Endocrine-Disrupting Chemicals and Fertility: Mechanisms, Evidence, and Future Directions in Biomedical Research
This comprehensive review synthesizes current scientific evidence on the impact of endocrine-disrupting chemicals (EDCs) on human fertility, addressing a critical concern for researchers and drug development professionals.
Endocrine-Disrupting Chemicals and Fertility: Mechanisms, Evidence, and Future Directions in Biomedical Research
Abstract
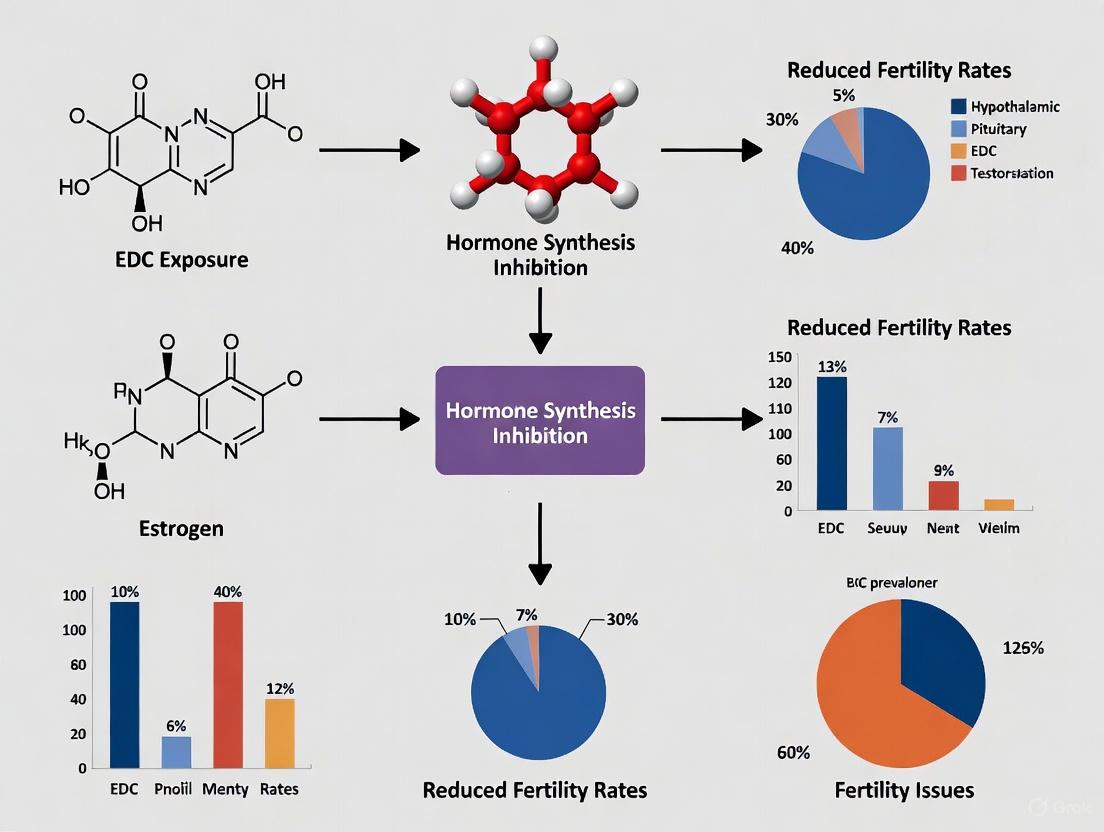
This comprehensive review synthesizes current scientific evidence on the impact of endocrine-disrupting chemicals (EDCs) on human fertility, addressing a critical concern for researchers and drug development professionals. We explore the foundational mechanisms by which EDCs like bisphenols, phthalates, and pesticides disrupt hormonal homeostasis, focusing on receptor-mediated signaling, oxidative stress, and epigenetic modifications. The article evaluates methodological approaches in human epidemiological studies, including challenges in risk assessment such as low-dose effects and chemical mixtures. We further analyze strategies for mitigating EDC exposure and optimizing reproductive outcomes, concluding with a validation of the significant disease burden and economic costs attributable to EDCs, and proposing essential future research avenues for regulatory science and therapeutic development.
Unraveling the Mechanisms: How EDCs Disrupt Reproductive Biology
Endocrine-disrupting chemicals (EDCs) are natural or human-made substances that can mimic, block, or interfere with the body's hormones, which are part of the endocrine system [1]. The endocrine system consists of glands distributed throughout the body that produce hormones acting as signaling molecules after release into the circulatory system, controlling biological processes including normal growth, fertility, and reproduction [1]. Hormones act in extremely small amounts, and minor disruptions in their levels may cause significant developmental and biological effects, which is why EDC exposure is a substantial concern for human health, particularly in reproductive and metabolic disorders [1]. This whitepaper details the core concepts of endocrine disruption and focuses on four key chemical classes—Bisphenol A (BPA), phthalates, pesticides, and per- and polyfluoroalkyl substances (PFAS)—within the specific context of their impact on fertility research.
Core Concepts of Endocrine Disruption
Endocrine disruption occurs through several molecular mechanisms. EDCs can interfere with hormonal signaling by binding to hormone receptors, acting as agonists or antagonists, and thus activating or inhibiting their activity [2]. They can also alter the expression of hormone receptors in cells, up-regulating or down-regulating their production [2]. A critical mechanism involves affecting co-regulatory proteins that interact with hormone receptors, resulting in changes to receptor function [2]. Furthermore, EDCs can modify signal transduction pathways downstream of the hormone receptor, affecting the cell's response to hormones, and cause epigenetic modifications, such as DNA methylation, which can alter gene expression and hormone receptor function [2]. The delicate balance of the endocrine system, which depends on very small changes in hormone levels, means that even low-dose exposures to EDCs can alter the body's sensitive systems and lead to health problems [1].
Key Chemical Classes
Bisphenol A (BPA) and Analogs
Bisphenol A (BPA) is a synthetic chemical used extensively to manufacture polycarbonate plastics and epoxy resins, found in food packaging, toys, and the lining of canned foods and beverages [3] [1] [2]. Human exposure occurs when BPA migrates from containers into food and drink, especially upon heating [3]. BPA is classified as an endocrine disruptor due to its xenoestrogenic activity, exerting effects by binding weakly to estrogen receptors ERα and ERβ, activating the membrane receptor GPER, and interacting with estrogen-related receptors [3]. Its structure similarity to estradiol allows it to influence numerous estrogen-related pathways [3].
Due to safety concerns and regulatory restrictions, many BPA analogs—such as bisphenol S (BPS), bisphenol F (BPF), and bisphenol AF (BPAF)—have been introduced as alternatives [2]. However, studies show these analogs can have comparable or even stronger endocrine and toxic effects than BPA, disrupting the endocrine system via interactions with nuclear receptors and related signaling pathways [2]. The order of ERα agonistic activity induced by nine BPA analogs was BPAF > BPB > BPZ > BPA, BPE, BPF > BPS > BPAP > BPP, with BPAF's affinity being about tenfold stronger than BPA's [2].
Table 1: BPA and Analog Health Effects and Research Implications
| Chemical | Key Health Effects on Fertility | Molecular Targets | Implications for Research |
|---|---|---|---|
| Bisphenol A (BPA) | Reduced egg quality, oocyte yield, and normal fertilization; increased risk of miscarriage; altered ovarian cycle; linked to hormone-related cancers (breast, ovary, prostate) [3] [4] [5] | ERα, ERβ, GPER, ERRγ [3] [2] | A model EDC for studying mechanisms; requires investigation of low-dose effects and transgenerational inheritance [3] [6]. |
| Bisphenol S (BPS) | Estrogen-like effects; potential for stronger endocrine disruption than BPA via alternative mechanisms (e.g., epigenetic changes) [2] | Estrogen receptors (weaker agonist, potential antagonist) [2] | Key substitute in "BPA-free" products; research should assess full mechanism spectrum, not just receptor affinity [2]. |
| Bisphenol AF (BPAF) | Potent estrogenic activity; acts as ERα/ERβ agonist at some concentrations and antagonist at others [2] | Estrogen receptors (stronger agonist than BPA) [2] | High-potency analog; crucial for studying non-monotonic dose responses and receptor cross-talk [2]. |
Phthalates
Phthalates are a group of synthetic chemicals used primarily as plasticizers to increase the flexibility and durability of polyvinyl chloride (PVC) plastics [7]. They are classified into high molecular weight (HMW) phthalates, such as di(2-ethylhexyl) phthalate (DEHP), used in food packaging, medical devices, and building materials, and low molecular weight (LMW) phthalates, such as diethyl phthalate (DEP) and dibutyl phthalate (DBP), used in personal care products like fragrances, lotions, and cosmetics [7]. Exposure occurs mainly through diet from contaminated food and beverages, but also via dermal absorption from cosmetics and inhalation from indoor air and dust [7]. Phthalates interfere with the production of androgens, including testosterone, a hormone critical for male development and relevant to female reproductive health [5]. Their ability to cross the placental barrier makes them a significant concern for maternal and fetal health [7].
Table 2: Phthalate Health Effects and Research Implications
| Chemical / Metabolite | Key Health Effects on Fertility & Metabolism | Molecular Targets | Implications for Research |
|---|---|---|---|
| DEHP / MEHP | Decreased oocyte yield, clinical pregnancy rate, and live birth rate in ART; associated with Gestational Diabetes Mellitus (GDM) [4] [7] | PPARs, androgen synthesis pathways [7] | A key model for studying metabolic disruption; links plasticizer exposure to adverse pregnancy outcomes [7]. |
| MEP (Monoethyl Phthalate) | Decreased fecundability; decreased odds of normal fertilization in ART [4] | Androgen signaling [5] | Common LMW phthalate metabolite; useful non-invasive biomarker for exposure assessment in cohort studies [4] [7]. |
| MBP (Monobutyl Phthalate) | Decreased odds of normal fertilization [4] | Androgen signaling [5] | Like MEP, a key urinary biomarker for correlating exposure with reproductive endpoints in epidemiological studies [4] [7]. |
Pesticides
Pesticides, including insecticides and herbicides, are designed to be toxic to pests' nervous or reproductive systems and often act by disrupting endocrine systems, with effects that can extend to humans and other animals due to similarities in endocrine systems [5]. Exposure occurs through contaminated food, water, air, dust, and soil [4]. Organochlorine pesticides like DDT (dichlorodiphenyltrichloroethane) and its metabolite DDE, as well as β-hexachlorocyclohexane (β-HCH) and hexachlorobenzene (HCB), are persistent organic pollutants linked to adverse reproductive effects despite many being banned [4]. Atrazine, a widely used herbicide, has been shown to affect the hypothalamus and pituitary glands [1] [5].
Table 3: Pesticide Health Effects and Research Implications
| Chemical | Key Health Effects on Fertility | Molecular Targets | Implications for Research |
|---|---|---|---|
| DDT/DDE | Increased risk of miscarriage, preterm birth, early pregnancy loss; decreased fertilization rate and number of high-quality embryos in ART [4] | Estrogen receptor pathways [5] | A classic, persistent EDC; ideal for studying long-term exposure effects and transgenerational inheritance [4]. |
| β-HCH, HCB | Decreased fecundability; decreased fertilization rate and proportion of high-quality embryos [4] | Estrogen and other steroid hormone signaling pathways [4] | Often co-occur with DDT; research should focus on mixture effects and impacts on oocyte quality and early embryogenesis [4]. |
| Atrazine | Altered puberty, impaired reproductive development [1] [5] | Hypothalamic-pituitary-gonadal (HPG) axis [5] | Model for studying central disruption of the HPG axis and its impact on development and fertility [1] [5]. |
Per- and Polyfluoroalkyl Substances (PFAS)
Per- and polyfluoroalkyl substances (PFAS) are a large group of human-made chemicals containing strong carbon-fluorine bonds, used for their oil- and water-repellent properties in products like nonstick cookware, food packaging, carpets, textiles, and firefighting foam [8] [1] [5]. They are often called "forever chemicals" because they do not break down in the environment and can bioaccumulate in the body and biomagnify through the food chain [8]. Exposure is widespread through contaminated drinking water and diet [8] [9]. PFAS have been linked to a wide range of harmful health effects, including developmental toxicity, liver damage, immune system suppression, endocrine disruption, and kidney or testicular cancer [8]. Their persistence and ubiquitous presence make them a long-term concern for public health.
Table 4: PFAS Health Effects and Research Implications
| Chemical | Key Health Effects | Molecular Targets | Implications for Research |
|---|---|---|---|
| PFOA (Perfluorooctanoic acid) | Liver damage, endocrine disruption, immune suppression (diminished vaccine response), testicular and kidney cancer [8] | PPARs, lipid metabolism pathways [8] | A legacy PFAS; critical for establishing toxicity pathways and health-based regulatory standards for the entire class [8]. |
| PFOS (Perfluorooctane sulfonic acid) | Similar to PFOA: immune toxicity, endocrine disruption, neurotoxicity, carcinogenicity [8] | PPARs, thyroid hormone transport [8] | Like PFOA, a well-studied legacy compound; research on its mechanisms informs risk assessment for newer analogs [8]. |
| Short-Chain PFAS (e.g., PFBS) | Higher water solubility and mobility; difficult to remove with conventional water treatment [8] | Potential interaction with various cellular receptors [8] | Represent a key technical challenge; research needed on their specific toxicity, bioaccumulation potential, and effective remediation [8]. |
Experimental Methodologies in Fertility Research
In Vitro Assays for Receptor Binding and Transactivation
A foundational approach for identifying potential EDCs involves in vitro assays that assess a chemical's ability to bind to hormone receptors and activate or inhibit transcriptional activity.
- Cell-Based Reporter Gene Assays: These assays use mammalian cells (e.g., human breast cancer MCF-7 cells, BG1Luc cells) engineered to contain a hormone-responsive element (e.g., Estrogen Response Element, ERE) linked to a reporter gene like luciferase [6]. Cells are exposed to the test chemical, and receptor activation is quantified by measuring luminescence. Antagonists can be identified by co-exposing cells to the test chemical and a known agonist (e.g., 17β-estradiol) [6]. This method was pivotal in showing that BPA-free plastic products can leach chemicals with estrogenic activity [6].
- Receptor Binding Assays: These competitive assays use purified hormone receptors (e.g., ERα, ERβ) to measure the displacement of a radio- or fluorescently-labeled natural hormone (e.g., estradiol) by the test chemical. The half-maximal inhibitory concentration (IC50) provides a measure of binding affinity [2]. This methodology revealed that BPA's affinity for ERα and ERβ is about 10,000-fold lower than that of 17β-estradiol, while BPAF has about a tenfold stronger affinity than BPA [2].
In Vivo and Epidemiological Studies
To translate in vitro findings to health outcomes, particularly in reproduction, more complex study designs are required.
- Animal Models (e.g., Rodent Studies): These studies are crucial for assessing the effects of EDCs on development and fertility. A typical protocol involves exposing mice or rats during critical windows, such as gestation, lactation, or peripubertally [6]. Endpoints measured include age at puberty, ovarian and testicular histology, sperm quality, estrous cyclicity, mating success, and offspring health. For example, perinatal BPA exposure in CD-1 mice was shown to alter body weight and composition in a dose- and sex-specific manner [6].
- Human Biomonitoring and Cohort Studies: These observational studies link internal chemical doses to health outcomes. A standard methodology involves collecting biological samples (e.g., urine, blood, follicular fluid) from a cohort (e.g., couples seeking fertility treatment, pregnant women) and analyzing them for EDCs and their metabolites [4] [7]. Reproductive outcomes (e.g., time to pregnancy, fertilization rate, embryo quality, clinical pregnancy, live birth, miscarriage) are tracked. For instance, studies have correlated urinary levels of phthalate metabolites like MEP and MBP with decreased odds of normal fertilization and clinical pregnancy in women undergoing IVF [4]. A systematic review of such studies found that phthalate levels were significantly present in the urine of patients with Gestational Diabetes Mellitus (GDM) [7].
Advanced Models for Mechanistic and Translational Research
- 3D Spheroid Models: Emerging technologies like 3D spheroid models of human liver cells are being used to investigate how pollutants like PFAS contribute to complex diseases in a system that more closely mimics the human organ's architecture and function [9]. These models can be used to study mechanisms of toxicity and test whether effects are reversible [9].
- Exposomics Frameworks: This approach examines the full range of environmental exposures across the life course. The Southern California ShARP Center, for example, uses exposomics to examine how PFAS together with other environmental exposures affect liver disease, collaborating with large consortia to compare data across different communities [9].
Visualization of Signaling Pathways and Experimental Workflows
Estrogenic Signaling Pathway Disruption by BPA and Analogs
Experimental Workflow for EDC Fertility Risk Assessment
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Research Reagents and Materials
| Reagent / Material | Function / Application | Example Use Case |
|---|---|---|
| MCF-7 Cell Line | An estrogen-sensitive human breast adenocarcinoma cell line used in reporter gene assays (e.g., ERE-luciferase) to detect estrogenic/anti-estrogenic activity [6]. | Identifying estrogenic leachates from BPA-free plastics [6]. |
| BG1Luc Cell Line | A human ovarian cell line stably transfected with an estrogen-responsive luciferase reporter, used for high-throughput screening of ER agonists and antagonists. | Quantifying the estrogenic potency of BPA analogs relative to BPA and estradiol [6]. |
| 3D Liver Spheroid Models | Multicellular, three-dimensional structures that mimic human liver architecture and function for studying organ-specific toxicity [9]. | Investigating the mechanisms of PFAS-induced liver disease and testing reversibility [9]. |
| Certified Reference Materials | Matrices with known concentrations of EDCs (e.g., in urine, serum) used to calibrate equipment and validate analytical methods for biomonitoring. | Ensuring accuracy and inter-laboratory comparability in human cohort studies measuring phthalate metabolites [7]. |
| Specific Antibodies | For immunohistochemistry (IHC) and Western Blot to assess tissue morphology, protein expression, and signaling pathway activation in animal models. | Evaluating the effect of BPA on HOXB9 protein expression in mammary tumor tissue [3]. |
| LC-MS/MS Systems | Liquid Chromatography with Tandem Mass Spectrometry for the sensitive and specific quantification of EDCs and their metabolites in complex biological and environmental samples [7]. | Measuring concentrations of multiple phthalate metabolites in urine samples from GDM patients and controls [7]. |
| 4-(Methylthio)quinazoline | 4-(Methylthio)quinazoline|CAS 13182-59-7 | 4-(Methylthio)quinazoline (CAS 13182-59-7) is a versatile quinazoline derivative for pharmaceutical research. This product is For Research Use Only. Not for human or veterinary use. |
| H-Arg-Gly-D-Asp-OH.TFA | H-Arg-Gly-D-Asp-OH.TFA RGD Peptide|For Research | H-Arg-Gly-D-Asp-OH.TFA is an integrin-binding RGD peptide for cell adhesion research. For Research Use Only. Not for human use. |
Endocrine-disrupting chemicals (EDCs) are exogenous compounds that interfere with the synthesis, secretion, transport, binding, action, or elimination of natural hormones in the body, thereby disrupting homeostasis and the normal functioning of the endocrine system [10] [11]. The global decline in fertility rates has become a significant public health concern, with substantial evidence pointing to the role of environmental factors, including exposure to EDCs, as a contributing factor [12] [13]. These chemicals can exert their effects at extremely low doses and are particularly damaging during critical developmental windows, such as fetal development, leading to irreversible and even transgenerational effects on reproductive health [14] [11].
EDCs comprise a heterogeneous group of chemicals found in various industrial and consumer products, including plasticizers (e.g., bisphenol A, phthalates), pesticides (e.g., vinclozolin, DDT), heavy metals, and persistent organic pollutants [10] [14] [15]. The molecular pathways through which EDCs disrupt fertility are complex and involve direct interactions with nuclear hormone receptors (genomic pathways) and rapid signaling cascades initiated at the cell membrane (non-genomic pathways). This whitepaper provides an in-depth technical analysis of these mechanisms, focusing on EDC interactions with estrogen receptors (ERs), androgen receptors (ARs), and thyroid hormone receptors (TRs), which represent critical nodes in the endocrine control of reproduction [16] [17].
Estrogen Receptor (ER) Signaling Disruption
ER Subtypes and Structural Basis for Ligand Recognition
The estrogen signaling pathway is primarily mediated by two nuclear receptors: estrogen receptor alpha (ERα) and estrogen receptor beta (ERβ) [17]. These receptors, while binding the endogenous ligand 17β-estradiol (E2) with similar affinity, have distinct tissue distributions and often oppose each other's physiological functions. ERα, encoded by the ESR1 gene on chromosome 6, is a 66 kDa protein consisting of 595 amino acids and is the dominant receptor in the breast, uterus, and liver. ERβ, encoded by the ESR2 gene on chromosome 14, is a 54 kDa protein of approximately 530 amino acids and is prominently expressed in the ovary, prostate, and cardiovascular system [10] [18] [17].
Structurally, both ERs are modular proteins containing:
- An N-terminal domain (A/B domain) housing the ligand-independent activation function-1 (AF-1)
- A central DNA-binding domain (DBD or C domain) with two zinc finger motifs
- A hinge region (D domain) containing a nuclear localization signal
- A C-terminal ligand-binding domain (LBD or E/F domain) containing the ligand-dependent activation function-2 (AF-2) [18]
The LBD, composed of 12 alpha helices, undergoes significant conformational change upon agonist binding, particularly in the positioning of helix 12, which creates a hydrophobic groove for the recruitment of coactivator proteins with LXXLL motifs [18] [17]. The ligand-binding pockets of ERα and ERβ share high similarity but differ in two key amino acids (Leu384/Met336 and Met421/Ile373 in ERα/ERβ, respectively), which contribute to subtype selectivity for certain ligands [17].
Genomic Signaling Disruption by EDCs
In the classical genomic signaling pathway, E2 binding induces ER dissociation from heat shock proteins (e.g., Hsp90), receptor dimerization, and binding to estrogen response elements (EREs) in the promoter regions of target genes [10] [18]. The consensus ERE is a palindromic 13-base pair sequence (GGTCAnnnTGACC) [17]. The receptor-ligand complex then recruits coregulators and the general transcription machinery to initiate gene transcription.
EDCs such as bisphenol A (BPA), diethylstilbestrol (DES), octyl-phenol (OP), and nonyl-phenol (NP) can mimic natural estrogens by binding to ERs and initiating this transcriptional program [10] [17]. However, their effects are complex and tissue-specific, similar to selective estrogen receptor modulators (SERMs). For instance, BPA acts primarily as an ER agonist in most contexts, while the drug tamoxifen acts as an antagonist in breast tissue but an agonist in the uterus [18]. The transcriptional outcome of ER-EDC interaction depends on several factors, including the specific EDC, ER subtype (ERα vs. ERβ), cellular context, promoter architecture, and available cofactor repertoire [17].
Table 1: Common Estrogenic EDCs and Their Receptor Affinities
| EDC | Primary Source | ERα Activity | ERβ Activity | Relative Potency |
|---|---|---|---|---|
| Diethylstilbestrol (DES) | Pharmaceutical | Agonist | Agonist | High |
| Bisphenol A (BPA) | Plastics, food containers | Agonist/Weak Antagonist | Agonist/Weak Antagonist | Low (1000-fold lower than E2) |
| Octyl-phenol (OP) | Surfactants, detergents | Agonist | Agonist | Low |
| Nonyl-phenol (NP) | Surfactants, detergents | Agonist | Agonist | Low |
| Genistein (phytoestrogen) | Soy products | Agonist | Preferential Agonist | Low |
Non-Genomic Signaling Disruption by EDCs
Beyond genomic actions, EDCs can rapidly activate signal transduction pathways within minutes through membrane-associated ERs and G-protein coupled receptors (e.g., GPER) [10]. This non-genomic signaling involves the activation of kinases such as ERK1/2 (MAPK), Akt, and protein kinase A (PKA), leading to phosphorylation of transcription factors (e.g., ELK-1, CREB) and other cellular proteins [10] [17]. For example, BPA has been shown to rapidly activate ERK1/2 and Akt in various cell models [10]. These rapid signaling events can ultimately influence transcriptional activity through cross-talk with nuclear ERs, such as via phosphorylation of ERα at key residues (e.g., Ser118, Ser167) by MAPK and Akt, respectively, which enhances its transcriptional activity in a ligand-independent manner [18].
The following diagram illustrates the complex genomic and non-genomic signaling pathways disrupted by estrogenic EDCs:
Androgen Receptor (AR) Signaling Disruption
AR Structure and Signaling Pathway
The androgen receptor is a critical regulator of male reproductive development and function, including spermatogenesis, development of secondary sexual characteristics, and maintenance of sexual behavior [12]. AR belongs to the nuclear receptor superfamily and shares a common domain structure with ERs. Upon binding its natural ligands testosterone or dihydrotestosterone (DHT), AR undergoes conformational changes, dissociates from chaperone proteins, dimerizes, and translocates to the nucleus where it binds to androgen response elements (AREs) in target genes to regulate transcription [12] [13].
Mechanisms of AR Disruption by EDCs
EDCs can interfere with AR signaling through multiple mechanisms:
- Receptor Antagonism: Chemicals like vinclozolin (a fungicide) and p,p'-DDE (a DDT metabolite) act as competitive AR antagonists, binding to the receptor but failing to activate it properly, thereby blocking natural androgen action [12] [17].
- Inhibition of Androgen Synthesis: Phthalates such as DEHP and DBP can suppress the expression of genes involved in testosterone biosynthesis, including steroidogenic acute regulatory protein (StAR) and various cytochrome P450 enzymes [12] [13].
- Altered Metabolic Activation: Some EDCs can interfere with the enzymatic conversion of testosterone to the more potent DHT by inhibiting 5α-reductase [13].
The anti-androgenic effects of EDCs have significant implications for male reproductive health. Population studies have consistently associated EDC exposure with reduced sperm quality, and animal studies provide compelling evidence for transgenerational inheritance of reproductive dysfunction through epigenetic mechanisms [12].
Table 2: Anti-Androgenic EDCs and Their Mechanisms of Action
| EDC | Primary Source | Mechanism of Action | Observed Male Reproductive Effects |
|---|---|---|---|
| Vinclozolin | Fungicide | AR antagonism | Reduced sperm count, hypospadias, transgenerational effects |
| p,p'-DDE | DDT metabolite | AR antagonism | Cryptorchidism, reduced semen quality |
| Phthalates (DEHP, DBP) | Plastics, personal care products | Suppress testosterone synthesis | Reduced anogenital distance, malformations of reproductive tract |
| Procymidone | Fungicide | AR antagonism | Impaired masculinization, retained nipples |
| PBDEs | Flame retardants | Altered steroidogenesis | Reduced sperm count, altered thyroid function |
Thyroid Hormone Receptor (TR) Signaling Disruption
Thyroid Hormone System and Reproductive Health
Thyroid hormones (THs) - thyroxine (T4) and triiodothyronine (T3) - are essential for normal development, metabolism, and reproductive function [15]. The hypothalamic-pituitary-thyroid (HPT) axis regulates TH production and secretion. In reproduction, thyroid hormones interact with the hypothalamic-pituitary-gonadal (HPG) axis, modulating the secretion of gonadotropin-releasing hormone (GnRH) and gonadotropins, and directly influencing gonadal function [15].
Molecular Mechanisms of TR Disruption
EDCs can interfere with thyroid hormone signaling at multiple levels:
Receptor-Level Interference: EDCs such as bisphenol A and certain polychlorinated biphenyls (PCBs) can act as TR antagonists, competing with endogenous T3 for receptor binding [15]. Some EDCs can also bind to TRs and exhibit weak agonist activity.
Disruption of TH Synthesis and Transport: Numerous EDCs affect the sodium/iodide symporter (NIS), thyroperoxidase (TPO), or deiodinase enzymes:
- Perchlorate: Competes with iodide for NIS, reducing iodide uptake and TH synthesis [15].
- Thiocyanates and isoflavones: Inhibit TPO, blocking TH synthesis [15].
- PCBs and PBDEs: Alter TH transport by competing with T4 for binding to transport proteins (transthyretin) and affect TH metabolism by modifying deiodinase activities [15].
The following diagram summarizes the key sites of disruption in the thyroid hormone system by EDCs:
Non-Genomic Signaling Pathways
Characteristics and Significance
Non-genomic signaling refers to rapid, transcription-independent cellular responses to hormones that typically occur within seconds to minutes [10] [17]. These pathways are crucial for understanding EDC actions because:
- They often operate at low EDC concentrations
- They exhibit non-monotonic dose responses
- They can lead to altered cellular responses through cross-talk with genomic pathways [10] [14]
Key Non-Genomic Mechanisms
EDCs can activate various non-genomic signaling pathways:
Calcium and Kinase Signaling: EDCs like BPA and OP can rapidly increase intracellular calcium levels and activate protein kinase C (PKC) and mitogen-activated protein kinase (MAPK) cascades [10].
Cross-Talk with Growth Factor Signaling: Estrogenic EDCs can transactivate epidermal growth factor receptor (EGFR) and insulin-like growth factor receptor (IGF-1R), leading to downstream activation of ERK and Akt pathways [10] [18].
G-Protein Coupled Receptor Activation: Several EDCs mediate rapid effects through membrane receptors like GPER, which activates adenylate cyclase and phospholipase C, generating second messengers such as cAMP and IP3 [17].
The rapid activation of these signaling cascades by EDCs can profoundly influence cell proliferation, apoptosis, differentiation, and metabolism, with significant implications for reproductive tissue function and development [10] [17].
Experimental Approaches and Methodologies
In Vitro Assays for Detecting EDC Activity
A variety of in vitro assays have been developed to identify and characterize EDCs targeting ER, AR, and TR signaling:
Table 3: Key Experimental Assays for EDC Detection and Characterization
| Assay Type | Specific Method | Application | Key Endpoints |
|---|---|---|---|
| Receptor Binding Assays | Fluorescence polarization, competitive binding | Measure direct receptor-EDC interaction | Binding affinity (IC50, Ki) |
| Transcriptional Activation Assays | Reporter gene assays (Luciferase, GFP) | Detect agonist/antagonist activity | EC50, IC50, efficacy |
| Cell Proliferation Assays | MCF7 breast cancer cell proliferation (E-SCREEN) | Detect estrogenic activity | Cell number, thymidine incorporation |
| High-Throughput Screening | ToxCast/Tox21 programs | Large-scale EDC screening | Multiple activity profiles |
| Omic Technologies | Transcriptomics, QGexAR models | Predictive modeling of EDC activity | Gene expression signatures [16] |
Detailed Protocol: Transcriptional Reporter Assay for ER Activity
Principle: This assay measures the ability of test chemicals to activate or inhibit estrogen receptor-mediated transcription of a reporter gene (typically luciferase) under the control of an estrogen response element (ERE) [17].
Materials:
- Cell Line: hERα-HeLa-9903 cells (stably transfected with human ERα and ERE-luciferase reporter) [17]
- Controls: 17β-estradiol (E2, 10 nM) as positive control; ICI 182,780 (1 μM) as antagonist control; vehicle (DMSO <0.1%) as negative control
- Test Chemicals: BPA, DES, OP, NP, genistein prepared in DMSO
- Reagents: Luciferase assay kit, cell culture media, phenol-red free DMEM, charcoal-dextran treated FBS
Procedure:
- Cell Preparation: Plate hERα-HeLa-9903 cells in 96-well plates at 2×10^4 cells/well in phenol-red free DMEM supplemented with 5% charcoal-dextran treated FBS. Incubate at 37°C, 5% CO2 for 24 hours.
- Chemical Treatment: Treat cells with test chemicals at various concentrations (e.g., 10^-12 to 10^-5 M) in triplicate. Include controls. Incubate for 16-24 hours.
- Luciferase Measurement: Aspirate media, lyse cells with 50 μL passive lysis buffer (Promega) for 15 minutes at room temperature. Transfer 20 μL lysate to white plates, inject 50 μL luciferase assay substrate, and measure luminescence immediately.
- Data Analysis: Normalize luminescence to protein content or cell viability. Calculate fold induction relative to vehicle control. Determine EC50/IC50 values using four-parameter logistic curve fitting.
Validation: The assay should demonstrate a dose-dependent response to E2 with typical EC50 of 0.1-0.3 nM. Antagonists should inhibit E2-induced activity in a dose-dependent manner.
Detailed Protocol: Detection of Non-Genomic ERK Activation
Principle: This protocol detects rapid phosphorylation of ERK1/2 as an indicator of non-genomic signaling activation by EDCs [10].
Materials:
- Cell Line: MCF-7 breast cancer cells or primary granulosa cells
- Antibodies: Anti-phospho-ERK1/2 (Thr202/Tyr204), anti-total ERK1/2, HRP-conjugated secondary antibodies
- Inhibitors: U0126 (MEK inhibitor, 10 μM), ICI 182,780 (ER antagonist, 1 μM)
- Reagents: SDS-PAGE reagents, ECL detection system, serum-free media
Procedure:
- Cell Preparation: Culture cells to 70-80% confluence in appropriate media. Serum-starve for 4-6 hours before treatment to reduce basal phosphorylation.
- Chemical Treatment: Treat cells with test EDCs (e.g., BPA, OP) at relevant concentrations for 5-60 minutes. Include E2 (10 nM) as positive control and vehicle as negative control.
- Inhibition Studies: Pre-treat cells with U0126 (30 minutes) or ICI 182,780 (30 minutes) to determine MEK-dependence and ER involvement, respectively.
- Protein Extraction and Western Blot: Lyse cells in RIPA buffer with protease and phosphatase inhibitors. Separate 20-30 μg protein by SDS-PAGE, transfer to PVDF membranes, block with 5% BSA, and incubate with primary antibodies (1:1000) overnight at 4°C.
- Detection: Incubate with HRP-conjugated secondary antibodies (1:2000) for 1 hour at room temperature. Develop with ECL substrate and visualize using chemiluminescence detection system.
