Proximity Search Mechanisms: A New Paradigm for Interpretable Clinical AI and Drug Discovery
This article explores the transformative potential of proximity-based mechanisms in enhancing the interpretability and trustworthiness of artificial intelligence for clinical decision-making and drug development.
Proximity Search Mechanisms: A New Paradigm for Interpretable Clinical AI and Drug Discovery
Abstract
This article explores the transformative potential of proximity-based mechanisms in enhancing the interpretability and trustworthiness of artificial intelligence for clinical decision-making and drug development. It provides a comprehensive examination of the foundational principles, drawing parallels from biologically inspired induced proximity in therapeutics. The scope covers methodological applications, including uncertainty-aware evidence retrieval and explainable AI (XAI) frameworks, that leverage proximity to create transparent, auditable models. The article further addresses critical troubleshooting and optimization strategies to overcome implementation challenges, and concludes with rigorous validation and comparative analysis frameworks essential for clinical adoption. Aimed at researchers, scientists, and drug development professionals, this work synthesizes cutting-edge research to outline a roadmap for building reliable, interpretable, and clinically actionable AI systems.
The Foundations of Proximity: From Biological Principles to Computational Interpretability
The concept of induced proximity represents a paradigm shift across multiple scientific disciplines, from fundamental molecular biology to advanced computational clinical research. In molecular biology, it describes the deliberate bringing together of cellular components to trigger specific biological outcomes [1]. In computational research, proximity searching provides a methodological framework for finding conceptually related terms within a body of text, enhancing data interpretability [2]. This article explores this unifying principle through application notes and detailed experimental protocols, framing them within the context of clinical interpretability research. By examining proximity-based mechanisms across these domains, researchers can identify transferable strategies for enhancing the precision, efficacy, and explainability of both therapeutic interventions and clinical risk prediction models.
Molecular Proximity: Mechanisms and Applications
Fundamental Mechanisms of Induced Proximity
Molecular proximity technologies function as "matchmakers" within the cellular environment, creating transient but productive interactions between disease-causing proteins and cellular machinery that can neutralize them [1] [3]. These systems typically consist of a heterobifunctional design where one domain binds to a target protein, another domain recruits an effector protein, and a linker connects these domains to facilitate new protein-protein interactions [1]. The matchmaker component subsequently dissociates, allowing for catalytic reuse and enabling a single molecule to eliminate multiple target proteins sequentially [1] [3].
The table below summarizes the primary classes of molecular proximity inducers and their mechanisms of action:
Table 1: Classes of Molecular Proximity Inducers and Their Mechanisms
| Class | Mechanism of Action | Cellular Location | Key Components | Outcome |
|---|---|---|---|---|
| PROTACs (Proteolysis Targeting Chimeras) [1] | Recruit E3 ubiquitin ligase to target protein | Intracellular | Target binder, E3 ligase recruiter, linker | Ubiquitination and proteasomal degradation |
| BiTE Molecules (Bispecific T-cell Engagers) [1] | Connect tumor cells with T cells | Extracellular, cell surface | CD3 binder, tumor antigen binder | T-cell mediated cytotoxicity |
| Molecular Glues (e.g., LOCKTAC) [1] | Stabilize existing protein interactions | Intracellular/Extracellular | Monovalent small molecule | Target stabilization or inhibition |
| LYTACs (Lysosome Targeting Chimeras) [1] | Link extracellular proteins to lysosomal receptors | Extracellular, cell surface | Target binder, lysosomal receptor binder | Lysosomal degradation |
| RNATACs (RNA-Targeting Chimeras) [1] | Target faulty RNA for degradation | Intracellular | RNA binder, nuclease recruiter | RNA degradation and reduced protein translation |
Experimental Protocol: DNA-Encoded Library Screening for Proximity Inducers
Purpose: To identify novel proximity-inducing molecules from vast chemical libraries using DNA-encoded library (DEL) technology [1].
Materials and Reagents:
- DNA-encoded chemical library (contains billions of unique small molecules tagged with DNA barcodes)
- Target protein of interest (purified, with known involvement in disease pathology)
- Effector protein (appropriate for desired outcome, e.g., E3 ubiquitin ligase for degradation)
- Solid support with immobilized binding partner
- PCR reagents for amplification of recovered DNA barcodes
- Next-generation sequencing platform for barcode identification
- Buffer systems (appropriate for maintaining protein stability and interactions)
Procedure:
- Library Preparation: Dilute the DNA-encoded library in appropriate binding buffer to ensure optimal diversity representation [1].
- Incubation with Target: Combine the library with immobilized target protein and incubate for 2-4 hours at 4°C with gentle agitation to facilitate binding.
- Wash Steps: Perform sequential wash steps (5-10 cycles) with buffer containing mild detergents to remove non-specifically bound molecules.
- Elution of Binders: Release specifically bound molecules using mild denaturing conditions (e.g., low pH or high salt) that preserve DNA barcode integrity.
- PCR Amplification: Amplify recovered DNA barcodes using primers compatible with subsequent sequencing platforms.
- Next-Generation Sequencing: Sequence the amplified DNA barcodes to identify molecules that bound to the target protein.
- Hit Validation: Resynthesize identified hit compounds without DNA tags and validate their binding and functional activity in secondary assays.
Troubleshooting Notes:
- Low library diversity can lead to limited hit identification; ensure proper library storage and handling.
- High background noise may require optimization of wash stringency.
- False positives may occur due to promiscuous binders; include appropriate counter-screens.
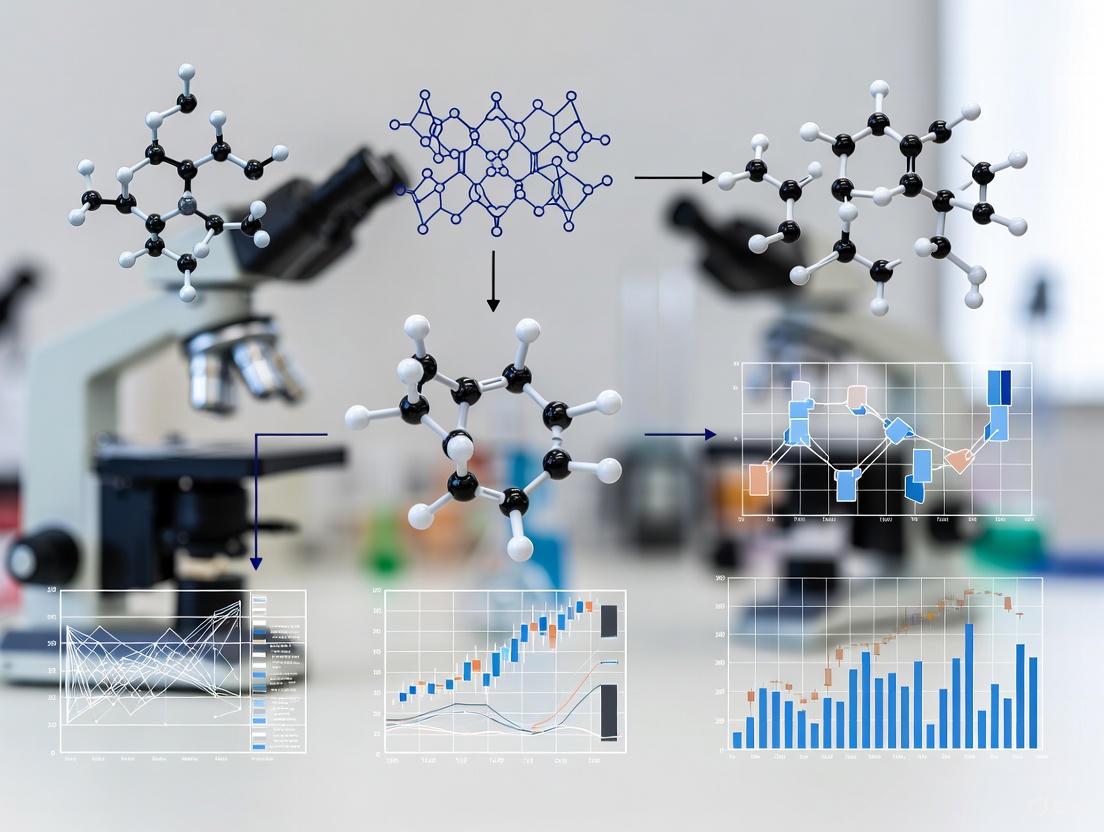
Diagram 1: DEL Screening Workflow for identifying proximity-inducing molecules.
Computational Proximity: Enhancing Clinical Interpretability
Proximity Search Mechanisms for Clinical Data Mining
In computational research, proximity searching enables researchers to locate conceptually related terms that appear near each other in text, regardless of the exact phrasing [2]. This methodology is particularly valuable for clinical interpretability research, where understanding relationships between clinical concepts, symptoms, and outcomes is essential. Different database systems implement proximity operators with varying syntax but consistent underlying principles.
The table below compares proximity search operators across different research database platforms:
Table 2: Proximity Search Operators Across Research Platforms
| Database Platform | Near Operator (Unordered) | Within Operator (Ordered) | Maximum Word Separation |
|---|---|---|---|
| EBSCO Databases [2] | N5 (finds terms within 5 words, any order) | W5 (finds terms within 5 words, specified order) | Varies (typically 10-255 words) |
| ProQuest [2] | N/5 or NEAR/5 | W/5 | Varies by implementation |
| Web of Science [2] | NEAR/5 (must spell out NEAR) | Not typically available | Varies by implementation |
| Google [2] | AROUND(5) | Not available | Limited contextual proximity |
Experimental Protocol: Proximity-Enhanced Clinical Risk Prediction
Purpose: To develop an interpretable clinical risk prediction model using proximity-based rule mining for acute coronary syndrome (ACS) mortality prediction [4].
Materials and Software:
- Clinical dataset (de-identified patient records including demographics, clinical measurements, and outcomes)
- Data preprocessing tools (for handling missing values and normalization)
- Rule mining algorithm (for creating dichotomized risk factors)
- Machine learning classifier (e.g., logistic regression, neural networks)
- Model evaluation framework (discrimination and calibration metrics)
- Statistical software (R, Python with appropriate libraries)
Procedure:
- Data Preparation:
- Collect and de-identify patient data including clinical parameters, lab values, and 30-day mortality outcomes [4].
- Handle missing data using appropriate imputation methods.
- Split data into training (70%), validation (15%), and test (15%) sets.
Rule Generation through Conceptual Proximity:
- Identify key clinical concepts related to ACS mortality through literature review.
- Create dichotomized rules by applying thresholds to continuous variables (e.g., "age > 65", "systolic BP < 100") [4].
- Use proximity searching in clinical literature databases to validate and expand rule concepts.
Model Training:
- Train a machine learning classifier to predict the "acceptance degree" (probability of correctness) for each rule for individual patients [4].
- Combine rule acceptance degrees to compute personalized mortality risk scores.
- Incorporate reliability estimates for each prediction.
Model Evaluation:
- Assess discrimination using Area Under the ROC Curve (AUC).
- Evaluate calibration using calibration curves and metrics.
- Compare performance against established clinical risk scores (e.g., GRACE score) [4].
Validation Metrics:
- Area Under ROC Curve (AUC): Target >0.80 for good discrimination [4].
- Geometric Mean (GM): Combined measure of sensitivity and specificity.
- Positive Predictive Value (PPV) and Negative Predictive Value (NPV): Clinical relevance of predictions.
- Calibration Slope: Target接近 1.0 (e.g., 0.96) for ideal calibration [4].
Diagram 2: Clinical Risk Prediction Workflow using proximity-based rules.
Integrated Application: Bridging Molecular and Computational Proximity
The table below details key research reagents and computational resources essential for proximity-based research across biological and computational domains:
Table 3: Research Reagent Solutions for Proximity Studies
| Category | Item | Specifications | Application/Function |
|---|---|---|---|
| Molecular Biology | DNA-encoded Libraries [1] | Billions of unique small molecules with DNA barcodes | High-throughput screening for proximity inducers |
| E3 Ubiquitin Ligase Recruiters [1] | CRBN, VHL, or IAP-based ligands | Targeted protein degradation via PROTACs | |
| Bispecific Scaffolds [1] | Anti-CD3 x anti-tumor antigen formats | T-cell engagement via BiTE technology | |
| Cell-Based Assays | Reporter Cell Lines | Engineered with pathway-specific response elements | Functional validation of proximity inducers |
| Primary Immune Cells | T-cells, macrophages from human donors | Ex vivo efficacy testing of immunomodulators | |
| Computational Resources | Research Databases [2] | EBSCO, ProQuest, Web of Science | Proximity searching for literature mining |
| Clinical Data Repositories | De-identified patient records with outcomes | Training and validation of risk prediction models | |
| Machine Learning Frameworks | Python/R with scikit-learn, TensorFlow | Implementation of interpretable AI models |
Advanced Protocol: Integrating Molecular and Computational Proximity for Target Validation
Purpose: To create an integrated workflow combining computational proximity searching with molecular proximity technologies for novel target validation.
Procedure:
- Target Identification via Literature Proximity Mining:
- Use proximity search operators (e.g., "disease N5 pathway N5 mechanism") to identify novel disease mechanisms [2].
- Apply natural language processing to extract protein-protein interaction networks from scientific literature.
- Prioritize targets based on network connectivity and druggability predictions.
Molecular Proximity Probe Design:
- Design PROTAC molecules or other proximity inducers for prioritized targets using structural informatics.
- Synthesize and validate target binding and degradation efficacy in cellular models.
Clinical Correlate Analysis:
- Apply proximity-based clinical rule mining to electronic health records.
- Identify patient subgroups most likely to respond to target modulation based on clinical特å¾.
Iterative Refinement:
- Use clinical insights to refine molecular design.
- Apply molecular insights to improve clinical risk stratification.
Validation Metrics:
- Computational: Precision and recall of target-disease association mining.
- Molecular: Degradation efficiency (DC50), maximum degradation (Dmax), and selectivity.
- Clinical: Model interpretability, reliability estimation, and clinical utility measures.
The principle of proximity—whether molecular or computational—provides a powerful framework for enhancing precision and interpretability in biomedical research. Molecular proximity technologies enable targeted manipulation of previously "undruggable" cellular processes, while computational proximity methods enhance our ability to extract meaningful patterns from complex clinical data. The integrated application of both approaches, as demonstrated in these application notes and protocols, offers a promising path toward more interpretable, reliable, and effective strategies for drug development and clinical decision support. As both fields continue to evolve, their convergence will likely yield novel insights and methodologies that further advance the precision medicine paradigm.
Chemically Induced Proximity (CIP) represents a transformative approach in biological research and therapeutic development, centered on using small molecules to control protein interactions with precise temporal resolution. Proximity, or the physical closeness of molecules, is a pervasive regulatory mechanism in biology that governs cellular processes including signaling cascades, chromatin regulation, and protein degradation [5]. CIP strategies utilize chemical inducers of proximity (CIPs)—synthetic, drug-like molecules that bring specific cellular proteins into close contact, thereby activating or modifying their function. This technology has evolved from a basic research tool to a promising therapeutic modality, enabling scientists to manipulate biological pathways in ways that were previously impossible. The lessons learned from applying CIP principles to targeted protein degradation platforms, particularly PROTACs and Molecular Glues, are now reshaping drug discovery and expanding the druggable proteome.
Fundamental Mechanisms of CIP, PROTACs, and Molecular Glues
Core Principles of Chemically Induced Proximity
At its foundation, CIP relies on creating physical proximity between proteins that may not naturally interact. This induced proximity can trigger downstream biological events such as signal transduction, protein translocation, or targeted degradation. The core mechanism involves a CIP molecule acting as a bridge between two protein domains—typically a "receptor" and a "receiver" [6]. This ternary complex formation can occur within seconds to minutes after CIP addition, allowing for precise experimental control over cellular processes. Unlike genetic approaches, CIP offers acute temporal control, enabling researchers to study rapid biological responses and avoid compensatory adaptations that may occur with chronic genetic manipulations.
PROTACs: Heterobifunctional Inducers of Degradation
PROteolysis TArgeting Chimeras (PROTACs) represent a sophisticated application of CIP principles for targeted protein degradation. These heterobifunctional molecules consist of three key elements: a ligand that binds to a Protein of Interest (POI), a second ligand that recruits an E3 ubiquitin ligase, and a chemical linker that connects these two moieties [7] [8] [9]. The PROTAC molecule simultaneously engages both the target protein and an E3 ubiquitin ligase, forming a ternary complex that brings the POI into proximity with the cellular degradation machinery. This induced proximity results in the ubiquitination of the target protein, marking it for destruction by the proteasome [9]. A significant advantage of the PROTAC mechanism is its catalytic nature—after ubiquitination, the PROTAC molecule is released and can cycle to degrade additional target proteins, enabling efficacy even at low concentrations [9].
Molecular Glues: Monovalent Stabilizers of Interaction
Molecular Glues represent a distinct class of proximity inducers that function through a monovalent mechanism. Unlike the heterobifunctional structure of PROTACs, molecular glues are typically smaller, single-pharmacophore molecules that induce proximity by stabilizing interactions between proteins [8] [9]. These compounds often work by binding to an E3 ubiquitin ligase and altering its surface, creating a new interface that can recognize and engage target proteins that would not normally interact with the ligase [9]. This induced interaction leads to ubiquitination and degradation of the target protein, similar to the outcome of PROTAC activity but through a different structural approach. Classic examples include thalidomide and its analogs, which bind to the E3 ligase cereblon (CRBN) and redirect it toward novel protein substrates [8].
Comparative Mechanisms Visualization
The diagram below illustrates the fundamental mechanistic differences between Molecular Glues and PROTACs in targeted protein degradation:
Figure 1: Molecular Glues vs. PROTACs - Comparative Mechanisms in Targeted Protein Degradation
Quantitative Comparison and Characteristics
Structural and Functional Properties
Table 1: Comparative Analysis of Molecular Glues vs. PROTACs
| Characteristic | Molecular Glues | PROTACs |
|---|---|---|
| Molecular Structure | Monovalent, single pharmacophore | Heterobifunctional, two ligands connected by linker |
| Molecular Weight | Typically lower (<500 Da) | Typically higher (>700 Da) [9] |
| Rule of Five Compliance | Usually compliant | Often non-compliant due to size [9] |
| Mechanism of Action | Binds to E3 ligase or target, creating novel interaction surface | Simultaneously binds E3 ligase and target protein, inducing proximity [8] [9] |
| Degradation Specificity | Can degrade proteins without classical binding pockets | Requires accessible binding pocket on target protein [7] [9] |
| Design Approach | Often discovered serendipitously; rational design challenging | Rational design based on known ligands and linkers [9] |
| Cell Permeability | Generally good due to smaller size | Can be challenging due to larger molecular weight [9] |
| Catalytic Activity | Yes, can induce multiple degradation events | Yes, recycled after each degradation event [9] |
Performance Metrics of CIP Systems
Table 2: Quantitative Comparison of CIP Systems in Experimental Models
| CIP System | Ligand Structure | Time to Effect (t~0.75~) | Effective Concentration (EC~50~) | Interacting Fraction | Key Applications |
|---|---|---|---|---|---|
| Mandi System | Synthetic agrochemical | 10.1 ± 1.7 s (500 nM) [6] | 0.43 ± 0.17 µM [6] | 77 ± 12% [6] | Protein translocation, network shuttling, zebrafish embryos |
| Rapamycin System | Natural product with synthetic analogs | 107.9 ± 16.4 s (500 nM) [6] | Varies by analog | 71 ± 3% [6] | Signal transduction, transcription control, immunology |
| ABA System | Phytohormone (ABA-AM) | 3.5 ± 0.1 min (5 µM) [6] | 30.8 ± 15.5 µM [6] | 41 ± 6% [6] | Gene expression, stress response pathways |
| GA3 System | Phytohormone (GA3-AM) | 2.4 ± 0.5 min (5 µM) [6] | Not specified | Not specified | Plant biology, developmental studies |
Experimental Protocols and Applications
Protocol: Mandi-Induced Protein Translocation Assay
Purpose: To quantitatively measure Mandi-induced protein translocation kinetics in mammalian cells [6].
