Decoding Fertility: How Omics Technologies Are Revolutionizing Reproductive Biology and Medicine
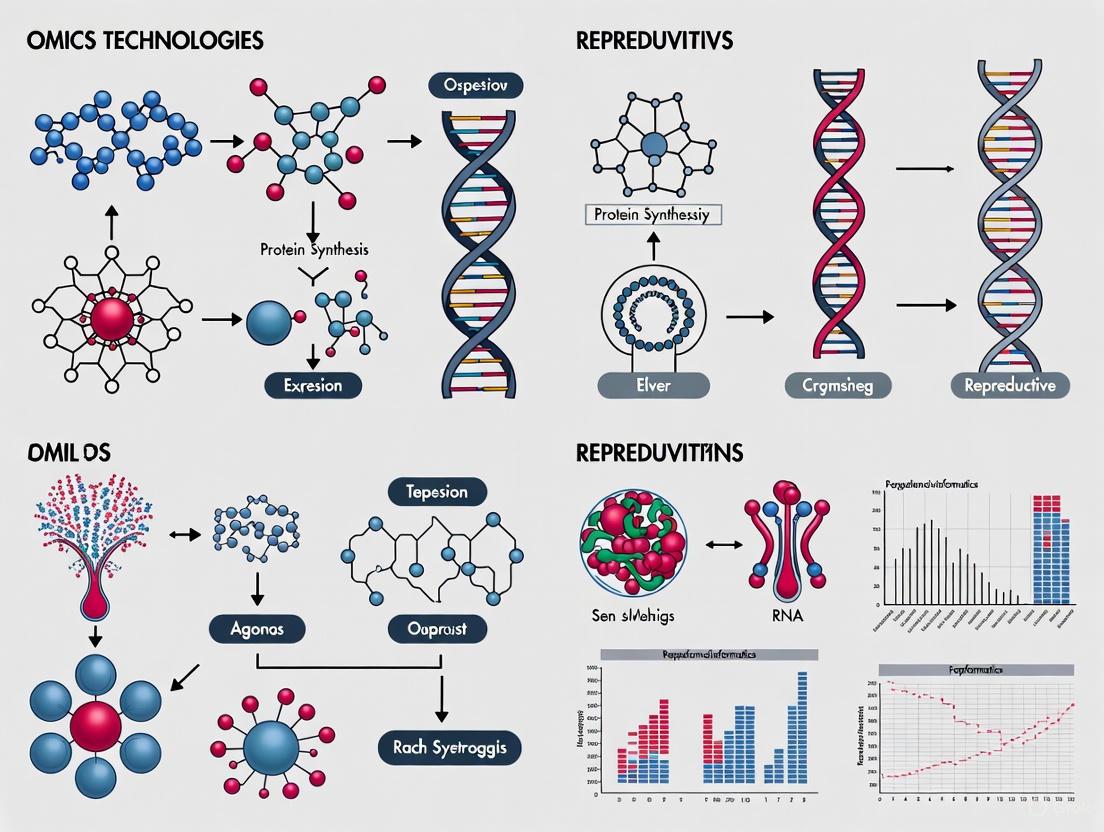
This article provides a comprehensive overview of the transformative impact of omics technologies—including genomics, transcriptomics, proteomics, and epigenomics—on reproductive biology.
Decoding Fertility: How Omics Technologies Are Revolutionizing Reproductive Biology and Medicine
Abstract
This article provides a comprehensive overview of the transformative impact of omics technologies—including genomics, transcriptomics, proteomics, and epigenomics—on reproductive biology. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of these technologies, their methodological applications in diagnosing and treating infertility, the current challenges in optimization and clinical integration, and the rigorous validation frameworks required for their translation into precision medicine. By synthesizing the latest advancements and evidence, this review serves as a critical resource for navigating the current landscape and future trajectory of high-throughput data in reproductive medicine.
The Omics Landscape: Core Technologies and Their Role in Decoding Reproductive Biology
The field of omics technologies has revolutionized biological research by enabling comprehensive analysis of the molecular components that define life. These technologies—including genomics, epigenomics, transcriptomics, proteomics, and metabolomics—provide complementary layers of information that collectively describe the flow of genetic information from DNA to functional metabolites. In reproductive biology, understanding these interconnected systems is particularly crucial due to the complex hormonal regulation, cellular differentiation, and rapid developmental processes that characterize reproductive tissues and functions [1]. The emergence of reproductomics, which applies multi-omics technologies to study reproductive processes, underscores the potential of these approaches to unravel the molecular mechanisms underlying infertility, pregnancy disorders, and gynecologic conditions [1] [2].
This technical guide provides an in-depth examination of the core omics technologies, their methodologies, applications in reproductive research, and the computational strategies required for their integration. By framing this information within the context of reproductive biology, we aim to equip researchers and drug development professionals with the knowledge needed to design and interpret multi-omics studies that can advance reproductive medicine.
The Central Dogma and Omics Cascade
The relationship between major omics layers follows the central dogma of molecular biology, with each layer representing a distinct stage of biological information flow. The diagram below illustrates these relationships and their applications in reproductive biology.
Core Omics Technologies: Methodologies and Applications
Genomics
Definition and Scope Genomics represents the foundational layer of omics sciences, dealing with the discovery and characterization of the complete set of DNA sequences within an organism [3]. While genomics focuses on the static DNA sequence, its applications extend to functional genomics (studying gene functions), comparative genomics (comparing genes across organisms), and structural genomics (determining 3D protein structures) [3].
Sequencing Technologies and Methodologies
Table 1: Comparison of DNA Sequencing Technologies
| Generation | Platform | Year Introduced | Sequencing Technology | Read Length | Throughput | Accuracy | Computing Requirements |
|---|---|---|---|---|---|---|---|
| First-Generation | Sanger | 1987 | Chain termination method | 800-1,000 bp | Low | High | Low |
| Second-Generation (NGS) | Illumina | 2006 | Sequencing by synthesis | 100-300 bp | High | High | High |
| Third-Generation | PacBio | 2009 | Circular consensus sequencing | 10,000-25,000 bp | High | Moderate | High |
| Third-Generation | Oxford Nanopore | 2015 | Electrical detection | 10,000-30,000 bp | Moderate | Low | High |
Experimental Workflow for Whole Genome Sequencing
- Library Preparation: DNA fragmentation and adapter ligation
- Cluster Amplification: Bridge amplification on flow cell (Illumina) or DNA fragment circularization (PacBio)
- Sequencing: Cyclic reversible termination (Illumina) or real-time sequencing (PacBio, Nanopore)
- Quality Control: Assessment of base call quality using Phred scores
- Read Alignment: Mapping to reference genome using BWA [4] or Bowtie2 [4]
- Variant Calling: Identification of genetic variants using GATK or Bcftools [4]
Reproductive Biology Applications In reproductive medicine, genomics has been instrumental in identifying genetic determinants of conditions such as premature ovarian insufficiency, endometriosis, and male factor infertility [1]. Genome-Wide Association Studies (GWAS) have revealed numerous genetic loci associated with endometriosis risk, demonstrating remarkable congruence across populations with minimal heterogeneity [1].
Epigenomics
Definition and Scope Epigenomics involves the comprehensive analysis of epigenetic modifications that regulate gene expression without altering the DNA sequence itself. These modifications include DNA methylation, histone modifications, and chromatin accessibility changes that collectively influence cellular identity and function [4].
Key Methodologies
DNA Methylation Analysis
- Bisulfite Sequencing: Treatment of DNA with bisulfite converts unmethylated cytosines to uracils, allowing precise mapping of methylated cytosines
- Whole Genome Bisulfite Sequencing: Provides single-base resolution methylation maps across the entire genome
- Reduced Representation Bisulfite Sequencing: Cost-effective method focusing on CpG-rich regions
Chromatin Accessibility and Histone Modification
- ATAC-seq: Assay for Transposase-Accessible Chromatin using sequencing identifies open chromatin regions
- ChIP-seq: Chromatin Immunoprecipitation followed by sequencing maps histone modifications and transcription factor binding sites
Experimental Workflow for Whole Genome Bisulfite Sequencing
- DNA Extraction: High molecular weight DNA isolation from tissue or cells
- Bisulfite Conversion: Treatment with sodium bisulfite to deaminate unmethylated cytosines
- Library Preparation: Fragmentation, adapter ligation, and PCR amplification
- Sequencing: High-throughput sequencing on Illumina platform
- Alignment: Mapping to reference genome using specialized bisulfite-aware aligners like Bismark or BSMAP
- Methylation Calling: Quantification of methylation levels at each cytosine position
Reproductive Biology Applications Epigenomics plays a critical role in reproductive processes including endometrial receptivity, germ cell development, and embryo implantation [1]. Studies of the endometrial methylome have revealed dynamic changes throughout the menstrual cycle, suggesting epigenetic regulation in response to hormonal fluctuations [1]. The non-linear relationship between DNA methylation and gene expression adds complexity to understanding reproductive processes [1].
Transcriptomics
Definition and Scope Transcriptomics encompasses the comprehensive study of all RNA molecules transcribed from the genome, including mRNA, non-coding RNAs, and small RNAs [4]. This field provides insights into gene expression patterns and regulatory mechanisms under different physiological conditions.
Methodological Approaches
Table 2: Transcriptomics Technologies and Applications
| Technology | Resolution | Throughput | Key Applications in Reproductive Biology |
|---|---|---|---|
| Bulk RNA-seq | Population average | High | Endometrial receptivity biomarkers [1] |
| Single-Cell RNA-seq | Single-cell | Moderate | Sperm and oocyte development, endometrial cell heterogeneity [5] |
| Spatial Transcriptomics | Single-cell with spatial context | Moderate | Embryo implantation, placental development [6] |
| Microarrays | Population average | High | Historical studies of menstrual cycle gene expression |
Experimental Workflow for Single-Cell RNA Sequencing
- Single-Cell Isolation: Tissue dissociation and cell sorting using FACS or microfluidics
- Cell Barcoding: Labeling individual cells with unique barcodes (e.g., 10x Genomics)
- cDNA Synthesis: Reverse transcription and amplification
- Library Preparation: Fragmentation and adapter addition
- Sequencing: High-throughput sequencing on Illumina platforms
- Bioinformatic Analysis:
- Quality control (FastQC)
- Alignment (STAR, HISAT2)
- Cell clustering (Seurat, Scanpy)
- Differential expression analysis
Reproductive Biology Applications Transcriptomic analyses have identified biomarkers of endometrial receptivity, with meta-analyses revealing 57 potential biomarkers including SPP1, PAEP, and GPX3 [1]. Single-cell transcriptomics has enabled the characterization of cellular heterogeneity in reproductive tissues, providing insights into mechanisms behind reproductive tract dysfunction [5].
Proteomics
Definition and Scope Proteomics involves the large-scale study of proteins, including their structures, functions, modifications, and interactions [3]. Unlike the static genome, the proteome is highly dynamic and changes in response to environmental stimuli and cellular states [3].
Methodological Approaches
Mass Spectrometry-Based Proteomics
- Bottom-Up Proteomics: Analysis of proteolytically digested peptides
- Top-Down Proteomics: Analysis of intact proteins
- Data-Independent Acquisition (DIA): Comprehensive peptide fragmentation
- Data-Dependent Acquisition (DDA): Targeted fragmentation of most abundant peptides
Protein Microarrays: High-throughput detection of protein abundances and interactions
Experimental Workflow for LC-MS/MS Proteomics
- Protein Extraction: Lysis of tissue or cells in appropriate buffer
- Digestion: Cleavage with trypsin or other proteases
- Fractionation: Separation by liquid chromatography (LC)
- Ionization: Electrospray ionization (ESI)
- Mass Analysis: Tandem mass spectrometry (MS/MS)
- Database Search: Protein identification using search engines (MaxQuant, Proteome Discoverer)
- Quantification: Label-free or isobaric labeling (TMT, iTRAQ) methods
Reproductive Biology Applications Proteomics has identified potential biomarkers for endometrial receptivity and polycystic ovary syndrome (PCOS) [1]. Large-scale studies have demonstrated that proteins outperform other omics biomarkers for predicting complex diseases, with as few as five proteins achieving area under the curve (AUC) values of 0.79-0.84 for disease incidence and prevalence [7]. In reproductive cancers, proteomic analyses have revealed differentially expressed proteins that may serve as diagnostic markers or therapeutic targets.
Metabolomics
Definition and Scope Metabolomics focuses on the comprehensive analysis of low molecular weight compounds (typically <1,500 Da) within a biological system [3]. As the closest link to phenotype, metabolomics provides insights into the functional outcomes of cellular processes.
Analytical Platforms
Mass Spectrometry (MS)
- Liquid Chromatography-MS (LC-MS)
- Gas Chromatography-MS (GC-MS)
- Capillary Electrophoresis-MS (CE-MS)
Nuclear Magnetic Resonance (NMR) Spectroscopy
- Provides structural information and absolute quantification
- Minimal sample preparation required
Experimental Workflow for LC-MS Metabolomics
- Sample Preparation: Metabolite extraction using methanol/water/chloroform
- Chromatographic Separation: Reversed-phase or HILIC chromatography
- Mass Spectrometry Analysis: High-resolution mass spectrometry (Orbitrap, Q-TOF)
- Data Preprocessing:
- Peak detection (XCMS, MS-DIAL)
- Retention time alignment
- Peak integration
- Statistical Analysis:
- Multivariate analysis (PCA, PLS-DA)
- Metabolic pathway analysis (MetaboAnalyst)
Reproductive Biology Applications Metabolomic studies have identified metabolic signatures associated with PCOS, endometriosis, and ovarian aging [1]. In assisted reproductive technologies, metabolomic profiling of embryo culture media has been explored as a method for embryo selection. Metabolomics has also been used to determine nutritional differences and identify plant defense metabolites in agricultural applications [3].
Integrative Analysis and Computational Challenges
Multi-Omics Integration Strategies
The integration of multiple omics datasets presents both conceptual and practical challenges. Five distinct strategies have emerged for vertical data integration (combining different omics types) [8]:
- Early Integration: Raw datasets are concatenated into a single matrix before analysis
- Mixed Integration: Each dataset is transformed separately then combined
- Intermediate Integration: Simultaneous integration yielding common and omics-specific representations
- Late Integration: Separate analysis of each omics type with final prediction combination
- Hierarchical Integration: Incorporates prior knowledge of regulatory relationships between omics layers
Special Considerations for Reproductive Biology
Reproductive omics data presents unique challenges due to cyclic hormonal regulation, tissue heterogeneity, and ethical considerations [1]. Systems biology approaches that combine genomics, epigenomics, transcriptomics, proteomics, and metabolomics have been employed to generate computational models of reproductive processes including endometrial receptivity, placental function, and sperm analysis [1].
Spatial transcriptomics technologies have recently been applied to study gametogenesis, embryogenesis, and reproductive pathologies, preserving the spatial context that is often crucial for understanding reproductive tissue function [6].
Table 3: Essential Research Reagents and Computational Tools for Reproductive Omics
| Category | Specific Tools/Reagents | Function/Application | Reproductive Biology Examples |
|---|---|---|---|
| Sequencing Reagents | Illumina Nextera XT, PacBio SMRTbell | Library preparation for genomic, epigenomic, and transcriptomic analysis | Endometrial receptivity sequencing [1] |
| Single-Cell Platforms | 10x Genomics Chromium, BD Rhapsody | Single-cell partitioning and barcoding | Sperm and oocyte development studies [5] |
| Spatial Transcriptomics | 10x Visium, Nanostring GeoMx | Spatial mapping of gene expression | Embryo implantation studies [6] |
| Mass Spectrometry Reagents | TMT isobaric labels, Trypsin | Protein and metabolite identification and quantification | PCOS biomarker discovery [1] |
| Bioinformatic Tools | FastQC, Trimmomatic, Seurat, MaxQuant | Quality control, preprocessing, and analysis of omics data | Reproductive atlas construction [4] [5] |
| Data Repositories | GEO, ArrayExpress, PRIDE | Public data storage and retrieval | Endometriosis gene expression mining [1] |
| Integration Platforms | BioStrand MindWalk, STATegra | Multi-omics data integration | Reproductive pathway analysis [8] [9] |
The omics spectrum represents a powerful framework for investigating the complex molecular interactions that underlie reproductive biology. From the static information contained in the genome to the dynamic functional readouts of the proteome and metabolome, each layer provides complementary insights that, when integrated, can reveal novel mechanisms of reproductive health and disease. As single-cell and spatial technologies continue to advance, and as computational methods for data integration become more sophisticated, reproductomics promises to transform our understanding of reproductive processes and accelerate the development of diagnostic and therapeutic approaches for reproductive disorders.
The successful application of omics technologies in reproductive research requires careful experimental design, appropriate methodological choices, and sophisticated computational analysis. By understanding the strengths, limitations, and appropriate applications of each omics technology, researchers can design studies that effectively address the unique challenges of reproductive biology and contribute to improved reproductive health outcomes.
The integration of high-throughput omics technologies has revolutionized reproductive biology research, enabling unprecedented resolution in studying the molecular underpinnings of development, endocrinology, and disease. These platforms facilitate the comprehensive analysis of biological molecules at unprecedented scale, from genetic variants and epigenetic modifications to protein expression and metabolic profiles. The convergence of sequencing, mass spectrometry, and microarray technologies within reproductive research has accelerated discoveries in gametogenesis, embryo development, implantation failure, and endocrine disorders, providing crucial insights into the complex regulatory networks governing reproductive function [10].
In modern reproductive biology, multi-omics approaches—which integrate data from genomics, transcriptomics, proteomics, and metabolomics—have become particularly valuable for understanding the intricate interplay between different biological layers during critical reproductive events. Workflow management systems like Nextflow have emerged as essential tools for implementing reproducible, scalable bioinformatics pipelines that can handle the vast datasets generated by these technologies [11] [12]. These computational frameworks allow researchers to construct and manage data pipelines that parse, process, and analyze vast datasets across multiple omics disciplines, thereby facilitating the integration of diverse data types essential for comprehensive systems biology approaches to reproductive research [10].
Sequencing Technologies
Fundamental Principles and Methodologies
Sequencing technologies determine the precise nucleotide order of DNA or RNA molecules, providing fundamental insights into genetic architecture, gene expression, and regulatory elements. Next-generation sequencing (NGS) platforms operate on the principle of massive parallel sequencing, enabling the simultaneous analysis of millions to billions of DNA fragments. The core workflow begins with library preparation, where nucleic acid samples are fragmented and adapter sequences are ligated to facilitate amplification and sequencing. Subsequent cluster generation amplifies single DNA molecules onto a solid surface, creating colonies of identical templates that are then sequenced using cyclic reversible termination (Illumina) or other detection methods [13].
For reproductive biology applications, specific sequencing methodologies have proven particularly valuable. Whole-genome sequencing identifies genetic variants and structural variations associated with reproductive disorders and inheritable conditions. RNA sequencing (RNA-seq) profiles transcriptomes without prior knowledge of gene sequences, enabling discovery of novel expressed genes and splice variants critical for gonad development and embryonic gene expression patterns. Targeted sequencing panels focus on genes known to be involved in reproductive processes, providing cost-effective analysis for clinical applications. Epigenomic sequencing approaches such as ChIP-seq and bisulfite sequencing map protein-DNA interactions and DNA methylation patterns that regulate gene expression during gametogenesis and early embryonic development [14] [13].
Experimental Protocols
RNA Sequencing Protocol for Reproductive Tissues:
- Sample Preparation: Homogenize 30-50 mg of reproductive tissue (ovary, testis, endometrium) in TRIzol reagent using a mechanical homogenizer. Isolate total RNA following the manufacturer's protocol, with special attention to prevent RNA degradation.
- RNA Quality Control: Assess RNA integrity using an Agilent Bioanalyzer; samples must have RNA Integrity Number (RIN) >8.0 for optimal results. Quantify RNA concentration using fluorometric methods such as Qubit to ensure accurate measurements.
- Library Preparation: Use 500 ng - 1 μg of high-quality total RNA for library construction. Select poly-A tails for mRNA enrichment using oligo-dT magnetic beads. Fragment mRNA using divalent cations at 94°C for 5-8 minutes. Synthesize cDNA using reverse transcriptase with random hexamer primers. Ligate sequencing adapters with unique dual indexes to enable sample multiplexing.
- Library Quantification and Pooling: Quantify libraries using qPCR with standards for absolute quantification. Normalize libraries to 4 nM and pool equimolarly based on quantification results.
- Sequencing: Load pooled libraries onto the sequencing platform at appropriate concentration (typically 1.8-2.2 pM for Illumina platforms). Perform 75-150 bp paired-end sequencing depending on application requirements. Include 1% PhiX control DNA to improve base calling accuracy for diverse transcriptomes [14] [13].
Data Analysis Workflows
The nf-core framework provides robust, community-supported pipelines for sequencing data analysis. The nf-core/rnaseq pipeline implements best practices for RNA sequencing analysis, utilizing STAR, RSEM, HISAT2, or Salmon for alignment and quantification, followed by extensive quality control metrics [10]. For chromatin accessibility studies, the nf-core/hicar pipeline processes multi-omic data measuring transcriptome, chromatin accessibility, and cis-regulatory chromatin contacts simultaneously [10]. These workflows can be configured for reproductive-specific applications by incorporating appropriate reference genomes and annotation files.
Table 1: Sequencing Platforms and Their Applications in Reproductive Biology
| Platform | Read Length | Throughput | Key Applications in Reproductive Biology | Limitations |
|---|---|---|---|---|
| Illumina NovaSeq | 50-300 bp | 2-6 Tb | GWAS of infertility, transcriptome profiling of embryos, methylation analysis | High equipment cost, longer run times |
| PacBio Sequel | 10-25 kb | 5-50 Gb | Haplotype phasing for inheritance patterns, full-length transcript isoforms | Higher error rate, lower throughput |
| Oxford Nanopore | Up to 2 Mb | 10-50 Gb | Real-time analysis of embryo gene expression, structural variant detection | Higher raw read error rate requires validation |
| Ion Torrent | Up to 400 bp | 1-15 Gb | Rapid screening for known mutations in reproductive disorders | Homopolymer errors, lower throughput |
Figure 1: Next-Generation Sequencing Workflow for Reproductive Biology Applications
Mass Spectrometry Platforms
Fundamental Principles and Methodologies
Mass spectrometry (MS) enables precise identification and quantification of proteins, metabolites, and lipids by measuring the mass-to-charge ratio (m/z) of ionized molecules. The core components of a mass spectrometer include an ion source that converts molecules into gas-phase ions, a mass analyzer that separates ions based on their m/z values, and a detector that records the number of ions at each m/z value. In reproductive biology, liquid chromatography coupled to tandem mass spectrometry (LC-MS/MS) has become the gold standard for proteomic and metabolomic analyses, allowing researchers to investigate protein expression patterns in gametes, embryonic secretomes, and uterine fluid compositions, as well as metabolic changes throughout reproductive cycles [15].
Two primary ionization methods dominate reproductive MS applications: electrospray ionization (ESI), which works well with liquid chromatography separation and is ideal for complex mixtures like reproductive tissue proteomes, and matrix-assisted laser desorption/ionization (MALDI), particularly useful for spatial mapping of molecules in tissue sections of ovaries, testes, or endometrium. Mass analyzers commonly employed include quadrupoles for targeted quantification, time-of-flight (TOF) for high-mass accuracy measurements, and Orbitrap instruments for high-resolution proteomic profiling of reproductive samples. These technologies have enabled comprehensive characterization of the sperm proteome, oocyte maturation markers, implantation-associated proteins, and pregnancy-related metabolic changes [15].
Experimental Protocols
LC-MS/MS Proteomics Protocol for Reproductive Fluids:
- Sample Preparation: Collect uterine fluid, follicular fluid, or seminal plasma by centrifugation at 14,000 × g for 15 minutes at 4°C to remove cells and debris. Precipitate proteins using ice-cold acetone (4:1 ratio) overnight at -20°C. Pellet proteins by centrifugation at 15,000 × g for 15 minutes at 4°C.
- Protein Digestion: Resuspend protein pellets in 8 M urea, 50 mM ammonium bicarbonate. Reduce disulfide bonds with 5 mM dithiothreitol (DTT) at 56°C for 30 minutes. Alkylate with 15 mM iodoacetamide at room temperature for 30 minutes in the dark. Dilute urea concentration to 1.5 M with 50 mM ammonium bicarbonate. Digest with sequencing-grade trypsin (1:50 enzyme-to-protein ratio) overnight at 37°C.
- Peptide Desalting: Acidify digested peptides with 1% formic acid. Desalt using C18 solid-phase extraction cartridges. Condition cartridges with 100% acetonitrile followed by 0.1% formic acid. Load samples, wash with 0.1% formic acid, and elute with 60% acetonitrile/0.1% formic acid. Dry peptides in a vacuum concentrator.
- LC-MS/MS Analysis: Reconstitute peptides in 2% acetonitrile/0.1% formic acid. Separate using a nanoflow LC system with a C18 column (75 μm × 25 cm) with a 60-minute gradient from 5% to 35% acetonitrile in 0.1% formic acid at 300 nL/min. Interface with the mass spectrometer via nanoelectrospray ionization. Acquire data in data-dependent acquisition mode with a top-20 method: full MS scan (300-1600 m/z) at resolution 120,000, followed by MS/MS scans of the most intense precursors at resolution 30,000 [15].
Data Analysis Workflows
The nf-core framework offers specialized pipelines for mass spectrometry data, including nf-core/proteomicslfq for label-free quantification, nf-core/diaproteomics for data-independent acquisition proteomics, and nf-core/metaboigniter for pre-processing of mass spectrometry-based metabolomics data [10]. For metabolomics, the Nextflow4MS-DIAL workflow provides a reproducible solution for liquid chromatography-mass spectrometry metabolomics data processing, supporting software containerization to ensure computational reproducibility [15]. These workflows can be adapted for reproductive biology applications by incorporating appropriate spectral libraries and databases relevant to reproductive tissues and fluids.
Table 2: Mass Spectrometry Platforms and Applications in Reproductive Biology
| Platform Type | Mass Analyzer | Resolution | Key Applications in Reproductive Biology | Throughput |
|---|---|---|---|---|
| LC-ESI-Q-TOF | Quadrupole Time-of-Flight | 40,000 | Endometrial fluid metabolomics, seminal plasma protein profiling | Medium (20-40 samples/day) |
| LC-ESI-Orbitrap | Orbitrap | 240,000 | Phosphoproteomics of signaling pathways in embryos, comprehensive reproductive proteomics | Medium (15-30 samples/day) |
| MALDI-TOF/TOF | Time-of-Flight | 20,000 | Spatial mapping of lipids in ovarian tissue, biomarker discovery | High (100+ samples/day) |
| GC-EI-Q | Quadrupole | 5,000 | Hormone level monitoring, small molecule metabolism in reproductive cycles | High (50-80 samples/day) |
Figure 2: Mass Spectrometry Workflow for Reproductive Biology Applications
Microarray Technologies
Fundamental Principles and Methodologies
Microarray technology enables parallel measurement of thousands to millions of molecular targets simultaneously through hybridization-based detection on solid surfaces. The fundamental principle involves immobilized probe molecules arranged in a grid pattern on a solid substrate, which hybridize with labeled target molecules from biological samples. In reproductive research, DNA microarrays have been extensively used for genotyping single nucleotide polymorphisms (SNPs) associated with reproductive disorders, while gene expression microarrays have profiled transcriptional changes during the menstrual cycle, embryo development, and pathological conditions like endometriosis and polycystic ovary syndrome (PCOS) [13].
Although partially supplanted by sequencing technologies for some applications, microarrays remain relevant in reproductive biology due to their cost-effectiveness, standardized analysis pipelines, and well-established databases for comparison. DNA methylation microarrays specifically designed for epigenetic profiling have provided valuable insights into imprinting disorders and epigenetic reprogramming during gametogenesis and preimplantation development. Protein microarrays have been used to autoantibody profiling in autoimmune reproductive disorders and signal transduction pathway analysis in reproductive cancers. The technology continues to evolve, with newer high-density arrays offering improved coverage of genetic variants and epigenetic markers relevant to reproductive health and disease [13].
Experimental Protocols
Gene Expression Microarray Protocol for Endometrial Tissue:
- RNA Extraction and Quality Control: Homogenize 20-30 mg of endometrial biopsy tissue in RLT buffer using a rotor-stator homogenizer. Isolate total RNA using silica-membrane spin columns with DNase I treatment to remove genomic DNA contamination. Assess RNA quality using Agilent Bioanalyzer; samples must have RIN >7.0. Quantify RNA using UV spectrophotometry (A260/A280 ratio should be 1.8-2.1, A260/A230 >1.8).
- Labeling and Amplification: Use 100-500 ng of total RNA for reverse transcription with oligo(dT) primers incorporating T7 RNA polymerase promoter sequence. Perform in vitro transcription with T7 RNA polymerase in the presence of biotin-labeled ribonucleotides for amplification and labeling. The reaction is incubated at 37°C for 16 hours to generate biotin-labeled complementary RNA (cRNA).
- Fragmentation and Hybridization: Fragment 15 μg of labeled cRNA by metal-induced hydrolysis in 40 mM Tris-acetate, pH 8.1, 100 mM potassium acetate, 30 mM magnesium acetate at 94°C for 35 minutes. Confirm fragmentation by gel electrophoresis (optimal size range: 35-200 nucleotides). Hybridize fragmented, labeled cRNA to the microarray in appropriate hybridization buffer at 45°C for 16 hours in a rotating hybridization oven.
- Washing, Staining, and Scanning: Wash arrays stringently with non-stringent wash buffer (6× SSPE, 0.01% Tween-20, 0.005% Antifoam) followed by stringent wash buffer (100 mM MES, 0.1 M NaCl, 0.01% Tween-20). Stain with streptavidin-phycoerythrin conjugate, followed by antibody amplification with biotinylated anti-streptavidin antibody and a second streptavidin-phycoerythrin stain. Scan arrays using a confocal laser scanner with appropriate excitation and emission wavelengths for phycoerythrin [13].
Data Analysis Workflows
Microarray data analysis typically involves several standardized preprocessing steps including background correction, normalization, and summarization of probe-level data. For gene expression arrays, the Robust Multi-array Average (RMA) algorithm is commonly employed. Differential expression analysis can be performed using linear models with empirical Bayes moderation as implemented in the limma package. For reproductive biology applications, these standard workflows can be implemented through platforms like Omics Pipe, which provides automated processing pipelines for various microarray-based analyses with built-in version control for reproducibility [14] [13].
Table 3: Microarray Platforms and Applications in Reproductive Biology
| Platform Type | Probe Density | Application Specificity | Key Applications in Reproductive Biology | Current Status |
|---|---|---|---|---|
| SNP Genotyping Array | 300,000 - 5 million | Genome-wide association studies | Genetic basis of infertility, preimplantation genetic screening | Widely used |
| Gene Expression Array | 25,000 - 60,000 genes | Transcriptome profiling | Endometrial receptivity assessment, gonad development studies | Being replaced by RNA-seq |
| DNA Methylation Array | 450,000 - 900,000 CpG sites | Epigenome-wide association | Imprinting disorders, epigenetic age of reproductive tissues | Widely used |
| miRNA Expression Array | 1,900 - 2,600 miRNAs | Small RNA profiling | Trophoblast invasion regulation, sperm-borne miRNA characterization | Being replaced by small RNA-seq |
| Protein Array | 9,000 - 21,000 proteins | Autoantibody detection | Anti-sperm antibody profiling, reproductive autoimmune disease | Niche applications |
Figure 3: Microarray Workflow for Reproductive Biology Applications
Integrated Multi-Omics Approaches
Data Integration Strategies
The integration of data from sequencing, mass spectrometry, and microarray technologies enables a comprehensive understanding of reproductive biology that transcends the limitations of single-technology approaches. Multi-omics integration strategies can be classified as conceptual, statistical, or model-based. Conceptual integration involves independent analysis of each omics layer with subsequent biological interpretation combining the findings—this approach has been used to correlate genetic variants with protein expression changes in polycystic ovary syndrome. Statistical integration employs multivariate methods like multiple co-inertia analysis to identify relationships between different omics datasets, revealing coordinated molecular responses during the window of implantation. Model-based integration uses prior knowledge of biological pathways and networks to interpret multi-omics data in the context of established reproductive physiological systems [10].
In reproductive biology, these integrated approaches have uncovered novel regulatory mechanisms in gametogenesis, identified biomarker panels for infertility diagnosis, and revealed molecular subclasses of reproductive cancers with therapeutic implications. The nf-core framework provides dedicated pipelines for multi-omics data analysis, such as nf-core/hicar, which processes data from multi-omic co-assays that simultaneously measure transcriptome, chromatin accessibility, and cis-regulatory chromatin contacts [10]. Such integrated analyses are particularly powerful for studying complex reproductive processes that involve dynamic interactions between different molecular layers, such as follicular development, embryo implantation, and placental formation.
Workflow Management for Reproducibility
Reproducible computational workflows are essential for robust multi-omics research in reproductive biology. Nextflow has emerged as a leading workflow management system that enables reproducible computational workflows through containerization and version tracking [12]. The nf-core community, established in 2018, maintains a curated collection of pipelines implemented according to agreed-upon best-practice standards, characterized by reproducibility, standardization, and rapid result generation [11]. As of February 2025, nf-core includes 124 pipelines covering a broad range of data types, supported by over 2,600 GitHub contributors and more than 10,000 users on nf-core's primary communication platform Slack [11].
These workflows can be configured for specific reproductive biology applications through modular design. Nextflow's Domain-Specific Language (DSL2) allows splitting of complex workflows into smaller modular components, including modules that encapsulate specific computational tasks and subworkflows of orchestrated groups of module tasks, both reusable across multiple workflows [11]. Configuration profiles enable adaptation to different computational infrastructures, from local high-performance computing clusters to cloud environments, ensuring that workflows remain portable across different research environments [16]. This is particularly valuable for reproductive biology research, which often involves collaborative projects across clinical and basic science institutions with varied computational resources.
Computational Implementation
Implementation of multi-omics workflows requires careful configuration of computational resources and software environments. Nextflow configuration is typically managed through nextflow.config files that define parameters, processes, and executor settings separately from the workflow implementation [16]. Process-specific resources can be defined using selectors such as withName or withLabel to apply configurations to specific processes or groups of processes. For example, memory-intensive processes like alignment might be allocated more resources than quality control steps [16].
Software dependencies are managed through container technologies like Docker and Singularity or package managers like Conda. The nf-core pipelines automatically download and use pre-configured containers, ensuring consistent software environments across executions [16]. This containerization approach is crucial for reproducibility in reproductive biology research, where consistent software versions ensure comparable results across studies conducted at different times or in different laboratories. The Nextflow4MS-DIAL workflow exemplifies this approach for mass spectrometry data processing, providing a reproducible solution for liquid chromatography-mass spectrometry metabolomics data through software containerization [15].
Figure 4: Multi-Omics Integration Framework for Reproductive Biology
The Scientist's Toolkit
Table 4: Essential Research Reagent Solutions for Omics Technologies in Reproductive Biology
| Reagent/Category | Specific Examples | Function in Experimental Workflow | Application Notes for Reproductive Biology |
|---|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp DNA Mini Kit, RNeasy Kit, TRIzol | Isolation of high-quality DNA/RNA from diverse sample types | Optimized protocols needed for polysaccharide-rich reproductive tissues (e.g., ovary, placenta) |
| Library Preparation Kits | TruSeq DNA/RNA Library Prep, Nextera Flex | Fragmentation, adapter ligation, and amplification for sequencing | Lower input protocols valuable for limited clinical samples (e.g., endometrial biopsies, single embryos) |
| Mass Spectrometry Grade Solvents | LC-MS/MS grade water, acetonitrile, methanol | Mobile phase preparation, sample reconstitution | Essential for minimizing background noise in sensitive reproductive fluid proteomics |
| Digestion Enzymes | Sequencing-grade trypsin, Lys-C | Protein digestion for bottom-up proteomics | Critical for efficient digestion of complex reproductive tissue proteomes |
| Labeling Reagents | TMT, iTRAQ, biotinylation kits | Multiplexing and detection in various assays | Enable comparative analysis across multiple reproductive conditions or time points |
| Quality Control Kits | Agilent RNA/DNA QC kits, BioRad protein assay | Assessment of sample quality and quantity | Crucial for ensuring data quality from precious reproductive samples |
| Microarray Hybridization Kits | GeneChip Hybridization Wash and Stain Kit | Target hybridization, washing, and staining | Standardized protocols ensure reproducibility across reproductive studies |
| Reference Standards | Mass spectrometry iRT kits, sequencing phage controls | Retention time calibration, instrument performance monitoring | Essential for longitudinal reproductive studies conducted over extended timeframes |
| Software Platforms | Nextflow, nf-core pipelines, Omics Pipe | Workflow management, data analysis, and reproducibility | Community-curated frameworks for reproducible multi-omics analysis in reproductive research [14] [11] |
| Cnk5SS3A5Q | Cnk5SS3A5Q, CAS:748131-14-8, MF:C13H19NO2S, MW:253.36 g/mol | Chemical Reagent | Bench Chemicals |
| Isoscutellarin | Isoscutellarin | Isoscutellarin, a Scutellarin metabolite, is for research applications. This product is for Research Use Only (RUO). Not for human or veterinary diagnosis or therapy. | Bench Chemicals |
The completion of the Human Genome Project in 2003 marked a pivotal transition from the genomic to the post-genomic era, characterized by a fundamental paradigm shift from a gene-centered view to a more holistic understanding of genome function and regulation [17]. This era is defined not merely by the availability of complete genome sequences but by the conceptual redefinition of the gene itself—from a static functional entity to a fluid unit of "genome expression" whose function is determined by physiological and environmental contexts [18]. Where the genomic era focused on sequencing and mapping, the post-genomic era focuses on functional interpretation, leveraging vast biological datasets to understand complex biological systems and translate this knowledge into clinical applications [17] [19].
