array is scanned to measure fluorescence intensity at each probe location [25].
The resulting fluorescence ratio between the two dyes at each probe indicates relative copy number: balanced fluorescence suggests normal copy number, increased test DNA signal indicates duplication, and decreased test DNA signal indicates deletion [25]. This methodology represents a significant advancement over traditional cytogenetic techniques, offering substantially higher resolution (typically detecting variants as small as 50-200 kb compared to the 5 Mb resolution of standard karyotyping) and enabling genome-wide assessment without prior hypothesis about specific chromosomal regions [25].
Table 1: Comparison of Genomic Analysis Techniques
| Technique | Resolution | CNV Detection | Balanced Rearrangements | Sequence Variants |
|---|---|---|---|---|
| Karyotyping | ~5 Mb | Limited (large changes only) | Yes | No |
| Array-CGH | 50-200 kb | Yes | No | No |
| SNP Array | Higher than array-CGH | Yes | No (but detects UPD and consanguinity) | Limited |
| Whole Genome Sequencing | Single base | Yes | Yes | Yes |
Array-CGH Experimental Workflow
The following diagram illustrates the core array-CGH workflow, from sample preparation to final data analysis:
Detailed Methodology for POI Research Applications
For research on idiopathic Premature Ovarian Insufficiency, the following protocol has been specifically optimized based on recent studies that successfully identified CNVs in POI patients [7]:
Sample Quality Control and DNA Preparation
- Obtain high-quality genomic DNA from peripheral blood samples using standardized extraction kits (e.g., QIAsymphony DNA midi kits) [7]
- Assess DNA purity and concentration via spectrophotometry; acceptable A260/280 ratio: 1.8-2.0
- Ensure DNA integrity through gel electrophoresis; minimal degradation required
- Input requirement: 0.5-2.5 μg of genomic DNA per labeling reaction [26]
DNA Labeling and Hybridization (Optimized for Agilent Platform)
- Utilize oligonucleotide array-CGH with SurePrint G3 Human CGH Microarray 4×180 K technology [7]
- Label test and reference DNA with Cy5 and Cy3 respectively using genomic DNA labeling kits
- Perform fragmentation of labeled DNA at 60°C for 30 minutes
- Mix labeled test and reference samples with Cot-1 DNA and hybridization buffer
- Hybridize to microarray for 24-40 hours at 65°C with rotation [7]
Data Acquisition and Bioinformatics Analysis
- Scan arrays using dual-laser scanner (e.g., Agilent DNA Microarray Scanner)
- Extract feature data using appropriate software (e.g., Agilent Feature Extraction software)
- Analyze CNVs using specialized bioinformatics tools (e.g., Agilent CytoGenomics software v5.0 with Cartagenia Bench Lab CNV software v5.1) [7]
- Implement minimum CNV detection threshold of 60 kb for optimal resolution [7]
- Annotate identified CNVs using population databases (gnomAD, DGV) and clinical databases (DECIPHER, ClinVar) [7]
Troubleshooting Common Experimental Challenges
Frequently Encountered Technical Issues and Solutions
Table 2: Array-CGH Troubleshooting Guide for POI Research
| Problem | Potential Causes | Solution | Prevention Strategy |
|---|---|---|---|
| High background noise | Incomplete washing, insufficient blocking, dye precipitation | Increase stringency of washes, validate Cot-1 DNA quality, filter hybridization solution | Use fresh hybridization buffer, optimize wash temperatures, implement quality control checks |
| Channel bias (dye effect) | Differential dye incorporation, probe-specific dye biases | Implement dye-swap experiments, use validated labeling kits with optimized dyes [27] | Employ balanced block experimental designs instead of reference designs [28] |
| Poor signal-to-noise ratio | Suboptimal DNA labeling, insufficient DNA input, degraded samples | Use enzymatic random primed amplification methods, quantify DNA accurately pre-labeling [27] | Verify DNA quality before processing, use specialized kits for suboptimal samples (e.g., FFPE) [26] |
| Inconsistent replication | Array-to-array variability, batch effects in processing | Process case and control samples simultaneously, randomize arrays across experimental batches | Include technical replicates, implement rigorous quality control metrics (DLRSD, SNR) [26] |
| Artifactual CNV calls | DNA quality issues, sample mix-ups, reference sample variability | Replicate findings with alternative method (MLPA, qPCR), use matched reference samples | Use standardized reference samples (e.g., pooled reference), process samples in same batch [28] |
Optimizing Experimental Design for POI Studies
Research indicates that alternative experimental designs can significantly enhance efficiency and statistical power in array-CGH studies:
Reference Design Limitations
- Traditional reference designs allocate half of all hybridizations to reference samples not of biological interest [28]
- This approach fails to account for probe-specific dye biases that can affect copy number estimates [28]
- Variance component analyses demonstrate that subject-to-subject variance is typically nearly twice the array-to-array variance, suggesting resources are better allocated to additional biological samples rather than reference replicates [28]
Enhanced Design Strategies
- Balanced block designs: When comparing two groups (e.g., POI patients vs. controls), hybridize one sample from each group on the same array [28]
- Balanced incomplete-block designs: For studies with multiple groups, ensure balanced dye labeling across samples despite not all groups fitting on each array [28]
- Off-chip reference approaches: Process reference samples separately from experimental arrays to double throughput without sacrificing data quality when samples are processed simultaneously [28]
FAQs: Addressing Researcher Questions on Array-CGH in POI
Q1: What detection sensitivity can be expected for CNVs in POI research using array-CGH? Array-CGH reliably detects CNVs down to approximately 60 kb when using modern high-density platforms (e.g., 4x180K arrays), with some platforms offering even higher resolution [7]. However, detection limits depend on probe density in specific genomic regions. For POI research, this resolution is sufficient to identify clinically relevant CNVs but may miss smaller single-exon deletions/duplications that require techniques like MLPA.
Q2: How does array-CGH compare to next-generation sequencing (NGS) for POI genetic diagnosis? Array-CGH and NGS provide complementary information in POI diagnostics. Recent studies combining both technologies in the same idiopathic POI patients demonstrated that array-CGH identified causal CNVs in 3.6% of patients, while NGS identified causal SNVs/indels in 28.6% of patients [7] [24]. The combined diagnostic yield reached 57.1% when including variants of uncertain significance, highlighting the value of a multi-technology approach [7].
Q3: What are the specific challenges when working with limited DNA samples, and how can they be addressed? Limited DNA availability, common with rare patient cohorts like POI, presents significant challenges for array-CGH. Whole Genome Amplification (WGA) techniques enable successful analysis with as little as 1 ng of input DNA while maintaining detection accuracy for known chromosomal aberrations [26]. For severely fragmented DNA (e.g., from FFPE samples), fragmentation to ~400 bp average size still produces comparable results to intact DNA when using appropriate WGA methods [26].
Q4: Which chromosomal regions require special attention in POI array-CGH studies? While array-CGH assesses the entire genome, particular attention should be paid to the X chromosome, given its established role in POI pathogenesis. However, research indicates that submicroscopic X chromosomal CNVs may play a more limited role than previously hypothesized, with one large study finding no major association between Xq21.3 CNVs and POI after rigorous validation [29]. This underscores the importance of genome-wide analysis rather than targeted X chromosome assessment.
Q5: How can the limitations of array-CGH regarding balanced rearrangements be addressed in POI research? Array-CGH cannot detect balanced translocations or inversions, which represent a known limitation for comprehensive genetic assessment [25]. In POI research, where these balanced rearrangements can contribute to pathogenesis, complementary karyotyping should be performed alongside array-CGH, particularly for patients with syndromic features or family histories suggestive of chromosomal rearrangements.
Essential Research Reagent Solutions
Table 3: Key Reagents for Array-CGH in POI Research
| Reagent/Kit | Function | Application Notes |
|---|---|---|
| GenomePlex WGA Kit | Whole genome amplification from limited DNA | Enables analysis from 1-100 ng input DNA; crucial for rare POI cohorts [26] |
| BioPrime Total Array CGH System | Genomic DNA labeling with optimized dyes | Reduces channel bias; improves signal-to-noise ratios [27] |
| Agilent Genomic DNA Labeling Kit PLUS | Fluorophore incorporation for hybridization | Compatible with Agilent platform; optimized for 2.0-2.5 μg DNA input [26] |
| Agilent SurePrint G3 CGH Microarrays | High-resolution CNV detection | 4x180K format provides optimal balance of resolution and cost for POI studies [7] |
| BioPrime Total FFPE System | DNA labeling from suboptimal samples | Specifically designed for challenging samples like FFPE tissues [27] |
The strategic implementation of array-CGH technology has fundamentally transformed the research landscape for idiopathic Premature Ovarian Insufficiency, moving a substantial proportion of cases from the idiopathic category to genetically explained diagnoses. Through attention to experimental design considerations, appropriate troubleshooting protocols, and integration with complementary technologies like NGS, researchers can continue to leverage array-CGH to unravel the genetic architecture of POI. The optimization strategies presented in this technical guide address historical limitations of the technology while providing frameworks for enhancing detection accuracy, managing limited samples, and interpreting results in the context of POI pathogenesis. As genetic research progresses, array-CGH remains an essential component in the comprehensive genomic toolkit required to dissect this complex and clinically significant disorder.
Primary Ovarian Insufficiency (POI) is a clinically heterogeneous disorder characterized by the loss of ovarian function before age 40, affecting approximately 1% of the female population [7] [30]. Despite established associations with genetic, autoimmune, and iatrogenic factors, the etiology of POI remains elusive in a significant proportion of cases, classified as idiopathic. Genetic causes account for an estimated 20-25% of POI cases, but this figure is likely an underestimation given the limitations of previous diagnostic approaches [31]. The transition to Next-Generation Sequencing (NGS) technologies has revolutionized the molecular diagnosis of idiopathic POI, enabling simultaneous analysis of multiple known and candidate genes. This technical guide explores the implementation, optimization, and troubleshooting of NGS panels within the context of POI research, providing a framework for researchers and clinical scientists to enhance diagnostic yield and expand our understanding of the genetic architecture underlying this complex disorder.
Technical Foundation: NGS Panel Design and Workflow
Core Components of an NGS Panel for POI Research
Table 1: Essential Research Reagent Solutions for POI NGS Studies
| Reagent Category | Specific Examples | Research Function |
|---|---|---|
| Library Preparation | Ion Plus Fragment Library Kit, SureSelect XT-HS reagents, HaloPlex Target Enrichment System | Fragments and prepares genomic DNA for sequencing with adapter ligation and barcode incorporation |
| Target Enrichment | Custom Ampliseq Panels, SurePrint G3 CGH Microarray, Haloplex ICCG panel | Selectively captures genomic regions of interest to enrich POI-associated genes |
| Sequencing | Ion Torrent PGM System, Illumina NextSeq 500, Ion S5 Sequencing Kit | Performs massively parallel sequencing of enriched libraries |
| Variant Calling | Torrent Variant Caller, GATK Unified Genotyper, SAMtools | Identifies sequence variations from aligned sequencing data |
| Variant Annotation | Ion Reporter, Varsome, Ensembl VEP | Characterizes identified variants with population frequency and functional impact data |
Standardized Experimental Protocol for POI Gene Panel Sequencing
The following protocol outlines a standardized approach for NGS panel sequencing in POI research, compiled from multiple established methodologies [7] [32] [33]:
DNA Extraction and Quality Control: Extract genomic DNA from peripheral blood using validated extraction kits (e.g., QIAsymphony DNA midi kits). Quantify DNA using fluorometric methods (e.g., Quant-iT PicoGreen) and assess quality via spectrophotometry. Input requirement: 50-225 ng of high-quality DNA (A260/A280 ratio of 1.8-2.0).
Library Preparation: Utilize targeted amplification (e.g., Ion AmpliSeq Library Kit Plus) or hybrid capture-based (e.g., SureSelectXT) approaches. For amplification-based methods, employ multiplexed PCR with target-specific primers covering exonic regions and splice sites of POI-associated genes. Incubation conditions: 99°C for 2 minutes, followed by 19 cycles of 99°C for 15 seconds and 60°C for 4 minutes.
Template Preparation and Sequencing: Perform emulsion PCR (Ion Torrent) or bridge amplification (Illumina) depending on platform specification. For Ion Torrent systems, enrich template-positive Ion Sphere Particles using the Ion OneTouch ES system. Sequence enriched libraries on appropriate platforms (Ion PGM, Illumina NextSeq) using manufacturer-recommended sequencing kits.
Bioinformatic Analysis Pipeline:
- Base Calling and Demultiplexing: Use platform-specific software (Torrent Suite, MiSeq Reporter).
- Sequence Alignment: Map reads to reference genome (hg19/GRCh37) using optimized aligners (TMAP, BWA-MEM).
- Variant Calling: Identify SNPs, indels using variant callers (Torrent Variant Caller, GATK UnifiedGenotyper) with minimum coverage depth of 30x.
- Variant Annotation and Filtering: Annotate variants using curated databases (gnomAD, ClinVar, HGMD) and prediction algorithms (SIFT, PolyPhen-2, CADD).
Figure 1: End-to-End Workflow for NGS Panel Analysis in POI Research
Troubleshooting Guide: Addressing Common Experimental Challenges
Low Coverage and Incomplete Target Enrichment
Problem: Inadequate sequencing depth (<30x) for critical regions, resulting in potential missed variants.
Solutions:
- Verify DNA Input Quality: Degraded DNA or insufficient input quantity directly impacts library complexity. Always use fluorometric quantification rather than spectrophotometry alone.
- Optimize Hybridization Conditions: For capture-based approaches, increase hybridization time to 16+ hours and optimize temperature conditions [34].
- Amplification Bias Mitigation: For amplicon-based approaches, increase the number of PCR cycles (up to 21) while monitoring for duplicate rate increases.
- Supplement with Sanger Sequencing: As implemented in multiple studies, regions with persistent poor coverage (<30x) should be supplemented with Sanger sequencing to ensure comprehensive variant detection [35].
Preventive Measures:
- Regular calibration of enrichment equipment
- Implementation of unique molecular identifiers (UMIs) to correct for amplification biases
- Use of control samples with known variant profiles in each sequencing run
Variant Interpretation and Classification Challenges
Problem: High number of variants of uncertain significance (VUS) complicating clinical interpretation and reporting.
Solutions:
- Implement Tiered Filtering Strategy:
- Filter against population databases (gnomAD) with frequency threshold <0.1%
- Retain protein-altering variants (nonsense, frameshift, splice-site, missense)
- Apply in silico prediction tools (MetaSVM, CADD, DANN) with conservative thresholds [31]
- Prioritize genes with established POI associations and plausible biological mechanisms
- Segregation Analysis: When possible, perform familial segregation studies to establish co-segregation with phenotype [34].
- Functional Validation Pipeline: Establish collaboration networks for functional studies (e.g., luciferase reporter assays for transcriptional effects, as performed for FOXL2 variants) [31].
Table 2: Diagnostic Yields of NGS Panels in POI Research Cohorts
| Study Cohort | Panel Size (Genes) | Patients (n) | Diagnostic Yield | Most Frequently Implicated Genes |
|---|---|---|---|---|
| French Multicenter [30] | 18 | 269 | 25% (pathogenic variants) 38% (including VUS) | NOBOX (9%) |
| Chinese Han [31] | 28 | 500 | 14.4% | FOXL2 (3.2%) |
| Hungarian [32] | 31 | 48 | 16.7% (monogenic) 29.2% (risk factors) | EIF2B, GALT |
| Italian [33] | 295 | 64 | 75% (≥1 variant) | Multiple pathways |
| Amiens University [7] | 163 | 28 | 57.1% (causal CNV/SNV) | FIGLA |
Handling Oligogenic Inheritance and Complex Genetics
Problem: Emerging evidence suggests oligogenic involvement in POI, where multiple variants collectively contribute to phenotype [33].
Solutions:
- Comprehensive Panel Design: Include genes from multiple biological pathways (meiosis, folliculogenesis, DNA repair, hormone signaling) rather than focusing on a single mechanism.
- Burden Testing: Implement statistical approaches to assess variant burden across biological pathways compared to control populations.
- Pathway Integration: Group identified variants by biological processes to identify potential synergistic effects:
- Cell cycle, meiosis, and DNA repair
- Extracellular matrix remodeling
- NOTCH and WNT signaling pathways
- Hormone response and folliculogenesis
Figure 2: Addressing POI Genetic Complexity Through Multipronged Methodological Approaches
Frequently Asked Questions: Technical Considerations for POI Research
Q1: What is the optimal number of genes to include in a POI NGS panel? Panel sizes in published studies vary significantly, from 18 to 295 genes [33] [30]. The optimal size depends on research objectives: smaller panels (15-30 genes) focusing on established POI genes may be sufficient for clinical diagnostics with clearer interpretation, while larger panels (100-300 genes) including research candidates are more appropriate for gene discovery. Consider including genes involved in meiosis, folliculogenesis, DNA repair, and hormone signaling pathways based on recent literature [33].
Q2: How does NGS panel testing compare to exome sequencing for POI genetic diagnosis? NGS panels offer deeper coverage (mean depth >500x vs ~130x for WES) of targeted regions, higher sensitivity for variant detection in known genes, reduced incidental findings, and lower cost per sample [35]. However, exome sequencing enables novel gene discovery and can be re-analyzed as new POI genes are identified. For clinical diagnostics where known POI genes are the primary target, panels are generally preferred, while for research settings with unsolved cases, exome sequencing provides additional value [36] [35].
Q3: What quality control metrics are essential for reliable NGS panel results?
