Comparative Effectiveness of Ovarian Cancer Biomarkers: A Strategic Guide for Research and Development
This article provides a comprehensive analysis of the comparative effectiveness of ovarian cancer biomarkers for an audience of researchers, scientists, and drug development professionals.
Comparative Effectiveness of Ovarian Cancer Biomarkers: A Strategic Guide for Research and Development
Abstract
This article provides a comprehensive analysis of the comparative effectiveness of ovarian cancer biomarkers for an audience of researchers, scientists, and drug development professionals. It explores the foundational landscape of diagnostic, prognostic, and predictive biomarkers, from established clinical tools like CA125 and HE4 to emerging targets such as CHI3L1 and metabolomic signatures. The content delves into advanced methodological applications, including artificial intelligence and multi-omics integration, for novel biomarker discovery. It further addresses critical challenges in biomarker validation and optimization, including assay standardization and overcoming tumor heterogeneity. Finally, the article presents a rigorous comparative framework for evaluating biomarker performance, synthesizing evidence levels from recent clinical trials and network meta-analyses to guide future research and clinical translation.
The Evolving Landscape of Ovarian Cancer Biomarkers: From Established Tools to Emerging Targets
Ovarian cancer remains the most lethal gynecologic malignancy, primarily due to the fact that an estimated 60-75% of cases are diagnosed at advanced stages, when five-year survival plummets to less than 30%, compared to over 90% for localized disease [1] [2] [3]. This stark diagnostic challenge has intensified the search for reliable biomarkers that can enable earlier detection, guide personalized treatment, and ultimately improve patient outcomes. This guide provides a comparative analysis of the current and emerging biomarker landscape in ovarian cancer, evaluating their performance characteristics, underlying technologies, and clinical applications to inform research and development strategies.
Comparative Performance of Established and Emerging Biomarkers
The diagnostic and prognostic utility of ovarian cancer biomarkers varies significantly based on histological subtype, disease stage, and lead time before clinical diagnosis. The table below summarizes the performance characteristics of key biomarkers.
Table 1: Comparative Performance of Ovarian Cancer Biomarkers
| Biomarker | Type | Primary Role/Function | Reported Sensitivity/Specificity/Other Performance Metrics | Notable Subtype Limitations |
|---|---|---|---|---|
| CA125 | Protein (Blood serum) | Diagnostic, Monitoring [3] | C-statistic=0.92 (≤6 mos pre-dx); Declines with longer lead time [1] | Lower sensitivity in mucinous tumors (~69%) [4] |
| HE4 | Protein (Blood serum) | Diagnostic, Prognostic [3] | C-statistic=0.84 (≤6 mos pre-dx) [1]; Combined with CA125: 72% sensitivity for Stage I [2] | - |
| CA72.4 | Protein (Blood serum) | Diagnostic | C-statistic=0.77 (≤6 mos pre-dx) [1] | - |
| CA15.3 | Protein (Blood serum) | Diagnostic | C-statistic=0.73 (≤6 mos pre-dx) [1] | - |
| CHI3L1 (YKL-40) | Protein (Blood serum) | Diagnostic, Prognostic [3] | 80% Sensitivity, 70% Specificity; Multi-marker model (with CA125, HE4): 85.7% sensitivity at 95.4% specificity [3] | - |
| BRCA1/2 | Genetic (Germline/Tumor) | Predictive, Prognostic [5] | PARP inhibitors: 70% reduction in risk of progression/death in advanced BRCA-mutated OC [3] | Not prevalent in low-grade serous or mucinous subtypes [4] [6] |
| KRAS Mutation | Genetic (Tumor) | Predictive, Prognostic | In LGSOC: 44% ORR with avutometinib+defactinib [2] | Most common in mucinous ovarian carcinoma (43.6-64.9%) [4] |
Detailed Experimental Protocols for Biomarker Evaluation
Understanding the methodologies behind key biomarker studies is crucial for evaluating their validity and applicability.
Protocol: Prospective Phase III Biomarker Performance Study (EPIC Cohort)
This landmark study evaluated the early detection capacity of a biomarker panel in prospectively collected samples [1].
- Objective: To evaluate the performance of CA125, HE4, CA72.4, and CA15.3 for discriminating between future ovarian cancer cases and matched controls, stratified by time-to-diagnosis.
- Study Design: Nested case-control study within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort [1].
- Participants: 810 incident invasive epithelial ovarian cancer cases and 1,939 matched controls [1].
- Sample Collection: Baseline blood samples collected prospectively (before diagnosis) and stored under liquid nitrogen or at -80°C [1].
- Biomarker Measurement: Serum levels of CA125, HE4, CA72.4, and CA15.3 were measured using standardized immunoassays [1].
- Data Analysis:
- Calculated sensitivity at fixed specificities (95%, 98%).
- Determined Area Under the Receiver Operator Curve (C-statistic) for individual markers and combinations.
- Stratified analysis by stage at diagnosis and time between blood draw and diagnosis [1].
Protocol: Machine Learning-Enhanced Multi-Marker Detection
Recent approaches leverage computational power to improve detection algorithms and integrate novel biomarker types.
- Objective: To develop and validate a machine learning model for early-stage ovarian cancer detection using combined biomarker data.
- Data Input: Proteomic (CA125, HE4) and/or lipidomic profiling data from patient blood samples [2].
- Algorithm Training: Use of machine learning models (e.g., Random Forest, XGBoost, sPLS) to identify complex patterns distinguishing early-stage cancer from benign conditions or healthy controls [7] [2].
- Validation: Model performance is tested on independent, held-out datasets to ensure robustness and avoid overfitting [7].
- Output: A predictive model or algorithm that can classify samples with high accuracy (e.g., 88% for lipidomics/proteomics model distinguishing early-stage OC from other conditions) [2].
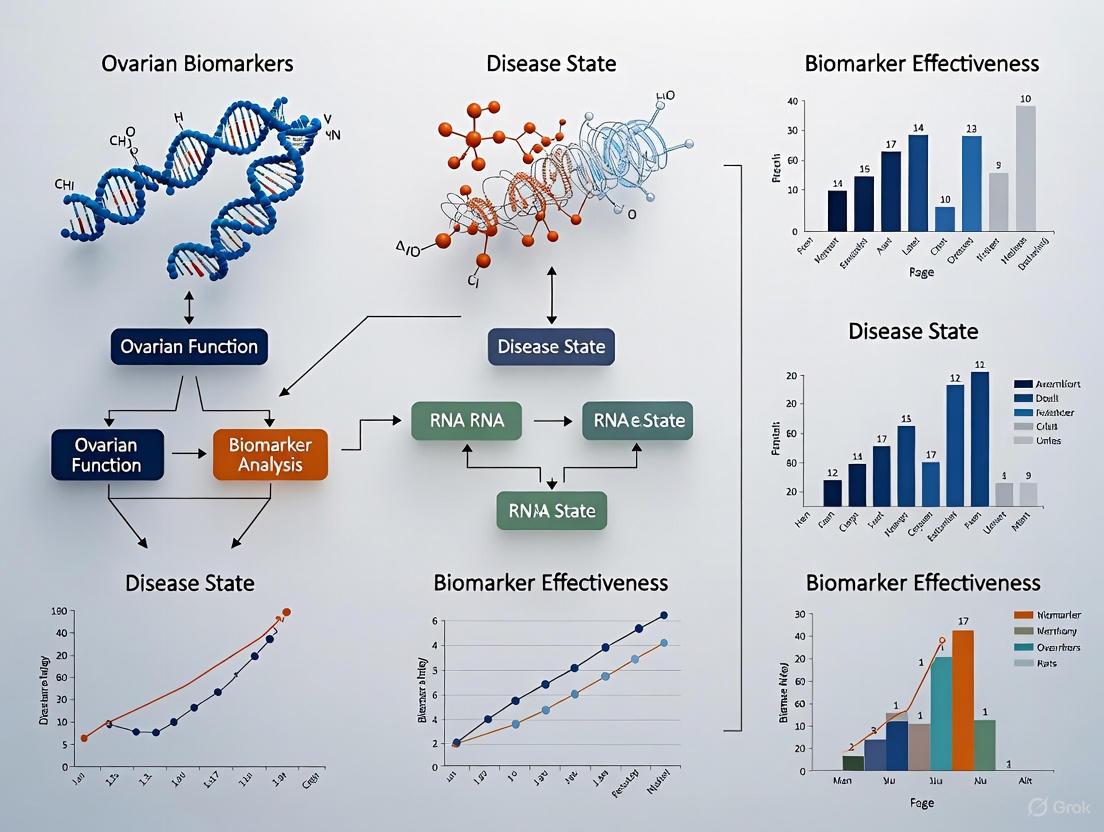
Visualizing Key Biomarker Applications and Pathways
The following diagrams illustrate the functional role of a promising biomarker and a generalized workflow for biomarker evaluation.
CHI3L1 Role in Ovarian Cancer Progression
Biomarker Evaluation Workflow
Essential Research Reagent Solutions
The following table details key reagents and tools required for conducting ovarian cancer biomarker research.
Table 2: Essential Research Reagents for Ovarian Cancer Biomarker Studies
| Reagent / Tool | Function in Research | Specific Examples / Targets |
|---|---|---|
| Validated Immunoassays | Quantifying protein biomarker levels in serum/plasma [1] | ELISA kits for CA125, HE4, CA15.3, CA72.4, CHI3L1/YKL-40 [1] [3] |
| ctDNA Isolation & Analysis Kits | Isolating and analyzing circulating tumor DNA for mutation detection and minimal residual disease monitoring [5] [6] | Kits for extracting cell-free DNA; PCR/NGS panels for BRCA, KRAS, TP53 mutations [2] [6] |
| Spatial Transcriptomics/ Proteomics Platforms | Characterizing gene expression and protein distribution within intact tumor tissue, preserving spatial context [2] | Multiplexed immunofluorescence (e.g., Phenocycler); RNAscope; digital spatial profiling [2] |
| Machine Learning Software & Biomarker Analysis Tools | Identifying complex biomarker signatures and building predictive models from high-dimensional omics data [7] | R/Python packages (glmnet, XGBoost, randomForest); integrated platforms like Omics Playground [7] |
| Cell Line Panels | Modeling different ovarian cancer subtypes for functional validation of biomarkers and drug testing [4] | panels of high-grade serous, mucinous, low-grade serous, and clear cell ovarian cancer cell lines |
The comparative analysis underscores that while CA125 remains a cornerstone, its limitations are being effectively addressed by multi-marker strategies incorporating HE4 and novel proteins like CHI3L1. The future of ovarian cancer management lies in the integration of traditional protein biomarkers with genetic alterations (e.g., BRCA, KRAS) and advanced analytical techniques like ctDNA analysis and machine learning. This multi-faceted approach promises to shift the paradigm from late-stage intervention to early detection and highly personalized, biomarker-driven therapy, ultimately challenging the high mortality rate associated with this disease.
Ovarian cancer remains the most lethal gynecologic malignancy, largely because a majority of cases are diagnosed at an advanced stage. The establishment of accurate diagnostic biomarkers is therefore critical for improving patient outcomes through timely intervention. For decades, Cancer Antigen 125 (CA125) has been the cornerstone serum biomarker in ovarian cancer management. However, its limitations in sensitivity and specificity have driven the development of additional biomarkers, most notably Human Epididymis Protein 4 (HE4). The combination of these markers within the Risk of Ovarian Malignancy Algorithm (ROMA) represents a significant advancement in the preoperative assessment of adnexal masses. This guide provides a comparative analysis of these established biomarkers, detailing their diagnostic performance, underlying biology, and practical application in clinical research and practice.
Biomarker Characteristics and Biological Basis
Carbohydrate Antigen 125 (CA125)
CA125, also known as Cancer Antigen 125, is a mucin-type glycoprotein produced by the MUC16 gene and associated with the cellular membrane [8]. It was first isolated in the early 1980s by Bast et al. from ovarian cancer tissue [8]. While it is the most extensively used biomarker for ovarian lesions, its serum concentration lacks adequate specificity or sensitivity for effective population screening [2]. Levels can be elevated in various physiological conditions (menstruation, pregnancy) and benign pathologies (endometriosis, inflammatory diseases of the peritoneum), leading to a high rate of false positives [8]. Its sensitivity is particularly low in early-stage ovarian cancer, with only 23-50% of stage I cases showing elevated levels [8].
Human Epididymis Protein 4 (HE4)
HE4 is a glycoprotein belonging to the whey acidic four-disulfide core (WFDC) protein family, accounting for its alternative name, WFDC2 [8]. It was initially isolated from the epididymis and is believed to play a role in sperm maturation [8]. While weakly expressed in the normal epithelium of respiratory and reproductive organs, HE4 is overexpressed in ovarian tumors, particularly in endometrioid ovarian cancer [8]. A key advantage of HE4 over CA125 is that its serum levels are not elevated in patients with endometriotic cysts, making it a more specific biomarker in this clinical context [8].
The ROMA Algorithm
The Risk of Ovarian Malignancy Algorithm (ROMA) is a predictive index that combines the serum values of HE4, CA125, and the patient's menopausal status to generate a numerical score indicating a high or low likelihood of malignancy [9] [10]. The algorithm uses specific formulas based on menopausal status [9] [10]:
- Premenopausal: Predictive Index (PI) = -12.0 + (2.38 × LN(HE4)) + (0.0626 × LN(CA125))
- Postmenopausal: PI = -8.09 + (1.04 × LN(HE4)) + (0.732 × LN(CA125)) The Predicted Probability (PP) is then calculated as: PP = 100 × exp(PI) / (1 + exp(PI)) [10]. This probability is used to classify patients into risk groups, guiding referrals to specialized care.
Table 1: Established Cut-off Values for ROMA
| Menopausal Status | Recommended ROMA Cut-off | Risk Classification |
|---|---|---|
| Premenopausal | 11.4% - 12.5% [9] [10] | PP ≥ cut-off: High risk of ovarian cancer |
| Postmenopausal | 14.4% - 29.9% [9] [10] | PP < cut-off: Low risk of ovarian cancer |
Comparative Diagnostic Performance
Extensive research has compared the diagnostic accuracy of CA125, HE4, and ROMA in differentiating benign from malignant ovarian masses. The following table synthesizes key performance metrics from recent studies.
Table 2: Comparative Diagnostic Performance of Individual Biomarkers and ROMA
| Biomarker / Algorithm | Sensitivity (%) | Specificity (%) | Area Under Curve (AUC) | Study Details |
|---|---|---|---|---|
| CA125 | 69.4 [9] - 79.6 [11] | 82.5 [9] - 82.5 [11] | 0.679 [9] - 0.883 [11] | Varies by population and cut-off |
| HE4 | 77.5 [9] - 81.7 [11] | 96.8 [9] - 85.1 [11] | 0.845 [9] - 0.899 [11] | Higher specificity than CA125 |
| ROMA | 64.8 [12] - 87.3 [11] | 86.3 [12] - 85.5 [11] | 0.898 [10] - 0.921 [11] | Combines HE4, CA125, menopausal status |
A 2025 prospective study from Thailand directly compared ROMA with the Assessment of Different NEoplasias in the adneXa (ADNEX) model. Using a 10% malignancy risk cutoff for ADNEX, the study found that ADNEX demonstrated superior sensitivity (91.9%) compared to ROMA (64.8%), while ROMA showed higher specificity (86.3%) than ADNEX (65.7%) [12]. This highlights a common trade-off in diagnostic tests, where sensitivity and specificity are often inversely related.
The performance of ROMA is particularly notable in early-stage disease. A meta-analysis of five studies found that ROMA had numerically superior diagnostic performance compared to CA125 or HE4 alone, especially in early-stage ovarian cancer and postmenopausal patients [11]. The log diagnostic odds ratio (DOR) for ROMA was better than for HE4 and CA125, particularly in the early-stage patient group [11].
Table 3: Performance in Early-Stage Ovarian Cancer (Meta-Analysis Data [11])
| Biomarker / Algorithm | Sensitivity (%) | Specificity (%) | Area Under Curve (AUC) |
|---|---|---|---|
| CA125 | 79.6 | 82.5 | 0.883 |
| HE4 | 81.7 | 85.1 | 0.899 |
| ROMA | 87.3 | 85.5 | 0.921 |
Experimental Protocols and Methodologies
For researchers aiming to validate or utilize these biomarkers, understanding standardized experimental protocols is essential.
Serum Sample Collection and Processing
The integrity of biomarker results depends on rigorous pre-analytical sample handling. Key steps derived from cited studies include [9] [10]:
- Phlebotomy: Blood samples should be collected preoperatively from fasting patients and before the commencement of any medications.
- Collection: Use 10 mL venous blood samples collected in clot-activating tubes.
- Centrifugation: Centrifuge tubes at 2,500 rpm for 10 minutes to separate serum.
- Aliquoting and Storage: Withdraw the serum, dispense into multiple cryotubes, and freeze at -20°C or -80°C. The targeted time between sampling and freezing should be within 4 hours.
Immunoassay Protocols for Biomarker Measurement
The quantitative measurement of CA125 and HE4 relies on immunoassay techniques.
- CA125 Analysis: Can be performed using the Abbott Axsym system based on Microparticle Enzyme Immunoassay (MEIA) technology [9]. Alternatively, the CanAg CA125 EIA assay (Fujirebio Diagnostics) is a solid-phase, non-competitive immunoassay based on the direct sandwich technique [10].
- HE4 Analysis: Can be conducted using the fully automated ARCHITECT instrument (Abbott Diagnostics) based on Electro-Chemiluminescent Immunoassay (ECLIA) [9]. The HE4 EIA assay (Fujirebio Diagnostics) is also a validated manual method run in duplicate [10].
Standard cut-off values are often set at 35 U/mL for CA125 and 70 pM/L for HE4, though these can vary, and determining population-specific optimal cut-offs using Receiver Operating Characteristic (ROC) analysis is recommended [9] [10].
ROMA Calculation and Interpretation
After obtaining the serum concentrations of HE4 and CA125:
- Determine the patient's menopausal status.
- Apply the corresponding formula (premenopausal or postmenopausal) to calculate the Predictive Index (PI) [9] [10].
- Convert the PI to a Predicted Probability (PP) of malignancy using the formula: PP = 100 × exp(PI) / (1 + exp(PI)) [10].
- Classify the patient into a high-risk or low-risk category using established cut-offs (e.g., 11.4% for premenopausal and 29.9% for postmenopausal women, though values can vary) [9] [10].
Biomarker Pathways and Clinical Workflow
The following diagram illustrates the clinical and analytical workflow from patient presentation to risk stratification using the ROMA algorithm.
Diagram 1: Clinical Workflow for ROMA-based Risk Stratification. This diagram outlines the sequential steps from patient presentation to final risk classification, integrating clinical data (menopausal status) with laboratory biomarker measurements.
The Scientist's Toolkit: Essential Research Reagents and Materials
For laboratories conducting research on these biomarkers, the following table details key reagents and materials used in the featured studies.
Table 4: Essential Research Reagents and Materials for Biomarker Analysis
| Item | Function / Description | Example Specifications / Kits |
|---|---|---|
| Clot-Activating Blood Collection Tubes | For serum sample collection and separation. | BD Vacutainer Serum Tube [10] |
| CA125 Immunoassay Kit | For quantitative measurement of serum CA125 levels. | CanAg CA125 EIA (Fujirebio Diagnostics) [10] or Abbott Axsym CA125 assay [9] |
| HE4 Immunoassay Kit | For quantitative measurement of serum HE4 levels. | HE4 EIA (Fujirebio Diagnostics) [10] or ARCHITECT HE4 assay (Abbott) [9] |
| Centrifuge | For separating serum from whole blood. | Capable of 2,500 rpm / 800 g [9] [10] |
| Freezer (-20°C to -80°C) | For long-term storage of serum aliquots to preserve biomarker integrity. | [9] [10] |
| ROMI Components | For novel index comparison; includes Thymidine Kinase 1 (TK1) assay. | Used in research for the Risk of Ovarian Malignancy Index (ROMI) [13] |
| 2H-Pyran-2,5-diol | 2H-Pyran-2,5-diol|CAS 113895-83-3|RUO | |
| 4-Ethyl-6-methylpyrimidine | 4-Ethyl-6-methylpyrimidine|CAS 74647-33-9 | High-purity 4-Ethyl-6-methylpyrimidine (CAS 74647-33-9) for pharmaceutical and chemical research. For Research Use Only. Not for human or therapeutic use. |
The comparative analysis of CA125, HE4, and the ROMA algorithm demonstrates a clear evolution in the diagnostic approach to ovarian cancer. While CA125 remains a widely available and useful marker, its limitations are substantial. HE4 offers superior specificity, particularly in distinguishing ovarian cancer from benign conditions like endometriosis. The integration of these biomarkers into the ROMA algorithm enhances overall diagnostic accuracy, providing a valuable tool for preoperative risk stratification and helping to ensure that patients with a high likelihood of malignancy are referred to specialized gynecologic oncology centers. Future research directions include the validation of novel multi-marker panels, the integration of biomarker data with advanced imaging models like ADNEX, and the exploration of liquid biopsy biomarkers such as circulating tumor DNA (ctDNA) for early detection and monitoring.
Ovarian cancer remains the most lethal gynecologic malignancy, with approximately 20,890 new cases and 12,730 deaths projected in the United States for 2025 [14]. The poor prognosis is largely attributable to late-stage diagnosis, with about 75% of patients presenting with advanced disease [15]. Within this challenging clinical context, predictive biomarkers have emerged as transformative tools for personalizing treatment strategies and improving patient outcomes. BRCA mutations and homologous recombination deficiency (HRD) status now serve as critical biomarkers guiding therapeutic decisions, particularly for poly(ADP-ribose) polymerase inhibitors (PARPi) and platinum-based chemotherapies [15] [16].
The homologous recombination repair (HRR) pathway represents a high-fidelity mechanism for repairing DNA double-strand breaks. When compromised through genetic or epigenetic alterations, this deficiency creates a therapeutic vulnerability that can be exploited through synthetic lethality [16]. PARPi trap PARP proteins on DNA, blocking repair of single-strand breaks that subsequently evolve into double-strand breaks during replication. In HRD cells, particularly those with BRCA1/2 mutations, these damages accumulate lethally while sparing healthy cells with intact HRR pathways [15] [16]. This scientific foundation has positioned HRD assessment as a cornerstone of precision oncology in ovarian cancer.
This guide provides a comprehensive comparison of BRCA and HRD biomarker testing methodologies, offering experimental validation data and technical protocols to inform their implementation in research and clinical contexts.
Biomarker Fundamentals: Mechanisms and Clinical Implications
BRCA Mutations: From Hereditary Risk to Therapeutic Target
BRCA1 and BRCA2 genes encode proteins integral to the HRR pathway, maintaining genomic stability through precise repair of DNA double-strand breaks [15]. Mutations in these genes, occurring in approximately 10-20% of ovarian cancers, compromise this repair function and increase lifetime ovarian cancer risk to 39-54% for BRCA1 and 11-30% for BRCA2 carriers [15] [3]. Beyond their established role in hereditary cancer syndromes, BRCA mutations have profound therapeutic implications:
- PARPi Sensitivity: BRCA-deficient cells exhibit extreme vulnerability to PARPi through synthetic lethality. In the SOLO1 trial, olaparib reduced the risk of progression or death by 70% compared to placebo in advanced BRCA-mutated ovarian cancer [3].
- Platinum Sensitivity: BRCA-mutated tumors demonstrate enhanced response to platinum-based chemotherapy, which induces DNA crosslinks requiring HRR for resolution [15].
- Prognostic Value: BRCA-mutated patients typically experience better initial outcomes, though long-term survival may be impacted by developing resistance mechanisms [15].
Homologous Recombination Deficiency: Expanding Beyond BRCA
HRD represents a broader phenotypic state encompassing BRCA mutations alongside other genetic and epigenetic alterations that impair HRR function [16]. Approximately 50% of high-grade serous ovarian carcinomas exhibit HRD, extending the potential benefit of PARPi beyond just BRCA-mutated cases [15] [17]. This "BRCAness" phenotype can arise through multiple mechanisms:
- Genetic Alterations: Mutations in HRR genes beyond BRCA1/2, including ATM, PALB2, RAD51C, RAD51D, CHEK2, and others [16] [17].
- Epigenetic Silencing: BRCA1 promoter hypermethylation, which silences gene expression without altering DNA sequence [16].
- Consequential Genomic Scars: The functional outcome of HRD manifests as characteristic genomic patterns including loss of heterozygosity (LOH), telomeric allelic imbalance (TAI), and large-scale state transitions (LST) [16].
Table 1: Comparative Analysis of Key Predictive Biomarkers in Ovarian Cancer
| Biomarker | Prevalence in Ovarian Cancer | Primary Predictive Value | Key Therapeutic Implications |
|---|---|---|---|
| BRCA1/2 Mutations | 10-20% [15] [3] | PARPi and platinum sensitivity [15] | Olaparib reduced progression risk by 70% in BRCA-mutated advanced ovarian cancer [3] |
| HRD Status | ~50% of HGSOC [17] | PARPi and platinum sensitivity [16] | Extends PARPi benefit to non-BRCA mutated tumors; in PRIMA trial, niraparib showed median PFS benefit (HR, 0.40) regardless of BRCA status [14] |
| BRCA1 Promoter Methylation | 5-15% [16] | PARPi sensitivity [16] | Epigenetic silencing creates HRD phenotype without mutation |
| Genomic Scar Signatures | Varies by cancer type [18] | Historical HRD regardless of current mechanism [16] | Foundation for GIS assessment (LOH+TAI+LST); may not reflect current HR status if reversion mutations occur |
Comparative Analytical Platforms: Technical Specifications and Performance Metrics
FDA-Approved and Regulated HRD Tests
The current clinical landscape features several validated platforms for HRD assessment, each with distinct technological approaches and performance characteristics.
Table 2: Analytical Comparison of Major HRD Testing Platforms
| Test Name | Technology | Biomarkers Assessed | Cut-off Values | Performance Metrics | Regulatory Status |
|---|---|---|---|---|---|
| MyChoice CDx Plus HRD (Myriad) [17] | NGS-based genomic scar analysis | GIS (LOH+TAI+LST), BRCA1/2 mutations | GIS ≥42 [17] | Used as reference in multiple clinical trials (PRIMA, PAOLA-1) [17] | FDA-approved |
| FoundationOne CDx (F1CDx) [18] | NGS-based (324 genes) | HRD signature (HRDsig), BRCA1/2 mutations | HRDsig score ≥0.7 [18] | PPA: 90.00%, NPA: 94.44% vs. reference; LoD: 23.04% tumor purity [18] | FDA-approved |
| AmoyDx HRD Kit [19] | NGS-based genomic scar analysis | GIS, BRCA1/2, TP53 mutations | Not specified | 88.6% concordance with Myriad; faster turnaround (5-9 days) [19] | China NMPA special review (2024) |
| GS Focus HRD (QIAseq) [17] | NGS-based (13,809 SNPs) | GIS, 15 HRR genes | GIS ≥65 [17] | 90% accuracy, 90% sensitivity, 90% specificity vs. MyChoice; kappa: 0.8 [17] | Laboratory-developed test |
Emerging and Research-Use Only Methodologies
Beyond established platforms, innovative approaches show significant promise for future clinical implementation:
- Pathological Image Analysis: Deep learning models like SuRe-Transformer can predict HRD status from H&E-stained whole slide images with AUROC of 0.887, offering a potentially faster, more cost-effective alternative to molecular assays [20].
- Liquid Biopsy Approaches: Circulating tumor DNA (ctDNA) analysis enables non-invasive HRD assessment and monitoring. After surgery, ctDNA presence strongly predicted relapse (hazard ratio ~17.6), outperforming CA-125 [14].
- Functional Assays: Nuclear RAD51 foci formation tests directly evaluate homologous recombination functionality rather than inferring from genetic scars [21].
- Transcriptomic Signatures: Long non-coding RNA panels (e.g., 29-lncRNA classifier) can stratify HRD status with random forest models achieving R² of 0.52 for HRD score prediction [22].
Experimental Protocols: Methodologies for HRD Assessment
Next-Generation Sequencing-Based Genomic Scar Analysis
Principle: This approach quantifies genomic instability patterns (LOH, TAI, LST) that accumulate in HRD tumors due to impaired DNA repair [16] [17].
Sample Requirements:
- Formalin-fixed paraffin-embedded (FFPE) tumor tissue blocks
- Tumor purity >20-30% (varies by platform)
- Necrosis <10%
- Matched normal tissue (for germline comparison) [17]
Procedure:
- DNA Extraction: Using ReliaPrep FFPE System or similar with minimum 100ng DNA input [17].
- Library Preparation: Hybridization-based capture using customized panels (e.g., 13,809 SNPs for GS Focus HRD) [17].
- Sequencing: Illumina platforms (NextSeq CN500) with paired-end reads (2×150 bp) [17].
- Bioinformatic Analysis:
- Alignment to reference genome (GRCh37/hg19)
- SNP allele frequency calculation
- Copy number variant calling
- LOH, TAI, and LST scoring
- GIS calculation (sum of three scores) [17]
- Interpretation: Compared to validated cut-offs (e.g., GIS ≥42 for MyChoice, ≥65 for GS Focus) [17].
Quality Control:
- Minimum sequencing depth (typically >500x)
- Target region coverage uniformity
- Internal controls for extraction and amplification [18]
Orthogonal Validation Methodology
Principle: Establish test performance against reference methods using clinically annotated samples.
Study Design:
- Sample Cohort: 41 patients with advanced/relapsed platinum-sensitive ovarian cancer [17].
- Reference Method: MyChoice CDx Plus HRD (Myriad Genetics) [17].
- Index Test: GS Focus HRD (QIAseq Custom Panel) [17].
- Statistical Analysis:
- Cohen's kappa for agreement (κ=0.8 indicates substantial agreement)
- Sensitivity/specificity calculation
- Positive/negative percent agreement [17]
Visualization of Key Concepts
Homologous Recombination Repair Pathway
Diagram 1: Homologous Recombination Repair Pathway. This diagram illustrates the sequential process of DNA double-strand break repair through the homologous recombination pathway, highlighting key proteins whose dysfunction can lead to HRD.
HRD Testing Methodologies and Applications
Diagram 2: HRD Testing Framework. This diagram outlines the causes and consequences of homologous recombination deficiency, detection methodologies, and clinical applications in ovarian cancer management.
Table 3: Key Research Reagent Solutions for HRD Biomarker Investigation
| Reagent/Resource | Specific Example | Research Application | Technical Considerations |
|---|---|---|---|
| NGS HRD Panels | MyChoice CDx, FoundationOne CDx, AmoyDx HRD Kit, GS Focus HRD | Comprehensive genomic scar analysis and HRR gene sequencing | Varying SNP densities (e.g., 13,809 SNPs in GS Focus); different GIS cut-offs [19] [18] [17] |
| DNA Extraction Kits | ReliaPrep FFPE System | High-quality DNA extraction from challenging FFPE samples | Minimum 100ng input required; optimized for degraded samples [17] |
| Library Prep Systems | QIAseq Custom Panel (QIAGEN) | Target enrichment and NGS library construction | Hybridization-based capture; customizable gene content [17] |
| Bioinformatics Tools | CLC Genomics Workbench, HRDsig algorithm | Variant calling, GIS calculation, HRD classification | FoundationOne's HRDsig uses >100 copy-number features in machine learning model [18] |
| Reference Materials | HRD-positive and negative control samples | Test validation and quality control | Characterized by orthogonal methods (biallelic BRCA1/2 loss) [18] |
| Image Analysis Platforms | SuRe-Transformer | H&E whole slide image analysis for HRD prediction | Cluster-size-weighted patch selection; radial decay self-attention [20] |
The comparative analysis of BRCA and HRD biomarker testing reveals a dynamic landscape where multiple technological approaches deliver robust predictive information for ovarian cancer therapy selection. While NGS-based genomic scar analysis currently represents the clinical standard, emerging methodologies including pathological AI, liquid biopsy, and functional assays offer complementary advantages for specific research and clinical scenarios.
Future development will likely focus on overcoming current limitations, particularly the static nature of genomic scars that may not reflect functional HRD status after reversion mutations occur [16]. Integration of multimodal approaches—combining genetic, transcriptomic, and proteomic data—promises enhanced predictive accuracy. Furthermore, standardization of testing methodologies and interpretation criteria across platforms will be essential for advancing comparative effectiveness research and validating these biomarkers across diverse patient populations.
For research and drug development professionals, selection of appropriate biomarker assessment strategies should be guided by specific experimental objectives, sample characteristics, and required performance parameters outlined in this comparison guide.
The diagnostic and prognostic assessment of ovarian cancer (OC) has traditionally relied on a limited set of biomarkers, with Cancer Antigen 125 (CA125) serving as the longstanding clinical standard. However, the quest for improved accuracy in early detection and prognostic prediction has catalyzed the investigation of novel molecular indicators. This review provides a comparative analysis of three emerging serum protein biomarkers—Chitinase-3-like protein 1 (CHI3L1/YKL-40), Osteopontin (OPN), and Kallikreins (KLKs)—within the context of ovarian cancer research. We evaluate their respective diagnostic power, prognostic value, and functional roles in tumor biology, supported by experimental data and structured comparisons to guide researchers and drug development professionals in prioritizing biomarker candidates for specific applications.
Biomarker Profiles and Functional Roles
CHI3L1 (YKL-40)
CHI3L1 is a secreted glycoprotein belonging to the glycoside hydrolase family 18, though it lacks enzymatic activity [23] [24]. It is produced by various cells, including macrophages, neutrophils, astrocytes, and cancer cells [24]. In ovarian cancer, CHI3L1 drives tumor progression through multiple mechanisms: it promotes cell proliferation and invasion, induces tumor blood vessel formation (angiogenesis), confers chemotherapy resistance, and facilitates tissue breakdown [3]. Critically, CHI3L1 enhances the properties of ovarian cancer stem-like cells, including spheroid formation, increased ALDH+ cell population, and resistance to cytotoxic drug-induced apoptosis [25]. This occurs via activation of Akt and Erk signaling pathways, leading to β-catenin stabilization and subsequent SOX2 expression [25]. Elevated CHI3L1 levels strongly predict worse survival outcomes in ovarian cancer patients, positioning it as both a diagnostic and prognostic marker [25] [3].
Osteopontin (OPN)
Osteopontin is a phosphorylated glycoprotein that regulates diverse physiological processes, including immune response, wound healing, and vascularization [3]. It is expressed in various cell types, such as osteoblasts, fibroblasts, macrophages, neutrophils, and epithelial cells [26]. In ovarian cancer, OPN levels are significantly elevated in the blood of patients compared to healthy women or those with benign ovarian disease [3]. High OPN expression is associated with more advanced disease, chemoresistance, and poor survival rates [3]. Its functional role in cancer involves regulating cell survival, adhesion, and inflammatory processes within the tumor microenvironment [26].