- Analysis: Quantify band intensities using densitometry software. Normalize phospho-ERK to total ERK levels. Perform statistical analysis of at least three independent experiments.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools for Investigating EDC Mechanisms
| Reagent/Cell Line | Supplier Examples | Application in EDC Research |
|---|---|---|
| MCF-7 cells | ATCC (HTB-22) | Model for estrogenic activity; express ERα endogenously |
| MDA-kb2 cells | ATCC (CRL-2713) | Androgen-responsive cell line for anti-androgen screening |
| hERα-HeLa-9903 | NIEHS Chemical Repository | Stably transfected with ERα and ERE-luciferase reporter |
| ERE-Luc Reporter Plasmid | Addgene | For creating custom ER-responsive cell lines |
| Recombinant human ERα/ERβ | Invitrogen, Sino Biological | For direct binding assays (fluorescence polarization) |
| Phospho-ERK1/2 Antibody | Cell Signaling Technology (#9101) | Detection of non-genomic signaling activation |
| Charcoal-dextran treated FBS | Thermo Fisher Scientific | Estrogen-depleted serum for hormone-responsive assays |
| Luciferase Assay Systems | Promega | Reporter gene assays for receptor activity |
| ToxCast/Tox21 Database | EPA/NIEHS | Pre-screened data on thousands of chemicals [16] |
| LINCS L1000 Database | NIH | Transcriptomic profiles of chemical perturbations [16] |
| Befotertinib mesylate | Befotertinib mesylate, CAS:2226167-02-6, MF:C30H36F3N7O5S, MW:663.7 g/mol | Chemical Reagent |
| 1H-Silolo[1,2-a]siline | 1H-Silolo[1,2-a]siline, CAS:918897-39-9, MF:C8H8Si, MW:132.23 g/mol | Chemical Reagent |
The molecular pathways through which EDCs disrupt fertility involve complex interactions with nuclear receptors (ER, AR, TR) and activation of non-genomic signaling cascades. Understanding these mechanisms at a detailed level is crucial for developing better risk assessment strategies, identifying susceptible populations, and designing interventions to mitigate the adverse effects of EDCs on human reproduction. The integration of traditional endocrine assays with modern high-throughput screening and computational modeling approaches represents the future of EDC research, enabling more comprehensive assessment of these chemicals and their mixtures on reproductive health across generations.
The hypothalamic-pituitary-gonadal (HPG) axis is a tiered, linearly organized endocrine system dedicated to the regulation and support of reproductive processes [19]. This axis functions through a precise signaling cascade: a small subset of hypothalamic neurons secretes gonadotropin-releasing hormone (GnRH), which is delivered to the anterior pituitary via the hypophyseal portal circulation [19]. Upon binding to GnRH receptors on pituitary gonadotrope cells, this triggers the synthesis and secretion of the gonadotropins luteinizing hormone (LH) and follicle-stimulating hormone (FSH) [19]. These gonadotropins then act on the gonads (ovaries or testes) to stimulate steroidogenesis and gametogenesis.
A critical feature of this system is its pulsatile regulation. The precise frequency and amplitude of GnRH pulses are essential for adequate gonadotropin production, with different pulse frequencies preferentially promoting LH or FSH synthesis [19]. This pulsatile activity is highly regulated by kisspeptins, neuropeptides that bind to the GPR54 receptor on GnRH neurons and serve as central processors for relaying peripheral signals [20] [19]. The gonadal steroids (estradiol, progesterone, testosterone) produced in response to LH and FSH then complete the axis by exerting feedback mechanisms on the hypothalamus and pituitary to maintain homeostasis [19]. It is this meticulously balanced system that endocrine-disrupting chemicals (EDCs) target, leading to widespread reproductive consequences.
Mechanisms of HPG Axis Disruption by Endocrine-Disrupting Chemicals
Endocrine-disrupting chemicals interfere with the normal function of the HPG axis through multiple mechanisms, ultimately leading to hormonal imbalance and impaired fertility. Their actions can be broadly categorized into the following pathways.
Direct Receptor Agonism and Antagonism
Many EDCs structurally mimic natural steroid hormones, allowing them to directly bind to and activate or block hormone receptors.
- Estrogen Receptor (ER) Mediated Signalling: Numerous EDCs, including bisphenol A (BPA), octyl-phenol (OP), nonyl-phenol (NP), and diethylstilbestrol (DES), act as xenoestrogens by binding to estrogen receptors (ERα and ERβ) with an affinity up to 1000-fold lower than that of endogenous estradiol [10]. This binding can induce tissue-specific oestrogenic responses, acting as either an ER agonist or antagonist, and leading to the dysregulation of ER-dependent transcriptional signalling pathways [10]. The binding of EDCs to nuclear ERs can trigger genomic pathways that alter gene expression over hours, while interaction with membrane ERs can rapidly activate non-genomic pathways, such as ERK1/2 and Akt, within minutes [10].
- Androgen and Progesterone Receptor Interference: EDCs can also bind to and disrupt the function of other steroid hormone receptors, including the androgen receptor (AR) and progesterone receptor (PR) [10]. This interference can block the action of endogenous androgens and progesterone, which are critical for normal reproductive function in both males and females. The disruption of progesterone signalling, for instance, is particularly relevant given progesterone's pivotal role in the growth and development of uterine fibroids [21].
Disruption of Hormone Synthesis and Metabolism
Beyond receptor interactions, EDCs can interfere with the enzymatic pathways responsible for hormone synthesis and clearance.
- Steroidogenic Enzyme Inhibition: EDCs can inhibit key enzymes involved in steroid hormone biosynthesis, such as cytochrome P450 enzymes (e.g., CYP17A1, aromatase) [22]. For example, reduced aromatase activity would impair the conversion of androgens to estrogens, disrupting the critical balance between these hormones [19].
- Alteration of Hormone Transport and Metabolism: Some EDCs can influence the synthesis of sex hormone-binding globulin (SHBG), affecting the bioavailability of sex steroids [20]. Others may induce liver enzymes that accelerate the metabolic clearance of hormones, effectively reducing their circulating levels [22].
Indirect Effects via the Neuroendocrine System
EDCs can also exert their effects higher up the HPG axis by interfering with central regulatory systems.
- Disruption of GnRH and Kisspeptin Signalling: Exposure to EDCs can alter the expression and release of kisspeptin, a master regulator of GnRH neurons [19] [23]. This disruption can distort the pulsatile secretion of GnRH, which is a prerequisite for normal gonadotropin release. An aberrant GnRH pulse pattern can favour the production of one gonadotropin (e.g., LH) over another (e.g., FSH), leading to conditions like hyperandrogenism, which is often seen in polycystic ovary syndrome (PCOS) [20] [19].
- Induction of Oxidative Stress and Apoptosis: EDC exposure can induce cellular stress in reproductive tissues. For instance, BPA and BPF have been shown to induce apoptosis in ovarian granulosa cells via the intrinsic mitochondrial pathway, compromising follicle health and female fertility [23]. Similarly, oxidative stress in testicular Sertoli and Leydig cells can impair spermatogenesis and steroidogenesis [22].
Table 1: Summary of Key Mechanisms of HPG Axis Disruption by EDCs
| Mechanism of Action | Representative EDCs | Key Molecular/Cellular Effects | Reproductive Outcome |
|---|---|---|---|
| ER Agonism/Antagonism | BPA, DES, OP, NP, DDT [10] | Altered ER-dependent transcription; Activation of non-genomic signalling (ERK, Akt) [10] | Altered ovarian function, impaired folliculogenesis, cancer growth [10] [23] |
| AR/PR Antagonism | Phthalates, certain pesticides [10] [22] | Blockade of endogenous androgen/progesterone action [10] | Malefactorize: undermasculinization; Female: uterine disorders [21] [22] |
| Steroidogenic Disruption | Phthalates, cadmium, azole fungicides [22] | Inhibition of CYP enzymes (e.g., aromatase, CYP17A1) [22] | Altered sex steroid ratios (e.g., low E2, high T), anovulation [19] [22] |
| Neuroendocrine Disruption | PCBs, BPA, dioxins [23] [22] | Altered kisspeptin and GnRH pulsatility [19] [23] | Gonadotropin imbalance (e.g., elevated LH:FSH), ovulatory dysfunction [20] [19] |
| Oxidative Stress & Apoptosis | Cadmium, BPA, BPF [23] [22] | Generation of ROS; mitochondrial apoptosis in granulosa/Sertoli cells [23] [22] | Reduced sperm quality; ovarian follicle atresia; decreased fertility [23] [22] |
The figure below provides a simplified overview of the HPG axis and the major sites where EDCs exert their interfering effects.
Experimental Models and Methodologies for Investigating EDC Effects
Understanding the impact of EDCs on the HPG axis requires a multi-faceted experimental approach, utilizing everything from in vitro models to human epidemiological studies.
In Vitro Models
In vitro systems are invaluable for elucidating the specific molecular mechanisms of EDC action.
- Cell-Based Reporter Assays: These assays are designed to detect receptor activity (e.g., ER, AR). A common method involves transfecting cells with a plasmid containing an estrogen-response element (ERE) linked to a reporter gene (e.g., luciferase). Exposure to an ER-activating EDC results in receptor binding, transcription of the reporter gene, and a measurable signal (e.g., luminescence), allowing for the quantification of estrogenic potency [10].
- Primary Cell and Tissue Culture Models: Using primary human cells, such as granulosa cells or ovarian cortex tissue explants, provides a more physiologically relevant model. For instance, ovarian cortical tissue culture can be used to assess the direct effects of EDCs on follicle survival and function. The protocol involves obtaining consented human ovarian tissue, dissecting it into small pieces, and culturing them in a specialized medium. Tissues are then exposed to EDCs like BPA or BPF, after which endpoints such as gene expression profiling (e.g., RNA-sequencing), hormone secretion (estradiol), and histology for follicle health are analyzed [24].
- Mechanistic Toxicity Testing: Beyond receptor binding, in vitro models can probe deeper into mechanisms like oxidative stress and apoptosis. For example, to investigate EDC-induced apoptosis in granulosa cells, researchers can treat cells with EDCs and then measure markers like caspase activation, mitochondrial membrane potential (using JC-1 dye), and the ratio of pro- and anti-apoptotic Bcl-2 family proteins via Western blot [23].
In Vivo Animal Models
Animal studies are crucial for understanding the complex, system-wide consequences of EDC exposure during different developmental windows.
- Immature Rat Uterotrophic Assay: This is a classic, OECD-validated bioassay for detecting estrogenic activity. Immature female rats are ovariectomized to remove endogenous estrogen and allowed to recover. They are then administered the test EDC for 3-5 days. The uterus is subsequently weighed (wet and blotted wet weight). A statistically significant increase in uterine weight in the treated group compared to the control is indicative of estrogenic activity [10].
- Assessment of Pubertal Timing and Ovarian Morphology: To study long-term effects on the HPO axis, perinatal or pubertal animals are exposed to EDCs. Parameters monitored include the day of vaginal opening (a marker of puberty onset), estrous cyclicity via daily vaginal cytology, and terminal analysis of ovarian morphology, looking for signs like polycystic ovaries or reduced follicle counts [20] [23].
- Transgenerational Epigenetic Studies: These experiments involve exposing pregnant females (F0 generation) to EDCs and then studying the offspring (F1) and their subsequent, unexposed generations (F2, F3). Germ cells (sperm or oocytes) and somatic tissues from these generations are analyzed for epigenetic marks, such as DNA methylation patterns via bisulfite sequencing, to identify epimutations that may underlie inherited disease susceptibility [22].
Human Cohort Studies and Exposure Assessment
Translating findings from models to human health requires epidemiological studies.
- Assisted Reproductive Technology (ART) Cohorts: Women and couples undergoing fertility treatments like IVF represent a highly informative cohort. Studies can investigate correlations between internal concentrations of EDCs (measured in urine, blood, or follicular fluid) and ART outcomes such as oocyte yield, fertilization rate, embryo quality, and live birth rates [25] [23]. For example, a study by Guo et al. linked the use of personal care products (a source of EDCs like phthalates and parabens) with lower oocyte maturation rates and a higher risk of miscarriage in women undergoing IVF/ICSI [23].
- Mixture Risk Assessment: Given that humans are exposed to complex mixtures of EDCs, advanced statistical models are employed to assess combined effects. Concentration Addition (CA) and Independent Action (IA) models are two primary predictive frameworks used to estimate the toxicity of chemical mixtures based on data from individual compounds [22].
The workflow for a comprehensive investigation of an EDC's impact on female fertility, integrating these various models, is depicted below.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Research Reagents for Investigating EDC Effects on the HPG Axis
| Reagent / Material | Function and Application in EDC Research |
|---|---|
| Immature Rat Model (Uterotrophic Assay) | In vivo bioassay for detecting estrogenic activity of a test compound by measuring increase in uterine weight [10]. |
| Primary Human Granulosa Cells | Used in in vitro cultures to study direct EDC effects on steroidogenesis (e.g., estradiol production), apoptosis, and gene expression relevant to ovarian function [23]. |
| Human Ovarian Cortex Explants | Ex vivo tissue culture model that preserves the ovarian microenvironment, allowing study of EDC effects on early follicle development and survival [24]. |
| Kisspeptin Antibodies | Used for immunohistochemistry or Western blot to localize and quantify kisspeptin expression in hypothalamic tissues after EDC exposure [19]. |
| RNA-sequencing Reagents | For comprehensive, unbiased profiling of transcriptomic changes in tissues (e.g., hypothalamus, pituitary, gonad) or cells after EDC exposure to identify disrupted pathways [24]. |
| Bisulfite Conversion Kit | Essential for preparing DNA for methylation analysis to investigate EDC-induced epigenetic changes (e.g., in transgenerational studies) [22]. |
| Caspase-3/7 Activity Assay Kit | Fluorometric or luminescent kit to quantify apoptosis activation in cells (e.g., granulosa cells) treated with EDCs like BPA or BPF [23]. |
| LC-MS/MS (Liquid Chromatography-Tandem Mass Spectrometry) | Gold-standard analytical technique for precise quantification of EDCs (e.g., BPA, phthalate metabolites) and endogenous hormones in biological samples like urine and serum [23] [22]. |
| ER-Specific Reporter Gene Assay | Cell line (e.g., HeLa, MCF-7) engineered with an ERE-luciferase construct to specifically quantify ER agonist/antagonist activity of test chemicals [10]. |
| 1-Isopropylazulene | 1-Isopropylazulene|Research Grade|RUO |
| Malathion beta-Monoacid-d5 | Malathion beta-Monoacid-d5, MF:C8H15O6PS2, MW:307.3 g/mol |
Implications for Drug Development and Therapeutic Interventions
The insights gained from research on HPG axis disruption are directly informing the development of novel therapeutic strategies, particularly in the realm of reproductive medicine.
- GnRH Antagonists as a Targeted Therapy: Understanding the central role of GnRH has led to the development and clinical use of oral, non-peptide GnRH antagonists such as elagolix, relugolix, and linzagolix [26] [21]. Unlike GnRH agonists, which cause an initial "flare effect" of increased gonadotropin and estrogen secretion, antagonists competitively block the GnRH receptor, leading to a rapid, dose-dependent suppression of the HPG axis without a flare [26]. These drugs are approved for managing conditions like endometriosis-associated pain and heavy menstrual bleeding associated with uterine fibroids [26] [21].
- The Critical Role of Add-Back Therapy (ABT): The suppression of the HPG axis by GnRH antagonists creates a hypoestrogenic state, leading to side effects such as hot flushes and bone mineral density loss. To mitigate these effects while maintaining therapeutic efficacy, add-back therapy with low-dose estradiol and progestins (e.g., norethindrone acetate) is co-administered [26] [21]. This approach demonstrates a sophisticated application of HPG axis knowledge: achieving a "window" of estrogen suppression sufficient to treat the disease while providing just enough hormone replacement to protect against major side effects, thereby enabling longer-term treatment [26].
- Informing Fertility Treatment Protocols: Research on EDCs that disrupt the HPO axis, such as those found in personal care products, reinforces the need for careful patient history and exposure assessment in clinical fertility practice [23]. Furthermore, the use of hormonal contraceptives to pretreat patients before IVF cycles is a direct application of controlling the HPO axis to synchronize follicular cohorts and time cycles, despite ongoing research into its nuanced effects on outcomes like live birth rates [25].
In conclusion, the systematic interrogation of HPG axis interference by EDCs has not only revealed profound insights into the origins of reproductive diseases but has also catalysed the development of sophisticated, targeted therapeutics. The continued use of integrated experimental models and advanced molecular tools is essential for fully understanding the risks posed by complex EDC mixtures and for designing effective interventions to safeguard and restore reproductive health.
Endocrine-disrupting chemicals (EDCs) are exogenous substances that interfere with hormone action, thereby increasing the risk of adverse health outcomes, including reproductive impairment and infertility [27]. A growing body of evidence links EDC exposure to dysfunctional cellular processes within the reproductive system, primarily oxidative stress, apoptosis, and impaired steroidogenesis [28] [29] [30]. These intertwined molecular pathways form a core mechanistic basis for the adverse fertility outcomes observed in contemporary research. This whitepaper details the specific cellular and molecular consequences of EDC exposure, framing them within the broader context of fertility research for scientists and drug development professionals. It synthesizes current findings, provides structured experimental data, and outlines key methodological approaches for investigating these critical pathways.
Core Cellular Pathologies Induced by EDCs
Oxidative Stress
Oxidative stress occurs when the production of reactive oxygen species (ROS) overwhelms the capacity of the antioxidant defense system. EDCs can directly promote ROS generation or deplete antioxidant reserves, leading to lipid, protein, and DNA damage [28]. The nuclear factor erythroid 2-related factor 2 (Nrf2) pathway is a primary cellular defense mechanism against oxidative stress. Under normal conditions, Nrf2 is sequestered in the cytoplasm by its repressor, Kelch-like ECH-associated protein 1 (Keap1), and targeted for degradation. During oxidative stress, Nrf2 is stabilized, translocates to the nucleus, and activates the transcription of antioxidant genes, including heme oxygenase-1 (HO-1) [28]. EDC-induced disruption of this pathway critically compromises cellular resilience.
Apoptosis
EDCs can trigger programmed cell death, or apoptosis, through both intrinsic (mitochondrial) and extrinsic (death receptor) pathways. This leads to the activation of caspase enzymes, such as caspase-3, which execute the cell death program [28]. In testicular and ovarian tissues, this results in the loss of germ cells and supporting somatic cells (e.g., Leydig and Sertoli cells), directly reducing gamete quality and count, and impairing reproductive function [28] [31] [32].
Impaired Steroidogenesis
Steroidogenesis is the process by which cholesterol is converted into biologically active steroid hormones. EDCs can disrupt the intricate hormonal feedback loops of the hypothalamic-pituitary-gonadal (HPG) axis and directly inhibit the expression and activity of key steroidogenic enzymes and proteins, such as cytochrome P450 side-chain cleavage enzyme (CYP11A1), 17β-hydroxysteroid dehydrogenase (HSD17B3), and steroidogenic acute regulatory protein (StAR) [28] [30]. This leads to insufficient production of sex steroids like testosterone and estradiol, which are essential for reproductive development, function, and fertility [28] [31].
Quantitative Data from Experimental Models
Recent in vivo studies provide quantitative evidence of these cellular consequences and the potential for therapeutic intervention. The following tables summarize key findings from a rat model investigating cisplatin-induced testicular damage and the protective effects of Lisinopril (LSP), which highlighted the involvement of the Nrf2/Keap1/HO-1 and PPARγ signaling pathways [28].
Table 1: Impact of Lisinopril (LSP) on Cisplatin (CDDP)-Induced Hormonal Changes and Oxidative Stress in Rat Testis
| Parameter | CDDP Group vs. Control | LSP + CDDP Group vs. CDDP Group | Effect Size (f) & Statistical Power |
|---|---|---|---|
| Luteinizing Hormone | Decreased | Effectively Increased | f=2.56, Power=1.00 [28] |
| Follicle-Stimulating Hormone | Decreased | Effectively Increased | f=2.32, Power=1.00 [28] |
| Testosterone | Decreased | Effectively Increased | f=3.02, Power=1.00 [28] |
| Reduced Glutathione | Decreased | Increased Levels | f=1.72, Power=0.99 [28] |
| Superoxide Dismutase | Decreased | Increased Levels | f=1.72, Power=0.99 [28] |
| Malondialdehyde | Increased | Decreased Levels | f=3.07, Power=1.00 [28] |
Table 2: Molecular and Genetic Alterations in Testis Tissue from CDDP and LSP+CDDP Treatment
| Parameter | CDDP Group vs. Control | LSP + CDDP Group vs. CDDP Group | Effect Size (f) & Statistical Power |
|---|---|---|---|
| Cleaved Caspase-3 | Increased | Decreased | f=4.61, Power=1.00 [28] |
| Interleukin-1β, TNF-α, IL-6 | Increased | Decreased | f=4.61, Power=1.00 [28] |
| Nuclear Factor Kappa B | Increased | Decreased | f=4.61, Power=1.00 [28] |
| Keap1 Protein | Increased | Reduction in Level | f=5.50, Power=1.00 [28] |
| Nrf2 Protein | Decreased | Increase in Level | f=5.50, Power=1.00 [28] |
| HO-1 Protein | Decreased | Increase in Level | f=3.66, Power=1.00 [28] |
| PPARγ Protein | Decreased | Increase in Level | Reported [28] |
| CYP11a1, HSD17B3, StAR Genes | Downregulated | Upregulated | Reported [28] |
Detailed Experimental Protocol
The following methodology is adapted from a recent study investigating chemoprotective agents against chemotherapy-induced testicular toxicity [28].
Animal Model and Study Design
- Animals: Adult male Sprague-Dawley rats (or comparable strain).
- Groups: Rats are randomly assigned into four groups (n=8-10/group):
- Control Group: Receives vehicle only (e.g., saline orally).
- LSP Group: Receives Lisinopril (10 mg/kg) orally for 10 days.
- CDDP Group: Receives a single dose of Cisplatin (e.g., 10 mg/kg intraperitoneally).
- LSP + CDDP Group: Pre-treated with Lisinopril (10 mg/kg orally) for a set period (e.g., 5 days) before receiving a single Cisplatin dose, with Lisinopril treatment continuing for a total of 10 days.
- Sacrifice and Sample Collection: Animals are sacrificed at a predetermined endpoint (e.g., 10 days post-CDPP). Blood is collected for serum hormone profiling, and target tissues (e.g., testes) are rapidly excised. One portion is fixed for histopathology, and another is snap-frozen for biochemical and molecular analyses.
Histopathological Analysis
- Tissue Fixation: Testis samples are fixed in Bouin's solution or 10% neutral buffered formalin for 24 hours.
- Processing and Staining: Tissues are processed through graded alcohols and xylene, embedded in paraffin, sectioned at 5μm thickness, and stained with Hematoxylin and Eosin (H&E).
- Evaluation: Slides are examined under a light microscope by a pathologist blinded to the treatment groups. The Johnsen's biopsy score count or a similar scoring system can be used to semiquantitatively assess spermatogenesis. A minimum of 100 tubular cross-sections per animal are scored [28].
Biochemical Assays
- Oxidative Stress Markers:
- Lipid Peroxidation: Measured as malondialdehyde (MDA) content using the thiobarbituric acid reactive substances (TBARS) method.
- Antioxidant Enzymes: Superoxide dismutase (SOD) activity is assessed via spectrophotometric methods. Reduced glutathione (GSH) levels are determined using Ellman's reagent [28].
- Hormone Assays: Serum levels of luteinizing hormone (LH), follicle-stimulating hormone (FSH), and testosterone are quantified using commercial enzyme-linked immunosorbent assay (ELISA) kits.
Molecular Analyses
- RNA Extraction and Quantitative Real-Time PCR (qRT-PCR): Total RNA is isolated from frozen tissue using TRIzol reagent. cDNA is synthesized, and the expression levels of target genes (e.g., CYP11a1, HSD17B3, StAR) are quantified using SYBR Green chemistry, with normalization to housekeeping genes (e.g., Gapdh, Actb).
- Protein Extraction and Western Blotting: Proteins are extracted using RIPA buffer. Equal amounts of protein are separated by SDS-PAGE, transferred to PVDF membranes, and probed with specific primary antibodies against targets of interest (e.g., Nrf2, Keap1, HO-1, PPARγ, cleaved caspase-3). Protein bands are visualized using enhanced chemiluminescence and quantified by densitometry.
Signaling Pathways
The protective effects against EDC or toxicant-induced damage often involve the modulation of specific cytoprotective signaling pathways, notably the Nrf2/Keap1/HO-1 axis and PPARγ signaling.
Nrf2 and PPARγ Signaling Pathways: This diagram illustrates the cytoprotective Nrf2/Keap1/HO-1 pathway and the anti-inflammatory PPARγ pathway, which are often impaired by EDCs and can be targeted for therapeutic intervention.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating EDC-Induced Cellular Consequences
| Reagent / Assay | Primary Function in Research | Specific Application Example |
|---|---|---|
| Cisplatin (CDDP) | Chemotherapeutic agent; induces DNA damage, oxidative stress, and apoptosis. | Used in vivo and in vitro to model EDC-like damage, particularly in testicular and ovarian toxicity studies [28]. |
| Lisinopril (LSP) | Angiotensin-converting enzyme (ACE) inhibitor; investigational protective agent. | Used to investigate mitigation of oxidative stress, inflammation, and apoptosis via modulation of Nrf2/HO-1 and PPARγ pathways [28]. |
| ELISA Kits | Quantify protein concentrations (hormones, cytokines) in serum and tissue homogenates. | Measure testosterone, LH, FSH, and inflammatory cytokines like TNF-α and IL-6 [28]. |
| qRT-PCR Reagents | Quantify mRNA expression levels of target genes. | Assess expression of steroidogenic genes (StAR, CYP11a1, HSD17B3) and inflammatory markers [28]. |
| Western Blot Antibodies | Detect and quantify specific proteins and post-translational modifications. | Analyze protein levels of Nrf2, Keap1, HO-1, PPARγ, and cleaved caspase-3 [28]. |
| SOD & GSH Assay Kits | Spectrophotometric measurement of antioxidant enzyme activity. | Evaluate the status of the cellular antioxidant defense system in tissue samples [28]. |
| MDA (TBARS) Assay Kit | Measures lipid peroxidation as a marker of oxidative stress. | Quantify malondialdehyde levels to assess oxidative damage to cell membranes [28]. |
| Histopathology Stains (H&E) | Visualize tissue architecture and cellular morphology. | Score spermatogenesis and identify histopathological aberrations in gonadal tissues [28]. |
| Tobramycin A | Tobramycin A, MF:C12H25N3O7, MW:323.34 g/mol | Chemical Reagent |
| (E)-5-Decen-1-yne | (E)-5-Decen-1-yne|CAS 53963-07-8|C10H16 | (E)-5-Decen-1-yne (CAS 53963-07-8) is a high-purity, C10H16 alkenyne for pheromone and organic synthesis research. For Research Use Only. Not for human or veterinary use. |
The mechanistic link between EDC exposure and impaired fertility is robustly underpinned by the induction of oxidative stress, apoptosis, and dysregulation of steroidogenesis. Advanced experimental models continue to elucidate the complex signaling networks, such as Nrf2/Keap1/HO-1 and PPARγ, that are compromised by these chemicals. The quantitative data and detailed methodologies outlined herein provide a framework for researchers to further investigate these pathways, identify novel biomarkers, and develop targeted therapeutic strategies to mitigate the detrimental effects of EDCs on reproductive health.
This whitepaper synthesizes current scientific understanding of how epigenetic modifications facilitate transgenerational inheritance, with specific focus on implications for endocrine-disrupting chemical (EDC) research in fertility studies. Mounting evidence demonstrates that environmental exposures can induce epigenetic changes that persist across multiple generations, potentially contributing to the declining fertility rates observed globally. This technical review comprehensively examines molecular mechanisms, experimental methodologies, and key findings that establish the conceptual framework for transgenerational epigenetic inheritance, providing researchers and drug development professionals with critical insights for advancing this evolving field.
Epigenetics represents the study of mitotically and/or meiotically heritable changes in gene function that cannot be explained by changes in DNA sequence [33]. These mechanisms enable the transmission of environmental information across generations through non-genetic pathways, creating a potential biological substrate for the inheritance of acquired traits. The fundamental epigenetic mechanisms include DNA methylation, histone modifications, and regulation by non-coding RNAs, all of which alter chromatin structure and accessibility without changing the underlying DNA sequence [33] [34].
Within the context of endocrine disruption research, transgenerational epigenetic inheritance (TEI) has emerged as a critical area of investigation. TEI occurs when environmental factors induce epigenetic marks that persist beyond the generation directly exposed, potentially affecting the health and fertility of subsequent generations [35] [36]. For EDCs, this phenomenon raises significant concerns as exposure to these chemicals during sensitive developmental windows may program physiological responses that manifest as reproductive impairments in future generations [37] [38]. The growing body of evidence linking EDC exposure to transgenerational reproductive effects underscores the urgent need to understand the precise molecular mechanisms involved and their implications for human fertility and therapeutic development.
Molecular Mechanisms of Epigenetic Inheritance
DNA Methylation and Hydroxymethylation
DNA methylation, involving the addition of methyl groups to cytosine bases primarily at CpG sites, represents one of the most extensively characterized epigenetic modifications. This process is catalyzed by DNA methyltransferases (DNMTs) and typically results in transcriptional repression when occurring in promoter regions [33]. During germline reprogramming, most DNA methylation marks are erased, but some resistant loci escape this erasure, potentially enabling transgenerational inheritance [35] [36]. The conversion of 5-methylcytosine to 5-hydroxymethylcytosine by TET enzymes serves as an intermediate in DNA demethylation but may also function as an epigenetic mark with distinct regulatory functions [33].
Recent evidence suggests that EDCs can disrupt normal DNA methylation patterns in gametes and reproductive tissues. For instance, exposure to bisphenol A (BPA) has been shown to alter DNA methylation patterns in genes involved in hormonal signaling, potentially contributing to reproductive abnormalities that persist across generations [37] [39]. Similarly, phthalate exposure has been associated with differential methylation in genes regulating the hypothalamic-pituitary-gonadal (HPG) axis, providing a plausible mechanism for their transgenerational effects on fertility [30] [40].
Histone Modifications
Histone proteins undergo numerous post-translational modifications that influence chromatin architecture and gene expression. These include acetylation, methylation, phosphorylation, ubiquitination, and newer modifications such as lactylation [33]. Specific histone modifications establish chromatin states that either facilitate or repress transcription; for example, histone H3 lysine 9 trimethylation (H3K9me3) and H3 lysine 27 trimethylation (H3K27me3) are generally associated with transcriptional repression [35] [41].
The transmission of histone modifications across generations represents a more complex mechanism of epigenetic inheritance, as histones are largely replaced during gametogenesis. However, certain histone variants and their associated modifications can escape this reprogramming. Research has demonstrated that H3K4me3, H3K9me3, and H3K27me3 can be transmitted transgenerationally in various model organisms, potentially mediating the inheritance of EDC-induced phenotypic effects [41]. In Drosophila, stable Polycomb-dependent transgenerational inheritance of chromatin states has been documented, with H3K27me3 playing a central role in maintaining these epigenetic states across generations [41].
Non-Coding RNAs
Multiple classes of non-coding RNAs (ncRNAs), including small interfering RNAs (siRNAs), Piwi-interacting RNAs (piRNAs), and microRNAs (miRNAs), participate in epigenetic regulation and have been implicated in transgenerational inheritance [36] [34]. These RNA species can guide DNA methylation and histone modifications to specific genomic loci, establishing and maintaining epigenetic states across cell divisions and generations.
In the context of EDC exposure, studies have shown that sperm ncRNAs can carry information about parental environmental exposures to offspring. For example, in mouse models of early life stress, alterations in sperm miRNA profiles were associated with behavioral and metabolic changes in subsequent generations [35]. Similarly, exposure to EDCs such as vinclozolin has been shown to alter the expression of ncRNAs in sperm, potentially contributing to the transgenerational inheritance of reproductive abnormalities [41]. The RNA interference pathway has been demonstrated to be essential for TEI in several organisms, including C. elegans and plants [36].
Table 1: Primary Molecular Mechanisms of Transgenerational Epigenetic Inheritance
| Mechanism | Molecular Players | Function in TEI | Evidence Level |
|---|---|---|---|
| DNA Methylation | DNMT1, DNMT3A/B, TET enzymes, MBD proteins | Stable gene silencing; some marks escape reprogramming | Strong in plants and mammals |
| Histone Modifications | Histone methyltransferases, demethylases, acetyltransferases, deacetylases | Chromatin state memory; certain modifications resist erasure | Strong in fungi, plants, invertebrates; emerging in mammals |
| Non-Coding RNAs | siRNAs, piRNAs, miRNAs, ncRNAs | Guide chromatin modifications; direct epigenetic regulation | Strong in plants, C. elegans; emerging in mammals |
| Prion-like Proteins | Prion proteins, structural templating factors | Self-templating protein conformations | Limited to specific model systems |
Integrated Epigenetic Regulation
These epigenetic mechanisms do not function in isolation but rather form a complex, integrated regulatory network. Cross-talk between DNA methylation and histone modifications has been well-documented; for instance, DNA methylation can recruit proteins that promote specific histone modifications, and vice versa [33]. Additionally, ncRNAs can guide both DNA methylation and histone modifications to specific genomic loci, establishing self-reinforcing epigenetic loops that can persist across generations [36] [41].
Recent research has revealed that EDCs can disrupt this integrated epigenetic network, potentially leading to cascading effects on gene expression and phenotype. For example, studies have shown that exposure to a mixture of EDCs can simultaneously alter DNA methylation patterns, histone modification profiles, and ncRNA expression in reproductive tissues, resulting in transgenerational inheritance of reproductive abnormalities [41]. This integrated perspective is essential for understanding the full scope of EDC effects on epigenetic programming and inheritance.
Diagram 1: EDC-Induced Epigenetic Transgenerational Inheritance Pathways. This diagram illustrates the sequential processes through which endocrine-disrupting chemicals establish epigenetic marks that can be transmitted across generations, ultimately resulting in impaired fertility and other health consequences.