Materials:
- Mandi compound (commercially available synthetic agrochemical) [6]
- Plasmids: pPYR~Mandi~-TOM20 (receptor fused to mitochondrial outer membrane protein) and pABI-EGFP (cytosolic receiver fused to EGFP) [6]
- Cell line: HEK293T or other mammalian cell lines
- Imaging system: Automated epifluorescence microscope with environmental control and integrated liquid handling
- Analysis software: Image analysis platform with machine learning cell segmentation capabilities
Procedure:
- Cell preparation and transfection: Plate HEK293T cells in 96-well imaging plates at 50,000 cells/well. Transfect with both pPYR~Mandi~-TOM20 and pABI-EGFP using standard transfection reagents. Incubate for 24-48 hours to allow protein expression.
- Microscope setup: Configure automated microscope with temperature (37°C) and CO~2~ (5%) control. Set up time-lapse imaging with appropriate filter sets for EGFP and mitochondrial markers. Program liquid handling system for Mandi addition during imaging.
- Baseline imaging: Acquire images for 2 minutes to establish baseline localization of ABI-EGFP.
- Mandi addition: Add Mandi to final concentrations ranging from 10 nM to 5 µM while continuing time-lapse imaging. For kinetic comparisons with other CIPs, use 500 nM concentration.
- Image acquisition: Continue imaging for 15-30 minutes post-Mandi addition, capturing images every 5-10 seconds.
- Quantitative analysis: Use machine learning algorithms for automated cell segmentation and intensity measurement. Calculate translocation ratio as the fraction of ABI-EGFP signal colocalized with mitochondrial markers over time.
- Kinetic parameter extraction: Determine t~0.75~ values (time at which translocation reaches 75% of maximum) from translocation curves. Compare across different CIP systems and concentrations.
Troubleshooting: Optimize transfection efficiency if basal interaction is observed. Adjust Mandi concentration if translocation is too fast to resolve. Include controls with empty vector transfection to account for non-specific effects.
Protocol: PROTAC-Induced Protein Degradation Assessment
Purpose: To evaluate efficiency of PROTAC-mediated protein degradation in cellular models.
Materials:
- PROTAC molecules (heterobifunctional compounds with target protein ligand and E3 ligase recruiter)
- Cell lines expressing target protein of interest
- Western blot equipment or target-specific immunoassays
- Proteasome inhibitor (e.g., MG132) as control
- E3 ligase ligands (e.g., CRBN or VHL ligands depending on PROTAC design)
Procedure:
- Cell treatment: Seed appropriate cell lines in 6-well plates and allow to adhere overnight. Treat cells with varying concentrations of PROTAC (typically 1 nM to 10 µM) for different time points (4-24 hours).
- Control conditions: Include vehicle control, proteasome inhibitor control (MG132, 10 µM), and competition control with excess E3 ligase ligand.
- Sample collection: Harvest cells at designated time points and prepare lysates for protein quantification.
- Target protein detection: Perform Western blotting or specific immunoassays to quantify target protein levels. Normalize to loading controls (e.g., GAPDH, actin).
- Dose-response analysis: Calculate percentage degradation relative to vehicle control across different PROTAC concentrations.
- Ternary complex assessment: For mechanistic studies, employ techniques like cellular thermal shift assays or proximity ligation assays to confirm ternary complex formation.
- Functional consequences: Assess downstream biological effects of target degradation, such as pathway modulation or cell viability.
Applications: This protocol enables characterization of PROTAC efficiency, specificity, and kinetics, supporting optimization of degrader molecules for therapeutic development [7] [9].
Experimental Workflow Visualization
The following diagram illustrates a generalized experimental workflow for evaluating CIP systems:
Figure 2: Generalized Experimental Workflow for CIP System Evaluation
Research Reagent Solutions
Essential Research Tools for CIP Studies
Table 3: Key Research Reagents for CIP and Targeted Protein Degradation Studies
| Reagent Category | Specific Examples | Function/Application | Commercial Sources |
|---|---|---|---|
| CIP Molecules | Mandipropamid, Rapamycin, Abscisic Acid (ABA), Gibberellic Acid (GA3) | Induce proximity between engineered protein pairs; study kinetics of induced interactions [6] | Commercial chemical suppliers (e.g., Sigma-Aldrich, Tocris) |
| E3 Ubiquitin Ligases | Cereblon (CRBN), Von Hippel-Lindau (VHL), BIRC3, BIRC7, HERC4, WWP2 | Key components of ubiquitination machinery; recruited by PROTACs and molecular glues [9] | SignalChem Biotech, Sino Biological |
| PROTAC Components | Target protein ligands (e.g., AR binders, ER binders), E3 ligase ligands, Chemical linkers | Building blocks for PROTAC design and optimization; enable targeted degradation of specific proteins [9] | Custom synthesis, specialized chemical suppliers |
| Molecular Glue Compounds | Thalidomide, Lenalidomide, Pomalidomide, CC-90009, E7820 | Induce novel protein-protein interactions; redirect E3 ligase activity to non-native substrates [8] [9] | Pharmaceutical suppliers, chemical manufacturers |
| Detection Tools | Ubiquitination assays, Proteasome activity probes, Protein-protein interaction assays | Validate mechanism of action; confirm ternary complex formation and degradation efficiency | Life science suppliers (e.g., Promega, Abcam, Thermo Fisher) |
| Cell-Based Assays | Luciferase reporter systems, Split-TEV protease assays, Colocalization markers | Quantitative assessment of CIP efficiency; dose-response characterization [6] | Academic repositories, commercial assay developers |
Clinical Applications and Therapeutic Impact
Clinical Translation of CIP Technologies
The transition of CIP technologies from basic research to clinical applications represents a significant milestone in chemical biology and drug discovery. PROTACs have demonstrated remarkable progress in clinical development, with multiple candidates advancing through Phase I-III trials [9]. Bavdegalutamide (ARV-110), an androgen receptor-targeting PROTAC, has completed Phase II studies for prostate cancer, while Vepdegestrant (ARV-471), targeting the estrogen receptor for breast cancer, has advanced to NDA/BLA submission [9]. These clinical successes validate the CIP approach for targeting historically challenging proteins, including transcription factors that lack conventional enzymatic activity.
Molecular glue degraders have an established clinical track record, with drugs like thalidomide, lenalidomide, and pomalidomide approved for various hematological malignancies [9]. These immunomodulatory drugs (IMiDs) serendipitously discovered to function as molecular glues, have paved the way for deliberate development of glue-based therapeutics. Newer clinical-stage candidates include CC-90009 targeting GSPT1 and E7820 targeting RBM39, demonstrating expansion to novel target classes [9].
Clinical-Stage PROTACs
Table 4: Representative Clinical-Stage PROTACs in Development
| Molecule Name | Target Protein | E3 Ligase | Clinical Phase | Indication |
|---|---|---|---|---|
| ARV-471 (Vepdegestrant) | Estrogen Receptor (ER) | CRBN | NDA/BLA | ER+/HER2− breast cancer [9] |
| ARV-766 | Androgen Receptor (AR) | CRBN | Phase II | Prostate cancer [9] |
| ARV-110 (Bavdegalutamide) | Androgen Receptor (AR) | CRBN | Phase II | Prostate cancer [9] |
| DT-2216 | Bcl-XL | VHL | Phase I/II | Hematological malignancies [9] |
| NX-2127 | BTK | CRBN | Phase I | B-cell malignancies [9] |
| NX-5948 | BTK | CRBN | Phase I | B-cell malignancies [9] |
| CFT1946 | BRAF V600 | CRBN | Phase I | Melanoma with BRAF mutations [9] |
| KT-474 | IRAK4 | CRBN | Phase II | Auto-inflammatory diseases [9] |
Technical Challenges and Optimization Strategies
Addressing Limitations in CIP Implementation
Despite the considerable promise of CIP technologies, several technical challenges require careful consideration in experimental design and therapeutic development:
PROTAC-Specific Challenges: The relatively large molecular weight (>700 Da) of many PROTACs often places them outside the "Rule of Five" guidelines for drug-likeness, potentially leading to poor membrane permeability and suboptimal pharmacokinetic properties [9]. Optimization strategies include rational linker design incorporating rigid structures such as spirocycles or piperidines, which can significantly improve degradation potency and oral bioavailability [9]. Additionally, expanding the repertoire of E3 ligase ligands beyond the commonly used CRBN and VHL recruiters may enhance tissue specificity and reduce potential resistance mechanisms.
Molecular Glue Challenges: The discovery and rational design of molecular glues remain challenging due to the unpredictable nature of the protein-protein interactions they stabilize [9]. While serendipitous discovery has historically driven the field, emerging approaches include systematic screening of compound libraries and structure-based design leveraging structural biology insights. Recent strategies have shown promise in converting conventional inhibitors into degraders by adding covalent handles that promote interaction with E3 ligases [9].
General CIP Considerations: For all CIP systems, achieving optimal specificity and minimal off-target effects requires careful validation. Control experiments should include catalytically inactive versions, competition with excess ligand, and assessment of pathway modulation beyond the intended targets. The temporal control offered by CIP systems is a distinct advantage, but researchers must optimize timing and duration of induction to match biological contexts.
The field of Chemically Induced Proximity has revolutionized our approach to biological research and therapeutic development, providing unprecedented control over protein interactions and cellular processes. The lessons learned from PROTACs and Molecular Glues highlight both the immense potential and ongoing challenges in proximity-based technologies. As these approaches continue to evolve, several exciting directions are emerging: the integration of artificial intelligence and computational methods for rational degrader design; the expansion of E3 ligase toolbox beyond current standards; and the development of conditional and tissue-specific CIP systems for enhanced precision. The continuing translation of CIP technologies into clinical applications promises to expand the druggable proteome and create new therapeutic options for diseases previously considered untreatable. By applying the principles, protocols, and considerations outlined in these application notes, researchers can leverage the full potential of proximity-based approaches in their scientific and therapeutic endeavors.
The Core Concept of Proximity Search in Information Retrieval and Machine Learning
Proximity search refers to computational methods for quantifying the similarity, dissimilarity, or spatial relationship between entities within a dataset. In clinical interpretability research, these mechanisms enable researchers to identify patterns, cluster similar patient profiles, and elucidate decision-making processes of complex machine learning (ML) models. By measuring how "close" or "distant" data points are from one another in a defined feature space, proximity analysis provides a foundational framework for interpreting model behavior, validating clinical relevance, and ensuring that automated decisions align with established medical knowledge [10]. The translation of these technical proximity measures into clinically actionable insights remains a significant challenge, necessitating specialized application notes and protocols for drug development professionals and clinical researchers [11].
Foundational Concepts and Measures
Proximity measures vary significantly depending on data type and clinical application. The core principle involves converting clinical data into a representational space where distance metrics can quantify similarity.
Proximity Measures for Different Data Types
Table: Proximity Measures for Clinical Data Types
| Data Type | Common Proximity Measures | Clinical Application Examples | Key Considerations |
|---|---|---|---|
| Binary Attributes | Jaccard Similarity, Hamming Distance | Patient stratification based on symptom presence/absence; treatment outcome classification | Differentiate between symmetric and asymmetric attributes; pass/fail outcomes are typically asymmetric [12]. |
| Nominal Attributes | Simple Matching, Hamming Distance | Demographic pattern analysis; disease subtype categorization | Useful for categorical data without inherent order (e.g., race, blood type) [12]. |
| Ordinal Attributes | Manhattan Distance, Euclidean Distance | Severity staging (e.g., cancer stages); priority scoring | Requires rank-based distance calculation to preserve order relationships [12]. |
| Text Data | Cosine Similarity, Doc2Vec Embeddings | Patent text analysis for drug discovery; clinical note similarity | Captures semantic relationships beyond keyword matching; Doc2Vec outperforms frequency-based methods for document similarity [13]. |
| Geospatial Data | Haversine Formula, Euclidean Distance | Healthcare access studies; epidemic outbreak tracking | Requires specialized formulas for earth's curvature; often optimized with spatial indexing [14]. |
Technical Implementation of Binary Proximity Measures
For binary data commonly encountered in clinical applications (e.g., presence/absence of symptoms, positive/negative test results), asymmetric proximity calculations are particularly relevant. The dissimilarity between two patients m and n can be calculated using the following approach for asymmetric binary attributes:
Step 1: Construct a contingency table where:
a= number of attributes where both patients m and n have value 1 (e.g., both have the symptom)b= number of attributes where m=1 and n=0c= number of attributes where m=0 and n=1e= number of attributes where both m and n have value 0 (e.g., both lack the symptom)
Step 2: Apply the asymmetric dissimilarity formula:
dissimilarity = (b + c) / (a + b + c)
This approach excludes e (joint absences) from consideration, which is appropriate for many clinical contexts where mutual absence of a symptom may not indicate similarity [12].
Applications in Clinical Interpretability Research
Interpretable Machine Learning for Clinical Prediction
Recent research demonstrates how proximity-based interpretability methods can bridge the gap between complex ML models and clinical decision-making. In a comprehensive study on ICU mortality prediction, researchers developed and rigorously evaluated two ML models (Random Forest and XGBoost) using data from 131,051 ICU admissions across 208 hospitals. The random forest model demonstrated an AUROC of 0.912 with a complete dataset (130,810 patients, 5.58% ICU mortality) and 0.839 with a restricted dataset excluding patients with missing data (5,661 patients, 23.65% ICU mortality). The XGBoost model achieved an AUROC of 0.924 with the first dataset and 0.834 with the second. Through multiple interpretation mechanisms, the study consistently identified lactate levels, arterial pH, and body temperature as critical predictors of ICU mortality across datasets, cross-validation folds, and models. This alignment with routinely collected clinical variables enhances model interpretability for clinical use and promotes greater understanding and adoption among clinicians [11].
Evaluating Model Consistency with Clinical Protocols
A critical challenge in clinical ML is ensuring model predictions align with established medical protocols. Researchers have proposed specific metrics to assess both the accuracy of ML models relative to established protocols and the similarity between explanations provided by clinical rule-based systems and rules extracted from ML models. In one approach, researchers trained two neural networks—one exclusively on data, and another integrating a clinical protocol—on the Pima Indians Diabetes dataset. Results demonstrated that the integrated ML model achieved comparable performance to the fully data-driven model while exhibiting superior accuracy relative to the clinical protocol alone. Furthermore, the integrated model provided explanations for predictions that aligned more closely with the clinical protocol compared to the data-driven model, ensuring enhanced continuity of care [10].
Advanced Proximity Applications in Drug Development
Proximity-based methods are revolutionizing multiple aspects of drug development:
Patent Analysis and Innovation Tracking: Researchers have applied document vector representations (Doc2Vec) to patent abstracts followed by cosine similarity measurements to quantify proximity in "idea space." This approach revealed that patents within the same city show 0.02-0.05 standard deviations higher text similarity compared to patents from different cities, suggesting geographically constrained knowledge flows. This method provides an alternative to citation-based analysis of knowledge transfer in pharmaceutical innovation [13].
Genetic Disorder Classification: For complex genetic disorders like thalassemia, probabilistic state space models leverage the spatial ordering of genes along chromosomes to classify disease profiles from targeted next-generation sequencing data. One approach achieved a sensitivity of 0.99 and specificity of 0.93 for thalassemia detection, with 91.5% accuracy for characterizing subtypes. This spatial proximity-based method outperforms alternatives, particularly in specificity, and is broadly applicable to other genetic disorders [15].
Protein Representation Learning: Multimodal bidirectional hierarchical fusion frameworks effectively merge sequence representations from protein language models with structural features from graph neural networks. This approach employs attention and gating mechanisms to enable interaction between sequential and structural modalities, establishing new state-of-the-art performance on tasks including enzyme classification, model quality assessment, and protein-ligand binding affinity prediction [15].
Experimental Protocols
Protocol: Measuring Proximity in Clinical Text Data for Knowledge Discovery
Objective: Quantify similarity between clinical text documents (e.g., patent abstracts, clinical notes) to map knowledge relationships and innovation pathways.
Materials:
- Collection of text documents (e.g., patent abstracts from USPTO Bulk Data Products)
- Computational environment with Python and libraries (gensim, scikit-learn, numpy)
- Document metadata (e.g., location, time, technology classification)
Methodology:
- Text Preprocessing:
- Extract and clean relevant text (e.g., patent abstracts)
- Perform standard NLP preprocessing: tokenization, lowercasing, removal of stop words and punctuation
- Optionally apply stemming or lemmatization
Document Vectorization:
- Implement Document Vectors (Doc2Vec) with the following parameters:
- Vector size: 300 dimensions
- Window size: 5-10 words
- Minimum word count: 5-10
- Training epochs: 20-40
- Negative sampling: 5-25
- Train model on entire document corpus
- Implement Document Vectors (Doc2Vec) with the following parameters:
Similarity Calculation:
- Extract document vectors for all documents of interest
- Calculate pairwise cosine similarities between document vectors:
similarity = (A · B) / (||A|| ||B||)
- For localization studies, compare similarity distributions for:
- Documents from same geographic region (e.g., same city)
- Documents from different geographic regions
Statistical Analysis:
- Normalize similarity scores using z-score transformation
- Perform t-tests or ANOVA to compare similarity between groups
- Calculate effect sizes for significant differences
Validation:
- Confirm known relationships: documents sharing classes, citations, or inventors should have higher similarity
- Compare with alternative measures (e.g., term frequency-inverse document frequency)
- Assess robustness through cross-validation [13]
Protocol: Binary Proximity Analysis for Patient Stratification
Objective: Identify similar patient profiles based on binary clinical attributes (e.g., symptom presence, test results) for cohort identification and comparative effectiveness research.
Materials:
- Binary patient dataset (patients × attributes)
- Computational environment with standard statistical software
- Clinical expertise for attribute interpretation
Methodology:
- Data Preparation:
- Code all attributes as binary (0/1) values
- Determine attribute symmetry:
- Symmetric: Both presences (1,1) and absences (0,0) contribute equally to similarity
- Asymmetric: Only co-presences (1,1) indicate similarity; co-absences (0,0) are uninformative or excluded
Dissimilarity Matrix Calculation:
- For asymmetric binary attributes (most common in clinical applications):
- For each patient pair (i, j), calculate:
- a = number of attributes where both patients have 1
- b = number of attributes where i=1 and j=0
- c = number of attributes where i=0 and j=1
- e = number of attributes where both have 0
- Compute dissimilarity:
d(i,j) = (b + c) / (a + b + c)
- For each patient pair (i, j), calculate:
- For symmetric binary attributes:
- Use:
d(i,j) = (b + c) / (a + b + c + e)
- Use:
- For asymmetric binary attributes (most common in clinical applications):
Analysis and Interpretation:
- Construct dissimilarity matrix across all patient pairs
- Identify patient clusters using hierarchical clustering or similar methods
- Validate clusters with clinical outcomes or expert assessment
- Characterize clusters by their defining clinical features
Application Example: In a study of 57 individuals with thalassemia profiles, a probabilistic state space model leveraging spatial proximity along chromosomes achieved 91.5% accuracy for characterizing subtypes, rising to 93.9% when low-quality samples were excluded using automated quality control [15].
