DNA Methylation Heterogeneity in the Tumor Microenvironment: Drivers, Detection, and Clinical Translation
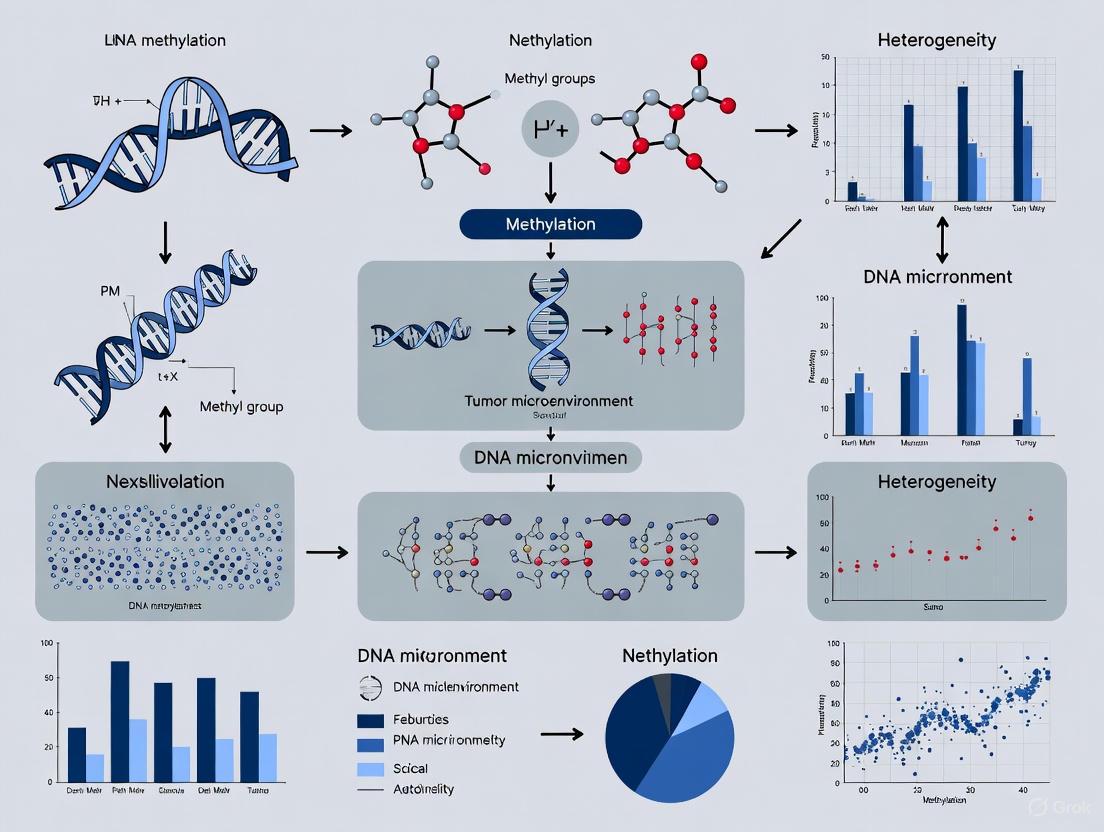
This article comprehensively explores the critical role of DNA methylation heterogeneity (DNAmeH) within the tumor microenvironment (TME), a key driver of tumor progression, immune evasion, and therapeutic resistance. We examine the foundational sources of intratumoral and intertumoral epigenetic variation, from diverse cell compositions to allele-specific methylation. The review details advanced methodologies for quantifying DNAmeH, including bisulfite sequencing, microarrays, and machine learning, and discusses their application in developing predictive biomarkers for cancer diagnosis and prognosis. Furthermore, we address the challenges in data interpretation and clinical integration, presenting optimization strategies and validation frameworks. By synthesizing insights from single-cell analyses to pan-cancer studies, this work provides a roadmap for leveraging DNAmeH to refine cancer diagnostics and develop novel epigenetic therapies, ultimately advancing the field of precision oncology.
DNA Methylation Heterogeneity in the Tumor Microenvironment: Drivers, Detection, and Clinical Translation
Abstract
This article comprehensively explores the critical role of DNA methylation heterogeneity (DNAmeH) within the tumor microenvironment (TME), a key driver of tumor progression, immune evasion, and therapeutic resistance. We examine the foundational sources of intratumoral and intertumoral epigenetic variation, from diverse cell compositions to allele-specific methylation. The review details advanced methodologies for quantifying DNAmeH, including bisulfite sequencing, microarrays, and machine learning, and discusses their application in developing predictive biomarkers for cancer diagnosis and prognosis. Furthermore, we address the challenges in data interpretation and clinical integration, presenting optimization strategies and validation frameworks. By synthesizing insights from single-cell analyses to pan-cancer studies, this work provides a roadmap for leveraging DNAmeH to refine cancer diagnostics and develop novel epigenetic therapies, ultimately advancing the field of precision oncology.
Unraveling the Sources and Significance of Epigenetic Diversity in Tumors
The Tumor Microenvironment (TME) represents a complex and dynamic ecosystem that surrounds cancer cells, playing a pivotal role in tumor initiation, progression, metastasis, and treatment response. Comprising diverse cellular and non-cellular components, the TME consists of malignant cells, stromal cells, immune cells, blood vessels, extracellular matrix (ECM) components, and soluble factors such as growth factors and cytokines [1]. These components engage in continuous crosstalk, creating a network of interactions that can either suppress or promote tumor development. The TME is not merely a passive bystander but actively contributes to the malignant phenotype by offering a favorable niche for cancer cell survival, proliferation, and dissemination [1]. Understanding the intricate architecture and cellular origins within the TME has become paramount in cancer research, particularly with the growing recognition of its influence on therapeutic resistance and immune evasion mechanisms.
Within the context of modern cancer biology, the TME framework provides essential insights for developing novel therapeutic strategies. The immunosuppressive nature of the TME, mediated through immune checkpoint molecules (like PD-L1/PD-1), cytokines (such as TGF-β and IL-10), and specific immune cells (including regulatory T-cells and tumor-associated macrophages), inhibits effective anti-tumor immune responses [1]. Furthermore, cancer cells within the TME adapt to extreme conditions like hypoxia, acidic pH, and nutrient deprivation, enhancing their resistance to conventional therapies including radiation, chemotherapy, and targeted treatments [1]. This review explores the cellular origins and diverse components of the TME, with particular emphasis on how DNA methylation heterogeneity serves as both a driver and biomarker of this complexity, offering new avenues for diagnostic and therapeutic innovation.
Cellular Composition of the Tumor Microenvironment
Tumor Cells: The Architects of the TME
Cancer cells constitute the fundamental building blocks of tumors and act as primary architects of the TME. Tumor initiation begins when a single cell undergoes genetic or epigenetic alterations that allow it to evade typical growth regulators like apoptosis and senescence [1]. These transformations often result from mutations in tumor suppressor genes (such as TP53 or BRCA1) or oncogenes (like KRAS or EGFR), leading to uncontrolled cell division and survival [1]. As the tumor expands, cancer cells not only proliferate locally but also actively reshape their surrounding environment by releasing signaling molecules that promote immune evasion, angiogenesis (formation of new blood vessels), and extracellular matrix remodeling [1].
A critical aspect of tumor biology that significantly impacts therapeutic outcomes is tumor heterogeneity, which exists at two distinct levels:
- Inter-tumor heterogeneity: Refers to variations between tumors from different patients, even within the same cancer type. These differences influence prognosis and therapeutic response, underscoring the necessity for personalized treatment approaches.
- Intra-tumor heterogeneity: Describes the genetic, epigenetic, and phenotypic diversity among cancer cells within a single tumor. This heterogeneity arises through clonal evolution, where subpopulations of cancer cells acquire unique mutations that provide competitive advantages [1].
The interactions between tumor cells and their surrounding TME further amplify this heterogeneity, creating a complex landscape where different cellular subpopulations may exhibit varying responses to the same treatment, ultimately contributing to therapy failure and disease relapse [1].
Stromal Cells: The Supportive Framework
Stromal cells provide essential structural and functional support within the TME, contributing significantly to tumor growth and dissemination.
- Cancer-Associated Fibroblasts (CAFs): As the most abundant stromal cells in the TME, CAFs influence cancer cell invasion, migration, and treatment resistance by secreting soluble molecules and extracellular matrix (ECM) proteins [1]. They represent activated fibroblasts that have been co-opted by cancer cells to support tumorigenic processes.
- Mesenchymal Stem Cells (MSCs): These pluripotent cells are recruited to tumors where they differentiate into various cell types, including CAFs, and secrete growth factors and cytokines that promote tumor growth [1].
- Endothelial Cells: These cells form the lining of blood vessels and play vital roles in angiogenesis, the process of new blood vessel formation that provides essential oxygen and nutrients to growing tumors, enabling their expansion and metastatic spread [1].
Immune Cells: The Dual-Natured Components
The immune compartment within the TME exhibits remarkable complexity and functional ambivalence, capable of either suppressing or promoting tumor progression.
Table 1: Key Immune Cells in the Tumor Microenvironment
| Immune Cell Type | Primary Functions in TME | Pro-tumor Activities | Anti-tumor Activities |
|---|---|---|---|
| Tumor-Associated Macrophages (TAMs) | ECM remodeling, cytokine secretion | M2 polarization: promotes angiogenesis, immune suppression [1] | M1 polarization: promotes inflammation, anti-tumor immunity [2] |
| Regulatory T-cells (Tregs) | Immune regulation | Suppresses effector immune cells, enables immune evasion [1] | - |
| CD8+ T-cells | Cytotoxic activity | - | Recognizes tumor antigens, releases IFN-γ and granzyme B [2] |
| CD4+ T-cells | Immune cell activation | - | Releases IL-2, IL-4, IL-17 to activate other immune cells [2] |
| Natural Killer (NK) Cells | Immune surveillance | - | Targets tumor cells for destruction, produces IFN-γ [2] |
| Myeloid-Derived Suppressor Cells (MDSCs) | Immune suppression | Inhibits T-cell function, promotes immune tolerance [1] | - |
| Neutrophils | Inflammation, tissue remodeling | Secretes VEGFA and MMP9 to promote angiogenesis and invasion [2] | - |
The dynamic and often immunosuppressive nature of the TME represents a major challenge for cancer therapy. The presence of immunosuppressive cells like Tregs and MDSCs, combined with the expression of immune checkpoint molecules, creates a barrier to effective anti-tumor immunity [1]. Understanding these cellular interactions provides the foundation for developing innovative immunotherapies that can reprogram the TME to favor tumor elimination.
DNA Methylation Heterogeneity as a Central Regulator
Fundamentals of DNA Methylation in Cancer
DNA methylation, specifically 5-Methylcytosine (5mC), represents the most prevalent DNA methylation modification in the human genome, and its abnormal patterns are strongly associated with tumor progression [3]. This epigenetic mechanism involves the addition of a methyl group to cytosine bases in CpG dinucleotides, resulting in altered gene expression without changing the underlying DNA sequence. In normal cells, approximately 60-80% of CpG sites in the human genome are methylated, maintaining transcriptional stability and cellular identity [4]. However, cancer cells exhibit widespread disruption of DNA methylation patterns, characterized by global hypomethylation (leading to genomic instability) and localized hypermethylation of tumor suppressor gene promoters (silencing their expression) [3].
The emergence of DNA methylation heterogeneity (DNAmeH) within tumors represents a crucial aspect of cancer evolution. Intratumoral and intertumoral DNAmeH primarily arises from cancer epigenome heterogeneity and the diverse cell compositions within the TME [3]. While methylation at a single CpG site in an individual cell is typically binary (either fully methylated or unmethylated), bulk tumor tissue analysis often reveals intermediate methylation signals. This intermediate methylation (approximately 2% of the 26.9 million CpG sites in the human genome) reflects the heterogeneous mixture of different cell types within the tumor immune microenvironment [4]. The coexistence of cells with distinct methylation patterns in tumor tissues creates this mosaic of methylation states, serving as a molecular fingerprint of the TME's cellular complexity.
Quantitative Assessment of DNA Methylation Heterogeneity
Advancements in high-throughput sequencing and microarray technologies have facilitated the development of robust quantitative methods for measuring DNAmeH [3]. These approaches enable researchers to dissect the epigenetic landscape of tumors with unprecedented resolution.
Table 2: Methods for Quantifying DNA Methylation Heterogeneity
| Method | Principle | Application in TME Research |
|---|---|---|
| PIM (Proportion of sites with Intermediate Methylation) | Calculates the proportion of CpG sites with β-values between 0.2-0.6 across the genome [4] | Measures intertumoral DNA methylation heterogeneity; higher PIM reflects stronger heterogeneity and immune cell infiltration [4] |
| PDR (Proportion of Discordant Reads) | Captures the methylation status of individual CpG sites in different cells from sequencing data [4] | Analyzes DNA methylation heterogeneity within samples at single-molecule resolution |
| Epiallele Analysis | Identifies and quantifies distinct epigenetic alleles in a cell population [4] | Facilitates analysis of DNA methylation heterogeneity within samples |
| CMHC (Cell-type-associated DNA Methylation Heterogeneity Contribution) | Dissects the effect of different immune cell types on β-values of cell-type-associated heterogeneous CpG sites (CpGct) [4] | Quantifies contribution of specific immune cell types to overall methylation heterogeneity |
| Shannon Entropy-Based Method | Quantifies methylation differences using Shannon entropy to identify cell type-specific methylation sites [2] | Identifies informative methylation sites for deconvolution algorithms; higher entropy indicates more informative sites |
The PIM score, calculated as PIM = numCpGinter/N (where numCpGinter represents the number of CpG sites with β-values from 0.2 to 0.6, and N represents the total number of genome-wide CpG sites for each patient), has emerged as a particularly valuable metric [4]. A higher PIM score indicates greater enrichment of intermediate methylation sites in tumor tissue, reflecting stronger DNA methylation heterogeneity. This measure has demonstrated clinical relevance across various cancer types, including glioma, where enhanced DNA methylation heterogeneity associates with stronger immune cell infiltration, better survival rates, and slower tumor progression [4].
Methodologies for Deconvoluting TME Cellular Composition
Reference-Based Deconvolution Using DNA Methylation Data
Deconvolution algorithms mathematically dissect bulk tumor methylation data into its constituent cellular components by leveraging reference methylation profiles of purified cell types. The fundamental principle assumes that DNA methylation data from tissues represent a convolution of cell type-specific methylation patterns and the proportions of different cell types [2]. The process can be represented as:
Bulk Tissue Methylation = Σ(Cell Type Proportion × Cell Type-Specific Methylation) + Error
The experimental workflow for deconvolution typically involves:
- Reference Database Construction: Collecting DNA methylation profiles of purified immune cells from public repositories like GEO (e.g., GSE35069), encompassing various immune cell types including CD4+ T cells, CD8+ T cells, CD56+ NK cells, CD19+ B cells, CD14+ monocytes, neutrophils, and eosinophils [2].
- Feature Selection: Identifying informative CpG sites that show maximal variation between cell types using methods like Shannon entropy-based selection [2].
- Algorithm Application: Employing mathematical deconvolution approaches to estimate cell type proportions in bulk tumor samples using the reference matrix and selected features.
Deconvolution Workflow for TME Cellular Composition
Experimental Protocols for DNA Methylation Analysis in TME Studies
Protocol 1: Pan-Cancer Immune Heterogeneity Analysis Based on DNA Methylation
This protocol outlines the methodology for large-scale analysis of TME composition across multiple cancer types [2]:
Data Collection and Preprocessing:
- Obtain DNA methylation profiles, gene expression data, and clinical data from TCGA (14 cancer types, 5323 tumor samples).
- Acquire immune cell methylation references from GEO (GSE35069 for 7 immune cell types).
- Map chip probe locations to specific gene sites and average methylation values for identical gene sites.
Cell Type-Specific Methylation Gene Selection:
- Apply Shannon entropy-based method (QDMR software) to identify specific methylation sites.
- Calculate Shannon entropy value (H₀ = -Σps/r log₂ps/r) for each gene site across 7 immune cell types.
- Select top 1256 specific methylation sites based on entropy values for deconvolution input.
Pan-Cancer Tissue Deconvolution:
- Utilize deconvolution algorithm to calculate cell subtype proportions in tissue.
- Apply non-negative matrix factorization (NMF) clustering to identify tumor immune microenvironment subtypes.
- Validate results with phenotypic data (survival, tumor stage) and gene expression correlations.
Protocol 2: Glioma DNA Methylation Heterogeneity and Immune Microenvironment Analysis
This specialized protocol focuses on glioma TME characterization [4]:
Tumor Immune Microenvironment Subtyping:
- Calculate single-sample gene set enrichment scores (ssGSEA) for 34 cell types using R package gsva.
- Perform NMF clustering with k=3-8, repeated 50 times, selecting optimal k based on coupling coefficient.
- Group patients into three tumor immune microenvironmental subtypes (NMF-1, NMF-2, NMF-3).
DNA Methylation Heterogeneity Evaluation:
- Calculate PIM scores using β-value range 0.2-0.6.
- Correlate PIM scores with clinical parameters and survival outcomes.
Cell-type-associated Heterogeneity Analysis:
- Identify cell-type-associated heterogeneous CpG sites (CpGct) for 6 immune cell types.
- Construct CMHC score to quantify immune cell type impact on CpGct β-values.
- Develop Cell-type-associated DNA Methylation Heterogeneity Risk (CMHR) score using 8 prognosis-related CpGct.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful investigation of cellular origins and TME components requires carefully selected reagents and methodologies. The following table outlines essential resources for conducting TME DNA methylation studies.
Table 3: Research Reagent Solutions for TME DNA Methylation Studies
| Reagent/Material | Function | Example Specifications |
|---|---|---|
| Illumina Methylation BeadChip | Genome-wide methylation profiling | HumanMethylation450K or EPIC array covering >850,000 CpG sites [4] [2] |
| DNA Bisulfite Conversion Kit | Converts unmethylated cytosines to uracils for methylation detection | High-efficiency conversion (>99%) with minimal DNA degradation [4] |
| Purified Immune Cell Populations | Reference profiles for deconvolution algorithms | CD4+ T cells, CD8+ T cells, CD56+ NK cells, CD19+ B cells, CD14+ monocytes, neutrophils from healthy donors [2] |
| QDMR Software | Identifies specific methylation sites using Shannon entropy | Version 1.0; quantifies methylation differences for feature selection [2] |
| Deconvolution Algorithm Package | Mathematical decomposition of bulk tissue methylation | R-based implementation supporting non-negative matrix factorization [4] [2] |
| ssGSEA Software | Calculates single-sample gene set enrichment scores | R package gsva with method = 'ssgsea' for immune cell infiltration estimation [4] |
| 3,5-Dibromopyridine-d3 | 3,5-Dibromopyridine-d3, CAS:1219799-05-9, MF:C5H3Br2N, MW:239.91 g/mol | Chemical Reagent |
| Rufinamide-15N,d2 | Rufinamide-15N,d2 Stable-Labeled Isotope | Rufinamide-15N,d2 internal standard for epilepsy research. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Clinical Implications and Translational Applications
The analysis of cellular heterogeneity within the TME through DNA methylation profiling carries significant clinical implications across multiple domains of cancer management. In diagnostic applications, DNA methylation signatures serve as powerful tools for tumor classification and subtyping. For instance, in glioma, the Cell-type-associated DNA Methylation Heterogeneity Risk (CMHR) score demonstrates remarkable predictive performance for IDH status (AUC = 0.96) and glioma histological phenotype (AUC = 0.81) [4]. Such precision in molecular classification exceeds conventional histopathological examination and enables more accurate diagnosis.
In the realm of prognostic assessment, DNA methylation heterogeneity provides valuable insights into disease trajectory. The PIM score, reflecting DNA methylation heterogeneity, shows distinct correlations with patient survival outcomes. Counterintuitively, in glioma patients, enhanced DNA methylation heterogeneity associates with stronger immune cell infiltration, better survival rates, and slower tumor progression [4]. This relationship highlights the complex interplay between tumor epigenetics, immune response, and clinical outcomes, challenging simplistic interpretations of heterogeneity as purely detrimental.
For therapeutic decision-making, TME deconvolution offers guidance for treatment selection and response prediction. The identification of specific immune cell populations within the TME helps identify patients most likely to benefit from immunotherapies, such as those with high cytotoxic T-lymphocyte infiltration [4]. Additionally, DNA methylation alterations of prognosis-related CpGct sites may be associated with responses to specific drug treatments in glioma patients, including Temozolomide, Bevacizumab, and radiation therapy [4]. This emerging approach enables a more personalized treatment strategy based on the unique cellular and molecular composition of each patient's TME.
The potential for therapy resistance monitoring represents another critical application. Tumor heterogeneity, reflected in DNA methylation patterns, contributes significantly to treatment resistance and disease relapse [1]. Different cellular subpopulations within the TME may exhibit varying sensitivities to therapeutic agents, leading to selective pressure and expansion of resistant clones. Longitudinal monitoring of DNA methylation heterogeneity could therefore provide early indicators of emerging resistance, allowing for timely intervention and regimen modification.
Future Directions and Concluding Perspectives
The investigation of cellular origins within the TME through the lens of DNA methylation heterogeneity represents a rapidly advancing frontier in cancer biology. Future research directions will likely focus on several key areas, including the integration of multi-omics approaches that combine DNA methylation data with transcriptomic, proteomic, and metabolomic profiles to achieve a more comprehensive understanding of TME dynamics [3]. The development of single-cell methylation sequencing technologies promises to revolutionize this field by enabling direct observation of epigenetic heterogeneity without the limitations of deconvolution algorithms, providing unprecedented resolution of the cellular landscape within tumors [3].
Technical advancements in spatial methylation profiling will further enhance our understanding by preserving the architectural context of cellular interactions within the TME. The translation of methylation-based TME classification into clinically applicable biomarkers requires rigorous validation across diverse patient populations and cancer types [2]. Additionally, the exploration of epigenetic therapies that specifically target the dysregulated methylation patterns in cancer cells and TME components offers promising therapeutic avenues [3]. Such approaches might include demethylating agents that reverse immunosuppressive epigenetic programming or compounds that selectively modulate methylation in specific cellular compartments of the TME.
In conclusion, the cellular origins and diverse components of the TME create a complex ecosystem that significantly influences tumor behavior and treatment response. DNA methylation heterogeneity serves as both a driver and biomarker of this complexity, providing valuable insights into tumor classification, prognosis, and therapeutic targeting. The methodologies for deconvoluting TME composition using DNA methylation data, as detailed in this review, empower researchers and clinicians to dissect this complexity with increasing precision. As these approaches continue to evolve and integrate with other technological advancements, they hold tremendous promise for advancing personalized cancer medicine and improving patient outcomes through more precise diagnostic stratification and targeted therapeutic intervention.
The complex orchestration of oncogenesis involves a dynamic interplay between genetic alterations and epigenetic modifications, creating a sophisticated regulatory network that drives tumor development and progression. DNA methylation heterogeneity (DNAmeH) has emerged as a critical mediator in this cross-talk, serving as a molecular bridge that translates genetic instability into diverse and plastic cellular states within the tumor microenvironment (TME) [3]. This heterogeneity arises from both cancer epigenome heterogeneity and the diverse cell compositions within the TME, forming a complex landscape that influences therapeutic response and clinical outcomes [3]. The convergence of mutational burden, copy number variations (CNVs), and cellular stemness represents a particularly crucial axis in this network, contributing to the adaptive capabilities of tumors and posing significant challenges for effective cancer management. Understanding these interconnected relationships provides valuable insights for developing novel diagnostic and therapeutic strategies that can address the dynamic nature of malignant progression.
Theoretical Framework: Mechanisms of Genetic-Epigenetic Integration
Mutational Burden and Epigenetic Consequences
Tumor mutational burden (TMB) represents a key genetic feature that significantly influences epigenetic states. Research across multiple cancer types has demonstrated that elevated TMB correlates with increased DNA methylation heterogeneity, suggesting a coordinated relationship between genetic instability and epigenetic diversity [3]. This relationship may be mediated through several mechanisms, including mutations in genes encoding epigenetic regulators and broader disruptions to chromatin organization. The resulting epigenetic heterogeneity contributes to phenotypic diversity within tumor populations, enhancing their adaptive potential.
In stomach adenocarcinoma (STAD), comprehensive bioinformatics analyses have revealed significant associations between cancer cell stemness, gene mutations, and the immune microenvironment [5]. The mutational landscape directly influences the stemness properties of cancer cells, quantified through the mRNA expression-based stemness index (mRNAsi), with higher stemness indices correlating with greater tumor dedifferentiation and more aggressive clinical behavior [5]. This relationship underscores how genetic alterations can establish epigenetic and cellular states that favor tumor progression.
Copy Number Variations as Epigenetic Modulators
Copy number variations (CNVs) serve as another genetic element that significantly impacts epigenetic regulation. CNVs can alter the dosage of genes involved in epigenetic processes, including DNA methyltransferases, demethylases, and chromatin modifiers, thereby creating widespread changes in the epigenomic landscape [3]. Studies have identified CNVs as a significant factor influencing DNAmeH, with specific amplifications or deletions correlating with distinct methylation patterns that contribute to tumor evolution [3].