Kallikreins (KLKs)
Kallikreins represent a family of 15 serine protease enzymes, several of which are overexpressed in ovarian tumor cells [27] [3]. These proteases are implicated in inflammation and the management of blood flow [3]. In ovarian cancer, specific KLKs have been identified as potential diagnostic and prognostic markers, with expression patterns correlating with resistance to chemotherapy, tumor burden, and overall patient prognosis [27] [3]. Research is actively exploring their utility as early detection markers, leveraging their abundant presence in patient sera and ascites [27].
Comparative Diagnostic and Prognostic Performance
Table 1: Comparative Diagnostic Performance of Emerging Ovarian Cancer Biomarkers
| Biomarker | Reported Sensitivity | Reported Specificity | Key Strengths | Principal Limitations |
|---|---|---|---|---|
| CHI3L1 (YKL-40) | 80% [3] | 70% [3] | Superior predictor vs CA125 alone; strong prognostic value for poor outcome [3]. | Requires further validation in multi-center cohorts. |
| Osteopontin (OPN) | Data specific to OC not available in search | Data specific to OC not available in search | Significant elevation in OC vs healthy/benign disease; associated with advanced stage [3]. | Less specific than HE4; can be elevated in other benign and malignant conditions. |
| Kallikreins (KLKs) | Data specific to OC not available in search | Data specific to OC not available in search | Family of 15 proteins provides multiple signals; potential for early detection [27] [3]. | Individual KLKs may lack standalone power; best used in panels. |
Table 2: Prognostic Value and Functional Associations in Ovarian Cancer
| Biomarker | Prognostic Association | Associated Biological Processes | Therapeutic Implications |
|---|---|---|---|
| CHI3L1 (YKL-40) | Shorter survival; chemoresistance [25] [3] | Cancer stemness, proliferation, invasion, angiogenesis [25] [3] | Potential target for inhibiting stem-like properties and overcoming chemoresistance. |
| Osteopontin (OPN) | Poor survival; chemoresistance [3] | Immune modulation, vascularization, cell adhesion [26] [3] | Associated with advanced disease and aggression; potential target for disrupting TME. |
| Kallikreins (KLKs) | Correlates with tumor burden and prognosis [27] [3] | Proteolysis, inflammation, metastasis [3] | Specific KLK signatures may inform disease course and treatment response. |
The integration of these biomarkers into multi-marker panels has demonstrated enhanced performance. For instance, a model incorporating CA125, HE4, and CHI3L1 achieved a sensitivity of 85.7% at a specificity of 95.4% for detecting ovarian cancer up to one year before clinical diagnosis [3]. Furthermore, artificial intelligence (AI) algorithms analyzing complex biomarker data from blood samples have shown outstanding diagnostic capability, with a pooled area under the curve (AUC) of 0.95 in a recent meta-analysis, highlighting the future potential of high-dimensional biomarker integration [28].
Experimental Protocols and Methodologies
Serum Biomarker Quantification
The measurement of circulating CHI3L1, OPN, and KLKs typically relies on enzyme-linked immunosorbent assay (ELISA). The general protocol involves:
- Sample Collection: Fasting venous blood samples are collected from patients and controls. Serum is obtained by centrifugation (e.g., at 3000 rpm for 10 minutes at 4°C) and stored at -80°C until analysis [29] [26] [30].
- Assay Procedure: Commercially available ELISA kits are used following manufacturer protocols. Briefly, diluted serum samples are added to plates pre-coated with capture antibodies. After incubation and washing, a biotin-conjugated detection antibody is added, followed by a streptavidin-HRP (horseradish peroxidase) conjugate. A tetramethylbenzidine (TMB) substrate is added for color development, which is stopped with acid. The optical density is measured at 450 nm, and biomarker concentrations are determined by interpolation from a standard curve [29] [26].
- Data Analysis: Concentrations are reported in ng/mL or pg/mL. Statistical analyses correlate biomarker levels with clinical parameters like disease stage, treatment response, and survival outcomes.
Functional Analysis in Cellular Models
In vitro experiments are crucial for elucidating the functional roles of these biomarkers.
- CHI3L1 Overexpression/Knockdown: Studies utilize ovarian cancer cell lines (e.g., OVCAR3, CA5171) engineered to overexpress or knockdown CHI3L1 using transfection methods [25].
- Functional Assays:
- Tumor Spheroid Formation: Assesses self-renewal and stem-like properties. Cells are cultured in low-attachment plates, and the number/size of spheroids are quantified [25].
- Side-Population and Aldefluor Assays: Flow cytometry-based methods to identify and isolate cancer stem-like cell populations [25].
- Apoptosis Assays: Cells are treated with cytotoxic drugs, and apoptosis is measured via flow cytometry (Annexin V staining) or caspase-3/7 activity assays [25].
- Proliferation Assays: Evaluated by 5-ethynyl-2’-deoxyuridine (EdU) incorporation or proliferating cell nuclear antigen (PCNA) expression [23].
- Pathway Analysis: Western blotting and qRT-PCR are used to analyze downstream signaling pathways (e.g., Akt, Erk, β-catenin, SOX2) in manipulated cells [25].
Key Signaling Pathways
The signaling mechanisms of these biomarkers underscore their pro-tumorigenic roles. CHI3L1 binding to receptors like CRTH2 triggers a downstream cascade involving IKKβ, S6K1, and S6 phosphorylation, impairing neural stem cell function but also promoting cancer cell survival [23]. In ovarian cancer, CHI3L1 activates Akt and Erk pathways, stabilizing β-catenin and inducing the stemness transcription factor SOX2 [25]. Osteopontin signals through receptors including CD44 and integrins, activating PI3K-Akt and NF-κB pathways to drive inflammation and cell survival [26]. Kallikreins, as serine proteases, exert their effects by cleaving and activating Protease-Activated Receptors (PARs), remodeling the extracellular matrix (ECM), and activating growth factors, thereby influencing tumor cell signaling and the microenvironment [27] [3].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Biomarker Investigation
| Reagent / Assay | Primary Function | Example Application |
|---|---|---|
| Commercial ELISA Kits | Quantify biomarker concentration in serum/plasma/ascites. | Measuring baseline CHI3L1, OPN, or specific KLK levels in patient cohorts [29] [26] [30]. |
| Validated Antibodies | Detect protein expression via Western Blot (WB) and Immunohistochemistry (IHC). | Assessing CHI3L1 or OPN expression and localization in tumor tissues [29] [25]. |
| qRT-PCR Assays | Measure mRNA expression levels of biomarkers and pathway genes. | Validating CHI3L1/KLK overexpression in cell lines or tumor tissues [25] [31]. |
| Lentiviral shRNA/ cDNA Constructs | Genetically knock down or overexpress target genes in cell lines. | Establishing CHI3L1-knockdown or overexpressing transfectants for functional studies [25]. |
| Low-Attachment Plates | Culture cells in suspension to form 3D tumor spheroids. | Evaluating the effect of CHI3L1 on cancer stem-like cell properties [25]. |
| Aldefluor Assay Kit | Identify and isolate cells with high aldehyde dehydrogenase (ALDH) activity. | Quantifying the ALDH+ cancer stem-like cell population in manipulated cells [25]. |
| Acetoximebenzoate | Acetoximebenzoate, MF:C9H9NO2, MW:163.17 g/mol | Chemical Reagent |
| N-(Hex-5-en-2-yl)aniline | N-(Hex-5-en-2-yl)aniline, MF:C12H17N, MW:175.27 g/mol | Chemical Reagent |
CHI3L1, Osteopontin, and Kallikreins each present distinct profiles as promising biomarkers that augment the traditional CA125-based framework for ovarian cancer management. CHI3L1 stands out for its strong prognostic power and direct role in promoting cancer stemness and chemoresistance. Osteopontin serves as a valuable indicator of advanced disease and aggression. The Kallikrein family offers a rich source of complementary signals for multi-analyte panels. The future of ovarian cancer diagnostics lies not in identifying a single superior biomarker, but in strategically combining these molecules—potentially using AI-driven models—to achieve the sensitivity and specificity required for early detection and personalized prognostic stratification. Further research and clinical validation are essential to translate these promising biomarkers from the research bench to the clinical bedside.
Ovarian cancer (OC) remains the most lethal gynecological malignancy, with a stark disparity in survival rates between early and late-stage disease. The 5-year survival rate for early-stage OC reaches 92.4%, but plummets to 31–50% for advanced-stage disease [32]. Unfortunately, approximately 75% of epithelial ovarian cancer (EOC) patients present with advanced-stage disease at diagnosis due to the disease's asymptomatic nature and the limitations of current diagnostic tools [33]. The conventional biomarker CA-125 has demonstrated significant limitations, including elevation in less than 50% of early-stage cases and non-expression by about 20% of all OC tumors [32]. Furthermore, large screening trials have shown that while CA-125 combined with transvaginal ultrasound increased early-stage detection rates, it failed to reduce mortality [33]. These critical diagnostic gaps have accelerated research into metabolomic biomarkers, which capture functional readouts of cellular processes and offer promising avenues for early detection through liquid biopsy approaches [34]. The integration of machine learning with multi-omics data further enhances the potential to transform ovarian cancer diagnosis through improved sensitivity, specificity, and clinical utility.
Comparative Performance of Diagnostic Biomarker Panels
Diagnostic Accuracy of Emerging Biomarker Panels
Table 1: Comparative Performance of Novel Biomarker Panels vs. Traditional Biomarkers
| Biomarker Panel | Sensitivity (%) | Specificity (%) | AUC | Sample Size | Clinical Context |
|---|---|---|---|---|---|
| 4-protein + 3-metabolite panel [33] | 95.2 | 91.2 | 0.975 | Training: 96 | Distinguishing EOC from non-OC individuals |
| Same panel (Validation Cohort 1) [33] | - | - | 0.962 | 25 | Independent validation |
| Same panel (Validation Cohort 2) [33] | - | - | 0.965 | 130 | Independent validation |
| Methionyl-Cysteine, Citrulline, TTCA + CA-125 [32] | - | - | 0.970 | Training: 84 | Differentiating malignant from benign OC |
| Same metabolites + CA-125 (Validation) [32] | - | - | 0.960 | 36 | Independent validation |
| Mercy Halo EVP test [35] | 89 | 98 | - | - | Preclinical Stage I/II HGSC detection |
| Traditional CA-125 [32] | <50 (early-stage) | - | - | - | Early-stage detection |
Machine Learning-Enhanced Diagnostic Models
Table 2: Performance of Machine Learning Models in Ovarian Cancer Diagnosis
| ML Model | Biomarkers Used | Performance | Clinical Application |
|---|---|---|---|
| Ensemble Methods (Random Forest, XGBoost) [36] | Multi-modal data (CA-125, HE4, inflammatory, metabolic, hematologic parameters) | AUC >0.90, Accuracy up to 99.82% | Diagnosing OC, distinguishing malignant from benign tumors |
| Deep Learning (RNNs) [36] | Similar multi-modal data | Survival prediction AUC up to 0.866 | Treatment response forecasting |
| Biomarker-driven ML models [36] | CA-125, HE4 combined with CRP, NLR | Enhanced specificity and sensitivity | Risk stratification and treatment planning |
Experimental Protocols and Methodologies
Integrated Proteomic and Metabolomic Workflow
A landmark 2025 study established a comprehensive protocol for developing a multi-omics diagnostic panel for epithelial ovarian cancer [33]. The experimental workflow encompassed patient recruitment, sample processing, multi-omics data acquisition, and computational analysis:
Patient Cohort and Sample Collection: The prospective diagnostic cohort study included 536 participants with imaging-suspected adnexal masses, uterine fibroids, or pelvic organ prolapse. After exclusions, the final cohort comprised 251 participants: EOC (n=97), borderline ovarian tumors (n=38), benign ovarian tumors (n=54), and healthy controls (n=62). Blood samples were collected after an 8-12-hour fasting period using K2-EDTA tubes, immediately placed on ice, and processed within 4 hours. Plasma separation was performed by centrifugation at 1750×g for 10 minutes at 4°C, with aliquots stored at -80°C until analysis [33].
Proteomic Analysis: High-abundance proteins were removed using ProteoMiner Protein Enrichment kits. Protein concentration was measured via BCA assay, with equal amounts digested. Proteins were reduced with 10 mM DTT (37°C, 45 min), alkylated with 50 mM iodoacetamide (dark, 15 min), and precipitated with acetone (-20°C, 2h). The pellet was resuspended in 25 mM ammonium bicarbonate, digested overnight with trypsin (37°C), and desalted using C18 cartridges. For comprehensive library generation, peptides were fractionated on a reversed-phase column at pH 10, with 52 fractions collected and concatenated into 10 [33].
Metabolomic Profiling: The study employed both untargeted and targeted metabolomics approaches, though specific methodological details for metabolite extraction and analysis were not elaborated in the available excerpt. The identified diagnostic panel included three key metabolites: kynurenine, indole, and 3-hydroxybutyrate [33].
Data Integration and Validation: A machine learning model was trained on a cohort of 34 EOC patients and 62 non-OC individuals to distinguish EOC from other groups. The model was rigorously validated in two independent cohorts (validation cohort 1, n=25; validation cohort 2, n=130) using targeted proteomics and untargeted metabolomics [33].
Metabolic Pathway Alterations in Ovarian Cancer
Metabolomic studies have revealed consistent alterations in several key metabolic pathways in ovarian cancer patients, providing insights into the underlying disease mechanisms and potential diagnostic targets:
Tryptophan Metabolism: The kynurenine pathway of tryptophan metabolism has emerged as significantly dysregulated in ovarian cancer. A 2025 study identified kynurenine as one of three key diagnostic metabolites in their panel [33]. External transcriptomic data from TCGA-OV and GTEx bulk RNA-seq confirmed upregulation of TDO2 (tryptophan 2,3-dioxygenase) in ovarian cancer tissues, particularly in fibroblasts. This TDO2 upregulation was experimentally validated through quantitative PCR, immunohistochemistry, and immunofluorescence using clinical specimens, establishing a mechanistic link between tumor metabolism and circulating metabolite levels [33].
Sphingolipid and Steroid Hormone Metabolism: Metabolite analysis revealed aberrant sphingolipid metabolism and steroid hormone biosynthesis in EOC patients' plasma, though specific metabolites in these pathways were not detailed in the available excerpt [33].
Energy Metabolism Pathways: Alterations in energy metabolism, including elevated lactate production via aerobic glycolysis (the Warburg effect), have been consistently observed across multiple cancer types [34]. While not specifically documented in the ovarian cancer studies reviewed, this pathway represents a common metabolic adaptation in cancer cells that may contribute to the metabolic signatures detectable in liquid biopsies.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Analytical Platforms for Metabolomic Biomarker Discovery
| Reagent/Platform | Specific Function | Application in Ovarian Cancer Studies |
|---|---|---|
| ProteoMiner Protein Enrichment Kit [33] | Depletion of high-abundance proteins to enhance detection of low-abundance biomarkers | Proteomic analysis of plasma samples |
| K2-EDTA Blood Collection Tubes [33] | Anticoagulation and preservation of blood samples during collection and processing | Standardized blood collection from patient cohorts |
| Liquid Chromatography-Mass Spectrometry (LC-MS) [33] [37] | High-sensitivity separation, identification, and quantification of metabolites and proteins | Untargeted and targeted metabolomic/proteomic profiling |
| Nuclear Magnetic Resonance (NMR) Spectroscopy [37] [34] | Non-destructive metabolite identification and quantification with high reproducibility | Metabolic fingerprinting and structural elucidation |
| Gas Chromatography-Mass Spectrometry (GC-MS) [37] | Analysis of volatile and thermally stable metabolites after derivatization | Targeted metabolomic studies of specific metabolite classes |
| Trypsin [33] | Proteolytic digestion of proteins into peptides for mass spectrometric analysis | Sample preparation for proteomic studies |
| C18 Cartridges [33] | Desalting and purification of peptides prior to mass spectrometry | Sample clean-up in proteomic workflows |
| BCA Assay [33] | Colorimetric quantification of protein concentration | Standardization of protein input for assays |
| 2-Methyl-2-phenylpentanal | 2-Methyl-2-phenylpentanal|C12H16O|Research Chemical | |
| 3-Cyclopentylbutan-2-ol | 3-Cyclopentylbutan-2-ol|C9H18O |
The integration of metabolomic biomarkers with proteomic data and machine learning algorithms represents a transformative approach to ovarian cancer diagnosis. The exceptional performance of multi-analyte panels, achieving AUC values exceeding 0.96 in validation cohorts, demonstrates the considerable potential of this approach to overcome the limitations of single-marker strategies [33]. Future research directions should prioritize multi-center validation studies to establish generalizability across diverse populations, standardization of analytical protocols to ensure reproducibility, and integration with other omics technologies for comprehensive molecular profiling [36] [33]. The successful application of machine learning for pattern recognition in complex metabolomic data further enhances the potential for developing clinically viable diagnostic tests that can significantly impact early detection and patient outcomes in ovarian cancer. As these technologies mature and validation studies expand, metabolomic biomarkers are poised to transition from research tools to essential components of ovarian cancer diagnostic workflows, potentially enabling the early detection that has remained elusive with conventional approaches.
Ovarian cancer (OC) remains the most lethal gynecological malignancy, largely due to late-stage diagnosis and nonspecific early symptoms [36]. The heterogeneous nature of epithelial ovarian cancer (EOC), comprising distinct histopathological subtypes with varying clinical behaviors and molecular profiles, further complicates effective treatment [38]. In this challenging landscape, biomarkers have emerged as indispensable tools for navigating clinical decision-making. These measurable biological indicators—found in blood, tissue, or other bodily fluids—provide critical information about cancer presence, disease trajectory, and potential response to therapies [3].
The comparative effectiveness of ovarian cancer management increasingly depends on precisely understanding the distinct clinical functions of biomarkers: diagnostic markers that identify the presence of cancer, prognostic markers that forecast disease course regardless of therapy, and predictive markers that anticipate response to specific treatments [3]. This framework enables more personalized therapeutic strategies, moving beyond one-size-fits-all approaches to account for the unique biological characteristics of both the patient and their cancer. As biomarker research evolves with technological advancements in proteomics, machine learning, and molecular profiling, the potential for transforming ovarian cancer outcomes through precision medicine continues to expand [36] [39].
Biomarker Classification and Clinical Applications
Biomarkers serve distinct, specialized functions in clinical management, each contributing specific information to guide patient care decisions. The table below delineates the three primary biomarker categories and their clinical applications in ovarian cancer.
Table 1: Classification of Ovarian Cancer Biomarkers and Their Clinical Roles
| Biomarker Type | Primary Function | Clinical Application Examples | Representative Biomarkers |
|---|---|---|---|
| Diagnostic | Detects the presence of cancer [3] | - Differentiate malignant from benign pelvic masses [36]- Early-stage detection [40] | CA-125, HE4, ROMA algorithm (CA-125 + HE4), Osteopontin (OPN) [36] [40] [3] |
| Prognostic | Forecasts disease aggressiveness and overall patient outcome, independent of therapy [3] | - Predict overall survival (OS) and disease-specific survival (DSS) [39]- Assess risk of recurrence [36] | Bikunin, VEGF, SMOC1, GDPGP1, EPRS1 [36] [40] [38] |
| Predictive | Anticipates response to a specific therapeutic intervention [3] | - Guides use of PARP inhibitors [40]- Predicts platinum-based chemotherapy response [3] | BRCA1/2 mutations, KRAS mutations, HRD status, CHI3L1 (YKL-40) [40] [3] |
Comparative Performance of Key Ovarian Cancer Biomarkers
The clinical utility of a biomarker is quantified through its performance in validation studies. Sensitivity measures its ability to correctly identify patients with the disease, while specificity reflects its ability to correctly identify patients without the disease. The following table compares the documented performance of established and emerging ovarian cancer biomarkers.
Table 2: Comparative Performance Metrics of Ovarian Cancer Biomarkers
| Biomarker / Panel | Reported Sensitivity (%) | Reported Specificity (%) | AUC | Clinical Context & Notes |
|---|---|---|---|---|
| CA-125 (alone) | ~50 (early-stage) [41] | Varies; can be elevated in benign conditions [3] | - | Most widely used; limited by false positives and negatives [36] [41] |
| HE4 (alone) | - | Higher than CA-125 for ovarian cancer [3] | - | Less likely elevated in benign conditions; improves specificity [36] [3] |
| CA-125 + HE4 (ROMA) | - | Improved vs. CA-125 alone [36] | - | Algorithm for classifying malignancy risk [36] |
| Multi-marker ML Model | Up to 99.82 [36] | - | >0.90 [36] | Integrates biomarkers (e.g., CA-125, HE4, CRP, NLR) with machine learning [36] |
| CHI3L1 (YKL-40) | 80 [3] | 70 [3] | - | Emerging biomarker; drives cancer growth and chemoresistance [3] |
| CA-125 + HE4 + CHI3L1 | 85.7 [3] | 95.4 [3] | - | Predictive up to one year before diagnosis [3] |
| Proteomic Panel (inc. CA-125) | 94 [3] | 98 [3] | - | For early-stage identification using mass spectrometry [3] |
Experimental Protocols for Biomarker Validation
Proteomic Workflow for Histotype-Specific Biomarker Discovery
Objective: To identify differentially abundant proteins (DAPs) that stratify ovarian cancer histotypes and discover candidate prognostic biomarkers using mass spectrometry-based proteomics [39].
Methodology:
- Sample Preparation: 300 patient tissue samples (including high-grade serous carcinoma (HGSC), clear cell carcinoma (CCC), mucinous carcinoma (MC), endometrioid carcinoma (EC), borderline, and benign tumors) are processed. Proteins are extracted and digested into peptides.
- Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS): Peptides are separated by liquid chromatography and ionized. Mass-to-charge ratios of peptides and their fragments are measured in the mass spectrometer.
- Data Analysis: Proteomic data are analyzed to identify DAPs across histotypes. Bioinformatics tools are used for enrichment analysis of biological processes. Survival analysis (e.g., Cox regression) correlates protein abundance with overall survival (OS) and disease-specific survival (DSS) to identify prognostic biomarkers like GLYR1 (favorable) and SDF4 (unfavorable) [39].
Proteomic Biomarker Discovery Workflow
Machine Learning Integration with Biomarker Data
Objective: To develop a model that outperforms traditional statistical methods in diagnosing ovarian cancer and predicting survival by integrating multi-modal biomarker data [36].
Methodology:
- Data Collection & Feature Engineering: Clinical data and biomarker levels (e.g., CA-125, HE4, inflammatory markers like CRP and NLR) are compiled. Features are normalized and selected.
- Algorithm Training: Ensemble methods like Random Forest or XGBoost are trained on the dataset. The model learns patterns associated with malignant vs. benign tumors and patient outcomes.
- Validation & Performance Metrics: The model is tested on a held-out validation set. Performance is evaluated using Area Under the Curve (AUC), accuracy, sensitivity, and specificity. Studies report AUC values exceeding 0.90 for diagnosis and up to 0.866 for survival prediction [36].
Machine Learning Model Development
Structural Analysis of CA-125 for Improved Assay Development
Objective: To redefine the accurate molecular structure of the CA-125 protein using long-read sequencing, enabling the development of more precise diagnostic tests [41].
Methodology:
- Long-Read Sequencing: Third-generation DNA sequencing technology (e.g., PacBio SMRT sequencing) is applied to multiple ovarian cancer cell lines and banked tumor tissues. This technology generates long contiguous reads that span repetitive regions.
- Subunit Identification & 3D Modeling: The sequencing data is analyzed to identify the correct number and sequence of protein subunits. The new sequence is fed into an AI-powered system (e.g., AlphaFold2) to predict the three-dimensional structure of the CA-125 protein.
- Implications: This foundational research corrects the long-held model of CA-125 from 63 "beads" to 19, allowing researchers to pinpoint which subunits are critical for antibody binding in clinical tests, thereby reducing false positives and negatives [41].
Essential Research Reagent Solutions
The following table details key reagents and materials essential for conducting the described biomarker validation experiments.
Table 3: Essential Research Reagent Solutions for Biomarker Studies
| Research Reagent / Material | Function / Application |
|---|---|
| Ovarian Cancer Patient Samples (Tissue, Serum, Plasma) | Primary source for biomarker discovery and validation; requires appropriate consent and ethical approval [39] [38]. |
| Immunoassay Kits (e.g., ELISA) | Quantitatively measure specific protein biomarkers (e.g., CA-125, HE4, VEGF) in serum/plasma [40]. |
| Mass Spectrometry Grade Solvents & Enzymes | Essential for sample preparation and protein digestion for proteomic analysis via LC-MS/MS [39]. |
| Long-Read Sequencing Kits | Enable accurate sequencing of complex, repetitive genes like MUC16 (encodes CA-125) for structural analysis [41]. |
| Primary Antibodies for IHC (e.g., WT1, p53, Napsin A) | Critical for histotype classification and validating protein localization in tissue sections [38]. |
| Programming Libraries for ML (e.g., Scikit-learn, XGBoost in R/Python) | Implement machine learning algorithms for integrating and analyzing multi-modal biomarker data [36]. |
The comparative effectiveness of ovarian cancer biomarkers is unequivocally enhanced when their distinct diagnostic, prognostic, and predictive roles are leveraged in concert. No single biomarker provides a complete picture; however, integrating multiple biomarkers into panels, refining existing tests through structural insights, and harnessing the power of machine learning for data integration represent the most promising path forward [36] [3] [41].
The future of ovarian cancer management lies in personalized, histotype-specific treatment strategies. This will be powered by a deeper molecular understanding of the disease, facilitated by the continuous discovery and validation of biomarkers. As research unravels the unique biological pathways of each histotype, the development of targeted therapies guided by predictive biomarkers will become increasingly precise [39] [38]. Overcoming current challenges related to clinical adoption—such as the need for multi-center validation, standardization of assays, and integration of explainable AI—will be crucial to translating these advanced biomarker strategies into improved survival and quality of life for patients [36].
Innovative Methodologies and Translational Applications in Biomarker Discovery
Comparative Performance of Ovarian Cancer Immunotherapy Regimens
Table 1: Efficacy Rankings of Treatment Regimens for Advanced Recurrent Ovarian Cancer (Network Meta-Analysis) [42]
| Treatment Regimen | Surface Under the Cumulative Ranking Curve (SUCRA) Value | Key Efficacy Findings |
|---|---|---|
| PARP inhibitor + Anti-angiogenic | 95.26% | Superior to eight other regimens; significant improvement in patient survival. |
| Double Immunotherapy + Chemotherapy | 87.24% | Demonstrated strong efficacy. |
| Anti-angiogenic + Chemotherapy | 60.14% | Similar efficacy to single anti-angiogenic and single-agent PARP regimens. |
| Single-agent PARP inhibitor | 61.82% | Similar efficacy to anti-angiogenic plus chemotherapy regimens. |
| Single-agent Anti-angiogenic | 52.30% | Similar efficacy to other non-immunotherapy regimens. |
| Immunotherapy + Chemotherapy | 31.61% | Significant improvement compared to chemotherapy alone. |
| Double Immunotherapy | 36.49% | Superior efficacy compared to single immunotherapy regimen. |
| Single Immunotherapy | 8.53% | Demonstrated limited efficacy. |
Table 2: Comparative Effectiveness of Immunotherapeutic Strategies in Ovarian Cancer [43]
| Immunotherapeutic Strategy | Overall Survival (Hazard Ratio) | Progression-Free Survival | Key Safety Findings |
|---|---|---|---|
| Cancer Vaccines (CV) | HR = 0.56 (95% CI: 0.43–0.73) | Standardized Mean Difference (SMD) = 0.95 (95% CI: 0.16–1.75) | N/A |
| Dual Immune Checkpoint Blockade (DICB) | HR = 0.65 (95% CI: 0.46–0.92) | N/A | N/A |
| CTLA-4 Inhibitors | N/A | N/A | Markedly increased Objective Response Rate (ORR = 99.32); no significant difference in Disease Control Rate. |
| PD-1 Inhibitors | N/A | N/A | Best safety profile; reduced grade ≥3 Adverse Events (OR = 0.16) and overall Treatment-Related Adverse Events. |
Detailed Experimental Protocols in AI-Driven Biomarker Discovery
- Study Population and Data Source: Utilized data from the China Health and Retirement Longitudinal Study (CHARLS). The baseline survey (2011/2012) included 9,702 participants (≥45 years), and the third wave (2015/2016) with 9,455 participants was used for test set validation.
- Blood-Based Biomarkers: Sixteen biomarkers were used as features, including total cholesterol, triglyceride, glycated hemoglobin (HbA1c), urea, creatinine, high-sensitivity C-reactive protein, platelet count, white blood cell count, mean corpuscular volume, glucose, high-density lipoprotein, low-density lipoprotein, hemoglobin, cystatin C, uric acid, and hematocrit.
- Machine Learning Modeling:
- Target Variables: Two separate predictors were developed: one for Biological Age (BA) using chronological age as the target, and another for Frailty Status using a binarized frailty index (cut-point of 0.25).
- Algorithms: Four tree-based ML algorithms (Random Forest, Gradient Boosting, CatBoost, eXtreme Gradient Boosting) were trained and validated.
- Data Preprocessing: Missing data were imputed with the mean, and data were normalized using a min-max scalar. The frailty predictor used the Synthetic Minority Over-sampling Technique (SMOTE) to address class imbalance.
- Model Validation: Dataset was split into training (80%) and test set (20%). Models were trained using tenfold cross-validation. Hyperparameters were optimized via grid search.
- Explainable AI (XAI) Analysis: SHapley Additive exPlanations (SHAP) analysis was conducted on the best-performing models to interpret the contribution of individual biomarkers.
- Predictive Biomarker Modeling Framework (PBMF): This framework uses contrastive learning to systematically extract predictive biomarkers from rich clinical data. It is designed to distinguish between predictive biomarkers (which report on treatment effectiveness) and prognostic biomarkers (which indicate likely disease outcome independent of treatment).
- Data Integration: AI models amalgamate multiple data modalities, including radiography, histology, genomics, and electronic health records, to enhance diagnostic precision and reliability.
- Validation: Retrospective studies have demonstrated the potential of this framework, revealing significant improvements in patient survival rates through its predictive capabilities.
Visualizing Pathways and Workflows
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Platforms for AI-Driven Biomarker Discovery
| Reagent / Platform | Function | Application Example |
|---|---|---|
| Absolute IDQ p180 Kit (Biocrates) | Targeted metabolomics kit quantifying 194 endogenous metabolites from 5 compound classes. [44] | Plasma metabolite measurement for biomarker discovery in large-artery atherosclerosis. [44] |
| PandaOmics | AI-driven platform for analyzing multimodal omics data to identify therapeutic targets and biomarkers. [45] | Identification of intricate correlations within multi-omics datasets for target discovery in oncology. [45] |
| SHapley Additive exPlanations (SHAP) | Explainable AI (XAI) method for interpreting output of machine learning models. [46] | Quantifying relative contribution of blood-based biomarkers (e.g., cystatin C) in biological age and frailty predictors. [46] |
| Cohort Data (e.g., CHARLS) | Large-scale, longitudinal cohort data with linked biospecimens. [46] | Training and validation dataset for developing ML predictors of biological age and frailty from blood biomarkers. [46] |
| scikit-learn, Pandas, NumPy (Python) | Open-source specialized Python packages for data preprocessing, analysis, and machine learning. [46] [44] | Building and validating ML models (e.g., Logistic Regression, Random Forest) for disease prediction and biomarker discovery. [46] [44] |
| (2-Ethoxyethyl) vinyl ether | (2-Ethoxyethyl) vinyl ether, MF:C6H12O2, MW:116.16 g/mol | Chemical Reagent |
| Dimethoxy Chlorimuron | Dimethoxy Chlorimuron, MF:C16H18N4O7S, MW:410.4 g/mol | Chemical Reagent |
Ovarian cancer remains the most lethal gynecological malignancy, primarily due to late-stage diagnosis and significant molecular heterogeneity that complicates treatment strategies [47] [48]. The limitations of single-omics approaches and single-marker biomarkers like CA-125 have driven the adoption of multi-omics integration, which provides a more comprehensive understanding of tumor biology by combining proteomic, glycoproteomic, and metabolomic data [47] [49]. This integrated approach enables the discovery of biomarker panels with superior diagnostic and prognostic performance compared to traditional methods, ultimately supporting the advancement of personalized oncology [49]. By systematically analyzing molecular patterns across multiple biological layers, researchers can identify functional subtypes, reveal druggable vulnerabilities, and develop more accurate classifiers for distinguishing benign from malignant conditions [47] [48] [49].
The technological evolution of high-throughput platforms, including next-generation sequencing, advanced mass spectrometry, and affinity-based proteomics, has made large-scale multi-omics studies feasible [49]. Concurrently, sophisticated computational tools and machine learning algorithms have emerged to integrate and extract meaningful biological insights from these complex, heterogeneous datasets [47] [49]. This review provides a comparative analysis of current multi-omics methodologies within ovarian cancer research, focusing on experimental data, technical protocols, and the translation of integrated findings into clinically applicable tools.
Comparative Performance of Multi-Omic Biomarker Panels
The integration of proteomic, glycoproteomic, and metabolomic data has yielded several promising biomarker panels for ovarian cancer diagnosis. The table below summarizes the performance characteristics of recently developed multi-omic signatures compared to established clinical biomarkers.
Table 1: Performance Comparison of Ovarian Cancer Biomarker Panels
| Biomarker Panel / Test | Omic Technology | Sample Size (Discovery/Validation) | Sensitivity (%) | Specificity (%) | AUC | Key Strengths |
|---|---|---|---|---|---|---|
| 8-Protein Panel [48] | Deep Plasma Proteomics | 171 / 233 | 97 (All-stage) 91 (Early-stage) | 68 | 0.96 | Excellent sensitivity for early-stage tumors; high-throughput |
| GlycoKnow Ovarian [50] | Serum Glycoproteomics | Internal & External Validation Cohorts | 86.7 (All-stage) 63.6 (Early-stage) | 89.7 | 0.909 | CA-125 independent; high specificity |
| EV Metabolite Panel [51] | Plasma EV Metabolomics | 37 OC, 22 BE, 46 CON | N/A | N/A | 0.94 (OC vs BE) | Focuses on extracellular vesicles; uses multiple ML algorithms |
| ROMA Score [48] | CA-125 + HE4 (Protein) | Established Test | 77.8-81.4 (Early-stage) | 77.2-80.9 | N/A | Current clinical standard |
| CA-125 Alone [48] | Single Protein | Established Test | ~85 (Early-stage) | ~54 | N/A | Widely available but limited specificity |
The experimental data reveal that multi-omic panels consistently outperform single-marker assays like CA-125. The 8-protein plasma proteomic panel demonstrates exceptionally high sensitivity, particularly for early-stage tumors, which is critical for improving patient outcomes [48]. The glycoproteomic classifier offers the advantage of high specificity, which can reduce false positives and unnecessary surgical interventions [50]. Meanwhile, EV-based metabolomics represents a novel approach that captures metabolic alterations in tumor-derived extracellular vesicles, providing a unique window into tumor pathophysiology [51].