- Pre-sequencing: DNA quality (A260/A280), quantity (fluorometric), and integrity (gel electrophoresis)
- Sequencing: ≥80% bases ≥Q30, >70% on-target reads, mean coverage >100x with >98% of targets ≥30x
- Variant calling: Transition/transversion ratio (~3.0 for whole exome, higher for panels), SNP concordance with known genotypes >99%, sensitivity >99% for known variants [35]
Q4: What are the key considerations for transitioning from research to clinical diagnostic application?
- Establish validated protocols meeting CLIA/CAP standards
- Implement rigorous variant classification according to ACMG/AMP guidelines [7]
- Develop reporting frameworks that appropriately communicate VUS and oligogenic findings
- Establish multidisciplinary review teams including clinical geneticists, genetic counselors, and reproductive endocrinologists
- Create systems for periodic re-analysis and updating of variant classifications as new evidence emerges
Q5: How should we approach the increasing evidence of oligogenic inheritance in POI? Recent studies indicate that 10-15% of POI cases may involve oligogenic contributions [33] [31]. Research approaches should include:
- Analysis of variant burden across biological pathways
- Statistical tests for gene-gene interactions
- Functional validation of combinatorial effects
- Development of scoring systems that account for cumulative variant impact
- Consideration of digenic inheritance models, as demonstrated for MSH4/MSH5 [31]
The implementation of NGS panels has dramatically improved our understanding of the genetic architecture of Primary Ovarian Insufficiency, moving beyond monogenic models to recognize the contributions of oligogenic inheritance, gene-environment interactions, and complex genetic risk profiles. The technical frameworks and troubleshooting guides presented here provide researchers with practical tools to enhance their molecular studies of idiopathic POI. As our knowledge of POI genetics continues to expand, iterative refinement of NGS panels—incorporating new gene discoveries while maintaining analytical robustness—will be essential to unravel the remaining diagnostic challenges. Through standardized methodologies, comprehensive bioinformatic analysis, and thoughtful interpretation of genetic findings, the research community can accelerate progress toward precision medicine approaches for this complex reproductive disorder.
Premature Ovarian Insufficiency (POI) is a clinically heterogeneous disorder characterized by the loss of ovarian function before age 40, affecting approximately 1-3.7% of women [1] [33]. Despite advancing diagnostic capabilities, a significant portion of cases—historically up to 70%—remain classified as idiopathic, presenting a substantial challenge for researchers and clinicians alike [7] [37]. The complex genetic architecture of POI, encompassing chromosomal abnormalities, single gene disorders, and oligogenic influences, necessitates a multifaceted diagnostic approach [33].
Recent studies demonstrate that combining Array Comparative Genomic Hybridization (Array-CGH) and Next-Generation Sequencing (NGS) provides a powerful strategy for elucidating the genetic etiology of idiopathic POI. This technical guide explores the implementation of this combined approach, addressing common experimental challenges and providing troubleshooting resources to maximize diagnostic yield in research settings.
Technical Foundations: How Array-CGH and NGS Complement Each Other
Array-CGH and NGS target different but complementary types of genetic variation in POI research:
Array-CGH detects copy number variations (CNVs) - structural alterations ranging from 60 kb to several Mb that can encompass entire genes or regulatory regions. In POI, clinically significant CNVs often involve the X chromosome or contain genes critical for ovarian function [7].
NGS (typically using targeted gene panels) identifies single nucleotide variants (SNVs) and small insertions/deletions (indels) in a predefined set of candidate genes. These include genes involved in folliculogenesis, meiosis, DNA repair, and ovarian development [7] [33].
The technologies work synergistically: Array-CGH captures larger genomic rearrangements that NGS might miss, while NGS pinpoints subtle sequence changes undetectable by Array-CGH.
Experimental Workflow Integration
The combined experimental workflow proceeds through several critical stages, each with specific quality control checkpoints, as illustrated below:
Key Research Reagent Solutions
Successful implementation of the combined Array-CGH and NGS approach requires specific laboratory reagents and platforms. The table below details essential materials and their functions based on published methodologies:
| Reagent Category | Specific Product/Platform | Research Function | Key Considerations |
|---|---|---|---|
| DNA Extraction | QIAsymphony DNA midi kits (Qiagen) | High-quality DNA extraction from peripheral blood | Ensure DNA integrity for both platforms; minimal degradation |
| Array-CGH Platform | SurePrint G3 Human CGH Microarray 4×180K (Agilent) | Genome-wide CNV detection | 60 kb minimum resolution; optimized for POI-related regions |
| NGS Capture | SureSelect XT-HS custom capture (Agilent) | Target enrichment of POI genes | Custom designs of 163-295 genes common in POI research |
| NGS Sequencing | NextSeq 550/500 systems (Illumina) | High-throughput sequencing | 90% target coverage at 50× minimum depth recommended |
| Analysis Software | CytoGenomics, Cartagenia Bench Lab CNV, Alissa Interpret | Variant annotation/classification | ACMG guidelines for pathogenicity assessment |
Diagnostic Performance Data
Recent studies employing the combined Array-CGH and NGS approach have demonstrated significantly improved diagnostic yields for idiopathic POI:
| Study Population | Array-CGH Diagnostic Yield | NGS Diagnostic Yield | Combined Diagnostic Yield | Key Findings |
|---|---|---|---|---|
| 28 idiopathic POI patients [7] | 14.3% (4/28 patients) | 28.6% (8/28 patients) | 57.1% (16/28 patients) | 75% yield in primary amenorrhea subgroup |
| 64 early-onset POI patients [33] | Not separately reported | Not separately reported | 75% (48/64 patients with ≥1 variant) | Oligogenic patterns observed (2-6 variants per patient) |
| Variant Type Distribution [7] | Causal CNVs: 3.6% (1/28) | Causal SNVs/Indels: 28.6% (8/28) | VUS Findings: 25.0% (7/28) | Multiple VUS complicate interpretation |
Frequently Asked Questions (FAQ) for Researchers
Q1: What is the optimal gene panel size for NGS in POI research? A: Current studies utilize panels ranging from 163 to 295 genes [7] [33]. The optimal size balances comprehensive coverage with manageable data interpretation. Larger panels (250-300 genes) are preferable for discovery research, while smaller, validated panels (150-200 genes) may suffice for clinical application. Include genes involved in folliculogenesis, meiosis, DNA repair, and ovarian development.
Q2: How should we handle variants of uncertain significance (VUS) in reporting? A: VUS are common in POI research (25% of cases in recent studies) [7]. Document all VUS findings but clearly distinguish them from pathogenic variants in reports. Use multiple prediction algorithms and population frequency databases for assessment. Family segregation studies can help reclassify VUS when possible.
Q3: What quality metrics are critical for NGS data in POI studies? A: Ensure >90% of target bases are covered at ≥50× depth [33]. Monitor sequencing uniformity (≥80% of targets covered at 20% mean coverage), and include positive controls for known variant types. For Array-CGH, establish clear thresholds for CNV calling based on control samples.
Q4: How does the combined approach address POI's oligogenic nature? A: Emerging evidence suggests POI often involves multiple variants in interacting genes [33]. The combined approach enables detection of both CNVs and SNVs/indels that may act cumulatively. Patients with more severe phenotypes often carry higher numbers of pathogenic variants across different genes.
Q5: What are the specific bioinformatic challenges in integrating Array-CGH and NGS data? A: Key challenges include: (1) reconciling different coordinate systems and genome builds; (2) distinguishing pathogenic CNVs from benign polymorphisms using population databases; (3) interpreting the combined effect of multiple variant types; and (4) visualizing complex results for clinical interpretation.
Troubleshooting Guide for Common Experimental Issues
| Problem | Potential Causes | Solutions | Prevention Strategies |
|---|---|---|---|
| Low DNA yield affecting both platforms | Suboptimal blood collection, degradation during storage | Use whole genome amplification methods; prioritize NGS if limited DNA | Extract DNA within 48h of collection; use specialized DNA stabilization tubes |
| Array-CGH showing excessive noise | DNA degradation, poor labeling efficiency, batch effects | Repeat with fresh DNA; optimize labeling protocol; use different array batch | Quality control DNA before proceeding (A260/280 ratio >1.8, minimal degradation) |
| NGS with uneven coverage | Poor capture efficiency, PCR duplicates, GC bias | Optimize hybridization conditions; include unique molecular identifiers; adjust GC-rich protocols | Use updated capture kits; fragment DNA to optimal size (200-300bp) |
| Inconsistent variant calling | Different bioinformatic pipelines, low-quality reads | Standardize pipeline parameters; implement joint calling; increase coverage depth | Establish reproducible workflows; use version-controlled pipelines |
| Difficulty interpreting multiple VUS | Limited population data, unclear functional impact | Implement functional studies; seek collaboration for segregation analysis; use gene-specific literature | Use conservative reporting; document evidence for each classification |
Biological Pathways Implicated in POI
The genetic landscape of POI reveals involvement of multiple critical biological pathways, with the combined Array-CGH/NGS approach detecting disruptions at multiple levels:
The combined application of Array-CGH and NGS represents a significant advancement in idiopathic POI research, increasing diagnostic yields from traditional rates below 30% to over 50-75% in recent studies [7] [33]. This approach effectively addresses the complex genetic architecture of POI, which encompasses diverse variant types from large chromosomal rearrangements to subtle sequence changes.
For research implementation, success depends on: (1) careful quality control at each experimental step; (2) utilization of comprehensive gene panels; (3) integration of bioinformatic analyses; and (4) systematic interpretation of combined findings. Future developments will likely include more standardized variant classification frameworks, expanded gene panels incorporating newly discovered candidates, and improved functional validation protocols.
As evidence grows for the oligogenic nature of POI [33], the combined Array-CGH and NGS approach will remain essential for unraveling the complex genetic interactions underlying this clinically heterogeneous condition. Researchers should consider this dual-platform strategy as a foundational element in POI diagnostic research programs.
Premature Ovarian Insufficiency (POI) is a highly heterogeneous disorder characterized by the loss of ovarian function before age 40, affecting approximately 3.5% of women globally [4] [38]. A significant challenge in POI management has been the high percentage of cases historically classified as idiopathic, where no specific cause could be identified despite comprehensive clinical evaluation. Recent advances in genetic technologies, particularly next-generation sequencing (NGS) and array-based comparative genomic hybridization (array-CGH), have dramatically improved our ability to identify pathogenic variants in previously unexplained cases [1] [37].
This case study analysis examines how modern genetic approaches are reshaping our understanding of POI etiology by uncovering molecular diagnoses in cohorts once deemed idiopathic. We explore the technical methodologies enabling these discoveries, present quantitative findings from recent studies, and provide practical guidance for researchers navigating the challenges of POI genetic diagnosis.
Technical FAQs: Addressing Key Methodological Challenges
What is the current diagnostic yield from genetic investigations of idiopathic POI?
The diagnostic yield from genetic investigations has improved significantly with advanced technologies. The table below summarizes findings from recent studies:
| Study Cohort | Sample Size | Primary Genetic Method | Overall Diagnostic Yield | Key Findings |
|---|---|---|---|---|
| French idiopathic POI cohort [37] | 28 patients | Combined array-CGH + NGS (163-gene panel) | 57.1% (16/28 patients) | • 14.3% with causal CNVs• 28.6% with causal SNVs/indels• 75% diagnostic yield in primary amenorrhea subgroup |
| Large-scale Chinese cohort [9] | 1,030 patients | Whole-exome sequencing | 23.5% (242/1,030 patients) | • 18.7% with P/LP variants in known genes• 4.8% with variants in 20 novel candidate genes• 25.8% diagnostic yield in primary vs. 17.8% in secondary amenorrhea |
| Turkish POI cohort [39] | 68 patients | Targeted NGS (26-gene panel) | 5.9% (4/68 patients) | • 1 likely pathogenic variant (STAG3)• 3 VUS in NOBOX and GDF9 genes• First genetic epidemiology study in Turkish population |
How have etiological patterns changed with improved genetic diagnosis?
Recent evidence demonstrates a substantial shift in the etiological landscape of POI. A comparative analysis between historical (1978-2003) and contemporary (2017-2024) cohorts from a single tertiary center revealed statistically significant changes (p < 0.05) in etiology distribution [1]:
| Etiological Category | Historical Cohort (n=172) | Contemporary Cohort (n=111) | Change |
|---|---|---|---|
| Genetic | 11.6% | 9.9% | -1.7% |
| Autoimmune | 8.7% | 18.9% | +10.2% |
| Iatrogenic | 7.6% | 34.2% | +26.6% |
| Idiopathic | 72.1% | 36.9% | -35.2% |
This fourfold increase in identifiable iatrogenic cases and halving of idiopathic POI demonstrates how enhanced diagnostic capabilities, alongside changing clinical factors (such as improved survival after oncologic treatments), have reshaped our understanding of POI causation [1].
What are the key methodological considerations for optimal genetic diagnosis?
Experimental Protocol: Comprehensive Genetic Testing Workflow
Sample Preparation and Quality Control
- Collect peripheral blood samples in EDTA tubes (minimum 2ml) [37] [39]
- Extract genomic DNA using commercial kits (e.g., QIAsymphony DNA midi kits)
- Quantify DNA concentration and purity (A260/A280 ratio >1.8)
- Ensure DNA integrity (minimum 50ng/μL concentration)
Multi-Technique Genetic Analysis
- Array-CGH for CNV Detection
- Platform: SurePrint G3 Human CGH Microarray 4×180K [37]
- Detection threshold: CNVs ≥60kb
- Analysis software: CytoGenomics v5.0 with Cartagenia Bench Lab CNV
- Key targets: X-chromosome abnormalities, known POI-associated regions
- Next-Generation Sequencing
Bioinformatic Analysis and Variant Interpretation
- Alignment: Burrows-Wheeler Aligner (BWA) or similar
- Variant calling: GATK best practices
- Annotation: gnomAD, ClinVar, HGMD, population-specific databases
- Pathogenicity assessment: ACMG/AMP guidelines [37] [9]
- Functional prediction: PolyPhen-2, SIFT, CADD scores
Troubleshooting Common Experimental Challenges
Low Diagnostic Yield Despite Comprehensive Testing
Problem: Limited identification of pathogenic variants despite using NGS approaches.
Solution Strategies:
- Expand genetic targets: Move beyond known POI genes to include novel candidates identified in large-scale studies [9]. Recent research has identified 20 new POI-associated genes involved in gonadogenesis (LGR4, PRDM1), meiosis (CPEB1, KASH5, MCMDC2), and folliculogenesis (ALOX12, BMP6, ZP3).
- Implement multi-omics approaches: Integrate genomic data with transcriptomic and epigenetic analyses. Studies show distinct DNA methylation patterns in ovarian granular cells of women with diminished ovarian reserve [2].
- Consider oligogenic inheritance: Evaluate potential compound effects of variants in multiple genes. Evidence suggests cumulative effects of genetic defects may influence POI severity, particularly in primary amenorrhea [9].
Interpretation of Variants of Uncertain Significance (VUS)
Problem: High frequency of VUS findings complicating clinical translation.
Solution Framework:
- Functional validation: Implement experimental assays to assess variant impact:
- For missense variants: Protein structure modeling and in vitro functional studies
- For putative loss-of-function variants: Sanger sequencing confirmation and minigene splicing assays [9]
- Familial segregation studies: Test variant presence in affected and unaffected family members
- Population frequency filtering: Compare against ethnically-matched control databases
- Computational prediction concordance: Require multiple algorithms (SIFT, PolyPhen-2, CADD) to support pathogenicity
Technical Artifacts and Platform-Specific Limitations
Problem: False positives/negatives due to methodological constraints.
Quality Control Measures:
- Array-CGH: Validate all potentially pathogenic CNVs with alternative method (qPCR or MLPA)
- NGS: Implement orthogonal validation (Sanger sequencing) for reported pathogenic variants
- Coverage gaps: Supplement with targeted sequencing of poorly captured regions
- Platform comparison: Consider that different NGS capture kits may have varying efficiency for GC-rich regions
Research Reagent Solutions: Essential Materials for POI Genetic Studies
| Reagent Category | Specific Product/Platform | Application in POI Research | Key Considerations |
|---|---|---|---|
| DNA Extraction | QIAsymphony DNA midi kits [37] | High-quality genomic DNA preparation | Ensure high molecular weight DNA for array-CGH |
| Array-CGH | SurePrint G3 Human CGH Microarray 4×180K [37] | Genome-wide CNV detection | 60kb resolution sufficient for known POI-associated CNVs |
| Targeted Enrichment | SureSelect XT-HS Custom Capture [37] | Gene panel sequencing | Custom designs should include 80+ known POI genes |
| NGS Sequencing | Illumina NextSeq 550/MiSeq [37] [39] | High-throughput sequencing | MiSeq suitable for panels, NextSeq for WES |
| Variant Annotation | Alissa Interpret v5.3 [37] | Clinical-grade variant interpretation | Integrates ACMG guidelines and population databases |
| Functional Prediction | PolyPhen-2, SIFT, CADD [9] [39] | In silico pathogenicity assessment | Use multiple algorithms for consensus |
| Variant Validation | Sanger Sequencing | Orthogonal confirmation | Essential for reporting pathogenic variants |
Future Directions and Conceptual Framework
The genetic architecture of POI is increasingly recognized as complex, involving monogenic, oligogenic, and potentially polygenic components. Large-scale sequencing studies have demonstrated that nearly one-quarter of POI cases harbor pathogenic genetic variants, with higher yields in primary amenorrhea and familial cases [9]. The continued reduction of idiopathic cases through genetic advances is reshaping both clinical practice and research priorities.