Endocrine-Disrupting Chemicals and Reproductive Health
EDC Exposure and Female Reproductive Health
The pervasive presence of EDCs in the environment raises significant concerns for reproductive health, particularly due to their potential to induce epigenetic changes that may persist across generations [30] [38]. Epidemiological studies have consistently demonstrated associations between EDC exposure and various female reproductive disorders, including diminished ovarian reserve, polycystic ovary syndrome (PCOS), endometriosis, and premature ovarian insufficiency [30] [38] [40]. These associations are supported by experimental evidence from animal models showing that developmental exposure to EDCs can reprogram the female reproductive system, leading to impaired fertility in adulthood and subsequent generations.
Specific EDCs have been particularly well-studied for their effects on female reproduction. Bisphenol A (BPA), a component of polycarbonate plastics and epoxy resins, has been shown to interfere with estrogen signaling and alter the development of the hypothalamic-pituitary-ovarian axis [30] [37]. Women with higher urinary BPA levels demonstrate decreased ovarian reserve, lower antral follicle counts, and increased incidence of PCOS and implantation failure [30]. Similarly, phthalates, used as plasticizers in numerous consumer products, have been associated with reduced serum inhibin B levels and advanced-stage endometriosis [30] [40]. These chemicals appear to exert their effects through multiple mechanisms, including epigenetic reprogramming of genes involved in hormonal signaling and folliculogenesis.
EDC Exposure and Male Reproductive Health
Male reproductive health has also been significantly impacted by EDC exposure, with compelling evidence linking prenatal and adult exposure to impaired spermatogenesis, reduced semen quality, and altered testosterone production [39] [40]. The increasing incidence of these abnormalities over recent decades correlates with the rise in production and environmental dissemination of industrial chemicals, suggesting a potential causal relationship [37] [40].
Numerous studies have documented the specific effects of various EDCs on male reproduction. Phthalates have been associated with reduced sperm count and motility, while BPA exposure has been linked to decreased sperm quality and DNA damage [40]. Persistent organic pollutants, including dioxins and organochlorine pesticides, have also been implicated in male reproductive impairments, potentially through epigenetic mechanisms that become apparent across generations [37] [40]. These findings are particularly concerning given the transgenerational nature of some EDC effects, with exposure in one generation potentially affecting the reproductive health of subsequent, unexposed generations.
Table 2: Endocrine-Disrupting Chemicals and Documented Reproductive Effects
| EDC Class | Common Sources | Documented Reproductive Effects | Epigenetic Mechanisms Implicated |
|---|---|---|---|
| Bisphenols (BPA, BPS, BPF) | Plastics, food containers, receipts | Reduced ovarian reserve, PCOS, impaired spermatogenesis, implantation failure | DNA methylation changes in hormone response genes, histone modifications in reproductive tissues |
| Phthalates (DEHP, DBP, BBP) | Plastics, personal care products, medical devices | Endometriosis, reduced sperm quality, altered ovarian function, hormonal imbalances | Altered DNA methylation in HPG axis genes, ncRNA expression changes |
| Perfluorinated Compounds (PFAS) | Non-stick coatings, stain-resistant fabrics | Reduced fertility, menstrual irregularities, preeclampsia, testicular cancer | DNA methylation changes in imprinted genes, histone modifications |
| Persistent Organic Pollutants (PCBs, DDT) | Pesticides, industrial processes | Early puberty, reduced semen quality, ovarian dysfunction, endometriosis | Global hypomethylation, transgenerational epigenetic inheritance |
| Parabens | Cosmetics, pharmaceuticals, food preservatives | Reduced testosterone, sperm DNA damage, altered ovarian steroidogenesis | DNA methylation changes in steroidogenic genes |
Experimental Models and Methodological Approaches
Animal Models of Transgenerational Inheritance
Animal models have been instrumental in establishing causal relationships between EDC exposure and transgenerational epigenetic inheritance of reproductive phenotypes. Studies in rodents have provided particularly compelling evidence, with exposure to EDCs such as vinclozolin, methoxychlor, and plastic mixtures resulting in reproductive abnormalities that persist across multiple generations [36] [41]. These models allow for precise control of exposure timing, dose, and duration, enabling researchers to identify critical windows of susceptibility and dose-response relationships.
The standard experimental design for transgenerational inheritance studies involves exposing gestating females (F0 generation) to the EDC of interest during the period of gonadal sex determination in the fetus (F1 generation). The germ cells that will give rise to the F2 generation are also directly exposed during this critical developmental window. True transgenerational effects are observed in the F3 generation and beyond, which were never directly exposed to the EDC [35] [34]. This rigorous experimental approach helps distinguish between direct exposure effects and truly heritable epigenetic changes.
Other model organisms, including C. elegans, Drosophila, and zebrafish, have also contributed significantly to our understanding of TEI. These models offer advantages such as short generation times, genetic tractability, and well-characterized development, facilitating detailed mechanistic studies. Research in C. elegans has been particularly informative regarding the role of small RNAs in TEI, demonstrating that RNAi pathways can transmit environmental information across multiple generations [36] [41].
Epigenomic Profiling Techniques
Advanced molecular techniques have enabled comprehensive mapping of epigenetic modifications across the genome in response to EDC exposure. Whole-genome bisulfite sequencing allows for base-resolution mapping of DNA methylation patterns, while ChIP-seq facilitates genome-wide profiling of histone modifications and transcription factor binding sites [41]. Additionally, RNA-seq provides a comprehensive view of transcriptome changes, including altered expression of ncRNAs.
These techniques have revealed that EDC exposure can induce widespread changes in the epigenome, with specific patterns associated with particular reproductive phenotypes. For example, studies in animal models exposed to vinclozolin have identified specific genomic regions with altered DNA methylation patterns that are transmitted across generations and associated with reproductive abnormalities [41]. Similarly, research on BPA exposure has revealed effects on histone modification patterns at genes involved in hormonal signaling and reproductive development [37] [39].
Diagram 2: Transgenerational Experimental Design. This workflow illustrates the standard approach for studying transgenerational epigenetic inheritance, where true transgenerational effects are observed in the F3 generation (and beyond) that was never directly exposed to the environmental stressor.
Research Reagent Solutions and Methodological Toolkit
Table 3: Essential Research Reagents for Epigenetic Inheritance Studies
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| DNA Methylation Analysis Kits | Whole-genome bisulfite sequencing kits, Methylated DNA immunoprecipitation (MeDIP) kits, Pyrosequencing assays | Comprehensive mapping of 5mC and 5hmC patterns, quantitative analysis of specific loci | Bisulfite conversion efficiency critical; antibody specificity important for enrichment-based methods |
| Histone Modification Reagents | Histone modification-specific antibodies, ChIP-seq kits, Histone extraction kits | Genome-wide mapping of histone marks, assessment of histone modification levels | Antibody validation essential; chromatin shearing optimization required |
| Non-Coding RNA Analysis | Small RNA sequencing kits, miRNA inhibitors/mimics, piRNA cloning kits | Profiling of small RNA populations, functional validation of ncRNA roles | RNA stability challenges; specific isolation methods for different ncRNA classes |
| Epigenetic Editing Tools | CRISPR-dCas9 systems, DNMT/ TET fusions, histone modifier fusions | Targeted epigenetic manipulation, causal validation of epigenetic marks | Efficiency of targeted recruitment; stability of induced epigenetic states |
| Animal Models | Rodent EDC exposure models, C. elegans, Drosophila | Transgenerational inheritance studies, mechanistic investigations | Species-specific reprogramming events; generational time considerations |
| 1,2,5-Triphenylpyrrole | 1,2,5-Triphenylpyrrole, CAS:851-33-2, MF:C22H17N, MW:295.4 g/mol | Chemical Reagent | Bench Chemicals |
| Sydnone, 3-cyclohexyl- | Sydnone, 3-cyclohexyl-, CAS:20600-69-5, MF:C8H12N2O2, MW:168.19 g/mol | Chemical Reagent | Bench Chemicals |
The accumulating evidence unequivocally demonstrates that epigenetic modifications can be transmitted across generations, with significant implications for understanding the impact of EDCs on fertility. The molecular mechanisms underlying this transgenerational inheritance involve complex interactions between DNA methylation, histone modifications, and non-coding RNAs, which together establish stable epigenetic states that can escape germline reprogramming. EDCs, by interfering with hormonal signaling during critical developmental windows, can disrupt these epigenetic processes, leading to reproductive abnormalities that persist in subsequent generations.
Future research in this field should focus on several key areas. First, there is a need to better understand the windows of maximum susceptibility to EDC-induced epigenetic changes and the specific signaling pathways involved. Second, research should aim to identify epigenetic biomarkers of EDC exposure and transgenerational effects that could be used in risk assessment and clinical practice. Third, studies exploring the potential for dietary or pharmacological interventions to prevent or reverse EDC-induced epigenetic changes could have significant clinical implications. Finally, continued methodological advancements in epigenomic profiling and editing will be essential for unraveling the complexity of TEI and developing effective strategies to mitigate the transgenerational impacts of EDCs on human fertility.
From Bench to Biomarkers: Research Methodologies and Epidemiological Evidence
The systematic investigation of endocrine-disrupting chemicals (EDCs) and their impact on human fertility represents a critical challenge in modern public health and toxicology. EDCs are natural or human-made chemicals that can mimic, block, or interfere with the body's hormones, which are part of the endocrine system [1]. These chemicals are linked with many health problems in both wildlife and people, with particular concern for reproductive health [1]. Research indicates that exposure to EDCs may be linked to declining fertility rates and increasing reproductive disorders observed over recent decades [38]. The complexity of these chemicals' effects on the human reproductive system necessitates robust analytical frameworks for evaluating human observational studies (HOS), which provide essential evidence for quantitative risk assessment (QRA).
Human observational studies, including cohort and case-control designs, are crucial for understanding the relationship between EDC exposure and fertility outcomes in real-world settings. However, these studies vary considerably in quality, particularly in their approaches to exposure assessment, confounding control, and outcome measurement. The Navigation Guide methodology, developed specifically for evaluating environmental health evidence, provides a structured, transparent framework for assessing this evidence base [42]. This framework is particularly valuable for reconciling findings from epidemiological studies, in vitro experiments, and animal models to draw conclusions about EDCs and reproductive health.
The need for standardized evaluation is underscored by trends in reproductive health. Between 1950 and 2000, the incidence of several conditions deleteriously affecting male sexual organs increased annually, with epidemiological studies showing rising rates of prostate and testicular cancer, maldescended testes, anatomical malformations of the male genitalia, and declining sperm quality [43]. Similarly, female reproductive disorders have shown concerning increases, with EDCs implicated in conditions including abnormal puberty, impaired fertility, premature menopause, and polycystic ovarian syndrome [38]. This technical guide outlines comprehensive analytical frameworks for navigating human observational studies on EDCs and fertility using the Navigation Guide approach, providing researchers with standardized methodologies for evidence evaluation.
The Navigation Guide Framework: Principles and Methodology
Historical Development and Core Principles
The Navigation Guide framework emerged from the recognized need to standardize the evaluation of evidence linking environmental exposures to health outcomes. Originally developed through systematic review methodologies, it provides a structured protocol for integrating and assessing human and non-human evidence to support decision-making in environmental health [42]. The framework was specifically designed to address challenges unique to environmental toxicants, where randomized controlled trials are often ethically impossible and researchers must rely on observational evidence, animal studies, and mechanistic data.
The methodology is built upon three core principles: systematic and transparent processes, explicit and rigorous methodology, and separation of science from policy [42]. These principles ensure that evidence assessment remains objective, reproducible, and minimally susceptible to bias. The systematic approach is particularly valuable for EDC and fertility research, where studies may exhibit heterogeneity in design, exposure measurement, and outcome assessment. By applying consistent criteria across the evidence base, the Navigation Guide facilitates more reliable conclusions about potential reproductive hazards.
Systematic Implementation Workflow
The Navigation Guide follows a staged approach to evidence integration, progressing from problem formulation through evidence identification, evaluation, integration, and conclusion. The initial problem formulation phase requires precisely defining the population, exposure, comparator, and outcomes (PECO statement), which creates a structured foundation for the evidence review. For EDC and fertility research, this typically involves specifying the chemical class (e.g., bisphenol A, phthalates), exposure windows (e.g., prenatal, adult), and specific reproductive endpoints (e.g., sperm quality, time to pregnancy, ovarian reserve).
The evidence identification phase employs systematic search strategies across multiple databases to capture all relevant human, animal, and mechanistic studies. Subsequent evaluation involves quality assessment of individual studies using domain-based tools, followed by rating the overall strength of evidence for each stream (human, animal, mechanistic) considering factors such as risk of bias, consistency, directness, and precision [42]. The final integration phase synthesizes findings across evidence streams to develop hazard conclusions, which then inform evidence-based recommendations.
Table 1: Navigation Guide Implementation Stages for EDC and Fertility Research
| Stage | Key Activities | EDC-Fertility Application Examples |
|---|---|---|
| Problem Formulation | Develop PECO statement, establish protocol | Population: Reproductive-age humans; Exposure: EDCs like BPA, phthalates; Comparator: Unexposed/low-exposed; Outcome: Fertility metrics |
| Evidence Identification | Systematic literature search, screening, data extraction | Search multiple databases (PubMed, Scopus, Web of Science) using controlled vocabulary and keywords for EDCs and reproductive outcomes |
| Evidence Evaluation | Quality assessment of individual studies, rating body of evidence | Apply tailored tools for human observational studies; evaluate risk of bias, consistency, precision across studies |
| Evidence Integration | Synthesize human, animal, mechanistic evidence | Weight evidence streams to determine level of evidence for EDC-fertility relationship |
| Conclusion | Develop hazard identification, evidence-based recommendations | Translate scientific findings into public health or clinical recommendations |
Evaluating Human Observational Studies for EDC and Fertility Research
Quality Assessment Framework for HOS
The evaluation of human observational studies for quantitative risk assessment requires a structured approach to determine their suitability for informing decisions about EDCs and fertility. A specialized three-tiered framework consisting of 20 evaluation criteria has been developed specifically for this purpose [42]. This framework places particular emphasis on the quality of quantitative exposure assessment, which is a crucial aspect of HOS to be considered for QRA, especially given the challenges in accurately characterizing EDC exposures which often occur at low levels through multiple routes.
The assessment framework evaluates studies across several domains: study design and participant selection, exposure assessment methods, outcome measurement, statistical approaches, and reporting completeness. For each domain, specific criteria determine whether studies provide sufficient methodological detail and appropriate design to support reliable conclusions. Application of this framework to studies on the relation between exposure to benzene and acute myeloid leukemia (AML) demonstrated its utility, with five of seven evaluated studies deemed suitable for QRA and ranked based on quality [42]. This suggests similar application is feasible for EDC-fertility research.
Critical Evaluation Criteria for EDC-Fertility Studies
When applying the evaluation framework to EDC and fertility research, several criteria warrant particular attention. For exposure assessment, studies should ideally incorporate biomonitoring data rather than relying solely on environmental measurements or self-report, given the multi-route exposure pathways for many EDCs. The timing of exposure assessment is also critical, as susceptibility to EDCs varies across the life course, with prenatal and early-life periods being particularly vulnerable windows for reproductive system development [38] [43].
For outcome measurement, studies should employ clinically validated endpoints rather than surrogate measures whenever possible. In male fertility research, this includes direct semen analysis parameters (count, motility, morphology) rather than relying solely on fertility rates, while female fertility studies benefit from direct measures of ovarian reserve (antral follicle count, anti-Müllerian hormone) in addition to time-to-pregnancy metrics. Confounding control is another essential domain, with studies expected to account for key potential confounders such as age, body mass index, smoking, sexual activity, and other co-exposures that might correlate with both EDC exposure and fertility outcomes.
Table 2: Quality Assessment Criteria for EDC-Fertility Observational Studies
| Assessment Domain | Key Quality Indicators | Common Methodological Limitations |
|---|---|---|
| Exposure Assessment | Biomarker measurement, timing relative to critical windows, multiple sampling to account to variability | Reliance on single spot samples, poor temporal alignment with susceptible windows, use of indirect exposure proxies |
| Outcome Measurement | Clinical endpoints, validated measures, blinded assessment | Self-reported outcomes, use of surrogate endpoints without validation, potential for diagnostic bias |
| Confounding Control | Measurement and adjustment for key confounders, consideration of co-exposures | Incomplete adjustment, residual confounding, failure to account for mixed chemical exposures |
| Statistical Approach | Appropriate model selection, handling of missing data, assessment of nonlinear relationships | Overadjustment, multiple testing without correction, inadequate handling of censored data in time-to-pregnancy studies |
| Reporting | Complete reporting of methods, results, and limitations | Selective reporting, insufficient detail on analytical methods, unclear eligibility criteria |
EDC Mechanisms and Reproductive Impacts
Molecular Mechanisms of Endocrine Disruption
EDCs interfere with hormonal action through diverse molecular mechanisms, contributing to their adverse effects on reproductive health. Unlike endogenous hormones that exhibit specific receptor binding, EDCs often have multiple hormonal activities and targets. For example, bisphenol A (BPA), which has estrogenic activity, is also a thyroid hormone antagonist and has been shown to bind prostatic androgen receptors in men with castration-resistant prostate tumors [43]. This promiscuous receptor interaction complicates straightforward dose-response relationships and contributes to non-monotonic response curves where effects at low doses differ from those at high doses.
The primary mechanisms of endocrine disruption include nuclear receptor binding (estrogen, androgen, thyroid, peroxisome proliferator-activated receptors), interference with hormone synthesis and metabolism enzymes, and disruption of transport proteins [43]. EDCs can also affect hormone receptor expression; for instance, perinatal exposure to BPA showed dysregulation of steroid receptors and co-regulators in rat testes, with some effects persisting across generations [43]. Additionally, EDCs can operate through non-genomic signaling pathways by binding to membrane receptors and rapidly activating intracellular signaling cascades that influence cellular function.
Epigenetic and Transgenerational Effects
Beyond direct receptor interactions, EDCs can alter the epigenetic landscape of reproductive tissues, potentially leading to heritable changes that affect fertility across generations. Exposure to BPA, cadmium, vinclozolin, and diethylhexyl phthalate (DEHP) has been shown to alter DNA methylation patterns in both prostate and testicular cells [43]. Histone modification patterns can also be affected, as demonstrated in testes exposed to vinclozolin and dibutyl-phthalate (DBP) [43]. These epigenetic changes provide a plausible mechanism for how transient EDC exposures during critical developmental windows can cause persistent reproductive effects manifesting in adulthood.
The impact of EDCs on non-coding RNAs represents another epigenetic mechanism influencing reproductive development. MicroRNAs (miRNAs) are involved in proper differentiation of primordial germ cells and have been shown to be dysregulated in testicular germ cell tumors [43]. Alterations in miRNA expression have been observed in mouse Sertoli cells exposed to nonyl-phenol, and other EDCs like BPA and DDT have been linked to altered miRNA expression in estrogen-responsive human breast cancer cells and placental cell lines [43]. These findings underscore the complexity of EDC mechanisms and the potential for long-lasting effects on fertility from developmental exposures.
Diagram 1: EDC Mechanisms Impacting Fertility. This diagram illustrates the molecular, cellular, and organ-level pathways through which endocrine-disrupting chemicals impair reproductive function.
Experimental Protocols for EDC Fertility Research
Human Observational Study Designs
Research investigating the relationship between EDCs and human fertility employs several observational designs, each with distinct methodological considerations. Cohort studies follow participants over time, assessing EDC exposures and subsequent fertility outcomes. These designs are particularly valuable for establishing temporal relationships between exposure and effect. The "Cohort study among workers exposed to benzene in China" exemplifies this approach, with its detailed exposure assessment methodology providing a model for EDC research [42]. For fertility outcomes, cohort designs can incorporate time-to-pregnancy analyses, which provide sensitive measures of fecundity.
Case-control studies offer efficiency for investigating rare fertility outcomes such as specific reproductive disorders. These designs identify cases (e.g., individuals with infertility, endometriosis, or poor semen quality) and controls, then compare historical EDC exposures. The case-control methodology applied in studies on benzene and acute myeloid leukemia demonstrates how this approach can be adapted for EDC-fertility research [42]. Cross-sectional designs provide snapshot assessments of EDC exposure and fertility status simultaneously, though they are limited in establishing temporality.
Exposure Assessment Methodologies
Accurate exposure assessment presents significant challenges in EDC research due to the complex pharmacokinetics, non-persistent nature of many compounds, and multiple exposure routes. Optimal protocols incorporate biomonitoring using biological matrices (urine, blood, serum) that capture integrated exposure from all routes. For non-persistent EDCs like bisphenol A and phthalates, protocols should account for short half-lives through repeated sampling or pooled samples to characterize typical exposure [44]. Timing of sample collection should align with critical windows of susceptibility for reproductive development, which often necessitates prenatal or early-life sampling for outcomes manifesting in adulthood.
Analytical chemistry methods for EDC quantification must demonstrate sufficient sensitivity to detect environmentally relevant concentrations, with quality control procedures including blanks, spikes, and duplicate samples. For chemicals with multiple metabolites (e.g., phthalates), measuring the specific metabolites rather than parent compounds improves accuracy. Some studies incorporate silicone wristbands or other passive samplers to complement biomonitoring data and identify exposure sources. The "Field comparison of inhalable aerosol samplers applied in the European rubber manufacturing industry" illustrates methodological considerations for environmental sampling that can inform EDC exposure assessment strategies [42].
Outcome Assessment Protocols
Fertility outcome measurement requires careful protocol specification to ensure validity and comparability across studies. For male fertility, standard semen analysis parameters (concentration, motility, morphology) should follow World Health Organization guidelines with quality-controlled laboratory procedures. Additional advanced measures include sperm DNA fragmentation, nuclear integrity, or aneuploidy assessment. Clinical endpoints such as infertility diagnosis or time to pregnancy provide complementary measures.
Female fertility assessment incorporates multiple potential endpoints, including ovarian reserve biomarkers (anti-Müllerian hormone, antral follicle count), ovulatory function, clinical disorders (endometriosis, polycystic ovary syndrome), and fertility outcomes (fecundability, infertility). The review "Endocrine-disrupting chemicals and female reproductive health: a growing concern" outlines how EDCs affect the ovarian reserve during early development and its maintenance during adulthood [38]. Study protocols should specify standardized procedures for specimen collection, processing, and analysis, with blinding to exposure status to prevent assessment bias.
Diagram 2: Observational Study Design for EDC-Fertility Research. This workflow outlines methodological approaches for investigating EDC effects on human reproduction.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for EDC Fertility Studies
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Chemical Standards | Bisphenol A, Di(2-ethylhexyl) phthalate (DEHP), Mono(2-ethylhexyl) phthalate (MEHP), Polychlorinated biphenyls (PCBs) | Analytical method development, quality control, dose-response studies, mechanistic investigations |
| Immunoassay Kits | Anti-Müllerian hormone ELISA, Estradiol RIA, Testosterone ELISA, Thyroid hormone panels | Endocrine profiling, reproductive status assessment, HPG axis function evaluation |
| Cell Culture Models | MCF-7 breast cancer cells, TM3 Leydig cells, GC-1 spermatogonial cells, Human granulosa cell lines | In vitro screening, mechanistic studies, receptor activation assays, high-throughput toxicity testing |
| Molecular Biology Reagents | ERα/ERβ antibodies, AR antibodies, DNA methylation kits, miRNA profiling arrays, qPCR primers for steroidogenic genes | Mechanistic investigation of endocrine pathways, epigenetic alterations, gene expression changes |
| Animal Models | Sprague-Dawley rats, CD-1 mice, Zebrafish reproductive assays | In vivo toxicity testing, developmental origins studies, transgenerational effects investigation |
| 2-Nitro-4-phenylazophenol | 2-Nitro-4-phenylazophenol|CAS 55936-40-8|Supplier | High-purity 2-Nitro-4-phenylazophenol (CAS 55936-40-8) for research applications. This phenylazophenol compound is For Research Use Only. Not for human or veterinary use. |
| Bromobis(methylthio)borane | Bromobis(methylthio)borane|29877-98-3 | Bromobis(methylthio)borane (CAS 29877-98-3) is for research use only. Not for human or veterinary use. Explore its applications in organic synthesis. |
Data Analysis and Visualization in EDC Fertility Research
Statistical Approaches for EDC-Fertility Data
The analysis of EDC and fertility data presents specific statistical challenges due to the complex exposure patterns, correlated outcomes, and often-censored fertility data. For continuous outcomes such as hormone levels or semen parameters, multiple linear regression forms the foundation, with appropriate transformation of exposure metrics to account for frequently observed non-linear relationships. Time-to-event analyses (Cox proportional hazards) are preferred for time-to-pregnancy data, which accounts for couples who have not conceived by study end (right-censoring). For correlated data within couples or longitudinal measures, mixed-effects models appropriately account for within-subject correlation.
Multiple chemical exposures present analytical challenges, as humans are exposed to EDC mixtures rather than single compounds. Statistical approaches for mixtures include weighted quantile sum regression, Bayesian kernel machine regression, and principal component analysis, which help identify important mixture components and potential interactions. Additionally, measurement error from using single spot samples for non-persistent chemicals requires consideration, with methods like regression calibration or simulation-extraction to address resulting bias. Model selection should be guided by subject matter knowledge rather than purely statistical criteria, with careful attention to confounding control and potential mediation pathways.
Data Visualization Strategies
Effective data visualization enhances interpretation and communication of complex EDC-fertility relationships. For exposure distributions, which often exhibit right-skewing, kernel density plots or histograms with log-transformed axes appropriately display the data pattern. Box plots effectively compare fertility outcomes across exposure quartiles, showing median, interquartile range, and potential outliers simultaneously [45]. Scatter plots with smoothing splines illustrate exposure-response relationships, particularly valuable for displaying non-monotonic patterns often observed with EDCs.
For multivariate relationships, directed acyclic graphs (DAGs) visually represent hypothesized causal structures, clarifying confounding and mediation assumptions. Effect modification can be displayed through stratified analyses or interaction plots. In systematic reviews, evidence tables summarize study characteristics and quality ratings, while forest plots display effect estimates and confidence intervals across studies, facilitating visual assessment of heterogeneity [45]. Timeline figures help communicate critical exposure windows relative to reproductive development stages.
The application of structured analytical frameworks like the Navigation Guide to human observational studies on EDCs and fertility provides a rigorous methodology for evidence-based decision-making. The three-tiered evaluation framework for HOS, with its emphasis on exposure assessment quality, enables transparent identification of studies suitable for quantitative risk assessment [42]. As research in this field advances, several areas warrant continued methodological development.
Future directions include improved exposure assessment strategies that capture the complex mixture nature of real-world EDC exposures and their variable timing relative to critical windows of reproductive susceptibility. Statistical methods that better account for exposure measurement error and complex mixture effects will enhance inference from observational data. Integration of mechanistic data from in vitro and animal models with human evidence will strengthen causal inference, particularly through systematic application of key characteristics of endocrine disruptors. Finally, translation of research findings into evidence-based public health recommendations and chemical policy decisions remains the ultimate application of these analytical frameworks for protecting reproductive health across generations.
Human biomonitoring (HBM) serves as a critical tool in environmental health research, defined as the analytical measurement of biomarkers in specified units of tissues or body products, which indicate an exposure, susceptibility, or potential health outcome [46]. For endocrine disrupting chemicals (EDCs)—compounds that interfere with the hormonal system and produce adverse effects in humans—biomonitoring provides essential data linking environmental exposures to health endpoints [47]. The measurement of EDCs and their metabolites in biological matrices has become increasingly important in understanding the impact on human fertility, with growing evidence suggesting that EDCs contribute to declining reproductive health worldwide [47] [48]. Large-scale population studies such as the National Health and Nutrition Examination Survey (NHANES) in the United States and similar cohorts in Europe have been instrumental in documenting the widespread exposure to EDCs across general populations and investigating the correlation between internal chemical doses and reproductive outcomes [46] [49].
The application of biomonitoring data to fertility research allows scientists to move beyond external exposure estimates to direct measurements of internal dose, thereby reducing uncertainty in exposure assessment and enhancing our understanding of the biological mechanisms through which EDCs impair reproductive function [50] [46]. This technical guide explores the methodologies, findings, and applications of population-based biomonitoring studies with a specific focus on their implications for EDC-related fertility research.
Major Population Cohorts and Study Designs
Key Biomonitoring Programs and Their Focus
Several major population cohorts have generated significant biomonitoring data on EDCs. These studies employ rigorous sampling methodologies to provide representative data on chemical exposure profiles across different demographic groups.
Table 1: Major Population Biomonitoring Cohorts and Their Characteristics
| Cohort Name | Region | Sample Size | Key EDCs Measured | Fertility-Related Assessments |
|---|---|---|---|---|
| NHANES | USA | ~5,000 annually | Phthalates, BPA, parabens, pesticides | Self-reported fertility, reproductive aging markers |
| HBM4EU | Europe | Varied by country | Phthalates, BPA, PFAS, pesticide metabolites | Hormone levels, clinical biomarkers |
| Danish Cohorts | Denmark | >3,600 across cohorts | Phthalates, BPA, triclosan, parabens | Semen quality, female reproductive health |
| REED Study | USA | 600 (planned) | BPA, phthalates, parabens, oxybenzone | EDC exposure reduction intervention outcomes |
The NHANES program, conducted by the Centers for Disease Control and Prevention (CDC), employs a stratified, multistage, probability-cluster sampling design to represent the non-institutionalized U.S. population [51] [49]. Data collection includes in-home interviews, physical examinations, and biological sample collection in mobile examination centers. The comprehensive nature of NHANES allows for correlation of biomonitoring data with a wide range of health parameters, including those relevant to reproductive health [49].
The European HBM4EU initiative (Human Biomonitoring for Europe) aimed to harmonize biomonitoring practices across Europe and develop informative effect biomarkers for application in large-scale studies [50]. This program specifically focused on linking exposure data with early biological effects through the implementation of a panel of validated effect biomarkers, including oxidative stress markers, reproductive and thyroid hormones, and novel epigenetic markers such as DNA methylation status of genes relevant to neurological and reproductive health [50].
Study Design Considerations for Fertility Research
When designing biomonitoring studies focused on fertility outcomes, several methodological considerations are paramount. Temporal aspects of exposure assessment are particularly critical for EDCs due to their short half-lives and the potential for windows of susceptibility during reproductive development [47]. The Danish cohort studies addressed this challenge by collecting serial samples across different population groups, including children, adolescents, young men, and pregnant women, recognizing that the timing of exposure measurement significantly impacts the ability to detect associations with health outcomes [52].
The REED (Reducing Exposures to Endocrine Disruptors) study employs a randomized controlled trial design to test the efficacy of an EDC reduction intervention, incorporating pre- and post-intervention biomonitoring to quantify exposure changes [53]. This design allows for direct assessment of whether exposure reduction leads to improvement in clinical biomarkers relevant to reproductive health. The study specifically targets reproductive-aged men and women (18-44 years), recognizing the particular importance of EDC exposure during the reproductive years [53].
Analytical Methodologies and Protocols
Sample Collection and Storage Protocols
Standardized protocols for biological sample collection, processing, and storage are essential for generating reliable and comparable biomonitoring data. Major studies typically collect urine samples as the primary matrix for measuring non-persistent EDCs due to the non-invasive collection procedure and relatively high concentrations of EDC metabolites.
The NHANES protocol involves spot urine collection during the mobile examination center visit, with samples immediately frozen at -20°C and shipped to the CDC's National Center for Environmental Health for analysis [49]. Similar protocols are followed in European studies, with additional considerations for sample stability during transport between participating countries in the HBM4EU program [50].
Analytical Techniques for EDC Measurement
Advanced analytical methods are required to measure the low concentrations of EDCs and their metabolites present in biological samples from general populations. Isotope-dilution high-performance liquid chromatography tandem mass spectrometry (LC-MS/MS) has emerged as the gold standard for quantifying phthalate metabolites, bisphenols, parabens, and other phenolic EDCs in urine [52] [49].
Table 2: Analytical Methods for Key EDC Classes in Biomonitoring Studies
| EDC Class | Specific Analytics | Matrix | Analytical Method | LOD Range |
|---|---|---|---|---|
| Phthalates | MEP, MBP, MBzP, MEHP, MEHHP, MEOHP | Urine | HPLC-MS/MS | 0.2-1.0 ng/mL |
| Bisphenols | BPA, BPS, BPF | Urine | HPLC-MS/MS | 0.1-0.4 ng/mL |
| Parabens | Methyl-, ethyl-, propyl-, butyl-paraben | Urine | HPLC-MS/MS | 0.1-0.5 ng/mL |
| Organophosphate esters | TBP metabolites | Urine | HPLC-MS/MS | Variable by metabolite |
For phthalates, which are ubiquitous in the environment and susceptible to contamination during sample collection and analysis, measurement of hydrolytic monoester metabolites and oxidative metabolites is preferred over measuring the parent diester compounds [46] [49]. This approach both avoids contamination issues and provides data on the toxicologically relevant forms of these chemicals [46].
The HBM4EU program advanced method harmonization across laboratories by implementing quality assurance programs and developing standardized operating procedures for sample preparation, instrumental analysis, and data processing [50]. This harmonization enables valid comparison of data across different studies and populations, enhancing the utility of biomonitoring data for regulatory decision-making.
Key Quantitative Findings on EDC Exposure
Population Exposure Levels
Biomonitoring studies have consistently demonstrated widespread exposure to multiple EDCs across general populations. NHANES data from 1999-2002 revealed detectable levels of phthalate metabolites in more than 75% of the U.S. population, with specific patterns of exposure varying by age, gender, and race/ethnicity [49]. More recent data indicate that more than 90% of U.S. adults have detectable levels of BPA and phthalates in their urine [53].
Similar findings have been reported in European populations. Danish cohort studies that analyzed urine samples from more than 3600 individuals found that nearly all participants were exposed to the six most common phthalates, BPA, triclosan, benzophenone-3, and at least two parabens [52]. The study also observed decreasing excretion of two common phthalates (DnBP and DEHP) over time, suggesting that regulatory actions to reduce these specific phthalates may be having a positive effect [52].