This paradigm shift has particular significance for reproductive biology, where the integration of multi-omics technologies and bioinformatics is transforming our understanding of fertility, embryonic development, and reproductive disorders. The emergence of translational bioinformatics (TBI) represents the critical bridge between massive genomic data collections and clinically actionable insights, enabling the conversion of biomedical data into predictive, preventive, and proactive health applications in reproductive medicine [20]. This transition has positioned reproductive biology at the forefront of precision medicine, where deep molecular phenotyping enables unprecedented understanding of germ cells, embryonic development, and reproductive pathologies.
The Evolving Conceptual Framework: From Genes to Complex Systems
Redefining Genetic Epistemology
The post-genomic era has witnessed a fundamental rethinking of Mendelian genetics and its application to complex diseases. Where the genomic era operated under a model where genes were viewed as discrete entities with predictable functions, the post-genomic understanding recognizes that "biological family members who share a specific genetic variant may well not have a similar risk for future disease" [18]. This realization has profound implications for both basic research and clinical translation, particularly in reproductive genetics where inheritance patterns have traditionally been interpreted through a Mendelian lens.
The omnigenic model represents one of the most significant theoretical advances of the post-genomic era, proposing that many disease-related traits are modulated by the indirect effects of mutations scattered across the genome rather than clustered within specific candidate genes [19]. This model challenges the reductionist approach of seeking "jackpot" mutations that explain everything and instead embraces the inherent complexity of genetic contributions to phenotypes. For reproductive biology, this means that conditions like polycystic ovary syndrome, endometriosis, and male infertility must be understood as emergent properties of complex networks rather than consequences of single-gene defects.
Beyond Sequence: Environmental Integration and Social Context
Post-genomic science recognizes that genetic information alone is insufficient to explain phenotypic outcomes. Gene-environment interactions have emerged as a critical focus, with studies demonstrating how environmental exposures can shape genomic function and disease risk [19]. For example, an international collaboration discovered that tumors from self-reported Black patients show elevated signatures of whole-genome duplications and linked these patterns to exposure to combustion byproducts associated with poor air quality [19]. This research exemplifies the post-genomic integration of genomic technology, environmental exposure data, and social context to address health disparities.
Reproductive health is particularly susceptible to environmental influences, with research showing how toxins, nutrition, stress, and socioeconomic factors can induce epigenetic modifications that affect fertility and developmental trajectories [18]. The post-genomic framework therefore necessitates the development of new experimental designs that can account for these complex interactions, such as case co-twin studies that control for genetic background while examining environmental influences on epigenetic marks and disease-associated processes [18].
Omics Technologies in Reproductive Biology Research
Multi-Omics Integration in Reproductive Medicine
The post-genomic era has been defined by the rise of multi-omics approaches that integrate various molecular layers to provide a comprehensive view of biological systems. The table below summarizes the core omics technologies and their applications in reproductive biology research:
Table 1: Omics Technologies and Applications in Reproductive Biology
| Omics Technology | Analytical Focus | Key Applications in Reproductive Biology |
|---|---|---|
| Genomics [21] [22] | DNA sequence and variation | Identification of genetic markers for infertility; preimplantation genetic testing; genomic selection in ART |
| Epigenomics [21] [22] | Heritable changes in gene expression without DNA sequence alteration | Analysis of DNA methylation patterns in sperm and oocytes; imprinting disorders; environmental influences on fertility |
| Transcriptomics [21] [22] | RNA expression patterns | Gene expression profiling in embryos; endometrial receptivity testing; molecular subtyping of reproductive cancers |
| Proteomics [21] [22] | Protein abundance, modifications, and interactions | Biomarker discovery for sperm quality; non-invasive embryo selection; therapeutic target identification |
| Metabolomics [21] [22] | Small molecule metabolites and metabolic pathways | Assessment of oocyte and embryo viability; endometrial fluid analysis; monitoring ART outcomes |
The integration of these omics layers has been particularly transformative for assisted reproductive technologies (ART), where they have improved the assessment of germ cells, embryos, and endometrium quality beyond traditional morphological evaluation [21]. For example, transcriptomic analyses of cumulus cells can reveal oocyte competence, while proteomic and metabolomic profiling of embryo culture media offers non-invasive means for embryo selection [21]. These approaches address a critical limitation in reproductive medicine, where morphological assessment alone has proven insufficient for predicting developmental potential.
Single-Cell and Spatial Technologies in Reproductive Research
The emergence of single-cell omics represents a particularly significant advancement for reproductive biology, allowing unprecedented resolution in analyzing the molecular characteristics of individual germ cells and embryos [20]. This technology has enabled researchers to understand the cellular heterogeneity within ovarian and testicular tissues, identify rare cell populations critical for fertility, and trace developmental trajectories from oocyte to embryo at unprecedented resolution.
Spatial transcriptomics extends this capability by mapping gene expression patterns within the architectural context of tissues [23] [24]. For reproductive biology, this means understanding the spatial organization of the endometrium during the implantation window, the cellular microenvironment of developing follicles in the ovary, and the complex tissue interactions in placental development. These technologies move beyond bulk tissue analysis to reveal how positional information influences cellular function in reproductive tissues.
Diagram 1: Spatial transcriptomics workflow for reproductive tissue analysis, enabling mapping of gene expression within tissue architecture.
Translational Bioinformatics: Methodologies and Applications
Analytical Frameworks for Multi-Omics Data Integration
The massive datasets generated by multi-omics technologies require sophisticated bioinformatic pipelines for integration and interpretation. Systems biology approaches have emerged as essential frameworks for understanding the complex networks connecting genetic variation to phenotypic outcomes in reproduction [25] [22]. These approaches utilize machine learning algorithms to identify patterns in high-dimensional data, reconstruct regulatory networks, and predict key molecular players in reproductive processes [20].
One particularly powerful application is the identification of molecular biomarkers for reproductive conditions. Traditional single-analyte biomarkers (like PSA for prostate cancer) have limitations in specificity and predictive value [20]. Bioinformatics enables the development of multiparameter biomarker signatures that integrate genomic, transcriptomic, proteomic, and metabolomic data to improve diagnostic and prognostic accuracy [20]. For example, in male infertility, bioinformatic analysis of multi-omics data has identified molecular signatures that predict sperm function beyond conventional semen analysis parameters [20].
Mendelian Randomization for Causal Inference in Reproductive Health
Mendelian randomization (MR) has emerged as a powerful statistical genetics approach for evaluating causal relationships between biomarkers and disease states in reproductive medicine [26]. MR uses genetic variants as instrumental variables to test whether observed associations between exposures and outcomes are likely to be causal, effectively creating a "natural randomized controlled trial" [26].
In reproductive epidemiology, MR has been applied to resolve questions about the causal effects of hormonal factors on disease risk, the relationship between fertility treatments and long-term health outcomes, and the developmental origins of reproductive disorders. For example, MR studies have helped establish causal relationships between polycystic ovary syndrome and cardiometabolic risk factors, providing insights into the long-term health implications of this common endocrine disorder.
Diagram 2: Mendelian randomization framework for causal inference in reproductive epidemiology.
AI and Machine Learning in Reproductive Bioinformatics
Artificial intelligence and machine learning have become indispensable tools for analyzing the complex datasets generated in post-genomic research [23]. In reproductive medicine, AI algorithms are being applied to diverse challenges including embryo selection in IVF, interpretation of genomic variants in infertility, and prediction of treatment outcomes [20].
Deep learning models have demonstrated remarkable performance in image analysis tasks such as automated assessment of sperm morphology, classification of oocyte quality, and embryo grading based on time-lapse imaging [20]. These applications leverage convolutional neural networks to extract subtle morphological features that may not be apparent to human observers but have predictive value for reproductive potential.
Natural language processing (NLP) approaches are also being applied to extract structured information from unstructured clinical notes and scientific literature, enabling the integration of phenotypic data with molecular profiles to build more comprehensive models of reproductive health and disease [23].
Experimental Protocols and Research Workflows
Comprehensive Multi-Omics Profiling in Reproductive Tissues
The integration of multiple omics technologies requires standardized protocols for sample processing, data generation, and computational analysis. The following workflow outlines a comprehensive approach for multi-omics profiling of reproductive tissues:
Sample Collection and Preparation:
- Collect tissue samples (endometrial biopsy, testicular biopsy, ovarian cortex) under standardized conditions with appropriate consent and ethical approval
- Divide samples for parallel omics analyses: flash-freeze for genomics/transcriptomics, preserve in stabilizing solutions for proteomics, and snap-freeze for metabolomics
- For single-cell analyses, immediately process tissues to create single-cell suspensions using optimized dissociation protocols that preserve cell viability and RNA integrity
Library Preparation and Sequencing:
- Genomics: Extract high-molecular-weight DNA and prepare sequencing libraries using methods appropriate for the application (whole genome, exome, or targeted sequencing)
- Transcriptomics: Extract total RNA, assess quality (RIN > 8), and prepare libraries (bulk RNA-seq or single-cell RNA-seq using platforms like 10x Genomics)
- Epigenomics: Process samples for bisulfite sequencing (WGBS or RRBS) to assess DNA methylation, or use ChIP-seq for histone modifications
- Proteomics: Prepare protein extracts for mass spectrometry analysis, using either data-dependent acquisition (DDA) or data-independent acquisition (DIA) methods
- Metabolomics: Extract metabolites using appropriate solvents for the metabolite classes of interest, with quality control using internal standards
Data Processing and Integration:
- Process raw sequencing data through standardized pipelines (e.g., BWA/GATK for genomics, STAR/featureCounts for transcriptomics, MethylKit for epigenomics)
- Perform quality control at each step using tools like FastQC, MultiQC, and platform-specific QC metrics
- Integrate multi-omics datasets using statistical methods (MOFA, iCluster) or network-based approaches (WGCNA) to identify cross-omic regulatory relationships
Functional Validation Using CRISPR and Stem Cell Models
Bioinformatic predictions from multi-omics analyses require experimental validation to establish causal relationships. CRISPR-based functional genomics provides powerful tools for this validation:
CRISPR Screening in Reproductive Cell Models:
- Design sgRNA libraries targeting candidate genes identified from multi-omics analyses
- Transduce reproductive cell lines (e.g., endometrial cells, ovarian granulosa cells, prostate epithelial cells) with lentiviral sgRNA libraries at appropriate MOI to ensure single integration
- Apply selective pressure relevant to the reproductive phenotype (e.g., hormone treatment, oxidative stress, chemotherapeutic agents)
- Harvest genomic DNA at multiple time points and sequence sgRNA regions to quantify enrichment/depletion
- Analyze results using specialized algorithms (MAGeCK, CERES) to identify genes whose perturbation affects cellular fitness under test conditions
Stem Cell-Based Functional Assays:
- Differentiate human induced pluripotent stem cells (hiPSCs) into reproductive relevant cell types (e.g., ovarian granulosa-like cells, Leydig cells, endometrial stromal cells)
- Introduce candidate genetic variants using CRISPR-Cas9 genome editing
- Assess functional consequences through transcriptomic profiling, hormone production assays, or cellular behavior in response to physiological stimuli
Table 2: Essential Research Reagents for Post-Genomic Reproductive Research
| Reagent Category | Specific Examples | Research Applications |
|---|---|---|
| Sequencing Kits [23] [24] | Illumina NovaSeq X, PacBio Revio, Oxford Nanopore | Whole genome sequencing, long-read sequencing for structural variation, epigenomic profiling |
| Single-Cell Platforms [23] | 10x Genomics Chromium, BD Rhapsody, Parse Biosciences | Single-cell transcriptomics of ovarian/testicular tissues, embryo development atlas creation |
| CRISPR Tools [23] [22] | Cas9 nucleases, base editors, prime editors, sgRNA libraries | Functional validation of infertility genes, gene editing in stem cell models, high-throughput screens |
| Antibodies for Epigenomics [22] | Anti-5mC, anti-histone modifications (H3K4me3, H3K27ac), CUT&Tag kits | ChIP-seq for histone modifications, DNA methylation analysis, chromatin accessibility profiling |
| Mass Spectrometry Kits [21] | TMTpro, SWATH acquisition kits, phospho-enrichment kits | Proteomic analysis of seminal plasma, endometrial fluid, follicular fluid, reproductive tissues |
| Spatial Biology Reagents [24] | 10x Visium, CODEX, MERFISH reagents | Spatial transcriptomics of endometrial biopsies, testicular sections, placental tissue architecture |
Data Management, Security, and Ethical Considerations
Computational Infrastructure for Reproductive Omics Data
The volume and complexity of omics data necessitate robust computational infrastructure and sophisticated data management strategies. Cloud computing platforms like Amazon Web Services (AWS), Google Cloud Genomics, and Microsoft Azure have become essential for storing, processing, and analyzing large-scale genomic and multi-omics datasets [23]. These platforms provide the scalability needed for population-scale reproductive genomics while ensuring compliance with regulatory frameworks like HIPAA and GDPR [23].
The integration of multi-modal data presents particular challenges for data harmonization and interoperability. Successful multi-omics integration requires careful attention to data standards, metadata annotation, and the use of common data models that facilitate combining genomic data with electronic health records, imaging data, and other clinical information [24]. Initiatives like the Alliance for Genomic Discovery are developing frameworks for generating and analyzing hundreds of thousands of genomes together with multimodal phenotypic and multiomic data to accelerate therapeutic target discovery [24].
Ethical Framework for Reproductive Genomics
Reproductive genomics raises distinctive ethical considerations related to consent, privacy, and the potential for genetic discrimination. Genomic data concerning reproductive health carries particular sensitivity because it can reveal information not only about the individual but also about potential future offspring and relatives [18]. The secure handling of this data requires both technical safeguards (encryption, access controls) and robust governance frameworks.
Informed consent processes for reproductive genomic research must address potential incidental findings, data sharing arrangements, and future use of samples and data [18]. Special considerations apply to embryonic and fetal samples, where ethical frameworks continue to evolve alongside technological capabilities. The research community has developed specific guidelines for responsible conduct of reproductive genomic research, emphasizing transparency, participant autonomy, and equitable access to benefits.
Therapeutic Applications and Precision Reproductive Medicine
Genomics-Driven Drug Discovery and Repurposing
The post-genomic era has enabled more efficient drug discovery by leveraging human genetic evidence to identify and prioritize therapeutic targets [26]. Drugs developed with genetic support are significantly more likely to progress through clinical trials to approval, with one study reporting approximately two-fold greater success rates for genetically supported targets [26]. This approach is particularly valuable for drug repurposing, where existing medications can be redirected to new indications based on genetic insights.
In reproductive medicine, this approach has identified potential new applications for existing drugs. For example, bioinformatic analysis revealed that rheumatoid arthritis susceptibility genes were significantly correlated with targets of known RA drugs through protein-protein interaction networks, and further identified CDK4 and CDK6 (targets of approved cancer drugs) as potential therapeutic targets for RA [26]. Similar approaches can be applied to reproductive conditions such as endometriosis, where network-based analysis of disease-associated genes may identify repurposing opportunities from other therapeutic areas.
Personalized Approaches in Reproductive Medicine
Precision reproductive medicine tailors diagnostic and therapeutic strategies to individual molecular profiles rather than applying one-size-fits-all approaches [20]. Examples include:
- Pharmacogenomics in reproductive medicine: Genetic variants influencing metabolism of medications used in ART (e.g., FSH preparations, GnRH analogs) can guide dosage individualization to optimize ovarian stimulation while minimizing risks [20]
- Molecular subtyping of reproductive cancers: Genomic profiling of cancers like prostate, ovarian, and endometrial cancer identifies molecular subtypes with distinct prognostic and therapeutic implications [20]
- Preimplantation genetic testing: Comprehensive molecular analysis of embryos using techniques like next-generation sequencing enables selection of euploid embryos and avoidance of monogenic disorders [21]
The implementation of precision approaches requires the development of clinical decision support systems that integrate molecular data with clinical parameters to generate actionable recommendations at point-of-care. These systems increasingly incorporate machine learning algorithms trained on multi-modal data to improve predictive accuracy and clinical utility.
Future Perspectives and Emerging Trends
Technological Innovations on the Horizon
The post-genomic era continues to evolve with emerging technologies that promise to further transform reproductive biology research and clinical practice:
Single-Cell Multi-Omics: Technologies that simultaneously measure multiple molecular layers (e.g., genome, epigenome, transcriptome, proteome) from the same single cell are revealing new dimensions of cellular heterogeneity in reproductive tissues [24]. These approaches are particularly powerful for studying rare cell populations like primordial germ cells, specific stages of developing gametes, and specialized endometrial cell types.
Spatial Multi-Omics: The integration of spatial context with multi-omics measurements is enabling unprecedented views of tissue organization and cell-cell communication in reproductive organs [24]. These technologies are shedding light on the molecular dialogue between embryos and endometrium during implantation, and the complex tissue remodeling that occurs in the placenta throughout gestation.
Long-Read Sequencing: Advances in long-read sequencing technologies from PacBio and Oxford Nanopore are improving the characterization of structurally complex genomic regions relevant to reproductive health, including regions prone to chromosomal rearrangements and repeat expansions associated with infertility [24].
Challenges and Opportunities in Reproductive Bioinformatics
Despite significant advances, the field faces several important challenges that represent opportunities for future development:
Data Integration Complexity: The integration of diverse omics datasets remains technically challenging, requiring continued development of statistical methods and computational tools that can account for batch effects, different data distributions, and missing data [22]. Successfully addressing these challenges will enable more comprehensive systems biology models of reproductive function and dysfunction.
Health Equity and Diversity: Genomic databases remain disproportionately populated with data from populations of European ancestry, limiting the generalizability of findings and potentially exacerbating health disparities [19]. Concerted efforts to diversify reproductive genomics research populations are essential to ensure that the benefits of post-genomic research are distributed equitably.
Functional Annotation Gap: Despite the wealth of genomic data, there remains a significant gap in understanding the biological function of most genes, particularly in the context of reproductive tissues [19]. Initiatives focused on systematic functional characterization, such as the International Mouse Phenotyping Consortium, provide models for addressing this challenge in reproductive biology.
The continued convergence of technological innovation, analytical sophistication, and clinical translation promises to further advance our understanding of reproductive biology and improve outcomes for individuals and families affected by reproductive disorders. As these advances unfold, the post-genomic era will increasingly deliver on the promise of precision reproductive medicine, transforming how we understand, diagnose, and treat reproductive conditions across the lifespan.
The functioning of a cell is a highly orchestrated process involving multiple interconnected biological layers, from the genetic blueprint to the functional metabolites that drive cellular operations. These processes—including the flow of genetic information, signal transduction, and metabolic pathways—are not isolated but form an elaborate network of interactions that ultimately define the cell's phenotype [27]. Understanding these molecular layers is fundamental to unraveling the complexities of cellular life, and this understanding is being revolutionized by omics technologies. In the context of reproductive biology research, these technologies provide unprecedented insights into the molecular physiology of germ cells, embryos, and the endometrium, thereby offering new diagnostic and therapeutic avenues for managing infertility and improving assisted reproduction techniques [28].
The central dogma of molecular biology outlines the fundamental flow of genetic information: from DNA to RNA to protein. This sequence represents the core principle that guides cellular function and inheritance. However, this linear view is now understood to be part of a much more complex, interconnected system where information flows bidirectionally through various regulatory mechanisms. Epigenetic modifications, including DNA methylation, histone modifications, and regulation by non-coding RNAs, add another layer of control that heritably alters gene expression without changing the underlying DNA sequence [29] [30]. These sophisticated regulatory mechanisms ensure precise control of gene expression in different tissues and at various developmental stages, which is particularly crucial in reproductive processes where precise timing and spatial organization are critical for success.
The Central Dogma: From Genetic Code to Functional Proteins
DNA Replication: The Semi-Conservative Mechanism
DNA replication is a fundamental process that ensures the accurate transmission of genetic information from one generation to the next. This process is semi-conservative, meaning that each newly synthesized DNA molecule consists of one parental strand and one newly synthesized strand [31]. The replication process begins with the enzyme helicase, which unwinds the double helix and separates the two DNA strands by breaking the hydrogen bonds between complementary base pairs. This action creates a replication bubble at the origin of replication. As helicase unzips the DNA, the enzyme topoisomerase relieves the resulting helical tension by cutting and resealing the DNA with fewer twists [31].
The actual synthesis of new DNA strands is catalyzed by DNA polymerase, which links nucleotides together to form a new strand using the pre-existing strand as a template [31]. DNA polymerase always works in a 5' to 3' direction, which has important implications for how the two strands are replicated. The leading strand is synthesized continuously in the same direction as the replication fork movement, while the lagging strand is synthesized discontinuously in the opposite direction as short segments known as Okazaki fragments. These fragments are later joined together by the enzyme DNA ligase to form a continuous strand [31]. The Meselson-Stahl experiment of 1957 provided crucial evidence supporting the semi-conservative model of DNA replication by demonstrating that DNA molecules from bacteria grown in different nitrogen isotopes contained one original and one newly synthesized strand [31].
Transcription: DNA to RNA Synthesis
Transcription is the process by which an RNA sequence is produced from a DNA template. This process is catalyzed by RNA polymerase, which binds to specific promoter sequences on the DNA and initiates the synthesis of messenger RNA (mRNA) [31]. The transcription process occurs in three main stages: initiation, elongation, and termination. During initiation, RNA polymerase binds to the promoter region and begins to unwind the DNA double helix. In the elongation phase, RNA nucleotides are added to the growing RNA strand in the 5' to 3' direction, with complementary base pairing (C-G, A-U) to the template strand of the DNA. The DNA strand used as a template is known as the template or antisense strand (3' to 5'), while the unused DNA strand is called the coding or sense strand (5' to 3') and has the same sequence as the mRNA (with thymine instead of uracil) [31].
In eukaryotic cells, the initial RNA transcript undergoes processing before becoming mature mRNA. This processing includes the removal of non-coding sequences called introns by a complex molecular machine called a spliceosome, and the splicing together of the protein-coding sequences called exons. The processed mRNA then leaves the nucleus through nuclear pores and moves to the cytoplasm, where it directs protein synthesis [31].
Translation: Protein Synthesis on Ribosomes
Translation is the process of protein synthesis in which the genetic information encoded in mRNA is translated into a sequence of amino acids in a polypeptide chain. This process occurs on ribosomes, which are complex molecular machines composed of ribosomal RNA (rRNA) and proteins [31]. The genetic code is written in triplets of bases called codons, with each codon corresponding to one specific amino acid. Transfer RNA (tRNA) molecules serve as adaptors that recognize specific codons on the mRNA and carry the corresponding amino acids. Each tRNA has an anticodon sequence that can recognize and bind to a complementary mRNA codon, and the corresponding amino acid attached to its end [31].
The process of translation occurs in three stages:
- Initiation: The small ribosomal subunit binds to the mRNA strand, and the first tRNA (with the anticodon UAC carrying methionine) recognizes the start codon (AUG). The large ribosomal subunit then joins to form the complete ribosome.
- Elongation: The ribosome moves along the mRNA, and a new complementary tRNA anticodon matches with the next mRNA codon in the aminoacyl (A) site. A condensation reaction occurs, covalently bonding the amino acid in the peptidyl (P) site to the amino acid in the A site. The ribosome then translocates, moving the tRNA in the A site to the P site, and the process repeats.
- Termination: When the ribosome encounters a stop codon (UAA, UAG, or UGA), a release factor binds to the A site, causing the ribosome to dissociate and release the completed polypeptide chain [31].
Table 1: Key Molecular Components of the Central Dogma
| Component | Type | Function |
|---|---|---|
| DNA Polymerase | Enzyme | Catalyzes DNA synthesis during replication [31] |
| RNA Polymerase | Enzyme | Catalyzes RNA synthesis during transcription [31] |
| mRNA | RNA | Carries genetic information from DNA to ribosomes [31] |
| tRNA | RNA | Brings amino acids to ribosomes during translation [31] |
| rRNA | RNA | Structural and functional component of ribosomes [31] |
| Ribosome | Complex | Cellular machinery that catalyzes protein synthesis [31] |
Regulatory Networks: Epigenetics and Non-Coding RNAs
Epigenetic Mechanisms of Gene Regulation
Epigenetics represents a critical layer of regulatory control, defined as "heritable changes in gene expression that occur without any changes in gene sequence" [28]. During human development, there are two critical periods of extensive epigenetic reprogramming: gametogenesis and early pre-implantation development. During these periods, female and male germ cells undergo a process where all imprinting marks are erased from the genome, and then methylation marks are reestablished before fertilization and during early embryonic life [28]. These epigenetic marks are essential for achieving cell-type specific gene expression patterns in different tissues, including X-chromosome inactivation, despite all cells in an organism having the same genotype [28].
The main epigenetic mechanisms include:
- DNA Methylation: This process involves the selective methylation of cytosine within CpG dinucleotides, forming 5-methylcytosine. DNA methyltransferases (DNMTs) catalyze this process, with DNMT1 primarily responsible for maintenance methylation and DNMT3a and DNMT3b responsible for de novo methylation. DNA methylation is generally associated with gene silencing, while demethylation is associated with gene activation [30].
- Histone Modifications: Histone proteins can undergo various post-translational modifications, including methylation, acetylation, phosphorylation, and ubiquitination. These modifications constitute a sophisticated "histone code" that influences chromatin structure and gene expression. For example, methylation of H3K9, H3K27, and H4K20 are typically repressive marks associated with heterochromatin formation, while methylation of H3K4 and H3K36 are activation marks. Similarly, acetylation of lysine residues on histones H3 and H4 is associated with chromatin activation, while deacetylation leads to chromatin compression and gene silencing [30].
- Other Modifications: Additional epigenetic mechanisms include post-translational modifications such as phosphorylation, ubiquitylation, nitrosylation, and sumoylation in germ cells [28].
Non-Coding RNAs as Epigenetic Regulators
Non-coding RNAs (ncRNAs) represent a diverse class of RNA molecules that do not encode proteins but play crucial regulatory roles in epigenetic control. These can be broadly divided into short-chain non-coding RNAs and long non-coding RNAs (lncRNAs) [30].
Table 2: Major Types of Regulatory Non-Coding RNAs
| ncRNA Type | Size | Primary Function |
|---|---|---|
| siRNA | 19-24 nt | Transcriptional gene silencing via DNA methylation and histone modification [30] |
| miRNA | 19-24 nt | Post-transcriptional gene regulation through target mRNA degradation or translational repression [30] |
| piRNA | 26-31 nt | Silencing of transposable elements in germline cells [29] |
| lncRNA | >200 nt | Diverse regulatory functions including chromatin modification and genomic imprinting [29] [30] |
Small Interfering RNAs (siRNAs) are derived from long double-stranded RNA molecules that are cleaved by the Dicer enzyme into 19-24 nucleotide fragments. These fragments exercise their functions when loaded onto Argonaute (AGO) proteins [30]. siRNA can lead to transcriptional gene silencing (TGS) through DNA methylation and histone modification. For example, Zhou et al. demonstrated that siRNA could silence EZH2 (a histone methyltransferase) and reverse cisplatin resistance in human non-small cell lung and gastric cancer cells [30].
MicroRNAs (miRNAs) are single-stranded RNAs of approximately 19-24 nucleotides, about 50% of which are located in chromosomal regions prone to structural changes [30]. miRNAs are processed from hairpin-shaped precursor molecules by the enzymes Drosha and Dicer. The current model suggests that the regulatory mechanism of miRNA depends on the degree of complementarity between the specific loading protein AGO, the miRNA, and the target mRNA. Most miRNAs are only partially complementary to their target mRNAs, typically with 6-7 nucleotides of complementarity in the "seed region" at the 5' end, which is the most critical factor in target selection [30].
The emerging role of non-coding RNAs in epigenetic regulation highlights the complex interplay between different molecular layers, with RNA molecules feeding back into the epigenetic regulatory network to fine-tune gene expression patterns in development and disease [29] [30].
Metabolic Pathways: Cellular Energy and Building Blocks
Fundamentals of Metabolic Pathways
In biochemistry, a metabolic pathway is defined as a linked series of chemical reactions occurring within a cell, where the reactants, products, and intermediates (collectively known as metabolites) are modified by a sequence of chemical reactions catalyzed by enzymes [32]. In most metabolic pathways, the product of one enzyme acts as the substrate for the next, creating an interconnected network of chemical transformations. These pathways are fundamental to cellular operation, allowing cells to harvest energy from nutrients, synthesize building blocks for macromolecules, and maintain homeostasis [32] [33].
Metabolic pathways can be conceptually divided into three main categories:
- Catabolic Pathways: These are degradative pathways that break down complex molecules into simpler ones, releasing energy in the process. Catabolism provides the energy required for cellular functions through the production of energy carriers such as ATP, GTP, NADH, NADPH, and FADH2 from energy-containing sources like carbohydrates, fats, and proteins [32].
- Anabolic Pathways: These are biosynthetic pathways that construct complex macromolecules from simpler precursors, requiring an input of energy. Anabolic pathways use the energy produced by catabolic pathways to synthesize polypeptides, nucleic acids, proteins, polysaccharides, and lipids [32].
- Amphibolic Pathways: These pathways can function either catabolically or anabolically depending on the cell's energy needs and substrate availability. The citric acid cycle (Krebs cycle) and the glyoxylate cycle are prime examples of amphibolic pathways [32].
Key Metabolic Pathways and Their Regulation
Different metabolic pathways function in specific compartments within eukaryotic cells. For instance, the electron transport chain and oxidative phosphorylation occur in the mitochondrial membrane, while glycolysis, the pentose phosphate pathway, and fatty acid biosynthesis occur in the cytosol [32]. This compartmentalization allows for efficient regulation and coordination of metabolic processes.
Some of the major metabolic pathways include:
- Glycolysis: This catabolic pathway breaks down glucose into pyruvate and occurs in the cytosol. It was the first metabolic pathway discovered and results in a net gain of ATP and NADH. Glycolysis is regulated by feedback inhibition, with certain reactions running in reverse (gluconeogenesis) to produce glucose 6-phosphate when energy sources are abundant [32].
- Cellular Respiration: This core set of energy-producing catabolic pathways includes glycolysis, the citric acid cycle, and oxidative phosphorylation. While all cells can perform anaerobic respiration via glycolysis, most organisms can perform more efficient aerobic respiration through the citric acid cycle and oxidative phosphorylation [32].
- Gluconeogenesis: This anabolic pathway is essentially the reverse of glycolysis and occurs in the liver and sometimes in the kidney to maintain proper glucose concentration in the blood. Although similar to the reverse pathway of glycolysis, it contains four distinct enzymes (pyruvate carboxylase, phosphoenolpyruvate carboxykinase, fructose 1,6-bisphosphatase, glucose 6-phosphatase) that allow the pathway to occur spontaneously [32].
The flux of metabolites through metabolic pathways is tightly regulated to maintain homeostasis. The entire pathway's flux is regulated by rate-determining steps, which are typically the slowest steps in the network of reactions. These rate-limiting steps usually occur near the beginning of the pathway and are regulated by feedback inhibition, controlling the pathway's overall rate [32]. Metabolic regulation occurs through covalent or non-covalent modifications of enzymes, with the metabolic flux being regulated based on the stoichiometric reaction model, metabolite utilization rate, and the translocation pace of molecules across membranes [32].
Diagram 1: Integration of signaling and metabolic pathways
Integration of Molecular Layers: Signaling, Regulation, and Metabolism
Interconnected Cellular Processes
The phenotype of a cell results from the interoperation of three different layers of biological processes: metabolism, gene regulation, and signaling, which are tightly interconnected through diverse interactions [27]. Signaling networks are activated by external signals, such as ligands binding to receptors on the cell membrane. These signals are then propagated inside the cell through mechanisms like protein phosphorylation cascades, which can lead to alterations in gene expression by activating or inhibiting transcription factors [27]. Gene regulatory networks control the transcriptional level of genes and thus the production of mRNA molecules, which are subsequently translated into proteins. These proteins are involved in various cellular functions, including signal transduction and the catalysis of metabolic reactions [27].
Specific metabolites can also influence protein activity (e.g., through allosteric binding) and gene regulation, creating complex feedback loops [27]. An excellent example of this integration is the regulation of blood sugar in humans by the liver, which releases or stores glucose in response to extracellular signals like insulin and glucagon. These hormonal signals are synthesized and released from pancreatic cells in a glucose-dependent manner, and their information is decoded by liver cells via signaling and regulatory processes that ultimately affect metabolic fluxes [27].
Mathematical Modeling of Integrated Systems
Mathematical modeling has become a key methodology for understanding these complex biological interactions and predicting cellular phenotypes under different conditions. However, due to the complexity involved, signaling, gene expression, and metabolism are often modeled separately using different mathematical formalisms suited to each domain's specific characteristics [27].
Various modeling approaches include:
- Ordinary Differential Equations (ODEs): These describe underlying biochemistry in detail and have high explanatory power but face limitations in scalability and parameter acquisition for genome-scale models.
- Boolean Networks: These simple representations identify node states as either active/on or inactive/off and can reveal important structural features of signaling pathways despite their simplicity.
- Constraint-Based Models: These approaches, including flux balance analysis (FBA), are used for larger networks like metabolic pathways where they can predict flux distributions through the network [27].
Integrated models that connect these different layers face significant challenges but represent the future of systems biology. Such integrated approaches could be particularly powerful tools for studying genotype-phenotype relationships and how they are affected by specific conditions or perturbations, with important applications in biotechnology, biomedicine, and pharmaceutical research [27].
Omics Technologies in Reproductive Biology Research
Multi-Omics Approaches and Applications
The emergence of omics technologies has revolutionized reproductive biology research by providing comprehensive tools to study the molecular physiology of germ cells, embryos, and endometrium—the three key components conditioning reproductive success [28]. These omics approaches include epigenomics, genomics, transcriptomics, proteomics, and metabolomics, which together offer a holistic view of the complex biological systems involved in reproduction [28] [22].
Table 3: Omics Technologies and Their Applications in Reproductive Biology
| Omics Technology | Analysis Focus | Key Techniques | Reproductive Applications |
|---|---|---|---|
| Epigenomics | Heritable changes in gene expression without DNA sequence changes [28] | Bisulfite sequencing, Pyrosequencing [28] | Analysis of imprinting disorders, embryonic development [28] |
| Genomics | Complete set of genes and their functions [28] | FISH, CGH arrays, SNPs arrays [28] | Identification of genetic variants affecting fertility [22] |
| Transcriptomics | Complete set of RNA transcripts [28] | mRNA microarrays, RT-PCR [28] | Gene expression patterns in oocytes, embryos, endometrium [28] [22] |
| Proteomics | Comprehensive study of proteins and their functions [28] | 2D-PAGE, HPLC, LC-MS/MS [28] | Biomarker identification for oocyte/embryo quality [28] [22] |
| Metabolomics | Simultaneous study of metabolite concentrations and fluctuations [28] | GC-MS, LC-MS, NMR [28] | Assessment of embryo viability through culture media analysis [28] |
In assisted reproduction, omics technologies help define the optimal molecular traits of cells and tissues involved in reproduction, including spermatozoa, oocytes, granulosa cells, embryos, and endometrium, as well as their metabolic products in seminal plasma, follicular fluid, and culture media [28]. This systems biology approach can identify the best spermatozoa and oocytes for fertilization and the best embryos for implantation, ultimately improving assisted reproduction success rates [28].
Epigenomics in Assisted Reproduction
Epigenetic modifications are particularly important in reproductive biology because they play crucial roles during two critical periods of epigenetic reprogramming in human development: gametogenesis and early pre-implantation development [28]. During these periods, female and male germ cells undergo a process where all imprinting marks are erased from the genome, and then methylation marks are reestablished before fertilization and during early embryonic life [28].
The association between assisted reproductive technologies (ART) and imprinting disorders has gained increasing attention in recent years. Children conceived through ART appear to have an increased incidence of rare genomic imprinting diseases such as Beckwith-Wiedemann syndrome (related to hypomethylation of the maternal KCNQ1OT1 DMR), Angelman's syndrome (caused by a shortage of maternal UBE3A expression), and Silver-Russell Syndrome (often caused by H19 DMR hypomethylation) [28]. However, it remains unclear whether these adverse effects result from ART techniques themselves or are a consequence of parental subfertility [28].
