Machine Learning Prediction Models for Rare Fertility Outcomes: From Data to Clinical Decision Support
This article provides a comprehensive examination of machine learning (ML) applications in predicting rare and complex fertility outcomes for researchers, scientists, and drug development professionals. It explores the foundational principles underpinning ML prediction models in assisted reproductive technology (ART), analyzes diverse methodological approaches and their specific clinical applications, addresses critical optimization challenges in model development, and evaluates validation frameworks and comparative performance across algorithms. By synthesizing recent advancements and evidence, this review aims to guide the development of more robust, clinically applicable prediction tools that can enhance patient counseling, personalize treatment strategies, and ultimately improve success rates in infertility treatment.
Machine Learning Prediction Models for Rare Fertility Outcomes: From Data to Clinical Decision Support
Abstract
This article provides a comprehensive examination of machine learning (ML) applications in predicting rare and complex fertility outcomes for researchers, scientists, and drug development professionals. It explores the foundational principles underpinning ML prediction models in assisted reproductive technology (ART), analyzes diverse methodological approaches and their specific clinical applications, addresses critical optimization challenges in model development, and evaluates validation frameworks and comparative performance across algorithms. By synthesizing recent advancements and evidence, this review aims to guide the development of more robust, clinically applicable prediction tools that can enhance patient counseling, personalize treatment strategies, and ultimately improve success rates in infertility treatment.
Understanding ML for Rare Fertility Outcomes: Foundations and Clinical Imperatives
Quantitative Definitions of Key Fertility Outcomes
Fertility outcomes represent critical endpoints for evaluating assisted reproductive technology (ART) success. The table below summarizes quantitative definitions and performance metrics for key outcomes based on clinical and laboratory standards.
Table 1: Definitions and Performance Metrics for Key Fertility Outcomes
| Outcome | Definition | Key Performance Metrics | Reported Rates |
|---|---|---|---|
| Clinical Pregnancy | Detection of an intrauterine gestational sac via transvaginal ultrasound 28–35 days post-embryo transfer [1]. | Clinical Pregnancy Rate (CPR) = (Number of clinical pregnancies / Number of embryo transfers) × 100 [1]. | 46.08% (overall CPR in FET cycles); 61.14% (blastocyst transfers) vs. 34.13% (cleavage-stage transfers) [1]. |
| Live Birth | Delivery of one or more living infants after ≥24 weeks of gestation [2]. | Live Birth Rate (LBR) = (Number of live births / Number of embryo transfers) × 100 [2]. | 26.96% (overall LBR in IVF/ICSI cycles) [2]. |
| Blastocyst Formation | Development of a fertilized egg to a blastocyst by day 5 or 6, characterized by blastocoel expansion, inner cell mass (ICM), and trophectoderm (TE) [3]. | Blastocyst Formation Rate = (Number of blastocysts / Number of fertilized eggs cultured to day 5/6) × 100 [3]. | 53.6% (from good-quality day 3 embryos) vs. 19.3% (from poor-quality day 3 embryos) [3]. |
Experimental Protocols for Outcome Assessment
Protocol for Clinical Pregnancy Confirmation
Objective: To confirm clinical pregnancy post-embryo transfer. Workflow:
- Serum β-hCG Testing:
- Transvaginal Ultrasound:
Diagram 1: Clinical Pregnancy Confirmation Workflow (79 characters)
Protocol for Blastocyst Formation Assessment
Objective: To evaluate embryo development to the blastocyst stage using standardized grading. Workflow:
- Embryo Culture:
- Culture fertilized eggs in sequential media under tri-gas incubators (6% CO₂, 5% O₂, 89% N₂) at 37°C until day 5/6 [3].
- Blastocyst Grading (Gardner Criteria):
- High-Quality Blastocyst Definition: Expansion stage ≥3 with ICM and TE grades ≥B [1].
Diagram 2: Blastocyst Formation Assessment Workflow (85 characters)
Protocol for Live Birth Documentation
Objective: To document live birth resulting from ART cycles. Workflow:
- Post-Transfer Monitoring:
- Track pregnancy progress via obstetric care until delivery.
- Live Birth Certification:
- Criteria: Delivery of ≥1 living infant at ≥24 weeks gestation [2].
- Data Collection: Record gestational age, birth weight, and neonatal outcomes.
Machine Learning Prediction Models for Fertility Outcomes
Machine learning (ML) models leverage demographic, clinical, and laboratory variables to predict ART success. The table below outlines key predictors and ML applications for each fertility outcome.
Table 2: Machine Learning Models and Predictors for Fertility Outcomes
| Outcome | Key Predictors | ML Algorithms | Model Performance |
|---|---|---|---|
| Clinical Pregnancy | Female age (OR: 0.93), number of high-quality blastocysts (OR: 1.67), AMH level (OR: 1.03), blastocyst transfer (OR: 2.31), endometrial thickness on transfer day (OR: 1.10) [1]. | Random forest, binary logistic regression [1]. | Random forest identified 7 top predictors; logistic regression provided odds ratios (OR) with 95% CI [1]. |
| Live Birth | Maternal age, duration of infertility, basal FSH, progressive sperm motility, progesterone on HCG day, estradiol on HCG day, luteinizing hormone on HCG day [2]. | Random forest, XGBoost, LightGBM, logistic regression [2]. | AUROC: 0.674 (logistic regression), 0.671 (random forest); Brier score: 0.183 [2]. |
| Blastocyst Formation | Day 3 embryo morphology, maternal age, fertilization method [3]. | Predictive models using lab-environment data (e.g., incubator metrics) [4]. | Blastocyst euploidy rate unaffected by day 3 quality (42.6–43.8%) [3]. |
Diagram 3: ML Prediction Model Framework (81 characters)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Fertility Outcomes Research
| Item | Function | Application Example |
|---|---|---|
| Tri-Gas Incubators | Maintain physiological Oâ‚‚ (5%), COâ‚‚ (6%), and Nâ‚‚ (89%) levels for optimal embryo culture [3]. | Blastocyst formation assays [3]. |
| Sequential Culture Media | Support embryo development from cleavage to blastocyst stage with stage-specific nutrients [3]. | Embryo culture to day 5/6 [3]. |
| Anti-Müllerian Hormone (AMH) ELISA Kits | Quantify serum AMH levels to assess ovarian reserve [1]. | Predicting clinical pregnancy (OR: 1.03) [1]. |
| Preimplantation Genetic Testing for Aneuploidy (PGT-A) | Screen blastocysts for chromosomal abnormalities to select euploid embryos [3]. | Live birth prediction; euploidy rate assessment (42.6–43.8%) [3]. |
| β-hCG Immunoassay Kits | Detect pregnancy via serum β-hCG levels 12–14 days post-transfer [1]. | Biochemical pregnancy confirmation [1]. |
| Embryo Grading Materials | Standardize blastocyst assessment using Gardner criteria (ICM, TE, expansion) [1]. | Classifying high-quality blastocysts [1]. |
| Ledipasvir D-tartrate | Ledipasvir D-tartrate|CAS 1502654-87-6|HCV Inhibitor | Ledipasvir D-tartrate is a potent, research-grade HCV NS5A inhibitor. This product is for Research Use Only and is not intended for diagnostic or therapeutic applications. |
| Tigecycline hydrochloride | Tigecycline hydrochloride, CAS:197654-04-9, MF:C29H40ClN5O8, MW:622.1 g/mol | Chemical Reagent |
Assisted Reproductive Technology (ART) represents a landmark achievement in treating infertility, a condition affecting an estimated 15% of couples globally [5]. Despite the growing utilization of ART, success rates have plateaued at approximately 30-40% per cycle, presenting a significant clinical challenge [6] [5]. The unpredictable nature of ART outcomes generates substantial emotional and financial burdens for patients, underscoring the critical need for reliable prognostic tools.
Traditional methods for predicting ART success have historically relied on clinicians' subjective assessments, often based primarily on patient age and historical clinic success rates [5]. However, the complex, multifactorial nature of human reproduction involves numerous interrelated variables, making accurate prediction a formidable task. Machine learning (ML), a subset of artificial intelligence, has emerged as a promising approach to enhance predictive accuracy by analyzing complex patterns in large datasets that may elude conventional statistical methods or human interpretation [7]. This application note explores the clinical challenges in ART prediction and details advanced ML methodologies to address them within rare fertility outcomes research.
Quantitative Landscape of ART Prediction Models
The performance of machine learning models in predicting ART success varies considerably based on algorithm selection, feature sets, and dataset characteristics. The table below summarizes the performance metrics of various ML algorithms as reported in recent studies, providing a comparative overview for researchers.
Table 1: Performance Metrics of Machine Learning Models for ART Outcome Prediction
| Study Reference | ML Algorithms Used | Dataset Size | Key Predictors | Best Performing Model | Performance (AUC/Accuracy) |
|---|---|---|---|---|---|
| Systematic Review (2025) [6] | SVM, RF, LR, KNN, ANN, GNB | 107 features across 27 studies | Female age (most common) | Support Vector Machine (SVM) | AUC: 0.997 (Best reported) |
| Wang et al. (2024) [2] | RF, XGBoost, LightGBM, LR | 11,486 couples | Maternal age, duration of infertility, basal FSH, progressive sperm motility, P on HCG day, E2 on HCG day, LH on HCG day | Logistic Regression | AUC: 0.674 (95% CI 0.627-0.720) |
| Shanghai Cohort (2025) [5] | RF, XGBoost, GBM, AdaBoost, LightGBM, ANN | 11,728 records | Female age, grades of transferred embryos, number of usable embryos, endometrial thickness | Random Forest | AUC: >0.8 |
| Advanced ML Paradigms (2024) [7] | LR, Gaussian NB, SVM, MLP, KNN, Ensemble Models | Not specified | Patient demographics, infertility factors, treatment protocols | Logit Boost | Accuracy: 96.35% |
The variation in model performance across studies highlights several critical challenges in ART prediction. First, feature heterogeneity is apparent, with different studies prioritizing distinct predictor combinations. Second, dataset size and quality significantly impact model robustness, with larger datasets generally yielding more reliable models. Third, algorithm selection plays a crucial role, with no single model consistently outperforming others across all datasets and contexts.
Key Experimental Protocols in ML-Driven ART Prediction
Data Collection and Preprocessing Protocol
Purpose: To systematically collect and prepare ART cycle data for predictive modeling.
Materials:
- Electronic Health Record (EHR) system with ART cycle data
- Data anonymization software
- Statistical software (R, Python, SPSS)
Procedure:
- Data Extraction: Retrieve comprehensive ART cycle data including:
- Demographic parameters (female and male age, BMI, ethnicity)
- Infertility factors (duration, type, cause)
- Treatment parameters (Gn dosage, stimulation protocol, insemination method)
- Laboratory values (basal FSH, E2, LH, progesterone on HCG day)
- Embryology data (number of oocytes, fertilization rate, embryo quality)
- Outcome measures (clinical pregnancy, live birth) [2] [5]
Data Cleaning:
Feature Engineering:
Data Partitioning:
Predictive Model Development Protocol
Purpose: To construct and validate ML models for ART success prediction.
Materials:
- ML platforms (R with caret, xgboost, bonsai packages; Python with PyTorch)
- High-performance computing resources
Procedure:
- Algorithm Selection: Choose multiple ML algorithms representing different approaches:
Hyperparameter Tuning:
- Implement grid search or random search approaches
- Use 5-fold cross-validation on training data
- Optimize for AUC (Area Under the ROC Curve) as primary metric [5]
Model Training:
- Train each algorithm on the training dataset
- Apply regularization techniques to prevent overfitting
- For ensemble methods, set appropriate number of estimators and learning rates
Model Validation:
Model Interpretation:
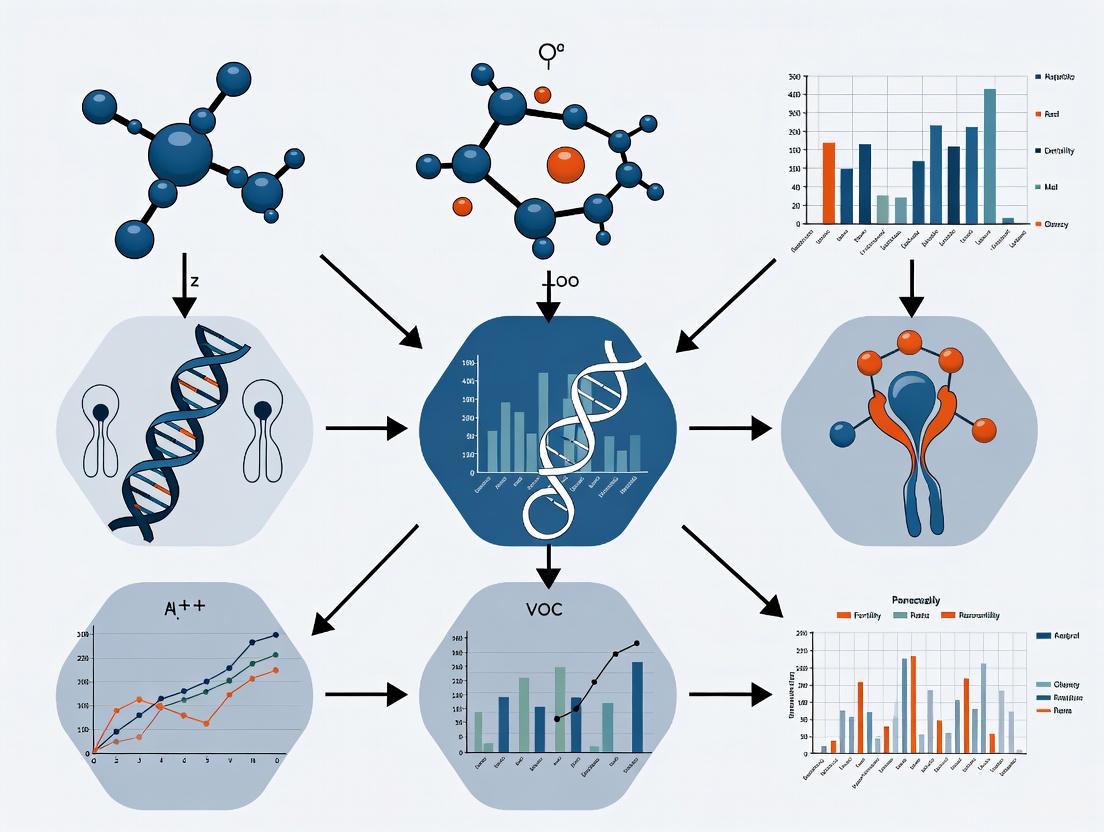
Visualization of ML Workflow for ART Prediction
The following diagram illustrates the comprehensive workflow for developing ML models in ART success prediction, from data collection to clinical application.
Diagram 1: ML Workflow for ART Outcome Prediction. This diagram illustrates the comprehensive process from data collection to clinical implementation, highlighting key challenges at each stage.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Materials and Computational Tools for ML in ART Research
| Item Category | Specific Examples | Function in ART Prediction Research |
|---|---|---|
| Data Collection Tools | Electronic Health Record (EHR) systems, Laboratory Information Management Systems (LIMS), Clinical data abstraction forms | Standardized capture of demographic, clinical, and laboratory parameters essential for model development [2] [5] |
| Statistical Software | R (version 4.4.0+), Python (version 3.8+), SPSS (version 26+) | Data preprocessing, statistical analysis, and implementation of machine learning algorithms [2] [5] |
| Machine Learning Libraries | caret (R), xgboost (R/Python), bonsai (R), Scikit-learn (Python), PyTorch (Python) | Provides algorithms for classification, regression, and ensemble methods; enables model training and validation [5] |
| Feature Selection Tools | Random Forest importance scores, Multivariate logistic regression, Recursive feature elimination | Identifies most predictive variables from numerous potential features to create parsimonious models [2] |
| Model Validation Frameworks | k-fold cross-validation, Bootstrap methods, Train-test split | Assesses model performance and generalizability while mitigating overfitting [2] [5] |
| Mycophenolate Mofetil-d4 | Mycophenolate Mofetil-d4, MF:C23H31NO7, MW:437.5 g/mol | Chemical Reagent |
| D,L-erythro-PDMP | D,L-erythro-PDMP, MF:C23H38N2O3, MW:390.6 g/mol | Chemical Reagent |
Discussion and Future Directions
The clinical challenge of predicting ART success persists due to the complex, multifactorial nature of human reproduction and the limitations of traditional statistical approaches. Machine learning offers promising avenues to address these challenges by identifying complex, non-linear patterns in high-dimensional data. However, several methodological considerations must be addressed to advance the field.
First, feature standardization across studies is crucial. While female age consistently emerges as the most significant predictor across studies [6], the inclusion of additional features varies considerably. Developing a core outcome set for ART prediction research would enhance comparability and facilitate model generalizability. Second, model interpretability remains essential for clinical adoption. While complex ensemble methods and neural networks may achieve high accuracy, their "black box" nature can limit clinical utility. Techniques such as partial dependence plots and feature importance rankings help bridge this gap [5].
Future research should prioritize external validation of existing models across diverse populations and clinical settings. Most current models demonstrate robust performance in internal validation but lack verification in external cohorts [2] [5]. Additionally, temporal validation is necessary to assess model performance over time as clinical practices evolve. The integration of novel data types, including imaging data (embryo morphology), -omics data (genomics, proteomics), and time-series laboratory values, may further enhance predictive accuracy.
Finally, the development of user-friendly implementation tools, such as web-based calculators and clinical decision support systems integrated into electronic health records, will be essential for translating predictive models into routine clinical practice [5]. Such tools can facilitate personalized treatment planning, set realistic patient expectations, and ultimately improve the efficiency and success of ART treatments.
Core Machine Learning Concepts for Biomedical Researchers
The application of machine learning (ML) in biomedical research represents a paradigm shift from traditional statistical methods, offering powerful capabilities for identifying complex patterns in high-dimensional data. Within reproductive medicine, this is particularly crucial for researching rare fertility outcomes, where conventional approaches often struggle due to limited sample sizes and multifactorial determinants. ML predictive models can analyze extensive datasets to uncover subtle relationships that may escape human observation or standard analysis, potentially accelerating discoveries in assisted reproductive technology (ART) success optimization [8]. For researchers investigating rare fertility events—such as specific implantation failure patterns or unusual treatment responses—these methods provide an unprecedented opportunity to develop personalized prognostic tools and enhance clinical decision-making.
The inherent complexity of human reproduction, combined with the ethical and practical challenges of conducting large-scale clinical trials in fertility research, makes ML approaches particularly valuable. By leveraging existing clinical data, ML models can help identify key predictive features for outcomes like live birth following embryo transfer, enabling more targeted interventions and improved resource allocation in fertility treatments [9]. However, the implementation of ML in this sensitive domain requires rigorous methodology and a thorough understanding of both computational and clinical principles to ensure models are both technically sound and clinically relevant.
Core Machine Learning Concepts
Fundamental Terminology and Processes
Machine learning encompasses a diverse set of algorithms that can learn patterns from data without explicit programming. For biomedical researchers, understanding several key concepts is essential for appropriate model selection and interpretation:
Supervised Learning: The most common approach in biomedical prediction research, where models learn from labeled training data to make predictions on unseen data. This includes both classification (predicting categorical outcomes) and regression (predicting continuous values) tasks. In fertility research, this might involve predicting live birth (categorical) or estimating implantation potential (continuous) based on patient characteristics [8].
Unsupervised Learning: Algorithms that identify inherent patterns or groupings in data without pre-existing labels. These methods are particularly valuable for exploratory analysis, such as identifying novel patient subgroups with similar phenotypic characteristics that may correlate with rare fertility outcomes.
Overfitting: A critical challenge in ML where a model learns the training data too well, including its noise and random fluctuations, consequently performing poorly on new, unseen data. This risk is especially pronounced when working with rare outcomes where positive cases may be limited [8].
