Balancing Accuracy and Speed in Fertility AI: A Research and Clinical Implementation Framework
This article provides a comprehensive analysis for researchers and drug development professionals on the critical trade-offs between predictive accuracy and computational speed in artificial intelligence (AI) models for reproductive medicine. It explores the foundational principles of AI model architecture in fertility applications, examines specific high-performance methodologies, addresses key optimization challenges like interpretability and data limitations, and establishes robust validation and comparative frameworks. By synthesizing current research and clinical survey data, this review aims to guide the development of next-generation fertility AI tools that are both clinically actionable and scientifically rigorous, ultimately accelerating their translation from research to clinical practice.
Balancing Accuracy and Speed in Fertility AI: A Research and Clinical Implementation Framework
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on the critical trade-offs between predictive accuracy and computational speed in artificial intelligence (AI) models for reproductive medicine. It explores the foundational principles of AI model architecture in fertility applications, examines specific high-performance methodologies, addresses key optimization challenges like interpretability and data limitations, and establishes robust validation and comparative frameworks. By synthesizing current research and clinical survey data, this review aims to guide the development of next-generation fertility AI tools that are both clinically actionable and scientifically rigorous, ultimately accelerating their translation from research to clinical practice.
The Core Trade-Off: Understanding Accuracy-Speed Dynamics in Fertility AI
Troubleshooting Guides
Guide 1: Addressing Low Model Accuracy in Clinical Validation
Problem: Your AI model for embryo selection shows high performance on internal validation data but demonstrates significantly lower accuracy (e.g., below 60%) when applied to new clinical datasets or external patient populations.
Diagnosis Steps:
- Check for Data Drift: Compare the statistical properties (e.g., image resolution, lighting conditions, patient demographics) of your new data against the training data. A significant mismatch is a primary cause of performance degradation.
- Validate Ground Truth Consistency: Ensure the clinical outcomes used as labels in your new dataset (e.g., clinical pregnancy confirmation) are defined and determined consistently with your model's training protocol.
- Perform Error Analysis: Categorize the types of embryos or cases where the model is failing. Determine if errors are random or systematic (e.g., the model consistently misclassifies a specific morphological feature).
Solutions:
- Implement Data Augmentation: If data drift is detected, augment your training dataset to better represent the variations in the new clinical environment. This may include simulating different image qualities or patient demographics.
- Initiate Model Retraining: Fine-tune your model on a small, carefully curated dataset from the new clinical site. This helps the model adapt to local variations without forgetting previously learned knowledge.
- Review Labeling Protocols: Work with clinical embryologists to re-validate the ground truth labels for a subset of problematic cases, ensuring they align with the original training standards.
Guide 2: Managing Unacceptable Computational Speed During Inference
Problem: The AI model's inference speed is too slow for practical clinical use, causing delays in the embryo transfer workflow or requiring prohibitively expensive computational hardware.
Diagnosis Steps:
- Profile Model Architecture: Use profiling tools to identify the specific layers or operations in your deep learning model that are the primary bottlenecks (e.g., specific convolutional layers).
- Assess Hardware Compatibility: Determine if the current deployment environment (e.g., CPU vs. GPU, memory bandwidth) is suitable for the model's architecture.
- Evaluate Model Complexity: Check the model's size (number of parameters) and computational complexity (FLOPs - Floating Point Operations). Excessively large models are often slow.
Solutions:
- Apply Model Optimization Techniques:
- Pruning: Remove redundant neurons or weights from the network that contribute little to the final decision [1] [2].
- Quantization: Convert the model's weights from 32-bit floating-point numbers to lower-precision formats (e.g., 16-bit or 8-bit integers). This drastically reduces model size and increases inference speed [1] [2].
- Invest in Optimized Hardware: Deploy the model on hardware optimized for AI inference, such as GPUs with TensorRT or specialized edge AI processors, which can significantly reduce latency [2].
Guide 3: Resolving the Trade-off Between High Sensitivity and Specificity
Problem: Tuning your model to achieve higher sensitivity (detecting more viable embryos) results in an unacceptable drop in specificity (increased false positives of viability), or vice versa.
Diagnosis Steps:
- Analyze the ROC Curve: Plot the Receiver Operating Characteristic (ROC) curve to visualize the trade-off at different classification thresholds. The Area Under the Curve (AUC) provides a single measure of overall performance [3].
- Review Clinical Priorities: Consult with clinical partners to determine the acceptable balance for your specific use case. Is it more critical to avoid discarding a viable embryo (high sensitivity) or to maximize the chance of success for each transfer (high specificity)?
- Inspect Class Imbalance: Check if your training data has a significant imbalance between "viable" and "non-viable" embryo classes, which can bias the model.
Solutions:
- Adjust the Decision Threshold: Move the classification threshold away from the default value of 0.5. Lowering the threshold increases sensitivity, while raising it increases specificity.
- Use a Weighted Loss Function: During training, assign a higher cost to misclassifying the minority class. This encourages the model to pay more attention to those cases.
- Explore Advanced Architectures: Investigate models or loss functions specifically designed for imbalanced data or that directly optimize for the clinical metric of interest.
Frequently Asked Questions (FAQs)
FAQ 1: What are the typical performance benchmarks for AI in embryo selection? Performance can vary, but recent meta-analyses provide aggregate benchmarks. One systematic review reported that AI-based embryo selection methods achieved a pooled sensitivity of 0.69 and specificity of 0.62 in predicting implantation success, with an Area Under the Curve (AUC) of 0.7 [3]. Specific commercial systems, like Life Whisperer, have demonstrated an accuracy of 64.3% for predicting clinical pregnancy [3].
FAQ 2: My model has high accuracy but clinicians don't trust it. How can I improve interpretability? High accuracy alone is often insufficient for clinical adoption. To build trust, you should:
- Provide Explainable AI (XAI) Outputs: Use techniques like Grad-CAM or attention maps to generate visual explanations that highlight which image features (e.g., specific cell structures) the model used to make its decision.
- Conduct Rigorous Clinical Validation: Perform prospective studies that demonstrate the model's performance improves upon standard morphological assessment by embryologists.
- Integrate into Workflow Seamlessly: Ensure the AI tool fits into the existing clinical workflow without disrupting efficiency, presenting clear and actionable information to the embryologist [4].
FAQ 3: What are the key regulatory considerations when validating a clinical AI model? Regulatory bodies require robust evidence of both analytical and clinical validity.
- Analytical Validation: You must prove the model is accurate, reliable, and reproducible. This involves extensive benchmarking on diverse datasets to establish performance metrics like sensitivity, specificity, and precision [5].
- Clinical Validation: You must demonstrate that the model's predictions lead to clinically beneficial outcomes, such as improved pregnancy or live birth rates, through well-designed studies [4].
- Transparency and Monitoring: Be prepared to address potential ethical concerns, provide transparency into the AI's limitations, and implement plans for post-market surveillance to monitor performance over time [4].
FAQ 4: How can I reduce the computational cost of training without sacrificing performance? Several optimization techniques can achieve this balance:
- Hyperparameter Tuning: Use automated tools like Amazon SageMaker Automatic Model Tuning or Optuna to find the most efficient model configuration [1].
- Knowledge Distillation: Train a large, accurate "teacher" model, then use it to train a smaller, faster "student" model that retains most of the performance [1].
- Efficient Model Architectures: Start with inherently efficient architectures (e.g., MobileNet, EfficientNet) that are designed for performance and speed.
- Cloud-Based Optimized Hardware: Utilize cloud services that offer hardware (e.g., AWS Inferentia) specifically designed for cost-efficient model training and inference [1].
Table 1: Diagnostic Performance Metrics of AI in Clinical Applications
| Clinical Application | Sensitivity | Specificity | Accuracy | AUC | Source / Model |
|---|---|---|---|---|---|
| Embryo Selection (IVF) | 0.69 (Pooled) | 0.62 (Pooled) | N/A | 0.70 (Pooled) | Diagnostic Meta-Analysis [3] |
| Embryo Selection (IVF) | N/A | N/A | 64.3% | N/A | Life Whisperer AI Model [3] |
| Embryo Selection (IVF) | N/A | N/A | 65.2% | 0.70 | FiTTE System [3] |
| E-FAST Exam (Trauma) | 81.25% (Hemoperitoneum) | 100% (Hemoperitoneum) | 96.2% (Hemoperitoneum) | 0.91 (Hemoperitoneum) | Buyurgan et al. [6] |
| Nanopore Sequencing (Meningitis) | 50.0% | 55.6% | 47.1% | N/A | Clinical Pathogen Detection [7] |
Table 2: Impact of Model Optimization Techniques on Performance and Efficiency
| Optimization Technique | Primary Effect | Typical Performance Trade-off | Best-Suited Deployment Environment |
|---|---|---|---|
| Pruning | Reduces model size and inference latency. | Potential for minimal accuracy loss (<1%), which can often be recovered with retraining. | Edge devices, mobile applications. |
| Quantization | Speeds up inference and reduces memory usage. | Slight, often negligible, accuracy drop for significant speed gains. | Mobile, IoT, and cloud CPUs. |
| Knowledge Distillation | Creates a smaller, faster model from a larger one. | Student model accuracy should be very close to the teacher model. | When a large, accurate model exists but is too slow for production. |
| Hyperparameter Tuning | Improves model accuracy and efficiency by finding optimal settings. | Generally improves performance without trade-offs, but is computationally expensive. | Used during model development before final deployment. |
Experimental Protocols
Protocol 1: Clinical Validation of an AI Model for Embryo Selection
Objective: To prospectively validate the diagnostic accuracy of an AI model for predicting clinical pregnancy from blastocyst images.
Materials: Time-lapse microscopy images of day-5 blastocysts, associated de-identified patient data, and confirmed clinical pregnancy outcomes.
Methodology:
- Data Curation: Collect a cohort of blastocyst images with linked clinical outcomes. Divide the dataset into a training set (e.g., 70%), a validation set (e.g., 15%), and a held-out test set (e.g., 15%).
- Model Training: Train a convolutional neural network (CNN) on the training set, using the validation set for hyperparameter tuning and to prevent overfitting.
- Performance Assessment: Apply the trained model to the held-out test set. Calculate sensitivity, specificity, accuracy, and AUC by comparing model predictions against the confirmed clinical pregnancy outcomes [3].
- Benchmarking: Compare the AI model's performance against the success rates of traditional embryo selection by trained embryologists to establish clinical utility.
Protocol 2: Benchmarking Variant Calling Pipelines in Genomic Analysis
Objective: To evaluate the analytical performance (sensitivity, specificity, precision) of a germline variant calling pipeline for a clinical diagnostic assay.
Materials: Whole exome or genome sequencing data from reference samples with known truth sets (e.g., from the Genome in a Bottle consortium).
Methodology:
- Data Processing: Run the sequencing data through the variant calling pipeline (e.g., based on GATK HaplotypeCaller or SpeedSeq) to generate a VCF file of variant calls [5].
- Variant Comparison: Use a standardized benchmarking workflow (e.g., incorporating hap.py or vcfeval) to compare the pipeline's variant calls against the known truth set [5].
- Metric Calculation: The workflow calculates the number of true positives (TP), false positives (FP), true negatives (TN), and false negatives (FN). From these, it derives sensitivity (TP/(TP+FN)), specificity (TN/(TN+FP)), and precision (TP/(TP+FP)) across the genome and within specific regions of interest [5].
- Reporting: Generate a report detailing the pipeline's performance for different variant types (SNPs, InDels) and sizes, fulfilling regulatory requirements for assay validation [5].
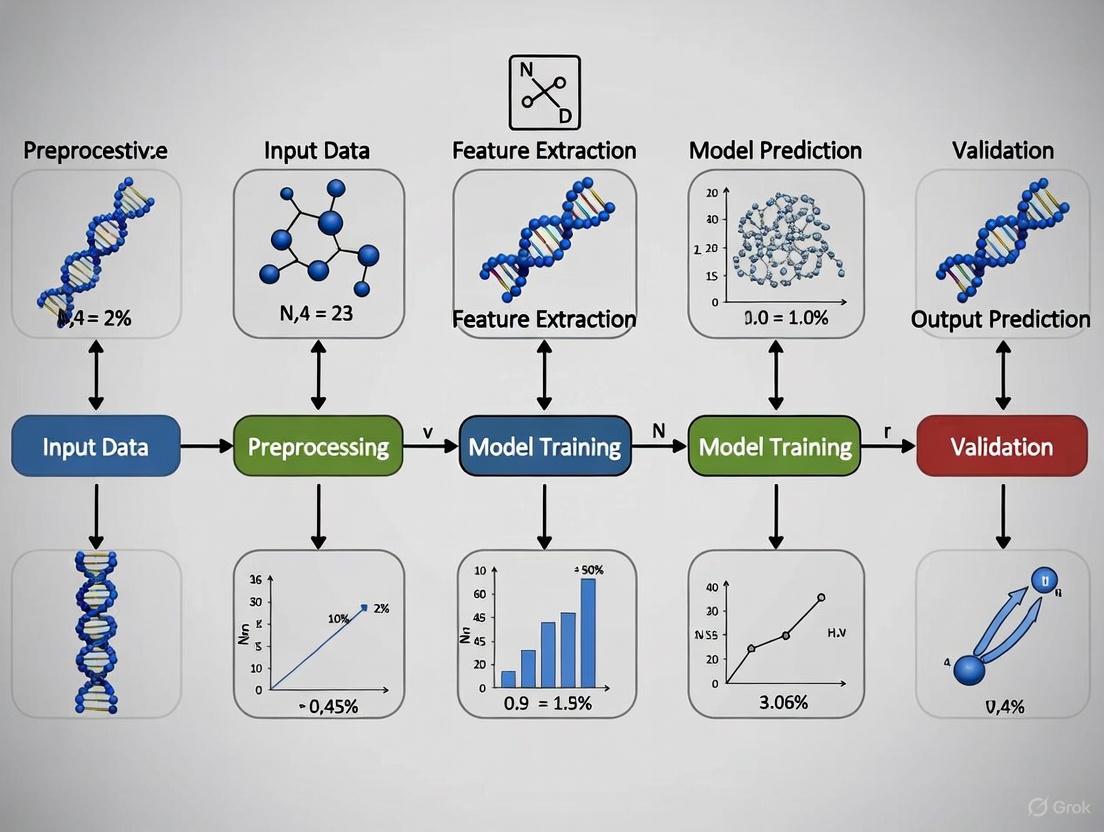
Workflow and Pathway Diagrams
Clinical AI Validation Workflow
Model Optimization Techniques Pipeline
The Scientist's Toolkit
Table 3: Essential Research Reagents and Tools for Clinical AI Research
| Tool / Reagent | Function / Purpose | Example Use Case |
|---|---|---|
| Time-lapse Microscopy Systems | Captures continuous images of embryo development for creating morphokinetic datasets. | Generating the primary image data used to train and validate embryo selection AI models. |
| Convolutional Neural Network (CNN) | A class of deep learning models designed for processing pixel data and automatically learning relevant image features. | The core architecture for analyzing embryo images and predicting viability. |
| Benchmarking Workflows (e.g., hap.py, vcfeval) | Standardized software tools for comparing variant calls against a known truth set to calculate performance metrics. | Essential for validating the analytical performance of genomic pipelines in a clinical lab [5]. |
| Model Optimization Tools (e.g., TensorRT, ONNX Runtime) | Software development kits (SDKs) and libraries designed to optimize trained models for faster inference and deployment on specific hardware. | Used to prune and quantize a large, accurate model for deployment in a real-time clinical setting [1] [2]. |
| Reference Truth Sets (e.g., GIAB) | Genomic datasets from reference samples where the true variants have been extensively validated by consortiums like Genome in a Bottle (GIAB). | Serves as the ground truth for benchmarking and validating the accuracy of clinical genomic pipelines [5]. |
| Daurichromenic acid | Daurichromenic acid, CAS:82003-90-5, MF:C23H30O4, MW:370.5 g/mol | Chemical Reagent |
| Bromomonilicin | Bromomonilicin, CAS:101023-71-6, MF:C16H11BrO7, MW:395.16 g/mol | Chemical Reagent |
The integration of artificial intelligence (AI) into in-vitro fertilization (IVF) represents a paradigm shift in reproductive medicine, offering the potential to enhance precision, standardize procedures, and improve clinical outcomes [8] [9]. This technical resource examines the global adoption and performance of AI in IVF, with a specific focus on the critical balance between model accuracy and operational speed. It provides troubleshooting guidance and foundational knowledge for researchers and clinicians navigating this evolving field.
Global AI Adoption & Performance: A Quantitative Snapshot
The tables below summarize key quantitative data on the adoption, performance, and perceived benefits of AI in IVF, based on recent global surveys and meta-analyses.
Table 1: Trends in Global AI Adoption among IVF Professionals [8]
| Metric | 2022 Survey (n=383) | 2025 Survey (n=171) |
|---|---|---|
| Overall AI Usage | 24.8% | 53.22% (Regular & Occasional) |
| Regular AI Use | Not Specified | 21.64% |
| Primary Application | Embryo Selection (86.3% of AI users) | Embryo Selection (32.75% of respondents) |
| Familiarity with AI | Indirect evidence of lower familiarity | 60.82% (at least moderate familiarity) |
Table 2: Diagnostic Performance of AI in Embryo Selection [3] Data from a systematic review and meta-analysis.
| Performance Metric | Pooled Result |
|---|---|
| Sensitivity | 0.69 |
| Specificity | 0.62 |
| Positive Likelihood Ratio | 1.84 |
| Negative Likelihood Ratio | 0.5 |
| Area Under the Curve (AUC) | 0.7 |
Table 3: Key Barriers to AI Adoption in IVF [8]
| Barrier | Percentage of 2025 Respondents (n=171) |
|---|---|
| Cost | 38.01% |
| Lack of Training | 33.92% |
| Ethical Concerns / Over-reliance on Technology | 59.06% |
Experimental Protocols & Methodologies
Protocol 1: Validating an AI Model for Embryo Implantation Prediction
This protocol is based on multi-center studies validating AI tools for embryo selection [10].
- 1. Objective: To validate the diagnostic accuracy of an AI model in predicting embryo implantation potential and to compare its performance against experienced embryologists.
- 2. Data Sourcing:
- Input Data: Collect time-lapse images or videos of blastocyst-stage embryos from multiple international IVF centers.
- Dataset Size: Use a large, diverse dataset (e.g., 2,075 embryo pairs from six centers) to ensure generalizability.
- Outcome Data: Pair embryo media with known clinical outcomes: implantation success or failure.
- 3. Experimental Setup:
- Test Design: Employ a randomized, multicenter study design.
- Control Group: Embryos are selected for transfer by experienced embryologists using standard morphological grading (e.g., the Gardner scale).
- Test Group: Embryos are selected based on the AI model's recommendations.
- 4. Performance Analysis:
- Primary Endpoint: Compare clinical pregnancy rates between the AI-selected and embryologist-selected groups.
- Model Benchmarking: Compare the AI's performance against individual embryologists and an expert consensus.
- Statistical Measures: Calculate accuracy, sensitivity, specificity, and AUC to quantify predictive performance.
- 5. Troubleshooting:
- Challenge: AI model performance degrades with images from a new clinic due to different microscopes or settings.
- Solution: Implement a calibration step using a small set of standardized images from the new clinic to fine-tune the model and minimize center-specific bias.
Protocol 2: Optimizing Ovarian Stimulation Trigger Timing with Machine Learning
This protocol details the methodology for using AI to improve the timing of the ovulation trigger [11].
- 1. Objective: To determine if a machine-learning model can optimize the day of ovulation trigger to improve mature oocyte yield.
- 2. Model Development:
- Training Data: Train a predictive algorithm on a large dataset of completed ovarian stimulation cycles (e.g., >53,000 cycles from 11 centers).
- Input Features: Use clinical data from the day of potential triggering, including hormone levels (e.g., estradiol) and ultrasound follicle measurements.
- Output: The model predicts the expected yield of total oocytes and mature (MII) oocytes for three potential trigger days: the current day, the next day, and the day after.