Environmental factors also significantly impact reproductive epigenetics. Endocrine-disrupting chemicals (EDCs) such as tobacco, pesticides, drugs, and plasticizers have been associated with perturbations in DNA methylation patterns [28]. The timing of epigenetic programming establishment differs between male and female germ cell differentiation, occurring earlier in the male germ line (prospermatogonia stage) than in the female germ line (after birth when oocytes grow), making them potentially more vulnerable to EDC effects [28].
Experimental Approaches and Research Tools
Key Experimental Methodologies
Studying the molecular layers from DNA to metabolites requires diverse experimental approaches tailored to each biological level. For epigenomic analysis, techniques such as bisulfite sequencing are used to analyze DNA methylation, the most common epigenetic marker [28]. Pyrosequencing provides a quantitative approach for assessing methylation levels at specific genomic loci [28].
Genomic analyses employ fluorescence in situ hybridization (FISH) for chromosomal visualization, comparative genomic hybridization (CGH) arrays for detecting copy number variations, and single nucleotide polymorphism (SNP) arrays for identifying genetic variants associated with reproductive traits [28]. Transcriptomic studies utilize mRNA microarrays and real-time polymerase chain reaction (RT-PCR) to profile gene expression patterns in reproductive tissues and cells [28].
Proteomics technologies include separation techniques such as one-dimensional and two-dimensional polyacrylamide gel electrophoresis (1D-/2D-PAGE), two-dimensional differential gel electrophoresis (2D-DIGE), high-pressure liquid chromatography (HPLC), and various mass spectrometry methods including reverse-phase liquid chromatography tandem mass spectrometry (RP-LC-MS/MS) [28]. Metabolomics employs gas chromatography-mass spectrometry (GC-MS), liquid chromatography-mass spectrometry (LC-MS), and nuclear magnetic resonance (NMR) spectroscopy to profile metabolites in biological samples relevant to reproduction [28].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Molecular Layer Analysis
| Reagent/Technology | Category | Primary Function |
|---|---|---|
| DNA Polymerase | Enzyme | Catalyzes DNA synthesis during replication and PCR amplification [31] |
| RNA Polymerase | Enzyme | Catalyzes RNA synthesis during transcription [31] |
| Helicase | Enzyme | Unwinds DNA double helix during replication [31] |
| Restriction Enzymes | Enzyme | Cut DNA at specific sequences for molecular cloning |
| Reverse Transcriptase | Enzyme | Synthesizes cDNA from RNA templates for transcriptomics |
| DNA Methyltransferases | Enzyme | Catalyzes DNA methylation for epigenetic studies [30] |
| Bisulfite Reagents | Chemical | Converts unmethylated cytosines to uracils for methylation analysis [28] |
| Antibodies | Biological | Detect specific proteins (Western blot) or histone modifications (ChIP) |
| Fluorescent Dyes | Chemical | Label nucleic acids, proteins, or metabolites for detection |
| Mass Spectrometry Standards | Chemical | Internal standards for quantitative proteomics and metabolomics [28] |
| Cell Culture Media | Biochemical | Support growth of gametes and embryos in vitro [28] |
| CRISPR-Cas9 System | Molecular Tool | Gene editing for functional studies [22] |
| 2-Ethyl-4-methylpiperidine | 2-Ethyl-4-methylpiperidine | High-purity 2-Ethyl-4-methylpiperidine (CAS 1492331-31-3) for research, such as LOHC studies. For Research Use Only. Not for human or veterinary use. |
| 2-Bromo-3-phenylquinoline | 2-Bromo-3-phenylquinoline, MF:C15H10BrN, MW:284.15 g/mol | Chemical Reagent |
Diagram 2: Integrated multi-omics workflow for reproductive biology
The journey from DNA blueprint to functional metabolites represents a sophisticated, multi-layered biological system where genetic information flows through various molecular pathways and is extensively regulated at multiple levels. Understanding these molecular layers—from DNA replication and transcription to translation, protein function, and metabolic pathways—provides crucial insights into the fundamental processes of life. The integration of omics technologies in reproductive biology research has particularly transformed our understanding of reproductive processes, offering new avenues for diagnosing and treating infertility. As these technologies continue to evolve and improve, they hold the promise of further enhancing our comprehension of the complex molecular networks that govern reproduction and ultimately improving outcomes in assisted reproduction and livestock biotechnology. The future of reproductive research lies in the continued development and integration of these multi-omics approaches, coupled with advanced computational models that can handle the complexity and dynamics of biological systems across different molecular layers.
The application of single-cell and spatial omics technologies is revolutionizing reproductive biology research by providing unprecedented resolution into cellular heterogeneity, molecular dynamics, and spatial organization within reproductive tissues. These advanced profiling technologies have enabled researchers to decipher complex cellular landscapes in ovaries, endometrium, placenta, and reproductive pathologies at a level of detail previously unattainable with bulk sequencing approaches. This technical guide comprehensively explores the methodological frameworks, experimental protocols, and analytical approaches that leverage single-cell and spatial omics to uncover novel biological insights into reproductive processes, from gametogenesis and embryo development to reproductive disorders and therapeutic development. By integrating multi-omics data at cellular resolution, researchers can now identify rare cell populations, delineate cellular developmental trajectories, characterize cellular communication networks, and map spatially restricted molecular patterns critical for reproductive function. This whitepaper synthesizes current methodologies, applications, and technical considerations for implementing these cutting-edge technologies within reproductive biology research programs, with particular emphasis on their transformative potential for understanding disease mechanisms and advancing diagnostic and therapeutic innovation.
Single-cell and spatial omics technologies represent a paradigm shift in reproductive biology research, enabling the systematic characterization of cellular heterogeneity and tissue organization that underlies reproductive function and dysfunction. These approaches have revealed that reproductive tissues contain diverse cell types and states that exhibit specialized functions based on their spatial positioning and molecular profiles [6]. The integration of these technologies provides a comprehensive framework for understanding how cellular interactions within their native tissue architecture coordinate complex processes such as folliculogenesis, endometrial cycling, embryo implantation, and placental development [6] [34].
The fundamental advantage of single-cell approaches over traditional bulk sequencing lies in their ability to resolve the cellular heterogeneity that averages out in population-level measurements. When applied to reproductive tissues, these technologies have identified previously uncharacterized cell subtypes, rare progenitor populations, and dynamic transitional states that are critical for reproductive success [35]. Meanwhile, spatial omics techniques preserve the architectural context of cells, revealing how positional information influences cellular identity and function in reproductive systems [6] [36]. Together, these approaches provide complementary layers of information that are particularly valuable for understanding the complex, multi-cellular interactions that define reproductive processes.
Technological Foundations and Methodological Approaches
Single-Cell Omics Platforms
Single-cell omics encompasses a suite of technologies that measure various molecular layers at individual cell resolution. Single-cell RNA sequencing (scRNA-seq) enables comprehensive profiling of transcriptional states across thousands of individual cells, revealing cell-to-cell heterogeneity in gene expression patterns within reproductive tissues [34] [37]. The foundational scRNA-seq workflow begins with tissue dissociation into single-cell suspensions, followed by cell capture, reverse transcription, cDNA amplification, library preparation, and sequencing [34]. Beyond transcriptomics, single-cell epigenomic approaches such as single-cell ATAC-seq map chromatin accessibility landscapes, providing insights into the regulatory programs that govern cellular identity and function in reproductive tissues [34]. Additionally, multimodal omics approaches like CITE-seq simultaneously measure transcriptome and cell-surface protein expression from the same single cells, offering a more integrated view of cellular identity [34].
Table 1: Single-Cell Omics Technologies and Applications in Reproductive Biology
| Technology | Molecular Target | Key Applications in Reproductive Biology | Considerations |
|---|---|---|---|
| scRNA-seq | mRNA transcripts | Cell type identification, differentiation trajectories, transcriptional heterogeneity | Requires tissue dissociation, loses spatial context |
| scATAC-seq | Accessible chromatin | Regulatory landscape mapping, epigenetic dynamics | Requires freshly isolated nuclei |
| CITE-seq | mRNA + surface proteins | Immunophenotyping, validation of cell identities | Limited to known protein targets |
| Single-cell epigenomics | DNA methylation, histone modifications | Germ cell development, imprinting regulation | Technically challenging, lower throughput |
| Single-cell proteomics | Protein expression | Signaling pathway activity, functional states | Limited multiplexing capacity |
Spatial Omics Platforms
Spatial omics technologies preserve the architectural context of cells within tissues while capturing molecular information, making them particularly valuable for studying the structured organization of reproductive tissues [6] [36]. These approaches can be broadly categorized into imaging-based and sequencing-based methods. Imaging-based spatial transcriptomics techniques utilize in situ hybridization (ISH) or in situ sequencing (ISS) to detect and localize mRNA molecules within intact tissue sections [36]. Commercial platforms such as 10x Genomics' Visium and NanoString's GeoMx enable genome-wide spatial transcriptomics by capturing mRNA onto spatially barcoded arrays [6] [36]. Emerging multi-omics spatial platforms like the Spatial Multi-Omics (SM-Omics) platform combine transcriptomic and proteomic measurements within their spatial context, providing complementary layers of molecular information [36].
Table 2: Spatial Omics Technologies for Reproductive Tissue Analysis
| Technology Type | Examples | Resolution | Advantages | Limitations |
|---|---|---|---|---|
| Imaging-based ISH | MERFISH, seqFISH+ | Subcellular | High resolution, single-cell sensitivity | Targeted approach, limited gene throughput |
| In situ sequencing | ST, HybISS | Subcellular | Whole transcriptome, single-cell | Lower detection efficiency |
| Sequencing-based | 10x Visium, Slide-seq | 10-100 μm | Whole transcriptome, easy implementation | Lower resolution, may not reach single-cell |
| Spatial proteomics | MIBI-TOF, IMC | Subcellular | High-plex protein quantification | Antibody-dependent, limited targets |
| Multi-omics spatial | SM-Omics platform | Cellular to subcellular | Integrated transcriptome + proteome | Complex workflow, data integration challenges |
Spatial Omics Workflow Comparison: This diagram illustrates the two primary methodological approaches for spatial omics analysis, highlighting the parallel pathways for imaging-based and sequencing-based techniques that converge on spatially resolved biological insights.
Experimental Design and Protocol Implementation
Single-Cell Transcriptome and Translatome Sequencing (T&T-seq) in Oocytes
A groundbreaking application of single-cell omics in reproductive research involves the implementation of single-cell T&T-seq to simultaneously profile both transcriptional and translational landscapes in individual oocytes from patients with ovarian endometriosis and control subjects [38]. This innovative approach is particularly valuable for studying oocyte biology because fully developed germinal vesicle (GV)-stage oocytes are transcriptionally silent, making translatome analysis a more accurate reflection of molecular activity than transcriptome sequencing alone [38]. The T&T-seq methodology enables researchers to identify post-transcriptional regulatory mechanisms that govern oocyte maturation and quality.
The experimental workflow for single-cell T&T-seq begins with the careful isolation of GV-stage oocytes from both ovarian endometriosis patients and control subjects with infertility due to tubal or male factors. Each oocyte is individually processed using the T&T-seq protocol, which partitions the transcriptome and translatome from the same single cell [38]. Following sequencing, bioinformatic analysis includes Spearman correlation assessment to verify consistency between biological replicates and principal component analysis (PCA) to evaluate clustering patterns between experimental groups. Differential expression analysis identifies genes that are translationally dysregulated in ovarian endometriosis oocytes despite unchanged transcriptional levels, revealing post-transcriptional regulatory mechanisms [38]. This approach successfully identified 2,480 differentially expressed genes at the translational level in oocytes from ovarian endometriosis patients, with key pathways including "oxidative stress," "oocyte meiosis," and "spliceosome" significantly impacted [38].
Spatial Transcriptomics in Reproductive Tissues
The implementation of spatial transcriptomics in reproductive tissue analysis requires careful experimental design to preserve spatial information while capturing comprehensive molecular profiles. For studies of reproductive tissues such as endometrium, ovaries, or placenta, optimal protocol begins with fresh frozen tissue preservation rather than formalin-fixed paraffin-embedded (FFPE) processing when possible, as this typically yields higher RNA quality [6]. Tissue sections of appropriate thickness (typically 10-20 μm) are mounted onto specialized spatial transcriptomics slides containing thousands of spatially barcoded capture probes [6] [36].
Following tissue mounting, the workflow includes tissue permeabilization to release RNA molecules, which then bind to spatially barcoded oligonucleotides on the array surface. After reverse transcription and library construction, sequencing is performed, and the resulting data undergoes computational reconstruction to map gene expression back to specific spatial coordinates within the tissue architecture [6]. This approach has been successfully applied to characterize the spatial heterogeneity of human endometrium across the menstrual cycle, revealing distinct transcriptional zones and cell-cell communication networks that correlate with functional states [6]. In placental research, spatial transcriptomics has illuminated the complex organizational patterns of trophoblast subtypes and their interactions with maternal decidual cells, providing insights into disorders such as preeclampsia [6] [39].
Analytical Frameworks and Data Integration
Computational Approaches for Single-Cell Data
The analysis of single-cell omics data requires specialized computational approaches designed to handle high-dimensionality, technical noise, and inherent biological variability. Initial processing typically involves quality control metrics to remove low-quality cells, normalization to account for technical variation, and dimensionality reduction using techniques such as PCA or UMAP to visualize cellular relationships [34]. Cell clustering algorithms then identify distinct cell populations, which can be annotated using reference datasets or marker gene expression [34]. More advanced analytical techniques include pseudotemporal ordering to reconstruct cellular differentiation trajectories (e.g., during folliculogenesis or trophoblast development) and cell-cell communication inference to predict signaling interactions between different cell types within reproductive tissues [34].
For the analysis of single-cell T&T-seq data from oocytes, researchers employed specialized analytical frameworks to distinguish four distinct classes of gene regulation: Class I (translationally repressed but transcriptionally constant), Class II (translationally enriched but transcriptionally constant), Class III (downregulated at both levels), and Class IV (upregulated at both levels) [38]. This classification revealed that the majority of affected genes in ovarian endometriosis oocytes fell into Class I and II, demonstrating the predominance of post-transcriptional regulation in determining oocyte quality [38].
Spatial Data Analysis and Integration
The analysis of spatial omics data introduces additional computational challenges related to spatial registration, pattern recognition, and integration with single-cell references. Analytical pipelines for spatial transcriptomics data typically begin with spatial preprocessing to align sequencing data with tissue morphology, followed by spatial clustering to identify tissue domains with similar expression profiles [6] [36]. Spatial pattern detection algorithms can then identify genes with non-random spatial expression distributions, which often have specialized functions in tissue organization and function [6].
A powerful analytical framework for spatial omics data involves integration with single-cell references using computational methods such as cell type deconvolution, which estimates the proportional composition of cell types within each spatial spot [6]. This integrated approach allows researchers to infer the spatial distribution of cell types identified in single-cell data while leveraging the architectural context preserved in spatial datasets. In reproductive biology, this has been particularly valuable for mapping the spatial organization of immune cell populations within the endometrium throughout the menstrual cycle and during embryo implantation [6] [40].
Omics Data Analysis Pipeline: This diagram outlines the core computational workflow for analyzing single-cell and spatial omics data, highlighting the integration between standard analytical steps and advanced specialized analyses that generate biological insights.
Key Applications in Reproductive Biology and Medicine
Understanding Reproductive Disorders
Single-cell and spatial omics have provided transformative insights into the pathophysiology of reproductive disorders such as endometriosis and polycystic ovary syndrome (PCOS). In endometriosis research, single-cell transcriptomics of ectopic and eutopic endometrial tissues has revealed distinct immune cell profiles and pathogenic mechanisms between endometriomas and peritoneal lesions [34]. Specifically, these approaches have identified specific macrophage attributes that contribute to endometriosis pathogenesis, revealing potential cellular targets for novel therapeutic interventions [34]. Similarly, in PCOS, single-cell analyses have uncovered aberrant stromal-immune interactions and theca cell dysfunction that contribute to the hyperandrogenic microenvironment characteristic of this disorder [39].
The application of single-cell T&T-seq to oocytes from ovarian endometriosis patients exemplifies how these technologies can elucidate molecular mechanisms underlying reproductive dysfunction. This approach demonstrated that oocytes from ovarian endometriosis patients exhibit significant alterations in global translational activity, with key pathways such as "oxidative stress," "oocyte meiosis," and "spliceosome" disruption contributing to poor oocyte quality [38]. Protein-protein interaction analysis of translationally downregulated genes identified hub genes including CCNB1, CDK1, CHEK1, and AURKB, which are critical regulators of oocyte meiosis and cell cycle progression [38].
Advancing Assisted Reproductive Technologies
Single-cell omics technologies are revolutionizing assisted reproductive technologies (ART) by providing unprecedented insights into the molecular mechanisms underlying oocyte competence, embryonic development, and endometrial receptivity [34] [22]. Comprehensive molecular profiling of individual oocytes and embryos has identified biomarkers of developmental potential that could significantly improve embryo selection in in vitro fertilization (IVF) [34]. In endometrial receptivity assessment, single-cell transcriptomics has revealed precise molecular signatures that distinguish receptive from non-receptive endometrium, potentially offering more accurate timing for embryo transfer than current morphological approaches [34].
Spatial omics technologies further enhance ART applications by preserving the architectural context of endometrial tissue, enabling researchers to investigate how spatial organization and cell-cell communication networks within the endometrium contribute to successful embryo implantation [6]. These approaches have identified specific endometrial regions and cellular neighborhoods that exhibit specialized transcriptional programs during the window of implantation, potentially leading to more targeted assessment of endometrial receptivity [6].
Table 3: Key Research Reagent Solutions for Reproductive Tissue Single-Cell and Spatial Omics
| Reagent/Category | Specific Examples | Function in Experimental Workflow | Reproductive Biology Applications |
|---|---|---|---|
| Tissue Dissociation Kits | Miltenyi Biotec GentleMACS, Worthington collagenase | Tissue digestion into single-cell suspensions | Ovary, testis, endometrium dissociation |
| Cell Viability Stains | Propidium iodide, DAPI, Calcein AM | Discrimination of live/dead cells | Assessment of gamete and embryo quality |
| Surface Protein Antibodies | TotalSeq, CITE-seq antibodies | Immunophenotyping alongside transcriptomics | Immune cell profiling in endometrium |
| Spatial Capture Slides | 10x Visium slides, NanoString GeoMx | Spatial barcoding of mRNA transcripts | Endometrial mapping, placental organization |
| Nuclei Isolation Kits | Nuclei EZ Prep, Nuclei PURE | Isolation of intact nuclei for sequencing | Archived tissues, hard-to-dissociate samples |
| Single-Cell Library Preps | 10x Chromium, SMART-seq2 | Amplification of single-cell transcriptomes | Oocyte and embryo transcriptome profiling |
| In Situ Hybridization Probes | MERFISH, seqFISH code sets | Multiplexed RNA imaging in tissue context | Spatial gene expression in reproductive tissues |
Pregnancy and Placental Research
In pregnancy research, single-cell and spatial omics have enabled comprehensive characterization of the maternal-fetal interface, revealing extraordinary cellular complexity and dynamic remodeling throughout gestation [6] [39]. Single-cell analyses of first-trimester placenta have identified previously unrecognized trophoblast subtypes and their differentiation trajectories, while spatial transcriptomics has mapped the precise organization of these subsets within the placental architecture [6]. These approaches have provided new insights into pregnancy disorders such as preeclampsia and fetal growth restriction, revealing disruptions in trophoblast differentiation pathways and immune cell interactions at the maternal-fetal interface [39].
Comparative analyses of term and preterm placental samples using single-cell approaches have identified distinct cellular gene signatures associated with pregnancy complications, offering potential biomarkers for early detection and intervention [34]. Spatial transcriptomics has further elucidated the microenvironmental factors that contribute to preterm birth by characterizing the cellular and molecular changes in fetal membranes and uterine tissues associated with premature labor [6] [39].
Technical Challenges and Future Directions
Current Methodological Limitations
Despite their transformative potential, single-cell and spatial omics technologies face several technical challenges when applied to reproductive tissues. The requirement for fresh, high-quality starting material can be particularly limiting for studies of human reproductive tissues, which are often difficult to obtain and process immediately [34]. Tissue heterogeneity introduces additional complications, as reproductive tissues such as the ovary or endometrium contain diverse structural regions and cell types with different physical properties that complicate complete dissociation into representative single-cell suspensions [34]. For spatial omics approaches, current limitations in resolution sensitivity remain significant barriers, as many commercial spatial transcriptomics platforms do not achieve true single-cell resolution and may fail to detect low-abundance transcripts that are functionally important in reproductive processes [6] [36].
The computational challenges associated with data integration across multiple omics layers, donors, and timepoints present additional hurdles, particularly for dynamic reproductive processes that involve cyclic remodeling (e.g., menstrual cycle) or rapid developmental transitions (e.g., early embryogenesis) [34] [39]. Analytical methods for spatial data continue to evolve, but currently lag behind the rapid pace of technological development in spatial omics [6]. Furthermore, the high costs associated with both single-cell and spatial omics platforms can limit their accessibility and sample throughput, potentially constraining statistical power and generalizability of findings in reproductive research [34].
Emerging Innovations and Future Applications
The field of single-cell and spatial omics is rapidly evolving, with several emerging technologies poised to address current limitations and open new frontiers in reproductive biology. Multi-omic integration approaches that simultaneously measure transcriptome, epigenome, and proteome from the same single cells are providing more comprehensive views of cellular identity and regulatory mechanisms in reproductive tissues [34] [37]. Advances in spatial resolution through technologies such as multiplexed error-robust fluorescence in situ hybridization (MERFISH) and expansion sequencing are beginning to enable nanoscale mapping of molecular distributions within subcellular compartments [6].
The integration of artificial intelligence and machine learning with single-cell and spatial omics data holds particular promise for reproductive biology, enabling predictive modeling of developmental trajectories, identification of novel cellular biomarkers for diagnostic applications, and discovery of therapeutic targets for reproductive disorders [39] [37]. These computational approaches can leverage large-scale single-cell atlases of reproductive tissues to identify subtle disease-associated perturbations that might be overlooked in conventional analyses [39].
Future applications in reproductive medicine will likely include the development of clinical diagnostic tools based on single-cell or spatial profiling of endometrial receptivity, oocyte competence, or placental function that could personalize and optimize fertility treatments [34]. In drug development, single-cell technologies are already enabling more precise target identification by resolving cell-type-specific disease mechanisms in conditions such as endometriosis and PCOS, potentially leading to more effective and targeted therapeutics [35] [37]. As these technologies continue to mature and become more accessible, they are poised to fundamentally transform both basic reproductive research and clinical practice in reproductive medicine.
From Bench to Bedside: Methodological Applications of Omics in Clinical Reproduction
The field of assisted reproductive technology (ART) is undergoing a fundamental transformation, moving from subjective morphological assessments to data-driven, predictive approaches for embryo viability evaluation. In vitro fertilization (IVF) success rates have historically been limited, with approximately only 30% of cycles resulting in clinical pregnancy based on traditional selection methods [41]. This limitation stems primarily from the subjective nature of conventional embryo assessment, which relies on visual evaluation of morphological characteristics by embryologists—an approach characterized by significant inter- and intra-observer variability [42]. The emergence of artificial intelligence (AI) and multi-omics technologies represents a paradigm shift within reproductive biology, enabling unprecedented precision in predicting embryo implantation potential and developmental competence.
This transformation holds particular significance for populations facing substantial genetic disease burdens. In countries like India, where between 50 to 100 million people are affected by inherited genetic disorders such as thalassemia, sickle cell anemia, and Fragile X syndrome, these advanced technologies offer immense promise for reducing disease transmission through improved embryo selection [43]. The integration of computational biology with reproductive medicine is thus not merely enhancing existing practices but fundamentally redefining the parameters of embryo assessment within the broader context of omics technologies in reproductive biology research.
Traditional Challenges in Embryo Assessment
Limitations of Morphological Evaluation
Conventional embryo assessment primarily utilizes standardized grading systems, such as the Gardner criteria, which evaluate developmental stage, inner cell mass (ICM) quality, and trophectoderm (TE) characteristics [42]. While universally employed, this approach faces several critical limitations:
- Subjectivity and Variability: Embryologist evaluations demonstrate significant inconsistency, with assessment agreement rates often compromised by human interpretation differences [41].
- Static Assessment Limitations: Traditional microscopy provides snapshot images that cannot capture the dynamic developmental processes essential for comprehensive viability assessment [41].
- Limited Predictive Value: Nearly half of morphologically high-quality embryos are aneuploid, indicating that visual assessment alone cannot reliably identify chromosomal normalcy [42].
Diagnostic Challenges in Genetic Screening
Preimplantation genetic testing for aneuploidy (PGT-A) has emerged as a solution for identifying chromosomal abnormalities but introduces its own limitations:
- Invasive Procedures: Trophectoderm biopsy requires specialized expertise and poses potential risks to embryo viability [42].
- Regulatory and Cost Barriers: Varying international regulations and high costs limit accessibility for many patients [44].
- Technical Limitations: Biopsy represents only a subset of cells, potentially missing mosaicism present in other embryonic regions [42].
Table 1: Comparison of Traditional Embryo Assessment Methods
| Method | Key Parameters | Advantages | Limitations |
|---|---|---|---|
| Morphological Assessment | Cell symmetry, fragmentation, developmental stage [41] | Rapid, inexpensive, universally applicable | Subjective, poor predictive value for aneuploidy [42] |
| Time-Lapse Imaging | Division timing, cleavage patterns, multinucleation [42] | Non-invasive, provides dynamic information | Still requires human interpretation, standardized criteria lacking |
| PGT-A (Invasive) | Chromosomal copy number, structural abnormalities [42] | Direct assessment of ploidy status | Invasive, requires specialized skills, cost prohibitive |
Artificial Intelligence in Embryo Assessment
Deep Learning Models for Embryo Evaluation
AI technologies, particularly deep learning algorithms, are revolutionizing embryo assessment by extracting quantitative features from embryo images that surpass human visual capabilities. Convolutional Neural Networks (CNNs) have demonstrated remarkable proficiency in analyzing embryo morphology across developmental stages:
- Early Development (0-3 days): Deep learning models like ResNet and U-Net achieve accuracy up to 0.98 AUC in predicting developmental potential, significantly outperforming traditional machine learning approaches (AUC 0.73-0.75) [41].
- Blastocyst Stage (5-6 days): AI systems utilize both semi-automated segmentation (U-Net with 0.96 accuracy) and fully automated classification (ResNet50 with 0.90 accuracy) to evaluate complex morphological structures [41].
- Full Developmental Timeline: Time-lapse imaging combined with 3D-CNN or RNN models captures spatiotemporal features, achieving 0.95 AUC in predicting viability [41].
Comparative studies demonstrate AI models significantly outperform embryologists, with median accuracy of 75.5% (range 59-94%) in grading embryo morphology compared to approximately 51% for clinical embryologists [43] [41]. When integrating clinical parameters with image data, AI performance increases to 81.5% median accuracy (range 67-98%) [43] [41].
Advanced AI Architectures and Foundation Models
Recent advances in AI architecture have introduced transformer-based foundation models specifically designed for embryo assessment:
FEMI (Foundational IVF Model for Imaging): Trained on approximately 18 million time-lapse images from multiple clinics, this Vision Transformer (ViT) model utilizes self-supervised learning to reconstruct original images from masked inputs [44]. The model's encoder-decoder architecture enables comprehensive feature learning from diverse datasets.
STORK Framework: Developed using over 50,000 human embryo images, this deep neural network achieves AUC greater than 0.98 and demonstrates 95.7% precision in predicting embryologist consensus on blastocyst quality [42].
iDAScore: A deep learning algorithm incorporating both spatial (morphological) and temporal (morphokinetic) features from time-lapse imaging, trained on over 115,000 embryos including 14,644 with known clinical outcomes [45].
Table 2: Performance Comparison of AI Embryo Assessment Models
| Model | Training Data | Architecture | Key Performance Metrics |
|---|---|---|---|
| FEMI [44] | 18 million time-lapse images | Vision Transformer (ViT) | Superior ploidy prediction; Accurate blastulation time prediction; Top-1 accuracy 60.31% stage prediction |
| STORK [42] | 50,000+ embryo images | Deep Neural Network (DNN) | >0.98 AUC blastocyst quality; 95.7% precision vs. embryologist consensus |
| iDAScore [45] | 115,000+ embryos | Deep Learning | Clinical pregnancy rate 46.5% in RCT (vs. 48.2% manual selection) |
| BELA [44] | Not specified | Multitask Learning | Predicts ploidy status without embryologist assistance |
AI Model Architecture for Embryo Assessment
Clinical Validation and Efficiency Metrics
Randomized controlled trials provide critical insights into AI implementation in clinical settings. A landmark double-blind non-inferiority trial comparing deep learning (iDAScore) to manual morphology assessment revealed several key findings:
- Clinical Pregnancy Rates: The AI group demonstrated 46.5% clinical pregnancy rate versus 48.2% in the manual assessment group, with a risk difference of -1.7 percentage points (95% CI: -7.7 to 4.3) [45].
- Operational Efficiency: AI assessment required approximately 21.3 seconds per case compared to 208.3 seconds for traditional morphology assessment—nearly a 10-fold reduction in evaluation time [45].
- Subgroup Variations: Performance differences emerged in subgroup analyses, with AI demonstrating better outcomes in fresh embryo transfers versus frozen cycles [45].
These findings suggest that while AI systems currently demonstrate equivalent rather than superior clinical outcomes compared to expert embryologists, they offer substantial advantages in standardization, efficiency, and scalability.
Omics Technologies in Embryo Viability Assessment
Genomic and Transcriptomic Approaches
Omics technologies provide complementary molecular perspectives on embryo viability beyond morphological assessment:
- Whole Genome Sequencing: Enables comprehensive screening for monogenic disorders, aneuploidies, and structural chromosomal rearrangements through preimplantation genetic testing (PGT) [43].
- Transcriptomic Profiling: Analysis of RNA expression patterns reveals critical insights into embryonic gene regulation during development [46].
- Single-Cell RNA Sequencing: The ReproGenomics Viewer resource provides cross-species transcriptomic data compatible with single-cell studies, enabling unprecedented resolution in developmental genetics [47].
Emerging Omics Applications
Innovative omics applications are expanding the analytical framework for embryo assessment:
- Epigenetic Profiling: Analysis of DNA methylation patterns and histone modifications provides insights into gene expression regulation influenced by environmental and developmental factors [43] [22].
- Proteomic Analysis: Identification of protein biomarkers in culture medium offers functional insights into embryonic metabolic activity and developmental competence [22].
- Metabolomic Screening: Assessment of spent culture medium metabolites serves as indicators of embryonic metabolic activity and viability [46].
Non-Invasive Assessment Modalities
Non-Invasive Genetic Assessment
Traditional PGT-A requires trophectoderm biopsy, but non-invasive approaches are emerging:
- Spent Culture Medium (SCM) Analysis: Embryos release cell-free DNA into culture medium, enabling niPGT-A with reported concordance rates approaching 90% with TE biopsy results in validation studies [42].
- Blastocoel Fluid (BF) Assessment: Aspiration of blastocoel fluid provides an alternative DNA source with variable concordance (37.5% to 97.4%) compared to TE biopsy [42].
- Combined SCM/BF Approaches: Simultaneous analysis of both media increases amplifiable DNA quantity, potentially improving diagnostic accuracy [42].
Multi-Modal Data Integration
The most significant advances emerge from integrating multiple data modalities:
- Time-lapse Imaging with Genetic Data: Combining morphokinetic patterns with genetic status improves ploidy prediction accuracy [44].
- AI-Omics Integration: Algorithms that incorporate imaging features with metabolomic profiles demonstrate enhanced predictive capability for implantation potential [46].
- Clinical Parameter Integration: Maternal age, infertility diagnosis, and previous IVF outcomes combined with embryo-specific data improve personalized selection algorithms [45].
Multi-Omics Integration in Embryo Assessment
Experimental Protocols and Methodologies
FEMI Model Development Protocol
The development of foundation models like FEMI follows rigorous methodological frameworks:
Data Collection:
- Acquisition of approximately 18 million time-lapse images from multiple clinics
- Selection of images taken after 85 hours post-insemination (hpi) at z-axis depths
- Tight cropping around embryos to augment feature learning
Model Architecture:
- Implementation of Vision Transformer masked autoencoder (ViT MAE)
- Self-supervised learning approach for reconstructing original images from masked inputs
- Encoder-decoder structure to learn essential dataset characteristics
Training Protocol:
- Dataset division: 80% training, 20% validation split
- Treatment of each image as an independent sample
- Incorporation of maternal age for ploidy prediction tasks
Validation Framework:
- Evaluation across six clinical tasks: ploidy prediction, blastulation time prediction, component segmentation, quality scoring, embryo witnessing, and stage prediction
- Comparison against benchmark models (MoViNet, VGG16, EfficientNet V2, ResNet101-RS, ConvNext, CoAtNet)
- Performance assessment across multiple datasets to evaluate generalizability [44]
Non-Invasive PGT-A Laboratory Protocol
Standardized methodology for niPGT-A implementation:
Sample Collection:
- Culture of embryos to blastocyst stage in designated medium
- Careful collection of spent culture medium avoiding cellular contamination
- Storage at -80°C until analysis
DNA Amplification and Processing:
- Whole genome amplification of cell-free DNA
- Library preparation and next-generation sequencing
- Bioinformatic analysis for chromosomal copy number assessment
Validation and Quality Control:
- Parallel analysis of matched trophectoderm biopsies
- Concordance rate calculation between SCM and TE results
- Implementation of stringent contamination controls [42]
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for AI-Omics Embryo Assessment
| Reagent/Technology | Application | Function | Example Use Cases |
|---|---|---|---|
| Time-lapse Incubators [42] | Continuous embryo monitoring | Captures developmental images every 5-20 minutes without disturbing culture environment | Morphokinetic analysis, division pattern assessment |
| Whole Genome Amplification Kits [42] | niPGT-A | Amplifies minute quantities of cell-free DNA from spent culture medium | Genetic screening without embryo biopsy |
| Next-Generation Sequencing Platforms [43] | Genomic analysis | Enables comprehensive chromosome screening and mutation detection | PGT-A, monogenic disorder screening |
| Mass Spectrometry Systems [22] | Metabolomic/Proteomic profiling | Identifies and quantifies small molecules/proteins in culture medium | Viability biomarker discovery, metabolic activity assessment |
| Single-Cell RNA Sequencing Kits [47] | Transcriptomic analysis | Profiles gene expression patterns in individual cells | Embryonic gene regulation studies, developmental competence biomarkers |
| AI Training Datasets [44] | Model development | Curated image libraries with known outcomes for algorithm training | FEMI development (18 million images), STORK framework |
| 4-(Methoxymethyl)thiazole | 4-(Methoxymethyl)thiazole|High-Quality Research Chemical | Bench Chemicals | |
| 6-Keto Betamethasone | 6-Keto Betamethasone Reference Standard | 6-Keto Betamethasone is a high-purity analytical reference standard for pharmaceutical research (RUO). For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
Future Directions and Research Challenges
Technological Advancements
Several emerging innovations promise to further transform embryo assessment:
- Federal Learning Frameworks: Enable multi-center data collaboration while maintaining privacy security, addressing data scarcity issues [41].
- Explainable AI (XAI): Implementation of techniques like SHAP and Grad-CAM to enhance model interpretability and clinical trust [41].
- Multi-Modal Data Fusion: Advanced algorithms for integrating imaging, genetic, epigenetic, and clinical data into unified predictive models [46].
- Polygenic Risk Scoring: Development of comprehensive risk profiles for complex diseases through analysis of multiple gene variants [43].
Implementation Challenges
Significant hurdles remain for widespread clinical adoption:
- Data Standardization: Heterogeneous data formats and acquisition protocols across clinics complicate model generalizability [44].
- Regulatory Frameworks: Evolving guidelines for clinical validation and approval of AI-based medical devices [45].
- Ethical Considerations: Equitable access, algorithmic bias mitigation, and patient autonomy in embryo selection decisions [41].
- Technical Infrastructure: Computational resource requirements for processing high-volume omics and imaging data [22].
The integration of artificial intelligence and multi-omics technologies represents a fundamental transformation in embryo assessment methodologies. Current evidence demonstrates that AI systems can achieve comparable clinical outcomes to expert embryologists while providing substantial efficiency improvements and reduced subjectivity. The continued refinement of foundation models like FEMI, trained on millions of embryo images, promises enhanced generalizability across diverse patient populations and clinical settings.