Data Leakage: Occurs when information from outside the training dataset is used to create the model, potentially leading to overly optimistic performance estimates that fail to generalize to real-world settings. This can happen when future information inadvertently influences model training, violating the temporal sequence of clinical events [8].
Machine Learning Model Categories
Table 1: Common Machine Learning Algorithms in Biomedical Research
| Algorithm Category | Key Examples | Strengths | Weaknesses | Fertility Research Applications |
|---|---|---|---|---|
| Tree-Based Ensembles | Random Forest, XGBoost, GBM, LightGBM | High predictive accuracy, handles mixed data types, provides feature importance | Can become complex, computationally intensive with large datasets | Live birth prediction, embryo selection, treatment response forecasting [9] |
| Neural Networks | Artificial Neural Networks (ANN), Deep Learning | Highly flexible, models complex non-linear relationships | Requires substantial computational resources, prone to overfitting | Image analysis (embryo quality assessment), complex pattern recognition |
| Other Ensemble Methods | AdaBoost | Focuses on misclassified instances, straightforward implementation | May struggle with noisy data and outliers | Risk stratification, outcome classification |
Practical Protocols for Predictive Modeling in Fertility Research
Data Preparation and Preprocessing Protocol
Objective: To transform raw clinical data into a structured format suitable for machine learning analysis while preserving biological relevance and preventing data leakage.
Materials and Reagents:
- R statistical environment (version 4.4 or higher) or Python (version 3.8 or higher)
- Specialized packages:
caret(R),missForest(R),xgboost(R/Python),bonsai(R) for LightGBM [9] - Clinical dataset with appropriate ethical approvals
Step-by-Step Procedure:
- Data Collection and Ethical Compliance: Retrieve anonymized patient data from electronic health records with appropriate institutional review board approval. For fertility research, key data elements may include patient age, ovarian reserve markers, embryo quality metrics, and treatment protocols [9].
Cohort Definition: Apply inclusion and exclusion criteria specific to the research question. For example, in studying fresh embryo transfer outcomes, one might include patients undergoing cleavage-stage embryo transfer while excluding those using donor gametes or preimplantation genetic testing [9].
Missing Data Imputation: Address missing values using appropriate methods such as the non-parametric
missForestalgorithm, which is particularly effective for mixed-type data commonly encountered in clinical datasets [9].Feature Selection: Implement a tiered approach combining statistical criteria (e.g., p < 0.05 in univariate analysis) and clinical expert validation to eliminate biologically irrelevant variables while retaining clinically meaningful predictors [9].
Data Partitioning: Split data into derivation (training) and validation sets using appropriate strategies such as random split, time-based split, or patient-based split to ensure independent model evaluation [8].
Model Training and Validation Protocol
Objective: To develop and validate robust predictive models using appropriate machine learning algorithms with rigorous evaluation protocols.
Step-by-Step Procedure:
- Algorithm Selection: Choose multiple ML algorithms based on the specific prediction task and dataset characteristics. Common choices include Random Forest, XGBoost, and Artificial Neural Networks [9].
Hyperparameter Tuning: Implement a grid search approach with 5-fold cross-validation to optimize model hyperparameters, using the area under the receiver operating characteristic curve (AUC) as the primary evaluation metric [9].
Model Training: Train each algorithm on the derivation dataset using the optimized hyperparameters, ensuring proper separation between training and validation data throughout the process.
Performance Evaluation: Assess model performance on the testing data using multiple metrics including AUC, accuracy, sensitivity, specificity, precision, recall, and F1-score to provide a comprehensive view of model capabilities [9] [8].
Validation and Generalizability Assessment: Conduct sensitivity analyses including subgroup analysis (stratified by key clinical variables) and perturbation analysis to assess model stability and generalizability across different patient populations [9].
Model Interpretation and Clinical Implementation Protocol
Objective: To extract clinically meaningful insights from trained models and facilitate their translation into practical tools for fertility research and clinical decision support.
Step-by-Step Procedure:
- Feature Importance Analysis: Identify the most influential predictors from the best-performing model using built-in importance metrics or permutation-based methods.
Partial Dependence Analysis: Generate partial dependence (PD) plots to visualize the marginal effect of key features on the predicted outcome, helping to elucidate complex relationships between predictors and fertility outcomes [9].
Interaction Effects Exploration: Construct 2D partial dependence plots to explore interaction effects among important features, revealing how combinations of factors jointly influence predicted outcomes.
Clinical Tool Development: For promising models, develop user-friendly interfaces such as web-based tools to assist clinicians in predicting outcomes and individualizing treatments based on patient-specific data [9].
Reporting and Documentation: Comprehensively document all aspects of the modeling process following established guidelines for transparent reporting of predictive models in biomedical research [8].
Visualization of Machine Learning Workflows
Figure 1: End-to-end machine learning workflow for fertility outcomes research, showing the progression from data collection through clinical implementation.
Figure 2: Model validation framework illustrating the process of algorithm comparison, hyperparameter tuning, and rigorous performance assessment essential for trustworthy fertility outcome predictions.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools for ML in Fertility Research
| Tool Category | Specific Solutions | Key Functionality | Application in Fertility Research |
|---|---|---|---|
| Programming Environments | R (v4.4+), Python (v3.8+) | Statistical computing, machine learning implementation | Primary platforms for data analysis and model development [9] |
| ML Packages & Libraries | caret, xgboost, bonsai, Torch | Algorithm implementation, hyperparameter tuning | Model training for outcome prediction [9] |
| Data Imputation Tools | missForest | Nonparametric missing value estimation | Handling missing clinical data in fertility datasets [9] |
| Model Interpretation Packages | PD, LD, AL profile generators | Visualization of feature effects and interactions | Understanding key predictors of ART success [9] |
| Web Development Frameworks | Shiny (R), Flask (Python) | Interactive tool development | Creating clinical decision support systems [9] |
| sec-O-Glucosylhamaudol | sec-O-Glucosylhamaudol, CAS:80681-44-3, MF:C21H26O10, MW:438.4 g/mol | Chemical Reagent | Bench Chemicals |
| Monodes(N-carboxymethyl)valine Daclatasvir | Monodes(N-carboxymethyl)valine Daclatasvir, CAS:1007884-60-7, MF:C33H39N7O3, MW:581.7 g/mol | Chemical Reagent | Bench Chemicals |
Application to Rare Fertility Outcomes Research
The implementation of machine learning in rare fertility outcomes research requires special methodological considerations. When dealing with infrequent events, several strategies can enhance model performance and clinical utility:
Addressing Class Imbalance: Rare outcomes naturally create imbalanced datasets where positive cases are substantially outnumbered by negative cases. Techniques such as strategic sampling, algorithm weighting, or ensemble methods can help mitigate the bias toward the majority class that might otherwise dominate model training.
Feature Selection for Rare Outcomes: Identifying predictors specifically relevant to rare outcomes often requires hybrid approaches combining data-driven selection with deep clinical expertise. Domain knowledge becomes particularly valuable in recognizing biologically plausible relationships that may have strong predictive power despite limited occurrence in the dataset.
Multi-Model Validation: Given the challenges of predicting rare events, employing multiple algorithms with different inductive biases provides a more robust approach than reliance on a single method. The comparative analysis of Random Forest, XGBoost, and other algorithms in fertility research has demonstrated that performance can vary significantly across different outcome types and patient subgroups [9].
Clinical Integration Pathways: For rare outcome prediction models to impact clinical practice, they must be integrated into workflows in ways that complement clinical expertise. Web-based tools that provide individualized risk estimates based on model outputs can support shared decision-making without replacing clinical judgment [9].
By adhering to rigorous methodology and maintaining focus on clinical relevance, biomedical researchers can leverage machine learning to advance understanding of rare fertility outcomes despite the inherent challenges of limited data. The continuous refinement of these models through iterative development and validation promises to enhance their predictive accuracy and ultimately improve outcomes for patients facing complex fertility challenges.
Within the expanding field of assisted reproductive technology (ART), a paradigm shift is underway towards data-driven prognostication. Infertility affects an estimated 15% of couples globally, yet success rates for interventions like in vitro fertilization (IVF) have plateaued around 30% [9]. This clinical challenge has intensified the focus on developing robust prediction models to enhance outcomes and personalize treatment. Machine learning (ML) models are now demonstrating superior performance for live birth prediction (LBP) compared to traditional statistical methods, with center-specific models (MLCS) showing significant improvements in minimizing false positives and negatives [10]. The clinical utility of these models hinges on identifying and accurately measuring key predictive features. This application note details the core biomarkers—female age, embryo quality, and critical hormonal and ultrasonographic markers—within the context of advanced predictive analytics for rare fertility outcomes research. We provide structured quantitative summaries and detailed experimental protocols to standardize their assessment for model integration.
Quantitative Data Synthesis of Key Predictive Features
The following tables consolidate quantitative evidence on the impact of key predictive features on fertility outcomes, as reported in recent clinical studies and ML model analyses.
Table 1: Impact of Female Age on Pregnancy and Live Birth Outcomes
| Age Group | Clinical Pregnancy Rate (CPR) | Ongoing Pregnancy Rate (OPR) | Live Birth Rate (LBR) | Key Statistical Findings |
|---|---|---|---|---|
| <30 years | 61.40% [11] | 54.21% [11] | Significantly higher [12] | Reference group for comparisons [12] |
| 30-34 years | Not Specified | Not Specified | Significantly higher than ≥35 group [12] | Implantation rate significantly lower than <30 group [12] |
| ≥35 years | Significantly lower [12] | Not Specified | Significantly lower [12] | CPR decreased by 10% per year after 34 (aOR 0.90, 95% CI 0.84–0.96) [11] |
| ≥40 years (Donor Oocytes) | Not Applicable | Not Applicable | Decreasing after age 40 [13] | Annual increase in implantation failure (RR=1.042) and pregnancy loss (RR=1.032) [13] |
Table 2: Impact of Embryo and Treatment Cycle Factors on Outcomes
| Predictive Feature | Outcome Measured | Effect Size & Statistical Significance | Study Details |
|---|---|---|---|
| Number of High-Quality Embryos Transferred | Clinical Pregnancy | Significantly higher in pregnancy group (t=5.753, P<0.0001) [12] | FET Cycles (N=1031) [12] |
| Number of Embryos Transferred | Clinical Pregnancy | Significantly higher in pregnancy group (t=4.092, P<0.0001) [12] | FET Cycles (N=1031) [12] |
| Blastocyst Transfer (vs. Cleavage) | Pregnancy Outcomes | "Significantly better," pronounced in older patients [11] | eSET Cycles (N=7089) [11] |
| Endometrial Thickness | Live Birth | Key predictive feature in ML model [9] | Fresh Embryo Transfer (N=11,728) [9] |
| Oil-Based Contrast (HSG) | Pregnancy Rate | 51% higher vs. water-based (OR=1.51, 95% CI 1.23-1.86) [14] | Meta-analysis (N=4,739 patients) [14] |
Experimental Protocols for Predictive Feature Analysis
Protocol 1: Development and Validation of a Center-Specific ML Model for Live Birth Prediction
This protocol outlines the procedure for developing a machine learning model to predict live birth outcomes following fresh embryo transfer, as validated in a large clinical dataset [9].
1. Data Collection and Preprocessing
- Data Source: Collect retrospective ART cycle records from a single or multicenter database. A study by Liu et al. (2025) initiated this process with 51,047 records [9].
- Inclusion/Exclusion Criteria:
- Inclusion: Cycles involving fresh embryo transfer with fully tracked outcomes.
- Exclusion: Apply filters for female age >55 years, male age >60 years, use of donor sperm, and non-cleavage-stage transfers. This refined the dataset to 11,728 records for analysis [9].
- Feature Set: Extract a comprehensive set of pre-pregnancy features (e.g., 55-75 variables), including female age, embryo grades, number of usable embryos, endometrial thickness, and hormonal markers [9].
- Data Imputation: Handle missing values using a non-parametric method such as
missForest, which is efficient for mixed-type data [9].
2. Model Training and Validation
- Algorithm Selection: Employ multiple machine learning algorithms to construct and compare prediction models. Common choices include:
- Random Forest (RF)
- eXtreme Gradient Boosting (XGBoost)
- Gradient Boosting Machines (GBM)
- Light Gradient Boosting Machine (LightGBM)
- Artificial Neural Network (ANN) [9]
- Hyperparameter Tuning: Use a grid search approach with 5-fold cross-validation on the training data to optimize hyperparameters, selecting those that yield the highest average Area Under the Curve (AUC) [9].
- Model Validation: Split the data into training and testing sets. Evaluate the final model's performance on the held-out test set using metrics including AUC, accuracy, sensitivity, specificity, precision, and F1 score [9].
3. Model Interpretation and Deployment
- Feature Importance: Analyze the best-performing model (e.g., Random Forest) to identify the most influential predictive features. Key features often include female age, grades of transferred embryos, number of usable embryos, and endometrial thickness [9].
- Model Explanation: Utilize techniques like Partial Dependence (PD) plots, Accumulated Local (AL) profiles, and breakdown profiles to explain the model's predictions at both the dataset and individual patient levels [9].
- Clinical Tool Development: Develop a web-based tool to allow clinicians to input patient data and receive a personalized live birth probability, facilitating individualized treatment planning [9].
Protocol 2: Assessing the Impact of Female Age on Outcomes in Elective Single Embryo Transfer (eSET) Cycles
This protocol describes a retrospective cohort study design to elucidate the non-linear relationship between female age and pregnancy outcomes in a first eSET cycle [11].
1. Cohort Definition and Data Acquisition
- Study Population: Identify patients undergoing their first IVF/ICSI cycle with an elective single embryo transfer, defined as a transfer where supernumerary embryos are available for freezing [11].
- Exclusion Criteria: Exclude patients with chromosomal abnormalities, endocrine diseases, recurrent abortion, or those undergoing operative sperm extraction cycles [11].
- Data Extraction: Obtain de-identified data from the ART database, including female age, infertility diagnosis, stimulation protocol, embryo stage and quality, and outcomes.
2. Outcome Measures and Statistical Analysis
- Primary Outcomes:
- Clinical Pregnancy Rate (CPR): Confirmed by the detection of at least one gestational sac via ultrasound 4-5 weeks post-transfer.
- Ongoing Pregnancy Rate (OPR): Defined as a living intrauterine pregnancy lasting until the 12th week of gestation [11].
- Statistical Modeling:
- Use a Generalized Additive Model (GAM) to examine the dose-response correlation between female age as a continuous variable and the log-odds of CPR/OPR, allowing for non-linear relationships.
- Employ a logistic regression model to ascertain the correlation and calculate odds ratios (ORs) with 95% confidence intervals (CIs), adjusting for potential confounders such as embryo stage (cleavage vs. blastocyst) [11].
- Threshold Analysis: Model the specific age at which CPR and OPR begin to decrease significantly. For example, one study found that for patients aged ≥34, CPR decreased by 10% for each 1-year age increase (aOR 0.90) [11].
Protocol 3: Evaluation of Contrast Media in Hysterosalpingography (HSG) for Fertility Enhancement
This protocol is based on a systematic review and meta-analysis methodology to compare the therapeutic effects of oil-based versus water-based contrast media in HSG [14].
1. Literature Search and Study Selection
- Search Strategy: Execute searches in major electronic databases (e.g., PubMed, Web of Science, Scopus) using keywords related to "hysterosalpingography," "oil-based contrast," "water-based contrast," and "tubal flushing" until the current date of analysis.
- Eligibility Criteria:
- Inclusion: Include all primary Randomized Controlled Trials (RCTs) comparing oil-based versus water-based contrast media in women of childbearing age with infertility.
- Exclusion: Exclude non-RCTs, such as case reports, reviews, and studies without a comparison group or that do not evaluate fertility outcomes [14].
2. Data Extraction and Quality Assessment
- Outcome Extraction: From each included RCT, extract data on primary and secondary outcomes, including:
- Pregnancy rate
- Live birth rate
- Miscarriage rate
- Ectopic pregnancy rate
- Adverse effects (abdominal pain, vaginal bleeding, intravasation) [14]
- Risk of Bias Assessment: Assess the quality of each included RCT using the Cochrane risk of bias tool, evaluating domains like random sequence generation, allocation concealment, blinding of participants and personnel, and blinding of outcome assessment [14].
3. Statistical Synthesis
- Meta-Analysis: Perform statistical analysis using software like RevMan. For dichotomous outcomes (e.g., pregnancy rate), calculate pooled odds ratios (ORs) with 95% CIs using the Mantel-Haenszel method.
- Heterogeneity: Assess statistical heterogeneity among the studies using the I² statistic and the chi-square test (p-value < 0.1 considered significant). If substantial heterogeneity exists, explore sources and consider using a random-effects model or performing sensitivity analyses (e.g., leave-one-out method) [14].
Visualizations
ML Model Workflow for Live Birth Prediction
Key Predictive Features and Pathways to Outcome
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Analytical Tools for Fertility Prediction Research
| Item / Solution | Function / Application | Specific Example / Note |
|---|---|---|
| Oil-Based Contrast Media | Used in HSG for tubal patency evaluation and therapeutic flushing. | Ethiodized poppyseed oil (e.g., Lipiodol). Associated with significantly higher subsequent pregnancy rates [14] [15]. |
| Water-Based Contrast Media | Aqueous agent for diagnostic HSG. | Provides diagnostic images but may be less effective in enhancing fertility compared to oil-based agents [14] [15]. |
| Gonadotropins (Gn) | Stimulate follicular development during controlled ovarian stimulation. | Dosage is personalized to maximize oocyte yield while minimizing OHSS risk [11] [12]. |
| GnRH Agonist/Antagonist | Prevents premature luteinizing hormone (LH) surge during ovarian stimulation. | Agonist (e.g., Diphereline) or antagonist protocol used based on patient profile [11]. |
| Human Chorionic Gonadotropin (hCG) | Triggers final oocyte maturation. | Administered subcutaneously (e.g., 4,000-10,000 IU) when follicles reach optimal size [11] [12]. |
| Vitrification Kit | For cryopreservation of supernumerary embryos. | Essential for freeze-thaw embryo transfer (FET) cycles. Includes equilibration and vitrification solutions [12]. |
| R Software with Caret Package | Primary platform for statistical analysis and machine learning model development. | Used for data preprocessing, model training (RF, GBM, AdaBoost), and validation [9]. |
| Python with Torch | Platform for developing complex models like Artificial Neural Networks (ANN). | Used for implementing deep learning architectures in predictive modeling [9]. |
| Phenylbutazone(diphenyl-d10) | Phenylbutazone(diphenyl-d10), CAS:1219794-69-0, MF:C19H20N2O2, MW:318.4 g/mol | Chemical Reagent |
| D-Arabinopyranose | D-Arabinopyranose, CAS:28697-53-2, MF:C5H10O5, MW:150.13 g/mol | Chemical Reagent |
ML Algorithms in Action: Methodologies for Fertility Outcome Prediction
This application note provides a structured framework for the comparative analysis of supervised learning algorithms—Random Forest (RF), eXtreme Gradient Boosting (XGBoost), Support Vector Machine (SVM), and Artificial Neural Networks (ANN)—within the context of rare fertility outcomes research. We present standardized protocols for model development, performance assessment, and implementation, supported by quantitative performance data from recent fertility studies. The document aims to equip researchers and drug development professionals with practical tools to build robust, clinically applicable prediction models for outcomes such as live birth, missed abortion, and clinical pregnancy.
