Endometrial RNA-seq Sample Preparation: Protocols and Best Practices for Reproductive Research
This comprehensive guide details current protocols and methodological considerations for endometrial RNA-seq sample preparation, a critical technique for advancing research in endometrial receptivity, endometriosis, and reproductive disorders.
Endometrial RNA-seq Sample Preparation: Protocols and Best Practices for Reproductive Research
Abstract
This comprehensive guide details current protocols and methodological considerations for endometrial RNA-seq sample preparation, a critical technique for advancing research in endometrial receptivity, endometriosis, and reproductive disorders. Covering foundational principles from tissue collection and preservation to advanced single-cell and spatial transcriptomics applications, it provides researchers and drug development professionals with actionable frameworks for experimental design. The content further addresses key troubleshooting areas such as managing sample heterogeneity and ensuring RNA integrity, and outlines rigorous validation strategies to confirm data fidelity and biological relevance. By synthesizing established and emerging methodologies, this resource aims to enhance reproducibility and drive innovation in women's health research.
Core Principles and Pre-Analytical Planning for Endometrial Transcriptomics
Frequently Asked Questions (FAQs) on Endometrial RNA-seq
Q1: What are the key considerations when choosing between bulk and single-cell RNA-seq for an endometrial study?
A1: The choice depends entirely on your biological question. The table below compares the core features of each technology to guide your experimental design [1].
| Feature | Bulk RNA-seq | Single-Cell RNA-seq (scRNA-seq) |
|---|---|---|
| Resolution | Tissue-level, average gene expression | Individual cell level |
| Best For | Identifying overall transcriptomic signatures, differential expression between patient groups | Uncovering cellular heterogeneity, identifying rare cell types, discovering new cell states |
| Spatial Context | Lost during tissue dissociation | Lost during tissue dissociation |
| Technical Complexity | Lower | Higher, requires specialized equipment and expertise |
| Cost per Sample | Lower | Significantly higher |
| Data Complexity | Lower, standard analysis pipelines | High, requires specialized bioinformatic analysis |
| Example Application | Comparing gene expression in fertile vs. infertile endometrial samples [2] | Identifying distinct stromal, epithelial, and immune cell subpopulations in endometriosis [3] |
Q2: How much endometrial tissue and RNA are typically required for a successful RNA-seq experiment?
A2: Requirements can vary by protocol, but general guidelines are [4] [5]:
- Tissue Amount: Protocols are optimized for amounts ranging from 10 mg to 100 mg of tissue.
- Total RNA Input: Most standard library preparations require a minimum of 100 ng to 1 µg of high-quality total RNA. Many core facilities recommend at least 500 ng for robustness.
Q3: What is the most critical factor for ensuring high-quality RNA-seq results from endometrial biopsies?
A3: RNA Integrity. The quality of the initial RNA sample is the single most important factor [4]. This is objectively measured by the RNA Integrity Number (RIN), determined using an Agilent TapeStation or similar instrument.
- Target RIN: Aim for RIN scores between 7 and 10 for optimal results.
- Sample Consistency: Ensure a narrow range of RIN scores (e.g., within 1-1.5) across all samples in your experiment to avoid misinterpretation of degradation as biological differential expression [4].
Q4: My single-cell experiment revealed fascinating cellular heterogeneity, but I've lost all spatial information. How can I resolve this?
A4: This is a common limitation of scRNA-seq. Spatial Transcriptomics (ST) is the ideal complementary technology [1]. ST maps gene expression data directly onto the two-dimensional coordinates of an intact tissue section. By integrating your scRNA-seq data with ST data, you can deconvolute the spatial spots to localize the specific cell subpopulations you discovered back into their original tissue architecture, revealing spatial niches and cell-cell communication networks [6] [1].
Q5: I am studying the Window of Implantation (WOI). Can RNA-seq be used to assess endometrial receptivity clinically?
A5: Yes. RNA-seq-based assays are being developed and validated for clinical assessment of endometrial receptivity. These tests, known as RNA-seq-based Endometrial Receptivity Tests (rsERT), analyze a specific gene signature to predict the optimal timing for embryo transfer (personalized Embryo Transfer, pET) in patients undergoing assisted reproduction [7]. One study reported a clinical pregnancy rate of 69.7% in cycles guided by this method [7].
Troubleshooting Common Experimental Issues
Problem 1: Low RNA Yield or Quality from Endometrial Biopsy
- Cause & Solution: Endometrial tissue is rich in RNases. Inadequate stabilization post-biopsy leads to rapid degradation.
- Preventative Protocol:
- Immediate Stabilization: Immediately post-collection, place the tissue biopsy in a sufficient volume of RNA stabilization reagent (e.g., RNAlater) [4] [2].
- Rapid Processing: If possible, proceed to RNA isolation immediately. For storage, keep samples at -80°C [5].
- Optimized Isolation: Use a column-based purification kit (e.g., RNeasy) or a combined Trizol-column method for higher purity and yield. Avoid Trizol alone, as it can leave contaminants that inhibit downstream library prep [4].
Problem 2: High Background in Sequencing Data from Ribosomal RNA (rRNA)
- Cause & Solution: Ribosomal RNA can constitute over 80% of total RNA, dominating your sequencing library if not removed.
- Protocol Adjustment:
- rRNA Depletion: Use commercial kits designed to selectively remove ribosomal RNA (e.g., RiboMinus technology) from your total RNA sample. This enriches for mRNA and other non-coding RNAs, allowing for deeper sequencing of the transcriptome [5].
- Quality Control: Always check the success of rRNA depletion using a TapeStation or Bioanalyzer before proceeding to library preparation [4].
Problem 3: Inconsistent Results Between Replicates in a scRNA-seq Experiment
- Cause & Solution: Inconsistency often stems from variations in tissue dissociation and cell handling.
- Standardized Workflow:
- Rapid, Cold Dissociation: Perform tissue dissociation and cell sorting procedures quickly and at low temperatures to minimize stress-induced changes in the transcriptome. One established endometrial protocol completes this within 90 minutes [8].
- Cell Viability: Ensure high cell viability (>90%) post-dissociation to reduce background noise from dying cells.
- Protocol Consistency: Once a dissociation and sorting protocol is established, use it for all samples in a project without variation [4] [8].
Experimental Protocols & Workflows
Standard Bulk RNA-seq Workflow for Endometrial Tissue
Integrated Single-Cell and Spatial Transcriptomics Pipeline
Key Research Reagent Solutions
Essential materials and kits used in endometrial RNA-seq studies, as cited in the literature.
| Reagent/Kits | Primary Function | Example Use Case |
|---|---|---|
| RNAlater (Thermo Fisher) | RNA stabilization for tissue storage | Preserving endometrial biopsies post-collection prior to RNA extraction [2] [7]. |
| miRNeasy / RNeasy Kits (Qiagen) | Total RNA isolation (including small RNAs) | Standardized RNA purification from endometrial tissue for bulk sequencing [2]. |
| RiboMinus Kits (Thermo Fisher) | Depletion of ribosomal RNA (rRNA) | Enriching for non-rRNA transcripts in bulk RNA-seq to increase meaningful sequencing depth [5]. |
| PAXgene Blood RNA Tubes (Qiagen) | RNA stabilization from whole blood | Paired blood collection for miRNA biomarker discovery in endometrial receptivity studies [2]. |
| TruSeq Small RNA Library Prep Kit (Illumina) | Preparation of sequencing libraries for small RNAs | Profiling endometrial and blood miRNome in fertile and infertile women [2]. |
| CD13 / CD9 Antibodies | Fluorescence-activated cell sorting (FACS) | Isolation of live stromal (CD13+) and epithelial (CD9+) cells for single-cell RNA-seq from endometrial biopsies [8]. |
Critical quality control metrics and quantitative findings from key studies.
Table 1: RNA Quality and Input Requirements for Sequencing [4] [5]
| Parameter | Minimum Requirement | Ideal Target |
|---|---|---|
| Total RNA Input | 100 ng | 500 ng - 1 µg |
| RNA Concentration | - | 100-200 ng/µL |
| Purity (A260/280) | >1.8 | ~2.0 |
| Purity (A260/230) | >1.8 | 2.0 - 2.2 |
| RNA Integrity (RIN) | 7 | 7 - 10 |
Table 2: Key Quantitative Findings from Endometrial Transcriptomic Studies
| Study Focus | Key Finding | Quantitative Result |
|---|---|---|
| Endometrial Receptivity (rsERT) | Clinical pregnancy rate with personalized embryo transfer (pET) | 69.7% (in a cohort of 33 cycles) [7]. |
| Endometrial Cancer | Differentially bound ERα sites in tumor vs. normal tissue | 10,292 genomic locations identified (6,488 lost, 3,804 gained in tumors) [9]. |
| Thin Endometrium (TE) | Differentially expressed genes (DEGs) in TE vs. healthy controls | 57 DEGs identified in bulk RNA-seq [10]. |
| Endometriosis | Diagnostic model accuracy using 8 key genes from integrated sequencing | AUC of 1.00 (training) and 0.8125 (validation cohort) [3]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary technical advantages and disadvantages of invasive biopsy versus menstrual effluence for RNA-seq?
| Feature | Endometrial Biopsy | Menstrual Effluence |
|---|---|---|
| Sample Collection | Invasive clinical procedure (e.g., Pipelle, Tao Brush) [11] | Non-invasive, self-collected at home (e.g., tampon, cup) [12] [13] |
| Cell Type Specificity | Enables precise isolation of specific endometrial cell populations (e.g., CD13+ stromal, CD9+ epithelial cells) via FACS [8] | Heterogeneous mix of shed endometrium, immune cells, and microbiota [12] |
| RNA Integrity Challenges | Requires rapid processing (<90 min) at low temperature to minimize transcriptome changes [8] | Contains nucleases from cell lysis; requires preservation buffer for ambient shipping [12] |
| Best Application | Single-cell transcriptome studies, detailed analysis of endometrial cell types [8] | Large-scale longitudinal studies, diagnostic screening, and population-level research [12] |
Q2: Our RNA yields from menstrual effluence are low and degraded. What preservation strategies are critical?
The key is immediate preservation to counteract nucleases released from lysed cells. A standardized system using a preservation buffer (e.g., Norgen Biotek) in the collection jar is essential. This allows RNA to remain stable for up to 14 days at ambient temperature without refrigeration, achieving >97% success rate in sequencing [12]. For cup-based collection, transporting the sample in a refrigerated box with antibiotics and Normocin within 24 hours has also proven effective without significant loss of cell viability or RNA quality [13].
Q3: Can menstrual effluence truly be used for clinical-grade molecular diagnostics?
Yes, validation studies confirm its clinical potential. Exome sequencing on DNA from menstrual effluence showed 100% concordance for single nucleotide variants when compared to matched venous blood [12]. Furthermore, transcriptomic analyses have revealed biologically meaningful patterns, such as impaired decidualization of stromal fibroblast cells in endometriosis patients and cycle-dependent variation in key reproductive and immune markers [12] [13].
Q4: When working with biopsies for single-cell RNA-seq, how is cell viability maintained during processing?
A rapid, cold-handling pipeline is crucial. The entire process from tissue disaggregation to single-cell sorting should be managed within 90 minutes and performed at low temperatures to minimize artifactual changes in the gene expression profile [8].
Troubleshooting Guides
Problem 1: Inadequate or Low-Quality RNA from Endometrial Biopsies
- Potential Cause 1: Delayed sample processing. Transcript degradation begins quickly after tissue collection.
- Solution: Implement a standardized, rapid protocol. Minimize the time from biopsy to preservation or cell dissociation. Keep samples on ice throughout [8].
- Potential Cause 2: Incorrect handling of single-cell suspensions.
- Solution: When sorting specific cell types (e.g., with CD13 or CD9 antibodies), use a fluorescence-activated cell sorter (FACS). Be aware that some epithelial cells (CD9-positive) may have low RNA content and be more susceptible to degradation [8].
Problem 2: High Contamination or Failed Sequencing from Menstrual Effluence
- Potential Cause 1: Bacterial or microbial overgrowth.
- Potential Cause 2: Sample composition variability.
- Solution: Standardize collection by using low-absorbency organic cotton tampons worn for a fixed period (e.g., 4 hours) and collect during specific cycle days (e.g., days 1-3). Capture metadata on flow rate and cycle day for downstream normalization [12].
Problem 3: Inconsistent Endometrial Receptivity (ER) Test Results
- Potential Cause: Incorrect timing of the biopsy in the hormone replacement therapy (HRT) cycle.
Experimental Protocols
Protocol 1: Single-Cell RNA-Seq from Endometrial Biopsies
This protocol is adapted from a foundational methodology for studying the full transcriptome of endometrial stromal and epithelial cells [8].
- Biopsy Collection & Cryopreservation: Obtain endometrial biopsy using a device like Pipelle. Immediately cryopreserve the tissue.
- Tissue Disaggregation: Thaw the frozen biopsy and disaggregate the tissue into a single-cell suspension using a combination of enzymatic and mechanical digestion.
- Cell Staining & Sorting (FACS):
- Incubate the cell suspension with fluorescently-labeled antibodies against cell-surface markers (e.g., CD13 for stromal cells, CD9 for epithelial cells).
- Use a fluorescence-activated cell sorter (FACS) to isolate live, single cells of the desired type into a lysis buffer.
- Library Preparation & Sequencing: Perform single-cell RNA-seq library preparation using a method such as Smart-seq2 for high sensitivity. Sequence the libraries on an Illumina platform.
- Bioinformatic Analysis: Process the raw sequencing data through a pipeline including alignment, gene counting, and statistical analysis to identify differentially expressed genes and cell populations.
Protocol 2: RNA Sequencing from Menstrual Effluence
This protocol is based on a validated, at-home collection system that enables clinical-grade RNA-seq [12].
- At-Home Collection:
- Provide participants with a standardized kit containing an organic cotton tampon and a jar with nucleic acid preservation buffer.
- Instruct participants to use the tampon for a set duration (e.g., 4 hours) during the first few days of menstruation.
- After use, the tampon is sealed in the jar, which releases the preservation buffer upon closing.
- Shipment & Receipt: Participants return the kit via standard mail at ambient temperature.
- Sample Processing:
- Upon receipt in the lab, extrude the tampon and centrifuge the sample to separate cellular material from the liquid fraction.
- Aliquot the cell pellet for storage at -80°C.
- Nucleic Acid Extraction: Extract total RNA using a column-based or magnetic bead-based RNA isolation kit, including a DNase treatment step to remove genomic DNA.
- Library Prep & Sequencing: Prepare RNA-seq libraries using a kit designed for ribodepletion (RiboFree) to enable analysis of both coding and non-coding RNA. Sequence on a platform such as Illumina NextSeq2000.
Research Reagent Solutions
| Item | Function / Application | Example / Note |
|---|---|---|
| Pipelle Biopsy Device | Minimally invasive endometrial tissue sampling for histology and RNA extraction [11] [16] | Gold standard for outpatient biopsy; high patient tolerance. |
| FACS Sorter | Isolation of pure populations of specific endometrial cell types (e.g., CD13+ stromal cells) for single-cell analysis [8] | Enables high-resolution cell-type-specific transcriptomics. |
| CD13 / CD9 Antibodies | Fluorescent labeling for identification and sorting of stromal and epithelial cells, respectively [8] | Critical for population-specific studies. |
| Nucleic Acid Preservation Buffer | Stabilizes RNA and DNA in menstrual effluence during ambient temperature shipment [12] | Enables at-home collection and mailing. |
| RiboFree Total RNA Library Kit | Prepares RNA-seq libraries from ribosomal RNA-depleted total RNA, capturing a broader transcriptome [12] | Ideal for analyzing both coding and non-coding RNA. |
| Norgen Column-Based RNA Kit | Nucleic acid extraction from complex samples like menstrual effluence [12] | Designed to handle challenging samples. |
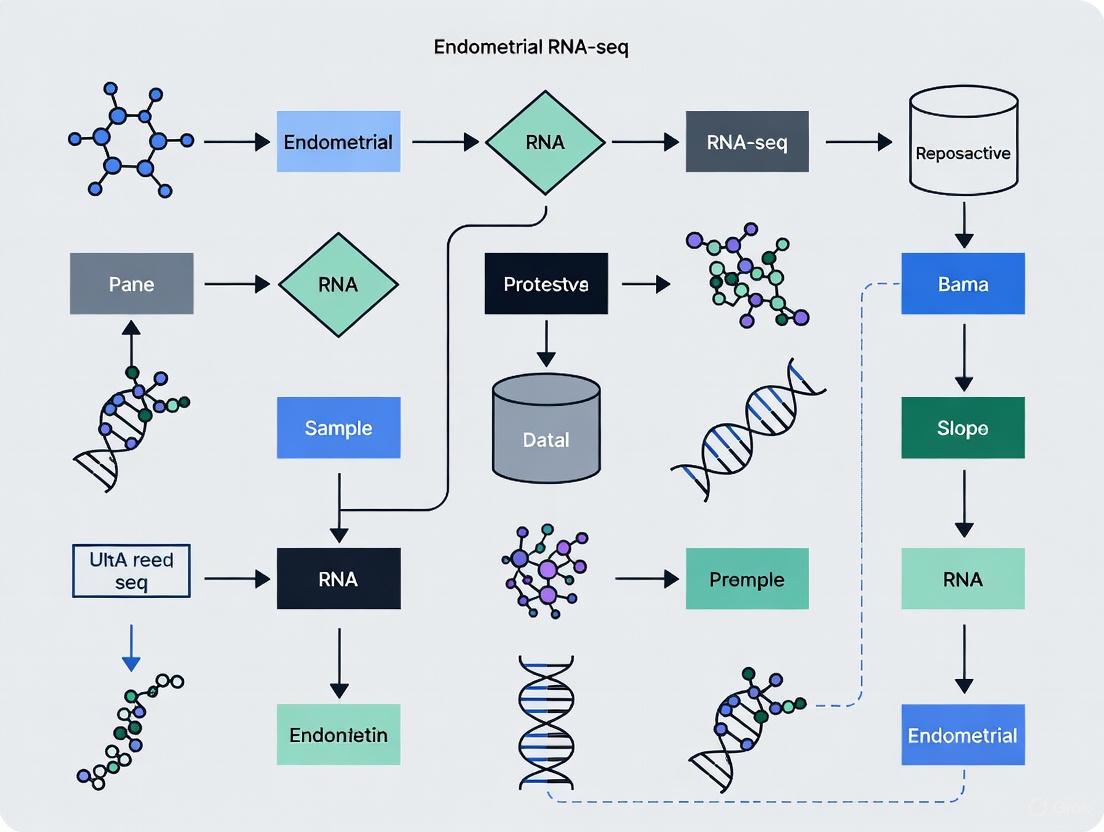
Visual Workflows
Endometrial RNA-seq Collection Pathways
Menstrual Effluence Analysis Workflow
Troubleshooting Guide: Sample Collection & Timing
Q1: What are the most common issues that lead to inaccurate endometrial receptivity (ER) data? The most common issues are sample collection from the incorrect cycle phase and a failure to independently verify receptivity status. Endometrial receptivity is a transient period, and even small displacements in timing can drastically alter the transcriptome [17]. Relying on calendar estimates alone without hormonal or molecular confirmation is a frequent source of error.
Q2: How can I precisely time an endometrial biopsy to the Window of Implantation (WOI)? The standard method for timing a biopsy in a natural cycle is to use the luteinizing hormone (LH) surge as a reference point. The WOI typically occurs on LH+7 to LH+9 [18] [2]. In a hormone replacement therapy (HRT) cycle, the equivalent timing is typically 5 days after progesterone administration (P+5) [17] [15]. It is critical to confirm the LH surge with urine or serum tests rather than estimating from menstrual history [19] [2].
Q3: What methods can I use to confirm the receptivity of my collected samples? Beyond histological dating, it is strongly recommended to use molecular tools to confirm receptivity. Several validated gene expression signatures can classify samples as pre-receptive, receptive, or post-receptive [19] [18] [17]. These tests analyze dozens to hundreds of receptivity biomarker genes and provide an objective status report, which is especially important for patient populations with suspected WOI displacement [17] [15].
Q4: My participant has an irregular cycle. How should I proceed? For women with irregular cycles, conducting the biopsy in a controlled HRT cycle is the most reliable approach. This method bypasses the body's natural hormonal fluctuations by using exogenous estrogen and progesterone, creating a standardized and predictable endometrial timeline [17] [15]. This ensures synchronization across study participants and is particularly useful for women with conditions like PCOS.
Detailed Experimental Protocols
Protocol for LH-Timed Endometrial Biopsy in a Natural Cycle
This protocol is adapted from established studies on endometrial receptivity [19] [18] [2].
- Participant Preparation: Recruit women with confirmed regular menstrual cycles (25-35 days). Participants should not have used hormonal medication for at least three months prior to recruitment.
- LH Surge Detection: Provide participants with urine luteinizing hormone (LH) detection kits (e.g., BabyTime hLH cassette). The first day of a positive test is designated as LH+0.
- Biopsy Procedure: Schedule the endometrial biopsy for LH+7 to LH+9. Perform the biopsy using a Pipelle catheter or similar device.
- Sample Processing:
- Immediately divide the biopsy.
- For RNA/DNA analysis: Rinse the tissue in sterile PBS and snap-freeze in RNAlater or a similar preservative. Store at -80°C.
- For histology/molecular confirmation: Place a portion of the tissue in 10% buffered formalin for standard histological dating or process for RNA to run a receptivity classifier (e.g., beREADY, rsERT) [19] [18].
- Verification: Confirm the receptivity status of all samples using a molecular tool to ensure data integrity [18].
Protocol for Sample Processing for Single-Cell RNA-Seq
Handling samples for single-cell RNA-seq requires extra care to preserve cell viability and RNA quality [20] [21].
- Cell Suspension: Wash and resuspend cells in EDTA-, Mg2+-, and Ca2+-free 1X PBS to prevent interference with downstream enzymatic reactions [20].
- Cell Sorting (FACS): For optimal results, sort single cells directly into a lysis buffer containing an RNase inhibitor. If this is not possible, sort into a minimal volume (<5 µl) of Mg2+/Ca2+-free PBS [20].
- Speed and Temperature: Work quickly to minimize RNA degradation. After cells are deposited into plates, centrifuge them gently and either process immediately or snap-freeze them on dry ice for storage at -80°C [20].
- Confirm Cellular Composition: Use flow cytometry to characterize the proportions of key cell populations (e.g., CD45+ immune cells, CD45-EPCAM+ epithelial cells, CD45-EPCAM- stromal cells) in your sample [21].
Data and Workflow Visualization
Sample Collection Workflow
The following diagram illustrates the critical decision points in the sample collection process to ensure accurate timing.
Synchronizing with the Window of Implantation
This diagram shows the temporal relationship between the LH surge, progesterone rise, and the opening of the WOI.