For the research community, these advances highlight the critical importance of standardized data collection, collaborative validation efforts, and interdisciplinary approaches bridging computational science and reproductive biology. The ongoing integration of omics technologies—from non-invasive genetic assessment to metabolomic profiling—will provide increasingly multidimensional assessment frameworks moving beyond morphology alone.
While clinical implementation challenges remain, the methodological frameworks and technical protocols outlined in this review provide a roadmap for continued innovation. Through rigorous validation and responsible development, AI and omics-driven embryo assessment holds significant potential to advance reproductive medicine, ultimately improving outcomes for the growing global population relying on assisted reproductive technologies.
Preimplantation genetic testing (PGT) has fundamentally transformed assisted reproductive technology (ART) by enabling direct assessment of embryonic chromosomal status before transfer. This field has evolved from limited chromosome screening to comprehensive molecular karyotyping, reflecting broader trends in omics technologies within reproductive biology. The journey from fluorescence in situ hybridization (FISH) to comprehensive chromosome screening (CCS) represents a technological revolution that has improved our understanding of embryonic aneuploidy and its clinical implications [48] [49]. This evolution parallels developments in other omics fields, where comprehensive data acquisition has replaced targeted analysis, providing unprecedented insights into biological systems [22]. The integration of these advanced genomic technologies into reproductive medicine has created new possibilities for selecting euploid embryos, thereby addressing one of the fundamental challenges in human reproduction – the high incidence of chromosomal abnormalities in preimplantation embryos.
Historical Technological Evolution in PGT
The FISH Era: Limited Chromosome Screening
The initial approach to preimplantation genetic screening utilized FISH technology, which allowed for the visualization of specific chromosomes using fluorescently-labeled DNA probes. This technique was historically the first used for PGS (now termed PGT-A) and was typically performed on day-3 cleavage-stage embryos [48] [50]. Table 1 summarizes the key characteristics and limitations of FISH-based PGT.
Table 1: Characteristics and Limitations of FISH-Based PGT
| Aspect | Technical Specification | Clinical Limitation |
|---|---|---|
| Chromosomes Screened | Typically 5-12 chromosome pairs | Majority of chromosomes not assessed [51] [50] |
| Analytical Platform | Fluorescence microscopy | Subjective interpretation potential |
| Diagnostic Accuracy | Variable per chromosome error rate | Limited detection accuracy [51] |
| Clinical Utility | No improvement in delivery rates | Actually reduced pregnancy chances in some populations [49] |
| Biopsy Timing | Day-3 cleavage stage | Potential embryo damage from blastomere biopsy |
FISH technology presented significant limitations in clinical efficacy. A systematic review revealed that after PGS-FISH with a negative result (euploid), the post-test probability of aneuploidy was 42% (CI: 35-49), which was only marginally better than the 55% (CI: 50-61) achieved through morphology-based selection alone [50]. This limited diagnostic capability, combined with the potential harm to IVF outcomes, led professional societies to declare the initial form of PGS (PGS#1) ineffective in improving pregnancy rates [49].
The Transition to Comprehensive Chromosome Screening
The recognition of FISH's limitations prompted the development of comprehensive chromosome screening (CCS) technologies that could assess all 24 chromosomes. This transition represented a fundamental shift in PGT capabilities and required parallel advances in embryo biopsy techniques and genetic analysis platforms [48].
Array-based technologies, including array comparative genomic hybridization (aCGH) and single nucleotide polymorphism (SNP) arrays, facilitated the first truly comprehensive screening of all chromosomes in embryos [48]. These platforms offered improved accuracy and more reliable results compared to FISH, marking the beginning of the PGS#2 era characterized by trophectoderm biopsy on day 5/6 embryos instead of day-3 embryo biopsy [49].
The most recent technological breakthrough came with next-generation sequencing (NGS), which offers reliable PGS results, streamlined workflows, higher throughput capabilities, and customizable assays [48]. This evolution from limited FISH analysis to comprehensive screening methods has fundamentally changed the precision and clinical utility of preimplantation genetic testing.
Modern Comprehensive Chromosome Screening Methodologies
Technical Approaches and Workflows
Modern CCS encompasses several sophisticated technological approaches that enable comprehensive aneuploidy screening. The fundamental workflow begins with blastocyst culture and biopsy, followed by whole-genome amplification, and culminates in chromosomal analysis using advanced genomic platforms.
Array Comparative Genomic Hybridization (aCGH) enables genome-wide copy number analysis by competitively hybridizing test and reference DNA samples. This method provides a comprehensive view of chromosomal imbalances across all chromosomes but requires a reference sample and specialized array platforms [48].
Next-Generation Sequencing (NGS) has set a new standard in PGT by providing base-level resolution across the entire genome. NGS-based approaches for PGT involve sequencing DNA libraries prepared from embryonic samples and aligning the sequences to a reference genome to determine chromosome copy numbers. The massively parallel sequencing capability of NGS platforms allows for high-resolution detection of aneuploidies and segmental imbalances, with customizable coverage and analysis parameters tailored to PGT requirements [48].
Single Nucleotide Polymorphism (SNP)-Based Haplotyping represents a sophisticated approach that combines copy number analysis with linkage-based assessment. This method utilizes genome-wide SNP genotyping and haplotype phasing to infer embryonic karyotypes. In this process, parental haplotypes are phased using genotypes from close relatives or unbalanced embryos, allowing for precise determination of chromosomal status and inheritance patterns [52]. A major advantage of this approach is its ability to distinguish between euploid embryos with normal karyotypes and those carrying balanced chromosomal rearrangements, enabling selection of embryos without inherited structural rearrangements [52].
Advanced Protocol: Genome-Wide SNP Haplotyping for Structural Rearrangements
A recent large-scale, multicenter validation study demonstrated an advanced application of CCS for detecting chromosomal structural rearrangements [52]. The methodology employed in this study provides an excellent example of modern PGT-SR (preimplantation genetic testing for structural rearrangements) protocols:
Study Population and Design: 1298 balanced chromosomal rearrangement (BCR) carriers were recruited across 12 academic fertility centers in a prospective cohort study. A total of 7867 blastocysts from 1603 PGT-SR cycles were biopsied, with 7750 (98.51%) successfully genotyped and analyzed [52].
Biopsy Protocol: Trophectoderm biopsy was performed on day 5/6 blastocysts, with only a single embryo transferred in each cycle [52].
Genetic Analysis: PGT-SR was performed using a genome-wide SNP genotyping and haplotyping approach. Parental haplotypes were phased by available genotypes from a close relative or an unbalanced embryo. The karyotypes of embryos were inferred from these haplotypes [52].
Validation: The method demonstrated high accuracy with 95% confidence intervals for sensitivity and specificity ranging from 98.34%-100% and 96.63%-100%, respectively [52].
This protocol highlights how comprehensive genotyping technologies can be universally applied to different BCR types, providing both aneuploidy screening and structural rearrangement detection in a single assay [52].
Diagram 1: Workflow for comprehensive PGT-SR using genome-wide SNP genotyping and haplotyping. This process enables detection of both aneuploidy and structural rearrangements in a single assay [52].
Comparative Analysis of PGT Technologies
Performance Metrics Across Platforms
The evolution from FISH to CCS technologies has resulted in substantial improvements in diagnostic accuracy and clinical utility. Table 2 provides a comprehensive comparison of the key performance metrics across different PGT platforms.
Table 2: Comparative Analysis of PGT Technology Performance Characteristics
| Technology | Chromosomes Assessed | Diagnostic Accuracy | Clinical Pregnancy Outcomes | Major Advantages | Significant Limitations |
|---|---|---|---|---|---|
| FISH | Limited (5-12 pairs) | Variable per-chromosome error rate [51] | No improvement; reduced rates in some populations [49] | Technically accessible; rapid results | Limited chromosome coverage; poor clinical validity [50] |
| Array CGH | All 24 chromosomes | High comprehensive accuracy [48] | Improved delivery rates per transfer [48] | Comprehensive screening; no reference required | Inability to detect balanced rearrangements |
| SNP Array | All 24 chromosomes | High comprehensive accuracy with haplotype data [52] | 817 healthy babies delivered in large cohort [52] | Detects uniparental disomy; haplotyping capability | Complex analysis pipeline |
| NGS | All 24 chromosomes | Highest resolution and accuracy [48] | Improved embryo selection efficiency [48] | Customizable resolution; detects mosaicism | Higher cost; bioinformatics complexity |
| SNP Haplotyping | All 24 chromosomes with linkage | Sensitivity: 98.34-100%, Specificity: 96.63-100% [52] | 73.07% newborns with normal karyotypes [52] | Distinguishes carrier from non-carrier embryos | Requires family genotype data |
The technological progression has substantially improved clinical outcomes. In the large multicenter study of SNP-haplotyping, 75.98% (1218/1603) of cycles obtained euploid embryos and 53.15% (852/1603) generated non-carrier embryos. Most significantly, this approach resulted in the birth of 817 healthy babies, with 73.07% (597/817) having normal karyotypes, thus avoiding inheritance of parental balanced chromosomal rearrangements [52].
Integration with Multi-Omics Approaches in Reproductive Biology
The evolution of PGT technologies mirrors broader developments in omics approaches within reproductive medicine. The integration of genomics, transcriptomics, proteomics, and epigenomics provides unprecedented insights into reproductive processes and embryo viability [22]. Specifically:
Genomics in PGT has evolved from targeted FISH analysis to comprehensive chromosome screening, enabling better prediction of embryonic reproductive potential [22] [48].
Transcriptomics offers potential for understanding gene expression patterns in embryos, though application in clinical PGT remains limited due to the need for embryo biopsy and amplification of minimal RNA quantities [22].
Proteomics and metabolomics contribute to identifying biomarkers for embryo viability assessment, potentially complementing genetic screening methods [22].
Epigenomics explores DNA methylation and histone modifications in embryonic development, with emerging evidence of its importance in fertility and embryogenesis [22].
The convergence of these omics technologies with advanced PGT platforms represents the future of embryo selection, where multi-parameter assessment may further improve reproductive outcomes.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Implementation of advanced PGT methodologies requires specific research reagents and technological platforms. Table 3 catalogues essential solutions for conducting comprehensive chromosome screening in reproductive research.
Table 3: Essential Research Reagent Solutions for Comprehensive Chromosome Screening
| Reagent/Platform | Specific Function | Application Context | Representative Example |
|---|---|---|---|
| Whole Genome Amplification Kits | Amplification of minute DNA quantities from biopsied cells | All CCS platforms requiring DNA amplification | Multiple displacement amplification kits |
| SNP Genotyping Arrays | Genome-wide polymorphism analysis for haplotyping | PGT-SR for structural rearrangements [52] | Illumina Infinium arrays |
| NGS Library Prep Kits | Preparation of sequencing libraries from amplified DNA | NGS-based PGT for aneuploidy screening [48] | Illumina Nextera XT |
| Bioinformatics Pipelines | Data analysis, alignment, and chromosome copy number calling | Interpretation of CCS data from arrays or NGS | BlueFuse Multi Analysis Software [48] |
| Embryo Biopsy Systems | Micromanipulation instruments for trophectoderm biopsy | All blastocyst-stage PGT procedures | Laser-assisted biopsy systems |
| Cell Lysis Solutions | Release of genetic material from single or few cells | Initial step in genetic analysis post-biopsy | Proteinase K-based lysis buffers |
| Stephodeline | Stephodeline, MF:C21H27NO5, MW:373.4 g/mol | Chemical Reagent | Bench Chemicals |
| Methyl lucidenate D | Methyl Lucidenate D | 98665-09-9 | Research Compound | High-purity Methyl Lucidenate D (Cas 98665-09-9), a Ganoderma lucidum triterpenoid. For Research Use Only. Explore its applications in cancer, antiviral, and anti-inflammatory research. | Bench Chemicals |
These research tools enable the implementation of advanced PGT protocols in both clinical and research settings. The integration of wet-bench laboratory techniques with sophisticated bioinformatics analysis represents the core of modern preimplantation genetic testing platforms.
The evolution of preimplantation genetic testing from limited FISH analysis to comprehensive chromosome screening technologies represents a remarkable advancement in reproductive medicine. This journey has transformed embryo selection from a morphology-based assessment to a precise genomic evaluation, significantly improving clinical outcomes for couples undergoing assisted reproduction.
The latest developments in genome-wide SNP genotyping and haplotyping have further expanded the capabilities of PGT, enabling not only aneuploidy detection but also identification of balanced chromosomal rearrangements and their segregation in embryos [52]. This allows couples carrying structural rearrangements to not only select against unbalanced embryos but also avoid transmitting balanced rearrangements to their offspring, potentially preventing fertility issues in the next generation [52].
Future directions in PGT will likely focus on integration with other omics technologies, including transcriptomic, proteomic, and epigenomic profiling, to create multi-dimensional assessments of embryonic viability [22]. Additionally, moves toward non-invasive approaches using spent embryo culture media for genetic analysis may further refine PGT protocols while maintaining embryo integrity.
As these technologies continue to evolve, their implementation must be guided by robust clinical validation and appropriate ethical frameworks. The lesson from the PGS#1 to PGS#2 transition underscores the importance of evidence-based adoption of new technologies in reproductive medicine [49]. Through continued refinement and validation, comprehensive chromosome screening technologies will remain essential tools in advancing both reproductive clinical practice and our fundamental understanding of human embryogenesis.
Male infertility affects approximately 8-12% of couples globally, with a male factor solely responsible in 30% of cases and contributing in another 20% [53] [54]. Traditionally, the diagnostic journey begins with conventional semen analysis, which assesses parameters including sperm concentration, motility, and morphology according to World Health Organization guidelines. Despite standardization efforts, this approach provides limited insight into the molecular mechanisms underlying sperm dysfunction [55] [56]. The seminal fluid represents a complex biological matrix containing secretions from the testis, epididymis, prostate, and seminal vesicles, yet routine biochemical tests of these components offer minimal clinical utility as biomarkers [56]. Consequently, nearly 50% of male infertility cases are classified as idiopathic, creating a pressing need for advanced diagnostic tools that can elucidate the molecular basis of impaired sperm function [54].
The emergence of multi-omics technologies—including genomics, proteomics, metabolomics, and microbiomics—has revolutionized our approach to male infertility diagnosis [55] [57]. These complementary disciplines enable comprehensive profiling of the molecular components that dictate sperm health and function, facilitating the discovery of novel biomarkers with potential clinical utility. This technical guide explores current advances in omics-driven biomarker discovery, detailing experimental methodologies, key findings, and integrative approaches that are reshaping our understanding of male reproductive physiology and pathology.
Omics Technologies in Male Infertility Research
Genomic and Epigenetic Approaches
Genetic factors contribute significantly to male infertility, with recognized causes including Y-chromosome microdeletions, Klinefelter syndrome, and monogenic disorders such as Kallman syndrome and cystic fibrosis [54]. Standard karyotyping remains a fundamental genetic test, particularly for patients with severe oligospermia or azoospermia, yet these known conditions account for only approximately 30% of male infertility cases [54]. Beyond chromosomal abnormalities and specific gene mutations, epigenetic modifications—including DNA methylation, histone modifications, and non-coding RNA expression—represent another crucial layer of regulatory information with diagnostic potential.
Spermatogenesis requires the coordinated expression of over 2,000 genes, making genomic and epigenomic profiling particularly valuable for identifying novel genetic markers [54]. The systematic evaluation of an organism's complete DNA sequence has been facilitated by advanced technologies including tiling arrays and RNA-Seq, which enable researchers to study both noncoding and protein-coding transcripts with unprecedented precision [58]. These approaches have revealed that chromosomal abnormalities are 8-10 times more common in infertile men, occurring in approximately 3% of patients with oligospermia and 19% of patients with azoospermia [54].
Table 1: Genomic Biomarkers in Male Infertility
| Genetic Factor | Clinical Presentation | Detection Method | Prevalence in Infertile Men |
|---|---|---|---|
| Y-chromosome AZF microdeletions | Azoospermia, severe oligospermia | PCR | 3-15% of azoospermic men |
| Klinefelter syndrome (47,XXY) | Azoospermia, testicular atrophy | Karyotyping | 14% of azoospermic men |
| CFTR gene mutations | CBAVD, obstructive azoospermia | PCR, gene sequencing | 1% of infertile men |
| Chromosomal abnormalities | Variable, often azoospermia | Karyotyping | 3% (oligospermia), 19% (azoospermia) |
Proteomic Technologies and Biomarkers
Proteomics has transformed our comprehension of male fertility by identifying potential infertility biomarkers and reproductive defects through comprehensive protein analysis [59]. The evolution from two-dimensional gel electrophoresis to advanced mass spectrometry has enabled researchers to identify and quantify thousands of proteins simultaneously, offering unprecedented analytical depth [59]. Early proteomic studies mapped the human sperm proteome, identifying over a thousand proteins and establishing a baseline for comparative fertility studies [59]. Recent technological advances have significantly expanded this catalog, with one 2025 study employing Data-Independent Acquisition mass spectrometry to identify an unprecedented 9,309 proteins from human sperm samples [60].
Liquid chromatography-tandem mass spectrometry has emerged as a cornerstone technology in sperm proteomics, providing deeper molecular insights into proteins critical for fertilization and embryonic development [60]. The exceptional accuracy and reproducibility of platforms like the Orbitrap Astral mass spectrometer support both biomarker discovery and targeted therapy development [60]. Proteomic analyses have revealed dynamic changes in protein expression as sperm cells undergo capacitation and acrosomal reactions, processes essential for successful egg penetration [59]. Furthermore, comparative studies of testicular tissues from fertile and infertile men have identified differentially expressed proteins associated with conditions including azoospermia, including phospholipid hydroperoxide glutathione peroxidase, peroxiredoxin 4, heat shock protein b-1, and cathepsin D [59].
Figure 1: Mass Spectrometry-Based Proteomics Workflow. DIA = Data-Independent Acquisition.
Metabolomic Profiling
Metabolomics focuses on the systematic study of small molecule metabolites, providing a direct readout of cellular activity and physiological status [53]. In the context of male infertility, seminal plasma metabolomic profiling has revealed distinct metabolic signatures associated with impaired sperm function. A 2025 integrated microbiota-metabolome study identified 147 differentially expressed metabolites in idiopathic infertility, with four specific metabolites—γ-Glu-Tyr, Indalone, Lys-Glu, and γ-Glu-Phe—demonstrating exceptional diagnostic potential (AUC > 0.97) [53]. This remarkable discriminatory power highlights the clinical promise of metabolic biomarkers.
Metabolomic studies typically employ untargeted liquid chromatography-mass spectrometry to profile seminal fluid components [53]. The analytical process involves protein precipitation using pre-cooled methanol/acetonitrile/water solutions, followed by centrifugation, vacuum drying, and LC-MS analysis using high-resolution platforms such as the AB Triple TOF 6600 or Orbitrap Exploris 480 mass spectrometers [53]. Bioinformatic processing includes peak alignment, retention time correction, and peak area extraction using software packages including XCMS, followed by multivariate statistical analysis to identify differentially abundant metabolites [53].
Table 2: Key Metabolomic Biomarkers in Male Infertility
| Metabolite | Biological Role | Association with Sperm Quality | Diagnostic Performance (AUC) |
|---|---|---|---|
| γ-Glu-Tyr | Antioxidant peptide | Negative correlation with infertility | >0.97 [53] |
| Lys-Glu | Dipeptide | Negative correlation with motility | >0.97 [53] |
| Arg-Arg | Energy metabolism | Positive correlation with motility [53] | Not specified |
| LPC 18:2 | Membrane integrity | Positive correlation with sperm quality [53] | Not specified |
| Fumarate | TCA cycle intermediate | Positive correlation with motility [53] | Not specified |
Seminal Microbiome Analysis
The seminal microbiome represents an emerging frontier in male reproductive health research, with evidence suggesting that microbial communities influence sperm metabolic health and function [55] [53]. Molecular profiling techniques, particularly 16S rRNA gene sequencing, have revealed distinct dysbiosis patterns in idiopathic male infertility. A 2025 integrated multi-omics study demonstrated significantly lower seminal microbiota α-diversity in infertile men, with 45 differentially abundant taxa identified between fertile and infertile groups [53].
Specific bacterial taxa demonstrate clinically relevant associations with sperm parameters. Providencia rettgeri, Pediococcus pentosaceus, and Streptococcus pneumoniae show positive correlations with sperm quality, while Proteus penneri abundance correlates negatively with sperm function [53]. Methodologically robust microbiome analysis requires careful attention to potential contaminants, with recommended exclusion of species prevalent in more than 7.5% of negative controls [53]. Advanced sequencing approaches, such as 5R 16S rRNA sequencing that combines multiple variable regions, enhance microbial community profiling resolution compared to single-region methods [53].
Integrated Multi-Omics Approaches
While individual omics technologies provide valuable insights, their integration offers a more comprehensive understanding of male infertility pathophysiology [55] [57]. Multi-omics data integration represents a powerful strategy for elucidating the complex molecular networks governing spermatogenesis and sperm function, moving beyond the limitations of single-platform analyses [57]. This holistic approach facilitates the identification of high-value biomarker panels that span molecular levels, from genetic predisposition to functional metabolic output.
The conceptual framework for multi-omics integration in male infertility recognizes that genetic and epigenetic factors regulate transcriptional activity, which directs protein expression, ultimately manifesting in the metabolic phenotype [57]. Bioinformatic tools and computational frameworks have evolved to manage the considerable challenges of heterogeneous data integration, dimensionality reduction, and biological interpretation [57] [58]. Successful applications of integrated multi-omics have illuminated previously obscure disease mechanisms in idiopathic male infertility, providing novel diagnostic and therapeutic targets [53].
Figure 2: Multi-Omics Data Integration Framework. PTMs = Post-Translational Modifications.
Experimental Protocols and Methodologies
Sample Collection and Preparation
Standardized protocols for semen sample collection and processing are fundamental to generating reliable, reproducible omics data. Participants should maintain abstinence for 2-7 days prior to sample collection, with evidence suggesting that 1-day abstinence may optimize semen quality in subfertile men [56]. Samples are typically collected via masturbation into sterile containers without lubricants, followed by complete liquefaction at 37°C for 30 minutes [60] [53]. Subsequent processing involves centrifugation to remove seminal plasma, followed by three washes with ice-cold phosphate-buffered saline to remove contaminants and cellular debris [60].
For proteomic analysis, protein extraction employs either tissue protein extraction reagent or urea-based lysis buffers, followed by sonication on ice and centrifugation to collect the supernatant [60]. Protein quantification using Bradford assay ensures standardized loading for subsequent analyses. Filter-aided sample preparation methods facilitate protein denaturation, reduction, and alkylation before enzymatic digestion [60]. For metabolomic studies, protein precipitation using pre-cooled methanol/acetonitrile/water solutions (2:2:1, v/v) followed by low-temperature sonication and centrifugation effectively extracts metabolites while preserving labile compounds [53].
Mass Spectrometry-Based Proteomics
Liquid chromatography-tandem mass spectrometry represents the gold standard for comprehensive proteomic profiling [60]. The workflow typically involves tryptic digestion of extracted proteins, followed by peptide fractionation using basic reversed-phase chromatography to reduce sample complexity [60]. Data-Independent Acquisition mass spectrometry has emerged as a powerful alternative to traditional Data-Dependent Acquisition methods, systematically selecting, fragmenting, and detecting all precursor ions within predetermined mass-to-charge windows [60]. This approach significantly reduces missing values while offering superior quantification accuracy, repeatability, and stability, particularly for large-scale biomarker discovery studies [60].
Instrument parameters critically influence data quality. High-resolution platforms like the Orbitrap Astral mass spectrometer independently operate Orbitrap full scan and Astral MS/MS to generate high-resolution full-scan spectra and high-quality secondary maps [60]. For a typical sperm proteomics experiment, raw mass spectrometry files are processed and searched against protein databases using software such as Spectronaut, followed by functional annotation and pathway analysis using Gene Ontology and gene set enrichment analysis [60]. This pipeline successfully identified 145,355 unique peptides and 9,309 corresponding proteins in a recent comprehensive analysis, establishing a valuable resource for the research community [60].
Microbiome Sequencing and Analysis
Seminal microbiome profiling typically employs 16S rRNA gene sequencing, with advanced approaches such as 5R 16S rRNA sequencing that combine multiple variable regions to enhance taxonomic resolution [53]. The experimental protocol begins with genomic DNA extraction from semen pellets using specialized kits, followed by quality assessment through agarose gel electrophoresis and spectrophotometric measurement [53]. After amplifying target regions, purified amplicons undergo paired-end sequencing on platforms such as the Illumina NextSeq 2000 [53].
Bioinformatic processing includes demultiplexing sequences for each sample, filtering based on quality parameters, and aligning reads to amplified regions [53]. The Short Multiple Regions Framework method effectively aggregates read counts from different regions into coherent taxonomic profiles [53]. To minimize noise, samples with fewer than 1,000 normalized reads and low-abundance species are typically excluded from analysis [53]. Subsequent statistical evaluation includes α-diversity assessment, β-diversity analysis using PCoA based on Bray-Curtis distance, and differential abundance testing using methods such as linear discriminant analysis effect size [53].
Research Reagent Solutions
Table 3: Essential Research Reagents for Male Infertility Omics Studies
| Reagent/Category | Specific Examples | Application and Function |
|---|---|---|
| Protein Extraction Reagents | T-PER (Tissue Protein Extraction Reagent), UA lysis buffer (8M urea, 100mM Tris-HCl) | Protein solubilization and extraction from sperm cells [60] |
| Digestion Enzymes | Trypsin | Proteolytic digestion of proteins into peptides for MS analysis [60] |
| Reduction/Alkylation Reagents | Dithiothreitol, Iodoacetamide | Breaking disulfide bonds and alkylating cysteine residues [60] |
| Chromatography Columns | Basic reversed-phase columns | Peptide fractionation to reduce sample complexity [60] |
| DNA Extraction Kits | FastPure Stool DNA Isolation Kit (Magnetic bead) | Microbial genomic DNA extraction from semen samples [53] |
| 16S rRNA Amplification Reagents | Region-specific primers, PCR master mixes | Amplification of target variable regions for microbiome sequencing [53] |
| Metabolite Extraction Solvents | Methanol/acetonitrile/water (2:2:1, v/v) | Protein precipitation and metabolite extraction from seminal plasma [53] |
The integration of multi-omics technologies represents a paradigm shift in male infertility diagnostics, moving beyond the limitations of conventional semen analysis to elucidate the molecular mechanisms underlying sperm dysfunction [55]. Proteomic profiling has identified thousands of sperm proteins, with distinctive expression patterns in conditions including asthenozoospermia [59] [60]. Metabolomic studies have revealed seminal metabolic signatures with exceptional diagnostic potential [53]. Genomic and epigenomic analyses continue to expand our understanding of hereditary factors, while emerging research on the seminal microbiome has uncovered previously unappreciated influences on sperm health [53] [54].
Despite these advances, challenges remain in translating omics discoveries into clinically applicable biomarkers [59]. Standardization of analytical protocols, validation in diverse patient populations, and development of cost-effective diagnostic platforms represent critical next steps for the field [61]. The continued integration of multi-omics data through advanced bioinformatic approaches promises to unravel the complex pathophysiology of idiopathic male infertility, ultimately enabling personalized diagnostic and therapeutic strategies [57]. As these technologies mature, they hold significant potential to revolutionize the clinical management of male infertility, offering new hope for the millions of couples struggling with unexplained reproductive challenges.
Proteomic and Metabolomic Profiling of Endometrial Receptivity
Within the broader context of omics technologies in reproductive biology, the precise evaluation of endometrial receptivity (ER) remains a pivotal challenge. Endometrial receptivity describes the transient state of the endometrium during the window of implantation (WOI), a critical period in the mid-secretory phase of the menstrual cycle when the uterine environment is conducive to blastocyst implantation [62] [63]. It is estimated that suboptimal endometrial receptivity and altered embryo-endometrial crosstalk account for approximately two-thirds of human implantation failures [63]. While genomic and transcriptomic approaches have provided valuable insights, proteomic and metabolomic profiling offer a direct window into the functional proteins and dynamic metabolic processes that ultimately govern the receptive state. This in-depth technical guide synthesizes current methodologies, key findings, and emerging applications of proteomics and metabolomics in the precise characterization of endometrial receptivity, providing a resource for researchers, scientists, and drug development professionals in the field of reproductive medicine.
The Biological Context of Endometrial Receptivity
The window of implantation is a highly coordinated, limited time span, typically occurring between days 20 and 24 of a 28-day menstrual cycle, during which the molecular and cellular conditions of the endometrium allow for embryo attachment and invasion [62] [64]. The transition from a non-receptive to a receptive state involves complex molecular and cellular changes, including endometrial remodelling, decidualization of stromal cells, and the recruitment of immune cells such as uterine natural killer (uNK) cells, which collectively establish a tolerogenic environment [62] [64]. This process is regulated by ovarian hormones and requires precise synchrony between the endometrial cells themselves, as well as between the endometrium and the developing embryo [63].
Dysregulation of the mechanisms controlling ER is a significant cause of infertility and recurrent implantation failure (RIF) [62] [65]. Traditional clinical assessments, such as ultrasound and hysteroscopy, focus primarily on morphological evaluation and lack the molecular-level insights necessary to fully diagnose receptivity issues [66]. Consequently, the field has increasingly turned to high-throughput omics technologies to decipher the complex molecular signature of a receptive endometrium, with proteomics and metabolomics providing direct insight into the functional effectors and metabolic state of the endometrium during the WOI [66] [67].
Proteomic Profiling of Endometrial Receptivity
Proteomic analysis provides a direct assessment of the protein players that execute the biological functions required for embryo implantation. By characterizing the proteome of endometrial tissue, uterine fluid, and secreted extracellular vesicles, researchers can identify key proteins and pathways that are dynamically regulated during the acquisition of receptivity.
Analytical Technologies and Workflows
The standard proteomic workflow for ER analysis involves sample collection, protein extraction and digestion, liquid chromatography-mass spectrometry (LC-MS) analysis, and bioinformatic processing.
Table 1: Key Experimental Protocols for Proteomic Profiling
| Protocol Step | Description | Key Technical Considerations |
|---|---|---|
| Sample Collection | - Endometrial Tissue Biopsy: Obtained during the mid-secretory phase (LH+7/9).- Uterine Lavage/Fluid Aspiration: Minimally invasive collection of uterine secretions [68]. | Tissue biopsies should be snap-frozen immediately. Uterine lavage is performed using a catheter and sterile saline, with minimal impact on pregnancy rates [67]. |
| Protein Extraction & Digestion | Proteins are extracted using lysis buffers (e.g., RIPA buffer). Complex protein mixtures are digested into peptides using trypsin. | For formalin-fixed paraffin-embedded (FFPE) tissue, specific de-crosslinking and antigen retrieval protocols are required. |
| Quantitative Proteomics | - LC-MS/MS: Couples liquid chromatography with tandem mass spectrometry for peptide separation and identification.- iTRAQ (Isobaric Tags for Relative and Absolute Quantitation): Uses isobaric tags for multiplexed relative quantification of proteins across multiple samples [66]. | LC-MS/MS is the workhorse technology. iTRAQ allows for the simultaneous comparison of up to 8 different sample conditions. |
| Data Analysis | Identification of proteins from MS/MS spectra using databases (e.g., Swiss-Prot). Bioinformatic analysis (e.g., GO, KEGG) to identify enriched pathways. | Tools like MaxQuant, Proteome Discoverer, and PEAKS are commonly used. Functional analysis uses tools like DAVID and Ingenuity Pathway Analysis. |
Figure 1: Proteomic Profiling Workflow. The standard pipeline for proteomic analysis of endometrial receptivity, from sample collection to biomarker validation, utilizes various biological samples.
Key Proteomic Findings in Endometrial Receptivity
Proteomic studies have identified numerous proteins that are differentially expressed during the WOI, highlighting critical pathways such as immune modulation, antioxidant activity, and cellular invasion.
Table 2: Key Proteins Identified by Proteomic Studies of Endometrial Receptivity
| Protein | Regulation in WOI | Proposed Function in ER | Study Model |
|---|---|---|---|
| HMGB1 | Upregulated | Promotes cellular adhesion and immune modulation; a potential receptivity marker [66]. | Endometrial Tissue |
| ACSL4 | Upregulated | Implicated in lipid metabolism and energy production for receptive endometrium [66]. | Endometrial Tissue |
| SOD1, CAT, GSTO1 | Enriched in Fertile sEVs | Key antioxidant proteins (Superoxide Dismutase 1, Catalase, Glutathione S-Transferase Omega 1) that protect against oxidative stress in the uterine environment [68]. | Uterine Fluid sEVs |
| LGALS1/3 (Galectins) | Enriched in Secretory Phase | Promote trophoblast invasion and immune tolerance at the maternal-fetal interface [68]. | Uterine Fluid sEVs |
| S100A4/11 | Enriched in Secretory Phase | Calcium-binding proteins involved in cell invasion and motility processes critical for implantation [68]. | Uterine Fluid sEVs |
A particularly impactful finding is the role of small extracellular vesicles (sEVs) in endometrial-embryo communication. Proteomic profiling of sEVs isolated from uterine lavage of fertile women revealed a striking enrichment of proteins implicated in antioxidant activity and invasion during the secretory phase compared to the proliferative phase [68]. Functionally, sEVs derived from endometrial cells have been shown to enhance antioxidant function in trophectoderm cells and promote the invasive capacity of trophoblasts, which is necessary for successful implantation [68]. This highlights the potential of sEVs and their protein cargo as both functional mediators and non-invasive biomarkers of ER.
Metabolomic Profiling of Endometrial Receptivity
Metabolomics, the systematic study of small-molecule metabolites, provides a direct snapshot of the physiological state of the endometrium by capturing the end products of cellular processes. Metabolic shifts are now recognized as fundamental to the establishment of a receptive state.
Analytical Methodologies
Metabolomic profiling relies primarily on two analytical platforms: Mass Spectrometry (MS) and Nuclear Magnetic Resonance (NMR) spectroscopy.
Table 3: Key Metabolomic Profiling Methodologies
| Methodology | Principle | Advantages | Disadvantages |
|---|---|---|---|
| Liquid Chromatography-MS (LC-MS) | Separates metabolites via liquid chromatography before ionization and mass analysis. | High sensitivity, broad coverage of metabolites, can detect low-abundance compounds. | Requires metabolite separation, can be subject to ion suppression. |
| Gas Chromatography-MS (GC-MS) | Volatilizes metabolites for separation by gas chromatography before MS analysis. | Excellent separation resolution, highly reproducible, powerful libraries for ID. | Requires chemical derivatization for non-volatile metabolites, destructive. |
| Nuclear Magnetic Resonance (NMR) | Measures the absorption of radiofrequency radiation by atomic nuclei in a magnetic field. | Non-destructive, highly quantitative, requires minimal sample preparation. | Lower sensitivity compared to MS, limited metabolite coverage. |
The typical workflow involves metabolite extraction from endometrial tissue or uterine fluid, data acquisition using platforms like LC-MS or GC-MS, and subsequent data processing using bioinformatic tools for peak identification, alignment, and multivariate statistical analysis (e.g., PCA, PLS-DA) to identify differentially abundant metabolites.
Metabolic Signatures of a Receptive Endometrium
Metabolomic studies have revealed that the transition to a receptive state is characterized by significant shifts in energy metabolism and lipid signaling. A key finding is the alteration of the arachidonic acid pathway in the secretory-phase endometrium [66]. Arachidonic acid is a polyunsaturated fatty acid that serves as a precursor for eicosanoids, which are potent signaling molecules involved in inflammation, immune regulation, and vascular permeability—all processes critical for implantation.
Furthermore, lipids are now understood to be strictly controlled during the implantation period [67]. Lipidomic analysis, a subset of metabolomics, has highlighted the importance of lipid metabolism in providing energy for the demanding processes of endometrial remodelling and embryo implantation. Changes in specific lipid species, such as phospholipids and prostaglandins, are integral to the formation of the receptive phenotype. These metabolic changes collectively create a microenvironment that supports embryo development, attachment, and subsequent invasion.
Figure 2: Metabolic Pathway Shifts in Receptive Endometrium. The establishment of receptivity involves coordinated changes in key metabolic pathways that support the biological functions of implantation.
Integration with Multi-Omics and Clinical Translation
The integration of proteomic and metabolomic data with other omics layers, such as transcriptomics and genomics, is transforming the assessment of ER from a focus on static markers to a dynamic network analysis.
Multi-Omics Integration and Computational Analysis
Single-cell and spatial multi-omics technologies are now being applied to resolve cellular heterogeneity and localized molecular interactions within the endometrium [66]. For example, single-cell RNA sequencing has identified distinct transcriptomic signatures for the six major endometrial cell types during the WOI [63]. Integrating this data with proteomic profiles from uterine fluid or tissue homogenates provides a more comprehensive picture of the molecular dialogue between different cell lineages.