The functional consequences of CNV-driven epigenetic changes are particularly evident in their effect on cellular stemness. In clear cell renal cell carcinoma (ccRCC), CNV patterns contribute to the establishment of distinct molecular subtypes with varying stemness characteristics [6]. These subtypes, designated as CRCS1 and CRCS2, demonstrate differential clinical behaviors, with the CRCS2 subtype associated with lower clinical stage/grading and better prognosis, highlighting the clinical relevance of these genetic-epigenetic interactions [6].
Signaling Pathways Governing Stemness Plasticity
The maintenance and regulation of cancer stemness involve multiple interconnected signaling pathways that respond to both genetic and epigenetic cues. Key developmental pathways, including Notch, WNT, Hedgehog (HH), and Hippo, play crucial roles in governing the stem-like qualities of tumor cells [6]. These pathways integrate signals from the TME and genetic alterations to establish and maintain stem cell states through epigenetic mechanisms.
Table 1: Key Signaling Pathways in Cancer Stemness Regulation
| Pathway | Core Components | Epigenetic Effects | Therapeutic Targeting |
|---|---|---|---|
| Notch | Notch receptors, CSL transcription factor | Histone modification, DNA methylation changes | γ-secretase inhibitors (in clinical trials) |
| WNT | β-catenin, TCF/LEF factors | Chromatin remodeling, DNA methylation | PORCN inhibitors, tankyrase inhibitors |
| Hedgehog | Patched, Smoothened, GLI factors | DNA methylation of target genes | Smoothened inhibitors (e.g., vismodegib) |
| Hippo | YAP, TAZ, TEAD factors | Histone acetylation, DNA methylation | YAP/TAZ-TEAD interaction inhibitors |
| mTORC1 | mTOR, Raptor | Metabolic regulation of epigenetics | mTOR inhibitors (e.g., rapalogs) |
Crosstalk between additional pathways, including NF-κB, MAPK, PI3K, and EGFR, further modulates stemness characteristics, creating a complex regulatory network that responds to genetic and environmental cues [6]. This network provides multiple nodes for therapeutic intervention, particularly when combined with inhibitors targeting cancer stem cells (CSCs) and immune agents, as explored in clinical trials such as NCT03548571, NCT02541370, and NCT03739606 [6].
Quantitative Assessment: Measuring Heterogeneity and Its Correlates
Metrics for DNA Methylation Heterogeneity
Advancements in high-throughput sequencing technologies have facilitated the development of sophisticated quantitative methods for measuring DNA methylation heterogeneity [3]. These metrics capture different aspects of epigenetic diversity, providing researchers with tools to characterize the epigenetic landscape of tumors comprehensively.
Table 2: Quantitative Metrics for DNA Methylation Heterogeneity
| Metric | Measurement Focus | Technical Approach | Biological Interpretation |
|---|---|---|---|
| Epipolymorphism | Diversity of methylation patterns | Sequencing read analysis | Measures epiallelic richness in cell population |
| Methylation Entropy | Disorder of methylation states | Information theory application | Quantifies epigenetic instability |
| Fraction of Discordant Read Pairs (FDRP) | CpG-level epiallelic diversity | Read pair analysis | Assesses local methylation heterogeneity |
| Quantitative FDRP (qFDRP) | Magnitude of methylation differences | Quantitative read analysis | Enhanced resolution of heterogeneity |
| Proportion of Discordant Reads (PDR) | Local methylation homogeneity | Single-read methylation state analysis | Measures cell-to-cell consistency |
| Methylation Haplotype Load (MHL) | Conservation of methylated haplotypes | Long-range methylation pattern analysis | Evaluates epigenetic signature stability |
| Local Pairwise Methylation Discordance (LPMD) | CpG pair discordance at fixed distances | Pairwise comparison within reads | Reduces read length bias in heterogeneity assessment |
Computational tools such as Metheor have dramatically improved the efficiency of calculating these heterogeneity measures, reducing execution time by up to 300-fold and memory footprint by up to 60-fold compared to previous implementations [7]. This computational advancement enables large-scale studies of DNA methylation heterogeneity profiles, facilitating the analysis of hundreds of cancer cell lines from resources like the Cancer Cell Line Encyclopedia (CCLE) [7].
Correlates of Methylation Heterogeneity in Cancer
Quantitative analyses across multiple cancer types have revealed consistent relationships between DNA methylation heterogeneity and various molecular and clinical features. In pancreatic ductal adenocarcinoma (PDAC), unsupervised clustering of methylation profiles identified two major groups with distinct characteristics [8]. Group 2 exhibited higher tumor purity and a significantly greater frequency of KRAS mutations compared to Group 1 (90.3% vs. 37.5%, p < 0.0001) [8]. This group also demonstrated worse overall survival outcomes (64.2% vs. 42.5% mortality, p = 0.0046), establishing a clear link between specific methylation patterns, genetic alterations, and clinical prognosis [8].
Similar analyses in stomach adenocarcinoma have revealed that stemness indices significantly correlate with tumor mutation burden and immune microenvironment composition [5]. These relationships enable the construction of prognostic models that integrate genetic and epigenetic features to predict patient outcomes and potential therapeutic responses.
Analytical Methodologies: Experimental and Computational Approaches
DNA Methylation Profiling Techniques
Comprehensive assessment of DNA methylation heterogeneity relies on robust experimental methodologies for generating high-quality methylation data. The Illumina Infinium Methylation EPIC BeadChip platform provides extensive genome-wide coverage of CpG sites, particularly focused on promoter-associated regions and enhancers [9]. This technology enables reproducible quantification of methylation levels across large sample sets, making it suitable for population-level studies in cancer research.
For sequencing-based approaches, bisulfite treatment of DNA followed by next-generation sequencing (bisulfite sequencing) remains the gold standard for basepair-resolution methylation analysis [7]. Both whole-genome bisulfite sequencing and reduced representation bisulfite sequencing (RRBS) approaches provide phased methylation information, capturing the co-occurrence of methylation states on individual DNA molecules, which is essential for heterogeneity quantification [7].
DNA Methylation Analysis Workflow
Computational Deconvolution of Tumor Microenvironment
A critical challenge in tumor epigenomics involves disentangling the contributions of various cellular components within the tumor microenvironment. Hierarchical deconvolution of DNA methylation data has emerged as a powerful method for inferring immune and stromal cell abundances in bulk tumor tissues, leveraging the stability and cell lineage specificity of methylation marks [8]. This approach enables researchers to stratify tumors based on their immune microenvironment composition, identifying distinct subtypes such as hypo-inflamed (immune-deserted), myeloid-enriched, and lymphoid-enriched microenvironments [8].
In pancreatic cancer, this deconvolution approach has revealed three distinct TME subtypes with varying cellular compositions and clinical implications [8]. These computational findings are further supported by gene co-expression modules identified through weighted gene co-expression network analysis (WGCNA), which show enrichment in immune regulatory and signaling pathways [8].
Stemness Quantification and Subtype Classification
The quantification of cellular stemness represents another critical methodological approach in understanding genetic-epigenetic cross-talk. The mRNA expression-based stemness index (mRNAsi) quantifies stemness using gene expression patterns, with values ranging from 0-1, where values closer to 1 indicate stronger stemness characteristics [5]. This index correlates with tumor dedifferentiation and is reflected in histopathological grades [5].
Genetic-Epigenetic Cross-talk Network
Unsupervised clustering algorithms applied to multi-omics data enable the identification of molecular subtypes with distinct stemness characteristics. In ccRCC, this approach has identified CRCS1 and CRCS2 subtypes, which demonstrate differential clinical behaviors, immune microenvironments, and drug sensitivities [6]. The CRCS2 subtype, associated with better prognosis, exhibits a hypoxic state characterized by suppression and exclusion of immune function, and shows sensitivity to specific therapeutic agents including gefitinib, erlotinib, and saracatinib [6].
Research Reagent Solutions: Essential Tools for Investigation
Table 3: Essential Research Reagents and Resources
| Category | Specific Product/Resource | Application | Key Features |
|---|---|---|---|
| Methylation Arrays | Illumina Infinium Methylation EPIC BeadChip | Genome-wide methylation profiling | 850,000 CpG sites, FFPE compatible |
| Bisulfite Conversion Kits | EZ DNA Methylation Kit (Zymo Research) | DNA treatment for bisulfite sequencing | High conversion efficiency, DNA protection |
| DNA Extraction Kits | QIAamp DNA FFPE Tissue Kit (Qiagen) | Nucleic acid isolation from archived samples | Effective paraffin removal, inhibitor reduction |
| Bioinformatics Tools | Metheor toolkit | Methylation heterogeneity calculation | Ultrafast computation, multiple metrics |
| Data Resources | TCGA Pan-Cancer Atlas | Multi-omics reference dataset | Clinical, genomic, epigenomic data integration |
| Stemness Analysis | StemChecker webserver | Stemness signature identification | 26 curated stemness signatures |
| Cell Line Resources | Cancer Cell Line Encyclopedia (CCLE) | Pre-clinical model systems | Multi-omics data for 928 cell lines |
| Deconvolution Algorithms | CIBERSORT, TIMER, ESTIMATE | TME composition inference | Cell-type abundance estimation |
Clinical Implications and Translational Applications
Prognostic Biomarkers and Patient Stratification
The integration of genetic and epigenetic features has powerful implications for cancer prognosis and patient stratification. In clear cell renal cell carcinoma, the development of a multi-omics prognostic model capturing tumor stemness has demonstrated significant value in predicting patient outcomes [6]. This model performed well in both training and validation cohorts, helping identify patients who may benefit from specific treatments or who are at risk of recurrence and drug resistance [6].
Similarly, in pancreatic ductal adenocarcinoma, DNA methylation profiling has identified distinct epigenetic subgroups with significant survival differences [9]. The T2 methylation profile, associated with poorly differentiated morphology and squamous features, demonstrates significantly shorter disease-free survival compared to the T1 profile (p = 0.04) [9]. These profiles also show differential methylation patterns in transcription regulation genes and upregulation of DNA repair and MYC target pathways, providing mechanistic insights into their aggressive behavior [9].
Therapeutic Implications and Biomarker Development
Understanding the cross-talk between genetic and epigenetic factors enables more targeted therapeutic approaches. Cancer stem-like cells represent a particularly important therapeutic target due to their association with therapy resistance, metastatic behavior, and self-renewal capacity [6]. Novel therapeutic targets such as SAA2, which regulates neutrophil and fibroblast infiltration in ccRCC, have been identified through stemness-focused analyses [6].
The stratification of tumors based on their immune microenvironment composition, derived from DNA methylation deconvolution, provides valuable insights for immunotherapy applications [8]. Myeloid-enriched versus lymphoid-enriched microenvironments may respond differently to various immunotherapeutic approaches, enabling more precise treatment matching [8].
The intricate cross-talk between genetic alterations, including mutational burden and CNVs, and epigenetic states manifested through DNA methylation heterogeneity creates a complex regulatory network that fundamentally shapes tumor behavior and therapeutic response. Cellular stemness serves as both a mediator and consequence of these interactions, contributing to the dynamic plasticity observed in cancer progression. Advanced analytical methodologies now enable researchers to quantify these relationships with unprecedented resolution, providing insights that span from molecular mechanisms to clinical applications. The continuing refinement of these approaches, coupled with the development of innovative computational tools and experimental techniques, promises to further elucidate these relationships and translate them into improved diagnostic and therapeutic strategies for cancer patients.
The regulation of gene expression is a complex process orchestrated by numerous cis-regulatory elements, among which super-enhancers (SEs) have emerged as master regulators of cell identity and disease pathogenesis. These specialized epigenetic structures function as powerful transcriptional hubs that drive the expression of genes critical for cell fate determination, including those involved in oncogenesis and tumor suppression. Within the tumor microenvironment (TME), the interplay between SE activity and DNA methylation heterogeneity creates a dynamic regulatory landscape that significantly influences tumor evolution, therapeutic resistance, and clinical outcomes. SEs are large clusters of enhancer elements that span several kilobases of genomic DNA and are characterized by their dense enrichment of transcription factors (TFs), coactivators, and specific histone modifications [10] [11]. Unlike typical enhancers, SEs exhibit exceptionally strong transcriptional activation potential and demonstrate high cell-type specificity, making them pivotal regulators of genes that define cellular identity [12] [13]. In cancer, particularly pancreatic ductal adenocarcinoma (PDAC), the transcriptional programs governed by SEs often become subverted to maintain oncogenic states, while simultaneously, the DNA methylation patterns within these regulatory domains contribute to tumor heterogeneity and adaptation [8] [9]. This review examines the intricate relationship between SE-mediated gene regulation and tumor suppressor mechanisms, with particular emphasis on how DNA methylation heterogeneity within the TME influences these processes and offers new avenues for therapeutic intervention.
Molecular Architecture and Mechanisms of Super-Enhancers
Structural Characteristics and Identification
Super-enhancers possess distinct structural features that differentiate them from typical enhancers and underlie their potent transcriptional activity. SEs are exceptionally large genomic regions, typically spanning 8 to 20 kilobases, compared to the 200-300 base pair range of typical enhancers [12] [13]. This extended architecture comprises multiple constituent enhancers that function cooperatively to amplify transcriptional output. SEs are densely enriched with master transcription factors, coactivators (including the Mediator complex, BRD4, and p300), and chromatin regulators that form a concentrated transcriptional apparatus [10] [11]. These regions also exhibit characteristic epigenetic signatures, including high levels of histone H3 lysine 27 acetylation (H3K27ac) and H3 lysine 4 monomethylation (H3K4me1), which mark actively transcribed enhancers [14] [11].
The identification and validation of SEs rely on integrated genomic approaches, primarily chromatin immunoprecipitation sequencing (ChIP-seq) for histone modifications (H3K27ac) and transcriptional coactivators (MED1, BRD4), complemented by assays for chromatin accessibility such as ATAC-seq and DNase-seq [11]. Bioinformatic algorithms like ROSE rank enhancer regions based on ChIP-seq signal intensity and merge adjacent enhancers within a defined distance (typically 12.5 kb) to define SE domains [11] [15]. The substantial differences in the binding density of regulatory factors between SEs and typical enhancers are visually apparent in ChIP-seq profiles, with SEs exhibiting dramatically higher signal peaks [12].
Three-Dimensional Organization and Phase Separation
Beyond linear genomic organization, SEs function within the three-dimensional (3D) architecture of the genome. They are frequently located within topologically associating domains (TADs)—self-interacting genomic regions bounded by CTCF and cohesin complexes that facilitate enhancer-promoter interactions [12] [11]. Approximately 84% of SEs reside within large CTCF-CTCF loops, compared to only 48% of typical enhancers, highlighting their privileged positioning within the 3D genome [13]. This spatial organization enables SEs to engage in long-range chromatin interactions with their target gene promoters, forming specialized transcriptional hubs.
Recent research has revealed that SEs undergo liquid-liquid phase separation (LLPS), a biophysical process that drives the formation of membraneless condensates enriched with transcriptional machinery [10] [11]. Through the intrinsically disordered regions (IDRs) of transcription factors and coactivators like BRD4 and MED1, SEs form phase-separated condensates that concentrate RNA polymerase II and other transcriptional components, thereby enabling the bursting transcription of SE-driven genes [11]. This phase separation model explains the remarkable transcriptional amplitude and cooperative behavior of SE components, providing a mechanistic basis for their function as specialized regulatory hubs.
Table 1: Key Characteristics of Super-Enhancers Versus Typical Enhancers
| Characteristic | Super-Enhancers | Typical Enhancers |
|---|---|---|
| Genomic size | 8-20 kb | 200-300 bp |
| Transcription factor density | Exceptionally high | Moderate |
| Histone modifications | High H3K27ac, H3K4me1 | Lower H3K27ac, H3K4me1 |
| Sensitivity to perturbation | High | Moderate to low |
| Location in 3D genome | 84% within CTCF loops | 48% within CTCF loops |
| Transcriptional output | Very strong | Moderate |
| Cell type specificity | High | Variable |
Super-Enhancer Dysregulation in Oncogenesis
Mechanisms of Oncogenic SE Activation
The pathological activation of oncogenes through SE reprogramming represents a key mechanism in cancer development. Tumor cells can acquire or form de novo SEs at oncogenic loci through multiple mechanisms, including chromosomal rearrangements, amplification of enhancer regions, and transcription factor dysregulation [16]. In various cancers, somatic mutations and structural variations can create novel SE configurations that drive oncogene expression. For example, in T-cell acute lymphoblastic leukemia (T-ALL), chromosomal rearrangements can lead to the formation of novel SEs that activate the TAL1 oncogene, while in other hematological malignancies, translocations may place powerful enhancers near oncogenes like MYC [10] [16].
The dysregulation of transcription factors represents another prevalent mechanism of oncogenic SE activation. Chimeric transcription factors generated through chromosomal translocations, such as TCF3-HLF in acute lymphoblastic leukemia and ETO2-GLIS2 in acute megakaryocytic leukemia, can hijack SE regulatory networks to drive oncogenic transcriptional programs [16]. Similarly, the aberrant expression or mutation of transcriptional coactivators like CREBBP and p300 can disrupt normal enhancer control, leading to the pathological activation of SE-driven oncogenes in lymphomas and other cancers [16].
SE-Driven Oncogenic Networks in Solid Tumors
In solid tumors, SEs play crucial roles in maintaining oncogenic transcriptional circuits that promote tumor growth and survival. SEs have been identified as key regulators of core oncogenic pathways in various cancers, including glioblastoma, breast cancer, and pancreatic cancer [11] [15]. These regulatory hubs often control master transcription factors that in turn regulate broad transcriptional programs essential for maintaining the malignant state.
The SE-mediated transcriptional addiction of cancer cells creates a therapeutic vulnerability that can be exploited through the inhibition of SE-associated coactivators. For instance, BRD4 inhibitors have shown efficacy in disrupting SE-driven oncogene expression in multiple cancer types, highlighting the functional significance of these regulatory elements in maintaining tumorigenesis [11] [16]. Additionally, SEs can drive the expression of non-coding RNAs, including enhancer RNAs (eRNAs) and long non-coding RNAs (lncRNAs), that further reinforce oncogenic transcriptional programs through feedback mechanisms [11].
Diagram 1: Oncogenic SE Activation Pathways
DNA Methylation Heterogeneity in the Tumor Microenvironment
Patterns and Measurement of DNA Methylation Heterogeneity
DNA methylation heterogeneity (DNAmeH) represents a critical dimension of tumor evolution and adaptation within the complex ecosystem of the TME. In pancreatic ductal adenocarcinoma (PDAC), comprehensive methylation profiling has revealed distinct methylation patterns that correlate with histopathological features and clinical outcomes [9]. Studies employing high-resolution methylation arrays have identified two major methylation profiles in PDAC: T1 profiles that resemble normal pancreatic tissue and are associated with well-differentiated histology, and T2 profiles that significantly diverge from normal tissue and correlate with poorly differentiated morphology and squamous features [9]. The T2 methylation profile is associated with shorter disease-free survival, highlighting the clinical significance of epigenetic heterogeneity.
DNAmeH arises from multiple sources, including cancer epigenome heterogeneity and the diverse cellular compositions within the TME [3]. The development of quantitative methods for measuring DNAmeH has enabled more precise characterization of this heterogeneity and its functional implications. Metrics for assessing DNAmeH consider differences across cancer types, among individual cells, and at allele-specific hemimethylation sites [3]. Factors influencing DNAmeH include the cell cycle phase, tumor mutational burden, cellular stemness, copy number variations, tumor subtypes, hypoxia, and tumor purity [3]. In PDAC, unsupervised hierarchical clustering of differentially methylated positions has revealed distinct subgroups with varying tumor purity and KRAS mutation frequency, with higher purity samples exhibiting significantly different methylation profiles and poorer survival outcomes [8].
Functional Consequences of DNA Methylation Heterogeneity
The heterogeneous nature of DNA methylation within tumors has profound functional consequences that impact gene regulatory networks and therapeutic responses. Differential methylation analysis of PDAC samples has identified substantial hypomethylation of transcription regulation genes in aggressive T2 profiles, alongside hypermethylation events that potentially silence tumor suppressor pathways [9]. Gene set enrichment analyses have further demonstrated the upregulation of DNA repair and MYC target genes in T2 samples, indicating that specific methylation patterns are associated with activated oncogenic pathways [9].
The hierarchical deconvolution of DNA methylation data has enabled researchers to profile the immune composition of the TME and uncover distinct patterns of tumor immune microenvironments [8]. In PDAC, this approach has revealed three major TME subtypes: hypo-inflamed (immune-deserted), myeloid-enriched, and lymphoid-enriched (notably T-cell predominant) microenvironments [8]. These immune clusters, supported by co-expression modules identified through weighted gene co-expression network analysis (WGCNA), reflect the interplay between epigenetic heterogeneity and immune cell infiltration, with significant implications for immunotherapy response and patient stratification.
Table 2: DNA Methylation Heterogeneity Patterns in Pancreatic Cancer
| Methylation Profile | Molecular Features | Histological Correlates | Clinical Outcomes |
|---|---|---|---|
| T1 Profile | Similar to normal tissue, lower KRAS mutation frequency | Well-differentiated morphology | Better survival outcomes |
| T2 Profile | Divergent from normal tissue, high KRAS mutation frequency | Poorly differentiated, squamous features | Shorter disease-free survival |
| Hypo-inflamed TIME | Immune-deserted methylation pattern | Low immune infiltration | Resistance to immunotherapy |
| Myeloid-enriched TIME | Myeloid cell methylation signature | Abundant myeloid cells | Immunosuppressive environment |
| Lymphoid-enriched TIME | T-cell predominant methylation pattern | High T-cell infiltration | Potential response to immunotherapy |
Interplay Between Super-Enhancers and DNA Methylation
Epigenetic Cross-talk in Gene Regulation
The functional relationship between DNA methylation and SE activity represents a critical interface in cancer gene regulation. SEs typically exhibit low levels of DNA methylation, which maintains chromatin accessibility and facilitates transcription factor binding [15]. However, in cancer, SEs frequently display abnormal DNA methylation patterns that can either repress or overexpress target genes. Hypomethylation at SE sites often accompanies oncogene hyperactivation, while hypermethylation can repress tumor suppressor mechanisms [15]. This dynamic regulation involves complex cross-talk between DNA methyltransferases, transcription factors, and histone modifications that collectively determine SE activity.
Research across multiple cancer types has revealed that the expression of SE-driven RNAs and CpG methylation are both pivotal in cancer progression [15]. Analyses of SE-associated CpG dinucleotides have identified distinct clusters of hypermethylation and hypomethylation that correlate with enhancer RNA activation or deactivation. Specifically, hypermethylation is linked to SE deactivation, while hypomethylation is associated with SE activation, highlighting the epigenetic regulation of SEs in cancer progression [15]. This relationship varies across genomic contexts, as observed in embryonic stem cells and epiblast stem cells, where differences in methylation levels correlate with distinct SE activity patterns, particularly at genes regulating pluripotency states [15].
Impact on Tumor Suppressor Networks
The interplay between SEs and DNA methylation extends to the regulation of tumor suppressor networks within the TME. Aberrant DNA methylation at SEs can lead to the silencing of tumor suppressor genes through either direct hypermethylation of SE elements controlling these genes or through hypomethylation-induced activation of SEs that suppress tumor suppressor pathways [15]. In head and neck squamous cell carcinomas and breast cancer, hypermethylated SEs are associated with reduced expression of genes critical for cellular homeostasis, resulting in the overexpression of oncogenic drivers that enhance tumorigenic traits such as proliferation, invasion, and angiogenesis [15].
The integration of SE biology with DNA methylation heterogeneity provides a framework for understanding how tumor cells maintain their identity while adapting to therapeutic pressures. Phylogenetic analyses using multi-sampling datasets have suggested evolutionary trajectories from T1 to T2 methylation profiles that coincide with increasingly aggressive phenotypes and genomic instability [9]. This evolution likely involves the progressive rewiring of SE networks through DNA methylation changes that enable tumor cells to overcome microenvironmental constraints and therapeutic challenges.
Experimental Approaches and Research Methodologies
Core Techniques for SE and DNA Methylation Analysis
The investigation of SEs and DNA methylation heterogeneity relies on integrated multi-omics approaches that combine genomic, epigenomic, and transcriptomic methodologies. Chromatin immunoprecipitation sequencing (ChIP-seq) for histone modifications (H3K27ac, H3K4me1) and transcriptional coactivators (MED1, BRD4) remains the gold standard for SE identification [11]. This technique enables genome-wide mapping of enhancer regions and their classification based on binding density and epigenetic signatures. Complementary approaches include DNase I sequencing (DNase-seq) and assay for transposase-accessible chromatin sequencing (ATAC-seq) for assessing chromatin accessibility, as well as chromosome conformation capture techniques (3C, 4C, Hi-C) for characterizing the 3D architecture of SE-promoter interactions [11].
For DNA methylation analysis, genome-wide profiling techniques such as the Illumina Infinium MethylationEPIC BeadChip and whole-genome bisulfite sequencing provide comprehensive coverage of methylation patterns across the genome [9]. These approaches enable the identification of differentially methylated regions (DMRs) and the quantification of methylation heterogeneity within tumor samples. The deconvolution of bulk methylation data using computational algorithms allows for the inference of cellular composition within the TME, providing insights into the interplay between cancer cells and various stromal and immune components [3] [8].
Integrative Analysis and Functional Validation
Advanced computational methods have been developed to integrate SE and DNA methylation data with transcriptomic profiles, enabling the construction of comprehensive regulatory networks. Weighted gene co-expression network analysis (WGCNA) identifies co-regulated gene modules that can be linked to specific SE activities and methylation patterns [8]. Bioinformatics resources such as SEdb and dbSUPER provide curated databases of SEs across multiple cell types and cancers, facilitating comparative analyses and hypothesis generation [11].