Protocol: Integrating Proximity Measures with Clinical Rules for Model Interpretability
Objective: Ensure ML model predictions align with clinical protocols and provide interpretable explanations consistent with medical knowledge.
Materials:
- Clinical dataset with outcomes
- Established clinical protocol or decision rules
- ML modeling environment (Python with scikit-learn, tensorflow/pytorch)
Methodology:
- Baseline Model Development:
- Train a standard data-driven ML model (e.g., neural network) using only patient data
- Evaluate performance using standard metrics (accuracy, AUROC)
Protocol-Integrated Model Development:
- Formalize clinical protocol as computable rules or constraints
- Integrate protocol knowledge during model training through:
- Custom loss functions that penalize protocol deviations
- Structured model architectures that encode protocol logic
- Multi-task learning that jointly predicts outcomes and protocol adherence
Explanation Similarity Assessment:
- Extract explanatory rules from both models (e.g., via rule extraction techniques)
- Extract rules from the clinical protocol
- Calculate explanation distance using:
- Rule syntax similarity (e.g., Jaccard similarity between condition sets)
- Semantic similarity (e.g., overlap in clinical concepts referenced)
- Outcome alignment (agreement in recommended actions)
Comprehensive Evaluation:
- Compare model performance metrics
- Assess protocol adherence on critical cases
- Measure explanation similarity between models and clinical protocol
- Evaluate clinical utility through expert review or simulated cases
Application: This approach has demonstrated that integrated models can achieve comparable performance to data-driven models while providing explanations that align more closely with clinical protocols, enhancing continuity of care and interpretability [10].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Computational Tools for Proximity Search in Clinical Research
| Tool/Category | Specific Examples | Function in Proximity Analysis | Implementation Considerations |
|---|---|---|---|
| Spatial Indexing Structures | R-trees, kd-trees, Geohashing | Enables efficient proximity search in large clinical datasets; essential for geospatial health studies | R-trees effective for multi-dimensional data; kd-trees suitable for fixed datasets; geohashing provides compact representation [14]. |
| Similarity Measurement Libraries | scikit-learn, gensim, NumPy | Provides implemented proximity measures (cosine, Jaccard, Euclidean) and embedding methods (Doc2Vec, Word2Vec) | Pre-optimized implementations ensure computational efficiency; gensim specializes in document embedding methods [13]. |
| Clinical Rule Formalization Tools | Clinical Quality Language (CQL), Rule-based ML frameworks | Encodes clinical protocols as computable rules for integration with ML models and explanation comparison | Requires collaboration between clinicians and data scientists; CQL provides standardized approach [10]. |
| Visualization Platforms | TensorBoard Projector, matplotlib, Plotly | Creates low-dimensional embeddings of high-dimensional clinical data for visual proximity assessment | Enables intuitive validation of proximity relationships; critical for interdisciplinary communication. |
| Optimization Services | Database spatial extensions (PostGIS), Search optimization services | Accelerates proximity queries in large clinical databases; essential for real-time applications | Reduces computational burden; PostgreSQL with PostGIS provides robust open-source solution [14]. |
| N-Desmethyl dosimertinib-d5 | N-Desmethyl Dosimertinib-d5 | Deuterium-labeled EGFR inhibitor for NSCLC research. N-Desmethyl Dosimertinib-d5 is for research use only. Not for human consumption. | Bench Chemicals |
| hDHODH-IN-8 | hDHODH-IN-8, MF:C21H15F6N3O4, MW:487.4 g/mol | Chemical Reagent | Bench Chemicals |
Proximity search mechanisms provide fundamental methodologies for enhancing interpretability in clinical machine learning applications. By quantifying similarities between patient profiles, clinical texts, and molecular structures, these approaches enable more transparent and clinically aligned AI systems. The experimental protocols and application notes presented here offer researchers and drug development professionals practical frameworks for implementing these techniques across diverse healthcare contexts. As the field advances, further integration of proximity-based interpretability methods into clinical workflow
Why Interpretability is Non-Negotiable in Clinical Decision-Making and Drug Development
In clinical decision-making and drug development, machine learning (ML) and artificial intelligence (AI) models are being deployed for high-stakes predictions including disease diagnosis, treatment selection, and patient risk stratification [16] [17]. While these models can outperform traditional statistical approaches by characterizing complex, nonlinear relationships, their adoption is critically dependent on interpretability—the ability to understand the reasoning behind a model's predictions [16] [18]. In contrast to "black box" models whose internal workings are opaque, interpretable models provide insights that are essential for building trust, ensuring safety, facilitating regulatory compliance, and ultimately, improving human decision-making [16] [19] [18].
The U.S. Government's Blueprint for an AI Bill of Rights and guidelines from the U.S. Food and Drug Administration (FDA) explicitly emphasize the principle of "Notice and Explanation," making interpretability a regulatory expectation and a prerequisite for the ethical deployment of AI in healthcare [16]. This document outlines the application of interpretable ML frameworks, provides experimental protocols for model interpretation, and situates these advancements within a novel research context: the use of proximity search mechanisms to enhance clinical interpretability.
Core Concepts and Definitions
Within the AI in healthcare landscape, key terms are defined with specific nuances [19] [18]:
- Transparency involves the disclosure of an AI system's data sources, development processes, limitations, and operational use. It answers the question, "What happened?" by making appropriate information available to relevant stakeholders [19].
- Explainability is a representation of the mechanisms underlying an AI system's operation. It answers the question, "How was the decision made?" by expressing the important factors that influenced the results in a way humans can understand [19] [18].
- Interpretability goes a step further, enabling humans to grasp the causal connections within a model and its outputs. It answers the question, "Why should I trust this prediction?" allowing a user to consistently predict the model's behavior [16] [18].
Applications and Quantitative Evidence
Interpretability is not a theoretical concern but a practical necessity across the clinical and pharmaceutical R&D spectrum. The table below summarizes evidence of its application and impact.
Table 1: Documented Applications and Performance of Interpretable ML in Healthcare
| Application Domain | Interpretability Method | Quantitative Performance / Impact | Key Interpretability Insight |
|---|---|---|---|
| Disease Prediction (Cardiovascular, Cancer) | Random Forest, Support Vector Machines [17] | AUC of 0.85 (95% CI 0.81-0.89) for cardiovascular prediction; 83% accuracy for cancer prognosis [17] | Identifies key risk factors (e.g., blood pressure, genetic markers) from real-world data [17]. |
| Medical Visual Question Answering (GI Endoscopy) | Multimodal Explanations (Heatmaps, Text) [20] | Evaluated via BLEU, ROUGE, METEOR scores and expert-rated clinical relevance [20] | Heatmaps localize pathological features; textual reasoning aligns with clinical logic, building radiologist trust [20]. |
| Psychosomatic Disease Analysis | Knowledge Graph with Proximity Metrics [21] | Graph constructed with 9668 triples; closer network distances predicted similarity in clinical manifestations [21] | Proximity between diseases and symptoms reveals potential comorbidity and shared treatment pathways [21]. |
| Drug Discovery: Hit-to-Lead | AI-Guided Retrosynthesis & Scaffold Enumeration [22] | Generated >26,000 virtual analogs, yielding sub-nanomolar inhibitors with 4,500-fold potency improvement [22] | Interpretation of structure-activity relationships (SAR) guides rational chemical optimization [22]. |
| Target Engagement Validation | Cellular Thermal Shift Assay (CETSA) [22] | Quantified dose-dependent target (DPP9) engagement in rat tissue, confirming cellular efficacy [22] | Provides direct, empirical evidence of mechanistic drug action beyond in-silico prediction. |
Experimental Protocols for Model Interpretation
Protocol: Global Feature Importance using Permutation
Objective: To rank all input variables (features) by their average importance to a model's predictive accuracy across an entire population or dataset [16]. Materials: A trained ML model, a held-out test dataset. Procedure:
- Calculate the model's baseline performance (e.g., accuracy, AUC) on the test set.
- For each feature (e.g.,
blood_pressure,genetic_marker_X): a. Randomly shuffle the values of that feature across the test set, breaking its relationship with the outcome. b. Recalculate the model's performance using this permuted dataset. c. Record the decrease in performance (e.g., baseline AUC - permuted AUC). - The average performance decrease for each feature, normalized across all features, represents its global importance.
- Features causing the largest performance drop when shuffled are deemed most critical. Interpretation: This model-agnostic method reveals which factors the model relies on most for its average prediction, useful for hypothesis generation and model auditing [16].
Protocol: Local Explanation using LIME (Local Interpretable Model-agnostic Explanations)
Objective: To explain the prediction for a single, specific instance (e.g., one patient) by approximating the complex model locally with an interpretable one [18]. Materials: A trained "black box" model, a single data instance to explain. Procedure:
- Select the patient of interest and obtain the model's prediction for them.
- Generate a perturbed dataset by creating slight variations of this patient's data.
- Get predictions from the complex model for each of these perturbed instances.
- Fit a simple, interpretable model (e.g., linear regression with Lasso) to this new dataset, weighting instances by their proximity to the original patient.
- The coefficients of the simple model serve as the local explanation. Interpretation: LIME answers, "For this specific patient, which factors were the primary drivers of their high-risk prediction?" This aligns with clinical reasoning for individual cases [18].
Protocol: Knowledge Graph Construction and Proximity Analysis
Objective: To structure clinical entities and their relationships into a network, and use proximity metrics to uncover novel connections for diagnosis and treatment [21]. Materials: Unstructured clinical text, medical ontologies, LLMs (e.g., BERT), graph database. Procedure:
- Entity Recognition: Use a fine-tuned LLM to perform Named Entity Recognition (NER) on clinical text to extract entities (e.g., diseases, symptoms, drugs) [21].
- Relationship Extraction: Identify and define relationships between entities (e.g.,
Disease-Amanifests_withSymptom-B,Drug-CtreatsDisease-A) to form subject-predicate-object triples [21]. - Graph Construction: Assemble the triples into a knowledge graph where nodes are entities and edges are relationships.
- Proximity Search: Calculate network-based proximity scores (e.g., shortest path distance, random walk with restart) between any two nodes (e.g., two diseases, a drug and a symptom) [21]. Interpretation: Closer proximity between diseases can predict similarities in their clinical manifestations and treatment approaches, providing a novel, interpretable perspective on disease relationships [21].
The Scientist's Toolkit: Essential Research Reagents & Platforms
Table 2: Key Tools and Platforms for Interpretable AI Research
| Item / Platform | Primary Function | Relevance to Interpretability |
|---|---|---|
| SHAP (Shapley Additive exPlanations) | Unified framework for feature attribution | Quantifies the marginal contribution of each feature to an individual prediction, based on game theory [18]. |
| LIME (Local Interpretable Model-agnostic Explanations) | Local surrogate model explanation | Approximates a complex model locally to provide instance-specific feature importance [18]. |
| Grad-CAM | Visual explanation for convolutional networks | Generates heatmaps on images (e.g., X-rays) to highlight regions most influential to the model's decision [18]. |
| CETSA (Cellular Thermal Shift Assay) | Target engagement validation in cells/tissues | Provides empirical, interpretable data on whether a drug candidate engages its intended target in a biologically relevant system [22]. |
| DALEX & lime R/Python Packages | Model-agnostic explanation software | Provides comprehensive suites for building, validating, and explaining ML models [16]. |
| Knowledge Graph Databases (e.g., Neo4j) | Network-based data storage and querying | Enables proximity analysis and relationship mining between clinical entities for hypothesis generation [21]. |
| C6 NBD Phytoceramide | C6 NBD Phytoceramide, MF:C30H51N5O7, MW:593.8 g/mol | Chemical Reagent |
| InhA-IN-4 | InhA-IN-4, MF:C14H12BrN3O2S, MW:366.23 g/mol | Chemical Reagent |
Visualizing Workflows for Interpretability
Workflow for Proximity-Based Clinical Interpretability Research
Diagram 1: Proximity-Based Clinical Insight Workflow
Multimodal Explanation for Medical VQA
Diagram 2: Multimodal Explainable VQA Framework
Application Note: Proximity Concepts in Clinical Research
Core Principles and Definitions
The concept of proximity—the physical closeness of molecules or computational elements—serves as a foundational regulatory mechanism across biological systems and computational networks. In clinical interpretability research, proximity-based analysis provides a unified framework for understanding complex systems, from protein interactions within cells to decision-making processes within neural networks. Chemically Induced Proximity (CIP) represents a deliberate intervention strategy using synthetic molecules to recruit neosubstrates that are not normally encountered or to enhance the affinity of naturally occurring interactions [23]. This approach has revolutionized both biological research and therapeutic development by enabling precise temporal control over cellular processes.
The fundamental hypothesis underlying proximity-based analysis is that effective interactions require physical closeness. In biological systems, reaction rates scale with concentration, which inversely correlates with the mean interparticle distance between molecules [24]. Similarly, in computational systems, mechanistic interpretability research investigates how neural networks develop shared computational mechanisms that generalize across problems, focusing on the functional "closeness" of processing elements that work together to solve specific tasks [25]. This parallel enables researchers to apply similar analytical frameworks to both domains, creating opportunities for cross-disciplinary methodological exchange.
Quantitative Foundations of Proximity Effects
The quantitative relationship between proximity and interaction efficacy follows well-established physical principles. The probability of an effective collision between two molecules is a third-order function of distance, allowing steep concentration gradients to produce qualitative changes in system behavior [24]. This mathematical foundation enables researchers to predict and model the effects of proximity perturbations in both biological and computational systems.
Table 1: Key Proximity Metrics Across Biological and Computational Domains
| Domain | Proximity Metric | Calculation Method | Interpretation |
|---|---|---|---|
| Biological Networks | Drug-Disease Proximity (z-score) | ( z = (dc - μ)/σ ) where ( dc ) = average shortest path between drug targets and disease proteins [26] [27] | z ≤ -2.0 indicates significant therapeutic potential [27] |
| Computational Networks | Component Proximity in Circuits | Analysis of attention patterns and activation pathways across model layers [25] | Identifies functionally related processing units |
| Experimental Biology | Chemically Induced Proximity Efficacy | Effective molarity and ternary complex stability measurements [28] [24] | Predicts functional consequences of induced interactions |
Experimental Protocols
Protocol 1: Network Proximity Analysis for Drug Repurposing
Purpose and Scope
Network Proximity Analysis (NPA) provides an unsupervised computational method to identify novel therapeutic applications for existing drugs by quantifying the network-based relationship between drug targets and disease proteins [26] [27]. This protocol details the steps for implementing NPA to identify candidate therapies for diseases with known genetic associations, enabling drug repurposing opportunities.
Materials and Reagents
- Computational Resources: Python environment with NetworkX or similar graph analysis libraries
- Data Sources:
- Human interactome data (protein-protein interaction network)
- Drug-target associations from DrugBank
- Disease-gene associations from GWAS catalog and OMIM
- Reference Implementation: Validated Python code from Guney et al. [27]
Procedure
Disease Gene Identification: Compile a list of genes significantly associated with the target disease through systematic literature review and database mining. Include only genes meeting genome-wide significance thresholds (p < 5 × 10â»â¸) [27].
Interactome Preparation: Assemble a comprehensive human protein-protein interaction network, incorporating data from validated experimental sources. The interactome should include approximately 13,329 proteins and 141,150 interactions for sufficient coverage [26].
Drug Target Mapping: For each drug candidate, identify its known protein targets within the interactome. Average number of targets per drug is approximately 3.5, with targets typically having higher-than-average network connectivity (degree = 28.6 vs. interactome average 21.2) [26].
Proximity Calculation:
- Calculate ( d_c ), the average shortest path length between each drug target and its nearest disease protein in the interactome
- Compute the relative proximity z-score using ( z = (d_c - μ)/σ ), where μ and σ represent the mean and standard deviation of distances from randomly selected protein sets
- Apply a z-score threshold of ≤ -2.0 to identify statistically significant drug-disease pairs [27]
Validation and Prioritization: Cross-reference significant results with known drug indications to validate methodology, then prioritize novel candidates based on z-score magnitude and clinical feasibility.
Expected Results and Interpretation
Application of this protocol to Primary Sclerosing Cholangitis (PSC) identified 42 medicinal products with z ≤ -2.0, including immune modulators such as basiliximab (z = -5.038) and abatacept (z = -3.787) as promising repurposing candidates [27]. The strong performance of this method is demonstrated by its ability to correctly identify metronidazole, the only previously researched agent for PSC that also showed significant proximity (z ≤ -2.0) [27].
Protocol 2: Development and Validation of Bio-Inspired Diagnostic Optimization
Purpose and Scope
This protocol describes the implementation of a hybrid diagnostic framework combining multilayer feedforward neural networks with nature-inspired optimization algorithms to enhance predictive accuracy in clinical diagnostics, specifically applied to male fertility assessment [29].
Materials and Reagents
- Clinical Dataset: 100 clinically profiled male fertility cases representing diverse lifestyle and environmental risk factors [29]
- Computational Framework:
- Multilayer feedforward neural network architecture
- Ant colony optimization (ACO) algorithm with adaptive parameter tuning
- Proximity search mechanism for feature selection
Procedure
Data Preparation and Feature Engineering:
- Collect comprehensive clinical profiles including sedentary habits, environmental exposures, and psychosocial stress factors
- Normalize continuous variables and encode categorical variables
- Partition data into training (70%), validation (15%), and test (15%) sets
Hybrid Model Implementation:
- Initialize feedforward neural network with one input layer, two hidden layers, and one output layer
- Integrate ant colony optimization for adaptive parameter tuning, mimicking ant foraging behavior to navigate parameter space
- Implement proximity search mechanism to identify optimal feature combinations
Model Training and Optimization:
- Train neural network using gradient descent with ACO-enhanced optimization
- Employ proximity-based feature importance analysis to identify key contributory factors
- Validate model generalizability using k-fold cross-validation
Performance Assessment:
- Evaluate classification accuracy, sensitivity, and specificity on unseen test samples
- Measure computational efficiency through inference time
- Assess clinical interpretability via feature importance rankings
Expected Results and Interpretation
Implementation of this protocol for male fertility diagnostics achieved 99% classification accuracy, 100% sensitivity, and an ultra-low computational time of 0.00006 seconds, demonstrating both high performance and real-time applicability [29]. Feature importance analysis highlighted key risk factors including sedentary habits and environmental exposures, providing clinically actionable insights [29].
Protocol 3: Targeted Protein Degradation Using PROTAC Technology
Purpose and Scope
PROteolysis TArgeting Chimeras (PROTACs) represent a leading proximity-based therapeutic modality that induces targeted protein degradation by recruiting E3 ubiquitin ligases to target proteins [28] [23]. This protocol details the design, synthesis, and validation of PROTAC molecules for targeted protein degradation.