Machine learning (ML) models are increasingly used to integrate these complex multi-omics datasets to predict ER status and implantation success. Some studies have reported models achieving an Area Under the Curve (AUC) of greater than 0.9, demonstrating high predictive accuracy [66]. These models can identify key biomarker panels from proteomic and metabolomic data that are most indicative of a receptive state, moving beyond single-molecule biomarkers to a more robust, multi-factorial signature.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagent Solutions for Proteomic and Metabolomic Studies
| Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| RIPA Lysis Buffer | Efficient extraction of total protein from endometrial tissue biopsies for downstream proteomic analysis. | Protein extraction prior to digestion and LC-MS/MS analysis. |
| Trypsin (Sequencing Grade) | Proteolytic enzyme used to digest complex protein mixtures into peptides for mass spectrometry. | In-solution or in-gel digestion of endometrial tissue or EV protein extracts. |
| iTRAQ / TMT Reagents | Isobaric chemical tags for multiplexed, relative and absolute quantification of proteins across multiple samples. | Comparing the endometrial proteome across pre-receptive, receptive, and non-receptive phases. |
| Differential Centrifugation & Ultracentrifugation Kits | Standard method for the isolation of extracellular vesicles (EVs) from uterine lavage fluid or cell culture supernatants. | Isolation of sEVs from uterine lavage for proteomic profiling [68]. |
| LC-MS Grade Solvents (Acetonitrile, Methanol) | High-purity solvents for liquid chromatography to minimize background noise and ion suppression during MS. | Mobile phase preparation for LC-MS/MS in both proteomic and metabolomic workflows. |
| Deuterated Solvents & Internal Standards | Essential for NMR-based metabolomics and for quantitative MS to correct for variability in extraction and ionization. | Adding a known concentration of deuterated amino acids to endometrial tissue extracts for absolute quantification. |
| Tetracene-1-carboxylic acid | Tetracene-1-carboxylic acid, MF:C19H12O2, MW:272.3 g/mol | Chemical Reagent |
| Pent-4-ene-1-thiol | Pent-4-ene-1-thiol|Bifunctional Reagent for Research | Pent-4-ene-1-thiol is a bifunctional reagent featuring thiol and alkene groups, ideal for thiol-ene click chemistry and polymer science. For Research Use Only. Not for human or veterinary use. |
Proteomic and metabolomic profiling have unequivocally demonstrated that the functional landscape of the receptive endometrium is defined by dynamic shifts in protein networks and metabolic pathways. The identification of key players like HMGB1, ACSL4, antioxidant proteins in sEVs, and arachidonic acid metabolites has provided mechanistic insights into the processes of immune tolerance, trophoblast invasion, and energy metabolism that are essential for implantation. The analysis of uterine fluid and its extracellular vesicles represents a particularly promising frontier for developing non-invasive, mechanism-based diagnostic tests.
Looking forward, the field is moving towards a fully integrated multi-omics understanding of endometrial receptivity. The application of single-cell and spatial multi-omics will further decode the cellular heterogeneity and precise cell-to-cell communication networks within the endometrium [66]. Furthermore, the refinement of AI-driven models using large-scale proteomic and metabolomic datasets holds the potential to generate highly predictive algorithms for personalized embryo transfer, ultimately improving live birth rates for patients undergoing assisted reproduction. The continued validation of these biomarkers and models in large, prospective clinical cohorts will be the critical next step in translating these research findings into clinical practice, thereby addressing one of the most significant challenges in reproductive medicine.
Integrating Multi-Omics Data for Systems Biology Views of Implantation and Early Development
The application of multi-omics technologies in reproductive biology represents a paradigm shift, enabling an unprecedented, systems-level investigation of the complex molecular events governing implantation and early embryonic development. These critical developmental stages were previously shrouded in mystery due to technological limitations and ethical considerations surrounding human embryo research. The integration of genomic, proteomic, transcriptomic, and metabolomic data provides a powerful framework for deciphering the intricate signaling networks, cellular interactions, and temporal dynamics that underpin successful reproduction. Framed within the broader context of omics technologies in reproductive research, this technical guide outlines comprehensive methodologies and analytical frameworks for generating holistic systems biology views of early reproductive processes, offering researchers, scientists, and drug development professionals actionable protocols and visualization strategies to advance this transformative field.
Core Multi-Omics Approaches in Reproductive Biology
The systematic application of multi-omics technologies has begun to illuminate the complex interplay between various molecular layers during early reproductive events. Several pioneering studies have established frameworks for integrating diverse omics datasets to uncover previously inaccessible biological insights into implantation and early development.
Reproductive Microbiome and Systems Biology
A comprehensive prospective, observational study employs a systems biology approach to investigate the microbiome profile across different body sites in relation to reproductive health. This research examines the normal menstrual cycle (with and without hormonal contraception), recurrent pregnancy loss (RPL) before and during pregnancy, and endometriosis before, during, and after surgery. The study design involves longitudinal profiling of 920 participants across three cohorts until 2024, specifically investigating how microbiome profiles interact with genetics, environmental exposures, and immunological and endocrine biomarkers. Microbiome profiles from saliva, feces, rectal mucosa, vaginal fluid, and endometrium are studied alongside omics profiles, endocrine-disrupting chemicals, and endocrine and immune factors in blood, hair, saliva, and urine. This integrated approach allows researchers to evaluate correlations between multi-omic signatures and mental and physical reproductive health outcomes [69].
Integrated Metagenomic and Metatranscriptomic Analysis
The Integrated Meta-omic Pipeline (IMP) provides a reproducible and modular framework for the reference-independent integrated analysis of coupled metagenomic and metatranscriptomic data. IMP incorporates robust read preprocessing, iterative co-assembly, analyses of microbial community structure and function, automated binning, and genomic signature-based visualizations. This workflow demonstrates that an integrated data analysis strategy enhances data usage, output volume, and output quality compared to single-omic approaches. The pipeline is particularly valuable for investigating host-microbiome interactions during early reproductive events, where microbial communities may influence implantation success and embryonic development through metabolic and immunomodulatory mechanisms [70].
Multi-Omics Integration for Identifying Therapeutic Targets
A recent study on ulcerative colitis demonstrates a powerful multi-omics integration methodology that can be adapted for reproductive biology research. This approach combines data samples from the Gene Expression Omnibus database and protein quantitative trait loci data from genome-wide association studies to identify overlapping genes. Researchers then employed three machine learning algorithms to screen core hub genes from these overlapping genes, followed by the construction and external validation of a diagnostic model. Single-cell sequencing data explored the expression profiles of core hub genes across different cell types, supplemented by immune infiltration analysis, functional enrichment, and regulatory network construction [71]. This methodological framework offers a transferable paradigm for identifying key molecular players in implantation and early development.
Spatial Multi-Omics in Developmental Biology
A groundbreaking study on human dental epithelium during tooth development exemplifies the power of integrating single-cell RNA sequencing, spatial transcriptomics, and secretome analysis to characterize developmental processes over time. This approach enabled the mapping of a spatiotemporal atlas of human tooth development at multiple levels, identifying previously uncharacterized epithelial subpopulations with distinct gene expression profiles and spatial localization. The research characterized dynamic changes in epithelial-mesenchymal interactions across developmental stages and used secretome analysis to confirm extensive paracrine signaling between tissue compartments [72]. This integrated multi-omics strategy is directly applicable to investigating the spatial and temporal dynamics of embryo-maternal communication during implantation.
Table 1: Quantitative Data Analysis Methods for Multi-Omics Data
| Analysis Method | Primary Function | Application in Reproductive Biology | Tools and Software |
|---|---|---|---|
| Cross-Tabulation | Analyzes relationships between categorical variables | Identifying associations between microbial taxa and reproductive outcomes | Excel, R, Python |
| MaxDiff Analysis | Identifies most preferred items from a set of options | Prioritizing biomarker candidates from multi-omics datasets | Custom survey tools, statistical packages |
| Gap Analysis | Compares actual performance to potential | Assessing differences in molecular profiles between fertile and infertile populations | Progress Charts, Radar Charts |
| Text Analysis | Extracts insights from unstructured textual data | Mining scientific literature and clinical notes for biomarker discovery | Voyant, Word Clouds |
| Data Mining | Detects hidden patterns and relationships in large datasets | Uncovering novel associations across multi-omics datasets | Python, R, specialized algorithms |
Experimental Protocols and Methodologies
Proteome-Wide Mendelian Randomization Analysis
Mendelian randomization (MR) analysis represents a powerful method for inferring causal relationships between exposure factors and disease outcomes using genetic variants as instrumental variables. The protocol for proteome-wide MR analysis involves several critical steps:
Exposure Data Preparation: Obtain genetic summary statistics related to plasma proteins from large-scale pQTL studies. Specifically, select cis-pQTLs (pQTLs located near the corresponding genes of specific proteins) as instrumental variables to minimize bias from horizontal pleiotropy. Apply stringent filters: genome-wide significant associations (P < 5 × 10â»â¸), independent associations (linkage disequilibrium r² < 0.001), and F-test value greater than 10 [71].
Outcome Data Sourcing: Acquire summary-level GWAS data for the reproductive outcome of interest from databases such as the IEU Open GWAS Project. Ensure case definitions are based on standardized diagnostic criteria, such as International Classification of Diseases codes for reproductive conditions [71].
MR Implementation: Conduct the proteome-wide MR analysis using the "TwoSampleMR" R package. Utilize the harmonize_data function to align effect alleles and effect sizes across datasets. Apply multiple MR methods for robust causal inference: MR Egger, weighted median, inverse variance weighted (IVW), simple mode, and weighted mode. The IVW method is generally considered the primary analysis when all genetic variants are valid instruments [71].
Sensitivity Analyses: Perform comprehensive sensitivity analyses to validate MR assumptions, including tests for horizontal pleiotropy using MR-Egger regression and Cochran's Q statistic to assess heterogeneity.
This MR framework can be adapted to investigate causal relationships between plasma proteins and reproductive outcomes such as implantation failure, early pregnancy loss, or endometriosis.
Integrated Metagenomic and Metatranscriptomic Processing
The IMP workflow provides a standardized protocol for processing coupled metagenomic and metatranscriptomic data:
Input Data Preparation: Collect MG and MT paired-end reads in FASTQ format. For MT data, perform ribosomal RNA depletion prior to sequencing whenever possible [70].
Preprocessing and Quality Control: Process MG and MT reads independently through quality control steps. This includes adapter trimming, quality filtering, and removal of low-complexity sequences. Optionally, screen for host/contaminant sequences using reference genomes relevant to reproductive studies (e.g., maternal genomic contamination) [70].
rRNA Filtering: Apply in silico ribosomal RNA sequence depletion exclusively to MT data using specialized databases of rRNA sequences [70].
Iterative Co-assembly: Begin with an initial assembly of preprocessed MT reads to generate an initial set of MT contigs. Perform iterative assembly of MT reads unmappable to the initial contig set. Use the combined MT contigs from initial and iterative assemblies to enhance subsequent co-assembly with MG data. Conduct co-assembly using de novo assemblers such as MEGAHIT or IDBA-UD with appropriate parameters for handling the uneven sequencing depths characteristic of multi-omic datasets [70].
Post-assembly Analysis: Map processed reads back to the co-assembled contigs for quantitative analysis. Perform taxonomic classification, functional annotation, and gene abundance quantification using standardized databases and protocols [70].
This integrated assembly strategy enhances data usage and output quality compared to analyzing MG and MT data separately, making it particularly valuable for investigating the functional potential and activity of reproductive microbiomes.
Machine Learning-Based Biomarker Discovery
The integration of machine learning algorithms with multi-omics data enables robust identification of diagnostic and prognostic biomarkers for reproductive conditions:
Data Integration and Preprocessing: Combine datasets from multiple sources (e.g., GEO microarray data, pQTL data, GWAS summary statistics) and apply batch correction using algorithms such as those implemented in the "sva" R package [71].
Differential Expression Analysis: Identify differentially expressed genes (DEGs) between case and control groups (e.g., recurrent pregnancy loss versus normal pregnancy) using appropriate statistical methods with multiple testing correction.
Identification of Overlapping Genes: Find the intersection between DEGs and genes identified through MR analysis or other causal inference methods [71].
Machine Learning Feature Selection: Apply multiple machine learning algorithms to screen core hub genes from the overlapping genes. Effective approaches include:
- Random Forest (RF) for assessing variable importance
- Support Vector Machine-Recursive Feature Elimination (SVM-RFE) for feature ranking and selection
- LASSO regression for feature selection with regularization
Diagnostic Model Construction: Build a nomogram model using the identified core hub genes and validate its predictive performance in an independent validation dataset [71].
Single-Cell Validation: Explore the expression profiles of core hub genes across different cell types using single-cell RNA sequencing data to validate cell-type-specific expression patterns [71].
Table 2: Essential Research Reagent Solutions for Multi-Omics Studies
| Reagent Category | Specific Examples | Function in Multi-Omics Research |
|---|---|---|
| Sample Collection | PAXgene Blood RNA tubes, Streck cell-free DNA blood collection tubes | Stabilizes nucleic acids in blood samples for transcriptomic and genomic analyses |
| Nucleic Acid Extraction | Qiagen AllPrep DNA/RNA/miRNA Universal Kit, Norgen Biotek Corp. BioFluid RNA/DNA Extraction Kit | Simultaneous isolation of high-quality DNA and RNA from limited clinical samples |
| Protein Analysis | Multiplexed aptamer-based binding assays (SOMAscan), Olink Proximity Extension Assay | High-throughput quantification of thousands of proteins from minimal sample volumes |
| Single-Cell RNA Sequencing | 10x Genomics Chromium Single Cell Gene Expression Solution, BD Rhapsody Cartridges | Enables transcriptome profiling at single-cell resolution from complex tissues |
| Spatial Transcriptomics | 10x Genomics Visium Spatial Gene Expression Slide, Nanostring GeoMx Digital Spatial Profiler | Correlates gene expression data with spatial localization in tissue sections |
Visualization and Data Integration Techniques
Effective visualization and integration of multi-omics data are essential for extracting biologically meaningful insights from these complex datasets. The following workflows and techniques facilitate comprehensive systems biology views of implantation and early development.
Multi-Omics Data Integration Workflow
The following diagram illustrates a comprehensive workflow for integrating multi-omics data to investigate implantation and early development, from experimental design through biological validation:
Quantitative Data Analysis and Visualization
Quantitative data analysis methods are crucial for discovering trends, patterns, and relationships within multi-omics datasets. Effective visualization techniques transform complex numerical data into interpretable formats that facilitate scientific communication and decision-making.
Descriptive Statistics: Begin with measures of central tendency (mean, median, mode) and dispersion (range, variance, standard deviation) to summarize dataset characteristics. These provide an initial snapshot of data distribution and variability across experimental groups [73].
Inferential Statistics: Employ hypothesis testing, T-tests, ANOVA, regression analysis, and correlation analysis to make generalizations from sample data to larger populations. These methods test relationships, identify significant differences between groups, and predict outcomes based on multi-omics patterns [73].
Specialized Analytical Techniques:
- Cross-Tabulation: Analyze relationships between categorical variables, such as associations between specific microbial taxa and reproductive outcomes, presented in contingency tables and visualized using stacked bar charts [73].
- Gap Analysis: Compare actual molecular profiles to expected or desired states (e.g., comparing biomarker levels between fertile and infertile populations) using progress charts or radar charts [73].
- Text Analysis: Extract insights from unstructured textual data, such as scientific literature or clinical notes, using word frequency analysis and word clouds to identify emerging themes or biomarker mentions [73].
Visualization Tools: Leverage specialized tools for creating advanced visualizations without coding, such as ChartExpo for Excel and Google Sheets, or programming-based approaches using R (ggplot2), Python (Matplotlib, Seaborn), and JavaScript libraries (D3.js) [73]. For specialized network visualizations, tools like RAWGraphs provide open-source, web-based solutions for creating more complex chart types that are difficult to produce with standard business intelligence software [74].
Accessibility in Data Visualization
When creating visualizations for multi-omics data, ensure sufficient color contrast between foreground elements (text, arrows, symbols) and their background to accommodate diverse viewers. The Web Content Accessibility Guidelines (WCAG) recommend a contrast ratio of at least 4.5:1 for standard text and 7:1 for smaller text [75]. For diagram creation, explicitly set text color (fontcolor) to have high contrast against node background colors (fillcolor). JavaScript libraries like chroma.js can assist with color conversions and contrast calculations, while specialized modules like font-color-contrast can automatically select optimal font colors (black or white) based on background brightness [76] [77].
The integration of multi-omics data represents a transformative approach for developing comprehensive systems biology views of implantation and early embryonic development. By combining genomic, transcriptomic, proteomic, metabolomic, and microbiome data through sophisticated computational frameworks, researchers can now decipher the complex molecular dialogues that govern successful reproduction. The methodologies outlined in this technical guide—from proteome-wide Mendelian randomization and integrated metagenomic-metatranscriptomic analysis to machine learning-based biomarker discovery—provide actionable protocols for generating and interpreting these complex datasets. As these multi-omics approaches continue to evolve and become more accessible, they hold tremendous promise for unraveling the mysteries of early human development, identifying novel therapeutic targets for reproductive disorders, and ultimately improving clinical outcomes in reproductive medicine. The ongoing standardization of analytical workflows and visualization techniques will further enhance the reproducibility and biological relevance of multi-omics studies in reproductive biology, cementing their role as indispensable tools in the modern reproductive researcher's toolkit.
Navigating Challenges: Technical Hurdles and Optimization Strategies in Reproductive Omics
The integration of preimplantation genetic testing for aneuploidy (PGT-A) into in vitro fertilization (IVF) protocols represents a significant advancement in reproductive medicine, yet it concurrently reveals critical evidence gaps concerning its clinical utility and long-term implications. The recent development of non-invasive PGT-A (niPGT-A) offers a paradigm shift by analyzing cell-free DNA from spent culture medium, potentially mitigating risks associated with conventional trophectoderm biopsy. This whitepaper provides a technical reassessment of both technologies within the broader context of omics-driven reproductive biology, examining their methodological frameworks, diagnostic accuracy, clinical validation pathways, and integration with multi-omics platforms. Through critical evaluation of comparative performance data, technical limitations, and emerging optimization strategies, we identify persistent evidence gaps and propose standardized validation frameworks essential for translating these technologies into reliable clinical applications for research and drug development communities.
The application of omics technologies in reproductive biology has revolutionized our understanding of embryonic development and chromosomal stability. Preimplantation genetic testing has evolved from a basic morphological assessment to a comprehensive chromosomal screening tool, with recent advances focusing on less invasive methodologies that align with the precision medicine paradigm.
- PGT-A Evolution: Conventional PGT-A utilizing trophectoderm biopsy has demonstrated clinical benefits in selected cases but raises concerns regarding embryo invasiveness, technical expertise requirements, and diagnostic accuracy for mosaic embryos [78].
- niPGT-A Emergence: The discovery of cell-free DNA (cfDNA) in spent blastocyst culture medium has enabled the development of niPGT-A, presenting a potentially safer alternative that avoids direct embryo manipulation [78] [79].
- Multi-omics Integration: The future of embryo selection lies in integrating genetic assessment with transcriptomic, metabolomic, and proteomic profiling, creating a comprehensive viability evaluation framework [78].
Despite technological advancements, significant evidence gaps persist in standardized protocols, clinical validation, and understanding the biological origins of cfDNA, necessitating critical reassessment before widespread clinical implementation.
Technical Methodologies and Workflows
Conventional PGT-A via Trophectoderm Biopsy
The established PGT-A methodology involves several technically complex steps requiring specialized equipment and expertise:
- Embryo Culture: Embryos are cultured to blastocyst stage (day 5-6) using sequential media systems under optimized conditions [80].
- TE Biopsy: Laser-assisted hatching precedes the excision of 5-10 trophectoderm cells using micromanipulation systems [78] [81].
- Genetic Analysis: Whole genome amplification followed by next-generation sequencing or microarray analysis detects chromosomal aneuploidies with resolution for segmental imbalances (>4-10 Mb) and mosaicism (>30%) [80].
Table 1: Key Research Reagent Solutions for PGT-A
| Reagent/Kit | Primary Function | Technical Specifications |
|---|---|---|
| SurePlex WGA System | Whole genome amplification | Amplifies limited DNA input from biopsy samples |
| VeriSeq PGS Kit | NGS-based aneuploidy detection | Detects whole chromosome aneuploidies and segmental imbalances |
| 24Sure Microarray | aCGH-based ploidy assessment | Provides rapid aneuploidy screening without sequencing |
| BlueFuse Multi Software | Bioinformatic analysis | Interprets NGS/microarray data for ploidy calling |
Non-Invasive PGT-A Methodologies
niPGT-A utilizes cfDNA released into spent culture medium through apoptotic and necrotic processes, with potential active DNA secretion mechanisms [79]. The procedural workflow encompasses:
- Medium Collection: Spent culture medium (10-25µL) is collected immediately before TE biopsy, typically on day 5 or 6 of embryo development [80] [81].
- Contamination Mitigation: Strict protocols minimize maternal DNA contamination, including cumulus cell removal, ICSI fertilization, and sterile handling procedures [81] [82].
- DNA Amplification and Sequencing: Whole-genome amplification of cfDNA using methods like MALBAC or NICSInst precedes NGS library preparation and sequencing [80] [79].
Diagram 1: niPGT-A Experimental Workflow. SCM = spent culture medium.
Comparative Performance Analysis
Diagnostic Accuracy Metrics
Recent studies demonstrate variable performance between niPGT-A and conventional PGT-A, highlighting persistent technical challenges:
Table 2: Comparative Performance Metrics of niPGT-A vs. TE Biopsy PGT-A
| Performance Parameter | niPGT-A Results | TE Biopsy PGT-A | Clinical Implications |
|---|---|---|---|
| Successful Amplification Rate | 69.4% (Day 5) to 97.9% (Day 6) [81] | ~100% [81] | Extended culture improves DNA yield |
| Ploidy Concordance Rate | 62.1% - 91.3% [83] [84] | Reference standard | Protocol optimization critical |
| Sensitivity | 81.6% - 91.6% [81] [84] | >99% [80] | High false-positive rates concerning |
| Specificity | 48.3% - 50.7% [81] [84] | >99% [80] | Risk of discarding viable embryos |
| Mosaicism Detection | Limited accuracy [79] | Detects 30-70% mosaicism [80] | Biological representation challenges |
Biological and Technical Limitations
The diagnostic performance of niPGT-A is constrained by several fundamental biological and technical factors:
- cfDNA Origin Uncertainty: The precise cellular origins of cfDNA remain debated, with potential contributions from trophectoderm, inner cell mass, and apoptotic fragments, potentially skewing chromosomal representation [78] [79].
- Maternal Contamination: Despite ICSI fertilization, maternal DNA contamination occurs in approximately 29.8% of SCM samples, with 2.5% showing contamination ratios ≥50% [82].
- Variable DNA Yield: cfDNA quantity and quality exhibit significant inter-embryo variability influenced by culture duration, embryo quality, and zona pellucida integrity [81] [79].
Clinical Validation and Outcomes
Pregnancy Outcome Correlation
The ultimate validation of any PGT methodology lies in its correlation with meaningful clinical outcomes:
- High False-Positive Rates: niPGT-A classifies more embryos as aneuploid (75.3%) compared to TE biopsy (58.5%), potentially leading to discarding of viable embryos [81].
- Unexpected Pregnancy Success: Blastocysts diagnosed as euploid by TE biopsy but aneuploid by niPGT-A demonstrated unexpectedly high pregnancy (94%) and live birth (88%) rates, indicating significant diagnostic inaccuracy [81].
- Optimized Protocol Performance: One recent study implementing an optimized niPGT-A workflow reported superior positive predictive value (92.1%) and accuracy (91.3%) compared to conventional PGT-A [83].
Ongoing Validation Initiatives
Several structured clinical trials are addressing the evidence gaps in niPGT-A clinical utility:
- Multicenter RCT: A double-blind, multicenter randomized controlled trial (ChiCTR2100051408) is comparing niPGT-A with conventional IVF in 1,140 patients across eight centers, with live birth rate after first embryo transfer as the primary endpoint [85].
- Backup Utility Applications: Research indicates SCM can serve as a backup genetic material source when mosaic results or amplification failures occur in conventional PGT-A, potentially avoiding harmful secondary biopsies [80].
Diagram 2: Comprehensive Validation Framework for niPGT-A
Emerging Innovations and Future Directions
Technical Optimization Strategies
Several promising approaches are emerging to address current niPGT-A limitations:
- Extended Culture Duration: Prolonging culture to day 6 significantly improves niPGT-A informativity rates from 69.4% to 97.9%, enhancing cfDNA yield [81].
- Advanced Contamination Control: Genotyping assays and bioinformatic subtraction methods enable identification and quantification of maternal DNA contamination [82].
- Integration with Morphokinetics: Combining niPGT-A with time-lapse imaging and artificial intelligence algorithms provides complementary embryo selection criteria [78].
Multi-Omics Integration Framework
The future of embryo selection lies in integrated diagnostic approaches:
- Metabolomic Profiling: Analysis of spent medium for metabolic biomarkers provides additional viability indicators beyond chromosomal status [78].
- Transcriptomic Analysis: Though technically challenging, transcriptomic profiling of cfDNA could reveal functional embryonic characteristics [86].
- Proteomic Signatures: Identification of embryonic and endometrial protein markers could enhance implantation prediction [86].
This critical reassessment identifies persistent evidence gaps in both conventional PGT-A and emerging niPGT-A technologies. While niPGT-A presents a promising non-invasive alternative to TE biopsy, its clinical implementation remains premature due to unresolved biological questions and technical limitations. The high diagnostic specificity reported in optimized workflows (91.3%) demonstrates potential, but widespread variability in performance metrics underscores the need for standardized protocols and rigorous validation.
For the research and drug development community, priority areas include elucidating the biological mechanisms of cfDNA release, establishing quantitative thresholds for contamination tolerance, and developing integrated multi-omics assessment platforms. Furthermore, prospective randomized trials with clinical outcome measures, rather than solely concordance rates with TE biopsy, are essential to validate niPGT-A's clinical utility. Only through addressing these evidence gaps can these technologies fulfill their potential in advancing reproductive precision medicine.
The application of omics technologies in reproductive biology research has revolutionized our understanding of complex processes from gametogenesis to embryogenesis. These advances have created unprecedented opportunities to address pressing reproductive challenges, including declining fertility rates and the need for improved diagnostic and therapeutic tools [87]. However, the transformative potential of genomic, transcriptomic, proteomic, and metabolomic data is hampered by significant technical and analytical challenges in data integration.
Multi-omics integration represents the methodological foundation for studying biological systems holistically by combining data from multiple molecular levels to highlight interrelationships among biomolecules and their functions [88]. In reproductive medicine, this approach is particularly valuable for understanding the precise molecular regulations required for successful reproduction, yet researchers face substantial hurdles in effectively combining and interpreting diverse data types [87]. The complexity of reproductive processes, which involve intricate molecular networks and intercellular communications, demands integration methods that can capture multidimensional biological information [89].
This technical guide examines the core challenges, methodologies, and practical implementations of multi-omics data integration frameworks specifically within the context of reproductive biology research. By addressing these integration hurdles, researchers can transition from accumulating large-scale omics data to generating actionable biological insights that advance both fundamental understanding and clinical applications in reproductive medicine.
Fundamental Challenges in Multi-Omics Data Integration
Technical and Analytical Hurdles
The path to effective multi-omics integration is fraught with technical challenges that must be systematically addressed. Data heterogeneity remains a primary obstacle, as omics technologies generate data with different scales, distributions, and statistical properties. This heterogeneity is compounded by the high dimensionality of omics data, where the number of features (genes, proteins, metabolites) vastly exceeds the number of samples, creating computational and statistical challenges for robust integration [88].
Missing data presents another significant hurdle, as not all omics layers are typically measured for every sample in a study. Batch effects and technical variability introduced during sample processing can substantially impact resulting biological interpretations [90]. Additionally, the substantial storage and computational demands for processing and integrating large-scale multi-omics datasets require sophisticated infrastructure that may not be accessible to all research groups [90].
Biological and Spatial Complexity
Reproductive biology introduces unique biological complexities that complicate data integration. The dynamic nature of reproductive processes, including gamete development and embryonic growth, requires methods that can incorporate temporal dimensions [89]. Cellular heterogeneity within reproductive tissues further complicates integration, as bulk omics measurements may obscure important cell-type-specific signals [89].
Spatial organization represents a critical dimension in reproductive tissues, where the physical arrangement of cells influences their function and communication. Traditional single-cell approaches, while valuable, sacrifice this spatial context, necessitating advanced integration methods that can preserve or reconstruct spatial relationships [91]. Understanding reproductive processes such as implantation or placental development requires capturing these complex spatial patterns alongside molecular measurements.
Data Quality and Metadata Standards
The reusability and reproducibility of integrated omics analyses are heavily dependent on data quality and comprehensive metadata reporting. Incomplete or incorrect metadata can lead to significant misinterpretations of biological phenomena [90]. The consistency of laboratory methods, including variations in sample processing kits and protocols, can dramatically impact resulting taxonomic community profiles or molecular measurements, complicating cross-study integration [90].
The FAIR (Findable, Accessible, Interoperable, and Reusable) data principles provide a framework for addressing these challenges, but their implementation requires careful attention to metadata standards, clear communication, and standardized protocols [90]. Without these safeguards, the integration of diverse datasets may produce misleading or irreproducible results.
Computational Frameworks and Integration Methodologies
Unsupervised Integration Approaches
Unsupervised methods for multi-omics integration identify patterns and structures in data without predefined sample labels or outcomes. These approaches are particularly valuable for exploratory analysis and hypothesis generation in reproductive biology, where the underlying molecular subtypes of reproductive conditions may not be fully characterized.
Matrix factorization techniques decompose high-dimensional omics data into lower-dimensional representations that capture the essential biological signals. Methods such as Joint Non-negative Matrix Factorization (NMF) project variations among datasets onto a dimension-reduced space to detect coherent patterns across omics layers [92]. The factorization follows the formula:
where X is the original data matrix, W represents common factors, and H contains the coefficients [92]. iCluster and its enhanced version iCluster+ employ a similar concept but without non-negative constraints, incorporating different modeling approaches for diverse data types including binary, continuous, and categorical measurements common in reproductive studies [92].
Joint and Individual Variation Explained (JIVE) extends these approaches by decomposing each omics layer into three components: joint variation across data types, structured variation specific to each data type, and residual noise [92]. This separation allows researchers to distinguish biological signals shared across omics platforms from those specific to individual measurements, which is particularly valuable for understanding coordinated molecular events in reproductive processes.
Table 1: Unsupervised Multi-Omics Integration Methods
| Method | Core Approach | Data Type Compatibility | Key Advantages | Limitations |
|---|---|---|---|---|
| Joint NMF | Matrix factorization with non-negativity constraints | Continuous, non-negative | Intuitive pattern recognition; clear biological interpretability | Requires non-negative input; sensitive to normalization |
| iCluster+ | Regularized latent variable model | Mixed types (continuous, binary, count) | Handles diverse data types; incorporates sparsity | Computationally intensive; requires feature selection |
| JIVE | Variance decomposition into joint and individual structures | Continuous | Separates shared and specific variation; PCA-based framework | Sensitive to outliers; requires rank selection |
| Bayesian Factor | Beta-Bernoulli process for factor estimation | Continuous | Identifies both shared and unique features; sparsity promotion | Assumes linear relationships; complex implementation |
Supervised and Semi-Supervised Integration
Supervised integration methods leverage known sample labels or clinical outcomes to guide the integration process, making them particularly valuable for translational research in reproductive medicine. These approaches can enhance prediction accuracy for clinically relevant endpoints such as infertility subtypes, pregnancy outcomes, or treatment responses.
Multiple Kernel Learning (MKL) combines similarity matrices (kernels) from different omics data types to build predictive models [92]. By optimally weighting the contribution of each omics layer, MKL can capture complementary biological information relevant to reproductive conditions. Network-based supervised integration incorporates biological network information to place multi-omics measurements in the context of known molecular interactions, which can reveal dysregulated pathways in reproductive disorders [92].
Semi-supervised approaches represent a middle ground, leveraging both labeled and unlabeled samples to improve integration performance. These methods are particularly useful in reproductive biology research where obtaining large datasets with complete clinical annotations remains challenging.
Spatial Multi-Omics Integration
The integration of spatial information with molecular profiles represents a cutting-edge approach in reproductive biology, where tissue architecture plays a crucial role in function. Novel tools such as the Multi-Omics Imaging Integration Toolset (MIIT) have been developed specifically for integrating spatially resolved multi-omics data from serial tissue sections [91].
MIIT employs a non-rigid registration algorithm called GreedyFHist to align serial sections, enabling the correlation of transcriptional and metabolic heterogeneity within tissue architecture [91]. This approach has been successfully applied to integrate spatial transcriptomics and mass spectrometry imaging data from prostate tissue, revealing relationships between gene signatures and metabolic measurements [91]. Similar methodologies can be adapted to reproductive tissues to explore spatial patterns of molecular expression in endometrium, placenta, or gonadal tissues.
Diagram 1: Spatial multi-omics integration workflow for serial tissue sections
Practical Implementation and Workflow
Data Acquisition and Preprocessing
Successful multi-omics integration begins with rigorous experimental design and data preprocessing. For reproductive biology studies, researchers must carefully consider sample collection methods, ensuring consistency across omics platforms. The initial preprocessing phase should include:
Quality Control and Normalization: Each omics dataset requires platform-specific quality assessment, including checks for batch effects, sample outliers, and technical artifacts. Normalization methods should be chosen to address the specific characteristics of each data type while preserving biological signals [88].
Feature Selection: Given the high dimensionality of omics data, strategic feature selection is essential to reduce noise and computational complexity. Methods may include filtering low-variance features, selecting known reproductive biology markers, or employing statistical criteria tailored to each data type [92].
Data Transformation and Scaling: Appropriate transformation (e.g., log transformation for RNA-seq data) and scaling ensure comparability across omics layers. The choice of scaling method (e.g., Z-score normalization, min-max scaling) depends on the distributional characteristics of each data type and the integration method to be employed.
Integration Workflows for Reproductive Biology
A typical multi-omics integration workflow for reproductive biology research involves several interconnected steps, each requiring careful methodological choices:
Diagram 2: Comprehensive multi-omics integration workflow for reproductive biology
The Scientist's Toolkit: Essential Research Reagents and Computational Tools
Successful implementation of multi-omics integration requires both wet-lab reagents and computational resources. The following table outlines key components of the integrated omics research toolkit:
Table 2: Essential Research Reagent Solutions for Multi-Omics Studies in Reproductive Biology
| Category | Specific Tools/Reagents | Function in Multi-Omics Pipeline | Reproductive Biology Applications |
|---|---|---|---|
| Sample Preparation | Single-cell dissociation kits | Tissue processing for single-cell assays | Analysis of heterogeneous reproductive tissues (ovary, testis, endometrium) |
| Spatial Transcriptomics | 10x Genomics Visium, Slide-seq | Spatial mapping of gene expression | Localization of gene expression in placental villi, uterine lining |
| Proteomics | TMT/Isobaric tags, Antibody panels | Protein quantification and identification | Signaling pathway analysis in embryo implantation |
| Metabolomics | Mass spectrometry columns, Standards | Metabolite identification and quantification | Assessment of embryo culture media, follicular fluid composition |
| Computational Tools | Seurat, Scanpy, MIIT | Single-cell and spatial data analysis | Cell type identification in reproductive tissues [89] |
| Integration Frameworks | MOGONET, PathIntegrate, MOFA | Multi-omics data integration | Subtype stratification of reproductive cancers [93] |
Applications in Reproductive Biology and Medicine
Advancing Fundamental Understanding of Reproductive Processes
Multi-omics integration has enabled significant advances in understanding fundamental reproductive processes. For example, single-cell multi-omics approaches have been used to delineate the complex molecular events during gametogenesis and embryogenesis [89]. By simultaneously measuring transcriptomes, epigenomes, and proteomes in individual cells, researchers have identified novel regulatory programs and cellular heterogeneity in developing gametes and embryos [87] [89].
These approaches have revealed unique aspects of gene expression during oocyte development, leading to new understanding of key regulators in donkey oocyte development from germinal vesicle to metaphase stage [87]. Similar strategies applied to human reproductive tissues have the potential to uncover previously uncharacterized molecular pathways relevant to fertility and early development.
Diagnostic Biomarker Discovery and Clinical Translation
The integration of multi-omics data has accelerated the identification of diagnostic biomarkers for reproductive conditions. For instance, integrating metabolomics and transcriptomics has revealed molecular perturbations underlying prostate cancer, with the metabolite sphingosine demonstrating high specificity and sensitivity for distinguishing prostate cancer from benign prostatic hyperplasia [88]. Similar approaches can be applied to reproductive cancers and benign conditions affecting fertility.
In reproductive medicine, multi-omics integration has been particularly valuable for understanding repeated implantation failure and recurrent pregnancy loss [87]. By combining genomic, transcriptomic, and proteomic data from endometrial samples, researchers have begun to identify molecular signatures associated with receptivity, offering potential biomarkers to guide clinical decision-making in assisted reproductive technologies.