Functional validation of SE elements and methylation-sensitive regulatory regions relies heavily on CRISPR-based genome editing approaches. CRISPR-Cas9-mediated deletion or perturbation of individual SE components enables researchers to assess their necessity for target gene expression and oncogenic phenotypes [10]. Similarly, targeted epigenetic editing using CRISPR-dCas9 systems fused to DNA methyltransferases or demethylases allows for precise manipulation of methylation status at specific SE regions to determine causal relationships with gene expression changes [10] [15]. These functional studies are essential for distinguishing driver epigenetic alterations from passenger events in cancer evolution.
Table 3: Essential Research Reagents and Experimental Tools
| Research Tool | Category | Primary Application | Key Utility |
|---|---|---|---|
| H3K27ac ChIP-seq | Epigenomic profiling | SE identification and mapping | Genome-wide mapping of active enhancers |
| Infinium MethylationEPIC | DNA methylation array | Methylation heterogeneity analysis | Comprehensive CpG coverage across functional regions |
| CRISPR-Cas9/dCas9 | Genome editing | Functional validation | Targeted manipulation of SE elements and methylation |
| ATAC-seq | Chromatin accessibility | Open chromatin mapping | Identification of accessible regulatory regions |
| BET inhibitors (JQ1) | Small molecule inhibitors | SE functional disruption | Pharmacological targeting of BRD4-dependent SEs |
| DNMT inhibitors (AZA) | Epigenetic drugs | DNA methylation modulation | Experimental alteration of methylation patterns |
Diagram 2: Integrated Workflow for SE and DNA Methylation Analysis
Therapeutic Implications and Future Perspectives
Targeting SE Components and DNA Methylation
The intricate relationship between SEs and DNA methylation heterogeneity presents multiple therapeutic opportunities for cancer intervention. SE-directed therapies primarily focus on disrupting the transcriptional machinery concentrated at these regulatory hubs. Small molecule inhibitors targeting key SE components, such as BRD4 bromodomain inhibitors (JQ1, I-BET) and cyclin-dependent kinase 7 (CDK7) inhibitors (THZ1), have demonstrated promising preclinical efficacy across diverse cancer types [10] [16]. These agents preferentially impair SE-driven oncogene transcription, exploiting the transcriptional addiction of cancer cells to specific SE-regulated networks. Additionally, proteolysis-targeting chimeras (PROTACs) designed to degrade SE-associated proteins offer an alternative approach for dismantling pathogenic enhancer complexes [10].
DNA methylation-targeting therapies, particularly DNA methyltransferase inhibitors (azacitidine, decitabine), represent another strategic approach for modulating the epigenetic landscape of cancer cells [15]. While traditionally used for myeloid malignancies, their application in solid tumors is being re-evaluated in combination with other agents, including immunotherapies. The potential of combining SE-directed therapies with DNA methyltransferase inhibitors lies in their complementary mechanisms for resetting dysregulated transcriptional programs, potentially reversing oncogenic SE states while reactivating silenced tumor suppressor genes [15].
Challenges and Future Directions
Despite the promising therapeutic implications, significant challenges remain in translating SE and DNA methylation research into clinical applications. Achieving cell-type specificity in targeting SE components presents a major hurdle, given the fundamental role of these regulatory elements in normal cellular physiology [10]. The dynamic reorganization of SEs in response to therapeutic pressure also necessitates adaptive treatment strategies and combination approaches. Furthermore, the development of effective delivery systems, particularly for crossing biological barriers like the blood-brain barrier in glioblastoma treatment, requires continued innovation [11].
Future research directions will likely focus on advancing single-cell multi-omics technologies to resolve the heterogeneity of SE activities and DNA methylation patterns at cellular resolution within the TME. The integration of artificial intelligence and machine learning approaches for predicting functional epigenetic alterations and modeling their impact on gene regulatory networks holds promise for identifying key dependencies and resistance mechanisms [10] [9]. Additionally, the development of more selective epigenetic modulators and improved delivery platforms will be essential for translating these strategies into clinically viable therapies that can effectively target the epigenetic drivers of cancer while minimizing effects on normal tissue function.
The functional impact of super-enhancers on gene regulation extends far beyond typical enhancer activity, positioning these epigenetic regulatory hubs as master coordinators of oncogenic programs and cell identity. When viewed through the lens of DNA methylation heterogeneity within the tumor microenvironment, the interplay between these regulatory layers reveals complex mechanisms of tumor evolution, adaptation, and therapeutic resistance. The integrated investigation of SE biology and DNA methylation patterns provides not only insights into fundamental cancer mechanisms but also unveils new therapeutic vulnerabilities that can be exploited through targeted epigenetic interventions. As research methodologies continue to advance, enabling more precise mapping and manipulation of these regulatory elements, the translation of these findings into clinical applications promises to enhance precision oncology approaches and improve outcomes for cancer patients.
Advanced Technologies for Mapping and Applying Methylation Landscapes
DNA methylation, the covalent addition of a methyl group to cytosine in CpG dinucleotides, represents a stable epigenetic mark that regulates gene expression without altering the underlying DNA sequence [17]. In oncology, aberrant DNA methylation patterns are now recognized as fundamental drivers of tumorigenesis and play a crucial role in shaping the tumor microenvironment (TME) [3]. The TME constitutes a complex ecosystem comprising malignant cells, immune cells, stromal elements, extracellular matrix, and various signaling molecules that collectively influence tumor progression, therapeutic response, and resistance mechanisms [18]. DNA methylation heterogeneity (DNAmeH) within this microenvironment arises from both cancer epigenome heterogeneity and diverse cell compositions, creating distinct methylation patterns that exhibit intratumoral and intertumoral variations [3].
Understanding this epigenetic landscape requires sophisticated detection technologies capable of mapping methylation patterns with precision and scalability. This technical guide examines three cornerstone technological platforms for DNA methylation analysis: bisulfite sequencing, microarray platforms, and emerging third-generation sequencing methods. Each platform offers distinct advantages in resolution, throughput, cost-effectiveness, and applicability to clinical samples, enabling researchers to decipher the complex epigenetic dialogue within the TME and its implications for cancer diagnosis, prognosis, and therapeutic development.
Technology Platforms: Principles and Methodologies
Bisulfite Sequencing Platforms
Bisulfite sequencing (BS-seq) operates on a fundamental chemical principle: bisulfite conversion selectively deaminates unmethylated cytosines to uracils (which are read as thymines during sequencing), while methylated cytosines remain unchanged [19]. This chemical treatment creates sequence polymorphisms that allow for base-resolution detection of methylation status. Conventional bisulfite sequencing (CBS-seq), despite being considered the gold standard, has historically suffered from significant limitations including severe DNA degradation, incomplete conversion in GC-rich regions, and long treatment durations [19].
Recent methodological advancements have substantially addressed these limitations:
- Ultra-Mild Bisulfite Sequencing (UMBS-seq): This innovative approach utilizes an optimized formulation of ammonium bisulfite with precisely controlled pH to maximize conversion efficiency while minimizing DNA damage. The protocol involves incubation at 55°C for 90 minutes with an alkaline denaturation step and inclusion of DNA protection buffer, resulting in significantly improved DNA preservation, higher library yields, and lower background noise compared to conventional methods [19].
- Targeted Panels: Custom targeted bisulfite sequencing panels (e.g., QIAseq Targeted Methyl Panels) enable focused analysis of specific CpG sites across many samples. This approach offers cost-effectiveness for validating biomarker signatures and analyzing larger sample sets, as demonstrated in ovarian cancer research where a custom panel covering 648 CpG sites provided comparable results to microarray platforms [20].
The bioinformatic analysis of BS-seq data requires specialized tools to account for bisulfite-converted sequences. The BEAT (BS-Seq Epimutation Analysis Toolkit) package implements a Bayesian binomial-beta mixture model that aggregates methylation counts from consecutive cytosines into regions, compensating for low coverage, incomplete conversion, and sequencing errors [21]. This statistical approach calculates posterior methylation probability distributions for robust comparison of DNA methylation between samples.
Microarray Platforms
Methylation microarrays, particularly Illumina's Infinium platforms (EPIC v1/v2), represent the workhorse technology for large-scale epigenome-wide association studies. These arrays utilize probe-based hybridization to quantify methylation levels at predefined genomic loci—850,000 to 930,000 CpG sites depending on the version [20] [17]. The technology relies on bisulfite-converted DNA hybridizing to locus-specific probes attached to beads on the array surface, with differential detection of methylated and unmethylated alleles [17].
The standard analytical workflow for microarray data involves:
- Quality Control: Removal of samples with average detection p-value > 0.05 and probes with detection p-value > 0.01 in any sample [20]
- Normalization: Application of normalization algorithms like functional normalization (preprocessFunnorm in R) to address technical variations [20]
- Filtering: Exclusion of probes affected by common SNPs and cross-reactive probes to enhance data reliability [20]
- Beta Value Calculation: Computation of methylation levels as β = intensitymethylated / (intensitymethylated + intensity_unmethylated + 100), producing values between 0 (completely unmethylated) and 1 (completely methylated) [20]
Microarrays have proven particularly valuable for methylation-based classification of tumor types. In central nervous system tumors, three classifier models—deep learning neural network (NN), k-nearest neighbor (kNN), and random forest (RF)—have been developed using microarray data, demonstrating accuracy above 95% in classifying 91 methylation subclasses [17]. The NN model showed particular robustness in maintaining performance with reduced tumor purity, a common challenge in TME research [17].
Third-Generation Sequencing Platforms
Third-generation sequencing technologies, including Single Molecule Real-Time (SMRT) sequencing and nanopore-based sequencing, offer distinctive capabilities for methylation detection without requiring bisulfite conversion. These platforms detect methylation through alternative mechanisms:
- SMRT Sequencing: Identifies DNA modifications including 5mC by monitoring kinetics of DNA polymerase during real-time sequencing
- Nanopore Sequencing: Detects base modifications including methylation through characteristic alterations in electrical current signals as DNA passes through protein nanopores
These bisulfite-free approaches present significant advantages for TME research by completely avoiding DNA fragmentation issues associated with bisulfite treatment, thereby better preserving molecular integrity, especially crucial for low-input samples like cell-free DNA (cfDNA) and formalin-fixed paraffin-embedded (FFPE) tissues [19]. While enzymatic methyl-sequencing (EM-seq) represents another bisulfite-free alternative that shows improved performance over conventional BS-seq in metrics like mapping efficiency and GC bias, it faces limitations including enzyme instability, complex workflow, and higher costs compared to bisulfite-based methods [19].
Comparative Performance Analysis
Table 1: Technical Comparison of DNA Methylation Detection Platforms
| Parameter | Bisulfite Sequencing | Methylation Microarrays | Third-Generation Sequencing |
|---|---|---|---|
| Resolution | Base-level | Predefined CpG sites (850K-930K) | Base-level (direct detection) |
| Coverage | Genome-wide or targeted | Targeted but comprehensive | Genome-wide |
| Input DNA | Varies by method: UMBS-seq enables low-input (10 pg) [19] | Higher input requirements | Lower input requirements |
| Cost Efficiency | Targeted panels cost-effective for large sample sets [20] | Moderate cost, high throughput | Higher cost, decreasing |
| Throughput | High for targeted panels, lower for WGBS | Very high, parallel processing | Increasing with technological advances |
| DNA Damage | Minimal with UMBS-seq [19] | Moderate (requires bisulfite conversion) | Minimal (no bisulfite conversion) |
| Clinical Utility | Excellent for biomarker validation [20] | Established for tumor classification [17] | Emerging for complex genomic regions |
Table 2: Performance Metrics in Clinical Application Contexts
| Application Context | Optimal Platform | Key Performance Metrics | Considerations for TME Research |
|---|---|---|---|
| Tumor Classification | Microarrays [17] | Accuracy: >95% for CNS tumors [17] | Robust to tumor purity variations (>50%) [17] |
| Biomarker Discovery | Bisulfite Sequencing [20] [19] | High reproducibility across platforms [20] | Enables analysis of low-input samples (cfDNA) [19] |
| TME Deconvolution | Microarrays [8] | Identifies immune subtypes in PDAC [8] | Reveals hypo-inflamed, myeloid-enriched, lymphoid-enriched TME [8] |
| Methylation Heterogeneity | Single-Cell BS-seq [3] | Quantifies intratumoral epigenetic diversity | Requires specialized statistical methods [3] |
The selection of an appropriate methylation detection platform must align with specific research objectives and sample characteristics. For large-scale biomarker screening studies, microarrays offer an optimal balance of throughput, cost, and coverage [20]. When base-resolution methylation data is required across specific genomic regions, particularly for clinical validation studies, targeted bisulfite sequencing provides superior cost-effectiveness for analyzing larger sample sets [20]. For samples with limited DNA quantity or quality, UMBS-seq demonstrates clear advantages with higher library yields and complexity at input levels as low as 10 pg [19].
Comparative studies have demonstrated strong concordance between bisulfite sequencing and microarray platforms. In ovarian cancer research, methylation profiles generated by bisulfite sequencing showed strong sample-wise correlation with Infinium Methylation Array data, particularly in tissue samples (Spearman correlation), though agreement was slightly reduced in cervical swabs likely due to lower DNA quality [20]. Both platforms preserved diagnostic clustering patterns, supporting bisulfite sequencing as a reliable alternative for larger-scale studies [20].
Experimental Design and Protocols
DNA Extraction and Bisulfite Conversion Protocol
Sample Preparation and DNA Extraction:
- Tissue Samples: Use Maxwell RSC Tissue DNA Kit (Promega) with proteinase K digestion overnight at 56°C followed by automated purification [20]
- Cervical Swabs/Biological Fluids: Employ QIAamp DNA Mini kit (QIAGEN) with carrier RNA to enhance recovery of low-concentration DNA [20]
- FFPE Samples: Implement QIAamp DNA FFPE Tissue Kit (QIAGEN) with extended deparaffinization and optimized incubation conditions [9]
- DNA Quantification: Use fluorometric methods (Qubit) rather than spectrophotometry for accurate concentration measurement of bisulfite-converted DNA
Bisulfite Conversion Methods:
- Conventional Protocol: EZ DNA Methylation-Gold Kit (Zymo Research) with recommended thermocycling conditions: 98°C for 10 minutes, 64°C for 2.5 hours, followed by desulphonation [20]
- UMBS-seq Protocol: Optimized formulation of 100 μL of 72% ammonium bisulfite and 1 μL of 20 M KOH, incubation at 55°C for 90 minutes with DNA protection buffer [19]
- Quality Assessment: Validate conversion efficiency using unconverted lambda DNA spike-in controls; target non-CpG cytosine conversion rate >99.5% [19]
Library Preparation and Sequencing
Targeted Bisulfite Sequencing Library Preparation:
- Library Construction: Use QIAseq Targeted Methyl Custom Panel kit (QIAGEN) following manufacturer's instructions with 15-18 PCR cycles [20]
- Quality Control: Assess library concentration with QIAseq Library Quant Assay Kit (QIAGEN) and size distribution with Bioanalyzer High Sensitivity DNA Kit (Agilent) [20]
- Overamplification Rescue: Implement reconditioning of overamplified libraries using GeneRead DNA Library Prep I Kit (QIAGEN) [20]
- Sequencing: Pool libraries in equimolar concentrations, spike with 1-5% PhiX, and sequence on Illumina MiSeq or similar platforms using 300-cycle kits [20]
Microarray Processing Protocol:
- Bisulfite Conversion: Process 500 ng genomic DNA using EZ DNA Methylation Kit (Zymo Research) [9]
- Array Processing: Perform whole-genome amplification, fragmentation, and hybridization to Infinium MethylationEPIC BeadChip per manufacturer protocol [9]
- Scanning: Process arrays using iScan or similar systems with standard settings [20]
- Data Extraction: Process raw IDAT files using R/Bioconductor packages (minfi) with background correction and dye bias correction [20]
Data Analysis Workflows
Bisulfite Sequencing Data Analysis:
- Alignment: Map bisulfite-converted reads to reference genome using dedicated aligners (Bismark, BSMAP) with in silico conversion approach
- Methylation Calling: Extract methylation counts at each cytosine position using binomial statistics
- Regional Analysis: Implement BEAT package for detecting regional epimutations using binomial-beta mixture model [21]
- Differential Methylation: Identify differentially methylated regions (DMRs) using tools like methylKit or dmrseq with multiple testing correction
Microarray Data Analysis Pipeline:
- Preprocessing: Perform background correction, dye bias adjustment, and functional normalization using minfi package in R [20]
- Quality Filtering: Remove probes with detection p-value > 0.01 in any sample, exclude cross-reactive probes, and filter SNP-affected probes [20]
- Beta Value Calculation: Compute methylation values using the standard beta value formula [20]
- Differential Methylation: Identify DMRs using linear modeling with empirical Bayes moderation (limma package) with false discovery rate correction [9]
Applications in Tumor Microenvironment Research
Deciphering TME Heterogeneity in Pancreatic Cancer
DNA methylation profiling has revealed critical insights into the complex heterogeneity of pancreatic ductal adenocarcinoma (PDAC). Through unsupervised clustering of methylation array data, researchers have identified two major PDAC subgroups with distinct molecular and clinical characteristics [8]. Group 1 tumors exhibit methylation profiles more similar to normal pancreatic tissue and are associated with well-differentiated histology, while Group 2 tumors display significantly divergent methylation patterns linked to poorly differentiated morphology, squamous features, and substantially worse prognosis (p = 0.0046 for survival difference) [8]. This methylation-based stratification proved more prognostically powerful than conventional histological assessment.
The application of hierarchical deconvolution algorithms to methylation data has further enabled resolution of the PDAC immune microenvironment into three distinct subtypes: hypo-inflamed (immune-deserted), myeloid-enriched, and lymphoid-enriched (notably T-cell predominant) [8]. This stratification provides a robust framework for patient selection in immunotherapy trials and reveals the profound influence of epigenetic regulation on immune cell recruitment and function within the TME.
Intratumoral Methylation Heterogeneity and Tumor Evolution
Multi-region methylation analysis using high-density arrays has uncovered extensive intratumoral methylation heterogeneity (DNAmeH) in PDAC, with important implications for tumor evolution and therapeutic resistance [9]. Phylogenetic reconstruction based on methylation profiles has demonstrated an evolutionary trajectory from well-differentiated T1 methylation patterns to poorly differentiated T2 profiles, coinciding with increasingly aggressive phenotypes and genomic instability [9].
This methylation heterogeneity manifests functionally through distinct gene expression programs. T2 methylation profiles show substantial hypomethylation of transcription regulation genes (FDR q < 0.001) and concomitant upregulation of DNA repair and MYC target pathways (FDR q < 0.001) [9]. These epigenetic-evolving subclones within the TME may represent reservoirs of therapeutic resistance, highlighting the importance of multi-region methylation assessment for comprehensive tumor characterization.
Methylation-Based TME Deconvolution
The cell-type specificity of DNA methylation patterns enables computational deconvolution of bulk tumor samples into their constituent cellular components [8]. This approach leverages reference methylation signatures of pure cell types to infer the proportional composition of cancer cells, immune subsets, and stromal elements within the TME [8]. The resulting cellular maps reveal clinically relevant TME states that correlate with therapeutic response and patient outcomes.
In PDAC, methylation-based deconvolution has demonstrated association between KRAS mutational status and specific TME configurations, with mutant KRAS tumors exhibiting distinct immune composition compared to wild-type counterparts [8]. Furthermore, epigenetic age acceleration calculated from methylation arrays has emerged as a biomarker of biological aging in the TME, showing significant association with KRAS mutation status (p = 0.0128) and potentially contributing to immunosuppressive microenvironments [8].
Visualizing Experimental Workflows and Signaling Pathways
Bisulfite Sequencing Workflow
Diagram 1: Bisulfite sequencing workflow from sample to results
Methylation Array Processing Pipeline
Diagram 2: Microarray processing pipeline steps
TME Deconvolution Through Methylation Profiling
Diagram 3: TME deconvolution using methylation data
Research Reagent Solutions
Table 3: Essential Research Reagents for Methylation Analysis
| Reagent/Kits | Manufacturer | Primary Function | Key Applications |
|---|---|---|---|
| QIAseq Targeted Methyl Custom Panel | QIAGEN | Targeted bisulfite sequencing library prep | Custom CpG panel analysis across many samples [20] |
| EZ DNA Methylation Kit | Zymo Research | Bisulfite conversion of DNA | Standard conversion for arrays and sequencing [20] |
| Infinium MethylationEPIC BeadChip | Illumina | Genome-wide methylation profiling | Epigenome-wide association studies [9] |
| NEBNext EM-seq Kit | New England Biolabs | Enzymatic methylation conversion | Bisulfite-free library preparation [19] |
| Maxwell RSC Tissue DNA Kit | Promega | Automated DNA extraction from tissues | High-quality DNA from various sample types [20] |
| QIAamp DNA Mini Kit | QIAGEN | Manual DNA extraction from swabs/fluids | Optimal for low-input samples [20] |
The detection arsenal for DNA methylation analysis provides powerful tools for deciphering the complex epigenetic landscape of the tumor microenvironment. Bisulfite sequencing, microarray platforms, and emerging third-generation technologies each offer distinct advantages that can be leveraged to address specific research questions in cancer epigenetics. The strong concordance demonstrated between bisulfite sequencing and microarray platforms supports their complementary use in biomarker discovery and validation pipelines [20].
Future developments in methylation detection technologies will likely focus on enhancing single-cell resolution, reducing input requirements further, and integrating multimodal omics data. The application of these advanced detection platforms to TME research will continue to reveal the dynamic epigenetic interactions between cancer cells and their microenvironment, ultimately informing the development of novel epigenetic therapies and biomarkers for precision oncology. As these technologies evolve, they will undoubtedly uncover new dimensions of methylation heterogeneity within the TME, providing unprecedented insights into cancer biology and therapeutic resistance mechanisms.
The tumor microenvironment (TME) is a complex ecosystem comprising cancer cells, immune cells, stromal cells, and vascular components, all engaged in dynamic crosstalk that fundamentally influences tumor progression, therapeutic response, and patient outcomes. While genetic heterogeneity has long been recognized as a driver of cancer evolution, non-genetic functional heterogeneity arising from epigenetic regulation represents an equally crucial layer of complexity [22]. Among epigenetic modifications, DNA methylation has emerged as a particularly stable and informative biomarker of cellular identity and state within the TME [23].
Traditional bulk sequencing approaches, which analyze thousands of cells simultaneously, produce an averaged methylome profile that masks the profound heterogeneity existing between individual cells [22]. This limitation has profound implications for understanding cancer biology, as small but critical subpopulations with distinct epigenetic states—such as therapy-resistant stem cells or metastatic precursors—can remain undetected [22]. The emergence of single-cell technologies has revolutionized this paradigm, enabling researchers to disentangle the intricate cellular composition and epigenetic states within tumors at unprecedented resolution [22] [24].
This technical guide explores how single-cell DNA methylation analysis is revealing new dimensions of TME biology, providing methodologies for quantifying epigenetic heterogeneity, and offering insights into how this information can be leveraged for therapeutic innovation. By moving beyond population averages to examine cellular epigenomes individually, researchers can now decode the functional diversity that drives tumor adaptability and treatment resistance [24].
DNA Methylation as a Blueprint of Cellular Identity and State
Fundamental Principles of DNA Methylation in Cancer
DNA methylation involves the covalent addition of a methyl group to the fifth position of cytosine residues, primarily within CpG dinucleotides [22]. In normal cells, this epigenetic mark plays crucial roles in gene regulation, genomic imprinting, and chromatin organization [22]. In cancer, this regulatory system becomes profoundly disrupted through two hallmark patterns: global hypomethylation that promotes genomic instability, and regional hypermethylation that silences tumor suppressor genes in CpG-rich promoter regions [23].
The binary nature of DNA methylation (methylated vs. unmethylated) at individual CpG sites, combined with its stability and cell-type specificity, makes it an ideal biomarker for tracing cellular lineage and identity within complex mixtures [25]. Unlike transcriptomic profiles, which can fluctuate rapidly in response to environmental cues, DNA methylation patterns represent more stable molecular footprints of a cell's developmental history and functional capacity [22].
Advantages of Single-Cell DNA Methylation Analysis
Single-cell DNA methylation analysis offers several distinct advantages for TME characterization compared to traditional approaches:
Resolution of Cellular Subpopulations: It enables identification of rare but clinically relevant cellular subtypes within tumors, such as cancer stem cells with enhanced therapeutic resistance [22].
Lineage Tracing: Epigenetic patterns can be used to reconstruct developmental trajectories and understand the relationships between different cellular components of the TME [22].
Integration with Multi-omics: When combined with transcriptomic and genomic data at single-cell resolution, DNA methylation profiles provide complementary information about regulatory mechanisms [22].
The stability of DNA also makes single-cell methylome analysis particularly suitable for clinical applications, including analysis of archival biospecimens such as formalin-fixed, paraffin-embedded (FFPE) tissues [25].
Methodological Framework for Single-Cell Epigenomic Analysis
Experimental Workflows and Quality Control
Single-cell DNA methylation analysis begins with the isolation of individual cells, followed by bisulfite conversion treatment, which deaminates unmethylated cytosines to uracils while leaving methylated cytosines unchanged [22]. The converted DNA is then amplified and sequenced using various platforms. A critical first step in any single-cell epigenomic workflow is rigorous quality control to exclude compromised cells and ensure data reliability [26].