- 3. Validation & Analysis:
- Performance Metrics: Validate model performance using metrics like R² (e.g., 0.81 for total oocytes) [11].
- Outcome Comparison: Compare cycle outcomes between cycles where the physician followed the AI recommendation versus those where they triggered earlier.
- Statistical Testing: Use statistical tests (e.g., t-tests) to determine if differences in oocyte and embryo yields are significant (p < 0.001).
- 4. Troubleshooting:
- Challenge: Physicians frequently trigger earlier than the AI model recommends, potentially due to clinical intuition or risk of ovarian hyperstimulation syndrome (OHSS).
- Solution: The AI tool should function as a decision-support system, presenting predictions for multiple days to inform—not replace—clinical judgment. Integrate OHSS risk scores into the algorithm.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for AI-Assisted IVF Research
| Item | Function in Research |
|---|---|
| Time-Lapse Incubation System (TLS) | Provides continuous, non-invasive imaging of embryo development, generating the morphokinetic data essential for training and deploying AI models. |
| Annotated Embryo Image Datasets | Large, diverse, and accurately labeled datasets of embryo images with known implantation outcomes are the fundamental substrate for training robust AI models. |
| AI Software Platform (e.g., EMA, Life Whisperer) | Commercial or proprietary software that contains the algorithms for embryo evaluation, sperm analysis, or follicular tracking. |
| Cloud Computing & Data Storage Infrastructure | Essential for handling the computational load of deep learning and for secure, centralized storage of large-scale, multi-center data. |
| Federated Learning Frameworks | Enables training AI models across multiple institutions without sharing sensitive patient data, addressing a major barrier in medical AI development [12]. |
| SspF protein | SspF protein, CAS:161705-83-5, MF:C9H8BrF3 |
| Ginsenoside RG4 | Ginsenoside RG4, CAS:181225-33-2, MF:C42H70O12, MW:767 g/mol |
Experimental Workflow Visualization
The following diagram illustrates a standard workflow for developing and validating an AI model for embryo selection.
AI Model Development Workflow for Embryo Selection
Frequently Asked Questions (FAQs) for Researchers
Q1: Our AI model for embryo selection shows high accuracy on internal validation but performs poorly on external data. What are the primary causes and solutions?
A: This is a common challenge related to model generalizability.
- Cause: Data Bias. The training data may lack diversity in patient demographics, laboratory protocols, or equipment (e.g., microscope types) [12] [4].
- Solution: Employ Federated Learning, which allows model training across multiple institutions without centralizing data, thus exposing the model to more varied data sources [12]. Ensure training datasets are large and represent a broad patient population.
- Cause: Overfitting. The model has learned noise and specific patterns from the training set that do not generalize.
- Solution: Implement rigorous regularization techniques during training and use external test sets from completely independent clinics for validation before clinical implementation.
Q2: How can we balance the need for a highly accurate, complex AI model with the speed required for clinical workflow efficiency?
A: The trade-off between accuracy and speed is central to clinical AI.
- Strategy 1: Model Optimization. After training a complex model, techniques like pruning and quantization can reduce its computational load and size, increasing inference speed with minimal accuracy loss.
- Strategy 2: Tiered Analysis. Use a fast, less complex model for initial, high-volume triage (e.g., initial embryo grading). A slower, more accurate model can then be used for final decision-making on a pre-selected subset.
- Strategy 3: Hardware Integration. Deploying models on dedicated, high-performance hardware within the clinic's infrastructure can significantly speed up processing times.
Q3: What are the key ethical considerations and potential biases we must address when developing AI for IVF?
A: Ethical and bias-related issues are critical for responsible AI deployment.
- Algorithmic Bias: AI models can perpetuate and even amplify existing biases in training data. If trained predominantly on data from specific ethnic or age groups, performance may be suboptimal for other groups, exacerbating health disparities [9] [13].
- Mitigation: Intentionally curate diverse training datasets and perform rigorous subgroup analysis to test for performance disparities.
- Transparency & Explainability: Many AI models are "black boxes." Clinicians may be hesitant to trust a recommendation without understanding the reasoning.
- Mitigation: Focus on developing explainable AI (XAI) techniques that highlight the image features or data points influencing the model's decision [12] [4].
- Over-reliance: A significant risk is that embryologists may defer to the AI's judgment, potentially overlooking errors.
- Mitigation: Design AI systems as decision-support tools, not autonomous decision-makers. The final clinical decision must remain with the human expert [8] [14] [4].
FAQs: Core Architectural Concepts
Q1: What is the fundamental difference between Traditional Machine Learning and Deep Learning for fertility research?
A1: The choice between Traditional Machine Learning and Deep Learning involves a direct trade-off between interpretability and automatic feature discovery, which is crucial in a sensitive field like fertility research.
- Traditional Machine Learning (e.g., Logistic Regression, Random Forest, XGBoost) requires researchers to manually define and engineer relevant features (e.g., follicle size, hormone levels) from the raw data. These models are typically more interpretable, computationally less intensive, and can be effective with smaller datasets [15]. For example, a study predicting natural conception used an XGB Classifier, achieving an accuracy of 62.5% [16].
- Deep Learning (e.g., CNNs, RNNs) automates feature extraction by learning hierarchical data representations through multiple network layers. This is powerful for complex, unstructured data like embryo time-lapse videos or ultrasound images, where manual feature engineering is difficult. However, these models are often seen as "black boxes," require large datasets, and are computationally expensive [15] [17].
Q2: My deep learning model for embryo classification performs well on training data but poorly on new clinical images. What is happening?
A2: This is a classic case of overfitting [18]. Your model has likely memorized the noise and specific patterns in your training data rather than learning generalizable features. Key strategies to overcome this are:
- Regularization & Dropout: Randomly deactivate neurons during training to prevent the model from over-relying on any single node [18] [19].
- Data Augmentation: Artificially expand your training dataset using techniques like rotation, flipping, or adjusting brightness on existing images to make the model more robust [18].
- Early Stopping: Halt the training process when the model's performance on a validation dataset stops improving, preventing it from learning the training data too specifically [18].
Q3: How can I make my large fertility prediction model fast enough for real-time clinical use without sacrificing accuracy?
A3: Several AI model optimization techniques can significantly improve inference speed:
- Pruning: Identifies and removes unnecessary weights or neurons in the network that contribute little to the final prediction, creating a smaller and faster model [20] [2] [21].
- Quantization: Reduces the numerical precision of the model's parameters (e.g., from 32-bit floating-point to 8-bit integers). This shrinks the model size and speeds up computation, which is ideal for deployment on edge devices [20] [2] [21].
- Knowledge Distillation: Trains a compact "student" model to mimic the performance of a larger, more accurate "teacher" model, preserving much of the accuracy while being far more efficient [21].
Troubleshooting Guides
Problem: Model Performance Degradation Over Time
Symptoms: A model that was once accurate for predicting ovarian response now shows declining performance on new patient data.
Diagnosis: This is likely model drift, where the statistical properties of the real-world data have changed over time compared to the data the model was originally trained on [21].
Resolution Protocol:
- Data Verification: Implement a continuous data monitoring pipeline to compare incoming data distributions with the original training data.
- Retraining Schedule: Establish a regular schedule for retraining the model with newly collected, validated data.
- Transfer Learning: Consider using a pre-trained model and fine-tuning its final layers on the new data, which can be more efficient than training from scratch [20] [21].
Problem: The "Black Box" Problem in Clinical Deployment
Symptoms: Clinicians are hesitant to trust an AI model's recommendation for embryo selection because the reasoning behind the decision is not transparent [17] [22].
Diagnosis: Lack of model interpretability, a common challenge with complex deep learning models.
Resolution Protocol:
- Model Selection: Prioritize "explainable AI†(XAI) methods or inherently more interpretable models where possible. For instance, research into follicle size optimization has used explainable AI to identify the specific follicle sizes most likely to yield mature oocytes, making the model's reasoning clear to clinicians [22].
- Utilize Interpretation Tools: Employ techniques like SHAP (SHapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) to generate post-hoc explanations for individual predictions.
- Clinical Validation & Collaboration: Conduct robust prospective validation studies to build trust and foster collaboration between AI engineers and clinicians to integrate AI as a decision-support tool, not a replacement [22].
Table 1: Performance Comparison of Machine Learning Models in a Fertility Study [16]
| Model Name | Accuracy | Sensitivity | Specificity | ROC-AUC |
|---|---|---|---|---|
| XGB Classifier | 62.5% | Not Reported | Not Reported | 0.580 |
| Logistic Regression | Not Reported | Not Reported | Not Reported | Not Reported |
| Random Forest | Not Reported | Not Reported | Not Reported | Not Reported |
| Study Context | This study used 63 sociodemographic and sexual health variables from 197 couples to predict natural conception. The limited performance highlights the complexity of fertility prediction. |
Table 2: Comparison of AI Optimization Techniques [20] [2] [21]
| Technique | Primary Benefit | Potential Drawback | Best Suited For |
|---|---|---|---|
| Pruning | Reduces model size and inference time. | May require fine-tuning to recover accuracy. | Deployment on mobile or edge devices. |
| Quantization | Decreases memory usage and power consumption. | Can lead to a slight loss in precision. | Real-time inference on hardware with limited resources. |
| Hyperparameter Tuning | Maximizes model accuracy and training efficiency. | Computationally intensive and time-consuming. | The initial model development phase to find the optimal configuration. |
| Knowledge Distillation | Creates a compact model that retains much of a larger model's knowledge. | Requires a high-quality, large teacher model. | Distributing models to clinical settings with lower computational power. |
Experimental Protocols
Protocol: Developing a Machine Learning Model for Natural Conception Prediction
Objective: To predict the likelihood of natural conception among couples using sociodemographic and sexual health data via machine learning [16].
Methodology:
- Data Collection:
- Cohorts: Recruit two distinct groups: fertile couples (achieved conception within one year) and infertile couples (unable to conceive after 12 months).
- Variables: Collect 63 parameters from both partners, including age, BMI, menstrual cycle characteristics, medical history, lifestyle factors (caffeine, smoking), and varicocele presence [16].
- Data Preprocessing:
- Apply inclusion/exclusion criteria to ensure clean cohort definitions.
- Use Permutation Feature Importance to select the 25 most predictive variables from the initial 63 [16].
- Model Training & Evaluation:
- Models: Train multiple models, such as XGB Classifier, Random Forest, and Logistic Regression.
- Training Scheme: Split data into 80% for training and 20% for testing.
- Metrics: Evaluate performance using accuracy, sensitivity, specificity, and ROC-AUC, with cross-validation to assess robustness [16].
Protocol: AI Workflow for Follicle Size Optimization in IVF
Objective: To use explainable AI to identify optimal follicle sizes that maximize mature oocyte yield and live birth rates during ovarian stimulation [22].
Methodology:
- Data Curation: Gather a large dataset (e.g., from over 19,000 patients) containing detailed follicle tracking data from ultrasound scans and corresponding cycle outcomes (oocyte maturity, live birth) [22].
- Model Development & Analysis:
- Employ explainable AI methods to analyze the entire cohort of follicles, moving beyond the simplification of using only lead follicles.
- The model identifies the specific size range of follicles most likely to yield mature oocytes post-trigger.
- Validation: Correlate the proportion of follicles within the AI-identified optimal range with key outcomes, specifically mature oocyte yield and live birth rates, to validate the clinical utility of the findings [22].
Workflow and Pathway Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential "Reagents" for Fertility AI Research
| Item | Function in the AI "Experiment" |
|---|---|
| Pre-trained Models (e.g., ImageNet, BERT) | Models already trained on massive general datasets. They serve as a starting point for transfer learning, reducing the data and time needed to develop specialized models for tasks like analyzing embryo images or medical literature [15] [21]. |
| Optimization Frameworks (e.g., TensorRT, ONNX Runtime) | Software tools used to "refine" the final model. They implement techniques like pruning and quantization to make models faster and smaller for clinical deployment [20] [2] [21]. |
| Data Augmentation Libraries | Algorithms that artificially expand training datasets by creating slightly modified versions of existing images (e.g., rotations, flips, contrast changes). This helps improve model robustness and combat overfitting [18] [21]. |
| Hyperparameter Tuning Tools (e.g., Optuna) | Automated systems that search for the best combination of model settings (hyperparameters), much like optimizing a chemical reaction's conditions to maximize yield (accuracy) [20] [21]. |
| Explainable AI (XAI) Toolkits | Software packages that help interpret the predictions of complex "black box" models. This is crucial for building clinical trust and understanding the model's reasoning, for example, in embryo selection [22]. |
| AR25 | AR25 Chromone Derivative |
| aTAG 2139 | aTAG 2139, MF:C42H38N8O8, MW:782.81 |
Troubleshooting Guides
Poor Model Generalizability to New Clinical Sites
Problem: Your model, trained on data from a single fertility center, performs poorly when validated on data from a new clinic, showing significant performance degradation.
Explanation: This is often caused by a distribution shift between your training data and the new site's data. Variations in laboratory protocols, equipment, patient demographics, or embryo grading practices can create this shift, making the model's learned patterns less applicable.
Solution:
- Action 1: Enhance Dataset Representativeness: Proactively collect training data from multiple clinical sites with varying protocols and patient populations. Ensure the data encompasses the diversity you expect in real-world deployment [23].
- Action 2: Implement Rigorous External Validation: Before deployment, always test your model on a completely held-out dataset from a different fertility center. This provides a realistic estimate of real-world performance [23] [12].
- Action 3: Adhere to Regulatory Guidance: Follow emerging regulatory frameworks, such as the FDA's credibility assessment, which emphasizes characterizing training data and ensuring its representativeness for the intended patient population [24] [25].
High Model Instability and Inconsistent Predictions
Problem: When retrained on the same data with different random seeds, your model produces vastly different embryo rankings, undermining clinical reliability.
Explanation: This instability indicates that the model is highly sensitive to small changes in initial training conditions. This is a fundamental issue in some AI architectures for IVF, leading to low agreement between replicate models and a high frequency of critical errors, such as ranking non-viable embryos as top candidates [23].
Solution:
- Action 1: Quantify Instability Metrics: Systematically evaluate model consistency. Train multiple replicate models (e.g., 50x with different seeds) and measure the agreement in their rankings using metrics like Kendall’s W. Also, track the critical error rate—how often poor-quality embryos are top-ranked [23].
- Action 2: Explore Alternative Modeling Approaches: If using Single Instance Learning (SIL) models, investigate whether more stable AI frameworks or architectures are available. The high variability in SIL models may necessitate a different methodological approach [23].
- Action 3: Prioritize Interpretability: Use tools like SHAP (SHapley Additive exPlanations) or gradient-weighted class activation mapping to understand the divergent decision-making strategies of unstable models. This can provide clues for improving model design [23] [26].
Inadequate Transparency and Reporting for Regulatory Scrutiny
Problem: Your model's development and performance details are insufficiently documented, making it difficult to satisfy internal review boards or regulatory body requirements.
Explanation: A lack of methodological transparency is a common challenge with complex AI models. Regulators are increasingly focusing on this issue, requiring detailed disclosures about data provenance, model development, and performance metrics to assess credibility and potential biases [27] [25] [28].
Solution:
- Action 1: Adopt a Comprehensive Documentation Framework: Create a detailed report covering:
- Data Management: Sources, collection methods, cleaning, annotation procedures, and demographic characteristics [25] [28].
- Model Development: Architecture, features, hyperparameters, and training protocols [25].
- Validation Results: Performance metrics (sensitivity, specificity, AUROC) on independent test sets, with subgroup analyses [29] [28].
- Action 2: Use Model Cards: Consider using a "model card," a concise document summarizing the model's intended use, performance, limitations, and training data, as suggested by the FDA for medical devices [25].
- Action 3: Follow Reporting Guidelines: Adhere to established guidelines like TRIPOD+AI for clinical prediction models to ensure all critical aspects of development and validation are reported [29].
Frequently Asked Questions (FAQs)
Q1: What is the minimum dataset size required to train a reliable fertility AI model? There is no universal minimum; the required size depends on model complexity and task difficulty. The key is to ensure the dataset is representative. However, performance is more critically linked to data quality and diversity than to sheer volume. A smaller, well-annotated, and multi-center dataset is far more valuable than a large, homogenous, single-center one [23] [12]. One study achieving reasonable performance used datasets of 10,713 and 648 embryos from different centers for training and external testing, respectively [23].
Q2: How can I assess the quality of my training dataset? Evaluate your dataset against these criteria:
- Representativeness: Does it reflect the target patient population? Analyze demographics and clinical characteristics [24].
- Annotation Quality: Are the labels (e.g., live birth outcomes, embryo grades) accurate and consistent? Using a single, expert team for annotations can reduce variability [23].
- Completeness: Is there a high proportion of missing values for key features?
- Balance: For classification tasks, is there a significant class imbalance? Techniques like stratification may be needed.
Q3: What are the most common data-related pitfalls in fertility AI research?
- Single-Center Data: Models trained on data from one clinic often fail to generalize [23] [12].
- Insufficient External Validation: Relying only on internal validation (e.g., a simple train-test split from the same source) overestimates real-world performance [12].
- Poor Transparency: Failing to document data sources, demographics, and model details, which is now a major focus of regulatory bodies [28].
- Ignoring Model Instability: Not testing for consistency across multiple training runs, which is crucial for reliable clinical ranking [23].
Q4: Our model works well in internal tests but fails in clinical deployment. What went wrong? This "deployment gap" typically stems from overfitting to the training environment and a failure to account for real-world variability. Internal tests may not capture the full spectrum of data quality, patient profiles, and operational workflows found in a live clinical setting. The solution is to perform robust external validation on data from completely independent sites before deployment [23] [12].
The following table consolidates key quantitative findings from recent studies on data and model performance in fertility AI.
Table 1: Quantitative Evidence on Data and Model Performance in Fertility AI
| Study Focus | Key Metric | Reported Value / Finding | Implication for Data & Model Performance |
|---|---|---|---|
| AI Model Stability in Embryo Selection [23] | Consistency in embryo ranking (Kendall's W) | ~0.35 (where 0=no agreement, 1=perfect agreement) | Highlights significant instability in model rankings even with identical training data. |
| Critical Error Rate | ~15% | High rate of non-viable embryos being top-ranked, a major clinical risk. | |
| Performance on External Data | Error variance increased by 46.07%² | Demonstrates high sensitivity to distribution shifts between datasets. | |
| Transparency in FDA-Reviewed AI Devices [28] | Average Transparency (ACTR Score) | 3.3 out of 17 points | Indicates a severe lack of transparency in reporting model characteristics and data. |
| Devices Reporting Clinical Studies | 53.1% | Nearly half of approved AI devices lack publicly reported clinical studies. | |
| Devices Reporting Any Performance Metric | 48.4% | Over half of devices do not report basic performance metrics, hindering evaluation. | |
| Machine Learning for Blastocyst Yield Prediction [29] | Model Performance (R²) | 0.673 - 0.676 (Machine Learning) vs. 0.587 (Linear Regression) | Machine learning models better capture complex, non-linear relationships in IVF data. |
| Model Accuracy for Multi-class Prediction | 0.675 - 0.71 | Demonstrates the predictive potential of ML with structured, cycle-level data. |
Experimental Protocol: Evaluating AI Model Stability
This protocol is based on a study that systematically investigated the instability of AI models for embryo selection [23].
Objective: To assess the stability and reliability of a Single Instance Learning (SIL) model for embryo rank ordering.
Materials & Methods:
- Datasets: Use at least two independent, retrospective datasets from different fertility centers.
- Primary Dataset: For model training and validation (e.g., 10,713 embryos from 1,258 patients).
- External Test Dataset: For final evaluation only (e.g., 648 embryos from 53 patients).
- Model Training:
- Define a fixed model architecture (e.g., a convolutional neural network).
- Train 50 replicate models using the exact same architecture and training data, but with different random seeds for weight initialization.
- Evaluation:
- Rank Order Consistency: For each patient cohort in the test sets, generate embryo rank orders based on the model's live-birth probability output from all 50 replicates. Calculate Kendall’s W coefficient to measure agreement between the rankings.