Predicting rare fertility outcomes, such as live birth or specific complications following Assisted Reproductive Technology (ART), presents a significant challenge in reproductive medicine. Traditional statistical methods often fall short in capturing the complex, non-linear relationships between multifaceted patient characteristics and these outcomes. Supervised machine learning (ML) offers a powerful alternative for constructing prognostic models. This document details a standardized protocol for comparing four prominent algorithms—RF, XGBoost, SVM, and ANN—to facilitate their effective application in predicting rare fertility endpoints, thereby supporting clinical decision-making and advancing personalized treatment strategies in reproductive health [9] [16].
Quantitative Performance Comparison in Fertility Research
The performance of ML algorithms can vary significantly based on the dataset, specific fertility outcome, and feature set. The following table summarizes the reported performance metrics of RF, XGBoost, SVM, and ANN across recent studies focused on ART outcomes.
Table 1: Comparative Performance of Supervised Learning Algorithms on Various Fertility Outcomes
| Fertility Outcome | Study/Context | Best Performing Algorithm(s) (Performance Metric) | Comparative Performance of Other Algorithms |
|---|---|---|---|
| Live Birth | Fresh embryo transfer (n=11,728); 55 features [9] | RF (AUC > 0.80) | XGBoost was second-best; GBM, AdaBoost, LightGBM, ANN were also tested. |
| Live Birth | IVF treatment (n=11,486); 7 key predictors [2] | Logistic Regression (AUC 0.674) & RF (AUC 0.671) | XGBoost and LightGBM were also constructed but were not top performers. |
| Live Birth | Prediction before IVF treatment [16] | RF (F1-score: 76.49%, AUC: 84.60%) | Models were also tested with and without feature selection. |
| Missed Abortion | IVF-ET patients (n=1,017) [17] | XGBoost (Training AUC: 0.877, Test AUC: 0.759) | Outperformed a traditional logistic regression model (Test AUC: 0.695). |
| Clinical Pregnancy | Embryo morphokinetics analysis [18] | RF (AUC: 0.70) | Used a supervised random forest algorithm on time-lapse microscopy data. |
| Fertility Preferences | Population survey in Nigeria (n=37,581) [19] | RF (Accuracy: 92%, AUC: 92%) | Outperformed Logistic Regression, SVM, K-Nearest Neighbors, Decision Tree, and XGBoost. |
Key Insights from Comparative Data
- Algorithm Dominance: Tree-based ensemble methods, particularly Random Forest and XGBoost, consistently rank among the top performers across diverse fertility prediction tasks, from clinical outcomes like live birth [9] to population-level analyses [19].
- Context Matters: The optimal algorithm is use-case dependent. For instance, while complex models like XGBoost excelled in predicting missed abortion [17], a simpler Logistic Regression model performed on par with Random Forest in a study focused on a limited set of seven key predictors for live birth [2].
- Performance Range: Areas Under the Curve (AUC) for these models in fertility research typically range from approximately 0.67 to over 0.80, and accuracy can exceed 90% for specific classification tasks [19], demonstrating the potential of ML to deliver clinically relevant predictive power.
Experimental Protocols for Model Development
Protocol 1: Data Preprocessing and Feature Engineering
Objective: To prepare a raw clinical dataset for robust model training by addressing data quality and enhancing predictive features.
Materials: Raw clinical data (e.g., from Electronic Health Records), computing environment (R or Python).
Procedure:
- Data Cleaning:
- Handle missing values using techniques like multiple imputation by chained equations (MICE) or the
missForestalgorithm for mixed-type data [9] [19]. - Address class imbalance in the outcome variable (e.g., using the Synthetic Minority Oversampling Technique (SMOTE)) to prevent model bias toward the majority class [19].
- Handle missing values using techniques like multiple imputation by chained equations (MICE) or the
- Feature Engineering:
- Create new, potentially informative variables from existing ones. For example, generate interaction terms such as the "Average," "Summation," and "Difference" of biochemical markers like hCG MoM and PAPP-A MoM in prenatal screening [20].
- Recode continuous variables into categorical bins and group low-frequency categories in categorical variables [19].
- Feature Selection:
- Employ a multi-step approach to identify the most predictive features:
- Initial Screening: Use bivariate analysis (e.g., logistic regression) to assess individual feature associations with the outcome [19].
- Advanced Filtering: Apply Recursive Feature Elimination (RFE) to iteratively remove the least important features [19].
- Expert Validation: Combine data-driven criteria (e.g., p-value < 0.05 or top-ranked features by RF importance) with clinical expert validation to eliminate biologically irrelevant variables and retain clinically critical ones [9]. This ensures model parsimony and clinical relevance.
- Employ a multi-step approach to identify the most predictive features:
Protocol 2: Model Training and Hyperparameter Tuning
Objective: To train the four candidate algorithms and optimize their hyperparameters to achieve maximum predictive performance.
Materials: Preprocessed dataset from Protocol 1, software libraries (e.g., scikit-learn, xgboost, caret in R).
Procedure:
- Data Splitting: Partition the preprocessed data into a training set (e.g., 70-80%) and a hold-out test set (e.g., 20-30%) [17].
- Model Training Setup:
- Initialize the four algorithms with a set of default or reasonable starting hyperparameters.
- Random Forest: Key parameters include number of trees (
n_estimators), maximum tree depth (max_depth), and number of features considered for a split (max_features). - XGBoost: Key parameters include learning rate (
eta), maximum depth (max_depth), number of boosting rounds (n_estimators), and L1/L2 regularization terms (alpha,lambda) [21]. - Support Vector Machine: Key parameter is the kernel type (e.g., Radial Basis Function, linear), and regularization parameter (
C). - Artificial Neural Network: Key parameters include the number of hidden layers and units, activation functions, learning rate, and dropout rate for regularization [9].
- Hyperparameter Tuning:
- Employ a grid search or random search approach [9].
- Use 5-fold or 10-fold cross-validation on the training set to evaluate each hyperparameter combination. This involves splitting the training data into k folds, training the model on k-1 folds, and validating on the remaining fold, repeating this process k times [2].
- Select the hyperparameter set that yields the highest average performance (e.g., AUC) across the k validation folds.
- Final Model Training: Retrain each algorithm on the entire training set using its respective optimized hyperparameters.
Protocol 3: Model Evaluation and Interpretation
Objective: To assess the generalizability and clinical utility of the trained models and interpret their predictions.
Materials: Trained models from Protocol 2, hold-out test set.
Procedure:
- Performance Evaluation:
- Apply the final models to the hold-out test set.
- Calculate a comprehensive set of metrics [9] [16]:
- Discrimination: Area Under the Receiver Operating Characteristic Curve (AUC).
- Calibration: Brier Score (closer to 0 indicates better calibration) [2].
- Overall Performance: Accuracy, F1-score, Precision, Recall.
- Model Interpretation:
- Global Interpretability: Use permutation importance or Gini importance (for tree-based models) to identify which features had the most significant overall impact on the model's predictions [19].
- Local Interpretability: For specific predictions, use techniques like SHAP (SHapley Additive exPlanations) or Breakdown profiles to understand the contribution of each feature to an individual patient's risk score [9].
- Visualization: Examine Partial Dependence Plots (PDPs) or Accumulated Local (AL) plots to understand the marginal effect of a key feature (e.g., maternal age) on the predicted outcome [9].
Visualization of the Model Development Workflow
The following diagram illustrates the end-to-end workflow for developing and validating a machine learning model for rare fertility outcomes, as outlined in the experimental protocols.
The Scientist's Toolkit: Essential Research Reagents & Solutions
This section catalogues critical data types and methodological components required for constructing robust fertility prediction models.
Table 2: Essential "Research Reagents" for Fertility Outcome Prediction Models
| Category | Item / Data Type | Function / Relevance in the Experiment | Example from Literature |
|---|---|---|---|
| Clinical Data | Maternal Age | Single most consistent predictor of ART success [2]. | Used in all cited studies; identified as a top feature [2] [9] [16]. |
| Clinical Data | Hormone Levels (FSH, AMH, LH, P, E2) | Assess ovarian reserve and endocrine status; key predictors of response and outcome [2] [9] [17]. | Basal FSH, E2/LH/P on HCG day were key for live birth model [2]. AMH was a selected feature [9]. |
| Clinical Data | Embryo Morphology/Grade | Assesses embryo viability for selection in fresh transfers [9]. | Grades of transferred embryos were a key predictive feature [9]. |
| Clinical Data | Endometrial Thickness | Assess uterine receptivity for embryo implantation [9]. | Identified as a significant feature for live birth prediction [9]. |
| Clinical Data | Semen Parameters | Evaluates male factor infertility (concentration, motility, morphology) [2] [16]. | Progressive sperm motility was a key predictor [2]. |
| Immunological Factors | Anticardiolipin Antibody (ACA), TPO-Ab | Identify immune dysregulations associated with pregnancy loss [17]. | Were independent risk factors for missed abortion [17]. |
| Methodology | Hyperparameter Optimization (HPO) | Systematically search for the best model parameters to maximize performance and avoid overfitting. | Grid search with cross-validation was used to optimize models [9]. |
| Methodology | Synthetic Data Generation (e.g., GPT-4) | Addresses class imbalance for rare outcomes by generating synthetic minority-class samples [20]. | Used GPT-4o to generate synthetic samples for Down Syndrome risk prediction [20]. |
| Software & Libraries | R (caret, xgboost) / Python (scikit-learn) | Primary programming environments and libraries for data preprocessing, model building, and evaluation. | R (caret, xgboost, bonsai) and Python (Torch) were used for model development [9]. |
| Erythromycin-d6 | Erythromycin-d6, CAS:959119-25-6, MF:C37H67NO13, MW:740.0 g/mol | Chemical Reagent | Bench Chemicals |
| 4-Methylpentanal-d7 | 4-Methylpentanal-d7|CAS 1794978-55-4|Isotopic Labeled Reagent | Bench Chemicals |
This application note establishes a standardized, end-to-end protocol for the comparative analysis of RF, XGBoost, SVM, and ANN in predicting rare fertility outcomes. The empirical evidence strongly supports the efficacy of ensemble tree-based methods, while emphasizing that the optimal model is context-dependent. By adhering to the detailed protocols for data preprocessing, rigorous model training with hyperparameter tuning, and comprehensive evaluation outlined herein, researchers can develop transparent, robust, and clinically actionable tools. These tools hold the potential to significantly advance the field of reproductive medicine by enabling personalized prognosis and improving success rates for patients undergoing fertility treatments.
Neural Networks and Support Vector Machines for Complex Pattern Recognition
The application of artificial intelligence (AI) in reproductive medicine represents a paradigm shift in the approach to diagnosing and treating infertility. Machine learning (ML) prediction models, particularly those designed for forecasting rare fertility outcomes, are increasingly critical in a field where treatment success hinges on complex, multifactorial processes. Among the plethora of ML algorithms, neural networks (NNs) and support vector machines (SVMs) have emerged as powerful tools for complex pattern recognition tasks. These models excel at identifying subtle, non-linear relationships within high-dimensional biomedical data, which often elude conventional statistical methods and human observation. Within in vitro fertilization (IVF), the ability to predict outcomes such as implantation, clinical pregnancy, or live birth can directly influence clinical decision-making, optimize laboratory processes, and ultimately improve patient success rates. This document provides detailed application notes and experimental protocols for employing NNs and SVMs in fertility research, framed within the context of a broader thesis on predicting rare fertility outcomes.
Performance Comparison of ML Models in Fertility Outcomes Prediction
Quantitative data from recent studies demonstrate the comparative performance of various ML models, including NNs and SVMs, in predicting critical fertility outcomes. The following tables summarize key performance metrics, providing a benchmark for researchers.
Table 1: Model Performance in Predicting Pregnancy and Live Birth Outcomes
| Study Focus | Best Performing Model(s) | Key Performance Metrics | Dataset Characteristics |
|---|---|---|---|
| General IVF/ICSI Success Prediction [22] | Random Forest (RF) | AUC: 0.97 | 10,036 patient records, 46 clinical features |
| General IVF/ICSI Success Prediction [22] | Neural Network (NN) | AUC: 0.95 | 10,036 patient records, 46 clinical features |
| Live Birth in Endometriosis Patients [23] | XGBoost | AUC (Test Set): 0.852 | 1,836 patients, 8 predictive features |
| Live Birth in Endometriosis Patients [23] | Random Forest (RF) | AUC (Test Set): 0.820 | 1,836 patients, 8 predictive features |
| Live Birth in Endometriosis Patients [23] | K-Nearest Neighbors (KNN) | AUC (Test Set): 0.748 | 1,836 patients, 8 predictive features |
| Embryo Implantation Success (AI-based selection) [24] | Pooled AI Models | Sensitivity: 0.69, Specificity: 0.62, AUC: 0.7 | Meta-analysis of multiple studies |
Table 2: Prevalence of Machine Learning Techniques in ART Success Prediction
| Machine Learning Technique | Frequency of Use | Reported Accuracy Range | Commonly Reported Metrics |
|---|---|---|---|
| Support Vector Machine (SVM) [6] | Most frequently applied (44.44% of studies) | Not Specified | AUC, Accuracy, Sensitivity |
| Random Forest (RF) [6] [22] [23] | Commonly applied | AUC up to 0.97 [22] | AUC, Accuracy, Sensitivity, Specificity |
| Neural Networks (NN) / Deep Learning [6] [22] | Commonly applied | AUC up to 0.95 [22] | AUC, Accuracy |
| Logistic Regression (LR) [6] [23] | Commonly applied | Not Specified | AUC, Sensitivity, Specificity |
| XGBoost [23] | Applied in recent studies | AUC up to 0.852 [23] | AUC, Calibration, Brier Score |
Experimental Protocols for Model Development and Validation
Protocol: Development of a Neural Network for Embryo Viability Scoring
This protocol outlines the steps for creating a convolutional neural network (CNN) to predict embryo implantation potential from time-lapse imaging data.
1. Data Acquisition and Preprocessing: - Image Collection: Acquire a large dataset of time-lapse images or videos of embryos cultured to the blastocyst stage (Day 5). The dataset should be linked to known outcomes (e.g., implantation, no implantation). Sample sizes in recent studies exceed 1,000 embryos [24]. - Labeling: Annotate each embryo image sequence with a binary label (e.g., 1 for implantation success, 0 for failure). Ensure labeling is based on confirmed clinical outcomes. - Preprocessing: Resize all images to a uniform pixel dimension (e.g., 224x224). Apply min-max normalization to scale pixel intensities to a [0, 1] range. This step ensures consistent scaling across variables and improves model convergence [25]. - Data Augmentation: Artificially expand the dataset by applying random, realistic transformations to the images, such as rotation, flipping, and minor brightness/contrast adjustments. This technique helps prevent overfitting. - Data Partitioning: Randomly split the dataset into three subsets: Training Set (70%), Validation Set (15%), and Test Set (15%). The validation set is used for hyperparameter tuning, and the test set for the final, unbiased evaluation.
2. Model Architecture and Training: - Architecture Design: Implement a CNN architecture, such as: - Input Layer: Accepts preprocessed images. - Feature Extraction Backbone: Use a pre-trained network (e.g., ResNet-50) with transfer learning. Remove its final classification layer and freeze the weights of early layers to leverage pre-learned feature detectors. - Custom Classifier: Append new, trainable layers: a Flatten layer, followed by two Dense (fully connected) layers with ReLU activation (e.g., 128 units, then 64 units), including Dropout layers (e.g., rate=0.5) to reduce overfitting. - Output Layer: A final Dense layer with a single unit and sigmoid activation for binary classification. - Compilation: Compile the model using the Adam optimizer and specify the binary cross-entropy loss function. Monitor the accuracy metric. - Model Training: Train the model on the training set for a specified number of epochs (e.g., 50) using mini-batch gradient descent (e.g., batch size=32). Use the validation set to evaluate performance after each epoch and implement early stopping if validation performance plateaus.
3. Model Validation and Interpretation: - Performance Evaluation: Use the held-out test set to calculate final performance metrics, including Area Under the Curve (AUC), Accuracy, Sensitivity, and Specificity [24] [6]. - Explainability: Apply explainable AI techniques like SHapley Additive exPlanations (SHAP) to interpret the model's predictions. This helps identify which morphological features in the embryo images (e.g., cell symmetry, fragmentation) were most influential in the viability score [23].
Protocol: Building an SVM for Predicting Live Birth from Clinical Data
This protocol details the use of an SVM to predict live birth outcomes using structured clinical and demographic data from patients prior to embryo transfer.
1. Feature Engineering and Dataset Preparation: - Feature Selection: From the patient's electronic health records (EHR), identify and extract relevant predictive features. Studies have shown the importance of female age, anti-Müllerian hormone (AMH), antral follicle count (AFC), infertility duration, body mass index (BMI), and previous IVF cycle history [6] [23]. Use algorithms like Least Absolute Shrinkage and Selection Operator (LASSO) or Recursive Feature Elimination (RFE) to select the most non-redundant, predictive features [23]. - Data Cleaning: Handle missing values through imputation (e.g., mean/median for continuous variables, mode for categorical) or removal of instances with excessive missingness. Address class imbalance in the outcome variable (e.g., more failures than live births) using techniques like SMOTE (Synthetic Minority Over-sampling Technique). - Data Scaling: Standardize all continuous features by removing the mean and scaling to unit variance. This is a critical step for SVMs, as they are sensitive to the scale of the data. - Data Splitting: Partition the data into Training (70%), Validation (15%), and Test (15%) sets, ensuring stratification to maintain the same proportion of outcomes in each set.
2. Model Training with Hyperparameter Optimization:
- Algorithm Selection: Choose the Support Vector Classifier (SVC) from an ML library such as scikit-learn.
- Hyperparameter Search: Define a search space for critical hyperparameters:
- Kernel: ['linear', 'radial basis function (RBF)', 'poly']
- Regularization (C): A range of values on a logarithmic scale (e.g., [0.1, 1, 10, 100])
- Kernel Coefficient (gamma): For RBF kernel, use ['scale', 'auto'] or a range of values.
- Optimization Execution: Use a Grid Search or Randomized Search strategy across the defined hyperparameter space, employing the validation set to evaluate performance. The optimal configuration is the one that maximizes the AUC on the validation set [23] [26].
3. Model Evaluation and Clinical Validation: - Final Assessment: Retrain the model on the combined training and validation sets using the optimal hyperparameters. Evaluate its final performance on the untouched test set, reporting AUC, sensitivity, and specificity. - Clinical Utility Assessment: Perform Decision Curve Analysis (DCA) to quantify the clinical net benefit of using the model across different probability thresholds [23].
Visualization of Workflows
The following diagrams, generated with Graphviz DOT language, illustrate the logical workflows for the experimental protocols described above.
Diagram Title: CNN for Embryo Viability Scoring
Diagram Title: SVM Clinical Prediction Workflow
The Scientist's Toolkit: Research Reagent Solutions
The following table details key software, algorithms, and data resources essential for conducting research in this field.