Table 1: Key Quality Control Metrics for Single-Cell DNA Methylation Data
| QC Metric | Target Value/Range | Purpose | Tool Examples |
|---|---|---|---|
| Bisulfite Conversion Rate | >99% | Verify efficient conversion of unmethylated cytosines | FastQC, Bismark |
| CpG Coverage per Cell | >1 million reads | Ensure sufficient genomic coverage | MethylKit |
| Mitochondrial DNA % | <10% | Detect apoptotic cells | Seurat |
| Number of Detected Genes | Cell-type dependent | Filter low-quality cells | Scater |
| Doublet Rate | <5% | Identify multiple cells in single partition | DoubletFinder |
The subsequent bioinformatic processing involves alignment to reference genomes, methylation calling, and data normalization to remove technical artifacts while preserving biological variation [26]. Specialized tools have been developed for these tasks, accounting for the unique characteristics of bisulfite-converted sequences and the sparse nature of single-cell methylation data [22] [26].
Computational Deconvolution of Bulk Data
While true single-cell analysis provides the highest resolution, computational deconvolution methods offer a practical alternative for estimating cellular composition from bulk DNA methylation data. These approaches leverage cell-type-specific methylation signatures to infer the relative proportions of different cell types within heterogeneous tissue samples [27] [28] [25].
Table 2: DNA Methylation-Based Deconvolution Algorithms for TME Analysis
| Algorithm | Resolved Cell Types | Key Features | Applications |
|---|---|---|---|
| HiTIMED [25] | 17 cell types across tumor, immune, and angiogenic compartments | Tumor-type-specific hierarchical model | Prognostic stratification in carcinomas |
| MDBrainT [28] | 13 CNS-specific cell types (astrocytes, microglia, neurons, etc.) | Brain TME-specific signatures | Glioma, ependymoma, medulloblastoma |
| Pan-Cancer Immune Deconv. [27] | 7 immune cell types (CD4+ T, CD8+ T, NK, B, monocytes, etc.) | 1256 immune-specific methylation genes | Pan-cancer immune heterogeneity analysis |
HiTIMED exemplifies the advancement in this field, employing a hierarchical deconvolution approach with tumor-type-specific reference libraries that progressively resolve major TME components (tumor, immune, angiogenic) into increasingly specific cell subtypes [25]. This method has demonstrated superior accuracy compared to earlier approaches, particularly because it uses DNA methylation signatures from primary tumors rather than cancer cell lines, which often harbor additional epigenetic alterations [25].
Quantifying Epigenetic Heterogeneity
Beyond identifying cell types, measuring the degree of epigenetic heterogeneity within cellular populations provides critical insights into tumor plasticity and developmental states. The epiCHAOS (Epigenetic/Chromatin Heterogeneity Assessment Of Single cells) metric has been developed specifically for this purpose [24].
This computational approach calculates heterogeneity scores based on pairwise distances between single-cell epigenomic profiles, typically derived from scATAC-seq or single-cell methylation data [24]. Validation studies have demonstrated that epiCHAOS scores effectively capture biologically significant heterogeneity patterns, with higher scores observed in multipotent progenitor cells and lower scores in terminally differentiated cells [24]. In cancer contexts, elevated epiCHAOS scores correlate with increased tumor plasticity and stemness, features associated with therapeutic resistance and metastatic potential [24].
Key Research Findings and Clinical Implications
Immune Heterogeneity Across Cancer Types
Large-scale pan-cancer analyses have revealed extensive heterogeneity in immune cell composition across different tumor types and individual patients. A comprehensive evaluation of 5,323 samples across 14 cancer types identified 42 distinct immune subtypes based on the infiltration patterns of seven immune cell types (CD4+ T cells, CD8+ T cells, CD56+ NK cells, CD19+ B cells, CD14+ monocytes, neutrophils, and eosinophils) [27].
These immune subtypes demonstrated significant associations with clinical phenotypes, including patient survival and tumor stage [27]. For example, subtypes characterized by high CD8+ T cell infiltration (identified in 24 subtypes across various cancers) generally correlated with improved responses to immunotherapy, while subtypes dominated by immunosuppressive cells like monocytes often exhibited more aggressive clinical courses [27].
DNA Methylation Patterns Shape Immune-Evasion Mechanisms
DNA methylation plays a direct role in facilitating immune evasion through several mechanisms:
Silencing of Antigen Presentation Machinery: Promoter hypermethylation of genes encoding major histocompatibility complex (MHC) components and other antigen-presentation proteins reduces tumor visibility to immune cells [29].
Suppression of Innate Immune Signaling: Methylation-mediated silencing of critical innate immune genes like STING (stimulator of interferon genes) dampens antitumor immune responses in various cancers, including triple-negative breast cancer [29].
Regulation of Immune Checkpoint Molecules: Epigenetic control of PD-L1 and other immune checkpoint molecules influences response to immunotherapy [29] [23].
In colorectal cancer, the CpG island methylator phenotype (CIMP) status defines distinct immune microenvironments in microsatellite instability-high (MSI-H) tumors. CIMP-high MSI-H colorectal cancers exhibit significantly higher densities of CD8+ tumor-infiltrating lymphocytes, increased PD-L1 expression, and elevated cytolytic activity scores compared to CIMP-low/negative tumors, independent of tumor mutational burden [30]. This suggests that DNA methylation patterns themselves actively shape immunogenic phenotypes beyond the influence of mutation load alone.
Therapeutic Targeting of Epigenetic Mechanisms
The dynamic and reversible nature of epigenetic modifications makes them attractive therapeutic targets. DNA methyltransferase inhibitors (DNMTis), such as azacitidine and decitabine, can reverse aberrant methylation patterns and potentially enhance antitumor immunity through multiple mechanisms [29] [23]:
Preclinical studies have demonstrated that DNMTis can synergize with immune checkpoint inhibitors (ICIs) to overcome resistance mechanisms in various solid tumors, including triple-negative breast cancer [29]. This combination approach is currently being evaluated in multiple clinical trials, with the goal of converting immunologically "cold" tumors into "hot" tumors that are more responsive to immunotherapy [29] [23].
The Scientist's Toolkit: Essential Reagents and Methodologies
Table 3: Essential Research Reagents and Platforms for Single-Cell DNA Methylation Analysis
| Category | Specific Products/Platforms | Key Applications | Technical Considerations |
|---|---|---|---|
| Bisulfite Conversion Kits | EZ DNA Methylation-Lightning, Epitect Bisulfite Kit | Convert unmethylated cytosines to uracils | Optimization needed for low-input single-cell applications |
| Single-Cell Platforms | 10x Genomics Single Cell Methylation, Fluidigm C1 | Partitioning individual cells for analysis | Throughput vs. coverage trade-offs |
| Methylation Arrays | Infinium MethylationEPIC v2.0 (~1.3M CpGs) | Bulk deconvolution approaches | Limited to predefined CpG sites |
| Whole-Genome Bisulfite Sequencing | scBS-seq, scWGBS | Comprehensive single-cell methylome | High sequencing depth required |
| Bioinformatic Tools | epiCHAOS, HiTIMED, MethylResolver | Data analysis and interpretation | Computational resource requirements |
| Sulfasalazine-d4 | Sulfasalazine-d4, CAS:1346606-50-5, MF:C18H14N4O5S, MW:402.4 g/mol | Chemical Reagent | Bench Chemicals |
| Dimethoate-d6 | Dimethoate-d6, CAS:1219794-81-6, MF:C5H12NO3PS2, MW:235.3 g/mol | Chemical Reagent | Bench Chemicals |
Single-cell resolution analysis of DNA methylation states within the TME represents a transformative approach in cancer research, revealing previously unappreciated layers of heterogeneity with profound biological and clinical implications. The methodologies outlined in this technical guide—from experimental workflows to computational deconvolution and heterogeneity quantification—provide researchers with powerful tools to dissect the complex epigenetic landscape of tumors.
As these technologies continue to evolve and become more accessible, they promise to unlock new opportunities for precision medicine, including improved patient stratification, identification of novel therapeutic targets, and rational design of combination therapies that leverage the synergistic potential of epigenetic drugs and immunotherapies. The integration of single-cell epigenomic data with other molecular modalities will further enhance our understanding of the regulatory networks governing tumor behavior, ultimately advancing our ability to combat cancer through epigenetically-informed strategies.
The tumor microenvironment (TME) is a complex ecosystem comprising malignant cells, immune populations, stromal elements, and vascular components whose interactions fundamentally influence cancer progression and therapeutic response [8]. A significant challenge in TME research stems from the pervasive heterogeneity observed across multiple molecular layers, with DNA methylation heterogeneity (DNAmeH) representing a particularly influential component [3]. DNAmeH arises from both cancer epigenome heterogeneity and the diverse cell compositions within the TME, creating complex patterns that confound traditional bulk analysis methods [3]. Computational deconvolution has emerged as an essential methodological approach to address this challenge, enabling researchers to infer cellular composition and cell-type-specific molecular features from bulk genomic, epigenomic, and transcriptomic data.
The integration of deconvolution methodologies into TME research represents a paradigm shift in how scientists investigate cancer biology. By mathematically dissecting bulk molecular measurements into their constituent cellular components, these methods provide critical insights into the cellular architecture of tumors while circumventing the technical and financial barriers associated with single-cell technologies for large cohort studies [31] [32]. Furthermore, DNA methylation-based deconvolution offers unique advantages due to the stability and cell lineage specificity of methylation patterns, making it particularly suited for characterizing TME composition from both fresh-frozen and formalin-fixed paraffin-embedded (FFPE) clinical specimens [8]. This technical guide comprehensively examines the principles, methodologies, and applications of computational deconvolution with specific emphasis on its role in elucidating DNA methylation heterogeneity in TME research.
DNA Methylation Heterogeneity: Biological Foundations and Technical Challenges
DNA methylation heterogeneity represents a fundamental aspect of tumor biology that directly influences deconvolution approaches. The most prevalent DNA methylation modification in the human genome, 5-Methylcytosine (5mC), demonstrates abnormal patterns strongly associated with tumor progression [3]. Intratumoral and intertumoral DNAmeH primarily arises from two key sources: cancer epigenome heterogeneity and the diverse cell compositions within the TME [3]. This heterogeneity manifests across multiple dimensions, including differences among cancer types, among individual cells, and at allele-specific hemimethylation sites, creating a complex molecular landscape that requires sophisticated analytical approaches.
From a technical perspective, several specific factors complicate the analysis of DNA methylation patterns in complex tumor samples. The cell cycle phase introduces dynamic methylation changes, while tumor mutational burden (TMB), cellular stemness, copy number variation (CNV), tumor subtype classification, and hypoxic regions all contribute to the observed methylation heterogeneity [3]. Additionally, tumor characteristics such as stage, cellular state, and tumor purity significantly influence methylation measurements, necessitating computational approaches that can account for these confounding variables [3]. In pancreatic ductal adenocarcinoma (PDAC), for instance, the typically low tumor cellularity (5-20% cancer cells) combined with a pronounced desmoplastic reaction creates substantial challenges for interpreting molecular data obtained from tumor biopsies [8]. These biological and technical complexities highlight the critical need for robust deconvolution methodologies capable of disentangling the contributions of various cell types to the overall methylation signal.
Recent research has demonstrated the clinical relevance of DNA methylation heterogeneity through the identification of distinct methylation profiles correlated with histopathological features and patient outcomes. In PDAC, two distinct methylation profiles (T1 and T2) have been identified, with T2 profiles significantly different from normal tissue and linked to poorly differentiated morphology, squamous features, and shorter disease-free survival [9]. Phylogenetic analyses further suggest an evolutionary trajectory from T1 to T2 profiles coinciding with aggressive phenotypes and increased genomic instability [9]. Such findings underscore the importance of deconvolution methods that can not only estimate cellular abundances but also resolve subtype-specific methylation patterns within the complex TME.
Methodological Approaches to Computational Deconvolution
Reference-Based Deconvolution Frameworks
Reference-based deconvolution methods utilize pre-defined cell-type-specific molecular signatures to estimate cellular proportions from bulk data. These approaches typically employ constrained regression models that express bulk measurements as linear combinations of reference profiles, with non-negativity constraints ensuring biologically plausible proportions [32]. The accuracy of these methods heavily depends on the quality and comprehensiveness of the reference signatures, which can be derived from purified cell populations, single-cell sequencing data, or established molecular databases.
xCell 2.0 represents a significant advancement in reference-based deconvolution, introducing automated handling of cell type dependencies through ontological integration and more robust signature generation [31]. This algorithm generates hundreds of signatures for each cell type using various predefined thresholds, then employs in-silico simulations to learn parameters that transform enrichment scores to linear proportions while correcting for spillover effects between related cell types [31]. Benchmarking evaluations have demonstrated xCell 2.0's superior performance across diverse biological contexts, with particular utility in predicting response to immune checkpoint blockade therapy [31].
OmicsTweezer addresses the critical challenge of batch effects between bulk data and reference single-cell data by integrating optimal transport with deep learning [33]. This distribution-independent model aligns simulated and real data in a shared latent space, effectively mitigating data shifts and inter-omics distribution differences. The method's versatility enables deconvolution of bulk RNA-seq, bulk proteomics, and spatial transcriptomics data, making it particularly valuable for multi-omics studies of the TME [33].
DiffFormer introduces a novel architecture that integrates conditional diffusion models with Transformer networks for bulk RNA-seq deconvolution [34]. This approach reframes deconvolution as a conditional generation task, structuring noisy cell proportion vectors, diffusion timesteps, and bulk RNA-seq profile embeddings as information tokens. The Transformer's self-attention mechanism effectively models complex, non-linear dependencies between these modalities, enabling precise denoising of cell proportion estimates [34]. Systematic evaluation demonstrates DiffFormer's consistent performance advantage over both traditional methods and baseline MLP-based diffusion models.
Reference-Free Deconvolution Strategies
Reference-free deconvolution methods estimate cellular heterogeneity without requiring prior cell-type marker information by simultaneously inferring both cell-type-specific signatures and proportions directly from bulk data. These approaches are particularly valuable for studying tissue types with limited reference data or when substantial disparities exist between target samples and available references [32].
The RFdecd (Reference-Free deconvolution based on cross-cell-type differential) method employs an iterative algorithm to search for cell-type-specific features through cross-cell-type differential analysis [32]. This approach systematically evaluates five feature selection options—variance (VAR), coefficient of variation (CV), single-vs-composite (SvC), dual-vs-composite (DvC), and pairwise-direct (PwD)—to identify optimal feature sets for proportion estimation [32]. Comprehensive validation across seven real datasets demonstrates RFdecd's excellent performance, particularly in scenarios where matched reference data are unavailable.
Other reference-free approaches include non-negative matrix factorization (NMF), hierarchical latent variable models, and Bayesian frameworks, each with distinct advantages and limitations [32]. While reference-free methods offer greater flexibility, they generally provide less accurate and robust estimations compared to reference-based approaches when high-quality references are available [32].
DNA Methylation-Based Deconvolution
DNA methylation data offers unique advantages for TME deconvolution due to its cell-type specificity and stability. Methylation-based deconvolution typically utilizes Illumina methylation arrays (EPIC or 450K platforms) to measure methylation levels at CpG sites throughout the genome [9]. The resulting beta values (β values), representing methylation ratios, are analyzed using either reference-based or reference-free approaches to infer cellular composition.
In pancreatic cancer research, hierarchical deconvolution of DNA methylation data has revealed three distinct TME subtypes: hypo-inflamed (immune-deserted), myeloid-enriched, and lymphoid-enriched microenvironments [8]. These immune clusters demonstrate significant associations with clinical outcomes and therapeutic responses, highlighting the clinical relevance of methylation-based TME stratification [8]. Similar approaches in breast cancer have identified distinct methylation profiles associated with immune cell infiltration patterns and patient survival [35] [36].
Table 1: Comparison of Major Computational Deconvolution Methods
| Method | Omics Data | Approach | Key Features | Limitations |
|---|---|---|---|---|
| xCell 2.0 [31] | RNA-seq, Microarray | Reference-based | Automated cell type dependencies; Spillover correction; Pre-trained references | Limited customization of reference sets |
| OmicsTweezer [33] | Multi-omics (RNA, Protein, Spatial) | Reference-based | Optimal transport with deep learning; Batch effect correction; Distribution-independent | Computational intensity for large datasets |
| DiffFormer [34] | RNA-seq | Reference-based | Transformer with diffusion model; Non-linear relationships; Conditional generation | Requires substantial training data |
| RFdecd [32] | DNA Methylation, RNA-seq | Reference-free | Cross-cell-type differential analysis; Iterative feature selection; Six selection options | Lower accuracy vs. reference-based with good references |
| Methylation Deconvolution [8] [9] | DNA Methylation | Both | Cell lineage specificity; Stable markers; FFPE compatibility | Platform-specific (Illumina arrays) |
| BayesPrism [32] | RNA-seq | Reference-free | Bayesian framework; Enhanced identifiability via prior integration | Complex implementation |
Experimental Protocols and Implementation
DNA Methylation Deconvolution Workflow
The standard workflow for DNA methylation-based deconvolution begins with sample processing and data generation. For FFPE tissues, 10μm sections are cut, deparaffinized, and subjected to macrodissection to enrich for target areas [9]. DNA extraction is performed using specialized kits (e.g., QIAamp DNA FFPE Tissue Kit), followed by bisulfite conversion (e.g., EZ DNA Methylation Kit) and array-based methylation analysis using the Infinium Methylation EPIC BeadChip [9]. Raw signal intensities are extracted from IDAT files using R-based pipelines, with background correction and dye bias correction applied to both color channels.
Quality control and preprocessing involve several critical steps:
- Probe Filtering: Removal of probes associated with non-CpG sites, sex chromosomes, single nucleotide polymorphisms (SNPs), and those with low signal intensity (mean β value < 0.1) [9]
- Normalization: Transformation of β values to M-values for statistical analysis
- Feature Selection: Retention of probes located in promoter-associated regions or selection of top variable probes (typically 1000-2000) for downstream analysis [9]
- Batch Effect Correction: Application of algorithms like Harmony to mitigate technical variations between samples [37]
For reference-based deconvolution, the preprocessed data is projected onto cell-type-specific methylation signatures using constrained regression models. For reference-free approaches, dimensionality reduction techniques (PCA, MDS) followed by clustering algorithms identify latent cell-type components [9]. Validation typically involves comparison with orthogonal methods such as immunohistochemistry, flow cytometry, or single-cell methylome analysis when available.
Single-Cell RNA Sequencing Analysis for Deconvolution Reference Generation
Single-cell RNA sequencing (scRNA-seq) provides essential reference data for transcriptome-based deconvolution. The standard analytical pipeline involves:
- Data Preprocessing: Quality control using Scanpy or Seurat to filter low-quality cells (<200 or >5000 genes, mitochondrial ratio >20%) and normalize counts to CP10k with log transformation [34]
- Feature Selection: Identification of top highly variable genes (2000) using the FindVariableFeatures function [37]
- Dimensionality Reduction: Principal component analysis (PCA) followed by uniform manifold approximation and projection (UMAP) for visualization [37]
- Cell Clustering: Application of graph-based clustering algorithms (FindNeighbors and FindClusters in Seurat) at appropriate resolutions (typically 0.4-0.8) [37]
- Cell Type Annotation: Marker-based identification of cell populations using reference databases and differential expression analysis [37]
InferCNV analysis distinguishes malignant cells from non-malignant stromal and immune populations by identifying large-scale chromosomal alterations, providing critical validation for deconvolution results in tumor samples [37]. Cell-cell communication analysis using tools like CellPhoneDB further characterizes TME interactions that may influence deconvolution accuracy [37].
Figure 1: DNA Methylation Deconvolution Workflow. The diagram illustrates the complete experimental pipeline from sample processing to TME characterization, highlighting key steps in DNA methylation-based deconvolution.
Integrative Analysis of Bulk and Single-Cell Data
The SCISSOR algorithm provides a robust framework for integrating single-cell and bulk RNA-seq data to identify cell subpopulations associated with clinical phenotypes [36]. This approach correlates bulk expression profiles with phenotypic traits while leveraging single-cell data to identify specific cell subpopulations driving these associations. The method has been successfully applied to breast cancer datasets to reveal mechanical stimulus-related genes influencing TME composition and patient prognosis [36].
Weighted Gene Co-expression Network Analysis (WGCNA) represents another powerful approach for identifying gene modules associated with TME features [35]. This systems biology method constructs scale-free co-expression networks, identifies modules of highly correlated genes, and relates these modules to external sample traits. In breast cancer research, WGCNA has identified cuproptosis-related gene modules associated with immunosuppressive TME features and poor clinical outcomes [35].
Table 2: Essential Research Reagents and Computational Tools for TME Deconvolution
| Category | Item/Resource | Specification/Function | Application Context |
|---|---|---|---|
| Wet-Lab Reagents | QIAamp DNA FFPE Tissue Kit | DNA extraction from archived specimens | Methylation analysis of clinical cohorts [9] |
| EZ DNA Methylation Kit | Bisulfite conversion for methylation analysis | Prepares DNA for Illumina methylation arrays [9] | |
| Infinium Methylation EPIC BeadChip | Genome-wide methylation profiling | Provides methylation data for ~850K CpG sites [9] | |
| TRIzol Reagent | RNA isolation from cells and tissues | Transcriptomic analysis for reference generation [37] | |
| Computational Tools | Seurat R package (v4.2.0+) | Single-cell RNA-seq analysis | Reference generation and cell type annotation [37] |
| xCell 2.0 | Cell type enrichment estimation | Reference-based deconvolution with spillover correction [31] | |
| OmicsTweezer | Multi-omics deconvolution | Handles batch effects across omics data types [33] | |
| RFdecd R package | Reference-free deconvolution | Methylation analysis without reference data [32] | |
| InferCNV | Copy number variation analysis | Identifies malignant cells in single-cell data [37] | |
| CellPhoneDB (v2.0.0) | Cell-cell interaction analysis | Characterizes TME communication networks [37] | |
| Reference Databases | Cell Ontology (CL) | Standardized cell type terminology | Enables automated cell type dependency mapping [31] |
| MSigDB | Curated gene sets | Functional enrichment analysis [35] [36] | |
| TCGA Pan-Cancer Atlas | Multi-omics cancer datasets | Benchmarking and validation studies [8] [9] |
Analytical Frameworks for TME Characterization
Cellular Hierarchy and Proportion Estimation
Deconvolution algorithms generate cellular proportion estimates that enable comprehensive TME characterization. These proportions can be analyzed in relation to clinical variables, therapeutic responses, and molecular subtypes to uncover biologically and clinically significant patterns. In pancreatic cancer, hierarchical deconvolution of DNA methylation data has established three major TME subtypes with distinct cellular compositions and clinical behaviors [8]. Similarly, retinoblastoma analysis has revealed distinct cone precursor subpopulations with varying proportions in invasive versus non-invasive tumors [37].
Figure 2: Computational Deconvolution Methodologies. The diagram categorizes major deconvolution approaches and their relationships, highlighting the diversity of algorithms available for TME characterization.
Differential Methylation Analysis
Identifying differentially methylated regions (DMRs) between TME subtypes provides critical insights into the epigenetic regulation of tumor biology. The standard analytical pipeline involves:
- DMP Identification: Linear modeling of M-values to identify differentially methylated positions (DMPs) with significance thresholds (e.g., log2 fold change ≥ 1, adjusted p-value < 0.05) [9]
- DMR Detection: Application of region-based algorithms (e.g., demarcate package) to identify coordinated methylation changes across genomic loci [9]
- Functional Annotation: Gene Ontology and pathway enrichment analysis of genes associated with DMRs to elucidate biological significance [9]
- Integration with Expression: Correlation of methylation changes with transcriptomic data to identify functionally relevant epigenetic alterations [9]
In PDAC, this approach has revealed substantial hypomethylation of transcription regulation genes in aggressive T2 profiles and upregulated DNA repair and MYC target pathways, providing mechanistic insights into tumor progression [9].
Validation and Benchmarking Strategies
Rigorous validation is essential for establishing deconvolution accuracy. Orthogonal experimental methods including fluorescence-activated cell sorting (FACS), immunohistochemistry, and single-cell sequencing provide ground truth measurements for benchmarking [31] [32]. Computational validation employs pseudo-bulk mixtures with known proportions, cross-validation against established signatures, and consistency checks across multiple algorithms [31].
The Deconvolution DREAM Challenge dataset provides a standardized benchmark for objective performance assessment [31]. Additionally, real-world datasets with experimentally determined cell proportions (e.g., GSE107011 with FACS-verified immune cell counts) offer valuable validation resources [34]. Performance metrics typically include root mean square error (RMSE), Pearson correlation coefficients, and spillover effects between related cell types [31].
Clinical Translation and Therapeutic Implications
Computational deconvolution has significant translational implications across multiple cancer types. In breast cancer, cuproptosis-related gene signatures derived from deconvolution analyses stratify patients into distinct risk groups with differential survival, TP53 mutation frequency, and TME composition [35]. Similarly, mechanical stimulus-related genes identified through integrated bulk and single-cell analysis reveal distinct TME subtypes with implications for personalized treatment strategies [36].