Table 1: Standardized Timing Parameters for Endometrial Sample Collection
| Cycle Type | Reference Point | Optimal Sampling Window | Key Verification Method |
|---|---|---|---|
| Natural Cycle | LH Surge (LH+0) | LH+7 to LH+9 [18] [2] | Molecular receptivity assay [19] |
| Artificial (HRT) Cycle | Progesterone Start (P+0) | P+5 [17] [15] | Molecular receptivity assay [17] |
Table 2: Key Cell Type Markers for Endometrial Single-Cell Studies
| Cell Type | Surface Protein Markers | Function in Endometrial Receptivity |
|---|---|---|
| Epithelial Cells | EPCAM+ / CD45- [21] | Express osteopontin (SPP1), galectins; direct embryo attachment [19] |
| Stromal Cells | CD45- / EPCAM- [21] | Decidualize; express progestagen-associated endometrial protein (PAEP) [3] |
| Immune Cells | CD45+ [21] | Modulate immune tolerance; include uterine NK cells, macrophages [3] [21] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Endometrial RNA-seq Research
| Reagent / Kit | Function | Example Use Case |
|---|---|---|
| Pipelle Catheter | Minimally invasive endometrial biopsy | Standardized tissue collection from the uterine lumen [19] [2] |
| RNAlater | RNA Stabilization Solution | Preserves RNA integrity in tissue samples during transport and storage [2] |
| PAXgene Blood RNA Tubes | Blood RNA Stabilization | Stabilizes whole blood transcriptome for paired peripheral blood studies [2] |
| TruSeq RNA Library Prep Kits | RNA-seq Library Preparation | Prepares high-quality sequencing libraries from total RNA [18] [2] |
| FACS Sorting Buffers | Cell Sorting and Isolation | Isulating specific cell populations (e.g., epithelial, stromal) for cell-type-specific sequencing [19] [20] |
| miRNeasy Mini Kit | RNA Extraction (incl. small RNA) | Simultaneous purification of large and small RNA species for ceRNA studies [22] [2] |
| Linear PBT Trimer | Linear PBT Trimer|210566-88-4|Research Chemical | |
| MENTHOL, (+)-neo- | MENTHOL, (+)-neo-, CAS:63975-60-0, MF:C10H20O, MW:156.26 g/mol | Chemical Reagent |
In endometrial RNA-seq research, the integrity of your nucleic acid samples is the foundation of reliable data. The unique challenges of working with endometrial tissue, which is rich in RNases, make robust preservation and storage protocols critical from the moment of collection. This guide provides targeted troubleshooting and best practices to ensure nucleic acid stability throughout your experimental workflow, specifically within the context of endometrial research.
The Scientist's Toolkit: Essential Reagents for Endometrial Research
The table below lists key reagents and materials essential for the preservation and processing of endometrial samples for RNA-seq.
Table 1: Key Research Reagent Solutions for Endometrial Nucleic Acid Preservation
| Reagent/Material | Primary Function | Specific Application in Endometrial Research |
|---|---|---|
| RNAlater Stabilization Solution | Immediately permeates tissue to inactivate RNases, stabilizing RNA at the point of collection. [23] | Preservation of endometrial biopsy RNA integrity prior to freezing and RNA isolation. [8] [7] |
| CD13 / CD9 Antibodies | Enable fluorescence-activated cell sorting (FACS) of specific cell populations. [8] | Isolation of pure stromal (CD13+) and epithelial (CD9+) cells from disaggregated endometrial biopsies for single-cell transcriptomics. [8] |
| Deep Eutectic Solvents (DESs) | Novel solvent systems that stabilize nucleic acid structure by forming hydrogen bonds, particularly at A-T base pairs. [24] | Promising alternative for ambient temperature storage of extracted DNA and RNA, maintaining helical structure. [24] |
| Nucleic Acid Preservation Solution | Specialized formulations to stabilize and protect DNA/RNA from degradation during storage/transport. [25] | Enables ambient temperature transport of samples (e.g., from clinic to lab), crucial for multi-site collaborations. [25] |
| 2-Bromo-6-isopropylpyrazine | 2-Bromo-6-isopropylpyrazine|CAS 1086382-94-6 | 2-Bromo-6-isopropylpyrazine (CAS 1086382-94-6) is a brominated pyrazine building block for pharmaceutical and chemical synthesis. For Research Use Only. Not for human or veterinary use. |
| 2,3,4-Trichlorobenzenethiol | 2,3,4-Trichlorobenzenethiol |
Frequently Asked Questions (FAQs) and Troubleshooting
Sample Collection & Initial Stabilization
Q: What is the best practice for preserving an endometrial biopsy intended for RNA-seq immediately after collection? A: Immediate stabilization is non-negotiable. The collected tissue should be submerged in approximately 5 volumes of RNAlater Stabilization Solution within a sterile tube. For thorough permeation, the tissue dimension should ideally be less than 0.5 cm in any direction. This step inactivates RNases, preserving the RNA's quality and quantity until you can proceed with RNA isolation. [23]
Q: I see a precipitate has formed in my RNAlater solution. Has it been compromised? A: A precipitate is common and does not indicate compromise. To redissolve it, heat the solution to 37°C for about 15 minutes and agitate (e.g., by vortexing). Once the solution is clear, it is ready for use. [23]
Storage & Transportation
Q: For how long can I store an endometrial biopsy in RNAlater before RNA extraction? A: RNAlater-treated tissue samples can be stored safely for:
- 1 day at 37°C
- 1 week at 25°C
- 1 month at 4°C
- Indefinitely at -20°C (the tissue does not freeze solid) [23] For long-term biobanking, storage at -80°C is recommended.
Q: Are there alternatives to cold chain logistics for shipping my samples? A: Yes. Using nucleic acid preservation solutions allows for ambient temperature shipping, for example overnight. These specialized formulations are designed to prevent enzymatic degradation and microbial growth without freezing, which was crucial for initiatives like widespread COVID-19 testing. [25]
Sample Processing & Cell Sorting
Q: My RNA yield from sorted endometrial epithelial cells is low. What could be the cause? A: This is a recognized challenge. Epithelial cells can be particularly sensitive. The low yield is often due to:
- High RNase activity released during natural cell processes or disaggregation.
- Apoptotic conditions induced by the enzymes or stresses of the freezing and single-cell suspension process. [8] Ensure the entire disaggregation and sorting workflow is performed as quickly as possible and on ice or at 4°C to minimize RNase activity and transcriptional changes. [8]
Q: Can tissues preserved in RNAlater be used for laser capture microdissection (LCM)? A: While not officially validated by the manufacturer, published evidence suggests it is possible. One study successfully performed LCM on prostate tissue that had been preserved in RNAlater, indicating its potential for this application. [23]
Long-Term Storage of Extracted Nucleic Acids
Q: What are the main risks to extracted DNA and RNA during long-term storage, even when frozen? A: The primary degradations are:
- Hydrolysis: Water molecules break the phosphodiester backbone of nucleic acids.
- Oxidation: Oxygen in the air can damage bases.
- Heat: Accelerates both hydrolysis and oxidation.
- RNases (for RNA): These resilient enzymes are a pervasive threat and can rapidly degrade RNA samples if introduced. [26]
Q: Beyond ultra-low freezers, what are the most reliable methods for long-term nucleic acid storage? A: The field is moving towards ambient temperature storage to overcome the cost and reliability issues of freezers. The following table compares the main alternatives.
Table 2: Comparison of Long-Term Nucleic Acid Storage Methods
| Method | Mechanism | Pros | Cons |
|---|---|---|---|
| Ultra-Low Freezing | Slows degradation and enzymatic activity with extreme cold. | Current gold standard; widely adopted. | High cost; energy-intensive; risk of freezer failure; freeze-thaw cycles cause damage. [26] |
| Additives (e.g., GenTegra) | Form a stabilizing matrix around nucleic acids. | Easy to use; compatible with downstream applications. | Can be rehydrated by ambient moisture, offering limited long-term protection. [26] |
| Encapsulation (e.g., Caching) | Seals nucleic acids in a protective, impermeable shell. | Superior protection; enables ambient storage; allows for non-destructive aliquoting. | Can be costly and difficult to scale depending on the technology. [26] |
| Deep Eutectic Solvents | Hydrogen bonding with DNA base pairs to stabilize structure. | Low toxicity; high stability; tunable properties. | Emerging technology, not yet widely commercialized for this specific use. [24] |
Workflow Visualization
The following diagram illustrates a recommended workflow for collecting and processing endometrial samples for RNA-seq analysis, integrating key stabilization steps to ensure nucleic acid integrity.
Ethical Considerations and Informed Consent in Endometrial Research
FAQs on Informed Consent and Ethics
1. What are the core ethical principles I should consider when designing my endometrial research study? When designing any biomedical research involving human participants, you should ground your study in seven main ethical principles [27]:
- Social and clinical value: The research should answer a question that contributes to scientific understanding or improves health, justifying the involvement of participants and any risks [27].
- Scientific validity: The study must be methodologically sound to yield reliable and useful results [27].
- Fair subject selection: Participant selection should be based on scientific goals, not vulnerability or privilege. Groups should not be excluded without a valid scientific reason [27].
- Favorable risk-benefit ratio: Everything must be done to minimize risks to participants and ensure potential benefits outweigh these risks [27].
- Independent review: The study protocol must be reviewed and approved by an independent ethics committee or Institutional Review Board (IRB) before commencement [27].
- Informed consent: Researchers must obtain voluntary, informed consent from all participants after explaining the study's purpose, methods, risks, and benefits [27].
- Respect for participants: This includes protecting participant privacy, allowing them to withdraw at any time, and monitoring their welfare throughout the study [27].
2. What specific information must be included in the informed consent form for an endometrial biopsy study? The informed consent process is a safeguard for participant autonomy. Based on historical ethical codes and current regulations, your consent form should clearly explain [28]:
- The research procedures: A description of what will be done, including the endometrial biopsy and any other interventions.
- The purpose of the research: Why the study is being conducted.
- Potential risks and benefits: Any foreseeable discomforts (e.g., from the biopsy procedure) and potential direct benefits to the participant or to society.
- Alternative options: For therapeutic research, this would include alternative treatments available to the participant.
- Voluntary participation: A clear statement that participation is voluntary and that the participant can refuse to join or withdraw at any time without penalty.
- Confidentiality: How the participant's data and personally identifiable information will be protected.
3. In endometrial research, when might the requirement for informed consent be waived? Informed consent is a fundamental requirement. However, under strictly regulated conditions for some retrospective studies, a waiver of consent might be granted by an ethics committee. This is typically considered only when [29]:
- The research involves no more than minimal risk to the participants.
- The waiver would not adversely affect the rights and welfare of the participants.
- The research could not practicably be carried out without the waiver.
- Whenever appropriate, participants will be provided with additional pertinent information after participation. It is crucial to consult with your institutional ethics board, as regulations vary by jurisdiction. A study on a retrospective cohort using archived, anonymized samples might receive such a waiver [29].
4. We are using a novel RNA-seq-based Endometrial Receptivity Test (rsERT). What specific ethical considerations does this introduce? Research involving novel molecular diagnostics like RNA-seq-based ERT introduces specific ethical duties:
- Explaining the purpose and methodology: The consent process should describe, in understandable language, that the research involves an investigational test to assess endometrial receptivity and that it requires an endometrial biopsy for RNA sequencing [15] [7].
- Managing participant expectations: It must be clear that the test is for research purposes and may not directly benefit the participant, unless it is part of a validated clinical trial [7].
- Handling genomic data: The consent form should address how the RNA-seq data will be stored, protected, and used, including whether it will be used for future research and if participants will be informed of incidental findings [27].
5. A participant in our study on recurrent implantation failure becomes distressed during the consent process. What should we do? This situation directly engages the principle of respect for persons. You should [27]:
- Pause the process: Immediately stop reviewing the consent form.
- Address concerns: Reassure the participant and empathetically explore the source of their distress.
- Reaffirm voluntariness: Remind them that participation is entirely voluntary and that they can decline without any consequence to their clinical care.
- Allow time: Offer to reschedule the consent discussion for another day, giving them more time to consider and discuss with family or their physician. The participant's psychological welfare takes precedence over the research objectives.
Troubleshooting Guides for Common Ethical and Protocol Challenges
Problem: A participant questions the necessity of a repeat endometrial biopsy after a failed cycle in a study on recurrent implantation failure (RIF).
| Potential Cause & Solution |
|---|
| Cause: The participant may feel that the risks and inconvenience are no longer justified, or may not fully understand the research protocol's requirements. |
| Solution: Revisit the informed consent form with the participant. Patiently re-explain the study design and why multiple time points may be necessary for the research question. Emphasize their right to withdraw from the study at any time without penalty. The principle of respect for persons requires that their decision be honored without coercion [27]. |
Problem: During RNA extraction from an endometrial biopsy sample, the yield is too low for sequencing.
| Potential Cause & Solution |
|---|
| Cause: Sample degradation due to improper handling, delay in processing, or inefficient extraction methods. |
| Solution: Review and optimize the standard RNA-seq sample preparation workflow [30]: 1. Tissue Preservation: Ensure the biopsy is immediately placed in RNAlater or similar RNA stabilization reagent and stored at -80°C [8] [30]. 2. Extraction Method: Use a validated RNA extraction kit suitable for your starting material (e.g., PureLink RNA Mini Kit for cells and tissue). For low yields, consider kits that capture both large and small RNAs, like the mirVana miRNA Isolation Kit [30]. 3. Quantity Check: Aim for the recommended input of 100 ng to 1 µg of purified total RNA for library preparation [30]. |
Problem: A funding body requests full access to our study's raw RNA-seq data, which may include potentially identifiable participant information.
| Potential Cause & Solution |
|---|
| Cause: Tension between data transparency for scientific verification and the ethical/legal duty to protect participant confidentiality. |
| Solution: This must be managed according to the promises made during the informed consent process and the principle of confidentiality. 1. Anonymize Data: Before sharing, de-identify the data to the fullest extent possible, removing all direct identifiers [27] [31]. 2. Data Use Agreements: If consented, data can be shared under a formal agreement that obligates the recipient to protect confidentiality and use the data only for the agreed purposes [27]. 3. Managed Access: Use controlled-access databases where requestors must justify their use of the data and agree to terms of use. |
Ethical Principles and Their Application in Endometrial Research
The table below summarizes how core ethical principles translate into practical actions for endometrial RNA-seq studies.
| Ethical Principle | Practical Application in Endometrial Research |
|---|---|
| Social & Clinical Value | Focusing research on conditions like recurrent implantation failure (RIF) or endometrial cancer to improve diagnosis and treatment [15] [7]. |
| Scientific Validity | Using validated protocols for endometrial biopsy, RNA extraction, and RNA-seq analysis to ensure reliable results [8] [30]. |
| Fair Subject Selection | Including women of diverse backgrounds in RIF studies, not just those who are easily available [27]. |
| Favorable Risk-Benefit Ratio | Minimizing biopsy-related risks (pain, infection) through skilled execution and clear instructions, while maximizing knowledge gain [27]. |
| Independent Review | Submitting the full study protocol, including consent forms and data handling plans, for approval by an Institutional Review Board (IRB) or Ethics Committee [15] [29]. |
| Informed Consent | Providing clear information on the purpose of the rsERT test, the biopsy procedure, and the handling of transcriptomic data [7]. |
| Respect for Participants | Allowing a participant to withdraw from a study and have their biopsy sample destroyed if they change their mind [27]. |
Research Reagent Solutions for Endometrial RNA-seq
| Reagent / Kit | Function in Endometrial RNA-seq Research |
|---|---|
| RNAlater Stabilization Solution | Preserves RNA integrity in endometrial biopsy samples immediately after collection, preventing degradation during transport or storage [7]. |
| PureLink RNA Mini Kit | Purifies high-quality total RNA from homogenized endometrial tissue samples for use in sequencing library preparation [30]. |
| mirVana miRNA Isolation Kit | Isoles a broad range of RNA species, including messenger RNA (mRNA) and microRNA (miRNA), from endometrial tissue [30]. |
| RiboMinus Technology | Depletes abundant ribosomal RNA (rRNA) from total RNA samples, thereby enriching for coding and non-coding transcripts and improving sequencing depth [30]. |
| ERCC RNA Spike-In Mixes | Adds known, synthetic RNA transcripts to a sample as external controls to assess technical variability, sensitivity, and dynamic range of the RNA-seq assay [30]. |
Ethical Protocol Workflow
Sample Processing for RNA-seq
Step-by-Step Protocols: From Tissue to Sequencing Library
Bulk RNA-seq has established itself as a fundamental technique in transcriptomics, providing a comprehensive snapshot of gene expression profiles from entire tissue samples [32]. For researchers studying the endometrium—a complex, dynamic tissue central to reproductive health and disorders like endometriosis—bulk RNA-seq offers a cost-effective and reliable method for uncovering the molecular basis of diseases and identifying key biomarkers [33] [32]. When applied to full-thickness endometrial biopsies, which capture the full tissue architecture, this technology can yield invaluable insights into average transcriptional activity across the diverse cell populations present. However, the technique's primary limitation is the loss of cellular resolution, as it provides an averaged expression profile across all cells in the sample, potentially obscuring heterogeneity within the tissue [32]. This guide outlines the complete workflow, troubleshooting advice, and methodological standards for applying bulk RNA-seq to full-thickness endometrial biopsies, providing a framework for robust and reproducible research within a thesis on endometrial RNA-seq protocols.
The bulk RNA-seq workflow for endometrial biopsies involves a multi-stage process, from sample collection to data analysis. The following diagram summarizes the key stages, highlighting critical decision points and quality control checkpoints specific to endometrial tissue.
Frequently Asked Questions (FAQs) & Troubleshooting
Pre-sequencing Experimental Design
Q1: What are the critical sample collection factors for endometrial biopsies to ensure reliable RNA-seq data?
The single most important factor is standardizing the menstrual cycle phase at the time of collection. The endometrium is a highly dynamic tissue, and gene expression profiles fluctuate dramatically between the proliferative and secretory phases [33]. Studies must clearly document the cycle phase and ideally analyze samples from the same phase (e.g., proliferative endometrium) together to avoid confounding biological variation with technical effects [33]. Furthermore, samples should be snap-frozen in liquid nitrogen immediately after collection and stored at -80°C to preserve RNA integrity. The use of formalin-fixed, paraffin-embedded (FFPE) tissue is strongly discouraged for RNA-seq as it causes RNA fragmentation and cross-linking, leading to poor-quality libraries [34].
Q2: How much RNA is typically required from an endometrial biopsy for library preparation?
Required RNA input can vary based on the library prep kit, but standard protocols typically require 25 ng to 1 µg of total RNA [35]. For samples with lower quantity or quality, specialized low-input protocols are available. It is crucial to use high sample input for potentially degraded samples to mitigate sequencing biases [34].
Wet-Lab Protocol & Library Preparation
Q3: What is the best method for RNA extraction from endometrial tissue?
Successful RNA-seq relies on the isolation of high-quality, intact RNA. While TRIzol (phenol-chloroform extraction) is common, it can lead to small RNA loss at low concentrations [34]. The mirVana miRNA isolation kit has been reported as a superior tool for producing high-yield and high-quality RNA from complex tissues [34]. Regardless of the method, rigorous quality control (e.g., via Bioanalyzer) is essential to confirm RNA Integrity Number (RIN) before proceeding.
Q4: What are the major sources of bias during library preparation and how can they be minimized?
Library construction is a critical source of potential biases. The table below summarizes common issues and their solutions.
Table 1: Common Library Preparation Biases and Mitigation Strategies
| Bias Source | Description of Issue | Suggestion for Improvement |
|---|---|---|
| mRNA Enrichment | Poly(A) selection with oligo-dT beads can introduce 3’-end capture bias. | For full transcriptome coverage, use ribosomal RNA (rRNA) depletion instead [34]. |
| Fragmentation | Enzymatic fragmentation (e.g., RNase III) is not completely random, reducing complexity. | Use chemical treatment (e.g., zinc) or fragment cDNA post-reverse transcription [34]. |
| Priming Bias | Random hexamer primers can bind with varying efficiency, skewing representation. | Use read count reweighing schemes in bioinformatics analysis to adjust for this bias [34]. |
| PCR Amplification | Preferential amplification of sequences with neutral GC content; over-amplification. | Use high-fidelity polymerases (e.g., Kapa HiFi), reduce PCR cycle number, or use PCR-free protocols for sufficient input [34]. |
Data Analysis & Interpretation
Q5: What bioinformatics tools are standard for bulk RNA-seq differential expression analysis?
For general bulk RNA-seq analyses, the use of DESeq2 is preferred and widely considered a standard [36]. DESeq2 models raw count data using a negative binomial distribution and internally corrects for library size. It provides robust differential expression testing (using the Wald Test by default) and includes a false discovery rate (FDR) correction for multiple comparisons to control for false positives [36].
Q6: Our bulk RNA-seq data from endometrial biopsies shows high variability between samples. How can we assess quality and identify outliers?
Principal Component Analysis (PCA) is the primary tool for this. PCA reduces the high-dimensionality of the gene expression data to visualize sample-to-sample distances. In a PCA plot, samples from the same experimental group (e.g., control proliferative endometrium) should cluster closely together. Clear separation between groups along a principal component (e.g., PC1) is desirable and indicates that the biological difference between groups is the largest source of variation in the dataset [36].
Q7: How can we interpret the cellular dynamics of the endometrium from bulk RNA-seq data, given it provides an averaged profile?
This is a key limitation of bulk RNA-seq. However, computational deconvolution methods can be used to infer the relative proportions of major cell types (e.g., epithelial, stromal, immune cells) within the bulk tissue sample based on cell-type-specific gene expression signatures [33]. Furthermore, studies can be complemented by integrating with single-cell RNA-seq (scRNA-seq) data from similar tissues to provide a cellular roadmap for interpreting the bulk signals [33] [37]. For instance, a study on endometriosis used this integrated approach to identify mesenchymal cells in the proliferative eutopic endometrium as major contributors to the disease pathogenesis [33].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Reagents for Endometrial Bulk RNA-seq
| Item | Function/Description | Example/Known Brands |
|---|---|---|
| RNA Stabilization Reagent | Preserves RNA integrity immediately after biopsy by inhibiting RNases. | RNAlater |
| Total RNA Extraction Kit | Isolves high-quality, intact total RNA from tissue. | mirVana miRNA Isolation Kit, Qiagen RNeasy Kit |
| RNA Quality Assessment | Assesses RNA integrity (RIN) prior to library prep. | Agilent Bioanalyzer or TapeStation |
| Poly(A) Selection or rRNA Depletion Kit | Enriches for mRNA by removing abundant ribosomal RNA. | Illumina Stranded mRNA Prep, Illumina Stranded Total RNA Prep (with Ribo-Zero) |
| Library Preparation Kit | Creates sequencing-ready libraries from purified RNA. | Illumina Stranded mRNA Prep, KAPA mRNA HyperPrep Kit |
| Sequence Alignment Software | Aligns sequenced reads to a reference genome. | STAR Aligner [38] |
| Gene Quantification Tool | Assigns reads to genes and generates count tables. | HTSeq-count [36] |
| Differential Expression Package | Performs statistical analysis to find differentially expressed genes. | DESeq2 [36] |
| 3-Fluoro-2-vinylphenol | 3-Fluoro-2-vinylphenol|C8H7FO | 3-Fluoro-2-vinylphenol (CAS 1823094-20-7) is a fluorinated phenol for research, used in developing high-voltage lithium battery binders. For Research Use Only. Not for human or veterinary use. |
| 9-Methyladenine 1-oxide | 9-Methyladenine 1-oxide|CAS 10184-51-7 |
Detailed Experimental Protocols
Protocol: Standard Bulk RNA-seq Analysis with DESeq2
This protocol outlines the standard computational workflow for differential gene expression analysis following the generation of a raw count matrix from aligned reads (e.g., via STAR and HTSeq-count [36] [38]).