- Critical Error Rate: Determine the frequency at which a model ranks a low-quality (e.g., degenerate) embryo as the top candidate when a higher-quality blastocyst is available.
- Interpretability Analysis: Use techniques like gradient-weighted class activation mapping to visualize the image regions influencing each model's decision, helping to identify divergent focus areas.
The workflow for this experiment is summarized in the following diagram:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Computational Tools for Fertility AI Research
| Item / Tool Name | Function / Application in Research |
|---|---|
| Time-Lapse Microscopy Systems (e.g., Embryoscope) | Generates high-volume, time-series imaging data of embryo development, which is the primary input for many deep learning models in embryo selection. |
| Convolutional Neural Networks (CNNs) | A class of deep learning models, particularly effective for analyzing visual imagery like embryo pictures. They are commonly used in both research and commercial embryo assessment platforms [23]. |
| SHapley Additive exPlanations (SHAP) | A game theory-based method for interpreting the output of any machine learning model. It is used to explain feature importance, helping researchers understand which factors (e.g., embryo morphology) most influence the model's prediction [26]. |
| XGBoost / LightGBM | Powerful machine learning algorithms based on gradient boosting. They are highly effective for structured data tasks, such as predicting cycle-level outcomes (e.g., blastocyst yield) from clinical and morphological features, and often offer high performance and interpretability [29] [26]. |
| Prophet | A time-series forecasting procedure developed by Facebook, useful for analyzing and projecting long-term fertility trends based on population-level data [26]. |
| Model Cards | A framework for transparent reporting of model characteristics, intended use, and performance metrics. Their use is encouraged by regulatory bodies like the FDA to improve communication between developers and users [25]. |
| BDPSB | BDPSB, MF:C36H28N6O8S2, MW:736.77 |
| GSK-LSD1 Dihydrochloride | GSK-LSD1 Dihydrochloride, CAS:1821798-25-7, MF:C14H22Cl2N2, MW:289.24 |
In the context of assisted reproductive technology (ART), the integration of artificial intelligence (AI) into clinical workflows represents a paradigm shift from retrospective analysis to real-time decision support. For researchers and drug development professionals, a central thesis is emerging: the ultimate clinical value of an AI model is contingent not only on its accuracy but also on its speed of integration into existing clinical workflows. AI tools that generate predictions in real time (<1 second) are essential to avoid disrupting the carefully timed processes of ovarian stimulation and embryo culture [30]. The primary challenge is to balance this requisite for instantaneous processing with the rigorous, evidence-based accuracy demanded of a medical intervention. This technical support document outlines the critical troubleshooting steps, experimental protocols, and key reagents for developing and validating AI solutions that meet these dual demands of speed and accuracy.
Troubleshooting Guides & FAQs
FAQ 1: Our AI model is accurate on retrospective data, but clinicians report it disrupts their workflow. What are the primary integration points we should optimize for speed?
Answer: The most critical speed-sensitive integration points in the ART workflow involve real-time monitoring and triggering decisions. Seamless integration is achieved through API-based EMR integration that avoids multiple logins, manual data entry, or switching between screens [31].
- Troubleshooting Steps:
- Verify EMR API Connectivity: Confirm that your AI tool uses the clinic's EMR API for real-time, bidirectional data exchange. This eliminates manual data transfer, a major source of delay and error [31].
- Benchmark Data Retrieval and Prediction Time: Measure the time from a clinician opening a patient's record in the EMR to the AI insights being displayed. This end-to-end latency should be under one second to be considered real-time [30].
- Profile Model Inference Speed: Isolate the AI model's prediction time. For image-based models (e.g., embryo analysis), optimize the deep learning architecture (e.g., using lighter-weight CNNs) to reduce processing time without sacrificing predictive performance.
FAQ 2: How can we validate that our model's speed does not come at the cost of clinical accuracy and patient safety?
Answer: Robust, prospective validation is the cornerstone of ensuring that speed does not compromise safety. A purpose-built AI must be validated against clinically relevant endpoints in a setting that mimics real-world use [22] [32].
- Troubleshooting Steps:
- Conduct a "Human-in-the-Loop" Simulation: Design a study where embryologists or clinicians use your AI tool in a simulated, time-pressured environment. Compare the accuracy and efficiency of decisions made with and without the AI support.
- Implement a "Silent Trial": Run the AI tool in parallel with the standard clinical workflow without showing its results to the clinical team. Record the AI's predictions and compare them to both the clinical decisions and the ultimate patient outcomes (e.g., blastocyst formation, live birth). This validates efficacy without risking patient safety [22].
- Audit for Model Drift: Establish a continuous monitoring system to track the model's performance over time as new patient data is acquired. A drop in accuracy, even if speed remains high, indicates model drift and the need for retraining.
FAQ 3: Our model for predicting blastocyst formation is accurate but computationally intensive, causing delays. What architectural strategies can improve inference speed?
Answer: For time-lapse image analysis, the choice of deep learning architecture directly impacts speed. Replacing a single, complex model with a staged or hybrid architecture can significantly reduce processing time [33].
- Troubleshooting Steps:
- Analyze Computational Bottlenecks: Use profiling tools to identify if the lag is due to data preprocessing, feature extraction, or the model's inference.
- Consider a Two-Stage Model: As demonstrated in a study predicting blastocyst formation, a two-stage model that first identifies cellular events and then uses a sequential model like a Gated Recurrent Unit (GRU) for prediction can achieve high accuracy (93%) with efficient processing [33].
- Optimize for Hardware Acceleration: Ensure the model software stack is configured to leverage GPU acceleration, which is critical for processing the high-volume image data from time-lapse systems in real-time.
Experimental Protocols for Validating Speed and Accuracy
To empirically balance speed and accuracy, researchers should adopt the following experimental protocols.
Protocol 1: Real-World Workflow Impact Study
This protocol assesses the integration of an AI clinical decision support system (CDSS) for FSH starting dose selection and trigger timing.
- Objective: To evaluate whether the adjunctive use of AI software changes treatment decisions and patient outcomes without introducing workflow delays [30].
- Methodology:
- Design: Retrospective cohort study with matched historical controls.
- Intervention: Physicians use an AI CDSS (e.g., Stim Assist) integrated into the EMR to guide FSH starting dose and trigger timing. The software provides predictions in real-time (<1 second) [30].
- Control: Historical patients treated by the same physicians without AI.
- Primary Endpoints:
- Speed Metric: Time from EMR access to AI recommendation display.
- Efficacy Metrics: Starting FSH dose (IU), total FSH dose (IU), number of metaphase II (MII) oocytes retrieved.
- Statistical Analysis: T-test to compare means between groups for efficacy metrics. Descriptive statistics for speed metrics.
Protocol 2: Prospective Validation of an AI for Embryo Selection
This protocol validates a deep learning model for predicting blastocyst formation from cleavage-stage embryos using time-lapse images.
- Objective: To predict blastocyst formation at the cleavage stage (Day 3) with high accuracy and speed, enabling earlier embryo transfer [33].
- Methodology:
- Model Architecture: A ResNet-GRU hybrid model.
- Stage 1 (Feature Extraction): A Residual Neural Network (ResNet) processes individual time-lapse frames to extract spatial features.
- Stage 2 (Temporal Analysis): A Gated Recurrent Unit (GRU) analyzes the sequence of extracted features to model embryo development over time [33].
- Data Input: Time-lapse video frames from Day 0 to Day 3 (72 hours post-insemination).
- Outcome: Binary classification (Blastocyst/No Blastocyst).
- Validation: Performance evaluated on a hold-out test set with metrics including accuracy, sensitivity, specificity, and per-image inference time.
- Model Architecture: A ResNet-GRU hybrid model.
Table 1: Performance Metrics of a ResNet-GRU Model for Blastocyst Prediction
| Metric | Value | Interpretation |
|---|---|---|
| Validation Accuracy | 93% | The model correctly classified blastocyst outcome in 93% of cases [33]. |
| Sensitivity | 0.97 | The model correctly identifies 97% of embryos that will form a blastocyst [33]. |
| Specificity | 0.77 | The model correctly identifies 77% of embryos that will not form a blastocyst [33]. |
| Inference Speed | Real-time (<1 sec/video) | The model processes a full time-lapse video sequence fast enough for clinical workflow integration [30]. |
Workflow Visualization: AI Integration in the IVF Pipeline
The following diagram illustrates the key touchpoints for real-time AI decision support within a standard IVF cycle, highlighting where speed of integration is most critical.
AI Integration in the IVF Pipeline
The Scientist's Toolkit: Research Reagent Solutions
For researchers developing and validating fertility AI models, the following table details essential "research reagents" – key data types and software components required to build effective systems.
Table 2: Essential Components for Fertility AI Research & Development
| Component | Function in the Experiment | Example in Context |
|---|---|---|
| Clinical & Demographic Data | Provides baseline patient characteristics for personalizing treatment protocols and understanding population biases. | Age, Body Mass Index (BMI), infertility diagnosis [30] [34]. |
| Endocrine & Biomarker Data | Used as key input features for models predicting ovarian response and optimizing drug dosing. | Anti-Müllerian Hormone (AMH), Antral Follicle Count (AFC), baseline Estradiol (E2) [30] [35]. |
| Ultrasound & Follicle Metrics | Serves as temporal, image-based data for monitoring follicle growth and predicting oocyte maturity. | 2D/3D ultrasound images; follicle diameters and areas grouped by size cohorts (e.g., 14-15mm, 16-17mm) [22] [34]. |
| Time-Lapse Imaging (TLI) Data | Provides continuous, non-invasive visual data of embryo development for morphokinetic analysis and blastocyst prediction. | Video frames from embryo culture incubators, annotated for key cellular events (e.g., cell division) [33]. |
| Electronic Medical Record (EMR) API | The critical conduit for seamless, real-time data exchange between the AI model and the clinical workflow. | An API connection that allows the AI to pull patient data and push predictions directly into the clinician's view without manual steps [31]. |
| Deep Learning Frameworks | Software libraries used to build, train, and validate complex AI models for image and sequence analysis. | TensorFlow or PyTorch used to implement architectures like CNNs for image analysis or GRUs for temporal modeling [33]. |
| KuWal151 | KuWal151|Potent CLK Inhibitor|For Research Use | KuWal151 is a potent, selective CLK4/1/2 inhibitor for cancer research. It shows antiproliferative activity in vitro. For Research Use Only. Not for human use. |
| MS31 | MS31|Spindlin-1 Inhibitor | MS31 is a potent Spindlin-1 inhibitor for cancer research. It is supplied for Research Use Only (RUO). Not for human, veterinary, or household use. |
High-Performance Architectures: Methodologies for Efficient and Accurate Fertility AI
Technical Troubleshooting Guide: Common LightGBM Issues in Fertility Research
This section addresses specific challenges you might encounter when using LightGBM for reproductive medicine research.
FAQ 1: My computer runs out of RAM when training LightGBM on a large dataset of IVF cycles. What can I do?
This is a common issue when working with extensive medical datasets. Several solutions exist [36]:
- Set the
histogram_pool_sizeparameter to control the MB of memory you want LightGBM to use. - Lower the
num_leavesparameter, as this is a primary controller of model complexity. - Reduce the
max_binparameter to decrease the granularity of feature binning.
FAQ 2: The results from my LightGBM model are not reproducible between runs, even with the same random seed. Why?
This is normal and expected behavior when using the GPU version of LightGBM [36]. For reproducibility, you can:
- Use the
gpu_use_dp = trueparameter to enable double precision (though this may slow down training). - Alternatively, use the CPU version of LightGBM for fully reproducible results [36].
FAQ 3: LightGBM crashes randomly with an error about "libiomp5.dylib" and "libomp.dylib". What does this mean?
This error indicates a conflict between multiple OpenMP libraries installed on your system [36]. If you are using Conda as your package manager, a reliable solution is to source all your Python packages from the conda-forge channel, as it contains built-in patches for this conflict. Other workarounds include creating symlinks to a single system-wide OpenMP library or removing MKL optimizations with conda install nomkl [36].
FAQ 4: My LightGBM model training hangs or gets stuck when I use multiprocessing. How can I fix this?
This is a known issue when using OpenMP multithreading and forking in Linux simultaneously [36]. The most straightforward solution is to disable multithreading within LightGBM by setting nthreads=1. A more resource-intensive solution is to use new processes instead of forking, though this requires creating multiple copies of your dataset in memory [36].
FAQ 5: Why is early stopping not enabled by default in LightGBM?
LightGBM requires users to specify a validation set for early stopping because the appropriate strategy for splitting data into training and validation sets depends heavily on the task and domain [36]. This design gives researchers, who understand their data's structure (such as time-series data from sequential IVF cycles), the flexibility to define the most suitable validation approach.
Experimental Protocol: Predicting Blastocyst Yield in IVF Cycles
The following methodology is based on a 2025 study that developed and validated machine learning models to quantitatively predict blastocyst yields [37] [29].
Data Source and Study Population
- Dataset: The study analyzed 9,649 IVF/ICSI cycles [38] [29].
- Outcome Distribution: The dataset included cycles that produced no usable blastocysts (40.7%), 1-2 usable blastocysts (37.7%), and 3 or more usable blastocysts (21.6%) [38] [29].
- Data Splitting: The dataset was randomly split into a training set and a test set for model development and internal validation [29].
Feature Preprocessing and Selection
- Initial Feature Set: The study incorporated potential clinical predictors established in reproductive medicine.
- Feature Selection: A recursive feature elimination (RFE) process was used. The analysis found that model performance remained stable with 8 to 21 features but declined sharply with 6 or fewer features [29].
- Final Feature Set: The optimal LightGBM model utilized 8 key features [37] [29].
Model Training and Validation
- Algorithms Compared: Three machine learning models (Support Vector Machine (SVM), LightGBM, and XGBoost) were trained and compared against a traditional Linear Regression baseline [37].
- Performance Metrics: Models were evaluated using the R-squared (R²) coefficient, Mean Absolute Error (MAE), and Root Mean Square Error (RMSE) for regression tasks. For the multi-classification task (predicting 0, 1-2, or ≥3 blastocysts), accuracy and Kappa coefficients were used [37] [29].
- Validation: Internal validation was performed on the held-out test set [29].
The workflow for this experiment is summarized in the diagram below.
Performance Results and Key Features
The following tables summarize the quantitative outcomes of the cited study and the essential "research reagents" – the key input features required for the model.
Table 1: Comparative Model Performance for Blastocyst Yield Prediction (Regression Task) [37] [29]
| Model | Number of Features | R² | Mean Absolute Error (MAE) | Root Mean Square Error (RMSE) |
|---|---|---|---|---|
| LightGBM | 8 | 0.675 | 0.813 | 1.12 |
| XGBoost | 11 | 0.673 | 0.809 | 1.12 |
| SVM | 10 | 0.676 | 0.793 | 1.12 |
| Linear Regression | 8 | 0.587 | 0.943 | 1.26 |
Table 2: LightGBM Performance on Multi-Class Prediction Task [29]
| Cohort | Accuracy | Kappa Coefficient |
|---|---|---|
| Overall Test Set | 0.678 | 0.500 |
| Advanced Maternal Age Subgroup | 0.710 | 0.472 |
| Poor Embryo Morphology Subgroup | 0.690 | 0.412 |
| Low Embryo Count Subgroup | 0.675 | 0.365 |
Table 3: Research Reagent Solutions - Critical Features for Prediction
| Key Feature | Function / Rationale | Relative Importance |
|---|---|---|
| Number of Extended Culture Embryos | The total number of embryos available for blastocyst culture is the fundamental base input. | 61.5% |
| Mean Cell Number on Day 3 | Indicates normal and timely embryo cleavage, a strong marker of developmental potential. | 10.1% |
| Proportion of 8-cell Embryos on Day 3 | The presence of embryos at the ideal cell stage on day 3 is a critical positive predictor. | 10.0% |
| Proportion of Symmetrical Embryos on Day 3 | Reflects embryo quality; symmetrical cleavage is associated with higher viability. | 4.4% |
| Proportion of 4-cell Embryos on Day 2 | Indicates early and timely embryo development. | 7.1% |
| Female Age | A well-established non-lab factor influencing overall oocyte and embryo quality. | 2.4% |
Balancing Accuracy and Speed in Fertility AI Models
The case study demonstrates that LightGBM effectively balances predictive accuracy and computational efficiency, a crucial consideration for clinical AI models.
- Accuracy vs. Interpretability: While all three ML models showed comparable performance, LightGBM was selected as optimal because it achieved this performance with fewer features (8) than SVM (10) and XGBoost (11), reducing overfitting risk and enhancing simplicity for clinical application [37] [29].
- Computational Efficiency: LightGBM is engineered for speed and lower memory usage. It uses a histogram-based algorithm to bucket continuous feature values, which accelerates the training process. Furthermore, it grows trees leaf-wise rather than level-wise, which can lead to higher accuracy with fewer trees, directly contributing to faster training times – a significant advantage when iterating on model development [39].
- Clinical Utility: The model's strong performance in poor-prognosis subgroups (e.g., advanced maternal age, low embryo count) is particularly valuable [29]. These patients face more urgent dilemmas regarding extended culture, and a fast, accurate prediction can directly support critical treatment decisions.
Frequently Asked Questions (FAQs)
Q1: What are the primary benefits of combining neural networks with bio-inspired optimization algorithms? Integrating neural networks (NNs) with bio-inspired optimization algorithms (e.g., Ant Colony Optimization) creates a powerful synergy. The neural network, often a Graph Neural Network (GNN), learns to generate instance-specific heuristic priors from data. The bio-inspired algorithm, such as ACO, then uses these learned heuristics to guide its stochastic search more efficiently through the solution space. This hybrid approach leverages the pattern recognition and generalization capabilities of NNs with the powerful exploration and combinatorial optimization strength of algorithms like ACO, often leading to faster convergence and higher-quality solutions than either method could achieve alone [40].
Q2: My hybrid model is converging to suboptimal solutions. How can I improve its exploration? Premature convergence often indicates an imbalance between exploration and exploitation. You can address this by:
- Adjusting Pheromone Parameters: In ACO-based hybrids, increase the influence of the heuristic information (beta parameter) relative to the pheromone trails (alpha parameter) in the early stages of training to encourage exploration of new paths [40].
- Entropy Regularization: Incorporate entropy regularization into your reinforcement learning training protocol (e.g., when using Proximal Policy Optimization). This technique encourages the policy to be more stochastic during training, preventing it from becoming overconfident in a narrow set of actions and promoting broader exploration [40].
- Hybridization for Balance: Intentionally combine algorithms with complementary strengths. For example, one study integrated the strong exploitation phase of Bacterial Foraging Optimization (BFO) into the Artificial Bee Colony (ABC) algorithm to improve its local search capabilities and accelerate convergence, achieving a more balanced search [41].
Q3: The inference speed of my hybrid model is too slow for practical use. What optimizations can I make? Slow inference is a common challenge. Consider these strategies:
- Implement Focused Search: Instead of rebuilding complete solutions from scratch every iteration, use a method like Focused ACO (FACO). This technique performs targeted modifications around a high-quality reference solution (provided by the neural network), preserving strong substructures and only refining weaker parts of the solution, which drastically reduces computational overhead [40].
- Use Candidate Lists: Restrict the neighborhood search for each node to a "candidate list" of the most promising connections, rather than evaluating all possible connections. This significantly reduces the decision space and speeds up each iteration of the optimization algorithm [40].
- Optimize Feature Set: For the neural network component, ensure you are not using redundant features. Perform feature importance analysis and recursive feature elimination to identify the minimal set of highly predictive features, which can reduce model complexity and inference time without sacrificing accuracy [29].
Q4: How can I effectively map a real-world fertility treatment problem, like embryo selection, onto this hybrid framework? Framing a fertility AI problem requires careful definition of the problem components:
- Problem as a Graph: Define your fertility data as a graph. For example, in time-lapse imaging of embryo development, each time point or morphological feature can be a node, with edges representing temporal or structural relationships.
- Solution as a Path/Ranking: The task of selecting the best embryo can be formulated as finding the optimal "path" or sequence of developmental stages that leads to a positive outcome (e.g., blastocyst formation or fetal heartbeat), or simply as a ranking problem where the hybrid model scores and ranks embryos.