Several large-scale data repositories provide foundational resources for multi-omics studies in reproductive biology. While not exclusive to reproductive tissues, these databases contain valuable datasets relevant to reproductive health:
Table 3: Public Data Repositories for Multi-Omics Research
| Repository | Data Types | Relevant Reproductive Content | Access Information |
|---|---|---|---|
| The Cancer Genome Atlas (TCGA) | Genomic, transcriptomic, epigenomic, proteomic | Uterine, ovarian, cervical cancers | https://cancergenome.nih.gov/ [88] |
| Clinical Proteomic Tumor Analysis Consortium (CPTAC) | Proteomic, phosphoproteomic | Proteogenomic analysis of endometrial and ovarian cancers | https://cptac-data-portal.georgetown.edu/ [88] |
| International Cancer Genome Consortium (ICGC) | Whole genome sequencing, genomic variations | Pediatric and adult reproductive cancers | https://icgc.org/ [88] |
| Omics Discovery Index | Consolidated multi-omics datasets | Reproductive relevant datasets from 11 repositories | https://www.omicsdi.org/ [88] |
Future Perspectives and Concluding Remarks
As multi-omics technologies continue to evolve, several emerging trends promise to further advance reproductive biology research. Single-cell multi-omics is rapidly developing beyond transcriptomics to include simultaneous measurement of chromatin accessibility, DNA methylation, protein expression, and spatial information [89]. These technological advances will enable increasingly comprehensive profiling of individual cells within complex reproductive tissues.
Computational methods are also progressing toward more sophisticated integration frameworks that can accommodate temporal dynamics, spatial relationships, and the unique characteristics of diverse molecular measurements. Machine learning and artificial intelligence approaches are being increasingly employed to extract subtle patterns from integrated omics data, with potential applications in predicting reproductive outcomes and personalizing treatment strategies [90] [89].
However, significant challenges remain in standardizing integration workflows, ensuring reproducibility, and translating computational findings into biological insights and clinical applications. The development of community standards and collaborative initiatives, such as the International Microbiome and Multi'Omics Standards Alliance (IMMSA) and the Genomic Standards Consortium (GSC), will be crucial for addressing these challenges [90].
In conclusion, overcoming data integration hurdles requires a multidisciplinary approach combining rigorous experimental design, appropriate computational methods, and biological expertise. By effectively implementing the frameworks and methodologies outlined in this guide, researchers in reproductive biology can transform big data into actionable biological insights that advance both fundamental knowledge and clinical practice in reproductive medicine.
The integration of omics technologies—including genomics, transcriptomics, proteomics, and metabolomics—into reproductive biology research has revolutionized our understanding of molecular regulations governing gametogenesis, embryogenesis, and reproductive pathologies [87]. However, the complexity and sheer volume of data generated by these high-throughput technologies necessitate rigorous standards to ensure analytical reliability. In fields such as infertility research, maternal-fetal biology, and assisted reproductive technologies, the implications of unreliable data extend beyond scientific publication to direct clinical applications affecting human reproduction and health [87]. This technical guide establishes a framework for maintaining analytical rigor through standardized protocols, robust quality control measures, and reproducible computational approaches specifically contextualized within reproductive biology research.
Standardization in Omics Workflows
The Imperative for Standardized Protocols
Standardization forms the foundational element of analytical rigor in omics sciences, enabling meaningful comparisons across different studies, platforms, and laboratories. In reproductive biology, where sample sizes are often limited due to the challenges of procuring clinical specimens, standardized protocols are particularly crucial for pooling data across multiple research centers to achieve sufficient statistical power [94]. The National Microbiome Data Collaborative (NMDC) has demonstrated the value of standardized bioinformatics workflows through its EDGE resource, which provides accessible, production-quality workflows for processing multi-omics microbiome data [95]. This approach ensures that data generated from different studies adhere to common processing standards, thereby facilitating comparative analyses and data reuse.
The experience from the Study for Future Families (SFF) multicenter research on semen quality highlights both the challenges and necessities of standardization. Their implementation of rigorously standardized laboratory protocols and centralized training sessions for technicians from all participating sites resulted in significantly improved comparability of semen quality data across multiple research locations [94]. This approach is directly applicable to reproductive biology studies involving multiple clinical centers collecting various types of omics data.
Framework for Standardized Multi-Omics Data Generation
Experimental Design Considerations:
- Sample Collection Protocols: Standardize collection methods, timing (circadian rhythms, menstrual cycle stages), storage conditions, and transportation logistics across all participating sites
- Batch Effects Management: Implement randomized processing schedules and include reference standards in each batch to account for technical variability
- Metadata Documentation: Adopt common metadata reporting standards capturing essential experimental parameters and clinical variables specific to reproductive biology
Computational Standardization: Layered software architecture, as implemented in the NMDC EDGE resource, ensures both flexibility and standardization in omics data processing [95]. This architecture typically consists of:
- Web Application Layer: Provides user-friendly interface for researchers to configure and execute analyses
- Orchestration Layer: Manages workflow execution and data dependencies
- Execution Layer: Leverages software containers to ensure consistent computational environments across different computing platforms
Table 1: Quality Control Metrics for Semen Evaluation in Multicenter Research
| QC Parameter | Inter-technician CV (%) | Intra-technician CV (%) | Difference from Central Standard (%) |
|---|---|---|---|
| MicroCell Count | 12.6 | 10.3 | 13.5 |
| Hemacytometer Count | 15.2 | 12.5 | 16.6 |
| Percent Motility | 10.5 | 5.2 | 11.9 |
Data from a multicenter study demonstrating the effectiveness of standardized training and protocols for semen analysis [94].
Quality Control Implementation
Analytical QC in Omics Assays
Quality control in omics research extends beyond wet-laboratory procedures to encompass computational quality assessment. The quantitative metrics established in seminal QC studies, such as those for semen evaluation, provide benchmarks for acceptable technical variability in reproductive biology assays [94]. For genomic and transcriptomic applications in reproductive medicine, QC measures should include:
- Sample Quality Metrics: DNA/RNA integrity numbers (RIN), fragment size distribution, adapter contamination levels
- Library Preparation QC: Amplification efficiency, molar concentration verification, complexity assessment
- Sequencing QC: Base quality scores, GC content distribution, duplication rates, coverage uniformity
The establishment of target CV values for different analytical techniques, as demonstrated in Table 1, provides concrete benchmarks for quality assessment in reproductive omics studies. The finding that hemacytometer standardization proved more difficult than MicroCell counts highlights how different methodologies may require customized QC approaches [94].
Quality Control in Computational Workflows
Computational QC represents an equally critical component in omics research. The NMDC EDGE resource addresses this through containerized execution environments that ensure consistent software versions and dependencies across analyses [95]. Key elements include:
- Reference Materials: Implementation of standardized control materials for benchmarking platform performance
- Automated QC Pipelines: Integration of tools like FastQC for sequencing data, MultiQC for aggregating results, and custom reproductive biology-specific QC checks
- Threshold Establishment: Defining empirically-derived thresholds for quality metrics based on reproductive tissue-specific characteristics
Diagram 1: Comprehensive QC Framework for Reproductive Omics. This workflow integrates quality checkpoints (red) at each analytical stage to ensure data reliability.
Computational Reproducibility
Enabling Reproducible Analysis
Reproducibility represents a significant challenge in omics research, particularly in reproductive biology where complex analytical pipelines are applied to heterogeneous datasets. The International Microbiome and Multi'Omics Standards Alliance (IMMSA) and the Genomic Standards Consortium (GSC) have identified key technical and social challenges impeding effective data reuse and reproducibility [96]. Addressing these challenges requires a multifaceted approach:
Computational Infrastructure:
- Containerization: Using Docker or Singularity containers to encapsulate complete analytical environments
- Workflow Management: Implementing workflow systems like Nextflow or Snakemake to ensure consistent execution order and parameters
- Version Control: Maintaining detailed records of software versions, parameters, and code changes through systems like Git
Methodological Documentation:
- Protocol Sharing: Detailed documentation of both wet-lab and computational procedures using platforms like protocols.io
- Data Provenance: Comprehensive tracking of data transformations from raw files to final results
- Parameter Reporting: Complete specification of all analytical parameters, including version numbers and random seeds for stochastic processes
Standards for Data and Metadata
Effective data reuse in reproductive biology requires standardized metadata frameworks that capture essential experimental conditions and clinical context. The "Year of Data Reuse" seminar series highlighted common metadata reporting as a critical prerequisite for reproducible research [96]. Key considerations include:
Table 2: Essential Metadata for Reproductive Omics Studies
| Category | Essential Elements | Reproductive Biology Specifics |
|---|---|---|
| Sample Characteristics | Tissue type, preservation method, storage conditions | Menstrual cycle stage, fertility status, pregnancy trimester |
| Donor Information | Age, sex, health status | Infertility diagnosis, ovarian reserve, previous ART outcomes |
| Experimental Conditions | Protocol version, processing dates, reagent lots | Hormonal stimulation regimen, embryo culture conditions |
| Data Generation | Platform, sequencing depth, quality metrics | Specific assays for embryonic development competence |
Multi-Omics Integration and Network Biology
Network-Based Integration Approaches
Network biology provides powerful frameworks for integrating diverse omics data types in reproductive research. Biological networks—including protein-protein interaction networks, gene regulatory networks, and metabolic pathways—represent the foundational architecture of biological systems and offer natural structures for data integration [97]. Network-based multi-omics integration methods can be categorized into four primary types:
- Network Propagation/Diffusion: Methods that simulate flow of information through biological networks to identify regions enriched for signals from multiple omics layers
- Similarity-Based Approaches: Techniques that construct integrated similarity networks combining multiple data types for clustering or classification
- Graph Neural Networks: Deep learning methods that operate directly on network structures to predict novel associations or classify nodes
- Network Inference Models: Approaches that reconstruct directed networks from omics data to elucidate regulatory relationships
These methods have shown particular promise in reproductive medicine for applications such as identifying novel drug targets for reproductive disorders, predicting patient-specific responses to fertility treatments, and repurposing existing drugs for reproductive applications [97].
Implementing Network Analysis in Reproductive Biology
The application of network-based integration methods to reproductive biology requires careful consideration of tissue-specific and process-specific network structures. For example, analyses of oocyte maturation should incorporate known temporal expression patterns and protein interaction networks specific to follicular development.
Diagram 2: Network-Based Multi-Omics Integration Framework. This approach integrates diverse data types using biological network structures to derive reproductive medicine insights.
Essential Research Reagent Solutions
The implementation of rigorous omics protocols in reproductive biology requires specific research reagents and materials designed to maintain standardization and quality. The following table details essential solutions for reproductive omics research:
Table 3: Essential Research Reagent Solutions for Reproductive Omics
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Standard Reference Materials | Benchmarking platform performance and technical variability | Commercial reference RNAs/DNAs; reproductive tissue-specific quality metrics |
| Solid Phase Extraction Kits | Nucleic acid purification from limited clinical samples | Optimized for low-input samples (oocytes, embryos, biopsies) |
| Single-Cell RNA-seq Kits | Transcriptomic profiling of individual reproductive cells | Critical for analyzing oocytes, sperm, and embryonic cells |
| Multiplex Immunoassay Panels | Simultaneous measurement of multiple proteins/cytokines | Customized for reproductive hormones and implantation markers |
| Library Preparation Kits | Preparation of sequencing libraries from various molecular types | Version-controlled to maintain protocol consistency |
| Quality Control Assays | Assessment of sample quality and quantity | RNA/DNA integrity tests specific to reproductive tissues |
| Software Containers | Computational environment standardization | Docker/Singularity images with version-pinned bioinformatics tools |
The integration of omics technologies into reproductive biology research offers unprecedented opportunities to understand complex processes in human reproduction, from gametogenesis to embryonic development and reproductive pathologies. However, realizing the full potential of these approaches requires unwavering commitment to analytical rigor through standardization, quality control, and computational reproducibility. The frameworks presented in this guide provide concrete strategies for implementing these principles across the research lifecycle—from experimental design through data generation, analysis, and interpretation. As the field advances toward increasingly clinical applications in diagnostic biomarker identification and therapeutic development [87], these rigorous approaches will ensure that research findings are robust, reproducible, and ultimately translatable to improved patient outcomes in reproductive medicine.
Ethical and Practical Considerations in Polygenic Risk Score (PGT-P) Application
The integration of polygenic risk scores (PRS) into preimplantation genetic testing (PGT-P) represents a frontier in reproductive genomics, enabling embryo risk profiling for complex polygenic diseases such as diabetes, coronary artery disease, and schizophrenia. This whitepaper provides an in-depth technical analysis of PGT-P methodologies, clinical validations, and the profound ethical considerations shaping its application. Framed within the broader thesis of omics technologies in reproductive biology, we examine how genome-wide association studies (GWAS), biobank-scale data, and polygenic scoring algorithms are transforming embryo selection. Despite demonstrated relative risk reductions for certain conditions, significant technical limitations concerning predictive accuracy, ancestry bias, and the probabilistic nature of risk estimates persist. Furthermore, the ethical landscape is marked by concerns over a "slippery slope" toward non-medical trait selection, societal inequities, and the challenges of informed decision-making. This analysis synthesizes current evidence and stakeholder perspectives to guide researchers, clinicians, and policymakers in the responsible development and potential integration of PGT-P within modern reproductive medicine.
The advent of high-throughput omics technologies has fundamentally reshaped reproductive biology, enabling a transition from the analysis of single-gene defects to complex polygenic architectures. Preimplantation genetic testing for polygenic risk (PGT-P) epitomizes this shift, leveraging whole-genome sequencing and computational biology to profile embryos for multiple common diseases simultaneously [98]. Unlike its predecessors—PGT for monogenic disorders (PGT-M), structural rearrangements (PGT-SR), or aneuploidy (PGT-A)—which target specific, highly penetrant genetic abnormalities, PGT-P interrogates thousands of single-nucleotide polymorphisms (SNPs) to calculate a cumulative risk estimate [98] [99].
The fundamental premise of PGT-P rests on the polygenic nature of most common human diseases. Conditions such as type 1 and type 2 diabetes, cardiovascular diseases, many cancers, schizophrenia, and autoimmune disorders are influenced by numerous genetic variants, each contributing minimally to overall heritability [98] [100]. Through genome-wide association studies (GWAS) conducted in large biobanks (e.g., UK Biobank, All of Us), researchers have identified thousands of robust variant-trait associations, enabling the development of polygenic risk scores (PRS) that stratify individual genetic susceptibility [98] [101]. The logical extension of this approach into reproductive medicine was perhaps inevitable; by applying PRS to embryos created via in vitro fertilization (IVF), clinicians and prospective parents can theoretically select embryos with lower genetic risk profiles for specified conditions [98].
The technical workflow of PGT-P is embedded within standard IVF and PGT protocols. Embryos created through IVF are cultured to the blastocyst stage (typically 5-7 days post-fertilization), at which point a few cells are biopsied from the trophectoderm. The extracted DNA undergoes universal genotyping via microarray or shallow whole-genome sequencing, generating comprehensive genomic data for each embryo [98]. This data serves as input for proprietary algorithms that compute polygenic risk scores for diseases of interest, ultimately producing a risk-ranked list of embryos to inform transfer decisions [98] [101]. This process, while technically sophisticated, introduces profound questions about predictive validity, utility, and ethics that this whitepaper will explore in detail.
Technical Foundations and Methodologies
Core Principles of Polygenic Risk Scoring
A polygenic risk score (PRS) is a quantitative metric that aggregates the effects of numerous genetic variants—often thousands—across an individual's genome to estimate their genetic predisposition for a particular trait or disease [98]. Mathematically, it is typically calculated as a weighted sum of risk alleles:
PRS = Σ (βi * Gi)
Where βi represents the estimated effect size (log odds ratio) of the i-th variant derived from GWAS summary statistics, and Gi denotes the genotype dosage (0, 1, or 2 copies of the effect allele) for that variant [98]. The resulting score places an individual on a continuous risk distribution relative to a reference population.
When applied to embryos (PGT-P), the methodology involves several additional layers of complexity. First, due to the limited DNA available from embryo biopsies, specialized whole-genome amplification techniques are employed [98]. Second, because embryos have not yet undergone recombination events to the same extent as adults, parental genotypes are typically used for phasing—determining which variants are co-inherited on the same chromosome—to improve the accuracy of haplotype reconstruction and subsequent score calculation [98]. Companies offering PGT-P have developed proprietary algorithms that incorporate these familial genetic data to compute embryo PRS with claimed accuracy exceeding 99% for genotype calling [100].
Experimental Workflow and Protocol
The complete PGT-P workflow integrates established IVF laboratory procedures with advanced genomic analysis, as visualized below.
Detailed Methodological Steps:
IVF and Embryo Culture: Oocytes are fertilized via standard IVF or ICSI. Resulting embryos are cultured for 5-7 days until they reach the blastocyst stage, comprising approximately 200-300 cells [98].
Trophectoderm Biopsy: Using a combination of laser technology and microscopic pipettes, a small opening is created in the blastocyst's outer layer (zona pellucida). Approximately 5-10 cells are removed from the trophectoderm, which is destined to become the placenta, minimizing potential impact on the inner cell mass (future fetus) [98].
Whole-Genome Amplification and Sequencing: The limited DNA from biopsied cells undergoes whole-genome amplification to generate sufficient material for analysis. Subsequent steps involve either genome-wide genotyping microarray or shallow whole-genome sequencing to determine the embryo's genotype at hundreds of thousands to millions of SNP markers [98].
PRS Calculation and Embryo Ranking:
- Data Integration: Embryo genotypes are combined with parental genomic data for accurate phasing. This determines which specific genetic variants are inherited together on each chromosome [98].
- Algorithmic Scoring: Proprietary algorithms, developed using large-scale GWAS reference data (e.g., from UK Biobank), calculate polygenic risk scores for each pre-selected disease. The algorithms apply weighting based on effect sizes from GWAS summary statistics [98] [101].
- Comparative Ranking: Each embryo receives a percentile rank for each condition relative to a general population. Embryos are then ranked based on their composite risk profiles to guide selection [98].
Embryo Transfer Decision: The lowest-ranking embryo(s) for the targeted polygenic conditions are prioritized for uterine transfer, following standard clinical protocols for frozen embryo transfer cycles [98].
Quantitative Assessment of Clinical Utility and Limitations
Predicted Risk Reduction and Clinical Outcomes
The theoretical benefit of PGT-P is a reduction in the lifetime risk of developing targeted polygenic diseases in children born after screening. Quantitative assessments, primarily derived from statistical modeling, simulations, and analyses of sibling pairs, suggest this potential is variable and context-dependent [98].
Table 1: Reported Quantitative Outcomes of PGT-P in Disease Risk Reduction
| Disease/Condition | Reported Relative Risk Reduction | Study Type / Notes | Citation |
|---|---|---|---|
| Type 1 Diabetes | Up to 72% | Sibling pair analysis and modeling | [100] |
| Type 2 Diabetes | Modest reductions | Modeling; lower heritability and stronger environmental influence limit gains | [100] |
| Coronary Artery Disease | 17-20% (composite score) | Modeling of theoretical "composite health score" combining multiple diseases | [98] |
| Breast Cancer | 12-26% (composite score) | Same modeling effort for composite score | [98] |
| Schizophrenia | 13-25% (composite score) | Same modeling effort for composite score | [98] |
It is critical to distinguish between relative and absolute risk reduction. The substantial relative risk reductions reported often translate to much smaller absolute reductions. For example, if the baseline lifetime risk of a disease is 5%, a 50% relative risk reduction only lowers the absolute risk to 2.5% [98] [102]. Furthermore, these models often represent best-case scenarios; the realized benefit in clinical practice is likely smaller due to a limited number of embryos available for selection and the imperfect accuracy of PRS [98].
Technical Limitations and Ancestry Bias
The clinical application of PGT-P is constrained by several significant technical and methodological limitations.
Table 2: Key Technical Limitations and Practical Challenges of PGT-P
| Category | Specific Limitation | Impact on PGT-P Utility | |
|---|---|---|---|
| Predictive Power | Probabilistic, not deterministic predictions | Cannot guarantee disease onset or prevention; environmental factors play a major role. | [98] [102] |
| Embryo Availability | Limited number of embryos (typically 1-5) | Constrains selection potential; sibling embryos share ~50% of DNA, limiting variability. | [98] [99] |
| Ancestry Bias | GWAS data predominantly from European-ancestry populations | PRS are significantly less accurate for individuals of non-European ancestries, exacerbating health disparities. | [98] [100] [101] |
| Trait Interdependence | Genetic correlations between traits | Selecting for a lower risk in one disease may inadvertently increase risk for another (e.g., BMI correlations with various diseases). | [98] |
| Commercial Context | Lack of peer-reviewed clinical validation | Most data on efficacy comes from company white papers or simulations, not independent clinical trials. | [98] [103] [101] |
The issue of ancestry bias warrants particular emphasis. The GWAS used to derive effect sizes for PRS are based overwhelmingly on individuals of European descent [98] [101]. This lack of diversity means that PRS have substantially diminished predictive power when applied to individuals of African, Asian, Hispanic, and other ancestral backgrounds. The clinical use of PGT-P in these populations could therefore be ineffective or misleading, potentially worsening existing health disparities [98] [100].
Ethical and Societal Considerations
The implementation of PGT-P raises profound ethical questions that extend beyond technical limitations, engaging with fundamental values in reproduction and society.
Primary Ethical Concerns
Stakeholder interviews and ethical analyses consistently identify several core areas of concern:
The "Slippery Slope" and Designer Babies: The most prevalent concern among healthcare professionals and in media coverage is that PGT-P could facilitate a slide from medical applications toward selection for non-medical traits such as intelligence, height, or aesthetic features [104] [99] [105]. This is often explicitly linked to fears of a new, consumer-based "eugenics," despite companies' assurances that they will not test for such traits [99] [105] [101].
Autonomy, Anxiety, and Parental Pressure: PGT-P could create new anxieties for prospective parents and impose a sense of responsibility to use the technology to have the "healthiest" child possible—a "technological imperative" [104] [102]. Patients who have undergone PGT-M report that the IVF and PGT process is psychologically and physically demanding, and may not be worthwhile for probabilistic risk information alone [102]. Furthermore, knowing a child's polygenic risks could lead to overprotection, a false sense of security, or altered parent-child dynamics [104] [102].
Justice and Equity: The high cost of IVF and PGT-P creates access inequities, potentially allowing wealthier individuals to reduce polygenic disease risk in their offspring, which could alter the disease burden distribution across socioeconomic groups over generations [98] [101]. Coupled with the ancestry bias in PRS, this threatens to exacerbate existing health disparities.
Discrimination and Stigmatization: There are concerns about how embryo risk information could be used by third parties, such as insurers, or how it might lead to stigmatization of individuals who develop a disease despite being selected for a low-risk profile [104] [99].
Stakeholder Perspectives
Different stakeholder groups exhibit markedly different attitudes toward PGT-P:
Healthcare Professionals: Are largely cautious and skeptical. A qualitative interview study with 31 professionals in reproductive medicine and genetics found that most believe clinical implementation is "premature" [103]. They express concerns about validity, utility, the potential for complicated decision-making, and difficulties in achieving truly informed consent given the complexity of the information [104] [103].
Patients: Perspectives are nuanced. Patients with experience in PGT-M/SR have expressed that PGT-P would only be worthwhile for serious conditions with a strong family history and substantial potential risk reduction, rather than as a general screening tool [102]. Studies indicate that in the United States, IVF patients and the public may have more positive attitudes than healthcare professionals, highlighting a need for improved patient education [98].
Media Portrayal: An analysis of 59 original news articles found that 36.8% were negative toward PGT-P, while only 8.8% were positive; the majority (54.4%) were neutral, often emphasizing the technology's limited practical value [99] [105].
The Scientist's Toolkit: Research Reagents and Materials
The development and application of PGT-P rely on a suite of sophisticated research reagents and platforms.
Table 3: Essential Research Reagents and Platforms for PGT-P Development
| Reagent / Technology | Function in PGT-P Workflow | Specific Examples / Notes | |
|---|---|---|---|
| Whole-Genome Amplification Kits | Amplifies nanogram quantities of DNA from embryo biopsies to microgram amounts suitable for genotyping/sequencing. | Multiple displacement amplification (MDA) kits to minimize amplification bias. | [98] |
| Genotyping Microarrays | Genotypes hundreds of thousands to millions of SNPs across the embryo's genome in a cost-effective manner. | Illumina Infinium arrays; customized arrays targeting PRS-relevant SNPs. | [98] |
| Next-Generation Sequencers | Provides an alternative to microarrays via shallow whole-genome sequencing for genome-wide SNP detection. | Illumina NovaSeq, HiSeq platforms; low-pass sequencing (~0.5x coverage) is often sufficient. | [98] |
| GWAS Summary Statistics | The reference data providing effect sizes (β) for each SNP used in the PRS calculation. | Publicly available data from UK Biobank, Finngen, etc.; consortium data (e.g., SSGAC). | [98] [101] |
| Phasing & Imputation Algorithms | Determines haplotype phases (co-inherited alleles on a chromosome) using parental data and infers missing genotypes. | Software like SHAPEIT, Eagle; imputation servers (e.g., Michigan Imputation Server). | [98] |
| Proprietary PRS Algorithms | Computes the final polygenic risk score for each embryo by integrating genotypes, effect sizes, and other weights. | Commercial algorithms (e.g., from Genomic Prediction, Orchid); often include additional proprietary adjustments. | [98] [101] |
PGT-P stands as a seminal example of the promises and perils of integrating omics technologies into reproductive medicine. While its theoretical potential to reduce the burden of common polygenic diseases is significant, its current technical limitations—including predictive uncertainty, ancestry bias, and constrained selection utility—are substantial. The ethical landscape is equally complex, fraught with concerns about a slippery slope toward enhancement, impacts on parental autonomy, and the potential to worsen social inequities.
The consensus among many professional societies and healthcare professionals is that PGT-P is not yet ready for routine clinical application and should ideally be offered only within a research context where its benefits and harms can be rigorously monitored [98] [103]. Future development must prioritize: 1) the diversification of GWAS datasets to improve equity; 2) long-term clinical studies to validate predicted risk reductions; and 3) the establishment of clear regulatory frameworks and guidelines that distinguish between medical applications and non-medical trait selection. For researchers and scientists driving the omics revolution, these challenges are not merely technical but deeply ethical, demanding a commitment to responsible innovation that prioritizes patient welfare and social justice.
The integration of omics technologies—genomics, transcriptomics, proteomics, and metabolomics—is revolutionizing reproductive biology research by enabling comprehensive molecular profiling of reproductive processes and pathologies. These technologies facilitate the discovery of biomarker panels with potential to diagnose conditions such as preterm birth, polycystic ovarian syndrome, endometriosis, and male infertility with unprecedented precision [57]. However, a significant translational challenge emerges: biomarker panels discovered through high-throughput omics platforms often perform optimally only within the experimental context of their discovery, failing to maintain predictive power when adapted to clinically feasible diagnostic platforms [106] [107]. This whitepaper outlines a systematic framework for optimizing multi-feature biomarker panels, balancing the imperative for high predictive accuracy with the practical requirements of clinical implementation, with specific application to reproductive biology.
Theoretical Foundation: The Biological Function-Based Optimization Principle
The core premise of effective biomarker optimization is that a diagnostic panel fundamentally measures the combined effect of dysregulated biological processes underlying a disease state [106]. Genes or proteins involved in the same biological processes and coordinately affected by a disease often share similar discriminatory power for classifying that disease [106] [107]. This principle provides the biological justification for substituting individual biomarkers within a panel without significantly compromising its overall predictive performance.
In reproductive biology, this approach is particularly powerful. For instance, a biomarker panel for endometriosis might reflect dysregulation in biological processes such as inflammation, cell adhesion, and angiogenesis. If one biomarker measuring inflammatory response proves problematic in a clinical assay, this principle allows for its substitution with another biomarker from the same inflammatory pathway that exhibits similar directional change in the disease state [106].
A Systematic Biomarker Panel Optimization Workflow
The optimization process involves a structured, iterative workflow designed to maintain diagnostic performance while enhancing clinical applicability. The key stages are detailed below.
Stage 1: Mapping Biomarkers to Biological Processes
The initial step involves annotating each biomarker in the discovery panel with its associated Gene Ontology Biological Processes (GOBP), KEGG pathways, or other relevant functional annotations. This mapping identifies the core biological processes represented by the panel. For example, analysis of an 11-gene sepsis diagnostic panel revealed its association with six key biological processes: (1) chemotaxis, adhesion, migration; (2) antigen processing and immune response; (3) transcription by RNA polymerase II; (4) platelet activation; (5) apoptosis; and (6) metabolism [106] [107]. This same methodology can be applied to a panel for recurrent pregnancy loss, identifying processes like immune tolerance, placental invasion, and coagulation.
Stage 2: Identifying Substitution Candidates
For each biomarker targeted for replacement or removal, identify alternative candidate biomarkers that participate in the same core biological process. Crucially, candidates must demonstrate directional change consistency with the original biomarker (e.g., increased or decreased expression in the disease state compared to controls) [106]. This ensures the substitute biomarker captures the same disease-related biological phenomenon.
Table 1: Criteria for Identifying Valid Substitution Candidates
| Criterion | Description | Rationale |
|---|---|---|
| Pathway Co-membership | Candidate belongs to the same biological pathway/process as the original biomarker. | Ensures biological equivalence in representing the dysregulated process. |
| Directional Change | Candidate shows the same direction of expression change (up/down) in disease. | Maintains the integrity of the biological signal being measured. |
| Performance Correlation | Candidate has similar discriminatory power (e.g., AUC) in initial analyses. | Preserves the panel's overall classification performance. |
Stage 3: Performance Validation
The impact of gene substitution and panel reduction must be rigorously validated. This involves evaluating the classification performance (e.g., Area Under the Curve (AUC)) of the optimized panel against the original panel using both the initial discovery datasets and, critically, independent validation cohorts [106] [108]. Research on the sepsis panel demonstrated that substituting more than half of the genes based on biological function did not negatively affect diagnostic performance across multiple validation sets [106]. This validation is essential for confirming that the optimized panel retains generalizability.
Critical Considerations for Clinical Translation in Reproductive Health
Translating a biomarker panel from a research discovery to a clinically viable diagnostic test for reproductive disorders involves navigating several critical hurdles.
Platform Transition and Analytical Validation
Biomarker panels identified via high-throughput sequencing or microarrays must often be adapted to platforms suitable for clinical settings, such as quantitative PCR (qPCR) or multiplex immunoassays [106] [109]. A major challenge is the inconsistency of measurement results between different platforms [106]. Analytical validation is therefore essential, characterizing the assay's performance parameters including precision, accuracy, sensitivity, specificity, and reproducibility according to guidelines like those from the Clinical Laboratory and Standards Institute (CLSI) [110] [109]. For a reproductive hormone panel, this would involve ensuring reliable performance in serum or plasma samples.
Panel Size and Cost Optimization
Large biomarker panels (e.g., 30-40 features) are often prohibitive for routine clinical use due to cost and complexity [106] [109]. A key goal of optimization is feature reduction to identify a minimal set of biomarkers that robustly represent the core dysregulated biology. The biological function-based approach allows for the removal of redundant biomarkers measuring the same process, thereby reducing cost and streamlining the assay without sacrificing predictive power [106] [111]. This is crucial for developing affordable prenatal or fertility tests.
Experimental Protocols for Optimization and Validation
Protocol 1: Identifying Substitutable Biomarkers via Functional Annotation
Purpose: To systematically map a discovered biomarker panel to core biological processes and identify substitution candidates.
- Input: A list of candidate biomarkers (e.g., genes, proteins) from the discovery phase.
- Functional Annotation: Use bioinformatics resources (e.g., DAVID, Enrichr, GO databases) to annotate each biomarker with its associated biological processes or pathways.
- Process Clustering: Group biomarkers into non-redundant, key biological processes based on their functional annotations.
- Identify Gaps: For each key process, determine if multiple biomarkers are present in the original panel. Processes represented by only one biomarker may be critical to retain.
- Candidate Pool Generation: For processes with multiple biomarkers, identify all other genes/proteins in the discovery dataset that are annotated to the same process and show consistent directional change in the disease state. This list forms the substitution candidate pool [106].
Protocol 2: Validating Panel Performance via Resampling
Purpose: To rigorously assess the classification performance of the original and optimized panels and ensure generalizability.
- Dataset Splitting: Divide the dataset into training and hold-out test sets, or use k-fold cross-validation [111] [108].
- Classifier Training: Train a classifier (e.g., Random Forest, Support Vector Machine, Logistic Regression) using the original panel on the training data.
- Baseline Performance: Calculate performance metrics (AUC, sensitivity, specificity) on the test/hold-out set.
- Optimized Panel Testing: Repeat steps 2-3 using the new, optimized panel.
- Statistical Comparison: Compare the performance metrics of the original and optimized panels. Non-inferiority testing is often appropriate to demonstrate that the optimized panel does not perform significantly worse [106] [108].
- External Validation: Finally, validate the final optimized panel on one or more completely independent validation cohorts not used in any part of the discovery or optimization process [106] [108].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Key Research Reagents and Platforms for Biomarker Optimization
| Reagent/Platform | Function in Optimization Workflow |
|---|---|
| GO (Gene Ontology) Databases | Provides standardized functional annotation for genes/proteins, enabling mapping to biological processes. |
| KEGG/Reactome Pathway Databases | Allows for enrichment analysis to identify overrepresented pathways in a biomarker panel. |
| qPCR Assays | Used to technically validate and implement RNA-based biomarker panels in a clinically adaptable format. |
| Multiplex Immunoassays | Enables simultaneous measurement of multiple protein biomarkers in scarce clinical samples (e.g., endometrial biopsies). |
| Next-Generation Sequencing | Discovery platform for identifying candidate biomarker panels from tissues or liquid biopsies. |
| Statistical Software (R/Python) | Essential for data pre-processing, normalization, hypothesis testing, and building classification models. |
Case Study: Application in Reproductive Health
Consider a hypothetical 10-gene mRNA panel discovered via RNA-Seq for diagnosing preterm birth risk from a maternal blood sample. Transitioning this panel to a clinical qPCR test encounters issues: two genes show poor assay performance, and a 10-plex assay is too costly for widespread screening.
- Mapping: Functional annotation reveals the panel represents processes like inflammatory response, steroid hormone response, and extracellular matrix organization.
- Substitution: The two poor-performing genes are both involved in the inflammatory response. From the original RNA-Seq data, other significantly upregulated inflammatory genes with high discriminatory power (AUC) are identified as candidates.
- Reduction: Two other genes in the panel are found to redundantly represent the steroid hormone response process. One is removed, reducing the panel size.
- Validation: The new 7-gene panel is evaluated. Its performance in classifying preterm birth risk in the original cohort and an independent validation cohort is statistically non-inferior to the original 10-gene panel [106]. The result is a more robust, cost-effective, and clinically feasible diagnostic test.
The journey from biomarker discovery to clinical utility in reproductive medicine is fraught with technical and practical obstacles. The biological function-based optimization process provides a rigorous, systematic, and biologically grounded methodology for overcoming these hurdles. By focusing on the dysregulated biological processes that a biomarker panel is designed to measure, researchers can confidently substitute problematic biomarkers and reduce panel size to enhance clinical feasibility, all while preserving the critical predictive power needed for diagnosing and managing complex reproductive conditions. This approach is indispensable for bridging the gap between high-throughput omics discovery and the development of practical diagnostic tools that can improve patient outcomes in reproductive health.
Evidence and Efficacy: Validating Omics Tools and Comparative Clinical Outcomes
The integration of artificial intelligence (AI) into in vitro fertilization (IVF) represents a paradigm shift in reproductive medicine, moving embryology from subjective morphological assessments toward data-driven, predictive science. This whitepaper synthesizes current evidence from comparative studies evaluating the performance of AI algorithms against trained embryologists in embryo selection, with a specific focus on accuracy metrics and live birth rate (LBR) prediction. Findings indicate that AI systems consistently outperform embryologists in embryo grading and viability prediction, with median accuracy improvements of approximately 10-30% across multiple studies. The evolution of this field is intrinsically linked to the broader adoption of omics technologies—including genomics, transcriptomics, and proteomics—which provide the multi-dimensional data necessary for robust AI model training. This technical analysis is intended to guide researchers, scientists, and drug development professionals in understanding the current landscape, methodological requirements, and future trajectory of AI-enabled embryo selection within the context of modern reproductive biology.
In vitro fertilization success rates have historically plateaued, with a significant proportion of transferred embryos failing to implant successfully. A primary challenge lies in the subjective nature of embryo selection, where embryologists visually assess embryos based on morphological criteria [112]. This process is prone to inter-observer variability and human error, contributing to the relatively low success rates of assisted reproductive technologies (ART), which typically do not exceed 30% across all age groups and can fall below 4% for women over 42 [112].