Workflow Diagram: DESeq2 Differential Expression Analysis
Key Steps:
- Input: The analysis begins with a matrix of raw, integer read counts. It is critical not to pre-normalize or transform this count matrix before inputting it into DESeq2, as the model performs its own internal normalization [36].
- Normalization: DESeq2 automatically calculates normalization factors for each sample to account for differences in sequencing depth, using the median of ratios method [36].
- Modeling and Testing: The core of DESeq2 fits a negative binomial generalized linear model (GLM) to the count data for each gene. The Wald test is then used to test the hypothesis of no differential expression between groups (e.g., diseased vs. healthy endometrium) [36].
- Multiple Testing Correction: Due to the thousands of simultaneous tests (one per gene), DESeq2 applies the Benjamini-Hochberg procedure to control the False Discovery Rate (FDR), outputting an adjusted p-value (
padj) [36]. - Log Fold Change Shrinkage: To improve the interpretability of results and prevent over-interpretation of large fold changes from low-count genes, DESeq2 can employ shrinkage estimators (e.g.,
apeglm) to generate more reliable and biologically meaningful log2 fold change estimates [36].
Protocol: Integrating Bulk RNA-seq with Single-Cell Data for Cell-Type Deconvolution
This protocol describes a conceptual workflow for using single-cell RNA-seq data as a reference to interpret bulk RNA-seq data from complex endometrial tissues, a method used in recent studies [33].
Workflow Diagram: Bulk and Single-Cell Data Integration
Key Steps:
- Obtain a Single-Cell Reference: Generate or acquire a scRNA-seq dataset from a similar endometrial tissue type. This data is clustered and annotated to define major cell types (e.g., epithelial, stromal, immune) and identify marker genes for each [33] [37].
- Run Deconvolution Algorithms: Use computational tools (e.g., CIBERSORTx, MuSiC) that leverage the scRNA-seq reference to estimate the relative abundance of each defined cell type within the bulk RNA-seq sample [33].
- Cross-Reference DEGs: After identifying Differentially Expressed Genes (DEGs) from the bulk analysis, cross-reference them with the cell-type-specific marker genes from the scRNA-seq atlas. This helps hypothesize which cell types are most associated with the observed transcriptional changes in the bulk tissue [33]. For example, a study might find that key genes identified in bulk data (like
SYNE2,TXN,NUPR1) are highly expressed in mesenchymal cells, pointing to that cell type's role in the disease [33].
Combining Fluorescence-Activated Cell Sorting (FACS) with single-cell RNA sequencing (scRNA-seq) on the 10x Genomics platform creates a powerful method for cell-type-specific transcriptomic profiling. This integration allows researchers to first isolate precise cellular subsets based on surface markers or intrinsic cellular properties before performing deep transcriptomic analysis [39] [40]. For endometrial RNA-seq sample preparation research, this approach enables specific investigation of rare endometrial cell populations, such as specific epithelial or stromal subtypes, that drive reproductive functions and disorders. The workflow preserves cellular identity while enabling unbiased transcriptome profiling, making it particularly valuable for understanding cellular heterogeneity in complex tissues like the endometrium [39].
Frequently Asked Questions (FAQs)
Q1: What are the key advantages of integrating FACS with 10x Genomics scRNA-seq?
Integrating FACS with 10x Genomics scRNA-seq provides several significant advantages:
- Pre-selection of Target Populations: FACS enables enrichment of rare cell types or specific cellular subsets before scRNA-seq, maximizing sequencing resources on biologically relevant cells [39] [40].
- Index Sorting Capability: Modern sorters can record all measured parameters (size, granularity, fluorescence) for each individually sorted cell, allowing retrospective correlation between surface marker expression and transcriptomic data [41] [39].
- Sample Quality Control: FACS provides an opportunity to remove dead cells, debris, and doublets before library preparation, significantly improving data quality [42].
- Flexibility in Experimental Design: Researchers can sort based on known markers, native cellular properties (size, granularity), or even computational predictions from previous scRNA-seq studies [40].
Q2: What are the critical sample preparation requirements for successful FACS before 10x Genomics scRNA-seq?
Proper sample preparation is crucial for obtaining high-quality data. Key requirements include:
Table 1: Sample Preparation Requirements for FACS before 10x Genomics scRNA-seq
| Parameter | Requirement | Importance |
|---|---|---|
| Cell Viability | >90% optimal; >70% acceptable with caution [43] | Ensures high-quality RNA and reduces background noise |
| Cell Concentration | Minimum 500,000 cells recommended [43] | Provides sufficient material for sorting and captures rare populations |
| Debris and Clumping | Minimal debris and cell clumps [43] [42] | Prevents sorter clogging and ensures single-cell suspensions |
| Buffer Composition | Cold PBS without Ca2+/Mg2+ + 1-2% BSA or commercial pre-sort buffer [42] | Maintains viability and prevents adhesion during sorting |
| Sorting Conditions | Large nozzle sizes, slower flow velocities [42] | Reduces mechanical stress on fragile cells |
Q3: How does FACS-based scRNA-seq compare to droplet-based approaches without pre-sorting?
Table 2: Comparison of FACS-Integrated vs. Standard 10x Genomics Approaches
| Characteristic | FACS-Integrated 10x | Standard 10x (without FACS) |
|---|---|---|
| Cell Input | Pre-enriched specific populations | Heterogeneous cell mixture |
| Throughput | Typically hundreds to thousands of cells [39] | Thousands to tens of thousands of cells [43] |
| Rare Cell Detection | Excellent for targeted rare populations [41] [40] | Limited by sequencing depth and budget |
| Surface Protein Data | Available via index sorting [41] [39] | Requires feature barcoding (CITE-seq) [43] |
| Cost per Target Cell | Lower for rare populations | Higher when targeting rare populations |
| Technical Complexity | Higher (two-step process) | Lower (streamlined workflow) |
Q4: What are the recommended collection methods for FACS-sorted cells intended for 10x Genomics?
For optimal results with 10x Genomics, FACS-sorted cells should be:
- Sorted into appropriate collection buffers: Use cold, RNase-free buffers containing RNase inhibitors to immediately stabilize RNA [42]. Different buffers are recommended depending on the subsequent library prep kit.
- Collected in low-bind tubes/plates: Prevents cell loss due to adhesion.
- Centrifuged gently after sorting: 100g for 15-30 seconds ensures cells are fully in collection buffer [42].
- Flash-frozen if not processing immediately: Place samples on dry ice and store at -80°C for up to several weeks [42].
Q5: Can fixed cells be used for FACS before 10x Genomics scRNA-seq?
Yes, fixed cells can be compatible with FACS and subsequent scRNA-seq with specific considerations:
- Fixation method matters: Formaldehyde fixation with Chromium sample preparation kit is compatible with 10x Genomics Fixed RNA Profiling (Flex) protocol [43].
- Timing is critical: Fixation should occur after staining but before sorting to preserve RNA integrity [44].
- Protocol adjustments needed: Fixed RNA Profiling uses a probe-based approach rather than reverse transcription, requiring specific experimental designs [43].
Troubleshooting Common Issues
Problem 1: Poor Cell Viability After Sorting
Potential Causes and Solutions:
- Cause: Harsh dissociation techniques or inappropriate sorting buffers.
- Solution: Optimize tissue dissociation protocols; use gentle mechanical dissociation combined with enzymatic digestion tailored to endometrial tissue [44]. Always use pre-sort buffers instead of culture media [42].
- Cause: Excessive pressure or inappropriate nozzle size during sorting.
- Solution: Use larger nozzle sizes (e.g., 100μm) and lower flow pressures, especially for fragile endometrial cells [42].
Problem 2: Low Cell Recovery After Sorting
Potential Causes and Solutions:
- Cause: Cell loss due to adhesion to tube surfaces.
- Solution: Use low-bind collection tubes and include BSA in sort buffers [42].
- Cause: Improper sorter calibration causing cells to miss collection vessel.
- Solution: Perform alignment checks using fluorescent beads or other QC methods to ensure accurate deposition [42].
Problem 3: High Ambient RNA in Sequencing Data
Potential Causes and Solutions:
- Cause: Cell lysis during sorting process.
- Solution: Optimize sorting conditions to minimize shear stress; include RNase inhibitors in all buffers [42].
- Cause: Excessive dead cells in starting material.
- Solution: Improve tissue dissociation methods; use viability dyes during sorting to exclude dead cells [43] [45].
Problem 4: Inadequate Sequencing Depth for Rare Populations
Potential Causes and Solutions:
- Cause: Insufficient number of target cells sorted.
- Solution: Pre-enrich target population using magnetic sorting before FACS; sort more cells than theoretically needed to account for losses [42].
- Cause: Suboptimal sequencing parameters.
- Solution: For targeted rare populations, increase sequencing depth to 50,000-100,000 reads per cell [43].
Experimental Workflows and Visualization
Standard Workflow for FACS-integrated 10x Genomics scRNA-seq
The following diagram illustrates the complete experimental workflow from tissue processing to data analysis:
Integration of FACS Index Data with Transcriptomics
This diagram shows how index sorting parameters are integrated with transcriptomic data:
Research Reagent Solutions
Table 3: Essential Reagents for FACS-integrated scRNA-seq Experiments
| Reagent Category | Specific Examples | Function | Considerations for Endometrial Samples |
|---|---|---|---|
| Tissue Dissociation | Collagenase, Trypsin, gentleMACS Dissociator [44] | Liberates individual cells from tissue matrix | Optimize enzyme combination for endometrial tissue integrity |
| Viability Stains | Propidium Iodide, DAPI, Fluorescent dyes [43] [42] | Identifies and excludes dead cells | Use membrane-impermeant DNA binding dyes |
| FACS Buffers | PBS without Ca2+/Mg2+, BSA, Commercial pre-sort buffers [42] | Maintain cell viability during sorting | Avoid culture media; can decrease viability during sorting [42] |
| Collection Buffers | Lysis buffer with RNase inhibitors [42] | Stabilizes RNA immediately after sorting | Composition varies by downstream kit (e.g., SMART-Seq vs. 10x) |
| Fixation Reagents | Formaldehyde, Methanol [43] [44] | Preserves cells for delayed processing | Compatibility with 10x Flex protocol required [43] |
Best Practices for Data Analysis
Quality Control Metrics for FACS-sorted scRNA-seq Data
After sequencing, careful quality control is essential. Key metrics to evaluate include:
- Cell calling quality: Ensure the number of recovered cells matches FACS records and displays proper barcode rank plot characteristics [45].
- Mitochondrial read percentage: Generally should be <10% for PBMCs, though this varies by cell type [45]. Higher percentages may indicate poor cell quality.
- Genes detected per cell: Should be consistent with expectations for your cell type (typically 1,000-3,000 genes/cell for 10x data) [45] [46].
- Integration of index sort data: Correlate surface protein expression from FACS with cluster identities from scRNA-seq [41] [39].
Addressing Technical Artifacts
Common technical artifacts in FACS-sorted scRNA-seq data include:
- Batch effects: Process all samples for the same experiment using identical sorting and library prep conditions.
- Ambient RNA: Use computational tools like SoupX or CellBender to remove background RNA signals [45].
- Multiplets: Employ computational doublet detection methods in addition to FACS gating strategies.
By following these comprehensive guidelines, researchers can successfully integrate FACS with 10x Genomics scRNA-seq to achieve robust cell-type-specific profiling, particularly valuable for investigating cellular heterogeneity in endometrial tissue environments and related reproductive research.
Spatial transcriptomics has revolutionized genomic research by enabling the precise mapping of gene expression within the context of tissue architecture. The 10x Genomics Visium platform represents a cutting-edge solution for spatial gene expression analysis, particularly valuable for complex tissues like the endometrium where cellular positioning and microenvironment interactions are critical to understanding both normal physiology and disease states. This technical support guide provides a comprehensive protocol specifically optimized for frozen endometrial sections, framed within the broader context of endometrial RNA-seq sample preparation research. The protocol integrates detailed methodologies, troubleshooting guides, and frequently asked questions to support researchers, scientists, and drug development professionals in implementing this powerful technology effectively. By preserving spatial information while capturing transcriptomic data, researchers can uncover novel insights into endometrial receptivity, menstrual cycle dynamics, and pathological conditions such as endometriosis and endometrial cancer, ultimately advancing both basic science and therapeutic development.
Experimental Workflow and Protocol
Complete Workflow Diagram
Sample Preparation Protocol
Tissue Collection and Preservation: Endometrial tissues should be collected under approved ethical guidelines and immediately snap-frozen in cold isopentane (rather than liquid nitrogen) to prevent tissue cracking and preserve RNA integrity [47]. For optimal results, tissues should be embedded in Optimal Cutting Temperature (OCT) compound simultaneously with freezing to ensure complete embedding without air pockets. The tissue block size must not exceed 6.5×6.5mm to fit within the Visium capture area [48] [47].
Cryosectioning Parameters: Section tissues at 10μm thickness using a cryostat maintained at -20°C [48] [47]. Place sections carefully on the Visium Spatial Gene Expression slides, ensuring proper orientation and minimizing folds or tears. Serial sections can be collected for H&E staining and tissue optimization tests. Maintain slides at -80°C until use to preserve RNA integrity.
Quality Assessment: Prior to proceeding with the full protocol, assess tissue morphology through H&E staining and RNA quality using Bioanalyzer or TapeStation. For endometrial tissues, aim for RNA Integrity Number (RIN) values >7 whenever possible [47]. While this is not always achievable with clinical endometrial samples, particularly those obtained through biopsy, RIN values below 7 may still yield usable data but with potentially reduced gene detection rates.
Visium Spatial Protocol Execution
Tissue Optimization: This critical step determines the optimal permeabilization time for each specific endometrial tissue type [47]. The Visium Spatial Tissue Optimization Slide & Reagent Kit (PN-1000193) is used to test different permeabilization times on serial sections [49]. The optimal time maximizes cDNA yield while maintaining tissue morphology. Endometrial tissues typically require permeabilization times between 12-24 minutes, but this should be empirically determined for each sample type.
Spatial Gene Expression Workflow: After determining optimal permeabilization conditions, proceed with the full Visium Spatial Gene Expression protocol using the Slide & Reagent Kit (PN-1000184 or PN-1000187) [49]. The process involves tissue permeabilization to release RNA, capture on barcoded Visium spots, reverse transcription to create cDNA, second strand synthesis, library construction, and sequencing. Each spot on the Visium slide contains millions of capture oligonucleotides with spatial barcodes that preserve positional information [48].
Sequencing Parameters: Visium libraries require specific sequencing parameters. Use the read configuration: Read 1: 28 cycles; i7 Index: 10 cycles; i5 Index: 10 cycles; Read 2: 90 cycles [47] [50]. The recommended sequencing depth is 50,000 read pairs per spot covered by tissue [47] [50]. For a capture area with approximately 5,000 spots completely covered by tissue, this equates to approximately 250 million read pairs per section.
Technical Specifications and Requirements
Visium Platform Specifications
Table 1: Technical Specifications of 10x Visium Spatial Platform
| Parameter | Specification | Relevance to Endometrial Research |
|---|---|---|
| Spot Diameter | 55 μm [48] | Ideal for capturing endometrial glands and stromal domains |
| Spot Center-to-Center Distance | 100 μm [48] | Enables mapping of tissue microarchitecture |
| Spots per Capture Area | 5,000 (V1) or 14,000 (V2) [50] | Sufficient resolution for endometrial tissue organization |
| Capture Area Dimensions | 6.5 × 6.5 mm (V1) or 11 × 11 mm (V2) [48] [50] | Accommodates most endometrial biopsy samples |
| Cells per Spot | 1-10 cells [48] | Appropriate for endometrial cellular resolution |
| Recommended Tissue Thickness | 10 μm [48] [47] | Optimal for RNA capture while maintaining morphology |
| Sequencing Depth | 50,000 read pairs per spot [47] [50] | Ensures comprehensive transcriptome coverage |
Sample Quality Requirements
Table 2: Sample Quality Control Parameters for Endometrial Tissues
| Parameter | Minimum Requirement | Optimal Target | Assessment Method |
|---|---|---|---|
| RNA Integrity Number (RIN) | >5 [47] | >7 [47] | Bioanalyzer/TapeStation |
| Tissue Size | Fits within 6.5×6.5mm area [47] | 5-6mm in largest dimension | Visual inspection |
| DV200 (FFPE only) | >30% [50] | >50% | Bioanalyzer/TapeStation |
| Tissue Morphology | Preserved architecture | No ice crystals, minimal tears | H&E staining |
| Cell Viability | N/A (spatial uses fixed tissue) | N/A | N/A |
Troubleshooting Guide
Common Experimental Issues and Solutions
Issue: Low Gene Detection Rates
- Potential Causes: Suboptimal permeabilization, RNA degradation, insufficient sequencing depth, or incorrect tissue thickness.
- Solutions:
- Verify RNA quality with Bioanalyzer before starting (RIN >7 ideal) [47]
- Optimize permeabilization time using tissue optimization slides [49] [47]
- Ensure tissue sections are precisely 10μm thick [48]
- Increase sequencing depth up to 50,000 read pairs per spot [50]
- Check that tissue is properly positioned over the capture area
Issue: Poor Tissue Morphology or Sectioning Quality
- Potential Causes: Improper freezing technique, incorrect cryosectioning temperature, dull blade, or improper OCT embedding.
- Solutions:
- Verify snap-freezing was performed in cold isopentane, not liquid nitrogen [47]
- Adjust cryostat temperature (typically -18°C to -22°C for endometrial tissue)
- Use fresh cryostat blades and ensure proper alignment
- Ensure complete OCT embedding without air bubbles
- Practice sectioning technique to minimize folds and tears
Issue: High Background or Non-Specific Staining
- Potential Causes: Excessive permeabilization, contaminated reagents, improper washing, or non-specific antibody binding.
- Solutions:
- Reduce permeabilization time based on optimization results
- Prepare fresh reagents and use nuclease-free techniques
- Increase wash stringency and number of washes
- Include appropriate blocking steps for antibody-based detection
Frequently Asked Questions
Q1: What is the maximum size of endometrial tissue that can be processed using Visium? A: The tissue block must not exceed 6.5×6.5mm for standard Visium slides to fit within the capture area [47]. Larger tissues must be trimmed or divided, though the newer Visium HD slides with 11×11mm capture areas can accommodate larger samples [50].
Q2: How does the gene expression profiling process differ between fresh frozen and FFPE endometrial samples? A: For fresh frozen endometrial tissues which contain mostly intact RNAs, whole transcriptome analysis is performed through poly-T-based cDNA reverse transcription followed by sequencing. For FFPE samples, which typically have more RNA fragmentation, analysis is achieved through hybridization of gene-specific probes followed by sequencing [50].
Q3: What is the typical turnaround time for a complete Visium experiment on endometrial samples? A: Once samples pass QC and sections are placed on Visium slides, slide processing typically takes 2-3 weeks, with sequencing requiring an additional two weeks [50]. Tissue optimization, if needed, adds 1-2 weeks to the timeline.
Q4: How many genes can be detected from fresh frozen endometrial tissue sections? A: The Visium platform can detect approximately 18,000 human genes from fresh frozen tissues [50]. The actual number detected in endometrial samples may vary based on tissue quality, permeabilization efficiency, and sequencing depth.
Q5: Can I use tissue sections that have already been prepared on regular glass slides? A: Yes, the 10x CytAssist instrument enables transfer of tissue analytes from existing slides to Visium slides for spatial analysis [50]. This is particularly valuable for precious endometrial samples that were previously sectioned.
Q6: What bioinformatics support is available for analyzing Visium data? A: 10x Genomics provides Space Ranger for initial data processing and Loupe Browser for visualization [51] [52]. For more advanced analyses, numerous R and Python packages are available, including Cumulus [53] and SpatialData [54]. Many core facilities also offer bioinformatics support services.
Q7: How is spatial resolution defined in the Visium platform, and is it sufficient for endometrial research? A: Spatial resolution is determined by spot diameter (55μm) and center-to-center distance (100μm) [48]. This resolution captures 1-10 cells per spot, which is sufficient for identifying endometrial glandular and stromal regions, but may not resolve individual epithelial and stromal cells in densely packed areas.
Essential Research Reagent Solutions
Core Reagents and Kits
Table 3: Essential Research Reagents for Visium Spatial Transcriptomics
| Reagent/Kit | Function | Specific Product References |
|---|---|---|
| Visium Spatial Gene Expression Slide & Reagent Kit | Contains slides with capture areas and reagents for library preparation | PN-1000184 (16 reactions), PN-1000187 (4 reactions) [49] |
| Visium Spatial Tissue Optimization Slide & Reagent Kit | Determines optimal permeabilization conditions for specific tissue types | PN-1000193 (4 slides) [49] |
| OCT Embedding Compound | Tissue embedding medium for cryosectioning | Various manufacturers; ensure compatibility with RNA work |
| Visium Accessory Kit | Additional reagents and consumables required for the workflow | PN-1000194 [49] |
| Dual Index Kit | For library multiplexing | PN-1000215 (TT Set A, 96 reactions) [49] |
| Cryosectioning Supplies | Blades, molds, and tools for tissue sectioning | Specific to cryostat model |
Data Analysis and Interpretation
Bioinformatics Workflow
The standard analysis pipeline for Visium data begins with Space Ranger, which processes sequencing data, aligns reads to a reference genome, generates feature-barcode matrices, and performs initial clustering and differential expression analysis [51] [53]. The output can then be visualized and explored in Loupe Browser, which enables interactive exploration of spatial gene expression patterns in the context of tissue morphology [51].
For more advanced analyses, researchers can utilize the growing ecosystem of spatial data analysis tools. The SpatialData framework provides a unified environment for handling and visualizing spatial omics data, compatible with both Python and R workflows [54]. This is particularly valuable for integrating Visium data with other data types, such as single-cell RNA sequencing or spatial proteomics, to gain deeper insights into endometrial tissue organization and function.
Integration with Endometrial Research Questions
When applying spatial transcriptomics to endometrial samples, consider these analytical approaches:
- Region-based Analysis: Identify transcriptomically distinct regions corresponding to functional endometrial zones (basalis vs. functionalis)
- Cell Type Decomposition: Use reference-based deconvolution to estimate cell type proportions within each spot, leveraging existing single-cell RNA sequencing data from endometrial tissues
- Spatially Variable Genes: Identify genes with non-random spatial patterns that may reflect localized functions or microenvironmental influences
- Cell-Cell Communication: Infer potential signaling interactions between neighboring cellular communities using ligand-receptor co-expression analysis
The integration of spatial transcriptomics with endometrial research provides unprecedented opportunities to understand the dynamic remodeling, receptivity, and pathological transformations of this complex tissue in its native architectural context.