Materials and Reagents
- Ligand Components: Target protein-binding ligand, E3 ligase-recruiting ligand
- Linker Chemistry: Flexible chemical spacers of varying length and composition
- Cell Lines: Appropriate cellular models expressing target protein and E3 ligase machinery
- Analytical Tools: Western blot equipment, quantitative PCR, cellular viability assays
Procedure
PROTAC Design:
- Select target-binding ligand with demonstrated affinity for protein of interest
- Choose E3 ligase ligand based on tissue distribution and compatibility (common choices: VHL, CRBN, IAP ligands)
- Design linker composition and length to optimize ternary complex formation
Synthesis and Characterization:
- Synthesize PROTAC molecules using modular conjugation chemistry
- Confirm molecular identity and purity through LC-MS and NMR
- Assess membrane permeability and physicochemical properties
Cellular Efficacy Assessment:
- Treat cells with PROTAC molecules across concentration gradient (typically 0.1 nM - 10 μM)
- Measure target protein degradation via western blot at multiple time points (2-24 hours)
- Assess downstream functional consequences through relevant phenotypic assays
Mechanistic Validation:
- Confirm ubiquitin-proteasome system dependence using proteasome inhibitors (e.g., MG132)
- Verify E3 ligase requirement through CRISPR knockout or dominant-negative approaches
- Demonstrate ternary complex formation using techniques such as co-immunoprecipitation or proximity assays
Expected Results and Interpretation
Successful PROTAC molecules typically demonstrate DCâ‚…â‚€ values in low nanomolar range and maximum degradation (Dmax) >80% within 4-8 hours of treatment [28]. The catalytic nature of PROTACs enables sub-stoichiometric activity, and the induced proximity mechanism can address both enzymatic and scaffolding functions of target proteins [28]. Currently, approximately 26 PROTAC degraders are advancing through clinical trials, validating this proximity-based approach as a transformative therapeutic strategy [28].
Visualization of Proximity Mechanisms
PROTAC Mechanism Diagram
Network Proximity Analysis Workflow
Hybrid Diagnostic Optimization Framework
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for Proximity-Based Investigations
| Reagent/Technology | Category | Function and Application | Key Characteristics |
|---|---|---|---|
| PROTAC Molecules | Bifunctional Degraders | Induce target protein degradation via E3 ligase recruitment [28] [23] | Modular design; catalytic activity; sub-stoichiometric efficacy |
| Molecular Glues | Monomeric Degraders | Enhance naturally occurring or create novel E3 ligase-target interactions [28] | Lower molecular weight; drug-like properties; serendipitous discovery |
| Network Proximity Analysis Code | Computational Tool | Quantifies drug-disease proximity in protein interactome [26] [27] | Python implementation; z-score output; validated thresholds |
| Ant Colony Optimization | Bio-inspired Algorithm | Adaptive parameter tuning through simulated foraging behavior [29] | Nature-inspired; efficient navigation of complex parameter spaces |
| Chemical Inducers of Proximity (CIPs) | Synthetic Biology Tools | Enable precise temporal control of cellular processes [5] [24] | Rapamycin-based systems; rapid reversibility; precise temporal control |
| Cox-2-IN-13 | Cox-2-IN-13, MF:C19H18N2O5S, MW:386.4 g/mol | Chemical Reagent | Bench Chemicals |
| S1P5 receptor agonist-1 | S1P5 Receptor Agonist-1|Selective S1P5 Agonist|RUO | Bench Chemicals |
The integration of proximity concepts across biological and computational domains provides a powerful unifying framework for clinical interpretability research. The experimental protocols and analytical methods detailed in this document enable researchers to leverage proximity-based approaches for therapeutic discovery, diagnostic optimization, and mechanistic investigation. As the field advances, emerging opportunities include the development of more sophisticated proximity-based modalities, enhanced computational methods for analyzing proximity networks, and novel clinical applications across diverse disease areas. The continued convergence of biological and computational proximity research promises to accelerate the development of interpretable, effective clinical interventions.
Building Transparent Clinical AI: Proximity-Based Methods and Applications
Theoretical Foundation & Mechanism
This protocol details the implementation of a proximity-based evidence retrieval mechanism designed to enhance the interpretability and reliability of uncertainty-aware decision-making in clinical research. The core innovation replaces a single, global decision cutoff with an instance-adaptive, evidence-conditioned criterion [30]. For each test instance (e.g., a new patient's clinical data), proximal exemplars are retrieved from an embedding space. The predictive distributions of these exemplars are fused using Dempster-Shafer theory, resulting in a fused belief that serves as a transparent, per-instance thresholding mechanism [30]. This approach materially reduces confidently incorrect outcomes and provides an auditable trail of supporting evidence, which is critical for clinical applications [30].
Application Protocol: Clinical Evidence Retrieval Workflow
Objective: To retrieve and fuse evidence from similar clinical cases to support a diagnostic or treatment decision for a new patient, providing a quantifiable measure of uncertainty.
Materials:
- Clinical Dataset: A structured database of historical patient records, including features (e.g., lab results, imaging features, demographics) and outcomes.
- Embedding Model: A pre-trained model (e.g., BiT, ViT, or a clinical NLP model) to project patient records into a numerical embedding space [30].
- Similarity Metric: A function (e.g., cosine similarity, Euclidean distance) to calculate proximity between patient records in the embedding space.
- Evidence Retrieval System: Computational framework to perform nearest-neighbor search.
Procedure:
- Query Instance Encoding: For a new patient (the "query instance"), encode their clinical data into a feature vector using the embedding model.
- Proximity Search: Execute a k-Nearest Neighbors (k-NN) search within the historical dataset to identify the
kmost proximal exemplars to the query instance. The distance metric defines the proximity constraint [31] [32]. - Evidence Extraction: Extract the known outcomes or predictive distributions associated with each of the
kretrieved exemplars. - Evidence Fusion: Fuse the predictive distributions of the retrieved exemplars using Dempster-Shafer theory to generate a combined belief and plausibility measure for each possible outcome [30].
- Uncertainty-Aware Decision:
- The fused belief is used as an adaptive confidence threshold.
- If the belief for a particular outcome exceeds a pre-defined operational minimum (e.g., 0.85), the decision is made with high confidence.
- If no outcome's belief meets the threshold, the case is flagged for manual review by a clinical expert, thus managing uncertainty sustainably [30].
Performance Data & Validation
Experimental validation on benchmark datasets demonstrates the efficacy of the proximity-based retrieval model compared to advanced baselines. The following tables summarize key quantitative findings.
Table 1: Model Performance Comparison on Clinical Retrieval Tasks
| Model | MAP (Mean Average Precision) | F1 Score | Key Feature |
|---|---|---|---|
| HRoc_AP (Proximity-Based) | 0.085 (improvement over PRoc2) | 0.0786 (improvement over PRoc2) | Adaptive term proximity feedback, self-adaptive window size [33] |
| PRoc2 | Baseline | Baseline | Traditional pseudo-relevance feedback [33] |
| TF-PRF | -0.1224 (vs. HRoc_AP MAP) | -0.0988 (vs. HRoc_AP F1) | Term frequency-based feedback [33] |
Table 2: Uncertainty-Aware Performance on CIFAR-10/100
| Model / Method | Confidently Incorrect Outcomes (%) | Review Load | Interpretability |
|---|---|---|---|
| Proximity-Based Evidence Retrieval | Materially Fewer | Sustainable | High (Explicit evidence) [30] |
| Threshold on Prediction Entropy | Higher | Less Controlled | Low (Black-box) [30] |
Workflow & System Visualization
The following diagram illustrates the logical workflow and data flow of the proximity-based evidence retrieval system.
Proximity-Based Clinical Evidence Retrieval Workflow
Research Reagent Solutions
Table 3: Essential Materials for Proximity-Based Clinical Retrieval Research
| Item | Function / Description | Example / Specification |
|---|---|---|
| TREC Clinical Datasets | Standardized corpora for benchmarking clinical information retrieval systems. | TREC 2016/2017 Clinical Support Track datasets [33]. |
| Pre-trained Embedding Models | Converts clinical text (e.g., EHR notes) or structured data into numerical vectors. | BiT (ResNet), ViT, or domain-specific clinical BERT models [30]. |
| Similarity Search Library | Software for efficient high-dimensional nearest-neighbor search. | FAISS (Facebook AI Similarity Search), Annoy, or Scikit-learn's NearestNeighbors. |
| Dempster-Shafer Theory Library | Implements the evidence fusion logic to combine predictive distributions. | Custom implementations or probabilistic programming libraries (e.g., PyMC3, NumPy). |
| Proximity Operator (N/W) | Defines the proximity constraint for retrieving relevant evidence. | N/5 finds terms within 5 words, in any order; W/3 finds terms within 3 words, in exact order [2] [32]. |
The integration of artificial intelligence in clinical diagnostics faces a significant challenge: the trade-off between model performance and interpretability. This is particularly critical in cardiology, where ventricular tachycardia (VT)—a life-threatening arrhythmia that can degenerate into ventricular fibrillation and sudden cardiac death—demands both high diagnostic accuracy and clear, actionable insights for clinicians [34]. Proximity-informed models present a promising pathway to bridge this gap. These models leverage geometric relationships and neighborhood information within data to make predictions that are not only accurate but also inherently easier to interpret and justify clinically. This document details the application of these models for VT diagnosis, framing the methodology within the broader thesis that proximity search mechanisms are fundamental to advancing clinical interpretability research.
Quantitative Performance of Diagnostic Models for Ventricular Tachycardia
Recent research demonstrates the potential of advanced computational models to achieve high performance in detecting and classifying cardiac arrhythmias. The following table summarizes key quantitative findings from recent studies, which serve as benchmarks for proximity-informed model development.
Table 1: Performance Metrics of Recent Computational Models for Arrhythmia Detection
| Model / Approach | Application Focus | Key Performance Metrics | Reference |
|---|---|---|---|
| Topological Data Analysis (TDA) with k-NN | VF/VT Detection & Shock Advice | 99.51% Accuracy, 99.03% Sensitivity, 99.67% Specificity in discriminating shockable (VT/VF) vs. non-shockable rhythms. | [35] |
| TDA with k-NN (Four-way Classification) | Rhythm Discrimination (VF, VT, Normal, Other) | Average Accuracy: ~99% (98.68% VF, 99.05% VT, 98.76% normal sinus, 99.09% Other). Specificity >97.16% for all classes. | [35] |
| Bio-inspired Hybrid Framework (Ant Colony Optimization + Neural Network) | Male Fertility Diagnostics (Conceptual parallel for diagnostic precision) | 99% Classification Accuracy, 100% Sensitivity, Computational Time: 0.00006 seconds. | [29] |
| Genotype-specific Heart Digital Twin (Geno-DT) | Predicting VT Circuits in ARVC Patients | GE Group: 100% Sensitivity, 94% Specificity, 96% Accuracy.PKP2 Group: 86% Sensitivity, 90% Specificity, 89% Accuracy. | [36] |
These results highlight the potential for machine learning and computational modeling to achieve high precision in VT diagnostics. The TDA approach, which explicitly analyzes the "shape" of ECG data, is a prime example of a proximity-informed method that yields both high accuracy and a geometrically-grounded interpretation of the signal [35].
Protocol for Implementing a Proximity-Informed VT Diagnostic System
This protocol outlines the steps for developing and validating a diagnostic model for VT using proximity-based methods, such as Topological Data Analysis.
Data Acquisition and Preprocessing
Objective: To gather and prepare a standardized electrocardiographic (ECG) dataset for topological analysis. Materials: Publicly available ECG databases (e.g., MIT-BIH Arrhythmia Database, AHA Database), computing environment (e.g., MATLAB, Python). Procedure:
- Data Source Identification: Obtain ECG recordings from standard databases such as MIT-BIH and AHA [35].
- Rhythm Labeling: Curate data segments with confirmed annotations for the following rhythms:
- Ventricular Tachycardia (VT)
- Ventricular Fibrillation (VF)
- Normal Sinus Rhythm
- Other Supraventricular Arrhythmias (e.g., SVT with aberrancy)
- Signal Preprocessing: Apply band-pass filtering (e.g., 0.5-40 Hz) to remove baseline wander and high-frequency noise.
- Data Segmentation: Extract contiguous 5-10 second episodes of each rhythm for analysis. Do not perform episode preselection to ensure robust model generalizability [35].
Topological Feature Extraction Using Persistent Homology
Objective: To convert the time-series ECG data into a topological point cloud and extract multi-scale geometric features. Materials: TDA software libraries (e.g., GUDHI, Ripser), Python/R programming environment. Procedure:
- Point Cloud Construction: Transform the preprocessed ECG time series into a point cloud in a high-dimensional space using Takens's Delay Embedding Theorem [35]. This technique reconstructs the phase space dynamics of the underlying cardiac system.
- Vietoris-Rips Filtration: Construct a simplicial complex from the point cloud by growing epsilon (
ϵ)-balls around each point and connecting points whose balls intersect. Systematically increase the radiusϵfrom zero to a maximum value. - Persistence Diagram Generation: For each value of
ϵ, compute the homological features (e.g., connected components, loops, voids) of the simplicial complex. Track the "birth" and "death" radii of these features. Plot these (ϵ_birth,ϵ_death) pairs to create a persistence diagram, which encapsulates the multi-scale topological signature of the ECG episode [35]. - Feature Vectorization: Convert the persistence diagram into a fixed-length feature vector suitable for machine learning classifiers. This can be achieved by:
- Calculating summary statistics from the diagram (e.g., persistence entropy, total number of features).
- Using persistence images, which are vectorized representations of the diagram [35].
Model Training and Validation
Objective: To train a classifier using the topological features to discriminate VT from other rhythms. Materials: Machine learning libraries (e.g., scikit-learn). Procedure:
- Classifier Selection: Employ a k-Nearest Neighbors (k-NN) classifier. The k-NN algorithm is a quintessential proximity-based method that classifies a new sample based on the majority class of its 'k' nearest neighbors in the feature space, making its decision process transparent and directly tied to data proximity [35].
- Model Training: Train the k-NN model using the topological feature vectors derived from the training set of ECG episodes.
- Performance Evaluation: Validate the model on a held-out test set. Report standard metrics including accuracy, sensitivity, specificity, and area under the receiver operating characteristic curve (AUROC). Compare performance against traditional ECG analysis methods.
Diagram 1: TDA-based VT diagnosis workflow.
The Scientist's Toolkit: Research Reagent Solutions
The following table lists key computational and data resources essential for research in proximity-informed VT diagnostics.
Table 2: Essential Research Tools for Proximity-Informed VT Modeling
| Tool / Resource | Type | Function in Research | Exemplar Use Case |
|---|---|---|---|
| MIT-BIH & AHA Databases | Data | Provides standardized, annotated ECG recordings for model training and benchmarking. | Used as the primary source of ECG episodes for evaluating TDA features [35]. |
| GUDHI / Ripser | Software Library | Open-source libraries for performing Topological Data Analysis and computing persistent homology. | Used to implement the Vietoris-Rips filtration and generate persistence diagrams from ECG point clouds [35]. |
| k-Nearest Neighbors (k-NN) | Algorithm | A simple, interpretable classifier that bases decisions on local data proximity. | Classifies ECG rhythms based on topological features; its decisions are explainable by identifying nearest neighbors in the training set [35]. |
| Heart Digital Twin (Geno-DT) | Computational Model | Patient-specific simulation that integrates structural imaging and genotype-specific electrophysiology. | Predicts locations of VT circuits in patients with ARVC by modeling the proximity and interaction of scar tissue and altered conduction [36]. |
| Clinical Guidelines (e.g., ESC) | Knowledge Base | Encodes expert-derived diagnostic and treatment protocols for formalization into computer-interpretable rules. | Serves as the source for knowledge acquisition in rule-based CDSS or for validating model outputs [37] [38]. |
| Terconazole-d4 | Terconazole-d4, MF:C26H31Cl2N5O3, MW:536.5 g/mol | Chemical Reagent | Bench Chemicals |
| Dabigatran-d4 | Dabigatran-d4, MF:C25H25N7O3, MW:475.5 g/mol | Chemical Reagent | Bench Chemicals |
Experimental Validation and Clinical Translation Protocol
Validating Against Clinical Standards
Objective: To ensure the model's predictions are clinically relevant and align with established diagnostic criteria. Materials: 12-lead ECG recordings, expert cardiologist annotations, clinical history. Procedure:
- Algorithm Comparison: Test the proximity-informed model on a dataset of Wide Complex Tachycardias (WCTs) and compare its diagnostic output against established ECG criteria (e.g., Brugada algorithm, Vereckei algorithm) [39].
- Expert Correlation: Conduct a blinded review where the model's output and its explanation (e.g., the closest matching cases from the training set) are presented to cardiologists. Assess the level of agreement between the model's reasoning and clinical intuition [37].
- Feature Importance Analysis: Conduct an analysis to determine which topological features contribute most to the classification. Correlate these features with known clinical markers of VT, such as AV dissociation, QRS width, and specific QRS morphologies, to ground the model's predictions in clinically understood phenomena [29] [34].
Integration into a Clinical Decision Support System (CDSS)
Objective: To frame the proximity-informed model within a usable CDSS that addresses documented clinical needs. Materials: CDSS framework, user interface design tools, electronic health record (EHR) system integration capabilities. Procedure:
- Requirements Analysis: Base the CDSS design on identified clinical gaps. A recent study found that 68% of cardiologists self-reported deficiencies in knowledge for VT diagnostic evaluation, and 60.7% expressed a need for CDSS support [37].
- Interpretable Output Design: The CDSS interface should present:
- The primary diagnosis (e.g., "Ventricular Tachycardia").
- A confidence score.
- Proximity-based justification: Display the most similar ECG cases from the knowledge base that led to the diagnosis, allowing the clinician to verify the reasoning.
- Key contributing ECG features highlighted in the context of clinical guidelines [40] [38].
- Workflow Integration: Design the system to function as an assistive tool, providing situation-specific knowledge without disrupting the clinical workflow. It should support, not replace, clinician judgment [37].
Diagram 2: Proximity-based CDSS rationale.
The application of proximity-informed models, exemplified by Topological Data Analysis and k-NN classifiers, offers a robust framework for achieving high diagnostic accuracy in Ventricular Tachycardia detection while providing the interpretability necessary for clinical trust. By translating the complex, temporal data of an ECG into a geometric and topological analysis, these models generate outputs that can be rationalized and verified by clinicians. The outlined protocols provide a roadmap for developing, validating, and integrating such systems into clinical practice. This approach, centered on proximity search mechanisms, demonstrates a viable path forward for building transparent, effective, and clinically actionable decision-support tools in critical care cardiology.
The inner workings of complex artificial intelligence (AI) models, particularly large neural networks, have traditionally functioned as "black boxes," limiting their trustworthiness and deployment in high-stakes domains like clinical medicine and drug development [41] [42]. Mechanistic interpretability, a subfield of AI research, seeks to understand the computational mechanisms underlying these capabilities [43]. The proximity search mechanism, which leverages semantic similarity within vector spaces, provides a foundational technique for this research. This document details the application of SemanticLens, a novel method that utilizes similarity search to map AI model components into a semantic space, thereby enabling component-level understanding and validation [42]. By framing this within clinical interpretability research, we provide researchers and drug development professionals with detailed protocols and application notes to audit AI reasoning, ensure alignment with biomedical knowledge, and mitigate risks such as spurious correlations.