Experimental Protocols and Methodological Frameworks
Deep Plasma Proteomics Workflow
The discovery of the 8-protein biomarker panel involved a rigorous multi-cohort experimental design [48]. Researchers analyzed 5,416 plasma proteins across two independent Swedish cohorts (Nâ‚=171, Nâ‚‚=233) comprising women surgically diagnosed with benign or malignant tumors.
- Sample Preparation: Plasma samples were collected according to standardized protocols, frozen, and stored at -70°C. Analysis was performed using high-throughput affinity-based proteomics.
- Experimental Design: One cohort served for discovery and training of risk-score models with a fixed cut-off for malignancy, while the second cohort was used for independent validation.
- Data Analysis: The team identified 327 biomarker associations (191 unique proteins) and replicated 99.7% of them. They performed protein-protein correlation network analysis and found that only 11% of the plasma protein changes correlated with corresponding tumor gene expression, suggesting that most associations reflect secondary effects of the tumor [48].
- Validation: The final model was validated in the replication cohort, achieving an AUC of 0.96 with 97% sensitivity at 68% specificity. For early-stage tumors, sensitivity was 91% at the same specificity, significantly outperforming CA-125 alone [48].
Glycoproteomic Analysis Pipeline
The GlycoKnow Ovarian diagnostic was developed using a targeted mass spectrometry approach to quantify glycopeptides in serum samples [50].
- Sample Collection: Serum samples were obtained from retrospective biobanks and prospective trials of patients with pelvic masses.
- Glycopeptide Quantification: Researchers quantified 38 peptides and glycopeptides using InterVenn's targeted mass spectrometry platform.
- Classifier Construction: A LASSO-regularized logistic regression model was applied in the training cohort, resulting in a locked classifier with 16 features.
- Validation Strategy: The classifier was evaluated on a hold-out test set and further validated in both internal and external cohorts from UT MD Anderson Cancer Center. The model maintained performance across all cohorts, demonstrating its robustness [50].
EV Metabolomics and Machine Learning Integration
The metabolic fingerprinting study employed a unique approach focusing on metabolites within plasma extracellular vesicles (EVs) [51].
- Participant Recruitment: The study included 37 ovarian cancer patients, 22 benign ovarian tumor patients, and 46 healthy controls.
- EV Isolation: EVs were isolated from plasma using a modified differential ultracentrifugation method. The isolated EVs were characterized by transmission electron microscopy and nanoparticle tracking analysis.
- Metabolomic Profiling: Global untargeted metabolic profiling was performed using sensitive thermal separation probe-based mass spectrometry.
- Machine Learning Classification: Seven machine learning algorithms were tested, including Artificial Neural Network (ANN), Decision Tree (DT), K-Nearest Neighbor (KNN), Logistics Regression (LR), Naïve Bayes (NB), Random Forest (RF), and Support Vector Machine (SVM). For distinguishing ovarian cancer from benign conditions, SVM achieved the highest AUC of 0.94 [51].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful multi-omics research requires specialized reagents, platforms, and computational tools. The table below details key solutions used in the featured studies.
Table 2: Essential Research Reagents and Platforms for Multi-Omics Studies
| Category | Specific Tool/Platform | Application/Function | Example Use Case |
|---|---|---|---|
| Proteomics Platforms | Affinity-based Proteomics (Olink, SomaScan) [48] [52] | High-throughput plasma protein quantification | Analysis of 5,416 plasma proteins [48] |
| Liquid Chromatography-Mass Spectrometry (LC-MS) [49] [51] | Protein identification and quantification | Glycopeptide quantification [50] | |
| Metabolomics Technologies | Thermal Separation Probe-MS [51] | Direct analysis of trace metabolites without derivatization | EV metabolome analysis [51] |
| Gas Chromatography-MS (GC-MS) [53] [51] | Separation and identification of volatile metabolites | Global untargeted metabolic profiling [51] | |
| Computational Tools | LASSO Regression [48] [50] [54] | Feature selection for biomarker panels | Developing 8-protein classifier [48] |
| Random Forest, SVM [51] | Classification and biomarker discovery | EV metabolite-based diagnosis [51] | |
| Specialized Reagents | EV Isolation Kits [51] | Purification of extracellular vesicles from biofluids | Plasma EV purification for metabolomics [51] |
| Glycoprotein Enrichment Materials [50] | Selective capture of glycopeptides | Serum glycoproteome analysis [50] | |
| 1-Hexene-d3 | 1-Hexene-d3 Deuterated Isotope | 1-Hexene-d3 is a deuterated isotope for research, used in spectroscopy, kinetic studies, and as a tracer. For Research Use Only (RUO). Not for human use. | Bench Chemicals |
| Glutamylisoleucine | Glutamylisoleucine, CAS:5879-22-1, MF:C11H20N2O5, MW:260.29 g/mol | Chemical Reagent | Bench Chemicals |
Integrated Signaling Pathways in Ovarian Cancer
Multi-omics studies have revealed several interconnected pathways that drive ovarian cancer pathogenesis. The integration of proteomic, glycoproteomic, and metabolomic data highlights how these pathways interact across molecular layers.
The pathway integration reveals that metabolic reprogramming is a central feature of ovarian cancer, characterized by altered phospholipid metabolism and amino acid depletion [55]. These changes are reflected in the proteomic landscape through alterations in established biomarkers like CA-125 and HE4, as well as newly identified proteins such as apolipoprotein A1 [48]. Simultaneously, glycoproteomic analyses detect aberrant glycosylation patterns that contribute to immune evasion and tumor microenvironment remodeling [50]. This multi-layer dysregulation creates a supportive niche for tumor progression and represents a promising source of therapeutic targets.
The integration of proteomic, glycoproteomic, and metabolomic data represents a transformative approach for ovarian cancer biomarker discovery. Experimental evidence demonstrates that multi-omic panels significantly outperform single-marker assays in both sensitivity and specificity, particularly for detecting early-stage disease [48] [50] [51]. However, challenges remain in standardizing analytical protocols, managing data heterogeneity, and validating findings across diverse patient populations [47] [49].
Future directions include the implementation of single-cell and spatial multi-omics technologies to resolve tumor heterogeneity at higher resolution [49]. Additionally, prospective clinical validation studies are needed to establish the utility of these integrated biomarkers in routine patient care. As computational methods for data integration continue to evolve, multi-omics approaches will increasingly enable personalized therapeutic strategies tailored to the molecular characteristics of individual ovarian cancers [49] [54].
Cancer management has traditionally relied on tissue biopsy as the gold standard for diagnosis and molecular profiling. However, this approach is invasive, subject to sampling bias due to tumor heterogeneity, and unsuitable for repeated monitoring. The emergence of liquid biopsy represents a transformative advancement in oncology, enabling minimally invasive detection and real-time monitoring of tumors through the analysis of circulating biomarkers in blood and other bodily fluids [56]. This approach facilitates dynamic assessment of tumor evolution, treatment response, and emerging resistance mechanisms, offering particular promise for malignancies such as ovarian cancer where early detection significantly improves survival outcomes [40] [41].
Liquid biopsies encompass multiple analyte classes, including circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), and extracellular vesicles (EVs), each providing complementary information about tumor biology [56] [57]. The clinical adoption of these biomarkers is accelerating rapidly, with the global circulating biomarkers market projected to grow from USD 5.17 billion in 2025 to USD 12.71 billion by 2033, reflecting a compound annual growth rate of 11.90% [58]. This growth is fueled by technological innovations in sequencing platforms, bioinformatics, and molecular analysis that continue to enhance the sensitivity and specificity of liquid biopsy applications across the cancer care continuum [59] [57].
Comparative Analysis of Circulating Biomarker Performance
Diagnostic Performance Across Biomarker Categories
Extensive research has evaluated the comparative performance of different liquid biopsy biomarkers for cancer detection. A comprehensive meta-analysis of 62 studies involving 18,739 individuals directly compared the diagnostic accuracy of three primary biomarker classes in colorectal cancer detection, providing robust comparative data relevant to solid tumors including ovarian cancer [60].
Table 1: Diagnostic Performance of Liquid Biopsy Biomarkers in Colorectal Cancer Detection
| Biomarker Type | Sensitivity (95% CI) | Specificity (95% CI) | Area Under Curve (AUC) | Diagnostic Odds Ratio |
|---|---|---|---|---|
| CTCs | 0.82 (0.79-0.85) | 0.97 (0.95-0.99) | 0.9772 | 65.34 |
| Exosomes | 0.76 (0.72-0.80) | 0.92 (0.89-0.94) | 0.9037 | 38.69 |
| ctDNA | 0.76 (0.75-0.77) | 0.88 (0.87-0.89) | 0.8963 | 22.41 |
| Overall Liquid Biopsy | 0.77 (0.76-0.78) | 0.89 (0.88-0.90) | 0.9004 | 25.93 |
The data reveal that CTCs demonstrated superior diagnostic performance with the highest sensitivity (0.82), specificity (0.97), and AUC (0.9772) among the biomarker categories evaluated [60]. This exceptional specificity suggests CTCs have particular utility in confirmatory testing scenarios where false positives must be minimized. Both exosomes and ctDNA showed comparable sensitivity (0.76), though exosomes exhibited moderately better specificity (0.92 vs. 0.88) [60].
Technical and Biological Characteristics of Major Biomarker Classes
Each biomarker category possesses distinct technical and biological characteristics that influence their clinical application and performance metrics.
Table 2: Technical and Biological Characteristics of Major Circulating Biomarker Classes
| Characteristic | CTCs | ctDNA | Exosomes/EVs |
|---|---|---|---|
| Biological Origin | Cells shed from primary/metastatic tumors | DNA fragments from apoptotic/necrotic tumor cells | Membrane-bound vesicles secreted by all cells |
| Approximate Concentration | 1-10 CTCs per 10 mL blood | 0.1-1.0% of total cfDNA | 10^9-10^12 particles per mL plasma |
| Half-Life | 1-2.5 hours | 16 minutes - 2.5 hours | ~30 minutes - 5 hours |
| Key Isolation Technologies | CellSearch, microfluidic devices, filtration | Silica membrane columns, magnetic beads, liquid phase extraction | Ultracentrifugation, precipitation, size-exclusion chromatography |
| Primary Analysis Methods | Immunofluorescence, RNA sequencing, functional assays | ddPCR, NGS, methylation analysis | Protein analysis, RNA sequencing, nanoparticle tracking |
| Information Content | Whole genomic/transcriptomic/proteomic data, functional status | Mutations, copy number variations, methylation patterns | Proteins, miRNAs, mRNAs, lipids, metabolic products |
Circulating Tumor Cells (CTCs) are intact cells shed from primary or metastatic sites that maintain viability in circulation. Their rarity presents significant technical challenges for isolation and analysis, with detection rates as low as approximately 1 CTC per million leukocytes [56]. Despite this limitation, CTCs provide comprehensive biological information, including whole genomes, transcriptomes, and proteomes, enabling functional characterization and serving as potential precursors to metastasis [56]. The CellSearch system remains the only FDA-cleared method for CTC enumeration in certain cancer types, demonstrating the clinical validity of CTC counts as prognostic biomarkers [56].
Circulating Tumor DNA (ctDNA) consists of fragmented DNA released predominantly through tumor cell apoptosis and necrosis, typically representing 0.1-1.0% of total cell-free DNA in cancer patients [56]. The short half-life of ctDNA (approximately 16 minutes to 2.5 hours) enables real-time monitoring of tumor dynamics and treatment response [56] [59]. ctDNA fragments in cancer patients tend to be shorter than non-malignant cell-free DNA, providing an additional discrimination feature for assay development [56]. Detection methods have evolved from single-mutation PCR assays to comprehensive next-generation sequencing approaches that simultaneously evaluate multiple genomic alterations [59].
Extracellular Vesicles (EVs), including exosomes, are membrane-bound nanoparticles secreted by all cells that carry molecular cargo from their cells of origin. Tumor-derived EVs play functional roles in cancer progression by facilitating communication between cancer cells and the tumor microenvironment [56]. Their stability in circulation and protection of internal cargo make them attractive biomarker sources, particularly for RNA and protein analytes that might otherwise degrade rapidly in plasma [57].
Liquid Biopsy Applications in Ovarian Cancer
Established and Emerging Ovarian Cancer Biomarkers
Ovarian cancer management has historically relied on protein biomarkers, particularly CA125 (also known as MUC16), which remains the most widely used biomarker for treatment monitoring and recurrence detection despite limitations in early detection sensitivity [40] [41]. Recent structural biology advances have revealed that the CA125 protein contains 19 rather than the previously believed 63 tandem repeat domains, information that may guide the development of improved detection assays [41].
Table 3: Established and Emerging Biomarkers in Ovarian Cancer
| Biomarker | Source | Clinical Utility | Performance Notes |
|---|---|---|---|
| CA125 | Serum | Treatment monitoring, recurrence detection | ~50% sensitivity for early-stage detection; non-specific elevation in benign conditions |
| HE4 | Serum | Diagnostic adjunct to CA125 | Improved specificity compared to CA125 alone |
| BRCA1/2 Mutations | Germline DNA/tumor tissue | Treatment selection, prognosis | ~15% of HGSOC cases; predicts PARP inhibitor sensitivity |
| CTCs | Blood | Prognostic assessment, disease monitoring | Independent predictor of progression-free and overall survival |
| Methylated ctDNA | Plasma | Early detection, monitoring | Tumor-specific methylation patterns offer high specificity |
| Exosomal miRNAs | Plasma | Early detection, subtype classification | Multi-analyte panels show promise for improved sensitivity |
The heterogeneous nature of ovarian cancer necessitates biomarker panels rather than single-analyte approaches for optimal detection accuracy. High-grade serous ovarian carcinoma (HGSOC), the most common and aggressive histological subtype, demonstrates distinct molecular features including TP53 mutations in over 95% of cases and homologous recombination deficiency in approximately 50%, creating opportunities for targeted biomarker development [40].
BRCA Pathway and Molecular Targeting in Ovarian Cancer
Approximately 15% of HGSOC cases harbor germline mutations in BRCA1 or BRCA2 genes, which play critical roles in DNA repair through homologous recombination [40]. The resulting genomic instability creates therapeutic vulnerabilities that have been successfully exploited with PARP inhibitors, demonstrating dramatically improved progression-free survival in clinical trials [40]. Liquid biopsy approaches enable non-invasive assessment of BRCA mutation status and monitoring of emerging resistance mechanisms, including reversion mutations that restore BRCA function [40].
Diagram 1: BRCA Pathway and PARP Inhibitor Mechanism in Ovarian Cancer. This diagram illustrates the synthetic lethality approach exploiting homologous recombination deficiency in BRCA-mutated ovarian cancers, a key therapeutic strategy where liquid biopsy can guide patient selection and monitor resistance development.
Evolution of Liquid Biopsy Technologies
Generational Progression in Liquid Biopsy Assays
The technological landscape of liquid biopsy has evolved through distinct generations, each with characteristic approaches and applications.
Diagram 2: Evolution of Liquid Biopsy Technologies. This diagram illustrates the progression from targeted mutation detection to comprehensive multi-analyte profiling enabled by advanced sequencing and computational approaches.
First-generation liquid biopsies utilized digital PCR to detect specific driver mutations in ctDNA, providing high specificity but limited sensitivity, particularly in early-stage disease or minimal residual disease settings [59]. Second-generation approaches expanded to targeted next-generation sequencing panels covering dozens to hundreds of cancer-associated genes, improving sensitivity through parallel mutation assessment but remaining constrained by the limited number of detectable mutations [59]. The emerging third-generation methodologies leverage whole-genome or epigenome analysis to identify analog signals including fragmentation patterns, epigenetic modifications, and chromosomal instability, enabling machine learning algorithms to detect cancer signals with significantly enhanced sensitivity for early detection applications [59].
Fragmentomics and Multi-Analyte Integration
A particularly promising advancement in third-generation liquid biopsy is fragmentomics - the analysis of cfDNA fragmentation patterns. Tumor-derived DNA fragments demonstrate characteristic size distributions, end motifs, and genomic positioning that reflect their nucleosomal origins and the chromatin landscape of their cells of origin [59]. These fragmentation patterns enable cancer detection with sensitivities surpassing mutation-based approaches, especially at low tumor fractions [59]. Multi-analyte integration combining ctDNA mutations, fragmentomics, and protein biomarkers has demonstrated particularly high sensitivity and specificity for multi-cancer early detection, with one study reporting 99% specificity at 51% sensitivity for over 50 cancer types [59].
Experimental Protocols and Methodological Considerations
Standardized Pre-Analytical Protocols for ctDNA Analysis
Reliable liquid biopsy results require stringent pre-analytical procedures to ensure analyte integrity and minimize contamination from cellular genomic DNA.
Table 4: Key Research Reagent Solutions for Liquid Biopsy Workflows
| Reagent/Category | Function | Examples/Alternatives |
|---|---|---|
| Blood Collection Tubes with Stabilizers | Preserve blood cell integrity during storage/transport | Cell-Free DNA BCT (Streck), PAXgene Blood ccfDNA (Qiagen) |
| Nucleic Acid Extraction Kits | Isolation of high-quality ctDNA from plasma | QIAamp Circulating Nucleic Acid Kit (Qiagen), Maxwell RSC ccfDNA (Promega) |
| Library Preparation Systems | Preparation of sequencing libraries from low-input DNA | KAPA HyperPrep, Illumina DNA Prep |
| Target Enrichment Panels | Hybrid capture or amplicon-based target enrichment | Illumina TSO500, Guardian, Tempus xF |
| Digital PCR Systems | Absolute quantification of rare mutations | Bio-Rad ddPCR, Thermo Fisher QuantStudio |
| Extracellular Vesicle Isolation Kits | Enrichment of exosomes and other EVs | Total Exosome Isolation reagent, exoRNeasy kit |
Blood Collection and Processing: Conventional EDTA tubes require plasma separation within 2-6 hours at 4°C to prevent leukocyte lysis and contamination of cfDNA with genomic DNA [61]. Specialty blood collection tubes containing cell-stabilizing preservatives (e.g., Streck, PAXgene) maintain sample integrity for up to 7 days at room temperature, facilitating clinical logistics [61]. Recommended blood volumes are typically 2×10 mL for single-analyte analysis, though larger volumes may be necessary for applications requiring ultra-high sensitivity such as minimal residual disease detection [61].
Plasma Processing: Double centrifugation is standard for optimal plasma preparation: an initial low-speed centrifugation (380-3,000 × g for 10 minutes) to separate plasma from blood cells, followed by high-speed centrifugation (12,000-20,000 × g for 10 minutes) to remove remaining cellular debris and platelets [61]. Plasma should be stored at -80°C if not processed immediately, with freeze-thaw cycles minimized to prevent nucleic acid degradation [61].
ctDNA Extraction: Solid-phase extraction methods using silica membranes generally yield higher quantities of ctDNA compared to magnetic bead-based approaches [61]. The QIAamp Circulating Nucleic Acid Kit demonstrates consistently high performance across multiple studies, though optimal extraction method may vary based on downstream applications [61].
Analytical Approaches for Different Biomarker Classes
CTCs: The CellSearch system remains the gold standard for CTC enumeration, employing immunomagnetic enrichment targeting EpCAM followed by immunofluorescence staining for epithelial markers and viability, with counterstaining for CD45 to exclude hematopoietic cells [56]. Emerging microfluidic platforms (e.g., CTC-iChip) enable label-free isolation based on physical properties or alternative surface markers, facilitating downstream molecular characterization [56].
ctDNA: Analytical approaches include targeted methods (ddPCR, BEAMing) for known mutations and next-generation sequencing for discovery applications or broader mutation profiling [56] [59]. Ultra-deep sequencing (>10,000× coverage) is typically required for confident detection of variants at allele frequencies below 1% [59]. Unique molecular identifiers are essential to distinguish true low-frequency variants from sequencing artifacts [59].
Exosomes/EVs: Isolation methods include ultracentrifugation, precipitation, size-exclusion chromatography, and immunoaffinity capture [57]. Downstream analysis may include nanoparticle tracking for quantification, transmission electron microscopy for morphological characterization, and protein or RNA analysis for molecular profiling [57].
Liquid biopsy technologies represent a paradigm shift in cancer management, moving from static tissue sampling to dynamic blood-based monitoring capable of capturing tumor evolution in real time. The comparative analysis presented in this guide demonstrates that each biomarker class—CTCs, ctDNA, and EVs—offers complementary strengths, with CTCs showing superior diagnostic performance in direct comparisons, while ctDNA provides exceptional versatility for monitoring tumor dynamics and targeted therapy selection [60].
The field continues to evolve rapidly, with emerging trends including the integration of multi-analyte approaches, application of artificial intelligence to complex fragmentomic and epigenomic data, and development of increasingly sensitive assays for minimal residual disease detection [59] [57]. For ovarian cancer specifically, ongoing research aims to address the critical need for improved early detection biomarkers through large-scale validation of multi-modal liquid biopsy panels that may incorporate protein markers, mutation profiles, and fragmentation patterns [40] [41].
As liquid biopsy technologies mature and standardization improves, their integration into routine clinical practice is expected to accelerate, ultimately fulfilling the promise of non-invasive dynamic monitoring to guide personalized cancer management and improve patient outcomes across the disease continuum.
Ovarian cancer remains the most lethal gynecological malignancy, largely due to late-stage diagnosis and the limited effectiveness of a one-size-fits-all treatment approach [62] [36]. The disease's biological complexity, comprising multiple subtypes with distinct molecular mechanisms, has rendered conventional chemotherapy inadequate for many patients [62]. This therapeutic challenge has catalyzed the development of precision medicine strategies, wherein companion diagnostics (CDx) serve as essential tools for identifying patients who are most likely to benefit from specific targeted therapies [63] [64]. Companion diagnostics are medically significant devices that provide information critical for the safe and effective use of corresponding therapeutic products [64] [65]. They enable clinicians to identify patients who will benefit from a particular treatment, those at increased risk for serious side effects, and to monitor treatment response for optimized therapy [63].
The evolution of CDx began in oncology with the 1998 approval of the HercepTest for identifying breast cancer patients with HER2 overexpression who would benefit from trastuzumab [64]. This landmark development established the drug-diagnostic co-development model that has since expanded across cancer types, including ovarian cancer. The regulatory landscape has subsequently evolved to accommodate more complex diagnostic approaches, including the approval of tests for group claims that can identify patients eligible for multiple therapies targeting the same biomarker [64]. The development of these essential tools involves several key stages—from biomarker discovery and validation to clinical trial assay implementation and regulatory approval—each with unique challenges and complexities that this guide will explore in the context of ovarian cancer [63].
Ovarian Cancer Biomarker Landscape: From Single Analytes to Complex Signatures
Traditional and Emerging Biomarkers
The biomarker landscape in ovarian cancer has expanded significantly beyond the conventional CA-125 (carbohydrate antigen 125) to include various molecular signatures with diagnostic, prognostic, and predictive utility. CA-125, while useful for monitoring treatment response and recurrence, lacks specificity as levels can elevate in various cancers and non-malignant conditions [36]. Human epididymis protein 4 (HE4) has emerged as a complementary biomarker with potentially superior diagnostic accuracy for distinguishing malignant from benign gynecological conditions [36]. Multi-biomarker panels and risk assessment models, such as the Risk of Ovarian Malignancy Algorithm (ROMA), which integrates CA-125 and HE4, have demonstrated improved specificity in ovarian cancer diagnosis [36].
Table 1: Established and Emerging Biomarkers in Ovarian Cancer
| Biomarker | Full Name | Source | Clinical Role | Diagnostic Utility | Prognostic Utility |
|---|---|---|---|---|---|
| CA-125 | Carbohydrate antigen 125 | Serum | Detection and monitoring | Yes | Yes |
| HE4 | Human epididymis protein 4 | Serum | Detection and diagnosis | Yes | No |
| LMTK3 | Lemur Tail Kinase 3 | Tissue | Novel therapeutic target | Under investigation | Yes [62] |
| HRDsig | Homologous Recombination Deficiency Signature | Genomic DNA | PARP inhibitor response | No | Predictive [66] |
| TMB | Tumor Mutational Burden | Genomic DNA | Immunotherapy response | No | Predictive [67] |
| MSI-H | Microsatellite Instability-High | Genomic DNA | Immunotherapy response | No | Predictive [67] |
More recently, novel targets such as Lemur Tail Kinase 3 (LMTK3) have emerged as both significant prognostic biomarkers and promising therapeutic targets in ovarian cancer [62]. Research has positioned LMTK3 as a predictor of patient outcomes and a target for treatment, with the development of TTX335o, which specifically targets cancer cells while sparing normal tissues [62]. Additionally, inflammatory biomarkers including systemic immune-inflammation index (SII), neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), and fibrinogen-to-albumin ratio (FAR) have shown diagnostic value, with combination markers demonstrating superior diagnostic capability compared to individual markers [68].
Biomarker Performance Characteristics
Table 2: Comparative Diagnostic Performance of Ovarian Cancer Biomarkers
| Biomarker/Model | AUC Value | Sensitivity | Specificity | Clinical Context |
|---|---|---|---|---|
| CA-125 | 0.70-0.85 [68] | ~80% (late-stage) [36] | Limited [36] | Monitoring, differential diagnosis |
| HE4 | 0.75-0.88 [36] | Varies | Higher than CA-125 [36] | Differential diagnosis |
| FAR (Fibrinogen-to-Albumin Ratio) | 0.795 [68] | 72.4% | 77.1% | Preoperative diagnosis |
| Six-marker inflammatory panel | 0.881 [68] | 85.1% | 77.1% | Preoperative diagnosis |
| Biomarker-enhanced ML models | >0.90 [36] | Up to 99.8% [36] | High | Early detection, classification |
The fibrinogen-to-albumin ratio (FAR) has demonstrated particularly strong diagnostic value among inflammatory-nutritional markers, with an area under the curve (AUC) of 0.795, sensitivity of 72.4%, and specificity of 77.1% at a cutoff of 0.075 [68]. However, combination approaches consistently outperform individual biomarkers. A logistic regression model incorporating six inflammatory-nutritional markers (PNI, NLR, PLR, MLR, SII, and FAR) achieved a significantly higher AUC value of 0.881 compared to any individual marker [68].
Companion Diagnostic Development Workflow
The development pathway for companion diagnostics follows a structured process from biomarker discovery through regulatory approval, with careful coordination between diagnostic and therapeutic development.
Companion Diagnostic Development Pathway
Biomarker Discovery and Validation
Companion diagnostic development begins with biomarker discovery and validation [63]. Biomarkers can be any measurable characteristic that indicates normal or pathogenic processes or predicts response to an intervention [63]. In ovarian cancer, this may include single mutated genes associated with disease state, immune markers associated with therapeutic efficacy, or complex signatures [63]. For example, LMTK3 was validated as a target on well over 700+ ovarian patient samples via a validated biobank of ovarian cancers including all stages and subtypes with prognostic data and full pathology [62]. The key biomarker identified was tied to the proposed mechanism, with molecule engineering confirming target binding and efficacy replicated by three independent labs [62].
When developing a single-gene oncology biomarker, it is ideal to have a locked biomarker definition specifying which alteration(s) constitute a "biomarker positive" result prior to enrolling patients in registrational studies [63]. For complex signature biomarkers, which provide a continuum of numerical values, establishing a cutoff for treatment eligibility is critical and can be determined through retrospective analysis of completed therapeutic studies [63].
Analytical and Clinical Validation
For a test to be considered a companion diagnostic, it must undergo rigorous evaluation to demonstrate analytical validity, clinical validity, and clinical utility [69]. Analytical validity refers to the ability of the test to accurately and reliably detect the specific biomarker of interest across various conditions [69]. Clinical validity is the proven ability of the test to predict the patient's response to treatment, while clinical utility refers to the ability of the test to improve patient outcomes through informed management decisions [69].
Before a biomarker is developed into a marketed CDx assay, it is clinically validated within a registrational study using a clinical trial assay (CTA) [63]. Optimally, the CTA will have been analytically validated within one central CLIA-validated laboratory, though multiple local tests may be used with careful evaluation of differences in cutoffs, analytical sensitivity, and accuracy [63]. Regulatory requirements for CTAs are determined based on device risk classification, with higher-risk applications requiring Investigational Device Exemption (IDE) submissions that include comprehensive validation data [63].
Technological Platforms in Companion Diagnostic Development
Evolution of Testing Modalities
The technology used in companion diagnostics has evolved significantly since the introduction of the first CDx in 1998 [64]. Early CDx assays were dominated by immunohistochemistry (IHC) and in situ hybridization (ISH) technologies [64]. By 2011, polymerase chain reaction (PCR) methods gained approval, with PCR-based platforms now representing the largest proportion of assays [64]. A significant advancement came in 2016 with the approval of the first liquid biopsy companion diagnostics, which utilize blood samples to detect somatic mutations in circulating free DNA, offering a less invasive alternative to tissue biopsies [64].
Next-generation sequencing (NGS) represents the current frontier in companion diagnostic technology, enabling multiple tests to be performed on limited amounts of tumor tissue within a rapid timeframe [64]. Comprehensive genomic profiling (CGP) via NGS allows physicians to build a comprehensive profile of a patient's cancer and requires only one sample for multiple tests, decreasing the need for repeated invasive procedures [64]. Foundation Medicine's FoundationOneCDx, approved in 2017 as the first broad companion diagnostic for cancer care, analyzes 324 cancer-related genes and has over 40 FDA-approved companion diagnostic indications for targeted therapies across multiple cancer types [69] [66].
Comparison of Diagnostic Platforms
Table 3: Companion Diagnostic Platform Comparison
| Platform | Key Features | Applications in Ovarian Cancer | Advantages | Limitations |
|---|---|---|---|---|
| Immunohistochemistry (IHC) | Protein detection in tissue | HER2, PD-L1 expression | Preserves tissue architecture, widely available | Semi-quantitative, limited multiplexing |
| PCR-based Methods | DNA/RNA amplification | Single gene mutations, fusion detection | High sensitivity, quantitative potential | Limited to known targets |
| Next-Generation Sequencing (NGS) | High-throughput DNA/RNA sequencing | Comprehensive genomic profiling, TMB, MSI | Unbiased approach, detects novel alterations | Higher cost, complex data analysis |
| Liquid Biopsy | Circulating tumor DNA analysis | Mutation detection, therapy monitoring | Minimally invasive, enables serial monitoring | Lower sensitivity for copy number changes |
Experimental Approaches in Biomarker and Companion Diagnostic Research
Research Reagent Solutions
Table 4: Essential Research Reagents for Ovarian Cancer Biomarker Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Biobank Specimens | Validated ovarian cancer biobanks (all stages/subtypes) [62] | Biomarker discovery and validation |
| Antibody-Based Reagents | IHC antibodies for LMTK3, PD-L1, HER2 | Protein expression analysis |
| PCR/NGS Assays | FoundationOneCDx, FoundationOneLiquid CDx [69] | Genomic alteration detection |
| Cell Line Models | Ovarian cancer cell lines with defined mutations | Functional validation of biomarkers |
| Animal Models | Patient-derived xenografts (PDX) | In vivo therapeutic efficacy studies |
| Analytical Tools | Random Forest, XGBoost, Neural Networks [36] | Biomarker-enhanced machine learning |
Methodological Framework for Biomarker Studies
Robust experimental design is critical for biomarker validation studies. A typical framework includes:
Patient Cohort Selection: Studies should include well-characterized patient populations with confirmed diagnoses. For example, recent ovarian cancer research included 170 individuals (87 with ovarian cancer, 83 with benign ovarian tumors) with strict inclusion/exclusion criteria [68]. Patients with infectious diseases, autoimmune disorders, severe liver or kidney issues, thrombotic conditions, other malignancies, pregnancy, or preexisting blood disorders were typically excluded [68].
Biomarker Measurement Protocols: Standardized protocols for biomarker measurement are essential. For inflammatory biomarkers, calculations include:
- FAR = fibrinogen (g/L) / albumin (g/L)
- PNI = albumin (g/L) + 5 × lymphocyte counts (10â¹/L)
- SII = platelet count (10â¹/L) × neutrophil count (10â¹/L) / lymphocyte count (10â¹/L)
- NLR = neutrophil count (10â¹/L) / lymphocyte count (10â¹/L)
- PLR = platelet count (10â¹/L) / lymphocyte count (10â¹/L)
- MLR = monocyte count (10â¹/L) / lymphocyte count (10â¹/L) [68]
Statistical Analysis Plans: Comprehensive statistical approaches include receiver operating characteristic (ROC) analysis to determine diagnostic accuracy, calculation of area under the curve (AUC), sensitivity, specificity, and positive/negative predictive values [68]. Optimal cut-off values are typically determined using Youden's index from ROC curves [68]. Multivariate logistic regression analysis assesses the combined value of multiple biomarkers, while Kaplan-Meier analysis with log-rank tests evaluates survival differences [68].
Comparative Effectiveness of Ovarian Cancer Biomarker Approaches
Performance Metrics Across Modalities
The comparative effectiveness of different biomarker approaches can be evaluated through multiple performance metrics. Biomarker-driven machine learning models significantly outperform traditional statistical methods, achieving AUC values exceeding 0.90 in diagnosing ovarian cancer and distinguishing malignant from benign tumors [36]. Ensemble methods such as Random Forest and XGBoost, and deep learning approaches such as RNNs, excel in classification accuracy (up to 99.82%), survival prediction (AUC up to 0.866), and treatment response forecasting [36].
Combining CA-125 and HE4 with additional markers such as CRP and NLR enhances specificity and sensitivity beyond either marker alone [36]. Similarly, systemic inflammatory indicators including PNI, NLR, PLR, MLR, SII, and FAR show excellent diagnostic performance for ovarian cancer, with combination approaches demonstrating superior diagnostic capability compared to individual markers [68].
Integration Pathways for Biomarker Technologies
The integration of various biomarker technologies creates a comprehensive diagnostic ecosystem that supports personalized treatment selection for ovarian cancer patients.
Multi-Modal Biomarker Integration for Ovarian Cancer
Regulatory and Implementation Considerations
Regulatory Framework
The regulatory landscape for companion diagnostics varies globally. In the United States, the FDA requires that CDx devices provide information essential for the safe and effective use of corresponding therapeutic products [64]. In the European Union, the new IVD Regulation (IVDR) (EU) 2017/746 provides a legal definition for companion diagnostics for the first time and introduces stricter clinical evidence requirements [65]. The regulation defines CDx as devices "essential for defining patients' eligibility for specific treatment with a medicinal product" by detecting treatment-specific biomarkers [65].