Table 3: Essential Research Tools for ML in Fertility Outcomes
| Tool / Reagent | Type | Function / Application | Examples / Notes |
|---|---|---|---|
| scikit-learn [6] | Software Library | Provides implementations of classic ML algorithms, including SVM, Random Forest, and data preprocessing tools. | Ideal for structured, tabular clinical data. Used for model development and hyperparameter tuning. |
| TensorFlow / PyTorch | Software Framework | Open-source libraries for building and training deep neural networks. | Essential for developing custom CNN architectures for image analysis (e.g., embryo time-lapse). |
| SHAP (SHapley Additive exPlanations) [23] | Interpretation Algorithm | Explains the output of any ML model by quantifying the contribution of each feature to a single prediction. | Critical for model transparency and identifying key clinical predictors like female age and AMH. |
| Hyperparameter Optimization Algorithms [26] | Methodology | Automated search strategies for finding the best model configuration. | Includes Grid Search and Random Search. Crucial for maximizing SVM and NN performance. |
| Structured Clinical Datasets [6] [22] [23] | Data | Retrospective data from IVF cycles including patient demographics, hormone levels, and treatment outcomes. | Must include key features like female age, AMH, AFC, and infertility duration. Sample sizes >1,000 records are typical. |
| Time-lapse Imaging (TLI) Datasets [24] | Data | Annotated image sequences of developing embryos linked to known implantation outcomes. | Used for training vision-based AI models like Life Whisperer and iDAScore. Requires significant data storage and processing power. |
| Ethylenediaminetetraacetic acid | Ethylenediaminetetraacetic acid, CAS:470462-56-7, MF:C₆¹³C₄H₁₆N₂O₈, MW:296.21 | Chemical Reagent | Bench Chemicals |
| Aldicarb-d3 Sulfone | Aldicarb-d3 Sulfone, CAS:1795135-15-7, MF:C₇H₁₁D₃N₂O₄S, MW:225.28 | Chemical Reagent | Bench Chemicals |
The accurate prediction of rare fertility outcomes, such as live birth following in vitro fertilization (IVF), represents a significant challenge in reproductive medicine. The development of robust machine learning (ML) models for this purpose is often hampered by high-dimensional datasets containing a multitude of clinical, demographic, and laboratory parameters. Feature selection is a critical preprocessing step that mitigates the "curse of dimensionality," enhances model performance, improves computational efficiency, and increases the interpretability of predictive models by identifying the most clinically relevant predictors [27] [28]. Within the specific context of rare fertility outcomes research, where datasets can be complex and imbalanced, the strategic implementation of feature selection is paramount for building reliable and generalizable models. This document provides detailed application notes and protocols for two prominent categories of feature selection strategies—filter methods and genetic algorithms (GAs)—framed within the scope of a broader thesis on ML prediction models for rare fertility outcomes.
Comparative Analysis of Feature Selection Strategies
The table below summarizes the core characteristics, performance, and applications of filter methods and genetic algorithms as identified in recent fertility research.
Table 1: Comparative analysis of feature selection strategies for fertility outcome prediction
| Strategy | Mechanism | Key Advantages | Limitations | Reported Performance in Fertility Research |
|---|---|---|---|---|
| Filter Methods (e.g., Chi-squared, PCA, VT) | Selects features based on statistical measures (e.g., correlation, variance) independent of the ML model [28]. | Computationally fast and efficient; Scalable to high-dimensional data; Less prone to overfitting [29]. | Ignores feature dependencies and model interaction; May select redundant features [27]. | PCA + LightGBM: 92.31% accuracy [30]; VT (Threshold=0.35): Used in hybrid pipeline [28]. |
| Genetic Algorithm (GA) | A wrapper method that uses evolutionary principles (selection, crossover, mutation) to find an optimal feature subset [27]. | Effective search of complex solution spaces; Captures feature interactions; Robust performance [27] [29]. | Computationally intensive; Requires a defined fitness function; Risk of overfitting without validation [29]. | GA + AdaBoost: 89.8% accuracy [27]; GA + Random Forest: 87.4% accuracy [27]. |
| Hybrid Approaches (Filter + GA) | A filter method performs initial feature reduction, followed by GA for refined optimization [29]. | Balances efficiency and performance; Reduces computational burden on GA; Leverages strengths of both methods. | Increased complexity in design and implementation. | Hybrid Filter-GA: Outperformed standalone methods on cancer classification [29]; HFS-based hybrid method: 79.5% accuracy, 0.72 AUC [28]. |
Experimental Protocols for Feature Selection in Fertility Research
Protocol 1: Genetic Algorithm-Based Feature Selection
This protocol outlines the steps for implementing a GA to identify pivotal features for predicting live birth outcomes in an IVF dataset, as demonstrated in recent studies [27].
1. Problem Definition & Initialization
- Objective: To select a subset of features from a pool of
Ntotal features (e.g., female age, AMH, endometrial thickness, sperm count) that maximizes the predictive accuracy for live birth. - Chromosome Encoding: Represent each potential solution (individual) as a binary string of length
N. A value of '1' indicates the feature is selected, and '0' indicates it is excluded. - Initial Population: Generate a population of
Prandom binary strings (e.g., P = 100-500 individuals).
2. Fitness Evaluation
- Fitness Function Definition: The performance of a feature subset is evaluated using a classifier (e.g., Random Forest, AdaBoost). The fitness score is the primary performance metric, typically the Area Under the ROC Curve (AUC) or Accuracy, estimated via cross-validation [27].
- Evaluation Process:
- For each individual in the population, subset the dataset to include only the features marked '1'.
- Train the chosen classifier on a training partition of the data.
- Calculate the fitness score (e.g., AUC) on a held-out validation set or via k-fold cross-validation.
- Assign this score as the individual's fitness.
3. Evolutionary Operations
- Selection: Employ a selection strategy (e.g., tournament selection, roulette wheel) to choose parent individuals for reproduction, favoring those with higher fitness scores.
- Crossover: Apply a crossover operator (e.g., single-point crossover) to pairs of parents to create offspring. This combines feature subsets from two parents.
- Mutation: Apply a mutation operator with a low probability (e.g., 0.01-0.05), which flips random bits in the offspring's chromosome. This introduces new features or removes existing ones, maintaining population diversity.
4. Termination and Output
- Stopping Criteria: Repeat steps 2 and 3 for a predefined number of generations (e.g., 100-500) or until fitness convergence is observed.
- Output: The algorithm returns the individual with the highest fitness score from the final generation, representing the optimal feature subset. Subsequent analysis, such as SHAP (SHapley Additive exPlanations), can be performed on a model trained with this subset to interpret feature importance [31].
Protocol 2: Hybrid Filter and Genetic Algorithm Workflow
This protocol leverages the speed of filter methods and the power of GAs, creating an efficient and high-performing pipeline suitable for high-dimensional fertility datasets [28] [29].
1. Preprocessing and Initial Filtering
- Data Cleaning: Handle missing values and normalize features as required.
- Apply Filter Method: Use a fast, univariate filter method (e.g., Chi-squared, Information Gain, Variance Threshold) to score and rank all
Nfeatures based on their statistical relationship with the outcome. - Feature Space Reduction: Select the top
Kfeatures from the ranked list (e.g., top 50-100 features, or features above a score threshold). This step drastically reduces the dimensionality of the dataset.
2. Genetic Algorithm Optimization on Reduced Set
- Chromosome Encoding: Create a binary chromosome representation of length
K, corresponding to the filtered feature set. - Execute GA: Run the Genetic Algorithm as described in Protocol 1, but using only the
Kfeatures from the filtering step. This significantly reduces the GA's search space and computational runtime. - Final Subset Selection: The GA outputs an optimal subset of the
Kfeatures, which is the final set of predictors for model building.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential computational tools and packages for implementing feature selection protocols
| Item Name | Function/Application | Implementation Example |
|---|---|---|
| Scikit-learn (Python) | Provides a comprehensive library for filter methods (e.g., SelectKBest, VarianceThreshold) and ML classifiers for fitness evaluation. |
from sklearn.feature_selection import SelectKBest, chi2 |
| DEAP (Python) | A robust evolutionary computation framework for customizing Genetic Algorithms, including selection, crossover, and mutation operators. | from deap import base, creator, algorithms, tools |
R caret Package |
A unified interface for building ML models in R, encompassing various filter methods and algorithms for model training and tuning. | library(caret); trainControl <- trainControl(method="cv", number=5) |
| Hesitant Fuzzy Sets (HFS) | A advanced mathematical framework for decision-making under uncertainty, used to rank and combine results from multiple feature selection methods in hybrid pipelines [28]. | Custom implementation as per [28] for scoring and aggregating feature subsets from filter and embedded methods. |
| SHAP (SHapley Additive exPlanations) | A game-theoretic method for explaining the output of any ML model, crucial for interpreting the clinical relevance of features selected by GA or hybrid models [31]. | import shap; explainer = shap.TreeExplainer(model) |
| Loteprednol Etabonate-d3 | Loteprednol Etabonate-d3, MF:C24H31ClO7, MW:470.0 g/mol | Chemical Reagent |
| Damnacanthal-d3 | Damnacanthal-d3, MF:C₁₆H₇D₃O₅, MW:285.27 | Chemical Reagent |
Workflow Visualization
The following diagram illustrates the logical sequence and integration of the two primary protocols detailed in this document.
Diagram 1: Integrated workflow for feature selection strategies
Accurately predicting blastocyst formation is a critical challenge in reproductive medicine, directly influencing decisions regarding extended embryo culture. This case study explores the application of the Light Gradient Boosting Machine (LightGBM) algorithm to predict blastocyst yield in In Vitro Fertilization (IVF) cycles. Within the broader context of machine learning for rare fertility outcomes, we demonstrate how LightGBM can be leveraged to forecast the quantitative number of blastocysts, moving beyond binary classification. The developed model achieved a high coefficient of determination (R²) of 0.673-0.676 and a Mean Absolute Error (MAE) of 0.793-0.809, outperforming traditional linear regression models (R²: 0.587, MAA: 0.943) [32]. Furthermore, when tasked with stratifying outcomes into three clinically relevant categories (0, 1-2, and ≥3 blastocysts), the model demonstrated robust accuracy (0.675-0.71) [32]. This protocol details the end-to-end workflow for constructing, validating, and interpreting a LightGBM-based predictive model for blastocyst yield, providing researchers and clinicians with a tool to potentially optimize embryo selection and culture strategies.
Infertility affects a significant portion of the global population, with assisted reproductive technologies (ART), particularly in vitro fertilization (IVF), serving as a primary treatment [30] [5]. A pivotal stage in IVF is extended embryo culture to the blastocyst stage (day 5-6), which allows for better selection of viable embryos and is associated with higher implantation rates [32]. However, not all embryos survive this extended culture, and a cycle yielding no blastocysts represents a significant clinical and emotional setback for patients.
The prediction of blastocyst formation has traditionally been challenging. While previous research often focused on predicting the binary outcome of obtaining at least one blastocyst, the quantitative prediction of blastocyst yield provides a more nuanced and clinically valuable metric [32]. This capability allows for personalized decision-making, setting realistic expectations, and potentially altering treatment strategies for predicted poor responders.
Machine learning (ML) models, known for identifying complex, non-linear patterns in high-dimensional data, are increasingly applied in reproductive medicine [30] [6] [33]. Among these, LightGBM has emerged as a powerful gradient-boosting framework. It offers high computational efficiency, lower memory usage, and often superior accuracy, making it suitable for clinical datasets [30] [32] [5]. This case study situates the use of LightGBM for blastocyst yield prediction within the broader research objective of developing robust ML models for rare and critical fertility outcomes.
Materials and Methods
Data Source and Study Population
A retrospective analysis is typically performed on data from a single or multi-center reproductive clinic.
- Data Origin: The dataset should comprise cycles from couples undergoing IVF or intracytoplasmic sperm injection (ICSI) treatment. For example, the model developed by Huo et al. was based on data from Nanfang Hospital [32].
- Inclusion/Exclusion Criteria: Standard criteria include women within a specific age range (e.g., 20-40 years) undergoing a fresh IVF/ICSI cycle with own gametes. Cycles with incomplete data, use of donor gametes, or preimplantation genetic testing are often excluded [32] [34].
- Ethical Approval: The study protocol must be approved by the relevant Institutional Review Board or Ethical Committee (e.g., approval number NFEC-2024-326 in the cited study [32]). Informed consent is often waived for retrospective studies by the ethics committee.
The Scientist's Toolkit: Predictor Variables and Outcome Definitions
The predictive model relies on specific clinical and embryological data points collected during the IVF cycle. The table below details the key features and the target outcome variable.
Table 1: Key Research Variables and Reagents
| Category | Item/Feature | Specification/Function |
|---|---|---|
| Patient Demographics | Maternal Age | Single most important prognostic factor for ovarian reserve and embryo quality [2] [6] [5]. |
| Body Mass Index (BMI) | Influences hormonal environment and treatment response [30] [35]. | |
| Duration of Infertility | Prognostic indicator; longer duration can be associated with poorer outcomes [30] [2]. | |
| Ovarian Stimulation | Gonadotropin (Gn) | Drugs (e.g., FSH) used for controlled ovarian hyperstimulation. Dosage and duration are recorded. |
| hCG Trigger | Injection used for final oocyte maturation prior to retrieval [30] [35]. | |
| Laboratory Reagents & Procedures | Fertilization Media | Culture medium supporting fertilization (IVF) and early embryo development. |
| Sequential Culture Media | Specialized media supporting embryo development to the blastocyst stage. | |
| Hyaluronidase | Enzyme used to remove cumulus cells from oocytes post-retrieval (for ICSI). | |
| Embryological Metrics | Number of Oocytes Retrieved | Raw count of oocytes collected, indicating ovarian response. |
| Number of 2PN Zygotes | Count of normally fertilized oocytes (with two pronuclei). | |
| Number of Extended Culture Embryos | Critical predictor: The number of embryos selected for extended culture beyond day 3 [32]. | |
| Mean Cell Number on Day 3 | Critical predictor: The average number of cells in the embryos on day 3, indicating cleavage speed [32]. | |
| Proportion of 8-cell Embryos | Critical predictor: The ratio of embryos that reached the ideal 8-cell stage on day 3 [32]. | |
| Outcome | Blastocyst Yield | The quantitative count of blastocysts formed by day 5/6, serving as the target variable for the model [32]. |
Experimental Workflow and Data Preprocessing
The following diagram outlines the end-to-end protocol for developing the LightGBM prediction model.
Protocol Steps:
- Data Preprocessing:
- Handling Missing Values: Impute missing values for corresponding attributes using statistical parameters like the median or mode [30] [35]. For mixed-type data, advanced non-parametric methods like
missForestcan be used [5]. - Outlier Detection: Identify and manage outliers using methods like Mahalanobis Distance to ensure model robustness [30] [35].
- Feature Scaling: Normalize continuous features to a common scale (e.g., [0,1]) using min-max scaling to ensure equal contribution during model fitting. The formula is:
D_Scaled = (D - D_min(axis=0)) / (D_max(axis=0) - D_min(axis=0))[30] [35].
- Handling Missing Values: Impute missing values for corresponding attributes using statistical parameters like the median or mode [30] [35]. For mixed-type data, advanced non-parametric methods like
- Data Partitioning: Randomly split the preprocessed dataset into a training set (e.g., 80%) for model development and a hold-out test set (e.g., 20%) for final evaluation [34].
- Model Training with Hyperparameter Tuning:
- Utilize the LightGBM algorithm, which is based on gradient boosting and uses a leaf-wise growth strategy with histogram optimization for efficiency [30] [35].
- Implement a 5-fold cross-validation on the training set to tune hyperparameters and prevent overfitting [30] [32].
- Key LightGBM hyperparameters to optimize via grid or random search include
max_depth,learning_rate,num_leaves,feature_fraction, andlambda_l1/lambda_l2regularization terms [5]. A regularization term in the loss function helps prevent overfitting:f_obj^k = Σ Loss(ŷ_i^k, y_i) + Σ ω(f_i)[30] [35].
Model Evaluation and Interpretation
- Performance Metrics: Evaluate the model on the held-out test set using regression and classification metrics.
- Model Interpretation:
- Analyze feature importance scores generated by LightGBM (e.g., "gain" which measures the total reduction in loss brought by a feature) to identify the most influential predictors [32].
- Use techniques like SHAP (SHapley Additive exPlanations) to understand the marginal contribution of each feature to individual predictions, enhancing model transparency [5].
Results and Performance
The application of the LightGBM model to blastocyst yield prediction demonstrates high predictive capability. The quantitative performance is summarized below.
Table 2: LightGBM Model Performance for Blastocyst Yield Prediction
| Model Task | Evaluation Metric | LightGBM Performance | Benchmark (Linear Regression) |
|---|---|---|---|
| Quantitative Prediction | R-squared (R²) | 0.673 - 0.676 | 0.587 [32] |
| Mean Absolute Error (MAE) | 0.793 - 0.809 | 0.943 [32] | |
| Categorical Stratification | Accuracy | 0.675 - 0.710 | - [32] |
| Kappa Coefficient | 0.365 - 0.500 | - [32] |
Key Findings:
- LightGBM significantly outperformed traditional linear regression in predicting the exact number of blastocysts, as evidenced by the higher R² and lower MAE [32].
- The model maintained robust performance when categorizing blastocyst yields, achieving fair-to-moderate agreement (as per Kappa interpretation) with the actual outcomes, which is notable for a multi-class problem [32].
- Feature importance analysis consistently identified three embryological factors as the top predictors: the number of extended culture embryos, the mean cell number on Day 3, and the proportion of 8-cell embryos [32]. This aligns with established embryological knowledge, where embryo quality and developmental competence on day 3 are strong indicators of blastulation potential.
Discussion and Clinical Implications
This case study confirms that LightGBM is a highly effective algorithm for constructing a blastocyst yield prediction model. Its performance advantages over traditional statistical methods underscore the value of machine learning in handling the complex, non-linear relationships inherent in embryological data.
The identified key predictors provide actionable insights for clinicians. The strong dependence on day-3 embryological morphology (cell number and 8-cell proportion) reinforces the importance of rigorous day-3 embryo evaluation. Integrating this model into clinical practice as a decision-support tool can help:
- Manage Patient Expectations: Provide a data-driven, personalized prognosis for blastocyst formation.
- Guide Culture Decisions: For patients predicted to have a very low chance of forming blastocysts, clinicians might consider a day-3 transfer to avoid the risk of no transfer.
- Optimize Resource Allocation: Laboratories can better plan their workload for extended culture.
This work fits into the broader thesis of machine learning for rare fertility outcomes by demonstrating a precise, quantitative approach. Future work should focus on external validation in diverse populations, prospective testing, and the integration of additional data types, such as time-lapse imaging and omics data, to further enhance predictive accuracy [33].
Appendix
LightGBM Algorithm Schematic
The following diagram illustrates the core mechanics of the LightGBM algorithm, which underpins the predictive model.
Code Snippet for Key Configuration
Below is an exemplary code block for initializing a LightGBM regressor with key parameters for this task.
Optimizing Predictive Performance: Addressing Data and Model Challenges
Navigating Small Datasets and Class Imbalance in Rare Outcomes
Machine learning (ML) prediction models hold significant promise for advancing research on rare fertility outcomes, such as specific causes of infertility or complications following assisted reproductive technology (ART). However, two interconnected methodological challenges frequently arise: small overall dataset sizes and severe class imbalance, where the outcome of interest is rare. This document provides application notes and detailed protocols to navigate these challenges, framed within the context of a broader thesis on ML for rare fertility outcomes. The guidance is tailored for researchers, scientists, and drug development professionals aiming to build robust and generalizable predictive models.
The following diagram outlines the core structured workflow for developing a prediction model for rare outcomes, integrating solutions for small datasets and class imbalance.
Application Notes & Protocols
Understanding the Challenges and Setting Requirements
The Small Dataset Problem in Fertility Research In digital mental health research, a study established that small datasets (N ≤ 300) significantly overestimate predictive power and that performance does not converge until dataset sizes reach N = 750–1500 [36]. Consequently, the authors proposed minimum dataset sizes of N = 500–1000 for model development [36]. This is particularly relevant to fertility research, where recruiting large cohorts for rare outcomes can be difficult. Using ML on small datasets is problematic because the power of ML in recognizing patterns is generally proportional to the size of the dataset; the smaller the dataset, the less powerful and accurate the algorithms become [37].
The Issue of Class Imbalance and Misleading Metrics For rare outcomes, the standard evaluation metric, the Area Under the Receiver Operating Characteristic Curve (AUC), can be highly misleading [38]. A model can achieve a high AUC while having an unacceptably low True Positive Rate (sensitivity), which is critical for identifying the rare events [38]. For instance, in predicting post-surgery mortality, models demonstrated moderate AUC but true positive rates were less than 7% [38]. Therefore, relying on a single metric, especially AUC, is "ill-advised" [38].