Background and Core Concepts
Semantic Similarity and Vector Representations
The evolution of semantic similarity measurement provides essential context for modern similarity search applications.
- Traditional Methods: Early approaches relied on lexical databases (e.g., WordNet) or statistical techniques like Latent Semantic Analysis (LSA). These methods, while intuitive, were often context-insensitive and suffered from coverage limitations [44].
- Embedding-Based Methods: The field transformed with word embeddings (e.g., Word2Vec, GloVe), which represent words as fixed vectors in a continuous space. Similarity is quantified using metrics like cosine similarity, which measures the cosine of the angle between two vectors, providing a measure of semantic alignment irrespective of vector magnitude [44] [45] [46].
- Contextualized Embeddings: Transformer-based models (e.g., BERT) generate dynamic, context-aware embeddings, leading to a more nuanced understanding of meaning. This capability is crucial for interpreting model components that respond to complex, context-dependent features [44].
The Need for Interpretability in Clinical AI
In clinical and drug development settings, the inability to understand model reasoning poses significant safety, regulatory, and ethical challenges [41]. AI models may develop "Clever Hans" behaviors, where they achieve high accuracy by leveraging spurious correlations in the training data (e.g., watermarks in medical images) rather than learning clinically relevant features [42]. The EU AI Act and similar regulations increasingly mandate transparency and conformity assessments, creating an urgent need for scalable validation tools [42].
SemanticLens: A Universal Explanation Method
SemanticLens addresses the scalability limitations of previous interpretability methods by automating the analysis of model components. Its core innovation lies in mapping a model's internal components into the semantically structured, multimodal space of a foundation model (e.g., CLIP) [42].
Core Principle and Mappings
The method establishes a multi-stage mapping process to create a searchable representation of the AI model's knowledge.
Table 1: Core Mappings in the SemanticLens Workflow
| Mapping Step | Description | Output |
|---|---|---|
| Components → Concept Examples | For a target component (e.g., a neuron), collect data samples that highly activate it. | A set of examples ℰ representing the component's "concept." [42] |
| Concept Examples → Semantic Space | Embed the set ℰ into the semantic space 𒮠of a foundation model ℱ. |
A vector Ï‘ in ð’® representing the component's semantic meaning [42]. |
| Prediction → Components | Use relevance scores (e.g., attribution methods) to quantify component contributions to a specific prediction. | Relevance scores ℛ linking predictions back to components [42]. |
This process transforms any AI model into a searchable vector database of its own components, enabling large-scale, automated analysis [42].
Key Functionalities for Clinical Research
- Search Capability: Researchers can textually or visually probe the model to identify components encoding specific concepts (e.g., "melanoma," "skin lesion texture," or potential biases like "watermark") [42].
- Automated Description and Auditing: The system can automatically label neurons and audit a model's decision strategy against a required reasoning process, such as the ABCDE rule for melanoma classification [42].
- Cross-Model Comparison: Learned concepts can be systematically compared across different models or training runs, providing insights into model robustness and generalization [42].
The following diagram illustrates the core SemanticLens workflow and its key functionalities for model analysis.
Experimental Protocols
This section provides detailed methodologies for implementing SemanticLens to audit a clinical AI model.
Protocol 1: Component Embedding and Concept Search
Objective: To map the neurons of a convolutional neural network (e.g., ResNet50) trained on a medical image dataset (e.g., ISIC 2019 for skin lesions) into a semantic space and enable concept-based search [42].
Materials: Table 2: Research Reagent Solutions for Component Embedding
| Item | Function/Description |
|---|---|
| Trained Model (M) | The AI model under investigation (e.g., ResNet50 trained on ISIC 2019). |
| Foundation Model (F) | A multimodal model like CLIP or a domain-specific variant like WhyLesionCLIP, which serves as the "semantic expert." [42] |
| Validation Dataset | A held-out set from the model's training domain (e.g., ISIC 2019 test split). |
| Computational Framework | Python with deep learning libraries (PyTorch/TensorFlow) and vector computation utilities (NumPy). |
Procedure:
- Component Selection: Iterate through every neuron in the target model's final convolutional layer.
- Concept Example Collection:
a. For each neuron, forward-pass the entire validation dataset.
b. Record the top k (e.g., k=100) image patches that elicit the highest activation values for that neuron. This set of patches is
â„°for the neuron. - Semantic Embedding:
a. Using the foundation model
ℱ, compute the embedding vector for each image patch inâ„°. b. Compute the mean vector of all patches inâ„°to obtain a single, representative vectorÏ‘for the neuron in the semantic spaceð’®ofℱ. - Indexing: Store all neuron vectors
Ï‘in a vector database (e.g., using pgvector) to enable efficient similarity search [46]. - Querying:
a. To search for a concept (e.g., "skin ulcer"), generate a text embedding for the query string using
ℱ's text encoder. This is the probing vectorϑ_probe. b. Perform a cosine similarity search across the database of neuron vectorsϑ. c. Return a ranked list of neurons with the highest similarity toϑ_probe, along with their associated image patchesℰ.
Protocol 2: Automated Audit of Clinical Reasoning
Objective: To validate that a medical AI model's decision-making relies on clinically relevant features rather than spurious correlations [42].
Materials: As in Protocol 1, with the addition of a formally defined clinical decision rule (e.g., the ABCDE rule for melanoma: Asymmetry, Border irregularity, Color variation, Diameter, Evolution).
Procedure:
- Rule Decomposition: Translate the clinical rule into a set of concrete, searchable concepts (e.g., "asymmetry," "irregular border," "multiple colors").
- Concept Search: For each concept in the rule, execute Protocol 1 to identify neurons that encode it.
- Relevance Scoring: For a set of test predictions, use an attribution method (e.g., Layer-wise Relevance Propagation) to compute relevance scores
â„›, quantifying each neuron's contribution to the final prediction. - Alignment Quantification: a. For each correct prediction, calculate the aggregate relevance of the rule-aligned neurons identified in Step 2. b. Similarly, search for and calculate the aggregate relevance of neurons encoding spurious concepts (e.g., "ruler," "hair," "watermark"). c. A model is well-aligned if the relevance of clinically valid concepts is consistently and significantly higher than that of spurious concepts.
- Reporting: Generate an audit report listing the dominant concepts used for predictions, flagging cases where spurious features have high relevance.
Data Presentation and Validation
The effectiveness of SemanticLens is demonstrated through its application in validating models for critical tasks.
Table 3: Quantitative Results from SemanticLens Auditing of a ResNet50 Model on ImageNet
| Probed Concept | Top Matching Neuron ID | Semantic Description of Neuron | Cosine Similarity | Use in Prediction |
|---|---|---|---|---|
| Person | Neuron 1216 | Encodes "hijab" | 0.32 | - |
| Person | Neuron 1454 | Encodes "dark skin" | 0.29 | Used in "steel drum" classification (potential bias) |
| Watermark | Neuron 882 | Encodes copyright text/watermarks | 0.41 | Used in "abacus" classification (spurious correlation) |
| ABCDE Rule (Melanoma) | Neuron 1101 | Encodes "color variegation" | 0.38 | High relevance in correct melanoma diagnoses |
Application in clinical trial risk assessment shows AI models can achieve high performance (e.g., AUROC up to 96%) in predicting adverse drug events or trial efficacy, but issues of data quality and bias persist [47]. Tools like SemanticLens are vital for explaining and validating these performance metrics.
The Scientist's Toolkit
Table 4: Essential Materials for Proximity Search in Clinical Interpretability
| Tool/Category | Examples | Role in Interpretability Research |
|---|---|---|
| Vector Databases | pgvector, Pinecone | Enable efficient storage and similarity search of high-dimensional component embeddings [45] [46]. |
| Embedding Models | CLIP, DINOv2, WhyLesionCLIP | Act as the "semantic expert" to provide the structured space for mapping model components [42]. |
| Interpretability Libs | TransformerLens, Captum | Facilitate the extraction of model activations and computation of relevance scores (â„›) [43]. |
| Medical Foundation Models | WhyLesionCLIP, Med-PaLM | Domain-specific foundation models offer more clinically meaningful semantic spaces for auditing medical AI. |
| Locustatachykinin I TFA | Locustatachykinin I TFA, MF:C45H64F3N13O13, MW:1052.1 g/mol | Chemical Reagent |
| Pcsk9-IN-1 | Pcsk9-IN-1, MF:C65H80FN11O12S2, MW:1290.5 g/mol | Chemical Reagent |
SemanticLens, powered by proximity search mechanisms, provides a scalable framework for transitioning clinical AI from an inscrutable black box to a comprehensible and auditable system. The detailed application notes and experimental protocols outlined herein equip researchers and drug developers with the methodologies to validate AI reasoning, ensure alignment with biomedical knowledge, and build the trust required for safe and effective deployment in healthcare. Future work will focus on standardizing these audit protocols and developing more sophisticated domain-specific semantic foundations.
Kolmogorov-Arnold Networks (KANs) for Intrinsically Interpretable Clinical Classification
The adoption of artificial intelligence (AI) in clinical practice is critically hindered by the "black-box" nature of many high-performing models, where the internal decision-making mechanisms are not understandable to humans [48]. This opacity is particularly problematic in healthcare, where clinicians are legally and ethically required to interpret and defend their actions [48]. Kolmogorov-Arnold Networks (KANs) have recently emerged as a promising alternative to traditional neural networks, offering both strong approximation capabilities and intrinsic interpretability by learning mappings through compositions of learnable univariate functions rather than fixed activation functions [48] [49] [50].
This framework of proximity and relationships is fundamental to clinical reasoning. Just as proximity search mechanisms identify closely related concepts in medical literature [51] [52] [2], KANs enable the discovery and visualization of mathematical proximities between clinical features and diagnostic outcomes. The network's structure naturally reveals how "close" or "distant" input features are to particular clinical classifications, providing clinicians with transparent decision pathways that mirror their own analytical processes.
Fundamental Principles of Kolmogorov-Arnold Networks
Architectural Foundation
KANs are grounded in the Kolmogorov-Arnold representation theorem, which states that any multivariate continuous function can be represented as a finite composition of continuous functions of a single variable [49] [50]. This theoretical foundation translates into a neural network architecture where:
- Edge-Based Activation: Unlike Multi-Layer Perceptrons (MLPs) that place fixed activation functions on nodes, KANs position learnable activation functions on edges
- Spline-Parametrized Weights: KANs replace linear weight parameters with univariate functions parametrized as splines [49]
- No Linear Weights: All transformation operations are performed through learned function compositions [50]
This architectural difference enables KANs to achieve comparable or superior accuracy to much larger MLPs while maintaining intrinsic interpretability through their mathematically transparent structure [50].
Proximity-Informed Clinical Interpretability
The interpretability of KANs aligns with proximity-based clinical reasoning through several key mechanisms:
- Local Feature Contributions: KANs naturally decompose complex clinical decisions into additive feature contributions, revealing which inputs are "proximal" or "distant" to particular diagnoses
- Symbolic Formula Extraction: The learned spline functions can be simplified into symbolic formulas that provide human-readable clinical decision rules [48]
- Visual Decision Pathways: The network structure can be directly visualized to show the functional relationships between input features and clinical outcomes [48] [49]
These properties position KANs as ideal "collaborators" for clinical researchers, helping to (re)discover clinical decision patterns and pathological relationships [49] [50].
Clinical Applications and Performance Evaluation
Model Variants for Clinical Classification
Two specialized KAN architectures have been developed specifically for clinical classification tasks:
- Logistic-KAN: A flexible generalization of logistic regression that enables nonlinear yet interpretable transformations of each input feature [48] [53]
- Kolmogorov-Arnold Additive Model (KAAM): A simplified additive variant that delivers transparent, symbolic formulas through an enforced additive decomposition where each variable contributes independently through a dedicated KAN block [48]
These models support built-in patient-level insights, intuitive visualizations, and nearest-patient retrieval without requiring post-hoc explainability tools [48] [53].
Performance Across Clinical Domains
KAN-based models have demonstrated competitive performance across diverse clinical classification tasks, matching or outperforming standard baselines while maintaining full interpretability [48].
Table 1: Performance of KAN Models in Clinical Classification Tasks
| Clinical Domain | Dataset | Task Type | Key Performance Metrics | Comparative Advantage |
|---|---|---|---|---|
| Thyroid Disease Classification | Three-class thyroid dataset | Multiclass classification | 98.68% accuracy, 98.00% F1-score [54] | Outperformed traditional neural networks; integrated GAN-based data augmentation for minority classes [54] |
| Lung Cancer Detection | Lung-PET-CT-DX dataset | Binary classification | 99.0% accuracy, 0.07 loss [55] | Ensemble approach with spline functions (linear, cubic, B-spline); required limited computational resources [55] |
| Cardiovascular Risk Prediction | Heart dataset | Binary classification | Competitive performance vs. baselines [48] | Enabled symbolic formulas, personalized reasoning, and patient similarity retrieval [48] |
| Diabetes Classification | Diabetes-130 Hospital dataset | Multiclass classification | Matched or outperformed standard baselines [48] | Native visual interpretability through KAAM framework [48] |
| Obesity Risk Stratification | Obesity dataset | 7-class and binary classification | Competitive across balanced and imbalanced scenarios [48] | Transparent, symbolic representations for complex multi-class settings [48] |
Implementation Workflow
The application of KANs to clinical classification follows a structured workflow that integrates data preparation, model configuration, and interpretability analysis:
Experimental Protocols
Protocol 1: Binary Clinical Classification with KAAM
This protocol details the implementation of Kolmogorov-Arnold Additive Models for binary classification tasks, such as heart disease prediction [48].
Data Preparation
- Data Source: Utilize clinically validated datasets (e.g., Heart dataset with 22 features across 1,000 samples) [48]
- Preprocessing: One-hot encode categorical variables and standardize continuous features [48]
- Class Imbalance Handling: Apply strategic sampling techniques for datasets with skewed distributions (e.g., 9.42% positive cases in Heart dataset) [48]
Model Configuration
- Architecture: Implement KAAM with independent KAN blocks for each input feature
- Additive Constraint: Enforce feature independence through separate processing pathways
- Spline Configuration: Parametrize edge functions using B-spline bases with customizable grid sizes and orders
Training Procedure
- Optimization: Use gradient-based optimizers (Adam/L-BFGS) with regularization on spline coefficients
- Interpretability Loss: Incorporate symbolic regularization to encourage simple, explainable functions
- Validation: Employ k-fold cross-validation with clinical relevance metrics beyond accuracy
Interpretation Analysis
- Feature Contribution Visualization: Generate radar plots showing individual feature contributions to final classification [48]
- Symbolic Formula Extraction: Simplify learned spline functions into human-readable clinical decision rules [48]
- Nearest-Patient Retrieval: Implement similarity matching to identify clinically analogous cases [48]
Protocol 2: Multiclass Classification with Ensemble KANs
This protocol outlines the procedure for multiclass clinical classification, as demonstrated in thyroid disease and lung cancer detection [55] [54].
Data Augmentation
- GAN Integration: Generate synthetic minority class samples using Generative Adversarial Networks to address class imbalance [54]
- Oversampling Techniques: Apply SMOTE or ADASYN for alternative data balancing [54]
- MixUp Implementation: Employ MixUp data augmentation to improve generalization through sample blending [54]
Ensemble Architecture
- Spline Diversity: Implement multiple KAN variants with different spline functions (linear, cubic, B-spline) [55]
- Feature Extraction: Enhance mobile architecture (MobileNet V3) and transformer models (LeViT) for image-based clinical data [55]
- Fusion Strategy: Apply weighted sum feature fusion technique to combine extracted features [55]
Voting Integration
- Soft Voting: Combine predictions from multiple KAN classifiers using probability-based averaging [55]
- Confidence Calibration: Implement temperature scaling to ensure well-calibrated uncertainty estimates
- Clinical Validation: Validate ensemble decisions against multi-specialist clinical assessments
Protocol 3: Proximity-Informed Clinical Interpretability
This protocol leverages KANs' intrinsic interpretability to establish proximity relationships between clinical features and outcomes.
Feature Proximity Mapping
- Functional Distance Calculation: Measure distances between learned spline functions to establish feature relationship networks
- Clinical Cluster Identification: Apply graph analysis to detect naturally occurring feature groupings with clinical significance
- Decision Pathway Tracing: Map the complete functional pathway from input features to clinical outcomes
Knowledge Graph Integration
- Entity Recognition: Utilize BERT models and LoRA-tuned LLMs for named entity recognition from clinical texts [52]
- Triple Construction: Build subject-predicate-object triples (e.g.,
) to formalize clinical knowledge [52] ,> - Graph Analysis: Perform network distance calculations between disease, symptom, and treatment modules [52]
Validation Framework
- Clinical Correlation: Validate discovered proximity relationships against established medical knowledge
- Expert Review: Conduct structured evaluations with clinical domain experts
- Utility Assessment: Measure impact on clinical decision-making efficiency and accuracy
The Scientist's Toolkit
Table 2: Essential Research Reagents and Computational Tools for KAN Clinical Research
| Tool/Reagent | Function/Purpose | Implementation Notes |
|---|---|---|
| Logistic-KAN Framework | Flexible generalization of logistic regression for clinical classification [48] | Provides nonlinear, interpretable transformations of input features; compatible with standard clinical data formats |
| KAAM Architecture | Kolmogorov-Arnold Additive Model for transparent, symbolic clinical formulas [48] | Enforces additive decomposition for individualized feature contribution analysis |
| Spline Functions Library | Parametrization of learnable activation functions on KAN edges [55] | Includes linear, cubic, and B-spline implementations for different clinical data characteristics |
| GAN Data Augmentation | Addresses class imbalance in clinical datasets through synthetic sample generation [54] | Critical for rare disease classification; integrates with existing clinical data pipelines |
| Ensemble Learning Framework | Combines multiple KAN variants for improved accuracy and robustness [55] | Implements soft-voting approaches for clinical decision fusion |
| Interpretability Visualization | Generates clinical decision pathways and feature contribution maps [48] | Produces radar plots, symbolic formulas, and patient similarity visualizations |
| Proximity Analysis Toolkit | Quantifies relationships between clinical features and outcomes [52] | Maps functional proximities in KANs to clinically meaningful relationships |
| Clinical Knowledge Graph | Structures medical knowledge for interpretability validation [52] | Built using BERT/LLM entity recognition and triple construction from clinical texts |
| eIF4A3-IN-5 | eIF4A3-IN-5, MF:C26H22N2O7, MW:474.5 g/mol | Chemical Reagent |
| Nefopam-d4 (hydrochloride) | Nefopam-d4 (hydrochloride), MF:C17H20ClNO, MW:293.8 g/mol | Chemical Reagent |
Integration with Proximity Search Mechanisms
The interpretability of KANs in clinical classification naturally aligns with proximity search methodologies through several key mechanisms:
Functional Proximity Mapping
KANs enable the quantification of "functional proximity" between clinical features by analyzing the learned spline relationships:
Cross-Domain Proximity Alignment
The proximity relationships discovered through KANs can be validated against established medical knowledge graphs:
- Symptom-Disease Association: Closer network distances between symptoms and diseases in KGs predict stronger clinical associations, validated through KAN decision pathways [52]
- Treatment Similarity: Diseases with closer network distances demonstrate similarities in treatment approaches, reflected in KAN feature contributions [52]
- Diagnostic Confidence: Symptom-disease pairs in primary diagnostic relationships show stronger associations than secondary relationships, aligning with KAN confidence metrics [52]
Clinical Decision Support Integration
KANs enhance clinical decision support systems through transparent, proximity-informed reasoning:
- Evidence-Based Justification: KANs provide clear functional relationships between input clinical features and outcomes, supporting diagnostic justification [48]
- Similar Case Retrieval: The functional proximity metrics enable identification of clinically similar patients for comparative analysis [48]
- Treatment Pathway Optimization: By revealing the strength and nature of feature-outcome relationships, KANs support personalized treatment planning [48] [54]
Kolmogorov-Arnold Networks represent a significant advancement in developing intrinsically interpretable AI systems for clinical classification. By combining mathematical transparency with competitive performance, KANs address the critical trust deficit that has hindered the adoption of black-box models in healthcare. The integration of proximity search principles with KAN-based clinical decision systems creates a powerful framework for discovering, validating, and implementing clinically meaningful patterns in complex medical data. As these technologies mature, they hold the potential to establish new standards for trustworthy AI in clinical practice, ultimately enhancing patient care through transparent, auditable, and clinically actionable decision support systems.