Uterine fluid extracellular vesicles (UF-EVs) have emerged as a promising, non-invasive source of RNA biomarkers for assessing endometrial receptivity (ER). The endometrium's receptivity, known as the window of implantation (WOI), is crucial for successful embryo implantation and is typically a short period of less than 48 hours that varies between individuals [55] [56]. Traditional assessment methods like endometrial biopsy are invasive, can alter the endometrial RNA expression profile, and may negatively impact implantation, making them unsuitable for the same active cycle of fertilization treatment [55]. UF-EVs, which are part of the uterine fluid—a mixture of endometrial secretions, plasma transudates, and oviductal fluid—contain a rich cargo of RNAs, DNAs, regulatory proteins, and other bioactive factors that facilitate embryo-endometrium communication [55]. Aspiration of uterine fluid prior to embryo transfer has been shown not to affect implantation rates, establishing the feasibility of developing diagnostic tools based on this medium [55]. The non-invasive RNA-seq based endometrial receptivity test (nirsERT) leverages transcriptomic data from uterine fluid, utilizing machine learning to accurately predict the WOI and guide successful embryo implantation in patients undergoing in vitro fertilization (IVF) [55] [56].
Frequently Asked Questions (FAQs) & Troubleshooting Guides
Pre-Analysis Phase: Sample Collection and Quality Control
Q1: What are the critical patient inclusion criteria for a study on UF-EVs and endometrial receptivity? To ensure reliable and interpretable results in UF-EV research, consider these key criteria [55]:
- Age: 20–39 years.
- Body Mass Index (BMI): 18–25 kg/m².
- Menstrual Cycle: Regular cycle length (25–35 days) with spontaneous ovulation.
- Ovarian Reserve: Normal (baseline FSH < 10 mIU/mL, AMH > 1.5 ng/ml, antral follicle count > 5).
- Exclusion Criteria: Presence of endometrial diseases (e.g., endometritis, polyps, hyperplasia, adhesions), hydrosalpinx, submucous myomas, endometriosis (stages III–IV), or uterine malformations.
Q2: When and how should uterine fluid be collected? Uterine fluid is optimally collected in a natural cycle [55].
- Timing: For model construction, samples are collected on specific days relative to the luteinizing hormone (LH) surge: LH+5 (pre-receptive), LH+7 (receptive), and LH+9 (post-receptive). For clinical validation, a single sample can be collected on the day of blastocyst transfer (LH+7 in a natural cycle or 5 days after progesterone administration in a hormone replacement cycle) prior to embryo transfer [55].
- Method: The cervix is cleansed with saline. An embryo transfer catheter is inserted through the cervix, and the inner catheter is introduced 1–2 cm from the uterine fundus to avoid cervical mucus contamination. Uterine fluid is gently aspirated using a 2.5 mL syringe [55].
Q3: How can I prevent RNA degradation during sample collection and processing? RNA integrity is paramount. The following practices are essential [57]:
- RNase-free Environment: Use certified RNase-free tubes, tips, and solutions. Wear a mask and clean gloves, and operate in a dedicated clean area.
- Rapid Processing: Process samples quickly at low temperatures to minimize changes in gene expression profiles. One protocol suggests completing tissue manipulation and sorting within 90 minutes [8].
- Proper Storage: Immediately freeze collected samples at -85°C to -65°C. Store samples in separate, single-use aliquots to avoid degradation from repeated freeze-thaw cycles [57].
Analysis Phase: RNA Extraction and Sequencing
Q4: My RNA yield from UF-EVs is low. What could be the cause? Low RNA yield can result from several factors [57]:
- Cause: Incomplete homogenization or lysis of the EV pellet, leading to inefficient RNA release.
- Solution: Ensure thorough and complete homogenization of the sample. For small sample quantities, adjust the lysis reagent volume proportionally to prevent excessive dilution.
- Cause: RNA precipitation loss during extraction.
- Solution: When discarding the supernatant, use pipette aspiration instead of decanting to avoid losing the often-invisible pellet. For very low RNA content, add 1 µL of glycogen (20 mg/mL) as a carrier during precipitation.
Q5: My extracted RNA appears to have genomic DNA contamination. How do I resolve this? gDNA contamination can interfere with accurate RNA-seq results [57].
- Cause: High sample input or incomplete lysis.
- Solutions:
- Reduce the starting sample volume or increase the volume of the lysis reagent.
- Use reverse transcription reagents that include a genomic DNA removal module.
- During subsequent PCR steps, design primers that span an intron to distinguish between cDNA and gDNA amplification.
Q6: How do I choose the right RNA-seq kit for UF-EV RNA? The choice of kit depends on your starting material's quantity and quality [58]:
- For Ultra-Low Input, High-Quality RNA (RIN ≥8): Use oligo(dT)-primed kits like the SMART-Seq v4 Ultra Low Input RNA Kit. These are designed for full-length mRNA sequencing from 1–1,000 cells or 10 pg–10 ng of total RNA and do not require prior rRNA removal [58].
- For Degraded or Low-Quality RNA (e.g., RIN 2-3): Use random-primed kits like the SMARTer Universal Low Input RNA Kit for Sequencing. This is suitable for sheared or degraded RNA but requires prior ribosomal RNA (rRNA) depletion to prevent over 90% of reads from mapping to rRNA [58].
Q7: Why is ribosomal RNA (rRNA) depletion necessary, and which method is recommended? Since the majority of cellular RNA is ribosomal, its presence will dominate the sequencing library, wasting sequencing depth on non-informative reads [58].
- Recommendation: For 10–100 ng samples of mammalian total RNA, use the RiboGone - Mammalian kit for effective rRNA depletion [58].
Post-Analysis Phase: Data and Validation
Q8: What is the typical performance of a UF-EV RNA-seq model like nirsERT? The nirsERT model, built using a random forest algorithm on uterine fluid transcriptomes from 48 IVF patients, demonstrated high predictive accuracy [55] [56].
- Model Components: 87 marker genes and 3 hub genes.
- Accuracy: 10-fold cross-validation resulted in a mean accuracy of 93.0% [55].
- Clinical Correlation: In a small validation cohort (n=22), 77.8% (14/18) of patients predicted to have a normal WOI achieved successful intrauterine pregnancy, while none of the patients (0/3) with a predicted displaced WOI had a successful pregnancy [55].
Experimental Protocol: From UF-EV Collection to nirsERT Prediction
The following diagram illustrates the complete experimental pathway for developing and applying a non-invasive endometrial receptivity test.
Detailed Methodologies
Step 1: Patient Recruitment and Uterine Fluid Collection Recruit IVF patients meeting the inclusion criteria outlined in FAQ Q1. Collect uterine fluid specimens at three key time points in a natural cycle: LH+5 (pre-receptive), LH+7 (receptive), and LH+9 (post-receptive) using the catheter-based method described in FAQ Q2 [55]. For clinical validation, a single sample is collected on the day of frozen-thaw blastocyst transfer [55].
Step 2: EV Isolation and RNA Extraction While specific EV isolation protocols from uterine fluid may vary, the general principles of RNA extraction apply. Isolate total RNA from the UF-EV fraction using a phenol-guanidine based method like TRIzol, ensuring an RNase-free environment. Key troubleshooting tips from FAQ Q4 and Q5 should be followed to ensure high RNA yield and purity [57]. Assess RNA quantity and quality using an Agilent 2100 Bioanalyzer with an RNA 6000 Pico Kit to determine the RNA Integrity Number (RIN) [58].
Step 3: RNA-Seq Library Preparation and Sequencing Based on the RNA quality (RIN), select an appropriate library prep kit as per FAQ Q6.
- For RIN ≥8: Use 1-10 ng of RNA with the SMART-Seq v4 Ultra Low Input RNA Kit for full-length cDNA synthesis and amplification, followed by Illumina library preparation [58].
- For degraded RNA (RIN 2-3): First, perform rRNA depletion using the RiboGone - Mammalian kit. Then, use 200 pg–10 ng of rRNA-depleted RNA with the SMARTer Universal Low Input RNA Kit for Sequencing, which employs random priming [58]. Sequence the resulting libraries on an Illumina platform (e.g., HiSeq 2500) for 200 cycles in paired-end mode (2x100 bp) [59].
Step 4: Bioinformatic Analysis and Machine Learning Model Construction Process the raw sequencing data through a standard pipeline:
- Quality Control: Use tools like FastQC to assess read quality.
- Alignment: Map reads to the human reference genome.
- Differential Expression: Identify differentially expressed genes (DEGs) between pre-receptive, receptive, and post-receptive samples. One study identified 864 ER-associated DEGs involved in endometrium-embryo crosstalk [55].
- Model Building: Apply a random forest machine learning algorithm to the transcriptomic profiles to build a classifier. The final nirsERT model was based on 87 marker genes and 3 hub genes [55] [56]. Validate the model's accuracy using 10-fold cross-validation.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key reagents and materials required for a UF-EV RNA-seq study.
| Item Name | Function/Application | Key Specifications |
|---|---|---|
| Embryo Transfer Catheter | Non-invasive aspiration of uterine fluid. | Cook Medical embryo transfer catheter [55]. |
| SMART-Seq v4 Ultra Low Input RNA Kit | cDNA synthesis & amplification for RNA-seq. | For 10 pg–10 ng high-quality RNA (RIN≥8); oligo(dT) priming [58]. |
| SMARTer Universal Low Input RNA Kit | cDNA synthesis & amplification for degraded RNA. | For 200 pg–10 ng degraded RNA (RIN 2-3); requires rRNA depletion; random priming [58]. |
| RiboGone - Mammalian Kit | Depletion of ribosomal RNA (rRNA). | For 10–100 ng mammalian total RNA; used prior to random-primed kits [58]. |
| Agilent RNA 6000 Pico Kit | Assessment of RNA concentration and integrity (RIN). | Used with the Agilent 2100 Bioanalyzer; ideal for low-concentration samples [58]. |
| NucleoSpin RNA XS Kit | RNA purification from a small number of cells. | For RNA isolation from up to 1x10^5 cultured cells; carrier-free [58]. |
| miRVana RNA Isolation Kit | Total RNA isolation (including small RNAs). | Suitable for tissue samples; used in endometrial cancer transcriptome studies [59]. |
| Cyclopentyl dodecanoate | Cyclopentyl Dodecanoate | Cyclopentyl dodecanoate for research applications. This product is for Research Use Only (RUO) and is not intended for personal use. |
| Fmoc-alpha-Me-Phe-OH | Fmoc-alpha-Me-Phe-OH, MF:C50H52N2O11, MW:857.0 g/mol | Chemical Reagent |
Signaling Pathways and Biological Processes in Endometrial Receptivity
Analysis of the uterine fluid transcriptome reveals key biological processes activated during the window of implantation. The 864 ER-associated differentially expressed genes (DEGs) identified in the nirsERT study are involved in critical functions for embryo-endometrium dialogue [55].
The pathways highlighted in the diagram, such as MAPK signaling and Wnt signaling, are not only critical for normal endometrial receptivity but have also been identified as among the most affected functional pathways in endometrial neoplastic transformation, underscoring their fundamental role in endometrial biology [59].
Platform Comparison and Selection Guide
Technical Comparison of RNA-seq Library Preparation Platforms
Table 1: Key characteristics of major RNA-seq library preparation platforms
| Platform/Kit | Primary Application | Key Technology | Starting Input | Multiplexing Capacity | Key Strengths |
|---|---|---|---|---|---|
| 10x Genomics Single Cell 3' | Single-cell RNA sequencing | Gel Bead-in-Emulsion (GEM), Barcoded Oligos | 700-1,200 cells/µL [60] | Varies by kit (e.g., Dual Index) [61] | High-throughput single-cell profiling, cell type identification |
| Illumina High-Throughput (HTR) | Bulk RNA sequencing | SPRI magnetic beads, Enzymatic fragmentation | Tissue (as low as 5 mg) [62] | 96 unique barcodes [62] | Cost-effective, high reproducibility, low technical variation |
| Zymo-Seq RiboFree | Total RNA sequencing (ribodepletion) | Unique Dual Indexes (UDIs) | Total RNA | 96 UDIs [63] | Effective ribosomal RNA removal, compatible with degraded samples |
Platform Selection FAQ
Q1: Which platform is most suitable for analyzing heterogeneous endometrial tissue samples at single-cell resolution? A: The 10x Genomics Single Cell 3' platform is specifically designed for this application. It enables the profiling of gene expression in individual cells from a tissue sample, which is crucial for identifying and characterizing different cell subpopulations (e.g., epithelial, stromal, immune) within the complex endometrial environment [61]. This is a significant advantage over bulk RNA-seq, which averages expression across all cells.
Q2: For bulk RNA-seq analysis of endometrial biopsies, how do I choose between the Illumina HTR and Zymo-Seq RiboFree protocols? A: The choice depends on your sample quality and experimental goals:
- Illumina HTR is highly cost-effective and reproducible for high-throughput studies. Its protocol minimizes technical variation, which increases the power to detect differentially expressed genes [62]. It is an excellent choice for well-preserved samples where high data consistency across many samples is a priority.
- Zymo-Seq RiboFree is ideal when working with samples that may have significant ribosomal RNA (rRNA) background or potential degradation. Its ribodepletion method effectively removes rRNA, and its compatibility with the Illumina NextSeq 2000 with onboard DRAGEN analysis streamlines the process [63].
Q3: What is the most critical factor for a successful 10x Genomics single-cell experiment? A: Sample quality is paramount. The initial cell suspension must be fully dissociated, contain single cells with high viability (>90%), and be free of contaminants. Dead or stressed cells, cellular debris, and excessive ambient RNA can severely compromise data quality [60] [61]. The protocol is highly sensitive to these factors.
Troubleshooting Common Experimental Issues
Troubleshooting Guide for Library Preparation
Table 2: Common issues, causes, and solutions in RNA-seq workflows
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low Cell Viability in 10x | Overly harsh tissue dissociation, prolonged processing at room temperature. | - Optimize dissociation protocol; consider cold-active proteases [60].- Keep cells and buffers on ice at all times [60].- Perform dead cell removal [60]. |
| High Multiplet Rate in 10x | Input cell concentration is too high. | - Load cells within the recommended range of 700-1,200 cells/µL [60].- Accurately determine cell concentration and viability before loading. |
| Adapter Dimers | Improper adapter ligation or inadequate cleanup. | - Follow recommended purification steps (e.g., SPRI bead cleanups) [64] [62].- Use validated kits and follow protocols precisely. |
| High Ribosomal RNA | Inefficient mRNA enrichment or ribodepletion. | - For bulk RNA-seq, select a dedicated ribodepletion kit like Zymo-Seq RiboFree [63].- Ensure oligo dT bead binding is efficient in direct mRNA protocols [62]. |
| Reduced Library Complexity (10x) | Carry-over of enzymatic inhibitors from tissue dissociation. | - Avoid using EDTA (>0.1 mM) or high magnesium (>3 mM) in dissociation buffers [60].- Wash cells thoroughly after dissociation or dead cell removal steps [60]. |
Protocol-Specific FAQ
Q4: During the 10x Genomics encapsulation, what specific pipette tips should I use and why? A: Rainin tips (preferably filtered) are strongly recommended. Tips from other brands like Denville, Axygen, Thermo ART, and Biorad can destabilize the GEMs (Gel Bead-in-Emulsions), which are the core microreactors for single-cell barcoding. Using non-validated tips may lead to GEM breakage and experimental failure [60].
Q5: In the Illumina HTR protocol, how is the issue of RNA over-fragmentation addressed? A: The Illumina HTR protocol replaces chemical fragmentation of RNA with enzymatic fragmentation of cDNA. Chemical fragmentation is rapid (5-10 minutes) and difficult to control consistently across a 96-well plate, leading to over-fragmentation and poor reproducibility. Enzymatic fragmentation of cDNA is a more controlled and reproducible process, which is essential for a high-throughput workflow [62].
Q6: For Zymo-Seq libraries, what are the critical parameters when setting up a sequencing run on an Illumina NextSeq 2000? A: When using the onboard DRAGEN pipeline for analysis, you must correctly specify the index read lengths and adapter sequences.
- Index Reads: Select "2 Indexes".
- Read Lengths: For the 8-bp Unique Dual Indexes, set both Index 1 and Index 2 read lengths to "8".
- Adapter Trimming: Provide the correct adapter sequences for the DRAGEN software to trim (e.g., AdapterRead1:
AGATCGGAAGAGCACACGTCTGAACTCCAGTCAC) [63].
Essential Workflow Diagrams
10x Genomics Single-Cell 3' RNA-seq Workflow
High-Throughput Bulk RNA-seq (HTR) Workflow
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential reagents and their functions in RNA-seq library preparation
| Reagent/Material | Function | Example Use Case |
|---|---|---|
| Oligo dT Magnetic Beads | Direct mRNA capture from lysate by binding poly-A tail. | Isolating mRNA directly from tissue in the HTR protocol, skipping total RNA extraction [62]. |
| SPRI/AMPure XP Beads | Solid-phase reversible immobilization for size-selective purification and cleanup of reactions. | Used in nearly all protocols for cleaning up enzymatic reactions and selecting desired fragment sizes [65] [62]. |
| Unique Dual Indexes (UDIs) | Molecular barcodes for multiplexing samples; unique combinations for i5 and i7 indexes. | Uniquely labeling samples in Zymo-Seq and other modern kits to prevent index hopping in sequencing [63]. |
| Template Switch Oligo (TSO) | Enables template switching during reverse transcription, facilitating full-length cDNA capture. | A key component in the 10x Genomics RT Master Mix for synthesizing complete cDNA transcripts [60]. |
| Reducing Agent B | Maintains a reducing environment to prevent disulfide bond formation between molecules. | Included in the 10x Genomics RT Master Mix to ensure GEM stability and reaction efficiency [60]. |
| LongAmp Hot Start Taq Master Mix | PCR enzyme for efficient amplification of long cDNA fragments. | Used in the Nanopore 5' cDNA protocol for amplifying cDNA amplicons from 10x kits [65]. |
| epsilon,epsilon-Carotene | epsilon,epsilon-Carotene, MF:C40H56, MW:536.9 g/mol | Chemical Reagent |
| N-cyclohexylpyridin-3-amine | N-cyclohexylpyridin-3-amine |
Solving Common Challenges and Enhancing Data Quality
In endometrial RNA-seq research, the integrity of your RNA samples is the cornerstone of reliable data. The endometrium, a dynamically changing tissue, presents a uniquely RNase-rich environment where essential molecular signatures can be rapidly degraded, compromising transcriptome-wide studies on receptivity. This guide provides targeted, practical solutions to identify and prevent RNA degradation, ensuring the success of your experiments.
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: My endometrial RNA Integrity Number (RIN) is consistently low after extraction. What are the most likely causes?
- Cause A: Inadequate RNase inhibition during tissue collection. Endometrial biopsies are rich in endogenous RNases released upon cell rupture. Immediate and effective inhibition is critical.
- Solution: Snap-freeze biopsies in liquid nitrogen immediately after collection. Alternatively, immerse the tissue completely in a commercial RNA stabilization reagent (e.g., RNAlater) as was done in the endometrial receptivity study [7].
- Cause B: Introduction of exogenous RNases during handling.
- Solution: Establish a dedicated RNase-free workspace. Use sterile, disposable plasticware and treat surfaces with RNase decontamination sprays. Always wear gloves to prevent introduction of RNases from skin [66].
Q2: My cDNA yield from endometrial samples is low in reverse transcription reactions. Is this due to RNA degradation?
- Answer: Yes, degraded RNA is a primary cause of low cDNA yield. However, the RT reaction itself is vulnerable. Ensure your reaction mix includes a robust RNase inhibitor.
- Solution: Supplement your RT reaction with a high-quality, recombinant RNase inhibitor. A common working concentration is 0.5-1 U/μL [67]. For a thermostable option that survives the initial denaturation step, consider newer synthetic inhibitors [68].
Q3: How can I verify if RNA degradation is occurring during my specific RNA-seq library preparation steps?
- Answer: Utilize the ERCC RNA Spike-In Mixes. These are exogenous RNA controls with known sequences and concentrations added to your sample at the start of library prep [69].
- Troubleshooting: If the recovery and sequencing results of these spike-in controls deviate significantly from expectations, it indicates degradation or inefficiency during the library preparation process, helping you pinpoint the problematic step.
Q4: Are there specific RNase inhibitors that work better for high-temperature steps in protocols?
- Answer: Yes, traditional protein-based inhibitors can denature at high temperatures. For protocols involving heat steps (e.g., cell lysis at 72°C in Smart-seq2), a synthetic thermostable RNase inhibitor is superior. Recent studies show they maintain efficacy even after incubation at 50°C for 24 hours, eliminating the need for a second addition of inhibitor to the RT mix and simplifying the workflow [68].
Quantitative Data for Informed Reagent Selection
The table below summarizes key performance data for different types of RNase inhibitors to guide your selection.
Table 1: Comparison of RNase Inhibitor Types for RNA-seq Workflows
| Inhibitor Type | Effective Temperature Range | Key Feature / Advantage | Reported Performance in RNA-seq | Considerations |
|---|---|---|---|---|
| Recombinant Murine RNase Inhibitor [67] | Up to ~50°C | Inhibits RNase A, B, C. Resistant to oxidation. | The long-standing standard; provides effective inhibition for most enzymatic steps. | Requires a reducing agent (e.g., DTT) for full activity; can be thermally inactivated. |
| Synthetic Thermostable Inhibitor (e.g., SEQURNA) [68] | Up to at least 50°C for 24h; survives 72°C lysis steps. | Thermostable, non-protein-based, reduces primer-dimers in PCR. | Produces scRNA-seq libraries of equal or superior quality to recombinant inhibitors. | Has a defined optimal concentration range that must be determined for each protocol. |
| Chemical Denaturants (e.g., Guanidine Thiocyanate in Trizol) [66] | Room temperature & during extraction. | A potent protein denaturant; component of common RNA extraction reagents. | Essential for initial tissue homogenization and RNA isolation. | Chaotropic nature interferes with downstream enzymatic steps; must be removed. |
Experimental Protocols for Validation and Diagnostics
Protocol 1: Assessing RNA Integrity in Endometrial Biopsies
This protocol should be performed prior to costly library construction.
- Extraction: Isolate total RNA from a punch of your endometrial biopsy using a silica-column based kit. Include a DNase digestion step to remove genomic DNA contamination [69].
- Quantification and Quality Control:
- Use a microvolume spectrophotometer to determine RNA concentration and ensure the A260/A280 ratio is ~2.0.
- Run an Automated Electropherogram (e.g., Bioanalyzer/TapeStation): This is critical. The RNA Integrity Number (RIN) should be >7.0 for standard RNA-seq and >8.0 for single-cell or low-input applications. Look for sharp, distinct ribosomal RNA peaks and the absence of a "smear" towards lower molecular weights, which indicates degradation [68].
Protocol 2: Diagnostic Assay for RNase H Activity Using CRISPR/Cas12a
This highly sensitive protocol can detect aberrant RNase H activity, which is crucial for genomic stability and a potential confounder in sequencing [70].
- Prepare HybProbe: Generate a DNA/RNA hybrid probe via in vitro transcription from a template containing a T7 promoter sequence [70].
- Set Up Reaction:
- Combine in a tube:
- 1x NEBuffer 2
- 40 nM Cas12a enzyme
- 0.625 μM ssDNA fluorescence reporter (e.g., FAM-TTATTATT-BHQ1)
- 30 nM HybProbe complex
- Your test sample (e.g., cell extract from endometrial cells) [70].