- Neural Network's Role: A GNN or CNN processes the graph or image data to extract meaningful features and generate a heuristic matrix (H_θ). This matrix predicts the "desirability" of certain developmental patterns or morphological features [40].
- Optimizer's Role: The ACO (or other bio-inspired algorithm) uses these learned heuristics to intelligently explore the vast space of possible embryo quality rankings, efficiently identifying the embryos with the highest predicted potential for success, as demonstrated by AI models that correlate embryo images with implantation success [10].
Troubleshooting Guides
Performance Degradation: Low Predictive Accuracy
Description: The hybrid model's predictions are inaccurate and do not generalize well to unseen data, failing to outperform baseline models.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Poor Heuristic Guidance | Check the correlation between the NN's output heuristics and solution quality on a validation set. | Refine the NN's training. Use a more stable RL algorithm like Proximal Policy Optimization (PPO) with a value function to reduce variance and improve the quality of the learned heuristics [40]. |
| Feature Inefficacy | Perform feature importance analysis (e.g., using LightGBM's built-in methods) to identify non-predictive features [29]. | Conduct recursive feature elimination to find the optimal subset of features. Incorporate domain knowledge (e.g., number of extended culture embryos, mean cell number on Day 3 for blastocyst prediction) to select biologically relevant features [29]. |
| Algorithm Imbalance | Analyze the search behavior; is it stuck in local optima (over-exploitation) or wandering randomly (over-exploration)? | Fine-tune the metaheuristic's parameters. For ACO, adjust the α (pheromone weight) and β (heuristic weight) parameters. Consider hybridizing two bio-inspired algorithms to balance exploration and exploitation [41]. |
Training Instability and Non-Convergence
Description: During training, the model's loss or performance metric fluctuates wildly and fails to stabilize or improve over time.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| High-Variance Gradients | Monitor the gradient norms and the variance of the reward signals in RL-based training. | Implement Gradient Clipping and Entropy Regularization. Using PPO, which constrains policy updates, is specifically designed to enhance training stability and prevent destructive policy changes [40]. |
| Incompatible Components | Test the neural network and the optimization algorithm independently to see if one is fundamentally failing. | Ensure the NN's output scale is compatible with the optimizer's expected input. Normalize heuristic values and pheromone trails to prevent one from dominating the other prematurely [40]. |
| Data Inconsistency | Verify the consistency of data preprocessing and labeling between training and validation splits. | Standardize data pipelines and augment the training set with techniques like synthetic data generation, which has been used to refine embryo evaluation models and improve robustness [14]. |
Computational Bottlenecks and Scalability Issues
Description: The model takes too long to train or perform inference, especially as problem size (e.g., number of nodes in a network, number of embryo features) increases.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Inefficient Search | Profile the code to identify if the bio-inspired optimizer is the bottleneck. | Integrate Focused ACO (FACO) and candidate lists. FACO refines existing solutions instead of building new ones from scratch, which narrows the search space and improves scalability for large problems [40]. |
| Overly Complex NN | Analyze the NN's architecture; is it deeper than necessary? | Simplify the NN model. Explore more efficient architectures or use model compression techniques like pruning. A study on blastocyst prediction found that LightGBM provided excellent accuracy with fewer features, enhancing simplicity and speed [29]. |
| Inadequate Hardware | Monitor GPU/CPU and memory utilization during training and inference. | Leverage hardware acceleration. Ensure the framework is configured to utilize GPUs for the NN's forward/backward passes and that the optimizer's code is efficiently vectorized. |
Experimental Protocols & Workflows
Protocol: Implementing a Neural-FACO Hybrid for Combinatorial Optimization
This protocol outlines the steps for building a hybrid framework like NeuFACO, which combines a GNN with a Focused Ant Colony Optimization for problems like optimal resource scheduling in IVF labs [40].
1. Problem Formulation:
- Define the problem on a graph
G = (V, E), whereVrepresents entities (e.g., cities for TSP, treatment steps, embryo samples) andErepresents connections with associated costs or distances.
2. Neural Network Training (Amortized Inference):
- Architecture: Employ a Graph Neural Network (GNN) to process the graph
G. - Outputs: The GNN should output two things: 1) A heuristic matrix
H_θ, which provides learned priors over edges, and 2) A value estimateV_θ, which predicts the expected solution quality for the instance. - Training Method: Train the GNN using Proximal Policy Optimization (PPO), an on-policy Reinforcement Learning algorithm. The reward is typically the negative of the solution cost (e.g.,
R = -C(Ï€)). Using PPO with entropy regularization encourages exploration and stabilizes training [40].
3. Focused ACO for Solution Refinement:
- Initialization: Initialize pheromone trails, often using the neural heuristic
H_θas a prior. - Solution Construction: Let ants build solutions probabilistically using a rule that combines pheromone (
τ) and neural heuristic (H_θ):p_ij ∠(τ_ij^α) * (H_θ(i,j)^β). - Focused Search: Instead of rebuilding full tours, implement FACO. Select a high-quality reference solution (e.g., the best solution from the initial phase or the NN's greedy solution). FACO then iteratively identifies and refines the weakest segments of this reference solution through local search operators like 2-opt or node relocation, dramatically improving efficiency [40].
- Pheromone Update: Update pheromone trails based on the quality of the new solutions found, reinforcing paths in the promising regions identified by the focused search.
The workflow below visualizes the architecture and data flow of this hybrid system.
Protocol: Quantitative Blastocyst Yield Prediction with Machine Learning
This protocol is adapted from a study that successfully used machine learning models (LightGBM, SVM, XGBoost) to quantitatively predict blastocyst yields in IVF cycles, a key task for balancing accuracy and speed in fertility AI [29].
1. Data Collection and Preprocessing:
- Cohort: Collect data from a large number of IVF cycles (e.g., n > 9,000).
- Feature Set: Compile a comprehensive set of potential predictors, including:
- Demographic: Female age.
- Stimulation-related: Number of oocytes retrieved, number of 2PN embryos.
- Embryo Morphology (Day 2 & 3): Number of extended culture embryos, mean cell number, proportion of 8-cell embryos, proportion of 4-cell embryos, proportion of symmetry, mean fragmentation.
- Outcome: The target variable is the number of usable blastocysts formed per cycle.
- Data Splitting: Randomly split the dataset into training and test sets (e.g., 70/30 or 80/20).
2. Model Training and Feature Selection:
- Model Selection: Train multiple machine learning models, such as LightGBM, XGBoost, and Support Vector Machines (SVM).
- Baseline Comparison: Include a traditional linear regression model as a baseline.
- Feature Selection: Use Recursive Feature Elimination (RFE) to identify the optimal subset of features. Iteratively remove the least important features until model performance (e.g., R², Mean Absolute Error) begins to drop significantly. The goal is a parsimonious model for speed and interpretability [29].
3. Model Evaluation and Interpretation:
- Performance Metrics: Evaluate models on the held-out test set using:
- R² (Coefficient of Determination): Measures the proportion of variance explained.
- Mean Absolute Error (MAE): The average absolute error between predicted and actual blastocyst counts.
- Model Interpretation: For the chosen model (e.g., LightGBM), perform:
- Feature Importance Analysis: Identify the top predictors of blastocyst yield.
- Partial Dependence Plots (PDPs) & Individual Conditional Expectation (ICE) Plots: Visualize the relationship between key features and the predicted outcome [29].
The following workflow diagram illustrates the key stages of this predictive modeling process.
Performance Data & Benchmarks
Performance of Hybrid Optimization Models
The table below summarizes the performance of various hybrid models as reported in recent research, providing benchmarks for expected improvements.
| Model / Protocol Name | Core Hybrid Approach | Key Performance Improvement | Application Context |
|---|---|---|---|
| QChOA-KELM [42] | Quantum-Inspired Chimp Optimizer + Kernel Extreme Learning Machine | 10.3% accuracy improvement over baseline KELM; outperforms conventional methods by ≥9% [42]. | Financial Risk Prediction |
| NeuFACO [40] | GNN (PPO) + Focused Ant Colony Optimization | Outperforms neural and classical baselines; solves large-scale problems (up to 1,500 nodes) [40]. | Traveling Salesman Problem |
| HBIP Protocol [41] | Artificial Bee Colony (ABC) + Bacterial Foraging Optimization (BFO) | Increased data collection by 84.40% over LEACH, 19.43% over BFO, and 7.26% over ABC [41]. | IoT Sensor Network Data Gathering |
| Hybrid ACO2 + Tabu Search [43] | ACO + Tabu Search | 73% longer network lifetime, 36% lower latency, 25% better network stability vs. existing methods [43]. | Clustered Wireless Sensor Networks |
Performance of Fertility AI Models
This table provides quantitative results from AI models applied to fertility-related tasks, illustrating the balance between accuracy and speed.
| Model / Tool Name | Task | Key Performance Metric | Notes |
|---|---|---|---|
| LightGBM Model [29] | Quantitative Blastocyst Yield Prediction | R²: 0.673-0.676, MAE: 0.793-0.809 [29] | Outperformed linear regression (R²: 0.587, MAE: 0.943); used only 8 key features for speed and interpretability [29]. |
| MAIA AI Platform [14] | Embryo Selection for IVF | 66.5% overall accuracy, 70.1% success rate for predicting clinical pregnancy [14]. | Reduces human error and standardizes embryo evaluation. |
| AI Model [14] | Embryo Development Stage Classification | Up to 97% accuracy [14] | Utilized synthetic data generation to refine the model. |
| EMBRYOAID [10] | Predicting Fetal Heartbeat | Up to 74% prediction accuracy [10] | AI outperformed traditional morphology assessments for frozen-thawed embryos. |
The Scientist's Toolkit: Research Reagent Solutions
The table below lists key computational "reagents" – algorithms, models, and tools – essential for building and experimenting with hybrid neural/bio-inspired frameworks.
| Item / Algorithm | Function / Purpose | Key Characteristics |
|---|---|---|
| Graph Neural Network (GNN) | Encodes graph-structured problem instances into meaningful feature representations and heuristic priors [40]. | Learns from graph topology and node/edge features; provides instance-specific guidance. |
| Proximal Policy Optimization (PPO) | Trains the neural network policy in a stable and sample-efficient manner [40]. | Reduces training variance via clipped objectives; supports entropy regularization for exploration. |
| Ant Colony Optimization (ACO) | A bio-inspired metaheuristic that performs stochastic, population-based search for combinatorial problems [40]. | Uses pheromone trails and heuristics; excellent for path-finding and routing problems. |
| Focused ACO (FACO) | An enhanced ACO variant that refines a reference solution via localized search [40]. | Dramatically improves convergence speed and scalability by avoiding full solution reconstruction. |
| LightGBM | A gradient boosting framework based on decision tree algorithms, used for classification and regression [29]. | High accuracy, fast training speed, and native support for feature importance analysis. |
| Recursive Feature Elimination (RFE) | Selects the most relevant features by recursively removing the least important ones [29]. | Improves model interpretability, reduces overfitting, and can increase inference speed. |
FAQs: Model Performance and Generalizability
Q1: My CNN model for embryo selection performs well on training data but generalizes poorly to new clinical datasets. What could be the cause?
A1: Poor generalization often stems from dataset bias and overfitting. To address this:
- Source Diverse Data: Ensure your training set includes embryos from diverse patient ages, stimulation protocols, and culture conditions [44]. Models trained on single-center data often fail when applied externally.
- Employ Data Augmentation: Apply random rotations, flips, and contrast adjustments to embryo time-lapse images to improve model robustness [45].
- Use Simplified Architectures: Consider very lightweight, purpose-built CNNs like SugarcaneShuffleNet (9.26 MB), which achieved 98% accuracy in agricultural diagnostics by optimizing the speed-accuracy trade-off, a principle applicable to embryo analysis [46].
Q2: How can I improve the prediction accuracy of my sperm morphology classification CNN?
A2: Enhancing accuracy involves both data refinement and model adjustments:
- Leverage Deep Learning on Videos: For motility, use CNNs and RNNs on video recordings to extract movement features, going beyond static image analysis [34] [47].
- Multi-Region Analysis: Train models to detect deformities in multiple sperm regions (acrosome, head, neck, tail) simultaneously, rather than focusing on a single segment [34].
- Optimize Feature Selection: Integrate feature optimization techniques like Principal Component Analysis (PCA) or Particle Swarm Optimization (PSO) to refine input features, which has been shown to boost model performance in related predictive tasks [48].
Q3: My model's inference time is too slow for real-time clinical use. How can I increase speed without sacrificing too much accuracy?
A3: Balancing speed and accuracy is a core research challenge.
- Architecture Choice: Implement lightweight CNN architectures like MobileNet or ShuffleNet. These models use depthwise convolutions to reduce computational load and parameters, enabling faster inference [46].
- Model Compression: Apply techniques such as pruning (removing insignificant neurons/channels) and quantization (reducing numerical precision of weights) to shrink the model size and accelerate deployment [46].
- On-Device Deployment: Deploy the optimized model on dedicated edge devices, which avoids network latency and allows for real-time analysis in the lab [46].
Performance Benchmarks: Accuracy vs. Speed
The table below summarizes key performance metrics from recent studies, illustrating the balance between accuracy and operational speed in fertility AI models.
Table 1: Performance Benchmarks for AI Models in Fertility Applications
| Application | Model / System | Key Performance Metric | Reported Performance | Inference Speed/Size | Source Context |
|---|---|---|---|---|---|
| Embryo Selection | Various AI Models (Systematic Review) | Median Accuracy (Morphology Grade) | 75.5% (Range: 59-94%) | Not Specified | [44] |
| Deep Learning Model (Time-Lapse) | AUC (Implantation Prediction) | 0.64 | Not Specified | [45] | |
| Sperm Analysis | Deep Learning for Morphology | Classification Accuracy | High Accuracy (Specific % not stated) | Real-time analysis reported | [34] |
| Live Birth Prediction | TabTransformer with PSO | Accuracy / AUC | 97% / 98.4% | Not Specified | [48] |
| Male Fertility Diagnostics | Hybrid ML-ACO Framework | Classification Accuracy | 99% | 0.00006 seconds | [49] |
| Reference Lightweight CNN | SugarcaneShuffleNet | Classification Accuracy | 98.02% | 4.14 ms per image; 9.26 MB model | [46] |
Experimental Protocols for Key Tasks
Protocol: Building a CNN for Embryo Selection from Time-Lapse Videos
Objective: To develop a CNN model capable of predicting embryo implantation potential from raw time-lapse videos.
Materials:
- Time-Lapse Incubator (e.g., EmbryoScope+) [45].
- Computing Hardware: GPU workstation for model training.
- Software: Python with deep learning libraries (e.g., TensorFlow, PyTorch).
Method:
- Data Collection & Curation:
- Collect raw time-lapse videos of embryos cultured to day 5 or 6. Each video is a sequence of images captured at set intervals (e.g., every 10 minutes) [45].
- Label videos with known implantation data (KID), categorizing them as KID-positive (clinical pregnancy) or KID-negative (implantation failure) [45].
- Video Preprocessing:
- Cropping: Automatically crop images to focus on the embryo region, reducing irrelevant background data [45].
- Frame Selection: Discard poor-quality frames with artifacts or visual defects [45].
- Resolution Adjustment: Resize frames to a lower resolution (e.g., 224x224 pixels) to manage computational load [45].
- Data Augmentation: Apply transformations (rotation, flipping, brightness/contrast variation) to the training set to improve model generalization.
- Model Training with Self-Supervised Learning:
- Phase 1 (Self-Supervised): Train a convolutional neural network using a contrastive learning framework on a large corpus of unlabeled embryo videos. This teaches the model an unbiased representation of general morphokinetic features [45].
- Phase 2 (Fine-Tuning): Transfer the pre-trained model to the specific task of implantation prediction. Use a Siamese network architecture to fine-tune the model on pairs of matched embryos from the same patient cohort but with different implantation outcomes [45].
- Phase 3 (Prediction): Use a final classifier (e.g., XGBoost) on the extracted features to make the implantation prediction, helping to prevent overfitting [45].
- Model Validation:
- Evaluate model performance on a held-out test set using metrics like Area Under the Curve (AUC), accuracy, sensitivity, and specificity [45].
The following workflow diagram illustrates this multi-stage experimental protocol.
Protocol: CNN-Based Analysis of Sperm Morphology
Objective: To automate the classification of sperm into "normal" and "abnormal" categories based on morphological features.
Materials:
- Microscopes with digital cameras for capturing sperm images.
- Computer-Aided Sperm Analysis (CASA) System for initial image acquisition [47].
- Computing Hardware: Standard GPU-enabled computer.
Method:
- Image Dataset Creation:
- Image Preprocessing:
- Normalize pixel values and resize images to a uniform input size for the CNN.
- Apply augmentation techniques (rotation, scaling, color jitter) to increase dataset diversity and robustness.
- Model Training:
- Architecture Selection: Use a Convolutional Neural Network (CNN), such as a standard architecture (e.g., ResNet) or a custom lightweight CNN [34] [46].
- Training: Train the CNN to perform multi-region classification, where the model learns to identify defects in different parts of the sperm simultaneously [34].
- Explainability: Integrate Grad-CAM or similar techniques to produce heatmaps highlighting the regions of the sperm that most influenced the classification decision, aiding clinical trust and verification [46].
- Validation:
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for Fertility AI Experiments
| Item Name | Function/Application | Specific Example / Note |
|---|---|---|
| Time-Lapse Incubator | Provides a stable culture environment while continuously capturing images of embryo development. | EmbryoScope+ [45] |
| Global Culture Medium | Supports embryo development from fertilization to blastocyst stage under time-lapse conditions. | G-TL medium [45] |
| Hyaluronidase | Enzymatically removes cumulus cells from oocytes for ICSI and precise morphological assessment. | Used during oocyte denudation [45] |
| Vitrification Kits | For cryopreserving embryos via ultra-rapid cooling, allowing for frozen-thawed embryo transfers. | Vit Kit-Freeze/Thaw (using CBS High Security straws) [45] |
| Gonadotropins | Used for controlled ovarian stimulation to obtain multiple oocytes. | Recombinant or urine-derived FSH [45] |
| GnRH Agonist/Antagonist | Prevents premature ovulation during ovarian stimulation cycles. | Triptorelin (agonist) or Ganirelix (antagonist) [45] |
| Computer-Aided Sperm Analysis (CASA) System | Automated system for initial sperm motility and concentration analysis; can be integrated with AI. | Serves as a platform for image/video data acquisition [47] |
Quantitative Performance Comparison of Predictive Models
The table below summarizes key performance metrics for Logistic Regression (LR) and Support Vector Machine (SVM) models in predicting Assisted Reproductive Technology (ART) outcomes, as reported in recent literature.
| Outcome Predicted | Model | Reported Performance | Source / Context |
|---|---|---|---|
| Live Birth | Logistic Regression | AUC: 0.74 | [50] |
| Live Birth | Support Vector Machine (SVM) | Accuracy: 0.45-0.77 (range) | [50] |
| Live Birth | Neural Network (NN) | Accuracy: 0.69-0.9 (range) | [50] |
| Clinical Pregnancy | Deep Learning (Logit Boost Ensemble) | Accuracy: 96.35% | [51] |
| Clinical Pregnancy | Life Whisperer AI | Accuracy: 64.3% | [3] |
| Clinical Pregnancy | FiTTE System (image + clinical data) | Accuracy: 65.2%, AUC: 0.7 | [3] |
| Implantation Success | AI-based Embryo Selection (Pooled) | Sensitivity: 0.69, Specificity: 0.62, AUC: 0.7 | [3] |
Essential Research Reagent Solutions
This table lists key materials and their functions for setting up experiments in fertility outcome prediction.
| Reagent / Material | Function in Experiment |
|---|---|
| MATLAB Machine Learning Toolbox | Platform for developing and comparing SVM, NN, and LR models [50]. |
| Embryo Image Capture Software (e.g., Alife Embryo Assist) | Standardized acquisition of embryo images for training and validating AI models [52]. |
| Time-Lapse Imaging Systems | Generates morphokinetic data for embryo assessment and feature extraction [3]. |
| Pre-annotated Datasets (e.g., HFEA dataset) | Provide structured, labeled historical data on IVF cycles for model training and validation [51]. |
| Feature Selection Algorithms (e.g., RReliefF) | Rank and select the most contributive features from a large set of clinical variables [50]. |
Experimental Protocol: Comparing SVM and LR for IVF Outcome Prediction
1. Objective: To assess whether machine learning algorithms (SVM and Neural Networks) provide an advantage over classic statistical modeling (Logistic Regression) for predicting intermediate and clinical IVF outcomes.