For clinical trial assays used in early-phase studies, regulatory requirements depend on the level of risk introduced by using the assay in the clinical trial [63]. An Investigational Device Exemption allows a medical device that has not received marketing clearance to be shipped for use in a clinical study [63]. The requirement for an IDE is determined based on how the clinical trial assay is used in the context of the clinical study and the associated risk level [63].
Clinical Implementation Challenges
Despite advancements, several challenges hinder the widespread implementation of companion diagnostics in ovarian cancer. There can be a significant disconnect between test availability and clinical access, with research showing that in oncology, it can take up to three years after the launch of a companion diagnostic to achieve sufficient laboratory coverage to provide required testing to oncologists [64]. Additional challenges include the availability of quality samples, test turnaround time, and reimbursement issues [64].
The clinical implementation landscape is further complicated by the rapid pace of biomarker discovery and the need for continuous validation. For instance, while PD-L1 expression, MSI-H status, and tumor mutational burden have emerged as potential predictors of immunotherapy response in ovarian cancer, each has limitations as a standalone biomarker [67]. This underscores the need for multi-biomarker approaches and validated algorithms that can robustly predict treatment responses across diverse patient populations.
The future of companion diagnostics in ovarian cancer lies in the integration of multi-modal data sources, including genomic, proteomic, radiomic, and clinical variables [36]. Next-generation technologies such as comprehensive genomic profiling and liquid biopsy monitoring are poised to transform ovarian cancer management by enabling dynamic assessment of treatment response and resistance mechanisms [66]. Foundation Medicine's FoundationOneMonitor, for example, is a tissue-free circulating tumor DNA monitoring test that shows promise in detecting molecular response to therapy in triple-negative breast cancer, with potential applications in ovarian cancer [66].
The successful development of companion diagnostics requires close collaboration between diagnostic developers, pharmaceutical companies, clinicians, and regulatory agencies throughout the entire process—from biomarker identification through commercial implementation [63]. As precision medicine continues to evolve, companion diagnostics will play an increasingly critical role in ensuring that ovarian cancer patients receive the most appropriate targeted therapies based on the molecular characteristics of their disease, ultimately improving survival and quality of life outcomes.
Ovarian cancer remains the most lethal gynecological malignancy, primarily due to late-stage diagnosis and the absence of reliable early detection methods [70] [71]. The high mortality rate—three times that of breast cancer despite lower incidence—underscores the urgent need for advanced diagnostic approaches [71]. High-throughput technologies, particularly mass spectrometry (MS) and next-generation sequencing (NGS), are revolutionizing ovarian cancer biomarker research by enabling comprehensive molecular profiling at unprecedented scale and precision. These platforms facilitate the discovery and validation of molecular signatures across the proteomic and genomic landscapes, moving beyond traditional single-marker approaches like CA125, which lacks adequate sensitivity and specificity for population screening [36] [3].
The comparative effectiveness of these technological platforms lies in their complementary strengths: NGS excels at identifying genetic alterations and mutations, while MS-based proteomics characterizes functional protein endpoints and their modifications [72] [73]. This guide provides a systematic comparison of MS and NGS platforms within ovarian cancer biomarker research, detailing their performance characteristics, experimental protocols, and applications for researchers, scientists, and drug development professionals seeking to implement these technologies in precision oncology initiatives.
Next-Generation Sequencing (NGS) Platforms
NGS technologies perform massive parallel sequencing of DNA or RNA, enabling comprehensive genomic profiling of ovarian tumors through targeted panels, whole exome, or whole transcriptome sequencing [72]. These platforms identify single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), gene fusions, and genomic signatures including tumor mutation burden (TMB), microsatellite instability (MSI), and homologous recombination deficiency (HRD) [72]. In ovarian cancer, NGS has revealed critical molecular subtypes, with high-grade serous ovarian carcinoma (HGSOC) characterized by ubiquitous TP53 mutations and frequent BRCA1/2 deficiencies, while low-grade serous (LGSOC), clear cell, and endometrioid subtypes demonstrate distinct mutational profiles in KRAS, BRAF, ARID1A, and PIK3CA [72].
Commercial NGS platforms vary in their technical approaches, gene coverage, and regulatory status, as shown in Table 1. Tissue-based assays generally offer more comprehensive genomic assessment, while liquid biopsy approaches analyzing circulating tumor DNA (ctDNA) provide non-invasive alternatives for mutation profiling [72]. The analytical sensitivity of these platforms for detecting variant alleles typically ranges from 1% to 5% for tissue-based tests, with liquid biopsies generally having slightly lower sensitivity due to variable ctDNA shedding [70].
Table 1: Comparison of Commercial NGS Platforms for Ovarian Cancer Profiling
| Testing Platform | Specimen Type | Genes Assessed | HRD Detection | MSI Detection | TMB Detection | FDA Approval Status |
|---|---|---|---|---|---|---|
| FoundationOne CDx | FFPE tissue | 324 | Yes | Yes | Yes | Full approval |
| CARIS MI Profile | FFPE tissue | 592 | Yes | Yes | Yes | Partial approval |
| Tempus xT | FFPE + matched normal | 648 | Yes | Yes | Yes | Pending |
| FoundationOne Liquid CDx | Peripheral blood | 324 | Yes | Yes | Yes | Approved |
| Guardant360 | Peripheral blood | 83 | Yes | Yes | Yes | Not approved |
Mass Spectrometry-Based Proteomics Platforms
Mass spectrometry technologies enable high-throughput protein identification and quantification from biological samples, including tissue, plasma, and serum [71] [74]. These platforms have emerged as powerful tools for ovarian cancer biomarker discovery and verification, overcoming limitations of antibody-based methods through unbiased protein profiling [73]. MS-based approaches can detect protein biomarkers, post-translational modifications, and pathway alterations that reflect the functional state of ovarian tumors beyond what can be inferred from genomic data alone [74].
Advanced proteomic technologies like proximity extension assay (PEA) have demonstrated particular utility in ovarian cancer research, enabling simultaneous measurement of thousands of proteins from minimal sample volumes [73]. Recent studies utilizing PEA technology analyzed 2,943 plasma proteins across independent clinical cohorts, identifying a three-protein panel (WFDC2/HE4, KRT19, RBFOX3) that achieved an AUC of 0.92 for distinguishing malignant from benign ovarian tumors, with sensitivity and specificity of 0.93 and 0.77 respectively [73]. This performance exceeds that of CA125 alone and highlights the potential of MS-based proteomics for developing precise diagnostic signatures.
Table 2: Performance Comparison of Proteomic Biomarker Panels in Ovarian Cancer Detection
| Biomarker Panel | Technology Platform | Sample Size | Sensitivity | Specificity | AUC | Stage Detection | Reference |
|---|---|---|---|---|---|---|---|
| WFDC2, KRT19, RBFOX3 | PEA Explore3072 | 350 discovery, 171 replication | 0.93 | 0.77 | 0.92 | Stage I-IV | [73] |
| EEF1G, MSLN, BCAM, TAGLN2 | ML-enhanced MS proteomics | 153 participants | N/A | N/A | 0.97 | Stage I-IV | [74] |
| CRISP3, MMP9 | ML-enhanced MS proteomics | 153 participants | N/A | N/A | 0.98 | Stage I-IV | [74] |
| CA125 alone | Immunoassay | Variable | 0.50-0.60 | 0.90 | ~0.80 | Limited early stage | [75] |
| ROMA (CA125 + HE4) | Immunoassay | Variable | 0.77-0.92 | 0.75-0.94 | 0.89-0.94 | Improved early stage | [73] |
Experimental Protocols and Workflows
NGS Wet-Lab and Bioinformatics Protocol
The standard NGS workflow for ovarian cancer biomarker research encompasses sample preparation, library construction, sequencing, and bioinformatic analysis. For tissue samples, formalin-fixed paraffin-embedded (FFPE) blocks with tumor content >20% are preferred, with DNA extraction yielding typically 50-200ng required for library preparation [72]. For liquid biopsy approaches, 2-10mL of peripheral blood is collected in cell-stabilizing tubes, with plasma separation and cell-free DNA extraction yielding sequencing-ready material [70].
Key Methodology Steps:
- DNA Extraction and Quality Control: Qubit fluorometry and fragment analyzer assessment to ensure DNA integrity
- Library Preparation: Fragmentation, end-repair, A-tailing, and adapter ligation with sample barcodes
- Target Enrichment: Hybridization capture using ovarian cancer-specific gene panels
- Sequencing: Massively parallel sequencing on Illumina platforms (typically NovaSeq 6000) to achieve >500x mean coverage
- Bioinformatic Analysis:
- Alignment to reference genome (hg38) using BWA-MEM or similar
- Variant calling with MuTect2 for SNVs and Indels, Control-FREEC for CNVs
- Annotation using Ensembl VEP and filtering against population databases
- Genomic signature calculation (TMB, MSI, HRD) using vendor-specific algorithms
The entire process from extracted DNA to variant reports typically requires 7-10 days, with analytical sensitivity for mutation detection demonstrated at 1-5% variant allele frequency for tissue and 0.1-0.5% for liquid biopsy applications [72].
NGS Analysis Workflow: Comprehensive genomic profiling from sample to clinical report
Mass Spectrometry Proteomics Protocol
MS-based proteomic analysis follows a standardized workflow with specific adaptations for ovarian cancer biomarker studies. For plasma or serum samples, high-abundance protein depletion is often performed using immunoaffinity columns to enhance detection of lower-abundance potential biomarkers [74]. Tissue samples require homogenization and protein extraction with detergent-containing buffers, followed by quantification via BCA assay.
Key Methodology Steps:
- Sample Preparation: Protein extraction, reduction, alkylation, and digestion (typically with trypsin)
- Peptide Labeling: Isobaric tagging (TMT or iTRAQ) for multiplexed quantification
- Liquid Chromatography: Nano-flow LC separation using C18 columns with 60-120min gradients
- Mass Spectrometry Analysis:
- Data-Dependent Acquisition (DDA): Orbitrap-based MS1 scanning with TopN MS2 fragmentation
- Data-Independent Acquisition (DIA): Sequential window acquisition of all fragment ions
- Data Processing:
- Database searching with MaxQuant, Proteome Discoverer, or DIA-NN
- False discovery rate (FDR) control at protein and peptide level (<1%)
- Statistical analysis for differential expression (limma, ANOVA)
- Pathway enrichment analysis (Gene Ontology, KEGG, Reactome)
For targeted verification, parallel reaction monitoring (PRM) provides highly specific quantification of candidate biomarkers with exceptional reproducibility (CVs <15%) [71]. The proximity extension assay (PEA) technology represents an alternative high-throughput approach, combining immunoassay specificity with DNA-based amplification for highly multiplexed protein quantification without traditional mass spectrometry [73].
MS Proteomics Workflow: Comprehensive protein analysis from sample to biomarker validation
Comparative Performance Data
Diagnostic Performance in Ovarian Cancer Detection
Multiple studies have directly or indirectly compared the performance of NGS and MS-derived biomarkers for ovarian cancer detection and classification. NGS approaches excel at identifying hereditary risk (BRCA1/2 mutations) and molecular subtypes with therapeutic implications, while MS-based proteomics demonstrates superior performance for direct cancer detection, particularly in early stages [72] [73].
Recent research integrating machine learning with proteomic data has identified novel biomarker combinations that significantly outperform traditional markers. A 2024 study analyzing serum proteomics datasets from 153 participants identified two biomarker panels (EEF1G+MSLN+BCAM+TAGLN2 and CRISP3+MMP9) achieving AUCs of 0.97 and 0.98 respectively, representing 59.1-60.7% improvement over CA125 alone [74]. These panels demonstrated accurate classification across all tumor stages, including early-stage disease where detection is most critical for improving survival outcomes.
NGS-based liquid biopsy approaches analyzing circulating tumor DNA (ctDNA) have shown promise for monitoring treatment response and detecting minimal residual disease. In advanced-stage HGSOC, ctDNA positivity after initial therapy correlates with worse progression-free survival (HR: 3.2; p<0.001) and overall survival (HR: 2.9; p=0.002), with approximately half of patients in clinical remission harboring molecular evidence of residual disease [2].
Analytical Performance Characteristics
The analytical performance of NGS and MS platforms differs significantly in their sensitivity, dynamic range, and reproducibility. NGS demonstrates exceptional sensitivity for DNA mutation detection, with limits of detection reaching 0.1% variant allele frequency for some liquid biopsy applications, enabling detection of minimal residual disease [70]. However, this high sensitivity comes with challenges in distinguishing true low-frequency variants from sequencing artifacts, requiring sophisticated bioinformatic filtering.
MS-based proteomics typically has higher limits of detection for low-abundance proteins but provides direct quantification of functional effectors without inference from genomic data. The dynamic range of MS platforms spans 4-5 orders of magnitude, which can be extended to 6-7 orders of magnitude through pre-fractionation or enrichment strategies [74]. Reproducibility of quantitative proteomics is generally excellent, with median coefficients of variation <15% for label-free approaches and <10% for isobaric labeling methods when proper normalization is applied [73].
Table 3: Analytical Performance Comparison of NGS and MS Platforms
| Performance Characteristic | NGS Platforms | MS Proteomics Platforms |
|---|---|---|
| Sensitivity | 0.1-5% VAF for mutations | Low ng/mL to μg/mL range for proteins |
| Dynamic Range | >5 orders of magnitude | 4-7 orders of magnitude |
| Reproducibility | >99% concordance for SNVs | 10-15% CV for quantification |
| Multiplexing Capacity | 50-600 genes per panel | 100-3000 proteins per run |
| Sample Throughput | 8-96 samples per run | 8-48 samples per week |
| Turnaround Time | 7-14 days | 3-7 days |
| Key Applications in OC | Mutation detection, HRD status, molecular subtyping | Diagnostic biomarkers, pathway activity, treatment response |
Research Reagent Solutions
Successful implementation of high-throughput technologies requires carefully selected research reagents and materials optimized for ovarian cancer studies. The following table details essential solutions for NGS and MS workflows in ovarian cancer biomarker research.
Table 4: Essential Research Reagents for Ovarian Cancer Biomarker Studies
| Reagent Category | Specific Products | Application in Ovarian Cancer Research |
|---|---|---|
| NGS Library Prep | Illumina Nextera Flex, KAPA HyperPrep | DNA library construction for mutation profiling |
| Target Enrichment | IDT xGen Pan-Cancer, Twist Oncology Panel | Capture of ovarian cancer-relevant genes |
| NGS QC Kits | Agilent Bioanalyzer/TapeStation, Qubit dsDNA HS | Quality control of input DNA and final libraries |
| Protein Digestion | Trypsin (sequencing grade), RapiGest SF | Proteolytic digestion for bottom-up proteomics |
| Peptide Labeling | TMTpro 16/18plex, iTRAQ 4/8plex | Multiplexed quantitative proteomics |
| LC-MS Columns | C18 nanoLC columns (75μm id, 25cm) | Peptide separation prior to MS analysis |
| Immunoaffinity Depletion | Agilent MARS-14, Seppro IgY14 | Depletion of high-abundance plasma proteins |
| Data Analysis Software | FoundationOne CDx, MaxQuant, DIA-NN | Bioinformatic processing of NGS and MS data |
Integration and Complementary Applications
The most powerful applications in ovarian cancer biomarker research emerge from integrating NGS and MS technologies to create comprehensive molecular portraits. NGS identifies genetic alterations and potential therapeutic targets, while MS-based proteomics verifies whether genomic alterations manifest as functional protein changes and pathway activities [72] [74]. This integrated approach is particularly valuable for assessing homologous recombination deficiency (HRD) status, where genomic scars identified by NGS can be correlated with actual DNA repair protein expression and phosphorylation status measured by MS [72].
Machine learning approaches further enhance the synergy between these platforms. A 2024 study demonstrated that ML algorithms applied to proteomic data could identify high-performing biomarker combinations for HGSOC detection that significantly outperformed existing clinical tests [74]. Similarly, AI-driven analysis of multi-omics datasets is enabling development of personalized risk prediction models that combine germline mutation status (from NGS) with protein biomarker levels (from MS) and clinical variables [36].
Spatial multi-omics represents the cutting edge of integrated technology applications, combining spatial transcriptomics with proteomic profiling within intact tissue sections. This approach preserves architectural context while measuring hundreds of molecular features simultaneously, revealing tumor heterogeneity and microenvironment interactions in ovarian cancer [2]. These advanced applications highlight how NGS and MS technologies, while powerful individually, provide transformative insights when integrated to address the complexity of ovarian cancer biology.
Mass spectrometry and next-generation sequencing platforms represent complementary pillars of modern ovarian cancer biomarker research, each with distinct strengths and applications. NGS excels at comprehensive genomic characterization, identifying hereditary risk factors, therapeutic targets, and molecular subtypes with implications for treatment selection. MS-based proteomics provides direct measurement of functional protein effectors, enabling development of highly accurate diagnostic signatures and monitoring of pathway activities. The continuing evolution of both technologies—including single-cell applications, spatial multi-omics, and AI-enhanced data analysis—promises to further advance ovarian cancer detection, classification, and treatment in the era of precision oncology. For research and clinical implementation, selection between these platforms should be guided by specific application requirements, with integrated approaches offering the most comprehensive molecular insights for addressing the challenges of this lethal disease.
Ovarian cancer remains the most lethal gynecologic malignancy, with a majority of cases diagnosed at advanced stages due to the disease's asymptomatic progression and the limitations of single-marker detection strategies [76] [36]. The high mortality rate associated with ovarian cancer underscores the critical need for improved diagnostic tools that can detect the disease earlier and with greater accuracy. For over three decades, CA-125 has served as the primary biomarker for ovarian cancer, but its limitations are well-documented, including elevated levels in benign conditions and limited sensitivity for early-stage detection [36] [75]. These diagnostic shortcomings have driven research toward multi-marker panels and sophisticated algorithmic approaches that integrate multiple biomarkers to enhance both sensitivity and specificity beyond what single markers can achieve.
The evolution from single biomarkers to integrated panels represents a paradigm shift in ovarian cancer diagnostics. By combining multiple biomarkers that capture different aspects of tumor biology, these approaches can detect a broader range of ovarian cancer subtypes while reducing false positives from benign conditions [77]. Furthermore, the integration of machine learning algorithms has enabled more sophisticated pattern recognition within complex biomarker data, leading to significant improvements in classification accuracy, risk stratification, and prediction of treatment response [36] [78]. This guide provides a comprehensive comparison of current biomarker panels and algorithmic models, supported by experimental data and methodological details to inform researchers and drug development professionals working in ovarian cancer diagnostics.
Performance Comparison of Biomarker Panels and Algorithmic Models
The following tables provide a systematic comparison of established and emerging biomarker panels and algorithmic models for ovarian cancer detection and stratification, based on recent research findings and validation studies.
Table 1: Performance Comparison of Established Biomarker Panels and Algorithms
| Panel/Algorithm Name | Biomarkers Included | Sensitivity (%) | Specificity (%) | AUC | Clinical Application |
|---|---|---|---|---|---|
| ROMA | CA-125, HE4 | 93.8 | 74.9 | 0.892 | Triage of pelvic masses [79] |
| 4-Marker Panel (MD Anderson) | CA-125, HE4, MMP-7, CA72-4 | 83.2 | 98.0 | N/R | Early detection (Stage I) [77] |
| OvarianTag | TNFRSF10C, TNFRSF10B, CASP8 | N/R | N/R | N/R | Platinum response prediction [76] |
| UKCTOCS MMS | CA-125 + ultrasound | N/R | N/R | N/R | Population screening [36] |
Table 2: Performance of Machine Learning Models in Ovarian Cancer Classification
| ML Model | Data Inputs | Accuracy (%) | AUC | Clinical Utility |
|---|---|---|---|---|
| Random Forest | 10 blood parameters | 99.82 | 0.86 | Benign vs. malignant classification [80] |
| Logistic Regression | 10 blood parameters | 78.0 | 0.95 | Pathological tissue diagnosis [80] |
| UMORSS AI System | Ultrasound + clinical data | N/R | 0.955 | Risk assessment in complex cases [81] |
| High Reliability UMORSS | Ultrasound + clinical data | N/R | 0.955 | Filtered high-certainty cases [81] |
| OvarianTag Decision Tree | Gene expression | 83.3 (platinum), 79.2 (recurrence) | N/R | Chemotherapy response prediction [76] |
N/R = Not Reported in the available sources
Detailed Methodologies of Key Experimental Studies
OvarianTag Biomarker Panel Development and Validation
The OvarianTag panel was developed through a multi-phase observational study focusing on genes involved in apoptosis and necroptosis pathways, which are crucial mechanisms in chemotherapy response [76].
Experimental Protocol:
- Phase 1 (Discovery): 45 patients were recruited, and RNA was extracted from fresh ovarian tissues (normal, benign, and malignant). qRT-PCR was performed to assess the relative expression of genes involved in apoptosis and necroptosis-regulated cell death pathways. Machine learning algorithms were applied to identify relevant prognostic markers.
- Phase 2 (Validation): 55 additional epithelial ovarian cancer (EOC) patients were included, and their formalin-fixed, paraffin-embedded (FFPE) tumor samples were analyzed using qRT-PCR. The classifier algorithm incorporated hierarchical clustering to stratify patients based on gene expression profiles.
- Key Findings: Significant differences in TNFRSF10C/TRAIL-R3, TNFRSF10B/TRAIL-R2, and CASP8 expression levels were observed between patient groups. CASP8 downregulation was strongly correlated with platinum resistance and poor prognosis. Decision tree models achieved 83.3% accuracy in predicting platinum response and 79.2% accuracy in recurrence risk stratification [76].
Validation of the 4-Marker Panel for Early Detection
A rigorous retrospective study was conducted to identify an optimal multimarker panel for early-stage ovarian cancer detection [77].
Experimental Protocol:
- Sample Collection: Pretreatment sera from 142 stage I ovarian cancer cases and 5 annual samples each from 217 healthy controls were analyzed.
- Biomarker Measurement: Researchers measured CA125, HE4, matrix metalloproteinase-7 (MMP-7), CA72-4, CA19-9, CA15-3, carcinoembryonic antigen, and soluble vascular cell adhesion molecule (sVCAM) concentrations using immunoassays.
- Statistical Analysis: After random division into training and validation sets, all possible biomarker combinations were explored exhaustively using linear classifiers to identify the panel with the greatest sensitivity for stage I disease at a high specificity of 98%. Within-person and between-person coefficient of variation (CV) were estimated to evaluate longitudinal performance.
- Key Findings: The 4-marker panel comprising CA125, HE4, MMP-7, and CA72-4 performed with the highest sensitivity (83.2%) at 98% specificity. The within-person CVs were lower for these markers compared to their corresponding between-person CV, indicating stable baselines in healthy volunteers suitable for longitudinal algorithm development [77].
UMORSS AI System Development and Validation
The Uncertainty-aware Multimodal Ovarian Risk Scoring System (UMORSS) represents a cutting-edge approach integrating ultrasound imaging with clinical data and uncertainty quantification [81].
Experimental Protocol:
- Dataset: Retrospective data from 97,013 patients who underwent ovarian ultrasound examinations was used, with strict inclusion criteria resulting in 6,931 patients with 8,800 US images for development. External validation included 421 patients from three other centers.
- Model Architecture: UMORSS employs a two-phase approach: Phase I rapidly triages low-risk lesions via initial ultrasound analysis, and Phase II provides uncertainty-aware multimodal analysis for complex cases.
- Uncertainty Quantification: A novel UQ module was developed as a streamlined bypass method that can be applied to any pre-trained model, providing quantitative assessment of prediction reliability.
- Validation: A prospective reader study (n=284 cases, six radiologists) evaluated the performance of radiologists alone, AI alone, and AI-assisted radiologists.
- Key Findings: Phase I accurately identified 68.7% of physiological cysts and 13.8% of benign tumors as low-risk with zero false negatives. Phase II achieved an AUC of 0.955 (internal testing) and 0.926 (external validation). The human-AI collaborative tool increased radiologists' average AUC by 10.58% and sensitivity by 22.48% [81].
Visualizing Experimental Workflows and Biological Pathways
OvarianTag Panel Signaling Pathways
Diagram Title: Apoptosis and Necroptosis Pathways in OvarianTag
UMORSS Two-Phase Diagnostic Workflow
Diagram Title: UMORSS Two-Phase Diagnostic Pathway
Research Reagent Solutions for Biomarker Studies
Table 3: Essential Research Reagents for Ovarian Biomarker Studies
| Reagent/Kit | Manufacturer | Primary Application | Key Features |
|---|---|---|---|
| Absolute IDQ p180 Kit | Biocrates Life Science AG | Targeted metabolomics | Quantifies 194 endogenous metabolites from 5 compound classes [44] |
| ARCHITECT CA125II Assay | Abbott | CA-125 quantification | Automated immunoassay platform with strong clinical validation [79] |
| HE4 EIA Kit | Fujirebio Diagnostics | HE4 quantification | ELISA-based detection used in ROMA algorithm development [79] |
| Biocrates MetIDQ Software | Biocrates Life Science AG | Metabolomics data analysis | Software for metabolite level quantification from mass spectrometry data [44] |
| RNA Extraction Kits | Various | Gene expression studies | RNA isolation from fresh frozen or FFPE ovarian tissues [76] |
| qRT-PCR Reagents | Various | Gene expression validation | Quantification of apoptosis/necroptosis pathway genes [76] |
The evolution from single biomarkers to integrated panels and algorithmic models represents significant progress in ovarian cancer detection and stratification. The experimental data presented in this comparison guide demonstrates that multi-marker approaches consistently outperform single biomarkers in both diagnostic accuracy and clinical utility. The integration of machine learning algorithms further enhances these panels by identifying complex patterns in high-dimensional data that escape conventional statistical methods.
Future developments in ovarian biomarker research will likely focus on several key areas: the incorporation of multi-omics data (genomics, proteomics, metabolomics), enhanced longitudinal tracking algorithms, more sophisticated uncertainty quantification in AI systems, and the development of standardized validation protocols across diverse populations. As these technologies mature, the translation of biomarker panels from research tools to clinical practice promises to significantly impact early detection, treatment selection, and ultimately, patient outcomes in ovarian cancer.
Navigating Challenges and Optimizing Biomarker Performance in Research and Clinical Settings
The early and accurate detection of ovarian cancer remains a significant challenge in clinical oncology. Traditional biomarkers, while foundational, are often hampered by limited specificity, frequently resulting in false positives and unnecessary invasive procedures. This guide provides a comparative analysis of traditional and emerging ovarian cancer biomarkers, focusing on their performance characteristics, underlying biological pathways, and the experimental protocols used in their evaluation. The objective data presented herein is intended to inform researchers and drug development professionals in their efforts to advance diagnostic strategies and develop more reliable tools for early detection.
Comparative Performance of Ovarian Cancer Biomarkers
The quest for improved ovarian cancer diagnostics has led to the evaluation of numerous biomarkers, both alone and in combination. The following table summarizes key performance metrics for several prominent biomarkers, highlighting the trade-offs between sensitivity and specificity.
Table 1: Performance Metrics of Selected Ovarian Cancer Biomarkers
| Biomarker | Reported Sensitivity (%) | Reported Specificity (%) | Key Limitations & Characteristics |
|---|---|---|---|
| CA125 (Traditional) | ~50% (Early-Stage)~80% (Late-Stage) [82] [3] | Limited; elevated in benign conditions (endometriosis, fibroids) [82] [3] | Lacks sensitivity for early-stage disease; limited specificity [82] [3] |
| HE4 | Information missing | More specific than CA125; fewer false positives in benign conditions [82] | Less likely to be elevated in non-malignant conditions [82] [3] |
| CHI3L1 (YKL-40) | 80% [3] | 70% [3] | Potential for superior diagnostic performance versus CA125 alone [3] |
| CA125 + HE4 | Increased by 21% in early-stage vs CA125 alone [82] | 90% (at stated sensitivity) [82] | Combined use improves detection rates over a single marker [82] [3] |
| CA125 + HE4 + CHI3L1 | 85.7% (up to one year pre-diagnosis) [3] | 95.4% [3] | Multi-marker models can achieve high sensitivity and specificity [3] |
Beyond the markers in Table 1, other promising biomarkers are under investigation. For instance, osteopontin levels are significantly higher in women with epithelial ovarian cancer and are associated with advanced disease and chemoresistance [82] [3]. The kallikrein family of proteins (e.g., hK10) is also overexpressed in ovarian tumors; some kallikreins can detect a fraction of CA125-negative cancers, and when combined with CA125, improve early-stage sensitivity [82]. Conversely, bikunin demonstrates that low pre-operative plasma levels are a strong unfavorable prognostic marker, associated with shorter survival [82].
Experimental Protocols for Biomarker Validation
The transition of a biomarker from a research concept to a clinically useful tool requires rigorous validation. The following methodologies are commonly employed in the field.
Serum Biomarker Assay (e.g., CA125 and HE4 ELISA)
The most common approach for quantifying protein biomarkers like CA125 and HE4 is a blood test using an enzyme-linked immunosorbent assay (ELISA) [3].
Detailed Protocol:
- Sample Collection: Collect peripheral blood samples from patients and matched controls. Allow blood to clot and then centrifuge to isolate serum or plasma. Aliquot and store frozen at -80°C until analysis.
- Antibody-Based Detection: Use a commercial ELISA kit specific for the target biomarker (e.g., CA125 or HE4). Coat a microtiter plate with a capture antibody that binds the biomarker. After blocking, add serum samples and standards in duplicate. Incubate to allow the biomarker to bind to the capture antibody.
- Detection and Quantification: Add a detection antibody conjugated to an enzyme (e.g., horseradish peroxidase). Following a wash step, add a substrate solution that produces a colorimetric change when cleaved by the enzyme. Stop the reaction and measure the absorbance of each well using a microplate reader.
- Data Analysis: Generate a standard curve from the known concentrations of the standards and use it to interpolate the concentration of the biomarker in the patient samples. Establish a cutoff value for clinical interpretation.
Mass Spectrometry-Based Proteomics for Biomarker Discovery
Advanced techniques like mass spectrometry (MS) allow for the identification of novel biomarker "fingerprints" from small samples [3].
Detailed Protocol:
- Sample Preparation: Deplete high-abundance proteins (e.g., albumin) from serum or plasma samples to enhance the detection of lower-abundance potential biomarkers. Digest the proteins into peptides using a protease like trypsin.
- Liquid Chromatography-Mass Spectrometry (LC-MS/MS): Separate the complex peptide mixture using liquid chromatography. The eluted peptides are then ionized and introduced into a tandem mass spectrometer (MS/MS).
- Data Acquisition and Analysis: The MS/MS instrument fragments the peptides and measures the mass-to-charge ratio of both the intact peptides and their fragments. The resulting spectra are compared against protein sequence databases using search engines (e.g., MaxQuant, SEQUEST) for identification. Statistical analysis is performed to find proteins that are differentially expressed between cancer and control groups.
Key Signaling Pathways and Biomarker Function
Understanding the biological context of biomarkers is crucial for interpreting their clinical significance. The following diagram illustrates the functional roles and interactions of key ovarian cancer biomarkers within the tumor microenvironment.
Diagram: Functional Roles of Key Biomarkers in Ovarian Cancer. This figure illustrates how biomarkers are secreted by tumor cells and their involvement in critical processes driving disease progression, such as metastasis (via HE4 and CHI3L1), treatment resistance (Osteopontin and CHI3L1), and modulation of the tumor microenvironment (Osteopontin).
Advancing biomarker research requires a suite of reliable reagents and tools. The following table outlines key solutions for experimental work in this field.
Table 2: Essential Research Reagent Solutions for Biomarker Investigation
| Research Reagent / Solution | Primary Function in Experimentation |
|---|---|
| Specific Antibodies (Monoclonal/Polyclonal) | Core reagents for immuno-based detection and quantification methods like ELISA and immunohistochemistry; used as capture and detection antibodies [3]. |
| Commercial ELISA Kits | Provide a standardized, optimized system for accurately measuring biomarker concentrations (e.g., CA125, HE4) in serum/plasma samples [82] [3]. |
| Mass Spectrometry Grade Enzymes (Trypsin) | For precise and efficient digestion of proteins into peptides during sample preparation for LC-MS/MS-based biomarker discovery [3]. |
| Protein Standard Panels | Used to generate calibration curves in ELISA and MS workflows, enabling the absolute quantification of target biomarkers in patient samples. |
| Cell Line Models (e.g., OVCAR, SKOV3) | Provide a controlled in vitro system to study biomarker function, regulation, and response to therapeutic compounds [82]. |
| High-Affinity Chromatography Columns | Essential for separating complex peptide or protein mixtures by liquid chromatography prior to mass spectrometry analysis [3]. |
The data and methodologies presented underscore a clear trajectory in ovarian cancer biomarker research: moving from single, imperfect markers like CA125 toward integrated, multi-analyte panels. While CA125 remains a cornerstone for monitoring therapy and recurrence, emerging biomarkers such as HE4, CHI3L1, and others offer complementary information that significantly enhances diagnostic and prognostic accuracy, especially in early-stage disease. The ongoing challenge for researchers is to standardize detection methods, validate these panels in large, prospective trials, and continue to unravel the complex biology that these biomarkers represent. The ultimate goal is a highly sensitive and specific diagnostic tool that can reliably detect ovarian cancer at its earliest and most treatable stages.
Ovarian cancer represents a formidable challenge in oncology, not as a single disease but as a collection of distinct malignancies with varying origins, molecular profiles, and clinical behaviors. This tumor heterogeneity is a primary obstacle to early detection and effective treatment, necessitating a sophisticated, biomarker-driven approach to patient management. High-grade serous ovarian carcinoma (HGSOC), the most common and aggressive subtype, accounts for approximately 70% of cases and is characterized by widespread genomic instability and frequent TP53 mutations [2] [40]. In contrast, low-grade serous ovarian cancer (LGSOC), representing 5-10% of serous carcinomas, is a slower-growing but often chemotherapy-resistant disease typically featuring mutations in the MAPK pathway genes like KRAS and BRAF [2] [40]. This review systematically compares the performance of biomarker-based strategies across ovarian cancer subtypes, providing researchers and drug development professionals with experimental data and methodologies to navigate this complex landscape.
Comparative Biomarker Performance Across Subtypes
Diagnostic, Prognostic, and Predictive Biomarkers
The clinical utility of biomarkers varies significantly across the pathological spectrum of ovarian cancer. The table below summarizes the performance characteristics of key biomarkers.