In pancreatic cancer, DNA methylation-based TME stratification identifies patient subgroups with varying responses to conventional therapies and potential susceptibility to emerging immunotherapeutic approaches [8]. The hypo-inflamed, myeloid-enriched, and lymphoid-enriched TME subtypes demonstrate fundamentally different immune contexts that may require tailored therapeutic interventions [8].
The predictive value of deconvolution-derived features extends to immunotherapy response forecasting. xCell 2.0-derived TME features significantly improve prediction accuracy for immune checkpoint blockade response compared to models using only cancer type and treatment information [31]. This capability addresses a critical clinical challenge in oncology and highlights the practical utility of advanced deconvolution methodologies.
Deconvolution-guided biomarker discovery also facilitates non-invasive monitoring strategies through liquid biopsy approaches. The cell specificity of DNA methylation patterns enables tracking of TME dynamics in circulating tumor DNA, offering potential for early detection of therapeutic resistance and disease progression [3]. As deconvolution methodologies continue to evolve, their integration into clinical trial design and treatment decision-making represents a promising frontier in precision oncology.
Computational deconvolution has emerged as an indispensable methodology for characterizing the cellular heterogeneity of the tumor microenvironment, with particular utility for investigating DNA methylation heterogeneity. The integration of reference-based and reference-free approaches, coupled with advanced machine learning architectures, has substantially improved our ability to resolve cellular composition from bulk molecular data. These methodological advances have yielded fundamental insights into TME biology, revealing clinically relevant subtypes with distinct therapeutic vulnerabilities.
Future methodological developments will likely focus on several key areas: enhanced multi-omics integration, improved handling of spatial relationships within the TME, more sophisticated modeling of cellular plasticity and transitional states, and development of single-cell resolved deconvolution approaches. Additionally, the creation of comprehensive, pan-cancer reference atlases will further improve deconvolution accuracy and biological interpretability. As these technical capabilities advance, computational deconvolution will play an increasingly central role in both basic cancer biology and clinical translation, ultimately contributing to more effective, personalized cancer therapies.
The tumor microenvironment (TME) represents a complex ecosystem where heterogeneous cell populations interact to influence cancer progression, therapeutic response, and clinical outcomes. Within this context, DNA methylation heterogeneity has emerged as a critical epigenetic layer reflecting cellular diversity, with different cell subpopulations exhibiting distinct methylation patterns that can be leveraged for biomarker discovery [38] [39]. This cellular heterogeneity represents one of the largest contributors to DNA methylation variability and must be accounted for to accurately interpret analysis results in epigenome-wide association studies [38]. The integration of artificial intelligence (AI) and machine learning (ML) technologies now provides unprecedented capabilities to decode this complexity, enabling researchers to extract meaningful biological insights from high-dimensional epigenetic data.
Methylation patterns in a population of cells can range from completely methylated to completely unmethylated, with intermediate patterns indicating variations in DNA methylation among cells [39]. This heterogeneity results from various epigenetic regulations and can serve as fingerprints of genetic or epigenetic factors during biological development or disease progression [39]. The emerging synergy between methylation analysis and computational intelligence is transforming oncology research, facilitating the development of precise diagnostic classifiers and revealing novel therapeutic targets within the TME.
Computational Frameworks for Quantifying DNA Methylation Heterogeneity
Methodological Approaches for Heterogeneity Assessment
Both experimental and computational methods have been developed to assess methylation heterogeneity. While single-cell bisulfite sequencing (scBS-seq) enables direct measurement, it faces challenges including low read mapping ratios, high costs, and technical difficulties in sample preparation [39]. Consequently, computational methods utilizing bulk sequencing data have been developed to quantify heterogeneity from pooled cell populations.
Table 1: Comparison of DNA Methylation Heterogeneity Scoring Methods
| Method | Basis of Calculation | Genomic Context | Linear Scoring | Considers Pattern Similarity | Independent of Methylation Level |
|---|---|---|---|---|---|
| PDR [40] | Proportion of discordant reads | CG sites | No | No | No |
| MHL [40] | Methylation haplotype load | CG sites | No | Partial | No |
| Epipolymorphism [40] | Entropy of epiallele frequencies | 4-CpG windows | No | No | Yes |
| Methylation Entropy [40] | Shannon entropy of patterns | 4-CpG windows | No | No | Yes |
| FDRP [40] | Fraction of discordant read pairs | Single CpG resolution | No | No | No |
| qFDRP [40] | Quantitative discordant read pairs | Single CpG resolution | No | Yes | No |
| MeH [39] | Biodiversity-inspired models | CG and non-CG sites | Yes | Yes | Yes |
Advanced Frameworks: Model-Based Heterogeneity Estimation
Novel model-based methods adopted from mathematical biodiversity frameworks have demonstrated advantages in estimating genome-wide DNA methylation heterogeneity. The MeH (Methylation Heterogeneity) method applies a unified framework based on Hill numbers to quantify diversity in methylation patterns [39]:
[ {}^{q}AD\left(\overline{V }\right)={ \left[\sum{u\in C}{v}{u}{\left(\frac{{a}_{u}}{\overline{V} }\right)}^{q}\right]}^{\frac{1}{1-q}} ]
where (q) determines sensitivity to relative abundances, (C) is the collection of methylation patterns, (au) is the abundance of pattern (u), and (vu) is its attribute value. This approach provides scoring linearity, enabling fair assessment of heterogeneity across genomic regions and between samples, and can analyze both CG and non-CG methylation contexts [39].
Diagram 1: Computational workflow for DNA methylation heterogeneity analysis from bulk bisulfite sequencing data, showing multiple scoring methodologies.
AI and Machine Learning Approaches for Methylation-Based Biomarker Discovery
Traditional Machine Learning Frameworks
Machine learning has revolutionized diagnostic medicine by enabling analysis of complex datasets to identify patterns and make predictions. Conventional supervised methods, including support vector machines (SVM), random forests (RF), and gradient boosting, have been employed for classification, prognosis, and feature selection across tens to hundreds of thousands of CpG sites [41]. These approaches can be streamlined by AutoML (Automated Machine Learning), serving as the foundation for creating tools applicable to clinical settings.
The extreme gradient boosting (XGBoost) algorithm has demonstrated particular efficacy in cancer classification using DNA methylation profiles. In comparative studies, XGBoost achieved an average AUC (Area Under the Curve) of 0.672 for cancer stage prediction using paracancerous tissue methylation data, outperforming SVM, Naïve Bayes, K-Nearest Neighbors, and Random Forests by significant margins [42]. Furthermore, XGBoost achieved 100% accuracy in classifying nine different cancer types based on DNA methylation profiles of paracancerous tissues from TCGA datasets [42].
Deep Learning and Foundation Models
Deep learning improves DNA methylation studies by directly capturing nonlinear interactions between CpGs and genomic context from data. Multilayer perceptrons and convolutional neural networks (CNNs) have been employed for tumor subtyping, tissue-of-origin classification, survival risk evaluation, and cell-free DNA signal identification [41]. Recently, transformer-based foundation models have undergone pretraining on extensive methylation datasets. MethylGPT, trained on more than 150,000 human methylomes, supports imputation and subsequent prediction with physiologically interpretable focus on regulatory regions, while CpGPT exhibits robust cross-cohort generalization and produces contextually aware CpG embeddings [41].
Table 2: AI/ML Approaches in DNA Methylation Analysis
| Method Category | Key Algorithms | Applications | Advantages | Limitations |
|---|---|---|---|---|
| Traditional ML | XGBoost, Random Forest, SVM | Cancer classification, Stage prediction, Feature selection | Interpretable, Works with smaller datasets, Feature importance scores | Limited capacity for complex nonlinear relationships |
| Deep Learning | CNNs, RNNs, Multilayer Perceptrons | Tumor subtyping, Survival prediction, Image analysis | Automatic feature extraction, Handles complex patterns | Requires large datasets, Computationally intensive, Less interpretable |
| Foundation Models | Transformer architectures (MethylGPT, CpGPT) | Cross-cohort generalization, Imputation tasks | Transfer learning, Context-aware embeddings, High performance on downstream tasks | Extensive pretraining required, Complex implementation |
AI-Powered Tumor Microenvironment Deconvolution
AI acquires characteristics not yet known to humans through extensive learning, enabling handling of large amounts of pathology image data [43]. Divided into machine learning and deep learning, AI has the advantage of processing large datasets and performing image analysis, consequently possessing great potential in accurately assessing TME models [43]. With the complex composition of the TME, AI can learn the spatial location of each cell through supervised learning methods, further analyzing whether cells in various locations have varied relevance in the TME [43].
CNNs are commonly used for pathology image analysis and visual feature extraction of tumor tissues to identify tumor regions and cell types [43]. CNNs can identify and quantify various cells in the TME such as neutrophils and lymphocytes at the cellular level, and also separate tumor from non-tumor regions, grade malignancy of tumors, and perform other classification tasks [43].
Diagnostic Classification and Clinical Translation
DNA Methylation-Based Tumor Classification
DNA methylation has emerged as a diagnostic tool to classify tumors based on a combination of preserved developmental and mutation-induced signatures [44]. The DNA methylation-based classifier for central nervous system cancers standardized diagnoses across over 100 subtypes and altered the histopathologic diagnosis in approximately 12% of prospective cases, accompanied by an online portal facilitating routine pathology application [41].
The classifier developed by Capper et al. uses a machine learning algorithm (Random Forest classifier) that generates a calibrated score representing the probability that a tumor belongs to a specific subclass [44]. A threshold score greater than 0.9 must be reached to achieve sensitivity of 0.989 and specificity of 0.999 [44]. This approach has been particularly valuable for classifying histologically challenging tumors, with DNA methylation profiling revealing that many tumors originally diagnosed as CNS-PNETs actually represented different entities, leading to reclassification into four distinct molecular subgroups [44].
Diagram 2: Clinical translation workflow for AI-powered DNA methylation analysis in diagnostic classification.
Integration of Multi-Omics Data and Spatial Biology
The complex heterogeneity of tumors makes it challenging to identify new biomarker candidates. The emergence of spatial biology techniques has been one of the most significant advances in biomarker discovery as they can reveal the spatial context of dozens of markers within a single tissue, enabling full characterization of the complex and heterogeneous TME [45]. Unlike traditional approaches, spatial transcriptomics and multiplex immunohistochemistry allow researchers to study gene and protein expression in situ without altering spatial relationships or interactions between cells [45].
When paired with multi-omics profiling, these technologies provide a holistic approach to biomarker discovery. By combining different data types, multi-omics can reveal novel insights into the molecular basis of diseases and drug responses, identify new biomarkers and therapeutic targets, and predict and optimize individualized treatments [45]. AI plays a crucial role in integrating these diverse data modalities, with machine learning algorithms capable of identifying subtle patterns across genomics, transcriptomics, proteomics, and epigenomics datasets.
Experimental Protocols and Research Toolkit
DNA Methylation Profiling Technologies
Genome-wide DNA methylation analysis can be performed using various analytical platforms, either sequencing or array-based. Whole genome bisulfite sequencing, targeted bisulfite sequencing, and DNA methylation arrays represent the three most common approaches [44]. The DNA methylation EPIC array has emerged as a dominant molecular assay for genome-wide analysis of DNA methylation in FFPE tissue due to its compatibility with archival samples, relatively low DNA input requirements (250 ng), and cost-effectiveness [44].
Table 3: Research Reagent Solutions for DNA Methylation Analysis
| Technology/Reagent | Function | Application Context | Key Features |
|---|---|---|---|
| Infinium MethylationEPIC Kit | Genome-wide methylation profiling | FFPE and fresh frozen samples | 850,000 CpG sites, FFPE compatibility, Low DNA input |
| Zymo Research EX-96 DNA Methylation Kit | Bisulfite conversion | Sample preparation for methylation analysis | High conversion efficiency, 96-well format |
| Infinium HD FFPE Restore Kit | DNA restoration | Repair of degraded FFPE DNA | Enhances data quality from archival samples |
| Methylation-specific PCR (MSP) | Targeted methylation analysis | Biomarker validation | Specific detection of methylated alleles |
| Whole-genome bisulfite sequencing | Comprehensive methylation mapping | Discovery applications | Single-base resolution, genome-wide coverage |
| ELSA-seq | Liquid biopsy methylation detection | Circulating tumor DNA analysis | High sensitivity for MRD monitoring |
| Isopedicin | Isopedicin, MF:C18H18O6, MW:330.3 g/mol | Chemical Reagent | Bench Chemicals |
| Domperidone-d6 | Domperidone-d6, MF:C22H24ClN5O2, MW:431.9 g/mol | Chemical Reagent | Bench Chemicals |
Methodological Protocol: DNA Methylation Array Analysis
DNA methylation array analysis is a well-established four-day process [44]:
Day 1: DNA Extraction and Bisulfite Conversion
- Extract DNA using standard clinical isolation methods
- Quantify DNA using fluorometric methods (e.g., Qubit dsDNA BR Assay)
- Perform bisulfite conversion using the EX-96 DNA Methylation kit
- For FFPE samples: use Infinium HD FFPE Restore kit for DNA restoration
Day 2: Array Processing
- Perform whole-genome amplification of bisulfite-converted DNA
- Fragment amplified DNA enzymatically
- Precipitate and resuspend DNA in appropriate hybridization buffer
- Dispense samples onto BeadChip arrays
Day 3: Hybridization and Extension
- Hybridize samples to BeadChips for 16-24 hours
- Perform single-base extension with fluorescently labeled nucleotides
- Resin coat arrays to protect signals
Day 4: Imaging and Data Extraction
- Scan arrays using iScan system
- Generate raw data files with fluorescence intensity data for each probe
- Process data through customized bioinformatics pipelines including removal of poorly performing probes, SNP probes, and sex chromosome probes, with batch corrections and normalization as needed
The integration of AI and machine learning with DNA methylation analysis has created a powerful paradigm for understanding tumor heterogeneity and improving cancer diagnostics. The ability to quantify and interpret DNA methylation heterogeneity within the tumor microenvironment provides unique insights into cellular diversity that complement genetic and transcriptomic approaches. As foundation models like MethylGPT and CpGPT continue to evolve, and as spatial multi-omics technologies mature, the resolution at which we can characterize the TME will further increase.
Future developments will likely focus on enhancing the interpretability of AI models for clinical adoption, standardizing analytical pipelines across platforms, and integrating real-time methylation profiling into therapeutic decision-making. The promising results from paracancerous tissue analysis suggest that methylation patterns in the tumor microenvironment, not just within cancer cells themselves, hold valuable diagnostic and prognostic information [42]. As these technologies mature, they will increasingly enable personalized treatment approaches based on comprehensive molecular profiling of both tumor cells and their microenvironment.
The management of cancer is poised for a transformation driven by liquid biopsy—a minimally invasive approach that analyzes tumor-derived material in bodily fluids. Circulating tumor DNA (ctDNA), a fraction of cell-free DNA (cfDNA) shed into the bloodstream from apoptotic or necrotic tumor cells, has emerged as a particularly powerful analyte for capturing tumor-specific alterations [46] [47]. While genetic mutations in ctDNA are used for companion diagnostics, the analysis of epigenetic modifications, especially DNA methylation, offers a more robust and universally applicable approach for cancer detection and monitoring [47].
DNA methylation involves the addition of a methyl group to the 5' position of cytosine, typically at CpG dinucleotides, regulating gene expression without altering the underlying DNA sequence [48]. In cancer, this process is profoundly dysregulated, characterized by global hypomethylation and site-specific hypermethylation of CpG-rich gene promoters, often silencing critical tumor suppressor genes [48]. These methylation alterations frequently occur early in tumorigenesis and remain stable throughout tumor evolution, making them ideal biomarker candidates [48] [49]. Furthermore, the methylome provides a richer source of biomarkers than mutations; while genetic mutations can be rare and heterogeneous, DNA methylation changes are abundant, tissue-specific, and occur in predictable patterns [50] [49].
This technical guide explores the application of ctDNA methylation analysis in non-invasive cancer diagnostics, with a specific focus on its role in deciphering tumor heterogeneity. Tumor heterogeneity—the molecular variation between different regions of a tumor (spatial heterogeneity) or within a tumor over time (temporal heterogeneity)—poses a significant challenge for cancer diagnosis and treatment [51]. Traditional tissue biopsies capture only a snapshot of this complexity and are impractical for repeated sampling. In contrast, liquid biopsies, through ctDNA methylation profiling, offer a dynamic and comprehensive view of the entire tumor ecosystem, enabling real-time monitoring of clonal evolution and emergent resistance [51]. This whitepaper details the methodologies, clinical applications, and experimental protocols that are positioning ctDNA methylation as an indispensable tool in precision oncology.
Technical Foundations: Methods for ctDNA Methylation Analysis
The successful interrogation of methylation patterns in ctDNA relies on advanced molecular techniques capable of detecting subtle epigenetic signals against a high background of normal cfDNA. The selection of an appropriate method depends on the specific application, required sensitivity, and available resources.
Established Detection Technologies
Established methods range from targeted, cost-effective assays to comprehensive genome-wide sequencing.
- PCR-Based Methods: Techniques like methylation-specific PCR (MSP) and its quantitative counterpart (qMSP) are highly sensitive for validating known hypermethylated loci. Droplet digital PCR (ddPCR) provides absolute quantification of methylation at specific CpG sites, making it particularly suitable for analyzing low-abundance ctDNA in liquid biopsies due to its high sensitivity and resistance to PCR biases [49].
- Methylation BeadChips: Illumina's Infinium MethylationEPIC BeadChip is a high-throughput microarray that Interrogates over 850,000 CpG sites across the genome. It is widely used for biomarker discovery in large cohorts and has been successfully combined with artificial intelligence to develop highly accurate cancer classifiers [52].
- Sequencing-Based Methods:
- Whole-Genome Bisulfite Sequencing (WGBS) is the gold standard for unbiased, base-resolution methylation profiling across the entire genome. Recent advances, such as low-input and low-pass WGBS, have made it more feasible for ctDNA analysis, generating high-quality profiles from as little as 1 ng of input DNA [47] [49].
- Reduced Representation Bisulfite Sequencing (RRBS) provides a cost-effective alternative by enriching for CpG-rich regions of the genome, covering most promoters and enhancers [48] [49].
Emerging and Next-Generation Methodologies
Innovative approaches are continuously being developed to overcome the limitations of traditional techniques, particularly concerning DNA damage and incomplete coverage.
- Bisulfite-Free Sequencing: Methods like Enzymatic Methyl Sequencing (EM-seq) and Tet-assisted pyridine borane sequencing (TAPS) avoid the harsh bisulfite conversion process, which degrades DNA. This preservation of DNA integrity leads to higher library complexity and more accurate sequencing, which is crucial for fragmented ctDNA samples [48] [49].
- Third-Generation Sequencing: Platforms such as Oxford Nanopore and Single-Molecule Real-Time (SMRT) Sequencing enable direct detection of DNA modifications, including methylation, from long-read, native DNA molecules. This allows for the simultaneous assessment of genetic and epigenetic information from the same DNA strand [48].
- Targeted Methylation Sequencing: Approaches like AnchorIRIS and Enhanced Linear-Splinter Amplification Sequencing (ELSA-seq) use hybrid capture or amplicon-based strategies to enrich for panels of cancer-specific methylated regions. This focused method increases sequencing depth on relevant loci, thereby enhancing sensitivity and reducing cost, which is ideal for developing multi-cancer early detection (MCED) tests [49].
Table 1: Comparison of Key ctDNA Methylation Detection Methods
| Method | Principle | Coverage | Sensitivity | Best Use Case |
|---|---|---|---|---|
| ddPCR / qMSP | Locus-specific amplification after bisulfite conversion | Targeted (1-10s of CpGs) | High (0.1%-0.001%) | Validating known biomarkers; minimal residual disease (MRD) monitoring [49] |
| Methylation EPIC Array | Hybridization to probe arrays | Genome-wide (850,000+ CpGs) | Moderate | Biomarker discovery; large cohort studies [52] |
| WGBS | Sequencing after bisulfite conversion | Comprehensive, genome-wide | High (with sufficient depth) | Discovery of novel methylation patterns; comprehensive profiling [48] [49] |
| RRBS | Sequencing of restriction enzyme-digested, bisulfite-converted DNA | CpG-rich regions (promoters, enhancers) | Moderate | Cost-effective discovery in regulatory regions [48] |
| EM-seq / TAPS | Enzymatic conversion or chemical oxidation | Genome-wide | High | Sensitive analysis requiring maximal DNA integrity [48] [49] |
| Targeted Methyl-Seq | Hybrid-capture or PCR of selected regions after bisulfite conversion | Targeted (100s-1000s of CpGs) | Very High | High-sensitivity early detection and MRD assays [49] |
The Scientist's Toolkit: Essential Reagents and Kits
A successful ctDNA methylation workflow depends on specialized reagents and kits optimized for handling low-input, fragmented DNA.
Table 2: Key Research Reagent Solutions for ctDNA Methylation Analysis
| Reagent / Kit | Function | Key Consideration |
|---|---|---|
| Streck Cell-Free DNA BCT Tubes | Blood collection tube that stabilizes nucleated blood cells, preventing genomic DNA contamination and preserving ctDNA profile [52]. | Critical for pre-analytical sample integrity; enables shipment and storage. |
| QIAamp Circulating Nucleic Acid Kit | Extraction of cell-free DNA from plasma, optimized for short-fragment recovery [50] [52]. | High recovery of fragmented ctDNA is essential for sensitivity. |
| EZ DNA Methylation Kit | Bisulfite conversion of unmethylated cytosines to uracils, while methylated cytosines remain protected [52]. | The industry standard; however, causes significant DNA degradation. |
| Illumina Infinium MethylationEPIC BeadChip | Microarray for high-throughput, cost-effective methylation profiling of >850,000 sites [52]. | Ideal for large-scale discovery studies without the need for sequencing. |
| EM-seq Kit | Enzymatic conversion of unmethylated cytosines, avoiding DNA degradation from bisulfite [48]. | Emerging best practice for sequencing-based assays requiring high DNA quality. |
| Plazomicin | Plazomicin | Plazomicin is a next-generation aminoglycoside antibiotic for research against multidrug-resistant bacteria. This product is for Research Use Only (RUO). Not for human use. |
Decoding Heterogeneity: ctDNA Methylation in the Tumor Microenvironment
The analysis of ctDNA methylation provides a unique lens through which to view and decipher the profound heterogeneity of the tumor microenvironment (TME). This heterogeneity exists at multiple levels: between patients (inter-tumor), within a single tumor (spatial intra-tumor), and as the tumor evolves over time (temporal heterogeneity) [51]. ctDNA, shed from various tumor subclones and regions, carries an aggregate signal of this diversity, offering a "molecular summary" of the entire tumor burden that is inaccessible through a single tissue biopsy [51].
Spatial and Temporal Heterogeneity
Spatial heterogeneity arises from distinct geographic regions of a tumor evolving under different selective pressures, leading to subclones with divergent genetic and epigenetic profiles. A tissue biopsy from one region may miss critical driver events present elsewhere. ctDNA methylation analysis circumvents this limitation. For instance, differing methylation patterns in genes like ESR1 and RASSF1A in breast cancer ctDNA can reflect the presence of multiple subclones, each with its own epigenetic identity [50] [49]. This is crucial for selecting effective therapies, as a treatment targeting a pathway active in only a fraction of cells may ultimately fail.
Temporal heterogeneity refers to the evolution of tumor cell populations over time, often in response to therapy. The short half-life of ctDNA (approximately 2 hours) makes it an ideal tool for monitoring this dynamic process in near real-time [53]. The emergence of therapy-resistant clones is often accompanied by distinct methylation changes. For example, hypermethylation of the TMEM240 gene in ctDNA has been linked to poor response to hormone therapy in breast cancer patients [50]. By tracking such methylation markers serially, clinicians can detect resistance early and switch treatments before clinical progression becomes evident.
The Role of the Tumor Microenvironment
The TME, composed of non-malignant cells like cancer-associated fibroblasts (CAFs) and immune cells, is not a passive bystander but an active participant in tumor progression. This cellular ecosystem also exhibits significant heterogeneity [51]. While ctDNA is primarily derived from malignant cells, methylation profiling can indirectly reveal the state of the TME. Certain methylation signatures in ctDNA have been associated with immune cell infiltration and immunosuppressive phenotypes [47]. For example, hypermethylation of STAT5A in squamous cell carcinomas has been linked to regulatory suppression and immune cell depletion, providing an epigenetic insight into the immunosuppressive landscape of the TME [47]. This information could predict response to immunotherapies and guide combination treatment strategies.
Figure 1: Decoding Tumor Heterogeneity via ctDNA Methylation. The primary tumor, comprising spatially distinct subclones, a temporally evolving cell population, and a heterogeneous tumor microenvironment, sheds ctDNA into the bloodstream. A single liquid biopsy captures an aggregate of these signals, providing a comprehensive molecular profile that overcomes the limitations of single-site tissue biopsies.
Clinical Applications and Workflows
The translation of ctDNA methylation analysis from research to clinical practice is accelerating, with applications spanning the entire cancer care continuum.