2. Dataset Preparation:
- Cohort: Data from 136 women undergoing fresh IVF cycles [50].
- Inclusion Criteria: Patients undergoing treatment for male factor or unexplained infertility, oocyte donors, or those undergoing PGD for autosomal recessive diseases. All treated with a GnRH antagonist protocol [50].
- Exclusion Criteria: Women >38 years old, those with endometriosis, PCOS, or decreased ovarian reserve (Day 3 FSH <10 IU, E2 <200 pmol/L) [50].
- Key Features: Patient age and BMI were included in all models. Clinical features added included number of previous pregnancies/deliveries, baseline estradiol, duration of stimulation, total FSH dose, number of oocytes retrieved, mature oocytes, fertilized oocytes, top-quality embryos, and maximal endometrial thickness [50].
- Predicted Outcomes: Intermediate outcomes (number of oocytes retrieved, mature oocytes, fertilized oocytes, top-quality embryos) and clinical outcomes (positive beta-hCG, clinical pregnancy, live birth) [50].
- Data Preprocessing: Data was randomly split into a training set (70%) and a test set (30%). For machine learning analyses, continuous feature values were replaced by their tertiles (1st, 2nd, or 3rd) [50].
3. Model Training & Evaluation:
- Algorithms: Logistic Regression (LR), Support Vector Machine (SVM) with Gaussian and Radial Basis Function (RBF) kernels, and Artificial Neural Networks (NN) [50].
- Model Tuning: For Neural Networks, the optimal number of nodes (10 to 50) was determined by running the algorithm on the test set 50 times for each node number and selecting the count that maximized performance [50].
- Validation: Models were created based on the training set only and then tested on the held-out test set. This process was repeated 50 times for the machine learning models due to their stochastic nature, and average performances were calculated [50].
- Performance Metrics: Accuracy, error rate (1-accuracy), and precision were calculated. Receiver operating characteristic (ROC) curves were used to assess performances for clinical outcome models [50].
Experimental Workflow for Model Comparison
Researcher's Troubleshooting Guide: FAQs
Q1: In a scenario with limited computational resources but a need for model interpretability, which model—Linear SVM or Logistic Regression—is more suitable, and why?
A: Logistic Regression is typically the better choice. It provides calibrated probabilities that are directly interpretable as confidence in a decision and outputs an unconstrained, smooth objective function [53]. The model's weights are also directly interpretable, showing the influence of each feature on the predicted outcome, which is valuable for clinical understanding.
Q2: We are dealing with a high-dimensional dataset after incorporating many engineered features from clinical records. Which model generally handles this better without overfitting?
A: Linear SVM often has an advantage in high-dimensional spaces. It relies on the support vectors and the margin, which can lead to good generalization even when the number of dimensions is high [53]. However, proper regularization is critical for both models. Logistic Regression with L1 (Lasso) or L2 (Ridge) regularization can also effectively prevent overfitting in these scenarios.
Q3: Our primary goal is to maximize the prediction accuracy for clinical pregnancy, even if the model is a "black box." Should we consider more complex models beyond Linear SVM and Logistic Regression?
A: Yes. Recent research indicates that ensemble learning methods and deep learning models can achieve significantly higher accuracy. For instance, one study using the Logit Boost ensemble method reported an accuracy of 96.35% in predicting live birth occurrences [51]. Another study found that a deep learning model was associated with an 8.9% higher pregnancy rate compared to a logistic regression model's 4.1% improvement [52].
Q4: What are the critical ethical and technical hurdles in validating these AI models for clinical use in fertility treatments?
A: Key challenges include:
- Algorithmic Bias: Models trained on non-representative datasets (e.g., predominantly from Western populations) may underperform for diverse patient groups, exacerbating health disparities [54].
- Validation Scope: Many AI tools are validated in single-center studies using surrogate endpoints like clinical pregnancy rates rather than the definitive metric of live birth rates, limiting their generalizability and proven clinical utility [54].
- Regulatory Hurdles: Evolving frameworks like the FDA's "Software as a Medical Device" (SaMD) and the EU's CE mark (e.g., for iDAScore) are still adapting to continuously learning AI systems [54].
- Data Privacy: Strict compliance with regulations like GDPR and HIPAA is required when handling sensitive genetic and clinical data [54].
Model Selection: SVM vs. Logistic Regression
Overcoming Implementation Hurdles: Optimizing Fertility AI for Clinical Use
Fundamental Concepts: Black-Box vs. Glass-Box AI
What is the fundamental difference between "black-box" and "glass-box" AI in embryology?
Black-box AI models, particularly deep learning neural networks, provide decisions without revealing their reasoning process, making it impossible to understand how input data leads to a specific embryo selection [55]. In contrast, glass-box AI uses interpretable machine learning models where the logic behind each prediction is transparent and easily understandable by human embryologists [55] [56]. This transparency allows researchers to verify that models use clinically relevant features appropriately.
Why is the "black-box" problem particularly critical in clinical embryology?
The black-box problem raises significant ethical and epistemic concerns in embryology, including: inability to trust model outputs without understanding their reasoning; potential poor generalization to different patient populations; introduction of responsibility gaps when selection choices fail; and more paternalistic decision-making that excludes clinical expertise [56]. These issues are magnified in a field where decisions impact human reproduction and future generations.
What concrete advantages do interpretable AI models offer for fertility research?
Interpretable AI models enhance research by: enabling validation of biological plausibility in predictions; facilitating feature importance analysis to discover new biomarkers; ensuring compliance with regulatory requirements; building trust through transparent decision processes; and allowing continuous refinement based on understandable failure modes [55] [56] [49]. These advantages are crucial for both scientific advancement and clinical translation.
Implementation Strategies for Glass-Box AI
What technical approaches can convert black-box predictions into interpretable insights?
Model explanation techniques like SHAP (SHapley Additive exPlanations) and LIME (Local Interpretable Model-agnostic Explanations) can be applied post-hoc to black-box models to approximate their reasoning [49]. However, inherently interpretable models like logistic regression, decision trees, and Bayesian networks provide more reliable and directly understandable outputs [55] [56]. The Proximity Search Mechanism represents another approach that provides feature-level interpretability by identifying clinically relevant patterns [49].
How can researchers validate that a "interpretable" model is truly trustworthy?
Validation should include: feature importance analysis confirming biologically plausible weighting; ablation studies testing model robustness to feature removal; cross-validation across diverse patient demographics; comparison against established clinical benchmarks; and prospective testing in real-world laboratory settings [55] [49]. A truly trustworthy model should demonstrate consistent performance degradation when clinically significant features are perturbed.
What hybrid approaches balance interpretability with complex pattern recognition?
Decomposable models that use separate neural network components for distinct measurement tasks (e.g., embryo morphology assessment) provide a middle ground [56]. These systems generate outputs that embryologists can directly verify while maintaining some deep learning advantages. Another approach combines automatically extracted image features with interpretable ranking algorithms, creating a matte-box solution [55].
Experimental Protocols for Model Development
Protocol: Developing an Interpretable Embryo Viability Prediction Model
- Objective: Create a glass-box AI model for predicting blastocyst viability using clinically interpretable features.
- Data Preparation: Curate a dataset of time-lapse embryo images with known implantation outcomes. Annotate embryos using standardized morphokinetic parameters (e.g., time to division cycles, blastulation timing) [55]. Ensure class balance through techniques like SMOTE for underrepresented outcomes.
- Feature Selection: Apply nature-inspired optimization algorithms like Ant Colony Optimization to identify the most predictive feature subset [49]. Validate feature biological relevance through embryologist consultation.
- Model Training: Implement multiple interpretable models including logistic regression, decision trees with depth limitation, and random forests. Compare against black-box benchmarks like deep neural networks.
- Interpretability Assessment: Generate feature importance rankings and decision rules. Conduct ablation studies to measure performance degradation when key features are removed.
- Validation: Use nested cross-validation and hold-out clinical testing. Measure both traditional performance metrics (AUC, accuracy) and interpretability metrics (rule complexity, feature plausibility).
Table 1: Performance Comparison of AI Approaches in Embryology
| Model Type | Representative Algorithms | Interpretability Level | Key Advantages | Documented Limitations |
|---|---|---|---|---|
| Black-Box | Deep Neural Networks (CNN) | Very Low | Handles raw image data; detects subtle patterns | Unexplainable reasoning; difficult to validate [55] |
| Matte-Box | PCA + Random Forest | Medium | Automated feature extraction | Final ranking remains opaque [56] |
| Glass-Box | Logistic Regression, Decision Trees | High | Fully transparent reasoning; clinically verifiable | May sacrifice some complex pattern recognition [55] [56] |
| Hybrid | Decomposable Neural Networks | Medium-High | Partial verification possible | Complex implementation [56] |
Troubleshooting Common Implementation Challenges
Problem: Interpretable models show significantly lower performance than black-box alternatives
- Diagnosis: This typically occurs when the interpretable model is too simplified to capture complex morphokinetic patterns, or when feature engineering fails to represent biologically relevant information.
- Solution: Implement feature engineering using convolutional neural networks for automatic annotation, then apply interpretable models for ranking [55]. Use ensemble methods combining multiple simple, interpretable models. Expand feature set to include novel biomarkers beyond traditional parameters.
Problem: Model demonstrates excellent training performance but fails in external validation
- Diagnosis: Likely caused by dataset shift, where training data doesn't represent target populations, or by the model relying on spurious correlations rather than causal relationships.
- Solution: Incorporate domain adaptation techniques; collect more diverse training data; perform extensive external validation early in development; and use causal feature selection methods to identify robust predictors [56].
Problem: Clinical embryologists resist adopting AI recommendations despite good performance
- Diagnosis: Typically stems from trust deficit due to lack of model interpretability and inability to reconcile AI recommendations with clinical expertise.
- Solution: Implement model explanation interfaces that show feature contributions to each decision; involve embryologists in feature selection and model validation; provide comprehensive interpretability reports alongside predictions [55] [56].
Problem: Model updates degrade interpretability over time
- Diagnosis: Occurs when iterative model improvements prioritize performance over explainability, gradually introducing black-box elements.
- Solution: Establish interpretability constraints in the model update protocol; regularly audit feature importance stability; maintain version-controlled interpretability documentation alongside performance metrics.
Research Reagent Solutions for Interpretable AI Experiments
Table 2: Essential Research Materials for Interpretable AI Development
| Reagent/Resource | Function in Interpretable AI Research | Implementation Considerations |
|---|---|---|
| Time-Lapse Imaging Systems | Generates rich morphokinetic data for model training and feature extraction | Ensure consistent imaging parameters across experiments for reproducible feature extraction [55] |
| Standardized Annotation Software | Creates ground truth labels for embryo development stages and quality metrics | Use systems with multiple annotator support to measure and account for human subjectivity [55] |
| Public Benchmark Datasets | Enables model comparison and reproducibility validation | Prefer datasets with diverse patient demographics and complete outcome documentation [49] |
| Model Interpretation Libraries (e.g., SHAP, LIME) | Provides post-hoc explanations for model predictions | Recognize that post-hoc explanations are approximations rather than true representations of model logic [56] |
| Clinical Outcome Data with Long-Term Follow-up | Validates that AI predictions correlate with meaningful endpoints like live birth | Prioritize datasets with comprehensive outcome tracking beyond short-term implantation [56] |
Workflow Visualization for Interpretable AI Implementation
Interpretable AI Development Workflow
Performance Benchmarking and Validation Framework
Table 3: Quantitative Performance Metrics for AI Model Evaluation
| Performance Dimension | Evaluation Metric | Black-Box Model Benchmark | Interpretable Model Benchmark | Validation Protocol |
|---|---|---|---|---|
| Predictive Accuracy | AUC-ROC | 0.93 [56] | 0.89-0.92 [55] | Nested cross-validation with held-out test set |
| Clinical Utility | Sensitivity/Specificity | 96.94% accuracy on good/poor quality [56] | Comparable to experienced embryologists [55] | Comparison against expert embryologist consensus |
| Generalizability | Performance drop across sites | Up to 30% decrease [56] | <15% decrease with proper feature engineering | Multi-center external validation |
| Computational Efficiency | Inference time per embryo | Varies by model complexity | 0.00006s demonstrated in similar domains [49] | Benchmark on standardized hardware |
| Interpretability | Feature plausibility score | Not applicable | High (directly verifiable) | Embryologist assessment of feature relevance |
Frequently Asked Questions (FAQs)
FAQ 1: Why is class imbalance a critical problem in medical AI, particularly for fertility research? Class imbalance occurs when the clinically important "positive" cases (the minority class) make up a small fraction of the dataset, while the majority class is over-represented [57] [58]. In fertility research, this is common when studying rare conditions or successful treatment outcomes. Standard machine learning models trained on such data become biased towards the majority class, systematically reducing sensitivity for detecting the minority class [57]. For example, a model might achieve high accuracy by always predicting "no disease," but this fails to identify patients with fertility issues, rendering the model clinically useless [59] [58].
FAQ 2: What are the primary sources of imbalance in medical datasets? Imbalance in medical data arises from several patterns [58]:
- Bias in data collection: Certain groups may be underdiagnosed or underrepresented.
- The prevalence of rare classes: The condition of interest is inherently rare in the population.
- Longitudinal studies: Patient drop-out or class progression over time can create imbalance.
- Data privacy and ethics: Access to data for certain sensitive conditions may be restricted.
FAQ 3: When should I use data-level methods (like resampling) versus algorithm-level methods? The choice depends on your dataset and goals [57] [59].
- Data-level methods (e.g., oversampling, undersampling) are often more intuitive and help make the dataset more suitable for traditional classification models. They are a good starting point, especially when you want to use an interpretable model like logistic regression [59].
- Algorithm-level methods (e.g., cost-sensitive learning) modify the learning algorithm itself to penalize errors on the minority class more heavily. Evidence suggests these can outperform data-level methods, especially at very high imbalance ratios (e.g., below 10%), but they are less frequently reported and can add complexity [57].
- Hybrid approaches that combine both data-level and algorithm-level strategies are increasingly common and can be highly effective [58] [49].
FAQ 4: Beyond accuracy, what metrics should I use to evaluate my model on imbalanced fertility data? Accuracy is a misleading metric for imbalanced datasets [59] [60]. A comprehensive evaluation should include [57] [58]:
- Discrimination Metrics: AUC (Area Under the ROC Curve), Sensitivity (Recall), Specificity, F1-Score, and Balanced Accuracy.
- Calibration Metrics: These assess how well the predicted probabilities match the actual observed probabilities. This is crucial for clinical risk estimation but is often under-reported [57].
- Precision-Recall Curve (PRC) and MCC: The Area Under the Precision-Recall Curve (AUPRC) and Matthews Correlation Coefficient (MCC) are considered more informative than AUC under high class skew [57].
FAQ 5: What are the common pitfalls when applying oversampling techniques like SMOTE? While powerful, oversampling techniques have limitations [57] [61]:
- Overfitting: Random oversampling can lead to overfitting due to the creation of exact duplicates of minority class examples [57].
- Unrealistic Synthetic Samples: SMOTE and its variants can generate synthetic examples that do not conform to the real data distribution, potentially introducing noise and distorting the class boundaries [57] [61]. This is a significant concern with complex medical data.
- Ignoring Data Distribution: Basic SMOTE does not account for the underlying complexity and heterogeneity of the data [61].
Troubleshooting Guides
Problem 1: My model has high overall accuracy but is failing to identify the rare positive cases (e.g., patients with a specific fertility disorder).
- Potential Cause: The model is biased towards the majority class due to severe class imbalance.
- Solution Steps:
- Diagnose: Check the confusion matrix and focus on sensitivity (recall) for the minority class. This metric will be very low.
- Apply Resampling: Implement a resampling strategy on the training set only (to avoid data leakage) to balance the class distribution.
- Start Simple: Begin with Random Oversampling (ROS) or Random Undersampling (RUS) to establish a baseline [62].
- Advance to Synthetic Methods: If performance is insufficient, try synthetic oversampling with SMOTE or ADASYN [59] [62].
- Evaluate Correctly: Monitor the change in sensitivity and F1-score on a held-out test set that has not been resampled.
Problem 2: After applying SMOTE, my model's performance degraded, or the synthetic data seems unrealistic.
- Potential Cause: SMOTE is generating noisy or unrealistic synthetic samples that do not align with the true data manifold.
- Solution Steps:
- Try Advanced Variants: Use SMOTE variants that are more robust, such as Borderline-SMOTE or SMOTE-NC, which are designed to handle data complexity better.
- Clean with Undersampling: Combine SMOTE with an undersampling technique like Tomek Links (SMOTE-Tomek) to remove noisy majority class examples that lie close to the decision boundary [62].
- Explore Deep Learning Methods: For complex, high-dimensional data, consider deep learning-based oversampling like Auxiliary-guided Conditional Variational Autoencoders (ACVAE), which can better capture the underlying data distribution [61].
- Switch Strategies: Consider algorithm-level approaches like cost-sensitive learning, which avoids altering the training data altogether [57].
Problem 3: I have a very small dataset, and I am concerned that undersampling will discard critical information.
- Potential Cause: Undersampling the majority class in a small dataset can indeed lead to significant loss of information and poor model generalization.
- Solution Steps:
- Prioritize Oversampling: In this scenario, oversampling techniques (random or synthetic) are generally preferred over undersampling [59].
- Use Hybrid Sampling: Apply a hybrid method that performs a gentle undersampling of the majority class (e.g., using Edited Nearest Neighbors) combined with oversampling of the minority class to retain more information [58] [61].
- Employ Cost-Sensitive Learning: This is an ideal alternative, as it uses all available data but assigns a higher misclassification cost to the minority class during model training [57] [60].
- Leverage Ensemble Methods: Use ensemble methods like Balanced Random Forests or EasyEnsemble, which internally use undersampling in a way that mitigates information loss by building multiple models on different subsets of data [58].
Problem 4: I need to deploy a fast, real-time fertility diagnostic model, but the resampling process is slowing down my pipeline.
- Potential Cause: Some resampling techniques, especially complex synthetic ones, are computationally expensive and may not be suitable for real-time applications.
- Solution Steps:
- Preprocess and Cache: Perform all resampling during the data preprocessing and model training phase. The final deployed model should be trained on the resampled dataset but does not need to perform resampling at inference time.
- Consider Algorithmic Solutions: Implement cost-sensitive learning. While the training process might be slightly more complex, the inference speed is the same as a standard model, as no data-level preprocessing is required for new predictions [57].
- Optimize with Bio-Inspired Algorithms: As demonstrated in male fertility diagnostics, integrating nature-inspired optimization like Ant Colony Optimization (ACO) can enhance learning efficiency and convergence speed, leading to faster model training without sacrificing accuracy [49].
The following tables consolidate key quantitative findings from recent research on handling class imbalance.