The emerging application of artificial intelligence in embryo selection aims to address these limitations by introducing objectivity, standardization, and predictive analytics based on vast datasets. AI adoption in reproductive medicine is growing rapidly, with usage among fertility specialists increasing from 24.8% in 2022 to 53.22% in 2025 (including both regular and occasional use) [113]. This growth parallels advancements in omics technologies that provide the foundational data for sophisticated AI algorithms, creating new opportunities for precision in reproductive biology.
Comparative Performance Data: AI vs. Embryologists
Quantitative Accuracy Metrics
A systematic review of 20 studies conducted between 2005 and 2022 provides comprehensive performance data comparing AI to embryologists across two critical parameters: embryo morphology grade prediction and clinical pregnancy prediction [112]. The results demonstrate AI's consistent superiority across both domains.
Table 1: Performance Comparison in Embryo Morphology Grade Prediction
| Method | Median Accuracy | Accuracy Range | Sample Characteristics |
|---|---|---|---|
| AI Models | 75.5% | 59% - 94% | Various models trained on embryo images/time-lapse data |
| Embryologists | 65.4% | 47% - 75% | Using local respective assessment guidelines |
Table 2: Performance Comparison in Clinical Pregnancy Prediction
| Method | Input Data Type | Median Accuracy | Accuracy Range |
|---|---|---|---|
| AI Models | Clinical information only | 77.8% | 68% - 90% |
| AI Models | Images/time-lapse + Clinical data | 81.5% | 67% - 98% |
| Embryologists | Images/time-lapse + Clinical data | 51% | 43% - 59% |
The performance advantage of AI is most pronounced when integrating multiple data types, with AI models achieving a 30.5% higher median accuracy compared to embryologists when utilizing both image/time-lapse and clinical information [112]. This demonstrates the synergistic potential of multimodal data integration, a core principle of omics-informed approaches.
Emerging Commercial Applications
Beyond research settings, commercial AI applications are demonstrating promising results. Gaia, a UK startup offering AI-powered IVF success prediction, reports 90% accuracy in predicting treatment outcomes [114]. Their model analyzes personal biometrics alongside datasets from millions of historical IVF cycles to forecast the optimal treatment pathway and number of cycles likely needed for success, enabling novel financial models where patients only pay if treatment is successful [114].
Methodological Frameworks for AI in Embryo Selection
Experimental Protocols and Workflows
The development and validation of AI models for embryo selection follow structured experimental protocols that integrate traditional embryology laboratory practices with computational analytics.
Data Acquisition and Preprocessing Protocols
Image Data Collection:
- Time-lapse Imaging Systems: Embryos are cultured in integrated time-lapse systems capturing images at 5-20 minute intervals throughout development (days 1-6) [112].
- Standardization: Consistent lighting, magnification, and culture conditions maintained across all samples.
- Annotation Ground Truth: Labels established by consensus among multiple senior embryologists following standardized grading systems (e.g., Gardner blastocyst grading) [112].
Clinical and Omics Data Integration:
- Patient Clinical Data: Maternal age, ovarian reserve markers (AMH, AFC), infertility diagnosis, previous ART cycles, and stimulation protocol details [112].
- Genomic Data: Preimplantation genetic testing for aneuploidy (PGT-A) and polygenic risk scores (PGT-P) when available [115].
- Data Cleaning: Handling of missing values, normalization of continuous variables, and encoding of categorical variables [116].
AI Model Architectures and Training
Current approaches utilize diverse machine learning architectures:
Convolutional Neural Networks (CNNs):
- Primary application: Analysis of static embryo images and time-lapse videos
- Architecture variants: ResNet, Inception, custom CNN architectures
- Training: Transfer learning from natural image datasets with fine-tuning on embryo-specific data
Ensemble Methods:
- Implementation: Gradient boosting algorithms (LightGBM, CatBoost) for tabular clinical data
- Preprocessing: Native categorical feature handling without extensive preprocessing [116]
- Advantage: Resilience to overfitting through ordered boosting techniques [116]
Multimodal Integration Architectures:
- Approach: Separate feature extraction pathways for image and clinical data with late fusion
- Challenge: Heterogeneous data types and sampling rates
- Solution: Attention mechanisms to weight feature importance across modalities
Omics Integration in AI-Driven Embryo Selection
The convergence of AI with multi-omics technologies represents the cutting edge of embryo selection research, enabling a systems biology approach to embryonic viability assessment.
Genomic Data Integration
Preimplantation Genetic Testing:
- PGT-A: Detection of chromosomal aneuploidies; standard of care for many clinics
- PGT-P: Emerging technology using polygenic risk scores for complex disease risk and non-disease traits [115]
- Algorithm Integration: Genomic data combined with morphological assessment in AI models
Advanced Genomic Tools:
- BELA System: Fully automated AI tool predicting embryo ploidy using time-lapse imaging and maternal age, trained on nearly 2,000 embryos [113]
- Performance: Demonstrates higher accuracy than predecessor STORK-A, offering non-invasive alternative to PGT-A [113]
- Limitations: Not yet considered diagnostic; requires further validation
Multi-Omics Integration Frameworks
The combination of multiple omics layers provides a more comprehensive viability assessment than any single data type:
Transcriptomics:
- Methodology: Single-cell RNA sequencing of trophectoderm cells or spent culture medium analysis
- Application: Identification of gene expression signatures associated with implantation potential
Proteomics/Metabolomics:
- Approach: Mass spectrometry analysis of spent culture media
- Biomarkers: Identification of metabolic footprints correlated with embryo viability
- Integration: Combined with morphological parameters in ensemble AI models
Research Reagent Solutions and Experimental Tools
Table 3: Essential Research Tools for AI Embryo Selection Studies
| Category | Specific Tools/Reagents | Research Application | Technical Considerations |
|---|---|---|---|
| Embryo Culture & Imaging | Time-lapse incubation systems (EmbryoScope+) | Continuous embryo development monitoring | Standardized imaging protocols essential for model generalizability |
| Sequential culture media (G-T系列, Continuous Single Culture) | Supporting development to blastocyst stage | Batch-to-batch consistency critical for reproducible results | |
| Genomic Analysis | PGT-A kits (Illumina, Thermo Fisher) | Aneuploidy screening | Library preparation efficiency impacts diagnostic accuracy |
| Whole genome amplification kits | Amplification of limited embryonic DNA | Amplification bias must be minimized for reliable sequencing | |
| AI/Computational | Deep learning frameworks (TensorFlow, PyTorch) | Custom model development | GPU acceleration required for image analysis models |
| Bioinformatic pipelines (Plink, GATK) | Genomic data preprocessing | Quality control metrics must be standardized across cohorts | |
| Data Management | Cloud computing platforms (AWS, Google Cloud) | Scalable data storage and processing | HIPAA/GDPR compliance essential for patient data security [23] |
Discussion and Future Directions
Clinical Implementation Challenges
Despite promising performance metrics, several significant barriers impede widespread AI adoption in clinical embryology:
Technical and Infrastructural Barriers:
- Cost: Cited as the primary barrier by 38.01% of fertility specialists in 2025 surveys [113]
- Training: Lack of appropriate training resources reported by 33.92% of specialists [113]
- Data Quality: Dependence on high-quality, standardized input data for reliable predictions
Validation and Generalizability:
- Prospective Validation: Most AI models lack prospective validation in real-world clinical settings [112]
- Dataset Bias: Training datasets often lack diversity in patient demographics and clinical protocols [115]
- Outcome Measures: Need for shift from implantation rate prediction to ongoing pregnancy/live birth [112]
Ethical Considerations in AI-Driven Selection
The application of AI in embryo selection raises important ethical questions that intersect with evolving omics capabilities:
Polygenic Risk Score Applications:
- Current State: Emerging capabilities for selecting embryos based on polygenic risk scores for both medical and non-medical traits [115]
- Limitations: Significant scientific concerns about predictive validity, especially for behavioral traits like intelligence [115]
- Equity: Risk of exacerbating health disparities due to Eurocentric bias in genomic databases [117]
Regulatory Landscape:
- Professional Guidelines: Major genetics and reproductive medicine organizations express caution about clinical use of polygenic embryo screening [115]
- Validation Requirements: Need for rigorous clinical validation before widespread implementation
Future Research Trajectories
The next generation of AI-based embryo selection tools will likely focus on:
Enhanced Multi-Omics Integration:
- Development of unified models incorporating genomic, transcriptomic, proteomic, and metabolomic data
- Temporal multi-omics capturing dynamic molecular changes during development
Advanced AI Architectures:
- Transformer-based models for better interpretation of time-series embryo development data
- Federated learning approaches enabling multi-institutional collaboration while preserving data privacy
Clinical Workflow Integration:
- Real-time decision support systems embedded in laboratory workflows
- Automated quality control and anomaly detection in embryo development
The comparative evidence between AI and embryologist-driven embryo selection demonstrates a clear and consistent performance advantage for AI systems across multiple metrics, particularly when integrating multimodal data sources. This advantage must be contextualized within the current limitations of clinical validation and implementation challenges. The ongoing integration of omics technologies provides a pathway for more comprehensive embryo assessment beyond morphological evaluation alone, potentially addressing the persistent challenge of low IVF success rates.
For researchers and drug development professionals, the rapidly evolving landscape of AI in embryo selection represents both an opportunity and a responsibility. Opportunity exists in developing increasingly sophisticated, validated tools that can transform clinical practice. Responsibility lies in addressing ethical considerations, ensuring equitable access, and maintaining scientific rigor in the validation and implementation of these technologies. As omics technologies continue to mature and AI algorithms become more refined, the potential for truly personalized, predictive embryo selection represents the next frontier in reproductive medicine.
The integration of 'omics' technologies into reproductive biology is fundamentally reshaping the landscape of embryo assessment. For years, preimplantation genetic testing for aneuploidy (PGT-A) has relied on trophectoderm (TE) biopsy, an invasive procedure that involves extracting several cells from the blastocyst. While this method provides crucial genetic information, concerns regarding its potential impact on embryo development and its incomplete representation of the entire embryo have persisted [118]. The emergence of non-invasive PGT (niPGT) methodologies, which analyze cell-free DNA (cfDNA) secreted into the spent culture medium (SCM), represents a paradigm shift. This technical guide examines the validation of niPGT, focusing specifically on its concordance with the gold-standard TE biopsy, and situates this advancement within the broader context of multi-omics in reproductive medicine.
Concordance Metrics: niPGT vs. TE Biopsy
The clinical validation of niPGT hinges on rigorous comparisons with established methods. Key metrics include ploidy concordance (whether both methods agree on euploid/aneuploid status), diagnostic concordance (agreement on the specific chromosomal diagnosis), and sex concordance. A 2025 meta-analysis of 36 studies, providing the most comprehensive evidence to date, evaluated the diagnostic accuracy of different sampling techniques using the whole blastocyst or inner cell mass (ICM) as the gold standard [119]. Table 1 summarizes the aggregated findings.
Table 1: Diagnostic Performance of PGT-A Sampling Methods Against Whole Blastocyst/ICM Gold Standard (Meta-Analysis Data)
| Sample Type | Sensitivity | Specificity | Area Under the Curve (AUC) |
|---|---|---|---|
| Trophectoderm (TE) Biopsy | 0.839 | 0.791 | 0.878 |
| Spent Culture Medium (SCM) | 0.874 | 0.719 | 0.869 |
| Blastocoel Fluid (BF) | Information Missing | Information Missing | 0.656 |
The meta-analysis concludes that while TE biopsy is currently the most robust method, SCM-based niPGT demonstrates significant diagnostic potential, with high sensitivity and a strong AUC [119]. Individual studies provide further granularity. One investigation that directly compared TE biopsy, SCM, and the inner cell mass (ICM) reported a ploidy concordance rate of 58.33% between SCM and ICM, versus 68.75% between TE biopsy and ICM [120]. This suggests that while niPGT is promising, it does not yet surpass the accuracy of a well-executed TE biopsy in reflecting the embryonic ICM, which ultimately forms the fetus.
Another 2025 study of 146 blastocysts found an overall concordance rate of 82.9% between paired TE and SCM samples. Notably, in cases where TE biopsy indicated aneuploidy but niPGT suggested euploidy, follow-up with the ICM revealed that niPGT was correct in 70% of cases (a true negative rate of 70%), highlighting its potential as a confirmatory tool [80].
Key Experimental Protocols for niPGT Validation
The validation of niPGT relies on standardized, meticulous laboratory protocols. The following workflow details the primary methods used in key validation studies.
Sample Collection and Preparation
- Embryo Culture: Embryos are cultured individually in sequential media following intracytoplasmic sperm injection (ICSI). The use of ICSI is critical to avoid paternal DNA contamination from residual sperm [121] [80].
- SCM Collection: After blastocyst formation (Day 5 or 6) and prior to TE biopsy, approximately 20-25 µL of the spent culture medium is carefully aspirated, ensuring the blastocyst itself is not disturbed. The SCM is transferred to a nuclease-free PCR tube containing a cell lysis buffer and stored at -80°C [121] [80].
- TE Biopsy (Gold Standard): Blastocysts graded 3-6 on the Gardner scale are subjected to biopsy. Using a laser and mechanical dissection, 4-8 trophectoderm cells are removed from the area opposite the inner cell mass. The biopsied cells are placed in a lysis buffer and frozen [80] [122].
- ICM/Whole Embryo Collection (Validation Gold Standard): For research validation, donated embryos are dissected to isolate the ICM or the entire residual blastocyst after TE biopsy. This provides the definitive genetic profile against which TE and SCM results are compared [120] [121].
Genetic Analysis and Sequencing
- Whole Genome Amplification (WGA): Due to the extremely low DNA concentration in SCM, WGA is an essential step. The two predominant methods are:
- Multiple Annealing and Looping-Based Amplification Cycles (MALBAC): Used in the Non-Invasive Chromosome Screening (NICS) assay. This method provides better coverage uniformity, which is advantageous for detecting copy number variations [121].
- PicoPLEX WGA: Known as the "gold standard" for PGT-A due to its superior reproducibility, fidelity, and uniformity. It is a core component of commercial kits like the Embgenix PGT-A Kit [123].
- Library Preparation and Sequencing: WGA products are enzymatically fragmented, and Illumina-compatible adapters with unique dual indexes (UDIs) are ligated. This allows for multiplex sequencing of up to 96 samples simultaneously, streamlining the workflow and reducing hands-on time [123].
- Bioinformatic Analysis: Sequencing data is aligned to a reference genome (e.g., hg38). Cloud-based software (e.g., Embgenix Analysis Software, ChromGo) uses specialized algorithms to detect copy number variations (CNVs) across all 24 chromosomes, identifying whole-chromosome aneuploidies, segmental aneuploidies (typically ≥10 Mb), and mosaicism [123] [80].
Table 2: Key Research Reagent Solutions for niPGT
| Reagent/Kit | Primary Function | Key Characteristics |
|---|---|---|
| MALBAC WGA Kit | Whole-genome amplification of trace DNA from SCM. | Provides uniform amplification coverage; used for NICS. |
| PicoPLEX WGA Kit | Whole-genome amplification of DNA from SCM or TE cells. | High reproducibility and fidelity; considered a gold-standard method. |
| Embgenix PGT-A Kit | End-to-end solution for NGS-based PGT-A. | Integrates PicoPLEX WGA, library prep, and analysis software; detects mosaicism and segmental aneuploidies. |
| NICSInst / ChromInst | WGA and NGS library construction for SCM and biopsy samples. | Optimized for non-invasive testing; used with CNV-Seq platforms. |
| SurePlex DNA Amplification System | WGA for TE biopsy samples. | Used prior to array CGH (aCGH) analysis; a established method in many PGT labs. |
niPGT in the Multi-Omics Landscape of Reproductive Biology
The evolution of PGT is moving beyond a single-data-type approach toward a multi-omics framework that integrates layers of molecular information for a more comprehensive embryo assessment.
- Genomics and niPGT: niPGT-A is a genomic application that assesses chromosomal copy number. Its validation against TE biopsy establishes its role as a less invasive genomic tool. The ultimate genomic profile, however, is considered to be that of the ICM [119].
- Transcriptomics and Implantation Potential: Research is now exploring the transcriptome (the complete set of RNA transcripts) of blastocysts. A 2024 study performed parallel DNA-seq (for PGT-A) and RNA-seq on the same TE biopsy. Machine learning models trained on differentially expressed genes (DEGs) between euploid blastocysts that did or did not lead to clinical pregnancy were able to further stratify euploid embryos by implantation potential, achieving an area under the curve (AUC) of 0.88 with a random forest model [122] [124]. This "multi-omics PGT" approach demonstrates that genetic normality (euploidy) and functional metabolic activity (transcriptome) provide complementary insights.
- Integrating Omics Data: The future of embryo selection lies in synthesizing data from the genome (ploidy status from niPGT or TE biopsy), transcriptome (gene expression related to developmental competence), and other omics layers like the epigenome (e.g., DNA methylation). This integrated profile could unlock a deeper understanding of embryo-endometrial dialogue and significantly improve live birth rates per transfer [118] [122].
Diagram 1: Multi-omics integration for embryo potential assessment. Data from genomic, transcriptomic, and other molecular layers are synthesized via machine learning models to stratify euploid embryos by their likelihood of successful implantation, moving beyond ploidy assessment alone [122] [124].
Critical Analysis and Future Directions
Despite its promise, niPGT faces several challenges that must be addressed for widespread clinical adoption.
- Sources of Error and Discordance: Discordance between niPGT and TE biopsy can arise from biological and technical factors. Biologically, embryonic mosaicism—where the TE and ICM have different chromosomal constitutions—is a primary cause. Technically, low cfDNA concentration in SCM and the risk of maternal DNA contamination (from cumulus cells or the zona pellucida) are significant hurdles. Furthermore, the origin of cfDNA is not fully understood, though it is hypothesized to stem from apoptotic cells, potentially with a bias toward the ICM lineage [118] [119].
- The "Backup" and "Combination" Utility: Given current limitations, niPGT's most immediate application may not be as a full replacement for TE biopsy, but as a complementary tool. The 2025 study by BMC Medical Genomics proposed that frozen SCM can serve as a reliable backup sample. When TE biopsy yields a mosaic result, fails to amplify, or is technically challenging, the stored SCM can be analyzed to provide a second, non-invasive opinion, thereby avoiding a harmful second biopsy [80]. The meta-analysis further supports this, showing that a combination of TE biopsy and SCM achieves a superior AUC (0.927) than either method alone [119].
- Future Outlook: Future developments will focus on optimizing embryo culture conditions to minimize contamination, refining WGA and bioinformatic protocols to improve sensitivity and specificity, and standardizing niPGT workflows across laboratories. As the multi-omics paradigm gains traction, niPGT will likely become a key genomic component in a holistic, multi-parameter embryo evaluation system [118] [119].
Diagram 2: niPGT as a clinical backup tool. In cases of ambiguous results from a primary trophectoderm (TE) biopsy, analyzing the spent culture medium (SCM) provides a second genetic opinion without subjecting the embryo to another invasive procedure [80].
The validation of non-invasive PGT against the gold-standard trophectoderm biopsy reveals a rapidly advancing field with significant clinical potential. Quantitative data from recent studies and meta-analyses demonstrate that niPGT using spent culture medium achieves good concordance with TE biopsy, with high sensitivity for detecting aneuploidy. While challenges related to DNA source, contamination, and diagnostic specificity remain, the integration of niPGT into a multi-omics framework—alongside transcriptomics and other data layers—heralds a new era in embryo selection. For researchers and clinicians, niPGT presents an opportunity to augment traditional PGT, either as a primary screening method or, more imminently, as a valuable backup to optimize embryo selection and maximize the efficacy of assisted reproductive technologies.
The integration of multi-omics technologies has revolutionized reproductive biology, providing unprecedented insights into the molecular underpinnings of development and disease. Within assisted reproductive technologies (ART), which have enabled over 10 million births globally, these tools are pivotal for assessing epigenetic safety [22] [125]. Concerns regarding potential long-term health risks in ART-conceived offspring have shifted research focus towards understanding the epigenetic disturbances induced by procedures such as in vitro fertilization (IVF), intracytoplasmic sperm injection (ICSI), and embryo cryopreservation [126] [125]. Multi-omics profiling—encompassing genomics, epigenomics, transcriptomics, and proteomics—provides a comprehensive framework to decode these complex molecular implications. This whitepaper synthesizes current evidence and methodologies, serving as a technical guide for researchers and drug development professionals engaged in ensuring the long-term safety of ART.
Documented Epigenetic Alterations in ART Offspring
Accumulating evidence from human and model organisms reveals that ART procedures can induce specific, functionally relevant epigenetic alterations.
- Human Umbilical Cord Blood Studies: A landmark integrated multi-omics study on human umbilical cord blood revealed that different ART procedures introduce distinct epigenetic disturbances. DNA methylation and the histone modification H3K4me3 were identified as particularly vulnerable. The study concluded that ICSI and frozen embryo transfer (FET) induced more profound disturbances than conventional IVF with fresh embryo transfer. These alterations were enriched in genes and pathways related to nervous system development, cardiovascular function, and glycolipid metabolism, aligning with epidemiological observations of increased health risks in ART-conceived children [126].
- Intergenerational Effects of Sperm Storage: Research on common carp demonstrates that short-term sperm storage, a common practice in aquaculture and with parallels to human ART, induces heritable molecular changes. Offspring derived from stored sperm exhibited altered DNA methylation patterns in their own genomes, which correlated with changes in transcriptomic and proteomic profiles. These molecular changes manifested phenotypically as reduced cardiac performance and altered early growth rates, providing strong evidence for the intergenerational inheritance of storage-induced epimutations [127].
The table below summarizes key quantitative findings from these studies.
Table 1: Documented Epigenetic and Phenotypic Alterations in ART/Stored Gamete-Derived Offspring
| Study Model | ART Procedure / Stressor | Key Epigenetic Findings | Downstream Molecular & Phenotypic Outcomes |
|---|---|---|---|
| Human (Wang et al.) [126] | IVF-FET vs. IVF-ET vs. ICSI-ET | • H3K4me3 most impacted histone mark.• ICSI & freeze-thaw introduced more disturbance.• Decreased DNA methylome similarity in twins. | Alterations enriched in genes for nervous system, cardiovascular, and metabolic processes. |
| Common Carp (BMC Biology, 2025) [127] | In vitro sperm storage (14 days) | • 24,583 DMRs in aged sperm; 26,109 DMRs in F1 embryos.• Global hypermethylation in sperm and embryos. | • Altered transcriptome & proteome.• Reduced offspring cardiac performance.• Increased early body length. |
| Literature Review [125] | Embryo Cryopreservation (Vitrification) | Exposure to cryoprotectants (DMSO, EG) can induce DNA methylation changes, chromatin structural changes, and DNA double-strand breaks. | Associated with large-for-gestational-age babies and potential increased risk of childhood cancer in epidemiological studies. |
Core Multi-Omatics Methodologies for Epigenetic Safety Assessment
A robust multi-omics assessment relies on specific, high-throughput experimental protocols. The following workflows are fundamental for a comprehensive epigenetic safety evaluation.
Sample Collection and Preparation
The foundational step involves collecting relevant biological samples from both parents and offspring. Common samples include:
- Parental Peripheral Blood (PPB): Serves as a reference to control for parental epigenetic contributions [126].
- Sperm: Analyzed for epigenetic integrity post-storage or processing [127].
- Umbilical Cord Blood (UCB): A non-invasive source for offspring multi-omics analysis [126].
- Embryos/Oocytes: Used in studies involving cryopreservation and early development [125].
Omics Profiling Workflows
Integrated workflows are required to capture the different layers of molecular regulation.
Experimental Protocol Details:
Epigenomic Profiling (DNA Methylation & Histone Modifications)
- Reduced Representation Bisulfite Sequencing (RRBS): This cost-effective method profiles DNA methylation in CpG-rich regions. Genomic DNA is digested with a restriction enzyme (e.g., MspI), size-selected, bisulfite-converted, and sequenced to identify methylated cytosines [126].
- Whole-Genome Bisulfite Sequencing (WGBS): The gold standard for a base-resolution methylome. Fragmented genomic DNA undergoes bisulfite conversion, where unmethylated cytosines are deaminated to uracils, and are read as thymines during sequencing, allowing for genome-wide quantification of methylation levels [127].
- Chromatin Immunoprecipitation Sequencing (ChIP-seq): Used to map histone modifications (e.g., H3K4me3, H3K27me3). Chromatin is cross-linked, sheared, and immunoprecipitated with antibodies specific to the histone mark of interest. The bound DNA is then sequenced and mapped to the genome to identify enriched regions [126].
Transcriptomic Profiling
Proteomic Profiling
- Liquid Chromatography with Tandem Mass Spectrometry (LC-MS/MS): Proteins are extracted from tissues (e.g., offspring heart, embryos), digested into peptides, and separated by liquid chromatography. The peptides are ionized and analyzed by mass spectrometry, where their mass-to-charge ratio and fragmentation patterns are used to identify and quantify proteins [127].
Data Integration and Analysis
Data from the various omics layers are integrated bioinformatically.
- Differential Analysis: Identification of Differentially Methylated Regions (DMRs), Differentially Expressed Genes (DEGs), and Differentially Expressed Proteins (DEPs) between ART and control groups.
- Pathway Enrichment Analysis: Tools like DAVID or Metascape are used to determine if the altered genes/proteins are significantly enriched in specific biological pathways (e.g., nervous system development, immune function) [126] [127].
- Correlation Analysis: Integrating datasets to find correlations, for example, between hypermethylation in a gene's promoter and its reduced expression.
The Scientist's Toolkit: Essential Reagents and Technologies
Table 2: Key Research Reagent Solutions for Multi-Omics Profiling
| Item / Technology | Function in Multi-Omics Assessment |
|---|---|
| Bisulfite Conversion Kit | Chemically modifies unmethylated cytosine to uracil, enabling the detection and quantification of DNA methylation via sequencing (RRBS, WGBS). |
| Histone Modification Specific Antibodies | Essential for ChIP-seq to immunoprecipitate chromatin fragments bearing specific histone post-translational modifications (e.g., H3K4me3). |
| mRNA Enrichment Kits | Isolate poly-adenylated mRNA from total RNA to construct high-quality RNA-seq libraries for transcriptome analysis. |
| Single-Cell Omics Platforms | Allow for the profiling of epigenomic, transcriptomic, or proteomic data from individual cells, critical for understanding heterogeneity in early embryos [5]. |
| LC-MS/MS Mass Spectrometer | The core instrument for high-throughput identification and quantification of proteins and their post-translational modifications in proteomic studies. |
| Cryoprotectants (e.g., DMSO, Ethylene Glycol) | Used in vitrification to prevent ice crystal formation; however, their potential toxicity and epigenetic impact are a direct focus of safety research [125]. |
Implications for Drug Development and Future Research
The findings from multi-omics profiling have direct implications for drug development and toxicology. Understanding the specific pathways disturbed by ART (e.g., nervous system, immune function, metabolism) can inform the safety pharmacology assessment of new drugs, particularly for pregnant women or those of reproductive age [126] [127]. Furthermore, this research drives innovation in several directions:
- Optimization of Culture Media and Cryoprotectants: Identifying specific epigenetic risks enables the development of safer, more physiologically accurate ART protocols and reagents.
- Biomarker Discovery: Multi-omics can identify molecular biomarkers predictive of successful outcomes or potential health risks, enabling personalized reproductive medicine [128] [22].
- Advanced Single-Cell and Spatial Technologies: The application of single-cell multi-omics and spatial transcriptomics/proteomics will provide an even higher-resolution view of how ART affects each cell lineage in the developing embryo [5].
The following diagram illustrates the logical pathway from ART procedure to potential long-term outcome and the points of intervention identified by multi-omics research.
Multi-omics profiling has unequivocally demonstrated that ART procedures can induce local and functional epigenetic abnormalities in conceived offspring. These findings frame a new paradigm in reproductive biology, where ensuring epigenetic safety is as crucial as achieving successful pregnancy. For researchers and drug developers, this underscores the necessity of integrating advanced omics technologies into the safety assessment framework for developing new reproductive therapies and protocols. Continued research is vital to fully elucidate the mechanisms, mitigate the risks, and safeguard the long-term health of future generations conceived through ART.
Comparative Effectiveness of Omics vs. Morphological Assessment in IVF Success
The selection of embryos with the highest developmental potential remains a pivotal challenge in in vitro fertilization (IVF). While morphological assessment has been the cornerstone of embryo evaluation for decades, emerging omics technologies promise a more objective and biologically grounded approach. This whitepaper synthesizes current evidence from meta-analyses and systematic reviews to critically evaluate the comparative effectiveness of omics-based profiling versus traditional morphological grading in predicting IVF success. We examine the predictive power of these methodologies for key outcomes, including live birth and miscarriage, and explore the integration of multi-omics data with artificial intelligence (AI) as a pathway toward a more holistic and personalized embryo selection paradigm. The analysis underscores a transitional period in reproductive medicine, where omics technologies, though not yet fully validated for routine clinical use, hold significant potential to enhance the precision and success of assisted reproductive technologies.
In vitro fertilization (IVF) success is fundamentally constrained by the challenge of identifying the single most viable embryo from a cohort, a process known as embryo selection. The conventional method for this selection is morphological assessment, where embryologists evaluate embryo quality based on visual characteristics under a microscope [129]. For cleavage-stage embryos (day 2-3), this involves grading the number and symmetry of cells and the degree of fragmentation. For blastocysts (day 5-6), the Gardner grading system is most common, providing a three-part score for the blastocyst's expansion stage (1-6), the inner cell mass (ICM; A-C), and the trophectoderm (TE; A-C) [130] [131].
Despite its widespread use, morphology has inherent limitations. Its subjective nature leads to inter-observer variability, and it provides only a static snapshot of embryonic development, potentially missing critical dynamic events [129] [132]. Consequently, even morphologically "normal" embryos often fail to implant, driving the search for more robust, non-invasive biomarkers of viability [132].
The field is now witnessing the rise of omics technologies, which aim to assess the embryo's molecular footprint. This includes analyzing the metabolome (small-molecule metabolites), transcriptome (RNA expression), and proteome (proteins) from the spent embryo culture media (SECM) or associated cumulus cells [133] [134] [135]. The central hypothesis is that these molecular profiles offer a more direct, functional readout of the embryo's physiological state and developmental competence than morphology alone.
Framed within a broader thesis on omics in reproductive biology, this review investigates whether these novel analytical approaches can surpass the predictive power of traditional morphology to improve IVF success rates.
Morphological Assessment: An Established but Limited Tool
Methodologies and Predictive Value
Morphological assessment relies on standardized grading protocols. At the blastocyst stage, the expansion grade indicates developmental progress, the ICM quality predicts fetal development potential, and the TE quality is indicative of the future placenta and implantation likelihood [131].
A recent network meta-analysis by Zhang et al. (2025), which incorporated 33 studies and nearly 70,000 embryos, provides high-quality evidence on the predictive strength of each morphological parameter for live birth [130]. The analysis used SUCRA scores (Surface Under the Cumulative Ranking Curve), where a higher percentage indicates a stronger association with live birth.
Table 1: Predictive Value of Blastocyst Morphological Grades for Live Birth (Based on Zhang et al., 2025)
| Morphological Feature | Grade | SUCRA Score (%) | Interpretation |
|---|---|---|---|
| Trophectoderm (TE) | A | 97.1% | Strongest predictor of live birth |
| B | 59.4% | Intermediate | |
| C | 21.1% | Poor | |
| Inner Cell Mass (ICM) | A | 91.1% | Strong predictor |
| B | 44.5% | Intermediate | |
| C | 10.0% | Poor | |
| Expansion Stage | 5 | 83.9% | Optimal |
| 4 | 72.6% | Good | |
| 6 | 49.1% | Lower chance, potentially more fragile | |
| 3 | 43.0% | Fair | |
| 2 | 27.8% | Poor | |
| 1 | 0.4% | Very poor |
The data reveals that an A-grade TE is the single most predictive morphological feature for live birth, followed closely by an A-grade ICM [130]. Notably, full expansion is not optimal; expansion grade 5 is superior to grade 6 (fully hatched), suggesting that a hatched blastocyst may be more fragile and less likely to result in a live birth [130].
Furthermore, specific morphological grades are linked to the risk of miscarriage. Blastocysts with an expansion grade of 2 are most strongly associated with miscarriage, along with those possessing C-grade ICM and TE [130].
Limitations of Morphological Assessment
The primary limitation of morphology is its subjectivity, as grading can differ between labs and even between embryologists within the same lab [130]. Furthermore, it is an indirect measure of viability. A morphologically "beautiful" embryo can be chromosomally abnormal (aneuploid), and conversely, a lower-graded embryo can sometimes self-correct and lead to a healthy live birth [131]. This inherent limitation has fueled the investigation into more direct, molecular-based assessment methods.
Omics Technologies: A New Frontier in Embryo Viability Testing
Omics technologies represent a paradigm shift, moving from visual inspection to the analysis of the embryo's molecular signature. The primary advantage of these approaches, particularly metabolomics and secretomics, is their non-invasiveness, as they often utilize the spent culture medium.
Metabolomic Profiling
Metabolomic analysis of spent embryo culture media (SECM) involves profiling the nutrients consumed and metabolites released by the embryo, providing a window into its energy metabolism and overall health [133] [134]. Key energy substrates monitored include glucose, pyruvate, and lactate [134]. Amino acid turnover is also a critical area of investigation, with specific profiles linked to developmental potential [134]. For instance, higher levels of asparagine and lower levels of glycine on day 2 of culture have been associated with pregnancy and live birth rates [129].
A 2025 Bayesian meta-analysis by Frontiers in Cell and Developmental Biology synthesized data from studies reporting absolute metabolite concentrations in SECM. It identified several metabolites with significant associations with IVF outcomes, highlighting the potential of this approach [134].
Table 2: Key Metabolites in Spent Culture Media Associated with IVF Outcomes
| Metabolite Class | Examples of Metabolites | Association with Favorable Outcome | Proposed Biological Role |
|---|---|---|---|
| Amino Acids | Asparagine, Glutamine | Positive [129] [134] | Energy production, cellular signaling, osmoregulation |
| Glycine | Negative [129] | Not fully understood, potential marker of stress | |
| Carbohydrates & Energy Substrates | Pyruvate, Glucose uptake | Positive [129] [134] | Key energy sources, especially during early cleavage and blastocyst formation |
| Lactate production | Positive (in later stages) [129] | Indicator of aerobic glycolysis during increased energy demand | |
| Lipids | Specific Acyl Carnitines, Glycerophospholipids | Both positive and negative associations found [134] | Components of cell membranes, energy metabolism |
Diagram 1: Metabolomic Profiling Workflow from Spent Culture Media.
Transcriptomic and Other Omics Analyses
Beyond metabolomics, other omics layers offer complementary insights:
- Transcriptomics: This involves analyzing the gene expression profiles of the cumulus cells that surround the oocyte. The hypothesis is that the health and competence of the oocyte are reflected in the transcriptome of these associated somatic cells. Studies have identified genes such as HAS2, GREM1, STAR, and AREG as potential biomarkers of oocyte quality and subsequent embryo viability [129] [135].
- Proteomics and Secretomics: This field focuses on identifying proteins secreted by the embryo into the culture medium (the "secretome"). Proteins like IL-1 beta, HLA-G, and Ubiquitin have been investigated for their association with blastocyst development and implantation potential [129].
Limitations of Omics Technologies
Despite their promise, omics technologies face significant barriers to clinical adoption. A major challenge is the lack of standardization across multiple variables, including culture media composition from different manufacturers, analytical platforms, and experimental protocols [133] [134]. This heterogeneity has led to inconsistent findings between studies, making it difficult to define universal biomarkers. Consequently, a recent meta-analysis concluded that the live birth rate is not significantly different when metabolomic profiling is used alongside morphology compared to morphology alone [129]. As of now, no omics biomarker has been fully validated for routine clinical use.
Direct Comparison and Integration of Methods
Quantitative Comparison of Predictive Performance
Directly comparing the diagnostic accuracy of morphology and emerging technologies is complex due to different outcome measures. However, recent meta-analyses allow for a preliminary comparison.
Table 3: Comparative Diagnostic Performance of Embryo Assessment Methods
| Assessment Method | Reported Performance Metric | Value | Context / Outcome |
|---|---|---|---|
| Morphology (Gardner Blastocyst Grading) | Odds Ratio (OR) for Live Birth | TE (A) vs. TE (B): OR = -0.32 [130] | Represents significantly lower odds for grade B |
| SUCRA Score | TE (A): 97.1% [130] | Highest probability for live birth | |
| AI-based Embryo Selection | Pooled Sensitivity | 0.69 [132] | For predicting implantation |
| Pooled Specificity | 0.62 [132] | For predicting implantation | |
| Area Under the Curve (AUC) | 0.7 [132] | Indicates "high overall accuracy" | |
| Metabolomic Profiling | Live Birth Rate | No significant improvement over morphology alone [129] | Based on current evidence from meta-analysis |
The table indicates that while standard morphology provides a solid baseline, AI models that can learn from morphological and morphokinetic data show improved and more objective predictive performance [132]. The current evidence for metabolomic profiling, however, has not yet demonstrated a conclusive improvement in live birth rates.