Key Clinical Applications
Table 3: Clinical Applications of ctDNA Methylation Analysis
| Application | Description | Example |
|---|---|---|
| Early Detection & Diagnosis | Identifying cancer-specific methylation signatures in asymptomatic individuals or those with suspicion of cancer. | The Galleri (GRAIL) and OverC tests, designated FDA Breakthrough Devices, use targeted methylation sequencing for multi-cancer early detection (MCED) [48]. |
| Minimal Residual Disease (MRD) & Recurrence Monitoring | Detecting molecular relapse after curative-intent treatment long before clinical or radiographic recurrence. | Post-surgical presence of ctDNA with specific methylation markers is a highly predictive biomarker of recurrence in colorectal cancer (CRC), enabling consideration of adjuvant therapy [47] [53] [54]. |
| Therapy Selection & Monitoring | Identifying targetable epigenetic alterations and monitoring dynamic changes in methylation patterns during treatment to assess response. | In small cell lung cancer (SCLC), ctDNA methylation analysis can identify molecular subtypes (e.g., SCLC-I) that respond better to immunotherapy combined with chemotherapy [47]. |
| Tissue of Origin Determination | Tracing the primary site of a cancer of unknown origin based on the tissue-specific nature of DNA methylation patterns. | Methylation profiles are highly tissue-specific. When a methylation signature is detected in cfDNA without a known primary, it can be matched to a database to identify the likely origin, guiding subsequent diagnostic workup [47]. |
Integrated Experimental Protocol
A robust workflow for ctDNA methylation analysis involves several critical steps, from sample collection to data interpretation. The following protocol outlines a typical process for a targeted sequencing-based approach, such as that used in many MCED tests.
Sample Collection & Processing:
- Collect peripheral blood (typically 10-20 mL) into cell-stabilizing tubes (e.g., Streck Cell-Free DNA BCT).
- Process within 24-48 hours with a double-centrifugation protocol to obtain platelet-poor plasma.
- Store plasma at -80°C until DNA extraction [52].
cfDNA Extraction & Bisulfite Conversion:
- Extract cfDNA from plasma using a silica-membrane or magnetic bead-based kit optimized for short-fragment recovery (e.g., QIAamp Circulating Nucleic Acid Kit).
- Quantify extracted cfDNA using a fluorescence-based assay sensitive to low concentrations.
- Subject a defined amount of cfDNA (e.g., 10-30 ng) to bisulfite conversion using a commercial kit (e.g., EZ DNA Methylation Kit). This step deaminates unmethylated cytosines to uracils, while methylated cytosines remain as cytosines [52] [49].
Library Preparation & Targeted Enrichment:
- Prepare sequencing libraries from bisulfite-converted DNA. This involves end-repair, adapter ligation, and limited-cycle PCR amplification.
- For targeted approaches, perform hybrid capture using biotinylated probes designed to enrich for a pre-defined panel of several thousand hypermethylated regions associated with cancer. Alternatively, use a multiplex PCR (amplicon) approach.
- Amplify the enriched libraries and validate quality using capillary electrophoresis [49].
Sequencing & Bioinformatic Analysis:
- Sequence the libraries on a high-throughput platform (e.g., Illumina NovaSeq) to a sufficient depth (e.g., 10,000x - 30,000x coverage).
- Perform bioinformatic analysis:
- Alignment: Map bisulfite-converted reads to a in-silico bisulfite-converted reference genome.
- Methylation Calling: Calculate methylation ratios (β-values) at each CpG site by comparing base calls (C for methylated, T for unmethylated) to the reference sequence.
- Classification: Input the methylation data into a machine learning classifier (e.g., Random Forest, Support Vector Machine, Deep Learning) trained on reference datasets of cancer and normal methylation profiles to generate a cancer probability score and, if applicable, a predicted tissue of origin [52] [49].
Figure 2: ctDNA Methylation Analysis Workflow. The process begins with blood collection and plasma separation, followed by cfDNA extraction and bisulfite conversion. Libraries are prepared and enriched for cancer-specific regions before sequencing. Bioinformatics pipelines align reads and call methylation, with final classification performed by machine learning models.
The mining of ctDNA methylation for non-invasive diagnostics represents a paradigm shift in oncology. By providing a stable, abundant, and information-rich source of tumor-specific data, DNA methylation overcomes many limitations of mutation-based liquid biopsies. Its unique capacity to reflect the complex spatial and temporal heterogeneity of the tumor microenvironment, coupled with the inherent tissue specificity of epigenetic patterns, makes it an unparalleled tool for comprehensive tumor profiling.
As bisulfite-free sequencing methods mature and machine learning algorithms become more sophisticated, the sensitivity and specificity of methylation-based assays will continue to improve, particularly for the early detection of low-ctDNA tumors. The ongoing integration of multi-omics data—combining methylation with fragmentomics, copy number alterations, and proteomics—promises to further enhance diagnostic accuracy. For researchers and drug developers, ctDNA methylation is not merely a diagnostic tool but a dynamic window into tumor biology, enabling a deeper understanding of disease mechanisms, therapy resistance, and the path toward truly personalized cancer medicine.
Navigating Technical and Biological Challenges in DNAmeH Analysis
In the study of DNA methylation heterogeneity (DNAmeH) within the tumor microenvironment (TME), technical noise from batch effects and platform-specific biases presents a fundamental challenge to data integrity and biological interpretation. DNA methylation is a key epigenetic modification that regulates gene expression by adding methyl groups to cytosine bases, primarily at CpG dinucleotides, without changing the underlying DNA sequence [41]. In cancer, these patterns are frequently altered, with tumors typically displaying both genome-wide hypomethylation and hypermethylation of CpG-rich gene promoters [48]. The inherent stability of DNA methylation and its emergence early in tumorigenesis make it particularly valuable for cancer research and clinical biomarker development [48].
However, the diverse cell compositions within the TME create complex methylation patterns that technical artifacts can easily obscure. Batch effects occur when technical variations—such as differences in library preparation, sequencing runs, reagent lots, instrument calibration, or sample handling—create systematic biases in data [55] [56]. In multi-omics studies, these effects are particularly problematic as each data type carries its own sources of noise, and integration across layers multiplies complexity [55]. Left uncorrected, batch effects generate misleading results, mask true biological signals, delay translational research, and ultimately jeopardize the identification of robust biomarkers that persist across biological layers [55]. As tumor methylation research increasingly focuses on subtle heterogeneity patterns within complex microenvironments, addressing these technical challenges becomes indispensable for meaningful scientific discovery.
Understanding Batch Effects in DNA Methylation Analysis
Batch effects in DNA methylation analysis arise from multiple technical sources throughout the experimental workflow. In microarray-based approaches, differences in sample processing times, reagent lots, array chips, and scanner settings can introduce systematic variations [57]. For sequencing-based methods, inconsistencies in bisulfite conversion efficiency, library preparation protocols, sequencing depth, and instrument performance across runs create substantial technical noise [41] [56]. Even sample collection and storage conditions can contribute to batch effects, particularly when comparing samples processed at different times or locations [58].
The consequences of uncorrected batch effects are severe in tumor methylation studies. They can create false positives where technical artifacts are mistaken for biologically significant methylation patterns, or false negatives where true biological signals are obscured by technical noise [55] [58]. This is particularly problematic when studying DNA methylation heterogeneity in complex tumor environments, where subtle but biologically important methylation differences between cell populations may be lost in technical variation. The reproducibility crisis in omics research has been largely attributed to batch effects, with findings from one laboratory failing to validate in another due to uncontrolled technical variables [56]. In clinical translation, batch effects can compromise the development of reliable diagnostic biomarkers, as technical rather than biological differences may drive apparent methylation signatures [48].
Quantitative Assessment of Batch Effects
Before implementing correction strategies, researchers must first quantify the presence and magnitude of batch effects in their data. Several statistical approaches have been developed for this purpose, each with specific strengths for different data types.
Table 1: Methods for Quantifying Batch Effects in Methylation Data
| Method | Principle | Application Context | Interpretation |
|---|---|---|---|
| kBET [56] | K-nearest neighbor batch effect test measures local batch mixing | Single-cell and bulk methylation data | Lower p-values indicate significant batch separation |
| PCA Visualization [56] | Dimensionality reduction to visualize sample clustering by batch | Exploratory analysis of all methylation data types | Clustering by batch rather than biology indicates strong batch effects |
| Average Silhouette Width [56] | Measures how similar samples are to their cluster versus neighboring clusters | Validation after correction | Values near 1 indicate good mixing; near 0 or negative indicate poor mixing |
| APITH Index [59] | Average Pairwise Intra-Tumoral Heterogeneity quantifies methylation diversity | Multi-region tumor methylation studies | Higher values indicate greater heterogeneity within a tumor |
For DNA methylation data specifically, the Average Pairwise Intra-Tumoral Heterogeneity (APITH) index has been developed as a validated metric to quantify intra-tumoral heterogeneity independently of the number of tumor samples evaluated [59]. This approach is particularly valuable in multi-region methylation studies of solid tumors, where distinguishing technical artifacts from true biological heterogeneity is essential.
Batch Effect Correction Methodologies
Established Correction Algorithms
Multiple computational approaches have been developed to address batch effects in DNA methylation data, ranging from traditional statistical methods to emerging machine learning techniques.
Table 2: Batch Effect Correction Methods for DNA Methylation Data
| Method | Underlying Principle | Strengths | Limitations |
|---|---|---|---|
| ComBat [57] | Empirical Bayes framework with location/scale adjustment | Robust for small sample sizes; widely validated | Linear assumptions; may not capture complex nonlinear effects |
| iComBat [57] | Incremental version of ComBat for sequential data | No reprocessing of existing data when adding new batches | Relatively new method with limited implementation |
| Quantile Normalization [57] | Standardizes signal intensity distributions across samples | Simple, fast computation | Assumes identical distribution across batches |
| SVA/RUV [57] | Removes unobserved sources of variation via latent factors | Captures unknown covariates; flexible | Risk of removing biological signal if not carefully tuned |
| Harmony [55] | Iterative clustering and integration using PCA | Effective for complex single-cell data | Computational intensity for very large datasets |
| Deep Learning Methods [41] [56] | Autoencoders learn nonlinear data representations | Captures complex batch effects; no linear assumptions | Large sample size requirements; "black box" interpretation |
The ComBat algorithm deserves particular attention as it remains one of the most widely used methods for DNA methylation data. ComBat employs a location/scale adjustment model that corrects data across batches by adjusting the mean and scale parameters using empirical Bayes estimation within a hierarchical model [57]. This approach borrows information across methylation sites within each batch, providing stability even with small sample sizes. The standard ComBat model can be represented as:
Yijg = αg + Xijᵀβg + γig + δigεijg
Where Yijg is the M-value for batch i, sample j, and methylation site g; αg is the site-specific effect; Xijᵀβg represents covariate effects; γig and δig are the additive and multiplicative batch effects respectively; and εijg is the error term [57].
The iComBat Framework for Longitudinal Studies
For long-term methylation studies involving repeated measurements, the incremental iComBat framework represents a significant advancement [57]. Traditional batch correction methods require simultaneous processing of all samples, meaning that adding new batches necessitates re-processing all existing data—a computationally expensive and potentially disruptive process. iComBat addresses this limitation by enabling correction of newly included data without modifying already-corrected existing data, maintaining consistent interpretation across the entire dataset [57].
The iComBat methodology follows a multi-step process: (1) initial estimation of global parameters (αg, βg, σg) for each methylation site using ordinary least squares; (2) standardization of observed data; (3) estimation of batch effect parameters using empirical Bayes methods; and (4) application of location and scale adjustments to remove batch effects while preserving biological signals [57]. This approach is particularly valuable for clinical trials of anti-aging interventions or long-term cancer monitoring studies based on DNA methylation or epigenetic clocks, where data collection occurs sequentially over extended periods.
Experimental Design Strategies for Batch Effect Prevention
While computational correction is essential, optimal experimental design remains the most effective strategy for minimizing batch effects:
- Randomization: Distribute biological groups and sample types across processing batches rather than processing all samples from one condition together [56]
- Balanced Processing: Ensure each batch contains similar numbers of cases and controls, and process samples in a balanced order to avoid confounding biological conditions with processing time [58]
- Reference Standards: Include control reference samples in each batch to monitor technical variability—the IROA technologies approach using isotopic labeling provides one such framework [58]
- Replication: Incorporate technical replicates across batches to assess reproducibility and provide anchors for batch correction algorithms [56]
- Metadata Documentation: Meticulously record all processing variables (dates, technicians, reagent lots) to facilitate proper modeling of batch effects during analysis [55]
Batch Effect Sources in Methylation Workflow
Platform-Specific Biases in Methylation Analysis
Comparative Analysis of Methylation Platforms
Different DNA methylation analysis platforms exhibit distinct technical characteristics, coverage biases, and resolution capabilities that must be considered when integrating data across platforms or comparing results across studies.
Table 3: Technical Characteristics of Major DNA Methylation Analysis Platforms
| Platform/Method | Coverage | Resolution | DNA Input | Cost | Primary Applications |
|---|---|---|---|---|---|
| Infinium Methylation BeadChip [41] | ~850,000 CpG sites | Single CpG | 250-500 ng | Moderate | EWAS, biomarker validation |
| Whole-Genome Bisulfite Sequencing (WGBS) [41] [48] | Genome-wide | Single-base | 100-200 ng | High | Discovery, comprehensive profiling |
| Reduced Representation Bisulfite Sequencing (RRBS) [41] [48] | ~2-3 million CpGs | Single-base | 100-200 ng | Moderate-high | CpG island and promoter regions |
| Enzymatic Methyl-Sequencing (EM-seq) [48] | Genome-wide | Single-base | 100-200 ng | High | Preservation of DNA integrity |
| Methylated DNA Immunoprecipitation (MeDIP) [41] | Enriched methylated regions | ~100-500 bp | 50-100 ng | Moderate | Methylome enrichment studies |
| Pyrosequencing [41] | Targeted loci | Single CpG | 10-50 ng | Low | Validation, specific loci |
Each platform demonstrates specific biases in CpG coverage, with bead arrays focusing on predefined CpG sites of biological interest, while sequencing methods offer more comprehensive coverage but with varying efficiency across genomic regions [41]. WGBS provides the most comprehensive coverage but remains cost-prohibitive for large studies, while bead arrays offer a practical balance between coverage, cost, and throughput for epidemiological and clinical studies [41] [48].
Cross-Platform Harmonization Strategies
Integrating DNA methylation data across different platforms requires careful consideration of several technical factors:
- Probe Mapping: When comparing array and sequencing data, ensure consistent genomic coordinate systems and account for probe binding efficiency variations in array-based methods [41]
- Coverage Imputation: For sites missing in one platform but present in another, imputation methods can be employed, though with careful validation—foundation models like MethylGPT show promise for this application [41]
- Batch Effect Correction Across Platforms: Treat different platforms as distinct batches in correction algorithms, using overlapping samples or reference standards to establish correspondence [56]
- Validation with Targeted Methods: Use highly quantitative targeted methods like pyrosequencing or digital PCR to validate cross-platform findings for critical CpG sites [48]
The emerging generation of foundation models pretrained on extensive methylome datasets (e.g., MethylGPT trained on >150,000 human methylomes) offers promising approaches for cross-platform harmonization by learning generalizable representations of methylation patterns that transfer across measurement technologies [41].
DNA Methylation Heterogeneity in Tumor Microenvironments
Analytical Frameworks for Tumor Methylation Heterogeneity
The tumor microenvironment comprises multiple cell types—cancer cells, fibroblasts, immune cells, and vascular cells—each with distinct methylation patterns. This cellular complexity creates challenges in distinguishing true methylation heterogeneity from technical artifacts. Several analytical frameworks have been developed specifically to address this challenge:
Deconvolution Approaches: These methods computationally separate the methylation signal of tumor samples into constituent cell types using reference methylation profiles of pure cell populations. A recent pan-cancer study identified 1,256 immune cell population-specific methylation markers to deconvolute 5,323 tumor samples across 14 cancer types, revealing significant immune heterogeneity between subtypes [2]. The mathematical foundation of deconvolution represents tissue methylation data as a linear combination of cell type-specific methylation patterns weighted by cell type proportions:
yᵢ = ∑ⱼ xᵢⱼpⱼ + εᵢ
Where yᵢ is the methylation value for gene i in the tissue sample, xᵢⱼ is the methylation level for gene i in cell type j, pⱼ is the proportion of cell type j, and εᵢ represents error term [2].
Epipolymorphism Analysis: This approach quantifies methylation heterogeneity within individual samples by measuring the probability that two randomly sampled DNA molecules from the same locus differ in their methylation status [59]. In clear cell renal cell carcinoma, differential epipolymorphism between tumor and normal tissue in gene promoters has been shown to predict gene expression independent of average methylation levels, providing insights into tumor evolution and functional heterogeneity [59].
Single-Cell Methylation Profiling: Techniques like single-cell bisulfite sequencing (scBS-Seq) enable direct assessment of methylation heterogeneity at cellular resolution, revealing methylation patterns in individual cells within complex tissues [41]. While technically challenging and computationally intensive, this approach provides the most direct window into cellular heterogeneity without requiring computational deconvolution.
Case Study: Multi-Region Methylation Analysis in Renal Cancer
A comprehensive multi-region study of clear cell renal cell carcinoma (ccRCC) illustrates both the challenges and solutions for analyzing methylation heterogeneity in complex tumors. This research generated DNA methylation data from 136 multi-region tumor and normal tissue samples from 18 ccRCC patients, with matched whole exome sequencing and gene expression data for subsets [59].
The study revealed that while most tumors showed greater methylation heterogeneity between patients than within a single patient, there were notable exceptions with substantial intra-tumoral heterogeneity [59]. Comparison of phylogenetic trees based on copy number alterations and methylation patterns revealed variable evolutionary relationships—while some patients showed similar genetic and epigenetic trees suggesting co-evolution, others demonstrated distinctly different patterns indicating independent evolution of genetic and epigenetic alterations [59].
This case study highlights the importance of multi-region sampling and integrated analysis approaches for properly characterizing tumor methylation heterogeneity and distinguishing technical artifacts from true biological variation.
Multi-Region Methylation Analysis Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential Research Reagents for Methylation Studies Resistant to Batch Effects
| Reagent/Solution | Function | Batch Effect Consideration | Application Context |
|---|---|---|---|
| IROA Isotopic Standards [58] | Mass spectrometry internal standards for metabolomics | Enables precise correction of technical variation | Metabolomic integration with methylation data |
| Bisulfite Conversion Kits | Converts unmethylated cytosines to uracils | Efficiency variations create batch effects; require standardization | All bisulfite-based methylation analyses |
| Universal Methylated Controls | Reference samples for normalization | Allows cross-batch comparability | Quality control across experiments |
| Cell Type-Specific Methylation Panels [2] | 1,256 immune cell-specific methylation markers | Standardized deconvolution reference | Tumor microenvironment analysis |
| EM-seq Enzymatic Conversion [48] | Enzymatic alternative to bisulfite conversion | Reduces DNA degradation bias | Liquid biopsy with limited DNA |
| Methylated DNA Immunoprecipitation Antibodies [41] | Enriches methylated DNA fragments | Antibody lot variations require normalization | Enrichment-based methylation studies |
Best Practices and Validation Framework
Integrated Quality Control Pipeline
Implementing a robust quality control and validation framework is essential for ensuring that batch effect correction preserves biological signals while removing technical noise:
- Pre-Correction Assessment: Quantify batch effects using kBET, PCA visualization, or other appropriate metrics before applying corrections [56]
- Staged Correction Approach: Apply correction methods sequentially, starting with the least aggressive approach and monitoring impact on biological variables of interest
- Positive Control Validation: Verify that known biological differences (e.g., tumor vs normal, established subtype differences) persist after correction using positive control samples [55]
- Negative Control Verification: Confirm that technical replicates cluster together after correction, indicating successful removal of batch effects [58]
- Independent Validation: Validate findings in independently processed sample sets to confirm that results generalize beyond the discovery cohort [48]
Emerging Solutions and Future Directions
The field of batch effect management continues to evolve with several promising developments:
- Foundation Models: Models like MethylGPT and CpGPT, pretrained on large methylome datasets, show robust cross-cohort generalization and offer task-agnostic approaches to methylation analysis [41]
- Multi-Omics Integration Platforms: Commercial solutions like Pluto Bio provide unified platforms for multi-omics data harmonization without requiring coding expertise, though careful validation remains essential [55]
- Agentic AI Systems: Emerging autonomous or multi-agent systems show potential for orchestrating comprehensive bioinformatics workflows including quality control, normalization, and batch correction with human oversight [41]
- Longitudinal Correction Methods: Incremental approaches like iComBat address the growing need for long-term studies with sequential data collection [57]
As DNA methylation analysis continues to advance toward clinical applications—particularly in liquid biopsy for early cancer detection—rigorous attention to batch effects and platform biases will remain essential for developing robust, reproducible biomarkers that successfully translate from research to clinical practice [48].
Optimizing Biomarker Selection for Sensitivity, Specificity, and Clinical Utility
In the evolving landscape of oncology, biomarkers have transitioned from ancillary diagnostic tools to fundamental components of precision medicine. Broadly defined as measurable indicators of biological processes, pathogenic states, or pharmacological responses to therapeutic intervention, biomarkers provide critical insights into disease diagnosis, prognosis, and treatment selection [60]. The optimization of biomarker selection represents a significant methodological challenge, requiring careful balancing of analytical performance metrics—primarily sensitivity and specificity—with demonstrated clinical utility that directly impacts patient management and outcomes [60] [61].
Within the complex ecosystem of the tumor microenvironment (TME), DNA methylation heterogeneity (DNAmeH) has emerged as a particularly promising class of biomarker. This epigenetic modification, primarily involving 5-methylcytosine (5mC), exhibits remarkable stability and cell lineage specificity, making it an ideal candidate for deciphering tumor biology [3] [8]. Intratumoral and intertumoral DNAmeH arises from both cancer epigenome heterogeneity and the diverse cellular compositions within the TME, creating distinct patterns that can be quantitatively measured through advanced technologies [3]. This technical guide provides a comprehensive framework for optimizing biomarker selection, with specific emphasis on DNA methylation biomarkers in TME research, addressing both methodological rigor and clinical relevance for researchers, scientists, and drug development professionals.
Foundational Concepts: From Analytical Performance to Clinical Value
Defining Key Performance Metrics
The evaluation of biomarker performance begins with fundamental metrics that quantify test characteristics. These metrics provide the foundation for understanding how a biomarker distinguishes between disease states and informs clinical decision-making.
Table 1: Core Biomarker Performance Metrics and Definitions
| Metric | Definition | Clinical Interpretation |
|---|---|---|
| Sensitivity | Proportion of true positives correctly identified | Ability to detect disease when present |
| Specificity | Proportion of true negatives correctly identified | Ability to exclude disease when absent |
| Positive Predictive Value (PPV) | Probability that a positive test indicates true disease | Depends on prevalence and test performance |
| Negative Predictive Value (NPV) | Probability that a negative test excludes disease | Depends on prevalence and test performance |
| Area Under Curve (AUC) | Overall measure of discriminative ability | Value of 1.0 indicates perfect discrimination |
| Likelihood Ratio | How much a test result changes odds of disease | Combines sensitivity and specificity into single metric |
These conventional metrics, while essential, primarily describe test characteristics in isolation. To fully assess a biomarker's value in clinical practice, researchers must evaluate how these metrics translate into tangible health impacts through three fundamental mechanisms: (1) improving patient understanding of disease or risk, thereby directly enhancing quality of life or mental health; (2) motivating patients to adopt health-promoting behaviors or treatment adherence; and (3) enabling clinicians to make better treatment decisions that improve patient outcomes [60].
The Clinical Utility Paradigm
Clinical utility extends beyond traditional performance metrics to encompass the test's actual impact on health outcomes when integrated into clinical practice. A biomarker with excellent sensitivity and specificity may lack clinical utility if it does not lead to improved patient management or outcomes [61]. The highest level of evidence for clinical utility typically comes from randomized controlled trials (RCTs) where participants are assigned to strategies that either incorporate or omit the biomarker measurement, with subsequent comparison of health outcomes between groups [60].
Alternative methods for establishing clinical utility include systematic reviews, post-market surveillance, expert opinion, cost-effectiveness analysis, and decision analysis modeling [61]. The appropriate evidence threshold depends on factors such as the significance of the clinical outcome (e.g., mortality reduction versus symptom management) and the potential risks associated with incorrect test results [61].
Quantitative Frameworks for Biomarker Evaluation and Cut-Point Optimization
Clinical Utility-Based Cut-Point Selection
Traditional cut-point selection methods focused primarily on maximizing accuracy metrics, but emerging approaches now incorporate clinical consequences directly into the optimization process. Four clinical utility-based methods have been developed for cut-point selection, each with distinct mathematical foundations and clinical interpretations [62].
Table 2: Clinical Utility-Based Methods for Cut-Point Selection
| Method | Objective | Formula | Interpretation |
|---|---|---|---|
| Youden-Based Clinical Utility (YBCUT) | Maximize total clinical utility | PCUT + NCUT | Balances positive and negative utility |
| Product-Based Clinical Utility (PBCUT) | Maximize product of utilities | PCUT × NCUT | Emphasizes balanced performance |
| Union-Based Clinical Utility (UBCUT) | Minimize utility imbalance | ∣PCUT - AUC∣ + ∣NCUT - AUC∣ | Aligns utilities with overall accuracy |
| Absolute Difference of Total Utility (ADTCUT) | Minimize difference from optimal | ∣(PCUT + NCUT) - 2×AUC∣ | Compares total utility to maximum potential |
Where:
- PCUT (Positive Clinical Utility) = Sensitivity × PPV
- NCUT (Negative Clinical Utility) = Specificity × NPV
- AUC = Area Under the ROC Curve
These utility-based methods demonstrate particular importance in scenarios with low disease prevalence (<10%) and skewed distributions of test results, where traditional accuracy-based cut-points may diverge significantly from those optimizing clinical outcomes [62]. For high AUC values (>0.90) and prevalence exceeding 10%, the four methods typically yield similar optimal cut-points [62].