Table 1: Comparative Performance of Biomarkers Across Ovarian Cancer Subtypes
| Biomarker | Primary Subtype Utility | Clinical Role | Sensitivity/Specificity Notes | Experimental Detection |
|---|---|---|---|---|
| CA125 | All subtypes, especially HGSOC | Diagnosis, monitoring recurrence | Limited specificity for early stage; 34% sensitivity for Stage I alone [2] | ELISA [40] |
| HE4 | All subtypes | Diagnosis, especially early stage | Improves early detection to 72% sensitivity when combined with CA125 [2] | ELISA [40] |
| BRCA1/2 | HGSOC | Predictive for PARP inhibitor response | Germline or somatic mutations present in ~20% of HGSOC [83] [40] | Next-generation sequencing |
| HRD Status | HGSOC | Predictive for PARP inhibitor response | Present in approximately 50% of HGSOC [83] [40] | Genomic scar analysis |
| KRAS/BRAF | LGSOC | Diagnostic, predictive for MEK inhibitor response | Common mutations in LGSOC [2] | DNA sequencing |
| MiR-203a | Aggressive subtypes (e.g., HGSOC) | Prognostic, potential therapeutic target | Associated with chemoresistance [2] | Blood-based miRNA profiling |
Emerging Biomarkers and Technologies
Beyond established biomarkers, novel approaches show significant promise for advancing personalized care. Circulating tumor DNA (ctDNA) analysis, or "liquid biopsy," detects tumor-specific mutations in blood and has demonstrated strong prognostic value. Research shows that ctDNA positivity following initial therapy is linked to worse progression-free and overall survival in advanced HGSOC, serving as a marker for minimal residual disease [2]. Spatial transcriptomics represents another frontier, enabling researchers to map gene expression within intact tissue architecture. This technology has revealed significant multidrug resistance properties of specific cellular phenotypes in epithelial ovarian cancer, uncovering sensitivities to alternate FDA-approved drug classes [2]. Other emerging biomarkers include exosomes from ascites for monitoring cancer progression, aldehyde dehydrogenase 1 (ALDH1) as an early diagnostic and progression marker, and folate receptor alpha (FOLR1) for targeted therapy [40].
Analysis of Therapeutic Regimens and Supporting Biomarkers
Comparative Efficacy of Treatment Strategies
Network meta-analyses of randomized controlled trials provide crucial insights into the comparative effectiveness of various treatment regimens, particularly for recurrent disease. The following table summarizes efficacy findings based on Surface Under the Cumulative Ranking Curve (SUCRA) values, where higher percentages indicate better performance.
Table 2: Network Meta-Analysis of Treatment Efficacy in Advanced Recurrent Ovarian Cancer [42]
| Treatment Regimen | SUCRA Value (%) | Comparative Efficacy Interpretation |
|---|---|---|
| PARP inhibitor + Anti-angiogenic | 95.26% | Superior to all other regimens, significant survival improvement |
| Double Immunotherapy + Chemotherapy | 87.24% | Strong efficacy profile |
| PARP inhibitor monotherapy | 61.82% | Similar efficacy to anti-angiogenic regimens |
| Anti-angiogenic + Chemotherapy | 60.14% | Similar efficacy to PARP inhibitor monotherapy |
| Anti-angiogenic monotherapy | 52.30% | Similar efficacy to PARP inhibitor combinations |
| Double Immunotherapy | 36.49% | Superior to single immunotherapy |
| Immunotherapy + Chemotherapy | 31.61% | Significant improvement over chemotherapy alone |
| Single Immunotherapy | 8.53% | Limited efficacy as monotherapy |
Biomarker-Enabled Targeted Therapies
The integration of biomarkers has been particularly successful in developing targeted therapies:
- PARP Inhibitors (Olaparib, Niraparib, Rucaparib): These agents exploit synthetic lethality in tumors with homologous recombination deficiency (HRD), particularly those with BRCA1/2 mutations. In the SOLO-1 trial, PARP inhibitor maintenance therapy resulted in a 70% lower risk of disease progression in women with BRCA-mutated HGSOC [83] [40].
- MEK/FAK Inhibition (Avutometinib + Defactinib): This combination represents a breakthrough for LGSOC, which is characterized by MAPK pathway alterations. In the RAMP-201 phase II trial, the combination achieved an overall response rate of 31% in the overall LGSOC population and 44% in patients with KRAS mutations [2].
- Anti-angiogenic Agents (Bevacizumab): This VEGF inhibitor normalizes tumor vasculature, improving chemotherapeutic drug delivery. It demonstrates particular efficacy in BRCA-mutated patients when combined with platinum-based chemotherapy [42].
Experimental Protocols and Methodologies
Key Experimental Workflows
Diagram: Biomarker Discovery and Validation Workflow
Circulating Tumor DNA (ctDNA) Analysis for Minimal Residual Disease
Purpose: To detect minimal residual disease and predict recurrence in advanced-stage HGSOC through non-invasive liquid biopsy [2].
Protocol:
- Sample Collection: Collect peripheral blood in cell-free DNA collection tubes.
- Plasma Separation: Centrifuge blood at 1600 × g for 10 minutes, followed by 16,000 × g for 10 minutes to obtain platelet-poor plasma.
- DNA Extraction: Isolate cell-free DNA using commercially available kits (e.g., QIAamp Circulating Nucleic Acid Kit).
- Library Preparation & Sequencing: Prepare sequencing libraries targeting a personalized panel of 16-28 single-nucleotide variants previously identified in the patient's tumor tissue. Use hybrid capture-based next-generation sequencing.
- Bioinformatic Analysis: Sequence to a minimum depth of 100,000X. Identify tumor-derived variants using unique molecular identifiers to correct for sequencing errors and distinguish low-frequency variants.
Key Technical Considerations: This approach can detect ctDNA at variant allele frequencies as low as 0.01%. In research settings, ctDNA positivity after completion of initial therapy correlates with significantly worse progression-free survival (HR: 10.6) and overall survival (HR: 11.0) [2].
Spatial Transcriptomics for Tumor Microenvironment Analysis
Purpose: To characterize multicellular resistance phenotypes in epithelial ovarian cancer while preserving tissue architecture [2].
Protocol:
- Tissue Preparation: Section formalin-fixed paraffin-embedded (FFPE) tumor specimens at 5μm thickness.
- Histology-Directed Region Selection: Stain adjacent section with H&E to identify and mark regions of interest.
- Spatial Barcoding: Deparaffinize slides and apply oligonucleotide barcodes with spatial coordinates.
- cDNA Synthesis & Library Construction: Perform on-slide reverse transcription, followed by second-strand synthesis and amplification.
- Sequencing: Use Illumina platform for high-throughput sequencing.
- Data Integration & Clustering: Map sequencing reads to spatial barcodes. Use sophisticated statistical models to resolve distinct cell populations and their spatial relationships.
Key Technical Considerations: This methodology overcomes the computational complexity of spatial data, enabling identification of therapy-resistant niches and their specific vulnerabilities to alternative FDA-approved drug classes [2].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Ovarian Cancer Biomarker Studies
| Reagent/Category | Specific Example | Research Function |
|---|---|---|
| Cell-Free DNA Collection Tubes | Streck Cell-Free DNA BCT | Preserves blood sample integrity for ctDNA analysis by preventing genomic DNA release from white blood cells [2]. |
| Immunoassay Kits | HE4 ELISA Kit | Quantifies Human Epididymis Protein 4 levels in serum for early detection studies [40]. |
| Next-Generation Sequencing Panels | Homologous Recombination Deficiency (HRD) Panel | Detects genomic scar signatures (LOH, TAI, LST) to identify HRD-positive tumors beyond BRCA mutations [83]. |
| Spatial Transcriptomics Platforms | 10x Genomics Visium | Enables genome-wide mRNA expression mapping within morphological context of intact tissue sections [2]. |
| Primary Cell Culture Systems | Patient-Derived Organoids (PDOs) | Maintains tumor heterogeneity ex vivo for functional drug sensitivity testing and biomarker validation [2]. |
| Vinyldifluoroborane | Vinyldifluoroborane|High-Purity Reagent for Research | Vinyldifluoroborane is a specialized organoboron reagent for synthesizing fluorinated compounds in drug discovery and materials science. For Research Use Only. Not for human use. |
| Temazepam glucuronide | Temazepam glucuronide, CAS:3703-53-5, MF:C22H21ClN2O8, MW:476.9 g/mol | Chemical Reagent |
Signaling Pathways and Biomarker Mechanisms
Understanding the molecular pathways underlying ovarian cancer subtypes is essential for contextualizing biomarker function and therapeutic response.
Diagram: Key Signaling Pathways in Ovarian Cancer Subtypes
Pathway-Specific Biomarker-Therapy Relationships
MAPK/ERK Pathway in LGSOC: This pathway promotes migration and invasion, contributing to metastasis and chemoresistance. KRAS and BRAF mutations serve as both diagnostic biomarkers and predictors of response to MEK inhibitors like avutometinib [40]. The combination of avutometinib with the FAK inhibitor defactinib has demonstrated particular efficacy, causing tumor regressions in preclinical models by blocking parallel resistance pathways [2].
Homologous Recombination Pathway in HGSOC: BRCA1/2 genes are critical for DNA repair via homologous recombination. Their mutation causes genomic instability and creates vulnerability to PARP inhibitors through synthetic lethality [40]. The broader concept of homologous recombination deficiency (HRD) has expanded the population eligible for PARP inhibitor therapy beyond just BRCA mutation carriers [83].
Angiogenesis Pathway Across Subtypes: VEGF overexpression is common in ovarian cancer and serves as a biomarker for anti-angiogenic therapy. Bevacizumab, a VEGF inhibitor, demonstrates efficacy across subtypes, particularly in combination with chemotherapy or PARP inhibitors [83] [42]. The combination of olaparib and bevacizumab has demonstrated improved efficacy in HRD-positive patients [83].
The confrontation with ovarian cancer heterogeneity demands an increasingly sophisticated biomarker toolkit that aligns specific molecular features with optimized therapeutic strategies. The evidence presented demonstrates that biomarker-enabled approaches—from PARP and MEK inhibitors to immunotherapy combinations—consistently outperform conventional chemotherapy in defined patient subgroups. The future of ovarian cancer management lies in comprehensive molecular profiling that integrates genomic, transcriptomic, and proteomic data to match each patient's unique tumor biology with the most effective available therapies. As biomarker technologies continue to evolve—particularly in the realms of liquid biopsy, spatial multi-omics, and artificial intelligence-driven pathology—researchers and drug developers have an unprecedented opportunity to translate biological insights into meaningful clinical progress against this complex disease.
The translation of ovarian cancer biomarkers from discovery to clinical application has been persistently hampered by challenges in standardization and reproducibility. Despite the identification of numerous promising biomarkers, few have successfully transitioned to routine clinical practice due to inconsistent performance across validation studies [84]. The imperative for standardized methodologies becomes evident when examining the trajectory of biomarker research, where initial promising findings frequently fail to validate in independent cohorts or across different laboratories [85]. This reproducibility crisis underscores the fundamental need for rigorous assay validation protocols and cross-laboratory consistency measures to ensure that biomarker performance characteristics remain stable and transferable.
Multivariate index assays (MVIs) such as OVA1, ROMA, and Overa represent significant advances in ovarian cancer diagnostics by combining multiple biomarkers with clinical parameters [85]. However, their development has highlighted the critical importance of standardized validation pathways. These algorithms demonstrate that consistent performance requires not only technical precision in individual biomarker measurements but also standardized approaches to algorithmic interpretation and integration of clinical variables [85]. The Food and Drug Administration's (FDA) approval of these MVIs established important precedents for the level of validation rigor required for clinical implementation, creating benchmarks for subsequent biomarker development.
Experimental Protocols: Methodologies for Biomarker Validation
Proximity Extension Assay (PEA) Technology
Proximity Extension Assay (PEA) technology represents an advanced methodology for biomarker validation that combines traditional sandwich immunoassay principles with quantitative PCR detection [86]. The experimental protocol begins with sample collection, where paired serum and follicular fluid samples are obtained from participants following standardized phlebotomy and follicular aspiration procedures. Samples are immediately processed through centrifugation at 3,000 × g for 10-15 minutes, with supernatants aliquoted and stored at -80°C to maintain protein stability [86].
The core PEA procedure involves incubating samples with matched antibody pairs conjugated to DNA oligonucleotides. When these antibody pairs bind to their target protein in close proximity, the DNA tails hybridize and serve as templates for extension by DNA polymerase. The resulting DNA sequence is subsequently amplified and quantified using microfluidic quantitative PCR [86]. This methodology enables highly specific and sensitive multiplexed protein detection across 92 inflammatory biomarkers simultaneously, as demonstrated in studies of ovarian function biomarkers. The protocol incorporates multiple standardization controls including internal extension controls, inter-plate calibrators, and normalization to internal background signals to ensure cross-laboratory consistency [86].
Machine Learning-Enhanced Biomarker Discovery Workflow
Recent advances incorporate machine learning (ML) into biomarker validation workflows to enhance feature selection and model robustness. The strategic ML-based feature extraction workflow applied to high-grade serous ovarian carcinoma (HGSOC) proteomics data involves several standardized phases [74]. First, co-dysregulated proteins (CDPs) are identified from differentially expressed proteins in tissue and serum datasets using predefined statistical criteria. Next, recursive feature selection (RFS) and sequential feature selection (SFS) methods are applied to CDPs using 20% of patient samples, coupled with 5-fold cross-validation using multiple classifier algorithms including logistic regression, support vector machine, random forest, and extreme gradient boosting [74].
The validation phase employs hold-out datasets comprising 20% of patient samples not used in model training. Model performance is benchmarked against established clinical markers like CA125 and HE4 using receiver operating characteristic (ROC) analysis [74]. This workflow successfully identified novel biomarker combinations including EEF1G + MSLN + BCAM + TAGLN2 and CRISP3 + MMP9, which demonstrated superior performance to traditional markers with AUC values exceeding 0.97 [74]. Critical to reproducibility, this approach incorporates external validation using independent cohorts to verify transferability across populations.
Table 1: Key Analytical Performance Metrics for Biomarker Detection Technologies
| Technology | Sensitivity | Specificity | Multiplexing Capacity | Sample Volume | Standardization Features |
|---|---|---|---|---|---|
| Proximity Extension Assay | ~85% [28] | ~91% [28] | High (92-96 targets) [86] | Low (1-10 µL) [86] | DNA-barcoded antibodies, internal controls [86] |
| Machine Learning-Enhanced Proteomics | 77-85% [28] | 85-92% [28] | Very High (1000+ proteins) [74] | Moderate (50-100 µL) [74] | Cross-validation, feature selection algorithms [74] |
| ELISA (Traditional) | 50-62% (CA125) [87] | 73-77% (CA125) [87] | Low (single-plex) | Moderate (50-100 µL) | Standard curves, quality controls |
Diagram 1: Standardized workflow for biomarker validation assays illustrating critical control points for ensuring reproducibility.
Comparative Performance of Ovarian Cancer Biomarker Assays
Analytical Performance Across Validation Studies
Rigorous validation studies have revealed significant variability in the performance of ovarian cancer biomarker assays across different laboratories and patient populations. A comprehensive meta-analysis of artificial intelligence-derived blood biomarkers for ovarian cancer, encompassing 40 independent studies, demonstrated pooled sensitivity of 85% (95% CI 83%-87%) and specificity of 91% (95% CI 90%-92%) with an area under the curve (AUC) of 0.95 [28]. Importantly, this analysis revealed substantial performance differences based on methodology, with machine learning approaches (sensitivity=85%, specificity=92%) outperforming deep learning methods (sensitivity=77%, specificity=85%) in current implementations [28].
The type of sample matrix significantly influences assay reproducibility, with studies utilizing serum demonstrating substantially higher sensitivity (94%) and specificity (96%) compared to those using plasma (sensitivity=83%, specificity=91%) [28]. This highlights the critical importance of standardizing pre-analytical conditions. Furthermore, studies incorporating external validation showed significantly higher specificity (94% versus 89%) compared to those without external validation, though sensitivity was lower (74% versus 90%), indicating that internal validation alone may overestimate real-world performance [28].
Multivariate Index Assays: Standardization Challenges
Multivariate index assays (MVIs) face unique standardization challenges due to their incorporation of multiple biomarkers and clinical parameters. The Risk of Ovarian Malignancy Algorithm (ROMA), which integrates CA125, HE4, and menopausal status, demonstrates how algorithmic standardization complements analytical standardization. In validation studies, ROMA showed sensitivity of 95% and specificity of 83% for detecting ovarian cancer, outperforming individual biomarkers [85]. Similarly, the OVA1 assay, which combines CA125 with transthyretin, transferrin, apolipoprotein A1, and β-2 microglobulin, demonstrated sensitivity of 94% but specificity of only 54%, highlighting the trade-offs in multivariate test development [85].
The second-generation MIA (Overa) improved specificity to 69% while maintaining sensitivity by incorporating CA125, HE4, apolipoprotein A1, follicle-stimulating hormone, and transferrin [85]. These MVIs illustrate the progressive refinement of multivariate algorithms through iterative validation, though their variable performance across studies underscores the persistent challenges in standardizing complex diagnostic algorithms.
Table 2: Cross-Study Performance Comparison of Ovarian Biomarker Assays
| Assay Type | Biomarkers Included | Sensitivity Range | Specificity Range | AUC | Key Standardization Factors |
|---|---|---|---|---|---|
| Single Marker: CA125 | CA125 only | 50-62% (early stage) [87] 92% (late stage) [87] | 73-77% [87] | 0.75-0.85 | Cut-off variation (35->70 U/mL) [87] |
| Dual Marker: ROMA | CA125, HE4, menopausal status | 85-95% [85] | 83-90% [85] | 0.89-0.94 | Algorithm consistency, menopausal status criteria [85] |
| Multivariate: OVA1 | 5 biomarkers + imaging | 87-94% [85] | 54-69% [85] | 0.82-0.92 | Reference standard alignment [85] |
| ML-Enhanced Panel | EEF1G+MSLN+BCAM+TAGLN2 [74] | >90% [74] | >90% [74] | 0.97 [74] | Feature selection stability, external validation [74] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Ovarian Biomarker Validation Studies
| Reagent/Material | Function | Standardization Considerations | Representative Examples |
|---|---|---|---|
| DNA-Barcoded Antibody Pairs | Target protein recognition and signal amplification via DNA hybridization | Lot-to-lot consistency, epitope mapping validation, cross-reactivity profiling | Olink Target 96 Inflammation Panel [86] |
| Quality Control Materials | Monitoring assay performance, inter-laboratory standardization | Commutability with clinical samples, stability documentation, target value assignment | Olink Internal Extension Controls [86] |
| Algorithm Training Cohorts | Development and optimization of multivariate models | Population representativeness, pre-analytical documentation, reference standard uniformity | PLCO Cancer Screening Trial samples [84] |
| Reference Standard Materials | Establishing calibrator traceability, harmonizing across platforms | Purity characterization, matrix appropriateness, stability data | NIST Standard Reference Materials |
| Cross-Validation Cohorts | Assessing model generalizability and preventing overfitting | Independent collection protocols, demographic diversity, blinding procedures | Independent serum proteomics datasets [74] |
| DBCO-PEG4-TFP ester | DBCO-PEG4-TFP Ester|Heterobifunctional Crosslinker | Bench Chemicals | |
| Dimethylchlorophosphite | Dimethylchlorophosphite, CAS:3743-07-5, MF:C2H6ClO2P, MW:128.49 g/mol | Chemical Reagent | Bench Chemicals |
Diagram 2: Critical standardization components for cross-laboratory consistency in ovarian biomarker research.
The establishment of standardized protocols and validation frameworks represents the most critical pathway toward improving reproducibility in ovarian cancer biomarker research. The evidence reviewed demonstrates that consistency in pre-analytical processing, analytical measurement, and post-analytical interpretation collectively determine the translational potential of biomarker discoveries [84] [85] [28]. The growing incorporation of machine learning approaches necessitates even more rigorous standardization, as algorithmic models must demonstrate stability across diverse populations and healthcare settings [36] [74].
Future directions for the field should prioritize the development of reference materials for emerging biomarkers, standardized protocols for multivariate algorithm validation, and guidelines for external validation requirements prior to clinical implementation. Additionally, the establishment of consortium-based initiatives for cross-laboratory method verification would significantly advance the field. Only through such comprehensive standardization efforts can the promise of ovarian cancer biomarkers for early detection and improved patient outcomes be fully realized [84] [85] [28].
Platinum-based chemotherapy and Poly (ADP-ribose) polymerase inhibitors (PARPi) represent cornerstone treatments for high-grade serous ovarian cancer (HGSOC). Their efficacy is deeply rooted in exploiting DNA damage response (DDR) pathways, particularly homologous recombination (HR) repair. Synthetic lethality, where PARPi selectively kill cells with pre-existing HR deficiencies (HRD) like BRCA1/2 mutations, has been a transformative concept in oncology [88]. However, a majority of patients ultimately develop resistance to both platinum agents and PARPi, leading to disease recurrence and poor survival outcomes [89] [90]. In fact, 40-70% of patients develop resistance to PARPi, presenting a major clinical challenge [89]. Overcoming this resistance hinges on a detailed molecular understanding of its mechanisms and the development of robust biomarkers to guide patient stratification and therapeutic strategies. This guide provides a comparative analysis of the biomarker landscape, enabling researchers and drug development professionals to navigate the complexities of therapy resistance.
Mechanisms of Resistance: A Shared Landscape
Resistance to platinum and PARPi is complex and interrelated, often involving the restoration of DNA repair capacity or alterations in drug target engagement. The table below summarizes the primary resistance mechanisms.
Table 1: Key Mechanisms of Resistance to Platinum Chemotherapy and PARP Inhibitors
| Resistance Mechanism | Impact on Platinum | Impact on PARPi | Key Molecular Alterations |
|---|---|---|---|
| Restoration of HR Repair | Reduces accumulation of lethal DSBs | Overcomes synthetic lethality by repairing PARPi-induced DSBs | BRCA1/2 reversion mutations; upregulation of HR genes (RAD51, BRCA1) [90] |
| Replication Fork Protection | Enhances replication tolerance to platinum adducts | Prevents replication fork collapse and DSB formation | Loss of fork destabilizers (e.g., PTIP, CHD4); upregulation of fork protection factors [88] [90] |
| Alterations in Drug Targets | Not directly applicable | Reduces PARP trapping on DNA; maintains BER activity | Reduction in PARP1 protein levels or mutations in PARP1 that prevent trapping [89] [90] |
| Upregulation of Drug Efflux Pumps | Increases cellular export of platinum drugs | Increases cellular export of PARPi | Overexpression of P-glycoprotein and other transmembrane transporters [90] |
| Tumour Microenvironment Alterations | Impacts drug delivery and survival signaling | Influences immune response and cellular survival | Changes in immune cell infiltration, cytokine release, and angiogenic factors [90] |
The following diagram illustrates how these mechanisms enable cancer cells to survive the DNA damage induced by platinum and PARPi therapy.
Comparative Analysis of Predictive Biomarkers
Biomarkers for predicting response and resistance can be categorized into genomic, functional, and emerging integrative types. Each offers distinct advantages and limitations for clinical and research applications.
Table 2: Comparative Analysis of Biomarkers for PARPi and Platinum Response
| Biomarker Category | Specific Marker | Predicts PARPi Response | Predicts Platinum Response | Methodology | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| Genomic | BRCA1/2 mutations | Strong predictor of sensitivity [88] | Strong predictor of sensitivity [91] | NGS of germline/tumour DNA | Strong validation; clear biological rationale | Does not capture all HRD tumours; reversion mutations cause resistance [90] |
| Genomic Scar | HRD Scores (e.g., LOH, TAI, LST) | Predicts sensitivity in clinical trials [21] | Correlates with sensitivity [91] | Genomic profiling (NGS/SNP array) | Captures historical HRD regardless of cause | "Scars" persist after HR restoration, poor for dynamic resistance [92] |
| Functional | RAD51 nuclear foci | Functional readout of HR capacity; low foci predict sensitivity [93] | Functional readout of HR capacity; predicts response [93] | IF on tumour tissue post-ex vivo irradiation | Directly measures functional HR status; real-time assessment | Requires viable tumour tissue and ex vivo culture; not yet routine [91] |
| Gene Expression | SLFN11 | Emerging sensitive biomarker [21] | Emerging sensitive biomarker | RNA-seq, qPCR | Potential for IHC application; mechanistic link to replication stress | Requires further large-scale validation [21] |
| Epigenetic | HOXA9 methylation | Emerging resistant biomarker [21] | Not established | Methylation-specific PCR, bisulfite sequencing | Potential for liquid biopsy application | Requires further large-scale validation [21] |
Experimental Protocols for Key Biomarker Assays
RAD51 Foci Formation Assay (Functional HR Capacity)
This functional assay directly measures a tumour's ability to perform the critical step of RAD51 recruitment during HR repair.
- 1. Sample Preparation: Use fresh tumour tissue or patient-derived organoids (PDOs). Alternatively, formalin-fixed paraffin-embedded (FFPE) tissue sections can be used [93].
- 2. Ex Vivo Irradiation: Irradiate samples with a defined DNA damage dose (e.g., 5-10 Gy) to induce DSBs. Include a non-irradiated control.
- 3. Immunofluorescence (IF) Staining: Fix, permeabilize, and stain samples with antibodies against γH2AX (a marker of DSBs) and RAD51. Use fluorescently labelled secondary antibodies.
- 4. Imaging and Quantification: Acquire high-resolution confocal microscopy images. Score the number of RAD51 foci co-localizing with γH2AX foci in at least 50 nuclei.
- 5. Interpretation: A high number of RAD51 foci indicates proficient HR and predicts resistance. A low number indicates HR deficiency and predicts sensitivity to PARPi and platinum [93] [91].
The workflow for this functional assay is outlined below.
Computational Identification of Biomarkers from Genetic Interactions
This in silico protocol uses public pharmacogenomic datasets to identify novel sensitive and resistant biomarkers.
- 1. Data Acquisition: Download data from CRISPR/Cas9 and RNAi screens (e.g., DepMap) to identify gene knockouts that affect cell viability. Obtain PARPi response data (IC50/AUC) from resources like GDSC and CTRP [94].
- 2. Analysis of Genetic Interactions (GIs):
- Synthetic Lethality (SL): Identify genes where mutation combined with PARP1/2/3 knockdown significantly reduces cell viability. These are candidate sensitive biomarkers.
- Synthetic Viability (SV): Identify genes where mutation combined with PARP1/2/3 knockdown significantly enhances cell viability. These are candidate resistant biomarkers [94].
- 3. Statistical Validation: Use non-parametric tests (e.g., Wilcoxon rank-sum) to confirm that cell lines with mutations in candidate genes have significantly different PARPi IC50/AUC values versus wild-type lines.
- 4. Biological Validation: Correlate candidate biomarkers with known HR pathway activity, e.g., by analyzing expression of RAD51, BRCA2 in mutated vs. wild-type tumours from TCGA [94].
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and their applications in the study of PARPi and platinum resistance.
Table 3: Key Research Reagent Solutions for Resistance Biomarker Studies
| Reagent / Solution | Function in Research | Example Application |
|---|---|---|
| Validated PARP Inhibitors | Small-molecule inhibitors for in vitro and in vivo studies | Olaparib, Rucaparib, Niraparib, Talazoparib for dose-response assays [88] |
| Anti-RAD51 Antibody | Detects formation of RAD51 nuclear foci, a key step in HR | Primary antibody for IF-based functional HR capacity assays [93] |
| Anti-γH2AX Antibody | Detects DNA double-strand breaks (DSBs) | Co-staining with RAD51 to confirm DNA damage sites in IF assays [93] |
| Patient-Derived Organoids (PDOs) | 3D ex vivo models that retain tumour heterogeneity and genetics | Functional drug testing and biomarker validation in a clinically relevant model [21] |
| CRISPR/Cas9 Gene Editing Systems | For targeted knockout of candidate genes to validate function | Validating the role of a candidate resistant gene (e.g., TRIP12) in conferring PARPi resistance [94] |
| circulating tumour DNA (ctDNA) Kits | For isolation and analysis of tumour DNA from blood plasma | Monitoring for BRCA reversion mutations as a mechanism of acquired resistance [89] [91] |
| (3r)-Abiraterone acetate | (3r)-Abiraterone acetate, MF:C26H33NO2, MW:391.5 g/mol | Chemical Reagent |
The relentless challenge of therapy resistance in ovarian cancer necessitates a move beyond single, static biomarkers. While BRCA status and genomic scar-based HRD scores are currently the best-validated predictors for initial response, they fail to dynamically capture the evolution of resistance. The future lies in integrative biomarker approaches that combine multiple data types [91]. Functional assays like RAD51 foci offer a real-time snapshot of HR proficiency and hold great promise for better patient stratification. Furthermore, the use of ctDNA for liquid biopsies enables minimally invasive monitoring of clonal evolution and the emergence of resistance mechanisms, such as BRCA reversion mutations [89]. For researchers, the focus must be on validating novel biomarkers like SLFN11 and HOXA9 methylation in large prospective cohorts and developing standardized, accessible functional assays. Ultimately, overcoming resistance will require a deep molecular understanding of each tumour's unique adaptive pathways, guiding the rational combination of PARPi and platinum with novel agents such as ATR, WEE1, or immune checkpoint inhibitors to preempt or reverse treatment failure.
Ovarian cancer (OC) remains the most lethal gynecological malignancy, largely due to the diagnostic challenge of detecting the disease at an early, more treatable stage [36]. The pursuit of effective biomarkers is central to overcoming this challenge, yet the analytical pathway from discovery to clinical application is fraught with methodological hurdles. The complex heterogeneity of ovarian cancer, encompassing distinct histopathological subtypes such as high-grade serous carcinoma (HGSC), low-grade serous carcinoma (LGSC), endometrioid carcinoma (EC), clear cell carcinoma (CCC), and mucinous carcinoma (MC), further complicates this pursuit [38]. Researchers are increasingly turning to high-dimensional multi-omics data and sophisticated machine learning (ML) algorithms to identify novel biomarkers and develop predictive models [95]. While these approaches offer unprecedented power for pattern recognition, they simultaneously introduce significant analytical challenges in data integration, model overfitting, and validation that must be addressed to ensure scientific rigor and clinical translatability. This guide objectively compares the performance of various analytical approaches within ovarian cancer biomarker research, providing a framework for evaluating methodological robustness across studies.
Data Integration in Multi-Omics Biomarker Studies
The integration of diverse molecular data types—genomics, transcriptomics, proteomics, and metabolomics—represents a powerful frontier in ovarian cancer biomarker discovery. Multi-omics approaches provide a systems-level view of tumor biology, enabling the identification of comprehensive biomarker signatures that reflect the complexity of the disease [95]. However, the technical and analytical challenges of integrating these heterogeneous datasets are substantial.
Integration Methodologies and Comparative Performance
Different computational strategies have been developed to integrate multi-omics data, each with distinct strengths and applications. A recent systematic integration of 51 multi-omics publications identified 1,649 potential ovarian cancer biomarkers, highlighting both the promise and the challenge of extracting meaningful signals from such vast datasets [95]. The study revealed that multi-omics studies are more promising than mono-omics-based approaches, but also face significant reproducibility issues due to heterogeneity in data sources, differences in data acquisition protocols, and a lack of uniform analytical standards.
Table 1: Comparative Analysis of Multi-Omics Data Integration Techniques in Ovarian Cancer Research
| Integration Method | Underlying Principle | Reported Applications in OC | Key Advantages | Identified Limitations |
|---|---|---|---|---|
| PINSPlus [95] | Integrative subtype discovery | DNA methylation + gene expression data integration | Identified novel OC subtypes with distinct survival outcomes and therapeutic vulnerabilities | Limited validation in independent cohorts |
| CIMLR [95] | Multi-kernel learning | Multi-omics data from HGSC | Identified a high-risk subgroup characterized by dysregulated immune pathways and poor prognosis | Computational complexity may limit accessibility |
| iCluF [95] | Clustering fusion | Copy number variation, methylation, and RNA-Seq data | Discovered a chemoresistant subgroup with elevated BRCA2 methylation and HRD | Requires high-quality data from multiple platforms |
| Subtype-GAIN [95] | Imputation and clustering | Multi-omics data with missing values | Identified a stromal-rich subtype associated with ECM remodeling and worse overall survival | Performance dependent on pattern of missingness |
| Joint Dimensionality Reduction [95] | Factor analysis | Identifying key biological processes | Effective for identifying associations with clinical features | May oversimplify complex biological interactions |
Experimental Protocols for Multi-Omics Integration
A representative protocol for multi-omics biomarker discovery, as implemented in a 2025 study, involves several key stages [95]:
- Sample Preparation and Data Generation: Tumor and control samples are subjected to parallel molecular profiling. This typically includes RNA sequencing for transcriptomics, mass spectrometry or immunoassays for proteomics, and liquid chromatography-mass spectrometry (LC-MS) for metabolomics and lipidomics [96].
- Data Preprocessing and Normalization: Each datatype is processed independently using platform-specific pipelines. For RNA-seq, this includes quality control, adapter trimming, alignment, and gene-level quantification. For mass spectrometry data, peak detection, alignment, and normalization are performed.
- Batch Effect Correction: The "Sva" R package or similar tools are used to merge datasets from different sources or batches, correcting for technical variation that could confound biological signals [97].
- Integrative Analysis: The normalized multi-omics data layers are integrated using one of the computational methods outlined in Table 1. The choice of method depends on the research objective—for disease subtyping, clustering methods like PINSPlus are preferred, while for predictive modeling, regression-based approaches may be more suitable [95].
- Validation: Findings must be validated using independent technical methods (e.g., qPCR for RNA-seq hits, immunohistochemistry for proteomic hits) and in independent patient cohorts to ensure robustness [38].
Diagram 1: Multi-omics data integration workflow for ovarian cancer biomarker discovery.
The Challenge of Overfitting in Machine Learning Models
Overfitting occurs when a model learns not only the underlying patterns in the training data but also the noise and random fluctuations, resulting in poor performance when applied to new, unseen data. In ovarian cancer research, where datasets often have a high number of features (genes, proteins, etc.) relative to the number of patient samples, the risk of overfitting is particularly acute.
Comparative Performance of ML Algorithms
Multiple studies have evaluated machine learning algorithms for ovarian cancer biomarker discovery and diagnosis, with performance varying significantly based on the dataset and feature selection methods used.