Practical Applications in Target Identification and Validation for Drug Discovery
Target identification and validation represent the critical foundation of the drug discovery pipeline, serving as the initial phase where potential molecular targets are discovered and their therapeutic relevance is confirmed. This process has been revolutionized by integrated methodologies that combine advanced computational approaches with robust experimental validation. The emergence of proximity search mechanisms—concepts adapted from information retrieval systems where relationships are inferred based on contextual closeness—provides a powerful framework for analyzing biological networks and multi-omics data. By applying this principle to clinical interpretability research, scientists can identify biologically proximate targets with higher translational potential, ultimately reducing late-stage attrition rates in drug development [56] [57].
This article presents practical application notes and experimental protocols for implementing these methodologies, with a specific focus on network-based multi-omics integration and high-throughput mass spectrometry techniques that are reshaping modern target validation paradigms.
Key Applications in Target Identification and Validation
The integration of advanced technologies has enabled more precise target identification and validation strategies, as summarized in the table below.
Table 1: Key Applications in Target Identification and Validation
| Application Area | Technology/Method | Key Advantage | Typical Output |
|---|---|---|---|
| Network-Based Target Identification | Graph Neural Networks (GNNs) [57] | Captures complex target-disease relationships within biological networks | Prioritized list of potential therapeutic targets |
| Multi-omics Data Integration | Similarity-based approaches & network propagation [57] | Reveals complementary signals across molecular layers | Integrated disease models with candidate targets |
| Cellular Target Engagement | Cellular Thermal Shift Assay (CETSA) [22] | Confirms direct drug-target binding in physiologically relevant environments | Quantitative data on target stabilization |
| High-Throughput Biochemical Screening | Mass Spectrometry (e.g., RapidFire) [58] | Label-free detection reduces false positives | Identification of enzyme inhibitors/modulators |
| Mechanism of Action Studies | Thermal Proteome Profiling (TPP) [58] | Monitors melting profiles of thousands of proteins simultaneously | Unbiased mapping of drug-protein interactions |
Experimental Protocols
Protocol: Network-Based Multi-Omics Target Identification Using Graph Neural Networks
Purpose: To identify novel drug targets by integrating multi-omics data (genomics, transcriptomics) into biological networks using a Graph Neural Network (GNN) framework, applying proximity principles to find clinically relevant targets [57].
Materials and Reagents:
- Multi-omics Datasets: DNA sequencing (genomics), RNA sequencing (transcriptomics) data from disease and control tissues.
- Protein-Protein Interaction (PPI) Network: From databases like STRING or BioGRID.
- Computational Environment: High-performance computing cluster with ≥ 32 GB RAM, Python 3.8+, and relevant libraries (PyTorch Geometric, DGL, Scanpy).
Procedure:
- Data Preprocessing: Normalize transcriptomics data (e.g., using Scanpy) and process genomics variants. Annotate genes with known disease associations from public repositories (e.g., DisGeNET).
- Heterogeneous Network Construction:
- Represent genes/proteins as nodes in a graph.
- Establish edges based on:
- Protein-protein interactions (from PPI databases).
- Gene co-expression (calculated from transcriptomics data).
- Functional similarity (based on Gene Ontology annotations).
- GNN Model Implementation:
- Implement a GNN block architecture (e.g., GNNBlockDTI) to process the graph.
- Capture drug substructure and pocket-level protein features at different granularity levels.
- Apply a gating mechanism to reduce noise and redundancy in the features.
- Proximity-Based Target Prioritization:
- Use network propagation to measure the proximity between differentially expressed genes and known disease modules in the network.
- Rank candidate targets based on their multi-omics integration scores and network proximity to established disease genes.
- Validation: Perform in silico validation by testing the association of top-ranked targets with relevant disease pathways (e.g., via KEGG or Reactome enrichment analysis).
Protocol: Cellular Target Engagement Validation Using CETSA
Purpose: To quantitatively confirm direct binding of a drug molecule to its intended protein target in a physiologically relevant cellular context, bridging the gap between biochemical potency and cellular efficacy [22].
Materials and Reagents:
- Cell Line: Relevant human cell line (e.g., primary cells or established cell models).
- Test Compound: Drug candidate compound dissolved in DMSO.
- Equipment: Thermal cycler or precise heat blocks, cell lysis equipment, centrifuge, Western blot apparatus or mass spectrometer.
- Buffers: Phosphate-buffered saline (PBS), cell lysis buffer with protease inhibitors.
Procedure:
- Compound Treatment: Treat cell aliquots (~ 2 million cells/sample) with a range of concentrations of the test compound or vehicle control (DMSO) for a predetermined incubation time (e.g., 1-2 hours).
- Heat Challenge: Divide each cell aliquot into smaller samples and expose them to a gradient of temperatures (e.g., from 37°C to 65°C, across 10-12 points) for 3 minutes in a thermal cycler.
- Cell Lysis and Fractionation: Lyse the heat-challenged cells. Centrifuge the lysates at high speed (20,000 x g) to separate the soluble (stable) protein fraction from the insoluble (aggregated) fraction.
- Target Protein Quantification: Detect and quantify the amount of the target protein remaining in the soluble fraction at each temperature. This can be achieved via:
- Immunoblotting: Using a target-specific antibody, followed by densitometric analysis.
- Mass Spectrometry: For an unbiased proteome-wide approach, as used in Thermal Proteome Profiling (TPP) [58].
- Data Analysis:
- Plot the soluble protein fraction against the temperature to generate melting curves.
- Compare the melting curves of compound-treated samples versus the vehicle control. A rightward shift (increase in protein melting temperature, Tm) in treated samples indicates stabilization of the target protein due to compound binding.
- Generate dose-response curves at a fixed temperature to estimate the apparent binding affinity (EC50) of the compound for its target in cells.
Protocol: High-Throughput Mass Spectrometry Screening for Enzyme Inhibitors
Purpose: To identify inhibitors of an enzyme target in a high-throughput (HT) screening format using label-free mass spectrometry, minimizing false positives common in traditional fluorescence-based assays [58].
Materials and Reagents:
- Purified Enzyme: Recombinant enzyme of interest.
- Compound Library: A diverse collection of small molecules (e.g., 100,000+ compounds) in 384-well plate format.
- Substrate and Cofactors: Natural substrate and required cofactors (e.g., NADH, ATP).
- HT-MS System: Automated liquid handling system coupled to a RapidFire MS system or an acoustic droplet ejection (ADE) open port interface (OPI) MS system and a triple quadrupole mass spectrometer.
Procedure:
- Assay Setup: Using an automated liquid handler, dispense the enzyme reaction buffer, followed by the compound library (in nanoliter volumes), into a 384-well plate.
- Biochemical Reaction: Initiate the enzyme reaction by adding the substrate. Allow the reaction to proceed for a fixed time under optimal conditions (pH, temperature).
- Reaction Quenching: Stop the reaction at a predetermined time point by adding a quenching solution (e.g., acid or organic solvent).
- High-Throughput MS Analysis:
- For a RapidFire System: The system automatically aspirates samples from the plate, rapidly desalts them online using solid-phase extraction (SPE), and elutes the purified analytes directly into the ESI-MS.
- For an ADE-OPI MS: Acoustic droplet ejection transfers sample droplets directly to an open port interface for ionization, enabling extremely fast analysis (cycling times of ~2.5 seconds per sample).
- Data Acquisition and Analysis:
- The mass spectrometer is operated in multiple reaction monitoring (MRM) mode to specifically quantify the substrate and product based on their mass-to-charge ratios (m/z).
- The ratio of product to substrate is calculated for each well.
- Compounds that significantly reduce the product-to-substrate ratio compared to control wells (containing no inhibitor) are identified as hits.
Workflow and Pathway Visualizations
Network-Based Multi-Omics Target Identification
Cellular Target Engagement (CETSA) Workflow
High-Throughput MS Screening Protocol
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Target Identification and Validation
| Reagent/Material | Function/Application | Example Use Case |
|---|---|---|
| CETSA Reagents [22] | Validate direct target engagement of small molecules in intact cells and native tissue environments. | Confirming dose-dependent stabilization of DPP9 in rat tissue. |
| RapidFire MS Cartridges [58] | Solid-phase extraction (SPE) for rapid online desalting and purification of samples prior to ESI-MS. | High-throughput screening for enzyme inhibitors in 384-well format. |
| Graph Neural Network (GNN) Models [57] [59] | Integrate multi-omics data (e.g., genomics, transcriptomics) with biological networks for target discovery. | Predicting novel drug-target interactions by learning from network topology and node features. |
| Photoaffinity Bits (PhAbit) [58] | Reversible ligands with a photoreactive warhead to facilitate covalent binding for target identification (chemoproteomics). | Identifying cellular targets of uncharacterized bioactive compounds. |
| Thermal Proteome Profiling (TPP) Kits [58] | Reagents and protocols for monitoring the thermal stability of thousands of proteins in a single experiment. | Unbiased mapping of drug-protein interactions and mechanism of action studies. |
| D-Dimannuronic acid | D-Dimannuronic acid, MF:C12H18O13, MW:370.26 g/mol | Chemical Reagent |
| Hpk1-IN-29 | Hpk1-IN-29, MF:C26H18F3N5O2, MW:489.4 g/mol | Chemical Reagent |
Overcoming Implementation Hurdles: Troubleshooting and Optimizing Proximity Search Systems
Identifying and Mitigating Spurious Correlations and 'Clever Hans' Phenomena
The Clever Hans effect represents a significant challenge in the development of reliable artificial intelligence (AI) systems for clinical and biomedical applications. This phenomenon occurs when machine learning models learn to rely on spurious correlations in training data rather than clinically relevant features, ultimately compromising their real-world reliability and generalizability [60] [61]. Named after the early 20th-century horse that appeared to perform arithmetic but was actually responding to subtle cues from his trainer, this effect manifests in AI systems when they utilize "shortcut features"—superficial patterns in data that are not causally related to the actual outcome of interest [61]. In clinical settings, this can lead to diagnostic models that appear highly accurate during development but fail dramatically when deployed in different healthcare environments or patient populations.
The clinical interpretability research landscape, particularly frameworks incorporating proximity search mechanisms, provides essential methodologies for detecting and mitigating these deceptive patterns. As AI systems become increasingly integrated into drug development and clinical decision-making, addressing the Clever Hans effect transitions from a theoretical concern to a practical necessity for ensuring patient safety and regulatory compliance [60]. This document establishes comprehensive application notes and experimental protocols to identify and counteract these spurious correlations, with particular emphasis on their implications for clinical interpretability and therapeutic development.
Current research indicates that the Clever Hans effect persists as a prevalent challenge across medical AI applications. A recent scoping review analyzed 173 papers published between 2010 and 2024, with 37 studies selected for detailed analysis of detection and mitigation approaches [60]. The findings reveal that the majority of current machine learning studies in medical imaging do not adequately report or test for shortcut learning, highlighting a critical gap in validation practices [60] [61].
Table 1: Performance Impact of Clever Hans Effects in Clinical AI Models
| Clinical Domain | Model Architecture | Reported Performance | Debiased Performance | Primary Shortcut Feature |
|---|---|---|---|---|
| COVID-19 Detection from Chest X-Rays | Deep Convolutional Neural Network | AUROC: 0.92 [61] | AUROC: 0.76 [61] | Hospital-specific positioning markers |
| ICU Mortality Prediction | XGBoost | AUROC: 0.924 [11] | AUROC: 0.834 [11] | Hospital-specific data collection patterns |
| Dementia Diagnosis from MRI | 3D CNN | Accuracy: 89% [61] | Accuracy: 74% [61] | Scanner manufacturer metadata |
| Pneumonia Detection from X-Rays | ResNet-50 | Sensitivity: 94% [61] | Sensitivity: 63% [61] | Portable vs. stationary equipment |
The quantitative evidence demonstrates that models affected by Clever Hans phenomena can exhibit performance degradation of up to 30% when evaluated on data without spurious correlations [61]. This performance drop disproportionately impacts models deployed across multiple clinical sites, with one study reporting a 22% decrease in accuracy when models trained on single-institution data were validated externally [61]. These findings underscore the critical importance of implementing robust detection and mitigation protocols, particularly in drug development contexts where model failures could impact therapeutic efficacy and safety assessments.
Detection Methodologies and Experimental Protocols
Model-Centric Detection Approaches
Model-centric detection methods focus on analyzing the internal mechanisms and decision processes of machine learning models to identify reliance on spurious correlations. The following protocol provides a standardized approach for model-centric detection:
Protocol 1: Model-Centric Detection of Clever Hans Phenomena
- Purpose: To identify model dependency on shortcut features through analysis of model internals and behavior.
- Experimental Setup:
- Train the model using established clinical datasets with appropriate performance validation.
- Implement gradient-based attribution methods (e.g., Saliency Maps, Integrated Gradients) to visualize feature importance.
- Apply layer-wise relevance propagation to trace model decisions back to input features.
- Procedure:
- Generate attribution maps for a representative validation set (minimum n=200 samples).
- Quantify the proportion of decisions primarily attributed to clinically non-relevant features.
- Implement counterfactual analysis by systematically removing or altering putative shortcut features.
- Measure performance degradation when potential shortcut features are ablated.
- Interpretation: Models exhibiting >15% performance degradation after feature ablation or showing >20% of decisions relying on non-clinical features indicate significant Clever Hans effects [61].
Data-Centric Detection Approaches
Data-centric methods examine the training data and its relationship to model performance to identify spurious correlations:
Protocol 2: Data-Centric Detection of Spurious Correlations
- Purpose: To identify dataset biases that could facilitate shortcut learning.
- Experimental Setup:
- Curate multiple datasets from diverse clinical settings and patient populations.
- Establish ground truth annotations for potential confounding variables (acquisition parameters, demographic factors, institutional signatures).
- Procedure:
- Perform stratified analysis across potential confounding variables (e.g., hospital site, imaging equipment, demographic subgroups).
- Measure performance disparities exceeding 10% between subgroups as indicators of potential spurious correlations.
- Implement cross-validation where models are trained on subsets excluding potential shortcuts and tested on challenging cases.
- Apply dataset cartography to identify "ambiguous" examples that may promote shortcut learning.
- Interpretation: Performance variations >15% across subgroups or significant performance drop (>20%) on ambiguous examples indicate susceptibility to Clever Hans effects [60].
The detection workflow integrates these approaches systematically, as illustrated below:
Diagram 1: Clever Hans detection workflow integrating model and data approaches
Mitigation Strategies and Implementation Protocols
Data Manipulation Techniques
Data manipulation approaches directly address spurious correlations in training datasets through strategic preprocessing and augmentation:
Protocol 3: Data Manipulation for Clever Hans Mitigation
- Purpose: To reduce model dependency on shortcut features through dataset curation and augmentation.
- Experimental Setup:
- Identify potential shortcut features through preliminary detection analyses.
- Establish a multi-site dataset with consistent annotation protocols.
- Procedure:
- Implement data balancing across identified confounding variables (e.g., ensure equal representation of different scanner types, clinical sites, or demographic groups).
- Apply targeted data augmentation that preserves clinically relevant features while altering potential shortcuts (e.g., modifying hospital-specific metadata while preserving pathological signatures).
- Utilize causal data collection to acquire counterexamples where shortcut features are dissociated from outcomes.
- Create challenge sets specifically enriched with cases where shortcuts and genuine features conflict.
- Validation: Evaluate model performance on held-out challenge sets and measure reduction in performance gap between majority and minority subgroups (target: <5% disparity) [61].
Feature Disentanglement and Suppression
Feature disentanglement approaches modify model architecture and training objectives to explicitly separate robust features from spurious correlations:
Protocol 4: Feature Disentanglement for Robust Clinical AI
- Purpose: To learn representations that explicitly separate clinically relevant features from spurious correlations.
- Experimental Setup:
- Implement neural network architectures with separate embedding spaces for clinical features and potential shortcuts.
- Design training protocols that incorporate invariance constraints.
- Procedure:
- Implement invariant risk minimization (IRM) to learn features that maintain predictive power across environments.
- Apply adversarial training to actively suppress model reliance on identified shortcut features.
- Utilize contrastive learning objectives that maximize similarity between clinically similar cases despite differences in non-relevant features.
- Implement feature distillation from domain experts to prioritize clinically plausible features.
- Validation: Measure cross-site generalizability performance and feature attribution alignment with clinical expertise (target: >85% alignment with clinical feature relevance) [60].
Domain Knowledge-Driven Approaches
Domain knowledge integration leverages clinical expertise to identify and mitigate biologically implausible model behaviors:
Protocol 5: Domain Knowledge Integration for Mitigation
- Purpose: To incorporate clinical expertise directly into model development to prevent shortcut learning.
- Experimental Setup:
- Establish a multidisciplinary team including clinical domain experts.
- Develop formal specifications of clinically relevant features and implausible shortcuts.
- Procedure:
- Conduct feature importance review sessions with clinical experts to identify biologically implausible feature dependencies.
- Implement rule-based constraints that penalize model reliance on predefined shortcut features.
- Develop hybrid models that integrate knowledge-driven reasoning with data-driven learning.
- Establish clinical plausibility metrics for model explanations and incorporate them into validation criteria.
- Validation: Quantitative assessment of model explanations against clinical ground truth and failure mode analysis by domain experts [60].