- Combine in a tube:
- Incubate and Detect:
- Run the reaction in a real-time PCR machine at 37°C for 20 minutes, measuring fluorescence every minute.
- Interpretation: A increase in fluorescence signal indicates the presence of RNase H, which cleaves the RNA in the HybProbe, releasing a DNA activator that triggers trans-cleavage of the reporter by Cas12a [70]. This method can detect levels as low as 9.02 x 10â»Â¹â° U/μL [70].
The logical flow of this diagnostic assay is as follows:
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Protecting RNA Integrity
| Reagent / Kit | Function / Application | Specific Example (Supplier) |
|---|---|---|
| RNA Stabilization Reagent | Preserves RNA in tissues and cells immediately after collection/biorpsy. | RNAlater (Thermo Fisher) [7] |
| Total RNA Extraction Kit | Isolates high-quality, intact total RNA from tissue. | PureLink RNA Mini Kit (Thermo Fisher) [69] |
| Recombinant RNase Inhibitor | Protects RNA during enzymatic reactions (RT, PCR). | Protector RNase Inhibitor (Sigma-Aldrich) [71] |
| RNase H | Used in specific protocols to selectively degrade RNA in DNA-RNA hybrids. | Available from multiple biotech suppliers (e.g., TransGen Biotech) [70] |
| Synthetic Thermostable RNase Inhibitor | Protects RNA during high-temperature steps and in complex workflows. | SEQURNA [68] |
| ERCC RNA Spike-In Mix | External RNA controls for monitoring technical performance of RNA-seq assays. | ERCC ExFold RNA Spike-In Mixes (Thermo Fisher) [69] |
Visualizing the RNA Degradation Defense Strategy
A comprehensive defense strategy involves layering protections at every stage of your experimental workflow, from the patient biopsy to the final sequencing library.
Frequently Asked Questions
1. What is the main challenge with RNA-seq from mixed cell populations? The primary challenge is that data from a mixed population represents an averaged expression profile across all cell types present. This can mask critical, cell-specific gene expression signals, especially when the cell types have distinct or even opposite functions. In endometrial research, for example, this could obscure the distinct roles of epithelial and stromal cells in establishing receptivity [8].
2. My endometrial RNA-seq results show ambiguous receptivity markers. Could cellular heterogeneity be the cause? Yes. The human endometrium is composed of multiple cell types, including epithelial cells, stromal fibroblasts, endothelial cells, and various immune cells. If the proportion of these cells varies significantly between samples (e.g., due to biopsy technique or underlying pathology like endometriosis), the bulk RNA-seq signal can be confounded. Single-cell studies have shown that these cell types have unique transcriptomes, and their proportions can change with disease states [72].
3. What are my primary strategic options for managing heterogeneity? There are two core strategic paths, which can also be combined:
- Wet-Lab Strategy: Separate the cell populations before sequencing using techniques like fluorescence-activated cell sorting (FACS) based on known surface markers (e.g., CD9 for epithelial cells and CD13 for stromal cells in endometrium) [8].
- Computational Strategy: Sequence the mixed population and use bioinformatic tools post-sequencing to deconvolute the data and infer cell type-specific expression. This can be alignment-based or use alignment-free methods like convolutional neural networks [73].
4. When should I use single-cell RNA-seq (scRNA-seq) instead of bulk RNA-seq? scRNA-seq is the most powerful method for directly characterizing heterogeneity, as it profiles the transcriptome of individual cells. It is ideal for:
- Discovering new or rare cell subpopulations.
- Mapping cellular developmental trajectories (e.g., fibroblast differentiation in endometriosis) [72].
- Studying cell-to-cell interactions and variability. However, it is more expensive, technically demanding, and noisier than bulk RNA-seq. Bulk RNA-seq remains suitable for measuring overall transcript levels in a tissue, detecting low-abundance transcripts, and is more accessible for many laboratories [73] [72].
5. How does sample quality affect the choice of strategy? The quality and quantity of your RNA are critical. For low-quality or highly degraded RNA (e.g., from FFPE tissues), ribosomal RNA depletion (Ribo-Zero) or exome-capture (RNA Access) protocols outperform standard poly(A) selection, which is sensitive to RNA integrity [74]. For low-quantity samples, specialized low-input protocols are required, and the choice between cell sorting and direct sequencing depends on whether you can obtain enough cells for sorting without excessive amplification bias.
Troubleshooting Guides
Problem: Inconsistent Results from Endometrial Receptivity Tests
- Potential Cause: Variation in the cellular composition of sequential endometrial biopsies.
- Solution:
- Standardize biopsy collection: Ensure consistent anatomical location and depth for all biopsies.
- Document histology: Perform a parallel histological analysis to confirm the tissue composition and cycle stage for each sample.
- Adopt single-cell resolution: If resources allow, use scRNA-seq to build a definitive, cell-type-specific receptivity signature, moving beyond averages from bulk tissue [8] [72].
Problem: Suspected Contamination from Non-Target Cells
- Potential Cause: The tissue dissection or biopsy contains a significant amount of non-endometrial cell types (e.g., blood, myometrium).
- Solution:
- Optimize dissection: Carefully trim the tissue sample to remove visible non-target areas.
- Use cell sorting: Employ FACS or magnetic-activated cell sorting (MACS) to positively select your target cell population using validated surface markers before RNA extraction [8] [75].
- Bioinformatic decontamination: After sequencing, align reads to a combined human genome and a "contaminant" reference (e.g., mouse genome for xenograft models) to identify and filter out non-target reads. Alignment-based methods have been shown to achieve >97% accuracy in classifying reads by species [73].
Problem: Low RNA Yield from Sorted Cell Populations
- Potential Cause: Cell sorting procedures can be stressful to cells and may start with a low number of cells, resulting in minimal RNA.
- Solution:
- Optimize sorting conditions: Use a sorter with a large nozzle (e.g., 100 µm), keep the collection tube on ice, and use a collection buffer containing RNase inhibitors.
- Choose an appropriate RNA-seq kit: For low-input samples (down to 1 ng), ribosomal RNA depletion kits (e.g., Ribo-Zero) have been shown to perform robustly on both intact and degraded RNA, providing more accurate gene expression data than poly(A) selection methods in these scenarios [74].
- Include a whole-transcriptome amplification step if the input is extremely low, but be aware this may introduce amplification bias.
Experimental Protocols for Key Scenarios
Protocol 1: Cell Type-Specific Isolation and RNA-seq from Endometrial Biopsy
This protocol is designed to obtain separate expression profiles from epithelial and stromal compartments [8].
- Tissue Collection & Transport: Collect endometrial biopsy in sterile PBS or a specialized transport medium like RNAlater. Process immediately or store at 4°C for short periods.
- Tissue Dissociation: Mince the tissue finely and digest using a combination of collagenase and DNase in a shaking incubator at 37°C for 60-90 minutes.
- Cell Staining: Resuspend the single-cell suspension and incubate with fluorescently conjugated antibodies against surface markers. For human endometrium, use anti-CD9-APC (epithelial cell marker) and anti-CD13-FITC (stromal fibroblast marker) [8].
- Cell Sorting: Using a FACS sorter, collect the CD9+ epithelial cells and the CD13+ stromal cells into separate tubes containing lysis buffer with RNase inhibitors.
- RNA Extraction & QC: Extract total RNA using a column-based method. Assess RNA quantity and integrity (RIN > 7.0 is desirable).
- Library Preparation & Sequencing: For low-input amounts from sorted cells, use a ribosomal RNA depletion protocol (e.g., Illumina's Ribo-Zero) followed by library construction. Sequence on an Illumina platform.
Protocol 2: Computational Deconvolution of Mixed-Species RNA-seq Data
This method is useful for analyzing data from co-cultures or xenograft models, distinguishing human-specific signals from mouse-specific ones [73].
- Sequencing & Raw Data Generation: Perform standard bulk RNA-seq on the mixed cell population.
- Alignment to a Pooled Reference Genome:
- Create a concatenated reference genome (e.g.,
hg38+mm10). - Align the raw sequencing reads (FASTQ files) to this pooled genome using a splice-aware aligner like HISAT2.
- Create a concatenated reference genome (e.g.,
- Read Classification:
- Parse the alignment file (BAM). Classify each read pair as "human" or "mouse" based on its primary alignment to a chromosome in the respective genome.
- Re-alignment and Quantification:
- Separate the reads classified as "human" and "mouse" into new FASTQ files.
- Re-align the human reads to the human genome (hg38) and the mouse reads to the mouse genome (mm10) independently.
- Perform transcript quantification (e.g., using featureCounts) on the separate alignment files to generate accurate, species-specific gene counts.
Table 1: Comparison of Computational Deconvolution Methods
| Method | Principle | Pros | Cons | Best For |
|---|---|---|---|---|
| Alignment-Based (Pooled Genome) [73] | Aligns reads to a combined reference genome, then classifies by origin. | High accuracy (>97%), lower error rates, uses established tools. | Computationally intensive, requires multiple alignment steps. | Most applications, especially when high accuracy is critical. |
| Alignment-Free (CNN-based) [73] | Uses machine learning (Convolutional Neural Networks) to classify reads by sequence patterns. | Time-efficient, does not require reference alignment. | Lower accuracy (~85%) compared to alignment-based methods. | Rapid screening or when a high-quality reference genome is unavailable. |
Research Reagent Solutions
Table 2: Essential Materials for Managing Heterogeneity
| Item | Function | Example Product(s) |
|---|---|---|
| Cell Sorting Markers (Human) | Antibodies for isolating specific endometrial cell populations by FACS/MACS. | Anti-CD9 (Epithelial cells), Anti-CD13 (Stromal cells) [8] |
| RNase Inhibitor | Prevents degradation of RNA during and after cell sorting, crucial for preserving sample integrity. | Included in Takara Bio Lysis Buffer, other commercial RNase inhibitors [76] |
| Low-Input RNA-seq Kit | Library preparation kits designed for minimal RNA input, often utilizing rRNA depletion. | Illumina Ribo-Zero, TruSeq RNA Access [74] |
| Single-Cell RNA-seq Platform | Integrated solutions for capturing single cells and preparing sequencing libraries. | 10x Genomics Chromium System [72] |
Workflow Visualization
The following diagram illustrates the two main strategic pathways for addressing sample heterogeneity, from sample collection to data analysis.
Decision Workflow for Heterogeneity
Signaling Pathways in Endometrial Cell Populations
Single-cell transcriptomic studies have revealed that different cell types in the endometrium activate distinct signaling pathways. For example, in endometriosis, fibroblasts in lesions show upregulation of pathways related to inflammation and hormone synthesis compared to normal endometrium [72]. The following diagram summarizes key pathways and their cellular context.
Pathways in Endometrial Cells
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of using RNA-seq over histology for endometrial dating? Traditional histology (Noyes' criteria) is subjective and often lacks reproducibility for pinpointing the window of implantation (WOI). In contrast, RNA-seq-based molecular staging analyzes the expression of hundreds of genes (e.g., 175 biomarkers in the rsERT), providing an objective, quantitative, and highly accurate assessment of endometrial receptivity status, which leads to better synchronization between the embryo and endometrium [77] [15].
Q2: My endometrial RNA-seq samples show low RNA integrity. What are the critical pre-analytical steps to prevent this? Optimal RNA quality begins at the biopsy stage. Key steps include:
- Rapid Processing: Minimize the time from tissue collection to preservation. One established protocol completes tissue disaggregation, cell-specific labelling, and sorting within 90 minutes at low temperature to preserve the gene expression profile [8].
- Proper Preservation: Immediately place the endometrial biopsy in a specialized RNA stabilization buffer (e.g., RNAlater) and store at -80°C to prevent degradation [77] [7].
Q3: How does molecular staging handle patient-specific variability in the window of implantation (WOI)? Molecular models like the RNA-seq-based Endometrial Receptivity Test (rsERT) are designed to diagnose a displaced WOI. The test can classify the endometrium as pre-receptive, receptive, or post-receptive. For patients with a displaced WOI, the test calculates a personalized embryo transfer (pET) timing, shifting the transfer to synchronize with the individual's unique receptive period [77] [7] [15].
Q4: Are there specific considerations for preparing endometrial samples from patients with PCOS for RNA-seq analysis? Yes, research indicates that the endometrium of patients with Polycystic Ovary Syndrome (PCOS) may exhibit altered transcriptomic profiles and delayed decidualization, which can affect receptivity [78]. While a 2025 RCT showed that rsERT-guided pET did not improve pregnancy rates in PCOS patients without recurrent implantation failure (RIF), the molecular differences underscore the importance of rigorous patient stratification and the potential need for tailored bioinformatic analysis when studying such cohorts [78].
Troubleshooting Guides
Issue 1: High Sample-to-Sample Variability in Gene Expression Profiles
A lack of consistency in sample processing can introduce significant technical noise, obscuring true biological signals.
- Potential Cause & Solution
- Cause: Inconsistent endometrial biopsy handling, processing times, or storage conditions.
- Solution: Implement a Standardized Operating Procedure (SOP).
- Sample Collection: Use a consistent biopsy technique and location.
- Time to Preservation: Record and minimize the time from biopsy to immersion in RNAlater or flash-freezing.
- Storage: Ensure uninterrupted storage at -80°C and avoid freeze-thaw cycles.
- Batch Effects: Process samples from different clinical groups (e.g., healthy vs. tumor) in parallel to minimize technical batch effects, a critical consideration highlighted in studies comparing healthy and tumor endometrial tissues [9].
Issue 2: Low RNA Yield or Quality from Luminal Epithelial Cells
Single-cell or population-specific transcriptomics can be challenging due to the fragility of certain cell types.
- Potential Cause & Solution
- Cause: High levels of RNases released during natural cell processes, particularly in epithelial cells, leading to rapid RNA degradation [8].
- Solution:
- Optimized Dissociation: Use gentle, cold-activated enzymatic dissociation protocols to preserve RNA integrity.
- Cell Sorting: Utilize rapid, fluorescence-activated cell sorting (FACS) with specific surface markers (e.g., CD9 for epithelial cells, CD13 for stromal cells) at low temperatures to isolate viable cells [8].
- Protocol Validation: Always check RNA quality (e.g., using RIN) after sorting and before proceeding to library preparation.
Issue 3: Suspected Sample Contamination
Unexpected sequences in RNA-seq data can lead to erroneous conclusions.
- Potential Cause & Solution
- Cause: Cross-contamination during sample processing or the presence of microbial organisms.
- Solution:
- Bioinformatic Screening: Perform a dedicated computational analysis of unmapped sequence reads to identify potential viral or bacterial contaminants. This is crucial, as evidenced by the discovery of HPV sequences in endometrial cancer samples from TCGA, which was later suggested to be a batch-specific contamination [79].
- Process Review: Audit laboratory protocols to prevent cross-contamination between samples processed in the same batch.
Experimental Protocols for Endometrial RNA-seq
Protocol 1: Endometrial Biopsy Processing for Bulk RNA-seq
1. Patient Preparation & Biopsy:
- For hormone replacement therapy (HRT) cycles, administer estrogen followed by progesterone. The first day of progesterone supplementation is designated P+0 [77].
- Perform an endometrial biopsy using a standard pipelle sampler on the specified day (e.g., P+5 for a standard receptivity check) [7] [15].
2. Tissue Stabilization:
- Immediately rinse the biopsy in saline to remove blood.
- Place the tissue directly into 1.5 mL of RNAlater buffer.
- Seal the tube and cryopreserve at -80°C. Sequencing should ideally be performed within 7 days [7].
3. RNA Extraction & Sequencing:
- Homogenize the stabilized tissue.
- Extract total RNA using a column-based kit with DNase I treatment.
- Assess RNA quality and quantity (e.g., Bioanalyzer, Qubit).
- Construct sequencing libraries from high-quality RNA (RIN > 7) using a stranded mRNA-seq library prep kit.
- Sequence on an Illumina platform to a minimum depth of 30 million paired-end reads per sample.
Protocol 2: Single-Cell RNA-seq from Endometrial Biopsies
1. Tissue Dissociation and Cell Sorting:
- Cryopreserve the biopsy and use a frozen-thawed method for dissociation. Single-nuclei RNA-seq (snRNA-seq) can be a superior alternative for archived tissues or hard-to-dissociate cells, reducing dissociation bias [80].
- Alternatively, for fresh tissue, perform rapid enzymatic dissociation at low temperatures [8].
- Label cells with fluorescent antibodies (e.g., anti-CD13 for stromal cells, anti-CD9 for epithelial cells).
- Use FACS to sort live, target cells directly into lysis buffer.
2. Library Preparation and Bioinformatics:
- Perform single-cell RNA-seq library preparation using a high-throughput platform (e.g., 10x Genomics).
- For data analysis, use tools like Seurat or Scanpy for quality control, normalization, clustering, and differential expression analysis. This allows for the dissection of cellular heterogeneity and the identification of rare cell populations in the endometrium [80] [8].
The Scientist's Toolkit: Essential Research Reagents
Table 1: Key Reagents for Endometrial RNA-seq Research
| Reagent/Material | Function in the Protocol | Specific Example / Note |
|---|---|---|
| RNAlater Stabilization Buffer | Preserves RNA integrity immediately after biopsy by inhibiting RNases. | Critical for maintaining accurate transcriptome profiles during transport and storage [77] [7]. |
| Hormones for HRT Cycle | Creates a synchronized, artificial menstrual cycle for timing the biopsy. | Estradiol and progesterone; allows for precise timing relative to progesterone administration (e.g., P+5) [77] [15]. |
| Cell Surface Markers (Antibodies) | Enables isolation of specific endometrial cell populations via FACS. | Anti-CD13 for stromal cells; Anti-CD9 for epithelial cells [8]. |
| Single-Cell/Nuclei RNA-seq Kits | For generating sequencing libraries from individual cells or nuclei. | 10x Genomics Chromium; snRNA-seq is advantageous for frozen tissues [80] [8]. |
| ERα Antibody | For chromatin immunoprecipitation (ChIP-seq) to study transcriptional regulation. | Used in integrative multi-omics studies to map enhancer activity in endometrial cancer [9]. |
Workflow and Pathway Diagrams
Endometrial Receptivity Testing Workflow
The following diagram illustrates the complete clinical and laboratory workflow for implementing an RNA-seq-based endometrial receptivity test, from patient preparation to personalized embryo transfer.
ERα Epigenetic Reprogramming in Tumorigenesis
This diagram summarizes the complex epigenetic and genomic interplay in endometrial cancer development, as revealed by integrated multi-omics approaches, explaining how non-coding mutations can drive cancer by altering 3D genome structure.
Table 2: Key Quantitative Findings from Recent Endometrial Transcriptomic Studies
| Study Focus | Key Metric | Result / Value | Context and Implication |
|---|---|---|---|
| ERα Binding in EC [9] | Differentially bound ERα sites (Tumor vs. Normal) | 10,292 sites (6,488 lost; 3,804 gained) | Identifies profound ERα enhancer plasticity during endometrial tumorigenesis. |
| rsERT vs. Pinopode [77] | Clinical Pregnancy Rate | 50.0% (rsERT) vs. 16.7% (Pinopode) | Supports superior diagnostic performance of transcriptomic tools over morphological assessment. |
| rsERT in PCOS (no RIF) [78] | Intrauterine Pregnancy Rate | 60.0% (pET) vs. 61.2% (FET) | Suggests rsERT may not be beneficial for all patient populations (e.g., PCOS without RIF). |
| Natural vs. Programmed FET [81] | Live Birth Rate | 51.2% (Natural) vs. 50.1% (Programmed) | Natural cycles show equal efficacy but significantly better maternal safety outcomes. |
| ERα Genomic Distribution [9] | Tumor-enriched ERα sites at promoters | ~5% | Confirms tumor-specific ERα binding is overwhelmingly at distal enhancer regions. |
Optimizing Cell Viability and Input for Single-Cell Genomics
Single-cell RNA sequencing (scRNA-seq) has revolutionized biological research by enabling the characterization of genome-scale molecular information at the individual cell level, providing unprecedented insights into cellular heterogeneity and complexity. For researchers working with clinically relevant samples such as endometrial tissue, optimizing cell viability and input is paramount to generating robust, high-quality data. This technical support center addresses the specific challenges and solutions for preparing viable single-cell suspensions from delicate tissue types, with a particular focus on endometrial RNA-seq protocols, providing essential troubleshooting guides and FAQs to support your research success.
Single-cell genomics workflows present several common challenges that can compromise data quality. The table below summarizes key issues and their impact on experiments, particularly in the context of endometrial research.
Table 1: Key Challenges in Single-Cell Genomics with Endometrial Tissue Applications
| Challenge | Impact on Data Quality | Endometrial-Specific Considerations |
|---|---|---|
| Low Cell Viability [82] | Compromised data utility; fails platform viability thresholds (typically ≥80%) [82] | Increased vulnerability due to tissue dissociation sensitivity [83] |
| RNA Dropout [82] | Incomplete transcriptome representation; missing low-abundance transcripts | Epithelial cells particularly susceptible due to high RNase activity [83] [8] |
| Artificial Stress Responses [84] | Altered transcriptional profiles; inaccurate cell type identification | Dissociation at 37°C induces stress genes; low-temperature processing recommended [84] |
| Inaccurate Cell/Nuclei Counting [82] | Suboptimal sequencing library preparation; data artifacts | Critical for library prep to minimize unlysed cells and debris [82] |
Frequently Asked Questions (FAQs) and Troubleshooting Guides
FAQ 1: What is the minimum cell viability required for a successful single-cell RNA-seq experiment, and how can I achieve it with endometrial biopsies?
Most single-cell sequencing platforms recommend a minimum cell viability threshold of 80% or above to ensure generated data truly represents the living cell population. [82] Low viability compromises data relevance and wastes valuable sequencing resources.
Troubleshooting Guide for Improving Viability:
- Implement Dead Cell Removal: Use magnetic cell separation systems, such as dead cell removal kits that employ negative selection to selectively remove dead and dying cells from your suspension before loading samples into the single-cell workflow. [82]
- Optimize Tissue Dissociation: For endometrial tissue, perform physical and enzymatic dissociation at low temperatures (e.g., 4°C) when possible. While dissociation at 4°C requires longer incubation times, it significantly minimizes the induction of artificial transcriptional stress responses that occur at 37°C. [84] [83]
- Cryopreservation Best Practices: When processing biopsies, use proper cryopreservation media containing DMEM with 30% fetal bovine serum (FBS) and 7.5% DMSO. Use a controlled freezing container and store frozen biopsies in liquid nitrogen to conserve intact, living cells for subsequent sorting. [83]
FAQ 2: How can I overcome the challenge of RNA dropout, especially in sensitive endometrial epithelial cells?
RNA dropout, where lowly expressed genes are not detected, is a major challenge in scRNA-seq. This is especially pertinent for endometrial epithelial cells, which can have low RNA data yield due to high natural RNase activity. [83] [8]
Troubleshooting Guide for Reducing RNA Dropout:
- Adopt Multi-Omics Approaches: Implement CITE-seq (Cellular Indexing of Transcriptomes and Epitopes by Sequencing). This method combines gene expression profiling with the measurement of surface protein markers using oligonucleotide-labeled antibodies (e.g., TotalSeq reagents). [82] As protein is more abundant than RNA, this provides a more consistent detection method to help characterize cell types and states, thereby compensating for transcriptional dropouts.