Exposure-Response Relationships in Fertility
Biomonitoring data have enabled researchers to investigate quantitative relationships between EDC exposure levels and fertility-related endpoints. A cross-sectional analysis of NHANES data revealed significant associations between urinary phthalate metabolite concentrations and obesity indicators, with notable differences by age and gender subgroups [49]. For example, in males aged 20-59, BMI and waist circumference increased across quartiles of MBzP, with similar positive associations observed for MEOHP, MEHHP, MEP, and MBP [49].
The HBM4EU Aligned Studies incorporated effect biomarkers to investigate early biological effects of EDC exposures, including oxidative stress biomarkers and reproductive hormones [50]. One study within this initiative demonstrated the mediating role of brain-derived neurotrophic factor (BDNF) status in the longitudinal association between infant BPA exposure and adolescent behavioral outcomes, illustrating how biomonitoring data can elucidate mechanistic pathways [50].
Figure 1: Mechanistic Pathways Linking EDC Exposure to Female Reproductive Pathology
Biomarkers of Effect and Susceptibility
Traditional and Novel Effect Biomarkers
The integration of effect biomarkers in biomonitoring studies represents a significant advancement in understanding the health implications of EDC exposures. Effect biomarkers provide mechanistically-based information on early biological changes preceding clinical disease, offering insights into the pathways through which EDCs impact reproductive health [50].
The HBM4EU program implemented a panel of effect biomarkers in aligned studies, including traditional oxidative stress biomarkers and reproductive hormones, as well as novel biomarkers such as DNA methylation status of BDNF and kisspeptin (KISS) genes as molecular markers of neurological and reproductive health, respectively [50]. These biomarkers have demonstrated utility in detecting early biological effects of chemical exposures and identifying population subgroups at higher risk [50].
Epigenetic Biomarkers
Epigenetic modifications represent a promising class of biomarkers for understanding how EDC exposures influence fertility outcomes. EDCs can affect the epigenome, causing modifications in gene expression of ovulation regulators without altering their DNA sequence [47] [48]. These epigenetic changes may explain how early-life EDC exposures can predispose individuals to reproductive disorders later in life, consistent with the Developmental Origins of Health and Disease (DOHaD) concept [47].
The REED study incorporates assessment of epigenetic markers to evaluate whether exposure reduction interventions can modify these biological signatures [53]. This approach recognizes that epigenetic changes may serve as more stable indicators of long-term exposure effects than chemical metabolite measurements alone, which reflect only recent exposures due to the short half-lives of most EDCs.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for EDC Biomonitoring Studies
| Reagent/Material | Application | Function | Example Usage |
|---|---|---|---|
| Isotope-labeled internal standards | Analytical chemistry | Quantification correction | HPLC-MS/MS analysis of phthalate metabolites |
| Solid-phase extraction cartridges | Sample preparation | Analyte enrichment and cleanup | Urine sample preparation prior to LC-MS/MS |
| Glucuronidase/sulfatase enzymes | Sample hydrolysis | Deconjugation of phase II metabolites | Freeing glucuronidated EDC metabolites for measurement |
| Quality control materials | Quality assurance | Method validation | Pooled urine samples with known analyte concentrations |
| DNA methylation kits | Epigenetic analysis | Assessment of epigenetic modifications | Measuring DNA methylation status of BDNF or KISS genes |
| ELISA kits | Effect biomarker measurement | Quantifying protein biomarkers | Measuring oxidative stress markers (8-oxo-dG, MDA) |
| Stable isotope-dilution reagents | Analytical chemistry | Improved quantification accuracy | HPLC-MS/MS analysis with reduced matrix effects |
| 1-(Bromoethynyl)cyclohexene | 1-(Bromoethynyl)cyclohexene, CAS:21983-34-6, MF:C8H9Br, MW:185.06 g/mol | Chemical Reagent | Bench Chemicals |
| 2'',3''-Dihydroochnaflavone | 2'',3''-Dihydroochnaflavone | Bench Chemicals |
Research Workflow and Data Integration
Figure 2: Comprehensive Workflow for EDC-Fertility Biomonitoring Studies
Implications for Future Research and Public Health
The integration of biomonitoring data from large population cohorts has significantly advanced our understanding of EDC exposures and their impact on fertility. Future research directions should focus on prospective study designs with repeated measures of both exposure and effect biomarkers to better capture windows of susceptibility and dynamic changes in exposure over time [47] [53]. Additionally, the development of novel effect biomarkers that can capture subtle changes in reproductive function prior to clinical manifestation of disease will enhance the utility of biomonitoring for early detection and prevention [50].
From a public health perspective, biomonitoring data provide critical evidence for regulatory decision-making and the development of interventions to reduce EDC exposures [46] [53]. The success of intervention studies such as the REED study in reducing phthalate exposures demonstrates the potential for targeted strategies to mitigate risks [53]. As biomonitoring methodologies continue to advance and incorporate multi-omics approaches, our ability to elucidate the complex relationships between EDC exposures and fertility outcomes will be further enhanced, ultimately contributing to improved reproductive health across populations.
The global decline in fertility rates represents a significant public health challenge, with male factors contributing to over 20% of infertility cases among reproductive-aged couples [54]. While assisted reproductive technology (ART) has achieved increasing maturity, clinicians continue to face challenges such as low embryo implantation and clinical pregnancy rates, the success of which depends heavily on embryo quality influenced by both female and male factors [54]. In recent years, research has illuminated the critical role of endocrine-disrupting chemicals (EDCs) – exogenous substances that interfere with hormone action – in impairing fertility parameters through multiple pathways [30] [40]. These chemicals, which include bisphenol A (BPA), phthalates, per- and polyfluoroalkyl substances (PFAS), and persistent organic pollutants (POPs), are ubiquitously present in personal care products, food packaging, plastics, and environmental contaminants [30] [40]. This technical review synthesizes current evidence linking EDC exposure to impairments in semen quality, ovarian reserve, and ultimately, success rates in ART, providing researchers and clinicians with a comprehensive framework for understanding these exposure-outcome relationships.
EDCs comprise a structurally diverse group of compounds that can interfere with the endocrine system by mimicking, blocking, or altering the synthesis, transport, metabolism, or elimination of endogenous hormones including estrogens, androgens, and thyroid hormones [40]. The estrogen, androgen, and thyroid hormone (EAT) receptors represent particularly important targets for EDC activity, with reproductive functions being especially vulnerable to disruption [16]. Table 1 summarizes the most prevalent EDCs, their common sources of exposure, and primary mechanisms of action relevant to reproductive health.
Table 1: Key Endocrine-Disrupting Chemicals: Exposure Sources and Reproductive Mechanisms
| EDC Class | Common Exposure Sources | Primary Reproductive Mechanisms |
|---|---|---|
| Bisphenol A (BPA) | Plastics, food containers, dental sealants, canned food linings [30] | Estrogen receptor agonist/antagonist; interacts with estrogen-signaling pathways [30] |
| Phthalates (PAEs) | Personal care products, cosmetics, fragrances, plasticizers [30] | Androgen receptor antagonism; interference with hypothalamic-pituitary-gonadal (HPG) axis feedback mechanisms [30] |
| Per- and Polyfluoroalkyl Substances (PFAS) | Non-stick cookware, food packaging, waterproof textiles [40] | Thyroid hormone disruption; estrogenic activity; potential impact on steroidogenesis [40] |
| Persistent Organic Pollutants (POPs) | Pesticides, industrial chemicals, environmental contaminants [40] | Estrogen receptor modulation; altered steroid hormone metabolism; oxidative stress induction [40] |
The following diagram illustrates the multifaceted mechanisms through which EDCs disrupt the hypothalamic-pituitary-gonadal (HPG) axis in both males and females, affecting reproductive function at multiple levels:
Diagram 1: Mechanisms of Endocrine Disruption in the HPG Axis. EDCs interfere with reproductive function at multiple levels including hypothalamic neuroendocrine signaling, pituitary gonadotropin secretion, direct gonadal toxicity, and hormone receptor binding.
Impact on Semen Quality Parameters
Conventional semen analysis remains the gold standard for assessing male fertility, with parameters established by the World Health Organization providing critical benchmarks for evaluation [55]. The integrity of sperm DNA has emerged as an increasingly important parameter, with the sperm DNA fragmentation index (DFI) now recommended by the 6th edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen as a conventional semen assay [54]. Table 2 outlines the standard semen quality parameters alongside documented effects of EDC exposure.
Table 2: Semen Quality Parameters and Documented EDC Effects
| Parameter | WHO Reference Value | EDC-Associated Alterations | Key EDCs Implicated |
|---|---|---|---|
| Semen Volume | ≥1.5 mL [55] | Reduced volume (<2 mL) [56] | Phthalates, pesticides, heavy metals [56] |
| Sperm Concentration | ≥15 million/mL [55] | Oligozoospermia; reduced total sperm count [40] [56] | BPA, phthalates, persistent organic pollutants [40] |
| Total Motility | ≥40% [55] | Asthenozoospermia; reduced progressive motility [40] | BPA, phthalates, pesticides [40] |
| Progressive Motility | ≥32% [55] | Decreased progressive movement [40] | BPA, phthalates [40] |
| Vitality | ≥58% live [55] | Increased sperm cell death [40] | Phthalates, heavy metals [56] |
| Morphology | ≥4% normal forms [55] | Teratozoospermia; increased abnormal forms [40] | BPA, phthalates, pesticides [40] |
| DNA Fragmentation Index (DFI) | <30% (variable) [54] | Increased DNA fragmentation [54] | Oxidative stress-inducing EDCs [54] |
Emerging evidence indicates that the detrimental effects of EDCs on semen quality may originate during fetal development. A landmark study examining occupational exposure found that men whose mothers were exposed to endocrine disruptors during pregnancy were twice as likely to have semen volume and total sperm count per ejaculation below WHO reference values [56]. The most significant associations were observed with pesticides, phthalates, and heavy metals [56]. The sperm DFI has demonstrated a negative correlation with conventional semen parameters including sperm motility, concentration, and normal morphology [54], establishing it as a valuable biomarker of sperm health in the context of EDC exposure.
Impact on Ovarian Reserve and Female Reproductive Function
In females, EDCs have been associated with multiple adverse reproductive outcomes including diminished ovarian reserve, polycystic ovary syndrome (PCOS), endometriosis, and hormonal imbalances [30] [40]. The hypothalamic-pituitary-ovarian axis is particularly vulnerable to disruption during critical windows of exposure, potentially leading to long-term consequences for reproductive function. Table 3 summarizes key ovarian reserve parameters and their alterations associated with EDC exposure.
Table 3: Ovarian Reserve Parameters and EDC-Associated Alterations
| Parameter | Clinical Significance | EDC-Associated Alterations | Key EDCs Implicated |
|---|---|---|---|
| Anti-Müllerian Hormone (AMH) | Marker of ovarian reserve; relatively stable throughout menstrual cycle [57] | Reduced AMH levels; lower ovarian reserve [40] | BPA, phthalates [30] [40] |
| Antral Follicle Count (AFC) | Ultrasonographic assessment of follicles (2-10 mm) [57] | Reduced antral follicle count [30] [40] | BPA, phthalates [30] |
| Day 3 FSH | Follicle-stimulating hormone level in early follicular phase [57] | Elevated FSH (>10 IU/L) indicating diminished reserve [40] | Multiple EDC classes [40] |
| Estradiol (E2) | Ovarian hormone production [57] | Altered estradiol levels; disrupted feedback mechanisms [30] | BPA, phthalates (estrogenic effects) [30] |
Bisphenol A has been specifically linked to lower antral follicle counts and reduced ovarian maturation in clinical studies, with some evidence suggesting this reduction may be reversible upon cessation of exposure [30]. Higher urinary BPA concentrations have been associated with an increased risk of implantation failure [30] and may play a role in the pathophysiology of PCOS, as evidenced by statistically significant positive associations between androgens and BPA levels in women with PCOS compared to controls [30]. Phthalate exposure has demonstrated a negative correlation with serum inhibin B levels, indicating a deleterious influence on antral follicle development [30].
The following experimental workflow outlines a comprehensive methodology for assessing the impact of EDC exposure on reproductive parameters in both clinical and research settings:
Diagram 2: Comprehensive EDC Reproductive Impact Assessment Workflow. This methodology integrates exposure assessment, biological sampling, advanced analytical techniques, and clinical evaluation to establish correlations between EDC exposure and reproductive outcomes.
ART Outcomes and Predictive Factors
The impact of EDCs on ART success rates represents a critical endpoint in the exposure-outcome relationship. Recent research has examined the correlation between EDC exposure and various ART parameters, including fertilization rates, embryo quality, and clinical pregnancy rates. A comprehensive retrospective analysis of 913 ART cycles found that sperm DNA fragmentation index demonstrated a negative correlation with fertilization rate but showed limited predictive efficacy for other embryological parameters [54]. Receiver operating characteristic (ROC) curve analysis revealed a DFI cut-off value of 21.15% for predicting high fertilization rate (≥80%), though with modest sensitivity (36.7%) and specificity (28.9%) [54].
Notably, the same study found no significant connection between DFI and embryological parameters in separate IVF and ICSI groups, suggesting that the technique used may modulate the impact of sperm DNA damage on ART outcomes [54]. These findings indicate that while EDC exposure may impair initial fertilization, its effects on subsequent embryonic development stages may be more complex and multifactorial.
Advanced Assessment Methodologies
Sperm DNA Fragmentation Index Assessment
The evaluation of sperm DNA fragmentation has emerged as a valuable tool in male fertility assessment, particularly in the context of EDC exposure. The acridine orange test (AOT) conducted under flow cytometry provides a robust methodology for DFI determination [54]. The experimental protocol involves:
- Sample Collection and Preparation: Fresh semen samples are collected by masturbation and placed in a 37°C incubator for liquefaction. Semen analysis is performed according to WHO guidelines [54].
- Sperm Processing: PureSperm density gradients are used for sperm preparation according to manufacturer's instructions. After centrifugation, the upper layer seminal plasma is aspirated and the 90% layer is collected, followed by washing twice with Hams F10 medium and centrifugation at 300 g for 10 minutes [54].
- DNA Fragmentation Assessment: Liquefied semen (10 µL) is incubated with 90 µL of disodium hydrogen phosphate sperm diluent. The solution is transferred to a flow cytometry test tube and mixed with 200 µL of pretreatment fluid. After 30 seconds, 600 µL of mixed solution (FCM buffer and acridine orange) is incorporated and blended for 5 minutes [54].
- Flow Cytometry Analysis: Specific parameter settings include: threshold of 'FSC-H greater than 100,000', 'Ungated' storage gate, 560 PerCP channel voltage, 340 FITC channel voltage, and low sample flow rate. Data are collected from at least 5000 particles, with sperm DFI computed as the ratio of red to total (red + green) spermatozoa × 100% [54].
In Silico Approaches for EDC Identification
Advances in computational toxicology have enabled the development of sophisticated models for predicting endocrine-disrupting activity. Machine learning approaches utilizing transcriptomics data have shown particular promise:
- Qualitative Gene expression Activity Relationship (QGexAR) Models: These models use gene expression profiles from exposed cell lines (e.g., MCF7 breast cancer cells and A549 alveolar basal epithelial cells) to predict chemical disruption of estrogen, androgen, and thyroid hormone modalities [16].
- Feature Selection and Algorithm Optimization: Different feature selection methods and classification algorithms including CATBoost, XGBoost, Random Forest, SVM, Logistic Regression, AutoKeras, TPOT, and deep learning models can be tested for optimal prediction [16].
- Consensus Prediction: For each endocrine endpoint, the final prediction is made according to a consensus prediction based on the best model obtained for each cell line. Successful models have demonstrated consensus balanced accuracy on validation sets ranging from 0.725 to 0.840 for predicting receptor binding and antagonistic effects [16].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagents and Materials for EDC Reproductive Studies
| Reagent/Material | Application | Function | Example Specifications |
|---|---|---|---|
| PureSperm Density Gradients | Sperm preparation for ART and analysis [54] | Isolation of motile sperm with reduced DNA damage | 45% and 90% layers; centrifugation at 300g for 10 minutes [54] |
| Acridine Orange | Sperm DNA fragmentation assessment [54] | Fluorescent staining of single-stranded (red) and double-stranded (green) DNA | AOT conducted under flow cytometry; excitation at 450-490nm [54] |
| Anti-Müllerian Hormone (AMH) Assay | Ovarian reserve testing [57] | Quantitative measurement of AMH serum levels | ELISA-based; stable throughout menstrual cycle [57] |
| Recombinant FSH | Ovarian stimulation in ART cycles [54] | Controlled ovarian hyperstimulation | 150-300 IU daily in GnRH agonist/antagonist protocols [54] |
| Cell Lines (MCF7, A549) | In vitro EDC screening [16] | Assessment of gene expression changes following EDC exposure | LINCS L1000 project; 978 landmark genes [16] |
| Molecular Docking Software | In silico EDC prediction [58] | Prediction of binding affinity between chemicals and hormone receptors | CDocker energy parameters; Bayesian optimization [58] |
| Pyrrolo[3,2-c]pyrazole | Pyrrolo[3,2-c]pyrazole, CAS:250-88-4, MF:C5H3N3, MW:105.10 g/mol | Chemical Reagent | Bench Chemicals |
| Fmoc-N-Me-D-Phe(3-CN)-OH | Fmoc-N-Me-D-Phe(3-CN)-OH, MF:C26H22N2O4, MW:426.5 g/mol | Chemical Reagent | Bench Chemicals |
The evidence linking EDC exposure to impairments in semen quality, ovarian reserve, and ART outcomes continues to accumulate, revealing complex exposure-outcome relationships mediated through multiple endocrine pathways. Sperm DNA fragmentation index demonstrates clinical utility as a biomarker of male reproductive toxicity, while ovarian reserve parameters such as AMH and antral follicle count provide sensitive indicators of female reproductive impairment. Advanced assessment methodologies including flow cytometric DFI measurement and machine learning approaches for EDC identification represent valuable tools for researchers and clinicians working to understand and mitigate the reproductive health impacts of endocrine-disrupting chemicals. Future research directions should prioritize longitudinal studies to assess cumulative EDC effects, investigation of cocktail effects from mixed exposures, and development of refined threshold levels for reproductive toxicity.
The Developmental Origins of Health and Disease (DOHaD) paradigm represents a fundamental shift in understanding how environmental exposures during sensitive developmental periods program lifelong health and disease trajectories [59]. This framework posits that developmental plasticity enables a single genotype to produce multiple phenotypes in response to specific environmental conditions during critical windows of susceptibility [60]. When environmental exposures—particularly to endocrine-disrupting chemicals (EDCs)—occur during these vulnerable periods, they can cause permanent alterations in tissue development and function, leading to increased disease risk in adulthood and potentially across generations [60] [59].
The context of endocrine disruption has brought particular urgency to DOHaD research, as EDCs can interfere with hormonal signaling at extremely low concentrations, often following non-monotonic dose-response curves that challenge traditional toxicological models [61]. For fertility research specifically, the implications are profound: exposures to EDCs during critical developmental windows are increasingly linked to the rising incidence of reproductive disorders observed globally, including diminished semen quality, female reproductive pathologies, and early puberty [62] [63] [64]. This whitepaper synthesizes current scientific understanding of how EDCs acting during development establish trajectories that impact reproductive health across the lifespan.
Windows of Developmental Susceptibility to EDCs
Critical windows of susceptibility represent specific developmental stages when organisms exhibit heightened vulnerability to environmental influences due to rapid cell division, tissue differentiation, and metabolic programming [62] [59]. For the reproductive system, these windows encompass precisely orchestrated sequences of hormonal signaling that direct sexual differentiation, organogenesis, and functional maturation.
Table 1: Critical Windows of Susceptibility for Human Reproductive Development
| Developmental Window | Key Reproductive Developmental Processes | Potential Consequences of EDC Exposure |
|---|---|---|
| Germline Programming | Epigenetic reprogramming, genomic imprinting | Transgenerational inheritance of reproductive disorders [60] [65] |
| Fetal Development | Gonadal sex determination, testis/ovarian development, Müllerian/Wolfian duct differentiation | Cryptorchidism, hypospadias, reduced anogenital distance, ovarian dysgenesis [62] [11] |
| Late Gestation | Masculinization of the brain, testicular descent, folliculogenesis in females | Altered mating behaviors, impaired fertility, altered hypothalamic-pituitary-gonadal axis function [60] [11] |
| Early Postnatal Period | Mini-puberty, steroidogenic cell maturation, Sertoli cell proliferation, follicular assembly | Premateure ovarian failure, altered testosterone production, reduced sperm production capacity [62] [64] |
| Puberty/Adolescence | Reactivation of hypothalamic-pituitary-gonadal axis, development of secondary sexual characteristics, brain maturation | Early or delayed puberty, altered cyclicity, impaired brain programming of reproductive behaviors [64] |
The fetal and perinatal periods represent perhaps the most vulnerable windows for EDC exposure, as sexual differentiation is highly dependent on the precise timing and concentration of steroid hormones [62]. During this period, EDCs can mimic or antagonize endogenous hormones, leading to permanent organizational effects that manifest as reproductive disorders at birth or later in life [62] [11]. The concept of faulty hormonal imprinting describes how developmental exposure to EDCs can program lifelong alterations in receptor sensitivity and hormonal response pathways [64].
Molecular Mechanisms of EDC Action During Development
Epigenetic Reprogramming
Epigenetic mechanisms serve as the primary molecular interface between environmental exposures and long-term phenotypic changes in the DOHaD framework [60] [61]. EDCs have been shown to disrupt the establishment of epigenetic marks during critical developmental windows when widespread epigenetic reprogramming occurs [60].
Table 2: Epigenetic Mechanisms of EDC Action in Reproductive Tissues
| Epigenetic Mechanism | EDCs Implicated | Reproductive Health Consequences |
|---|---|---|
| DNA Methylation Alterations | BPA, DES, phthalates, PCBs, dioxins [61] | Altered expression of genes involved in ovarian function, implantation, and placental development; uterine pathologies including endometrial hyperplasia and fibrosis [61] |
| Histone Modifications | BPA, DES [60] [61] | Changes in chromatin accessibility affecting steroid hormone receptor expression and function [61] |
| Non-coding RNA Expression | BPA, phthalates [60] | Dysregulation of cellular differentiation and metabolic pathways in reproductive tissues [60] |
The uterus is particularly vulnerable to epigenetic dysregulation by EDCs, with studies demonstrating that developmental exposures to BPA, DES, and other EDCs alter DNA methylation patterns in genes critical for uterine development and function, including HOXA10 and other imprinted genes [61]. These epigenetic changes can persist long after the initial exposure has ended and may be transmitted to subsequent generations [65].
Specific Signaling Pathways Disrupted by EDCs
The following diagram illustrates key signaling pathways disrupted by EDCs during critical developmental windows:
Diagram 1: EDC disruption of nuclear receptor signaling and epigenetic regulation. EDCs bind to nuclear hormone receptors (estrogen receptor-ER, androgen receptor-AR, thyroid receptor-TR), recruiting epigenetic modifiers that alter gene expression patterns critical for normal reproductive development.
Experimental Models and Methodologies
Animal Models of Developmental EDC Exposure
Animal models remain essential for investigating DOHaD mechanisms because they allow controlled exposure during specific developmental windows and multigenerational tracking [60]. Standardized protocols have been established to mimic human exposure scenarios:
Table 3: Experimental Protocols for Developmental EDC Exposure Studies
| Experimental Approach | Key Methodological Elements | Endpoint Assessments |
|---|---|---|
| In Utero Exposure | Direct administration of EDCs to pregnant dams via oral gavage, subcutaneous injection, or diet from conception through gestation [60] [61] | Fetal gonad histology, steroid hormone levels, gene expression analyses in reproductive tissues [62] [60] |
| Lactational Transfer | Exposure during lactation only; cross-fostering experiments to separate in utero from lactational exposure [60] | Postnatal reproductive tract development, pubertal timing, adult fertility assessments [62] [64] |
| Multigenerational Studies | Continuous exposure across multiple generations to distinguish direct exposure effects from transgenerational inheritance [65] | Germ cell epigenome analyses, reproductive organ pathology in unexposed generations (F3 and beyond) [65] [61] |
| Human Tissue Xenografts | Transplantation of human fetal reproductive tissues into immunocompromised mice followed by EDC exposure [61] | Assessment of human-specific responses, tissue remodeling, and differentiation patterns [61] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for DOHaD-EDC Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Prototypic EDCs | Diethylstilbestrol (DES), Bisphenol A (BPA), Di(2-ethylhexyl) phthalate (DEHP) [1] [61] | Positive controls for establishing experimental models of endocrine disruption [1] [61] |
| EDC Mixtures | Agricultural pesticide mixtures, plasticizer combinations, "real-world" environmental extracts [59] | Assessing cumulative effects and chemical interactions relevant to human exposure scenarios [59] |
| Epigenetic Inhibitors | 5-azacytidine (DNMT inhibitor), Trichostatin A (HDAC inhibitor) [60] [61] | Mechanistic studies to establish causal relationships between epigenetic changes and phenotypic outcomes [60] [61] |
| Steroid Hormone Assays | ELISA, LC-MS/MS for testosterone, estradiol, progesterone, AMH [63] | Quantifying endocrine function and steroidogenic capacity in exposed animals and human cohorts [63] |
| Epigenomic Analysis Tools | Methylated DNA immunoprecipitation (MeDIP), Reduced Representation Bisulfite Sequencing (RRBS), ChIP-seq [60] [61] | Genome-wide mapping of DNA methylation and histone modifications in reproductive tissues [60] [61] |
| Reproductive Tissue Biobanks | Human fetal gonad banks, ovarian cortex repositories, semen sample cohorts [62] [63] | Translational studies comparing animal model findings with human tissue responses [62] [63] |
| Phenazine-1-carbaldehyde | Phenazine-1-carbaldehyde|CAS 1082-80-0|RUO | Phenazine-1-carbaldehyde is a key chemical intermediate for research. This product is for Research Use Only. Not for human or veterinary use. |
Transgenerational Inheritance and EDCs
Perhaps the most conceptually challenging aspect of the DOHaD framework is the potential for EDC exposures to cause effects that persist across multiple generations without additional exposure [65]. This transgenerational inheritance occurs when the germline (sperm or egg cells) is reprogrammed during development, allowing the transmission of epigenetic information to subsequent generations [65].
The following diagram illustrates the experimental approach for detecting transgenerational effects:
Diagram 2: Experimental design for detecting transgenerational inheritance. EDC exposure of the F0 pregnant dam exposes the F1 generation in utero and the F2 generation through germline exposure. Effects observed in the completely unexposed F3 generation represent true transgenerational inheritance.
The molecular basis of transgenerational inheritance involves epigenetic reprogramming of the germline that escapes the widespread erasure of epigenetic marks that normally occurs during gametogenesis and early embryogenesis [65]. Studies have shown that EDCs such as vinclozolin, DES, and BPA can induce transgenerational effects on reproductive health, including reduced sperm quality, ovarian abnormalities, and premature reproductive aging [65] [61].
The DOHaD paradigm has fundamentally transformed our understanding of how environmental exposures during development shape lifelong reproductive health trajectories. The evidence is compelling that EDCs, by interfering with hormonal signaling during critical windows of susceptibility, can reprogram developmental pathways through epigenetic mechanisms, leading to increased risk of reproductive disorders across the lifespan and potentially across generations.
Significant challenges remain in translating these findings into clinical practice and public health policy. The non-monotonic dose responses exhibited by many EDCs, the complex mixtures present in real-world exposures, and the long latency between exposure and disease manifestation complicate risk assessment [61]. Future research priorities should include: developing more sensitive biomarkers of developmental EDC exposure; elucidating the precise mechanisms of transgenerational epigenetic inheritance; and identifying nutritional or pharmacological interventions that might mitigate or reverse the developmental programming effects of EDCs.
For fertility researchers and drug development professionals, incorporating DOHaD principles means considering developmental exposure history as a critical variable in understanding reproductive disease etiology and treatment response. As we move toward more personalized approaches to medicine, recognizing the developmental origins of reproductive dysfunction will be essential for developing effective prevention and treatment strategies.
Research on the impact of endocrine-disrupting chemicals (EDCs) on fertility is fraught with methodological complexities that challenge the establishment of clear causal relationships. EDCs are natural or human-made chemicals that can mimic, block, or interfere with the body's hormones [1]. The endocrine system operates through hormones acting in extremely small amounts, meaning even minor disruptions at low exposure levels can cause significant developmental and biological effects [1]. In fertility research, this sensitivity is paramount, as EDCs can disrupt the hypothalamic-pituitary-gonadal (HPG) axis crucial for reproductive function in both males and females [48] [66].
The core challenge lies in the multifaceted nature of EDC exposure. Humans encounter a complex mixture of these chemicals from numerous everyday sources, including food packaging, cosmetics, pesticides, and household products [67] [1]. This reality creates three persistent methodological hurdles: controlling for confounding factors, accurately classifying exposure levels, and understanding the combined effects of chemical mixtures. A study analyzing 213 consumer products found 55 distinct EDCs and asthma-related compounds, many not listed on labels, highlighting the exposure complexity researchers must unravel [67]. This guide details these challenges and presents advanced methodological approaches to address them, aiming to enhance the rigor and interpretability of fertility research in this field.
Core Methodological Challenges in EDC and Fertility Research
Confounding by Lifestyle, Genetic, and Demographic Factors
A significant obstacle in isolating the effect of EDCs on fertility is the potential for confounding. This occurs when an apparent association between an EDC and a fertility outcome is actually driven, wholly or partially, by a third, extraneous variable associated with both the exposure and the outcome.
- Lifestyle and Comorbidities: Factors such as body mass index (BMI), smoking status, stress, and food habits are associated with infertility and may also correlate with exposure levels to certain EDCs [48] [68]. For example, dietary patterns can influence both the intake of EDCs from food sources and metabolic health, which independently affects fertility.
- Genetic and Epigenetic Factors: Individual genetic variation can influence susceptibility to EDCs. Polymorphisms in genes involved in hormone receptor function, xenobiotic metabolism, or DNA repair can modify the relationship between exposure and effect [68]. Furthermore, EDCs themselves can induce epigenetic modifications, such as changes in DNA methylation, which alter gene expression without changing the DNA sequence and may mediate long-term effects on fertility [48].
- Demographic and Socioeconomic Variables: Age, particularly the trend toward later childbearing, is a strong independent predictor of fertility status and must be carefully controlled for in analyses [48]. Socioeconomic status can be a proxy for a range of factors, including occupational exposure, diet quality, and access to consumer products, all influencing EDC exposure profiles.
Table 1: Common Confounding Factors in EDC-Fertility Research
| Factor Category | Specific Examples | Potential Influence |
|---|---|---|
| Lifestyle | BMI, smoking, alcohol consumption, stress | Affects hormonal balance and metabolic health; correlates with product use. |
| Genetic/ Biological | Gene polymorphisms (e.g., in hormone receptors), epigenetic status | Determines individual susceptibility to EDC effects. |
| Demographic | Age, socioeconomic status, geographic location | Strongly correlated with fertility potential and exposure opportunities. |
| Timing | Developmental stage (in utero, puberty, adult) | Critical windows of susceptibility (e.g., DOHaD concept) [48]. |
Exposure Misclassification
Accurately assessing an individual's exposure to EDCs is notoriously difficult, and misclassification is a major source of bias and measurement error that often obscures true effects.
- Complex Exposure Pathways: Human exposure occurs through ingestion (food, water), inhalation (air, dust), dermal absorption (cosmetics), and transplacental transfer [69] [1]. Quantifying aggregate exposure from all routes is complex.
- Variable Chemical Half-Lives: EDCs have vastly different half-lives within the body. Some, like BPA and phthalates, are metabolized and excreted within hours [68]. Others, like DDT or TCDD, persist for years, accumulating in adipose tissue [69] [68]. A single urine or serum measurement may adequately represent exposure for persistent chemicals but can be a poor indicator of long-term exposure for non-persistent chemicals, leading to misclassification.
- Limitations of Job-Exposure Matrices: In occupational studies, job titles are often used as a proxy for exposure via a Job-Exposure Matrix (JEM). However, this can lead to non-differential misclassification, as the actual exposure can differ significantly from the JEM estimate [70]. This bias typically attenuates risk estimates toward the null.
- Lack of Product Labeling: Many products containing EDCs do not list them on labels, making it difficult for researchers to fully account for all exposure sources through questionnaires [67].
Mixture Effects
Humans are never exposed to a single EDC in isolation, yet most toxicological data and many epidemiological studies focus on individual chemicals. This creates a significant gap between experimental conditions and real-world exposure.
- Synergistic and Antagonistic Interactions: Chemicals in a mixture can interact, leading to combined effects that are greater (synergy) or less (antagonism) than the sum of their individual effects. For example, EDCs can have synergistic or antagonistic outcomes by interfering with multiple hormone receptors simultaneously [68].
- The "Cocktail Effect": The presence of complex mixtures of EDCs in the general population raises concerns about potential confounding in epidemiological studies, where an observed effect attributed to one chemical might be due to co-exposure to another, unmeasured substance [67] [69].
- Common Mechanism of Action: Many EDCs, despite different structures, share common mechanisms, such as binding to estrogen receptors (ER) or androgen receptors (AR), or activating the aryl hydrocarbon receptor (AhR) [68]. This makes additive or synergistic effects via the same pathway a distinct possibility.
Diagram: The Challenge of EDC Mixture Effects in Research
Advanced Methodological Approaches and Protocols
Mitigating Confounding and Bias
Addressing confounding requires a multi-pronged strategy implemented from the study design phase through to data analysis.
Study Design Protocol: Prospective Cohort Studies
- Objective: To assemble a population before the onset of the disease (infertility) and collect detailed exposure and covariate data over time.
- Methodology: Recruit couples planning pregnancy (e.g., from the general population or fertility clinics). Collect baseline data on demographics, medical history, lifestyle (smoking, alcohol, diet), and occupational history. Collect biospecimens (blood, urine) for EDC biomarker analysis at baseline and periodically during follow-up. Follow couples for 12 months or until pregnancy is achieved, meticulously tracking time-to-pregnancy (TTP) or clinical pregnancy.
- Rationale: This design allows for the measurement of potential confounders before the outcome is known, reducing the risk of certain biases. The collection of biospecimens enables objective exposure assessment.