Integrated Evaluation Framework
A comprehensive biomarker evaluation requires phased evidence development, beginning with establishing statistical association with the clinical state of interest, then demonstrating incremental information beyond established markers, and ultimately quantifying impact on clinical decision-making and patient outcomes [60]. This phased approach ensures that biomarkers advancing to clinical implementation provide genuine health benefits rather than merely statistical significance.
DNA Methylation Heterogeneity in the Tumor Microenvironment: A Paradigm for Biomarker Optimization
Biological Foundations of DNA Methylation Biomarkers
DNA methylation heterogeneity represents a particularly promising class of biomarkers due to its stability, cell-type specificity, and direct relationship to transcriptional regulation. The DNA methylation landscape within the TME arises from the complex interplay between neoplastic cells and diverse non-malignant components, including immune cells, cancer-associated fibroblasts, and vascular elements [3] [8]. This cellular diversity creates distinct methylation patterns that can be deconvoluted to infer TME composition and biological behavior [8].
In metastatic melanoma, integrated multi-omics profiling has revealed four distinct tumor subsets based on global DNA methylation patterns: DEMethylated, LOW, INTermediate, and CIMP (CpG Island Methylator Phenotype) classes, with progressively increasing methylation levels [63]. These methylation classes demonstrate significant clinical relevance, with patients bearing LOW methylation tumors showing significantly longer survival and reduced progression to advanced stages compared to those with CIMP tumors [63]. Similarly, in pancreatic ductal adenocarcinoma (PDAC), DNA methylation profiling has identified distinct tumor groups with varying KRAS mutation frequencies, tumor purity, and survival outcomes [8].
Analytical Methodologies for DNA Methylation Biomarker Development
The development of robust DNA methylation biomarkers requires specialized methodologies for methylation assessment, data processing, and analytical validation.
Experimental Workflow for DNA Methylation Analysis:
DNA Methylation Analysis Workflow
Reduced Representation Bisulfite Sequencing (RRBS) Protocol:
- Sample Preparation: Extract high-quality DNA from tumor tissues (FFPE or fresh frozen) with quality controls including TapeStation analysis and DNA integrity number (DIN) assessment [63].
- Bisulfite Conversion: Treat DNA with sodium bisulfite, converting unmethylated cytosines to uracils while preserving methylated cytosines. Include unmethylated lambda phage DNA spike-in to estimate conversion efficiency [63].
- Library Preparation: Use enzymatic digestion (typically Mspl) to generate reduced representation fragments, followed by end-repair, adapter ligation, and size selection [63].
- Sequencing: Perform high-throughput sequencing on platforms such as Illumina NovaSeq6000 with paired-end 150bp reads [63].
- Bioinformatic Processing:
- Trim adapters and quality filter using Trim Galore and FastQC
- Map reads to reference genome (GRCh38/hg38) using Bismark with default parameters
- Extract methylation data as β-values for CpG sites using RnBeads package
- Perform differential methylation analysis identifying hypo- and hypermethylated regions [63]
TME Deconvolution Analysis: Leveraging the cell-type specificity of DNA methylation patterns, computational deconvolution methods can infer the relative proportions of immune and stromal cell populations within bulk tumor samples [8]. This approach typically involves:
- Reference-based deconvolution using methylation signatures of pure cell types
- Unsupervised clustering to identify intrinsic methylation subtypes
- Correlation with transcriptional data to validate biological interpretations
- Association with clinical outcomes to establish prognostic significance [8]
Translating DNA Methylation Biomarkers to Clinical Application
Clinical Utility in Immunotherapy Response Prediction
The clinical utility of DNA methylation biomarkers is particularly evident in predicting response to immune checkpoint blockade (ICB) therapy. In metastatic melanoma, patients with DEM/LOW methylation pre-therapy lesions showed significantly longer relapse-free survival following adjuvant ICB compared to those with INT/CIMP lesions [63]. This association reflects underlying biological differences: LOW methylation tumors exhibit enrichment of pre-exhausted and exhausted T-cell populations, retained HLA Class I antigen expression, and a de-differentiated melanoma phenotype—all features associated with enhanced immune recognition and response to immunotherapy [63].
Treatment of differentiated melanoma cell lines with DNA methyltransferase inhibitors (DNMTi) induces global DNA demethylation, promotes dedifferentiation, and upregulates viral mimicry and IFNG predictive signatures of immunotherapy response, providing mechanistic validation of the causal role of DNA methylation in shaping the tumor-immune interface [63].
Integration into Comprehensive Biomarker Frameworks
DNA methylation biomarkers demonstrate greatest clinical utility when integrated into comprehensive multimodal frameworks that incorporate genetic, transcriptomic, proteomic, and histopathological data [64]. Such integrated approaches generate a molecular "fingerprint" for each patient, supporting individualized diagnosis, prognosis, treatment selection, and response monitoring [64]. This is particularly valuable for addressing tumor heterogeneity and immune evasion mechanisms that limit the effectiveness of single-marker approaches.
Table 3: Research Reagent Solutions for DNA Methylation Biomarker Development
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| DNA Extraction Kits | Maxwell RSC FFPE Plus DNA Kit | High-quality DNA from FFPE tissues |
| Bisulfite Conversion | Ovation RRBS Methyl-Seq Kit | Library preparation for methylation sequencing |
| Quality Control | TapeStation Genomic DNA ScreenTape, Qubit Fluorometer | Assess DNA quantity and integrity |
| Methylation Arrays | EPIC BeadChip | Genome-wide methylation profiling |
| Enzymatic Digestion | Mspl restriction enzyme | RRBS library preparation |
| Bioinformatic Tools | Bismark, RnBeads, Trim Galore | Read alignment, methylation calling, QC |
| Reference Materials | Unmethylated lambda phage DNA | Bisulfite conversion efficiency control |
| DNMT Inhibitors | Decitabine, Azacitidine | Experimental validation of methylation effects |
Optimizing biomarker selection for sensitivity, specificity, and clinical utility requires a multifaceted approach that balances statistical performance with demonstrable patient benefit. DNA methylation heterogeneity within the TME provides a powerful paradigm for biomarker development, offering stable, cell-type-specific signals that reflect underlying biological processes and predict therapeutic responses. The integration of quantitative cut-point selection methods with comprehensive multi-omics frameworks enables researchers to develop biomarkers that not only classify disease states but also directly inform clinical decision-making. As biomarker science continues to evolve, emphasis on clinical utility—measured through impact on patient outcomes, clinical decisions, and healthcare resource utilization—will ensure that novel biomarkers translate into genuine improvements in cancer care.
Benchmarking Biomarkers and Validating Clinical Utility Across Cancers
DNA methylation heterogeneity (DNAmeH) is a fundamental characteristic of the tumor microenvironment (TME), arising from diverse cell compositions and cancer epigenome variability [3]. This heterogeneity manifests as intratumoral (within individual tumors) and intertumoral (between different tumors) variations in 5-methylcytosine (5mC) patterns, significantly influencing tumor progression, therapeutic response, and clinical outcomes [3] [8]. The complex ecosystem of the TME—comprising malignant cells, immune infiltrates, stromal elements, and extracellular matrix—creates distinct epigenetic landscapes that can be deciphered through advanced profiling technologies [8].
DNA methylation biomarkers offer exceptional promise in clinical oncology due to their stability, early emergence in tumorigenesis, and cell lineage specificity [48] [65]. Unlike genetic mutations, epigenetic modifications are reversible and reflect dynamic interactions between tumor cells and their microenvironment [3]. This review examines validated DNA methylation biomarkers across three major cancers—colorectal, breast, and ovarian—within the context of TME heterogeneity, exploring their clinical applications, validation methodologies, and implications for precision oncology.
Colorectal Cancer Methylation Biomarkers
Clinically Implemented and Novel Biomarkers
Colorectal cancer (CRC) has been at the forefront of DNA methylation biomarker implementation, with several markers receiving FDA approval for clinical use. The current landscape includes both established biomarkers used in screening and novel biomarkers under investigation for improved diagnosis and risk stratification.
Table 1: Validated DNA Methylation Biomarkers in Colorectal Cancer
| Biomarker | Biological Function | Sample Type | Clinical Application | Performance/Notes |
|---|---|---|---|---|
| SEPT9 [66] | Cytoskeleton organization, cell division | Blood | FDA-approved for blood-based screening | Detects methylated SEPT9 in circulating tumor DNA |
| NDRG4/BMP3 [66] | Tumor suppressor activity | Stool | FDA-approved for stool-based tests | Combined biomarker approach for enhanced sensitivity |
| 27-Gene Panel [67] | Multiple pathways | Tumor tissue | Prognostic risk stratification for stage II CC | Stratifies high-risk recurrence; integrates clinical factors |
| GNG7 [66] | G-protein signaling | Tumor tissue | Candidate diagnostic biomarker | Identified via integrated methylome-transcriptome analysis |
| PDX1 [66] | Transcription factor | Tumor tissue | Candidate diagnostic biomarker | Common across all cohorts in multi-dataset study |
Biomarkers for Risk Stratification in Stage II Disease
A significant advancement in CRC methylation biomarkers is the development of a 27-gene methylation panel for stratifying recurrence risk in stage II colon cancer patients. This panel was identified through genome-wide tumor tissue DNA methylation analysis of 562 stage II CC patients, with external validation performed on an independent cohort [67]. The prognostic index (PI) incorporates both clinical factors (age, sex, tumor stage, location) and methylation markers, demonstrating consistently improved time-dependent AUC compared to baseline models in both internal (AUC: 0.66 vs. 0.52) and external validation (AUC: 0.72 vs. 0.64) cohorts [67].
The discovery methodology involved rigorous bioinformatic approaches. Differential analysis identified differentially methylated CPG sites (DMCs) using the Limma package with thresholds of Adj.P.Value < 0.05 and log2FC > 1 for rectal cancer, and more stringent thresholds (Adj.P.Value < 0.01 and log2FC > 2) for colon cancer due to larger sample sizes [66]. Integration of DMCs with differentially expressed genes (DEGs) identified 150 candidate methylation-regulated genes, with GNG7 and PDX1 emerging as common across all cohorts [66].
Breast Cancer Methylation Biomarkers
SEPT9 in Breast Cancer Progression and Diagnosis
SEPT9 methylation has emerged as a significant biomarker beyond colorectal cancer, demonstrating particular utility in distinguishing breast cancer progression stages. A 2025 study investigated SEPT9 methylation across 105 breast cancer cases classified into pure ductal carcinoma in situ (DCIS), DCIS with invasive components (DCIS-INV), invasive ductal carcinoma (IDC) alone, and metastatic breast cancer (MBC) [68].
Table 2: SEPT9 Methylation in Breast Cancer Progression
| Cancer Type/Stage | SEPT9 Methylation Positivity Rate | Clinical Significance |
|---|---|---|
| Pure DCIS [68] | 18.2% | Limited utility in low-grade DCIS |
| DCIS with Invasion [68] | 90.6% | Strong indicator of invasive potential |
| Invasive Ductal Carcinoma [68] | 77.8% | Diagnostic marker for invasive disease |
| Metastatic Breast Cancer [68] | 79.2% | Associated with advanced disease |
| Intermediate-High Grade DCIS [68] | 28.6% | Identifies high-risk DCIS lesions |
The study revealed striking differences in SEPT9 methylation positivity across disease stages, with significantly elevated rates in invasive and metastatic cases compared to pure DCIS [68]. Positive methylation status was significantly associated with high Ki-67 expression and lymph node metastasis, but showed no correlation with age, menopausal status, tumor size, or hormone receptor status [68]. Mechanistic investigations demonstrated that decitabine treatment reduced SEPT9 methylation levels and affected microtubule stability, suggesting a potential link to tumor invasion [68].
Prognostic Methylation Signatures
Beyond SEPT9, comprehensive methylation signatures have been developed for breast cancer prognosis. A 14-CpG DNA methylation signature was developed and validated using data from TCGA and GEO databases, significantly associated with progression-free interval (PFI), disease-specific survival (DSS), and overall survival (OS) in breast cancer patients [69].
The model construction involved identifying 216 differentially methylated CpGs by intersecting three datasets (TCGA, GSE22249, and GSE66695). Through univariate Cox proportional hazard and LASSO Cox regression analyses, the 14 most prognostically significant CpGs were selected [69]. The risk score was calculated using the formula: Risk score = Σ(Expn × βn), where Expn is the β-value of each CpG and βn is the corresponding coefficient [69]. Kaplan-Meier survival analysis effectively distinguished high-risk from low-risk patients, and ROC analysis demonstrated high sensitivity and specificity in predicting breast cancer prognosis [69].
Ovarian Cancer Methylation Biomarkers
Biomarkers for Chemoresistance and Survival
Ovarian cancer management faces significant challenges due to frequent chemoresistance development, and DNA methylation biomarkers offer promising solutions for predicting treatment response and survival outcomes.
Table 3: DNA Methylation Biomarkers in Ovarian Cancer
| Biomarker | Function | Methylation Change | Clinical Association | Validation |
|---|---|---|---|---|
| PLAT-M8 [70] | 8-CpG signature | Hypermethylation | Shorter OS in relapsed OC; predicts platinum response | Validated in BriTROC-1 (n=47) and OV04 (n=57) cohorts |
| CD58 [71] | Immune regulation | Hypermethylation (∆β=64%) | Poor prognosis in HGSC | Identified via HM850K array; associated with chemoresistance |
| SOX17 [71] | Transcription factor | Hypermethylation (∆β=79%) | Poor prognosis in HGSC | Top hypermethylated CpG in chemoresistant cells |
| FOXA1 [71] | Transcription factor | Hypermethylation | Poor prognosis in HGSC | Associated with chemoresistance pathways |
| ETV1 [71] | Transcription factor | Hypermethylation | Poor prognosis in HGSC | Validated in TCGA-OV dataset |
The PLAT-M8 methylation signature demonstrates particular clinical utility, with blood DNA methylation at relapse correlating with clinical outcomes. Class 1 methylation status is linked to shorter survival (summary OS: HR 2.50, 1.64-3.79) and poorer prognosis on carboplatin monotherapy (OS: aHR 9.69, 95% CI: 2.38-39.47) [70]. It is associated with older age (>75 years), advanced stage, platinum resistance, residual disease, and shorter PFS [70].
Biomarker Discovery in HGSC Chemoresistance
Methylome-wide profiling using Illumina Infinium MethylationEPIC BeadChip (HM850K) in HGSC cell lines identified 3,641 differentially methylated CpG probes (DMPs) spanning 1,617 genes between chemoresistant and sensitive cells [71]. Notably, 80% of these were hypermethylated CpG sites associated with resistant cells, with top hypermethylated CpGs including cg21226224 (SOX17, ∆β=79%), cg02538901 (ATP1A1, ∆β=75%), and cg17032184 (CD58, ∆β=64%) [71].
Functional enrichment analysis revealed several cancer-related pathways associated with chemoresistance, including phosphatidylinositol signaling, homologous recombination, and ECM-receptor interaction pathways [71]. Machine learning analysis identified a significant association between global hypermethylation in HGSC chemoresistant cells and poor overall and progression-free survival in patients [71].
Experimental Protocols and Methodologies
Methylation Analysis Workflow
Figure 1: DNA Methylation Analysis Workflow
Detailed Methodologies for Methylation Analysis
Sample Processing and DNA Extraction
Tissue samples are typically collected during surgical resections, with informed consent obtained prior to collection [68]. DNA extraction is performed using commercial kits (e.g., AllPrep DNA/RNA mini kit, DNeasy Blood & Tissue Kit, or AmoyDx DNA Extraction Kit) according to manufacturer protocols [68] [71]. DNA concentrations are quantified using spectrophotometry (NanoDrop) or fluorometry (Qubit), with final concentrations adjusted to 20 ng/μL for downstream applications [71].
Bisulfite Conversion and Methylation Profiling
Bisulfite conversion is critical for distinguishing methylated from unmethylated cytosines. Typically, 500 ng of extracted DNA is bisulfite converted using commercial kits (e.g., EZ DNA methylation kit) [71]. For genome-wide methylation profiling, the Illumina Infinium MethylationEPIC BeadChip (HM850K) provides comprehensive coverage of over 850,000 CpG sites at single-base resolution [71]. For targeted approaches, quantitative methods like methylation-specific real-time PCR (MS-PCR) or bisulfite pyrosequencing are employed [68] [70].
Data Processing and Differential Analysis
Raw data files (.idat) from array-based methods are processed using R/Bioconductor packages such as minfi [71]. Quality control involves filtering probes with detection p-value > 0.01, removing probes on sex chromosomes, within SNP loci, or demonstrating cross-reactivity [71]. Normalization is performed using methods like Noob and Quantile normalization [71]. Differential methylation analysis utilizes the limma package for linear model fitting, with false discovery rate (FDR) correction for multiple testing [66] [71]. DMPs are typically defined using thresholds of FDR-adjusted p-value < 0.05 and delta beta change ≥ 0.2 [71].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Methylation Biomarker Studies
| Reagent/Kit | Manufacturer | Function | Key Applications |
|---|---|---|---|
| Infinium MethylationEPIC BeadChip [71] | Illumina | Genome-wide methylation profiling | Discovery phase; covers >850,000 CpG sites |
| EZ DNA Methylation Kit [71] | Zymo Research | Bisulfite conversion of DNA | Prepares DNA for methylation-specific analyses |
| AllPrep DNA/RNA Mini Kit [71] | Qiagen | Simultaneous DNA/RNA extraction | Preserves sample integrity for multi-omics |
| DNeasy Blood & Tissue Kit [71] | Qiagen | DNA extraction from various sources | Flexible sample processing |
| Methylation-Specific PCR Kits [68] | BioChain | Targeted methylation detection | Clinical validation; IVD use |
| limma R Package [66] [71] | Bioconductor | Differential methylation analysis | Statistical analysis of methylation data |
| DMRcate R Package [66] | Bioconductor | DMR identification | Identifies regional methylation changes |
Signaling Pathways and Biological Implications
Figure 2: Methylation-Mediated Pathway Alterations in Cancer
DNA methylation biomarkers influence cancer progression through disruption of critical signaling pathways. In colorectal cancer, functional enrichment analyses have identified significant involvement of the Wnt signaling pathway and extracellular matrix (ECM) organization [66]. In ovarian cancer, chemoresistance-associated hypermethylation affects phosphatidylinositol signaling, homologous recombination, and ECM-receptor interaction pathways [71]. These pathway alterations collectively contribute to enhanced tumor invasion, chemotherapy resistance, immune evasion, and ultimately poor patient prognosis.
The relationship between methylation changes and cellular function is further modulated by tumor microenvironment heterogeneity. Studies in pancreatic ductal adenocarcinoma have demonstrated that DNA methylation-based deconvolution can identify distinct TME subtypes, including hypo-inflamed (immune-deserted), myeloid-enriched, and lymphoid-enriched microenvironments [8]. These subtypes exhibit different methylation patterns and respond differently to therapies, highlighting the importance of considering TME heterogeneity in biomarker development.
Validated DNA methylation biomarkers in colorectal, breast, and ovarian cancers demonstrate significant clinical utility for early detection, prognosis, and treatment response prediction. The integration of these biomarkers with clinical parameters enhances risk stratification, particularly in challenging clinical scenarios such as stage II colon cancer recurrence risk, breast cancer progression from DCIS to invasive disease, and platinum resistance in ovarian cancer. Future directions should focus on standardizing detection methodologies, validating biomarkers in large prospective trials, and developing integrated models that incorporate methylation signatures with other molecular and clinical features for personalized cancer management.
The tumor microenvironment (TME) represents a complex ecosystem characterized by significant cellular heterogeneity. Recent investigations have revealed that DNA methylation heterogeneity (DNAmeH) serves as a critical regulator of tumor biology, offering distinct advantages over traditional genetic and protein biomarkers. This technical review provides a comprehensive comparison of these biomarker classes, highlighting the unique capabilities of DNAmeH analysis in delineating TME composition, predicting therapeutic response, and informing drug development strategies. We present quantitative performance data, detailed experimental methodologies for DNAmeH assessment, and visualizations of key analytical workflows to equip researchers with practical tools for implementing these approaches in cancer research.
The classification and functional characterization of tumors have evolved substantially with the advent of molecular profiling technologies. Traditional biomarkers, including somatic mutations and circulating proteins, have provided foundational insights into cancer diagnostics and therapeutic targeting. However, the dynamic and heterogeneous nature of the TME necessitates more sophisticated analytical approaches. DNA methylation heterogeneity (DNAmeH) has emerged as a powerful biomarker class that captures both the diversity of cellular populations within tumors and the epigenetic regulation that drives tumor progression [3].
Unlike genetic mutations, which remain largely stable, DNA methylation represents a dynamic epigenetic modification that is mechanistically linked to gene expression regulation and is influenced by both genetic predispositions and environmental exposures [72]. This plasticity enables DNAmeH biomarkers to provide unique insights into TME composition, cellular states, and response to therapeutic interventions. The relative stability of DNA methylation compared to other epigenetic marks, combined with its mitotic heritability, positions DNAmeH as a particularly valuable tool for understanding tumor biology [72].
Comparative Performance Analysis
Fundamental Characteristics Across Biomarker Classes
Table 1: Comparative Analysis of Biomarker Classes in Cancer Research
| Characteristic | DNAmeH Biomarkers | Traditional Genetic Markers | Protein Markers |
|---|---|---|---|
| Molecular Basis | 5-methylcytosine (5mC) patterns at CpG sites [3] | DNA sequence variations (SNVs, CNVs) | Protein expression and secretion levels |
| Stability | Mitotically heritable, relatively stable yet dynamic [72] | Highly stable throughout lifespan | Variable half-lives, dynamic fluctuations |
| TME Insight | Reveals cellular composition and epigenetic states [3] [27] | Limited to mutational profiles | Reflects secretory activity and signaling |
| Measurement Platform | Microarrays (EPIC), bisulfite sequencing [72] | DNA sequencing (WGS, WES) | Immunoassays, proteomic platforms (Olink) |
| Therapeutic Utility | Predictive for immunotherapy response [73] | Targeted therapies (e.g., kinase inhibitors) | Limited predictive value |
| Technical Considerations | Bisulfite conversion, deconvolution algorithms [27] | Variant calling, tumor purity correction | Pre-analytical variables, degradation |
Quantitative Performance Metrics
DNAmeH biomarkers demonstrate distinctive performance characteristics across multiple clinical and research applications:
- TME Deconvolution: DNAmeH analysis enabled identification of 42 distinct subtypes across 14 cancer types based on immune infiltration patterns, significantly outperforming transcriptomic-based classification in stability and reproducibility [27].
- Cardiovascular Risk Prediction: In direct comparative analyses, DNA methylation-based biomarkers like GrimAgeAccel showed hazard ratios of 2.01 for all-cause death, independently predicting myocardial infarction (HR: 1.44) and stroke (HR: 1.42) [74].
- Cancer Biomarker Performance: DNA methylation-based assays have achieved clinical implementation for multiple cancers (bladder, breast, cervical, colon, liver, lung, glioblastoma) with sensitivity and specificity profiles comparable or superior to protein biomarkers for early detection [72].
- Predictive Power: Protein EpiScores (DNA methylation-based estimates of protein levels) demonstrated significant association with cardiovascular disease risk beyond established clinical risk scores, though with currently modest improvements in predictive accuracy in clinical settings [72].
DNAmeH Biomarkers in Tumor Microenvironment Research
Methodological Framework for DNAmeH Analysis
Experimental Protocol 1: Comprehensive DNAmeH Profiling in TME
Sample Preparation and Processing:
- Sample Collection: Obtain tumor tissues (fresh-frozen or FFPE) and matched blood samples as control [3].
- DNA Extraction: Use standardized kits (e.g., QIAamp DNA FFPE Tissue Kit) with quality control (QC) via spectrophotometry (A260/280 ratio ~1.8-2.0).
- Bisulfite Conversion: Process 500ng DNA using EZ DNA Methylation kits (Zymo Research) with conversion efficiency >99% verified by control DNA [72].
- Methylation Profiling: Hybridize to Illumina Infinium MethylationEPIC v2.0 arrays (900,000 CpG sites) following manufacturer protocols [72].
- Quality Control: Exclude probes with detection p-values >0.01, <3 beads in ≥5% samples, non-CpG probes, SNP-related probes, multi-hit probes, and sex chromosome probes [73].
Bioinformatic Analysis:
- Preprocessing: Perform background correction, normalization (ssNoob), and β-value calculation using
minfiorChAMPR packages [73]. - DNAmeH Quantification: Calculate intra-sample methylation heterogeneity using:
- Methylation Entropy: Measure disorder in methylation states across loci
- Methylation Variance: Average β-value variance across targeted regions
- Epiallele Frequency: Analysis of haplotype-specific methylation patterns [3]
- TME Deconvolution: Apply reference-based (CIBERSORT, EPIC) or reference-free algorithms to estimate cellular composition from bulk methylation data [27].
- Differential Methylation: Identify region-specific methylation changes (DMRs) using
bumphunterorDMRcatewith FDR correction.
Figure 1: DNAmeH Analysis Workflow. The diagram illustrates the comprehensive process from sample collection to biomarker identification, highlighting key steps in DNA methylation heterogeneity profiling.