Minimum Sample Size and Event Prevalence Considerations While no single rule fits all scenarios, the concept of "events per variable" (EPV) is a useful guideline, though it may not fully account for the complexity of rare event data [39]. A rigorous study design must justify the sample size for both model training and evaluation [40]. Inadequate sample sizes negatively affect all aspects of model development, leading to overfitting, poor generalizability, and ultimately, potentially harmful consequences for clinical decision-making [40].
Table 1: Quantitative Insights from Literature on Dataset Challenges
| Challenge | Key Finding | Proposed Guideline | Source |
|---|---|---|---|
| Small Dataset Size | Performance overestimated for N ≤ 300; convergence at N = 750–1500. | Minimum dataset size of N = 500–1000. | [36] |
| Class Imbalance | High AUC can accompany very low True Positive Rates (<7%). | Avoid relying solely on AUC; use multiple metrics. | [38] |
| Model Overfitting | Sophisticated models (e.g., RF, NN) overfit most on small datasets. | Use simpler models (e.g., Naive Bayes) or strong regularization for small N. | [36] |
| Feature-to-Sample Ratio | Models with many features require larger samples to avoid overfitting. | Implement aggressive feature selection and dimensionality reduction. | [36] [37] |
Protocol 1: Data Preparation and Augmentation
Objective: To maximize the informative value of a limited dataset and address class imbalance before model training.
Workflow:
Data Encoding and Cleaning:
- Encode categorical variables using appropriate methods (e.g., one-hot encoding for nominal variables).
- Handle missing data. For small datasets, simple imputation (e.g., median/mode) is often preferable to complex models. Consider multiple imputation if the dataset is sufficiently large.
- Scale numerical features to a standard range (e.g., [0, 1] or Z-scores) to ensure model stability.
Feature Selection and Dimensionality Reduction: This is critical when the number of features (p) is large compared to the number of samples (N).
- Filter Methods: Select features based on univariate statistical tests (e.g., Chi-squared, mutual information) against the target variable.
- Wrapper Methods: Use recursive feature elimination (RFE) with a conservative classifier to identify the most predictive feature subset.
- Embedded Methods: Employ models with built-in feature selection, such as Lasso regression, which shrinks coefficients of non-informative features to zero [39].
- Domain Knowledge: Always incorporate expert knowledge to retain clinically plausible predictors.
Addressing Class Imbalance in the Data:
- Synthetic Minority Over-sampling Technique (SMOTE): Generate synthetic samples for the rare outcome class by interpolating between existing instances [37]. This is superior to random over-sampling, which leads to overfitting.
- Informed Under-sampling: Carefully under-sample the majority class, potentially using ensemble methods that create multiple balanced sub-samples.
Protocol 2: Model Selection, Training, and Interpretation
Objective: To select, train, and interpret models that are robust to small sample sizes and class imbalance.
Workflow:
Algorithm Selection: Prioritize algorithms known to perform well with limited data or inherent regularization.
- Logistic Regression with Penalization: Firth's bias-reduced logistic regression or Lasso (L1) / Ridge (L2) regression are excellent starting points, as they reduce model complexity and combat overfitting [38] [39].
- Tree-Based Ensembles: Random Forest and Gradient Boosting Machines (e.g., XGBoost) often achieve high performance. They are less prone to overfitting than single trees and can handle complex interactions [41]. Ensure trees are pruned and depth is limited.
- Support Vector Machines (SVM): Can be effective, particularly with linear kernels, but require careful hyperparameter tuning [36].
- Naive Bayes: A strong baseline for small datasets, as it is simple and less prone to overfitting [36].
Model Training and Validation:
- Data Splitting: Use a stratified train-validation-test split (e.g., 70-15-15) to preserve the proportion of the rare outcome in each set. For very small datasets, a single hold-out test set may not be feasible.
- Nested Cross-Validation: Implement nested cross-validation for hyperparameter tuning and performance estimation. The outer loop estimates generalizability, while the inner loop performs model selection. This prevents optimistically biased results [42].
- Hyperparameter Tuning: Use Bayesian optimization or grid search within the inner CV loop. Focus on parameters that control model complexity (e.g., regularization strength, tree depth).
Model Interpretation with Explainable AI (XAI):
- SHapley Additive exPlanations (SHAP): Employ SHAP analysis to interpret the model's output and understand the contribution of each feature to individual predictions [41]. This addresses the "black-box" nature of complex models and is critical for building clinical trust.
- Application Example: A study on fertility preferences in Somalia used Random Forest and SHAP to identify that the woman's age group, region, and number of recent births were the top predictors, providing actionable insights beyond mere prediction [41].
Table 2: Summary of Key Algorithms for Rare Outcomes
| Algorithm | Best for Small Data? | Handles Imbalance? | Key Strengths | Considerations |
|---|---|---|---|---|
| Penalized Logistic Regression | Yes [39] | With careful evaluation [38] | High interpretability, inherent regularization, reduces overfitting. | Assumes linearity; may miss complex interactions. |
| Random Forest | With feature selection [41] | Yes (with tuning) [41] | Handles non-linear relationships; robust to outliers. | Can overfit on very small datasets without tuning [36]. |
| Naive Bayes | Yes [36] | Yes | Computationally efficient; performs well on very small datasets. | Makes strong feature independence assumptions. |
| Support Vector Machine (SVM) | Moderate [36] | With careful evaluation | Effective in high-dimensional spaces. | Performance sensitive to hyperparameters; less interpretable. |
Protocol 3: Comprehensive Model Evaluation
Objective: To assess model performance using a suite of metrics and visualizations that are robust to class imbalance.
Workflow:
- Move Beyond AUC: Do not rely on the Area Under the ROC Curve (AUC) as the primary metric. It can be dangerously optimistic for rare events [38].
- Adopt a Multi-Metric Approach: Calculate and report the following metrics simultaneously on the hold-out test set or via cross-validation:
- Precision (Positive Predictive Value): Of all predicted events, how many are actual events? High precision means fewer false alarms.
- Recall (Sensitivity/True Positive Rate): Of all actual events, how many did the model find? High recall means the model misses few events.
- F1-Score: The harmonic mean of Precision and Recall. Provides a single score that balances both concerns.
- Specificity (True Negative Rate): Of all non-events, how many were correctly identified?
- Balanced Accuracy: The average of Recall and Specificity. More informative than standard accuracy for imbalanced data.
- Use Complementary Curves:
- Precision-Recall (PR) Curve: The PR curve is more informative than the ROC curve when the positive class is rare. The Area Under the PR Curve (AUPRC) should be the primary summary metric for model comparison [38].
- Calibration Plots: Assess how well the predicted probabilities align with the observed frequencies. A model can be discriminative but poorly calibrated, which is risky for clinical decision-making [38].
- Validate on External Data: Whenever possible, test the final model on a completely independent dataset from a different source or time period to assess true generalizability [40].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools and Their Functions
| Tool / "Reagent" | Category | Function in the Workflow | Example Use-Case |
|---|---|---|---|
| SMOTE | Data Augmentation | Generates synthetic samples for the minority class to balance training data. | Correcting a 2% event rate to 20-30% for model training. |
| Lasso (L1) Regression | Feature Selection / Model | Performs variable selection and regularization by shrinking coefficients to zero. | Reducing a set of 150 patient characteristics to 15 key predictors. |
| SHAP | Model Interpretation | Explains the output of any ML model by quantifying each feature's contribution. | Identifying that "female age" and "specific infertility diagnosis" are the primary drivers of a prediction. |
| Nested Cross-Validation | Validation Framework | Provides an nearly unbiased estimate of a model's true performance on unseen data. | Reliably evaluating a model when only 800 total samples are available. |
| Precision-Recall Curve | Evaluation Metric | Visualizes the trade-off between precision and recall for different probability thresholds. | Determining the optimal threshold for a model predicting rare IVF complications. |
In the field of machine learning for rare fertility outcomes research, such as predicting live birth after assisted reproductive technologies (ART) or adverse birth outcomes, developing high-performance predictive models is paramount [9] [43]. The ability of a model to identify subtle patterns in complex, often imbalanced datasets directly impacts its clinical utility. Hyperparameter tuning is a critical step in this process, as it transforms a model with default settings into an optimized predictor capable of supporting clinical decisions [44] [45]. This document provides detailed application notes and experimental protocols for two fundamental hyperparameter tuning strategies—Grid Search and Bayesian Optimization—framed within the specific context of fertility research.
Theoretical Foundations
Hyperparameters vs. Model Parameters
A clear distinction exists between model parameters and hyperparameters. Model parameters are internal variables that the learning algorithm learns from the training data, such as the weights in a neural network or the split points in a decision tree [45]. In contrast, hyperparameters are external configuration variables set by the researcher before the training process begins. They control the learning process itself, influencing how the model parameters are updated [44] [46]. Examples include the learning rate for gradient descent, the number of trees in a Random Forest, or the kernel type in a Support Vector Machine [44] [47].
The Need for Hyperparameter Tuning in Fertility Research
Hyperparameter tuning is the systematic process of searching for the optimal combination of hyperparameters that yields the best model performance as measured on a validation set [44] [46]. In fertility research, where datasets can be high-dimensional and outcomes are rare, proper tuning is not a luxury but a necessity [9]. A model with poorly chosen hyperparameters may suffer from underfitting (failing to capture relevant patterns in the data) or overfitting (modeling noise in the training data, which harms generalization to new patients) [44]. Given that studies in this domain often employ ensemble models like Random Forest or complex neural networks, the hyperparameter search space can be large [9]. Efficient and effective tuning strategies are therefore essential to build models that are both accurate and reliable for clinical application.
Grid Search: Exhaustive Parameter Sweep
Principle and Workflow
Grid Search is an exhaustive search algorithm that is one of the most traditional and straightforward methods for hyperparameter optimization [46]. The core principle involves defining a discrete grid of hyperparameter values, where each point on the grid represents a unique combination of hyperparameters [44]. The algorithm then trains and evaluates a model for every single combination in this grid, typically using cross-validation to assess performance. The combination that maximizes the average validation score is selected as the optimal set of hyperparameters [44] [47].
The following diagram illustrates the standard Grid Search workflow.
Experimental Protocol
Objective: To identify the optimal hyperparameters for a Random Forest classifier predicting live birth outcomes following fresh embryo transfer.
Dataset: A pre-processed dataset of ART cycles with 55 pre-pregnancy features, including female age, embryo grades, and endometrial thickness [9]. The dataset should be split into training (e.g., 70%) and hold-out test (e.g., 30%) sets prior to tuning.
Model: Random Forest Classifier.
Software & Libraries: Python with scikit-learn.
Procedure:
Define the Hyperparameter Grid: Specify the grid of hyperparameters and their values to be searched. The values should be chosen based on literature, domain expertise, and computational constraints.
Initialize GridSearchCV: Configure the grid search object. Use a robust scoring metric relevant to the problem (e.g.,
roc_aucfor imbalanced classification of rare outcomes) and specify the number of cross-validation folds (cv).Execute the Search: Fit the
GridSearchCVobject to the training data. This will trigger the exhaustive search described in the workflow.Extract Results: After completion, the best hyperparameters and the corresponding best score can be retrieved.
Final Evaluation: Evaluate the performance of the best-estimated model (
best_estimator) on the held-out test set to obtain an unbiased estimate of its generalization performance.
Performance and Considerations
Table 1: Summary of Grid Search performance and characteristics.
| Aspect | Description | Implication for Fertility Research |
|---|---|---|
| Search Strategy | Exhaustive, brute-force [44] | Guarantees finding the best point within the defined grid. |
| Computational Cost | High; grows exponentially with added parameters [44] [46] | Can be prohibitive for large datasets or complex models, slowing down research iteration. |
| Parallelization | Embarrassingly parallel; each evaluation is independent [46] | Can leverage high-performance computing clusters to reduce wall-clock time. |
| Best For | Small, discrete hyperparameter spaces where an exhaustive search is feasible. | Ideal for initial exploration or when tuning a limited number of hyperparameters. |
Bayesian Optimization: Probabilistic Model-Based Search
Principle and Workflow
Bayesian Optimization is a powerful, sequential model-based global optimization strategy designed for expensive black-box functions [48] [46]. It addresses the key limitation of Grid Search by using past evaluation results to build a probabilistic surrogate model (e.g., Gaussian Process, Tree-structured Parzen Estimator) of the objective function (the model's validation score) [48]. An acquisition function (e.g., Expected Improvement), which balances exploration (sampling points with high uncertainty) and exploitation (sampling points predicted to have a high value), guides the selection of the next hyperparameter combination to evaluate [48] [49]. This informed selection process allows Bayesian Optimization to find high-performing hyperparameters in significantly fewer iterations compared to Grid or Random Search [48].
The sequential model-based nature of Bayesian Optimization is outlined below.
Experimental Protocol
Objective: To efficiently tune a complex machine learning model (e.g., XGBoost) for predicting adverse birth outcomes in Sub-Saharan Africa using Bayesian Optimization.
Dataset: A large-scale Demographic Health Survey (DHS) dataset with 28 features, where adverse birth outcomes are the target variable [43].
Model: XGBoost Classifier.
Software & Libraries: Python with scikit-learn and a Bayesian optimization library such as scikit-optimize or Hyperopt.
Procedure:
Define the Search Space: Specify the hyperparameters and their probability distributions. This allows the algorithm to sample values continuously and intelligently.
Initialize the Bayesian Optimizer: Configure the optimizer with the search space, base estimator, and the number of iterations.
Execute the Optimization: Fit the optimizer to the training data. The algorithm will sequentially choose the most promising hyperparameters to evaluate.
Extract Results: Access the best hyperparameters and score, just as with Grid Search.
Performance and Considerations
Table 2: Summary of Bayesian Optimization performance and characteristics.
| Aspect | Description | Implication for Fertility Research |
|---|---|---|
| Search Strategy | Sequential, model-based, informed by past evaluations [48] | Highly sample-efficient; ideal when model training is computationally expensive. |
| Computational Cost | Lower number of function evaluations required to find good solutions [48] | Faster turnaround in experimental cycles, enabling testing of more complex models. |
| Parallelization | Inherently sequential; next point depends on previous results. | Less parallelizable per iteration, but overall time to solution is often lower. |
| Best For | Medium to large search spaces, continuous parameters, and when each model evaluation is costly [48] [50]. | Excellent for fine-tuning models like XGBoost or neural networks on large patient datasets. |
Comparative Analysis and Application to Fertility Research
Strategic Comparison
Table 3: Direct comparison of Grid Search and Bayesian Optimization.
| Feature | Grid Search | Bayesian Optimization |
|---|---|---|
| Core Principle | Exhaustive search over a defined grid [44] | Probabilistic model guiding sequential search [48] |
| Efficiency | Low; scales poorly with dimensionality [46] | High; designed for expensive black-box functions [48] |
| Parameter Types | Best for discrete, categorical parameters. | Excels with continuous and mixed parameter spaces. |
| Optimal Solution | Best point on the pre-defined grid. | Can find a high-quality solution not necessarily on a grid. |
| Prior Knowledge | Requires manual specification of grid bounds and values. | Can incorporate prior distributions over parameters. |
| Use Case | Small, well-understood hyperparameter spaces (e.g., 2-4 parameters). | Larger, more complex spaces or when computational budget is limited. |
Application in Fertility Research: A Case Study
A recent study aiming to predict live birth outcomes from fresh embryo transfer utilized six different machine learning models, including Random Forest (RF), XGBoost, and neural networks [9]. The researchers employed Grid Search with 5-fold cross-validation to optimize the hyperparameters of these models, using the Area Under the Curve (AUC) as the evaluation metric [9]. This approach led to the development of a Random Forest model with an AUC exceeding 0.8, which was identified as the best predictor. The study highlights a practical scenario where Grid Search was a feasible and effective choice, likely due to the manageable number of models and hyperparameters being tuned. For even more complex tuning tasks, such as optimizing a deep neural network or performing large-scale feature selection, Bayesian Optimization could offer a more efficient alternative [48] [50].
The Scientist's Toolkit
Table 4: Essential research reagents and computational tools for hyperparameter tuning in fertility prediction research.
| Research Reagent / Tool | Function / Description | Application Example |
|---|---|---|
| scikit-learn | A core Python library for machine learning, providing implementations of models, Grid Search, Random Search, and data preprocessing utilities [47]. | Implementing Random Forest classifier and GridSearchCV. |
| scikit-optimize | A Python library that provides a BayesSearchCV implementation for performing Bayesian optimization with scikit-learn compatible estimators [49]. |
Efficiently searching a continuous parameter space for an XGBoost model. |
| Hyperopt / Optuna | Advanced libraries for hyperparameter optimization that offer more flexibility and algorithms (e.g., TPE) than scikit-optimize [48] [50]. | Complex, large-scale tuning tasks requiring distributed computing and advanced pruning. |
| XGBoost / Random Forest | Powerful ensemble learning algorithms frequently used in medical prediction tasks due to their high performance and interpretability features [9] [43]. | The base predictive model for classifying live birth or adverse birth outcomes. |
| Pandas / NumPy | Foundational Python libraries for data manipulation and numerical computation. | Loading, cleaning, and preprocessing clinical dataset features before model training. |
| Matplotlib / Seaborn | Libraries for creating static, animated, and interactive visualizations in Python. | Plotting validation curves, learning curves, and results comparison plots. |
Feature Engineering for Enhanced Predictive Power
Predicting rare fertility outcomes, such as live birth following specific assisted reproductive technology (ART) procedures, presents a significant challenge in reproductive medicine. Machine learning (ML) offers powerful tools to address this challenge, yet the performance and clinical applicability of these models depend critically on the features used to train them. Feature engineering—the process of creating, selecting, and transforming variables—serves as the foundational step that directly enhances a model's predictive power. This protocol details advanced feature engineering methodologies tailored for constructing robust ML models aimed at predicting rare fertility outcomes, providing researchers and drug development professionals with a structured framework to improve model accuracy, interpretability, and clinical relevance.
Current Landscape of ML in Fertility Prediction
Recent systematic reviews and primary research demonstrate a concerted effort to apply ML models in fertility outcome prediction. The table below summarizes quantitative performance data from recent studies, highlighting the models used and the key features that contributed to their predictive power.
Table 1: Performance of Machine Learning Models in Fertility Outcome Prediction
| Study (Year) | Dataset Size | Best Performing Model(s) | Key Performance Metrics | Top-Ranked Predictive Features |
|---|---|---|---|---|
| Sadegh-Zadeh et al. (2024) [33] | Not Specified | Logit Boost | Accuracy: 96.35% | Patient demographics, infertility factors, treatment protocols |
| Shanghai First Maternity (2025) [9] | 11,728 records | Random Forest (RF) | AUC > 0.8 | Female age, embryo grades, usable embryo count, endometrial thickness |
| Mehrjerd et al. (2022) [51] | 1,931 records | Random Forest (RF) | Sensitivity: 0.76, PPV: 0.80 | Female age, FSH levels, endometrial thickness, infertility duration |
| Nigerian DHS (2025) [19] | 37,581 women | Random Forest (RF) | Accuracy: 92%, AUC: 0.92 | Number of living children, woman's age, ideal family size |
A 2025 systematic literature review confirmed that female age was the most universally utilized feature across all identified studies predicting Assisted Reproductive Technology (ART) success [6]. Supervised learning approaches dominated the field (96.3% of studies), with Support Vector Machines (SVM) being the most frequently applied technique (44.44%) [6]. Evaluation metrics are crucial for comparing models; the Area Under the ROC Curve (AUC) was the most common performance indicator (74.07%), followed by accuracy (55.55%), and sensitivity (40.74%) [6] [51].
Experimental Protocols for Feature Engineering
This section provides detailed, step-by-step methodologies for the key experiments and processes cited in the literature, focusing on data preprocessing, feature generation, and selection.