The remaining unexplained cases represent the next frontier in POI research, likely involving:
- Non-coding variants in regulatory regions
- Somatic mosaicism not detectable in blood DNA
- Epigenetic modifications affecting gene expression
- Gene-environment interactions with environmental toxicants [2]
- Oligogenic inheritance with threshold effects
For researchers, the imperative is to continue expanding genetic investigations while developing functional validation pipelines to interpret the growing number of variants discovered through high-throughput sequencing approaches.
Premature Ovarian Insufficiency (POI) is a clinically heterogeneous disorder characterized by the loss of ovarian activity before age 40, affecting approximately 1-3.5% of women [1] [4]. Despite advances in genetic testing, the etiology of POI remains elusive in a significant number of cases. While whole exome sequencing focuses on the protein-coding 1-2% of the genome [40] [41], the vast non-coding genome and mitochondrial DNA (mtDNA) represent crucial frontiers for explaining the "missing heritability" of idiopathic POI. This technical support center provides specialized guidance for researchers investigating these complex genomic regions within POI pathology.
FAQs: The Non-Coding Genome and mtDNA in POI Research
1. Why should POI researchers investigate regions beyond the exome? Despite the known genetic contribution to POI, a substantial diagnostic gap remains. One study of idiopathic POI patients found that 57.1% had a detectable genetic anomaly when assessed with array-CGH and next-generation sequencing, yet 28.6% of patients in that cohort still carried variants of uncertain significance (VUS) [37]. The non-coding genome, which constitutes approximately 98% of our DNA [42], is rich in regulatory elements like enhancers and non-coding RNAs (ncRNAs) that govern crucial processes in ovarian development and function. Overlooking this region means missing potential key regulators of genes implicated in folliculogenesis, meiosis, and DNA repair.
2. What types of functional elements in the non-coding genome are most relevant to POI? Two primary classes of non-coding elements are of significant interest:
- Cis-regulatory elements (e.g., Enhancers): These distal regulatory sequences can be located upstream, downstream, or within introns of genes and control temporal and tissue-specific transcriptional activity via long-distance interactions with promoters [40]. Their disruption has been linked to various neurodevelopmental disorders, providing a model for investigating similar mechanisms in POI.
- Non-coding RNAs (ncRNAs): These RNA molecules, which include microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), are pivotal epigenetic regulators of gene and protein expression [42] [41]. They can influence mRNA stability, translation, and chromatin remodeling—processes critical for maintaining the ovarian follicular reserve.
3. What are the common pitfalls in mitochondrial DNA analysis for POI studies? mtDNA is particularly prone to sequencing artifacts and errors that can compromise data integrity. Common issues include:
- Phantom Mutations: These are artifactual base calls, often G→C or C→G transversions, generated during the sequencing process itself due to suboptimal sequencing chemistry or capillary array performance [43].
- Documentation and Base-Shift Errors: Manual errors during data entry, editing, or alignment can introduce mistakes [44].
- Low Penetrance and Heteroplasmy: The relationship between an mtDNA variant and a phenotype like POI can be complex, influenced by the percentage of mutant mtDNA (heteroplasmy) and threshold effects, making definitive causal links challenging.
4. How has the etiological landscape of POI changed, and what does this mean for genetic research? The relative prevalence of POI causes has shifted significantly. A comparison of historical (1978-2003) and contemporary (2017-2024) cohorts reveals a more than fourfold increase in identifiable iatrogenic causes (from 7.6% to 34.2%) and a doubling of autoimmune cases (from 8.7% to 18.9%). Consequently, the proportion of idiopathic cases has halved (from 72.1% to 36.9%) [1]. This underscores that while clinical factors are increasingly identified, a substantial portion of "idiopathic" POI likely has a genetic basis residing in the non-coding genome or mtDNA.
5. What tools are available for identifying conserved non-coding elements? Specialized software and databases exist to align and identify functional non-coding regions, which often rearrange and conserve function without maintaining linear sequence alignment.
- MULAN (MUltiple sequence Local AligNment): This tool performs multiple sequence local alignment and visualization, ideal for identifying patches of conservation that may be in a different order or orientation, such as enhancer elements [45].
- Genomicus & UCNEbase: These browsers and databases help explore synteny (conserved gene order) and identify Ultra-Conserved Non-coding Elements (UCNEs) within genomic regulatory blocks [45].
Troubleshooting Guides
Guide 1: Addressing Non-Coding Sequence Alignment Challenges
Problem: Standard alignment tools (e.g., BLAST) fail to identify conserved non-coding elements because functional conservation persists despite sequence rearrangement, inversion, or fragmentation.
Solution: Utilize tools designed for local alignment and synteny conservation.
- Step 1: Use MULAN for multi-species local alignment.
- Protocol: Input sequence data from several species for the same genomic locus (e.g., a gene of interest plus ~5kb of upstream and downstream sequence). Ensure all exons in the region are annotated. MULAN performs pairwise comparisons against a reference species to find conserved patches, highlighting their position on the reference sequence [45].
- Step 2: Validate findings using a synteny-based browser like Genomicus.
- Protocol: Select your gene and species of interest. Genomicus will generate a phylogenetic tree and display surrounding genes conserved in synteny. Enable the "CNE" (Conserved Non-coding Elements) view to visualize areas of non-coding conservation among the syntenic genes [45].
- Step 3: Consult UCNEbase for pre-computed data on ultra-conserved non-coding elements and genomic regulatory blocks across many model species [45].
Interpretation: A conserved non-coding element identified by MULAN and located within a region of conserved synteny by Genomicus is a high-priority candidate for functional validation in the context of POI.
Guide 2: Preventing and Detecting mtDNA Sequencing Errors
Problem: mtDNA sequencing data contains artifacts and phantom mutations, leading to false positives and incorrect haplogroup assignment, which can mislead association studies with POI.
Solution: Implement a rigorous quality control pipeline.
- Step 1: Prophylaxis During Sequencing
- Step 2: Post-Sequencing Error Detection
- Check for an over-representation of transversions. mtDNA evolves primarily through transitions; a high transversion rate in your dataset can indicate technical artifacts [44].
- Perform phylogenetic analysis. Place each new sequence within the known mtDNA phylogeny. Any mutation that does not fit the expected pattern for its haplogroup is a potential error [44].
- Screen for known problematic sites. Check positions like 500, 7927, 7985, 14160, 14460, 14974, and 16239, which have been previously identified as hotspots for phantom mutations [43].
- Step 3: Database Screening
- Search for reported mutations in existing literature and databases like MITOMAP. Check if combinations of mutations in your sequence are previously documented [44].
Interpretation: A sequence that fits cleanly into the established phylogenetic tree and lacks over-represented transversions is of high quality and suitable for further analysis in POI studies.
Experimental Protocols & Workflows
Workflow 1: Identifying and Validating a Non-Coding Regulatory Element
This workflow integrates computational and experimental methods to link a non-coding variant to POI pathogenesis.
1. Identification & Prioritization:
- Input: WGS data from a cohort of idiopathic POI patients and controls.
- Analysis: Perform an association analysis to identify variants in non-coding regions significantly enriched in the POI cohort.
- Filtering: Use tools like INFERNO to infer the molecular mechanisms of non-coding variants [40]. Prioritize variants that:
- Fall within chromatin marks (e.g., H3K27ac) indicative of active enhancers in ovarian tissue.
- Are located in regions conserved across species (using MULAN/UCNEbase).
- Reside in the topological associating domain (TAD) of a gene known to be involved in ovarian function.
2. Functional Validation (Massively Parallel Reporter Assay - MPRA):
- Objective: To test hundreds to thousands of candidate sequences for enhancer activity simultaneously.
- Protocol: a. Cloning: Synthesize oligonucleotides containing the candidate regulatory sequence (both reference and variant alleles) and clone them into a reporter vector upstream of a minimal promoter and a fluorescent reporter gene. b. Transfection: Introduce the pooled library of constructs into a relevant cell line (e.g., a granulosa cell line). c. Sequencing & Analysis: After 48 hours, harvest cells, extract genomic DNA and RNA, and perform high-throughput sequencing. Compare the abundance of each regulatory element in the DNA (input) to its abundance in the RNA (output). A higher RNA/DNA ratio indicates stronger enhancer activity. A significant difference in activity between the reference and variant alleles suggests a functional impact [40].
3. In-depth Mechanistic Study (CRISPR-Cas9):
- Objective: To study the function of the validated regulatory element in its native genomic context.
- Protocol: Use CRISPR-Cas9 to delete or alter the specific enhancer element in a cell model. Follow up with assays to measure:
- Expression of the putative target gene (via qPCR or RNA-seq).
- Chromatin conformation (e.g., 3C or 4C) to confirm physical looping to the gene's promoter.
- Changes in the local epigenomic landscape (via ChIP-seq for histone marks).
Workflow 2: A Rigorous mtDNA Analysis Pipeline for POI
This protocol outlines a comprehensive approach to generate high-quality, clinically relevant mtDNA data.
1. Wet-Lab Sequencing:
- Long-Range PCR & NGS: Amplify the entire ~16.5kb mtDNA genome using long-range PCR. Fragment the amplicons and prepare libraries for deep sequencing on a platform like Illumina MiSeq/NextSeq. Aim for high coverage (>1000x) to reliably detect heteroplasmy [37].
2. Bioinformatics & Quality Control (QC):
- Alignment & Variant Calling: Map reads to the revised Cambridge Reference Sequence (rCRS) using a dedicated mtDNA-aware aligner.
- QC Steps: a. Heteroplasmy Thresholding: Set a minimum variant allele frequency (e.g., 2-5%) to filter low-level sequencing noise. b. Phantom Mutation Check: Cross-reference all variants, especially transversions, against a list of known artifact-prone sites [43] [44]. c. Phylogenetic Tree Placement: Use software like HaploGrep to assign a haplogroup. Manually inspect any sequence that does not cleanly fit its designated haplogroup.
3. Data Interpretation & Reporting:
- Pathogenicity Assessment: For identified homoplasmic or high-heteroplasmy variants, use criteria such as:
- Evolutionary conservation.
- Presence in established pathogenic variant databases (e.g., MITOMAP).
- Predicted impact on protein structure or tRNA secondary structure.
- Previous reports of association with a relevant phenotype.
- Segregation Analysis: Whenever possible, test for the variant in maternal relatives to confirm inheritance and correlate with phenotype.
Data Presentation
Table 1: Diagnostic Yields from Genetic Testing in a Contemporary POI Cohort
This table summarizes the findings from a 2025 study of 28 idiopathic POI patients, illustrating the contribution of modern genetic techniques. The overall diagnostic yield was 57.1% [37].
| Genetic Technique | Pathogenic/Likely Pathogenic Findings | Variants of Uncertain Significance (VUS) | Key Findings / Implicated Genes |
|---|---|---|---|
| Array-CGH | 1 patient (3.6%) | 3 patients (10.7%) | Pathogenic 15q25.2 microdeletion (CPEB1). VUS involved SLCO3A1, NAIP, FANCB. |
| Next-Generation Sequencing (NGS) | 8 patients (28.6%) | 5 patients (17.9%) | Pathogenic variants in FIGLA, GALT, TWNK, POLG, ERCC6, MCM9. |
| Combined Diagnostic Yield | 9 patients (32.1%) | 7 patients (25.0%) | 57.1% of idiopathic cases had a causal genetic variant or VUS. |
Table 2: Common mtDNA Sequencing Errors and Detection Strategies
This table classifies frequent mtDNA artifacts and provides practical solutions for their identification and prevention [43] [44].
| Error Type | Description | Common Sites | Detection & Prevention Strategies |
|---|---|---|---|
| Phantom Mutations (Type III) | Artifactual base calls from sequencing process. | nt 500, 7927, 7985, 14160, 14460, 14974, 16239. | Visual electropherogram inspection; phylogenetic analysis; screen for G→C/C→G transversions. |
| Reference Bias (Type II) | Overlooking nucleotides that differ from the reference sequence. | Variable. | Double-blind manual review; use of updated reference sequences. |
| Base Shift (Type I) | Mis-scoring due to alignment or reading shifts. | Variable. | Careful manual data entry and table preparation; independent verification. |
| Documentation Errors | Mistakes during data entry or editing. | Variable. | Implement a strict protocol for data handling and cross-verification. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Non-Coding and mtDNA Research in POI
| Tool / Reagent | Function | Example Use in POI Research |
|---|---|---|
| MULAN Software | Multiple sequence local alignment and visualization. | Identifying conserved enhancer elements near POI candidate genes (e.g., NOBOX, GDF9) across species [45]. |
| Massively Parallel Reporter Assay (MPRA) | High-throughput functional screening of non-coding variants. | Testing the enhancer activity of hundreds of non-coding variants identified in a POI WGS cohort [40]. |
| CRISPR-Cas9 System | Precise genome editing for functional validation. | Knocking out a candidate enhancer in a granulosa cell line to study its effect on target gene expression [40]. |
| Long-Range PCR Kit | Amplification of the entire mitochondrial genome. | Preparing mtDNA for high-coverage NGS sequencing to detect low-level heteroplasmy in POI patients [37]. |
| UCNEbase / Genomicus | Databases for Ultra-Conserved Non-coding Elements and synteny. | Determining if a non-coding variant lies within a conserved regulatory block linked to a known POI gene [45]. |
| mtDNA Phylogenetic Tools (e.g., HaploGrep) | Automated haplogroup classification. | Placing a new mtDNA sequence into the phylogenetic tree to check for consistency and flag potential errors [44]. |
| Antide | Antide | Gonadotropin-Releasing Hormone Antagonist | Antide is a potent GnRH antagonist for endocrine and cancer research. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
| YM-26734 | YM 26734 | Selective 5-HT2B Antagonist | RUO | YM 26734 is a potent and selective 5-HT2B receptor antagonist for cardiovascular and fibrosis research. For Research Use Only. Not for human or veterinary use. |
Navigating Pitfalls in Test Interpretation and Clinical Application
FAQs: Navigating VUS in Idiopathic POI Research
What is a Variant of Uncertain Significance (VUS)? A VUS is a genetic variant for which there is not enough scientific evidence to classify it as either disease-causing (pathogenic) or harmless (benign) [46]. It is a finding of uncertainty, not a confirmed diagnosis [47].
How common are VUS results in genetic testing for POI? With multi-gene panel testing, the chance of finding a VUS increases. For instance, while a BRCA1/2 analysis has a 1-3% VUS rate, a 25-gene panel can have a VUS rate of 30% or more [48]. In POI, which involves over 75 candidate genes, the potential for VUS findings is significant [6] [1].
Should a VUS be used for clinical decision-making? No. Professional guidelines, such as those from the American College of Medical Genetics and Genomics, specify that "a variant of uncertain significance should not be used in clinical decision-making" [47]. Clinical management should be based on personal and family history.
How can a VUS be reclassified? Reclassification requires gathering more evidence. Key strategies for researchers include:
- Phenotypic Data: Correlating the variant with highly specific clinical presentations [49].
- Segregation Studies: Tracing the variant in affected and unaffected family members [48] [50].
- Population Data: Determining the variant's frequency in large population databases [49] [47].
- Functional Studies: Conducting experiments to assess the variant's biological impact [50].
- Data Sharing: Contributing findings to public databases like ClinVar [47].
What is the typical outcome of VUS reclassification? The vast majority of reclassified VUS are downgraded to benign. One study found that 91% of reclassified variants were deemed "benign/likely benign," while only 9% were upgraded to "pathogenic/likely pathogenic" [47].
Troubleshooting Guides: Addressing Common VUS Challenges
Challenge 1: Interpreting a VUS Finding in a POI Cohort
Problem: A VUS is identified in a novel gene in a patient with idiopathic POI. Its pathogenicity is unknown.
Methodological Guide:
- Systematic Reassessment: Apply the latest variant interpretation guidelines. The 2015 ACMG/AMP guidelines provide a baseline, but newer, quantitative frameworks like the ClinGen point-based system can offer greater reclassification power [49].
- Leverage Phenotype Specificity (PP4): For genes with a strong, specific link to POI, the phenotypic evidence can be weighted more heavily. Recent ClinGen guidance allows for assigning higher pathogenicity scores when a patient's phenotype is highly specific to the gene in question [49].
- Utilize Computational Prediction Tools: Incorporate in silico prediction scores (e.g., REVEL ≥0.7, SpliceAI ≥0.2) as supporting evidence (PP3) [49].
- Check Population Frequency: Apply the PM2 criterion if the variant is absent from population databases (e.g., gnomAD) [49].
Visual Guide: VUS Interpretation Workflow The following diagram outlines the logical workflow for interpreting a VUS finding.
Challenge 2: Designing a Study to Resolve Idiopathic POI VUS
Problem: A high burden of VUS findings in idiopathic POI cases is hindering gene discovery and clinical translation.
Methodological Guide:
- Cohort Aggregation: Assemble a large, well-phenotyped cohort of idiopathic POI patients. A recent meta-analysis suggests a global POI prevalence of 3.7%, providing a substantial potential study population [6].
- Define Phenotype Rigorously: Use consistent diagnostic criteria. The ESHRE guideline recommends diagnosing POI in women under 40 with irregular cycles and an elevated FSH level >25 IU/L on one occasion [4].
- Implement Genomic Analyses:
- Functional Validation: For top VUS candidates, proceed to in vitro or in vivo functional assays to demonstrate a direct impact on ovarian function.
Visual Guide: Idiopathic POI Research Framework This diagram illustrates the strategic framework for researching VUS in idiopathic POI.