DNAmeH-Driven TME Subtyping in Gastric Cancer
Experimental Protocol 2: Multi-Omics Integration for TME Classification
A landmark study demonstrates the power of DNAmeH analysis in gastric cancer (GC) stratification [73]:
Experimental Design:
- Cohort Composition: Retrospective analysis of 359 GC samples with multi-omics data (transcriptomic RNA, DNA methylation, mutation data, clinical parameters).
- Clustering Integration: Application of 10 distinct clustering algorithms (CIMLR, iClusterBayes, MoCluster, COCA, ConsensusClustering, IntNMF, LRAcluster, NEMO, PINSPlus, SNF) implemented through MOVICS R package [73].
- Optimal Cluster Determination: Gap-statistic and CPI analysis identified three robust molecular subtypes (CS1, CS2, CS3) with distinct clinical outcomes and TME characteristics.
- Validation: External validation using independent GEO cohorts (GSE84437, GSE26253, GSE62254, GSE15459) sequenced on different platforms.
Key Findings:
- CS3 Subtype: Exhibited immunologically active TME with significantly improved response to immunotherapy and favorable prognosis.
- CS2 Subtype: Characterized by immunologically exhausted TME and poor outcomes.
- Biomarker Discovery: Identified Cathepsin V (CTSV) as a novel classifier, significantly downregulated in CS3 and upregulated in CS2 subtypes [73].
Analytical Approaches and Research Tools
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 2: Essential Research Tools for DNAmeH and Comparative Biomarker Studies
| Category | Specific Product/Platform | Research Application | Key Features |
|---|---|---|---|
| Methylation Arrays | Illumina Infinium MethylationEPIC v2.0 [72] | Genome-wide CpG methylation profiling | >900,000 CpG sites, single-site resolution |
| Bisulfite Kits | EZ DNA Methylation Kit (Zymo Research) | Bisulfite conversion of DNA | >99% conversion efficiency, FFPE compatible |
| Deconvolution Algorithms | CIBERSORT, EPIC, MethylCIBERSORT [27] | TME cellular composition estimation | Cell-type specificity using reference methylomes |
| Bioinformatics Packages | ChAMP, minfi, wateRmelon [73] | Methylation data preprocessing and QC | Normalization, batch correction, DMR detection |
| Multi-Omics Integration | MOVICS R package [73] | Integrative clustering across data types | 10 clustering algorithms, subtype discovery |
| Proteomic Platforms | Olink Explore 1536 [75] | High-throughput protein biomarker quantification | 1,459 proteins, high sensitivity |
Signaling Pathways in DNAmeH-Mediated Tumor Progression
Figure 2: DNAmeH-Affected Signaling Pathways. The diagram illustrates key biological pathways influenced by DNA methylation heterogeneity and their impact on clinical outcomes in cancer.
Clinical Translation and Therapeutic Applications
The translational potential of DNAmeH biomarkers is increasingly recognized across multiple cancer types. DNA methylation-based assays have received regulatory approval for cancer detection, monitoring, and treatment response prediction for several malignancies, including bladder, breast, cervical, colon, liver, lung, and glioblastoma [72]. These liquid biopsy approaches provide minimally invasive alternatives to traditional biopsies while potentially better capturing tumor heterogeneity.
In the cardiovascular domain, DNA methylation biomarkers demonstrate significant predictive value. GrimAgeAccel and DNAm-related mortality risk scores show strong associations with all-cause death, myocardial infarction, and stroke, independent of chronological age [74]. Recent studies have identified 609 methylation markers significantly associated with cardiovascular health, with 141 showing potential causality for cardiovascular disease including stroke, heart failure, and gestational hypertension [76].
The integration of DNAmeH biomarkers with traditional risk factors demonstrates incremental predictive value. For instance, models incorporating 36 protein EpiScores showed association with cardiovascular disease risk beyond established clinical scores like ASSIGN and cardiac troponin I concentrations [72]. Similarly, in very old adults, the addition of NT-pro-BNP to traditional risk factors significantly improved prediction of cardiovascular morbidity and mortality (NRI 0.56, relative IDI 4.01) [77].
DNA methylation heterogeneity biomarkers represent a transformative approach in cancer research and clinical oncology, offering unique capabilities for delineating tumor microenvironment complexity and predicting therapeutic response. While traditional genetic and protein biomarkers continue to provide valuable diagnostic and prognostic information, DNAmeH analysis captures the dynamic epigenetic regulation that underlies tumor evolution and therapeutic resistance.
The integration of multi-omics approaches, combining DNA methylation with transcriptomic, proteomic, and mutational data, provides the most comprehensive framework for understanding tumor biology [73]. Future directions should focus on standardizing DNAmeH quantification metrics, validating findings across diverse populations, and developing clinically implementable assays that leverage the stability and information richness of epigenetic markers. As single-cell methylation technologies mature and computational deconvolution algorithms improve, DNAmeH biomarkers are poised to become indispensable tools for precision oncology and drug development.
Within the evolving paradigm of cancer research, the tumor microenvironment (TME) represents a critical determinant of therapeutic efficacy and clinical outcome. DNA methylation heterogeneity (DNAmeH), arising from the complex cellular composition of the TME and cancer epigenome variability, is increasingly recognized as a fundamental source of tumor biological diversity [3] [4]. This technical guide explores the association between molecular subtypes, defined by distinct DNA methylation patterns, and their power to predict patient survival and response to therapeutic interventions. The stability of DNA methylation alterations, which often emerge early in tumorigenesis and remain through tumor evolution, makes them exceptionally suitable for biomarker development [48]. Furthermore, the interplay between DNA methylation patterns and the cellular components of the TME provides a mechanistic link to therapy response, particularly in the context of immunotherapy [23]. This document provides researchers and drug development professionals with a comprehensive framework for exploring methylation subtypes, with structured data presentation, experimental protocols, and visualization tools to advance this critical field.
Clinical Evidence: Methylation Subtypes as Predictors of Outcome
Numerous studies across cancer types have established that DNA methylation-based molecular subtyping provides significant prognostic information beyond conventional staging systems. These subtypes demonstrate distinct survival patterns and respond differently to various therapeutic modalities.
Prognostic Value Across Cancers
Table 1: DNA Methylation Subtypes and Prognostic Associations Across Cancers
| Cancer Type | Subtype Classification Basis | Key Prognostic Findings | References |
|---|---|---|---|
| Colon Adenocarcinoma | 7 subgroups from 356 survival-associated CpG sites | Clusters 3 & 4: Best prognosis; Cluster 7: Worst prognosis | [78] |
| Lung Adenocarcinoma (LUAD) | 7 subgroups from 205 prognostic CpG sites | Cluster 6: Worst prognosis; Clusters 3 & 7: Best prognosis | [79] |
| Glioma | Tumor immune microenvironment (TIME) subtypes via PIM score | Lower PIM (less heterogeneity): Better survival, slower progression | [4] |
| Gastrointestinal Cancers | CpG Island Methylator Phenotype (CIMP) | Association with survival varies; CIMP-high in HCC: dismal survival; CRC: inconsistent conclusions | [80] |
The prognostic power of these classifications often stems from their ability to capture intrinsic biological differences. In colon adenocarcinoma, molecular subgroups identified through consensus clustering of DNA methylation sites showed significant survival differences independent of traditional TNM staging [78]. Similarly, in lung adenocarcinoma, methylation subgroups demonstrated varying survival outcomes that correlated with specific clinical parameters, including T category, N category, and disease stage [79].
Predictive Value for Therapy Response
Table 2: DNA Methylation Biomarkers for Therapy Response Prediction
| Cancer Type | Therapy Context | Methylation Biomarker | Predicted Response | References |
|---|---|---|---|---|
| Colorectal Cancer | Chemotherapy | CIMP-high status | Potentially higher efficacy for 5-FU (due to higher intracellular folate) | [80] |
| Renal Cell Carcinoma (RCC) | Various systemic agents | Multiple gene-specific markers (e.g., ABCG2) | Methylation-dependent sensitivity patterns identified | [81] |
| Glioma | Temozolomide, Bevacizumab, Radiation | 8 prognosis-related CpGct | DNA methylation alterations associated with treatment | [4] |
| Solid Tumors | Immune Checkpoint Inhibitors | Global methylation patterns | DNMT inhibitors remodel TIME, synergize with ICIs | [23] |
The relationship between methylation subtypes and therapy response is particularly evident in the context of immunotherapies. DNA methylation plays a crucial role in remodeling the tumor immune microenvironment (TIME), which directly affects response to immune checkpoint inhibitors (ICIs) [23]. Pharmaceutical interventions targeting DNA methylation, such as DNA methyltransferase inhibitors (DNMTis), have shown potential to enhance antitumor immunity by inducing viral mimicry through transposable element transcription, upregulating tumor antigen expression, mediating immune cell recruitment, and reactivating exhausted immune cells [23].
Methodological Framework: From Subtyping to Validation
Robust methodology is essential for establishing meaningful associations between methylation subtypes and clinical outcomes. The following section outlines key experimental approaches and analytical frameworks.
DNA Methylation Subtyping Workflows
Experimental Protocol 1: Construction of DNA Methylation Subtypes for Prognostic Prediction
Sample Preparation and Data Generation:
- Obtain tumor tissue samples or appropriate liquid biopsy sources (e.g., plasma, urine, CSF) [48].
- Extract high-quality DNA using standardized protocols.
- Perform genome-wide DNA methylation profiling using established platforms:
- Illumina Infinium Methylation BeadChips (e.g., EPIC array) for cost-effective genome-wide coverage [78] [4] [79].
- Whole-genome bisulfite sequencing (WGBS) for comprehensive base-resolution methylation data [48] [4].
- Reduced representation bisulfite sequencing (RRBS) for targeted, cost-efficient coverage of CpG-rich regions [48].
- Process raw data: Normalize using appropriate algorithms (e.g., BMIQ, SWAN), and filter probes with detection p-value > 0.01, cross-reactive probes, and SNPs.
Identification of Prognostic Methylation Markers:
- Annotate CpG sites to genomic regions, focusing on promoter regions (TSS1500, TSS200, 5'UTR, 1st Exon) [79].
- Divide dataset into training and testing cohorts, ensuring balanced clinical characteristics.
- Perform univariate Cox regression analysis on methylation β-values against overall survival (OS) to identify candidate CpG sites (p < 0.05) [78] [79].
- Conduct multivariate Cox regression including relevant clinical covariates (TNM stage, age, etc.) to identify independent prognostic methylation sites.
Consensus Clustering for Subtype Identification:
- Apply consensus clustering (e.g., using R package
ConsensusClusterPlus) to the identified prognostic CpG sites [78] [79]. - Determine optimal cluster number (k) based on cumulative distribution function (CDF) curve stability, consensus matrix heatmap, and cluster consistency [78].
- Validate cluster stability through multiple iterations (e.g., 50-100 repetitions).
- Perform survival analysis (Kaplan-Meier curves with log-rank test) to assess prognostic differences between methylation subtypes.
- Apply consensus clustering (e.g., using R package
Functional and Pathway Analysis:
- Annotate significant CpG sites to corresponding genes.
- Conduct functional enrichment analysis (GO, KEGG) using packages such as
clusterProfilerto identify biological pathways enriched in each subtype [78] [79]. - Analyze gene expression patterns (if RNA-seq data available) across methylation subtypes to validate regulatory implications.
Assessing DNA Methylation Heterogeneity in TME
Experimental Protocol 2: Quantifying DNA Methylation Heterogeneity in Tumor Immune Microenvironment
Quantification of DNAmeH:
- PIM Calculation: Compute Proportion of sites with Intermediate Methylation (PIM) as:
PIM = (Number of CpG sites with β-value 0.2-0.6) / (Total number of CpG sites)[4]. Higher PIM scores indicate greater DNA methylation heterogeneity, reflecting diverse cellular composition in TME. - Single-Cell Analysis: For higher resolution, perform single-cell DNA methylation sequencing (e.g., scBS-seq, scNMT-seq) to directly measure cell-to-cell variation [3].
- Bioinformatic Deconvolution: Estimate cellular composition from bulk tissue data using reference-based (e.g., CIBERSORT, MethylCIBERSORT) or reference-free methods.
- PIM Calculation: Compute Proportion of sites with Intermediate Methylation (PIM) as:
Association with Immune Context:
- Calculate immune cell enrichment scores (e.g., using ssGSEA) for predefined immune cell gene signatures [4].
- Classify Tumor Immune Microenvironment (TIME) subtypes using non-negative matrix factorization (NMF) clustering of immune cell enrichment profiles [4].
- Correlate PIM scores with TIME subtypes and cytotoxic T-lymphocyte infiltration levels.
Construction of Heterogeneity-Based Risk Scores:
- Identify cell-type-associated heterogeneous CpG sites (CpGct) specific to immune cell types (B cell, CD4+ T cell, CD8+ T cell, etc.) [4].
- Calculate Cell-type-associated DNA Methylation Heterogeneity Contribution (CMHC) scores to quantify immune cell type impact on specific CpG sites.
- Develop a Cell-type-associated DNA Methylation Heterogeneity Risk (CMHR) score from prognosis-related CpGct for clinical outcome prediction [4].
- Validate CMHR score through survival analysis and ROC curves for phenotype prediction (e.g., IDH status in glioma).
Pathways and Mechanisms: Connecting Methylation to Phenotype
The association between DNA methylation subtypes and clinical outcomes is underpinned by specific biological mechanisms, particularly those involving immune regulation and gene silencing.
DNA Methylation Remodeling in the Tumor Immune Microenvironment
DNA methylation plays a crucial role in shaping the tumor immune microenvironment, which subsequently influences therapy response and survival outcomes. In cancer cells, a characteristic pattern emerges featuring global hypomethylation (leading to genomic instability and oncogene activation) alongside regional hypermethylation at promoter CpG islands (silencing tumor suppressor genes) [23]. This aberrant methylation landscape contributes to immune cell exclusion from the TME, creating an "immune-cold" phenotype characterized by poor response to immune checkpoint inhibitors [23].
Therapeutic targeting of DNA methylation through DNMT inhibitors can remodel the TIME by:
- Promoting CD4+ T-cell differentiation through demethylation of key loci like FOXP3 [23]
- Reactivating exhausted CD8+ T-cells [23]
- Inducing viral mimicry through transposable element transcription [23]
- Upregulating tumor antigen expression [23]
These mechanisms collectively can convert an immune-cold TME into an "immune-hot" one, thereby enhancing response to immunotherapy and potentially improving survival outcomes.
Table 3: Essential Research Reagents and Platforms for Methylation Subtyping Studies
| Category | Specific Reagents/Platforms | Key Function in Research |
|---|---|---|
| Methylation Profiling Platforms | Illumina Infinium Methylation BeadChips (450K, EPIC) | Genome-wide methylation screening at single-CpG resolution [78] [4] [79] |
| Whole-genome bisulfite sequencing (WGBS) | Comprehensive base-resolution methylation mapping [48] | |
| Reduced representation bisulfite sequencing (RRBS) | Cost-effective targeted methylation analysis of CpG-rich regions [48] | |
| Bioinformatic Tools | R/Bioconductor packages: minfi, ChAMP, DSS |
Quality control, normalization, and differential methylation analysis [78] [79] |
ConsensusClusterPlus |
Molecular subtyping via consensus clustering algorithms [78] [79] | |
| CIBERSORT, MethylCIBERSORT | Cellular deconvolution from bulk methylation data [4] | |
| Functional Validation Reagents | DNMT inhibitors (Decitabine, Azacitidine) | Demethylating agents for mechanistic studies [23] [81] |
| CRISPR/dCas9-DNMT/ TET systems | Targeted methylation editing for causal validation [23] | |
| Reference Data Resources | The Cancer Genome Atlas (TCGA) | Multi-omics datasets with clinical annotations [78] [4] [79] |
| Gene Expression Omnibus (GEO) | Repository for methylation array and sequencing data [4] |
DNA methylation subtypes, reflecting the inherent heterogeneity of the tumor microenvironment, provide a powerful framework for predicting therapy response and survival outcomes across cancer types. The association between specific methylation patterns and clinical trajectories offers opportunities for refined patient stratification and personalized treatment approaches. The methodological framework presented in this guide—encompassing robust subtyping protocols, heterogeneity quantification, and mechanistic pathway analysis—provides researchers with the tools necessary to advance this field. As single-cell technologies and spatial methylation profiling continue to evolve, the resolution of methylation-based stratification will further improve, enabling more precise association of methylation subtypes with therapeutic vulnerabilities and ultimately enhancing clinical decision-making in oncology.
Conclusion
DNA methylation heterogeneity is a fundamental property of the tumor microenvironment that profoundly influences cancer biology and patient outcomes. The integration of advanced detection technologies, sophisticated computational models, and single-cell approaches has transformed our ability to decipher this epigenetic complexity. Validated methylation biomarkers and classifiers are already demonstrating significant potential for improving early cancer detection, prognostication, and tissue-of-origin identification. Future efforts must focus on standardizing analytical pipelines, prospectively validating biomarkers in diverse clinical cohorts, and developing therapeutic strategies that directly target the epigenetic drivers of heterogeneity. By bridging the gap between epigenetic research and clinical practice, the field is poised to deliver powerful new tools for precision oncology, ultimately enabling more personalized and effective cancer management.
References
- 1. Tumor Microenvironment: A Complex Landscape of Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12066109/]
- 2. Evaluation of Pan-Cancer Immune Heterogeneity Based on DNA Methylation [https://www.mdpi.com/2073-4425/16/2/160]
- 3. DNA methylation heterogeneity in complex tumor microenvironment: Quantitative methods, influencing factors, and clinical implications - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2352304225003216]
- 4. DNA methylation heterogeneity attributable to a complex tumor immune microenvironment prompts prognostic risk in glioma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10936651/]
- 5. Bioinformatics Analysis Reveals an Association Between ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.595477/full]
- 6. A Multi-Omics Prognostic Model Capturing Tumor Stemness ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11504857/]
- 7. Metheor: Ultrafast DNA methylation heterogeneity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10062925/]
- 8. Deciphering the Heterogeneity of Pancreatic Cancer: DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452622/]
- 9. Epigenetic evolution and clinicopathological implications of ... [https://www.nature.com/articles/s41598-025-13919-y]
- 10. Super-enhancers in immune system regulation: mechanisms ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12394480/]
- 11. Superenhancers as master gene regulators and novel ... [https://www.nature.com/articles/s12276-023-00934-0]
- 12. Current progress and future perspective of super-enhancers [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1611905/full]
- 13. Current progress and future perspective of super-enhancers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12263373/]
- 14. Functional Enhancers As Master Regulators of Tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5386954/]
- 15. Super-enhancer DNA methylation in cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1610579/full]
- 16. Super-enhancers in tumors: unraveling recent advances in ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06098-x]
- 17. Comparison of DNA methylation based classification ... [https://www.nature.com/articles/s41698-024-00718-3]
- 18. Decoding the Tumor Microenvironment: Insights and New ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468534/]
- 19. Ultra-mild bisulfite outperforms existing methods for 5- ... [https://www.nature.com/articles/s41467-025-66033-y]
- 20. Comparative Performance of Methylation Array and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12589796/]
- 21. Genome-wide quantitative analysis of DNA methylation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4071208/]
- 22. Single-Cell DNA Methylation Analysis in Cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9777108/]
- 23. Reshaping the tumour immune microenvironment in solid ... [https://www.nature.com/articles/s41416-023-02292-0]
- 24. EpiCHAOS: a metric to quantify epigenomic heterogeneity in ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03446-w]
- 25. HiTIMED: hierarchical tumor immune microenvironment ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-022-03736-6]
- 26. Quantitative transcriptomic and epigenomic data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC10997052/]
- 27. Evaluation of Pan-Cancer Immune Heterogeneity Based on DNA ... [https://pubmed.ncbi.nlm.nih.gov/40004489/]
- 28. -Based Cell Type Deconvolution Reveals the... | CoLab DNA Methylation [https://colab.ws/articles/10.1101%2F2025.01.19.633794]
- 29. Frontiers | DNA and immune evasion in triple-negative... methylation [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1534055/full]
- 30. Immune microenvironmental heterogeneity according to tumor ... DNA [https://link.springer.com/article/10.1007/s00262-024-03805-3]
- 31. xCell 2.0: robust algorithm for cell type proportion estimation ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03784-3]
- 32. Reference-free deconvolution of complex samples based ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1570781/full]
- 33. A distribution-independent cell deconvolution model for ... [https://www.sciencedirect.com/science/article/pii/S2666979X2500206X]
- 34. A Transformer-Based Deep Diffusion Model for Bulk RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467303/]
- 35. Integrating single-cell and bulk RNA sequencing data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12480286/]
- 36. Integrating bulk and single-cell RNA sequencing analysis to ... [https://breast-cancer-research.biomedcentral.com/articles/10.1186/s13058-025-02130-6]
- 37. Comprehensive analysis of single-cell and bulk RNA ... [https://www.nature.com/articles/s41598-025-23779-1]
- 38. Examining cellular heterogeneity in human DNA ... [https://www.sciencedirect.com/science/article/pii/S2666166725000449]
- 39. Estimating genome-wide DNA methylation heterogeneity with ... [https://epigeneticsandchromatin.biomedcentral.com/articles/10.1186/s13072-023-00521-7]
- 40. Quantitative comparison of within-sample heterogeneity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7192612/]
- 41. DNA methylation and machine learning - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512482/]
- 42. Diagnostic classification of cancers using DNA methylation ... [https://www.nature.com/articles/s41598-022-14786-7]
- 43. Artificial intelligence: illuminating the depths of the tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11360846/]
- 44. DNA methylation as a diagnostic tool - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9080136/]
- 45. Emerging Technologies in Biomarker Discovery You ... [https://blog.crownbio.com/emerging-technologies-in-biomarker-discovery-you-should-know-about]
- 46. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 47. Circulating tumor DNA methylation detection as biomarker ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11550092/]
- 48. a roadmap for DNA methylation biomarkers in liquid biopsies [https://www.nature.com/articles/s41388-025-03624-5]
- 49. DNA methylation in breast cancer: early detection and ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06495-2]
- 50. Liquid Biopsy-Based DNA Methylation Biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12285340/]
- 51. Deciphering Tumour Heterogeneity: From Tissue to Liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8946040/]
- 52. Precision Oncology: Artificial Intelligence and DNA ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.790645/full]
- 53. Research trends and prospects of Circulating tumor DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360996/]
- 54. Clinical applications of cell-free DNA-based liquid biopsy ... [https://www.sciencedirect.com/science/article/pii/S1936523325002505]
- 55. Stop Wasting Time: Correcting Batch Effects in Multi-Omics ... [https://pluto.bio/resources/Learning%20Series/batch-effects-multi-omics-data-analysis]
- 56. Are batch effects still relevant in the age of big data? [https://www.sciencedirect.com/science/article/pii/S0167779922000361]
- 57. An incremental framework for batch effect correction in DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495439/]
- 58. How Metabolomics Data Correction Reduces Experimental ... [https://www.iroatech.com/uncategorized/how-metabolomics-data-correction-minimizes-experimental-bias/]
- 59. Evidence of DNA methylation heterogeneity and ... [https://www.nature.com/articles/s41388-024-03270-3]
- 60. Evaluating the Clinical Utility of a Biomarker - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3138723/]
- 61. Methods for determining clinical utility [https://www.sciencedirect.com/science/article/abs/pii/S0009912023002023]
- 62. an analysis based on population-level parametric distributions ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02656-5]
- 63. Integrated multi-omics profiling reveals the role of the DNA ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03474-9]
- 64. A Comprehensive Oncological Biomarker Framework Guiding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466961/]
- 65. DNA methylation in breast cancer: early detection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12020129/]
- 66. Colorectal Cancer Biomarker Identification via Joint DNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12191883/]
- 67. Identification and external validation of tumor DNA ... [https://www.sciencedirect.com/science/article/pii/S1936523325001366]
- 68. SEPT9 methylation as a diagnostic and predictive ... [https://www.nature.com/articles/s41598-025-25096-z]
- 69. Development and Validation of a 14-CpG DNA Methylation ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1548726/abstract]
- 70. Clinical validation of a DNA methylation biomarker ... [https://pubmed.ncbi.nlm.nih.gov/41175040/]
- 71. Global DNA methylation signatures associated with ... [https://www.nature.com/articles/s41598-025-20827-8]
- 72. DNA Methylation-based Biomarkers of Protein Levels and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11021153/]
- 73. Prognostic molecular subtype reveals the heterogeneity of ... [https://www.nature.com/articles/s41598-025-96686-0]
- 74. DNA methylation-based biomarkers of age acceleration ... [https://www.sciencedirect.com/science/article/pii/S2352396420305272]
- 75. Integrative proteomic analyses across common cardiac ... [https://www.nature.com/articles/s44161-024-00567-0]
- 76. Novel Biomarkers May Help Improve Cardiovascular Disease ... [https://news.feinberg.northwestern.edu/2025/09/10/novel-biomarkers-may-help-improve-cardiovascular-disease-risk-prediction/]
- 77. Biomarkers versus traditional risk factors to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7322328/]
- 78. Molecular subtypes based on DNA methylation predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6949097/]
- 79. DNA methylation molecular subtypes for prognosis prediction ... [https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-022-01924-0]
- 80. Insight into the role of DNA methylation in prognosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12026041/]
- 81. DNA Methylation as Drug Sensitivity Marker in RCC [https://www.mdpi.com/2075-4655/8/3/28]