- Utilize Unique Molecular Identifiers (UMIs): Ensure your scRNA-seq protocol incorporates UMIs. These barcodes label each individual mRNA molecule during reverse transcription, improving quantitative accuracy by effectively eliminating PCR amplification bias and providing a more digital readout of transcript counts. [84]
- Consider Single-Nucleus RNA-seq (snRNA-seq): For tissues like endometrium that are difficult to dissociate or are particularly sensitive, snRNA-seq can be a viable alternative. It sequences mRNA from the nucleus and minimizes artificial stress responses induced by whole-cell dissociation. It is also applicable for frozen samples. [84]
FAQ 3: What is the best method for accurate cell counting prior to library preparation, and why is it critical?
Accurate nuclei counting is crucial for reliable downstream analysis and to prevent issues like cell aggregation or low capture efficiency during library preparation. [82]
Troubleshooting Guide for Accurate Cell Counting:
- Embrace Automated Cell Counters: Replace manual counting with automated cell counters (e.g., Cellaca PLX). Automation efficiently handles large sample quantities, removes user bias, and provides standardized, reproducible results. [82] These systems often have low volume requirements, preserving limited sample material.
- Use Fluorescent Staining: Utilize fluorescent dyes that specifically bind to DNA to visualize and enumerate individual cell nuclei. This allows for better distinction between intact cells/nuclei and cellular debris compared to brightfield methods. [82]
- Filter Suspensions: Before counting and loading, filter your single-cell suspension through appropriate strainers (e.g., 50µm and 35µm filters) to remove undigested tissue fragments and large aggregates that could clog microfluidic devices. [83]
Experimental Protocols for Endometrial scRNA-seq
The following workflow diagram and detailed protocol outline a optimized method for preparing single-cell suspensions from endometrial biopsies for scRNA-seq, incorporating strategies to maximize viability and data quality.
Diagram 1: Endometrial scRNA-seq workflow.
Detailed Protocol for Endometrial Tissue Single-Cell Suspension [83] [8]:
Sample Collection & Cryopreservation: Immediately place the endometrial biopsy obtained via Pipelle catheter into cryopreservation medium (1x DMEM, 30% FBS, 7.5% DMSO). Place the vial in a controlled-rate freezing container at -80°C overnight, then transfer to long-term storage in liquid nitrogen. This preserves cell integrity.
Thawing & Dissociation: Thaw the frozen biopsy rapidly and wash twice with DMEM. Dissociate the tissue in DMEM containing 0.5% collagenase. Critical: Perform this dissociation step at 4°C with shaking to minimize artificial stress responses, even though it requires longer incubation (e.g., >20 min). [84] [83]
Single-Cell Suspension Preparation: After dissociation, add ice-cold FBS to stop the reaction. Use ACK lysing buffer to remove red blood cells. Centrifuge the suspension and resuspend the pellet in ice-cold PBS with 5% FBS. Filter the suspension sequentially through 50µm and 35µm cell strainer caps to obtain a clean single-cell suspension.
Cell Sorting & Viability Enhancement: Stain the single-cell suspension with fluorophore-conjugated antibodies (e.g., CD13 for stromal cells, CD9 for epithelial cells) on ice. Perform Fluorescence-Activated Cell Sorting (FACS) to isolate specific cell populations. The entire process from thawing to sorting should be completed within 90 minutes at low temperature to preserve the native gene expression profile. Optionally, use a dead cell removal kit (e.g., MojoSort) prior to FACS to enrich for viable cells. [83] [82]
Downstream Processing: Lyse sorted single cells immediately and proceed with your chosen scRNA-seq library preparation protocol, ensuring it includes barcoding and UMIs for optimal data quality. [84]
Research Reagent Solutions
The table below lists key reagents and tools essential for optimizing cell viability and input in single-cell genomics, with specific applications for challenging samples like endometrial tissue.
Table 2: Essential Research Reagents for Single-Cell Genomics
| Reagent / Tool | Function | Application in Endometrial Research |
|---|---|---|
| Dead Cell Removal Kit [82] | Magnetic negative selection to remove dead/dying cells | Improves viability prior to FACS or library loading; crucial for low-viability biopsies. |
| Collagenase [83] | Enzymatic digestion of tissue matrix | Dissociates endometrial biopsy into single-cell suspension; use at low temperature (4°C). |
| Fetal Bovine Serum (FBS) [83] | Component of cryopreservation and wash buffers | Protects cells during freezing and quenching of enzymatic reactions. |
| FACS Antibodies (CD13, CD9) [83] [8] | Cell surface markers for specific cell type isolation | Enables sorting of endometrial stromal (CD13+) and epithelial (CD9+) cells. |
| TotalSeq Antibodies [82] | Oligonucleotide-labeled antibodies for CITE-seq | Combats RNA dropout by adding protein expression data to transcriptomic data. |
| Unique Molecular Identifiers (UMIs) [84] | Barcodes for individual mRNA molecules | Corrects for PCR amplification bias, improving quantitative accuracy of scRNA-seq. |
| DMEM with DMSO [83] | Cryopreservation medium | Maintains cell viability during freezing and long-term storage of biopsies. |
Successful single-cell genomics, particularly with complex tissues like the endometrium, hinges on meticulous attention to sample preparation. By prioritizing high cell viability through optimized dissociation and handling protocols, employing strategies to mitigate technical artifacts like RNA dropout, and utilizing accurate quality control measures, researchers can unlock the full potential of scRNA-seq to reveal cellular heterogeneity and drive meaningful discoveries in biomedical research.
Pre-Sequence Quality Control: Assessing Library Quality
What is the purpose of running my library on a Bioanalyzer before sequencing?
The Agilent Bioanalyzer uses micro-capillary electrophoresis to provide a detailed profile of your nucleic acid samples. For RNA-seq libraries, it is used to:
- Confirm Expected Library Size: Determine the average size of your library fragments, ensuring they fall within the optimal range for your sequencing platform [85] [86].
- Check Library Profile: Identify the presence of a single, clean peak corresponding to your library and confirm the absence of adapter dimers (a small peak around ~120-150 bp) or other contamination like primer dimers or genomic DNA (large peaks) [86].
- Assess Sample Integrity: While not recommended for absolute quantification, it provides a visual assessment of the sample's size distribution and integrity [85].
An ideal final library trace should show a single, narrow peak with a smooth distribution and no secondary peaks in the lower or higher size regions [86].
My Bioanalyzer trace shows a small peak around 150 bp. What does this mean and how can I correct it?
A small peak around 120-150 bp typically indicates the presence of adapter dimers, which are adapters that have ligated to each other without a cDNA insert [86].
- Cause: This is often the result of an excess of adapters during the ligation step, inefficient size selection, or using a starting RNA sample that is degraded or of low quantity.
- Solution: To prevent this in future preps:
- Optimize Adapter Concentration: Titrate the amount of adapter used in the ligation reaction.
- Perform Strict Size Selection: Use bead-based cleanups with optimized bead-to-sample ratios or perform manual size selection via gel extraction to remove short fragments effectively [86].
- Verify RNA Quality: Always start with high-quality, high-integrity RNA (RIN > 8) to ensure efficient cDNA synthesis and adapter ligation.
Which Bioanalyzer kit should I use for my RNA-seq library?
The choice of kit depends on your sample type and concentration [85]:
| Kit Name | Sensitivity Range | Samples per Chip | Recommended Use |
|---|---|---|---|
| RNA 6000 Nano Kit | 25–500 ng/µL | 12 | Standard analysis of total RNA quality and quantity; assessing fragmented RNA. |
| RNA 6000 Pico Kit | 0.5–2 ng/µL | 11 | For low-concentration RNA samples. |
| Small RNA Kit | 1–100 ng/µL (total RNA) | 11 | Specifically for analyzing microRNAs and other small RNAs. |
Sequencing and Data Quality Control
How can I monitor error rates during Illumina sequencing?
While Illumina's Sequencing Analysis Viewer (SAV) provides a quality score (Q-score), this metric can be overestimated and is platform-dependent [87] [88]. A robust alternative is the Percent Perfect Reads (PPR) metric.
- Principle: PPR uses an external control, typically a PhiX bacteriophage genome spiked into your sequencing run, to directly measure the intrinsic error rate [88]. It calculates the percentage of PhiX reads that have 0, ≤1, ≤2, ≤3, or ≤4 mismatches to the reference genome on a cycle-by-cycle basis.
- Advantages:
- Provides a direct, unbiased measurement of the error rate.
- Allows for cross-instrument comparison (e.g., HiSeq, MiSeq, NextSeq) [87].
- The resulting plot is rich in information and excellent for troubleshooting specific sequencing issues, such as a sudden drop in quality or errors localized to a specific part of the read [88].
My sequencing run failed with a "component failure" error. What should I do?
For a "component failed during sequencing" error on an Illumina NovaSeq 6000, the troubleshooting steps depend on when the error occurs [89]:
- Error within the first 10 minutes:
- Confirm that the reagent cartridges are unpierced and no run folder has been generated.
- Contact Illumina Technical Support with your Run ID.
- Error mid-run:
- If the other flow cell side (lane) is idle, perform a full power cycle on the instrument.
- If the instrument initializes successfully after the power cycle, you can continue sequencing on the side that did not have an error.
- Collect the required cycle logs and control software logs, then contact Illumina Technical Support for further instructions on the failed side [89].
Endometrial-Specific RNA-seq Considerations
What is the best RNA-seq library preparation method for degraded or low-quantity endometrial samples?
The optimal protocol depends on the quality and quantity of your endometrial RNA. A comprehensive study compared three main approaches [74]:
| Protocol Type | Representative Kit | Intact RNA Performance | Degraded RNA Performance | Highly Degraded RNA Performance |
|---|---|---|---|---|
| Poly(A) Enrichment | TruSeq Stranded mRNA | Excellent at recommended inputs (100 ng) | Performance drops with quality | Not recommended |
| Ribosomal RNA Depletion | Ribo-Zero Gold rRNA Removal | Excellent down to 10 ng; good alignment at 1 ng | Best performance for degraded samples, accurate even at 1-2 ng | Poor performance; substantial loss of aligned reads |
| Exome Capture | RNA Access | Good and constant alignment across inputs (1-100 ng) | Good performance | Best performance; reliable data down to 5 ng input |
Recommendation for Endometrial Research:
- For fresh-frozen endometrial biopsies with high-quality RNA, poly(A) enrichment is a standard and sensitive choice.
- For FFPE-derived endometrial samples, which are typically highly degraded, the RNA Access (exome capture) protocol is superior as it targets specific exons and is less dependent on RNA integrity [74].
- For low-input samples like endometrial fluid or single-cell preparations, rRNA depletion methods have been shown to work well with inputs as low as 1 ng [74]. This is corroborated by studies using single-cell RNA-seq to analyze endometrial tissues [90].
How should I handle and preserve endometrial tissue for RNA-seq?
Proper sample handling is critical to prevent RNA degradation, which is a major source of bias [34].
- Gold Standard: The best preservation method for transcriptomic studies is immediate snap-freezing in liquid nitrogen and storage at -80°C [34].
- FFPE Tissues: While formalin-fixed paraffin-embedded (FFPE) tissues are widely available, the fixation process causes RNA fragmentation, cross-linking, and chemical modifications [34]. If using FFPE samples:
- Use a high sample input during library preparation to compensate for degradation.
- In the reverse transcription step, use random primers instead of oligo-dT, as the latter will fail to bind to degraded transcripts lacking poly-A tails [34].
- RNA Extraction: For optimal yield and quality from endometrial tissue, the mirVana miRNA isolation kit has been reported as one of the best methods [34]. Always use RNase-free reagents and equipment to prevent RNA degradation by ubiquitous RNases.
The Scientist's Toolkit: Essential Reagents and Kits
| Item | Function/Application |
|---|---|
| Agilent Bioanalyzer 2100 | Micro-capillary electrophoresis system for assessing nucleic acid sample integrity, size distribution, and approximate quantification [85] [86]. |
| RNA 6000 Nano/Pico Kits | Bioanalyzer assays for analyzing total RNA integrity and quantifying ribosomal ratios (RIN) [85]. |
| High Sensitivity DNA Kit | Bioanalyzer assay for precise sizing and quantification of DNA libraries, crucial for final library QC [85]. |
| TruSeq Small RNA Library Prep Kit | Protocol for constructing sequencing libraries specifically for microRNAs and other small non-coding RNAs, commonly used in endometrial studies [2]. |
| PhiX Control v3 | A highly stable bacteriophage genome used as a spike-in control for sequencing runs to monitor error rates, calculate cluster density, and align sequences [88]. |
| mirVana miRNA Isolation Kit | A robust method for purifying high-quality total RNA, including small RNAs, from challenging samples like tissue [34]. |
| TruSeq RNA Access Library Prep Kit | An exome-capture based protocol designed to profile degraded and low-quality RNA samples, such as those from FFPE tissue [74]. |
Experimental Workflow and Quality Control Decision Diagram
The following diagram outlines the key quality control checkpoints in a typical endometrial RNA-seq workflow, from sample preparation to data acquisition.
Ensuring Analytical Rigor and Translational Relevance
Sample Type Comparison and Selection Guide
The choice of sample type for endometrial transcriptomic analysis is critical, as each offers distinct advantages and limitations regarding invasiveness, biological richness, and technical handling.
Table 1: Comparative Analysis of Endometrial RNA-seq Sample Types
| Feature | Endometrial Tissue Biopsy | Uterine Fluid Extracellular Vesicles (UF-EVs) | Menstrual Effluence (Tampon-Based) |
|---|---|---|---|
| Invasiveness | Invasive (Pipelle catheter) [91] | Minimally invasive (Uterine lavage) [92] | Non-invasive (At-home collection) [12] |
| Primary RNA Source | Whole tissue: epithelium, stroma, endothelium [83] | EV-encapsulated RNA (mRNA, miRNA) from endometrial cells [91] [92] | Shed endometrial tissue, immune cells, microbiota [12] |
| Correlation to Endometrial Tissue | Gold standard (reference) | High (Pearson's r = 0.70) [91] | High transcriptomic profile similarity to tissue-derived organoids [12] |
| Key Advantage | Direct tissue profiling; single-cell resolution possible [83] | "Liquid biopsy"; reflects functional secretory activity; can be performed in the same cycle as embryo transfer [91] [92] | Allows for frequent, longitudinal sampling; ideal for large-scale studies [12] |
| Main Limitation | Cannot be performed immediately before embryo transfer; site-specific sampling [92] | Requires specialized EV isolation protocols; complex data analysis [91] [93] | Represents the menstrual breakdown phase, not the receptive window [12] |
| Sample Stability | Requires immediate freezing or cryopreservation [83] | Stable in uterine fluid | RNA stable at ambient temperature for up to 14 days in preservation buffer [12] |
Detailed Experimental Protocols
Protocol: Endometrial Tissue Biopsy for Single-Cell RNA-seq
This protocol enables the study of cell-to-cell heterogeneity within the endometrium [83].
- Sample Collection & Cryopreservation: Collect biopsy using a Pipelle catheter. Immediately place tissue into cryopreservation medium (e.g., DMEM with 30% FBS and 7.5% DMSO). Freeze slowly at -80°C using a "Mr. Frosty" container, then transfer to liquid nitrogen for storage [83].
- Tissue Disaggregation: Thaw sample and wash. Dissociate in DMEM with 0.5% collagenase at 37°C for ~20 minutes with shaking. Quench with FBS and lyse red blood cells. Filter suspension through 50µm and 35µm strainers to obtain single cells [83].
- Fluorescence-Activated Cell Sorting (FACS): Label cells with fluorescent antibodies (e.g., anti-CD13 for stromal cells, anti-CD9 for epithelial cells). Sort live, single cells into lysis buffer. Critical: Complete the entire process from disaggregation to sorting within 90 minutes on ice to minimize gene expression changes [83].
- Library Preparation & Sequencing: Use a single-cell RNA-seq method such as a modified Single-cell Tagged Reverse Transcription (STRT) protocol to construct Illumina-compatible libraries [83].
Protocol: Isolation and RNA-seq of UF-EVs
This protocol outlines a method for a less-invasive assessment of endometrial receptivity [91] [92].
- Uterine Fluid Collection: Perform lavage of the uterine cavity during the desired cycle phase (e.g., LH+2 for pre-receptive, LH+7 for receptive). Fresh-process samples for optimal results [91].
- EV Isolation & Validation: Isolate EVs from UF via ultracentrifugation or commercial kits. Validate isolation using Western Blot for EV protein markers (e.g., CD63, CD81). Characterize physical properties (size, concentration) using Nanoparticle Tracking Analysis [91] [92].
- RNA Extraction & Library Prep: Extract total RNA from the isolated UF-EVs. Prepare RNA-seq libraries using kits designed for low-input RNA. Sequence on a platform such as Illumina NextSeq2000 [91] [93].
- Bioinformatic Analysis: Process data through alignment (e.g., to hg38 genome) and gene count quantification. Conduct differential gene expression analysis and gene set enrichment analysis (GSEA) to identify receptivity-associated pathways [91] [93].
Protocol: At-Home Collection of Menstrual Effluence
This protocol enables decentralized, population-scale sampling for genomic and transcriptomic analysis [12].
- Standardized Collection: Participants use a specific organic cotton tampon for a standardized duration (e.g., 4 hours) during the first few days of menstruation [12].
- Immediate Preservation: After collection, the tampon is sealed in a jar containing a nucleic acid preservation buffer (e.g., from Norgen Biotek). This is critical for preventing RNA degradation during transport [12].
- Shipment & Processing: Participants return the kit via standard mail at ambient temperature. Upon receipt, the lab processes the sample, which includes extrusion, centrifugation, and aliquoting for storage at -80°C before nucleic acid extraction [12].
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: Our RNA yields from UF-EVs are low and variable. How can we improve this?
- A: Low RNA yield from UF-EVs is a common challenge. Ensure you are starting with an adequate volume of uterine fluid. Concentrate your sample via ultracentrifugation and use RNA extraction kits specifically optimized for low-concentration and fragmented RNA, such as those with carrier RNA. Always profile your isolated EVs with Nanoparticle Tracking Analysis and Western Blot to confirm you have successfully isolated a vesicle population before proceeding to RNA extraction [91] [92].
Q2: We detect high ribosomal RNA in our endometrial tissue total RNA-seq. What is the best method for rRNA removal?
- A: For eukaryotic mRNA-seq, poly(A) selection is the standard method to enrich for polyadenylated mRNA and deplete rRNA. As an alternative, especially if studying non-polyadenylated RNAs, use probe-based ribosomal RNA depletion kits (e.g., Ribo-Zero). These are also the only option for prokaryotic RNA or heavily degraded RNA from FFPE samples [34].
Q3: Our single-cell data from endometrial biopsies has a high background from non-viable cells. How can we mitigate this?
- A: Cell viability is paramount. Key steps include:
- Minimize Warm Ischemia: Process the biopsy immediately upon collection.
- Optimized Dissociation: Use a controlled enzymatic dissociation protocol (e.g., 0.5% collagenase for <20 min) and perform it at low temperature (4°C) if possible, though duration will be longer.
- Viability Staining: Incorporate a live/dead fluorescent dye (e.g., propidium iodide) during FACS to gate out non-viable cells.
- Speed: Keep the tissue and cells cold and complete the disaggregation-to-sorting pipeline within 90 minutes [83].
Q4: Can we use menstrual fluid to assess the window of implantation (WOI)?
- A: No, not directly. Menstrual fluid is a snapshot of the shedding endometrium at the end of the cycle (late-secretory and menstrual phases). It is biologically distinct from the mid-secretory endometrium, which is when the window of implantation opens. Therefore, menstrual fluid is excellent for studying conditions like endometriosis or for genetic screening, but it cannot be used to profile the receptive state for embryo implantation [12] [92].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for Endometrial RNA-seq Workflows
| Reagent / Kit | Function | Application Note |
|---|---|---|
| Pipelle Catheter | Minimally invasive endometrial tissue biopsy collection. | Standard of care for clinical endometrial sampling [91] [83]. |
| Collagenase, Type IV | Enzymatic dissociation of biopsy tissue into single-cell suspensions. | Concentration and incubation time must be optimized to balance yield and cell viability [83]. |
| FACS Antibodies (CD13, CD9) | Fluorescent labeling of stromal (CD13) and epithelial (CD9) cells for sorting. | Enables population-specific analysis from a heterogeneous tissue sample [83]. |
| Norgen Biotek Preservation Buffer | Stabilizes RNA in self-collected samples at ambient temperature. | Critical for maintaining RNA integrity in menstrual effluence during postal transport [12]. |
| RNA Extraction Kit (e.g., mirVana) | Isolation of high-quality total RNA, including small RNAs. | Superior for yields from difficult sources like menstrual fluid compared to TRIzol [34]. |
| Zymo-Seq RiboFree Total RNA Library Kit | Preparation of RNA-seq libraries without rRNA depletion. | Used successfully for metatranscriptomic profiling of menstrual effluence [12]. |
Frequently Asked Questions (FAQs) on Endometrial RNA-seq Analysis
Q1: What are the most critical quality control metrics to check after sequencing and why? The most critical QC metrics depend on your sequencing platform. For bulk RNA-seq, key metrics include the alignment rate (should typically be >70-80%), read distribution across genomic features (exonic regions should be the highest), and library complexity [94]. For single-cell RNA-seq, essential metrics are UMI counts per cell (indicates capture efficiency), genes detected per cell, and mitochondrial read percentage (a quality indicator; high percentages often signal stressed or dying cells) [95] [96]. Checking these metrics first helps determine if your data is of sufficient quality for downstream biological interpretation.
Q2: My single-cell data has a high percentage of mitochondrial reads. What does this mean and should I filter these cells out? A high percentage of mitochondrial reads is often associated with unhealthy cell states or can result from broken cells where cytoplasmic RNAs have leaked out [95]. While filtering is common practice, the decision requires caution. Some cell types, like cardiomyocytes, naturally have high mitochondrial gene expression [95]. Therefore, it is recommended to visualize the distribution of this metric (e.g., with a violin plot) and compare it with other metrics like UMI count. Cells that are outliers (e.g., with mt-read percentage >3 standard deviations from the median) are typically removed [95]. However, always check literature for your specific cell type before applying a universal threshold.
Q3: How do I validate that my chosen reference genes are stable in an endometrial study? Validation involves both computational and experimental steps. In your RNA-seq dataset, you should assess the expression stability of candidate reference genes across all your samples using established algorithms like geNorm or NormFinder [97]. The ideal reference genes should show low variability in expression (e.g., low standard deviation) between different experimental conditions (e.g., disease vs. control, different menstrual cycle phases) [97]. Finally, this computational stability should be confirmed experimentally using a second method like qRT-PCR to ensure they are reliable for normalization in validation experiments [97] [98].
Q4: What are common pitfalls in sample preparation for endometrial RNA-seq studies? Common pitfalls include:
- Inaccurate Cycle Phase Dating: Relying solely on histology can be unreliable. Using LH surge timing (e.g., LH+7 to LH+9 for mid-secretory phase) provides a more standardized approach [83] [2].