Table 1: Etiological Spectrum of Premature Ovarian Insufficiency (POI)
This table compares the distribution of causes between a historical and a contemporary cohort, highlighting the shift in idiopathic cases and the stable, significant role of genetics [1].
| Etiology | Historical Cohort (1978-2003) (n=172) | Contemporary Cohort (2017-2024) (n=111) |
|---|---|---|
| Genetic | 11.6% | 9.9% |
| Autoimmune | 8.7% | 18.9% |
| Iatrogenic | 7.6% | 34.2% |
| Idiopathic | 72.1% | 36.9% |
Table 2: VUS Reclassification Outcomes in Tumor Suppressor Genes
This table demonstrates the impact of applying updated classification criteria (new ClinGen PP1/PP4) on VUS reclassification rates in a study of seven tumor suppressor genes [49].
| Gene | Unique VUS Assessed | VUS Reclassified as Likely Pathogenic (New Criteria) | Reclassification Rate |
|---|---|---|---|
| STK11 | 9 | 8 | 88.9% |
| NF1 | 39 | 12 | 30.8% |
| TSC2 | 17 | 5 | 29.4% |
| FH | 11 | 3 | 27.3% |
| Overall | 101 | 32 | 31.4% |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for VUS Investigation in POI Research
| Research Reagent / Tool | Function in VUS Research |
|---|---|
| Illumina NGS Systems (e.g., NovaSeq 6000, NextSeq 550) | High-throughput sequencing to identify variants across multiple candidate genes or the entire exome/genome [49]. |
| Sanger Sequencing (ABI 3730xl DNA Analyzer) | Gold-standard method for validating variants discovered by NGS and for testing family members in segregation analyses [49]. |
| Multiplex Ligation-dependent Probe Amplification (MLPA) | Detects exon-level deletions or duplications that may be missed by sequencing, a known mechanism in POI-related genes [49]. |
| Computational Prediction Tools (REVEL, SpliceAI) | In silico analysis to predict the potential functional impact of a missense or splice-site variant, providing supporting evidence for pathogenicity [49]. |
| Population Databases (gnomAD) | Determines the frequency of a variant in the general population; rarity supports further investigation (PM2 criterion) [49]. |
| Variant Databases (ClinVar) | A public archive of reports on genotype-phenotype relationships, crucial for finding other cases with the same VUS [50]. |
| Deltorphin I | Deltorphin I | High-Purity Delta Opioid Receptor Agonist |
| BU224 hydrochloride | 2-(4,5-dihydro-1H-imidazol-2-yl)quinoline;hydrochloride |
Premature Ovarian Insufficiency (POI) is a clinically heterogeneous condition characterized by the loss of ovarian function before age 40, affecting approximately 3.5% of women [4] [51]. Despite advances in genetic testing, a significant diagnostic gap persists, with 70% of POI cases initially classified as idiopathic [37]. This high rate of unexplained cases presents major challenges for researchers and clinicians in distinguishing pathogenic genetic variants from benign findings, directly impacting patient counseling, prognosis, and the development of targeted therapies.
The etiological landscape of POI is shifting. Recent comparative studies between historical (1978-2003) and contemporary (2017-2024) cohorts reveal a more than fourfold increase in identifiable iatrogenic causes (from 7.6% to 34.2%) and a doubling of autoimmune cases (from 8.7% to 18.9%), resulting in idiopathic POI being halved (from 72.1% to 36.9%) [1]. This transformation underscores the critical need for refined genetic diagnostic protocols to further reduce the idiopathic category and improve clinical management.
Quantitative Landscape: POI Etiological Distribution and Diagnostic Yields
Contemporary Etiological Distribution of POI
Table 1: Current prevalence of POI etiologies based on contemporary cohort data (2017-2024)
| Etiology | Prevalence (%) | Key Characteristics |
|---|---|---|
| Idiopathic | 36.9% | Decreasing due to improved diagnostics |
| Iatrogenic | 34.2% | Rising due to improved oncologic treatments and gynecologic surgeries |
| Autoimmune | 18.9% | Hashimoto's thyroiditis most common association |
| Genetic | 9.9% | Remained stable prevalence; numerous genes involved |
Source: [1]
Genetic Diagnostic Yield in Idiopathic POI
Table 2: Diagnostic yield of genetic investigations in idiopathic POI
| Testing Methodology | Patient Cohort | Diagnostic Yield | Key Findings |
|---|---|---|---|
| Combined array-CGH + NGS | 28 idiopathic POI patients | 57.1% (16/28 patients) | 1 causal CNV, 8 causal SNV/indel variations, 7 VUS |
| Array-CGH alone | Same cohort | 14.3% (4/28 patients) | 1 pathogenic CNV, 3 VUS |
| NGS alone (163-gene panel) | Same cohort | 46.5% (13/28 patients) | 8 pathogenic/likely pathogenic variants, 5 VUS |
| Primary Amenorrhea (PA) subgroup | 4 PA patients | 75% (3/4 patients) | Higher yield in PA vs secondary amenorrhea |
| Familial POI history | 11 patients | 45% (5/11 patients) | Moderate increase in diagnostic yield |
Source: [37]
FAQs: Troubleshooting Genetic Interpretation in Idiopathic POI Research
How do I resolve variants of uncertain significance (VUS) in POI research?
Challenge: VUS constitute a major interpretation bottleneck, occurring in 25% (7/28) of idiopathic POI cases in recent studies [37].
Solution: Implement a multi-modal validation framework:
- Functional assays: For genes involved in folliculogenesis (FIGLA, BMP15, GDF9), develop in vitro oocyte maturation assays
- Family segregation studies: Track variant inheritance patterns in affected and unaffected family members
- Population frequency filtering: Compare against ethnically matched control databases (gnomAD)
- Computational prediction: Utilize multiple in silico tools (SIFT, PolyPhen-2, CADD) with consistent results
- Literature curation: Maintain updated knowledgebase of newly reported variants in POI-associated genes
Protocol: Functional Validation for VUS in Meiosis Genes
- Clone candidate variant into appropriate expression vector
- Transfer into mammalian oocyte cell line or mouse oocytes
- Assess meiotic progression via immunostaining for synaptonemal complexes
- Quantify DNA repair efficiency following induced double-strand breaks
- Compare against wild-type controls and known pathogenic variants
Why does my genetic testing panel miss causal variants in idiopathic POI?
Challenge: Standard gene panels capture only known POI genes, while novel candidates continue to be identified.
Solution: Employ complementary technologies:
- Array-CGH detects copy number variations (CNVs) missed by NGS: In one study, array-CGH identified a pathogenic 15q25.2 microdeletion containing CPEB1 that would be missed by sequence-based approaches alone [37]
- Whole exome/genome sequencing reveals variants in novel genes beyond standardized panels
- Repeat expansion analysis specifically for FMR1 premutation (55-200 CGG repeats), which accounts for substantial portion of genetic POI
Protocol: Comprehensive Genetic Testing Workflow for Idiopathic POI
- Initial screening: Karyotype and FMR1 premutation testing
- Chromosomal microarray analysis for CNVs (resolution ≥60 kb)
- Targeted NGS panel of known POI genes (minimum 163 genes)
- Research-based WES for negative cases with strong family history
- Functional validation of novel candidates using animal models or cell systems
How do I distinguish true pathogenic variants from population polymorphisms?
Challenge: Benign polymorphisms are frequently misclassified as pathogenic, leading to false positive results.
Solution: Apply ACMG variant interpretation guidelines with POI-specific modifications:
- Population frequency threshold: <0.1% in gnomAD for recessive, <0.001% for dominant inheritance
- Functional evidence: Prioritize variants affecting genes with established roles in ovarian biology
- Hotspot awareness: Recognize mutation clusters in genes like FSHR, BMP15
- Informed consent: Communicate limitations of testing and possibility of VUS identification
Why is there variability in genetic testing implementation for POI?
Challenge: Knowledge gaps persist among healthcare providers, particularly regarding FMR1 testing guidelines.
Solution: Standardize testing indications and provider education:
- FMR1 testing: Recommended for all women with POI regardless of family history [52]
- Specialty collaboration: Involvement of genetic counselors improves testing appropriateness and interpretation [52]
- Educational interventions: Focus on general OBGYNs as first points of contact for POI symptoms
Visualizing Genetic Analysis Workflows
Genetic Analysis Workflow for POI
Diagram 1: Comprehensive genetic analysis workflow for idiopathic POI
Variant Interpretation and Classification Pathway
Diagram 2: Variant interpretation and classification pathway
Research Reagent Solutions for POI Genetic Studies
Table 3: Essential research reagents and materials for POI genetic investigation
| Reagent/Material | Function/Application | Specifications/Alternatives |
|---|---|---|
| Custom NGS Panel | Targeted sequencing of POI-associated genes | 163+ genes covering oogenesis, folliculogenesis, meiosis, DNA repair |
| Array-CGH Platform | Genome-wide CNV detection | 4×180K format, minimum 60 kb resolution (Agilent Technologies) |
| DNA Extraction Kit | High-quality DNA from peripheral blood | QIAsymphony DNA midi kits (Qiagen) |
| Bioinformatics Software | Variant calling and annotation | Alissa Align&Call v1.1 + Alissa Interpret v5.3 (Agilent) |
| CNV Analysis Tool | Interpretation of copy number variations | Cartagenia Bench Lab CNV v5.1 (Agilent) |
| Variant Databases | Pathogenicity assessment and frequency data | gnomAD, DECIPHER, ClinGen, HGMD, ClinVar |
| Functional Assay Systems | Validation of VUS pathogenicity | In vitro oocyte models, meiotic progression assays |
The integration of multiple genetic technologies significantly improves the diagnostic yield in idiopathic POI, with combined array-CGH and NGS approaches identifying causal variants in over 57% of previously unexplained cases [37]. However, variant interpretation remains challenging, with approximately 25% of cases yielding VUS that require functional validation. Future directions must focus on standardizing variant interpretation protocols, expanding gene panels as new candidates are discovered, and developing high-throughput functional assays to resolve VUS. For researchers and drug development professionals, these advances in genetic diagnosis create opportunities for targeted therapeutic development and personalized management approaches for this complex condition.
Challenges in Oligogenic and Digenic Inheritance Model Interpretation
FAQs: Understanding Genetic Complexity in Idiopathic POI
1. What is the difference between monogenic, digenic, and oligogenic inheritance? In monogenic inheritance, a variant in a single gene is both necessary and sufficient to cause disease. Digenic inheritance involves variants in two genes that interact to produce a disease, which neither variant causes alone. Oligogenic inheritance extends this concept to include variants in a small number of genes. In idiopathic POI, what appears to be a single-gene disorder may actually be modified by variants in other genes, leading to variable expressivity and incomplete penetrance [54] [55].
2. Why might a researcher suspect a digenic/oligogenic model in a case of idiopathic POI? Several clues point to a more complex genetic model:
- Variable expressivity: Patients with the same primary mutation show stark differences in phenotypic severity, age-of-onset, or rate of progression [54].
- Reduced penetrance: Individuals carrying a known pathogenic variant do not develop the disease [55].
- Familial clustering: A high prevalence of POI or early menopause among first-degree relatives suggests a strong genetic component that may involve multiple modifiers [6].
- Unsolved monogenic cases: A significant proportion of suspected genetic POI cases remain unexplained under a monogenic model, suggesting more complex genetic architectures [7] [55].
3. What are the common pathomechanisms in digenic inheritance? Digenic interactions can occur through several mechanisms:
- Direct protein-protein interaction: Variants in genes whose products physically interact, such as within the same protein complex (e.g., PRPH2 and ROM1 in retinopathia pigmentosa) [55].
- Indirect functional link: Variants in genes whose products operate within the same biological pathway (e.g., CLCNKA and CLCNKB in Bartter syndrome) [55].
- Epigenetic modification: One variant causes a primary defect, while a variant in a modifier gene alters the epigenetic state, aggravating the phenotype (e.g., SMCHD1 and the D4Z4 repeat in FSHD) [55].
Troubleshooting Guides for Genetic Analysis
Problem: Inconsistent Genotype-Phenotype Correlation
Potential Cause: Undetected genetic modifiers or oligogenic inheritance masking a straightforward monogenic relationship.
Solution:
- Expand Genetic Screening: Move beyond targeted sequencing to whole-exome or whole-genome sequencing (WES/WGS) to identify potential modifier alleles in trans [7] [55].
- Conduct Segregation Analysis: Perform family studies to see if the phenotype co-segregates with haplotypes from multiple loci, not just one [55].
- Statistical & Bioinformatic Re-evaluation:
- For large cohorts: Use association analysis and transmission disequilibrium testing (TDT) to identify genetic modifiers associated with disease severity [54].
- For all cases: Re-analyze sequence data using tools and guidelines that account for the possibility of more than one pathogenic variant [55].
Problem: Negative Finding with Suspected Genetic Cause
Potential Cause: The analysis may be restricted to a single-gene model, missing digenic or oligogenic interactions.
Solution:
- Systematic Digenic Filtering: Implement a bioinformatics pipeline that actively searches for pairs of variants in known or candidate gene pairs that could interact digenically [55].
- Investigate Known Modifier Genes: Focus on genes already implicated as modifiers in your disease of interest. For example, in Bardet-Biedl syndrome, an allele in CCDC28B was identified as a "panmodifier" associated with more severe phenotypes [54].
- Functional Validation: Use in vitro or in vivo models to test the functional impact of candidate variant pairs, confirming their combined effect surpasses the threshold for disease manifestation [54] [55].
Problem: Interpreting Variants of Uncertain Significance (VUS)
Potential Cause: A VUS in one gene may become clinically significant when paired with a variant in another gene.
Solution:
- Look for a Partner Variant: In the presence of a VUS, scrutinize the data for a second variant in a functionally related gene. The combined effect may provide evidence for reclassification [7] [55].
- Leverage Interaction Networks: Use protein-protein interaction databases and known biological pathways to identify genes that are plausible partners for the VUS.
- Review Population Data: Check if the VUS is found at a higher-than-expected frequency in healthy populations, which would argue against a monogenic cause but not necessarily against a digenic contributor [55].
Experimental Protocols for Investigating Complex Inheritance
Protocol 1: Comprehensive Genetic Workup for Idiopathic POI
This protocol combines multiple techniques to maximize the diagnostic yield in idiopathic POI research [7].
- 1. Sample Collection: Collect peripheral blood samples from the proband and available family members. Extract DNA using standard kits (e.g., QIAsymphony DNA midi kits).
- 2. Karyotype and FMR1 Premutation Testing: Perform as first-line tests to rule out common known causes [7] [6].
- 3. Array-CGH Analysis: Identify copy number variations (CNVs) using microarray technology (e.g., Agilent SurePrint G3 Human CGH Microarray 4 × 180 K). Analyze with software like CytoGenomics and Cartagenia Bench Lab CNV.
- Objective: Detect chromosomal rearrangements or deletions/duplications ≥60 kb [7].
- 4. Next-Generation Sequencing (NGS):
- Panel Sequencing: Use a custom capture design targeting a panel of known and candidate POI genes (e.g., 163 genes) [7].
- Whole-Exome/Genome Sequencing: For a hypothesis-free approach, especially in cases negative for panel sequencing.
- Bioinformatics Analysis: Use pipelines (e.g., Alissa Align&Call and Alissa Interpret) for variant calling and annotation [7].
- 5. Variant Classification & Integration: Classify all identified variants (SNVs and CNVs) according to ACMG/AMP guidelines. Integrate findings from steps 3 and 4 to build a comprehensive genetic profile [7] [55].
Protocol 2: Evaluating Digenic Inheritance in Candidate Gene Pairs
This protocol outlines a approach to validate a suspected digenic interaction.
- 1. Gene & Variant Selection: Based on NGS data and bioinformatics filtering, select two candidate genes harboring variants of interest.
- 2. Segregation Analysis: Test for the co-segregation of the variant pair with the disease phenotype in the family. True digenic inheritance is supported if the phenotype manifests only when both variants are present [55].
- 3. Functional Assays:
- For direct protein interactions: Use co-immunoprecipitation (Co-IP) or yeast two-hybrid assays to test if the variants disrupt a physical interaction between the gene products [55].
- For pathway disruption: Use cell-based reporter assays or metabolomic profiling to assess if the combined variants disrupt a shared biological pathway more severely than either variant alone [55].
- 4. Model Organism Studies: Create single- and double-mutant models (e.g., in mice or zebrafish) to recapitulate the digenic phenotype and confirm the genetic interaction in vivo [54].
Research Reagent Solutions
Table 1: Essential materials for investigating oligogenic inheritance in POI.
| Reagent / Material | Function in Research |
|---|---|
| Oligonucleotide array-CGH (e.g., Agilent 180k) [7] | Genome-wide detection of copy number variations (CNVs). |
| NGS Panel Capture (custom POI gene panel) [7] | Targeted sequencing of a curated list of genes associated with ovarian function. |
| Whole Exome/Genome Sequencing Kits [55] | Hypothesis-free sequencing to identify novel candidate genes and modifiers. |
| Variant Annotation & Classification Software (e.g., Alissa Interpret, CytoGenomics) [7] | Automated pipeline for variant calling, annotation, and pathogenicity assessment. |
| Protein-Protein Interaction Assay Kits (e.g., Co-IP, Yeast Two-Hybrid) [55] | Functional validation of suspected direct interactions between gene products. |
| Cell Lines (e.g., HEK293T, Ovarian Granulosa Cell Lines) | In vitro models for conducting functional assays and pathway analysis. |
Visualizing the Genetic Diagnostic Workflow in POI
The following diagram illustrates a logical workflow for genetic analysis of idiopathic POI, incorporating steps to account for oligogenic inheritance.