The relationship between detection outcomes and appropriate mitigation strategies is systematized below:
Diagram 2: Mitigation strategy selection based on detection outcomes
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Tools for Clever Hans Investigation
| Tool Category | Specific Solution | Function | Implementation Considerations |
|---|---|---|---|
| Detection Libraries | SHAP (SHapley Additive exPlanations) [11] | Quantifies feature contribution to model predictions | Computational intensity increases with feature count |
| LIME (Local Interpretable Model-agnostic Explanations) [11] | Creates local surrogate models to explain individual predictions | Approximation fidelity varies across model types | |
| Anchor | Provides high-precision explanation with coverage guarantees | Rule complexity may limit interpretability | |
| Mitigation Frameworks | Invariant Risk Minimization (IRM) [61] | Learns features invariant across environments | Requires explicit environment definitions |
| Adversarial Debiasing | Actively suppresses reliance on protected attributes | Training instability requires careful hyperparameter tuning | |
| Contrastive Learning | Maximizes similarity between clinically similar cases | Positive pair definition critical for clinical relevance | |
| Validation Tools | Domain-specific Challenge Sets | Tests model performance on clinically ambiguous cases | Requires expert annotation and curation |
| Cross-site Validation Frameworks | Assesses model generalizability across institutions | Data sharing agreements may limit accessibility | |
| Feature Importance Consensus Metrics | Quantifies alignment between model and clinical reasoning | Dependent on quality and availability of clinical experts |
Integration with Proximity Search for Clinical Interpretability
The proximity search mechanism provides a powerful framework for enhancing clinical interpretability while addressing Clever Hans phenomena. This approach establishes semantic neighborhoods in feature space that enable explicit navigation between clinically similar cases, creating a natural validation mechanism for model behavior [29]. When integrated with proximity search, detection of spurious correlations is enhanced through anomaly identification in the neighborhood structure—cases that are "close" in model feature space but distant in clinical reality indicate potential shortcut learning.
In mitigation, proximity search enables the implementation of neighborhood-based constraints during model training, enforcing that clinically similar cases receive similar model representations regardless of spurious correlates. Furthermore, the explicit neighborhood structure provides a natural interface for domain expert validation, allowing clinicians to interrogate model decisions by examining nearby cases and flagging clinically implausible groupings [29]. This integration creates a powerful synergy where interpretability mechanisms directly contribute to model robustness, addressing the Clever Hans effect while enhancing clinical utility.
Implementation of proximity search for Clever Hans mitigation involves:
- Defining clinically meaningful similarity metrics for proximity calculations
- Establishing neighborhood-based regularization during model training
- Creating interactive interfaces for clinical experts to explore model neighborhoods
- Developing automated monitoring of neighborhood stability across clinical sites
This approach aligns with the broader objective of clinical interpretability research: developing AI systems whose decision processes are transparent, clinically plausible, and robust across diverse patient populations and healthcare environments [29] [11].
Addressing the Clever Hans effect through systematic detection and mitigation protocols is essential for developing clinically reliable AI systems. The frameworks presented here provide actionable methodologies for identifying spurious correlations and implementing robust countermeasures, with particular relevance to drug development and clinical decision support. The integration of these approaches with proximity search mechanisms for clinical interpretability represents a promising direction for creating more transparent and trustworthy clinical AI.
Future research should prioritize the development of standardized benchmarks for Clever Hans effects across clinical domains, automated detection tools integrated into model development workflows, and more sophisticated integration of clinical knowledge throughout the AI development lifecycle [60]. Establishing community-driven best practices and fostering interdisciplinary collaboration between AI researchers and clinical domain experts will be crucial for ensuring the development of reliable, generalizable, and equitable AI systems in healthcare [60] [61].
Optimizing Proximity Thresholds and Parameters for Clinical Specificity and Sensitivity
Proximity-based mechanisms are emerging as transformative tools for clinical interpretability research, enabling precise modulation of biological processes through controlled molecular interactions. This protocol details the application of proximity thresholds and parameter optimization to enhance diagnostic specificity and sensitivity in clinical and pharmaceutical development. We present a structured framework integrating real-world data with mechanistic multiparameter optimization (MPO) to balance often conflicting clinical requirements. The methodologies outlined provide researchers with standardized approaches for threshold calibration in diagnostic artificial intelligence (AI), clinical trial monitoring, and targeted therapeutic development, facilitating more reliable translation of computational insights into clinical practice.
Molecular proximity orchestrates biological function, and leveraging this principle through proximity-based modalities has opened new frontiers in clinical research and drug discovery [28]. These approaches, including proteolysis-targeting chimeras (PROTACs) and molecular glues, operate by artificially inducing proximity between target proteins and effector mechanisms, creating opportunities for therapeutic intervention with high selectivity [28]. Similarly, in clinical diagnostics and trial monitoring, establishing optimal thresholds for decision-making parameters ensures that sensitivity and specificity remain balanced across diverse patient populations and clinical scenarios.
This application note provides detailed protocols for optimizing these critical parameters within the context of proximity search mechanisms for clinical interpretability research. By integrating real-world clinical data with systematic optimization frameworks, researchers can enhance the predictive accuracy and clinical utility of their models and interventions.
Background Concepts
Proximity-Based Modalities in Biology and Medicine
Proximity-based modalities function by intentionally inducing proximity between a target and an effector protein to change the target's fate and modulate related biological processes [28]. These modalities can be categorized structurally into monomeric molecules (e.g., molecular glues), bifunctional molecules (e.g., PROTACs), or even higher-order multivalent constructs [28]. The clinical outcome depends entirely on which target-effector combination is brought together, offering researchers a versatile toolkit for therapeutic development.
Threshold Optimization in Clinical Decision-Making
In clinical applications, threshold optimization involves determining cutoff values that convert algorithmic confidence scores or biochemical measurements into binary clinical decisions. Traditional approaches often rely on vendor-defined defaults or prevalence-independent optimization strategies that may not account for specific clinical subgroup requirements [62]. Effective threshold management must balance sensitivity (correctly identifying true positives) with specificity (correctly identifying true negatives), while considering the clinical consequences of both false positives and false negatives.
Quantitative Data Synthesis
Performance Comparison of Optimization Approaches
Table 1: Threshold optimization performance across clinical scenarios
| Pathology | Patient Population | Default Threshold Sensitivity | Optimized Threshold Sensitivity | Alert Rate Impact |
|---|---|---|---|---|
| Pleural Effusion | Outpatient | 46.8% | 87.2% | +1% sensitivity per ≤1% alert rate increase |
| Pleural Effusion | Inpatient | 76.3% | 93.5% | +1% sensitivity per ≤1% alert rate increase |
| Consolidations | Outpatient | 52.1% | 85.7% | +1% sensitivity per ≤1% alert rate increase |
| Nodule Detection | Inpatient | 69.5% | 82.5% | Improved specificity without sensitivity loss |
Data adapted from chest X-ray AI analysis study comparing vendor default thresholds versus optimized thresholds [62].
Multi-Parameter Optimization in Drug Discovery
Table 2: Mechanistic MPO performance in small-molecule therapeutic projects
| Optimization Metric | Performance Achievement | Clinical Impact |
|---|---|---|
| Area Under ROC Curve (AUCROC) | >0.95 | Excellent predictive accuracy |
| Clinical Candidate Identification | 83% of short-listed compounds in top 2nd percentile | Enhanced lead selection efficiency |
| Chronological Optimization Recapitulation | Successful across different scaffolds | Validates progression tracking |
| In Vivo Testing Reduction | Markedly higher MPO scores for PK-characterized compounds | Reduced animal testing reliance |
Data from application of mechanistic multiparameter optimization in small-molecule drug discovery [63].
Experimental Protocols
Protocol 1: Subgroup-Specific Threshold Optimization for Clinical AI
Purpose: To optimize AI decision thresholds for specific clinical subgroups using real-world data and pathology-enriched validation sets.
Materials:
- Clinical dataset (minimum 5,000 cases recommended)
- Pathology-enriched validation dataset (balanced prevalence of 10-20% for target conditions)
- AI algorithm with continuous confidence scores
- Statistical analysis software (R, Python with scikit-learn)
Procedure:
- Cohort Definition: Define distinct clinical subgroups (e.g., inpatient vs. outpatient) based on relevant clinical characteristics [62].
- Data Preparation: Assemble a pathology-enriched study cohort with balanced prevalences of target pathologies and unremarkable findings. Ensure independent expert reference readings using standardized assessment scales (e.g., 5-point Likert scale) [62].
- Algorithm Application: Process both cohorts through the AI algorithm to obtain confidence scores for each target pathology.
- Threshold Sweep: Perform iterative receiver operating characteristic (ROC) analysis across the entire range of possible thresholds (0-100%) [62].
- Alert Rate Calculation: For each potential threshold, calculate the resulting AI alert rates in the clinical routine cohort.
- Optimization Criterion: Identify the "optimized threshold" (OT) where each additional 1% sensitivity gain leads to ≤1% increase in clinical alert rates [62].
- Validation: Compare performance of optimized thresholds against vendor default thresholds and Youden's thresholds using an independent validation set with expert radiologist reference.
Quality Control: Ensure reference readers are blinded to AI results and clinical information. Calculate inter-reader reliability for reference standards.
Protocol 2: Clinical Trial Site Performance Monitoring
Purpose: To establish threshold-based monitoring of clinical trial site performance using risk indicators.
Materials:
- Clinical trial database with site-level performance data
- Statistical software for descriptive statistics and visualization (Stata, R, Python)
- Predefined key risk indicators (KRIs) and quality tolerance limits (QTLs)
Procedure:
- Metric Selection: Identify relevant performance metrics from established core sets [64]. Essential metrics include:
- Screen failure rates
- Protocol deviation rates
- Data entry timeliness
- Query response times
- Patient discontinuation rates
- Threshold Definition: Establish initial thresholds for each metric based on trial requirements and historical performance data [65].
- Data Collection: Implement systematic collection of metric data at regular intervals (e.g., weekly, monthly).
- Trigger Calculation: Compute "total trigger scores" as the sum of metrics exceeding thresholds at each assessment point [64].
- Visualization: Create longitudinal plots of total trigger scores and individual trigger matrices for each site.
- Action Implementation: Define escalation pathways for sites exceeding threshold limits, ranging from simple contact to on-site visits [64].
- Iterative Refinement: Adjust thresholds based on accumulating trial experience and observed performance patterns.
Quality Control: Implement consistent data extraction methods across all sites. Maintain documentation of threshold justifications and modifications.
Protocol 3: Mechanistic Multiparameter Optimization for Lead Compound Selection
Purpose: To prioritize lead compounds using mechanistic modeling that integrates multiple pharmacological parameters.
Materials:
- Compound library with experimental data for target properties and ADME parameters
- Mechanistic MPO framework incorporating physiological relevance
- Machine learning platforms for prediction
- In vitro to in vivo correlation (IVIVC) capabilities
Procedure:
- Parameter Selection: Identify critical parameters for optimization based on project objectives (e.g., potency, selectivity, metabolic stability, safety margins) [63].
- Model Development: Create mechanistic models that integrate selected parameters, weighted according to their clinical relevance [63].
- Score Calculation: Compute MPO scores for all compounds, summarizing multiple properties into a single prioritized value [63].
- Validation: Assess MPO performance by evaluating its ability to identify historically successful compounds and recapitulate chronological optimization progress [63].
- Iterative Refinement: Refine parameter weights based on emerging experimental data and clinical requirements.
- Decision Support: Utilize MPO scores to prioritize compounds for further development, reducing reliance on extensive in vivo testing [63].
Quality Control: Regularly assess MPO performance against experimental outcomes. Guard against subjective bias in parameter weighting.
Visualization of Workflows and Mechanisms
Clinical Threshold Optimization Workflow
Proximity-Based Therapeutic Mechanisms
Research Reagent Solutions
Table 3: Essential research reagents for proximity threshold optimization studies
| Reagent/Category | Function/Application | Examples/Specifications |
|---|---|---|
| Pathology-Enriched Clinical Datasets | Validation of AI algorithms across balanced pathology spectra | Pleural effusions, consolidations, pneumothoraces, nodules (10-20% prevalence each) [62] |
| E3 Ligase Ligands | Enable targeted protein degradation via PROTAC technology | VHL and CRBN small-molecule ligands [28] |
| Molecular Glue Compounds | Induce proximity via protein-protein interaction stabilization | Thalidomide, lenalidomide, pomalidomide, indisulam [28] |
| Clinical Trial Metric Tracking Systems | Monitor site performance and protocol adherence | Key Risk Indicators (KRIs), Quality Tolerance Limits (QTLs) [65] |
| Multiparameter Optimization Platforms | Integrate multiple compound properties into prioritized scores | Mechanistic MPO frameworks incorporating ADME and safety parameters [63] |
| Reference Standard Annotations | Gold-standard validation for algorithm optimization | Expert radiologist readings using standardized scales (5-point Likert) [62] |
Optimizing proximity thresholds and parameters represents a critical advancement in clinical interpretability research, enabling more precise diagnostic and therapeutic interventions. The protocols outlined provide a standardized approach for researchers to enhance specificity and sensitivity across diverse clinical applications, from AI-based diagnostic tools to targeted therapeutic development and clinical trial monitoring. By systematically integrating real-world data with mechanistic optimization frameworks, researchers can overcome the limitations of one-size-fits-all thresholds and develop more clinically relevant, subgroup-specific solutions. The continued refinement of these approaches will accelerate the translation of proximity-based mechanisms into improved patient outcomes across therapeutic areas.
Addressing Computational Complexity and Scalability in High-Dimensional Clinical Data
The integration of high-dimensional biological data—encompassing genetic, molecular, and phenotypic information—into clinical research presents a significant challenge for computational analysis and interpretation. Such data, characterized by a vast number of variables (p) often far exceeding the number of observations (n), introduces substantial computational complexity and scalability issues in data processing, model training, and result interpretation. This document outlines application notes and experimental protocols for employing proximity-based mechanisms as a computational framework to mitigate these challenges. By quantifying the network-based relationships between biological entities—such as drug targets and disease proteins—this approach enhances the efficiency of analytical workflows and provides a biologically grounded structure for clinical interpretability research, ultimately supporting more effective drug development pipelines [66] [26].
Background and Key Concepts
The Nature of High-Dimensional Clinical Data
High-dimensional data in clinical trials typically includes diverse variable types, each requiring specific analytical considerations for proper interpretation and colorization in visualizations [67].
Table 1: Data Types in High-Dimensional Clinical Research
| Data Level | Measurement Resolution | Key Properties | Clinical Examples |
|---|---|---|---|
| Nominal | Lowest | Classification, membership | Biological species, blood type, gender [67] |
| Ordinal | Low | Comparison, level | Disease severity (mild, moderate, severe), Likert scales [67] |
| Interval | High | Difference, affinity | Celsius temperature, calendar year [67] |
| Ratio | Highest | Magnitude, amount | Age, height, weight, Kelvin temperature [67] |
Proximity in Biological Networks
The concept of chemical induced proximity (CIP) has emerged as a foundational mechanism in biology and drug discovery. CIP describes the process of intentionally inducing proximity between a target (e.g., a disease-related protein) and an effector (e.g., a ubiquitin E3 ligase) to modulate biological processes with high selectivity. This principle underlies several innovative therapeutic modalities, including:
- PROTACs (Proteolysis-targeting chimeras): Bifunctional molecules that induce target protein degradation [28].
- Molecular Glues: Monomeric molecules that promote interactions between proteins [28].
Translating this biological principle into a computational framework, network-based proximity measures quantify the relationship between drug targets and disease proteins within the human interactome, offering a powerful approach for predicting drug efficacy and repurposing opportunities [26].
Core Proximity Framework and Workflow
The following diagram illustrates the overarching workflow for applying proximity-based analysis to high-dimensional clinical data, from integration to interpretation.
Title: Proximity analysis workflow for clinical data.
Proximity Measurement Methodology
The core of the framework involves calculating a drug-disease proximity measure (z). This quantifies the network-based relationship between a set of drug targets (T) and disease-associated proteins (D) within the human interactome, which is a graph G comprising proteins as nodes and interactions as edges [26].
Protocol: Calculating Drug-Disease Proximity
- Input: A set of drug targets
Tand a set of disease proteinsDmapped onto the interactomeG. - Distance Calculation: Compute the shortest path length
d(t,d)for all pairs(t,d)wheret ∈ Tandd ∈ D. The overall distanced(T,D)between the drug and disease can be defined using several measures, with the closest measure (d_c) demonstrating superior performance [26]:d_c = mean( min( d(t,d) for all d ∈ D ) for all t ∈ T )
- Statistical Normalization (Z-score): Calculate the relative proximity
z_cby comparing the observed distanced_cto a null distribution generated by random sampling. This corrects for network topology biases (e.g., degree) [26].z_c = ( d_c - μ_{d_{rand}} ) / σ_{d_{rand}}- Here,
μ_{d_{rand}}andσ_{d_{rand}}are the mean and standard deviation of the distances betweenn_{rand}randomly selected protein sets (matched to the size and degree distribution ofTandD) and the disease proteinsD.
- Interpretation: A significantly negative
z_cvalue (e.g.,z_c < -1.5) indicates that the drug targets are closer to the disease proteins in the network than expected by chance, suggesting potential therapeutic efficacy [26].
Application Notes & Experimental Protocols
Protocol 1: In-silico Drug Efficacy Screening
This protocol uses the aforementioned proximity measure to screen for novel drug-disease associations (drug repurposing) and to validate known ones [26].
Table 2: Reagent Solutions for In-silico Screening
| Research Reagent | Function / Description | Example Source / Tool |
|---|---|---|
| Human Interactome | A comprehensive map of protein-protein interactions serving as the computational scaffold. | Consolidated databases (e.g., BioGRID, STRING) [26] |
| Drug-Target Annotations | A curated list of molecular targets for existing drugs. | DrugBank [26] |
| Disease-Gene Associations | A curated list of genes/proteins implicated in a specific disease. | OMIM database, GWAS catalog [26] |
| Proximity Calculation Script | Custom code (e.g., Python/R) to compute shortest paths and Z-scores on the network. | Implemented using graph libraries (e.g., NetworkX, igraph) |
Procedure:
- Data Curation:
- Obtain a high-quality, non-redundant human interactome.
- For the disease of interest (e.g., Type 2 Diabetes), compile a list of associated genes (
D) from OMIM and GWAS catalog. - For a library of drugs, compile their known protein targets (
T) from DrugBank.
- Network Proximity Analysis:
- For each drug-disease pair, calculate the proximity measure
z_cas detailed in Section 3.1. - Use a sufficient number of randomizations (
n_{rand} >= 1000) to generate a stable null model.
- For each drug-disease pair, calculate the proximity measure
- Result Validation:
- Known Associations: Confirm that drugs with established efficacy for the disease show significantly negative
z_cvalues. - Novel Predictions: Prioritize drug repurposing candidates based on strongly negative
z_cvalues for subsequent in vitro or clinical validation.
- Known Associations: Confirm that drugs with established efficacy for the disease show significantly negative
Protocol 2: A Hybrid ML-Bio Inspired Diagnostic Framework
This protocol combines a multilayer neural network with a nature-inspired Ant Colony Optimization (ACO) algorithm to handle high-dimensional clinical data for diagnostic purposes, enhancing predictive accuracy and computational efficiency [29].
Procedure:
- Data Preprocessing:
- Feature Encoding: Encode categorical clinical variables (e.g., lifestyle factors, nominal data) appropriately.
- Data Normalization: Scale all quantitative variables (interval, ratio) to a standard range.
- Model Training with ACO:
- Initialization: Train a multilayer feedforward neural network on the high-dimensional clinical dataset (e.g., male fertility profiles).
- Optimization: Use the ACO algorithm to perform adaptive parameter tuning, overcoming limitations of conventional gradient-based methods. The ACO's proximity search mechanism efficiently explores the complex parameter space [29].
- Model Evaluation:
- Assess the model on a held-out test set of clinically profiled cases.
- Key Metrics: Report classification accuracy, sensitivity (recall), specificity, and computational time.