Protocol 1: Data Preprocessing and Imputation for Clinical Fertility Data
Objective: To clean and prepare raw, heterogeneous clinical fertility data for robust feature engineering and model training.
Materials:
- Hardware: Standard computational workstation.
- Software: Python (v3.8+) with libraries (pandas, scikit-learn, missForest in R) or R (v4.4+) with
caretandmissForestpackages. - Data: De-identified patient records from ART cycles, typically including demographic, hormonal, embryological, and treatment outcome data.
Procedure:
- Data Anonymization and Integration: Merge data from disparate hospital sources (e.g., clinical records, lab results) using a unique patient identifier. Ensure all protected health information (PHI) is removed in compliance with ethical approvals [9].
- Handling Missing Data:
- Assess the percentage and pattern of missingness for each variable.
- For datasets with mixed data types (continuous and categorical), employ a non-parametric imputation method like
missForest[9] [51]. This method uses a Random Forest model to predict missing values and is efficient for complex clinical datasets. - Alternative for smaller datasets: Use Multilevel Perceptron (MLP) for imputation, which can provide better results than traditional mean/mode imputation [51].
- Class Imbalance Adjustment:
- For rare outcomes (e.g., live birth rates of ~34%), apply the Synthetic Minority Oversampling Technique (SMOTE) [19].
- Generate synthetic samples for the minority class to balance the class distribution before proceeding to feature engineering, thereby preventing model bias toward the majority class.
Protocol 2: Comprehensive Feature Selection Framework
Objective: To identify the most informative and non-redundant feature subset for predicting the target fertility outcome.
Materials:
- Preprocessed dataset from Protocol 1.
- Software: Python with
scikit-learnor R withcaret.
Procedure:
- Initial Filtering based on Clinical and Statistical Significance:
- Conduct univariate analysis (e.g., Chi-square test for categorical, Kruskal-Wallis test for continuous variables) to assess the association of each feature with the outcome [9] [51].
- Retain features with a p-value < 0.05 or those ranked in the top-20 by a preliminary Random Forest feature importance run [9].
- Clinical Validation: Have domain experts (e.g., reproductive endocrinologists) review the statistically significant features to eliminate biologically irrelevant variables and reinstate clinically critical features that may not have met the strict statistical threshold [9].
- Recursive Feature Elimination (RFE):
- Implement RFE using a tree-based estimator (e.g., Random Forest or XGBoost).
- RFE iteratively removes the least important feature(s), rebuilding the model each time until the optimal number of features is reached. This refines the feature set based on model performance [19].
- Multi-collinearity Check:
- Calculate a correlation matrix for the remaining continuous features.
- Use a correlation heatmap to visually identify and eliminate one feature from any pair with a correlation coefficient > |0.8| to ensure feature independence and model stability [19].
Protocol 3: Advanced Feature Engineering for Sperm Morphology Images
Objective: To create discriminative features from sperm microscopy images for deep learning-based morphology classification, a key factor in male fertility assessment.
Materials:
- Datasets: Publicly available sperm image datasets (e.g., SMIDS, HuSHeM).
- Models: Pre-trained CNN architectures (ResNet50, Xception) enhanced with Convolutional Block Attention Module (CBAM).
- Software: Python with PyTorch/TensorFlow, and
scikit-learn.
Procedure:
- Deep Feature Extraction:
- Use a CBAM-enhanced ResNet50 model as a feature extractor. The CBAM attention mechanism forces the model to focus on morphologically critical regions (head shape, acrosome, tail) [52].
- Extract high-dimensional feature vectors from global pooling layers (Global Average Pooling - GAP, Global Max Pooling - GMP) [52].
- Deep Feature Engineering (DFE) Pipeline:
- Apply feature selection and dimensionality reduction to the extracted deep features.
- Utilize Principal Component Analysis (PCA) to reduce noise and dimensionality.
- Alternative methods: Employ Chi-square tests, Random Forest importance, or variance thresholding on the deep features [52].
- Classification with Shallow Models:
- Train a Support Vector Machine (SVM) with RBF or linear kernel on the PCA-transformed feature set. This hybrid approach (CNN + SVM) has been shown to achieve superior accuracy (e.g., 96.08%) compared to end-to-end CNN classification [52].
Signaling Pathways and Workflows
The following diagram illustrates the logical workflow for feature engineering and model development in rare fertility outcome prediction, integrating the protocols described above.
Feature Engineering and Model Development Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for ML-based Fertility Research
| Item/Tool Name | Function/Application | Specification Notes |
|---|---|---|
| Clinical Data | Foundation for feature engineering on patient profiles. | Must include female age, endometrial thickness, embryo grades, infertility duration, FSH/AMH levels [6] [9] [51]. |
| SMIDS/HuSHeM Datasets | Benchmark image datasets for sperm morphology analysis. | Publicly available for academic use; enable development of deep feature pipelines [52]. |
| CBAM-enhanced ResNet50 | Deep learning backbone for extracting features from medical images. | Attention mechanism improves focus on morphologically critical sperm structures [52]. |
| missForest (R package) | Advanced data imputation for mixed-type clinical data. | Non-parametric method preferred over mean/mode for complex fertility datasets [9]. |
| SMOTE | Algorithmic solution to class imbalance in rare outcomes. | Generates synthetic samples of the minority class (e.g., live birth) [19]. |
| Recursive Feature Elimination (RFE) | Automated feature selection within model training. | Iteratively removes weakest features to optimize feature set size [19]. |
| FertilitY Predictor Web Tool | Example of a deployed ML model for specific conditions. | Predicts ART success in men with Y chromosome microdeletions [53]. |
The application of machine learning (ML) in reproductive medicine, particularly for predicting rare fertility outcomes, represents a frontier in computational biology and personalized healthcare. The core challenge in building effective predictive models lies not only in the choice of algorithm but also in the selection of the optimization process that guides the model's learning. Optimization algorithms are the engines of machine learning; they are the computational procedures that adjust a model's parameters to minimize the discrepancy between its predictions and the observed data, a quantity known as the loss function. The journey of these algorithms began with foundational methods like Gradient Descent and has evolved into sophisticated adaptive techniques such as Adam (Adaptive Moment Estimation). The performance of these optimizers is paramount when dealing with complex and often imbalanced datasets common in medical research, such as those aimed at predicting rare in vitro fertilization (IVF) outcomes or infertility risk. Selecting the appropriate optimizer can significantly influence the speed of training, the final model accuracy, and the reliability of the clinical insights derived, making a deep understanding of their mechanics and applications essential for researchers and drug development professionals in the field of reproductive health.
Theoretical Foundation of Key Optimizers
The development of optimization algorithms in machine learning follows a clear trajectory from simple, intuitive methods to complex, adaptive systems. Each algorithm was developed to address specific limitations of its predecessors, leading to the diverse toolkit available to researchers today.
Gradient Descent (GD) is the most fundamental optimization algorithm. It operates by iteratively adjusting model parameters in the direction of the steepest descent of the loss function, as determined by the negative gradient. The magnitude of each update is controlled by a single hyperparameter, the learning rate (η). A small learning rate leads to slow but stable convergence, whereas a large learning rate can cause the algorithm to overshoot the minimum, potentially leading to divergence. The primary drawback of vanilla Gradient Descent is its computational expense for large datasets, as it requires a complete pass through the entire dataset to compute a single parameter update [54].
Stochastic Gradient Descent (SGD) addresses this inefficiency by calculating the gradient and updating the parameters using a single, randomly chosen data point (or a small mini-batch) at each iteration. This introduces noise into the optimization process, which can help the algorithm escape shallow local minima. However, this same noise causes the loss function to fluctuate significantly, making convergence behavior difficult to monitor and interpret. SGD with Momentum enhances SGD by incorporating a moving average of past gradients. This adds inertia to the optimization path, helping to accelerate convergence in relevant directions and dampen oscillations, especially in ravines surrounding the optimum. This is governed by a momentum factor (γ), which determines the contribution of previous gradients [54].
Adaptive learning rate algorithms marked a significant evolution by assigning a unique, dynamically adjusted learning rate to each model parameter. Adagrad (Adaptive Gradient) performs larger updates for infrequent parameters and smaller updates for frequent ones by dividing the learning rate by the square root of the sum of all historical squared gradients. While effective for sparse data, a major flaw of Adagrad is that this cumulative sum causes the effective learning rate to monotonically decrease, often becoming infinitesimally small and halting learning prematurely. RMSprop (Root Mean Square Propagation) resolves this by using an exponentially decaying average of squared gradients, preventing the aggressive decay in learning rate and allowing the optimization process to continue effectively over many iterations [54].
Adam (Adaptive Moment Estimation) combines the core ideas of momentum and RMSprop. It maintains two moving averages for each parameter: the first moment (the mean of the gradients, providing momentum) and the second moment (the uncentered variance of the gradients, providing adaptive scaling). These moments are bias-corrected to account for their initialization at zero, leading to more stable estimates. This combination makes Adam robust to the choice of hyperparameters and has contributed to its status as a default optimizer for a wide range of deep learning applications. It is particularly well-suited for problems with large datasets and/or parameters, and for non-stationary objectives common in deep neural networks [54]. Recent theoretical analyses have revealed that Adam does not typically converge to a critical point of the objective function in the classical sense but instead converges to a solution of a related "Adam vector field," providing new insights into its convergence properties [55].
The table below summarizes the key characteristics, advantages, and disadvantages of these primary optimization algorithms.
Table 1: Comparative Analysis of Fundamental Optimization Algorithms
| Algorithm | Key Mechanism | Hyperparameters | Pros | Cons |
|---|---|---|---|---|
| Gradient Descent (GD) | Updates parameters using gradient of the entire dataset. | Learning Rate (η) | Simple, theoretically sound. | Slow for large datasets; prone to local minima. |
| Stochastic GD (SGD) | Updates parameters using gradient of a single data point or mini-batch. | Learning Rate (η) | Faster updates; can escape local minima. | Noisy convergence path; requires careful learning rate scheduling. |
| SGD with Momentum | SGD with a velocity term from exponential averaging of gradients. | Learning Rate (η), Momentum (γ) | Faster convergence; reduces oscillation. | Introduces an additional hyperparameter to tune. |
| Adagrad | Adapts learning rate per parameter based on historical gradients. | Learning Rate (η) | Suitable for sparse data; automatic learning rate tuning. | Learning rate can vanish over long training periods. |
| RMSprop | Adapts learning rate using a moving average of squared gradients. | Learning Rate (η), Decay Rate (γ) | Solves Adagrad's diminishing learning rate. | Hyperparameter tuning can be less intuitive. |
| Adam | Combines momentum and adaptive learning rates via 1st and 2nd moment estimates. | Learning Rate (η), βâ‚, β₂ | Fast convergence; handles noisy gradients; less sensitive to initial η. | Can sometimes converge to suboptimal solutions; memory intensive. |
Optimizer Selection for Rare Outcomes in Fertility Research
The prediction of rare fertility outcomes, such as blastocyst formation failure or specific infertility diagnoses, presents a classic case of class imbalance. In such datasets, the event of interest (the positive class) is vastly outnumbered by the non-event (the negative class). This imbalance poses significant challenges for model training and evaluation, which directly influences the choice and configuration of an optimization algorithm.
Standard metrics like accuracy or Area Under the Receiver Operating Characteristic Curve (AUC) can be highly misleading for rare outcomes. A model that simply predicts "no event" for every patient can achieve high accuracy but is clinically useless. Therefore, model evaluation must prioritize metrics such as Positive Predictive Value (PPV/Precision), True Positive Rate (TPR/Recall), and F1-score, which are more sensitive to the correct identification of the rare class [38]. This focus on the minority class affects the optimizer's task; the loss landscape becomes more complex, and the signal from the rare class can be easily overwhelmed.
When facing imbalanced data, the choice of optimizer can influence training stability and final model performance. Adaptive methods like Adam are often beneficial in the early stages of research and prototyping due to their rapid convergence and reduced need for extensive hyperparameter tuning. This allows researchers to quickly iterate on model architectures and feature sets. However, it has been observed that well-tuned SGD with Momentum can, in some cases, achieve comparable or even superior final performance, often with better generalization, though at the cost of more intensive hyperparameter search [54].
Furthermore, the loss function itself may need modification, such as using weighted cross-entropy or focal loss, which increases the penalty for misclassifying the rare class. The optimizer must then effectively navigate this modified loss landscape. The combination of a tailored loss function for imbalance and a robust adaptive optimizer like Adam or RMSprop is a common and effective strategy in fertility informatics for ensuring the model pays adequate attention to the rare outcomes of clinical interest [38].
Application Notes & Experimental Protocols
Protocol 1: Predicting Blastocyst Yield in IVF Cycles
1. Background & Objective: Quantitatively predicting the number of blastocysts (blastocyst yield) resulting from an IVF cycle is crucial for clinical decision-making regarding extended embryo culture. This protocol outlines the development of a machine learning model, specifically using the LightGBM algorithm, for this prediction task, enabling personalized embryo culture strategies [56].
2. Research Reagent & Data Solutions:
Table 2: Essential Components for Blastocyst Yield Prediction Model
| Component | Function/Description | Example/Format |
|---|---|---|
| Clinical Dataset | Cycle-level data from IVF/ICSI treatments. | Structured data from >9,000 cycles, including patient demographics, embryology lab data. |
| Feature: Extended Culture Embryos | The number of embryos selected for extended culture to day 5/6. | Integer count; identified as the most critical predictor [56]. |
| Feature: Day 3 Morphology | Metrics of embryo development on day 3. | Includes mean cell number, proportion of 8-cell embryos, symmetry, and fragmentation [56]. |
| LightGBM Framework | A high-performance gradient boosting framework that uses tree-based algorithms. | Preferred for its accuracy, efficiency with fewer features, and superior interpretability [56]. |
| Model Interpretation Tool (SHAP/LIME) | Post-hoc analysis to explain the output of the machine learning model. | Used to generate Individual Conditional Expectation (ICE) and partial dependence plots [56]. |
3. Experimental Workflow:
4. Step-wise Methodology:
- Step 1 - Data Curation: Assemble a comprehensive dataset of IVF cycles, including key variables such as female age, number of oocytes, number of 2PN embryos, number of embryos selected for extended culture, and detailed Day 2 and Day 3 embryo morphology parameters (cell number, symmetry, fragmentation) [56].
- Step 2 - Preprocessing & Splitting: Clean the data to handle missing values. Randomly split the entire dataset into a training set (e.g., 70%) for model development and a hold-out test set (e.g., 30%) for final validation [56].
- Step 3 - Feature Selection: Employ Recursive Feature Elimination (RFE) to identify the optimal subset of predictors. This process iteratively removes the least important features until model performance begins to degrade, ensuring a parsimonious and effective model [56].
- Step 4 - Model Training & Tuning: Train multiple machine learning models, including LightGBM, XGBoost, and Support Vector Machines (SVM). Use the training set and k-fold cross-validation to tune the hyperparameters of each model. Use an optimizer like Adam if the model is a neural network; otherwise, rely on the model's intrinsic boosting procedures (for LightGBM/XGBoost) or dedicated solvers (for SVM) [56].
- Step 5 - Model Evaluation: Evaluate the final model on the untouched test set. Use quantitative metrics like R-squared (R²) and Mean Absolute Error (MAE) for the regression task. For clinical utility, stratify predictions into categories (e.g., 0, 1-2, ≥3 blastocysts) and report multi-class accuracy and Kappa coefficient to assess agreement beyond chance [56].
- Step 6 - Interpretation & Deployment: Analyze the trained model using feature importance scores and Individual Conditional Expectation (ICE) plots. This reveals how key predictors, such as the number of extended culture embryos and Day 3 embryo quality, influence the predicted blastocyst yield, providing clinicians with actionable insights [56].
Protocol 2: Population-Level Infertility Risk Stratification
1. Background & Objective: To monitor public health trends and enable early intervention, this protocol describes the use of machine learning for predicting self-reported infertility risk in women using nationally representative survey data like NHANES, relying on a minimal set of harmonized clinical features [57].
2. Research Reagent & Data Solutions:
Table 3: Essential Components for Population-Level Infertility Risk Model
| Component | Function/Description | Example/Format |
|---|---|---|
| NHANES Data | A publicly available, cross-sectional survey of the U.S. population. | Data cycles (e.g., 2015-2018, 2021-2023) with reproductive health questionnaires. |
| Binary Infertility Outcome | Self-reported inability to conceive after ≥12 months of trying. | Binary variable (Yes/No) based on survey response [57]. |
| Harmonized Clinical Features | A consistent set of predictors available across all survey cycles. | Age at menarche, total deliveries, menstrual irregularity, history of PID, hysterectomy, oophorectomy [57]. |
| Ensemble ML Models | A combination of multiple models to improve robustness and prediction. | Logistic Regression, Random Forest, XGBoost, SVM, Naive Bayes, Stacking Classifier [57]. |
| GridSearchCV | Exhaustive search over specified parameter values for an estimator. | Used for hyperparameter tuning with 5-fold cross-validation [57]. |
3. Experimental Workflow:
4. Step-wise Methodology:
- Step 1 - Data Extraction & Harmonization: Download and combine relevant NHANES cycles. Extract a consistent set of clinical and reproductive health variables available across all selected cycles. This may require excluding demographic or behavioral variables not consistently collected, to ensure a harmonized dataset [57].
- Step 2 - Cohort Definition: Apply inclusion and exclusion criteria to define the study population (e.g., women aged 19-45 with complete data on the selected variables). This results in the final analytic sample [57].
- Step 3 - Model Development and Tuning: Train a diverse set of machine learning models, from interpretable Logistic Regression to complex ensembles like a Stacking Classifier. Use a rigorous tuning process such as
GridSearchCVwith 5-fold cross-validation on the training data to find the optimal hyperparameters for each model. Adaptive optimizers like Adam can be integral for training any neural network components within the ensemble [57]. - Step 4 - Comprehensive Performance Validation: Evaluate all models on the test set. Report a suite of metrics including AUC-ROC, Precision, Recall, and F1-score. Given the potential for class imbalance, the F1-score and Precision-Recall curves are especially critical for assessing performance on the minority (infertile) class [57].
- Step 5 - Trend Analysis and Reporting: Analyze the trained model to identify the most important predictive features (e.g., prior childbirth, menstrual irregularity). Furthermore, use the aggregated data to analyze temporal trends in infertility prevalence, providing valuable public health insights [57].
The Scientist's Toolkit
Table 4: Essential Computational Tools for ML in Fertility Research
| Tool Category | Specific Examples | Role in Optimization & Model Development |
|---|---|---|
| Gradient-Based Optimizers | Adam, RMSprop, SGD with Momentum, SGD | Core algorithms for updating model parameters to minimize loss during training. Adam is often the default choice for its adaptive properties [54]. |
| Gradient Boosting Frameworks | LightGBM, XGBoost | Intrinsic optimization via boosting; often outperform neural networks on structured tabular data common in medical records [56] [57]. |
| Hyperparameter Tuning Modules | GridSearchCV, RandomizedSearchCV, Bayesian Optimization | Automate the search for optimal optimizer and model parameters (e.g., learning rate, batch size), which is critical for performance [57]. |
| Model Interpretation Libraries | SHAP (SHapley Additive exPlanations), LIME (Local Interpretable Model-agnostic Explanations) | Provide post-hoc explanations for model predictions, essential for clinical trust and validating feature importance [56]. |
| Deep Learning Platforms | TensorFlow, PyTorch | Provide flexible, low-level environments for building custom neural networks and implementing a wide variety of optimizers [58]. |
Evaluating Model Performance: Validation Frameworks and Algorithm Comparison
In the specialized field of predicting rare fertility outcomes, selecting appropriate performance metrics is paramount for evaluating machine learning (ML) models accurately. Rare events in reproductive medicine, such as clinical pregnancy or live birth following assisted reproductive technology (ART), present unique challenges for model assessment. The 2022 study by Mehrjerd et al. highlighted this challenge in infertility treatment prediction, reporting clinical pregnancy rates of 32.7% for IVF/ICSI and 18.04% for IUI treatments [59]. For such contexts, relying on a single metric provides an incomplete picture of model utility. A framework incorporating the Area Under the Receiver Operating Characteristic Curve (AUC), Accuracy, and Brier Score offers a more comprehensive approach by measuring complementary aspects of model performance: discrimination, classification correctness, and calibration of probabilistic predictions.