Visualizing Digenic Inheritance Mechanisms
The diagram below summarizes the primary biological mechanisms that can underlie a digenic inheritance pattern.
FAQs: Navigating Complex Genetic Counseling Scenarios
FAQ 1: How should a diagnosis of idiopathic Premature Ovarian Insufficiency (POI) be communicated when no definitive genetic cause is found?
- Answer: Communicating an idiopathic POI diagnosis requires careful handling to mitigate patient distress. Emphasize that "idiopathic" means the cause is not currently identifiable with available science, not that the condition is not real. Frame it within the context of current research: while the proportion of idiopathic cases has decreased due to improved diagnostics, it remains a significant category, accounting for an estimated 36.9% of contemporary POI cases [1]. Counselors should:
- Acknowledge Uncertainty: Clearly state the limitations of current genetic testing while validating the patient's experience.
- Focus on Management: Redirect the conversation to actionable health management strategies, stressing that a clear etiology is not always necessary for effective treatment [4] [56].
- Provide Hope: Note that research is ongoing, and recommend patients reconnect for updated testing every few years as new genes are identified [57].
FAQ 2: What are the key communication skills required for effective pre-test counseling for POI?
- Answer: Pre-test counseling should be a foundational, non-directive process that sets clear expectations [58]. Essential skills include:
- Discussing Test Performance: Explain the sensitivity, specificity, and positive predictive value of the proposed genetic test(s) [58].
- Outlining Potential Results: Detail the types of results possible, including positive, negative, and variants of uncertain significance (VUS) [58].
- Informing about Risks: Address potential psychosocial impacts, insurance implications (life, disability, long-term care), and the possibility of uncovering non-paternity or consanguinity [58].
FAQ 3: How can counselors support patients in sharing complex genetic results with at-risk family members?
- Answer: Facilitating family communication is a critical counselor role. Strategies include:
- Explicit Encouragement: Strongly encourage patients to share clinically significant results with affected or at-risk relatives [58].
- Providing Resources: Offer to write family letters or provide summary documents that explain the result in accessible language.
- Verbal Motivational Techniques: Use motivational interviewing techniques to help patients overcome barriers to these difficult conversations [59].
FAQ 4: What specific communication challenges arise with the increasing use of multigene panel testing?
- Answer: Multigene panels heighten the complexity of result interpretation and communication. Key challenges include:
- Managing VUS: These tests increase the probability of finding VUS, which are difficult to explain and can cause anxiety without altering medical management [59].
- Interpreting Incidental Findings: Counselors must be prepared to discuss findings that may be outside the primary indication for testing.
- Ensuring Understanding: The volume and complexity of information require exceptional skill in providing clear, patient-centered education [59].
Troubleshooting Guides for Common Scenarios
Scenario: A patient expresses anxiety and confusion upon receiving a Variant of Uncertain Significance (VUS) result.
- Problem: The uncertain result is causing distress rather than providing clarity.
- Solution:
- Normalize the Finding: Explain that a VUS is a common and expected outcome of advanced genetic testing, not an error.
- Use Clear Analogies: Describe a VUS as a "spelling change" in the DNA whose medical impact is currently unknown, much like finding a word in a document you don't know how to pronounce.
- Clarify Clinical Action: Emphasize that medical management should not be based on a VUS alone. The patient should continue with risk management based on their personal and family history.
- Discuss Next Steps: Explain that the laboratory will continue to research the variant and that reclassification can occur. Advise the patient to check back with their genetic counselor periodically for updates [57] [58].
Scenario: A patient with idiopathic POI feels their condition is "not real" because no cause was found.
- Problem: The "idiopathic" label is leading to invalidation of the patient's diagnosis and symptoms.
- Solution:
- Reframe the Diagnosis: Use the established diagnostic criteria for POI (amenorrhea and elevated FSH >25 IU/L) to reinforce the medical validity of their condition, regardless of etiology [4] [1].
- Focus on the Pathophysiology: Explain that POI is a functional problem of the ovary, and the diagnosis is based on its clinical behavior, not just its cause [56].
- Reinforce Health Implications: Discuss the serious long-term health risks associated with POI (e.g., cardiovascular disease, osteoporosis) to underscore the importance of following the treatment plan, which is effective even for idiopathic cases [56].
Quantitative Data on POI Etiology and Diagnosis
| Etiology | Historical Cohort (1978-2003) Prevalence (n=172) | Contemporary Cohort (2017-2024) Prevalence (n=111) | Statistical Significance of Change |
|---|---|---|---|
| Idiopathic | 72.1% | 36.9% | p < 0.05 |
| Iatrogenic | 7.6% | 34.2% | p < 0.05 |
| Autoimmune | 8.7% | 18.9% | p < 0.05 |
| Genetic | 11.6% | 9.9% | Not Significant |
Table 2: Key Diagnostic and Epidemiological Data for POI
| Parameter | Current Guideline or Finding | Source |
|---|---|---|
| POI Prevalence | ~3.5% (higher than historical 1% estimates) | [4] |
| Diagnostic FSH Level | One elevated FSH >25 IU/L is sufficient for diagnosis. | [4] |
| Live Birth Rate | Limited outcomes; 7 live births in a contemporary cohort of 111 patients. | [1] |
Diagnostic and Communication Workflow for Idiopathic POI
The following diagram outlines the integrated diagnostic and communication pathway for a patient with suspected POI, culminating in the management of an idiopathic diagnosis.
Research Reagent Solutions for POI Genetic Research
Table 3: Essential Research Tools for Investigating Idiopathic POI
| Research Reagent / Tool | Function in POI Research |
|---|---|
| Multigene Panel Testing | High-throughput sequencing of known POI-associated genes (e.g., BMP15, GDF9, NOBOX) to identify novel mutations in idiopathic cases [57] [1]. |
| Karyotyping / Chromosomal Microarray | Detection of chromosomal abnormalities, particularly X-chromosome anomalies like Turner syndrome, which are a known genetic cause of POI [1]. |
| FMR1 CGG Repeat Analysis | PCR-based testing to identify fragile X premutation carriers, a common genetic etiology for familial POI [1]. |
| Anti-Müllerian Hormone (AMH) Assay | Used as a biomarker of ovarian reserve; helpful in assessing the continuum of ovarian dysfunction in POI, especially in cases of diagnostic uncertainty [4]. |
| Steroidogenic Cell Autoantibodies | Detecting autoantibodies (e.g., against 21-hydroxylase) to confirm an autoimmune etiology and reduce the pool of idiopathic cases [1]. |
Ethical Considerations and the Potential for Genetic Discrimination
Technical Troubleshooting Guides: Addressing Common Experimental Challenges
Guide: Low Diagnostic Yield in Genetic Sequencing
Problem: Despite performing NGS on idiopathic POI patients, the diagnostic yield of pathogenic variants remains low or inconclusive.
| Possible Cause | Diagnostic Approach | Solution |
|---|---|---|
| Inadequate Gene Panel Coverage | Compare panel content against recently discovered POI-associated genes [9]. | Expand gene panel to include novel candidates (e.g., LGR4, CPEB1, ZP3, KASH5) from recent large-scale studies [9]. |
| Over-reliance on Single-Nucleotide Variants (SNVs) | Analyze sequencing data for Copy Number Variations (CNVs) [37]. | Integrate array-CGH to identify pathogenic CNVs, increasing overall diagnostic yield by 14.3% [37]. |
| High Proportion of Variants of Uncertain Significance (VUS) | Re-analyze VUS using updated population databases (gnomAD) and functional prediction tools [37]. | Employ functional assays (e.g., for homologous recombination repair) to re-classify VUS; one study reclassified 55 of 75 VUS as deleterious [9]. |
| Phenotypic Heterogeneity | Corrogate genotype with amenorrhea type (Primary vs. Secondary) [9]. | Prioritize genetic analysis in patients with Primary Amenorrhea (PA), where genetic contribution is significantly higher (25.8%) than in Secondary Amenorrhea (SA) (17.8%) [9]. |
Guide: Managing Incidental Findings and VUS
Problem: Handling the ethical and clinical implications of unsolicited findings and Variants of Uncertain Significance (VUS).
| Challenge | Consideration | Recommended Action |
|---|---|---|
| Reporting Unsolicited Findings | Respect for patient autonomy and right to information vs. potential for psychological harm [60]. | Develop a pre-test consent protocol detailing the scope of findings that will be reported. Adhere to ACMG guidelines for reporting incidental findings. |
| Interpreting VUS | VUS should not be used for clinical decision-making [37]. | Report VUS with clear explanation of uncertainty. Implement periodic re-analysis pipelines to review VUS as knowledge evolves. |
| Communicating with Patients | Patients may misinterpret VUS as a definitive result [60]. | Use genetic counselors to explain the meaning of VUS, emphasizing that it is not a diagnostic finding and should not cause undue alarm. |
Frequently Asked Questions (FAQs)
Q1: What is the current identifiable genetic contribution to idiopathic POI? The genetic contribution is higher than previously thought. A 2023 large-scale WES study found that pathogenic/likely pathogenic variants in known POI-causative genes account for 18.7% of cases. When novel candidate genes are included, the cumulative genetic contribution rises to 23.5% [9]. Smaller, focused studies using combined array-CGH and NGS panels have reported diagnostic yields as high as 57.1% [37].
Q2: What are the key legal protections against genetic discrimination for my research participants? In the United States, the Genetic Information Nondiscrimination Act (GINA) is the primary federal law. It provides protections in two key areas:
- Health Insurance (Title I): Prohibits health insurers from using genetic information to make eligibility, coverage, underwriting, or premium-setting decisions. They cannot request or require genetic testing [61] [62].
- Employment (Title II): Prevents employers with 15 or more employees from using genetic information in hiring, firing, job assignments, or any other employment decisions [61].
Q3: What are the critical limitations of GINA that I should disclose during informed consent? GINA's protections are not all-encompassing. Key limitations include:
- Does not cover all forms of insurance: It explicitly does not apply to life insurance, long-term care insurance, or disability insurance [61] [62].
- Does not cover all employers: It does not apply to employers with fewer than 15 employees, the U.S. military, or veterans receiving care through the Veterans Health Administration [61] [62].
- Does not cover symptomatic individuals: Protections may not apply once an individual manifests symptoms of a genetic disorder [63].
Q4: How should I structure the informed consent process to adequately address genetic discrimination concerns? The consent process should be transparent and educational [60]. Key elements are:
- Explain GINA: Clearly describe the protections GINA offers, but also its limitations (e.g., no coverage for life insurance) [63] [61].
- Discuss Privacy: Explain how the participant's genetic data and samples will be stored, who will have access, and the security measures in place [60].
- Ensure Autonomy: Affirm the participant's right to withdraw from the study at any time without penalty [60].
Q5: Which ethical principles are most relevant when designing a POI genetic study? Four key principles should guide your research ethics [60]:
- Autonomy: Respecting the participant's right to make an informed decision about testing and the use of their genetic material.
- Privacy: Protecting the participant from unauthorized access to their genetic information.
- Confidentiality: Controlling further disclosure of information generated within the researcher-participant relationship.
- Equity (Justice): Ensuring fair access to the benefits of research and preventing the exploitation of vulnerable populations.
Visualizing Workflows and Relationships
Genetic Analysis & Ethical Review Workflow
GINA Protection Scope Diagram
The Scientist's Toolkit: Research Reagent Solutions
Essential materials and resources for conducting genetic research in idiopathic POI.
| Item | Function/Application in POI Research |
|---|---|
| Custom NGS Gene Panels | Targeted sequencing of known and candidate POI genes. A panel of 163 genes was used to achieve a 46.5% diagnostic yield in one study [37]. |
| Array-CGH | Detection of copy number variations (CNVs) and chromosomal abnormalities, which are a common genetic cause of POI. Contributed to 14.3% of diagnoses in a recent study [37]. |
| Whole-Exome Sequencing (WES) | Hypothesis-free approach to identify novel pathogenic variants and genes in idiopathic POI cohorts. A 2023 WES study of 1,030 patients identified 20 novel candidate genes [9]. |
| ACMG/AMP Guidelines | Standardized framework for classifying sequence variants as Pathogenic, Likely Pathogenic, VUS, Likely Benign, or Benign. Critical for consistent variant interpretation and reporting [9]. |
| Informed Consent Templates | Documents that transparently explain the research purpose, potential risks (including discrimination), data privacy measures, and participant rights, upholding ethical principles of autonomy and confidentiality [60]. |
Validating Genetic Findings and Comparing Diagnostic Frameworks
Premature Ovarian Insufficiency (POI) presents a significant diagnostic challenge, with approximately 70% of cases classified as idiopathic despite extensive clinical evaluation [7]. This diagnostic gap underscores the critical importance of robust functional validation strategies in research settings. The identification of pathogenic genetic variants through next-generation sequencing requires rigorous experimental confirmation to establish causality and elucidate molecular mechanisms [7] [9]. This technical support center addresses the specific methodological challenges researchers face when moving from genetic findings to functionally validated mechanisms in POI research, providing troubleshooting guidance for the most common experimental scenarios encountered in both in vivo and in vitro systems.
FAQs and Troubleshooting Guides for POI Research
Animal Model Selection and Development
Q: What are the key considerations when selecting an appropriate animal model for POI research, particularly for validating genetic findings?
A: The choice of animal model should align with your research question, available resources, and the specific genetic variant or pathway under investigation. Below is a comparative analysis of commonly used POI modeling approaches:
Table 1: Comparison of Premature Ovarian Insufficiency Animal Modeling Methods
| Model Type | Induction Method | Key Advantages | Limitations & Challenges | Best Applications |
|---|---|---|---|---|
| Chemotherapy-Induced (CTX) | Intraperitoneal injection of cyclophosphamide [64] [65] | Simple operation, short modeling cycle, mimics iatrogenic POI [66] | Systemic toxicity, weight fluctuation, higher mortality [64] | Drug efficacy testing, general ovarian damage studies |
| Ultrasound-Guided Ovarian Injection (POI-U) | Direct ovarian injection of CTX under ultrasound guidance [64] | Lower complications, stable weight, higher success rate, localized damage [64] | Technical expertise required, specialized equipment needed [64] | Localized therapeutic interventions, mechanistic studies |
| Genetic Manipulation Models | CRISPR/Cas9, transgenic approaches targeting POI genes [9] | Directly models genetic etiology, high pathological relevance [9] | Time-consuming, expensive, potential embryonic lethality [9] | Validation of specific genetic findings, pathway analysis |
| Autoimmune (ZP3-induced) | Immunization with ZP3 glycoprotein [66] | Models immune-mediated POI, high success rate (80-90%) [66] | Requires antigen preparation, may not represent all idiopathic cases [66] | Autoimmune pathophysiology, immunomodulatory therapies |
Troubleshooting Common Animal Model Issues:
- Problem: High mortality rate in chemotherapy-induced models.
Solution: Implement the ultrasound-guided approach (POI-U) which demonstrates reduced mortality while maintaining modeling efficacy [64]. Optimize dosing based on animal weight and monitor closely post-injection.
Problem: Inconsistent phenotype presentation in genetic models.
- Solution: Conduct comprehensive phenotypic characterization including hormone profiling (FSH, E2, AMH), histological analysis of follicle counts, and fertility assessment to establish penetrance [9] [65].
Functional Validation of Genetic Variants
Q: What integrated experimental approaches are recommended for validating newly identified genetic variants in POI?
A: A multi-level validation strategy combining bioinformatic prediction with experimental confirmation across biological systems provides the most compelling evidence for variant pathogenicity.
Table 2: Tiered Experimental Approach for Genetic Variant Validation
| Validation Tier | Experimental Method | Key Outcome Measures | Technical Considerations |
|---|---|---|---|
| In Silico Analysis | CADD, SIFT, PolyPhen-2, ACMG guidelines [9] | Pathogenicity prediction, conservation scores | Use multiple algorithms; PHRED-scaled CADD >20 suggests pathogenicity [9] |
| In Vitro Functional Assays | Plasmid transfection, primary cell culture, Western blot, qRT-PCR [65] | Protein expression, localization, functional activity | Use appropriate cell lines (granulosa cells, theca cells); confirm variant expression |
| Ex Vivo Analysis | Ovarian tissue culture, histology, immunohistochemistry [7] | Follicle development, cell-specific protein expression | Optimize culture conditions; use multiple staining markers |
| In Vivo Modeling | Transgenic mouse models, xenograft studies [65] | Ovarian function, fertility assessment, hormone levels | Consider temporal control of gene expression; monitor full reproductive lifespan |
Troubleshooting Genetic Validation Challenges:
- Problem: Variant of Uncertain Significance (VUS) with conflicting computational predictions.
Solution: Implement functional assays specific to gene function. For DNA repair genes (e.g., MCM8, MCM9, HFM1), assess DNA damage response; for metabolic genes, evaluate specific enzymatic activity [9]. The 2023 Nature Medicine study successfully reclassified 38 VUSs through functional studies [9].
Problem: Modeling oligogenic inheritance where multiple variants contribute to phenotype.
- Solution: Utilize multi-het animal models or combinatorial cell culture approaches to assess additive/synergistic effects, as approximately 7.3% of POI cases show multiple pathogenic variants [9].
Stem Cell and Exosome Therapeutic Validation
Q: What methodologies and quality controls are essential when investigating stem cell or exosome-based therapies for POI?
A: Rigorous characterization of cellular materials and standardized delivery protocols are fundamental for generating reproducible therapeutic data.