Table 2: Performance Comparison of Machine Learning Algorithms in Ovarian Cancer Diagnostic Studies
| Study & Context | Best Performing Algorithm(s) | Reported AUC | Key Biomarkers/Features | Overfitting Mitigation Strategies |
|---|---|---|---|---|
| Biomarker-Enhanced ML Review [36] | Ensemble Methods (Random Forest, XGBoost), Deep Learning (RNNs) | 0.90-0.99 | CA-125, HE4, CRP, NLR | Emphasis on external validation; Analysis of learning curves |
| AOA Dx Multi-Omic Platform [96] | Proprietary ML Algorithm | 0.92 (All-stage), 0.89 (Early-stage) | Lipids, Gangliosides, Proteins | Independent training (n=NA) and testing (n=1,000) cohorts |
| Diagnostic Model (5-Gene Signature) [97] | Logistic Regression | 0.93 | CD24, CLEC4M, SOX17, ADH1C, CHRDL1 | 10-fold cross-validation; Train-validation split (70:30) |
| CA125 and Age-Based Model (Ovatools) [98] | Logistic Regression | 0.95 (≥50 years), 0.89 (<50 years) | CA125, Age | Large external validation cohort (n=342,278) |
A 2025 review of biomarker-enhanced ML for ovarian cancer reported that ensemble methods like Random Forest and XGBoost, as well as deep learning approaches, could achieve exceptional classification accuracy (up to 99.82%) and AUC values exceeding 0.90 in diagnosing OC and distinguishing malignant from benign tumors [36]. However, the review cautioned that such high performance in initial studies is often tempered by limitations such as small sample sizes and a lack of external validation, which are hallmarks of potential overfitting [36].
Experimental Protocols for Mitigating Overfitting
The following experimental protocols are critical for identifying and preventing overfitting in ovarian cancer biomarker models:
- Data Splitting: The dataset is randomly partitioned into a training set (typically 70-80%) for model development and a hold-out test set (20-30%) for final evaluation. This provides an unbiased assessment of model performance [97].
- Cross-Validation: Within the training set, k-fold cross-validation (e.g., 10-fold) is employed. The data is split into k subsets, and the model is trained k times, each time using a different fold as the validation set and the remaining folds for training. This maximizes the use of available data for both training and validation [97].
- Regularization Techniques: Algorithms like LASSO (Least Absolute Shrinkage and Selection Operator) regression introduce a penalty term to the model's loss function, which shrinks coefficient values and can drive less important feature coefficients to zero, effectively performing feature selection and reducing model complexity [97].
- Feature Selection: Dimensionality reduction is achieved through methods like the F-test (to identify features with the most significant differences between groups) combined with correlation analysis (to remove highly correlated, redundant features) [97].
- Performance Monitoring: Learning curves (plots of model performance on the training and validation sets against the amount of training data) are analyzed. A growing gap between training and validation performance indicates overfitting [97].
Diagram 2: Model training and validation workflow to prevent overfitting.
Validation Frameworks for Robust Biomarker Evaluation
Robust validation is the cornerstone of credible biomarker research. It ensures that a model's predictive performance is genuine and generalizable beyond the specific dataset used for its creation.
Comparative Performance in Internal vs. External Validation
The performance gap between internal validation (using data from the same source) and external validation (using data from a different population or institution) is a critical metric for assessing a model's real-world applicability.
Table 3: Levels of Validation in Ovarian Cancer Biomarker Studies
| Validation Level | Description | Typical Performance Drop | Exemplar Study |
|---|---|---|---|
| Apparent Validation | Performance on the same data used for training | High risk of overfitting; Not recommended | N/A |
| Internal Validation | Cross-validation or bootstrap resampling within a single dataset | Minimal drop if properly executed | 10-fold cross-validation in 5-gene model [97] |
| External Temporal Validation | Model applied to new patients from the same institution collected at a later time | Moderate drop expected | N/A |
| External Geographical Validation | Model applied to patient data from a different clinical site or region | Significant drop often observed | AOA Dx: Training (Colorado) vs. Testing (Manchester) cohorts [96] |
| External Broad Validation | Large-scale validation in a diverse, representative population | Reveals true generalizability | Ovatools validation in 342,278 women from English primary care [98] |
The 2025 external validation study of the Ovatools model (which uses CA125 and age) in a population of 342,278 women from English primary care represents a gold standard in validation practice. The model maintained an AUC of 0.95 in women ≥50 years, demonstrating exceptional generalizability when validated on a massive, independent, real-world dataset [98]. Similarly, AOA Dx's AI-powered blood test demonstrated the importance of geographical validation. Their model, trained on samples from the University of Colorado, maintained an AUC of 0.92 for ovarian cancer detection when tested on an independent, prospectively collected cohort from The University of Manchester, indicating robust performance across different populations [96].
Experimental Protocols for External Validation
A robust external validation protocol involves:
- Fully Independent Cohorts: The validation cohort must be collected from different centers or time periods than the training cohort, with no patient overlap [96] [98].
- Protocol Standardization: While the data is independent, the laboratory protocols for biomarker measurement (e.g., LC-MS for lipids, immunoassays for proteins) should be standardized across sites to ensure consistency [96].
- Blinded Analysis: The validation should be performed blinded to the patient outcomes to prevent conscious or unconscious bias in the analysis.
- Comparison to Standard of Care: The new model's performance should be directly compared to existing standards (e.g., the CA125 ≥35 U/ml threshold) using metrics like AUC, sensitivity, specificity, and positive predictive value [98].
- Clinical Utility Assessment: Beyond statistical performance, the potential clinical impact should be evaluated. For example, the Ovatools study estimated how a two-threshold pathway could effectively triage women for ultrasound or urgent cancer referral [98].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following reagents, algorithms, and databases are fundamental to conducting rigorous ovarian cancer biomarker research.
Table 4: Essential Research Reagent Solutions for Biomarker Discovery and Validation
| Reagent / Solution | Function / Application | Exemplar Use in Context |
|---|---|---|
| Liquid Chromatography-Mass Spectrometry (LC-MS) | Detection and quantification of lipids, gangliosides, and metabolites from blood samples. | Used in AOA Dx's platform for multi-omic biomarker discovery [96]. |
| STRAND Bioinformatics Database | Provides access to multi-omics data from ovarian cancer studies for re-analysis and meta-analysis. | Serves as a resource for systematizing potential biomarkers [95]. |
| LASSO Regression | A regularization technique that performs variable selection to prevent overfitting in high-dimensional data. | Used for feature selection in diagnostic model development [97]. |
| R Package 'sva' | Contains tools for removing batch effects and normalizing data from different genomic studies. | Used to merge multiple ovarian cancer gene expression datasets [97]. |
| Circulating Tumor DNA (ctDNA) Assays | A "liquid biopsy" method to analyze tumor-specific mutations in cell-free DNA from blood for monitoring recurrence. | Used to detect minimal residual disease and predict prognosis in HGSC [2]. |
| Anti-SOX17 Antibody | Validates the protein expression of a key gene identified in transcriptomic analyses. | Used for Western blot analysis to confirm SOX17 protein levels in OC cell lines [97]. |
| Gene Expression Omnibus (GEO) | A public repository of high-throughput genomic data sets used for discovery and validation. | Source of 426 tissue RNA-seq samples for diagnostic model development [97]. |
The comparative analysis of analytical approaches in ovarian biomarker research reveals a clear hierarchy of evidence. While complex multi-omics integrations and sophisticated machine learning algorithms can generate high-performing models in initial studies [36] [95], their ultimate value is determined by the rigor of validation. The most promising models are those that demonstrate robust performance across large, geographically diverse external validation cohorts [96] [98]. The persistent analytical hurdles of data integration, overfitting, and validation are not merely technical obstacles but fundamental aspects of biomarker development that must be systematically addressed. Future progress will depend on increased data standardization, collaborative sharing of well-annotated datasets, and a commitment to transparent reporting of model performance at all validation stages. By adhering to these rigorous analytical frameworks, researchers can translate the promise of biomarkers into tangible improvements in the early detection and management of ovarian cancer.
Optimizing Cut-off Values and Interpretation for Different Patient Populations and Clinical Contexts
The high mortality rate of ovarian cancer is largely attributable to late-stage diagnosis and the frequent development of chemoresistance, underscoring the critical need for precise diagnostic and prognostic biomarkers [76] [99]. While established biomarkers like CA125 and HE4 have long been foundational in clinical practice, their limitations in sensitivity and specificity have driven the discovery of novel molecular signatures and algorithmic approaches [100] [101]. The comparative effectiveness of these biomarkers is highly dependent on their optimized application across diverse patient populations and specific clinical scenarios, such as distinguishing benign from malignant pelvic masses, predicting chemotherapy response, or detecting early-stage disease [76] [101]. This guide objectively compares the performance of emerging biomarkers against traditional alternatives, providing researchers and drug development professionals with a synthesized analysis of experimental data to inform future research and clinical application.
Comparative Performance of Biomarker Panels and Algorithms
The diagnostic and prognostic landscape for ovarian cancer has evolved from single-marker tests to multi-analyte panels and complex algorithms that integrate gene expression, protein biomarkers, and clinical data. The tables below summarize the performance data of established and emerging biomarkers from recent studies.
Table 1: Performance Comparison of Diagnostic Biomarkers and Algorithms
| Biomarker/Algorithm | Sensitivity (%) | Specificity (%) | AUC/Accuracy | Key Clinical Context |
|---|---|---|---|---|
| OCS (sEV CA125, HE4, C5a) [101] | 95.4 | 90.4 | N/A | Detection of EOC in patients with adnexal masses |
| 5-Gene Model (Logistic Regression) [99] | N/A | N/A | AUC: 0.93, Acc: 87.5% | Diagnostic model (CD24, CLEC4M, SOX17, ADH1C, CHRDL1) |
| CA125 Alone [101] | Lower than OCS | Lower than OCS | N/A | Inferior to OCS in multicenter study |
| CA125 + HE4 (Machine Learning) [2] | 72 (Stage I) | N/A | N/A | Early-stage detection (vs. 34% for CA125 alone) |
| 14-Gene Model (Machine Learning) [102] | N/A | N/A | Acc: 89.5% | Diagnostic model (HOXB2, FOLR1, NEK2, etc.) |
| Lipidomics/Proteomics Model [2] | N/A | N/A | Acc: 88% | Distinguishing early-stage OC from other conditions |
Table 2: Performance of Prognostic and Predictive Biomarkers
| Biomarker/Panel | Prediction Target | Performance/Outcome | Patient Population |
|---|---|---|---|
| OvarianTag Panel [76] | Platinum chemotherapy response | 83.3% accuracy | EOC patients |
| OvarianTag Panel [76] | Tumor recurrence risk | 79.2% accuracy | EOC patients |
| PPP2R1A mutation [103] | Immunotherapy survival benefit | Median OS: 66.9 vs. 9.2 months | Ovarian Clear Cell Carcinoma |
| CASP8 downregulation [76] | Platinum resistance & poor prognosis | Strong correlation | EOC patients |
| Immune Subtype (IMM/C2) [104] | Reduced benefit from Bevacizumab | Shorter PFS | Advanced EOC |
| Mesenchymal Subtype (MES/C1) [104] | Better-than-expected prognosis with BEV | Median PFS: 29-37 months | Advanced EOC (HGSOC) |
The Ovarian Cancer Score (OCS), which integrates small extracellular vesicle (sEV) proteins (CA125, HE4, and C5a), demonstrates a superior profile for diagnosing epithelial ovarian cancer (EOC) compared to CA125 alone, maintaining high sensitivity and specificity across menopausal status and FIGO stages [101]. Its high sensitivity for early-stage (FIGO I) disease is a significant advancement [101]. Meanwhile, machine learning models leveraging gene expression signatures are showing robust diagnostic capabilities. A 5-gene model developed via logistic regression achieved an AUC of 0.93, while a separate 14-gene model reported 89.5% accuracy [99] [102].
For predicting therapeutic response, the OvarianTag panel, which analyzes apoptosis and necroptosis pathways, can stratify patients by platinum response and recurrence risk with high accuracy [76]. Furthermore, specific genetic alterations are emerging as powerful predictive biomarkers. For instance, PPP2R1A mutations in ovarian clear cell carcinoma are linked to a dramatic improvement in overall survival following immunotherapy, suggesting their potential as a biomarker for patient selection [103]. Similarly, molecular subtyping can inform treatment efficacy; the immune-related molecular subtype (IMM/C2) is associated with shorter progression-free survival in bevacizumab-treated patients, indicating it may help identify patients less likely to benefit from this anti-angiogenic therapy [104].
Experimental Protocols for Key Biomarker Studies
OvarianTag Biomarker Panel Development
The OvarianTag panel was developed to predict chemotherapy benefit and disease progression in EOC patients by integrating genes from apoptosis and necroptosis pathways [76].
- Study Phases and Samples: The observational study was conducted in two phases. The first discovery phase recruited 45 patients, with RNA extracted from fresh ovarian tissues (normal, benign, and malignant). The second validation phase included 55 additional EOC patients, using RNA from formalin-fixed, paraffin-embedded (FFPE) tumor samples [76].
- Gene Expression Analysis: RNA was extracted from all tissues. Quantitative reverse transcription PCR (qRT-PCR) was performed to assess the relative expression of genes involved in apoptosis and necroptosis-regulated cell death pathways. Specific genes analyzed included TNFRSF10C/TRAIL-R3, TNFRSF10B/TRAIL-R2, and CASP8 [76].
- Data Analysis and Model Building: Machine learning algorithms were applied to the gene expression data to identify relevant prognostic markers. The classifier algorithm incorporated hierarchical clustering to stratify patients based on their gene expression profiles. Decision tree models were built to predict platinum response and recurrence risk [76].
Multicenter Validation of the Ovarian Cancer Score (OCS)
This study aimed to validate the performance of a serum sEV protein-based score for detecting ovarian cancer [101].
- Patient Cohort: This multicenter study included 1183 adult females with adnexal masses from four hospitals. The majority of samples were prospectively collected, with a subset from biobanks. All serum samples were obtained before surgery [101].
- sEV Protein Quantification: Serum levels of sEV-derived CA125, HE4, and C5a were quantified using chemiluminescence immunoassay. The concentrations of these three proteins were then used to calculate the OCS [101].
- Statistical Analysis: The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of the OCS were calculated for diagnosing ovarian cancer. Performance was evaluated across the entire cohort and in subgroups based on menopausal status and FIGO stage [101].
Identification of a Diagnostic Gene Model via Machine Learning
This study aimed to develop a robust diagnostic model for ovarian cancer by identifying a key gene signature [99].
- Data Acquisition and Pre-processing: Six ovarian cancer microarray datasets were retrieved from the Gene Expression Omnibus (GEO) repository, comprising 352 tumor and 74 non-tumor tissues. The datasets were merged, and batch effects were corrected using the R package "Sva" [99].
- Differential Expression and Feature Selection: Differentially expressed genes were identified using the R package "Limma" with a cutoff of |log2 fold change| > 2 and an adjusted p-value < 0.05. A tiered analytical approach combining F-test, LASSO regression, and Pearson correlation was used for diagnostic feature selection, identifying five key genes (CD24, CLEC4M, SOX17, ADH1C, CHRDL1) [99].
- Machine Learning Model Development and Validation: The cohort was partitioned into stratified training (70%) and validation (30%) subsets. Eleven distinct machine learning algorithms were evaluated through iterative 10-fold cross-validation. Model performance was quantified using receiver operating characteristic (ROC) analysis, precision-recall (PR) metrics, calibration curves, and decision curve analysis [99].
Signaling Pathways and Experimental Workflows
The following diagrams visualize key signaling pathways implicated in the biomarkers discussed and the general workflow for developing a machine learning-based diagnostic model.
OvarianTag Biomarker Pathways
Diagram 1: OvarianTag Apoptosis/Necroptosis Pathway. This diagram illustrates the extrinsic apoptosis pathway targeted by the OvarianTag panel. Key genes like TRAIL-R2 promote caspase-8 (CASP8) activation, leading to apoptosis. The decoy receptor TRAIL-R3 can inhibit this pathway. Downregulation of CASP8 shunts cell death towards necroptosis and is strongly correlated with platinum resistance and poor prognosis [76].
Diagnostic Model Development Workflow
Diagram 2: Machine Learning Diagnostic Model Workflow. This chart outlines the standard workflow for developing a machine learning-based diagnostic model for ovarian cancer, as employed in recent studies [99] [102]. The process begins with integrating multiple gene expression datasets, followed by rigorous pre-processing and identification of differentially expressed genes. Key features are selected before training multiple machine learning algorithms, which are evaluated and validated to identify the final, optimal model.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Ovarian Biomarker Research & Development
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Formalin-Fixed Paraffin-Embedded (FFPE) Tissue | Preserved tissue source for retrospective RNA/DNA analysis. | Validation phase gene expression analysis in OvarianTag study [76]. |
| qRT-PCR Assays | Quantify relative mRNA expression of target genes. | Assessing expression of apoptosis/necroptosis genes (e.g., CASP8) [76]. |
| Chemiluminescence Immunoassay Kits | Precisely quantify specific protein concentrations in serum. | Measuring sEV CA125, HE4, and C5a levels for OCS calculation [101]. |
| siRNAs (Small Interfering RNAs) | Knock down gene expression in vitro to study gene function. | Validating the oncogenic role of SOX17 in OC cell lines [99]. |
| CIBERSORTx Algorithm | Computational tool to infer immune cell composition from bulk RNA data. | Characterizing tumor immune microenvironment in bevacizumab-treated patients [104]. |
| Multiplex Immunofluorescence (MIF) | Simultaneously detect multiple biomarkers on a single tissue section. | Spatial analysis of immune cell infiltration in tumor and stromal compartments [104]. |
Comparative Effectiveness and Evidence-Based Validation of Biomarker Strategies
In the field of ovarian cancer research, the transition from biomarker discovery to clinical application requires robust and standardized evaluation frameworks. Biomarkers—objectively measurable indicators of biological processes—hold the potential to revolutionize early detection, prognosis, and personalized treatment strategies for this deadly disease [105] [106]. However, not all biomarkers achieve clinical utility, necessitating a systematic approach to evaluate their validity across a hierarchy of evidence levels (LOE). The National Institutes of Health Biomarkers Definitions Working Group defines a biomarker as "a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention" [106]. This definition underscores the fundamental role biomarkers play in connecting biological insights with clinical decision-making.
The clinical utility of a biomarker refers to the degree to which its use improves patient outcomes, clinical decisions, and healthcare utilization [107]. For ovarian cancer, where symptoms are often non-specific and late-stage diagnosis is common, the development of biomarkers with high clinical utility is particularly critical. The establishment of a structured hierarchy of evidence, from initial discovery (LOE I) to clinical validation (LOE IV), provides researchers and drug development professionals with a clear pathway for biomarker development and a standardized method for assessing the maturity and reliability of biomarker evidence. This framework is essential for distinguishing truly impactful biomarkers from numerous candidates, ultimately guiding investment in development and supporting regulatory approvals [108].
Hierarchies of Evidence: From Discovery to Clinical Application
The validation pathway for biomarkers follows a structured hierarchy of evidence, with each level building upon the previous to establish clinical utility. This systematic progression ensures that only biomarkers with robust and reproducible performance advance to clinical practice. The table below outlines this hierarchical framework.
Table 1: Evidence Levels for Biomarker Clinical Utility Assessment
| Evidence Level | Primary Focus | Study Design & Key Methodologies | Outcome Measures |
|---|---|---|---|
| LOE I: Discovery & Analytical Validation | Initial identification and technical performance assessment. | Mass spectrometry, NGS, microarray, ELISA; precision, accuracy, sensitivity, specificity, and reproducibility testing. | Proof of detectability, reliable measurement within defined parameters, and establishment of initial analytical performance. |
| LOE II: Clinical Validation | Establishing association with clinical phenotype or outcome. | Case-control, prospective cohort studies; ROC curve analysis, determination of sensitivity, specificity, and AUC. | Confirmed statistical association with a clinical endpoint (e.g., diagnosis, stage, prognosis). |
| LOE III: Clinical Utility | Demonstrating improvement in patient management and outcomes. | Randomized controlled trials (RCTs), clinical utility index (PCUT/NCUT) assessment, impact on decision-making. | Evidence that using the biomarker leads to better patient outcomes, more efficient resource use, or optimized treatment decisions. |
| LOE IV: Implementation & Real-World Impact | Assessing effectiveness and utilization in routine care. | Real-world evidence (RWE) studies, health economic analyses, clinical practice guideline adoption. | Demonstrated effectiveness in diverse populations, cost-effectiveness, and integration into standard clinical pathways. |
Level I: Discovery and Analytical Validation
The foundation of the evidence hierarchy begins with the discovery of a candidate biomarker and the rigorous analytical validation of the assay used to measure it. This initial stage focuses on proving that the biomarker can be detected and measured reliably, accurately, and reproducibly in a specific biological matrix [105] [109]. For ovarian cancer, relevant matrices include plasma, serum, tissue, or ascites fluid. Key parameters established at this stage include the assay's sensitivity (ability to correctly identify true positives), specificity (ability to correctly identify true negatives), precision, and accuracy [110]. Advanced multi-omics technologies are accelerating this discovery phase, with platforms like single-cell sequencing, high-throughput proteomics, and mass spectrometry generating comprehensive molecular profiles [109]. The establishment of a reliable and validated assay is a prerequisite for all subsequent clinical studies; without analytical validation, clinical findings cannot be trusted.
Level II: Clinical Validation
Once analytical performance is established, the biomarker must undergo clinical validation to confirm its association with a specific clinical endpoint. This phase answers the question: Does the biomarker level consistently correlate with the clinical state of interest? Study designs at this level often include case-control or prospective cohort studies that evaluate the biomarker's ability to distinguish, for example, ovarian cancer patients from healthy controls or those with benign ovarian conditions [105]. Performance is quantitatively assessed using Receiver Operating Characteristic (ROC) curve analysis, which plots sensitivity against 1-specificity across all possible biomarker cut-off values. The area under the ROC curve (AUC) provides a single metric of discriminatory power, where 1.0 represents perfect discrimination and 0.5 represents no better than chance [107]. For ovarian cancer, this is where biomarkers like CA-125 and the OVA1 panel demonstrated their diagnostic capability, though often with limitations in specificity that highlight the need for further development [105].
Level III: Clinical Utility
Clinical validation alone is insufficient to justify routine clinical use. The third evidence level requires demonstration of clinical utility—proof that using the biomarker to guide decisions actually improves patient outcomes, changes management in a beneficial way, or optimizes resource allocation compared to standard care without biomarker testing [107]. The most robust evidence for clinical utility comes from randomized controlled trials (RCTs), where patient outcomes are compared between a biomarker-guided arm and a control arm. An emerging quantitative framework for assessing utility involves calculating a clinical utility index, which integrates diagnostic accuracy with the consequences of clinical decisions. This index includes Positive Clinical Utility (PCUT = Sensitivity × PPV) and Negative Clinical Utility (NCUT = Specificity × NPV), with the total utility score being the sum of PCUT and NCUT [107]. For a predictive biomarker in ovarian cancer, such as HRD status predicting response to PARP inhibitors, clinical utility is demonstrated when its use leads to improved progression-free or overall survival by selecting the right patients for the right therapy [111].
Level IV: Implementation and Real-World Impact
The final level of evidence assesses the biomarker's performance and impact in real-world clinical practice, outside the controlled environment of clinical trials. This post-implementation phase evaluates generalizability across diverse populations, cost-effectiveness, and integration into standard clinical pathways, often reflected by inclusion in clinical practice guidelines [112] [109]. Real-world evidence (RWE) studies use data from electronic health records, registries, and other sources to monitor the biomarker's long-term performance and identify any implementation challenges. The recent clinical practice guideline from the Alzheimer's Association for blood-based biomarkers, which specifies performance thresholds (e.g., ≥90% sensitivity and specificity) for use in specialized care, is a prime example of a biomarker class reaching LOE IV in another disease area [112]. For ovarian cancer, a biomarker achieves this level when it becomes a standard, reimbursed test that is widely adopted and consistently improves care pathways on a population health level.
Comparative Analysis of Ovarian Cancer Biomarkers Across Evidence Levels
Ovarian cancer biomarkers exist at various stages of validation, providing a practical landscape for applying the hierarchy of evidence. The following table compares key ovarian cancer biomarkers based on their current evidence level and demonstrated clinical applications.
Table 2: Comparative Evidence Levels and Utility of Select Ovarian Cancer Biomarkers
| Biomarker / Test | Evidence Level | Clinical Application & Context of Use | Key Performance Data | Limitations & Gaps |
|---|---|---|---|---|
| CA-125 (Cancer Antigen 125) | LOE III - IV | Diagnosis, monitoring treatment response, and detecting recurrence. | Moderate sensitivity (~80% for advanced stage), but limited specificity; can be elevated in endometriosis, pregnancy, and other benign conditions [105]. | Lacks specificity for early detection and screening; not a stand-alone test for diagnosis [105]. |
| OVA1 (Multimarker Panel) | LOE III | Triage for assessing malignancy risk in an adnexal mass; aids in referral to a gynecologic oncologist [105]. | FDA-approved; measures five protein biomarkers (e.g., CA-125, transthyretin, apolipoprotein A1) to calculate a malignancy risk score [105]. | Not a screening or diagnostic test; used for pre-surgical risk stratification. |
| Circulating Tumor DNA (ctDNA) / Liquid Biopsy | LOE II - III | Detection of tumor-specific mutations (e.g., TP53), monitoring treatment response via ctDNA tumor fraction, and identifying minimal residual disease [105] [111]. | ctDNA tumor fraction is an independent prognostic biomarker; associated with worse clinical outcomes. High specificity for tumor-derived variants [111]. | Sensitivity can be limited in low-shed tumors; requires further validation in interventional trials for clinical utility in guiding therapy. |
| HRD (Homologous Recombination Deficiency) Signature | LOE III | Predictive biomarker for response to PARP inhibitor therapy; helps identify patients most likely to benefit from targeted treatment [111]. | Foundation Medicine's HRDsig (a genomic "scar" signature) shows clinical validity and utility as a pan-tumor biomarker for PARPi benefit [111]. | Standardization of testing methods and scoring criteria across platforms is needed. |
Methodological Toolkit for Biomarker Evaluation
Experimental Workflows for Biomarker Validation
A standardized experimental protocol is essential for generating reliable, comparable data across studies. The following diagram illustrates a generalized workflow for the development and validation of a novel biomarker from discovery through to clinical utility assessment.
Determining Clinically Relevant Cut-Points
Selecting the optimal cut-point for a continuous biomarker is a critical step that balances diagnostic accuracy with clinical consequences. While traditional methods like maximizing the Youden index (Sensitivity + Specificity - 1) focus on diagnostic accuracy, clinical utility-based methods are increasingly important for decision-makers [107]. These methods incorporate the clinical outcomes of diagnostic decisions.
The core of this approach involves calculating the Clinical Utility Index, which combines diagnostic accuracy with predictive values:
- Positive Clinical Utility (PCUT): Sensitivity × Positive Predictive Value (PPV)
- Negative Clinical Utility (NCUT): Specificity × Negative Predictive Value (NPV)
Several criteria can then be used to select the optimal cut-point:
- Maximize Total Utility (YBCUT): Maximize (PCUT + NCUT)
- Maximize Product (PBCUT): Maximize (PCUT × NCUT)
- Minimize Utility Imbalance (UBCUT): Minimize |PCUT - AUC| + |NCUT - AUC|
- Align with 2xAUC (ADTCUT): Minimize |(PCUT + NCUT) - 2×AUC|
The choice of method can lead to different optimal cut-points, especially at low disease prevalence or with low AUC values, highlighting the need to align the statistical approach with the clinical context of use [107].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Biomarker Development
| Tool / Reagent Category | Specific Examples | Primary Function in Biomarker Research |
|---|---|---|
| High-Throughput Sequencing | Next-Generation Sequencing (NGS) panels, Whole Genome/Exome Sequencing. | Comprehensive genomic profiling to identify somatic mutations, fusion genes, and copy number alterations (e.g., in HRD genes) [105] [111]. |
| Proteomic & Immunoassay Platforms | Mass Spectrometry, ELISA, Multiplex Immunoassays (e.g., OVA1 panel). | Quantification of protein biomarker levels from blood, tissue, or other biofluids. Critical for validating protein signatures [105] [109]. |
| Liquid Biopsy & ctDNA Analysis | FoundationOneCDx, Guardian360, In-house ctDNA NGS assays. | Non-invasive isolation and analysis of circulating tumor DNA (ctDNA) for mutation detection, monitoring tumor fraction, and tracking minimal residual disease [111]. |
| Bioinformatic & AI Analytics | Machine Learning Algorithms, HRDsig computational signature, Clinical Utility Index calculators. | Analysis of complex genomic and proteomic datasets; identification of hidden patterns; development of predictive signatures and determination of optimal biomarker cut-points [111] [107] [109]. |
The structured hierarchy of evidence—from analytical validation (LOE I) to real-world impact (LOE IV)—provides an indispensable roadmap for translating promising ovarian biomarker discoveries into clinically useful tools. This review demonstrates that while several biomarkers, including CA-125 and the OVA1 panel, have achieved varying levels of clinical integration, the field is rapidly evolving with emerging biomarkers like ctDNA and genomic signatures such as HRD. The rigorous application of this framework, coupled with robust methodological approaches for clinical utility assessment and cut-point selection, is paramount for advancing the field. It ensures that resources are directed toward biomarkers that truly improve early detection, prognostic stratification, and personalized therapy for ovarian cancer patients, ultimately fulfilling the promise of precision oncology. Future efforts must focus on standardizing assays, validating biomarkers in prospective interventional trials, and generating real-world evidence to solidify their role in clinical practice and guidelines.
The high mortality rate associated with ovarian cancer is primarily driven by late-stage diagnosis, underscoring the critical need for highly accurate diagnostic tools [113]. For decades, single protein biomarkers, most notably CA125, have formed the cornerstone of ovarian cancer detection and management in clinical practice [41]. However, the inherent biological complexity and heterogeneity of ovarian cancer limit the diagnostic performance of any single biomarker [114]. This analytical review provides a direct comparative assessment of the diagnostic accuracy of single biomarkers against multi-marker panels, synthesizing current evidence to demonstrate that multi-analyte approaches significantly enhance clinical utility for researchers and drug development professionals. The shift from single biomarkers to multiplexed panels represents a paradigm change in diagnostic strategy, mirroring the trend in therapeutic development toward combination therapies that target multiple molecular pathways simultaneously [113].
Comparative Performance Metrics: Single Biomarkers vs. Multi-Marker Panels
Quantitative Analysis of Diagnostic Accuracy
Table 1: Diagnostic performance of single biomarkers versus multi-marker panels in ovarian cancer detection
| Biomarker Type | Specific Biomarkers | Sensitivity (%) | Specificity (%) | AUC | Cohort Size | Reference |
|---|---|---|---|---|---|---|
| Single Biomarker | CA125 | ~50 (Early Stage) | Variable (Influenced by benign conditions) | Not Reported | N/A | [41] |
| Single Biomarker | CA153 | 64.35 | Not Reported | Not Reported | 101 | [115] |
| Multi-Marker Panel | CA125 + CA153 | 96.30 | Not Reported | Not Reported | 108 | [115] |
| Multi-Marker Panel | CA125, HE4, IL6, CXCL10 (active/total) | 95 | 95 | Not Reported | 334 | [116] |
| Multi-Omic Platform | Lipids, Gangliosides, Proteins (AI-powered) | Not Reported | Not Reported | 0.89-0.92 (Early Stage) | ~1,000 | [96] |
Contextualizing Performance Across Cancer Types
The superior performance of multi-marker panels is consistent across different cancer types, suggesting a universal principle in oncologic diagnostics. A comprehensive systematic review and meta-analysis of pancreatic ductal adenocarcinoma (PDAC) biomarkers demonstrated that the pooled AUC value for all multi-biomarker panels (AUC = 0.898) was significantly higher than all single biomarkers (AUC = 0.803; P < 0.0001) [114]. Similarly, in colorectal cancer, a pilot study showed that a combination of four blood-based biomarkers (mSEPT9, IGFBP2, DKK3, and PKM2) achieved an AUC of 74.4%, outperforming all individual biomarkers except IGFBP2 alone [117]. This consistent pattern across disparate malignancies reinforces the fundamental diagnostic advantage of panel-based approaches.
Experimental Protocols for Key Studies
Protocol 1: CXCL10-Based Multi-Marker Panel Development
Objective: Develop and validate a multi-marker panel for discriminating benign from malignant adnexal masses [116] [118].
Sample Collection: Retrospectively collected EDTA-chelated plasma samples from 334 patients (bio-banked specimens) undergoing surgery for suspected gynecological malignancies. Patients were excluded if they were <18 years, had recent cancer history, received recent chemo/radio/immunotherapy, or were immunocompromised.
Biomarker Measurement:
- CXCL10 Active Ratio ELISA: Performed as previously described [116], measuring both active and total CXCL10 to calculate the "active ratio."
- Luminex Magnetic Bead Immunoassay: Used for IL-6 and HE4 quantification according to manufacturer protocols (Thermo Fisher).
- CA125: Measured using standard clinical platforms.
Statistical Analysis and Model Building:
- Data transformation using Yeo–Johnson method
- Linear discriminant analysis to identify analytes with greatest linear separation between groups
- Multivariate logistic regression model fitted to transformed data
- Model performance estimated using repeated stratified K-fold cross-validation (4 folds × 5 repeats)
- Final model refit to entire dataset (n = 334)
- Cutoff point determined by Youden's J index
Validation: Performance compared against established scoring systems (CA125, RMI, ROMA) using published cutoff values.
Protocol 2: AI-Powered Multi-Omic Platform Validation
Objective: Validate an AI-powered multi-omic platform for ovarian cancer detection in symptomatic women [96].
Study Design: Two independent studies on clinically similar populations.
- Cohort 1 (Model Training): Samples from CU Anschutz Ovarian Cancer Innovations Group
- Cohort 2 (Independent Testing): Prospectively collected symptomatic samples from The University of Manchester
Sample Analysis:
- Platform Technology: Integration of lipid, ganglioside, and protein biomarkers from small blood samples
- Analytical Techniques: Liquid chromatography mass spectrometry (LC-MS) and immunoassays
- Data Integration: Machine learning algorithms to analyze complex multi-omic datasets
Performance Assessment:
- AUC calculations for distinguishing all stages of ovarian cancer from controls
- Separate analysis for early-stage (stage I/II) disease
- Cross-validation between independent cohorts
Signaling Pathways and Biomarker Relationships
Diagram 1: Biomarker signaling pathways and diagnostic integration in ovarian cancer. This diagram illustrates how multiple biomarkers originating from different cellular sources in the tumor microenvironment provide complementary information that is integrated in multi-marker panels for enhanced diagnostic accuracy compared to single-biomarker approaches.
Advantages of Multi-Marker Panels in Clinical Decision-Making
1Comprehensive Biological Capture
Multi-marker panels address the molecular heterogeneity of ovarian cancer by simultaneously measuring biomarkers from distinct biological pathways, including inflammation (IL-6, CXCL10), protease inhibition (HE4), and mucin proteins (CA125, CA153) [116] [115]. This approach acknowledges that ovarian cancer is not a single disease but rather a collection of distinct molecular subtypes with varying biological characteristics and clinical behaviors.