The importance of proper metric selection is further emphasized by research indicating that the behavior of performance metrics in rare event settings depends more on the absolute number of events than the event rate itself. Studies have demonstrated that AUC can be used reliably in rare-outcome settings when the number of events is sufficiently large (e.g., >1000 events), with performance issues arising mainly from small effective sample sizes rather than low prevalence rates [60]. This insight is particularly relevant for fertility research, where accumulating adequate sample sizes requires multi-center collaborations or extended data collection periods.
Metric Definitions and Interpretations
Core Metric Theory and Calculations
Area Under the ROC Curve (AUC) measures a model's ability to distinguish between events and non-events, representing the probability that a randomly selected positive instance will be ranked higher than a randomly selected negative instance. Mathematically, for a prediction model ( f ), (\text{AUC}(f,P) = P{f(X1) < f(X2) \mid Y1 = 0, Y2 = 1}), where ((X1,Y1)) and ((X2,Y2)) are independent draws from the distribution (P) [60]. AUC values range from 0.5 (no discrimination) to 1.0 (perfect discrimination), with values of 0.7-0.8 considered acceptable, 0.8-0.9 excellent, and >0.9 outstanding in medical prediction contexts.
Accuracy represents the proportion of correct predictions among all predictions: (\text{accuracy} = (TP + TN) / (TP + TN + FP + FN)), where TP = True Positives, TN = True Negatives, FP = False Positives, and FN = False Negatives [60]. While intuitively simple, accuracy can be misleading for imbalanced datasets, where the majority class dominates the metric.
Brier Score quantifies the accuracy of probabilistic predictions by calculating the mean squared difference between predicted probabilities and actual outcomes: (\text{BS} = \frac{1}{N}\sum{t=1}^{N}(ft - ot)^2), where (ft) is the predicted probability and (o_t) is the actual outcome (0 or 1) [61]. The score ranges from 0 to 1, with lower values indicating better-calibrated predictions. A perfect model would have a Brier Score of 0, while an uninformative model that predicts the average event rate for all cases would have a score equal to (\bar{o}(1-\bar{o})), where (\bar{o}) is the event rate [62].
Comparative Analysis of Metrics
Table 1: Key Characteristics of Clinical Prediction Metrics
| Metric | Measures | Value Range | Optimal Value | Strengths | Limitations |
|---|---|---|---|---|---|
| AUC | Discrimination | 0.5 - 1.0 | 1.0 | Independent of threshold and prevalence; Good for ranking | Does not measure calibration; Insensitive to predicted probabilities |
| Accuracy | Classification correctness | 0 - 1 | 1.0 | Simple interpretation; Direct clinical relevance | Misleading with class imbalance; Threshold-dependent |
| Brier Score | Overall accuracy of probabilities | 0 - 1 | 0.0 | Comprehensive (calibration + discrimination); Proper scoring rule | Less intuitive; Requires probabilistic predictions |
The Brier Score's particular strength lies in its decomposition into three interpretable components: reliability (calibration), resolution (separation between risk groups), and uncertainty (outcome variance) [61]. This decomposition provides nuanced insights into different aspects of prediction quality that are not apparent from the aggregate score alone. For clinical decision-making in fertility treatments, where probability estimates directly influence patient counseling and treatment selection, this granular understanding of prediction performance is invaluable.
Application in Fertility Outcome Prediction
Performance Metrics in Recent Fertility Studies
Table 2: Metric Performance in Recent Fertility Prediction Studies
| Study | Prediction Task | Best Model | AUC | Accuracy | Brier Score | Other Metrics |
|---|---|---|---|---|---|---|
| Mehrjerd et al. (2022) [59] | Clinical pregnancy (IVF/ICSI) | Random Forest | 0.73 | Not reported | 0.13 | Sensitivity: 0.76, PPV: 0.80 |
| Mehrjerd et al. (2022) [59] | Clinical pregnancy (IUI) | Random Forest | 0.70 | Not reported | 0.15 | Sensitivity: 0.84, PPV: 0.82 |
| Shanghai First Maternity (2025) [9] | Live birth (fresh embryo) | Random Forest | >0.80 | Not reported | Not reported | Feature importance: female age, embryo grade |
| Blastocyst Yield (2025) [56] | Blastocyst formation | LightGBM | Not applicable | 0.675-0.710 | Not reported | Kappa: 0.365-0.500, MAE: 0.793 |
| MLCS vs SART (2025) [10] | Live birth | MLCS | Not reported | Not reported | Used in validation | PR-AUC, F1 score, PLORA |
Recent research in fertility prediction models demonstrates the varied application of performance metrics across different prediction tasks. The 2025 study by the Shanghai First Maternity and Infant Hospital developed ML models for predicting live birth outcomes following fresh embryo transfer, with Random Forest (RF) achieving the best predictive performance (AUC > 0.8) [9]. Feature importance analysis identified key predictors including female age, grades of transferred embryos, number of usable embryos, and endometrial thickness. Similarly, a 2025 study on blastocyst yield prediction reported accuracy values between 0.675-0.71 with kappa coefficients of 0.365-0.5, indicating fair to moderate agreement beyond chance [56].
The comparative analysis between machine learning center-specific (MLCS) models and the Society for Assisted Reproductive Technology (SART) model demonstrated that MLCS significantly improved minimization of false positives and negatives overall (precision recall area-under-the-curve) and at the 50% live birth prediction threshold (F1 score) compared to SART (p < 0.05) [10]. This highlights the importance of selecting metrics aligned with clinical utility, particularly for decision support in fertility treatment planning.
Interrelationships and Trade-offs Between Metrics
The relationship between performance metrics involves important trade-offs that researchers must consider. A model can demonstrate high accuracy but poor calibration, as measured by the Brier Score, particularly when classes are imbalanced. Similarly, a model with high AUC may still produce poorly calibrated probability estimates, potentially misleading clinical decision-making. The Brier Score serves as a comprehensive measure that incorporates both discrimination and calibration aspects, with the mathematical relationship: (\text{BS} = \text{REL} - \text{RES} + \text{UNC}), where REL is reliability (calibration), RES is resolution (discrimination), and UNC is uncertainty [61].
For rare fertility outcomes, the behavior of these metrics is particularly important. Research has shown that the performance of sensitivity is driven by the number of events, while specificity is driven by the number of non-events [60]. AUC's reliability in rare event settings depends more on the absolute number of events than the event rate itself, with studies suggesting that approximately 1000 events may be sufficient for stable AUC estimation [60].
Experimental Protocols for Metric Evaluation
Model Training and Validation Protocol
Data Preprocessing and Model Development:
- Data Collection and Cleaning: Assemble retrospective cohort with complete treatment cycles. Exclude cycles with missing critical data (>50% missingness). Implement appropriate imputation methods such as Multi-Level Perceptron (MLP) for continuous variables or missForest for mixed-type data, as utilized in fertility prediction studies [59] [9].
- Feature Selection: Identify clinically relevant predictors through a combination of statistical methods (e.g., p-value thresholding, random forest importance ranking) and clinical expert validation. The 2022 infertility treatment prediction study utilized 17 features for IUI and 38 features for IVF/ICSI after rigorous selection [59].
- Class Imbalance Handling: For rare outcomes, employ techniques such as Synthetic Minority Over-sampling Technique (SMOTE), appropriate stratification during data splitting, or cost-sensitive learning algorithms to address class imbalance without distorting performance metrics.
- Model Training with Cross-Validation: Implement k-fold cross-validation (typically k=5 or 10) for hyperparameter tuning and model selection. Use random search or grid search approaches to optimize hyperparameters, as demonstrated in recent fertility prediction research [9].
Performance Evaluation Protocol
Comprehensive Metric Assessment:
- Calculate Core Metrics: Compute AUC, Accuracy, and Brier Score on the held-out test set using standardized formulas. For the Brier Score, consider also reporting the scaled Brier Score ((1 - \frac{BS}{BS_{max}})) to facilitate interpretation across datasets with different outcome prevalences [62].
- Statistical Validation: Generate confidence intervals for all performance metrics using appropriate methods (e.g., bootstrapping with 1000+ iterations). For model comparisons, utilize statistical tests such as DeLong's test for AUC differences [10].
- Calibration Assessment: Create calibration plots comparing predicted probabilities against observed event rates. Supplement with goodness-of-fit tests such as the Hosmer-Lemeshow test, though recognize their limitations for large samples [62].
- Clinical Utility Evaluation: Conduct decision curve analysis to evaluate the net benefit of the model across a range of clinically relevant probability thresholds, particularly important for fertility counseling and treatment selection [62].
Advanced Considerations for Rare Fertility Outcomes
Metric Limitations and Complementary Approaches
When evaluating prediction models for rare fertility outcomes, researchers should be aware of several critical considerations:
AUC Limitations: While valuable for measuring discrimination, AUC does not capture calibration and can be insensitive to improvements in prediction models, particularly when adding new biomarkers to established predictors [62]. Recent research suggests that for very rare outcomes (<1% prevalence), large sample sizes (n > 1000 events) are necessary for stable AUC estimation [60].
Brier Score Refinements: The standard Brier Score has limitations in capturing clinical utility, leading to proposals for weighted Brier Scores that incorporate decision-theoretic considerations [63]. These weighted versions align more closely with clinical consequences of predictions but require specification of cost ratios between false positives and false negatives.
Threshold Selection: For clinical implementation, optimal threshold selection should consider both statistical measures (Youden's index, closest-to-(0,1) criteria) and clinical consequences through decision curve analysis [62].
Emerging Best Practices
Current literature suggests several emerging best practices for metric selection in rare fertility outcome prediction:
- Always report discrimination and calibration measures together, as they provide complementary information about model performance [62].
- Include decision-analytic measures when models are intended for clinical decision support, particularly for treatment selection and patient counseling [10] [62].
- Provide confidence intervals for all metrics to communicate estimation uncertainty, especially important for rare outcomes where sample sizes may be limited [60].
- Consider the Brier Skill Score ((BSS = 1 - \frac{BS}{BS_{ref}})) to contextualize performance improvement over a naive baseline model [61].
- Report metric performance across relevant clinical subgroups (e.g., by age, infertility diagnosis, or treatment type) to identify potential performance variations [56].
Research Reagent Solutions
Table 3: Essential Methodological Components for Fertility Prediction Research
| Component | Function | Example Implementation |
|---|---|---|
| Data Imputation | Handles missing values in clinical datasets | MLP (Multi-Level Perceptron) for continuous variables; missForest for mixed-type data [59] [9] |
| Feature Selection | Identifies most predictive variables | Random Forest importance ranking; Clinical expert validation [9] [56] |
| Class Imbalance Handling | Addresses rare outcome distribution | SMOTE; Stratified sampling; Cost-sensitive learning [60] |
| Hyperparameter Tuning | Optimizes model performance | Random search with cross-validation; Grid search [9] |
| Model Interpretation | Explains model predictions and feature effects | Partial dependence plots; Individual conditional expectation; Break-down profiles [9] |
| Validation Framework | Assesses model generalizability | k-fold cross-validation; Hold-out testing; External validation [59] [10] |
In the field of rare fertility outcomes research, machine learning (ML) models offer significant potential for uncovering complex, non-linear relationships in high-dimensional data. However, their adoption in clinical practice hinges on clinician trust and model interpretability. Complex model types like Random Forests and Gradient Boosting Machines often function as "black boxes," where the reasoning behind predictions is not inherently clear. This protocol details the application of two essential model interpretability techniques—Feature Importance and Partial Dependence Plots (PDPs)—within the specific context of fertility research, enabling researchers to validate model logic and extract biologically plausible insights.
The integration of these techniques is crucial for translational research, ensuring that predictive models not only achieve high statistical performance but also provide actionable understanding that can inform clinical decision-making for conditions like blastocyst formation or live birth outcomes.
Theoretical Foundation
Feature Importance
Feature Importance quantifies the contribution of each input variable to a model's predictive performance [64]. In fertility research, this helps identify the most potent predictors from a vast set of clinical, morphological, and demographic variables.
- Gini Importance: Used in tree-based models like Random Forests, it calculates the total reduction in node impurity (using the Gini index) attributable to a feature, weighted by the number of samples reaching that node [64].
- Permutation Importance: A model-agnostic method that evaluates the increase in prediction error after randomly shuffling the values of a single feature. A significant increase in error indicates an important feature [64]. This method is particularly valuable for validating findings in complex fertility datasets where variables are often correlated.
Partial Dependence Plots (PDPs)
PDPs visualize the marginal effect of one or two features on the predicted outcome of an ML model, helping to elucidate the functional relationship between a feature and the prediction [65].
- Mathematical Definition: The partial dependence function for a feature or set of features ( XS ) is defined as: ( \hat{f}S(\mathbf{x}S) = \mathbb{E}{XC}\left[\hat{f}(\mathbf{x}S, XC)\right] = \int \hat{f}(\mathbf{x}S, XC) d\mathbb{P}(\mathbf{X}C) ) In practice, this is estimated by averaging over the dataset: ( \hat{f}S(\mathbf{x}S) = \frac{1}{n} \sum{i=1}^n \hat{f}(\mathbf{x}S, \mathbf{x}^{(i)}_{C}) ) [65] [66].
- Individual Conditional Expectation (ICE) Plots: ICE plots deconstruct the PDP by showing the prediction path for each individual instance as the feature of interest changes, revealing heterogeneity in the model's response and the presence of interactions [66].
Applications in Fertility Research
Recent studies demonstrate the critical role of interpretable ML in reproductive medicine.
- Predicting Blastocyst Yield: A 2025 study developed ML models to quantitatively predict blastocyst formation in IVF cycles. Feature importance analysis within a LightGBM model identified the number of extended culture embryos as the most critical predictor (61.5% importance), followed by Day 3 embryo metrics like mean cell number (10.1%) and proportion of 8-cell embryos (10.0%) [56]. Subsequent PDP analysis confirmed positive relationships between these top features and predicted blastocyst yield, providing clinicians with transparent, actionable biological insights [56].
- Live Birth Prediction: In developing models for live birth outcomes following fresh embryo transfer, Random Forests demonstrated superior performance (AUC >0.8). Interpretation of the model identified female age, grades of transferred embryos, number of usable embryos, and endometrial thickness as key predictive features [9]. Such insights move beyond mere prediction to offer potential explanations for treatment success or failure.
Table 1: Key Predictors from Recent Fertility ML Studies
| Study Focus | Top Features Identified | Feature Importance Method | Model Used |
|---|---|---|---|
| Blastocyst Yield [56] | Number of extended culture embryos (61.5%), Mean cell number (D3) (10.1%), Proportion of 8-cell embryos (D3) (10.0%) | Built-in Gini Importance (LightGBM) | LightGBM |
| Live Birth Outcome [9] | Female age, Grades of transferred embryos, Number of usable embryos, Endometrial thickness | Permutation Importance / Gini Importance | Random Forest |
Experimental Protocols
Protocol 1: Calculating and Visualizing Feature Importance
Objective: To identify and rank the most influential features in a predictive model for fertility outcomes.
Materials and Reagents:
- Python 3.8+ or R 4.4+
- Scikit-learn, XGBoost, or LightGBM libraries
- Pandas and NumPy for data handling
- Matplotlib, Seaborn, or ggplot2 for visualization
Procedure:
- Model Training: Train a tree-based model (e.g., Random Forest, XGBoost) on your fertility dataset, using a standard train-test split.
- Gini Importance Extraction:
- After training, access the
feature_importances_attribute of the model object. This returns a normalized array where the sum of all importances is 1. - In R, using the
randomForestpackage, theimportance()function can be used to retrieve the Mean Decrease Accuracy or Gini importance.
- After training, access the
- Permutation Importance Calculation:
- Use
sklearn.inspection.permutation_importance. The function shuffles each feature and calculates the decrease in model performance. - Specify the number of permutations (
n_repeats, e.g., 10) for stability and use an appropriate scoring metric (e.g.,accuracyfor classification,r2for regression).
- Use
- Visualization:
- Create a horizontal bar plot. Sort the features by their importance score in descending order and plot the top 10-15 features for clarity.
- For permutation importance, it is good practice to plot the distribution of importance scores from the multiple permutations as a boxplot.
Troubleshooting Tip: If the importance scores for all features are very low, check for high correlation among features, which can dilute the importance of individual variables. Consider using variance inflation factor (VIF) analysis to identify and remove highly correlated predictors.
Protocol 2: Generating Partial Dependence Plots (PDPs) and ICE Plots
Objective: To visualize the marginal effect of a key predictor (e.g., female age) on a predicted fertility outcome (e.g., live birth probability).
Materials and Reagents:
- Python with Scikit-learn
inspectionmodule or R withpdp/edarfpackage. - A trained ML model object.
- The pre-processed training dataset.
Procedure:
- Feature Selection: Select one or two features of interest based on the feature importance analysis (e.g., female age, endometrial thickness).
- Grid Creation: Define a grid of values for the feature(s) over which to evaluate the model. Typically, this is a linear space based on the feature's range or its quantiles.
- PDP Calculation (Monte Carlo Method):
- For each value in the grid, create a copy of the original dataset where the feature of interest is set to that value.
- Use the trained model to generate predictions for this modified dataset.
- Average the predictions across all data instances to get the PD value for that grid point [65] [66].
- In Python, use
sklearn.inspection.partial_dependenceorPartialDependenceDisplay.from_estimator.
- ICE Plot Calculation: During the PDP calculation, instead of averaging, retain all individual predictions. Each line in an ICE plot represents the prediction for a single instance as the feature changes [66].
- Visualization:
- For 1D PDP, plot the grid values on the x-axis and the average prediction on the y-axis. Overlay ICE lines to visualize heterogeneity.
- For 2D PDP, use a heatmap with the two features on the x and y axes and the prediction values represented by color intensity.
- Always include a rug plot on the 1D PDP to show the distribution of the underlying data.
Critical Consideration: PDPs assume that the feature(s) being analyzed are independent of the other features. This is often violated in medical data (e.g., female age and ovarian reserve are correlated). Be cautious in interpretation, as the plot may include unrealistic data combinations. Always check for strong feature correlations before relying on a PDP [65].
Diagram 1: Procedural flow for generating PDPs and ICE plots, highlighting the critical steps of data modification and aggregation.