Table 1: Optimal Thresholds for Stable Model Performance in Medical Data This table summarizes findings on minimum sample sizes and positive event rates required for stable logistic regression model performance [59].
| Parameter | Sub-Optimal Range | Optimal Cut-off | Context |
|---|---|---|---|
| Minority Class Prevalence | Performance low below 10% | 15% | Logistic model performance stabilized beyond this threshold. |
| Total Sample Size | Performance poor below 1200 | 1500 | Sample sizes above this threshold showed improved results. |
Table 2: Efficacy of Imbalance Treatment Methods on Low Positive Rate Data This table compares the effectiveness of different data-level methods applied to datasets with low positive rates and small sample sizes [59].
| Method | Category | Key Finding |
|---|---|---|
| SMOTE | Synthetic Oversampling | Significantly improved classification performance. |
| ADASYN | Synthetic Oversampling | Significantly improved classification performance. |
| OSS | Undersampling | Not specified in excerpt. |
| CNN | Undersampling | Not specified in excerpt. |
Table 3: Class Imbalance Classification and Thresholds This table defines the degree of imbalance and its impact, based on synthesis from multiple sources [57] [58].
| Imbalance Ratio (IR) | Description | Impact on Model |
|---|---|---|
| IR < 2 | Mild Imbalance | Often manageable by robust algorithms. |
| 2 < IR < 10 | Moderate Imbalance | Resampling or cost-sensitive methods are beneficial. |
| IR > 10 | Severe Imbalance | Significant bias; advanced methods (e.g., hybrid, cost-sensitive) are crucial [57]. |
Experimental Protocols
Protocol 1: Benchmarking Resampling Techniques for a Fertility Dataset
This protocol provides a step-by-step methodology for comparing different imbalance treatment strategies.
Data Preparation and Splitting:
- Obtain a labeled fertility dataset (e.g., clinical records with a binary outcome like "cumulative live birth").
- Split the data into a 70% training set and a 30% held-out test set. The test set must remain unmodified and reflect the original class distribution.
Training Set Resampling (Apply individually):
- Baseline: Train a model on the original, imbalanced training set.
- Random Oversampling (ROS): Duplicate minority class instances randomly until classes are balanced [62].
- Random Undersampling (RUS): Randomly remove majority class instances until classes are balanced [62].
- SMOTE: Generate synthetic minority class instances using the k-nearest neighbors algorithm (typical k=5) [59] [62].
- ADASYN: Generate synthetic minority class instances, focusing on those that are harder to learn [59].
Model Training and Evaluation:
- Train identical classification models (e.g., Logistic Regression, Random Forest) on each resampled training set.
- Apply all trained models to the untouched test set.
- Evaluate using a suite of metrics: AUC, Sensitivity, Specificity, F1-Score, and Precision-Recall Curve (PRC).
Protocol 2: Implementing a Hybrid ACO-NN Framework for Male Fertility Diagnosis
This detailed protocol is based on a study that achieved high sensitivity for male fertility diagnostics [49].
Data Preprocessing:
- Data Cleaning: Remove duplicate rows and handle missing values (e.g., by imputation or removal).
- Range Scaling: Normalize all features to a [0, 1] range using Min-Max normalization to ensure consistent scaling and model stability [49].
- Feature Selection: Use a method like Random Forest with Mean Decrease Accuracy (MDA) to identify the most important predictive variables [59].
Model and Optimization Setup:
- Initialize Neural Network (NN): Define a multilayer feedforward neural network (MLFFN) architecture.
- Integrate Ant Colony Optimization (ACO): Utilize ACO for adaptive parameter tuning of the NN. The ACO algorithm mimics ant foraging behavior to efficiently search for the optimal set of weights and biases that minimize the classification error.
Training and Interpretation:
- Hybrid Training: Train the MLFFN-ACO model, where the ACO algorithm guides the optimization process, enhancing convergence and predictive accuracy.
- Feature Importance Analysis: Use a technique like the Proximity Search Mechanism (PSM) to provide interpretable, feature-level insights, highlighting key contributory factors (e.g., sedentary habits, environmental exposures) [49].
Workflow and Relationship Diagrams
Diagram 1: Decision Workflow for Imbalance Treatment
This diagram outlines a logical workflow for selecting the appropriate technique to handle class imbalance in a medical dataset.
Diagram 2: Resampling Techniques Taxonomy
This diagram provides a visual taxonomy of common techniques for handling class imbalance at the data level.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Tools for Imbalanced Medical Data Research
This table details key software tools and libraries essential for implementing the techniques discussed in this guide.
| Item / Library | Function | Application Context |
|---|---|---|
| imbalanced-learn (Python) | Provides a wide range of resampling techniques including ROS, RUS, SMOTE, ADASYN, and Tomek Links. | The primary library for implementing data-level resampling strategies in Python [62]. |
| XGBoost / LightGBM | Advanced ensemble learning frameworks that can be made cost-sensitive by adjusting the scale_pos_weight parameter or using sample weights. |
For implementing powerful algorithm-level, cost-sensitive models without data modification. |
| ACVAE Model | A deep learning-based oversampling method using an Auxiliary-guided Conditional Variational Autoencoder to generate high-quality synthetic samples. | For addressing complex, high-dimensional medical data where traditional SMOTE may fail [61]. |
| Ant Colony Optimization (ACO) | A nature-inspired optimization algorithm used for tuning model parameters and feature selection. | Enhances model efficiency and accuracy, as demonstrated in male fertility diagnostics [49]. |
| SHAP / LIME | Explainable AI (XAI) libraries that provide post-hoc interpretations of model predictions. | Critical for understanding model decisions and building clinical trust, especially with complex models [49]. |
FAQs: Addressing Core Adoption Challenges
Question: What are the most significant financial barriers to adopting AI in fertility research?
The high cost of AI technologies is consistently reported as the primary financial barrier. A 2025 global survey of fertility specialists found that 38.01% of respondents cited cost as the main obstacle to implementation [8]. These costs are multifaceted, encompassing not only the initial purchase of commercial AI systems but also the significant capital expenditure required for in-house development, which involves high opportunity costs and limited data access [63].
Question: How does a lack of training hinder AI integration in research and clinical practice?
A deficiency in specialized training is a major impediment, cited by 33.92% of professionals in 2025 [8]. This barrier manifests as an inability to critically evaluate and trust AI tools. For instance, complex "black box" algorithms can lack transparency, making clinicians hesitant to adopt recommendations whose reasoning they cannot understand [22]. Furthermore, without proper training, staff may be unable to discern between well-validated AI tools and those marketed pre-maturely, potentially leading to the implementation of unreliable systems [22] [63].
Question: What are the key regulatory and validation challenges for new fertility AI models?
A core challenge is the rigorous prospective validation required before clinical implementation. Many novel AI technologies are commercially offered to clinics without robust scientific validation [22]. One trial highlighted this issue when an AI system for embryo selection, despite reducing evaluation time, resulted in statistically inferior live birth rates compared to manual assessment [22]. This underscores that improved efficiency (speed) does not guarantee superior clinical accuracy. Furthermore, the field lacks universal regulatory frameworks, and the fast-moving nature of AI technology means that algorithms can become outdated during the lengthy timeline of a traditional clinical trial [22] [4].
Question: What is the "AI hallucination" problem in fertility, and how can it be mitigated?
AI hallucination occurs when models generate inaccurate or fabricated information, a significant risk in high-stakes fields like fertility medicine [63]. This is often because many AI models are trained on generic, publicly available data that may be outdated or unverified, rather than on specific, real-world fertility data [63]. To mitigate this, researchers should prioritize methods like Retrieval-Augmented Generation (RAG), which supplements AI responses with verified, real-time data sources, and the use of graph database architectures, which better recognize complex relationships between diverse data points (e.g., hormonal levels, embryonic development) to improve predictive accuracy and reduce errors [63].
Troubleshooting Guides: Balancing Accuracy and Speed
Problem: High-Performance Model Fails to Generalize to New Clinic Data
This is a common problem where a model with high reported accuracy performs poorly on external data, often due to overfitting or data bias.
Investigation and Resolution Protocol:
Step 1: Data Bias Audit
- Action: Compare the demographic and clinical characteristics (e.g., patient age, infertility diagnosis, stimulation protocols) of your local dataset with the population the model was trained on.
- Rationale: Models trained on non-diverse datasets fail to generalize. Studies note that limited model generalizability and data bias are ongoing challenges that restrict equitable implementation [12] [13].
Step 2: Implement Federated Learning
- Action: Instead of centralizing data, propose a collaborative framework where the model is trained across multiple institutions without sharing sensitive raw data.
- Rationale: This technique allows for model improvement using diverse datasets from different clinics and populations, enhancing generalizability while maintaining data privacy [12].
Step 3: Recalibrate the Model
- Action: Use a portion of your local data to fine-tune or recalibrate the existing model's parameters.
- Rationale: This adjusts the model's predictions to better align with the local patient population and clinical practices, bridging the performance gap without building a new model from scratch.
Problem: Trade-off Between Model Interpretability and Predictive Performance
Researchers often face a choice between complex, high-accuracy models that are less interpretable and simpler, more transparent models.
Decision Framework and Mitigation Strategy:
Framework Application:
- Choose a complex model (e.g., Deep Learning) when the task requires detecting subtle, non-linear patterns imperceptible to humans (e.g., analyzing time-lapse embryo video for ploidy prediction) and where the primary goal is maximal predictive power, with interpretability as a secondary concern [22] [8].
- Choose an interpretable model (e.g., Logistic Regression, Decision Trees) for clinical decision support where understanding the rationale is crucial for clinician trust, or for regulatory submissions where explaining the model's reasoning is necessary [22].
Mitigation Strategy: Employ "Explainable AI" (XAI) Methods
- Action: Utilize XAI techniques like SHAP (SHapley Additive exPlanations) or LIME (Local Interpretable Model-agnostic Explanations) on your complex model.
- Example: A research team used explainable AI to identify the specific follicle sizes most likely to yield mature oocytes, transforming a complex model into actionable, clinically understandable insights [22]. This builds trust and allows clinicians to validate the model's logic against their own expertise.
Problem: Managing Computational Cost and Speed in Model Training
Large-scale model training, especially with images and time-lapse videos, is computationally expensive and time-consuming.
Optimization Checklist:
- Utilize Transfer Learning: Start with a pre-trained model on a large, general image dataset (e.g., ImageNet) and fine-tune it for your specific fertility task (e.g., sperm morphology analysis). This significantly reduces the required data and training time [34].
- Implement Data Pre-processing: Reduce image resolution or apply pruning and quantization techniques to the model architecture to decrease computational load without a significant loss in performance [4].
- Benchmark Resource Usage: Before full-scale training, run small-scale pilots to profile the memory and processing requirements of different algorithms to select the most efficient one for your available infrastructure.
Table 1: Barriers to AI Adoption in Reproductive Medicine (2025 Survey Data) [8]
| Barrier Category | Percentage of Respondents Citing (%) |
|---|---|
| Cost | 38.01% |
| Lack of Training | 33.92% |
| Ethical Concerns | Not Quantified |
| Over-reliance on Technology | 59.06% |
| Data Privacy Concerns | Not Quantified |
Table 2: Adoption Trends and Familiarity with AI in IVF (2022 vs. 2025) [8]
| Metric | 2022 | 2025 |
|---|---|---|
| AI Usage Rate | 24.8% | 53.22% (combined regular and occasional) |
| Regular Use | Not Specified | 21.64% |
| Occasional Use | Not Specified | 31.58% |
| Moderate-to-High Familiarity | Lower (indirect evidence) | 60.82% |
Experimental Protocol: Validating an AI Model for Embryo Selection
This protocol provides a methodology for prospectively validating a new AI model for embryo selection, balancing the need for speed (automated assessment) with the highest standard of accuracy (live birth outcome).
1. Objective: To determine if an AI model for selecting blastocysts for transfer is non-inferior to the standard morphological assessment by senior embryologists in achieving live birth rates.
2. Materials and Reagents:
Table 3: Key Research Reagent Solutions for Embryo Selection Validation
| Item | Function in Experiment |
|---|---|
| Time-lapse Incubator System | Provides the continuous imaging data (videos and images) required for both AI and manual embryologist assessment without disturbing the culture environment. |
| AI Model/Software | The intervention being tested; analyzes time-lapse images to predict embryo viability and select the one with the highest potential for live birth. |
| Structured Dataset for Training | A prerequisite for developing the model; must include de-identified time-lapse data linked to known clinical outcomes (e.g., implantation, live birth). |
| Electronic Health Record (EHR) System | Source for extracting key patient covariates (e.g., age, BMI, AMH) for subgroup analysis and ensuring proper blinding by only revealing patient allocation. |
3. Methodology:
- Study Design: A multi-center, randomized, double-blind, non-inferiority trial.
- Participants: Couples undergoing a single blastocyst transfer cycle. Key exclusion criteria include the use of donor gametes and preimplantation genetic testing.
- Randomization and Blinding:
- On the day of transfer, eligible embryos with adequate quality are randomized to be selected either by the AI model or by a senior embryologist using standard morphological grading.
- The clinical team performing the embryo transfer and the patients are blinded to the selection method.
- Primary Outcome: Live birth rate per randomized cycle.
- Statistical Analysis:
- A non-inferiority margin is set a priori (e.g., a 5% absolute difference).
- Analysis is performed on an intention-to-treat basis. The primary comparison will use a chi-square test to determine if the AI group's live birth rate is non-inferior to the embryologist group.
- Secondary Outcomes: Include clinical pregnancy rate, miscarriage rate, and time taken for embryo evaluation (to measure the "speed" advantage).
This rigorous design directly addresses the validation challenge highlighted in the literature, ensuring that a gain in speed does not come at the cost of reduced accuracy [22].
Workflow and System Architecture Diagrams
AI Validation and Implementation Workflow
Data Architecture for Minimizing AI Hallucination
Data Preprocessing and Feature Engineering for Enhanced Computational Efficiency
Troubleshooting Guides & FAQs
This technical support center provides solutions for common challenges in data preprocessing and feature engineering, specifically tailored for research on fertility Artificial Intelligence (AI) models where balancing predictive accuracy with computational speed is paramount [64].
Data Preprocessing
FAQ 1: My fertility dataset has a significant amount of missing clinical data (e.g., hormone levels, sperm motility). What is the most robust method to handle this without introducing bias?
The optimal strategy depends on the extent and nature of the missing data. For datasets with a small proportion of missing values, imputation is generally preferred over deletion to preserve data for training [65].
- Recommended Methodology:
- Evaluate Missingness Pattern: First, assess whether the data is missing completely at random (MCAR), at random (MAR), or not at random (MNAR). This influences the choice of imputation method.
- For Low Missingness (<5% per feature): Use statistical imputation. The median is recommended for numerical features to mitigate the effect of outliers, while the mode is suitable for categorical features [65].
- For High Missingness or Complex Patterns: Consider using advanced imputation techniques like Multiple Imputation by Chained Equations (MICE) or leverage algorithms that can handle missing values natively, such as Random Forests [66].
FAQ 2: My model's training time is excessively long due to the high-dimensional nature of my dataset, which includes genetic, clinical, and lifestyle factors. How can I accelerate this?
High-dimensional data leads to the "curse of dimensionality," significantly increasing computational cost and the risk of overfitting [67]. Implementing data parallelism and leveraging high-performance computing libraries can drastically reduce preprocessing and training times [68].
- Experimental Protocol for Parallelization:
- Tool Selection: Adopt a parallel computing framework like MPI4Py, which allows you to parallelize both data preprocessing and model training tasks across multiple CPU cores or nodes [68].
- Implementation:
- Partition your large fertility dataset (e.g., data from thousands of IVF cycles) across the available processors [68].
- Execute data cleaning, normalization, and feature scaling operations concurrently on each data partition.
- For model training, use a data-parallel approach where the model is replicated on each processor, and gradients are aggregated after processing individual data shards.
- Validation: Compare the total execution time (preprocessing + training) against a sequential processing baseline. The parallelized approach should show a near-linear speedup with the number of processors [68].
FAQ 3: My model's performance is degraded after one-hot encoding categorical variables (e.g., infertility diagnosis type, ovarian stimulation protocol). Why did this happen?
One-hot encoding can lead to a sparse matrix with many features, increasing dimensionality and potentially diluting the predictive signal. It can also introduce multicollinearity if not handled correctly [66].
- Troubleshooting Guide:
- Check for High-Cardinality Features: If a categorical variable has many unique values (e.g., "patient zip code"), one-hot encoding will create a large number of new columns. Consider alternative encoding like target encoding (replacing categories with the mean of the target variable) or frequency encoding (replacing categories with their frequency of appearance) [66].
- Address Multicollinearity: After one-hot encoding, drop one of the categories to serve as a reference baseline, preventing perfect multicollinearity which can destabilize some models [69].
- Evaluate Alternative Techniques: For ordinal categorical variables (e.g., "sperm motility grade"), use label encoding to preserve the order.
Feature Engineering & Selection
FAQ 4: Which feature selection technique is most effective for identifying the strongest predictors of IUI success from a set of 20+ clinical parameters?
The Permutation Feature Importance method is a model-agnostic and reliable technique for this task. It directly measures the contribution of each feature to your model's performance [16].
- Detailed Methodology:
- Train a Model: First, train a baseline model (e.g., Linear SVM or Random Forest) on your dataset of IUI cycles and record its performance score (e.g., AUC or accuracy) [69] [16].
- Permute and Measure: For each feature (e.g., maternal age, pre-wash sperm concentration), randomly shuffle its values across the dataset, breaking the relationship between that feature and the outcome.
- Re-evaluate Performance: Using the shuffled data and the previously trained model, recalculate the performance score. The drop in the performance score (e.g., AUC decrease from 0.78 to 0.72) quantifies the importance of that feature [69] [16].
- Rank Features: Rank all features based on the magnitude of their performance drop. A larger drop indicates a more important feature.
Table 1: Quantitative Feature Importance in IUI Outcome Prediction (based on a Linear SVM model) [69]
| Clinical Feature | Impact on Model Performance (AUC) | Relative Importance |
|---|---|---|
| Pre-wash Sperm Concentration | Strong positive predictor | Highest |
| Ovarian Stimulation Protocol | Strong positive predictor | High |
| Cycle Length | Strong positive predictor | High |
| Maternal Age | Strong positive predictor | High |
| Paternal Age | Weak predictor | Lowest |
FAQ 5: How do I balance the trade-off between using a complex, high-accuracy model and a faster, more interpretable one for clinical deployment?
This is a fundamental trade-off between model complexity and interpretability [64]. In fertility AI, a hybrid approach is often most effective.
- Decision Framework:
- For High-Stakes Diagnostic Support: Use the complex model (e.g., ensemble methods or deep learning) for its superior accuracy, but employ post-hoc explanation tools like SHAP (SHapley Additive exPlanations) to interpret individual predictions and build clinician trust [64].
- For Rapid Screening or Resource-Limited Settings: Prioritize simpler, more interpretable models like logistic regression or decision trees. Their decisions are easier to validate and explain to patients [64].
- Hybrid Strategy: Use the complex model for initial, high-confidence predictions and flag more complex cases for review by both the simpler model and a human expert [64].
FAQ 6: My model performs well on training data but poorly on new patient data from a different clinic. What feature engineering steps can improve generalizability?
This indicates overfitting and poor model generalization, often due to clinic-specific biases in the data. The solution involves feature scaling and creating more robust, domain-informed features.
- Experimental Protocol for Robust Feature Scaling:
- Identify Scale Variance: Check if your features (e.g., follicle size in mm, hormone levels in pg/mL, patient age) are on different scales. Models like SVMs and neural networks are highly sensitive to this [65].
- Choose a Scaler:
- Critical: Fit on Training, Transform on Test: To avoid data leakage, fit the scaler (calculate mean and standard deviation) only on the training set. Then use this fitted scaler to transform both the training and test sets. Never fit the scaler on the entire dataset [65].
Data Preprocessing Pipeline to Prevent Data Leakage
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools for Fertility AI Research
| Tool / Reagent | Function / Application | Technical Notes |
|---|---|---|
| MPI4Py | A Python library for parallel computing. Speeds up data preprocessing and model training on large datasets (e.g., 9500+ IUI cycles) [68]. | Enables data and model parallelism to minimize high computational costs [68]. |
| Scikit-learn | A core ML library for Python. Provides unified APIs for feature selection, imputation, scaling, and model training [69] [65]. | Includes SimpleImputer, StandardScaler, RobustScaler, and multiple feature selection algorithms [65]. |
| Permutation Feature Importance | A model-agnostic method for feature selection. Ranks variables (e.g., maternal age, sperm concentration) by impact on model performance [16]. | More reliable than filter-based methods as it uses the actual model's performance metric [16]. |
| SHAP (SHapley Additive exPlanations) | A game-theoretic approach to explain the output of any ML model. Critical for interpreting "black-box" models in a clinical context [64]. | Helps identify which patient factors most influenced a specific prediction (e.g., high FSH level was the key negative factor). |
| PowerTransformer | A normalization tool that maps data to a Gaussian distribution. Can improve model convergence and performance for skewed data [69]. | Used in state-of-the-art fertility prediction models to preprocess data before training a Linear SVM [69]. |
Taxonomy of Feature Engineering Techniques
Benchmarking Performance: Validation Frameworks and Comparative Analysis of Fertility AI
FAQs: Troubleshooting Your AI Validation RCT
This section addresses common challenges researchers face when designing and executing Randomized Controlled Trials (RCTs) for validating artificial intelligence (AI) tools in fertility and other medical fields.