Statistical Analysis Protocol: Directed Acyclic Graphs (DAGs) and Multivariate Modeling
- Objective: To visually map and statistically control for confounding pathways.
- Methodology:
- Construct a DAG: Based on subject-matter knowledge, map the assumed causal relationships between the EDC exposure, fertility outcome, and all relevant confounders (e.g., age, BMI, socioeconomic status).
- Identify Minimal Sufficient Adjustment Set: Use established rules (e.g., back-door criterion) to identify the smallest set of variables that need to be adjusted for to obtain an unbiased estimate of the EDC effect.
- Apply Statistical Models: Use multivariable regression models (e.g., Cox proportional hazards for TTP, logistic regression for clinical pregnancy) that include the EDC exposure and the identified sufficient adjustment set.
Refining Exposure Assessment
Overcoming exposure misclassification requires moving beyond crude proxies to more precise and temporally resolved metrics.
Experimental Protocol: Biospecimen Collection for Biomarker Analysis
- Objective: To obtain an internal dose measurement of EDC exposure.
- Methodology:
- Matrix Selection: For non-persistent chemicals (e.g., BPA, phthalates), collect first-morning void urine samples. Due to high intra-individual variability, collect multiple samples per participant (e.g., over a week or in each trimester of a study) to characterize medium-to-long-term exposure better. For persistent chemicals (e.g., PCBs, DDT), fasting serum or plasma is appropriate.
- Sample Handling: Store samples at -80°C to prevent degradation. Use certified, pre-cleaned containers to avoid contamination.
- Chemical Analysis: Utilize high-performance liquid chromatography (HPLC) or gas chromatography coupled with tandem mass spectrometry (GC-MS/MS or LC-MS/MS) for high sensitivity and specificity. Always include quality control/quality assurance (QC/QA) samples, including blanks and spiked samples, with each batch.
Exposure Modeling Protocol: Creating Aggregate Exposure Scores
- Objective: To combine multiple exposure metrics into a single, more robust score.
- Methodology: For non-persistent chemicals, calculate the geometric mean of EDC concentrations from multiple urine samples. Combine biomarker data with questionnaire data on product use (e.g., frequency of canned food consumption, cosmetic use) using statistical methods like principal component analysis (PCA) or weighted indices to create an aggregate exposure score that reflects multiple sources and routes.
Tackling Mixture Effects
Innovative statistical and experimental models are needed to move from single-chemical to mixture risk assessment.
Statistical Protocol: Mixture Analysis using Bayesian Kernel Machine Regression (BKMR)
- Objective: To model the complex, potentially non-linear, joint effect of an EDC mixture on a fertility outcome.
- Methodology:
- Variable Selection: Identify a priori a group of EDCs suspected to be correlated and have common biological targets (e.g., estrogenic chemicals).
- Model Fitting: Use BKMR, a flexible modeling approach that can handle correlated exposures, non-linear dose-responses, and interactions between mixture components.
- Output Interpretation: Examine the overall mixture effect and the component-wise effect of a single chemical when all other chemicals in the mixture are fixed at a particular percentile (e.g., median). Visualize results using plots to identify potential interactions and non-linearities.
Experimental Protocol: In Vitro Bioassay Screening of Mixtures
- Objective: To rapidly assess the combined biological activity of an EDC mixture without quantifying every individual chemical.
- Methodology:
- Sample Extraction: Extract chemicals from a relevant matrix (e.g., household dust, serum pools) using solid-phase extraction (SPE).
- In Vitro Bioassays: Use cell-based reporter gene assays (e.g., ERα CALUX, AR CALUX) to measure the total estrogenic or androgenic activity of the extract.
- Bioanalytical Equivalency: Compare the measured bioactivity to the activity predicted from the chemical analysis of known EDCs in the extract. A significant difference (e.g., higher measured activity) suggests the presence of unknown bioactive compounds or synergistic interactions.
Diagram: Integrated Workflow for Assessing EDC Mixture Effects
Table 2: Key Reagents and Tools for EDC Fertility Research
| Research Tool | Function/Application | Technical Notes |
|---|---|---|
| LC-MS/MS / GC-MS/MS | Gold-standard for quantifying specific EDCs (BPA, phthalates, pesticides) in biospecimens. | High sensitivity required for low environmental concentrations. Critical for biomarker validation. |
| CALUX Bioassays | Cell-based assays to measure integrated hormonal (ER, AR) or toxic (AhR) activity of mixtures. | Provides functional data complementary to chemical analysis. |
| Job-Exposure Matrix (JEM) | Links self-reported occupation to probable EDC exposure levels and agents. | Useful for large-scale studies but a source of potential misclassification [70]. |
| Directed Acyclic Graph (DAG) Software | Visual tool to map causal assumptions and identify confounders for statistical control. | Prevents over- or under-adjustment in multivariate models. |
| BKMR / WQS R/Python Packages | Statistical software for analyzing complex, high-dimensional exposure mixture data. | Essential for moving beyond single-chemical models. |
The path to robust and actionable evidence on the impact of EDCs on fertility necessitates a conscious shift away from fragmented, single-chemical approaches. Success hinges on directly confronting the intertwined challenges of confounding, exposure misclassification, and mixture effects. By adopting rigorous study designs like prospective cohorts, employing repeated biospecimen collection to refine exposure assessment, and implementing advanced statistical methods like BKMR to deconstruct mixture effects, researchers can significantly reduce methodological heterogeneity. The integration of chemical quantification with bioassay-derived biological activity data represents a particularly powerful frontier. Ultimately, overcoming these methodological hurdles is not merely an academic exercise; it is fundamental for generating the reliable evidence required to inform effective public health policies, clinical guidance, and preventive strategies aimed at preserving fertility in an increasingly chemicalized world.
Challenges and Mitigation: Navigating Complex Exposures and Protecting Reproductive Health
Non-monotonic dose-response curves (NMDRCs) represent a significant paradigm shift in toxicology, defined mathematically as a change in the sign (positive/negative) of the slope of a dose-response relationship over the range of doses tested [71]. Unlike traditional monotonic responses where effects consistently increase or decrease with dose, NMDRCs demonstrate complex patterns such as U-shaped or inverted U-shaped curves, where low doses produce effects that are not predicted by responses observed at higher doses [72]. This phenomenon fundamentally challenges the centuries-old toxicological dogma that "the dose makes the poison" and the regulatory practice of using high-dose testing to extrapolate to presumed "safe" low doses [72].
For endocrine disrupting chemicals (EDCs) affecting fertility research, NMDRCs are particularly relevant. The endocrine system operates through complex feedback loops and receptor-based mechanisms that are highly sensitive to low concentrations of hormones and hormonally-active compounds [73]. EDCs can interfere with the hypothalamic-pituitary-gonadal (HPG) axis—the primary regulator of reproductive function—through multiple pathways, including estrogen receptor interference, androgen receptor antagonism, and disruption of steroidogenic enzymes [44]. When NMDRCs occur below the toxicological no-observed-adverse-effect level (NOAEL) or even below the established reference dose (RfD), they invalidate a fundamental assumption of traditional risk assessment: that high-dose hazards can reliably predict low-dose safety [71]. This has profound implications for protecting reproductive health, as current safety thresholds may be insufficient to prevent EDC-induced damage to fertility.
Mechanisms Underlying Non-Monotonic Dose Responses
The biological mechanisms generating NMDRCs are well-established and reflect the complex dynamics of endocrine signaling. Understanding these mechanisms is crucial for designing appropriate testing strategies and interpreting dose-response data in fertility research.
Molecular and Cellular Mechanisms
- Receptor Competition and Saturation: At low concentrations, EDCs may interact with high-affinity hormone receptors to stimulate responses. As doses increase, receptor saturation or downregulation can occur, diminishing the response. Additionally, competition between endogenous hormones and EDCs for receptor binding sites can create complex response patterns [72].
- Opposing Effects via Receptor Subtypes: Many hormone systems feature multiple receptor subtypes with different ligand affinities and opposing cellular functions. For example, adenosine receptors A1 and A2 can mediate opposing downstream effects, leading to biphasic responses across dose ranges [74].
- Cytotoxicity and Cell Death: At higher concentrations, EDCs may induce cytotoxic effects that mask or counteract the responses observed at lower doses. This can produce an inverted U-shaped curve where lower concentrations stimulate cellular responses (e.g., proliferation) while higher concentrations cause cell death [72].
Endocrine System-Specific Mechanisms
- Feedback Loop Disruption: The HPG axis operates through sophisticated feedback mechanisms where hormones from gonads regulate their own production via hypothalamic and pituitary pathways. EDCs can interfere with these feedback loops, creating non-monotonic responses. For instance, negative feedback loops in steroidogenesis can produce NMDRCs when low doses of EDCs alter feedback regulation [72].
- Receptor Selectivity and Promoter Specificity: EDCs may exhibit different affinities for various nuclear receptor isoforms or exhibit selective activity on specific gene promoters. This selective receptor modulation can result in enhanced responses at low doses and suppressed responses at high doses [72].
- Metabolic Activation and Inactivation: Dose-dependent shifts in metabolic pathways can convert EDCs to more or less active metabolites. At low doses, specific metabolic enzymes with high affinity may generate active metabolites, while at higher doses, alternative metabolic pathways with greater capacity but lower activity may dominate [75].
The following diagram illustrates key molecular mechanisms that generate NMDRCs in endocrine systems:
Experimental Evidence in Fertility Research
Table 1: Documented NMDRCs for Endocrine-Disrupting Chemicals in Reproductive Studies
| EDC | Experimental Model | Reproductive Endpoint | Dose Range of NMDRC | Reference |
|---|---|---|---|---|
| Bisphenol A (BPA) | In vitro cell systems | Receptor-mediated responses | >20% of all experiments show NMDRCs | [72] |
| Di(2-ethylhexyl)phthalate (DEHP) | Animal studies | Maternal serum testosterone, anogenital distance | 0.5, 1, and 5 µg/kg/d (below RfD) | [71] |
| Permethrin | Mouse model | Dopamine transport | 1.5 mg/kg/d (between NOAEL and RfD) | [71] |
| Resveratrol | Mouse model | Stomach lesion severity | 1-2 mg/kg/d (between NOAEL and RfD) | [71] |
| Chlorothalonil | Amphibian study | Survival | 0.0000164-0.0164 ppm (below RfD) | [71] |
The evidence from fertility research demonstrates that NMDRCs are not rare anomalies but common occurrences for EDCs. Analysis of BPA studies reveals that greater than 20% of all experiments and at least one endpoint in more than 30% of all studies exhibit non-monotonicity [72]. These responses frequently occur at environmentally relevant exposure levels, highlighting their significance for human fertility risk assessment.
Experimental Design and Methodological Considerations
Optimal Study Design for NMDRC Detection
- Dose Selection and Spacing: Traditional toxicology studies typically test only 3-4 doses, usually at high concentrations to identify the NOAEL. To adequately capture NMDRCs, studies should include more doses (5-8) with closer spacing in the low-dose range relevant to human exposures [71]. This is particularly important for fertility studies where endocrine systems are sensitive to low concentrations.
- Number and Timing of Measurements: Endocrine systems operate in dynamic rhythms with pulsatile hormone secretion. Single time-point measurements may miss NMDRCs that occur at specific temporal windows. Studies should include multiple measurement time points aligned with critical developmental or reproductive stages [73].
- Endpoint Selection: NMDRCs are more likely to manifest in specific endocrine-sensitive endpoints. Fertility research should include assessments of sperm quality, ovarian follicle counts, hormone levels, gene expression of steroidogenic enzymes, and anatomical measurements like anogenital distance [44] [75].
Statistical Approaches for NMDRC Analysis
- Model Selection: Traditional monotonic dose-response models (e.g., linear, Hill equation) cannot adequately capture NMDRCs. Statistical approaches should include biphasic models, such as the Brain-Cousens model, that specifically test for non-monotonicity [76].
- Power Considerations: NMDRCs may be missed due to insufficient statistical power. Studies should be designed with adequate sample sizes to detect potentially subtle low-dose effects. EFSA recommends power analysis specifically for detecting non-monotonic responses [76].
- Testing for Trend Changes: Appropriate statistical methods should be employed to detect significant changes in the slope of dose-response curves. These include piecewise regression, quadratic terms in polynomial models, and specialized software designed for NMDRC detection [76].
The following workflow diagram outlines an optimized experimental approach for detecting NMDRCs in fertility research:
Essential Research Reagents and Experimental Tools
Table 2: Research Reagent Solutions for NMDRC Studies in Fertility Research
| Reagent/Tool Category | Specific Examples | Application in NMDRC Research | Key Considerations |
|---|---|---|---|
| EDC Standards | BPA, DEHP, atrazine, PCBs, PBDEs | Positive controls for endocrine disruption studies | Use certified reference materials with >99% purity |
| Hormone Assays | ELISA, RIA, LC-MS/MS kits for estradiol, testosterone, TSH | Quantifying endocrine endpoints across dose range | High sensitivity for low-dose measurements |
| Receptor Binding Assays | ERα, ERβ, AR, TR transfected cell lines | Mechanism determination for receptor-mediated NMDRCs | Include multiple receptor subtypes |
| Molecular Biology Kits | qPCR arrays for steroidogenic genes, chromatin immunoprecipitation | Assessing gene expression changes at low doses | Focus on endocrine-relevant gene pathways |
| Cell Viability Assays | MTT, WST-1, ATP-based luminescence | Differentiating true hormesis from cytotoxicity | Multiple assays recommended |
| Animal Models | Zebrafish, Xenopus, rat, mouse models | In vivo assessment of reproductive NMDRCs | Select sensitive developmental stages |
Risk Assessment Implications and Future Directions
Current Regulatory Challenges
The presence of NMDRCs in the low-dose range presents substantial challenges to conventional risk assessment frameworks. Regulatory agencies like the EFSA have acknowledged these challenges, noting that NMDRCs are "particularly relevant for receptor-mediated effects" [76]. The traditional approach of applying uncertainty factors to NOAELs obtained from high-dose studies becomes problematic when NMDRCs occur below these levels, as the fundamental assumption of monotonicity is violated [71]. Case studies with BPA and DEHP demonstrate how NMDRCs can complicate the determination of reference doses, requiring more sophisticated assessment approaches [76].
Recommended Framework for NMDRC-Informed Risk Assessment
- Mechanistic Data Integration: Risk assessment should incorporate mechanistic data on how EDCs interact with endocrine systems. The key characteristics of EDCs framework provides a structured approach for evaluating potential endocrine disruptors [1].
- Weight-of-Evidence Approach: Rather than relying on single studies, assessments should evaluate the consistency, reliability, and biological plausibility of NMDRC observations across multiple systems and species [73].
- Probabilistic Assessment Methods: EFSA recommends probabilistic approaches for evaluating NMDRCs, which can better account for uncertainty and variability in dose-response relationships [76].
- Targeted Testing Strategies: For EDCs with suspected NMDRCs, testing should include additional doses in the low-effect range and specific endpoints relevant to the endocrine mechanisms of action [77].
Future Research Priorities
Advancing risk assessment for EDCs in fertility research requires addressing critical knowledge gaps. Research should prioritize:
- Mixture Effects: Most real-world exposures involve multiple EDCs, yet NMDRC research has predominantly focused on single compounds. Studies are needed to examine how chemical mixtures interact to produce non-monotonic responses [78] [75].
- Epigenetic and Transgenerational Effects: EDCs can induce epigenetic modifications that alter disease susceptibility across generations. Research should explore how these effects manifest in NMDRCs and their implications for fertility [75].
- Improved Test Guidelines: Regulatory test guidelines (e.g., OECD protocols) need updating to require adequate dose spacing and endpoint selection capable of detecting NMDRCs [71].
- Biomarker Development: Sensitive biomarkers of early endocrine disruption could help identify NMDRCs before adverse fertility outcomes manifest [75].
The impact of NMDRCs on risk assessment necessitates a fundamental shift from traditional approaches toward more nuanced, biologically-informed frameworks that acknowledge the complex dynamics of endocrine systems and their disruption by environmental chemicals.
The "cocktail effect" refers to the combined biological impact of exposure to multiple endocrine-disrupting chemicals (EDCs) at low doses, which may produce significant adverse effects even when individual chemicals are present at concentrations below their no-observed-adverse-effect levels [79]. For researchers investigating fertility decline, this phenomenon presents particular challenges because EDCs from diverse sources—including plastics, pesticides, personal care products, and industrial contaminants—converge in human tissues through daily exposure [44] [48]. Current regulatory frameworks primarily assess chemicals individually, creating a significant gap between real-world exposure scenarios and toxicological evaluation methods [79] [80]. Understanding this complex interplay is especially crucial in fertility research, where EDCs can disrupt the delicate hormonal balance required for reproductive success through multiple synergistic mechanisms [81] [82].
The implications for reproductive health are substantial. Evidence suggests that combined exposure to EDCs may contribute to declining fertility rates through effects on ovarian reserve, oocyte maturation, ovulation, implantation, and embryonic development [81] [48]. Furthermore, these effects may transcend generations through epigenetic modifications, making the cocktail effect a critical area of investigation for understanding the multifaceted decline in reproductive health observed globally [48] [82].
Methodological Approaches for Studying Combination Effects
Experimental Models for Mixture Toxicity Assessment
Research into the cocktail effects of EDCs employs stratified experimental approaches, moving from epidemiological observation to mechanistic understanding. The EDC-MixRisk project developed a novel integrated strategy that begins with identifying real-life chemical mixtures through human biomonitoring studies [79]. This project utilized data from a Swedish cohort of more than 2,300 pregnant women to define reference chemical mixtures that mimic actual exposure patterns, which were then tested in various experimental models including cell-based assays and animal studies [79]. This approach provides a more realistic assessment compared to traditional methods that evaluate single chemicals in isolation.
The EuroMix project contributed to this framework by establishing tiered testing strategies to generate missing hazard data for mixtures and developing practical risk assessment methodologies [79] [83]. Their approach includes component-based methods where individual chemicals are tested and their combined effects modeled mathematically, and whole-mixture approaches where complex mixtures are tested directly [80]. For fertility-focused research, recommended experimental models include in vitro assays using human cell lines representing hypothalamic-pituitary-gonadal (HPG) axis components, ex vivo cultures of ovarian follicles, and in vivo models using sensitive developmental windows to capture endocrine-disrupting effects on reproductive capacity [44] [82].
Analytical Frameworks for Risk Assessment of Mixtures
Several mathematical models have been developed to predict and quantify the combined effects of chemical mixtures, each with specific applications and limitations:
Table 1: Methodologies for Cumulative Risk Assessment of Chemical Mixtures
| Methodology | Key Formula/Approach | Application in Fertility Research | Limitations |
|---|---|---|---|
| Hazard Index (HI) | HI = Σ (Exposureâ‚ᵢ₎ / Reference Doseâ‚ᵢ₎) | Screening-level assessment of EDC mixtures affecting HPG axis [80] | Assumes dose addition; may overlook interactions |
| Point of Departure Index (PODI) | PODI = Σ (Exposureâ‚ᵢ₎ / Point of Departureâ‚ᵢ₎) | Comparison of mixture potency relative to individual EDCs [80] | Requires high-quality dose-response data |
| Margin of Exposure (MOE) | MOEₘᵢₓ = 1 / Σ (1 / MOEâ‚ᵢ₎) | Identifying EDCs of concern for reproductive endpoints [80] | No established acceptability criteria for mixtures |
| Cumulative Risk Index (CRI) | CRI = Σ (Riskâ‚ᵢ₎) where Riskâ‚ᵢ₎ = Exposureâ‚ᵢ₎ / (Reference Doseâ‚ᵢ₎ × UFâ‚ᵢ₎) | Integrating uncertainty factors for different EDCs [80] | Complex implementation for diverse mixtures |
| Concentration Addition (CA) | Models mixture effects assuming similar mechanism of action [84] | Predicting effects of EDCs with common targets (e.g., ER binding) | Less accurate for chemicals with divergent mechanisms |
| Independent Action (IA) | Models mixture effects assuming dissimilar mechanisms [84] | Assessing EDCs affecting different reproductive pathways | Requires extensive mechanistic knowledge |
These methodologies enable researchers to move beyond single-chemical assessment, though each presents challenges in application to complex EDC mixtures affecting reproductive health. The CA and IA models have shown particular utility in predicting synergistic estrogenic and anti-androgenic effects of chemical mixtures relevant to fertility outcomes [84].
Key Research Findings on EDC Mixtures and Fertility
Documented Effects on Female Reproductive Health
Research on the cocktail effect has revealed multiple pathways through which EDC mixtures disrupt female reproductive function. The hypothalamic-pituitary-ovarian axis represents a primary target, with mixtures shown to interfere with gonadotropin-releasing hormone (GnRH) release, kisspeptin signaling, and steroid hormone feedback loops [44] [85]. These disruptions can manifest as altered ovarian function, impaired folliculogenesis, and reduced oocyte quality [48] [82].
Table 2: Documented Effects of EDC Mixtures on Female Reproductive Parameters
| Reproductive Endpoint | Impact of EDC Mixtures | Key EDCs Implicated | Evidence Level |
|---|---|---|---|
| Ovarian Reserve | Reduction in antral follicle count; accelerated follicle atresia [81] [82] | BPA, phthalates, PCBs, pesticides | Human epidemiological studies and animal models |
| Oocyte Quality | Increased mitochondrial dysfunction; spindle abnormalities; DNA damage [48] | BPA, phthalates, heavy metals | In vitro oocyte maturation studies |
| Ovulation Rate | Disrupted LH surge timing; impaired follicular rupture [44] [82] | Phthalates, parabens, BPA | Animal models and human cohort studies |
| Embryo Implantation | Altered endometrial receptivity; defective decidualization [81] [48] | BPA, phthalates, dioxins | Human IVF outcomes and endometrial cell cultures |
| Hormonal Balance | Disrupted feedback in HPG axis; altered steroidogenesis [44] [68] | PCBs, pesticides, plasticizers | Longitudinal fertility studies |
| IVF Outcomes | Reduced fertilization rates; lower clinical pregnancy rates [81] [82] | Phthalates, BPA, parabens | Clinical studies of infertile populations |
The EDC-MixRisk project specifically demonstrated that real-life relevant mixtures interfere with thyroid hormone signaling, which is essential for brain development and reproductive function, at concentrations found in pregnant women [79]. This finding is particularly relevant for fertility research as thyroid function is intricately connected to reproductive outcomes.
Mechanistic Insights into Combination Effects
The molecular mechanisms underlying the cocktail effect involve complex interactions at multiple biological levels. EDC mixtures have been shown to produce synergistic effects at hormone receptors, where the combined activity exceeds what would be predicted from simple addition of individual effects [84]. For example, combinations of estrogenic compounds can produce dramatic enhancements in receptor activation even when each component is present at negligible concentrations [44].
Epigenetic modifications represent another critical mechanism, with EDC mixtures shown to alter DNA methylation patterns in genes regulating reproductive function [48] [82]. These changes may explain the transgenerational effects observed in some studies, where exposure to EDC mixtures in one generation affects fertility outcomes in subsequent generations not directly exposed [82]. Oxidative stress pathways also integrate signals from multiple EDCs, resulting in cumulative damage to ovarian tissue and gametes that exceeds the impact of individual chemicals [48].
Figure 1: Integrated Mechanisms of EDC Mixtures in Fertility Impairment. Multiple EDCs converge on key cellular targets including hormone receptors, epigenetic regulators, and stress response pathways, collectively disrupting reproductive function through the hypothalamic-pituitary-gonadal (HPG) axis.
The Scientist's Toolkit: Essential Reagents and Methods
Research Reagent Solutions for EDC Mixture Studies
Table 3: Essential Research Tools for Investigating EDC Mixture Effects on Fertility
| Reagent/Method | Function | Application Example |
|---|---|---|
| Human serum samples from cohort studies | Biomonitoring of real-life EDC mixtures | Establishing relevant mixture ratios for experimental studies [79] |
| Kisspeptin immunoassays | Quantification of key neuroendocrine peptide | Assessing hypothalamic function in HPG axis disruption [85] |
| ERα and ERβ reporter gene assays | Detection of estrogenic/anti-estrogenic activity | Screening mixture effects on estrogen signaling [44] [68] |
| Antral follicle culture systems | Ex vivo model of ovarian function | Testing direct effects of mixtures on folliculogenesis [82] |
| CALUX bioassays | High-throughput screening of receptor activity | Rapid assessment of mixture effects on multiple nuclear receptors [84] |
| LC-MS/MS systems | Quantitative analysis of EDCs in biological samples | Measuring internal exposure levels in tissue and fluids [83] |
| DNA methylation arrays | Genome-wide epigenetic profiling | Identifying transgenerational effects of mixture exposure [48] [82] |
| Recombinant steroidogenic enzymes | In vitro assessment of hormone synthesis | Testing mixture effects on androgen/estrogen production [68] |
Standardized Experimental Workflow
A robust methodological framework for investigating cocktail effects on fertility should integrate exposure assessment, mixture preparation, and phenotypic evaluation:
Figure 2: Experimental Workflow for EDC Mixture Fertility Assessment. This tiered approach begins with human exposure data and progresses through increasingly complex biological systems to evaluate mixture effects.
The study of cocktail effects in endocrine disruption represents a paradigm shift in how we approach chemical safety assessment, particularly for complex endpoints like fertility. The evidence clearly indicates that mixtures of EDCs at environmentally relevant concentrations can disrupt multiple aspects of reproductive function through synergistic interactions that would not be predicted by single-chemical testing [79] [84]. For researchers and drug development professionals, this necessitates the development of more sophisticated testing strategies that account for real-world exposure scenarios.
Future research priorities should include the establishment of standardized EDC mixture panels representative of different exposure populations, the development of high-content screening platforms that capture complex endocrine interactions, and the integration of epigenetic endpoints into mixture assessment protocols [48] [83]. Additionally, there is an urgent need for regulatory frameworks that incorporate mixture effects into chemical safety evaluation, particularly for chemicals that may impact reproductive health across generations [79] [80]. As the evidence base grows, the scientific community must translate these findings into practical assessment tools that better protect reproductive health from the hidden threat of chemical mixtures.
Identifying Vulnerable Populations and Life Stages for Targeted Intervention
Endocrine-disrupting chemicals (EDCs) represent a diverse group of exogenous compounds that interfere with the normal function of the hormonal system, with profound implications for reproductive health across the lifespan [40] [1]. The central thesis of modern EDC research posits that susceptibility to these chemicals is not uniform; rather, it is critically dependent on the specific life stage during which exposure occurs and the unique physiological context of the exposed population [39]. A growing body of evidence demonstrates that EDCs, including bisphenol A (BPA), phthalates, per- and polyfluoroalkyl substances (PFAS), and persistent organic pollutants, disrupt delicate hormonal balances essential for normal reproductive development and function [40] [44].
The concept of "critical windows of vulnerability" has emerged as a fundamental principle in understanding EDC impacts on fertility. These windows—including fetal development, early childhood, puberty, and reproductive adulthood—represent periods when hormonal signaling is particularly active and organizational processes are underway, rendering them exceptionally sensitive to external disruption [40] [86]. Furthermore, emerging research indicates that genetic background, pre-existing health conditions, and simultaneous exposure to multiple EDCs ("cocktail effects") can significantly modulate individual susceptibility [39] [12]. This technical guide synthesizes current evidence on vulnerable populations and life stages to inform targeted intervention strategies in research and public health policy.
Critical Windows of Vulnerability to EDC Exposure
Developmental Origins: Fetal and Early Life Exposure
The fetal period represents perhaps the most critical window of vulnerability to EDC exposure. During development, the reproductive system undergoes organizational processes that are guided by precise hormonal cues and are exceptionally sensitive to disruption by exogenous chemicals [39] [86]. Exposure during this period can cause epigenetic reprogramming of germ cells, altering DNA methylation patterns and histone modifications in ways that may not manifest as observable health outcomes until much later in life [39] [12]. These early exposures have been linked to increased risk of reproductive disorders in adulthood, including testicular dysgenesis syndrome in males and polycystic ovary syndrome (PCOS) in females [12] [86].
Experimental models demonstrate that fetal EDC exposure can disrupt the formation of the hypothalamic-pituitary-gonadal (HPG) axis, the primary regulator of reproductive function [44]. This disruption can permanently alter the set points for hormonal feedback loops, leading to lifelong consequences for reproductive capacity [39]. Human epidemiological studies have confirmed that maternal exposure to EDCs during pregnancy is associated with altered anogenital distance in offspring, earlier age at menarche in daughters, and reduced sperm quality in sons [40] [86].
Pubertal Transition: A Period of Heightened Sensitivity
Puberty represents another crucial window of vulnerability due to the reactivation of the HPG axis and the surge of hormonal activity that drives sexual maturation [30] [86]. The precise timing of pubertal onset is controlled by complex neuroendocrine processes that are vulnerable to disruption by EDCs. Exposure during this period can alter the trajectory of pubertal development, with potential consequences for future reproductive health [86].
Recent evidence indicates that EDC exposure is associated with both precocious and delayed puberty, depending on the specific chemical properties and exposure timing [86]. For instance, lavender oil and tea tree oil contain potential endocrine disruptors that have been linked to premature breast development in girls and abnormal breast development in boys [1]. The vulnerability during puberty is further modulated by factors such as body mass index (BMI), with overweight or obese adolescents potentially experiencing different susceptibility profiles due to altered hormonal milieu and metabolic factors [86].
Reproductive Adulthood and Assisted Reproduction
While much research has focused on developmental exposures, the reproductive years represent a period of continued vulnerability to EDCs [40]. In adults, EDCs can disrupt cyclic hormonal patterns in females and spermatogenesis in males, leading to diminished fertility [40] [87]. Women undergoing assisted reproductive technologies (ART) represent a particularly important subpopulation for study, as EDCs measured in follicular fluid have been associated with poorer ART outcomes, including fewer mature oocytes, lower fertilization rates, and reduced implantation success [40] [86].
The table below summarizes key vulnerable populations and their specific susceptibilities to EDC exposure:
Table 1: Vulnerable Populations and Life Stages for Targeted Intervention
| Vulnerable Population/Life Stage | Key Susceptibilities | Potential Long-Term Consequences |
|---|---|---|
| Fetal Development | Organizational effects on reproductive system; Epigenetic reprogramming | Altered reproductive tract development; Increased risk of PCOS/testicular dysgenesis; Transgenerational effects [39] [12] [86] |
| Early Childhood | Ongoing brain and hormonal system development; Rapid growth periods | Altered neuroendocrine development; Precocious or delayed puberty; Metabolic programming effects [1] [86] |
| Puberty | Reactivation of HPG axis; Sexual maturation processes | Altered timing of puberty; Disrupted menstrual cyclicity; Impaired spermatogenesis; Long-term fertility impacts [30] [86] |
| Reproductive Age Adults | Cyclic hormonal patterns; Gametogenesis; Assisted reproduction | Reduced gamete quality; Hormonal imbalances; Impaired embryo development; Lower success with ART [40] [87] [86] |
| Individuals with Genetic Predispositions | Variants in hormone receptor genes; Detoxification pathway polymorphisms | Increased susceptibility to specific EDCs; Gene-environment interactions modifying risk profiles [39] |
Molecular Mechanisms of EDC Action Across Vulnerable Periods
Disruption of the Hypothalamic-Pituitary-Gonadal Axis
The HPG axis serves as the primary regulator of reproductive function across all life stages, and its disruption represents a fundamental mechanism through which EDCs impair fertility [44]. EDCs can interfere with multiple levels of this intricate neuroendocrine system by mimicking or blocking endogenous hormones, altering hormone synthesis and metabolism, or modifying hormone receptor expression and function [1] [44].
At the hypothalamic level, EDCs have been shown to disrupt the pulsatile secretion of gonadotropin-releasing hormone (GnRH), which governs the downstream release of pituitary gonadotropins [44]. This disruption can alter the feedback mechanisms that normally maintain hormonal balance, leading to impaired gametogenesis and steroidogenesis [44]. At the gonadal level, EDCs directly interfere with follicle development in females and spermatogenesis in males by binding to hormone receptors and modifying gene expression patterns essential for reproductive function [40] [12].
The following diagram illustrates the key points of HPG axis disruption by EDCs:
Epigenetic Modifications and Transgenerational Effects
A particularly concerning aspect of EDC exposure during vulnerable periods is the potential for epigenetic modifications that can be transmitted to subsequent generations [39] [12]. EDCs have been shown to alter DNA methylation patterns, histone modifications, and non-coding RNA expression in germ cells, creating a memory of exposure that persists long after the initial insult [12]. These epigenetic changes can reprogram the developmental trajectory of the reproductive system, leading to inherited susceptibilities to reproductive disorders.
Animal studies provide compelling evidence for transgenerational inheritance of reproductive dysfunction following developmental EDC exposure [12]. For example, exposure to vinclozolin or methoxychlor during fetal development has been associated with reduced sperm quality and fertility in multiple subsequent generations, despite the absence of direct exposure [12]. While human evidence for transgenerational effects remains limited, these findings from experimental models highlight the profound implications of early-life EDC exposure for future generations.