Data Presentation and Visualization Standards
Table 2: Comparison of Model Interpretation Techniques
| Characteristic | Feature Importance | Partial Dependence Plots (PDPs) | Individual Conditional Expectation (ICE) |
|---|---|---|---|
| Primary Purpose | Rank features by predictive contribution | Show average marginal effect of a feature | Show instance-level marginal effect of a feature |
| Scope | Global (entire model) | Global (entire model) | Local (per instance) & Global (aggregated) |
| Handles Interactions | Indirectly (can be masked) | Poorly; assumes feature independence | Explicitly reveals heterogeneity and interactions |
| Computational Cost | Low (Gini) to Medium (Permutation) | High (scales with dataset & grid size) | High (same as PDP, plus plotting many lines) |
| Key Insight Provided | "Which features matter most?" | "What is the average relationship between feature X and the prediction?" | "How consistent is the feature's effect across different patients?" |
The Scientist's Toolkit: Essential Research Reagents & Software
Table 3: Key Computational Tools for Model Interpretation
| Item Name | Function / Application | Example in Fertility Research |
|---|---|---|
Scikit-learn inspection Module |
Calculates permutation importance and partial dependence. | Quantifying the impact of shuffling "Female Age" on live birth prediction accuracy [66]. |
pdpbox Python Library |
Specialized library for creating rich PDP and ICE plots. | Visualizing the non-linear relationship between "Number of Oocytes" and predicted blastocyst yield [67] [68]. |
edarf R Package |
Efficiently computes partial dependence for Random Forests. | Rapidly analyzing the marginal effect of "Endometrial Thickness" across a large IVF cohort dataset [69]. |
| LightGBM/XGBoost | Gradient boosting frameworks with built-in feature importance. | Identifying "Number of extended culture embryos" as the top predictor in a blastocyst formation model [56]. |
| ColorBrewer Palettes | Provides color schemes for accessible data visualization. | Applying a diverging color palette in a 2D PDP to show interaction between "Age" and "BMI" while ensuring colorblind-readability [70]. |
Advanced Applications and Integration
PDP-based Feature Importance
An extension of the standard techniques involves calculating feature importance directly from the PDP itself. For a numerical feature, importance is defined as the standard deviation of the partial dependence values across its unique values. A flat PDP indicates low importance, while a PDP with high variance indicates high importance [65]. This provides an alternative, model-agnostic importance measure.
Integrating Findings for Clinical Insight
The true power of these tools is realized when they are used in concert.
- Use Feature Importance as a filter to narrow down dozens of potential predictors to a manageable number of top candidates (e.g., 5-10).
- Use PDPs to understand the average functional form of the relationship between these top features and the outcome (e.g., Is the effect of age linear or threshold?).
- Use ICE Plots to probe for interactions and heterogeneity. If the ICE lines are widely spread and cross, it suggests the effect of the primary feature depends on the values of other features, warranting further investigation with 2D PDPs [66].
Diagram 2: A sequential integration strategy for using interpretation techniques to move from a broad list of features to specific, clinically actionable insights.
Feature Importance and Partial Dependence Plots are indispensable components of the modern fertility researcher's toolkit. By moving beyond model performance metrics to interrogate the "why" behind predictions, these methods build the trust necessary for the clinical adoption of complex ML models. The rigorous application of the protocols outlined here—from calculating permutation importance to generating and interpreting ICE plots—ensures that models designed to predict rare fertility outcomes are not only powerful but also transparent, interpretable, and ultimately, more useful in guiding personalized patient care.
The integration of machine learning (ML) prediction models into clinical practice represents a paradigm shift in rare fertility outcomes research. While high predictive accuracy is a necessary first step, it alone is insufficient for clinical adoption. Clinical utility—the measure of a model's ability to improve actual patient outcomes and decision-making—has emerged as the critical benchmark for implementation. This Application Note establishes a framework for assessing ML models beyond traditional performance metrics, providing structured protocols for evaluating their readiness to enhance rare fertility research and therapeutic development.
The challenge is particularly acute in rare fertility outcomes, where limited dataset sizes, outcome heterogeneity, and profound clinical consequences of prediction errors create unique methodological hurdles. This document provides researchers, scientists, and drug development professionals with standardized protocols to systematically evaluate and demonstrate the clinical utility of ML prediction models, thereby accelerating their translation from research tools to clinical assets.
Quantitative Performance of Fertility Prediction Models
Recent studies demonstrate ML's capacity to predict various fertility outcomes with significant accuracy. The table below summarizes performance metrics from recent ML applications in reproductive medicine.
Table 1: Performance Metrics of Recent ML Models in Fertility Outcomes Prediction
| Prediction Target | Best-Performing Model | Key Performance Metrics | Sample Size | Citation |
|---|---|---|---|---|
| Blastocyst Yield | LightGBM | R²: 0.673-0.676; MAE: 0.793-0.809; Multi-class Accuracy: 0.675-0.71 | 9,649 cycles | [56] |
| Live Birth (Fresh ET) | Random Forest | AUC: >0.8 | 11,728 records | [9] |
| Embryo Selection | iDAScore/BELA | Correlates with cell numbers/fragmentation; Predicts live birth; Improved performance over morphological assessment | N/A | [71] |
These quantitative results establish a baseline for predictive accuracy. However, they represent only the initial step in the broader assessment of clinical readiness.
Conceptual Framework: From Accuracy to Utility
A model's journey to clinical integration requires a fundamental shift in evaluation philosophy, moving from purely statistical measures to patient-impact assessments.
The Clinical Utility Paradigm
Clinical utility is formally defined as the measure of a model's ability to improve patient outcomes and decision-making when compared to standard care or alternative approaches [72]. This concept demands evidence that using the model leads to better health outcomes, not just accurate predictions. In practice, this requires a clear understanding of the action space—the set of possible clinical decisions informed by the model's output [72]. For instance, a model predicting blastocyst yield might inform the decision between extended culture versus cleavage-stage transfer.
Key Evaluation Domains
Assessment of clinical readiness should encompass eight key domains derived from systematic reviews of AI in clinical prediction [73]:
- Diagnosis and Early Detection
- Prognosis of Disease Course
- Risk Assessment
- Treatment Response Prediction
- Disease Progression
- Readmission Risks
- Complication Risks
- Mortality Prediction
For rare fertility outcomes, domains 2, 3, 4, and 7 are typically most relevant, though context dictates priority.
Figure 1: The iterative pathway from model development to clinical impact, highlighting the critical transition from predictive accuracy to clinical utility assessment.
Experimental Protocols for Clinical Utility Assessment
Protocol 1: Emulated Target Trial for Prediction-Based Decision Rules
Purpose
To evaluate the clinical utility of an ML-based prediction rule for rare fertility outcomes using observational data, emulating a randomized controlled trial (RCT) design [72].
Materials
- Data Source: Large-scale, de-identified observational dataset of fertility treatment cycles
- Inclusion Criteria: Patients meeting specific clinical criteria for the rare outcome of interest
- Prediction Model: Pre-trained and validated ML model for the target outcome
- Statistical Software: R or Python with appropriate causal inference packages
Procedure
- Define Trial Components: Explicitly specify eligibility criteria, treatment strategies, assignment procedures, outcomes, and follow-up [72].
- Specify Prediction-Based Decision Rule: Formally define the mapping between model prediction and clinical action (e.g., if predicted probability of blastocyst formation <10%, recommend cleavage-stage transfer).
- Clone-Censor-Weight Analysis:
- Clone: Create copies of each eligible patient under both decision rules (model-based vs. standard care).
- Censor: Discontinue follow-up if a patient's treatment deviates from their assigned strategy.
- Weight: Use inverse probability of treatment weighting to adjust for confounding.
- Compare Outcomes: Estimate the difference in the outcome rate (e.g., cumulative live birth) between the two strategies.
Analysis
- Calculate the average treatment effect of following the prediction-based rule versus standard care.
- Perform sensitivity analyses to assess robustness to unmeasured confounding.
Protocol 2: Decision Curve Analysis for Clinical Impact
Purpose
To quantify the net benefit of using an ML model for clinical decision-making across different probability thresholds [74].
Materials
- Validation Dataset: Dataset with known outcomes not used in model training
- Model Predictions: Probability outputs from the ML model for all patients in validation set
- Clinical Outcome Data: Observed outcomes (e.g., live birth, cycle failure)
Procedure
- Calculate Net Benefit:
- For a range of probability thresholds (e.g., 0.05 to 0.50), calculate the net benefit using the formula:
- Net Benefit = (True Positives/n) - (False Positives/n) × (pₜ/(1-pₜ))
- Where pₜ is the threshold probability, and n is the total number of patients.
- Compare Strategies:
- Plot net benefit curves for three strategies: (1) using the ML model, (2) assuming all patients have the event, (3) assuming no patients have the event.
- Determine Clinical Usefulness:
- Identify threshold ranges where the model provides superior net benefit compared to alternative strategies.
Analysis
- Clinical Impact Curve: Generate a curve showing the reduction in unnecessary interventions across thresholds.
- Decision Threshold: Identify the optimal threshold for clinical implementation based on clinical consequences of false positives and negatives.
Implementation Workflow for Rare Fertility Outcomes
A standardized workflow ensures comprehensive assessment of ML models targeting rare fertility outcomes.
Figure 2: A standardized workflow for developing and implementing ML models for rare fertility outcomes, emphasizing the critical Clinical Readiness Phase where utility is assessed.
Key Considerations for Rare Outcomes
- Data Augmentation: Employ synthetic data generation or transfer learning to address limited sample sizes.
- Validation Techniques: Use leave-one-center-out cross-validation for multi-center studies to assess generalizability.
- Outcome Definition: Establish precise, clinically relevant definitions for rare outcomes (e.g., recurrent implantation failure).
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Methodological Tools for Clinical Utility Assessment in Rare Fertility Research
| Tool Category | Specific Tool/Technique | Function | Application Context |
|---|---|---|---|
| Utility Evaluation | Emulated Target Trial [72] | Estimates causal effect of prediction-based decision rules using observational data | Comparative effectiveness research |
| Clinical Impact | Decision Curve Analysis [74] | Quantifies net benefit across decision thresholds | Treatment selection optimization |
| Model Interpretation | Partial Dependence Plots [56] | Visualizes feature effects on predictions | Model explanation and validation |
| Bias Assessment | Fairness Audits [75] | Detects performance disparities across subgroups | Equity evaluation in diverse populations |
| Performance Tracking | Model Cards & Documentation | Standardizes reporting of limitations and intended use | Regulatory compliance and transparency |
Transitioning from predictive accuracy to demonstrated clinical utility requires rigorous, standardized assessment protocols tailored to the challenges of rare fertility outcomes. The frameworks and methodologies presented herein provide a roadmap for researchers to generate the evidence necessary for clinical adoption. By implementing these protocols, the field can advance beyond technically proficient models to those that genuinely improve patient care and outcomes in this challenging domain. Future work should focus on validating these approaches across diverse fertility populations and establishing consensus standards for clinical utility in reproductive medicine.
Conclusion
Machine learning represents a paradigm shift in predicting rare fertility outcomes, offering significant advantages over traditional statistical approaches through its ability to model complex, non-linear relationships in high-dimensional data. The evidence consistently demonstrates that algorithms like Random Forest, XGBoost, and LightGBM can achieve robust predictive performance for outcomes such as live birth and blastocyst formation, with key predictors including female age, embryo quality metrics, and hormonal parameters. Future directions must focus on developing standardized validation frameworks across diverse populations, enhancing model interpretability for clinical adoption, and integrating multi-omics data for improved personalization. For biomedical researchers and drug development professionals, these advancements create opportunities for developing decision support tools that can optimize treatment protocols, identify novel therapeutic targets, and ultimately improve the precision and success of infertility interventions. The convergence of machine learning and reproductive medicine holds promise for transforming infertility treatment from an uncertain journey into a more predictable, personalized, and successful experience for patients worldwide.
References
- 1. Analysis of factors influencing clinical pregnancy rates in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12237683/]
- 2. Machine learning algorithms in constructing prediction ... [https://www.nature.com/articles/s41598-024-83781-x]
- 3. Article Day 3 embryo quality impact on euploidy rate and ... [https://www.sciencedirect.com/science/article/abs/pii/S1472648325001312]
- 4. Why IVF Labs Must Track Digital KPIs to Enhance Outcomes [https://www.vitrifysoftware.com/why-every-ivf-lab-should-track-digital-kpis-to-improve-outcomes/]
- 5. Predictive models for live birth outcomes following fresh ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07045-6]
- 6. Machine learning in predicting infertility treatment success [https://pmc.ncbi.nlm.nih.gov/articles/PMC12017416/]
- 7. Catalyzing IVF outcome prediction: exploring advanced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11573753/]
- 8. Guidelines for Developing and Reporting Machine ... [https://www.jmir.org/2016/12/e323/]
- 9. Predictive models for live birth outcomes following fresh ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462326/]
- 10. Machine learning center-specific models show improved ... [https://www.nature.com/articles/s41467-025-58744-z]
- 11. The association between female age and pregnancy ... [https://www.nature.com/articles/s41598-024-70249-1]
- 12. Effect of maternal age, embryo number and quality on ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1596178/full]
- 13. Advanced maternal age was associated with an annual ... [https://www.sciencedirect.com/science/article/pii/S0015028225004388]
- 14. A meta-analysis of fertility and adverse outcomes in oil [https://pmc.ncbi.nlm.nih.gov/articles/PMC10013086/]
- 15. Fertility Outcomes and Contrast Media in ... [https://www.nature.com/research-intelligence/nri-topic-summaries/fertility-outcomes-and-contrast-media-in-hysterosalpingography-micro-397187]
- 16. Machine learning predicts live-birth occurrence before in- ... [https://www.nature.com/articles/s41598-020-76928-z]
- 17. Prediction model for missed abortion of patients treated ... [https://peerj.com/articles/14762/]
- 18. Development of a dynamic machine learning algorithm to ... [https://www.sciencedirect.com/science/article/pii/S2666334122000368]
- 19. Exploring machine learning algorithms for predicting ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2024.1495382/full]
- 20. Hyperparameter optimization based machine learning ... [https://link.springer.com/article/10.1007/s10791-025-09815-8]
- 21. A Tutorial and Use Case Example of the eXtreme Gradient ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11895769/]
- 22. Comparing machine learning approaches for predicting the ... [https://www.sciencedirect.com/science/article/pii/S2666521225000079]
- 23. Development and validation of a machine learning-based ... [https://pubmed.ncbi.nlm.nih.gov/40986161/]
- 24. Predicting pregnancy outcomes in IVF cycles: a systematic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476623/]
- 25. Artificial neural network-driven approaches to improved ... [https://www.nature.com/articles/s41598-025-05364-8]
- 26. Hyperparameter Optimization in Machine Learning [https://arxiv.org/html/2410.22854v1]
- 27. Comparative study of machine learning approaches ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11469510/]
- 28. A hybrid feature selection algorithm to determine effective ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10869959/]
- 29. Hybrid Filter and Genetic Algorithm-Based Feature ... [https://www.mdpi.com/2227-9717/11/2/562]
- 30. Using feature optimization and LightGBM algorithm to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10716466/]
- 31. An integrated optimization and deep learning pipeline for ... [https://www.sciencedirect.com/science/article/pii/S0169260725003967]
- 32. Development and validation of machine learning models ... [https://pubmed.ncbi.nlm.nih.gov/40596532/]
- 33. Catalyzing IVF outcome prediction: exploring advanced ... [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2024.1392611/full]
- 34. Predictive modeling of pregnancy outcomes utilizing multiple ... [https://bmcpregnancychildbirth.biomedcentral.com/articles/10.1186/s12884-025-07433-2]
- 35. Using feature optimization and LightGBM algorithm to ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2023.1305473/full]
- 36. Estimation of minimal data sets sizes for machine learning ... [https://www.nature.com/articles/s41746-024-01360-w]
- 37. Machine learning on small size samples: A synthetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10358596/]
- 38. Revisiting Performance Metrics for Prediction with Rare ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8561661/]
- 39. Advancements in predicting and modeling rare event ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-023-02060-x]
- 40. Importance of sample size on the quality and utility of AI ... [https://www.sciencedirect.com/science/article/pii/S2589750025000214]
- 41. Application of machine learning algorithms and SHAP ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277441/]
- 42. Prediction of pregnancy-related complications in women ... [https://www.sciencedirect.com/science/article/pii/S0015028224001122]
- 43. Predicting adverse birth outcome among childbearing women ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11285398/]
- 44. Hyperparameter tuning. Grid search and random search [https://www.yourdatateacher.com/2021/05/19/hyperparameter-tuning-grid-search-and-random-search/]
- 45. Hyperparameter tuning: Optimizing ML models for excellence [https://www.leewayhertz.com/hyperparameter-tuning/]
- 46. Hyperparameter optimization [https://en.wikipedia.org/wiki/Hyperparameter_optimization]
- 47. 3.2. Tuning the hyper-parameters of an estimator [https://scikit-learn.org/stable/modules/grid_search.html]
- 48. A Conceptual Explanation of Bayesian Hyperparameter ... [https://medium.com/data-science/a-conceptual-explanation-of-bayesian-model-based-hyperparameter-optimization-for-machine-learning-b8172278050f]
- 49. Hyperparameter Optimization Based on Bayesian ... [https://www.geeksforgeeks.org/machine-learning/hyperparameter-optimization-based-on-bayesian-optimization/]
- 50. Bayesian optimization with Optuna for enhanced soil ... [https://www.sciencedirect.com/science/article/pii/S2772375525003685]
- 51. Internal validation and comparison of predictive models to ... [https://www.nature.com/articles/s41598-022-10902-9]
- 52. Deep feature engineering for accurate sperm morphology ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0330914]
- 53. FertilitY Predictor—a machine learning-based web tool for the prediction of assisted reproduction outcomes in men with Y chromosome microdeletions | Journal of Assisted Reproduction and Genetics [https://link.springer.com/article/10.1007/s10815-024-03338-9]
- 54. Optimizers: A Deep Dive into Gradient Descent, Adam, and ... [https://medium.com/@ilyurek/optimizers-a-deep-dive-into-gradient-descent-adam-and-beyond-e6a1d00bc9b0]
- 55. [2407.21078] Convergence rates for the Adam optimizer [https://arxiv.org/abs/2407.21078]
- 56. Development and validation of machine learning models ... [https://www.nature.com/articles/s41598-025-06998-4]
- 57. A Cross-Cohort Analysis Using NHANES Data (2015–2023) [https://pmc.ncbi.nlm.nih.gov/articles/PMC12427665/]
- 58. a machine learning framework for predicting disease ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06308-6]
- 59. Internal validation and comparison of predictive models to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9068696/]
- 60. Behavior of prediction performance metrics with rare events [https://arxiv.org/html/2504.16185v2]
- 61. Brier score [https://en.wikipedia.org/wiki/Brier_score]
- 62. Assessing the performance of prediction models: a framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3575184/]
- 63. Weighted Brier Score - an Overall Summary Measure for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12523994/]
- 64. Understanding Feature Importance in Machine Learning [https://builtin.com/data-science/feature-importance]
- 65. 19 Partial Dependence Plot (PDP) - Christoph Molnar [https://christophm.github.io/interpretable-ml-book/pdp.html]
- 66. Partial dependence plots (PDP) and individual conditional ... [https://scikit-learn.org/stable/modules/partial_dependence.html]
- 67. Partial Dependence Plots (PDPs) to Interpret Complex ... [https://www.nb-data.com/p/partial-dependence-plots-pdps-to]
- 68. Understanding Partial Dependence Plots (PDPs) [https://medium.com/data-science-in-your-pocket/understanding-partial-dependence-plots-pdps-415346b7e7f1]
- 69. In Search of the Perfect Partial Plot - Artful Analytics [https://seth-dobson.github.io/in-search-of-the-perfect-partial-plot/]
- 70. What to consider when choosing colors for data visualization [https://academy.datawrapper.de/article/140-what-to-consider-when-choosing-colors-for-data-visualization]
- 71. Global Trends in the Use of Artificial Intelligence (AI) in ... [https://jivfww.scholasticahq.com/article/140673-global-trends-in-the-use-of-artificial-intelligence-ai-in-reproductive-medicine-insights-from-surveys-of-international-fertility-specialists]
- 72. Aim for Clinical Utility, Not Just Predictive Accuracy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7144757/]
- 73. Artificial Intelligence for Clinical Prediction: Exploring Key ... [https://www.sciencedirect.com/science/article/pii/S2666990024000156]
- 74. Aim for Clinical Utility, Not Just Predictive Accuracy [https://api.semanticscholar.org/arXiv:1909.03801]
- 75. AI Model Testing in 2025: The Complete Guide [https://www.prismetric.com/ai-model-testing-guide/]