FAQ 1: Our AI model performed well in development but shows no clinical benefit in the RCT. What happened? This is a common finding, underscoring the critical difference between technical and clinical performance. A model's high accuracy on retrospective data does not guarantee it will improve patient outcomes in practice.
- Troubleshooting Steps:
- Investigate Workflow Integration: Analyze if the AI tool's output is effectively presented and acted upon by clinicians. A poor user interface or integration into clinical workflow can nullify the tool's potential benefit.
- Check for Performance Drift: Evaluate if the real-world data in the RCT differs from the development data (e.g., different patient demographics, imaging equipment, or clinical procedures). This can cause a drop in performance.
- Re-examine the Primary Outcome: Ensure the RCT's primary outcome is appropriate and sensitive enough to capture the AI's effect. A surrogate outcome might not translate to a final patient outcome like live birth.
- Consult Existing Evidence: Note that a systematic review found that nearly two-fifths of trial interventions for AI prediction tools showed no clinical benefit over standard care [70].
- Troubleshooting Steps:
FAQ 2: We are getting pushback that our RCT is unethical as it withholds a potentially beneficial AI tool from the control group. How do we respond? This concern is often addressed through robust trial design and a clear understanding of clinical equipoise.
- Troubleshooting Steps:
- Establish Equipoise: Clearly state in your protocol that there is genuine uncertainty within the expert clinical community regarding the AI tool's net benefit. If the tool's superiority were known, an RCT would indeed be unethical [71].
- Use a Standard-of-Care Control: In almost all AI-RCTs, the control group receives the current standard of care, which is by definition an ethical treatment [72]. You are testing whether the AI tool is better than this existing standard.
- Design a Pragmatic Trial: Frame the trial as a necessary step to generate the high-quality evidence required for safe and effective implementation, thus ultimately benefiting all future patients.
- Troubleshooting Steps:
FAQ 3: How can we mitigate the risk of our AI tool becoming outdated by the time the lengthy RCT is complete? The rapid pace of AI development poses a unique challenge for traditional RCTs.
- Troubleshooting Steps:
- Adopt a "Living RCT" Framework: Consider a platform trial design that allows for continuous, pre-approved updates to the AI intervention arm as improved versions become available, while the control arm remains constant.
- Focus on Validating the Core Task: Ensure the RCT tests the fundamental clinical question the AI addresses. A robustly validated concept may remain relevant even as the underlying algorithm evolves.
- Plan for Iterative Validation: Acknowledge that a single RCT may not be the final word. Build a pathway for more efficient, ongoing evaluation, such as through registry-based trials, to keep pace with technological advances [22].
- Troubleshooting Steps:
FAQ 4: Our RCT is underpowered due to a rare primary outcome. What are our options? Underpowered trials are inconclusive and waste resources. Proactive planning is key.
- Troubleshooting Steps:
- Reconsider the Primary Outcome: If possible, select a more frequent, clinically relevant surrogate or process outcome that is strongly correlated with your original, rarer outcome.
- Initiate a Multi-Center Collaboration: Recruit patients from multiple sites to increase the sample size and diversity of your study population. Many AI-RCTs are multi-centered for this reason [72].
- Extend the Recruitment Period: If feasible, a longer recruitment duration can help reach the required sample size.
- Conduct a Sample Size Re-estimation: If blinded interim data allows, consider a formal sample size re-estimation to adjust your target based on the observed outcome rate.
- Troubleshooting Steps:
Experimental Protocol: Key Phases for an AI Validation RCT
The following workflow outlines the critical stages for conducting a rigorous RCT to validate a clinical AI tool.
Quantitative Landscape of AI RCTs
The table below summarizes data from systematic reviews on the characteristics and outcomes of published RCTs evaluating AI tools in medicine [72] [70].
| Aspect | Summary Data |
|---|---|
| Total Unique AI Tools Evaluated | 18 tools (across 23 RCTs) [72] |
| Median Target Sample Size | 298 (IQR 219–850) for protocols; 214 (IQR 100–437) for published trials [72] |
| RCTs with Positive Primary Outcome | 82% (14 of 17 completed trials) favored the AI intervention [72] |
| Trials with No Clinical Benefit | Nearly two-fifths (approx. 40%) of trials showed no benefit over standard care [70] |
| Rate of Low Risk of Bias | 26% (17 of 65 trials) were assessed as having a low risk of bias [70] |
| Multicenter Trials | 52% of identified AI-RCTs were multicenter studies [72] |
The Scientist's Toolkit: Key Reagents for AI Validation
This table details essential components and methodologies for developing and validating AI models in fertility research.
| Item / Solution | Function in AI Validation |
|---|---|
| Structured Health Records | Provides curated, tabular clinical data (e.g., patient history, hormone levels) for model training on tasks like predicting ovarian response or live birth [12]. |
| Time-Lapse Embryo Imaging | Generates rich, sequential image data for deep learning models to analyze embryo morphology and development, predicting implantation potential [22]. |
| TRIPOD+AI Statement | A reporting guideline ensuring transparent and complete reporting of AI prediction model development and validation, crucial for replication and review [22]. |
| CONSORT-AI Extension | A 37-item checklist with 14 new AI-specific items for reporting RCTs evaluating AI interventions, improving trial rigor and transparency [70]. |
| Federated Learning Platforms | An emerging technology that enables training AI models across multiple clinics without sharing sensitive patient data, helping to improve model generalizability and address data privacy [12]. |
| Explainable AI (XAI) Methods | Techniques used to interpret the predictions of complex models (e.g., identifying which follicle sizes most impact oocyte maturity), building clinical trust and providing biological insights [22]. |
In the rapidly evolving field of fertility research, artificial intelligence (AI) models offer promising tools for predicting outcomes ranging from in vitro fertilization (IVF) success to population-level fertility preferences. A central challenge for researchers and drug development professionals lies in selecting the optimal algorithmic approach that balances competing priorities: predictive accuracy against computational speed, and model performance against clinical interpretability. This technical support guide provides a structured framework for comparing traditional logistic regression against black-box deep learning models, with specific application to fertility AI research. Through comparative performance data, troubleshooting guidance, and experimental protocols, this resource aims to equip scientists with the practical knowledge needed to make informed methodological choices in their reproductive health investigations.
Performance Benchmarking: Quantitative Comparisons
The table below synthesizes performance metrics from recent fertility-related studies to facilitate direct algorithm comparisons.
Table 1: Comparative Performance of Algorithms in Fertility and Healthcare Research
| Study Context | Logistic Regression Performance | Deep Learning/ML Performance | Optimal Model | Key Performance Metrics |
|---|---|---|---|---|
| Abdominal Aortic Aneurysm Repair Prediction [73] | Accuracy: 91% ± 3%, AUROC: 79% ± 5% | XGBoost Accuracy: 95% ± 2%, AUROC: 86% ± 5% | XGBoost | Accuracy, Specificity, Sensitivity, AUROC |
| IVF Live Birth Prediction [48] | Not Reported | TabTransformer Accuracy: 97%, AUC: 98.4% | TabTransformer (Deep Learning) | Accuracy, AUC |
| Fertility Preferences in Nigeria [74] | Not Reported | Random Forest Accuracy: 92%, AUROC: 92% | Random Forest | Accuracy, Precision, Recall, F1-Score, AUROC |
| Fertility Preferences in Somalia [75] [76] | Not Reported | Random Forest Accuracy: 81%, AUROC: 0.89 | Random Forest | Accuracy, Precision, Recall, F1-Score, AUROC |
| Delayed Fecundability in Sub-Saharan Africa [77] | Not Reported | Random Forest Accuracy: 79.2%, AUC: 0.94 | Random Forest | Accuracy, AUC |
Technical Support: Troubleshooting Guides and FAQs
FAQ 1: When should I choose logistic regression over deep learning for fertility research?
Answer: Logistic regression is preferable when:
- Small to Moderate Datasets: Your dataset contains hundreds to thousands of samples rather than millions [78]
- Interpretability is Critical: You need transparent, clinically explainable models where feature coefficients provide clear insights [79] [73]
- Structured Tabular Data: You're working with structured clinical data (electronic health records, demographic surveys) [79] [78]
- Limited Computational Resources: You require faster training times and lower infrastructure costs [78]
- Linear Relationships: Your predictors have approximately linear relationships with the outcome [79]
Troubleshooting Tip: If logistic regression underperforms but interpretability remains crucial, consider using SHAP (Shapley Additive Explanations) with ensemble methods to create interpretable surrogate models [73].
FAQ 2: How can I address the "black box" problem of deep learning in fertility clinical applications?
Answer: Implement Explainable AI (XAI) techniques:
- SHAP Analysis: Quantifies feature contributions to individual predictions, making model decisions transparent [75] [73] [76]
- Surrogate Models: Train interpretable logistic regression models on deep learning outputs to maintain explainability [73]
- Feature Importance Visualization: Use permutation importance or Gini importance to identify influential predictors [74]
- Clinical Validation: Correlate model predictions with established clinical knowledge and biomarkers
Troubleshooting Tip: For journal submissions, include SHAP summary plots and individual prediction explanations to address reviewer concerns about model interpretability.
FAQ 3: What are the common data preparation challenges when applying deep learning to fertility datasets?
Answer: Common issues and solutions:
- Class Imbalance: Use Synthetic Minority Oversampling Technique (SMOTE) to balance fertility preference classes [74]
- Missing Data: Implement Multiple Imputation by Chained Equations (MICE) for datasets with <10% missingness [74]
- Feature Selection: Apply Recursive Feature Elimination (RFE) or Boruta algorithm to identify relevant predictors [74] [77]
- Data Scaling: Normalize continuous variables for neural network inputs
- Cross-Validation: Use stratified k-fold cross-validation to ensure representative performance estimation
Troubleshooting Tip: For small fertility datasets (n<1000), prefer traditional machine learning (Random Forest, XGBoost) over deep learning, as DL typically requires large datasets to avoid overfitting [79] [78].
FAQ 4: How do I determine sufficient sample size for deep learning in fertility research?
Answer: Sample size requirements depend on:
- Model Complexity: Deep learning typically requires 10-100x more samples than logistic regression [79]
- Number of Features: ML algorithms generally need 10-20 events per candidate predictor [79]
- Problem Complexity: Complex tasks like embryo image analysis require larger datasets than fertility preference prediction
Troubleshooting Tip: If collecting large datasets is infeasible, consider transfer learning using pre-trained models on related tasks, or use data augmentation techniques for image data.
Experimental Protocols and Methodologies
Protocol 1: Comparative Algorithm Evaluation for Fertility Prediction
Table 2: Essential Research Reagent Solutions for Fertility AI Experiments
| Research Reagent | Function in Experiment | Implementation Example |
|---|---|---|
| Python 3.9+ with scikit-learn | Baseline logistic regression and traditional ML implementations | LogisticRegression() with L2 regularization [74] |
| XGBoost or Random Forest | Ensemble tree methods for structured/tabular fertility data | RandomForestClassifier() with hyperparameter tuning [74] [75] |
| PyTorch/TensorFlow | Deep learning framework for neural network architectures | TabTransformer for structured clinical data [48] |
| SHAP (Shapley Additive Explanations) | Model interpretability and feature importance quantification | KernelExplainer() or TreeExplainer() for model-agnostic interpretation [75] [73] |
| Imbalanced-learn | Handling class imbalance in fertility datasets | SMOTE() for synthetic minority class oversampling [74] |
Workflow:
- Data Preprocessing: Handle missing data, encode categorical variables, address class imbalance
- Feature Selection: Apply RFE, correlation analysis, or domain knowledge for predictor selection
- Model Training: Implement multiple algorithms with appropriate hyperparameter tuning
- Performance Evaluation: Assess using AUC, accuracy, precision, recall, F1-score, and calibration metrics
- Interpretability Analysis: Apply SHAP, LIME, or feature importance analysis
- Clinical Validation: Correlate findings with established clinical knowledge
Diagram Title: Fertility AI Model Development Workflow
Protocol 2: SHAP-Based Model Interpretation Methodology
Purpose: To transform black-box model predictions into clinically interpretable insights for fertility research.
Procedure:
- Train optimal model (e.g., Random Forest, XGBoost, or Deep Learning)
- Compute SHAP values using appropriate explainer (TreeExplainer for tree-based models, KernelExplainer for others)
- Generate global feature importance plots
- Create individual prediction explanation plots
- Conduct subgroup SHAP analysis to identify context-specific predictor effects [77]
Algorithm Selection Framework
The diagram below illustrates a decision pathway for selecting between logistic regression and deep learning approaches in fertility research.
Diagram Title: Fertility AI Algorithm Selection Framework
The comparative analysis reveals that no single algorithm universally outperforms others across all fertility research contexts. Logistic regression provides exceptional interpretability and efficiency for smaller datasets with approximately linear relationships, while deep learning excels at capturing complex patterns in large, unstructured datasets. Ensemble methods like Random Forest and XGBoost frequently offer an optimal balance for structured fertility data, providing strong performance with moderate interpretability through SHAP analysis. The most effective approach involves matching algorithmic complexity to specific research questions, data characteristics, and clinical implementation requirements, while leveraging explainable AI techniques to bridge the gap between predictive accuracy and clinical utility in fertility care.
Frequently Asked Questions
Q1: Why is moving beyond the Area Under the Curve (AUC) important in fertility AI research? While AUC measures a model's diagnostic accuracy, it does not directly quantify its impact on clinical decisions or patient outcomes like live birth rates [80]. Clinical utility assessment incorporates the consequences of diagnostic decisions, helping researchers and clinicians optimize models for real-world impact rather than statistical performance alone [80].
Q2: What are the common methods for clinical utility-based cut-point selection? Several methods exist to select optimal biomarker thresholds based on clinical utility [80]:
- Youden-based Clinical Utility (YBCUT): Maximizes the sum of positive and negative clinical utilities.
- Product-based Clinical Utility (PBCUT): Maximizes the product of positive and negative clinical utilities.
- Union-based Clinical Utility (UBCUT): Minimizes the absolute difference between positive/negative utilities and AUC.
- Absolute Difference of Total Clinical Utility (ADTCUT): Minimizes the absolute difference between total clinical utility and twice the AUC.
Q3: What key features do machine learning models use to predict live birth outcomes in fresh embryo transfer? Analysis of over 11,000 ART records showed that Random Forest models (AUC >0.8) identified these as top predictive features [81]:
- Female age
- Grades of transferred embryos
- Number of usable embryos
- Endometrial thickness
Q4: How can researchers balance accuracy and speed when deploying fertility AI models? Choose model architectures based on clinical scenario [81] [82]. For rapid, clinical decision support (e.g., fresh embryo transfer), use faster models like Gradient Boosting Machines or optimized neural networks. For complex predictive tasks with longer timelines (e.g., treatment pathway optimization), prioritize accuracy with ensemble methods like Random Forests, which may have longer inference times but higher performance [81].
Q5: What are the limitations of using large language models (LLMs) for fertility data analysis? While LLMs can rapidly analyze datasets and generate reports, they struggle with medical image interpretation and require careful human validation [83]. One study found they achieved only 70% accuracy in diagnosing chromosomal abnormalities from karyotype images, highlighting the need for human expertise in clinical verification [83].
Clinical Utility Assessment Methods
Table 1: Comparison of Clinical Utility-Based Cut-Point Selection Methods
| Method | Objective | Best Use Case | Considerations |
|---|---|---|---|
| YBCUT [80] | Maximize PCUT + NCUT | Scenarios requiring balanced clinical utility | Becomes unstable with low prevalence (<10%) and low AUC |
| PBCUT [80] | Maximize PCUT × NCUT | Balanced optimization of positive/negative utilities | More stable than YBCUT at low prevalence |
| UBCUT [80] | Minimize |PCUT-AUC| + |NCUT-AUC| | When utility components should align with overall accuracy | Provides balanced utility from both test results |
| ADTCUT [80] | Minimize |Total Utility - 2×AUC| | Integrating traditional accuracy with clinical utility | Directly connects clinical utility with AUC framework |
Table 2: Performance of AI Models in Fertility Applications
| Application Area | Best-Performing Model | Performance | Sample Size |
|---|---|---|---|
| Live Birth Prediction [81] | Random Forest | AUC >0.80 | 11,728 records |
| Sperm Morphology Analysis [84] | Support Vector Machine | AUC 88.59% | 1,400 sperm |
| Sperm Motility Classification [84] | Support Vector Machine | Accuracy 89.9% | 2,817 sperm |
| NOA Sperm Retrieval Prediction [84] | Gradient Boosting Trees | AUC 0.807, Sensitivity 91% | 119 patients |
Experimental Protocols
Protocol 1: Developing Live Birth Prediction Models
Objective: Create machine learning models to predict live birth outcomes following fresh embryo transfer [81].
Methodology:
- Data Collection: Gather comprehensive ART records including patient demographics, clinical parameters, and cycle outcomes. One study analyzed 51,047 records, refining to 11,728 cases after applying inclusion criteria [81].
- Data Preprocessing: Handle missing values using nonparametric imputation methods like missForest. Perform feature selection combining statistical significance (p<0.05) and clinical relevance [81].
- Model Training: Implement multiple machine learning algorithms (Random Forest, XGBoost, GBM, AdaBoost, LightGBM, ANN) using 5-fold cross-validation for hyperparameter tuning. Use grid search with AUC as the primary optimization metric [81].
- Model Evaluation: Assess performance on held-out test data using AUC, accuracy, sensitivity, specificity, precision, recall, and F1 score. Perform subgroup and perturbation analyses to evaluate stability [81].
- Clinical Utility Assessment: Calculate positive clinical utility (PCUT = Sensitivity × PPV) and negative clinical utility (NCUT = Specificity × NPV) to evaluate real-world impact beyond traditional metrics [80].
Protocol 2: Utility-Based Cut-Point Selection for Diagnostic Biomarkers
Objective: Determine optimal biomarker thresholds based on clinical consequences rather than just accuracy [80].
Methodology:
- Distribution Modeling: Model test results using appropriate parametric distributions (binormal, bigamma, or biexponential) for diseased and non-diseased populations [80].
- Utility Calculation: For each possible cut-point, calculate sensitivity (Se) and specificity (Sp), then compute:
- Positive Predictive Value: PPV = (p × Se) / [p × Se + (1-p) × (1-Sp)]
- Negative Predictive Value: NPV = [(1-p) × Sp] / [(1-p) × Sp + p × (1-Se)]
- Positive Clinical Utility: PCUT = Se × PPV
- Negative Clinical Utility: NCUT = Sp × NPV where p represents disease prevalence [80].
- Cut-Point Selection: Apply multiple utility-based criteria (YBCUT, PBCUT, UBCUT, ADTCUT) to identify optimal thresholds [80].
- Validation: Evaluate selected cut-points across different prevalence scenarios (1%-50%) and AUC levels (0.60-0.90) to assess robustness [80].