Experimental Protocol: hUC-MSC Exosome Isolation and Ovarian Function Assessment
hUC-MSC Characterization:
Exosome Isolation and Characterization:
- Iscrete exosomes from conditioned media using ultracentrifugation or commercial kits
- Characterize by electron microscopy, nanoparticle tracking analysis, and Western blot for exosomal markers (CD63, CD81, TSG101) [64]
Therapeutic Administration:
Functional Assessment:
Diagram 1: hUMSC Exosome Mechanism in POI Recovery
Troubleshooting Stem Cell and Exosome Experiments:
- Problem: Low engraftment efficiency of transplanted stem cells.
Solution: Utilize exosome derivatives rather than whole cells, as they demonstrate therapeutic efficacy with reduced engraftment concerns [64]. Consider hydrogel-based delivery systems for improved retention.
Problem: Inconsistent therapeutic outcomes across experiments.
- Solution: Standardize exosome dosing by particle number or protein content rather than volume alone. Implement rigorous quality control batches and monitor animal hormone baseline variations.
Molecular Pathway Analysis
Q: How can researchers effectively map and validate signaling pathways implicated in POI pathogenesis?
A: Integrated approaches combining genetic, biochemical, and pharmacological methods provide the most comprehensive pathway validation.
Experimental Protocol: Mitochondrial Dynamics Assessment in Theca Cells
Establish In Vitro POI Model:
- Treat theca cells with 4-hydroperoxy cyclophosphamide (active metabolite of CTX) or specific pathway inhibitors [65]
- Confirm cytotoxicity via MTT assay and apoptosis via caspase-3 activation
Mitochondrial Function Analysis:
- Assess mitochondrial membrane potential using JC-1 staining (shift from red to green fluorescence indicates depolarization) [65]
- Measure ATP production using luciferase-based assays
- Evaluate reactive oxygen species using DCFDA fluorescence
Mitochondrial Dynamics Quantification:
- Analyze fusion/fission protein expression via Western blot (Mfn1, Mfn2, Drp1, OPA1) [65]
- Visualize mitochondrial morphology using Mitotracker Red and confocal microscopy
- Quantify mitochondrial network complexity using ImageJ plugins
Pathway Modulation:
Diagram 2: Mitochondrial Dysfunction Pathway in POI
Troubleshooting Pathway Analysis:
- Problem: Difficulty distinguishing primary pathway defects from secondary consequences.
Solution: Implement temporal analyses early in disease progression and use multiple complementary approaches (genetic, pharmacological, biochemical). For mitochondrial studies, assess parameters at multiple time points after CTX exposure [65].
Problem: Translational disconnect between in vitro findings and in vivo relevance.
- Solution: Validate in vitro findings using tissue-specific knockout models and human ovarian tissue explants when possible. Correlate molecular changes with functional ovarian parameters.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for POI Investigation
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| POI Modeling Compounds | Cyclophosphamide (CTX), Busulfan, ZP3 peptide [64] [66] | Induction of ovarian insufficiency in animal models | CTX: 75mg/kg initial + 4mg/kg daily maintenance [65] |
| Pathway Inhibitors/Activators | SB216763 (GSK3β inhibitor), Phosphoramide mustard (active CTX metabolite) [65] | Mechanistic studies of specific signaling pathways | Validate specificity with multiple complementary inhibitors |
| Cell Isolation & Culture | Theca cell medium, granulosa cell isolation kits, ovarian tissue digestion enzymes [65] | In vitro modeling of ovarian cell function | Confirm cell identity via marker expression (CYP17A1 for theca cells) |
| Antibodies for Ovarian Analysis | StAR, 17βHSD, PHB (steroidogenesis); Mfn1, Mfn2, Drp1 (mitochondria); GSK3β (signaling) [65] | Protein expression analysis via Western blot, IHC, IF | Optimize for specific species; validate with knockout controls |
| Hormone Assay Kits | FSH, E2, AMH, testosterone, LH ELISA kits [65] | Assessment of endocrine function | Establish standard curves; run duplicates; consider pulsatile secretion |
The functional validation strategies outlined in this technical resource provide a framework for addressing the critical challenges in idiopathic POI research. As genetic findings continue to expand, with recent studies identifying pathogenic variants in approximately 23.5% of POI cases through comprehensive sequencing approaches [9], the need for standardized, reproducible validation methodologies becomes increasingly urgent. By implementing these troubleshooting guides, experimental protocols, and analytical frameworks, researchers can strengthen the translational pathway from genetic discovery to mechanistic understanding, ultimately contributing to improved diagnostic and therapeutic strategies for this complex condition.
Premature Ovarian Insufficiency (POI) is a clinically heterogeneous condition characterized by the loss of ovarian function before age 40, affecting approximately 1-3.7% of women and representing a significant cause of female infertility [22] [4] [8]. Despite advances in genetic testing, the etiology of POI remains elusive in a substantial proportion of cases, classified as "idiopathic." Historically, up to 70% of POI cases were classified as idiopathic [37]. Recent research using next-generation sequencing (NGS) has dramatically improved our understanding, with genetic causes now identified in 20-29.3% of cases in large cohorts [22] [9]. This technical guide addresses the specific bioinformatic challenges in variant prioritization for idiopathic POI research, providing troubleshooting guidance for researchers and clinicians working to unravel the genetic complexity of this condition.
FAQs: Technical Challenges in POI Variant Prioritization
FAQ 1: What are the key population genomics databases for variant filtering in POI research, and how should they be utilized?
Answer: Population databases are essential for filtering common polymorphisms from rare, potentially pathogenic variants in POI research. The following table summarizes the core databases and their specific applications:
Table 1: Essential Population Genomic Databases for POI Research
| Database | Primary Utility | Key Considerations for POI |
|---|---|---|
| gnomAD [67] | Allele frequency filtering for rare variants; constraint scores for gene intolerance | Critical for excluding benign variants prevalent in general populations; v2 (GRCh37) preferred for exome analysis |
| ClinVar [68] | Curated database of variant pathogenicity assertions | Contains known POI-related variants but many novel findings will be absent |
| DECIPHER [37] | Database of genomic variation and phenotype data | Useful for assessing copy number variants (CNVs) and their phenotypic correlations |
| HGMD [68] | Catalog of disease-associated variants | Requires subscription; useful for known pathogenic mutations |
Troubleshooting Tip: Researchers often over-filter variants using population databases. For POI, which has genetic heterogeneity and likely undiscovered genes, consider a minor allele frequency (MAF) threshold <0.1% (or <0.01% for stronger filtering) rather than complete exclusion of all population variants. Be cautious of variants completely absent from gnomAD, as each individual carries ~27 novel coding variants on average [67].
FAQ 2: What specific gene constraint metrics are most informative for POI gene discovery?
Answer: Gene constraint metrics quantify how tolerant a gene is to functional variation, with intolerant genes being strong candidates for monogenic disorders. The pLI score (probability of being loss-of-function intolerant) is particularly valuable:
- pLI ≥ 0.9: Gene is extremely intolerant to LoF variants - strong candidate for POI
- pLI 0.1-0.9: Moderate constraint - consider with other evidence
- pLI ≤ 0.1: Tolerant to LoF variants - lower priority
Troubleshooting Tip: When discovering novel POI genes, combine constraint metrics with expression data from ovarian tissue. A gene with high constraint (pLI > 0.9) AND high ovarian expression represents a high-priority candidate. Remember that some established POI genes may not show extreme constraint due to partial redundancy or other biological factors.
FAQ 3: How should we approach the challenge of variants of uncertain significance (VUS) in POI genes?
Answer: VUS present a significant interpretation challenge in clinical POI diagnostics. A recent large-scale study addressed this by functionally validating 75 VUS, resulting in 55 variants (73.3%) being confirmed as deleterious and 38 being reclassified from VUS to likely pathogenic [9]. Implement this systematic approach:
- Prioritize VUS in known POI genes with strong functional evidence
- Apply ACMG/AMP guidelines with POI-specific modifications
- Utilize segregation analysis in family members when available
- Seek functional validation through collaboration with specialized labs
Troubleshooting Tip: For idiopathic POI cases where initial targeted testing is negative, consider expanding to whole exome sequencing. One study found a 57.1% diagnostic yield using combined array-CGH and NGS of 163 ovarian function genes in idiopathic POI patients [37].
FAQ 4: What are the common pitfalls in variant prioritization for idiopathic POI?
Answer: Common pitfalls include:
- Over-reliance on automated filtering without manual curation
- Insufficient consideration of complex inheritance patterns (digenic, oligogenic)
- Neglecting non-coding variants and structural variants
- Population bias in reference databases affecting frequency filtering
- Under-prioritizing genes without previous POI associations
Troubleshooting Tip: Implement a tiered review system. Tier 1: Variants in established POI genes; Tier 2: Variants in novel genes with strong biological plausibility; Tier 3: Remaining rare variants in constrained genes. This ensures systematic review while managing the variant load effectively.
Experimental Protocols for Variant Prioritization in POI
Protocol 1: Comprehensive Variant Filtering Workflow for POI
Table 2: Step-by-Step Variant Filtering Protocol
| Step | Filter | Parameters | Rationale |
|---|---|---|---|
| 1 | Quality Filter | GQ ≥ 20, DP ≥ 10, VQSR PASS | Ensures variant calling reliability |
| 2 | Population Frequency | gnomAD MAF < 0.001 | Filters common polymorphisms |
| 3 | Inheritance Pattern | De novo, recessive, X-linked based on pedigree | Matches variant effect to family structure |
| 4 | Impact Prediction | CADD > 20, Revel > 0.5 | Prioritizes biologically impactful variants |
| 5 | Gene Constraint | pLI > 0.9 for LoF variants | Identifies genes intolerant to variation |
| 6 | Phenotype Correlation | HPO term matching (e.g., HP:0008193) | Ensures clinical relevance |
This workflow enabled the identification of pathogenic variants in 23.5% of 1,030 POI patients in a recent large-scale study [9].
Protocol 2: Multi-Modal Genetic Testing Strategy for Idiopathic POI
For optimal diagnostic yield in idiopathic POI, implement this sequential testing strategy:
- Karyotype and FMR1 premutation testing (established first-line tests)
- Array-CGH for copy number variants (CNVs)
- Targeted NGS gene panels (88-163 POI-associated genes)
- Whole exome sequencing with analysis of both known and candidate genes
- Whole genome sequencing for non-coding variants (research setting)
A recent study implementing this approach achieved a 29.3% diagnostic yield in 375 POI patients [22]. The distribution of genetic abnormalities in POI cohorts is summarized below:
Table 3: Genetic Findings in Recent POI Cohort Studies
| Study | Cohort Size | Diagnostic Yield | Key Genetic Findings |
|---|---|---|---|
| Mouaret et al. (2022) [22] | 375 patients | 29.3% | Identified 9 novel POI genes and confirmed 13 others |
| Qin et al. (2022) [37] | 28 idiopathic patients | 57.1% | Combined array-CGH and NGS improved diagnosis |
| Wang et al. (2023) [9] | 1,030 patients | 23.5% | 20 novel POI-associated genes identified |
Visualizing Variant Prioritization Workflows
Diagram 1: Comprehensive Variant Prioritization Strategy for Idiopathic POI
Diagram 2: Etiological Spectrum and Research Focus in POI
The Scientist's Toolkit: Essential Research Reagents and Databases
Table 4: Key Research Reagents and Computational Tools for POI Genetics
| Tool/Resource | Type | Specific Application in POI Research |
|---|---|---|
| gnomAD Browser [67] | Population Database | Allele frequency filtering; constraint metrics for novel gene discovery |
| Custom NGS Panels [22] [37] | Wet-bench Reagent | Targeted sequencing of 88-163 known POI genes |
| ACMG/AMP Guidelines [68] | Classification Framework | Standardized variant pathogenicity assessment |
| HPO Terms [68] | Phenotype Ontology | Standardized phenotype data (e.g., HP:0008193 for POI) |
| Array-CGH [37] | Cytogenetic Tool | Detection of CNVs in idiopathic POI cases |
| seqr [68] | Analysis Platform | Family-based monogenic disease analysis |
| CRISPR Models | Functional Tool | In vitro validation of candidate variants in ovarian cell lines |
The evolving etiological landscape of POI—with idiopathic cases decreasing from 72.1% to 36.9% in contemporary cohorts [1]—demonstrates the profound impact of advanced genetic technologies. However, significant challenges remain in variant interpretation, particularly for the ~40% of cases still lacking a molecular diagnosis. Through implementation of the systematic variant prioritization strategies, troubleshooting guides, and experimental protocols outlined in this technical resource, researchers can accelerate the discovery of novel POI genes and mechanisms. The integration of population genomics, functional validation, and phenotype-genotype correlation will continue to bridge the diagnostic gap in idiopathic POI, ultimately enabling personalized management and genetic counseling for affected women and their families.
Comparative Analysis of International Clinical Guidelines for POI Genetic Testing
Premature Ovarian Insufficiency (POI) is a clinically heterogeneous disorder characterized by the loss of ovarian function before age 40, affecting approximately 3.5-3.7% of women globally [4] [56] [9]. The condition presents significant diagnostic challenges, with a substantial proportion of cases remaining idiopathic despite advances in genetic understanding. International clinical guidelines have evolved to address the complex genetic landscape of POI, which involves chromosomal abnormalities, single-gene disorders, and polygenic factors. The 2024 evidence-based guideline represents a collaborative effort by major societies including the European Society of Human Reproduction and Embryology (ESHRE), the American Society for Reproductive Medicine (ASRM), and the International Menopause Society (IMS), providing 145 recommendations across diagnosis, management, and genetic evaluation [4] [69] [70]. This technical analysis examines the comparative frameworks for genetic testing in POI, addressing key implementation challenges for researchers and clinical laboratories.
International Guideline Comparison
Diagnostic Criteria and Genetic Testing Indications
Table 1: Comparative Diagnostic Criteria and Genetic Testing Triggers Across Guidelines
| Guideline Source | Primary Diagnostic Criteria | Genetic Testing Indications | Special Populations |
|---|---|---|---|
| ESHRE/ASRM/IMS (2024) | Single FSH >25 IU/L with 4+ months amenorrhea/irregular cycles [4] [70] | All diagnosed cases; strong family history; associated syndromic features [4] | Primary amenorrhea; Turner syndrome features; FMR1 premutation risk [4] |
| Clinical Research Studies | FSH >25 IU/L on two occasions + amenorrhea [9] [37] | Idiopathic POI after exclusion of other causes; family history [37] | Primary amenorrhea (higher genetic yield); consanguineous families [9] |
Recommended Genetic Testing Modalities and Yields
Table 2: Genetic Testing Approaches and Diagnostic Yields
| Testing Method | Recommended For | Detection Yield | Key Genes/Anomalies Identified |
|---|---|---|---|
| Karyotype/Chromosomal Analysis | All POI patients [4] [6] | 4-5% (Turner syndrome) [71] | X-chromosome abnormalities; structural rearrangements [6] |
| FMR1 Premutation Testing | All POI patients [4] [71] | 2-5% [72] [71] | CGG trinucleotide repeats (55-199) [71] |
| Array-CGH | Idiopathic POI after normal karyotype [37] | 14.3% [37] | CNVs (e.g., 15q25.2 microdeletion/CPEB1) [37] |
| Gene Panel NGS/WES | Idiopathic POI; family history; primary amenorrhea [9] [37] | 20-25% (up to 57.1% in combined approaches) [9] [37] | Pathogenic variants in 79+ genes (e.g., NR5A1, MCM9, FIGLA) [9] [37] |
Technical Support Center
Frequently Asked Questions (FAQs)
What is the minimum genetic testing workup recommended for a new POI diagnosis? The 2024 international guidelines recommend a tiered approach. The initial workup must include standard karyotyping and FMR1 premutation testing for all diagnosed patients, regardless of family history or presentation type. These tests identify the most common genetic causes, with chromosomal abnormalities affecting approximately 4-5% of POI patients and FMR1 premutations accounting for 2-5% of cases [4] [71]. This baseline screening is crucial as it identifies conditions with implications beyond fertility, such as the risk of transmitting fragile X syndrome to offspring or associated health concerns in Turner syndrome [72] [71].
How should we approach the 70-90% of POI cases currently classified as idiopathic? For cases remaining idiopathic after initial workup, comprehensive genetic testing using next-generation sequencing is recommended. Recent studies employing NGS gene panels or whole-exome sequencing have identified pathogenic variants in known POI genes in 18.7-23.5% of cases, with higher yields in primary amenorrhea (25.8%) compared to secondary amenorrhea (17.8%) [9] [37]. The 2024 guidelines support NGS implementation while acknowledging the need for further validation of emerging gene-disease relationships. For clinical laboratories, a targeted panel of 80-160 well-curated POI-associated genes provides optimal balance between coverage and interpretability [9] [37].
What is the evidence for oligogenic inheritance in POI, and how does this impact testing strategies? Growing evidence supports an oligogenic model in which combinations of variants across multiple genes contribute to POI pathogenesis. One large-scale WES study found that 7.3% of patients with genetic findings carried multiple pathogenic variants in different genes [9]. This has important implications for genetic testing strategies, as comprehensive gene panels or whole-exome sequencing are more likely to detect these additive effects than single-gene tests. Laboratories should implement analysis pipelines that consider potential compound heterozygosity and digenic inheritance, particularly for genes involved in shared biological pathways such as meiosis and DNA repair [9] [6].