2Enhanced Early-Stage Detection
The combination of CXCL10, IL-6, CA125, and HE4 correctly identified 80% of stage I-II cancers in a retrospective cohort [116], addressing a critical clinical need where current single biomarkers like CA125 detect only approximately 50% of early-stage cases [41]. This improved early detection capability is further demonstrated by an AI-powered multi-omic platform that maintained an AUC of 0.89 for early-stage disease in an independent testing set [96].
3Improved Differentiation from Benign Conditions
Multi-marker panels significantly reduce false positives by leveraging multiple independent biomarkers that collectively improve specificity. The CXCL10-based panel achieved 95% specificity in differentiating malignant from benign disease, substantially outperforming CA125 alone, which is known to elevate in various benign conditions such as endometriosis and normal menstrual cycles [116] [41].
4Independent Predictive Value
Certain biomarkers in multi-analyte panels provide diagnostic information independent of traditional markers. The CXCL10 "active ratio" measurement was largely independent of cancer stage and menopausal status, providing orthogonal diagnostic value that complements existing biomarkers [116]. Similarly, the combination of CA125 and CA153 achieved significantly higher sensitivity (96.3%) than either biomarker alone [115].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key research reagents and materials for ovarian cancer biomarker studies
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| EDTA-Chelated Plasma Samples | Biomarker source material; preserves protein stability | Collected from bio-banked specimens; centrifuged at 16,000× g [116] |
| CXCL10 Active Ratio ELISA | Measures active and total CXCL10 forms | Custom antibodies against intact/total CXCL10; full-length protein standard [116] |
| Luminex Magnetic Bead Kits | Multiplexed protein quantification | Thermo Fisher cat# RDSLXSAHM05 (IL-6, HE4) [116] |
| Epi proColon 2.0 CE Test | Methylated SEPT9 detection | Polymedco Inc. (M5-02-001, M5-02-002, M5-02-003) [117] |
| Liquid Chromatography Mass Spectrometry (LC-MS) | Multi-omic biomarker discovery | Lipid, ganglioside, and protein analysis from blood samples [96] |
The cumulative evidence from recent studies unequivocally demonstrates that multi-marker panels significantly outperform single biomarkers in ovarian cancer diagnosis. The diagnostic superiority of panel-based approaches, evidenced by improvements in sensitivity, specificity, and AUC values, stems from their ability to capture the complex, multifactorial biology of ovarian cancer. For researchers and drug development professionals, these findings highlight the necessity of pursuing multi-analyte strategies in both diagnostic development and clinical trial design. Future directions should focus on standardizing analytical protocols, validating panels in diverse populations, and integrating novel biomarker classes with traditional protein markers to further enhance diagnostic precision. The transition from single biomarkers to comprehensive multi-marker panels represents the most promising pathway toward achieving the long-sought goal of early and accurate ovarian cancer detection.
The management of advanced ovarian cancer has been transformed by the advent of poly(ADP-ribose) polymerase inhibitors (PARPi), which exploit the principle of synthetic lethality in homologous recombination repair (HRR)-deficient cells [119]. The efficacy of these targeted therapies is intrinsically linked to the presence of specific molecular biomarkers, with BRCA1/2 mutations and homologous recombination deficiency (HRD) status serving as the primary predictive biomarkers for patient selection [21] [120]. As PARPi move into frontline maintenance settings and combination strategies with anti-angiogenics and immunotherapy emerge, understanding the comparative performance of these biomarkers becomes crucial for optimizing treatment outcomes [121] [122].
This guide provides a systematic comparison of BRCA/HRD biomarker performance for PARPi in ovarian cancer, contextualized within the broader framework of biomarker-driven oncology research. We evaluate analytical methodologies, clinical validation data, and emerging biomarkers that may refine patient stratification beyond current standards.
Biomarker Performance and Clinical Validation
Established Biomarkers for PARP Inhibitor Response
BRCA Mutations (germline and somatic) represent the best-validated predictive biomarkers for PARPi efficacy. Tumors with these mutations exhibit profound HRD, creating dependency on PARP-mediated DNA repair pathways [21] [119].
Homologous Recombination Deficiency (HRD) encompasses a broader spectrum of tumors with defective HRR, including both BRCA-mutated and BRCA-wildtype cases. HRD status is typically determined through genomic scarring patterns or mutational signatures [119].
Table 1: Clinical Performance of Established PARPi Biomarkers in First-Line Maintenance Therapy
| Biomarker Status | PARP Inhibitor | Trial | Median PFS (months) | Hazard Ratio (95% CI) | Overall Survival Benefit |
|---|---|---|---|---|---|
| BRCA mutation | Olaparib | SOLO1 | 56.0 vs. 13.8 (placebo) | 0.33 (0.25-0.43) | 7-year OS: 67% vs. 46.5% [121] |
| BRCA mutation | Olaparib + Bevacizumab | PAOLA-1 | NR | Significant in subgroup | Significant in subgroup [121] |
| HRD-positive (including BRCA) | Olaparib + Bevacizumab | PAOLA-1 | 37.2 vs. 17.7 (bev only) | 0.57 (0.43-0.76) | Improvement in lower-risk group [121] |
| HRD-positive | Niraparib | PRIMA | 11.5 vs. 8.3 (placebo) | 0.68 (0.49-0.94) | No significant difference [121] |
| HRP/HRD-negative | Olaparib + Bevacizumab | PAOLA-1 | 16.9 vs. 16.0 (bev only) | 0.92 (0.76-1.12) | Not significant [121] |
| HRP/HRD-negative | Niraparib | PRIMA | 8.1 vs. 5.4 (placebo) | 0.68 (0.49-0.94) | 5-year OS: 29% vs. 27% [121] |
Table 2: Biomarker Prevalence and Assay Methodologies in Ovarian Cancer
| Biomarker | Prevalence in Ovarian Cancer | Primary Detection Methods | Regulatory Status | Key Limitations |
|---|---|---|---|---|
| Germline BRCA1/2 mutations | 20% of EOC cases [21] | NGS of blood/saliva | FDA-approved companion diagnostics | Misses somatic mutations |
| Somatic BRCA1/2 mutations | ~2-3% (additional) [21] | NGS of tumor tissue | FDA-approved companion diagnostics | Tumor purity requirements |
| HRD (genomic scarring) | 41.4% across all histologic types [21] | LOH/TAI/LST scoring (MyChoiceCDx) | FDA-approved as companion diagnostic | Historical scar may not reflect current HR status |
| HRD (mutational signatures) | 24-44% by WGS/WES [123] | Whole genome/exome sequencing | Laboratory-developed tests | Cost and computational complexity |
Biomarker-Stratified Outcomes in Clinical Trials
Long-term follow-up from pivotal trials demonstrates that biomarker status significantly impacts the magnitude of benefit from PARPi therapy:
- SOLO1 (Olaparib maintenance): After 7 years of follow-up, patients with BRCA mutations maintained a remarkable overall survival (OS) advantage (67% vs. 46.5% with placebo), representing a 45% reduction in mortality risk [121].
- PAOLA-1 (Olaparib + Bevacizumab): OS benefit was confined to the HRD-positive population, particularly those with BRCA mutations. In HRD-negative patients, the addition of olaparib provided no significant OS benefit (HR 0.92, 95% CI 0.76-1.12) [121].
- PRIMA (Niraparib): While progression-free survival (PFS) benefit was observed across biomarker subgroups, mature OS data showed no significant improvement in the HRD-positive population, highlighting the complex relationship between PFS and OS gains in different trial contexts [121].
These findings have prompted regulatory refinements, including the recent FDA limitation of niraparib indication to HRD-positive patients only, reflecting evolving risk-benefit assessments based on biomarker status [121].
Experimental Approaches for Biomarker Evaluation
HRD Assessment Methodologies
Genomic Scarring Analysis The most established approach quantifies three genomic instability signatures:
- Loss of Heterozygosity (LOH): Genomic regions with loss of one parental allele
- Telomeric Allelic Imbalance (TAI): Allelic imbalance extending to telomeric regions
- Large-Scale State Transitions (LST): Chromosomal breaks between adjacent regions of at least 10Mb
A composite HRD score (typically ≥42 or ≥39, depending on the assay) indicates HRD-positive status [119] [124]. This approach captures historical HRD but may not reflect current functional status due to persistent genomic scars even after HRR restoration [92].
Next-Generation Sequencing-Based HRD Assessment The OncoWES-HRD assay exemplifies integrated approaches, combining:
- Targeted capture of 1,021 cancer-associated genes and 150kb HRD-score probe panel
- Simultaneous assessment of BRCA1/2 mutations and genomic instability markers
- LASSO regression modeling to generate predictive risk scores for PARPi response [124]
This methodology demonstrated superior predictive performance compared to HRD score alone, with significantly longer PFS in high-risk score patients (p<0.05) in both training and test cohorts [124].
Emerging Biomarker Detection Platforms
Genomic Methylation Sequencing (GM-seq) The Chinese HRD Harmonization Project developed a bisulfite-free TET enzyme-mediated sequencing pipeline that simultaneously detects genetic and epigenetic alterations:
Diagram Title: GM-seq Integrated Analysis Workflow
This approach identified distinct PARPi efficacy patterns based on HRD etiology: BRCA1/2 LOH group had the best outcomes (median PFS undefined), followed by BRCA1 methylation group (median PFS 23.4 months), and unknown HRD etiology group (median PFS 8.8 months; p<0.001) [125].
Functional HRD Assays Nuclear RAD51 foci formation serves as a functional readout of HRR capacity. This assay measures RAD51 recruitment to DNA damage sites, providing real-time assessment of HRR functionality independent of genomic scars [21].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Biomarker Investigation
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| DNA Extraction Kits | ReliaPrep FFPE gDNA Miniprep System [125] | Isolate high-quality DNA from archived specimens | DNA quality categorization (A-D) based on quantity and integrity |
| Targeted Capture Panels | 1021+HRD custom probes [125] | Simultaneous mutation profiling and HRD scoring | Covers 1.5Mb cancer genes + 150kb genome-wide HRD regions |
| Library Prep Kits | KAPA DNA Library Preparation Kit [125], Hieff NGS Ultima Pro DNA Library Prep Kit [125] | NGS library construction for genetic and methylation analysis | Compatibility with TET-oxidized DNA for GM-seq |
| Methylation Conversion Reagents | TET2 oxidase, pyridine borane [125] | Bisulfite-free methylation profiling | Preserves DNA integrity vs. traditional bisulfite treatment |
| Sequencing Platforms | Gene+seq2000 sequencer [125] | High-throughput sequencing | 2×101bp paired-end recommended for HRD analysis |
| Primary Antibodies | Anti-human DPP4 rabbit IgG [126], Anti-Granzyme B [126] | IHC analysis of novel biomarkers | Validation in FFPE tissues required |
| Analysis Software | QuPath, IGV, custom algorithms (realDcaller2, NCsv2) [125] [126] | Bioinformatic processing | Specialized tools for structural variant calling and methylation analysis |
Biomarker Correlations with Therapeutic Efficacy
Differential Response by HRD Etiology
Emerging evidence suggests that the specific mechanism underlying HRD significantly influences PARPi efficacy:
- BRCA1/2 LOH: Associated with superior outcomes (median PFS undefined in GM-seq study) [125]
- BRCA1 promoter methylation: Intermediate benefit (median PFS 23.4 months) [125]
- HRD of unknown etiology: Most limited benefit (median PFS 8.8 months) [125]
These findings underscore the importance of elucidating the specific HRD mechanism rather than relying solely on composite HRD scores.
Novel Predictive Biomarkers Beyond HRD
SLFN11 This gene encodes a protein that blocks replication fork progression under PARPi-induced stress. SLFN11 deficiency, observed in 30-40% of ovarian cancers, confers intrinsic resistance independent of HRD status [122].
Dipeptidyl Peptidase 4 (DPP4) This chemokine-inactivating protease suppresses PARPi-induced anti-tumor immune responses. DPP4 overexpression induces PARPi resistance in HRD models, while DPP4 inhibition reverses intrinsic resistance in HRP models [126].
PARP1 Expression and Trapping Efficiency Tumors with low PARP1 expression or hypomorphic PARP1 variants (e.g., E988K) exhibit reduced PARP trapping and diminished PARPi response, independent of HR status [122].
Emerging Biomarkers and Resistance Mechanisms
Biomarkers for Immunotherapy Combination Strategies
The immunomodulatory effects of PARPi create rationale for combination with immune checkpoint inhibitors. Key biomarkers under investigation include:
- STING pathway activation: PARPi-induced cytosolic DNA accumulation triggers STING-dependent chemokine production (CCL5, CXCL10) that recruits T cells [126]
- Tumor-infiltrating lymphocytes: Granzyme B+ cytotoxic T cells correlate with response in syngeneic models [126]
- DPP4 expression: High tumor DPP4 predicts poor outcome and may identify patients for DPP4 inhibitor combinations [126]
Diagram Title: PARPi Immune Activation and Biomarkers
Resistance Biomarkers and Monitoring Approaches
Acquired resistance to PARPi remains a significant clinical challenge, with several emergent biomarkers:
- BRCA reversion mutations: Restore HRR function and represent the most common resistance mechanism, occurring in 40-70% of ovarian cancer patients [122]
- HRR restoration: Epigenetic plasticity can lead to partial BRCA1 promoter demethylation and functional recovery [122]
- 53BP1 loss: Partially restores HRR in BRCA1-deficient cells [119]
- Replication fork stabilization: Through alterations in factors like Schlafen-11 [122]
Longitudinal monitoring through circulating tumor DNA (ctDNA) provides a non-invasive approach to detecting resistance mechanisms as they emerge during therapy.
The comparative performance of BRCA/HRD biomarkers for PARPi in ovarian cancer demonstrates a clear hierarchy of predictive power, with BRCA mutations showing the most robust correlation with therapeutic benefit, followed by HRD-positive status. However, substantial heterogeneity exists within these categories, necessitating more refined biomarker approaches.
Emerging methodologies that integrate genetic, genomic, and epigenetic markers show promise in resolving this heterogeneity and improving patient stratification. Furthermore, novel biomarkers related to immune activation and replication stress response may expand PARPi efficacy to biomarker-defined subsets beyond the current HRD paradigm.
As combination strategies evolve, multidimensional biomarker assessment will be essential for matching the right patients with the right therapies and overcoming the challenge of resistance. The ongoing refinement of these predictive biomarkers represents a critical frontier in personalized ovarian cancer therapy.
Ovarian cancer remains the most lethal gynecological malignancy worldwide, with poor long-term survival rates despite standard surgical and chemotherapeutic interventions. The majority of patients are diagnosed at advanced stages and face high rates of recurrence and chemoresistance, creating an urgent need for more effective treatment strategies [127]. Immunotherapy has emerged as a promising approach, leveraging the body's immune system to combat tumor cells. However, the comparative effectiveness and safety profiles of various immunotherapeutic strategies, and the biomarkers that predict their success, require systematic evaluation to guide clinical decision-making [128] [43].
Network meta-analysis (NMA) provides a powerful statistical framework for comparing multiple interventions simultaneously, even in the absence of direct head-to-head trials. This approach is particularly valuable in rapidly evolving fields like cancer immunotherapy, where new treatment modalities continue to emerge [43]. This review synthesizes evidence from recent network meta-analyses to rank immunotherapeutic strategies for ovarian cancer based on efficacy and safety outcomes, with a specific focus on the biomarkers that can optimize patient selection and treatment outcomes.
Methodological Framework for Network Meta-Analysis
Search Strategy and Study Selection
The network meta-analyses referenced in this review employed systematic literature searches across multiple electronic databases, including PubMed, Embase, Medline, Cochrane Central Register of Controlled Trials, and Web of Science. Searches typically extended from database inception to May 31, 2025, ensuring inclusion of the most recent evidence [128] [43]. The search strategy incorporated Medical Subject Headings (MeSH) and text words related to ovarian cancer, immunotherapy, and randomized controlled trials (RCTs), combined using Boolean operators.
Study selection followed strict inclusion criteria focusing on RCTs involving adult patients with histologically confirmed ovarian cancer, including primary peritoneal and fallopian tube cancers. Interventions of interest encompassed various immunotherapeutic approaches, including immune checkpoint inhibitors (targeting PD-1, PD-L1, and CTLA-4), cancer vaccines, dual immune checkpoint blockade, immunostimulants, and combination therapies. Comparators included usual care, placebo, standard chemotherapy, or other immunotherapeutic strategies [43].
Data Extraction and Quality Assessment
Data extraction covered study characteristics (authors, publication year, journal), patient demographics, intervention protocols, comparator regimens, treatment duration, and outcome measures. Key outcomes included overall survival (OS), progression-free survival (PFS), objective response rate (ORR), disease control rate (DCR), treatment-related adverse events (TRAEs), and grade ≥3 adverse events [128] [43].
Risk of bias assessment utilized the revised Cochrane Risk of Bias Tool (RoB 2), evaluating five domains: randomization process, deviations from intended interventions, missing outcome data, measurement of outcomes, and selection of reported results. Among the 26 RCTs included in the primary analysis, 12 were rated as low risk of bias, 11 had some concerns, and 3 were rated as high risk [128].
Statistical Analysis
The NMAs employed Bayesian or Frequentist framework using random-effects models. For time-to-event outcomes such as OS and PFS, hazard ratios (HRs) with 95% confidence intervals (CIs) were calculated. For dichotomous outcomes including ORR, DCR, and adverse events, odds ratios (ORs) with 95% CIs were computed. Continuous outcomes were analyzed using standardized mean differences (SMDs) or mean differences (MDs) with 95% CIs [128] [43] [129].
Network consistency was assessed using node-splitting methods, and publication bias was evaluated through funnel plots and Egger's test. For all outcomes analyzed in the primary study, p-values from Egger's test exceeded 0.05, indicating no significant publication bias, though some funnel plots showed asymmetry potentially attributable to study heterogeneity or small-sample effects [128].
Table 1: Key Methodological Components of Network Meta-Analyses in Ovarian Cancer Immunotherapy
| Component | Description | Implementation in Current Analysis |
|---|---|---|
| Search Strategy | Comprehensive database searching | PubMed, Embase, Cochrane, Web of Science up to May 31, 2025 |
| Study Design | Randomized controlled trials | 26 RCTs included with 5,982 patients |
| Interventions | Various immunotherapies | Checkpoint inhibitors, cancer vaccines, combination therapies |
| Outcomes | Efficacy and safety endpoints | OS, PFS, ORR, DCR, TRAEs, ≥3 AEs |
| Statistical Framework | Bayesian/Frequentist approach | Random-effects models for multiple treatment comparisons |
| Risk of Bias | Cochrane RoB 2 tool | 12 low risk, 11 some concerns, 3 high risk |
Comparative Efficacy of Immunotherapeutic Strategies
Survival Outcomes
The network meta-analysis revealed significant differences in survival benefits across immunotherapeutic strategies. Cancer vaccines (CV) demonstrated the most substantial improvement in overall survival (HR = 0.56, 95% CI 0.43–0.73), followed by dual immune checkpoint blockade (DICB) (HR = 0.65, 95% CI 0.46–0.92) [128]. These findings indicate that cancer vaccines reduced mortality risk by 44% compared to control treatments, establishing them as the most effective single modality for improving OS in ovarian cancer.
For progression-free survival, cancer vaccines also showed significant benefit (SMD = 0.95, 95% CI 0.16–1.75), while other immunotherapies including PD-1 inhibitors, PD-L1 inhibitors, and CTLA-4 inhibitors did not demonstrate statistically significant improvements in PFS compared to controls [128]. This suggests that while certain immunotherapies may extend overall survival, their ability to delay disease progression may be more limited.
A separate NMA focusing specifically on PD-1/PD-L1 inhibitors found that combination approaches yielded superior outcomes. PD-1/PD-L1 inhibitors combined with chemotherapy and PD-1/PD-L1 inhibitors plus ipilimumab showed the greatest PFS benefit (HR = 0.82, 95% CI 0.52–1.07; HR = 0.82, 95% CI 0.51–1.33, respectively) and OS benefit (HR = 0.85, 95% CI 0.64–1.14; HR = 0.83, 95% CI 0.45–1.54, respectively) [129]. These combinations represent promising strategies for enhancing the efficacy of checkpoint inhibitors in ovarian cancer.
Tumor Response Metrics
For objective response rate, CTLA-4 inhibitors demonstrated remarkable efficacy (OR = 99.32, 95% CI 1.18–8360.43), though the exceptionally wide confidence interval indicates substantial uncertainty in this point estimate [128]. Cancer vaccines also showed favorable response rates, consistent with their survival benefits.
Combination therapies incorporating PD-1/PD-L1 inhibitors with chemotherapy significantly improved ORR compared to chemotherapy alone (OR = 3.06, 95% CI 1.42–6.60) [129]. This nearly threefold increase in objective response highlights the potential of immunotherapy-chemotherapy combinations for achieving tumor shrinkage in ovarian cancer patients.
Interestingly, no significant differences were observed in disease control rates across most immunotherapeutic strategies [128]. This suggests that while certain immunotherapies can generate dramatic responses in subsets of patients, they may not consistently provide durable disease control across broader patient populations—a finding that may reflect the heterogeneous nature of ovarian cancer and its complex tumor microenvironment.
Table 2: Efficacy Outcomes of Immunotherapeutic Strategies in Ovarian Cancer
| Immunotherapy Strategy | Overall Survival HR (95% CI) | Progression-Free Survival HR/SMD (95% CI) | Objective Response Rate OR (95% CI) |
|---|---|---|---|
| Cancer Vaccines (CV) | 0.56 (0.43–0.73) | 0.95 (0.16–1.75)* | - |
| Dual Immune Checkpoint Blockade (DICB) | 0.65 (0.46–0.92) | - | - |
| CTLA-4 Inhibitors | - | - | 99.32 (1.18–8360.43) |
| PD-1/PD-L1 + Chemotherapy | 0.85 (0.64–1.14) | 0.82 (0.52–1.07) | 3.06 (1.42–6.60) |
| PD-1/PD-L1 + Ipilimumab | 0.83 (0.45–1.54) | 0.82 (0.51–1.33) | - |
| PD-1 Inhibitors | - | - | - |
*SMD reported instead of HR for this outcome
Safety Profile Ranking of Immunotherapies
The safety analysis revealed substantial differences in adverse event profiles across immunotherapeutic strategies. PD-1 inhibitors demonstrated the most favorable safety profile, with significant reductions in grade ≥3 adverse events (OR = 0.16, 95% CI 0.08–0.33) and overall treatment-related adverse events compared to other immunotherapies [128]. This favorable toxicity profile positions PD-1 inhibitors as an attractive option for patients who may be vulnerable to treatment-related complications.
Dual immune checkpoint blockade also showed acceptable safety outcomes, with low rates of severe adverse events (OR = 0.24, 95% CI 0.06–0.90) [128]. This is particularly noteworthy given that dual checkpoint blockade typically produces higher toxicity rates in other cancer types, suggesting potentially unique immune interactions in the ovarian cancer microenvironment.
In contrast, IDO1 inhibitors were associated with the highest rate of severe adverse events (OR = 0.04, 95% CI 0.01–0.28), indicating substantially increased toxicity risk [128]. Similarly, PD-L1 inhibitors combined with cancer vaccines showed elevated adverse event rates (OR = 0.17, 95% CI 0.03–0.84), highlighting the importance of careful toxicity management when using combination approaches.
A meta-analysis focusing specifically on pembrolizumab reported that any-grade adverse events occurred in 81% of patients (95% CI 0.71–0.91), with grade ≥3 events occurring in 32% (95% CI 0.09–0.54) [130]. This safety profile was deemed acceptable given the treatment efficacy, particularly in the advanced and recurrent disease setting.
Biomarkers for Predicting Immunotherapy Response
Established Predictive Biomarkers
PD-L1 Expression: PD-L1 status has emerged as a valuable, though imperfect, biomarker for predicting response to immune checkpoint inhibitors. Subgroup analyses from NMAs indicated that PD-1/PD-L1 inhibitors combined with chemotherapy provided the best PFS and OS outcomes in PD-L1-positive patients [129]. A separate meta-analysis of pembrolizumab reported an ORR of 24% (95% CI 0.12–0.36) in PD-L1-positive patients compared to 18% (95% CI 0.09–0.27) in PD-L1-negative patients, though this difference did not reach statistical significance [130]. This suggests that while PD-L1 enrichment enhances response likelihood, it does not exclusively determine treatment benefit.
Homologous Recombination Deficiency (HRD): The HRD status, including BRCA1/2 mutations, has shown promise as a biomarker for both PARP inhibitor and immunotherapy response. The OVATION-2 trial, which evaluated intraperitoneal IL-12 immunotherapy, demonstrated particularly strong efficacy in HRD-positive patients, with significant improvements in both PFS and OS [131]. This aligns with the understanding that tumors with deficient DNA repair mechanisms typically harbor higher neoantigen loads, potentially rendering them more susceptible to immune recognition and attack.
Tumor Mutational Burden (TMB): While not explicitly quantified in the included NMAs, the underlying biology suggests that tumors with higher mutational burden may respond more favorably to immunotherapy. The typically low TMB in ovarian cancer compared to other solid tumors (e.g., melanoma, lung cancer) may partially explain the relatively modest efficacy of checkpoint inhibitors in this disease [127]. However, specific ovarian cancer subtypes, such as those associated with hereditary predisposition or specific histologic features, may exhibit elevated TMB and enhanced immunotherapy sensitivity.
Emerging Biomarker Candidates
Tumor Microenvironment (TME) Characteristics: The composition of the tumor immune microenvironment increasingly appears to predict immunotherapy response. Features such as high tumor-infiltrating lymphocyte (TIL) density, particularly CD8+ T cells, M1 macrophage polarization, and favorable cytokine profiles correlate with improved outcomes [127]. The ability of therapies like IL-12 to convert "cold" tumors to "hot" tumors (as demonstrated in the OVATION-2 trial) highlights the dynamic nature of these microenvironmental features and their potential utility as biomarkers [131].
Molecular Subtypes: Different histologic and molecular subtypes of ovarian cancer exhibit distinct responses to immunotherapy. For instance, low-grade serous carcinomas frequently harbor RAS/RAF pathway mutations and may respond differently to immunotherapies compared to high-grade serous carcinomas [127]. Similarly, clear cell and endometrioid subtypes may have unique immune profiles that influence treatment sensitivity.
Table 3: Biomarkers for Predicting Immunotherapy Response in Ovarian Cancer
| Biomarker | Predictive Value | Evidence Strength | Clinical Utility |
|---|---|---|---|
| PD-L1 Expression | Moderately predicts response to PD-1/PD-L1 inhibitors | Moderate: Subgroup analysis from RCTs | Helps identify patients most likely to benefit from checkpoint inhibitors |
| HRD Status | Predicts response to multiple immunotherapies | Strong: Phase I/II trial data with biomarker analysis | May guide combination therapy selection |
| Tumor Mutational Burden | Theoretically predicts response but limited in ovarian cancer | Limited: Indirect evidence from other cancers | Currently investigational for ovarian cancer |
| Tumor-Infiltrating Lymphocytes | Correlates with improved survival across immunotherapies | Moderate: Multiple correlative studies | May help identify "immune-hot" tumors |
| Molecular Subtypes | Differential responses across histologic subtypes | Emerging: Retrospective analyses | May guide therapy selection based on histology |
Signaling Pathways in Ovarian Cancer Immunotherapy
The efficacy of immunotherapeutic strategies in ovarian cancer is fundamentally governed by complex signaling pathways that regulate immune cell activation, trafficking, and function within the tumor microenvironment. The following diagram illustrates key pathways targeted by current immunotherapies:
Figure 1: Signaling pathways targeted by immunotherapies in ovarian cancer. The diagram illustrates key immune checkpoint interactions (yellow), cancer vaccine targets (green), and immunostimulatory pathways (blue). Solid arrows represent activating interactions, while dashed arrows indicate inhibitory signals.
The diagram highlights several therapeutically relevant pathways:
PD-1/PD-L1 Axis: Tumor cell expression of PD-L1 engages PD-1 on T cells, transmitting an inhibitory signal that dampens antitumor immunity. Checkpoint inhibitors targeting this pathway (PD-1/PD-L1 inhibitors) block this interaction, restoring T cell function [127].
CTLA-4/B7 Pathway: CTLA-4 on T cells competes with CD28 for binding to B7 molecules on antigen-presenting cells, generating an inhibitory signal that limits T cell activation, particularly during the priming phase. CTLA-4 inhibitors prevent this interaction, enhancing early T cell activation [128].
Antigen Presentation Machinery: Cancer vaccines work by enhancing tumor antigen presentation via MHC molecules to T cell receptors, initiating a specific antitumor immune response. This approach aims to overcome the limited natural immunogenicity of ovarian cancer cells [128].
Cytokine Signaling: Immunostimulatory agents like IL-12 activate multiple immune pathways, stimulating IFN-γ production and enhancing both innate and adaptive immune responses. The OVATION-2 trial demonstrated that localized delivery of IL-12 can remodel the tumor microenvironment and generate meaningful clinical responses [131].
Research Reagent Solutions for Immunotherapy Studies
Advancing ovarian cancer immunotherapy research requires specialized reagents and tools for investigating immune responses and biomarker expression. The following table outlines essential research solutions for this field:
Table 4: Essential Research Reagents for Ovarian Cancer Immunotherapy Studies
| Reagent Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Immune Checkpoint Reagents | Anti-PD-1, anti-PD-L1, anti-CTLA-4 antibodies | IHC, flow cytometry, functional assays | Blockade and detection of checkpoint molecules |
| Cytokine/Antigen Tools | Recombinant IL-12, tumor antigen peptides, MHC multimers | T cell activation assays, vaccine development | Immune stimulation and antigen-specific response detection |
| Cell Isolation Kits | CD8+ T cell isolation kits, tumor dissociation kits | Immune cell purification, TIL expansion | Preparation of specific immune cell populations |
| Gene Expression Panels | Nanostring PanCancer IO 360, RNAseq libraries | Tumor microenvironment profiling | Comprehensive immune gene expression analysis |
| IHC/IF Antibodies | CD8, CD4, CD68, PD-L1, Granzyme B | Tissue-based immune profiling | Spatial analysis of immune cell infiltration |
| Cell Culture Supplements | T cell activation beads, cytokine cocktails | TIL expansion, immune cell functional assays | Maintenance and activation of immune cells in vitro |
These research tools enable comprehensive investigation of the ovarian cancer immune microenvironment and therapy mechanisms. For instance, multiplex immunohistochemistry panels containing antibodies against CD8, PD-L1, and other immune markers allow simultaneous evaluation of multiple immune parameters in tumor tissues, facilitating biomarker discovery and validation [127]. Similarly, specialized cell culture systems that maintain tumor-infiltrating lymphocyte viability and function enable critical functional assays for evaluating therapy mechanisms.
This network meta-analysis of immunotherapeutic strategies in ovarian cancer demonstrates that cancer vaccines and dual immune checkpoint blockade provide the most significant survival benefits, while PD-1 inhibitors offer the most favorable safety profile. The efficacy of these approaches is critically dependent on appropriate patient selection using biomarkers such as PD-L1 expression, HRD status, and tumor microenvironment characteristics.
The emerging evidence supports a biomarker-driven approach to immunotherapy in ovarian cancer, with combination strategies showing particular promise for overcoming the immunosuppressive tumor microenvironment. Future research directions should include robust biomarker validation in prospective trials, development of novel agents targeting alternative immune pathways, and optimized combination strategies that balance efficacy with toxicity.
As the ovarian cancer immunotherapy landscape continues to evolve, network meta-analyses will play an increasingly important role in synthesizing evidence across multiple trials and guiding the development of personalized treatment approaches that maximize survival outcomes while maintaining acceptable quality of life.
The high mortality rate of ovarian cancer is primarily attributable to late-stage diagnosis, with five-year survival rates plummeting from over 90% in localized disease to approximately 30% in advanced stages [2] [132]. This stark reality underscores the urgent need for reliable, clinically applicable biomarkers and robust validation frameworks to assess their true effectiveness. Validation frameworks—encompassing prospective trials, retrospective studies, and external validation—form the methodological backbone that determines whether promising biomarkers can transition from research settings to clinical practice.
Each validation approach offers distinct advantages and limitations in establishing the clinical validity and utility of ovarian cancer biomarkers. Prospective trials provide the highest level of evidence but require significant resources and time. Retrospective studies enable rapid preliminary validation using existing datasets and biobanks. External validation assesses generalizability across diverse populations and settings. For researchers and drug development professionals, understanding the comparative effectiveness of these frameworks is essential for designing robust biomarker development pipelines and interpreting the growing literature on ovarian cancer diagnostics.
This guide objectively compares these validation frameworks through the lens of ovarian biomarker research, synthesizing current evidence on their performance characteristics, implementation requirements, and appropriate applications within the biomarker development pathway.
Comparative Performance of Validation Frameworks
The table below summarizes the key performance metrics, applications, and limitations of the three primary validation frameworks as applied to ovarian cancer biomarker research.
Table 1: Comparative Analysis of Validation Frameworks for Ovarian Cancer Biomarkers
| Validation Framework | Typical Study Design & Timeline | Key Performance Metrics | Strengths | Limitations |
|---|---|---|---|---|
| Prospective Trials | Intervention-based; follows predefined protocol with future outcome assessment; typically 3-7 years [133]. | Sensitivity, specificity, PPV, NPV, clinical utility, mortality reduction [132]. | Highest evidence level; minimizes biases; assesses true clinical utility and impact on patient outcomes. | Resource-intensive; lengthy duration; ethical considerations if control group receives substandard care. |
| Retrospective Studies | Analysis of existing biospecimens and clinical data; typically 1-2 years [133]. | AUC, sensitivity, specificity, odds ratios, hazard ratios [36] [28]. | Faster and more cost-effective; ideal for initial validation and hypothesis generation. | Susceptible to selection and confounding biases; limited clinical utility assessment. |
| External Validation | Testing of pre-existing models or algorithms on entirely new datasets; typically 1-3 years [134]. | AUC, calibration metrics, sensitivity, specificity across different populations [28] [134]. | Essential for assessing generalizability and real-world performance; critical before clinical implementation. | Performance often drops ("spectrum bias"); requires available, high-quality independent datasets. |
Experimental Protocols for Biomarker Validation
Protocol for Prospective Validation Trials
The UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS) exemplifies a large-scale prospective trial design for validating a screening strategy. The protocol involved sequential application of biomarker tests and imaging, with long-term follow-up for mortality outcomes [36] [133].