Quantitative Assessment of EDC Impacts on Vulnerable Populations
Epidemiological studies have quantified the association between EDC exposure and adverse reproductive outcomes across different vulnerable populations. The table below summarizes key effect sizes from recent research:
Table 2: Quantitative Assessment of EDC Effects on Reproductive Outcomes in Vulnerable Populations
| EDC Class | Vulnerable Population | Key Reproductive Effects | Effect Size / Association |
|---|---|---|---|
| Bisphenol A (BPA) | Women of reproductive age | Reduced ovarian reserve; Implantation failure; PCOS risk | Higher urine BPA associated with 2-4x increased risk of implantation failure; Significant association with PCOS (OR: 1.5-2.0) [40] [30] [86] |
| Phthalates | Pregnant women; Reproductive age adults | Preterm birth; Altered pubertal timing; Reduced semen quality | High molecular weight phthalates associated with 2-3x increased risk of preterm birth; Urinary metabolites correlate with decreased sperm concentration (β: -0.15 to -0.25) [40] [1] |
| PFAS | Women with PCOS; General population | Reduced fertility; PCOS risk; Altered puberty | Women in high-PFAS areas had approximately 2x higher PCOS risk; 25% reduction in fecundability with high exposure [40] [86] |
| Persistent Organic Pollutants (POPs) | General population; Occupational exposure | Altered hormone levels; Reduced semen quality; Menopause timing | Significant associations with decreased testosterone (10-15%) and altered LH/FSH ratios; High exposure associated with 2-4 year earlier menopause [40] [86] |
Experimental Approaches for Studying Vulnerable Populations
Methodologies for Assessing EDC Impacts Across Life Stages
Epidemiological Study Designs for Vulnerable Populations
Cohort studies following individuals from prenatal development through adulthood provide the most comprehensive approach for identifying critical windows of vulnerability [40]. The Pregnancy and Childhood Network (PRIDE) study exemplifies this approach, enrolling pregnant women and following children through key developmental milestones to assess how early-life EDC exposures impact pubertal timing and reproductive development [86]. Case-control studies nested within larger cohorts allow for efficient investigation of specific reproductive outcomes such as PCOS, endometriosis, or infertility in relation to EDC exposure measured at different life stages [40] [87].
Longitudinal studies with repeated biomarker measurements are essential for capturing variations in exposure across developmental periods and accounting for the non-persistent nature of many EDCs [40]. These studies should incorporate sensitive windows for exposure assessment, including the first trimester of pregnancy (during reproductive tract differentiation), early infancy (during minipuberty), and the peripubertal period (during HPG axis maturation) [86]. Statistical approaches such as structured life-course models can help determine whether exposures during specific periods have distinct effects on later reproductive outcomes.
Molecular and Mechanistic Investigations
At the mechanistic level, gene expression biomarkers have emerged as powerful tools for identifying EDCs and understanding their molecular actions [88]. Established biomarkers for estrogen receptor α (ERα) and androgen receptor (AR) activity have demonstrated 94-98% accuracy in identifying agonists and antagonists in human cell lines [88]. These biomarkers can be applied to high-throughput transcriptomic technologies to screen large numbers of environmental chemicals for endocrine-disrupting potential.
For investigating transgenerational effects, multi-generational animal studies following the guidelines of the OECD Extended One-Generation Reproductive Toxicity Study (EOGRTS) provide the gold standard [12]. These studies should include detailed assessment of F1 (directly exposed) and F3 (transgenerational) offspring for reproductive abnormalities, coupled with epigenomic analyses of germ cells to identify heritable modifications [12]. Integration of epigenome-wide association studies with prospective birth cohort data represents a promising approach for translating these findings to human populations.
The following diagram outlines a comprehensive experimental workflow for assessing vulnerability to EDCs:
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for EDC Vulnerability Studies
| Research Tool Category | Specific Examples | Research Applications |
|---|---|---|
| Cell-Based Bioassays | ERα and AR reporter gene assays; MCF-7 and LNCaP cell lines | High-throughput screening for estrogenic/androgenic activity; Mechanism of action characterization [88] |
| Molecular Biology Reagents | DNA methylation kits; RNA sequencing platforms; Chromatin immunoprecipitation assays | Epigenetic profiling; Transcriptomic analysis; Histone modification assessment [12] [88] |
| Analytical Chemistry Standards | Isotope-labeled internal standards for BPA, phthalates, PFAS; Quality control materials | Precise quantification of EDCs in biological and environmental samples [40] |
| Animal Models | Rodent models (CD-1, Sprague-Dawley); Multi-generational breeding protocols | Assessment of developmental programming; Transgenerational inheritance studies [12] |
| Biomarker Panels | Validated gene expression signatures for ERα and AR activity | Evaluation of pathway-specific activity in exposed populations; Hazard identification [88] |
The identification of vulnerable populations and life stages represents a critical advancement in understanding the impact of EDCs on fertility. The evidence reviewed demonstrates that susceptibility is not uniform but is concentrated during specific developmental windows and among populations with particular genetic, physiological, or exposure characteristics. Future research must prioritize longitudinal studies that capture exposure across critical periods, incorporate multi-omics technologies to elucidate mechanisms, and develop more sophisticated models for assessing mixture effects and low-dose responses.
From a public health perspective, these findings underscore the urgent need for targeted interventions that prioritize protection of the most vulnerable. Regulatory frameworks should incorporate vulnerability considerations when establishing safety standards, with particular attention to early developmental periods where effects may be irreversible and transgenerational. Clinical guidelines for reproductive healthcare providers should include counseling on reducing EDC exposure, especially for patients planning pregnancy or those with existing fertility challenges. By focusing research and policy efforts on identified vulnerable populations and life stages, we can more effectively mitigate the impact of EDCs on human reproductive health now and for future generations.
Dietary and Lifestyle Modifications to Reduce EDC Exposure
Endocrine-disrupting chemicals (EDCs) represent a heterogeneous group of natural or synthetic chemicals that interfere with normal hormonal action, posing a significant concern for reproductive health worldwide [81]. The pervasive presence of these compounds in plastics, cosmetics, pesticides, food packaging, and household products contributes to constant human exposure [81]. For researchers investigating fertility, understanding exposure pathways and implementing reduction strategies is paramount, as evidence from both animal and human studies indicates that EDCs can reduce ovarian reserve, impair oocyte maturation, alter ovulation and implantation, and contribute directly to infertility [81]. Furthermore, associations have been observed with complex reproductive conditions such as polycystic ovary syndrome (PCOS) and endometriosis, along with poorer outcomes in assisted reproductive techniques [81]. This technical guide synthesizes current evidence on dietary and lifestyle interventions to reduce EDC exposure, providing methodologies and frameworks tailored for research and clinical applications focused on preserving fertility.
Key EDCs and Their Mechanisms of Action in Fertility
Major EDCs of Concern
The most studied EDCs with documented effects on reproductive health include bisphenol A (BPA), phthalates, parabens, dioxins, and certain pesticides [81]. These compounds are ubiquitous in modern environments, with consumption of foodstuffs considered one of the principal exposure routes [89]. Alternative exposure pathways include inhalation of chemicals and dermal contact, making comprehensive exposure reduction strategies essential [89].
BPA and its analogues, frequently found in food containers and canned goods, exhibit estrogenic activity that can interfere with the hypothalamic-pituitary-gonadal (HPG) axis [81]. Phthalates, commonly used as plasticizers in PVC and personal care products, have been associated with reduced semen quality in men and ovulatory dysfunction in women [90]. Parabens, used as preservatives in cosmetics and pharmaceuticals, demonstrate estrogenic properties that may affect fetal development when exposure occurs during vulnerable gestational windows [91].
Mechanisms of Endocrine Disruption
EDCs employ multiple mechanisms to disrupt hormonal homeostasis, with particular implications for reproductive function:
- Receptor Interaction: Many EDCs mimic natural hormones by binding to nuclear receptors such as estrogen receptors (ERα and ERβ) and androgen receptors, thereby either activating or blocking transcriptional pathways [81].
- Epigenetic Modulation: Compounds like BPA can alter DNA methylation patterns and histone modifications, potentially leading to transgenerational effects on fertility [81].
- Steroidogenesis Disruption: Several EDCs interfere with the synthesis and metabolism of steroid hormones, notably affecting estradiol and testosterone production critical for reproductive cycling [81].
- HPG Axis Interference: By disrupting the feedback loops between the brain and reproductive organs, EDCs can alter gonadotropin release, affecting ovulation in women and spermatogenesis in men [81].
The following diagram illustrates the primary mechanisms through which EDCs disrupt reproductive endocrine signaling:
Dietary Intervention Strategies
Dietary Modification Protocols
Research indicates that dietary interventions represent some of the most effective strategies for reducing bodily burden of EDCs. A scoping review of intervention studies found that dietary modification or replacement of household goods consistently reduced urinary concentrations of phthalates and phenols [91]. The following table summarizes key dietary intervention approaches and their measured outcomes:
Table 1: Dietary Intervention Studies for EDC Reduction
| Intervention Type | Duration | Population | Key EDCs Measured | Reported Reduction | Primary Reference |
|---|---|---|---|---|---|
| Dietary modification (mostly homegrown/organic) | 3 days - 6 months | Healthy adults, families | BPA, phthalate metabolites | Significant decrease (11 of 13 studies) | [91] |
| Mostly homegrown produce consumption | Not specified | Pregnant OOM women | BPA, MEHP, MiBP, MEP | Significantly lower vs. NHANES participants | [92] |
| Vegetarian diet | 5 days | "Temple Stay" participants | Phthalate metabolites | Significant reduction | [92] |
| Fresh food focus, reduced processing | Not specified | General population | BPA, phthalates, PFAS | Recommended strategy | [93] |
Experimental Protocol: Dietary Intervention Study
For researchers designing dietary intervention trials to assess EDC reduction, the following protocol provides a methodological framework:
Objective: To determine the efficacy of a dietary intervention in reducing urinary concentrations of non-persistent EDCs (phthalates, phenols, parabens) in reproductive-age adults.
Participant Selection:
- Recruit reproductive-age adults (18-45 years), stratified by sex
- Target sample: Minimum 25 participants per group to detect 25% difference in metabolite concentrations with 80% power
- Exclusion criteria: Chronic medical conditions, medication known to affect endocrine function
Intervention Design:
- Provide comprehensive dietary replacement focusing on organic produce, minimally processed foods, and fresh alternatives to canned and packaged items
- Replace plastic food containers with glass or stainless-steel alternatives
- Expose participants to the intervention for a minimum of 5 days, with longer interventions (3-6 months) recommended for assessment of sustained reduction [91]
Sample Collection and Analysis:
- Collect pre- and post-intervention urine samples (first morning void)
- Store samples at -80°C until analysis
- Analyze using liquid chromatography-electrospray ionization tandem mass spectrometry (LC-ESI-MS/MS) for phthalate metabolites, phenols, and parabens [94]
- Adjust for urinary creatinine to account for dilution
Data Analysis:
- Calculate geometric mean ratios (GMRs) for pre- and post-intervention metabolite concentrations
- Use multivariate regression models adjusting for age, BMI, and other covariates
The experimental workflow for such an investigation can be visualized as follows:
Lifestyle and Environmental Modification Strategies
Comprehensive Exposure Reduction
Beyond dietary changes, research indicates that modifications to personal care routines and household environments significantly reduce EDC exposure. A pilot intervention study confirmed that lifestyle modifications implemented by participants led to a significant decrease in both home-related exposure to EDCs and urine concentrations of these chemicals [94]. The Old Order Mennonite (OOM) population study revealed three key practices associated with significantly lower EDC levels: (1) consuming mostly homegrown produce; (2) using no cosmetics and limited personal care products; and (3) transportation primarily by sources other than automobiles [92].
Table 2: Lifestyle Modification Strategies for EDC Reduction
| Intervention Category | Specific Strategies | Targeted EDCs | Evidence Strength |
|---|---|---|---|
| Personal Care Product Use | Eliminate fragranced products; reduce cosmetic use; select natural alternatives | Phthalates, parabens, triclosan | Strong [92] |
| Household Environment | Use natural cleaning products; eliminate plastic furnishings; HEPA filtration | Phthalates, flame retardants, PFAS | Moderate [94] |
| Food Handling & Storage | Replace plastic containers with glass/stainless steel; avoid canned foods; never microwave plastics | BPA, phthalates, other plasticizers | Strong [93] |
| Transportation | Reduce automobile use; increase active transport | Phthalates (car interiors) | Preliminary [92] |
Product Replacement Protocol
For studies investigating the efficacy of product replacement interventions, the following methodology is recommended:
Objective: To determine whether replacing conventional personal care and household products with verified low-EDC alternatives reduces urinary concentrations of target EDCs.
Intervention Components:
- Replace conventional products with alternatives verified to contain no phthalates, parabens, or bisphenols
- Provide participants with glass or stainless-steel water bottles and food containers
- Replace vinyl shower curtains with fabric alternatives
- Substitute conventional cleaning products with vinegar- and baking soda-based alternatives
Outcome Measurement:
- Collect urine samples pre-intervention and at regular intervals during intervention (e.g., 3 days, 1 week, 1 month)
- Analyze for monoethyl phthalate (MEP), methylparaben, propylparaben, and BPA
- Administer product use questionnaires to assess adherence
Implementation Considerations:
- Intervention duration should be sufficient to observe measurable changes; studies with periods of less than ten days have shown effectiveness, but longer interventions may demonstrate more sustained reduction [91]
- Consider participant-centered approaches with meetings and support groups to enhance adherence [90]
The Researcher's Toolkit: Analytical Methods & Reagents
Accurate assessment of EDC exposure requires sophisticated analytical methodologies. The following table details essential research reagents and methodologies used in EDC intervention studies:
Table 3: Research Reagent Solutions for EDC Analysis
| Reagent/Method | Application | Key Features | Example Studies |
|---|---|---|---|
| LC-ESI-MS/MS | Quantification of phthalate metabolites, phenols, parabens in urine | High sensitivity (ng/mL), multi-analyte capability, gold standard for biomonitoring | [94] |
| Creatinine Assay Kits | Urine normalization | Corrects for urine dilution, essential for accurate comparison | [91] |
| Stable Isotope-Labeled Internal Standards | (e.g., 13C-BPA, d4-MEP) | MS quantification accuracy, accounts for extraction efficiency | [92] |
| Solid Phase Extraction (SPE) Cartridges | Sample cleanup and analyte concentration | Reduces matrix effects, improves detection limits | [92] |
| Questionnaires & Exposure Algorithms | Assessment of product use and dietary habits | Identifies exposure sources, complements biomonitoring | [94] |
Implications for Fertility Research and Clinical Applications
The reduction of EDC exposure through dietary and lifestyle modifications holds particular significance for fertility research and clinical practice. Evidence suggests that EDCs may contribute to the increasing prevalence of infertility and reproductive disorders, making exposure reduction a potential preventive strategy [81]. For reproductive-age individuals, especially those in the preconception period, implementing EDC reduction strategies could potentially improve reproductive outcomes.
Future research directions should include:
- Randomized controlled trials specifically designed for reproductive-age populations seeking conception [91]
- Investigation of the temporal relationship between EDC reduction and improvement in fertility biomarkers (e.g., antral follicle count, semen parameters) [90]
- Development of personalized intervention approaches based on individual exposure profiles [91]
- Studies addressing the "cocktail effect" of multiple EDCs and whether reduction interventions can mitigate combined effects [81]
While methodological challenges remain—including variable exposure assessment, lack of standardized biomarkers, and the complexity of real-world EDC mixtures—the current evidence provides a robust foundation for integrating exposure reduction strategies into fertility research and clinical care [81]. As the field advances, collaboration between environmental health scientists, reproductive endocrinologists, and policy makers will be essential to translate these findings into effective interventions that protect and promote reproductive health across populations.
Biomonitoring and Clinical Counseling Strategies for At-Risk Individuals
Endocrine-disrupting chemicals (EDCs) are exogenous substances that interfere with the synthesis, secretion, transport, binding, action, or elimination of natural hormones in the body, thereby disrupting normal endocrine function and contributing to reproductive disorders [1] [95]. The escalating prevalence of unexplained subfertility coincides with increasing environmental exposure to EDCs, establishing biomonitoring and targeted clinical counseling as critical components in managing fertility risks [96]. As the production of synthetic chemicals continues to rise globally, human exposure to EDCs has become almost ubiquitous through diet, air, skin contact, and water [44] [78].
This technical guide examines current biomonitoring methodologies for assessing EDC exposure and provides evidence-based clinical counseling strategies for at-risk individuals. Within the broader context of fertility research, understanding the pathophysiological mechanisms of EDCs is essential for developing effective interventions. Most EDCs exert their effects by competitively binding with hormone receptors, particularly estrogen receptors, thereby initiating adverse biological functions that impact reproductive health across the lifespan [96]. The bioaccumulative nature of many EDCs, along with their potential to produce effects at extremely low exposure levels, creates significant challenges for risk assessment and clinical management [97] [1].
EDCs of Clinical Concern for Reproductive Health
Reproductive function is particularly vulnerable to EDC exposure during critical developmental windows, including in utero development, puberty, and reproductive adulthood [82]. EDCs comprise a diverse group of chemicals used extensively in manufacturing, industrial, and agricultural applications [96]. Table 1 summarizes the primary EDCs associated with reproductive toxicity, their common sources, and key biomonitoring matrices.
Table 1: EDCs with Documented Reproductive Toxicity and Biomonitoring Approaches
| EDC Class | Specific Chemicals | Primary Exposure Sources | Biomonitoring Matrices |
|---|---|---|---|
| Bisphenols | BPA, BPS, BPF | Plastic containers, food can linings, medical equipment, dental sealants | Urine, serum, follicular fluid [96] |
| Phthalates | DEHP, MBzP, MEP, MBP | Personal care products, food packaging, medical tubing, vinyl flooring | Urine, serum, amniotic fluid [82] [96] |
| Persistent Organic Pollutants | PCBs, dioxins, PBDEs | Electrical equipment, flame retardants, industrial byproducts | Serum, adipose tissue, breast milk [97] [78] |
| Perfluorinated Compounds | PFOA, PFOS | Non-stick cookware, stain-resistant fabrics, firefighting foam | Serum [82] |
| Parabens | Methylparaben, ethylparaben | Cosmetics, pharmaceuticals, food preservatives | Urine [82] |
| Pesticides/Herbicides | Atrazine, DDT, glyphosate | Agricultural applications, contaminated food and water | Urine, serum [1] [98] |
| Metals | Lead, cadmium, mercury, arsenic | Contaminated water, food, industrial processes | Blood, urine [82] |
Mechanisms of Reproductive Toxicity
EDCs employ multiple mechanisms to disrupt reproductive function across the hypothalamic-pituitary-gonadal (HPG) axis. Figure 1 illustrates the primary pathways through which EDCs interfere with normal reproductive endocrinology.
Figure 1: Primary Mechanisms of EDC Interference with Reproductive Endocrinology
The molecular interactions depicted in Figure 1 translate to specific clinical reproductive outcomes. In females, EDCs have been associated with diminished ovarian reserve, premature ovarian insufficiency, polycystic ovary syndrome, endometriosis, uterine fibroids, and implantation failure [44] [82]. In males, EDCs contribute to reduced sperm quality and count, cryptorchidism, hypospadias, and altered testosterone levels [82] [78]. The estrogen-mimicking properties of many EDCs, including BPA and triclosan, enable them to interfere with estrogen signaling pathways critical for normal reproductive function [96].
Biomonitoring Strategies for EDC Exposure Assessment
Analytical Methodologies
Biomonitoring represents a critical tool for quantifying internal EDC doses by measuring the chemicals, their metabolites, or reaction products in biological specimens [97]. The selection of analytical methods depends on the specific EDC class, required sensitivity, and available instrumentation. Table 2 outlines the primary analytical techniques employed in EDC biomonitoring.
Table 2: Analytical Methodologies for EDC Biomonitoring
| Analytical Technique | Application | Sensitivity Range | Sample Requirements |
|---|---|---|---|
| Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) | Non-persistent EDCs (bisphenols, phthalates, parabens) | ppt-ppb | Urine (5-10 mL), serum (1-2 mL) [96] |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Persistent organic pollutants (PCBs, PBDEs, OCPs) | ppq-ppt | Serum (3-5 mL), adipose tissue (0.5-1 g) [97] |
| Inductively Coupled Plasma Mass Spectrometry (ICP-MS) | Heavy metals (lead, cadmium, mercury, arsenic) | ppq-ppb | Whole blood (1-3 mL), urine (3-5 mL) [82] |
| Immunoassays (ELISA) | High-throughput screening | ppb | Urine (0.1-0.5 mL), serum (0.1-0.5 mL) [97] |
| High-Performance Liquid Chromatography (HPLC) | Phytoestrogens, steroid hormones | ppb | Serum (1-2 mL), follicular fluid (1-2 mL) [97] |
The choice of biological matrix is critical for accurate exposure assessment. Urine is optimal for non-persistent EDCs with short half-lives, such as BPA and phthalates, while serum or adipose tissue is more appropriate for lipophilic, persistent EDCs like PCBs and PBDEs [97] [96]. Timing of sample collection should consider the pharmacokinetics of target EDCs, with multiple samples often needed to account for variable exposure patterns.
Emerging Biomarkers of Effect
Beyond measuring EDC concentrations, effect biomarkers provide valuable information about the biological responses to EDC exposure. These include:
- Hormone receptor transcriptional activation: In vitro cell-based assays (e.g., ER-CALUX, AR-CALUX) that measure receptor activation potential of serum samples [97].
- Steroidogenesis profiles: LC-MS/MS measurement of steroid hormones in serum or follicular fluid to identify disruptions in hormone production [96].
- Oxidative stress biomarkers: Measurement of 8-hydroxy-2'-deoxyguanosine (8-OHdG) in urine or antioxidant enzymes in blood components [78].
- Epigenetic markers: Analysis of DNA methylation patterns in blood or tissue that may reflect EDC exposure and potential transgenerational effects [82] [78].
Figure 2 illustrates a comprehensive biomonitoring workflow integrating both exposure and effect biomarkers.
Figure 2: Comprehensive Biomonitoring Workflow for EDC Assessment
Clinical Counseling Strategies for At-Risk Individuals
Risk Communication and Exposure Reduction
Effective clinical counseling for individuals at risk for EDC-related reproductive impairment involves clear communication about exposure sources and practical reduction strategies. Key counseling points should include:
- Dietary modifications: Recommend fresh, unpackaged foods over canned or plastic-wrapped alternatives; avoid microwaving food in plastic containers; filter drinking water [1] [95].
- Consumer product selection: Choose fragrance-free personal care products; review ingredient labels for phthalates, parabens, and triclosan; select alternatives to vinyl products [82] [98].
- Home environment interventions: Use wet mopping and vacuuming with HEPA filters to reduce dust containing EDCs; prioritize well-ventilated indoor spaces [78].
- Occupational assessment: Evaluate workplace exposure potential and implement appropriate protective equipment when working with pesticides, plastics, or electronic waste [98].
Preconception counseling represents a critical window for intervention, as reducing EDC exposure before conception may improve reproductive outcomes [96]. Healthcare providers should particularly emphasize the vulnerability of developing reproductive systems to EDCs during embryonic and fetal stages [82].
Interpretation of Biomonitoring Results
Clinicians should be prepared to interpret biomonitoring results within the context of population reference ranges and reproductive risk thresholds. Table 3 presents biomonitoring guidance values associated with adverse reproductive outcomes based on current evidence.
Table 3: Biomonitoring Guidance Values Associated with Reproductive Risks
| Biomarker | Matrix | Population Reference | Level of Concern | Associated Reproductive Effect |
|---|---|---|---|---|
| BPA | Urine | <1 µg/L | >2.5 µg/L [96] | Reduced oocyte yield, fertilization rate [96] |
| DEHP metabolites | Urine | ΣDEHP <50 µg/L | >100 µg/L [96] | Poor embryo quality, lower pregnancy rates [96] |
| PCB-153 | Serum | <10 ng/g lipid | >35 ng/g lipid [97] | Increased time to pregnancy, menstrual cycle irregularities [82] |
| PFOA | Serum | <2 ng/mL | >5 ng/mL [82] | Reduced fecundability, altered steroidogenesis [82] |
| Lead | Blood | <1 µg/dL | >5 µg/dL [82] | Spontaneous abortion, reduced sperm quality [82] |
| Parabens | Urine | <10 µg/L | >50 µg/L [82] | Shorter gestation, altered ovarian function [82] |
When discussing results with patients, clinicians should acknowledge the uncertainties in individual risk prediction, as EDCs typically act as mixture and individual susceptibility varies based on genetic polymorphisms, timing of exposure, and coexisting risk factors [78]. The non-monotonic dose-response relationships of many EDCs complicate risk interpretation, as low doses may have different effects than higher doses [99].
Special Considerations for ART Patients
For individuals undergoing assisted reproductive technology (ART), targeted EDC counseling may improve outcomes. Research demonstrates that specific EDCs measured in follicular fluid correlate with ART success parameters [96]. Clinical strategies for ART patients include:
- Pre-treatment exposure assessment: Consider urinary biomonitoring for phthalates and BPA before initiating ART cycles [96].
- Individualized protocol adjustments: Recognize that EDC exposure may necessitate adjustments to ovarian stimulation protocols in highly exposed individuals [96].
- Lifestyle timing interventions: Implement intensive exposure reduction strategies for at least 3 months before ART cycles to cover spermatogenesis and folliculogenesis windows [96].
Evidence from the EARTH study and other cohorts indicates that urinary BPA concentrations are associated with decreased peak serum estradiol levels, reduced oocyte yield, lower fertilization rates, and impaired embryo quality [96]. Similarly, phthalate metabolites have been associated with decreased implantation, clinical pregnancy, and live birth rates following IVF [96].
Research Gaps and Future Directions
Despite substantial progress in understanding EDC effects on reproduction, significant research gaps remain. Priority areas for future investigation include:
- Mixture effects: Most research examines individual EDCs, yet humans are exposed to complex mixtures that may interact synergistically or antagonistically [78]. Development of robust mixture assessment methodologies is needed.
- Sensitive exposure windows: Better characterization of critical developmental windows for EDC susceptibility across the lifespan would refine risk assessment and timing of interventions [82].
- Biomarker validation: Prospective validation of effect biomarkers for clinical use in predicting reproductive outcomes [97].
- Intervention studies: Controlled studies examining the efficacy of exposure reduction strategies on improving reproductive parameters [96].
- Transgenerational effects: Investigation of potential epigenetic mechanisms and transgenerational inheritance of EDC-induced reproductive impairments [82] [78].
The economic burden of EDC-related reproductive dysfunction provides compelling justification for enhanced research and clinical initiatives. Annual costs of EDC-attributable female reproductive disorders in the EU are estimated at €1.4 billion, with male reproductive disorders costing approximately €4 billion [98].
Biomonitoring and clinical counseling represent essential components of comprehensive care for individuals at risk for EDC-related reproductive impairment. Effective implementation requires integration of exposure assessment methodologies with evidence-based counseling strategies targeting exposure reduction. As research continues to elucidate the complex relationships between EDC exposures and reproductive outcomes, clinical approaches must evolve to incorporate new evidence and technologies.
Reproductive healthcare providers have a critical role in advocating for both individual-level interventions and policy initiatives that reduce population-level EDC exposure. By incorporating EDC assessment and counseling into standard reproductive care, clinicians can contribute to improved reproductive outcomes and potentially reduce the burden of unexplained subfertility associated with environmental chemical exposures.
Validating the Impact: Economic Burden, Regulatory Gaps, and Comparative Analyses
Endocrine-disrupting chemicals (EDCs) are exogenous substances known to interfere with the endocrine system's normal function, contributing to a diverse array of health effects, including infertility and reproductive dysfunction [100]. This whitepaper provides a comprehensive technical analysis quantifying the economic burden of EDC-associated infertility within the European Union and United States, contextualized within the broader scope of impact assessment studies on EDC-related diseases. The analysis synthesizes data from pioneering studies that have established methodology for attributing disease burden and corresponding economic costs to exposure from specific EDCs, including phthalates, bisphenol A (BPA), polybrominated diphenyl ethers (PBDEs), and organophosphate pesticides [101] [102] [103]. These economic valuations are critical for researchers, policymakers, and drug development professionals to prioritize research initiatives and inform regulatory decision-making for public health protection.
Economic Burden of EDC-Associated Disease
Groundbreaking studies have quantified the substantial economic burden resulting from exposure to endocrine-disrupting chemicals, with specific attribution to infertility and other reproductive disorders.
Table 1: Annual Economic Costs of EDC Exposure in the EU and US
| Region | Total Annual Cost | Percentage of GDP | Key EDCs Contributing to Infertility Costs | Primary Methodological Approach |
|---|---|---|---|---|
| European Union | €157 billion (USD $209 billion) [101] [100] [103] | 1.23% [101] [103] | Phthalates, PBDEs [101] | IPCC weight-of-evidence characterization for probability of causation; Delphi method for expert consensus [101] [100]. |
| United States | USD $340 billion [102] [103] | 2.33% [102] [103] | PBDEs, Phthalates, Pesticides [103] | Adaptation of Institute of Medicine approach for attributable disease burden and cost-of-illness [102] [103]. |
These cost estimates encompass multiple health endpoints beyond infertility, including neurobehavioral deficits, obesity, diabetes, and male reproductive disorders [101] [103]. The economic burden includes direct healthcare costs and indirect costs from lost productivity [102]. Notably, these figures are considered conservative, as they represent only those EDCs with the highest probability of causation; a broader analysis would yield greater cost estimates [101].
Specific Costs of Male and Female Reproductive Dysfunction
Expert panels have achieved consensus that several EDCs have a probable (>20%) causation for specific reproductive disorders contributing to infertility [101] [100].
Table 2: EDC-Attributable Male Reproductive Disorders and Associated Costs in the EU
| Health Endpoint | Key Associated EDCs | Attributable Fraction and Evidence Strength | Economic Cost (Annual) |
|---|---|---|---|
| Male Infertility | Phthalates [101] [100] | Probable causation (>20%) based on epidemiological and toxicological evidence [101] | Included in overall male reproductive disorder costs (see below) |
| Cryptorchidism | PBDEs [101] | Probable causation (>20%) [101] | Included in overall male reproductive disorder costs (see below) |
| Mortality from Reduced Testosterone | Phthalates [101] | Probable causation (>20%) [101] | Included in overall male reproductive disorder costs (see below) |
| All Male Reproductive Disorders Combined | Phthalates, PBDEs [101] | Consistent associations across multiple studies [101] [104] [40] | €4.99 billion [103] |
For women, EDC exposure is linked to conditions that severely impact fertility, including uterine fibroids (leiomyomas) and endometriosis [102] [105]. The associated economic costs are substantial, though specific breakdowns for infertility alone within the broader female reproductive disorder costs require further refinement.
Methodological Framework for Burden Assessment
Core Model for Attributable Disease Burden and Costs
The foundational model for estimating the disease burden and costs attributable to environmental exposures, including EDCs, follows the established approach used by the Institute of Medicine and described in Equations 1 and 2 [100]:
- Attributable Disease Burden = Disease rate × Attributable Fraction (AF) × Population size
- Attributable Costs = Disease rate × AF × Population size × Cost per case
The Attributable Fraction (AF) is a critical parameter defined as the proportional reduction in disease cases that would occur if the risk factor exposure were eliminated. It is calculated using the formula [100]:
AF = [Prevalenceexposure × (RR - 1)] / [1 + (Prevalenceexposure × (RR - 1))]
Where RR is the relative risk of morbidity associated with the exposure. This formula was applied consistently in studies of the EU, US, and Canada to ensure comparability [102].
Probability of Causation and Weight-of-Evidence Characterization
A Steering Committee of scientists adapted the Intergovernmental Panel on Climate Change (IPCC) weight-of-evidence framework to evaluate the probability of causation for each EDC-disease pair [101] [100]. This process integrated two streams of evidence:
- Toxicological Evidence: Evaluated using criteria adapted from the Danish Environmental Protection Agency, assessing the strength of evidence for endocrine disruption from laboratory and animal studies [101] [100].
- Epidemiological Evidence: Assessed using adapted WHO Grading of Recommendations Assessment, Development and Evaluation (GRADE) Working Group criteria. This evaluation considered study design, potential bias, limitations, strength of dose-response relationships, residual confounding, and consistency [101] [100].
Expert panels used the Delphi method to reach consensus on the strength of the data and assign probabilities of causation, which were then incorporated into Monte Carlo simulations to account for uncertainty and generate median cost estimates [101] [100].
- Biomonitoring Data: Studies utilized nationally representative human biomonitoring data to determine exposure prevalence. The EU and US analyses used data from the National Health and Nutrition Examination Survey (NHANES), while the Canadian study used the Canadian Health Measures Survey (CHMS) [102].
- Exposure-Response Relationships (ERRs): The core analysis relied on established ERRs from the scientific literature. For male infertility, the relationship with phthalate exposure was a key parameter [101] [102]. The analysis considered multiple EDCs, including PBDEs (linked to testicular cancer and cryptorchidism), and phthalates (linked to male infertility and mortality from reduced testosterone) [101] [102].
- Economic Valuation: A cost-of-illness approach was employed, capturing both direct medical costs and indirect costs such as lost productivity [102]. Costs were calculated based on population and economic data from the same year as the biomonitoring data to ensure consistency.
The following workflow diagram illustrates the complete methodology from evidence evaluation to cost calculation:
Biological Mechanisms and Experimental Models
Mechanisms of EDC Action on Reproductive Function
EDCs interfere with hormonal action through multiple mechanisms, adversely affecting both male and female fertility. Key disruptive actions include [100] [40] [105]:
- Hormone Receptor Interaction: Acting as receptor agonists or antagonists, thereby mimicking or blocking the action of endogenous hormones like estrogens and androgens.
- Altered Hormone Synthesis and Metabolism: Interfering with the synthesis, transport, metabolism, or elimination of natural hormones.
- Epigenetic Modification: Inducing changes in gene expression without altering the DNA sequence, which can have transgenerational effects.
In females, EDCs can target the ovary and disrupt the precise hormonal control of the hypothalamic-pituitary-ovarian (HPO) axis, which governs ovulation [106]. Defects in ovulation account for approximately 30% of all female infertility cases [106]. Epidemiological studies link EDC exposure to impaired fecundity, poorer outcomes in assisted reproductive technology (ART) such as in vitro fertilization (IVF) (including decreased egg yield, pregnancies, and births), and specific disorders like endometriosis and uterine fibroids [104] [40] [106].
In males, substantial evidence supports negative associations between exposure to phthalates, PCBs, and PBDEs and fertility markers [104]. These include adverse effects on semen quality, sperm count and motility, and increased risks of conditions like cryptorchidism and testicular cancer, which are major contributors to male factor infertility [101] [104] [105].