How do genetic testing yields differ between primary and secondary amenorrhea presentations? Significant differences exist in genetic detection rates between clinical presentations. Patients with primary amenorrhea show substantially higher genetic diagnostic yields (25.8%) compared to those with secondary amenorrhea (17.8%) [9]. Primary amenorrhea cases also demonstrate a different distribution of genetic causes, with higher rates of biallelic and multiple heterozygous pathogenic variants [9]. Additionally, specific genes show presentation associations - for example, FSHR mutations are more prevalent in primary amenorrhea (4.2% vs. 0.2% in secondary) [9]. These findings support more extensive genetic evaluation in primary amenorrhea cases.
What functional validation approaches are recommended for VUS (Variants of Uncertain Significance)? The 2024 guidelines emphasize the importance of functional studies for VUS interpretation. Research laboratories should implement structured validation pipelines, particularly for genes involved in homologous recombination repair and folliculogenesis [9]. In recent studies, 75 VUS across seven common POI genes underwent experimental validation, with 55 (73.3%) confirmed as deleterious and 38 subsequently reclassified as likely pathogenic [9]. Recommended approaches include in vitro functional assays for DNA repair efficiency, protein stability studies, and animal models where available. These validation protocols are essential for reducing variant interpretation ambiguity and improving clinical utility [9].
Troubleshooting Experimental Guides
Challenge: Low Diagnostic Yield Despite Comprehensive NGS Testing Solution: Implement a combined CNV-SNV detection approach. When NGS gene panel analysis identifies no clear pathogenic variants, integrate array-CGH or NGS-based CNV calling to detect structural variations. One study demonstrated that combining these methods increased overall diagnostic yield to 57.1% compared to 28.6% with NGS alone [37]. Specific steps include:
- Perform array-CGH using 180K+ oligonucleotide platforms for optimal resolution
- Apply dual bioinformatics pipelines for CNV detection from NGS data
- Prioritize CNVs containing known POI genes (e.g., 15q25.2 deletions affecting CPEB1)
- Validate putative CNVs by alternative methods (MLPA, qPCR) [37]
Challenge: High VUS Rate Complicating Clinical Interpretation Solution: Establish a tiered functional validation pipeline focusing on genes with strong biological plausibility. The high prevalence of VUS in POI genetic testing (17.9% in recent studies) necessitates systematic approaches to variant interpretation [37]. Recommended protocol:
- In silico prioritization: CADD scores >20, conservation metrics, population frequency filtering
- Family segregation studies: Co-segregation in affected family members when available
- Functional assays: For DNA repair genes (HFM1, MCM8, MCM9, MSH4), assess homologous recombination efficiency; for transcription factors (NOBOX, FIGLA), evaluate DNA binding and transactivation
- Animal models: Utilize established zebrafish or mouse oogenesis models for high-priority variants [9]
The Scientist's Toolkit
Research Reagent Solutions
Table 3: Essential Research Reagents for POI Genetic Studies
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| NGS Target Enrichment | Custom capture designs (163-200 genes) [37] | Comprehensive variant detection | Include genes across folliculogenesis, meiosis, DNA repair pathways |
| CNV Detection Array | SurePrint G3 Human CGH Microarray 4×180K [37] | Structural variant identification | 60kb minimum resolution; validate findings with alternate methods |
| Functional Validation | Homologous recombination repair assays [9] | VUS pathogenicity assessment | Particularly relevant for meiosis-associated genes (∼48.7% of cases) [9] |
| Animal Models | Zebrafish, Mouse oogenesis models [9] | In vivo variant validation | Crucial for established POI genes (NR5A1, MCM9) and novel candidates |
Experimental Workflow Visualization
POI Gene Pathway Classification
The comparative analysis of international guidelines reveals a evolving consensus on POI genetic testing while highlighting persistent challenges in idiopathic cases. The 2024 guidelines represent a significant advance with simplified diagnostic criteria and expanded genetic recommendations, yet the ~70% of idiopathic cases continues to present a substantial research challenge [37] [6]. Key priorities for the research community include: (1) validation of emerging candidate genes through functional studies; (2) development of standardized variant interpretation frameworks specific to ovarian function; (3) exploration of oligogenic and non-Mendelian inheritance patterns; and (4) development of integrated -omics approaches combining genomic, transcriptomic, and epigenetic data. The implementation of the recommended combined CNV-SNV detection approach, which increases diagnostic yield to 57.1%, should be considered a new standard in research protocols [37]. As genetic understanding advances, subsequent guideline iterations will need to address the complexities of variant classification, oligogenic inheritance, and clinical translation of polygenic risk scores, ultimately reducing the diagnostic odyssey for women with POI.
Premature Ovarian Insufficiency (POI) is a clinically heterogeneous condition characterized by the loss of ovarian function before age 40, affecting approximately 1-3.5% of women [38] [1]. The diagnostic landscape is particularly challenging for idiopathic POI, where no clear iatrogenic, autoimmune, or known genetic cause is immediately identifiable. Recent studies indicate that despite advanced diagnostic capabilities, the underlying etiology remains unknown in a significant proportion of cases, though this proportion has been decreasing over time [1]. Genetic factors play a crucial role in idiopathic POI, with familial forms identified in 12-31% of cases [37] [7]. This technical support guide addresses the critical need for standardized diagnostic protocols and benchmarking data to improve sensitivity and specificity across genetic testing platforms for idiopathic POI research.
Performance Benchmarking of Genetic Diagnostic Platforms
Diagnostic Yield Across Genetic Testing Modalities
Table 1: Diagnostic Performance of Genetic Testing Platforms for Idiopathic POI
| Testing Platform | Sample Size | Diagnostic Yield | Key Genetic Findings | Strengths | Limitations |
|---|---|---|---|---|---|
| Array-CGH | 28 patients [37] | 14.3% (4/28) [37] | CNVs in CPEB1, SLCO3A1, NAIP, FANCB/ASB9 [37] | Detects structural variants >60kb; identifies novel candidate regions [37] | Limited to larger CNVs; misses point mutations and small indels [37] |
| Targeted NGS (163-gene panel) | 28 patients [37] | 28.6% (8/28) pathogenic/likely pathogenic variants [37] | Pathogenic variants in FIGLA, GALT, TWNK, POLG, ERCC6, MCM9 [37] | High-resolution detection of SNVs/indels; customizable gene panels [37] | Limited to known genes; may miss novel genes and complex structural variants [37] |
| Combined Array-CGH + NGS | 28 patients [37] | 57.1% (16/28) overall diagnostic yield [37] | Combined CNV and SNV detection; improved variant interpretation [37] | Comprehensive approach; maximizes diagnostic sensitivity [37] | Higher cost and computational requirements [37] |
| Whole Exome Sequencing | 1,030 patients [9] | 23.5% (242/1030) with P/LP variants [9] | 195 P/LP variants in 59 known genes + 20 novel candidate genes [9] | Hypothesis-free approach; identifies variants in novel genes [9] | Higher variant interpretation burden; incidental findings [9] |
Sensitivity Analysis by Clinical Presentation
Table 2: Diagnostic Sensitivity Correlated with Phenotypic Presentation
| Phenotypic Subgroup | Sample Characteristics | Diagnostic Yield | Most Frequently Identified Pathogenic Variants |
|---|---|---|---|
| Primary Amenorrhea (PA) | 4/28 patients (14.3%) [37]; 120/1030 patients (11.7%) [9] | 75% (3/4) [37]; 25.8% (31/120) [9] | Higher rate of biallelic and multi-het variants [9] |
| Secondary Amenorrhea (SA) | 24/28 patients (85.7%) [37]; 910/1030 patients (88.3%) [9] | 54.2% (13/24) [37]; 17.8% (162/910) [9] | FSHR mutations more common in PA (4.2%) vs SA (0.2%) [9] |
| Familial POI | 11/28 patients (39.3%) [37] | 45% (5/11) [37] | Higher diagnostic yield in familial cases [37] |
Detailed Experimental Protocols
Protocol 1: Combined Array-CGH and NGS Workflow for Idiopathic POI
Diagram Title: Combined Genetic Analysis Workflow
Sample Preparation and Quality Control
- Patient Criteria: Idiopathic POI with primary or secondary amenorrhea >4 months before age 40 and elevated FSH >25 IU/L on two occasions [37] [9]
- Exclusion Criteria: Karyotype abnormalities, FMR1 premutation, autoimmune or iatrogenic causes [37]
- DNA Extraction: Use QIAsymphony DNA midi kits on QIAsymphony system (Qiagen) following manufacturer's protocol [37]
- Quality Metrics: DNA concentration >50ng/μL, A260/280 ratio of 1.8-2.0, minimal degradation on agarose gel electrophoresis [37]
Array-CGH Protocol
- Platform: SurePrint G3 Human CGH Microarray 4×180K (Agilent Technologies) [37]
- Hybridization: Follow manufacturer's recommended protocol with 500ng genomic DNA [37]
- Analysis: Use Feature Extraction and CytoGenomics software v5.0 (Agilent Technologies) with standard settings [37]
- CNV Calling: Minimum 60kb detection threshold along genome; analyze using Cartagenia Bench Lab CNV software v5.1 [37]
- Validation: Quantitative PCR for potentially pathogenic CNVs [37]
Next-Generation Sequencing Protocol
- Capture Design: Custom 163-gene panel covering known and candidate POI genes [37]
- Library Prep: SureSelect XT-HS reagents (Agilent Technologies) on Magnis system [37]
- Sequencing: NextSeq 550 system (Illumina) with minimum 100x coverage [37]
- Variant Calling: Alissa Align&Call v1.1 and Alissa Interpret v5.3 software [37]
- Variant Filtering: Remove common variants (MAF>0.01 in gnomAD); focus on rare, potentially pathogenic variants [9]
Bioinformatics Analysis Pipeline
- Database Annotation: gnomAD, DGV, DECIPHER, Clingen, HGMD, ClinVar [37]
- Pathogenicity Prediction: CADD, SIFT, PolyPhen-2, REVEL scores [9]
- Variant Classification: Follow ACMG guidelines (Class 1-5: benign, likely benign, VUS, likely pathogenic, pathogenic) [37]
- Functional Validation: For VUS in crucial genes, consider functional studies to upgrade/downgrade pathogenicity [9]
Protocol 2: Whole Exome Sequencing and Case-Control Analysis
Diagram Title: WES Case-Control Analysis Workflow
Cohort Selection and Sequencing
- Sample Size: 1,030 idiopathic POI patients, 5,000 controls [9]
- Sequencing Platform: Illumina system with minimum 30x mean coverage [9]
- Variant Calling: GATK best practices pipeline [9]
Case-Control Association Analysis
- Statistical Power: Ensure adequate power for rare variant association tests [9]
- Gene-Based Burden Testing: Compare burden of loss-of-function variants in cases vs controls [9]
- Multiple Testing Correction: Apply FDR <0.05 for statistical significance [9]
Functional Annotation and Pathway Analysis
- Gene Ontology: Meiosis, folliculogenesis, DNA repair pathways [9]
- Expression Data: Incorporate ovarian single-cell RNA sequencing data [9]
- Animal Models: Correlate with knockout mouse phenotypes [9]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for POI Genetic Studies
| Reagent/Platform | Manufacturer/Catalog | Application in POI Research | Technical Specifications |
|---|---|---|---|
| SurePrint G3 Human CGH Microarray 4×180K | Agilent Technologies [37] | Genome-wide CNV detection | 180,000 probes, 60kb resolution [37] |
| SureSelect XT-HS Target Enrichment | Agilent Technologies [37] | Custom gene panel sequencing | 163 POI-associated genes [37] |
| NextSeq 550 Sequencing System | Illumina [37] | High-throughput sequencing | ~120Gb output, 2×150bp reads [37] |
| QIAsymphony DNA Mid Kits | Qiagen [37] | Automated nucleic acid extraction | 50ng-2μg DNA yield from blood [37] |
| Alissa Interpret Software | Agilent Technologies [37] | Clinical variant interpretation | ACMG classification, phenotype correlation [37] |
Troubleshooting Guide: Frequently Asked Questions
Q1: Our diagnostic yield is significantly lower than published rates (e.g., <20% vs 57%). What are the potential causes and solutions?
A1: Low diagnostic yield can result from several factors:
- Inadequate phenotyping: Ensure strict adherence to ESHRE diagnostic criteria (amenorrhea >4 months + FSH >25 IU/L on two occasions) [37]
- Limited genetic coverage: Implement combined approach (Array-CGH + NGS) rather than single platform [37]
- Variant interpretation challenges: Utilize multidisciplinary team including clinical geneticists for VUS classification [37] [9]
- Population-specific variants: Incorporate population-matched control databases to reduce false positives [9]
Q2: How should we handle the high rate of Variants of Uncertain Significance (VUS) in our POI cohort?
A2: VUS management requires systematic approach:
- Functional validation: Implement in vitro assays for recurrent VUS in key genes (e.g., homologous recombination repair assays for DNA repair genes) [9]
- Segregation studies: Test affected and unaffected family members when available [37]
- International collaboration: Share VUS data through consortia to enable case matching [9]
- Periodic reclassification: Establish protocol for regular variant re-evaluation as new evidence emerges [37]
Q3: What is the optimal strategy for transitioning from research to clinical application of novel POI genes?
A3: Translation requires careful validation:
- Statistical rigor: Ensure novel associations meet genome-wide significance (p<5×10â»â¸) in independent cohorts [9]
- Functional evidence: Provide experimental data from animal models or cellular systems [9]
- Clinical utility: Demonstrate impact on patient management or reproductive choices [37]
- Guideline integration: Work with professional societies (ESHRE, ASRM) to update testing recommendations [4]
Q4: How can we improve detection of complex genetic architectures in POI (oligogenic, polygenic contributions)?
A4: Advanced analytical approaches are needed:
- Burden testing: Implement gene-based aggregation of rare variants [9]
- Machine learning: Develop algorithms to detect combinatorial variant effects [9]
- Pathway analysis: Shift focus from single genes to biological pathways (meiosis, DNA repair) [9]
- Integration with multi-omics: Combine genomic data with transcriptomic and epigenetic profiles [9]
Q5: What quality control metrics are most critical for ensuring reproducible results across sequencing platforms?
A5: Key QC parameters include:
- Sequencing depth: Minimum 100x mean coverage for targeted panels, 30x for WES [37] [9]
- Uniformity of coverage: >95% of targets covered at 20x for clinical reporting [37]
- CNV concordance: >90% agreement between Array-CGH and NGS-based CNV calls [37]
- Variant concordance: >99% for SNVs in overlapping regions between platforms [37]
Emerging Technologies and Future Directions
The field of POI genetic diagnosis is rapidly evolving with several promising technological advances. Artificial intelligence approaches are being developed to improve variant interpretation and prioritize candidate genes [73]. Multi-omics integration combining genomic, transcriptomic, and proteomic data may uncover novel disease mechanisms. Additionally, single-cell sequencing technologies offer potential to understand cellular heterogeneity in ovarian tissue and identify subtle defects in folliculogenesis. As these technologies mature, they will likely be incorporated into standardized diagnostic pipelines, further improving sensitivity and specificity for idiopathic POI genetic diagnosis.
FAQs: Navigating Translational Research in Idiopathic POI Genetics
FAQ 1: What are the primary phases of translating a basic genetic finding into a clinically validated diagnostic test for idiopathic POI?
The journey from a research finding to a clinical application is structured along the Clinical and Translational Research (CTR) spectrum. The process is not always linear but often involves parallel or iterative steps [74].
- T0 (Basic Research): Focuses on defining mechanisms of health and disease through preclinical or animal studies. In idiopathic POI, this involves discovering novel genetic variants or pathways (e.g., genes involved in meiosis or DNA repair) using models like cell lines or animal studies [1] [74].
- T1 (Translation to Humans): Applies the mechanistic understanding to humans. This phase involves credentialing a candidate biomarker, developing a practical assay (e.g., a genetic panel), and establishing proof of concept using human biospecimens [75] [74].
- T2 (Translation to Patients): Develops evidence-based practice guidelines through clinical trials. This includes validating the clinical validity of the diagnostic test—its ability to detect or predict POI in defined patient populations [75] [74].
- T3 (Translation to Practice): Integrates the validated test into general practice care through comparative effectiveness research and health services studies, evaluating its real-world impact [74].
- T4 (Translation to Communities): Assesses the broader impact on population health, including cost-effectiveness and the implementation of public health strategies for genetic screening [74].
FAQ 2: Our team has identified a novel genetic variant in a cohort of idiopathic POI patients. What are the key validation challenges, and how can we address them?
The central challenge after an initial discovery is validation, which encompasses both analytic and clinical validity [75].
- Challenge: Insufficient Biospecimens. Access to a sufficient quantity of well-annotated, clinically relevant biospecimens is a major hurdle [75].
- Solution: Utilize established biospecimen repositories or build collaborative networks to access independent sample sets. Successfully translated tests, like Oncotype DX in oncology, relied heavily on samples from large, established study networks [75].
- Challenge: Inadequate Study Design. Spurious correlations can lead to false positives if studies are not rigorously designed [75].
- Solution: Employ careful study design with blinding (so researchers performing assays do not know the status of the samples) and randomization of samples to assay allocations. Subsequent validation must be performed on truly independent sample sets to quantify the assay's specificity, sensitivity, and predictive value accurately [75].
FAQ 3: A genetic assay we are developing for idiopathic POI is producing inconsistent results between research sites. How should we troubleshoot this?
Inconsistencies in assay results often stem from a lack of standardization and rigorous procedural documentation.
- Action 1: Audit Procedural Variables. Generate a list of variables that could contribute to failure, such as DNA extraction methods, reagent lot numbers, storage conditions of samples, or equipment calibration. Change and test these variables one at a time to isolate the root cause [76].