The Integrated Future: Multi-Omics and Artificial Intelligence
The future of embryo selection lies not in replacing one tool with another, but in their integration. The most promising strategy involves combining morphological, morphokinetic (from time-lapse imaging), and multi-omics data within AI-driven algorithms [133] [132] [135].
AI and deep learning models, such as convolutional neural networks (CNNs), can analyze vast and complex datasets to identify subtle, non-linear patterns that are imperceptible to the human eye or traditional statistics [132]. For example, an AI system named IVY has demonstrated exceptional predictive accuracy, while another, the FiTTE system, which integrates blastocyst images with clinical data, achieved a 65.2% prediction accuracy for clinical pregnancy [132].
Diagram 2: AI-Driven Integration of Multi-Modal Data for Embryo Selection.
This integrated approach aligns with the vision of personalized IVF treatment, where a bespoke combination of biomarkers and data points can be used to select the optimal embryo for each individual patient, particularly those with unexplained infertility or repeated implantation failures [135].
The Scientist's Toolkit: Research Reagent Solutions
For research teams investigating omics in embryo assessment, the following reagents and tools are essential.
Table 4: Essential Research Reagents and Platforms for Omics Studies in IVF
| Reagent / Platform | Function in Research | Key Considerations |
|---|---|---|
| Defined Culture Media | Supports embryo development in vitro; the baseline for SECM analysis. | Formulations vary by manufacturer (e.g., nutrient content); a major source of variability. Use consistent batches per study. [133] |
| Mass Spectrometry (MS) | The primary analytical platform for identifying and quantifying metabolites in SECM. | High sensitivity and specificity. Requires method calibration and standardized protocols for reproducible results. [134] |
| Nucleotide Extraction Kits | For RNA extraction from cumulus cells for transcriptomic analysis. | Must ensure purity and integrity of RNA for accurate gene expression profiling (e.g., via microarrays or RNA-seq). [135] |
| Time-Lapse Imaging (TLI) Systems | Provides uninterrupted morphokinetic data for integration with omics data. | Allows correlation of dynamic developmental events (e.g., timing of cell divisions) with molecular profiles. [129] [132] |
| AI/ML Software Platforms | (e.g., Python with TensorFlow/PyTorch) | Used to develop predictive models by integrating complex, multi-modal datasets (images, omics, clinical). [132] [135] |
The comparative analysis of omics and morphological assessment reveals a dynamic and evolving landscape. Traditional morphology, particularly trophectoderm grade, remains a powerful and clinically validated predictor of live birth. However, its subjectivity and biological limitations are clear. Omics technologies, especially metabolomics, offer a non-invasive and functionally relevant window into embryonic physiology, yet they currently lack the standardization and robust validation required for widespread clinical adoption.
The path forward is not a competition between these methods but a strategic synthesis. The most significant gains in IVF success rates will likely come from integrated models that combine the established strengths of morphology with the deep biological insights of omics, all processed through the objective, pattern-recognition power of artificial intelligence. Future research must focus on standardizing omics protocols, conducting large-scale randomized controlled trials, and developing robust AI algorithms capable of translating multi-modal data into clinically actionable decisions. This synergistic approach holds the key to unlocking more personalized, effective, and successful IVF treatments.
The Role of Randomized Controlled Trials and Large-Scale Datasets in Clinical Validation
The integration of omics technologies—encompassing genomics, transcriptomics, proteomics, and metabolomics—is revolutionizing reproductive biology research and the development of novel therapeutic interventions. These technologies generate vast, multidimensional data that promise to unravel the complex molecular underpinnings of reproductive health and disease. However, this promise can only be realized through a rigorous clinical validation process that strategically combines the precision of Randomized Controlled Trials (RCTs) with the breadth and real-world relevance of large-scale datasets. Within reproductive medicine, this integrated approach is essential for translating molecular discoveries into clinically actionable insights that can improve outcomes in areas such as infertility, endometrial receptivity, and embryonic development.
The traditional hierarchy of evidence, which places RCTs at the apex, is being reconceptualized. While RCTs remain the gold standard for establishing causal efficacy under controlled conditions, large-scale real-world data (RWD) are now recognized as indispensable for assessing effectiveness in diverse patient populations and for addressing questions that RCTs are ill-equipped to answer. This whitepaper provides an in-depth technical guide for researchers and drug development professionals on leveraging both methodologies to robustly validate the clinical utility of omics-derived biomarkers and therapies in reproductive biology.
The Evolving Role of Randomized Controlled Trials
Methodological Foundations and Integrity
RCTs are designed to minimize bias by randomly assigning participants to experimental or control groups, thereby evenly distributing both known and unknown confounders. This design is paramount for establishing a causal relationship between an intervention and an outcome. The integrity of RCTs is critical, as flaws in design, conduct, analysis, or reporting can compromise the trustworthiness of the evidence base that informs clinical practice in reproductive medicine [136].
Recent initiatives, such as the Cairo consensus statements, provide discipline-specific research integrity guidelines tailored to the entire RCT lifecycle. These address issues from protocol registration and statistical analysis plan pre-specification to responsible publication practices, aiming to curb problems like selective reporting and p-hacking that have been observed in various fields, including medically assisted reproduction [136]. Furthermore, the updated CONSORT 2025 statement (Consolidated Standards of Reporting Trials) offers a revised 30-item checklist that includes a new section on open science, ensuring that trial reports are clear, complete, and transparent [137]. Adherence to these guidelines is non-negotiable for producing reliable evidence.
Experimental Protocol for an Omics-Driven RCT in Reproduction
Designing an RCT to validate an omics-based biomarker or therapy requires careful consideration of the unique challenges presented by multidimensional data and reproductive endpoints.
1. Protocol Definition and Registration:
- Primary Objective: To evaluate the efficacy of a personalized embryo transfer strategy, guided by a transcriptomic signature of endometrial receptivity, on live birth rates compared to standard morphological dating.
- PICO Framework:
- Population: Infertile women aged 25-38 undergoing single euploid blastocyst transfer.
- Intervention: Embryo transfer timed according to the results of the endometrial receptivity assay (ERA).
- Comparator: Embryo transfer timed according to standard progesterone exposure duration.
- Outcomes: Primary: Live birth rate per transfer. Secondary: Clinical pregnancy rate, implantation rate, ongoing pregnancy rate.
- Pre-registration: The final protocol, including the detailed statistical analysis plan, must be registered on a public platform such as ClinicalTrials.gov before participant enrollment begins [136].
2. Randomization and Blinding:
- Randomization Scheme: Use stratified block randomization (e.g., via computer-generated sequence) with stratification for key prognostic factors such as patient age and BMI to ensure balanced groups.
- Blinding: While the embryologist and clinician performing the transfer may be unblinded to assign the transfer day, the patient, the physician performing the pregnancy outcome assessment, and the data analyst must be blinded to group allocation to minimize assessment bias.
3. Sample Size Calculation and Statistical Analysis:
- Power Analysis: Based on an assumed live birth rate of 30% in the control group, to detect an absolute improvement of 10% (with 80% power and alpha of 0.05), approximately 440 patients per arm would be required.
- Analysis Plan: The primary analysis should follow the intention-to-treat (ITT) principle. A pre-specified per-protocol analysis may also be conducted. Statistical methods (e.g., logistic regression for the primary outcome) must be detailed in the registered analysis plan to prevent data dredging.
4. Data Collection and Reporting:
- Omics Data Management: Raw and processed omics data (e.g., RNA-seq files) must be deposited in public repositories such as Gene Expression Omnibus (GEO) upon publication.
- Reporting Standards: The final manuscript must adhere to the CONSORT 2025 statement to ensure all essential trial elements are fully reported [137].
The following diagram illustrates the key stages and integrity checks in the RCT lifecycle, from conception to post-publication.
Harnessing Large-Scale Real-World Data
When RCTs are not feasible, ethical, or sufficiently timely, large-scale real-world data (RWD) provide a powerful complementary source of evidence. RWD is defined as "data relating to patient health status and/or the delivery of healthcare routinely collected from a variety of sources" [138]. Key platforms and datasets relevant to reproductive research include:
- Analytics Platforms (TriNetX): This federated global health research network provides access to de-identified electronic health record (EHR) data from millions of patients across hundreds of healthcare organizations. Its architecture allows for real-time, privacy-compliant analytics on a massive scale, making it ideal for studying rare reproductive outcomes, long-term safety of fertility treatments, and therapy effectiveness in diverse populations [138].
- Clinical Datasets (MedCD): This is a large, real-world medical clinical dataset sourced from EHRs, clinical notes, and lab reports, designed to accelerate generative AI research in healthcare. It contains 1.7 million EHR examples and features supervised data for tasks like named entity recognition (NER) and summarization, which can be applied to model reproductive health journeys [139].
- Open-Access Data Repositories: Numerous public datasets are invaluable for discovery and validation. Examples include:
- MIMIC Critical Care Database: Contains de-identified health data from over 40,000 critical care patients, useful for studying severe obstetric or reproductive complications [140].
- 1000 Genomes Project: One of the largest accessible genome repositories, providing sequencing data from 2,500 individuals across 26 populations, crucial for studying genetic factors in infertility [140].
- BioASQ Challenges: Provide benchmark datasets for biomedical semantic indexing and question-answering, including tasks like clinical coding and information extraction that can be tailored to reproductive concepts [141].
Table 1: Selected Large-Scale Data Platforms for Clinical Validation in Reproductive Biology
| Platform/Dataset | Data Type and Scale | Primary Application in Reproductive Research |
|---|---|---|
| TriNetX [138] | Federated EHRs from >150 million patients (as of 2024) | Hypothesis generation, comparative effectiveness research, post-market surveillance of ART drugs/devices. |
| MedCD [139] | 1.7 million EHRs, clinical notes, lab reports. | Training AI models for clinical tasks (e.g., NER, summarization) in a reproductive context. |
| MIMIC-III/IV [140] | EHRs from >40,000 ICU patients. | Studying severe maternal morbidity and critical care outcomes in obstetrics. |
| 1000 Genomes Project [140] | Sequencing data from 2,500 individuals. | Identifying population-specific genetic variants linked to reproductive disorders. |
Methodological Workflow for RWD Analysis
Validating an omics finding using RWD requires a rigorous analytical approach to mitigate the inherent biases of non-randomized data.
1. Hypothesis and Cohort Definition:
- Objective: To validate whether a specific serum metabolomic profile associated with oxidative stress (identified in a discovery cohort) predicts lower live birth rates in patients undergoing IVF.
- Data Source: Use a large, de-identified EHR and ART cycle database (e.g., the SART CORS or a federated network like TriNetX).
2. Cohort Identification and Propensity Score Matching:
- Inclusion/Exclusion: Apply criteria to select a clean cohort of first, autologous IVF cycles.
- Matching: To control for confounding, patients with the "at-risk" metabolomic profile (Exposed group) should be matched 1:1 to patients without the profile (Control group) using propensity score matching. Scores are generated from a logistic regression model that includes confounders such as age, BMI, AFC, and diagnosis.
3. Outcome Analysis and Confounding Adjustment:
- Primary Comparison: Compare the live birth rate between the matched exposed and control cohorts using a conditional logistic regression.
- Sensitivity Analyses: Conduct analyses to assess the robustness of the findings, such as:
- E-value Calculation: Quantifies the minimum strength of association an unmeasured confounder would need to have to explain away the observed effect.
- Rule-Out Method: Test the impact of adding hypothesized unmeasured confounders (e.g., smoking status, if available) to the model.
The workflow for a robust RWD analysis is depicted below.
Integration for Validation of Omics Technologies in Reproductive Biology
The true power of modern clinical validation lies in the synergistic use of RCTs and RWD. This is particularly salient in reproductive biology, where omics technologies are identifying novel biomarkers for patient stratification and personalized treatment protocols.
For instance, a genomic classifier for predicting embryo ploidy or a proteomic signature for endometrial receptivity might first be discovered and validated retrospectively using large biobanks and RWD. This initial validation can assess the biomarker's association with outcomes across diverse, real-world populations. Subsequently, the findings must be prospectively validated in a rigorous RCT to establish that clinical decision-making based on the biomarker causes an improvement in patient outcomes, such as live birth rate or time to pregnancy [142] [143].
The integration of multi-omics data into clinical validation frameworks requires specialized analytical tools and workflows, as illustrated below.
Table 2: Key Reagent Solutions for Omics-Driven Reproductive Research
| Reagent / Tool Category | Specific Examples | Function in Clinical Validation |
|---|---|---|
| Genomic Profiling | Next-Generation Sequencing (NGS) Panels, Whole Genome/Exome Sequencing | Identifies genetic variants (SNPs, CNVs) associated with conditions like PCOS, premature ovarian insufficiency, and male factor infertility [142]. |
| Transcriptomic Analysis | RNA-seq Microarrays, Single-Cell RNA-seq | Profiles gene expression in endometrial tissue (e.g., for receptivity), oocytes, or embryos to discover developmental competence biomarkers [142] [143]. |
| Proteomic Kits | Mass Spectrometry Kits, Multiplex Immunoassays (e.g., Luminex) | Quantifies protein abundance in seminal plasma, follicular fluid, or uterine fluid to identify signatures of sperm/oocyte quality or endometrial status [142]. |
| Metabolomic Assays | NMR Spectroscopy Kits, LC-MS/MS Platforms | Measures small-molecule metabolites in biofluids to assess oocyte/embryo viability and maternal metabolic health [142]. |
| Bioinformatics Suites | QIAGEN Clinical Insight (QCI), Custom R/Python Pipelines | Provides structured, clinical-grade analysis and interpretation of complex omics data for reporting and decision support [144]. |
The validation of omics-driven discoveries in reproductive biology necessitates a sophisticated, dual-track approach. Randomized Controlled Trials provide the indispensable, methodologically rigorous foundation for establishing causal efficacy and are supported by evolving standards like the CONSORT 2025 guidelines and Cairo integrity statements. Concurrently, large-scale real-world datasets offer unprecedented opportunities for discovery, hypothesis generation, and assessing the generalizability and long-term effectiveness of interventions in heterogeneous patient populations.
For researchers and drug developers, the path forward involves the strategic integration of both paradigms. Initial findings from real-world data can inform the design of more targeted and efficient RCTs, while the results of RCTs must subsequently be monitored in real-world settings to ensure their broad applicability. By leveraging the complementary strengths of both methods, the field of reproductive medicine can accelerate the translation of groundbreaking omics research into validated clinical tools that ultimately improve patient care and outcomes.
Conclusion
Omics technologies have fundamentally reshaped reproductive medicine, offering unprecedented resolution into the molecular underpinnings of fertility and embryonic development. The integration of genomics, transcriptomics, proteomics, and epigenomics is driving a paradigm shift from empirical observation to data-driven, personalized care. However, the full potential of this revolution hinges on overcoming significant challenges: the rigorous validation of clinical tools like PGT-A and niPGT, the seamless integration of multi-omics data into predictive models, and the thoughtful navigation of associated ethical landscapes. Future directions will be characterized by the refinement of non-invasive diagnostics, the maturation of AI and machine learning applications, and a deepened investigation into the long-term health of ART-conceived offspring through epigenomic lenses. For researchers and drug developers, the imperative is to build robust, evidence-based frameworks that translate these powerful technological advances into safe, effective, and accessible clinical interventions, ultimately improving outcomes for patients worldwide.
References
- 1. Reproductomics: Exploring the Applications and Advancements of Computational Tools - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11629954/]
- 2. Reproductomics: Exploring the Applications and Advancements of Computational Tools - PubMed [https://pubmed.ncbi.nlm.nih.gov/39530905/]
- 3. 'Omics' Sciences: Genomics, Proteomics, and Metabolomics | ISAAA.org [https://www.isaaa.org/resources/publications/pocketk/15/default.asp]
- 4. From Omics to Multi-Omics: A Review of Advantages and Tradeoffs [https://pmc.ncbi.nlm.nih.gov/articles/PMC11675490/]
- 5. Single-cell omics technologies - Fundamentals on how to create single-cell looking glasses for reproductive health - PubMed [https://pubmed.ncbi.nlm.nih.gov/40253074/]
- 6. Dissecting mammalian reproduction with spatial transcriptomics [https://pubmed.ncbi.nlm.nih.gov/37353907/]
- 7. An interactive atlas of genomic, proteomic, and metabolomic ... - Nature [https://www.nature.com/articles/s41598-024-63399-9]
- 8. in multi- Challenges omics data integration [https://blog.biostrand.ai/challenges-in-multi-omics-data-integration]
- 9. in the era of Data : current and future integration omics challenges [https://bmcsystbiol.biomedcentral.com/articles/10.1186/1752-0509-8-S2-I1]
- 10. Nextflowomics: Untangling Biology with Data Analysis Pipelines | Seqera [https://seqera.io/blog/nextflowomics-untangling-biology-with-data-analysis-pipelines/]
- 11. Empowering bioinformatics communities with Nextflow and nf-core [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03673-9]
- 12. enables reproducible computational Nextflow workflows [https://www.nature.com/articles/nbt.3820?error=cookies_not_supported&code=829df90e-99a7-403b-8813-0cf0767aff25]
- 13. Omics Pipe: a community-based framework for reproducible multi-omics data analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4443682/]
- 14. Omics Pipe: a community-based framework for reproducible multi-omics data analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/25637560/]
- 15. 4MS-DIAL: A Reproducible Nextflow -Based Nextflow for... Workflow [https://pubmed.ncbi.nlm.nih.gov/39755959/]
- 16. Introduction to Bioinformatics workflows with Nextflow and nf-core... [https://carpentries-incubator.github.io/workflows-nextflow/09-configuration.html]
- 17. Postgenomic era - Wikipedia [https://en.wikipedia.org/wiki/Postgenomic_era]
- 18. Twin Research in the Post - Genomic : Dissecting the... Era [https://pmc.ncbi.nlm.nih.gov/articles/PMC7247668/]
- 19. What Does It Mean to Be In the ' Post - Genomic ' Age? [https://undark.org/2024/12/05/opinion-post-genomic-age/]
- 20. for Human Translational ... Bioinformatics Reproductive Biology [https://www.mdpi.com/1422-0067/24/1/4]
- 21. OMICS: Current and future perspectives in reproductive medicine and technology - PubMed [https://pubmed.ncbi.nlm.nih.gov/25191020/]
- 22. Frontiers | Integrating omics approaches in livestock biotechnology: innovations in production and reproductive efficiency [https://www.frontiersin.org/journals/animal-science/articles/10.3389/fanim.2025.1551244/full]
- 23. 2025 and Beyond: The Future of Genomic Data Analysis and Innovations in Genomics Services [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 24. 2025 Trends: NGS [https://www.genengnews.com/topics/genome-editing/2025-trends-ngs/]
- 25. for Human Translational ... Bioinformatics Reproductive Biology [https://pubmed.ncbi.nlm.nih.gov/36613446/]
- 26. Genomics-driven drug discovery based on disease-susceptibility genes | Inflammation and Regeneration | Full Text [https://inflammregen.biomedcentral.com/articles/10.1186/s41232-021-00158-7]
- 27. Bridging the layers: towards integration of signal transduction, regulation and metabolism into mathematical models - Molecular BioSystems (RSC Publishing) DOI:10.1039/C3MB25489E [https://pubs.rsc.org/en/content/articlehtml/2013/mb/c3mb25489e]
- 28. OMICS: Current and future perspectives in reproductive medicine and technology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4150148/]
- 29. - Non RNAs as coding in epigenetics (Review) regulators [https://pubmed.ncbi.nlm.nih.gov/27841002/]
- 30. - Non RNAs as coding in epigenetics (Review) regulators [https://www.spandidos-publications.com/or/37/1/3?text=fulltext]
- 31. 2.7 DNA , Transcription, Translation – The Biology... Replication [https://blogs.ubc.ca/mrpletsch/2017/02/04/2-7-dna-replication-transcription-translation/]
- 32. Metabolic pathway - Wikipedia [https://en.wikipedia.org/wiki/Metabolic_pathway]
- 33. Metabolic Pathway - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/metabolic-pathway]
- 34. - Single — Fundamentals on how to create... cell omics technologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC12090843/]
- 35. ZS insights: Single-cell data breakthroughs in drug development [https://www.zs.com/insights/future-of-drug-development-single-cell-biologic-maps]
- 36. Clinical Applications of Spatial in Disease Diagnosis and... Biology [https://www.news-medical.net/health/Clinical-Applications-of-Spatial-Biology-in-Disease-Diagnosis-and-Treatment.aspx]
- 37. Frontiers | Single-cell technology for drug discovery and development [https://www.frontiersin.org/journals/drug-discovery/articles/10.3389/fddsv.2024.1459962/full]
- 38. Frontiers | Single - cell dual- omics reveals translational and... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1534648/full]
- 39. Frontiers | Multi-omics and machine learning for the prevention and management of female reproductive health [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1081667/full]
- 40. Frontiers | Editorial: Single - cell and spatial - omics in delineating... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1365242/full]
- 41. 综述:辅助生殖技术ä¸èƒšèƒŽå¥åº·è¯„估的智能方法综述 - 生物通 [https://www.ebiotrade.com/newsf/2025-6/20250613173227570.htm]
- 42. Noninvasive Testing of Preimplantation Embryos in Assisted Reproductive Technology | IntechOpen [https://www.intechopen.com/chapters/1172998]
- 43. How AI is emerging as a valuable tool in predicting embryo viability [https://www.theweek.in/news/health/2025/06/27/how-ai-is-emerging-as-a-valuable-tool-in-predicting-embryo-viability.html]
- 44. FEMI helps predict IVF outcomes with greater accuracy [https://www.news-medical.net/news/20250715/FEMI-helps-predict-IVF-outcomes-with-greater-accuracy.aspx]
- 45. Nature Medicine | äººå·¥æ™ºèƒ½ä¸Žä¼ ç»ŸæŠ€æœ¯åœ¨IVF胚胎选择ä¸çš„首次对决:效率æå‡ä¸Žä¸´åºŠæˆæ•ˆçš„探索 - 医疗å¥åº·ä¸“区 - 生物谷 [https://news.bioon.com/article/3f6a83881160.html]
- 46. Omics and Artificial Intelligence to Improve In Vitro Fertilization (IVF) Success: A Proposed Protocol - PubMed [https://pubmed.ncbi.nlm.nih.gov/33919350/]
- 47. The ReproGenomics Viewer: a multi- omics and cross-species... [https://pubmed.ncbi.nlm.nih.gov/30668675/]
- 48. (PGS) Preimplantation Genetic Screening [https://www.illumina.com/techniques/popular-applications/genotyping/pgs.html]
- 49. Preimplantation genetic screening ( PGS ) still in search of a clinical... [https://rbej.biomedcentral.com/articles/10.1186/1477-7827-12-22]
- 50. - PGS in reproductive medicine and perspective directions for... FISH [https://link.springer.com/article/10.1007/s10815-011-9578-9]
- 51. PGD and PGS : The Use of FISH , CGH and aCGH for Identifying... [https://ovu.com/fertility-insights/pgd-and-pgs-the-use-of-fish-cgh-and-acgh-for-identifying-chromosome-mosaicism-correlation]
- 52. for structural rearrangements by... Preimplantation genetic testing [https://pmc.ncbi.nlm.nih.gov/articles/PMC11731775/]
- 53. Integrated profiling of semen microbiota and metabolome reveals... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07139-1]
- 54. Future diagnostics in male infertility: genomics, epigenetics, metabolomics and proteomics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7108983/]
- 55. Exploring Human Sperm Metabolism and Male : A Systematic... Infertility [https://pubmed.ncbi.nlm.nih.gov/40806673/]
- 56. Limitations of Semen Analysis as a Test of Male Fertility and Anticipated Needs from Newer Tests - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4254491/]
- 57. Multi- Omics Approaches for Reproductive Health Data | SpringerLink [https://link.springer.com/chapter/10.1007/978-981-97-7451-7_4]
- 58. The bioinformatics tool box for reproductive biology - PubMed [https://pubmed.ncbi.nlm.nih.gov/22687534/]
- 59. Bringing proteomics to bear on male fertility: key lessons - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11426281/]
- 60. A Comprehensive Mass Spectrometry-Based Proteomic Dataset of Human Spermatozoa | Scientific Data [https://www.nature.com/articles/s41597-025-05824-w]
- 61. Seminal biomarkers for the evaluation of male infertility - PubMed [https://pubmed.ncbi.nlm.nih.gov/26975492/]
- 62. -Lessons from "Omics" Endometrial Receptivity [https://pubmed.ncbi.nlm.nih.gov/39858500/]
- 63. Frontiers | Non-Invasive and Mechanism-Based Molecular Assessment... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2022.863173/full]
- 64. Endometrial Receptivity–Lessons from “Omics†- PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11764156/]
- 65. Commercially Available Molecular Approaches to Evaluate Endometrial Receptivity: A Systematic Review and Critical Analysis of the Literature - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9689742/]
- 66. Advances in endometrial receptivity and embryo implantation by multi-omics techniques - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2950248925000355]
- 67. Genomic, proteomic and lipidomic evaluation of endometrial ... [https://tjoddergisi.org/articles/genomic-proteomic-and-lipidomic-evaluation-of-endometrial-receptivity/tjod.98475]
- 68. (PDF) Proteomic of human uterine extracellular vesicles... profiling [https://www.academia.edu/122009184/Proteomic_profiling_of_human_uterine_extracellular_vesicles_reveal_dynamic_regulation_of_key_players_of_embryo_implantation_and_fertility_during_menstrual_cycle]
- 69. The microbiome in reproductive health: protocol for a systems ... [https://pubmed.ncbi.nlm.nih.gov/35441092/]
- 70. IMP: a pipeline for reproducible reference-independent integrated... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-016-1116-8]
- 71. Frontiers | Multi - omics analysis based on plasma... integration [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1686282/full]
- 72. - Integrated profiling characterizes the crucial role of... multi omics [https://pubmed.ncbi.nlm.nih.gov/40120109/]
- 73. Top 6 Visualizations for Quantitative Data Analysis Methods - [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 74. RAWGraphs [https://www.rawgraphs.io/]
- 75. Text has enhanced contrast | ACT Rule | WAI | W3C [https://www.w3.org/WAI/standards-guidelines/act/rules/09o5cg/]
- 76. chroma.js api docs! [https://gka.github.io/chroma.js/]
- 77. font-color-contrast - npm [https://www.npmjs.com/package/font-color-contrast]
- 78. The embryo non-invasive pre-implantation diagnosis era: how far are... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10503888/]
- 79. Evaluation of the Effectiveness and Accuracy of Non-Invasive Preimplantation Genetic Testing (niPGT) Compared to Invasive Embryo Biopsy - PubMed [https://pubmed.ncbi.nlm.nih.gov/40868262/]
- 80. Noninvasive preimplantation genetic testing for aneuploidy using blastocyst spent culture medium may serve as a backup of trophectoderm biopsy in conventional preimplantation genetic testing | BMC Medical Genomics | Full Text [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-025-02106-7]
- 81. Extended blastocyst culture improves DNA yield in non-invasive... [https://www.nature.com/articles/s41598-025-18764-7?error=cookies_not_supported&code=13114852-9ac9-4225-af33-e5582b349dc1]
- 82. Non-invasive preimplantation genetic testing for conventional IVF blastocysts | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-022-03596-0]
- 83. Optimizing Non-Invasive PGT - A : A Multi-Factorial Approach for... [https://pubmed.ncbi.nlm.nih.gov/41113626/]
- 84. A prospective study of non-invasive preimplantation genetic testing for aneuploidies (NiPGT-A) using next-generation sequencing (NGS) on spent culture media (SCM) - PubMed [https://pubmed.ncbi.nlm.nih.gov/31292818/]
- 85. Effect of noninvasive embryo viability testing versus conventional IVF... [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-023-05892-z]
- 86. Current and future therapies for abnormal early embryogenesis with... [https://www.techscience.com/biocell/v46n8/47567/html]
- 87. and the Omics in Reproductive Medicine Technologies Applications [https://www.frontiersin.org/research-topics/49551/omics-technologies-and-the-applications-in-reproductive-medicine/magazine]
- 88. Multi-omics Data Integration, Interpretation, and Its Application - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7003173/]
- 89. Single-cell sequencing to multi- omics : technologies and applications [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-024-00643-4]
- 90. Frontiers | A standards perspective on genomic data reusability and... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1572937/full]
- 91. Spatial integration of multi- omics from serial sections using the... data [https://pubmed.ncbi.nlm.nih.gov/40366868/]
- 92. Frontiers | More Is Better: Recent Progress in Multi-Omics Data Integration Methods [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2017.00084/full]
- 93. multi- omics - integration · GitHub Topics · GitHub [https://github.com/topics/multi-omics-integration]
- 94. of laboratory Quality for semen evaluation in... control methods [https://pubmed.ncbi.nlm.nih.gov/15223854/]
- 95. Standardized and accessible multi-omics bioinformatics workflows through the NMDC EDGE resource - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2001037024003064]
- 96. A standards perspective on genomic data reusability and... [https://pubmed.ncbi.nlm.nih.gov/40130011/]
- 97. Network-based multi-omics integrative analysis methods in drug discovery: a systematic review | BioData Mining | Full Text [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-025-00442-z]
- 98. Screening embryos for polygenic disease risk : a review of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11369226/]
- 99. Polygenic risk scoring of human embryos: a qualitative study of media coverage - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8449454/]
- 100. Preimplantation genetic testing for polygenic in... risk [https://www.jptcp.com/index.php/jptcp/article/view/10799]
- 101. The race to make the perfect baby is creating an ethical mess [https://www.technologyreview.com/2025/10/16/1125159/ethics-embryo-screening-reproduction-baby/1214/]
- 102. embryo screening – Patient perspectives and concerns | PET Polygenic [https://www.progress.org.uk/polygenic-embryo-screening-patient-perspectives-and-concerns/]
- 103. Limitations, concerns and potential: attitudes of healthcare... [https://www.nature.com/articles/s41431-023-01333-9?error=cookies_not_supported&code=c718fd5f-0bd7-45e9-ab84-9670fa23fcda]
- 104. "Are we not going too far?": Socio- ethical of... considerations [https://pubmed.ncbi.nlm.nih.gov/38244362/]
- 105. Polygenic risk scoring of human embryos: a qualitative study of media coverage | BMC Medical Ethics | Full Text [https://bmcmedethics.biomedcentral.com/articles/10.1186/s12910-021-00694-4]
- 106. A biological function based biomarker panel optimization process | Scientific Reports [https://www.nature.com/articles/s41598-019-43779-2]
- 107. A biological function based biomarker process... panel optimization [https://pmc.ncbi.nlm.nih.gov/articles/PMC6517383/]
- 108. Biomarker Discovery and Validation: Statistical Considerations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 109. From Biomarker Discovery to Clinical Use - Nordic Bioscience [https://www.nordicbioscience.com/why-biomarkers/from-biomarker-discovery-to-clinical-use/]
- 110. Biomarker Validation - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/biomarker-validation]
- 111. Statistical Approaches to Candidate Biomarker Panel Selection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7885896/]
- 112. through artificial intelligence versus embryologists... Embryo selection [https://pmc.ncbi.nlm.nih.gov/articles/PMC10426717/]
- 113. Global Trends in the Use of Artificial Intelligence ( AI ) in Reproductive... [https://jivfww.scholasticahq.com/article/140673]
- 114. This AI-powered tool predicts success 90% of the time IVF [https://nypost.com/2025/11/06/health/this-ai-powered-tool-predicts-ivf-success-90-of-the-time/]
- 115. The race to make the perfect baby is creating an ethical mess | MIT Technology Review [https://www.technologyreview.com/2025/10/16/1125159/ethics-embryo-screening-reproduction-baby/]
- 116. doondu/IVFSuccessPredictor-Aimers 2025 : AI research to predict ... [https://github.com/doondu/IVFSuccessPredictor-Aimers2025]
- 117. The future of genomics: 5 trends that will impact the next era of precision medicine - Bioinformatics Software | QIAGEN Digital Insights [https://digitalinsights.qiagen.com/news/blog/clinical/the-future-of-genomics-5-trends-that-will-impact-the-next-era-of-precision-medicine/]
- 118. Evolution of Minimally Invasive and Non-Invasive Preimplantation Genetic Testing: An Overview | MDPI [https://www.mdpi.com/2077-0383/13/8/2160]
- 119. The diagnostic accuracy of preimplantation genetic testing (PGT) in assessing the genetic status of embryos: a systematic review and meta-analysis | Reproductive Biology and Endocrinology | Full Text [https://rbej.biomedcentral.com/articles/10.1186/s12958-025-01376-1]
- 120. of Concordance for aneuploidies between blastocyst PGT ... biopsies [https://pubmed.ncbi.nlm.nih.gov/36642559/]
- 121. Frontiers | A Non-invasive Chromosome Screening Strategy for ... [https://www.frontiersin.org/articles/10.3389/fcell.2021.708322/full]
- 122. Multi-omics PGT: re-evaluation of euploid blastocysts for implantation potential based on RNA sequencing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11629973/]
- 123. Accurate aneuploidy detection with the Embgenix PGT-A kit [https://www.takarabio.com/learning-centers/next-generation-sequencing/technical-notes/reproductive-health-technologies/embgenix-pgt-a]
- 124. Multi-omics PGT: re-evaluation of euploid blastocysts for implantation potential based on RNA sequencing - PubMed [https://pubmed.ncbi.nlm.nih.gov/39413437/]
- 125. Frontiers | Update on the Epigenomic Implication of Embryo... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.881550/full]
- 126. Integrated multi - omics reveal epigenomic disturbance of assisted... [https://pubmed.ncbi.nlm.nih.gov/33099088/]
- 127. Comprehensive multi - omics analysis uncovers potential risks of aged... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-025-02379-5]
- 128. The 'omics' revolution: Use of genomic, transcriptomic, proteomic and metabolomic tools to predict male reproductive traits that impact fertility in livestock and poultry - PubMed [https://pubmed.ncbi.nlm.nih.gov/32482486/]
- 129. Emerging technologies for improving embryo selection: a systematic rev | AHCT [https://www.dovepress.com/emerging-technologies-for-improving-embryo-selection-a-systematic-revi-peer-reviewed-fulltext-article-AHCT]
- 130. Study evaluates which embryo grades predict IVF | Remembryo success [https://www.remembryo.com/study-evaluates-which-embryo-grades-predict-ivf-success/]
- 131. embryo grading: What it means for your fertility treatment | Nucleus IVF [https://mynucleus.com/blog/ivf-embryo-grading]
- 132. Predicting pregnancy outcomes in IVF cycles: a systematic review and diagnostic meta- analysis of artificial intelligence in embryo assessment | Contraception and Reproductive Medicine | Full Text [https://contraceptionmedicine.biomedcentral.com/articles/10.1186/s40834-025-00400-4]
- 133. Embryo Metabolism Shows Promise as Non-Invasive IVF Test - EMJ [https://www.emjreviews.com/reproductive-health/news/embryo-metabolism-emerges-as-a-promising-non-invasive-test-for-ivf-success/]
- 134. Frontiers | The quest for metabolic biomarkers of IVF outcomes... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1640807/full]
- 135. and Artificial Intelligence to Improve Omics ( In )... Vitro Fertilization IVF [https://pmc.ncbi.nlm.nih.gov/articles/PMC8143333/]
- 136. Frontiers | Editorial: The integrity of randomized ... clinical trials [https://www.frontiersin.org/journals/research-metrics-and-analytics/articles/10.3389/frma.2025.1588882/full]
- 137. CONSORT statement: updated guideline for reporting... [https://pubmed.ncbi.nlm.nih.gov/40228833/]
- 138. Frontiers | A comprehensive review of methodologies and application to use the real-world data and analytics platform TriNetX [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1516126/full]
- 139. MedCD: A Medical Clinical | IEEE DataPort Dataset [https://ieee-dataport.org/documents/medcd-medical-clinical-dataset]
- 140. 22 Free and Open Medical Datasets for AI Development in 2025 [https://www.shaip.com/blog/healthcare-datasets-for-machine-learning-projects/]
- 141. Overview of BioASQ : The thirteenth BioASQ challenge on... [https://arxiv.org/html/2508.20554v1]
- 142. Frontiers | Editorial: Exploring ‘ omic ' biomarkers in animal production... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1688780/full]
- 143. Integration of Bioengineered Tools in Assisted Reproductive Technologies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12365630/]
- 144. Fusing Omics and Advanced Cell Models - A New Era for Drug... | ATCC [https://www.atcc.org/resources/webinars/2025-webinars/fusing-omics-and-advanced-cell-models---a-new-era-for-drug-discovery-and-reproducibility]