- Cell Type Heterogeneity: Analyzing whole tissue without separating major cell types (epithelium, stroma) can mask cell-type-specific signals [83] [98]. Using methods like FACS sorting with cell-type-specific markers (e.g., CD9 for epithelium, CD13 for stroma) can resolve this [83].
- RNA Degradation: Endometrial biopsies, especially when processed for single-cell analysis, are sensitive to RNase activity. Rapid processing and working at low temperatures are crucial to maintain RNA integrity [83].
Troubleshooting Guide for Common Experimental Issues
Table 1: Troubleshooting Common Problems in Endometrial RNA-seq Workflows
| Problem | Potential Causes | Solutions & Validation Steps |
|---|---|---|
| Low Alignment Rate | Contaminated or degraded RNA; adapter sequences not trimmed properly. | Check RNA Integrity Number (RIN) >7 pre-library prep; use tools like Trimmomatic for rigorous adapter trimming [2]. |
| High Ambient RNA in scRNA-seq | High cell death during tissue dissociation; over-digestion with enzymes. | Optimize tissue dissociation protocol (time/temperature); use ambient RNA removal tools (e.g., SoupX, DecontX, CellBender) [95] [96]. |
| High Doublet Rate in scRNA-seq | Over-loading of cells on the single-cell platform. | Follow manufacturer's recommendations for cell loading concentration; computationally identify and remove doublets using tools like DoubletFinder or Scrublet [95]. |
| Inconsistent Cycle Phase Validation | Patient cycle variability; inaccurate LH surge prediction. | Use a multi-modal approach: LH surge tracking and histological dating and, if possible, validate with known molecular markers (e.g., PAEP, SPP1) from a receptivity signature [98]. |
| Poor Correlation Between Technical Replicates | Technical artifacts during library preparation or sequencing. | Ensure consistent RNA input and library prep kits; investigate sample-specific biases using PCA; use the RNA-SeQC tool for multi-sample quality evaluation [94]. |
Standardized Experimental Protocols from Literature
Protocol: Isolation and Primary Culture of Endometrial Stromal Cells (ESCs)
This protocol is adapted from a study on adenomyosis [97].
- Tissue Collection: Obtain endometrial tissues by hysterectomy or biopsy. Place tissue immediately in ice-cold sterile PBS for transport.
- Digestion: Mince tissue into small pieces and incubate with 0.1% (w/v) collagenase type II in a shaking water bath for 30 minutes at 37°C.
- Filtration and Separation: Sequentially filter the cell suspension through 100-μm and 40-μm cell strainers to remove debris and epithelial cells, respectively.
- Cell Culture: Centrifuge the filtrate to pellet stromal cells. Resuspend and culture the cells in DMEM/F12 medium supplemented with 10% FBS, 1% penicillin/streptomycin, 10 nmol/L 17β-estradiol, and 1 μmol/L medroxyprogesterone acetate.
- Validation: Identify cultured ESCs by immunocytochemical staining for vimentin (positive) and cytokeratin 8 (negative) [97].
Protocol: Single-Cell RNA-seq from Endometrial Biopsies
This protocol summarizes the pipeline for clinical samples [83].
- Sample Collection and Cryopreservation: Collect biopsy using a Pipelle catheter. Immediately place tissue in cryopreservation medium (DMEM, 30% FBS, 7.5% DMSO) and freeze at -80°C using a controlled-rate freezer.
- Tissue Thawing and Dissociation: Thaw tissue, wash, and dissociate in DMEM with 0.5% collagenase with shaking at 37°C until digested (~20 min).
- Cell Staining and Sorting: Add ice-cold FBS to stop digestion. Filter cells through strainer caps (50μm, then 35μm). Stain cells with fluorescent antibodies (e.g., CD13-APC for stromal cells, CD9-FITC for epithelial cells). Use FACS to sort single cells into plates. The entire process from thawing to sorting should be completed within 90 minutes at low temperatures to minimize changes in the gene expression profile [83].
- Library Preparation and Sequencing: Perform single-cell lysis and use a platform-specific library prep kit (e.g., modified STRT protocol). Sequence on an Illumina platform.
The following workflow diagram illustrates the key steps and quality checkpoints in this single-cell RNA-seq protocol.
Research Reagent Solutions
Table 2: Key Reagents and Kits for Endometrial RNA-seq Studies
| Reagent / Kit | Function / Application | Example Use in Endometrial Research |
|---|---|---|
| Collagenase Type II | Tissue dissociation into single cells. | Digestion of endometrial biopsies for isolation of stromal and epithelial cells [97] [83]. |
| DMEM/F12 Medium | Primary cell culture medium. | Culture medium for primary endometrial stromal cells, often supplemented with hormones [97]. |
| TruSeq RNA Sample Prep Kit (Illumina) | Library preparation for bulk RNA-seq. | Used in multiple studies for constructing transcriptome libraries from endometrial tissues [97] [22]. |
| PAXgene Blood RNA Tubes | Stabilization of blood RNA. | Collection of whole blood samples for miRNome analysis in paired endometrial-blood studies [2]. |
| miRNeasy Mini Kit (Qiagen) | Simultaneous isolation of miRNA and total RNA. | RNA extraction from endometrial tissue and blood buffy coat fractions for small RNA-seq [2]. |
| CD13 / CD9 Antibodies | Cell surface markers for sorting. | Fluorescence-activated cell sorting (FACS) to isolate pure populations of endometrial stromal (CD13+) and epithelial (CD9+) cells [83]. |
Reference Gene Stability in Endometrial Research
Validating reference genes is crucial for accurate qRT-PCR, the gold standard for confirming RNA-seq findings. The table below summarizes genes used in recent endometrial studies.
Table 3: Candidate Reference Genes from Recent Endometrial Transcriptomic Studies
| Gene Symbol | Full Name | Evidence of Use / Validation Context | Citation |
|---|---|---|---|
| Not Explicitly Listed | Varies | Studies performing qRT-PCR validation of RNA-seq data typically state the reference genes used. It is critical to consult the methods section of published papers in your specific area (e.g., adenomyosis, receptivity) and validate stability for your own experimental conditions. | [97] |
| Meta-Signature Genes | - | A meta-analysis of endometrial receptivity identified 57 mRNA genes as putative markers. While these are biomarkers, their consistent expression across cycles in fertile women makes them a valuable resource for informing reference gene selection and validation strategies. | [98] |
Biological validation is a critical step in endometrial RNA-seq research, ensuring that molecular discoveries from sequencing data translate to biologically and clinically meaningful insights. This process bridges the gap between computational findings and their functional significance in endometrial receptivity, disorders, and tumorigenesis. This technical support center provides comprehensive guidance for researchers navigating the challenges of validating RNA-seq results in endometrial studies.
Key Challenges in Endometrial RNA-seq Validation
| Challenge Category | Specific Issues | Impact on Data Quality |
|---|---|---|
| Sample Quality & Integrity | Low RNA mass (1-10 pg/cell) [20], RNase contamination [8], improper handling [20] | RNA degradation, altered transcriptome profiles, failed library prep |
| Technical Variation | Library preparation batch effects [99], lane/flow cell effects [99], PCR amplification bias [99] | Introduced technical artifacts, false positives/negatives in differential expression |
| Biological Complexity | Cellular heterogeneity [8], endometrial cycle timing [15] [7], patient-specific factors [7] | Difficulty distinguishing cell-type-specific signals, reduced reproducibility |
| Data Integration | Linking non-coding mutations to 3D genome organization [9], connecting transcriptomics with epigenetic data [9] | Incomplete mechanistic understanding, limited functional insights |
Frequently Asked Questions & Troubleshooting Guides
Q1: Our endometrial RNA-seq results show high variability between biological replicates. What are the potential causes and solutions?
Potential Causes:
- Inconsistent sample handling: Time between tissue collection and preservation is not standardized [8].
- Cellular heterogeneity: Samples contain varying proportions of epithelial and stromal cells [8].
- Undocumented cycle stage differences: Endometrial tissue collected at different phases of the menstrual cycle without proper documentation [15].
Troubleshooting Steps:
- Standardize Processing: Implement a strict protocol where tissue manipulation, disaggregation, and cell sorting are completed within 90 minutes at low temperatures [8].
- Implement Cell Sorting: Use fluorescence-activated cell sorting (FACS) with markers like CD13 for stromal cells and CD9 for epithelial cells to analyze homogeneous cell populations [8].
- Document Cycle Stage: Precisely document the menstrual cycle phase (e.g., LH+8 for mid-secretory) or hormone replacement therapy day (e.g., P+5) for all samples [15] [7].
Q2: We detected differentially expressed genes (DEGs) in our endometrial cancer study. How can we functionally validate their role in tumorigenesis?
Validation Workflow:
- Prioritize Candidates: Focus on DEGs enriched in specific pathways (e.g., ERα signaling, cell cycle regulation) or located in genomic regions with altered 3D conformation in tumors [9].
- In Vitro Functional Assays:
- Gene Modulation: Use siRNA/shRNA/CRISPR to knock down or knock out candidate genes in endometrial cell lines.
- Phenotypic Analysis: Assess changes in proliferation (MTT assay), invasion (Transwell), and colony formation.
- Mechanistic Studies:
- Confirm 3D Genome Alterations: If a DEG is near a tumor-specific enhancer, use Hi-C or 4C-seq to confirm changes in chromatin looping upon gene modulation [9].
- Identify Altered Complexes: Perform interaction proteomics (e.g., co-IP followed by mass spectrometry) to identify transcription factors or repressors (like EHMT2/G9a) whose recruitment is affected [9].
Q3: How can we validate the functional impact of a non-coding somatic mutation identified in an endometrial tumor?
Validation Strategy:
- Epigenetic Profiling: Perform ChIP-seq for histone marks like H3K27ac and ERα in healthy and tumor endometrial tissues to determine if the mutation falls within a regulatory element [9].
- Enhancer Activity Assays: Clone the wild-type and mutant genomic sequence into a luciferase reporter vector (e.g., pGL4.23) and transfert into relevant endometrial cell lines. Measure changes in luciferase activity.
- Protein Binding Assessment: Use electrophoretic mobility shift assays (EMSAs) to test if the mutation alters the binding of specific transcriptional repressors or activators [9].
- Functional Consequence: Correlate the mutation with the expression of its putative target gene (e.g., via CRISPRi/dCAS9 targeting) and assess downstream phenotypic effects [9].
Q4: Our single-cell RNA-seq of endometrial biopsies yields low transcript counts from epithelial cells. How can we improve this?
Solution:
- Optimize Cell Handling: Epithelial cells are particularly sensitive. Sort cells directly into lysis buffer containing a strong RNase inhibitor to immediately stabilize RNA [20] [8].
- Review FACS Parameters: Ensure the sorting process is gentle and occurs at low temperature to minimize stress-induced transcriptional changes and apoptosis [8].
- Pilot Experiments: Always perform a pilot experiment with positive controls (cells with known RNA content) to optimize RNA extraction and library preparation protocols specifically for your sample type [20].
Research Reagent Solutions for Endometrial Studies
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| RNAlater Stabilization Solution | Preserves RNA integrity in endometrial biopsies immediately after collection [7]. | Crucial for maintaining accurate transcriptome profiles during clinical sampling. |
| CD13 & CD9 Antibodies | Cell surface markers for isolating stromal (CD13+) and epithelial (CD9+) cells via FACS for single-cell or population studies [8]. | Enables analysis of cell-type-specific responses; purity is critical. |
| ERα (ESR1) Antibodies | For ChIP-seq to map ERα binding sites in healthy vs. tumor endometrial tissue [9]. | Identifies oncogenic transcription factor reprogramming. |
| H3K27ac Antibodies | For ChIP-seq to identify active enhancers and promoters [9]. | Helps correlate somatic mutations with altered regulatory activity. |
| Progesterone & Estradiol Valerate | For hormone replacement therapy (HRT) protocols to prepare the endometrium in sync with embryo transfer or research sampling [14] [15]. | Standardizes the "window of implantation" for receptivity studies. |
| SMART-Seq HT / Stranded Kits | For single-cell or low-input RNA-seq library preparation [20]. | Optimized for minimal RNA input; choice depends on need for strand-specificity. |
Detailed Experimental Protocols
Protocol 1: Validating Window of Implantation (WOI) Displacement Using RNA-seq-Based ER Testing
Background: Displaced WOI is a cause of recurrent implantation failure (RIF). RNA-seq-based endometrial receptivity testing (rsERT) can diagnose WOI displacement to guide personalized embryo transfer (pET) [14] [15] [7].
Methodology:
- Patient Cohort: Include women with RIF (e.g., failure after ≥2 euploid embryo transfers) [15].
- Endometrial Biopsy:
- RNA Sequencing & Analysis:
- Functional Outcome - Personalized Embryo Transfer (pET):
- Intervention Group: Perform frozen-thawed embryo transfer at the predicted optimal WOI based on rsERT results. For a sample predicted as pre-receptive on P+5, transfer might be scheduled 20 hours later than standard [7].
- Control Group: Perform standard embryo transfer at the conventional time (e.g., P+5 for blastocysts) [15].
- Correlation with Clinical Outcome:
WOI Validation via rsERT and pET
Protocol 2: Functional Validation of a Somatic Mutation in an ERα Enhancer
Background: Non-coding somatic mutations in metastatic endometrial cancer can alter 3D genome conformation and disrupt transcriptional repressor recruitment, enhancing oncogene expression (e.g., ESR1) [9].
Methodology:
- Identify Candidate Mutation:
- Integrate whole-genome sequencing (WGS) from metastatic tumors with ERα ChIP-seq and H3K27ac HiChIP data from healthy and tumor endometrial tissues [9].
- Identify a somatic mutation enriched in a tumor-specific, ERα-bound enhancer that loops to the ESR1 promoter.
- In Vitro Enhancer Activity Assay:
- Clone the wild-type and mutant enhancer sequence into a luciferase reporter plasmid.
- Transfect plasmids into an endometrial cancer cell line (e.g., Ishikawa).
- Measure luciferase activity. Expected Result: The mutant enhancer shows significantly higher activity [9].
- Protein Binding Assessment (e.g., EMSA):
- Synthesize biotin-labeled DNA probes for wild-type and mutant sequences.
- Incubate probes with nuclear extracts from endometrial cells.
- Resolve protein-DNA complexes on a native gel.
- Expected Result: The mutant probe shows diminished binding to the transcriptional repressor EHMT2/G9a [9].
- 3D Conformation Analysis (4C-seq):
- Design a viewpoint primer at the ESR1 promoter.
- Perform 4C-seq in cells where the wild-type or mutant enhancer sequence has been introduced.
- Expected Result: The mutation strengthens the chromatin loop between the enhancer and the ESR1 promoter [9].
- Functional Consequence:
- Measure ESR1 mRNA and protein levels (via qRT-PCR and Western blot) upon CRISPR-mediated introduction of the enhancer mutation.
- Assess downstream phenotypes like increased cell proliferation and estrogen-independent growth.
Enhancer Mutation Validation Workflow
Cross-Platform and Cross-Protocol Comparisons for Reproducibility
Frequently Asked Questions (FAQs)
Q1: What is the primary cause of Window of Implantation (WOI) displacement, and how can it be detected? WOI displacement, a major cause of unsuccessful embryo implantation particularly in patients with Recurrent Implantation Failure (RIF), occurs when the period of endometrial receptivity is shifted from its typical timing. It can be detected using RNA-seq-based Endometrial Receptivity Testing (ERT), which analyzes the expression of specific genes to identify the optimal window for implantation [15].
Q2: How does RNA-seq-based ERT (rsERT) improve upon traditional histological dating for endometrial receptivity? Traditional histological dating, based on microscopic examination of tissue, has been questioned regarding its accuracy, objectivity, and reproducibility [15]. In contrast, RNA-seq-based ERT uses whole transcriptome analysis to assess the endometrial receptivity status more accurately and objectively, providing reproducible results that can better guide personalized embryo transfer (pET) [15] [7].
Q3: What are the key steps in the endometrial biopsy protocol for rsERT? The standard methodology involves [15] [7]:
- Timing: The endometrium is sampled on a specific day of a hormone replacement therapy cycle, often on the sixth day of progesterone supplementation (P + 5).
- Sample Handling: The collected biopsy is immediately placed in RNAlater buffer and cryopreserved at -80°C.
- Sequencing: RNA sequencing analysis is performed promptly, ideally within 7 days of sampling.
Q4: My RNA-seq data shows inconsistent results between different sequencing platforms. What could be the cause? Inconsistencies can arise from technical variations, including:
- Platform-Specific Protocols: Differences in library preparation kits and sequencing instruments.
- Bioinformatic Pipelines: The use of different algorithms for data alignment and gene expression quantification. To ensure reproducibility, it is critical to document and standardize the wet-lab protocols, bioinformatic tools, and their versions across all experiments.
Q5: How should I handle sample degradation or low RNA quality?
- Prevention: Ensure immediate stabilization of samples after biopsy using reagents like RNAlater and maintain an unbroken cold chain.
- QC Check: Always perform RNA quality control using methods such as Bioanalyzer or TapeStation before proceeding to sequencing. Establish and adhere to a minimum RNA Integrity Number (RIN) threshold.
Troubleshooting Guides
Problem 1: Low Endometrial RNA Yield or Quality After Biopsy
- Potential Cause: Improper biopsy technique or delayed sample processing.
- Solution: Train personnel on standardized biopsy procedures. Immerse the tissue sample in RNAlater immediately after collection and freeze at -80°C without delay [7].
Problem 2: High Variability in Gene Expression Profiles Between Replicates
- Potential Cause: Inconsistent timing of the biopsy during the menstrual cycle or heterogeneity of the endometrial tissue itself.
- Solution: Strictly adhere to the hormone replacement therapy protocol and precisely calculate the biopsy timing (e.g., P + 5). Sample the same anatomical location of the uterus whenever possible [15].
Problem 3: Failure to Identify a Clear Receptive Status
- Potential Cause: The sampled endometrium may be pre-receptive or post-receptive, or there may be underlying pathological conditions affecting receptivity.
- Solution: Verify the hormone levels of the patient to ensure proper cycle synchronization. Consider a repeat biopsy in a subsequent cycle. For patients with RIF, a displaced WOI is common, and a personalized transfer time should be calculated based on the ERT prediction [15].
Experimental Protocols
Protocol 1: Endometrial Biopsy and Sample Preparation for RNA-seq
- Patient Preparation: Prepare the patient under a hormone replacement therapy (HRT) cycle.
- Biopsy Timing: Perform the endometrial biopsy on the predetermined day, typically P + 5 in an HRT cycle [15] [7].
- Sample Stabilization: Immediately place the tissue sample in a 1.5 mL tube containing RNAlater buffer [7].
- Storage: Seal the tube and cryopreserve at -80°C until RNA extraction [7].
- RNA Extraction & QC: Extract total RNA using a column-based kit. Assess RNA quality and quantity using an instrument like Agilent Bioanalyzer.
Protocol 2: RNA-seq Library Preparation and Bioinformatics Analysis for ERT
- Library Prep: Use a standardized library preparation kit (e.g., Illumina TruSeq Stranded mRNA) following the manufacturer's instructions.
- Sequencing: Sequence the libraries on an appropriate platform (e.g., Illumina NovaSeq) to a sufficient depth (e.g., 30 million paired-end reads per sample).
- Bioinformatic Processing:
- Quality Control: Use FastQC to check read quality.
- Alignment: Align reads to the human reference genome (e.g., GRCh38) using a splice-aware aligner like STAR.
- Quantification: Generate gene-level counts using featureCounts or HTSeq.
- Receptivity Classification: Input the normalized gene expression values into a pre-validated machine learning model (e.g., based on 175 predictive genes) to determine the endometrial receptivity status and predict the WOI [15].
Table 1: Key Outcomes from RCT on ERT-Guided Transfer in RIF Patients
| Study Group | Live Birth Rate (Primary Outcome) | Clinical Pregnancy Rate | Key Finding |
|---|---|---|---|
| Personalized Embryo Transfer (pET) | Target: 60% (estimated) | 69.7% [7] | pET guided by ERT significantly improved pregnancy outcomes in RIF patients [7]. |
| Standard Embryo Transfer (sET) | Baseline: 35% (estimated) | Not Specified | Serves as the control for comparison [15]. |
Table 2: Comparison of Endometrial Receptivity Assessment Methods
| Method | Technology Basis | Key Features | Limitations |
|---|---|---|---|
| Histological Dating | Microscopic tissue examination | Established for decades; relatively low cost | Subjective; poor reproducibility and accuracy [15]. |
| ERA (Endometrial Receptivity Array) | Microarray (238 genes) | First transcriptomic tool for WOI detection [15] | Based on older microarray technology. |
| rsERT (RNA-seq-based ERT) | RNA Sequencing (175 genes) | High sensitivity; whole-transcriptome capability; uses machine learning [15] | Higher cost; requires specialized bioinformatic analysis. |
Signaling Pathways and Workflows
rsERT Workflow for WOI Detection
Achieving Embryo-Endometrium Synchrony
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Endometrial RNA-seq Research
| Item | Function in the Protocol |
|---|---|
| RNAlater Stabilization Solution | Preserves RNA integrity immediately after tissue biopsy by inhibiting RNases [7]. |
| Hormone Replacement Therapy (HRT) Drugs | Creates a synchronized and controlled menstrual cycle for accurate timing of the biopsy and embryo transfer [15]. |
| Total RNA Extraction Kit | Isolves high-quality, intact total RNA from endometrial tissue samples. |
| RNA Quality Assessment Kit | Assesses the integrity and quality of the extracted RNA (e.g., RIN number) before proceeding to sequencing. |
| Stranded mRNA Library Prep Kit | Prepares sequencing libraries from the purified RNA, enriching for poly-A transcripts. |
| ERT/RsERT Classifier | A validated computational model that uses the RNA-seq data to diagnose endometrial receptivity status [15]. |
Troubleshooting Guide: Common RNA-seq Preparation Errors
FAQ 1: What are the most common causes of low library yield in endometrial RNA-seq and how can they be resolved?
Low library yield is a frequent challenge that can compromise transcriptomic data quality. The table below outlines primary causes and corrective actions.
Table 1: Troubleshooting Low Library Yield in Endometrial RNA-seq
| Cause | Mechanism of Yield Loss | Corrective Action |
|---|---|---|
| Poor Input Quality/Contaminants | Enzyme inhibition from residual salts, phenol, or polysaccharides [100]. | Re-purify input sample; ensure fresh wash buffers; target high purity (260/230 > 1.8) [100]. |
| Inaccurate Quantification | Over/under-estimating input leads to suboptimal enzyme stoichiometry [100]. | Use fluorometric methods (Qubit) over UV (NanoDrop); calibrate pipettes; use master mixes [100]. |
| Fragmentation Inefficiency | Over- or under-fragmentation reduces adapter ligation efficiency [100]. | Optimize fragmentation time/energy; verify fragmentation profile before proceeding [100] [34]. |
| Suboptimal Adapter Ligation | Poor ligase performance or incorrect adapter-to-insert molar ratio [100]. | Titrate adapter:insert ratios; use fresh ligase and buffer; maintain optimal temperature [100]. |
| Overly Aggressive Purification | Desired fragments are excluded during bead-based size selection [100]. | Optimize bead-to-sample ratio; avoid over-drying beads, which leads to inefficient resuspension [100]. |
FAQ 2: How can I minimize bias during library construction for sensitive endometrial samples?