Methodology:
- Participant Recruitment and Randomization: Over 200,000 postmenopausal women were enrolled and randomly assigned to one of three groups: multimodal screening (MMS) with annual CA-125 testing interpreted with the Risk of Ovarian Cancer Algorithm (ROMA), transvaginal ultrasound screening (USS), or no screening [36].
- Intervention Protocol:
- MMS Group: Annual CA-125 blood test. Based on the ROCA score, participants were triaged: low risk -> return in 12 months; intermediate risk -> repeat CA-125 in 6-8 weeks; elevated risk -> transvaginal ultrasound scan and referral to a gynecological oncologist [36] [132].
- USS Group: Annual screening with transvaginal ultrasound.
- Outcome Measurement: The primary outcome was death from ovarian cancer. Follow-up was achieved via national death registries and required a minimum of 10-15 years to ascertain [36].
- Analysis: Intention-to-treat analysis compared ovarian cancer mortality rates across the three groups.
Protocol for Retrospective Biomarker Validation
Retrospective studies often utilize archived serum/plasma samples and clinical data from biobanks to validate novel biomarker panels or machine learning algorithms.
Methodology (Based on AI-derived Blood Biomarker Research):
- Cohort Selection: Identify a defined cohort of patients with ovarian cancer and control individuals with benign conditions or healthy status from existing clinical repositories. Sample sizes vary but often range from hundreds to low thousands [28].
- Biomarker Measurement: Analyze banked serum or plasma samples using the technology/platform relevant to the new biomarker (e.g., immunoassays for proteins, sequencing for ctDNA or miRNAs, mass spectrometry for metabolites or lipids) [133] [28].
- Model Development and Training: A machine learning algorithm (e.g., Random Forest, XGBoost, Neural Networks) is trained on a portion of the data (training set) using the biomarker levels and, often, clinical variables like age to create a predictive model [36] [28].
- Internal Validation: The model's performance is tested on a held-out portion of the same dataset (validation set) to calculate preliminary performance metrics like AUC, sensitivity, and specificity. Cross-validation techniques are often applied [28].
Protocol for External Validation of Prediction Models
External validation tests a previously developed prediction model on completely new data, often from a different geographical region or healthcare system, as demonstrated by a recent UK study developing cancer prediction algorithms [134].
Methodology:
- Model Selection: Identify a fully specified prediction model for validation (e.g., a QCancer model or a specific biomarker algorithm). The model includes the exact biomarkers, coefficients, and risk calculation method [134].
- Independent Cohort Recruitment: Assemble a new cohort of patients that was not used in the model's development. This cohort should be representative of the target population for the model. The cited study used a validation cohort of 2.64 million patients from England and another 2.74 million from Scotland, Wales, and Northern Ireland [134].
- Application of Model: Apply the existing model to the new cohort's data without any retraining or modification.
- Performance Assessment:
- Discrimination: Evaluate using the Area Under the Receiver Operating Characteristic Curve (AUROC or c-statistic). For example, the validated model for "any cancer" achieved a c-statistic of 0.876 in men and 0.844 in women [134].
- Calibration: Assess how well the predicted probabilities of cancer align with the observed probabilities, often visualized with calibration plots.
- Clinical Utility: Analyze using decision curve analysis to determine the net benefit of using the model across different probability thresholds.
Visualization of Research Workflows
Prospective Trial Biomarker Triage Workflow
The following diagram illustrates the complex triage and decision-making process used in prospective screening trials like UKCTOCS, which is critical for understanding the operational implementation of biomarker validation.
Retrospective & External Validation Analysis Workflow
This diagram outlines the core computational and analytical process for both retrospective model development and its subsequent external validation, highlighting the critical separation of data.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in the development and validation of ovarian cancer biomarkers, as cited in recent experimental workflows.
Table 2: Essential Research Reagents for Ovarian Biomarker Validation Studies
| Reagent / Material | Specifications & Common Formats | Primary Function in Validation |
|---|---|---|
| Clinical Serum/Plasma Samples | Collected in EDTA/SST tubes; archived at -80°C; paired with clinical metadata [133] [28]. | The primary matrix for quantifying circulating biomarkers (CA-125, HE4, ctDNA, miRNAs); enables retrospective validation. |
| Anti-CA-125 & Anti-HE4 Antibodies | Monoclonal antibodies; conjugated to enzymes (ELISA) or fluorescent dyes (immunoassays) [36] [132]. | Critical reagents for immunoassays that measure the concentration of key protein biomarkers in serum. |
| ctDNA Enrichment & Sequencing Kits | Kits for cell-free DNA extraction; targeted NGS panels (e.g., for TP53, BRCA1/2); methyl-specific PCR reagents [133]. | Enable isolation and genomic/epigenomic analysis of circulating tumor DNA from liquid biopsy samples. |
| Machine Learning Algorithms | Implemented in R/Python (e.g., Random Forest, XGBoost, SVM); require structured clinical and biomarker data as input [36] [28]. | Computational tools to build multivariable predictive models that integrate multiple biomarkers and patient factors. |
| 3D Micro-Tumour Culture Matrices | Basement membrane extract (BME) or similar hydrogels to support 3D cell growth [135]. | Provides an ex vivo platform to culture patient-derived micro-tumors for functional drug sensitivity testing. |
| Programmed Cell Death Ligands | Recombinant proteins/inhibitors for PD-1/PD-L1 axis [136]. | Key reagents for investigating immunotherapy biomarkers and their role in the tumor microenvironment. |
The validation of ovarian cancer biomarkers is a multi-stage process where prospective trials, retrospective studies, and external validation serve complementary, non-interchangeable roles. Retrospective studies provide the initial, cost-effective evidence for biomarker-disease association. External validation is a non-negotiable step that rigorously tests the model's generalizability before clinical use. Finally, large-scale prospective randomized trials provide the definitive evidence on whether a biomarker or algorithm actually improves patient outcomes, such as reducing mortality, which remains the ultimate goal.
For researchers and drug development professionals, the strategic integration of these frameworks is paramount. Beginning with retrospective analyses to refine biomarker panels, followed by rigorous external validation across diverse populations, and culminating in prospective trials ensures that only the most robust and effective diagnostics advance to clinical practice. This systematic, evidence-based approach is crucial for overcoming the historical challenges in ovarian cancer diagnosis and making meaningful progress toward reducing mortality from this devastating disease.
Ovarian cancer remains the most lethal gynecological malignancy, largely due to late-stage diagnosis and nonspecific early symptoms [36]. The development of biomarkers for early detection, prognosis, and treatment guidance represents a critical frontier in oncology research. However, the translation of promising biomarkers from experimental settings to clinical practice necessitates rigorous evaluation of both their clinical performance and economic viability. Cost-effectiveness analysis (CEA) has emerged as an essential methodology for determining the value proposition of novel biomarkers and their guided interventions, providing crucial evidence for healthcare decision-makers regarding resource allocation and reimbursement policies [137]. This guide systematically compares current and emerging ovarian cancer biomarkers through the dual lenses of clinical utility and economic impact, providing researchers and developers with evidence-based frameworks for technology assessment.
Comparative Performance Analysis of Ovarian Cancer Biomarkers
Established and Emerging Biomarker Profiles
Table 1: Performance Characteristics of Ovarian Cancer Biomarkers and Algorithms
| Biomarker/Algorithm | Type | Sensitivity Range | Specificity Range | AUC | Key Clinical Applications |
|---|---|---|---|---|---|
| CA125 [36] [100] | Protein | ~80% (late-stage) | Limited (multiple non-cancer elevations) | 0.70-0.80 | Monitoring treatment response and recurrence |
| HE4 [36] [100] | Protein | Varies by study | Superior to CA125 for malignant vs. benign | 0.80-0.90 | Differential diagnosis of pelvic masses |
| ROMA (CA125 + HE4) [36] [100] | Algorithm | Improved over single markers | ~75-85% | ~0.89-0.93 | Risk stratification of pelvic masses |
| Ovatools (CA125 + age) [138] | Risk Prediction Model | Not specified | Not specified | Not specified | Primary care triage for suspected OC |
| Multi-omic AI (Lipids + Proteins) [139] | Multi-analyte + ML | 88% (early-stage) | Not specified | 0.88-0.92 | Early detection in symptomatic women |
| miRNA Signatures [100] | miRNA | Varies by specific panels | Varies by specific panels | ~0.85-0.90 | Potential diagnostic and prognostic biomarkers |
| EV RNA Biomarkers [140] | Extracellular Vesicle RNA | Not specified | Not specified | Not specified | Potential diagnostic biomarkers |
Advanced Biomarker Technologies and Methodologies
Table 2: Emerging Biomarker Technologies and Performance Metrics
| Technology Platform | Analytes Detected | Sample Type | Stage I/II Detection Capability | Key Advantages |
|---|---|---|---|---|
| Multi-omic AI Platform [139] | Lipids, Gangliosides, Proteins | Blood | 88% sensitivity (AUC: 0.88) | Integrates multiple molecular classes; machine learning analysis |
| Extracellular Vesicle Analysis [140] | mRNA, miRNA | Ascites, Peritoneal Fluid | Identifies differentially expressed patterns | Reflects disease stage; novel source for biomarkers |
| Circulating Tumor DNA [2] | Tumor-specific DNA mutations | Blood | Not specified | Detects minimal residual disease; predicts recurrence |
| miRNA Profiling [2] [100] | MicroRNAs (e.g., miR-203a) | Blood, Body Fluids | Potential for early detection | Regulates gene expression; resistant to degradation |
| Lipidomics Profiling [2] | Lipid molecules | Blood | 88% accuracy in early-stage detection | Reveals metabolic alterations; machine learning compatible |
Experimental Protocols and Methodologies
Multi-omic Biomarker Discovery and Validation
The development of novel multi-omic biomarkers involves sophisticated experimental workflows that integrate multiple analytical platforms:
Sample Collection and Processing: Blood samples are collected from symptomatic patients and controls using standardized venipuncture procedures. Samples are processed within 2-4 hours of collection, with plasma separated by centrifugation and stored at -80°C until analysis [139]. For extracellular vesicle studies, ascites and peritoneal fluids are collected during surgical procedures, centrifuged at 2000 × g for 15 minutes to remove cell debris, and supernatants stored at -80°C [140].
Multi-omic Analysis: Liquid chromatography-mass spectrometry (LC-MS) is employed for lipid and ganglioside profiling, while immunoassays (e.g., ELISA) detect protein biomarkers. For extracellular vesicle RNA analysis, EVs are isolated using ultracentrifugation or filter-based methods (e.g., ExoComplete filterplates), followed by RNA extraction using commercial kits (e.g., miRNeasy) [140]. RNA quality is assessed using Agilent Bioanalyzer, and sequencing libraries are prepared using Illumina TruSeq protocols [140].
Data Integration and Machine Learning: Multi-omic datasets are integrated using machine learning algorithms (e.g., Random Forest, XGBoost) to identify discriminatory biomarker patterns. The model is typically trained on one cohort and validated on an independent test set to ensure robustness [36] [139]. Performance metrics including sensitivity, specificity, and area under the curve (AUC) are calculated to assess diagnostic accuracy.
Cost-Effectiveness Analysis Methodologies
Economic evaluations of biomarker-guided strategies employ decision-analytic modeling to compare long-term costs and health outcomes:
Model Structure: Decision trees represent diagnostic pathways, while state-transition (Markov) models capture long-term survival, quality of life, and costs [138]. Models simulate patient pathways through various health states (e.g., no cancer, early-stage cancer, late-stage cancer) with annual cycle lengths [138].
Parameter Estimation: Test accuracy data (sensitivity, specificity) are derived from clinical studies. Cancer incidence and stage distribution are estimated from large databases (e.g., CPRD Aurum in the UK) [138]. Survival estimates are derived from parametric survival models fitted to patient-level data [138].
Outcome Measures: Cost-effectiveness is typically expressed as an incremental cost-effectiveness ratio (ICER), representing the additional cost per quality-adjusted life-year (QALY) gained compared to the next best strategy [138] [141]. Costs are considered from healthcare system or societal perspectives, and both costs and outcomes are discounted (typically 3% annually) [138].
Validation and Uncertainty: Models are validated against internal and external data sources [138]. Sensitivity analyses (deterministic and probabilistic) assess the impact of parameter uncertainty on results [138] [141].
Biomarker Development Workflow
Cost-Effectiveness of Biomarker-Guided Strategies
Economic Evaluations of Diagnostic Biomarkers
Table 3: Cost-Effectiveness of Ovarian Cancer Biomarker Strategies
| Biomarker Strategy | Comparator | Population | ICER (Cost per QALY) | Key Determinants of Cost-Effectiveness |
|---|---|---|---|---|
| Ovatools (CA125 + age-informed triage) [138] | CA125 ≥35 U/mL alone | Women ≥50 years with symptoms | £20,000-£30,000 | Risk threshold for imaging, age distribution |
| Multi-omic AI Blood Test [139] | Current standard (CA125 ± imaging) | Symptomatic women | Data pending (promising based on accuracy) | Test cost, adherence, early-stage detection rate |
| Biomarker-based HCC Screening [141] | Ultrasound + AFP | Cirrhosis patients | $14,800 (USD) | Test sensitivity >80%, cost <$210, adherence >58% |
| Companion Diagnostics for Targeted Therapies [137] | Untested therapy allocation | Various cancer patients | Highly variable | Test accuracy, drug cost, biomarker prevalence |
Methodological Considerations in Biomarker Economic Evaluations
Current practices in modeling companion biomarkers for targeted cancer therapies reveal significant methodological variations that can impact cost-effectiveness results [137]. A systematic review found that only 4 of 22 economic evaluations adequately incorporated companion biomarker characteristics, with most focusing solely on test cost or accuracy while omitting clinical outcomes, health state utilities, and the timing of testing [137]. The structure of comparator strategies substantially influences results, with some evaluations considering pre-selected biomarker-positive populations rather than all tested patients [137].
For biomarker-based screening strategies, cost-effectiveness is highly sensitive to test performance characteristics, adherence rates, and test costs. In hepatocellular carcinoma screening, for example, biomarker-based screening required sensitivity exceeding 80%, costs below $210, or adherence exceeding 58% to be cost-effective compared to ultrasound with AFP [141]. Similar principles apply to ovarian cancer biomarkers, where the balance between improved early detection and additional diagnostic costs determines economic viability.
Pathway Analysis for Targeted Therapies
Targeted Therapy Pathway
The KRAS signaling pathway represents a critical therapeutic target in low-grade serous ovarian cancer (LGSOC). KRAS mutations drive abnormal signaling through the RAF-MEK-ERK cascade, promoting tumor cell growth and proliferation [2]. Avutometinib inhibits MEK1/2 kinase activity and uniquely "clamps" RAF and MEK together to maintain them in an inactive state [2]. Defactinib inhibits focal adhesion kinase (FAK), which regulates RAS/RAF/MEK/ERK signaling and contributes to tumor invasion and metastasis [2]. This combination demonstrated significant efficacy in the RAMP-201 trial, with overall response rates of 31% in the overall LGSOC population and 44% in patients with KRAS mutations [2].
For homologous recombination deficiency (HRD) biomarkers, PARP inhibitor efficacy varies substantially based on biomarker status. Patients with BRCA1/2 mutations derive the greatest benefit (hazard ratio [HR] for progression-free survival: 0.33), followed by non-BRCA HRD (HR: 0.49), with limited benefit in homologous recombination proficient (HRP) tumors (HR: 0.78) [142]. This stratification has important economic implications, as careful cost-effectiveness analysis and consideration of alternative therapies are strongly recommended for HRP tumors [142].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Ovarian Cancer Biomarker Studies
| Reagent/Resource | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Sample Collection Kits | Cell-free DNA blood collection tubes, protease inhibitors | Biobanking for biomarker discovery | Standardization of processing protocols, storage conditions |
| EV Isolation Reagents | Ultracentrifugation protocols, ExoComplete filterplates, CD63 antibodies [140] | Extracellular vesicle biomarker studies | Purity and yield optimization, characterization methods |
| RNA Sequencing Kits | Illumina TruSeq mRNA stranded protocol, miRNeasy kits [140] | Transcriptomic biomarker discovery | RNA quality control, library preparation efficiency |
| Protein Assays | ELISA for CA125, HE4; LC-MS platforms for proteomics [139] | Protein biomarker quantification | Sensitivity, dynamic range, multiplexing capability |
| Machine Learning Platforms | Random Forest, XGBoost, Neural Networks [36] | Multi-omic data integration | Computational resources, validation frameworks |
| Cell Line Models | FTSEC, OSE, SKOV3, OVCA3 [140] | Functional validation of biomarkers | Relevance to ovarian cancer subtypes, authentication |
The evolving landscape of ovarian cancer biomarkers demonstrates a consistent trend toward multiplexed approaches that integrate multiple analyte classes with advanced computational analysis. While established biomarkers like CA125 and HE4 provide foundational value in specific clinical contexts, emerging multi-omic strategies show superior performance for early detection in symptomatic women [139]. The successful translation of these technologies requires simultaneous optimization of both clinical utility and economic value. Future development should prioritize multi-center validation studies, standardized economic evaluation methodologies that fully capture biomarker characteristics, and efficient integration with existing clinical pathways. By adopting a comprehensive approach that balances performance with practical implementation, researchers and developers can accelerate the delivery of transformative biomarker technologies that improve patient outcomes while ensuring sustainable healthcare resource utilization.
Conclusion
The comparative effectiveness of ovarian cancer biomarkers reveals a dynamic field transitioning from single-marker paradigms to integrated, multi-modal approaches. The highest levels of evidence currently support BRCA mutations and homologous recombination deficiency as predictive biomarkers for PARP inhibitor response, while AI-enhanced diagnostic models and multi-marker panels show exceptional promise for early detection. Future progress hinges on the rigorous validation of emerging biomarkers like CHI3L1 and metabolomic signatures through prospective, biomarker-driven clinical trials. For researchers and drug developers, success will require a concerted focus on overcoming tumor heterogeneity, standardizing assays, and developing sophisticated computational models that integrate diverse data streams. The ultimate goal is a precision oncology framework where biomarker-guided strategies transform ovarian cancer into a manageable chronic condition, significantly improving patient survival and quality of life.
References
- 1. A prospective evaluation of early detection biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5026545/]
- 2. New Approaches for Ovarian Cancer Treatment and ... [https://www.aacr.org/blog/2025/09/18/shining-a-light-on-new-approaches-for-ovarian-cancer-treatment-and-detection/]
- 3. Ovarian Cancer Biomarkers: Advancing Early Detection ... [https://www.nottheseovaries.org/ovarian-cancer-biomarkers/]
- 4. Recent Therapies and Biomarkers in Mucinous Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384067/]
- 5. Personalized Biomarker-Driven Therapy in Ovarian Cancer [https://medicine.yale.edu/publication-details/personalized-biomarker-driven-therapy-in-ovarian-cancer/]
- 6. Special Issue “Biomarkers and Early Detection Strategies ... [https://www.mdpi.com/1422-0067/26/18/9071]
- 7. Biomarker Identification: Characteristics, Methods and Tools [https://bigomics.ch/blog/how-to-find-biomarkers-biomarker-analysis-methods-and-practical-examples/]
- 8. CA125, HE4, RMI and ROMA, a review [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-019-0503-7]
- 9. Comparison of the diagnostic accuracy of HE4 with CA125 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10393307/]
- 10. HE4 and CA125 as a diagnostic test in ovarian cancer [https://www.nature.com/articles/6606092]
- 11. Diagnostic Performance of Risk of Ovarian Malignancy ... [https://www.sciencedirect.com/science/article/pii/S1048891X24031669]
- 12. Comparison of sensitivity for Risk of Ovarian Malignancy ... [https://pubmed.ncbi.nlm.nih.gov/40319538/]
- 13. A combined strategy of TK1, HE4 and CA125 shows better ... [https://www.sciencedirect.com/science/article/pii/S0009898121004010]
- 14. Special Issue “Biomarkers and Early Detection Strategies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12470875/]
- 15. Predictive biomarkers for targeted therapy in daily anatomic ... [https://surgexppathol.biomedcentral.com/articles/10.1186/s42047-025-00187-3]
- 16. Homologous recombination deficiency (HRD) testing landscape [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00740-y]
- 17. Homologous recombination deficiency test validation in ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1524594/full]
- 18. Analytical validation of a homologous recombination ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12622852/]
- 19. Homologous recombination deficiency in breast cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535909/]
- 20. Breast cancer homologous recombination deficiency ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125258/]
- 21. Predictive biomarkers for the efficacy of PARP inhibitors in ... [https://www.nature.com/articles/s44276-025-00122-9]
- 22. Long non-coding RNAs as a biomarker for homologous ... [https://www.nature.com/articles/s42003-025-08836-9]
- 23. CHI3L1/YKL-40 signaling inhibits neurogenesis in models of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12273788/]
- 24. Chitinase-3-like-1: a multifaceted player in neuroinflammation ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00801-8]
- 25. CHI3L1 results in poor outcome of ovarian cancer by ... [https://pubmed.ncbi.nlm.nih.gov/30121622/]
- 26. Serum osteopontin as a prognostic biomarker in acute ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1708595/full]
- 27. The prognostic and diagnostic potential of kallikrein-related ... [https://pubmed.ncbi.nlm.nih.gov/33947310/]
- 28. Journal of Medical Internet Research - AI-Derived Blood Biomarkers ... [https://www.jmir.org/2025/1/e67922]
- 29. Diagnostic and prognostic values of circulating growth ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12630631/]
- 30. The association of serum CHI3L1 levels with the presence ... [https://www.nature.com/articles/s41598-025-91935-8]
- 31. Frontiers | Uncovering key regulatory pathways and prognostic... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1591430/full]
- 32. Metabolomic biomarkers for benign conditions and ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898124019867]
- 33. Circulating proteins and metabolites panel for noninvasive ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-04341-2]
- 34. Frontiers | Metabolomic in liquid biopsy: biomarkers cancer... accurate [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1331215/full]
- 35. Mercy BioAnalytics Publishes Validation Study in ... [https://mercybio.com/2025/10/mercy-bioanalytics-publishes-validation-study-in-gynecologic-oncology-demonstrating-unprecedented-performance-of-blood-test-for-early-detection-of-ovarian-cancer/]
- 36. A Review on Biomarkerâ€Enhanced Machine Learning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421415/]
- 37. Metabolomics: Insights for Disease Mechanisms & ... [https://esmed.org/metabolomics-insights-for-disease-mechanisms-biomarkers/]
- 38. Diagnostic and prognostic biomarkers associated with ... [https://www.nature.com/articles/s41598-025-24938-0]
- 39. Unveiling histotype-specific biomarkers in ovarian ... [https://pubmed.ncbi.nlm.nih.gov/40778374/]
- 40. New Predictive Biomarkers for Ovarian Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7998656/]
- 41. Research Sheds New Light on a Key Ovarian Cancer ... [https://www.kucancercenter.org/news-room/news/2025/01/research-sheds-new-light-on-a-key-ovarian-cancer-biomarker]
- 42. Comparative effectiveness and safety of treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11983808/]
- 43. a systematic review and network meta-analysis [https://www.frontiersin.org/articles/10.3389/fonc.2025.1659897/full]
- 44. Machine learning approaches for biomarker discovery to ... [https://www.nature.com/articles/s41598-023-42338-0]
- 45. AI-driven biomarker discovery: enhancing precision in cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906928/]
- 46. Explainable machine learning framework for biomarker discovery by combining biological age and frailty prediction | Scientific Reports [https://www.nature.com/articles/s41598-025-98948-3]
- 47. Ovarian Cancer: Multi-Omics Data Integration [https://pubmed.ncbi.nlm.nih.gov/40649740/]
- 48. Deep plasma proteomics identifies and validates an eight- ... [https://www.nature.com/articles/s43856-025-00945-0]
- 49. Multi-omics strategies for biomarker discovery and ... [https://link.springer.com/article/10.1186/s43556-025-00340-0]
- 50. GlycoKnow Ovarian: a Glycoprotein-based, Serum ... [https://pubmed.ncbi.nlm.nih.gov/40661292/]
- 51. A metabolic fingerprint of ovarian cancer: a novel diagnostic ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01590-w]
- 52. Elucidating the mechanistic role of ovarian cancer ... [https://www.sciencedirect.com/science/article/pii/S1040842825002112]
- 53. Metabolomics and metabolites in cancer diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618785/]
- 54. Multi-omics study of prognostic models and molecular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12595189/]
- 55. The application of metabolomics in ovarian cancer ... [https://www.sciencedirect.com/science/article/pii/S1048891X24023429]
- 56. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 57. Circulating Biomarkers Market Intelligence | Future Growth & ... [https://www.congruencemarketinsights.com/report/circulating-biomarkers-market]
- 58. Circulating Biomarkers Market Revenue to Attain USD ... [https://www.precedenceresearch.com/press-release/circulating-biomarkers-market]
- 59. Next-Generation Liquid Biopsies: Embracing Data Science ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8408348/]
- 60. Diagnostic performance of various liquid biopsy methods in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7433831/]
- 61. Improvement of the sensitivity of circulating tumor DNA-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12332530/]
- 62. Oncology [https://templerx.com/pipeline/oncology/]
- 63. Companion Diagnostics: Strategies for Biomarker ... [https://www.precisionformedicine.com/blog/companion-diagnostics-strategies-for-biomarker-development-and-early-phase-clinical-studies/]
- 64. Companion diagnostics in targeted therapy | LabLeaders [https://diagnostics.roche.com/global/en/article-listing/lab-leaders/article/companion-diagnostics-targeted-therapy.html]
- 65. Biomarker and Companion Diagnostics—A Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8591033/]
- 66. Foundation Medicine Spotlights Scientific Achievements ... [https://www.foundationmedicine.com/press-release/esmo-2025]
- 67. Efficacy and Biomarker-Based Insights of Immunotherapy ... [https://ej-med.org/index.php/ejmed/article/view/2326]
- 68. Comparison of the diagnostic efficacy of systemic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1381268/full]
- 69. Companion Diagnostics Explained [https://www.foundationmedicine.com/blog/companion-diagnostics-explained-their-critical-role-cancer-care-and-our-latest-approvals]
- 70. Clinical utility of various liquid biopsy samples for the early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12259431/]
- 71. Quantitative Mass Spectrometry-Based Proteomics for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8125593/]
- 72. Next Generation Sequencing and Molecular Biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9030726/]
- 73. Large-scale proteomics reveals precise biomarkers for ... [https://www.nature.com/articles/s41598-024-68249-2]
- 74. Machine Learning-Enhanced Extraction of Biomarkers for ... [https://www.nature.com/articles/s41597-024-03536-1]
- 75. Biomarkers for Early Detection of Ovarian Cancer: A Review [http://waocp.com/journal/index.php/apjcb/article/view/1265]
- 76. The OvarianTagâ„¢ Biomarker Panel Emerges as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12428831/]
- 77. Validation of a Biomarker Panel and Longitudinal ... [https://www.sciencedirect.com/science/article/pii/S1048891X24021893]
- 78. The benefits and pitfalls of machine learning for biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10558383/]
- 79. Evaluation of the Diagnostic Accuracy of the Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3594110/]
- 80. Machine-learning diagnostic models for ovarian tumors [https://www.sciencedirect.com/science/article/pii/S2405844024130253]
- 81. A multimodal uncertainty-aware AI system optimizes ... [https://www.nature.com/articles/s41746-025-01986-4]
- 82. Ovarian Cancer Biomarkers: Current Options and Future ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3381792/]
- 83. How Biomarkers and Targeted Therapies are Reshaping ... [https://www.accc-cancer.org/acccbuzz/blog-post-template/accc-buzz/2025/05/08/precision-in-progress-how-biomarkers-and-targeted-therapies-are-reshaping-ovarian-cancer-care]
- 84. A framework for evaluating biomarkers for early detection: validation ... [https://pubmed.ncbi.nlm.nih.gov/21372037/]
- 85. Diagnostic biomarkers in ovarian cancer: advances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10908239/]
- 86. Frontiers | Proximity extension assay revealed novel inflammatory... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1525392/full]
- 87. Sensitivity and Specificity of Selected Biomarkers and Their ... [https://www.mdpi.com/2075-4418/14/9/949]
- 88. Biomarkers beyond BRCA: promising combinatorial treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9594904/]
- 89. PARP inhibitors in ovarian cancer: Mechanisms of ... [https://pubmed.ncbi.nlm.nih.gov/40203475/]
- 90. Overcoming Platinum and PARP-Inhibitor Resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7352566/]
- 91. Can integrative biomarker approaches improve prediction ... [https://www.sciencedirect.com/science/article/abs/pii/S1044579X21000316]
- 92. PARP Inhibition in Colorectal Cancer—A Comparison of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12196450/]
- 93. Functional Biomarkers of Platinum Chemotherapy and PARP ... [https://tech.wustl.edu/tech-summary/functional-biomarkers-of-platinum-chemotherapy-and-parp-inhibitor-response/]
- 94. Revealing biomarkers associated with PARP inhibitors based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8379270/]
- 95. Ovarian Cancer: Multi-Omics Data Integration [https://www.mdpi.com/1422-0067/26/13/5961]
- 96. AOA Dx Demonstrates High Accuracy in AI-Powered Blood ... [https://aoadx.com/aacr2025/]
- 97. Development of a diagnostic model for ovarian cancer based ... [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-025-01809-w]
- 98. CA125 and age-based models for ovarian cancer detection ... [https://www.nature.com/articles/s41416-025-03165-4]
- 99. Development of a diagnostic model for ovarian cancer based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584492/]
- 100. Developments in ovarian cancer markers and algorithms [https://www.ejgo.net/articles/10.22514/ejgo.2025.076]
- 101. Multicenter study of ovarian cancer score for diagnosing ... [https://www.sciencedirect.com/science/article/pii/S0090825824012356]
- 102. Integrative bioinformatics, statistical, and survival analysis ... [https://jmhg.springeropen.com/articles/10.1186/s43042-025-00779-4]
- 103. New genetic marker linked to improved survival with ... [https://www.mdanderson.org/newsroom/new-genetic-marker-linked-to-improved-survival-with-immunotherapy-in-ovarian-and-other-cancers.h00-159778023.html]
- 104. Tumour-infiltrating leucocytes as prognostic biomarkers of ... [https://www.nature.com/articles/s41698-025-01146-7]
- 105. Cancer Biomarkers: Reflection on Recent Progress, Emerging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468363/]
- 106. Role of Biomarkers in Diagnosing Disease, Assessing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12016010/]
- 107. an analysis based on population-level parametric distributions ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02656-5]
- 108. A unified classification approach rating clinical utility of ... [https://www.sciencedirect.com/science/article/pii/S235239642300021X]
- 109. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 110. Evidentiary Considerations [https://c-path.org/evidentiary-considerations-2/]
- 111. Demonstrating the Clinical Utility of Foundation Medicine's ... [https://www.foundationmedicine.com/blog/q3-research-recap-blog?utm_source=linkedin&utm_medium=organic-social&utm_campaign=q3-research-recap&utm_content=corporate]
- 112. New Clinical Practice Guideline for Blood-Based Biomarkers [https://aaic.alz.org/releases-2025/clinical-practice-guideline-blood-based-biomarkers.asp]
- 113. Therapeutic landscape of ovarian cancer: recent advances ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00818-7]
- 114. Diagnostic Accuracy of Blood-based Biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10035398/]
- 115. Integrative approach for enhanced ovarian cancer diagnosis [https://pubmed.ncbi.nlm.nih.gov/40784922/]
- 116. A Novel Predictive Multi-Marker Test for the Pre-Surgical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10650329/]
- 117. Diagnostic Accuracy of a Blood-Based Biomarker Panel for ... [https://www.mdpi.com/2072-6694/16/24/4176]
- 118. A Predictive Multi-Marker Test to Improve Ovarian Cancer ... [https://cdas.cancer.gov/approved-projects/5498/]
- 119. Unraveling Homologous Recombination Deficiency in Ovarian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12153926/]
- 120. Effectiveness and safety of PARP inhibitors in ovarian cancer [https://www.sciencedirect.com/science/article/abs/pii/S1040842825002811]
- 121. Long-Term OS Data Guide Use of PARP Inhibitors ... [https://www.targetedonc.com/view/long-term-os-data-guide-use-of-parp-inhibitors-in-ovarian-cancer]
- 122. Clinical approaches to overcome PARP inhibitor resistance [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02355-1]
- 123. PARP Inhibitors In Pancreatic Cancer: Breaking Beyond ... [https://globalrph.com/2025/11/parp-inhibitors-in-pancreatic-cancer-breaking-beyond-brca-mutations/]
- 124. Development of a prognosis model for PARP inhibitor ... [https://www.sciencedirect.com/science/article/pii/S1048891X25011077]
- 125. implications for PARP inhibitors efficacy | Biomarker Research [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00843-6]
- 126. PARP inhibitor-induced anti-tumour chemokine response ... [https://www.nature.com/articles/s41416-025-03076-4]
- 127. Promising new drugs and therapeutic approaches for ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-024-03826-w]
- 128. 综述:åµå·¢ç™Œå…疫治疗ç–略的比较疗效与安全性 [https://www.ebiotrade.com/newsf/2025-11/20251111000138287.htm]
- 129. Efficacy of PD-1/PDL-1 inhibitors for ovarian cancer [https://pubmed.ncbi.nlm.nih.gov/40650991/]
- 130. Efficacy and safety of pembrolizumab for the treatment ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1662455/full]
- 131. ASCO巅峰对è¯ä¸¨åˆ˜ç»§çº¢æ•™æŽˆ& Thaker教授共议ASCO 2025 ... [https://m.ioncol.com/weixin/detail.aspx?aid=11254]
- 132. Early Diagnosis of Ovarian Cancer: A Comprehensive ... [https://www.mdpi.com/2075-4418/15/4/406]
- 133. Clinical utility of various liquid biopsy samples for the early ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1594100/full]
- 134. Development and external validation of prediction ... [https://www.nature.com/articles/s41467-025-57990-5]
- 135. Ex vivo 3D micro-tumour testing platform for predicting ... [https://www.nature.com/articles/s41698-025-01080-8]
- 136. Emerging biomarkers for early cancer detection and diagnosis [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03003-6]
- 137. How are we evaluating the cost-effectiveness of companion ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-021-08725-4]
- 138. Cost-effectiveness of CA125- and age-informed risk-based ... [https://www.nature.com/articles/s41416-025-03166-3]
- 139. New Peer-Reviewed Publication Shows Multi-Omic AI ... [https://aoadx.com/peer-reviewed-multi-omic-oc-test/]
- 140. of benign peritoneal fluid- and Comparison cancer... ovarian [https://ovarianresearch.biomedcentral.com/articles/10.1186/s13048-018-0391-2]
- 141. Cost-Effectiveness of a Biomarker-Based Screening ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11649260/]
- 142. of PARPi efficacy according to homologous... Comparison [https://pubmed.ncbi.nlm.nih.gov/37211773/]