Key Signaling Pathways Targeted by EDCs
The following diagram summarizes the critical hormonal pathways in the female reproductive system that are vulnerable to disruption by EDCs, leading to ovulation defects and infertility:
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for EDC-Infertility Research
| Reagent/Material | Primary Function in Research | Example Application |
|---|---|---|
| Human Biomonitoring Samples (e.g., urine, serum) | Quantifying internal doses of EDCs and metabolites in study populations [102] | Measuring phthalate or BPA levels for correlation with reproductive endpoints [102] [40]. |
| Enzyme-Linked Immunosorbent Assay (ELISA) Kits | Measuring concentrations of reproductive hormones (e.g., LH, FSH, Estradiol, Testosterone, Progesterone) [106] | Assessing hormonal imbalances in cohort studies or animal models following EDC exposure [40] [106]. |
| Primary Granulosa/Theca Cells | In vitro model for studying ovarian follicle function and steroidogenesis [106] | Investigating direct effects of BPA or phthalates on progesterone production and ovulatory mediator expression [106]. |
| LHCGR (LH Receptor) Agonists/Antagonists | Pharmacologically modulating the key receptor initiating the ovulatory cascade [106] | Probing mechanisms of ovulatory disruption in experimental models. |
| Specific EDCs (e.g., BPA, DEHP, PBDEs) | Controlled application in experimental models to establish causality [101] [106] | Administering in animal models to study transgenerational effects or low-dose chronic exposure [104] [106]. |
| RNA Sequencing Reagents | Transcriptomic profiling to identify altered gene expression pathways [106] | Discovering novel pathways disrupted by EDCs in ovarian tissue or testes. |
The economic burden of EDC-associated infertility in the EU and US represents a substantial cost to society and public health, amounting to tens of billions of euros and dollars annually, and is embedded within an even larger burden of disease from EDC exposure overall [101] [103]. The methodological framework established for quantifying this burden provides researchers with a robust tool for ongoing assessment, relying on a weight-of-evidence approach, expert consensus, and comprehensive economic modeling [101] [100]. Future research directions must focus on elucidating the precise mechanisms by which EDCs disrupt ovulation and spermatogenesis, investigating the effects of cumulative "cocktail" exposures, and conducting longitudinal studies to understand the impact of chronic, low-dose exposure throughout the life course [104] [40] [106]. This evidence is critical for strengthening regulatory policies and developing targeted interventions to mitigate the significant economic and public health impact of EDCs on human fertility.
Comparative Analysis of Male vs. Female Reproductive Vulnerabilities to EDCs
Endocrine-disrupting chemicals (EDCs) represent a broad class of exogenous compounds that interfere with normal hormone action, posing significant threats to reproductive health worldwide [107]. The global decline in human fertility rates over the past fifty years coincides with increasing production and environmental dissemination of EDCs, suggesting a potential causal relationship [108] [38]. This technical review provides a comprehensive analysis of the differential vulnerabilities of male and female reproductive systems to EDC exposure, examining exposure pathways, molecular mechanisms, phenotypic outcomes, and transgenerational effects. Understanding these sex-specific vulnerabilities is crucial for researchers, toxicologists, and clinical professionals developing targeted interventions and regulatory policies.
EDC Classes and Exposure Pathways
EDCs encompass diverse chemical compounds with varying properties and environmental persistence. Table 1 summarizes the major EDC classes, their common sources, and primary exposure routes.
Table 1: Major Endocrine-Disrupting Chemicals: Sources and Exposure Pathways
| EDC Category | Specific Compounds | Common Sources | Primary Exposure Routes |
|---|---|---|---|
| Plasticizers | Bisphenol A (BPA), Phthalates (DEHP, DBP) | Food containers, packaging, personal care products, medical devices | Ingestion, dermal absorption [107] [75] |
| Persistent Organic Pollutants | Polychlorinated biphenyls (PCBs), Dioxins, Organochlorine pesticides (DDT) | Industrial processes, environmental contaminants, pesticides | Ingestion (food chain), inhalation [107] [22] |
| Pharmaceuticals & Personal Care Products | Parabens, Triclosan, Ethinylestradiol | Cosmetics, lotions, pharmaceuticals, antimicrobial products | Dermal absorption, ingestion [22] [109] |
| Heavy Metals | Lead, Cadmium, Arsenic | Industrial emissions, contaminated water, food | Ingestion, inhalation [75] |
| Per- and Polyfluoroalkyl Substances (PFAS) | PFOA, PFOS | Non-stick cookware, stain-resistant fabrics, fire-fighting foam | Ingestion, dust inhalation [110] |
Human exposure occurs through multiple pathways, with food intake representing a predominant route for many EDCs due to bioaccumulation and biomagnification within the food chain [22]. Dairy products, fish, meat, and their processed derivatives constitute primary exposure sources in developed countries [22]. Additional exposure occurs via inhalation of contaminated air particles and dermal absorption from personal care products [22] [75].
Critical Exposure Windows
Developmental timing of EDC exposure significantly influences resultant phenotypic severity, with critical windows including:
- In utero development: Germ cell programming and reproductive tract formation [107] [108]
- Early postnatal life: Continued organizational development [38]
- Puberty: Active hormonal maturation and organ development [111] [38]
- Adulthood: Functional maintenance of reproductive systems [104]
The "reproductive programming window" during first-trimester pregnancy represents a particularly vulnerable period for male reproductive development [108].
Molecular Mechanisms of Action
EDCs employ multiple mechanistic pathways to disrupt reproductive function in both sexes, as illustrated in Figure 1 below.
Figure 1: Molecular mechanisms through which EDCs disrupt male and female reproductive function. EDCs act through nuclear receptor signaling, cellular stress pathways, and epigenetic modifications to produce sex-specific adverse outcomes.
Nuclear Receptor Signaling Interference
EDCs directly modulate hormone receptor activity through multiple mechanisms:
- Receptor agonism/antagonism: Compounds like BPA exhibit estrogen receptor (ER) agonist activity, while vinclozolin functions as an androgen receptor (AR) antagonist [107] [111].
- Receptor expression modulation: Altered ER/AR expression patterns in reproductive tissues [75].
- Non-genomic signaling: Rapid membrane-initiated steroid signaling independent of transcriptional regulation [111].
Oxidative Stress and Mitochondrial Dysfunction
EDC-induced reactive oxygen species (ROS) generation represents a common pathogenic mechanism:
- Heavy metals (cadmium, lead) directly induce ROS production, depleting antioxidant defenses [75].
- BPA and phthalates disrupt mitochondrial electron transport chain function, increasing superoxide production [75].
- Resultant oxidative damage to gametes includes sperm DNA fragmentation and oocyte mitochondrial dysfunction [110] [75].
Epigenetic Modifications
Transgenerational effects of EDCs are mediated through epigenetic mechanisms:
- DNA methyltransferase alterations causing hyper/hypomethylation of germline genes [107].
- Histone modifications affecting chromatin accessibility in reproductive cells [107].
- Non-coding RNA expression changes that regulate gene silencing and activation [107].
Male Reproductive Vulnerabilities
Phenotypic Outcomes and Effect Sizes
Male reproductive development and function demonstrate particular vulnerability to EDC exposure. Table 2 summarizes key quantitative findings from experimental and epidemiological studies.
Table 2: Quantitative Effects of EDCs on Male Reproductive Parameters
| Reproductive Parameter | EDC(s) | Effect Size | Experimental Model | Reference |
|---|---|---|---|---|
| Sperm concentration | Phthalate mixture | ↓ 20-30% | Mouse (200 mg/kg/d) | [111] |
| Sperm motility | DEHP | ↓ 15-25% | Human (seminal: 0.77-1.85 μg/mL) | [75] |
| Anogenital distance | DEHP | ↓ 18-22% | Rat (20 mg/kg) | [109] |
| Testosterone levels | Vinclozolin | ↓ 30-40% | Rat (100 mg/kg/d) | |
| Testicular cancer risk | PCB mixtures | ↑ 2.5-fold | Human epidemiological | [108] |
Mechanistic Insights
Male reproductive vulnerabilities stem from several unique aspects of development and physiology:
- Developmental programming: Androgen action during the male programming window (gestational days 8-14 in rats) determines future reproductive capacity [108]. Anti-androgenic EDCs during this window cause irreversible effects.
- Blood-testis barrier permeability: Select EDCs including phthalates and BPA compromise blood-testis barrier integrity, allowing passage of toxicants into the adluminal compartment [75].
- Germ cell susceptibility: Developing germ cells exhibit limited antioxidant defenses and DNA repair capacity, enhancing vulnerability to oxidative insult [75].
The "1% effect" describes the approximately 1% per year increase in male reproductive problems including declining sperm counts, decreasing testosterone, and rising testicular cancer rates in Western countries [108].
Female Reproductive Vulnerabilities
Phenotypic Outcomes and Effect Sizes
Female reproductive system vulnerability to EDCs manifests across the lifespan, from in utero development through menopause. Table 3 summarizes key quantitative findings.
Table 3: Quantitative Effects of EDCs on Female Reproductive Parameters
| Reproductive Parameter | EDC(s) | Effect Size | Experimental Model | Reference |
|---|---|---|---|---|
| Ovarian follicle count | DEHP | ↓ 25-40% | Mouse (0.05-5 mg/kg/d) | [110] |
| Time to pregnancy | PFAS | ↑ 30-40% | Human epidemiological | [110] |
| IVF success rates | PM2.5, NO2 | ↓ 15-20% | Human clinical | [110] |
| Premature menopause | Mix of EDCs | ↑ 2-fold risk | Rat model | [107] |
| Pubertal timing | Atrazine | Accelerated by 5-7 days | Rat (25 mg/kg/d) |
Mechanistic Insights
Female reproductive vulnerabilities reflect the complex endocrine regulation required for normal function:
- Ovarian reserve establishment: EDCs like BPA and phthalates disrupt germ cell nest breakdown and primordial follicle formation during fetal development [38].
- Hypothalamic-pituitary-ovarian (HPO) axis disruption: EDCs alter pulsatile GnRH release, gonadotropin secretion, and steroid feedback sensitivity [111] [38].
- Follicular microenvironment alteration: EDCs impair steroidogenesis, oxidative balance, and nutrient availability within developing follicles [110] [75].
Female reproductive disorders linked to EDC exposure include polycystic ovarian syndrome (PCOS), endometriosis, uterine fibroids, and premature ovarian insufficiency [109] [38].
Transgenerational and Epigenetic Effects
Perhaps the most concerning aspect of EDC exposure is their ability to produce transgenerational effects, defined as phenotypic changes in generations never directly exposed to the EDC (F3 and beyond) [107]. The inheritance patterns differ based on exposure scenario, as detailed in Figure 2.
Figure 2: Transgenerational inheritance patterns following EDC exposure. The F3 generation represents the first unexposed generation when exposure occurs during pregnancy, while the F2 generation is first unexposed when the F0 male or non-pregnant female is exposed.
Epigenetic mechanisms mediate these transgenerational effects, with DNA methylation being the most extensively studied [107]. Specific epigenetic alterations include:
- Differential methylation of imprinted genes and transposable elements in sperm and oocytes [107].
- Histone modifications affecting chromatin structure and gene accessibility in primordial germ cells [107].
- Altered non-coding RNA expression profiles that regulate embryonic development [107].
Transgenerational reproductive effects documented in animal models include ovarian disease, sperm abnormalities, and pubertal abnormalities persisting for multiple generations [107].
Experimental Methodologies
Standardized Testing Guidelines
Regulatory assessment of EDC reproductive toxicity employs standardized OECD test guidelines:
- OECD 421: Reproduction/Developmental Toxicity Screening Test
- OECD 422: Combined Repeated Dose Toxicity Study with Reproduction/Developmental Screening
- OECD 415: One-Generation Reproduction Toxicity Study
- OECD 416: Two-Generation Reproduction Toxicity Study [112]
These tiered testing strategies incorporate in vivo endpoints across critical life stages, with two-generation studies (OECD 416) representing the gold standard for identifying transgenerational effects.
Advanced Mechanistic Protocols
Epigenetic Analysis Workflow
Comprehensive assessment of EDC-induced epigenetic modifications follows this methodological sequence:
- Germ cell isolation via fluorescence-activated cell sorting (FACS) or enzymatic digestion
- DNA extraction and quality verification
- Genome-wide methylation analysis using reduced representation bisulfite sequencing (RRBS) or whole-genome bisulfite sequencing
- Histone modification profiling via chromatin immunoprecipitation sequencing (ChIP-seq)
- Non-coding RNA sequencing for miRNA and lncRNA expression
- Bioinformatic integration of multi-omics datasets
Mixture Toxicity Assessment
Evaluating combined effects of EDC mixtures utilizes specific experimental designs:
- Fixed-ratio mixture designs with constant proportional composition across dose levels
- Ray designs with varying mixture ratios at fixed total concentrations
- Full factorial designs examining all possible combinations of mixture components
Data analysis employs prediction models including Concentration Addition (CA) for compounds with similar modes of action and Independent Action (IA) for dissimilar compounds [22].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for EDC Reproductive Toxicity Studies
| Reagent/Category | Specific Examples | Research Application | Functional Purpose |
|---|---|---|---|
| Animal Models | Sprague-Dawley rats, CD-1 mice, Zebrafish | In vivo toxicity assessment | Model organism for reproductive studies |
| Cell Lines | TM4 (Sertoli cells), GC-1 (spermatogonia), KGN (granulosa) | In vitro mechanistic studies | Cell-type specific response assessment |
| Antibodies | Anti-ERα, Anti-AR, Anti-CYP19A1, Anti-H3K27me3 | Immunohistochemistry, Western blot | Protein localization and quantification |
| Epigenetic Kits | EZ DNA Methylation Kit, EpiQuik Histone Modification Kits | Epigenetic analysis | DNA and histone modification assessment |
| Hormone Assays | ELISA for Testosterone, 17β-Estradiol, AMH, Inhibin B | Endpoint measurement | Hormone level quantification |
| qPCR Arrays | Steroidogenesis, DNA methylation, Oxidative stress pathways | Gene expression profiling | Multi-gene expression analysis |
Research Gaps and Future Directions
Despite significant advances, critical knowledge gaps remain in understanding sex-specific vulnerabilities to EDCs:
- Mixture effects: Most studies examine individual compounds, while human exposure involves complex mixtures with potentially synergistic effects [22] [75].
- Low-dose effects: Non-monotonic dose responses complicate traditional toxicological risk assessment [107] [75].
- Transgenerational human evidence: While animal studies demonstrate transgenerational effects, human epidemiological evidence remains limited [107] [75].
- Metabolic-EDC interactions: The intersection between metabolic status (obesity, rapid weight loss) and EDC toxicity represents an emerging research frontier [110].
Future research priorities should include development of epigenetic biomarkers for early detection of EDC effects, mechanism-based intervention strategies, and integrated testing approaches that better reflect real-world exposure scenarios.
The global decline in fertility rates represents a significant public health challenge, with a growing body of evidence pointing to the role of environmental factors, particularly endocrine-disrupting chemicals (EDCs). EDCs are exogenous substances that interfere with the normal function of the hormonal system, and their pervasive presence in the environment has been linked to a spectrum of reproductive disorders [44]. Establishing a causal link between EDC exposure and human fertility outcomes is methodologically complex, fraught with ethical constraints, long latency periods, and confounding variables. Consequently, the scientific community relies on a weight-of-evidence approach, integrating data from controlled animal models and epidemiological human studies. This whitepaper examines the consistency between these two evidentiary pillars, highlighting key areas of concordance, dissecting methodological protocols, and presenting a toolkit for strengthening future research on the impact of EDCs on fertility.
Key EDCs and Documented Effects on Fertility
Research has consistently identified several classes of EDCs that adversely affect reproductive health in both animal models and humans. These chemicals are characterized by their widespread occurrence and their ability to mimic or block the action of natural hormones, primarily estrogens and androgens.
Table 1: Key Endocrine-Disrupting Chemicals and Their Documented Effects on Fertility
| EDC Class | Common Sources | Primary Mechanisms of Action | Effects in Animal Models | Effects in Human Studies |
|---|---|---|---|---|
| Bisphenols (e.g., BPA) | Plastics, food can linings, receipts [30] | Estrogen receptor agonist/antagonist; alters steroid hormone synthesis [113] [44] | Disrupted oocyte meiosis; reduced blastocyst formation; altered ovarian follicle dynamics [113] | Linked to PCOS, impaired ovarian reserve, implantation failure [30] [86] |
| Phthalates (PAEs) | Personal care products, vinyl flooring, plastics [30] | Anti-androgenic; interferes with hypothalamic-pituitary-gonadal (HPG) axis feedback [30] | Reduced sperm count and motility; reproductive tract malformations [75] | Associated with endometriosis; reduced serum inhibin B; lowered sperm quality [114] [30] |
| Persistent Organic Pollutants (e.g., PCBs, Dioxins) | Pesticides, industrial contaminants, electrical equipment [114] | Alters gonadotropin receptor expression; induces oxidative stress [115] | Impaired follicular dynamics; decreased LH receptor expression in granulosa cells [115] | Linked to premature menopause, endometriosis, and reduced success in IVF [86] |
| Heavy Metals (e.g., Cd, Pb) | Contaminated water, food, industrial emissions [75] | Induces oxidative stress; compromises blood-testis barrier [75] | Accumulates in reproductive tissues; impairs sperm quality and testosterone synthesis [75] | Seminal lead accumulation linked to sperm DNA damage; arsenic disrupts testosterone biosynthesis [75] |
| Parabens | Preservatives in personal care products [114] [30] | Exhibits estrogenic activity [114] | Altered estrogen-responsive gene expression; developmental and reproductive toxicity [114] | Detected in urine; associations with altered menstrual cycle and reproductive hormones [115] |
Experimental Models: Methodologies and Converging Evidence
A critical analysis of experimental approaches reveals how animal and human studies complement each other to build a compelling case for EDC-mediated reproductive toxicity.
Animal Models: Controlled Exposure and Mechanistic Insight
Animal studies, primarily using rodents and non-human primates, provide controlled settings to establish causality and elucidate molecular mechanisms.
- Protocol for Assessing Ovarian Effects: A typical in vivo study involves exposing female mice or rats to environmentally relevant doses of an EDC (e.g., BPA at 0.1-4 µg/kg body weight/day [75]) during critical developmental windows (prenatal, perinatal, or pubertal). Ovarian function is assessed through histological analysis of follicle counts, measurement of atresia (cell death), and evaluation of meiotic abnormalities in oocytes. In vitro models often involve culturing mouse or human granulosa cells with EDCs and measuring hormone production (e.g., progesterone, estradiol) and gene expression of key steroidogenic enzymes (e.g., aromatase) and gonadotropin receptors [113] [115].
Key Findings: These studies have consistently shown that BPA exposure disrupts early oogenesis, leading to meiotic abnormalities and a reduced ovarian reserve [113]. Phthalates like DEHP have been shown to induce PCOS-like symptoms, including follicular cysts and hormonal imbalances in rodent models [86].
Protocol for Assessing Testicular Effects: Male rodents are exposed to EDCs such as cadmium or phthalates. Endpoints include sperm count, motility, and morphology analysis; measurement of serum testosterone and inhibin B levels; and histological examination of the testes for integrity of the seminiferous tubules [75].
- Key Findings: Cadmium exposure reliably impairs the blood-testis barrier and reduces sperm quality, while phthalates are associated with reproductive tract malformations and decreased sperm counts, mirroring trends observed in human populations [75].
Experimental Workflows in EDC Fertility Research
Human Studies: Real-World Exposure and Clinical Relevance
Human research translates findings from the lab to the population level, identifying associations between EDC exposure and clinical fertility outcomes.
- Protocol for Epidemiological Studies: These studies recruit cohorts (e.g., couples seeking infertility treatment or general population samples). Exposure is assessed by measuring EDC metabolites (e.g., BPA-glucuronide, monoethylhexyl phthalate) in urine, blood serum, or follicular fluid using techniques like liquid chromatography-mass spectrometry (LC-MS) [30] [115]. Reproductive outcomes are simultaneously measured, including semen quality parameters, serum hormone levels (e.g., FSH, LH, estradiol, testosterone), ovarian reserve markers (e.g., antral follicle count), and success rates of assisted reproductive technologies (ART) like IVF [114] [86].
- Key Findings: Human studies have confirmed associations between high urinary BPA levels and conditions like PCOS and implantation failure [30]. Phthalate metabolites in urine have been negatively correlated with serum inhibin B (a marker of ovarian follicle health) and sperm quality [30] [75]. Furthermore, EDCs in follicular fluid are linked with poorer IVF outcomes, including fewer mature oocytes and lower fertilization rates [86].
Molecular Mechanisms: A Convergent Pathway from Exposure to Effect
The consistency between animal and human data is underpinned by shared molecular pathways through which EDCs disrupt reproductive function. The hypothalamic-pituitary-gonadal (HPG) axis is a primary target.
EDC Mechanisms Targeting the HPG Axis
The diagram illustrates the core pathways: EDCs disrupt the feedback loops of the HPG axis, leading to altered secretion of GnRH and gonadotropins [44]. Concurrently, they cause direct damage to gonads by binding to hormone receptors (e.g., Estrogen Receptors), inducing oxidative stress, altering critical gene expression via epigenetic modifications, and disrupting the biosynthesis of steroid hormones [115] [75] [44]. These mechanisms explain the observed phenomena in both animal and human studies, such as impaired folliculogenesis, reduced sperm quality, and hormonal imbalances.
The Scientist's Toolkit: Key Research Reagents and Materials
Advancing research in this field relies on a standardized set of reagents and methodologies for exposure assessment and effect analysis.
Table 2: Research Reagent Solutions for EDC Fertility Studies
| Reagent / Material | Function in Research | Specific Application Example |
|---|---|---|
| Certified Reference Standards | Quantification of EDCs and their metabolites in biological samples via LC-MS. | Measuring BPA-glucuronide and monoethylhexyl phthalate (MEHP) in human urine and serum to correlate internal dose with health outcomes [115]. |
| Estrogen/Androgen Receptor Reporter Assays | To screen and confirm the endocrine-disrupting potential of a chemical. | Determining if a novel chemical acts as an agonist or antagonist for the estrogen receptor (ERα/β) in a cell-based luciferase assay [44]. |
| Species-Specific ELISA Kits | Quantify protein biomarkers and hormone levels in serum, plasma, and tissue homogenates. | Measuring changes in LH, FSH, Testosterone, and Inhibin B in rodent serum or human clinical samples following EDC exposure [115] [75]. |
| Primary Cell Culture Systems | For in vitro mechanistic studies without whole-animal complexity. | Culturing human or rat granulosa cells to investigate the direct impact of BPA on progesterone synthesis and LH receptor expression [113] [115]. |
| Antibodies for Steroidogenic Enzymes | Visualize and quantify expression of key proteins in steroidogenesis pathways. | Immunohistochemical staining for enzymes like aromatase (CYP19A1) in ovarian or testicular tissue sections from exposed animals [115]. |
| Epigenetic Analysis Kits | Investigate transgenerational effects and gene regulation mechanisms. | Analyzing DNA methylation patterns in sperm from F3 generation rodents whose ancestors were exposed to vinclozolin [75]. |
The evidence base linking EDC exposure to impaired fertility is robust and consistently reinforced by the triangulation of data from controlled animal models and human observational studies. The concordance spans specific chemical classes, molecular mechanisms—particularly HPG axis disruption and gonadal toxicity—and adverse clinical outcomes such as reduced sperm quality, ovarian dysfunction, and increased incidence of reproductive disorders. However, critical challenges remain. Future research must prioritize the study of complex, real-world mixture exposures rather than single chemicals [75], further investigate the implications of low-dose and non-monotonic dose responses, and validate the potential for transgenerational epigenetic inheritance of reproductive defects in humans [75]. Strengthening this evidence base is paramount for developing informed regulatory policies and effective public health interventions to mitigate the risks posed by these ubiquitous environmental contaminants.
Evaluating Current Regulatory Frameworks (REACH, EPA) and Identifying Gaps
The increasing prevalence of endocrine-disrupting chemicals (EDCs) in the environment has raised significant concerns regarding their impact on human fertility. Robust regulatory frameworks are crucial for identifying hazardous substances, assessing their risks, and implementing measures to protect human health and the environment [48]. The European Union's REACH (Registration, Evaluation, Authorisation and Restriction of Chemicals) regulation and the United States Environmental Protection Agency's (EPA) chemical management programs under the Toxic Substances Control Act (TSCA) represent two major approaches to chemical safety [116]. Within the specific context of fertility research, these frameworks aim to provide the scientific and regulatory foundation for mitigating risks associated with EDCs, which have been implicated in the decline of human fertility over recent decades [104] [48]. This whitepaper evaluates the current status, operational methodologies, and inherent gaps in the REACH and EPA frameworks, providing researchers and drug development professionals with a critical analysis of their effectiveness in addressing the public health challenge posed by EDCs.
Current Regulatory Frameworks: A Comparative Analysis
The REACH Regulation (EU)
REACH operates on the fundamental principle that industry is responsible for managing the risks posed by chemicals and providing safety information on substances [117]. This is achieved through a multi-step process:
- Registration: Industry must register substances manufactured or imported in quantities of one metric ton or more per year with the European Chemicals Agency (ECHA). The required data increases with production volume [117].
- Evaluation: ECHA and member states evaluate the registration dossiers for compliance and can subject substances to further in-depth investigation.
- Authorisation and Restriction: The regulation establishes processes for controlling substances of very high concern (SVHCs), which include carcinogenic, mutagenic, reprotoxic (CMR) substances, as well as those with persistent, bioaccumulative, and toxic (PBT) or very persistent and very bioaccumulative (vPvB) properties [118] [117]. The Authorisation List requires companies to seek permission for the use of SVHCs, while the Restriction List can limit or ban the manufacturing, placing on the market, or use of certain substances [116] [119].
A key feature of REACH is its dynamic nature. The Candidate List of SVHCs is updated biannually, typically in January and June [118]. As of January 2025, five new substances were added, bringing the total to 247 entries [118]. Furthermore, the Restriction List (Annex XVII) is continually amended. For instance, in June 2025, Regulation (EU) 2025/1090 introduced new restrictions on N,N-dimethylacetamide (DMAC) and 1-ethylpyrrolidin-2-one (NEP), both reproductive toxicants, with most applications requiring compliance by December 2026 [119]. A significant recast of REACH is also anticipated by the end of 2025, proposing changes to substance registration and an overhaul of restriction and authorization processes to support the "one substance, one assessment" principle [118].
The EPA and TSCA (US)
The US regulatory framework for chemicals is primarily governed by the Toxic Substances Control Act (TSCA), as updated by the Lautenberg Chemical Safety Act in 2016, and is enforced by the EPA [116]. Key characteristics of this framework include:
- Chemical Evaluation and Management: The EPA's OPPT is mandated to maintain a constant queue of chemical evaluations. Upon completing a high-priority chemical assessment, another must be designated for evaluation, creating a continuously moving compliance target [116].
- Substance Lists: Unlike REACH's tiered approach (Candidate, Authorisation, and Restricted Lists), TSCA maintains a single list of restricted substances and a list of approved substances. There is no sublist of SVHC-equivalent substances; a chemical is generally either allowed or banned [116].
- Enforcement and Penalties: The EPA can issue substantial fines for TSCA violations, up to $50,000 per day of violation, and/or imprisonment for up to one year [116].
Recent developments indicate a shift in the US regulatory landscape. The EPA has moved to eliminate greenhouse gas (GHG) reporting obligations for 46 source categories after the 2024 reporting year and to suspend GHG emissions reporting for select segments within the oil and gas sector until 2034 [120] [121]. This rollback of the Greenhouse Gas Reporting Program (GHGRP) has been criticized for hampering the government's capacity to formulate data-driven climate policy and track progress on emissions reductions [121]. The EPA's Spring 2025 Unified Agenda further outlines its regulatory and deregulatory priorities, emphasizing a focus on streamlining processes [122].
REACH vs. EPA/TSCA: Key Structural Differences
The following table summarizes the core differences between the two regulatory frameworks.
Table 1: Key Comparison Between REACH and EPA/TSCA Frameworks
| Aspect | REACH (EU) | EPA/TSCA (US) |
|---|---|---|
| Core Philosophy | Precautionary principle; industry bears responsibility for proving safety [117] | Risk-based management; EPA bears burden to demonstrate risk for restrictions [123] |
| List Structure | Tiered: Candidate List (SVHCs), Authorisation List, Restricted List [116] | Single list of restricted substances [116] |
| Data Requirements | Tonnage-based; increases with production volume (≥1 ton/year triggers registration) [117] | Prioritization-driven; constant queue of evaluations [116] |
| SVHC/EDC Focus | Explicitly identifies SVHCs, including endocrine disruptors, for authorization [118] [48] | No formal SVHC list; assesses chemicals for risk, which may include endocrine effects |
| Transparency | Public Candidate List and SCIP database for articles containing SVHCs [116] | Less public data; risk assessments and decisions are primarily agency-led |
| Recent Trend | Expanding SVHC list and restrictions; planned recast in 2025 [118] [119] | Reducing reporting requirements (e.g., GHGRP); streamlining regulations [120] [121] |
Identification of Critical Gaps and Challenges
Despite their intended purposes, both regulatory frameworks exhibit significant gaps that hinder a comprehensive understanding and mitigation of EDC-related fertility risks.
Data and Testing Gaps
A fundamental challenge under REACH is the inadequacy of data for low-volume substances. Chemicals produced or imported in volumes below 10 metric tons per year have minimal toxicity testing requirements, leaving potential hazards uncharacterized [117]. This is particularly concerning for EDCs, which may exert effects at very low doses. Furthermore, the validation and adoption of New Approach Methodologies (NAMs), such as in vitro and in silico ((Q)SAR) models, is slow. While intended to reduce animal testing, their application for prioritization and risk assessment under REACH remains flexible and on a case-by-case basis, leading to potential inconsistencies [117]. In the US, the voluntary nature of certain programs, like the former ChAMP initiative, was noted to provide far less protection than REACH's comprehensive and mandatory approach [123].
Regulatory and Policy Gaps
A significant gap in the US system is the divergence in data collection. The recent elimination of GHG reporting for major sources creates a substantial data void, undermining the ability to track environmental pollutants and their sources [120] [121]. While non-governmental actors like the Climate TRACE coalition are attempting to fill this gap, their data lacks the legal authority and standardization of federally mandated collections [121]. Both frameworks also struggle with the "regrettable substitution" problem, where a restricted chemical is replaced by a structurally similar, yet unassessed, analogue with potentially similar hazards. REACH has begun to address this, as seen with the SVHC identification of a reaction mass to prevent such substitutions [118], but it remains a systemic challenge. Finally, the pace of regulatory action is often out of sync with the rapid emergence of new scientific evidence on EDCs, leading to a significant lag between hazard identification and risk management.
Science-Policy Interface Gaps
For EDCs and fertility, a critical gap exists in translating mechanistic and epidemiological findings into regulatory criteria. The complex, non-monotonic dose responses and long-term, multi-generational effects of EDCs are not fully captured by traditional toxicological testing paradigms [104] [48]. While ECHA acknowledges EDCs as SVHCs, the process of formally establishing a substance as an endocrine disruptor for regulatory purposes is complex and protracted. There is also a paucity of specific testing requirements for female fertility endpoints compared to male fertility in many regulatory contexts, a concern raised by researchers who note fewer studies on women for major EDC classes [104].
Methodologies for Research and Regulatory Testing
To support and inform the regulatory frameworks, a robust set of experimental methodologies is employed. The following section outlines key protocols and the requisite tools for investigating the impact of EDCs on fertility.
Key Experimental Pathways and Workflows
Research on EDCs and fertility often follows a multi-tiered approach, progressing from mechanistic studies to whole-organism and human epidemiological investigations. The logical workflow for in vitro and in vivo assessment is depicted below.
Diagram: Logical workflow for EDC fertility assessment, integrating in vitro, in vivo, and human studies.
Detailed Experimental Protocols
In Vitro Steroidogenesis Assay (H295R Cell Line)
This protocol assesses the potential of a test chemical to disrupt the production of steroid hormones, a key mechanism of EDCs.
- Objective: To evaluate the effects of a test chemical on the production of estradiol (E2) and testosterone (T) in the H295R human adrenocortical carcinoma cell line.
- Materials and Reagents:
- H295R cell line (ATCC CRL-2128)
- Dulbecco's Modified Eagle Medium (DMEM)/Nutrient Mixture F-12 Ham, supplemented with 1% ITS+ Premix (Insulin, Transferrin, Selenium)
- 24-well cell culture plates
- Test chemicals dissolved in appropriate solvent (e.g., DMSO, final concentration ≤0.1%)
- ELISA kits for 17β-estradiol and testosterone
- Procedure:
- Cell Seeding and Culture: Seed H295R cells in 24-well plates at a density of 2.5 x 10^5 cells per well in complete medium. Incubate for 24 hours at 37°C in a 5% CO₂ atmosphere to allow cell attachment.
- Chemical Exposure: Replace the medium with fresh medium containing the test chemical at a minimum of five concentrations (e.g., 0.001, 0.01, 0.1, 1, 10, 100 µM). Include a solvent control (0.1% DMSO) and a positive control (e.g., 10 µM Forskolin). Perform each treatment in triplicate.
- Incubation: Expose the cells to the treatment for 48 hours.
- Sample Collection: After 48 hours, transfer the supernatant from each well to microcentrifuge tubes. Centrifuge at 1000 x g for 10 minutes to remove any cellular debris.
- Hormone Analysis: Analyze the supernatant for E2 and T concentrations using commercially available ELISA kits, strictly following the manufacturer's instructions.
- Cell Viability Assessment: Perform a parallel MTT assay on the treated cells to ensure that observed hormonal changes are not due to cytotoxic effects.
- Data Analysis: Hormone levels are normalized to total protein content or cell viability data. Dose-response curves are plotted, and the lowest observed effect concentration (LOEC) and benchmark concentration (BMC) are determined.
In Vivo One-Generation Reproductive Toxicity Study (OECD TG 415)
This guideline provides a foundational in vivo assessment of chemical effects on reproductive function.
- Objective: To evaluate the effects of a chemical on fertility and reproductive performance in a single generation.
- Test System: Typically young adult rats (e.g., Sprague-Dawley). At least 10 males and 20 females per dose group are recommended.
- Procedure:
- Pre-Mating Exposure: Males and females are exposed to at least three dose levels of the test substance and a concurrent control for a pre-defined period (e.g., 10 weeks for males, 2 weeks for females) before mating.