- Action 2: Implement Robust Reporting. Ensure the experimental protocol is documented with necessary and sufficient information. This includes precise details like catalog numbers of reagents, manufacturer information, storage conditions, and explicit instructions for each step, avoiding vague terms like "several" or "enough" [77] [78].
- Action 3: Establish a Troubleshooting Framework. Use a structured approach:
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key materials and resources essential for genetic research into idiopathic POI.
Table 1: Key Research Reagents and Resources for Idiopathic POI Genetic Studies
| Item Category | Specific Examples | Function & Importance |
|---|---|---|
| Key Genetic Assays | FMR1 CGG repeat analysis, Karyotyping (e.g., 45,X for Turner syndrome), Next-Generation Sequencing (NGS) panels | Identifies established (FMR1 premutation, X-chromosomal abnormalities) and novel genetic variants in over 75 genes linked to POI [1]. |
| Laboratory Reagents | DNA extraction kits, PCR reagents, NGS library preparation kits | Fundamental for generating high-quality genetic data. Requires precise reporting of catalog numbers, lot numbers, and storage conditions to ensure reproducibility [78]. |
| Software & Datasets | Genome Analysis Toolkit (GALT), Variant annotation software (e.g., ANNOVAR), Biostatistical packages (R, Python) | Critical for analyzing sequencing data, annotating genetic variants, and performing statistical analyses to establish clinical validity [78]. |
| Biospecimen Resources | Institutional biobanks, Collaborative network repositories (e.g., ESHRE-sponsored) | Provides the well-annotated, independent human sample sets required for rigorous analytical and clinical validation of candidate biomarkers [75]. |
Experimental Protocols for Key Translational Phases
Protocol 1: Validating a Novel Genetic Variant in an Idiopathic POI Cohort (T1-T2 Phase)
This protocol outlines the steps for moving from an initial genetic discovery toward clinical test development.
Background: Despite known genetic causes, up to 36.9% of POI cases are still classified as idiopathic, indicating a strong need for novel gene discovery [1]. This protocol aims to validate the association of a new genetic variant with POI.
Materials and Reagents:
- Biological Materials: DNA samples from a discovery cohort (e.g., 100 POI cases, 100 matched controls) and an independent validation cohort.
- Reagents: Commercially available TaqMan SNP Genotyping Assay or custom NGS panel, following precise reporting guidelines with catalog numbers and storage conditions [78].
- Equipment: Thermal cycler, real-time PCR system or NGS sequencer.
- Software: PLINK for association analysis, R for statistical computing.
Procedure:
- Assay Development: Design a robust genotyping assay for the candidate variant(s).
- Initial Screening: Genotype the variant in the discovery cohort. Critical Step: Laboratory personnel should be blinded to the case/control status of the samples to prevent bias [75].
- Statistical Analysis: Perform an association analysis to confirm a statistically significant link between the variant and POI in the discovery cohort.
- Validation Screening: Genotype the significant variants from step 3 in the independent validation cohort. This step is crucial for confirming clinical validity [75].
- Re-analysis: Repeat the association analysis in the validation cohort to quantify the variant's sensitivity, specificity, and predictive value for POI.
Data Analysis: Detail the statistical tests used (e.g., logistic regression adjusted for age), criteria for data inclusion/exclusion, and the threshold for statistical significance. Specify the required number of biological replicates (samples) to achieve adequate statistical power [74] [78].
Validation of Protocol: Provide evidence of the protocol's robustness by reporting the concordance rate of genotyping results from duplicate samples and the call rate across all samples. Reference any previously published data where this protocol was successfully applied [78].
Protocol 2: Implementing a Diagnostic POI Gene Panel in a Clinical Setting (T2-T3 Phase)
This protocol describes the workflow for applying a validated genetic test in a clinical diagnostic context.
Background: The updated guideline recommends genetic testing, including karyotyping and FMR1 premutation screening, for women with POI [4]. This protocol extends that principle to a multi-gene panel.
Materials and Reagents:
- Biological Materials: Patient blood sample.
- Reagents: DNA extraction kit, NGS library preparation kit, sequencing reagents.
- Equipment: NGS sequencer.
- Software: Bioinformatic pipeline for sequence alignment, variant calling, and annotation; clinical reporting software.
Procedure:
- Patient Consent & Sample Collection: Obtain informed consent, specifically discussing the potential for variants of uncertain significance (VUS). Collect peripheral blood samples.
- DNA Extraction: Isolate genomic DNA.
- Library Preparation & Sequencing: Prepare sequencing libraries targeting a defined panel of POI-associated genes and sequence on an NGS platform.
- Bioinformatic Analysis: Align sequences to a reference genome, call variants, and annotate them against population and clinical databases.
- Clinical Interpretation & Reporting: Interpret the pathogenicity of identified variants based on established guidelines (e.g., ACMG). Generate a clinical report that is clear and actionable for the healthcare provider.
Troubleshooting:
- Problem: Low sequencing coverage in specific genomic regions.
- Solution: Re-optimize the capture probes for those regions or use Sanger sequencing to fill in the gaps.
- Problem: High rate of VUS.
- Solution:
- Pre-analysis: Ensure the gene panel is clinically curated and includes only genes with strong evidence.
- Post-analysis: Implement family segregation studies to help re-classify VUS [76].
Data Presentation: The Evolving Etiological Landscape of POI
Recent studies highlight a significant shift in our ability to identify the causes of POI, directly impacting the "idiopathic" classification. The data below compare a historical cohort (1978-2003) with a contemporary cohort (2017-2024) [1].
Table 2: Changing Etiological Distribution in POI Over Time [1]
| Etiology | Historical Cohort (1978-2003) | Contemporary Cohort (2017-2024) | P-value |
|---|---|---|---|
| Genetic | 11.6% | 9.9% | Not Significant |
| Autoimmune | 8.7% | 18.9% | < 0.05 |
| Iatrogenic | 7.6% | 34.2% | < 0.05 |
| Idiopathic | 72.1% | 36.9% | < 0.05 |
Table 3: Established Genetic Causes of POI for Diagnostic Panel Development [1]
| Genetic Category | Key Genes/Syndromes | Notes on Prevalence & Diagnosis |
|---|---|---|
| Chromosomal Abnormalities | Turner Syndrome (45,X and mosaic variants) | More frequent in primary (21.4%) vs. secondary (10.6%) amenorrhea [1]. |
| Single Gene Mutations | FMR1 (premutation: 55-200 CGG repeats), BMP15, NOBOX, GDF9 | FMR1 premutation is the most common known monogenic cause, with a non-linear risk (highest with 70-100 repeats) [1]. |
| Syndromic Conditions | Perrault syndrome, Bloom syndrome, Ataxia-telangiectasia | POI is one component of a broader multi-system disorder [1]. |
Visualizing the Translational Pathway and Diagnostic Workflow
The following diagrams illustrate the journey from research to diagnosis and the specific clinical evaluation process for POI.
Diagram 1: The CTR Pathway for Idiopathic POI Genetic Discovery
Diagram 2: Clinical Diagnostic Workflow for POI
Conclusion
The genetic diagnosis of idiopathic POI is rapidly transitioning from an era of uncertainty to one of mechanistic discovery. The integration of advanced genomic technologies has successfully reclassified a significant portion of cases, revealing a complex genetic architecture influenced by chromosomal abnormalities, numerous autosomal genes, and potential oligogenic interactions. However, challenges persist in the consistent interpretation of variants, particularly VUS, and the functional validation of new candidate genes. Future progress hinges on large-scale collaborative efforts to aggregate genomic and clinical data, standardize variant interpretation, and develop functional assays to confirm pathogenicity. For researchers and drug developers, these advances illuminate potential therapeutic targets and underscore the necessity of genetically stratified patient cohorts for clinical trials, ultimately paving the way for personalized management strategies that address not only infertility but also the long-term health sequelae of POI.
References
- 1. Changing Etiological Spectrum of Premature Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12248835/]
- 2. The risk factors, pathogenesis and treatment of premature ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01714-2]
- 3. Research challenges current thinking on the genetic causes of ... [https://www.mrc-epid.cam.ac.uk/blog/2023/06/22/research-challenges-thinking-genetic-causes-early-menopause/]
- 4. Evidence-based guideline: Premature Ovarian Insufficiency [https://www.asrm.org/practice-guidance/practice-committee-documents/evidence-based-guideline-premature-ovarian-insufficiency--2024/]
- 5. Research challenges current thinking on the genetic ... [https://www.sciencedaily.com/releases/2023/06/230622120828.htm]
- 6. Primary ovarian insufficiency: update on clinical and ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1464803/full]
- 7. Investigation of Genetics ... Idiopathic Premature Ovarian [https://pmc.ncbi.nlm.nih.gov/articles/PMC11942377/]
- 8. Genetic insights into the complexity of premature ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11295921/]
- 9. Landscape of pathogenic mutations in premature ovarian ... [https://www.nature.com/articles/s41591-022-02194-3]
- 10. Monogenic, Oligogenic, and Polygenic... what's the ... [https://www.genomicmd.com/blog/monogenic-oligogenic-and-polygenic...-whats-the-difference]
- 11. Monogenic vs Oligogenic Reclassification [https://www.frontiersin.org/research-topics/13904/monogenic-vs-oligogenic-reclassification/magazine]
- 12. Epidemiology, Genetic Etiology, and Intervention of ... [https://www.endocrine.org/journals/endocrine-reviews/epidemiology-genetic-etiology-and-intervention-of-poi]
- 13. A Comparative Analysis of Two Cohorts from a Single Center [https://www.mdpi.com/2075-4418/15/13/1724]
- 14. Premature ovarian insufficiency — Knowledge Hub [https://www.genomicseducation.hee.nhs.uk/genotes/knowledge-hub/premature-ovarian-insufficiency/]
- 15. Identifying therapeutic targets for primary ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11446024/]
- 16. The risk factors, pathogenesis and treatment of premature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12175422/]
- 17. Genealogical Study of Primary Ovarian Insufficiency ... [https://www.ajmc.com/view/genealogical-study-of-primary-ovarian-insufficiency-suggests-strong-genetic-component]
- 18. Premature ovarian insufficiency: clinical orientations for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7722400/]
- 19. Primary Ovarian Insufficiency in Adolescents and Young ... [https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2014/07/primary-ovarian-insufficiency-in-adolescents-and-young-women]
- 20. Genetic insights into the complexity of premature ovarian ... [https://rbej.biomedcentral.com/articles/10.1186/s12958-024-01254-2]
- 21. Diagnostic challenges in suspected premature ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9801049/]
- 22. Genetic landscape of a large cohort of Primary Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9475279/]
- 23. Novel variants associated with premature ovarian ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1687148/full]
- 24. Contribution of Array-CGH and Next-Generation Sequencing [https://pubmed.ncbi.nlm.nih.gov/40149403/]
- 25. Microarray — Knowledge Hub [https://www.genomicseducation.hee.nhs.uk/genotes/knowledge-hub/microarray-array-cgh/]
- 26. Array CGH Analysis with Whole Genome Amplification [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/genomics/pcr/oligo-array-cgh?srsltid=AfmBOor55cH4rtfIa_ggq7p4BjJ5Kj80eTcCjcI73O_1-FEMZfX-c0-q]
- 27. Array Comparative Genomic Hybridization (Array CGH) [https://www.thermofisher.com/us/en/home/life-science/gene-expression-analysis-genotyping/genotyping-genomic-profiling/genomic-profilling-acgh.html]
- 28. Experimental Designs for Array Comparative Genomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3728659/]
- 29. Copy number variants on the X chromosome in women ... [https://www.sciencedirect.com/science/article/pii/S0015028211000288]
- 30. Next Generation Sequencing Should Be Proposed to Every ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8169040/]
- 31. Next-generation sequencing of 500 POI patients identified ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-023-01104-6]
- 32. Screening of premature ovarian insufficiency associated ... [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-024-01873-z]
- 33. Targeted Next-Generation Sequencing Indicates a ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2021.664645/full]
- 34. - Next using a pre-designed generation for the... sequencing gene panel [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-015-0055-x]
- 35. Benchmarking of Whole Exome Sequencing and Ad Hoc Designed... [https://www.nature.com/articles/srep37984?error=cookies_not_supported&code=0002c1c1-d575-49ae-b5c2-a94416a21fb3]
- 36. Diagnostics: Next , Exome or Whole Generation ? Gene Panel Genome [https://www.academia.edu/98012881/Next_Generation_Diagnostics_Gene_Panel_Exome_or_Whole_Genome]
- 37. Contribution of Array-CGH and Next-Generation Sequencing [https://www.mdpi.com/2073-4425/16/3/251]
- 38. Premature ovarian insufficiency: Updated concepts in ... [https://www.sciencedirect.com/science/article/pii/S1807593225001644]
- 39. Screening of Premature Ovarian Insufficiency-Associated ... [https://namikkemalmedj.com/articles/screening-of-premature-ovarian-insufficiency-associated-genes-in-turkish-patients/nkmj.galenos.2025.83435]
- 40. Beyond the Exome: The Non-coding Genome and ... [https://pubmed.ncbi.nlm.nih.gov/31417368/]
- 41. Non-coding RNAs guide [https://www.abcam.com/en-us/technical-resources/guides/non-coding-rnas-ncrnas]
- 42. Decoding the Non-coding: Tools and Databases Unveiling the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11249652/]
- 43. Errors, Phantom and Otherwise, in Human mtDNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1180320/]
- 44. A practical guide to mitochondrial DNA error prevention in ... [https://www.sciencedirect.com/science/article/abs/pii/S0006291X0501661X]
- 45. A Beginners' Guide to Non-coding Sequence Alignment [https://bitesizebio.com/10219/introduction-non-coding-sequence-alignment/]
- 46. Variant of Uncertain Significance (VUS) [https://www.genome.gov/genetics-glossary/Variant-of-Uncertain-Significance-VUS]
- 47. Genetic testing found a variant of uncertain significance. ... [https://www.mdanderson.org/cancerwise/genetic-testing-found-a-variant-of-uncertain-significance--now-what.h00-159464001.html]
- 48. Experiences of individuals with a variant of uncertain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9314499/]
- 49. Reassessment of variants of uncertain significance in ... [https://www.nature.com/articles/s41431-025-01911-z]
- 50. Considerations for Variants of Uncertain Significance (VUS) [https://www.rarediseasegenes.com/variants-of-uncertain-significance/]
- 51. New guidelines developed for the diagnosis and ... [https://www.news-medical.net/news/20241209/New-guidelines-developed-for-the-diagnosis-and-management-of-premature-ovarian-insufficiency.aspx]
- 52. Women's healthcare providers' knowledge and practices ... [https://link.springer.com/article/10.1007/s10815-024-03337-w]
- 53. Genetic Testing for Inherited Conditions 2025-09-20 updated ... [https://guidelines.carelonmedicalbenefitsmanagement.com/genetic-testing-for-inherited-conditions-2025-09-20-updated-2025-10-01/]
- 54. Genetic Modifiers and Oligogenic Inheritance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4448705/]
- 55. Digenic Inheritance in Rare Disorders and Mitochondrial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11083678/]
- 56. The overlooked and undertreated perils of premature ... [https://www.ccjm.org/content/92/8/475]
- 57. Frequently Asked Questions about Genetic Counseling [https://www.mskcc.org/cancer-care/risk-assessment-screening/genetic-counseling-and-testing/frequently-asked-questions-about-genetic-counseling]
- 58. Counseling About Genetic Testing and ... [https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2017/04/counseling-about-genetic-testing-and-communication-of-genetic-test-results]
- 59. Communication skills training for healthcare professionals ... [https://www.sciencedirect.com/science/article/abs/pii/S0738399120303918]
- 60. Social, Legal, and Ethical Implications of Genetic Testing - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK236044/]
- 61. Genetic Discrimination [https://www.genome.gov/about-genomics/policy-issues/Genetic-Discrimination]
- 62. Genetic Discrimination and Misuse of Genetic Information: ... [https://blogs.cdc.gov/genomics/2022/10/03/genetic-discrimination/]
- 63. Genetic Information, Non-Discrimination, and Privacy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4233176/]
- 64. Model construction and drug therapy of primary ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10880334/]
- 65. hUMSCs restore ovarian function in POI mice by regulating ... [https://www.nature.com/articles/s41598-024-69381-9]
- 66. Comparison of the different animal modeling and therapy ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-023-03333-4]
- 67. Variant interpretation using population databases [https://pmc.ncbi.nlm.nih.gov/articles/PMC9160216/]
- 68. Critical assessment of variant prioritization methods for rare ... [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-024-00604-w]
- 69. Evidence-based guideline: premature ovarian insufficiency†‡ [https://pubmed.ncbi.nlm.nih.gov/39647506/]
- 70. Evidence-based guideline: Premature Ovarian Insufficiency [https://www.sciencedirect.com/science/article/pii/S0015028224023859]
- 71. Premature Ovarian Insufficiency and Diminished Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609317/]
- 72. Primary Ovarian Insufficiency - StatPearls - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK589674/]
- 73. Agentic AI: Shaping the future of healthcare innovation [https://www.microsoft.com/en-us/industry/blog/healthcare/2025/11/18/agentic-ai-in-action-healthcare-innovation-at-microsoft-ignite-2025/]
- 74. A framework for clinical and translational research in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8057461/]
- 75. Translational Research Working Group Developmental ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2737183/]
- 76. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 77. A guideline for reporting experimental protocols in life sciences [https://pmc.ncbi.nlm.nih.gov/articles/PMC5978404/]
- 78. General Guidelines for Experimental Protocols [https://bio-protocol.org/en/authors?type=ep]