Bias introduced during library prep can skew transcript representation and impact downstream analysis. Key biases and mitigation strategies include:
- Fragmentation Bias: Non-random fragmentation can reduce library complexity. Use chemical treatment (e.g., zinc) instead of RNase III for a more random fragmentation pattern [34].
- Primer Bias: Random hexamer priming can introduce sequence-specific bias. Consider direct RNA sequencing where adapters are ligated to RNA fragments, bypassing cDNA synthesis with random primers [34].
- PCR Amplification Bias: Preferential amplification of certain sequences leads to inaccurate quantification and high duplicate rates. Solutions: 1) Use polymerases like Kapa HiFi; 2) Additives like TMAC or betaine can help with AT/GC-rich regions; 3) Minimize the number of PCR cycles [34].
- Adapter Ligation Bias: T4 RNA ligases have sequence preferences. Use adapters with randomized nucleotides at the ligation ends to ensure uniform ligation efficiency across different sequences [34].
FAQ 3: Our core facility experiences sporadic, operator-dependent prep failures. How can we improve consistency?
Intermittent failures often stem from subtle protocol deviations in manual preparations.
- Root Causes: Inconsistent mixing methods (vortexing vs. pipetting), evaporation of ethanol wash solutions altering concentration, and accidental discarding of beads instead of supernatant [100].
- Corrective Steps:
- Reinforce SOPs: Highlight critical steps in the protocol using bold text or color.
- Implement Checkpoints: Use operator checklists and redundant logging.
- Use "Waste Plates": Temporarily hold discarded material to allow for retrieval in case of error.
- Standardize Reagents: Switch to master mixes to reduce pipetting steps and variability [100].
Experimental Protocols: From Sample to Data
This section details the methodologies for key experiments linking endometrial transcriptomics to clinical outcomes in Recurrent Implantation Failure (RIF) and endometriosis.
Protocol: RNA-seq-based Endometrial Receptivity Test (rsERT) for RIF
The following workflow is used to identify the Window of Implantation (WOI) for personalized embryo transfer [101] [7].
Table 2: Key Reagents for Endometrial Receptivity Testing
| Research Reagent | Function/Application |
|---|---|
| RNAlater Buffer | Preserves RNA integrity in endometrial biopsy samples immediately after collection [7]. |
| Oligo-dT Beads | Enriches for polyadenylated mRNA from total RNA by binding to the poly-A tail [34]. |
| Illumina Sequencing Platform | High-throughput platform for generating RNA-seq data; used with kits like Illumina Next Seq [102] [7]. |
| Random Hexamer Primers | Used in reverse transcription to generate cDNA from the enriched mRNA; can be a source of bias [34]. |
| Kapa HiFi Polymerase | A high-fidelity PCR enzyme recommended to reduce amplification bias during library amplification [34]. |
Workflow Diagram: The following diagram illustrates the complete experimental and clinical pathway for the rsERT protocol.
Protocol: Single-Cell RNA-seq Analysis for Endometriosis Biomarker Discovery
This protocol is used to characterize cellular heterogeneity and identify novel biomarkers in endometriosis lesions [72] [103].
Methodology Details:
- Sample Collection: Ectopic endometrium (endometriosis lesions), eutopic endometrium from women with endometriosis, and normal endometrium from healthy controls are collected [72].
- Single-Cell Dissociation and Sequencing: Tissues are digested into single-cell suspensions. Cells are loaded onto a 10x Genomics Chromium system for barcoding and library preparation, followed by sequencing [72].
- Bioinformatic Analysis:
- Quality Control & Clustering: Filter cells based on gene counts and mitochondrial content. Use Seurat for graph-based clustering and t-SNE for visualization [72].
- Differential Expression & Trajectory Analysis: Identify marker genes for each cluster. Use pseudotime algorithms (e.g., Monocle) to map developmental trajectories of fibroblasts [72].
- Machine Learning for Biomarker Identification: Apply classifiers (e.g., Bagged CART, XGBoost) on transcriptomic data to identify genes with high diagnostic power for endometriosis [102] [104].
Workflow Diagram: The diagram below summarizes the single-cell analysis pipeline for endometriosis.
The tables below consolidate key performance and diagnostic data from the cited studies.
Table 3: Clinical Outcomes of rsERT-Guided Personalized Embryo Transfer (pET) in RIF
| Study Reference | Study Design | Group | Live Birth Rate (LBR) | Clinical Pregnancy Rate (CPR) | Implantation Rate (IR) |
|---|---|---|---|---|---|
| RCT Protocol [15] | Randomized Controlled Trial | pET (guided by ERT) | 60% (assumed) | Not specified | Not specified |
| sET (Standard) | 35% (from retrospective data) | Not specified | Not specified | ||
| Clinical Application [101] | Prospective Cohort | pET (guided by rsERT) | Significantly higher* | Significantly higher* | Significantly higher* |
| Conventional ET | - | - | - | ||
| PGT Cohort [7] | Retrospective Cohort | PGT + rsERT (pET) | Not specified | 69.7% | Not specified |
| PGT alone (control) | Not specified | Lower than pET group | Not specified | ||
| Statistical significance (P < 0.05) reported between groups after propensity score matching [101]. |
Table 4: Diagnostic Performance of Transcriptomic Biomarkers in Endometriosis
| Biomarker Type | Specific Gene/s | Reported Diagnostic Performance | Study Details |
|---|---|---|---|
| Machine Learning Classifier | Panel including CUX2, CLMP, CEP131, etc. | Accuracy: 85.7%, Sensitivity: 100%, Specificity: 75% [102] [104] | Bagged CART model on RNA-seq data [102]. |
| Programmed Cell Death (PCD) & Mitochondrial Biomarkers | AIFM1, PDK4 | Strong diagnostic performance (AUC > 0.7) [103] | Identified via integrated bioinformatics analysis [103]. |
| Single-cell Analysis | Fibroblast subpopulations (e.g., expressing StAR, C3) | Revealed distinct pathogenic states and trajectories in ectopic lesions [72] | scRNA-seq of patient tissues [72]. |
Conclusion
The evolving landscape of endometrial RNA-seq preparation is fundamentally enhancing our capacity to investigate the molecular underpinnings of reproductive health and disease. The integration of traditional bulk sequencing with high-resolution spatial and single-cell methods, coupled with the development of less invasive sampling techniques, provides a powerful, multi-faceted toolkit for researchers. Future directions will likely focus on standardizing these diverse protocols, further refining non-invasive diagnostic applications, and deepening the integration of genetic data with transcriptomic splicing events to uncover novel therapeutic targets. By adhering to rigorous preparation and validation frameworks outlined here, the field is poised to generate more reproducible, clinically actionable insights, ultimately advancing personalized care for conditions like infertility, endometriosis, and recurrent implantation failure.
References
- 1. Frontiers | Single - cell and spatial transcriptomics integration: new... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1649468/full]
- 2. A Two-Cohort RNA-seq Study Reveals Changes in Endometrial and Blood miRNome in Fertile and Infertile Women - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6315937/]
- 3. Integration of Single cell and Bulk -Sequencing Reveals Key... RNA [https://www.dovepress.com/integration-of-single-cell-and-bulk-rna-sequencing-reveals-key-genes-a-peer-reviewed-fulltext-article-JIR]
- 4. RNA-seq Sample Guidelines | Genomics Core Facility | The Huck Institutes (en-US) [https://www.huck.psu.edu/core-facilities/genomics-core-facility/sample-recommendations/rna-seq-sample-guidelines]
- 5. RNA Sequencing Sample Preparation | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/dna-rna-purification-analysis/rna-extraction/rna-applications/rna-sequencing-sample-preparation.html]
- 6. Integrated single †cell sequencing and RNA transcriptomics... spatial [https://pmc.ncbi.nlm.nih.gov/articles/PMC11035376/]
- 7. Frontiers | Integrated treatment guided by RNA - seq –based... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1224574/full]
- 8. Single-cell transcriptome analysis of endometrial tissue [https://pubmed.ncbi.nlm.nih.gov/26874359/]
- 9. tumorigenesis involves epigenetic plasticity demarcating... Endometrial [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03596-5]
- 10. Frontiers | Immune-related gene signatures of thin endometrium ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1626451/full]
- 11. Endometrial sampling devices for early diagnosis of endometrial lesions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5095161/]
- 12. Unlocking uterine biology at home: a validated system for DNA, RNA... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12155041/]
- 13. Analysis of menstrual : diagnostic potential for endometriosis effluent [https://molmed.biomedcentral.com/articles/10.1186/s10020-018-0009-6]
- 14. Improving pregnancy outcomes in patients with recurrent implantation... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11520988/]
- 15. Efficacy of endometrial receptivity testing for recurrent implantation... [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-024-08125-6]
- 16. A Comparative Evaluation of the Three Different Methods of Endometrial Sampling in the Diagnosis of Perimenopausal Bleeding | Patil | Journal of Clinical Gynecology and Obstetrics [https://jcgo.org/index.php/jcgo/article/view/271/140]
- 17. The role of transcriptomic biomarkers of endometrial receptivity in personalized embryo transfer for patients with repeated implantation failure - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8082865/]
- 18. Transcriptomics of receptive endometrium in women with sonographic features of adenomyosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8722101/]
- 19. Human endometrial cell-type-specific RNA sequencing provides new... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9632455/]
- 20. 5 tips for successful single-cell RNA-seq [https://www.takarabio.com/about/bioview-blog/tips-and-troubleshooting/5-tips-to-make-your-single-cell-rna-seq-experiments-a-success]
- 21. Single-cell characterization of menstrual fluid at homeostasis and in... [https://elifesciences.org/reviewed-preprints/99558]
- 22. Frontiers | Comprehensive Analysis of RNA-Seq in Endometriosis ... [https://www.frontiersin.org/articles/10.3389/fgene.2022.828238/full]
- 23. RNAlaterâ„¢ Stabilization Solution 500 mL | Contact... | thermofisher.com [https://www.thermofisher.com/order/catalog/product/AM7021]
- 24. Enhancing the stability of DNA: a new era for nucleic ... acid [https://www.ceric-eric.eu/2025/03/19/enhancing-the-stability-of-dna-a-new-era-for-nucleic-acid-preservation/]
- 25. What is Nucleic ? Uses, How It Works... Acid Preservation Solution [https://www.linkedin.com/pulse/what-nucleic-acid-preservation-solution-uses-how-works-uo3se]
- 26. Breaking the Ice: A Breakthrough Method for Ambient... | Medium [https://medium.com/@cache_blog/breaking-the-ice-a-breakthrough-method-for-ambient-temperature-dna-and-rna-preservation-c4b4fabfdbaa]
- 27. Guiding Principles for Ethical Research | National Institutes of Health (NIH) [https://www.nih.gov/health-information/nih-clinical-research-trials-you/guiding-principles-ethical-research]
- 28. in Ethical | IntechOpen Considerations Informed Consent [https://www.intechopen.com/chapters/1123544]
- 29. Development and Internal Validation of a Novel Risk... | F1000 Research [https://f1000research.com/articles/14-1281]
- 30. Sequencing RNA | Thermo Fisher Scientific - UK Sample Preparation [https://www.thermofisher.com/uk/en/home/life-science/dna-rna-purification-analysis/rna-extraction/rna-applications/rna-sequencing-sample-preparation.html]
- 31. Standards and Ethics - AAPOR [https://aapor.org/standards-and-ethics/]
- 32. and Considerations in Challenges - Bulk RNA seq [https://alitheagenomics.com/blog/challenges-and-considerations-in-bulk-rna-seq]
- 33. Integration of Single Cell and Bulk -Sequencing Reveals Key... RNA [https://pmc.ncbi.nlm.nih.gov/articles/PMC11871914/]
- 34. Bias in RNA - seq Library Preparation : Current Challenges and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8079181/]
- 35. RNA Sequencing | RNA - Seq methods & workflows [https://www.illumina.com/techniques/sequencing/rna-sequencing.html]
- 36. Bulk RNAseq Methodology and Analysis Guide [https://www.cores.emory.edu/eicc/_includes/documents/sections/resources/RNAseq_Methodology.html]
- 37. Single-cell transcriptomic analysis highlights origin and pathological process of human endometrioid endometrial carcinoma | Nature Communications [https://www.nature.com/articles/s41467-022-33982-7]
- 38. Bulk RNA-seq Data Standards and Processing Pipeline – ENCODE [https://www.encodeproject.org/data-standards/rna-seq/long-rnas/]
- 39. Frontiers | A Single-Cell Sequencing Guide for Immunologists [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2018.02425/full]
- 40. Cell Type Purification by Single-Cell Transcriptome-Trained Sorting - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6863042/]
- 41. Frontiers | FB5P-seq: FACS-Based 5-Prime End Single-Cell RNA-seq for Integrative Analysis of Transcriptome and Antigen Receptor Repertoire in B and T Cells [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2020.00216/full]
- 42. Top 5 tips for sorting (FACS) upstream of single-cell RNA-seq experiments [https://www.takarabio.com/about/bioview-blog/tips-and-troubleshooting/5-facs-tips-for-scrna-seq]
- 43. FAQ | 10x Genomics - 10x Genomics - Single Cell Discoveries [https://www.scdiscoveries.com/support/faq-10x-genomics/]
- 44. An Innovative Approach to Tissue Processing and Cell Sorting of Fixed Cells for Subsequent Single-Cell RNA Sequencing - PubMed [https://pubmed.ncbi.nlm.nih.gov/36142141/]
- 45. Best Practices for Analysis of 10 Single Cell RNA- x Data Genomics seq [https://www.10xgenomics.com/analysis-guides/best-practices-analysis-10x-single-cell-rnaseq-data]
- 46. Direct Comparative Analyses of 10 Chromium and... X Genomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC8602399/]
- 47. NGI Sweden » Visium 3´- PolyA-based [https://ngisweden.scilifelab.se/methods/10x-visium/]
- 48. 10x Visium 空间转录组-欧易生物 [https://www.oebiotech.com/danxibaocexu/10x_visium.html]
- 49. Spatial Visium – Tissue... | Official Protocols Genomics Support 10 x [https://www.10xgenomics.com/support/spatial-gene-expression-fresh-frozen/documentation/steps/tissue-prep/visium-spatial-protocols-tissue-preparation-guide]
- 50. Spatial Transcriptomics : Center for Genetic Medicine: Feinberg School... [https://www.cgm.northwestern.edu/cores/nuseq/services/next-generation-sequencing/spatial-transcriptomics.html]
- 51. åˆ†æž | Visium Genomics 空 é—´ 10 x [https://www.10xgenomics.com/cn/products/visium-analysis]
- 52. Spatial Transcriptomics & Spatial Biology | 10x Genomics [https://www.10xgenomics.com/spatial-transcriptomics]
- 53. — Cumulus 3.1.1 documentation 10 x Visium [https://cumulus.readthedocs.io/en/latest/spaceranger.html]
- 54. Technology focus: 10 Genomics x — spatialdata Visium [https://spatialdata.scverse.org/en/latest/tutorials/notebooks/notebooks/examples/technology_visium.html]
- 55. Can biomarkers identified from the uterine transcriptome be used... fluid [https://pmc.ncbi.nlm.nih.gov/articles/PMC9938621/]
- 56. transcriptome as potential Uterine - fluid ... | medRxiv non invasive [https://www.medrxiv.org/content/10.1101/2021.03.07.21253097v1.full]
- 57. : Troubleshooting Extraction for Sequencing - CD... Guide RNA [https://rna.cd-genomics.com/resource/troubleshooting-rna-extraction.html]
- 58. takarabio.com/learning-centers/next-generation-sequencing/ rna - seq ... [https://www.takarabio.com/learning-centers/next-generation-sequencing/rna-seq/rna-seq-faqs]
- 59. Identification of long non‑coding RNA expression patterns useful for... [https://www.spandidos-publications.com/10.3892/or.2018.6880?text=fulltext]
- 60. 10X RNAseq Library Prep [https://protocols.hostmicrobe.org/10x-rnaseq]
- 61. Guidance on Processing the 10x Genomics Single Cell Gene Expression Assay - PubMed [https://pubmed.ncbi.nlm.nih.gov/36495443/]
- 62. Frontiers | A High-Throughput Method for Illumina RNA-Seq Library Preparation [https://www.frontiersin.org/journals/plant-science/articles/10.3389/fpls.2012.00202/full]
- 63. A Step-by-Step Guide for Setting up a NextSeq... | ZYMO RESEARCH [https://www.zymoresearch.de/pages/technote-how-to-set-up-a-nextseq-sequencing-run]
- 64. | Troubleshooting Knowledge Illumina [https://knowledge.illumina.com/library-preparation/general/library-preparation-general-troubleshooting-list]
- 65. Single-cell transcriptomics sequencing from 5’ cDNA prepared with... [https://nanoporetech.com/document/ligation-sequencing-v14-single-cell-transcriptomics-with-5-cdna]
- 66. RNase and RNase Inhibitors - RNA / BOC Sciences [https://rna.bocsci.com/support/overviews-of-rnase-and-rnase-inhibitors.html]
- 67. RNase Inhibitor, Murine - RNA Degradation Prevention | APExBIO [https://www.apexbt.com/rnase-inhibitor-murine.html]
- 68. Introducing synthetic thermostable RNase inhibitors to single-cell RNA-seq | Nature Communications [https://www.nature.com/articles/s41467-024-52717-4]
- 69. Sequencing RNA | Thermo Fisher Scientific - ID Sample Preparation [https://www.thermofisher.com/id/en/home/life-science/dna-rna-purification-analysis/rna-extraction/rna-applications/rna-sequencing-sample-preparation.html]
- 70. Frontiers | Ultrasensitive RNase H activity detection using the transcription-based hybrid probe and CRISPR/cas12a signal amplifier [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1589150/full]
- 71. Protector RNase Inhibitor Protocol [https://www.sigmaaldrich.com/US/en/technical-documents/protocol/genomics/dna-and-rna-purification/protector-rnase-inhibitor]
- 72. Single-cell transcriptomic analysis of endometriosis provides insights into fibroblast fates and immune cell heterogeneity | Cell & Bioscience | Full Text [https://cellandbioscience.biomedcentral.com/articles/10.1186/s13578-021-00637-x]
- 73. Optimized splitting of mixed -species rna sequencing data - pmc [https://pmc.ncbi.nlm.nih.gov/articles/PMC9081140/]
- 74. A comprehensive assessment of RNA-seq protocols for degraded and low-quantity samples | BMC Genomics | Full Text [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-017-3827-y]
- 75. Unveiling heterogeneity in MSCs: exploring marker-based strategies ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05294-5]
- 76. Best practices for RNA-seq success, part I: Optimizing sample prep [https://www.takarabio.com/about/bioview-blog/tips-and-troubleshooting/best-practices-for-rna-seq-optimizing-sample-prep]
- 77. The RNA - seq based endometrial receptivity test (rsERT) compared to... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9634259/]
- 78. The efficacy of RNA - seq -based endometrial receptivity test... [https://link.springer.com/article/10.1007/s10815-025-03627-x]
- 79. - RNA reveals HPV contamination of Seq cancer endometrial ... samples [https://www.rna-seqblog.com/rna-seq-reveals-hpv-contamination-of-endometrial-cancer-samples-in-the-cancer-genome-atlas-database/]
- 80. Precision Oncology: Current Landscape, Emerging Trends, Challenges, and Future Perspectives [https://www.mdpi.com/2073-4409/14/22/1804]
- 81. Highlights from ESHRE 2025 : Advances in Endometrial ... Preparation [https://www.emjreviews.com/reproductive-health/congress-review/highlights-from-eshre-2025-advances-in-endometrial-preparation-strategies-for-frozen-embryo-transfer-j150125/]
- 82. Top Tips for Enhancing Single - Cell Sequencing | Technology Networks [https://www.technologynetworks.com/genomics/how-to-guides/top-tips-for-enhancing-single-cell-sequencing-387527]
- 83. Single-cell transcriptome analysis of endometrial tissue - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4791917/]
- 84. Singleâ€cell RNA sequencing technologies and applications: A brief overview - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8964935/]
- 85. Agilent Bioanalyzer 2100 | DNA Technologies Core [https://dnatech.genomecenter.ucdavis.edu/agilent-bioanalyzer-2100/]
- 86. Library QC and Troubleshooting with the BioAnalyzer and Fragment Analyzer | Illumina [https://www.illumina.com/company/video-hub/uie_UYNjFSk.html]
- 87. Monitoring Error Rates In Illumina Sequencing - PubMed [https://pubmed.ncbi.nlm.nih.gov/27672352/]
- 88. Monitoring Error Rates In Illumina Sequencing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5026502/]
- 89. How to troubleshoot “A component failed during sequencing†error messages on the NovaSeq 6000 | Illumina Knowledge [https://knowledge.illumina.com/instrumentation/novaseq-6000/instrumentation-novaseq-6000-troubleshooting-list/000001265]
- 90. Single cell analysis of endometriosis reveals a coordinated transcriptional program driving immunotolerance and angiogenesis across eutopic and ectopic tissues - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9901845/]
- 91. Global transcriptomic changes occur in uterine fluid -derived... [https://pubmed.ncbi.nlm.nih.gov/34190319/]
- 92. Multi-omics analysis of uterine fluid extracellular vesicles reveals a resemblance with endometrial tissue across the menstrual cycle: biological and translational insights - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11904304/]
- 93. Endometrial receptivity profiled through transcriptomic analysis of uterine fluid extracellular vesicles using systems biology and bayesian modeling for pregnancy prediction | Scientific Reports [https://www.nature.com/articles/s41598-025-19633-z]
- 94. RNA-SeQC: RNA - seq and process... metrics for quality control [https://pmc.ncbi.nlm.nih.gov/articles/PMC3356847/]
- 95. Common Considerations for Quality Filters for... | 10x Genomics Control [https://www.10xgenomics.com/analysis-guides/common-considerations-for-quality-control-filters-for-single-cell-rna-seq-data]
- 96. Comprehensive generation, visualization... | Nature Communications [https://www.nature.com/articles/s41467-022-29212-9?error=cookies_not_supported&code=e1da2037-928c-4d26-939e-0c5b5ba2c545]
- 97. Transcriptome analysis of eutopic endometrial stromal cells in women... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9275863/]
- 98. Meta-signature of human endometrial receptivity: a meta-analysis and validation study of transcriptomic biomarkers | Scientific Reports [https://www.nature.com/articles/s41598-017-10098-3]
- 99. RNA-seq Data: Challenges in and Recommendations for Experimental Design and Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4230301/]
- 100. How to Troubleshoot Sequencing Preparation Errors (NGS Guide ) [https://www.cd-genomics.com/resource-sequencing-preparation-troubleshooting.html]
- 101. Establishment and application of an RNA - seq -based predictive model... [https://pubmed.ncbi.nlm.nih.gov/40304883/]
- 102. Prediction of genomic biomarkers for endometriosis using the transcriptomic dataset - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12019090/]
- 103. Frontiers | Uncovering potential biomarkers of endometriosis: transcriptomic and single-cell analysis [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1528434/full]
- 104. Prediction of genomic biomarkers for endometriosis using the transcriptomic dataset - PubMed [https://pubmed.ncbi.nlm.nih.gov/40671745/]