- Mating: Each male is mated with females from the same dose group.
- Gestation and Lactation Exposure: Exposure of females continues throughout gestation and lactation.
- Necropsy and Examination:
- Parents: Assessed for clinical signs, body weight, food consumption, and reproductive organ weights and histopathology.
- Offspring (F1 Generation): Litters are examined for the number of live and dead pups, sex ratio, body weight, and gross visceral abnormalities.
- Endpoints: Mating and fertility indices, gestation length, parturition, litter size and viability, and morphological development of the F1 generation.
The Scientist's Toolkit: Essential Research Reagents
The following table details key materials and reagents used in EDC and fertility research.
Table 2: Key Reagent Solutions for EDC Fertility Research
| Research Reagent / Assay | Function in EDC Fertility Research |
|---|---|
| H295R Cell Line | An in vitro model for screening chemical effects on steroid hormone synthesis (e.g., estradiol, testosterone) [48]. |
| MCF-7 Cell Proliferation Assay (E-Screen) | A bioassay to detect estrogenic activity of chemicals by measuring the proliferation of human breast adenocarcinoma cells. |
| ELISA Kits | Used for quantitative measurement of reproductive hormones (LH, FSH, Estradiol, Progesterone, Testosterone) in serum and cell culture supernatant. |
| siRNA/shRNA for Gene Knockdown | Used to silence specific nuclear receptors (e.g., ERα, ERβ, AR) in cell models to elucidate specific pathways of EDC action. |
| Chromatin Immunoprecipitation (ChIP) Assay | Determines the direct binding of transcription factors or hormone receptors to genomic DNA in response to EDC exposure, revealing epigenetic effects [48]. |
| LC-MS/MS (Liquid Chromatography-Tandem Mass Spectrometry) | The gold standard for sensitive and accurate quantification of EDCs and their metabolites in biological samples (serum, urine, follicular fluid). |
| OECD TG 443 (Extended One-Generation Reproductive Toxicity Study) | A comprehensive guideline for in vivo testing that provides deeper insight into endocrine-sensitive endpoints across life stages. |
| Anti-Müllerian Hormone (AMH) ELISA | Measures AMH levels in serum as a clinical biomarker for ovarian reserve, used in both animal studies and human cohorts. |
The REACH and EPA/TSCA frameworks represent the two most comprehensive chemical management systems globally, yet both exhibit significant gaps in effectively addressing the complex challenge of EDCs and fertility decline. REACH is more proactive in identifying and subjecting SVHCs, including many EDCs, to authorization, but its data requirements for low-volume chemicals and the slow pace of inclusion on authorization lists are limitations. The upcoming REACH recast presents an opportunity to address some of these procedural inefficiencies [118]. In contrast, the EPA's system under TSCA is more reactive, and recent moves to reduce data collection, such as the rollback of the GHGRP, represent a significant step backward in the capacity to inform chemical and environmental health policy [120] [121].
For researchers and drug development professionals, this analysis underscores that regulatory compliance alone is insufficient to ensure chemical safety for reproductive health. The scientific community must drive innovation by:
- Developing and validating more sensitive and specific NAMs that can capture the unique low-dose and non-monotonic effects of EDCs.
- Prioritizing research on female fertility endpoints and the impact of chemical mixtures, which are currently underrepresented in regulatory toxicology.
- Conducting longitudinal human cohort studies with robust biomonitoring to strengthen the epidemiological evidence linking specific EDCs to fertility outcomes [104].
Bridging the identified gaps requires a concerted effort between regulators, scientists, and industry to evolve testing paradigms and regulatory frameworks towards a more preventative and health-protective model. Only through such an integrated approach can we hope to mitigate the impact of EDCs on fertility and safeguard reproductive health for future generations.
The documented global decline in human fertility rates over the past five decades coincides strikingly with increasing environmental contamination by endocrine-disrupting chemicals (EDCs) [124] [38]. These exogenous substances interfere with hormonal signaling pathways crucial for reproductive health, yet our understanding of their specific mechanisms and how to pharmacologically counteract them remains critically incomplete. The complex nature of EDCs—encompassing diverse chemical structures, multiple exposure routes, and potential transgenerational effects—presents extraordinary challenges for conventional drug development paradigms. Current research reveals strong epidemiological associations between EDC exposure and reproductive disorders including diminished ovarian reserve, impaired spermatogenesis, polycystic ovary syndrome (PCOS), and abnormal pubertal development [124] [40] [38]. However, transforming these associations into targeted therapeutic strategies requires systematically addressing fundamental knowledge gaps through prioritized research initiatives. This whitepaper synthesizes current evidence to identify the most critical research voids and proposes structured methodologies to advance the development of interventions that can mitigate or reverse EDC-induced fertility impairments.
Critical Knowledge Gaps in EDC Research and Fertility
Mixture Effects and Real-World Exposure Complexity
Human exposure to EDCs invariably involves simultaneous contact with multiple compounds, yet current toxicological assessments predominantly focus on single-chemical exposures [75]. This simplification fundamentally misrepresents real-world exposure scenarios and limits the predictive value of safety assessments.
Table 1: Key Knowledge Gaps in EDC Mixture Toxicology
| Research Gap | Current Limitation | Impact on Drug Development |
|---|---|---|
| Interactive Effects | Limited data on synergistic/antagonistic interactions between EDCs | Inaccurate risk assessment for pharmaceutical targeting |
| Priority Mixtures | No consensus on which chemical combinations are most prevalent or hazardous | Unable to prioritize research on most relevant exposure scenarios |
| Screening Methods | Lack of high-throughput systems for mixture toxicity assessment | Slow progress in identifying combination effects |
| Dose-Response | Non-monotonic dose responses complicate mixture effect prediction | Difficult to establish therapeutic thresholds |
The "cocktail effect" of multiple EDCs presents particular challenges for understanding cumulative health risks [75]. While substantial evidence supports negative associations between individual chemicals (phthalates, PCBs, PBDEs, pyrethroids, organochloride pesticides) and male fertility, the effects of their combinations remain poorly understood [104]. For female fertility, moderate evidence exists for BPA and PCBs, but mixture effects are virtually unstudied [104]. This gap significantly impedes the development of pharmaceuticals that could address the multifaceted nature of EDC-induced reproductive damage.
Transgenerational Impacts and Epigenetic Mechanisms
Compelling evidence from animal studies demonstrates that EDC exposure can induce heritable epigenetic modifications affecting offspring fertility across multiple generations, but human epidemiological evidence remains limited [14] [75].
Table 2: Transgenerational Research Challenges
| Aspect | Animal Evidence | Human Evidence | Implications for Therapeutics |
|---|---|---|---|
| Epigenetic Mechanisms | DNA methylation changes in germlines | Limited longitudinal studies | Potential for epigenetic-targeted therapies |
| Inheritance Patterns | Effects persist to F3-F4 generations | Case reports only | Requires completely new therapeutic paradigms |
| Windows of Susceptibility | Gestational exposure critical | Inferred from retrospective studies | Missed opportunities for preventive interventions |
| Biomarker Development | Candidate markers identified | No validated biomarkers | Unable to identify at-risk individuals early |
The transmission of EDC-induced reproductive dysfunction across generations occurs through epigenetic mechanisms (DNA methylation, histone modifications, and microRNA expression) mediated through germline modifications [14]. This phenomenon necessitates a fundamental rethinking of therapeutic interventions, as drugs would need to counteract not just direct chemical exposure effects but also inherited epigenetic programming. The extended timeframes required for multigenerational human studies (often exceeding decades) present practical challenges that have limited robust human evidence [75].
Low-Dose and Non-Monotonic Dose Response Effects
EDCs frequently exhibit non-monotonic dose-response (NMDR) patterns, where low-dose chronic exposure may produce more pronounced biological effects than acute high-dose exposure [14] [75]. This phenomenon contradicts traditional toxicological principles that guide pharmaceutical safety testing and therapeutic dose establishment.
Reported no observed adverse effect levels (NOAELs) for common EDCs vary by 2-3 orders of magnitude across studies, reflecting differences in metabolic processing, genetic susceptibility, and methodological approaches [75]. The European Food Safety Authority recently lowered the temporary tolerable daily intake for BPA to 0.2 ng/kg/day, reflecting heightened concern about low-dose effects [14]. This NMDR phenomenon complicates the establishment of therapeutic windows for pharmaceutical interventions and necessitates completely new approaches to dose-finding studies for drugs targeting EDC effects.
Proposed Experimental Methodologies to Address Research Gaps
Comprehensive Mixture Toxicity Screening Protocol
Objective: Systematically evaluate combined effects of prevalent EDC mixtures on reproductive endpoints to identify priority combinations for pharmaceutical targeting.
Workflow:
- Mixture Selection: Prioritize chemicals based on exposure prevalence data from biomonitoring studies (e.g., NHANES). Initial mixtures should include: BPA (4.2 µg/kg/day), phthalates (1-20 µg/kg/day), PFAS, and organochlorine pesticides [75].
- Dosing Strategy: Implement environmentally relevant concentrations reflecting human exposure levels, with special attention to low-dose ranges (0.1-10 µg/kg/day) that may demonstrate NMDR effects.
- In Vitro Screening:
- Utilize high-throughput platforms (e.g., Tox21) to screen mixture effects on 14 receptors critical for reproductive function: AhR, AR, CAR, ER-α, FXR, GR, PPAR-γ, PPAR-δ, PR, PXR, RAR, RXR, TR, and VDR3 [125].
- Apply conformal prediction (CP) frameworks to handle data imbalance and assess prediction uncertainty during screening [125].
- Implement clustering methods (t-SNE and Tanimoto similarity) to identify compounds with potential endocrine activity using known endocrine disruptors as reference [125].
- In Vivo Validation:
- Animal models: Expose during critical developmental windows (gestational, pubertal) and assess transgenerational effects (F0-F3 generations).
- Endpoints: Ovarian reserve (AMH, follicular count), spermatogenesis (sperm count, motility, morphology), hormone levels (testosterone, estradiol, LH, FSH, inhibin B), and epigenetic markers [124] [104] [126].
- Data Integration: Use bioinformatic approaches to identify common pathways and molecular initiating events (MIEs) for targeted drug development.
Transgenerational Study Design for EDC Effects
Objective: Establish causal relationships between EDC exposure and heritable fertility impairments and identify reversible epigenetic modifications for therapeutic targeting.
Methodology:
- Exposure Paradigm:
- F0 Generation: Expose during gametogenesis and continue through mating.
- Generational Tracking: Monitor F1 (direct exposure in utero), F2 (germline exposure), and F3 (first non-exposed generation) for true transgenerational effects [14].
- Epigenetic Profiling:
- Perform whole-genome bisulfite sequencing on sperm and oocytes from each generation.
- Conduct chromatin immunoprecipitation (ChIP-seq) for histone modifications in reproductive tissues.
- Analyze small non-coding RNA expression in germ cells.
- Reproductive Phenotyping:
- Male: Semen analysis (count, motility, morphology), testosterone levels, testicular histology.
- Female: Ovarian reserve (AMH, follicular counts), estrous cyclicity, hormone levels (estradiol, FSH, LH), ovarian histology.
- Intervention Trials: Test epigenetic-modifying compounds (DNMT inhibitors, HDAC inhibitors) and antioxidant therapies for their ability to reverse transgenerational effects.
Low-Dose and Non-Monotonic Dose-Response Characterization
Objective: Establish reliable testing frameworks for low-dose EDC effects to inform therapeutic threshold development.
Protocol:
- Dose Selection: Include at least 8 dose levels spanning environmental exposure ranges (0.01-100 μg/kg/day) with emphasis on low-end concentrations.
- Exposure Timing: Critical developmental windows (embryonic, pubertal) versus adult exposure.
- Endpoint Measurement:
- Reproductive outcomes: Time to pregnancy, litter size, gamete quality.
- Hormonal measures: LC-MS/MS for steroid hormones, LC-MS/MS for peptide hormones.
- Molecular analyses: Receptor expression, steroidogenic enzyme activity, oxidative stress markers.
- Statistical Approaches: Implement specialized models for NMDR curve fitting and benchmark dose analysis.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for EDC Fertility Research
| Reagent/Platform | Function | Application Examples |
|---|---|---|
| Tox21 qHTS Assays | High-throughput screening of 10,000+ compounds | Profiling activity across 14 endocrine receptors [125] |
| Conformal Prediction (CP) Framework | QSAR modeling with uncertainty assessment | Predicting endocrine activity with defined confidence levels [125] |
| LC-MS/MS Systems | Sensitive quantification of EDCs and hormones | Measuring BPA, phthalates, steroids in biological samples [40] |
| Epigenetic Editing Tools (CRISPR-dCas9) | Targeted DNA methylation/demethylation | Validating causal epigenetic modifications [14] |
| Multi-Generational Animal Models | Transgenerational effect assessment | Studying F0-F3 inheritance of EDC effects [14] |
| Organ-on-Chip Platforms | Human-relevant in vitro modeling | Reproductive tissue mimetics for toxicity screening |
Visualizing EDC Signaling Pathways and Experimental Outcomes
Bridging the critical knowledge gaps in EDC research requires a coordinated, multidisciplinary approach that integrates advanced computational methods, sophisticated experimental models, and comprehensive translational frameworks. The highest research priorities should include: (1) developing high-throughput screening platforms for EDC mixtures that reflect real-world exposure scenarios; (2) establishing validated epigenetic biomarkers for identifying at-risk individuals and monitoring intervention efficacy; (3) creating standardized testing guidelines that account for non-monotonic dose responses and sensitive developmental windows; and (4) implementing longitudinal human cohorts to track transgenerational effects. By systematically addressing these research voids through the methodologies outlined in this whitepaper, the scientific community can accelerate the development of targeted pharmaceuticals and interventions to combat the growing threat of EDC-induced infertility. The urgency of this research agenda cannot be overstated, given the pervasive nature of EDC exposure and its potentially irreversible impacts on human reproductive health across generations.
Conclusion
The body of evidence unequivocally establishes that exposure to endocrine-disrupting chemicals represents a significant threat to human fertility, with demonstrated effects on sperm quality, ovarian function, and hormonal balance through diverse and complex mechanisms. The economic burden, estimated in the hundreds of billions of dollars, underscores the profound public health implications. Future research must prioritize longitudinal studies to assess lifelong and transgenerational effects, develop robust methodologies to evaluate chemical mixtures, and elucidate epigenetic pathways. For biomedical and clinical research, this translates into an urgent need to integrate EDC exposure as a factor in fertility diagnostics, advocate for stronger chemical regulation grounded in the precautionary principle, and explore therapeutic interventions that can mitigate or reverse the adverse effects of these pervasive environmental contaminants.
References
- 1. Endocrine Disruptors | National Institute of Environmental Health Sciences [https://www.niehs.nih.gov/health/topics/agents/endocrine]
- 2. of bisphenol A and its analogs as Mechanisms disruptors... endocrine [https://link.springer.com/article/10.1007/s00204-025-04025-z]
- 3. The Endocrine Disruptor Bisphenol A ( BPA ) Exerts a Wide Range of... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6864600/]
- 4. Endocrine disruptors and female fertility: a review of pesticide and plasticizer effects - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9250118/]
- 5. Common EDCs and Where They Are Found | Endocrine Society [https://www.endocrine.org/topics/edc/what-edcs-are/common-edcs]
- 6. (PDF) Regulatory identification of BPA as an endocrine disruptor... [https://www.academia.edu/96696968/Regulatory_identification_of_BPA_as_an_endocrine_disruptor_Context_and_methodology]
- 7. Frontiers | Impact of phthalate exposure on gestational diabetes... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1638655/full]
- 8. PFAS in water environments: recent progress and challenges in monitoring, toxicity, treatment technologies, and post-treatment toxicity | Environmental Systems Research | Full Text [https://environmentalsystemsresearch.springeropen.com/articles/10.1186/s40068-025-00411-9]
- 9. Environmental Factor - August 2025: New Superfund Research Program Center to examine PFAS, liver disease [https://www.niehs.nih.gov/news/factor/2025/8/feature/2-feature-pfas-superfund]
- 10. Molecular mechanism(s) of endocrine - disrupting and their... chemicals [https://pmc.ncbi.nlm.nih.gov/articles/PMC3823132/]
- 11. Endocrine disruptor - Wikipedia [https://en.wikipedia.org/wiki/Endocrine_disruptor]
- 12. The impact, mechanisms and prevention strategies of environmental... [https://pubmed.ncbi.nlm.nih.gov/41103656/]
- 13. Impact of Endocrine Disrupting Chemicals (EDCs) on Reproductive ... [https://link.springer.com/article/10.1007/s12595-021-00412-3]
- 14. Frontiers | Intergenerational and transgenerational effects of... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1571689/full]
- 15. Impact of Chemical Endocrine Disruptors and Hormone Modulators on the Endocrine System - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145289/]
- 16. Prediction of Endocrine-Disrupting Chemicals Related to Estrogen, Androgen, and Thyroid Hormone (EAT) Modalities Using Transcriptomics Data and Machine Learning [https://www.mdpi.com/2305-6304/12/8/541]
- 17. Endocrine disrupting chemicals targeting estrogen receptor signaling: Identification and mechanisms of action - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3119362/]
- 18. Estrogen Receptor Alpha - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/estrogen-receptor-alpha]
- 19. 37 Disorders of the hypothalamic-pituitary-gonadal axis [https://clinical-laboratory-diagnostics.com/k37.html]
- 20. Hypothalamic-Pituitary-Ovarian Axis Disorders Impacting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6466056/]
- 21. Current approaches to overcome the side effects of GnRH ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8940613/]
- 22. Reproductive toxicity of combined effects of endocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10214012/]
- 23. Editorial: Endocrine disrupting chemicals in reproductive ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1478655/full]
- 24. Identification of biomarkers and outcomes of endocrine ... [https://www.sciencedirect.com/science/article/pii/S0300483X23000100]
- 25. The use of hormonal contraceptives in fertility treatments [https://www.asrm.org/practice-guidance/practice-committee-documents/the-use-of-hormonal-contraceptives-in-fertility-treatments-a-committee-opinion-2024/]
- 26. Oral Gonadotropin-Releasing Hormone Antagonists in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12239828/]
- 27. Consensus on the key characteristics of endocrine-disrupting chemicals as a basis for hazard identification | Nature Reviews Endocrinology [https://www.nature.com/articles/s41574-019-0273-8]
- 28. Impact of lisinopril on cisplatin-induced inflammation, oxidative ... stress [https://link.springer.com/article/10.1007/s00210-025-03924-3]
- 29. Latest Science Shows Endocrine Disrupting Chemicals in Plastics, Pesticides, and Other Sources Pose Health Threats Globally | Endocrine Society [https://www.endocrine.org/news-and-advocacy/news-room/2024/latest-science-shows-endocrine-disrupting-chemicals-in-pose-health-threats-globally]
- 30. Frontiers | Role of personal care products as endocrine disruptors... [https://www.frontiersin.org/journals/reproductive-health/articles/10.3389/frph.2025.1514060/full]
- 31. What are Endocrine-Disrupting Chemicals? | Plastic Pollution Coalition [https://www.plasticpollutioncoalition.org/blog/2025/4/21/what-are-endocrine-disrupting-chemicals]
- 32. Opinion | The Male Fertility Crisis Is Environmental - The New York... [https://www.nytimes.com/2025/08/12/opinion/freeze-sperm-infertility-chemicals.html]
- 33. Epigenetics - Wikipedia [https://en.wikipedia.org/wiki/Epigenetics]
- 34. Frontiers | Epigenetic Inheritance: Concepts, Mechanisms and Perspectives [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2018.00292/full]
- 35. - Wikipedia Transgenerational epigenetic inheritance [https://en.wikipedia.org/wiki/Transgenerational_epigenetic_inheritance]
- 36. : myths and Transgenerational ... Epigenetic Inheritance mechanisms [https://pmc.ncbi.nlm.nih.gov/articles/PMC4020004/]
- 37. - Endocrine & Disrupting Health - PMC Chemicals Reproductive [https://pmc.ncbi.nlm.nih.gov/articles/PMC6701840/]
- 38. - Endocrine and female reproductive health... disrupting chemicals [https://orbit.dtu.dk/en/publications/endocrine-disrupting-chemicals-and-female-reproductive-health-a-g]
- 39. Easy Targets: How Endocrine - Disrupting Affect... Chemicals [https://endocrinenews.endocrine.org/easy-targets-how-endocrine-disrupting-chemicals-affect-reproductive-endocrinology/]
- 40. Associations Between Endocrine - Disrupting Exposure and... Chemical [https://pmc.ncbi.nlm.nih.gov/articles/PMC12299029/]
- 41. Molecular mechanisms of transgenerational epigenetic inheritance [https://www.nature.com/articles/s41576-021-00438-5?error=cookies_not_supported&code=b1f3be1b-29ae-49dc-a578-1519acaae3a4]
- 42. Guidelines to evaluate human for quantitative... observational studies [https://pubmed.ncbi.nlm.nih.gov/19079723/]
- 43. Environmental Endocrine Disruptors: Effects on the human male reproductive system - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4803593/]
- 44. Frontiers | The adverse role of endocrine disrupting chemicals in the reproductive system [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1324993/full]
- 45. Data Analysis and Visualization - Research Data Management - LibGuides at Texas State University [https://guides.library.txstate.edu/research-data/analysis-visualization]
- 46. The Use of Biomonitoring Data in Exposure and Human Health Risk Assessments - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1665402/]
- 47. chemicals exposure and female Endocrine ... disruptor fertility [https://pmc.ncbi.nlm.nih.gov/articles/PMC11672798/]
- 48. Frontiers | Endocrine disruptor chemicals exposure and female fertility declining: from pathophysiology to epigenetic risks [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2024.1466967/full]
- 49. Association of urinary phthalate metabolite concentrations with body... [https://ehjournal.biomedcentral.com/articles/10.1186/1476-069X-7-27]
- 50. Implementation of effect biomarkers in human biomonitoring studies: A systematic approach synergizing toxicological and epidemiological knowledge - PubMed [https://pubmed.ncbi.nlm.nih.gov/36841007/]
- 51. Frontiers | Tributyl phosphate as a type of environmental endocrine ... [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1623830/full]
- 52. Human urinary excretion of non-persistent environmental chemicals ... [https://pubmed.ncbi.nlm.nih.gov/24395915/]
- 53. Reducing Exposures to Endocrine Disruptors (REED) study... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-024-08627-3]
- 54. Sperm DNA fragmentation index: limited effectiveness on predicting... [https://rbej.biomedcentral.com/articles/10.1186/s12958-025-01345-8]
- 55. parameters according to the World Health Organisation... Semen quality [https://www.institutobernabeu.com/en/blog/semen-quality-parameters-according-to-the-world-health-organisation-who/]
- 56. threatens Endocrine - Press... - UNIGE disruptors semen quality [https://www.unige.ch/communication/communiques/en/2021/les-perturbateurs-endocriniens-menacent-la-qualite-du-sperme]
- 57. SART: Patient Evaluation [https://www.sart.org/patients/sart-patient-evaluation/]
- 58. Application of machine learning to predict the inhibitory activity of organic chemicals on thyroid stimulating hormone receptor - PubMed [https://pubmed.ncbi.nlm.nih.gov/35351457/]
- 59. in Light of Endocrine : The Challenges of... Disruption DOHaD [https://www.frontiersin.org/research-topics/18355/endocrine-disruption-in-light-of-dohad-the-challenges-of-contaminants-of-emerging-concern-in-food-and-water/magazine]
- 60. Environmental factors, epigenetics, and developmental origin of... [https://pubmed.ncbi.nlm.nih.gov/27421580/]
- 61. Impact of endocrine (EDCs) on epigenetic... disrupting chemicals [https://rbej.biomedcentral.com/articles/10.1186/s12958-025-01413-z]
- 62. - Endocrine and reproductive health: with focus... disrupting chemicals [https://pubmed.ncbi.nlm.nih.gov/40339696/]
- 63. and Endocrine in Males | IntechOpen Disruptors Reproductive Health [https://www.intechopen.com/chapters/62177]
- 64. Human Reproduction : Target of Endocrine Disruptors [https://biomedres.us/fulltexts/BJSTR.MS.ID.003288.php]
- 65. Frontiers | Transgenerational Effects of Endocrine ... Disrupting [https://www.frontiersin.org/research-topics/66885/transgenerational-effects-of-endocrine-disrupting-chemicals-unraveling-hormonal-and-health-impacts-across-generations]
- 66. Frontiers | Endocrine disrupting chemicals and male fertility: from physiological to molecular effects [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2023.1232646/full]
- 67. disruptors and asthma-associated Endocrine in consumer... chemicals [https://pubmed.ncbi.nlm.nih.gov/22398195/]
- 68. The role of endocrine disruptors in female infertility - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10374778/]
- 69. Endocrine disrupting chemicals: exposure, effects on human health, mechanism of action, models for testing and strategies for prevention - PubMed [https://pubmed.ncbi.nlm.nih.gov/31792807/]
- 70. Maternal occupational exposure to endocrine - disrupting ... chemicals [https://dspace.library.uu.nl/handle/1874/431676]
- 71. Nonmonotonic Dose – Response Curves Occur in Dose Ranges That... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6137554/]
- 72. Non-Monotonic Dose Responses in Studies of Endocrine Disrupting Chemicals: Bisphenol A as a Case Study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4036398/]
- 73. Hormones and endocrine - disrupting : chemicals - low ... dose effects [https://pubmed.ncbi.nlm.nih.gov/22419778/]
- 74. Nonmonotonic dose-response relationships: mechanistic basis, kinetic modeling, and implications for risk assessment - PubMed [https://pubmed.ncbi.nlm.nih.gov/14600281/]
- 75. Frontiers | The impact, mechanisms and prevention strategies of... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1573526/full]
- 76. Opinion on the impact of non - monotonic on... dose responses [https://orbit.dtu.dk/en/publications/opinion-on-the-impact-of-non-monotonic-dose-responses-on-efsas-hu/]
- 77. Low dose effects and non-monotonic dose responses for endocrine active chemicals: science to practice workshop: workshop summary - PubMed [https://pubmed.ncbi.nlm.nih.gov/23932820/]
- 78. Frontiers | Reproductive toxicity of combined effects of endocrine disruptors on human reproduction [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2023.1162015/full]
- 79. The Chemical Cocktail: new research on mixture effects points to urgent need for action [https://chemtrust.org/chemical-cocktail-mixture-effects/]
- 80. Considering the cumulative risk of mixtures of chemicals – A challenge for policy makers - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3388441/]
- 81. of Impact on female fertility: an update endocrine disruptors [https://pubmed.ncbi.nlm.nih.gov/41180746/]
- 82. Endocrine disrupting chemicals and reproductive disorders in women, men, and animal models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9743013/]
- 83. - Combination Cocktail of effects disrupters - Welcome to... endocrine [https://orbit.dtu.dk/en/projects/cocktail-combination-effects-of-endocrine-disrupters]
- 84. Combined toxicity of endocrine - disrupting : A review chemicals [https://pubmed.ncbi.nlm.nih.gov/33735605/]
- 85. (PDF) Exposure to a Complex Cocktail of Environmental... [https://www.academia.edu/12989086/Exposure_to_a_Complex_Cocktail_of_Environmental_Endocrine_Disrupting_Compounds_Disturbs_the_Kisspeptin_GPR54_System_in_Ovine_Hypothalamus_and_Pituitary_Gland]
- 86. An Account of Endocrine Disruptors' Impact on Women's Reproductive... [https://blog.alor.org/an-account-of-endocrine-disruptors-impact-on-womens-reproductive-health-by-mrs-dr-abigail-knight-florida]
- 87. IN FEMALE FERTILITY | International... ENDOCRINE DISRUPTORS [https://rsglobal.pl/index.php/ijitss/article/view/3648]
- 88. Identification of potential endocrine disrupting chemicals using gene expression biomarkers - PubMed [https://pubmed.ncbi.nlm.nih.gov/31325560/]
- 89. Origin, dietary , and toxicity of exposure - endocrine food... disrupting [https://pubmed.ncbi.nlm.nih.gov/37539203/]
- 90. Lifestyle interventions to reduce endocrine-disrupting phthalate and phenol exposures among reproductive age men and women: A review and future steps - PubMed [https://pubmed.ncbi.nlm.nih.gov/36283156/]
- 91. Interventions on Reducing Exposure to Endocrine Disrupting Chemicals in Human Health Care Context: A Scoping Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9056072/]
- 92. behaviors associated with Lifestyle to exposures endocrine disruptors [https://www.academia.edu/110655965/Lifestyle_behaviors_associated_with_exposures_to_endocrine_disruptors]
- 93. Why Food Chemicals Are a Problem—And How to Reduce Exposure [https://time.com/7272178/are-food-chemicals-dangerous/]
- 94. in daily Changes reduce indoor life to selected exposure ... endocrine [https://pubmed.ncbi.nlm.nih.gov/32558529/]
- 95. - Endocrine (EDCs) | Disrupting Society Chemicals Endocrine [https://www.endocrine.org/patient-engagement/endocrine-library/edcs]
- 96. Endocrine-Disrupting Chemicals (EDCs) and Reproductive Outcomes | SpringerLink [https://link.springer.com/chapter/10.1007/978-3-031-36494-5_8]
- 97. and hormone- Biomonitoring effect biomarkers of... disrupting [https://pubmed.ncbi.nlm.nih.gov/24797035/]
- 98. Endocrine-disrupting chemicals: economic, regulatory, and policy implications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7437819/]
- 99. The regulation of endocrine-disrupting chemicals to minimize their impact on health - PubMed [https://pubmed.ncbi.nlm.nih.gov/37553404/]
- 100. Estimating Burden and Disease Costs of Exposure to Endocrine-Disrupting Chemicals in the European Union - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4399291/]
- 101. Estimating burden and disease costs of exposure to... [https://pubmed.ncbi.nlm.nih.gov/25742516/]
- 102. Exposure to Endocrine Disrupting Chemicals in Canada... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8948756/]
- 103. Disease Burden & Costs Due to Endocrine-Disrupting Chemicals | NYU Langone Health [https://med.nyu.edu/departments-institutes/pediatrics/divisions/environmental-pediatrics/research/policy-initiatives/disease-burden-costs-endocrine-disrupting-chemicals]
- 104. Endocrine disrupting chemicals: Impacts on human fertility and fecundity during the peri-conception period - PubMed [https://pubmed.ncbi.nlm.nih.gov/33385395/]
- 105. Impact of EDCs on Reproductive Systems | Endocrine Society [https://www.endocrine.org/topics/edc/what-edcs-are/common-edcs/reproduction]
- 106. The effects of endocrineâ€disrupting chemicals on ovarian†and ovulationâ€related fertility outcomes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10100123/]
- 107. Transgenerational Effects of Endocrine - Disrupting on... Chemicals [https://pmc.ncbi.nlm.nih.gov/articles/PMC6525581/]
- 108. A likely culprit is hormone- disrupting | Scientific American chemicals [https://www.scientificamerican.com/article/reproductive-problems-in-both-men-and-women-are-rising-at-an-alarming-rate/]
- 109. and Endocrine ... - Illinois Experts disrupting chemicals reproductive [https://experts.illinois.edu/en/publications/endocrine-disrupting-chemicals-and-reproductive-disorders-in-wome-2/]
- 110. Environmental Pollution, Endocrine Disruptors, and Metabolic Status: Impact on Female Fertility—A Narrative Review [https://www.mdpi.com/2673-3897/6/4/37]
- 111. Xenoestrogen - Wikipedia [https://en.wikipedia.org/wiki/Xenoestrogen]
- 112. (PDF) QSAR Models for Reproductive and Toxicity ... Endocrine [https://www.academia.edu/60309289/QSAR_Models_for_Reproductive_Toxicity_and_Endocrine_Disruption_Activity]
- 113. - Endocrine and Female Disrupting | SpringerLink Chemicals Fertility [https://link.springer.com/chapter/10.1007/978-3-319-90823-6_8]
- 114. and reproductive disorders in... Endocrine disrupting chemicals [https://pubmed.ncbi.nlm.nih.gov/34452686/]
- 115. Endocrine disruptors: Unravelling the link between chemical exposure and Women's reproductive health - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0013935123021898]
- 116. A Comparison of New TSCA & REACH | Assent [https://www.assent.com/blog/tsca-vs-reach/]
- 117. Registration, Evaluation, and Authorization of Chemicals (REACH) ... [https://ncbi.nlm.nih.gov/pmc/articles/PMC2831968]
- 118. Compliance Strategies for REACH : Staying Ahead of... | Assent 2025 [https://www.assent.com/blog/reach-compliance-2025-recast-svhcs/]
- 119. Restriction List REACH : Updated (EU) Regulation /1090 2025 [https://www.chemleg.nl/news-en/new-substances-added-to-reach-restriction-list]
- 120. Navigating evolving EPA in regulations | Sphera 2025 [https://sphera.com/resources/blog/navigating-evolving-epa-regulations-in-2025/]
- 121. The EPA Is Ending Greenhouse Gas Data Collection. Who Will Step Up to Fill the Gap? | WIRED [https://www.wired.com/story/the-epa-is-ending-greenhouse-gas-data-collection-who-will-step-up-to-fill-the-gap/]
- 122. Federal Register :: Spring 2025 Unified Agenda of Regulatory and... [https://www.federalregister.gov/documents/2025/09/22/2025-18333/spring-2025-unified-agenda-of-regulatory-and-deregulatory-actions]
- 123. May. 14 - US: EPA 's ChAMP vs . EU's REACH - Nexreg [https://www.nexreg.com/may-14-us-epa-s-champ-vs-eu-s-reach]
- 124. - Endocrine and female reproductive health... disrupting chemicals [https://pubmed.ncbi.nlm.nih.gov/40404936/]
- 125. Predicting Endocrine Using Conformal Prediction... Disruption [https://pmc.ncbi.nlm.nih.gov/articles/PMC9846826/]
- 126. Human exposure to endocrine disrupting chemicals and fertility: A case-control study in male subfertility patients - PubMed [https://pubmed.ncbi.nlm.nih.gov/26292060/]