Workflow Visualization
Clinical Utility Assessment Workflow
Utility-Based Cut-Point Selection
Research Reagent Solutions
Table 3: Essential Resources for Fertility AI Research
| Resource | Function/Application | Implementation Notes |
|---|---|---|
| Random Forest Algorithm [81] | Ensemble learning for outcome prediction | Highest performance for live birth prediction (AUC >0.80); provides feature importance rankings |
| XGBoost Algorithm [81] | Gradient boosting for tabular data | High predictive accuracy with regularization to prevent overfitting; requires careful parameter tuning |
| Clinical Utility Index [80] | Integrates diagnostic accuracy with clinical consequences | Combines sensitivity/specificity with predictive values; includes PCUT and NCUT calculations |
| 5-Fold Cross Validation [81] | Model validation and hyperparameter tuning | Divides data into 5 subsets; uses 4 for training, 1 for testing; repeats process rotating subsets |
| missForest Imputation [81] | Handles missing data in clinical datasets | Nonparametric method suitable for mixed data types; maintains data structure without distributional assumptions |
| Grid Search Optimization [81] | Systematic hyperparameter tuning | Tests all parameter combinations; uses cross-validation performance to select optimal settings |
| Partial Dependence Plots [81] | Model interpretation and visualization | Shows marginal effect of features on predictions; helps explain model decisions to clinicians |
Troubleshooting Guides
Guide 1: Addressing Performance Drop in External Validation
Problem: Your model, developed on a single-center dataset, shows a significant performance drop when tested on data from other fertility centers.
Explanation: This is a classic sign of overfitting and poor generalizability. Models often learn patterns specific to a single center's patient population, clinical protocols, and equipment.
Solution:
- Implement Center-Specific Retraining: Develop machine learning center-specific (MLCS) models that are trained and validated on local data. Research shows MLCS models significantly outperform center-agnostic national models like the SART model [85] [86].
- Use Internal-External Validation: Employ a validation procedure that rotates through different clinics in the training and testing phases. This method, used successfully in a study of 11 European IVF centers, helps ensure models generalize across diverse settings [87].
- Monitor for Data Drift: Continuously validate models on out-of-time test sets comprising patients from contemporaneous time periods to detect concept drift or data drift [85].
Guide 2: Managing Limited Data from Multiple Centers
Problem: You need to validate your model across multiple centers, but some have limited datasets.
Explanation: Small sample sizes can lead to underpowered models and unreliable performance estimates.
Solution:
- Apply Cross-Validation Rigorously: For centers with smaller datasets (e.g., 101-200 cycles), use internal validation with cross-validation. This maximizes the use of available data for both training and performance estimation [85].
- Consider Federated Learning: Emerging techniques allow clinics to collaborate on model development without sharing sensitive patient data, helping to build more robust models from diverse but distributed datasets [12].
- Evaluate Model Updates: As more data becomes available, update models. Studies show that updated MLCS models (MLCS2) trained on larger, more recent datasets show improved predictive power compared to their initial versions (MLCS1) [85].
Frequently Asked Questions (FAQs)
Q1: Why is external validation on multi-center datasets critical for fertility AI models?
A1: External validation is essential because fertility patient populations and clinical practices vary significantly across centers. A model demonstrating high accuracy at one center may fail elsewhere due to these variations. One study found that patient clinical characteristics varied significantly across fertility centers and these variations were associated with differential IVF live birth outcomes [85]. Proper external validation ensures that models are robust and clinically applicable beyond their development setting.
Q2: What are the key metrics for evaluating generalizability in fertility AI models?
A2: Beyond traditional metrics like AUC-ROC, researchers should prioritize:
- Precision-Recall AUC (PR-AUC): Especially important for overall minimization of false positives and negatives [85]
- F1 Score: Particularly at clinically relevant probability thresholds (e.g., 50% live birth prediction) [85]
- PLORA (Posterior Log of Odds Ratio): Measures how much more likely a model is to give a correct prediction compared to a baseline Age model [85]
- Calibration: How well predicted probabilities match observed outcomes across different centers [86]
Q3: How can we balance the need for generalizability with model performance?
A3: The research suggests that center-specific models (MLCS) actually achieve better performance metrics than generalized national models while maintaining relevance to local populations. One multi-center study found that MLCS models significantly improved minimization of false positives and negatives compared to the SART model [85]. This suggests that creating models tailored to center-specific populations, rather than forcing a one-size-fits-all approach, may offer the best balance.
Quantitative Data on Model Performance in Multi-Center Settings
Table 1: Performance Comparison of ML Center-Specific vs. National Models Across Multiple Centers
| Model Type | Number of Centers | Total Cycles | Key Performance Metrics | Advantages |
|---|---|---|---|---|
| ML Center-Specific (MLCS) | 6 US centers | 4,635 first-IVF cycles | Significantly improved PR-AUC and F1 score (p<0.05) vs. SART; 23% more patients appropriately assigned to LBP ≥50% [85] | Better reflects local patient characteristics; improved clinical utility for counseling |
| SART National Model | 121,561 cycles (development) | Same 4,635 cycles (testing) | Lower performance on minimization of false positives/negatives; appropriate for 23% fewer patients at LBP ≥50% threshold [85] | Broad dataset but may not capture center-specific variations |
| Explainable AI for Follicle Sizes | 11 European centers | 19,082 treatment-naive patients | Identified optimal follicle sizes (12-20mm) contributing to mature oocytes; MAE of 3.60 for MII oocyte prediction in ICSI cycles [87] | Large, diverse dataset; explainable insights for clinical decision-making |
Table 2: Live Model Validation Results Across Six Fertility Centers
| Center | Time Period for LMV | Number of Cycles for LMV | LMV Result | Implication |
|---|---|---|---|---|
| 916 | 2017-2020 (4 years) | 501-1000 cycles | No significant difference in ROC-AUC and PLORA | Model remained applicable over time [85] |
| 552 | 2016-2020 (4.5 years) | 101-200 cycles | No significant difference in ROC-AUC and PLORA | Model stable despite population changes [85] |
| 869 | 2019-2020 (2 years) | 201-300 cycles | No significant difference in ROC-AUC and PLORA | Consistent performance in contemporary patients [85] |
Experimental Protocols for External Validation
Protocol 1: Internal-External Validation for Multi-Center Studies
This protocol was successfully implemented in a study of 19,082 patients across 11 clinics [87]:
Data Collection: Collect de-identified patient data from multiple centers, including:
- Follicle sizes on day of trigger
- Number of mature oocytes retrieved
- Patient age and treatment protocol
- Laboratory outcomes (zygotes, blastocysts)
Model Training: For each clinic in rotation:
- Train the model on data from all other clinics
- Test the model on the held-out clinic
- Use histogram-based gradient boosting regression trees
Performance Assessment: Calculate mean performance metrics (MAE, R²) across all folds
- Report standard deviations to show variability
- Use permutation importance to identify most contributory features
Explainability Analysis: Implement SHAP analysis to verify feature importance patterns are consistent across clinics
Protocol 2: Live Model Validation for Ongoing Monitoring
This approach validates model applicability to contemporary patient populations [85]:
Initial Model Development:
- Train initial model (MLCS1) on historical data (e.g., 2014-2016)
- Validate using internal cross-validation
Out-of-Time Testing:
- Apply the trained model to more recent patients (e.g., 2017-2020)
- Ensure no significant differences in ROC-AUC and PLORA metrics
Model Updating:
- Develop updated model (MLCS2) with expanded dataset
- Compare performance metrics between MLCS1 and MLCS2
- Confirm improved predictive power with larger datasets
Workflow Visualization
External Validation Workflow for Fertility AI Models
Multi-Modal Data Integration for Robust Models
Research Reagent Solutions
Table 3: Essential Resources for Fertility AI Research and Validation
| Resource Category | Specific Tool/Solution | Function in Research | Example Use Case |
|---|---|---|---|
| Machine Learning Frameworks | Scikit-learn (Python) | Model development, normalization, cross-validation | Implementing linear SVM for IUI outcome prediction [69] |
| Validation Methodologies | Internal-External Validation | Rotating training/testing across multiple centers | Validating follicle size models across 11 clinics [87] |
| Explainability Tools | SHAP (SHapley Additive exPlanations) | Interpreting model predictions and feature importance | Identifying most contributory follicle sizes [87] |
| Performance Metrics | PLORA (Posterior Log of Odds Ratio) | Comparing model predictive power against baseline | Evaluating improvement over age-based models [85] |
| Data Processing | PowerTransformer | Normalizing skewed data distributions | Preprocessing clinical data for IUI outcome prediction [69] |
Conclusion
The successful integration of AI into reproductive medicine hinges on a deliberate and nuanced balance between analytical accuracy and computational speed. Foundational exploration reveals that model choice is context-dependent, where complex deep learning may suit image analysis, while more interpretable, faster models like LightGBM or optimized SVMs are superior for specific predictive tasks. Methodologically, hybrid approaches that combine different AI paradigms show great promise in enhancing both performance and efficiency. Troubleshooting efforts must prioritize interpretability and data quality to build clinical trust and ensure robust performance. Finally, rigorous, comparative validation against clinical standards is non-negotiable for translation into practice. Future directions must focus on developing standardized benchmarking frameworks, fostering collaborative open-source platforms for model development, and advancing federated learning techniques to leverage large, diverse datasets while preserving patient privacy. For researchers and drug developers, this balance is not merely a technical challenge but the key to creating clinically viable, scalable, and ethically sound AI tools that can truly revolutionize fertility care.
References
- 1. ML Model Optimization in 2025 [https://signiance.com/ml-model-optimization-in-2025/]
- 2. AI Optimization in 2025: Smarter Techniques and Tools [https://www.rolustech.com/blog/ai-optimization-2025]
- 3. Predicting pregnancy outcomes in IVF cycles: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476623/]
- 4. Artificial intelligence in assisted reproductive technology [https://www.sciencedirect.com/science/article/pii/S1472648325000628]
- 5. Benchmarking workflows to assess performance and ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-020-03934-3]
- 6. Diagnostic accuracy of E-FAST examination performed by ... [https://pubmed.ncbi.nlm.nih.gov/41204204/]
- 7. Clinical performance of real-time nanopore metagenomic ... [https://www.nature.com/articles/s41598-025-87858-z]
- 8. Global Trends in the Use of Artificial Intelligence (AI) in ... [https://jivfww.scholasticahq.com/article/140673-global-trends-in-the-use-of-artificial-intelligence-ai-in-reproductive-medicine-insights-from-surveys-of-international-fertility-specialists]
- 9. Review Artificial intelligence in in-vitro fertilization (IVF) [https://www.sciencedirect.com/science/article/pii/S246878472400182X]
- 10. Research - MIM Fertility - Expert-level AI for exceptional IVF ... [https://mimfertility.ai/research/]
- 11. AI Model Trained on 53000 IVF Cycles Outperforms ... [https://www.fertilitybridge.com/news-articles/ivf-ai-improves-stim-cycle-predictions]
- 12. Current progress and open challenges for applying ... [https://www.sciencedirect.com/science/article/pii/S2666389925001953]
- 13. FERTILITY CARE IN LOW- AND MIDDLE- INCOME ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12359024/]
- 14. AI-Powered IVF: Revolutionizing Fertility Treatments in 2025 [https://hegdefertility.com/blog/ai-in-ivf-how-artificial-intelligence-is-transforming-fertility-treatments-in-2025/]
- 15. Deep Learning Specialization [https://medium.com/data-science-collective/deep-learning-specialization-fundamentals-architectures-and-applications-5ce568b769e4]
- 16. A Novel Machine Learning Model for Predicting Natural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12361258/]
- 17. Top 9 Machine Learning Challenges in 2025 [https://www.netguru.com/blog/machine-learning-problems]
- 18. Deep Learning Demystified — Part 4: Common Challenges ... [https://medium.com/@indukishen/deep-learning-demystified-part-4-common-challenges-and-how-to-overcome-them-f365536f0093]
- 19. 8 Deep Learning Architectures Data Scientists Must Master [https://www.projectpro.io/article/deep-learning-architectures/996]
- 20. AI Model Optimization Techniques for Enhanced ... [https://www.netguru.com/blog/ai-model-optimization]
- 21. Optimize AI Models Like a Pro: 10 Techniques for Better ... [https://www.artiba.org/blog/optimize-ai-models-like-a-pro-10-techniques-for-better-results]
- 22. FERTILITY MEETS THE FUTURE AI IN THE REVOLUTION ... [https://www.endocrinology.org/endocrinologist/157-autumn-25/features/fertility-meets-the-future-ai-in-the-revolution-of-reproductive-care/]
- 23. Stability and reliability of artificial intelligence models in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494150/]
- 24. Considerations for the Use of Artificial Intelligence [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/considerations-use-artificial-intelligence-support-regulatory-decision-making-drug-and-biological]
- 25. FDA Reveals AI Development Cheat Sheet via Draft ... [https://www.mwe.com/insights/fda-reveals-ai-development-cheat-sheet-in-highly-anticipated-draft-guidances/]
- 26. Data-Driven Insights into Fertility Trends: An Explainable AI ... [https://nhsjs.com/2025/data-driven-insights-into-fertility-trends-an-explainable-ai-approach-to-forecasting-and-policy-implications/]
- 27. IP implications of the FDA guidance for use of AI in drug ... [https://ipkitten.blogspot.com/2025/06/ip-implications-of-fda-guidance-for-use.html]
- 28. Evaluating transparency in AI/ML model characteristics for ... [https://www.nature.com/articles/s41746-025-02052-9]
- 29. Development and validation of machine learning models ... [https://www.nature.com/articles/s41598-025-06998-4]
- 30. Real-world use of an artificial intelligence–powered clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223591/]
- 31. AI and EMR integration in IVF : 6 things you need to know [https://mimfertility.ai/ai-and-emr-intergartion-in-ivf-6-things-you-need-to-know/]
- 32. 6 Questions To Ask Before Integrating AI Into A Clinical ... [https://medcitynews.com/2025/06/6-questions-to-ask-before-integrating-ai-into-a-clinical-workflow/]
- 33. A deep learning model for predicting blastocyst formation ... [https://www.nature.com/articles/s41598-024-79175-8]
- 34. Artificial Intelligence in Assisted Reproductive Technology [https://pmc.ncbi.nlm.nih.gov/articles/PMC11966177/]
- 35. The prospect of artificial intelligence to personalize ... [https://www.nature.com/articles/s41746-024-01006-x]
- 36. LightGBM FAQ — LightGBM 4.6.0.99 documentation [https://lightgbm.readthedocs.io/en/latest/FAQ.html]
- 37. Development and validation of machine learning models ... [https://pubmed.ncbi.nlm.nih.gov/40596532/]
- 38. Development and validation of machine learning models ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217550/]
- 39. Using feature optimization and LightGBM algorithm to ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1305473/full]
- 40. NeuFACO: Neural Focused Ant Colony Optimization ... [https://arxiv.org/html/2509.16938v2]
- 41. A Hybrid Biologically-Inspired Optimization Algorithm for ... [https://link.springer.com/article/10.1007/s10922-025-09899-z]
- 42. A new hybrid neural network framework inspired by ... [https://www.nature.com/articles/s41598-025-21842-5]
- 43. Hybrid bio-inspired optimization based routing protocol for ... [https://www.sciencedirect.com/science/article/pii/S2590005625001080]
- 44. Embryo selection through artificial intelligence versus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10426717/]
- 45. Deep-learning model for embryo selection using time- ... [https://www.nature.com/articles/s41598-025-10531-y]
- 46. SugarcaneShuffleNet: A Very Fast, Lightweight ... [https://arxiv.org/html/2508.17107v1]
- 47. Revolutionizing Sperm Analysis with AI: A Review of ... [https://www.mdpi.com/2079-3197/13/6/132]
- 48. An integrated optimization and deep learning pipeline for ... [https://www.sciencedirect.com/science/article/pii/S0169260725003967]
- 49. Enhancing the precision of male fertility diagnostics ... [https://www.nature.com/articles/s41598-025-25052-x]
- 50. Machine learning vs. classic statistics for the prediction of IVF outcomes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7550518/]
- 51. Frontiers | Catalyzing IVF outcome prediction: exploring advanced machine learning paradigms for enhanced success rate prognostication [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2024.1392611/full]
- 52. TFC IVF Research Presented at ESHRE in Paris [https://txfertility.com/blog/tfc-ivf-research-presented-at-eshre-in-paris/]
- 53. Comparing SVM and logistic regression - Cross Validated [https://stats.stackexchange.com/questions/95340/comparing-svm-and-logistic-regression]
- 54. Artificial Intelligence in Reproductive Medicine: Transforming ... [https://jivfww.scholasticahq.com/article/137620-artificial-intelligence-in-reproductive-medicine-transforming-assisted-reproductive-technologies]
- 55. A brief history of artificial intelligence embryo selection [https://pmc.ncbi.nlm.nih.gov/articles/PMC11016335/]
- 56. Interpretable, not black-box, artificial intelligence should be ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8687137/]
- 57. Resampling methods for class imbalance in clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582444/]
- 58. Handling imbalanced medical datasets: review of a decade ... [https://link.springer.com/article/10.1007/s10462-024-10884-2]
- 59. Processing imbalanced medical data at the data level with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11373105/]
- 60. Modeling Rare Event Probability: An Advanced Machine ... [https://medium.com/@rahulg.isme2325/modeling-rare-event-probability-an-advanced-machine-learning-perspective-2280d5b364c7]
- 61. Synthetic minority oversampling using deep learning [https://www.sciencedirect.com/science/article/pii/S0010482525001805]
- 62. Class Imbalance Strategies — A Visual Guide with Code [https://medium.com/data-science/class-imbalance-strategies-a-visual-guide-with-code-8bc8fae71e1a]
- 63. The Promise - And Perils - of AI in Fertility [https://www.fertilitybridge.com/news-articles/ai-hallucination-fertility-data-problem]
- 64. 10 Essential Machine Learning Trade-offs: Balancing Act ... [https://medium.com/@mustaphaliaichi/10-essential-machine-learning-trade-offs-balancing-act-for-ai-success-d381d595348a]
- 65. Data Preprocessing in Machine Learning: Steps & Best ... [https://lakefs.io/blog/data-preprocessing-in-machine-learning/]
- 66. The Importance of Feature Engineering in Machine Learning [https://businessanalyticsinstitute.com/the-importance-of-feature-engineering-in-machine-learning/]
- 67. The Curse of Dimensionality | Feature Engineering [https://medium.com/@paghadalsneh/the-curse-of-dimensionality-feature-engineerin-c6d0609aa788]
- 68. Minimization of high computational cost in data ... [https://www.sciencedirect.com/science/article/pii/S2666827023000361]
- 69. An Artificial Intelligence-Based Model to Predict Pregnancy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300755/]
- 70. Clinical impact and quality of randomized controlled trials involving... [https://www.nature.com/articles/s41746-021-00524-2?error=cookies_not_supported&code=94318863-462b-4990-980e-6e7b684b15d1]
- 71. Strengths and Limitations of RCTs - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK584466/]
- 72. Development and validation pathways of artificial intelligence tools... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8718483/]
- 73. Comparing Logistic Regression and Ensemble Decision ... [https://www.sciencedirect.com/science/article/pii/S2949912725001175]
- 74. Exploring machine learning algorithms for predicting fertility ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11781225/]
- 75. Application of machine learning algorithms and SHAP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277441/]
- 76. Application of machine learning algorithms and SHAP ... [https://www.nature.com/articles/s41598-025-04704-y]
- 77. Application of machine learning to predict delayed ... [https://www.sciencedirect.com/org/science/article/pii/S2633838625000442]
- 78. Deep Learning vs Machine Learning: Key Differences [https://labelyourdata.com/articles/deep-learning-vs-machine-learning]
- 79. Beyond Comparing Machine Learning and Logistic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631085/]
- 80. an analysis based on population-level parametric distributions ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02656-5]
- 81. Predictive models for live birth outcomes following fresh ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462326/]
- 82. Using AI Right Now: A Quick Guide - by Ethan Mollick [https://www.oneusefulthing.org/p/using-ai-right-now-a-quick-guide]
- 83. Application of Large Language Models in Data Analysis and ... [https://formative.jmir.org/2025/1/e70107]
- 84. Artificial intelligence (AI) approaches to male infertility in IVF [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02479-6]
- 85. Machine learning center-specific models show improved ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12006386/]
- 86. Machine learning center-specific models show improved ... [https://www.nature.com/articles/s41467-025-58744-z]
- 87. Explainable artificial intelligence to identify follicles that ... [https://www.nature.com/articles/s41467-024-55301-y]