- Clinical Interpretability:
- Perform a feature-importance analysis (e.g., using permutation importance or SHAP values) on the trained model.
- This highlights key contributory risk factors (e.g., sedentary habits, environmental exposures), providing actionable insights for healthcare professionals [29].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Tool / Reagent | Category | Primary Function |
|---|---|---|
| Multi-layer Feedforward Neural Network | Machine Learning Model | Base predictive model for classifying complex clinical outcomes [29] |
| Ant Colony Optimization (ACO) | Bio-inspired Algorithm | Adaptive parameter tuning and efficient search in high-dimensional parameter spaces [29] |
| LASSO / Ridge Regression | Statistical Model | Regularized regression for variable selection and handling multicollinearity [66] |
| Random Forests / SVM | Machine Learning Model | Handling complex interactions in high-dimensional data for classification/regression [66] |
| PROTAC/Molecular Glue Degrader | Proximity-based Therapeutic | Induces proximity between a target protein and cellular machinery (e.g., E3 ligase) [28] |
| DrugBank / OMIM / GWAS Catalog | Data Resource | Provides critical drug-target and disease-gene annotation data [26] |
Advanced Analytical Pathways
The transition from traditional clinical data management to clinical data science necessitates the adoption of risk-based approaches and smart automation to manage computational complexity [68]. The following diagram details this analytical pathway.
Title: Evolving clinical data analysis pathways.
Protocol 3: Managing High-Dimensionality with Risk-Based Approaches
This protocol leverages a risk-based framework to focus computational resources on the most critical data points, thereby enhancing scalability [68].
Procedure:
- Cross-Functional Risk Assessment:
- Convene a team with clinical operations, data science, and biostatistics expertise.
- Identify critical-to-quality factors—the data points and endpoints most crucial to trial integrity and conclusions [68].
- Define Thresholds and Centralized Monitoring:
- Establish pre-defined thresholds for data trends that signal potential issues.
- Empower a centralized team to use smart automation tools to continuously monitor incoming data against these thresholds, rather than reviewing 100% of the data [68].
- Value Realization:
- This approach leads to higher data quality through proactive issue detection, greater resource efficiency, and shorter study timelines by reducing time to database lock [68].
Ensuring Robustness Against Data Disturbances and Noisy Clinical Inputs
The deployment of machine learning (ML) models in clinical environments presents a significant challenge: maintaining high performance when faced with data disturbances and noisy inputs that differ from curated training datasets. Model robustness—the ability to perform reliably despite variations in input data—is not merely an enhancement but a fundamental requirement for clinical safety and efficacy [69]. Within the context of proximity search mechanisms for clinical interpretability research, robustness ensures that the explanations and insights generated for researchers and clinicians remain stable and trustworthy, even when input data is imperfect. This document outlines application notes and experimental protocols to systematically evaluate and enhance model resilience, framing them as essential components for developing clinically interpretable and actionable AI systems.
Core Principles of Model Robustness
A model's performance in production can diverge significantly from its performance on clean test data. Understanding this distinction is critical.
- Accuracy vs. Robustness: Accuracy reflects a model's performance on clean, representative test data, whereas robustness measures its reliability when inputs are noisy, incomplete, adversarial, or drawn from a different distribution (out-of-distribution, or OOD) [69]. A model can be highly accurate yet brittle, failing on faint, rotated, or variably written digits in image analysis, or on clinical text with typos or non-standard abbreviations.
- Consequences of Non-Robust Models: Fragile models often result from overfitting to training data, lack of data diversity, or inherent biases [69]. In clinical settings, this can lead to security vulnerabilities (e.g., adversarial attacks), unfair treatment of patient subgroups, and critical diagnostic errors, potentially causing patient harm [69].
- The Role of Proximity Search: For clinical interpretability, a proximity search mechanism identifies and presents similar cases or influential data points from a repository to explain a model's prediction. If the underlying model is not robust, these explanations can be misleading or unstable. Ensuring model robustness thereby directly strengthens the credibility and utility of interpretability frameworks for research and drug development.
Quantitative Evidence of Robustness Challenges and Solutions
The following tables summarize empirical evidence from recent studies, highlighting the performance degradation caused by noisy inputs and the subsequent improvements achieved through robust optimization techniques.
Table 1: Impact of Noisy Inputs on Model Performance in Clinical Domains
| Clinical Domain | Model/Task | Clean Data Performance | Noisy Data Performance & Conditions | Key Findings |
|---|---|---|---|---|
| Clinical Text Processing [70] | High-performance NLP models | Outperformed human accuracy on clean benchmarks | Significant performance degradation with small amounts of character/word-level noise | Revealed vulnerability to real-world variability not seen in curated data. |
| Respiratory Sound Classification [71] | Deep Learning Classification | Established baseline on ICBHI dataset | ICBHI score dropped in multi-class noisy scenarios | Demonstrated challenge of real-world acoustic environments in hospitals. |
| ICU Mortality Prediction [11] | XGBoost (AUROC) | 0.924 (Dataset with imputation) | 0.834 (Dataset excluding missing data) | Highlighted performance sensitivity to data completeness and preprocessing. |
Table 2: Efficacy of Robustness-Enhancement Strategies
| Enhancement Strategy | Clinical Application | Performance Improvement | Key Outcome |
|---|---|---|---|
| Audio Enhancement Preprocessing [71] | Respiratory Sound Classification | 21.88% increase in ICBHI score (P<.001) | Significant improvement in robustness and clinical utility in noisy environments. |
| Data Augmentation with Noise [70] | Clinical Text Processing | Improved robustness and predictive accuracy | Fine-tuning on noisy samples enhanced generalization on real-world, noisy data. |
| Bio-Inspired Hybrid Framework [29] | Male Fertility Diagnostics | 99% accuracy, 100% sensitivity, 0.00006 sec computational time | Ant colony optimization for parameter tuning enhanced reliability and efficiency. |
| Ensemble Learning (Bagging) [69] | Image Classification (Generalizable) | Reduced classification errors | Combining multiple models (e.g., Random Forest) smoothed out errors and improved stability. |
Experimental Protocols for Assessing and Ensuring Robustness
Protocol: Robustness Checking and Stress Testing
This protocol provides a methodology for evaluating model resilience against data disturbances.
1. Objective To systematically assess a model's performance under various noisy and out-of-distribution conditions to identify failure modes and quantify robustness.
2. Materials and Reagents
- Trained ML Model: The clinical model under evaluation.
- Clean Test Dataset: A held-out, curated dataset for baseline performance.
- Noise Induction Tools: Software for perturbing inputs (e.g.,
nlpaugfor text,audiomentationsfor audio,albumentationsfor images). - OOD Datasets: Data from different sources, demographics, or clinical settings not seen during training.
- Evaluation Metrics: Task-specific metrics (e.g., AUROC, F1-score) and robustness-specific metrics (e.g., accuracy drop).
3. Procedure 1. Baseline Establishment: Evaluate the model on the clean test dataset to establish baseline performance. 2. Stress Testing with Noisy Inputs: - Text: Introduce character-level (random insertions, deletions, substitutions) and word-level (synonym replacement, random swap) perturbations [70]. - Audio: Add background noise from real clinical environments at varying Signal-to-Noise Ratios (SNRs) [71]. - Structured Data: Simulate sensor errors or missing data by randomly corrupting feature values. 3. OOD Evaluation: Test the model on the OOD datasets to simulate distribution shift. 4. Adversarial Example Testing (Optional for security-sensitive applications): Generate adversarial examples to probe for worst-case performance failures [69]. 5. Confidence Calibration Check: Assess whether the model's prediction probabilities align with the actual likelihood of being correct (e.g., via reliability diagrams) [69].
4. Analysis
- Compare performance metrics between clean, noisy, and OOD conditions.
- Calculate the relative performance degradation for each noise type.
- A robust model should exhibit minimal performance drop and well-calibrated confidence scores across all conditions.
Protocol: Integrating Audio Enhancement for Robust Clinical Audio Processing
This protocol details the integration of a deep learning-based audio enhancement module as a preprocessing step to improve robustness, as validated in [71].
1. Objective To enhance the quality of noisy respiratory sound recordings, thereby improving downstream classification performance and providing clean audio for clinician review.
2. Materials and Reagents
- Noisy Respiratory Sound Dataset: e.g., ICBHI dataset [71].
- Audio Enhancement Models: Pre-trained time-domain (e.g., Multi-view Attention Network) or time-frequency-domain (e.g., CMGAN) models.
- Classification Models: e.g., Convolutional Neural Networks (CNNs) or pretrained audio models like VGG16.
- Computational Environment: GPU-enabled hardware for efficient deep learning inference.
3. Procedure 1. Data Preparation: Segment respiratory audio recordings into standardized lengths. 2. Audio Enhancement: - Pass each noisy audio segment through the selected enhancement model. - The model will output a cleaned audio signal with background noise suppressed and respiratory sounds preserved. 3. Model-Assisted Diagnosis: - Path A (AI-Direct): Feed the enhanced audio directly into the classification model to obtain a prediction. - Path B (Clinician-Assisted): Provide the clinician with both the original and enhanced audio for listening, thereby improving diagnostic confidence and trust [71]. 4. Evaluation: Compare the classification performance (e.g., ICBHI score) using enhanced audio versus baseline (noisy audio or augmentation-only) across various noise conditions.
4. Analysis
- Quantify the improvement in classification metrics.
- Conduct a physician validation study to assess improvements in diagnostic sensitivity, confidence, and trust when using the enhanced audio [71].
Protocol: Data Augmentation with Noise Injection for Robust NLP
This protocol uses data augmentation to improve the robustness of clinical Natural Language Processing (NLP) models.
1. Objective To improve the robustness and generalization of clinical NLP models by fine-tuning them on text data that has been perturbed to simulate real-world noise and variability.
2. Materials and Reagents
- Clinical Text Corpus: A dataset of clinical notes, reports, or other text.
- Perturbation Methods: Libraries for character and word-level noise induction.
- Computational Resources: Standard CPU/GPU environment for NLP model training.
3. Procedure 1. Data Perturbation: - Apply a variety of perturbation methods to the training data. These can include: - Character-level: Random character insertion, deletion, substitution, or keyboard typo simulation. - Word-level: Random word deletion, synonym replacement, or local word swapping. - The goal is to create a augmented training set that mirrors the kinds of errors and variations found in real-world clinical documentation. 2. Model Fine-tuning: - Further fine-tune the pre-trained clinical NLP model on the combination of original and perturbed (noisy) samples. 3. Validation: - Evaluate the fine-tuned model on a held-out test set that contains both clean and noisy samples.
4. Analysis
- Compare the performance of the model fine-tuned with noise augmentation against the baseline model on noisy test data.
- The robust model should maintain higher accuracy and show less performance degradation when faced with perturbed inputs [70].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Robustness Research
| Item/Tool | Function/Benefit | Exemplar Use Case/Reference |
|---|---|---|
| Audio Enhancement Models (CMGAN) | Time-frequency domain model that enhances noisy audio, improving intelligibility for both models and clinicians. | Respiratory sound classification in noisy hospital settings [71]. |
Text Perturbation Libraries (e.g., nlpaug) |
Introduces character and word-level noise to simulate real-world text variability for training and stress-testing. | Improving robustness of clinical NLP systems via data augmentation [70]. |
| Bio-Inspired Optimization (Ant Colony) | Nature-inspired algorithm for adaptive parameter tuning, enhancing model generalizability and overcoming local minima. | Optimizing neural network parameters in male fertility diagnostics [29]. |
| Ensemble Methods (Random Forest) | Bagging (Bootstrap Aggregating) reduces model variance and overfitting by combining multiple models. | General image classification and structured data tasks; improves stability [69]. |
| Cross-Validation (k-Fold & Nested) | Assesses model generalizability across data splits and tunes hyperparameters without data leakage. | Standard practice in robust model development to prevent overfitting [69]. |
| Proximity Search Mechanism | Core to the thesis context; provides interpretability by finding similar cases, the reliability of which depends on underlying model robustness. | Foundation for clinical interpretability research [29]. |
Ensuring robustness against data disturbances is not an ancillary task but a core component of developing trustworthy AI for clinical research and drug development. The quantitative evidence and detailed protocols provided herein offer a roadmap for researchers to systematically harden their models against the inevitable noise and variability of real-world clinical data. By integrating these strategies—from audio enhancement and noise-based data augmentation to rigorous stress-testing—within a framework that prioritizes interpretability through proximity search, we can build clinical AI systems that are not only accurate but also reliable, transparent, and fit for purpose.
The integration of artificial intelligence (AI) into clinical and drug discovery research presents a fundamental challenge: the trade-off between model interpretability and predictive performance. Interpretable machine learning models provide understandable reasoning behind their decision-making process, though they may not always match the performance of their black-box counterparts [72]. This trade-off has sparked critical discussions around AI deployment, particularly in clinical applications where understanding decision rationale is essential for trust, accountability, and regulatory acceptance [73]. Within the context of clinical interpretability research, proximity-based mechanisms—which analyze relationships and distances within biological networks—offer a powerful framework for bridging this gap. These approaches allow researchers to quantify functional relationships between clinical entities, creating an explainable foundation for AI-driven insights [21]. The stakes for resolving this tension are particularly high in regulated drug development environments, where model transparency is not merely advantageous but often a prerequisite for regulatory submission and clinical adoption [73].
Quantitative Landscape: Measuring the Trade-off
Empirical studies reveal that the relationship between interpretability and performance is complex and context-dependent. Research indicates that, in general, learning performance improves as interpretability decreases, but this relationship is not strictly monotonic [72]. In certain scenarios, particularly where data patterns align well with interpretable model structures, interpretable models can demonstrate surprising competitive advantage over more complex alternatives.
Table 1: Quantitative Comparison of Model Archetypes in Clinical Applications
| Model Type | Predictive Accuracy Range | Interpretability Score | Clinical Validation Effort | Regulatory Acceptance |
|---|---|---|---|---|
| Linear Models | Moderate (65-75%) | High | Low | High |
| Tree-Based Models | Medium-High (75-85%) | Medium | Medium | Medium |
| Deep Neural Networks | High (85-95%) | Low | High | Low (Requires XAI) |
| XAI-Enhanced Black Box | High (85-95%) | Medium-High | Medium-High | Medium-High |
To better visualize the relationship between accuracy and interpretability, researchers have developed quantitative metrics such as the Composite Interpretability (CI) score, which helps visualize the trade-off between interpretability and performance, particularly for composite models [72]. This metric enables more systematic comparisons across different modeling approaches and helps identify optimal operating points for specific clinical applications.
Proximity-Based Frameworks for Clinical Interpretability
Network proximity analysis represents a powerful approach for embedding interpretability into clinical AI systems. By analyzing network distances between disease, symptom, and drug modules, researchers can predict similarities in clinical manifestations, treatment approaches, and underlying psychological mechanisms [21]. One study constructed a knowledge graph with 9,668 triples extracted from medical literature using BERT models and LoRA-tuned large language models, demonstrating that closer network distances between diseases correlate with greater clinical similarities [21].
Table 2: Proximity Metrics and Their Clinical Interpretations
| Proximity Relationship | Quantitative Measure | Clinical Interpretation | Referential Value |
|---|---|---|---|
| Disease-Disease | Shortest path distance in knowledge graph | Similarity in clinical manifestations, treatment approaches, and psychological mechanisms | Predictive for treatment repurposing |
| Symptom-Symptom | Co-occurrence frequency & modular distance | Likelihood of symptom co-occurrence in patient populations | Identifies clinical phenotypes |
| Symptom-Disease | Association strength in diagnostic pairs | Diagnostic confidence and pathological specificity | Higher for primary vs. differential diagnosis |
| Drug-Disease | Therapeutic proximity score | Efficacy prediction and mechanism similarity | Supports drug repositioning |
Proximity scores have demonstrated particular clinical utility in differentiating diagnostic relationships. Research shows that symptom-disease pairs in primary diagnostic relationships have a stronger association and are of higher referential value than those in general diagnostic relationships [21]. This quantitative approach to mapping clinical ontology creates an explainable foundation for AI-driven clinical decision support systems.
Experimental Protocols for Proximity-Informed Model Development
Protocol 1: Knowledge Graph Construction for Clinical Proximity Analysis
Objective: Construct a comprehensive clinical knowledge graph to enable proximity-based interpretability for AI models in drug discovery.
Materials & Reagents:
- Clinical corpus from biomedical literature (e.g., PubMed/MEDLINE)
- Computational infrastructure for natural language processing
- BERT-based models for named entity recognition
- LoRA (Low-Rank Adaptation) fine-tuning framework for large language models
- Graph database management system (e.g., Neo4j)
Methodology:
- Ontology Modeling: Establish entity types including diseases, symptoms, drugs, biomarkers, and biological mechanisms.
- Entity Recognition: Implement named entity recognition using BERT models fine-tuned on clinical text.
- Relationship Extraction: Use LoRA-tuned LLMs to extract semantic relationships between clinical entities from literature.
- Graph Population: Construct the knowledge graph with triples representing established relationships.
- Proximity Metric Calculation: Compute network distances between disease, symptom, and drug modules using shortest path algorithms.
- Validation: Correlate proximity scores with established clinical similarities and co-occurrence patterns.
Validation Criteria: Closer network distances among diseases should predict greater similarities in their clinical manifestations, treatment approaches, and psychological mechanisms [21].
Protocol 2: Explainable AI Integration for Drug-Target Interaction Prediction
Objective: Implement an explainable AI framework for drug-target interaction prediction that balances performance with mechanistic interpretability.
Materials & Reagents:
- Multi-omics datasets (genomics, proteomics, transcriptomics)
- Chemical compound libraries with structural information
- SHAP (SHapley Additive exPlanations) implementation
- Model interpretation libraries (LIME, Captum)
- High-performance computing cluster for deep learning
Methodology:
- Multi-Task Learning Architecture: Implement models that jointly learn multiple disease indications to boost statistical power while retaining disease-specific layers.
- Representation Learning: Generate low-dimensional embeddings of biological entities (proteins, compounds, diseases).
- Feature Attribution: Apply SHAP values to quantify the influence of each molecular feature on predictions.
- Biological Grounding: Interpret model outputs using concept activation vectors that link internal representations to human-understandable biological concepts.
- Proximity Integration: Incorporate network proximity metrics from Protocol 1 to constrain and explain model predictions.
- Experimental Validation: Prioritize compounds for in vitro testing based on explainable predictions.
Validation Criteria: Model explanations should align with established biological mechanisms and generate testable hypotheses for experimental validation [73].
Protocol 3: Regulatory-Grade Model Validation with Explainability Assessment
Objective: Establish validation protocols for AI models that meet regulatory standards for interpretability in clinical applications.
Materials & Reagents:
- Validation framework compliant with FDA/EMA guidelines
- Model interpretation toolkits (SHAP, LIME, prototype-based explanations)
- Cluster-based data splitting methodology
- Audit trail documentation system
Methodology:
- Cluster-Based Evaluation: Implement cluster-based data splitting to prevent model memorization of specific chemotypes and ensure generalization.
- Interpretability Metrics: Quantify explanation quality using fidelity, stability, and consistency measures.
- Domain Expert Review: Conduct structured reviews with clinical and biological experts to validate model explanations.
- Regulatory Documentation: Prepare comprehensive documentation of model reasoning, feature importance, and biological plausibility.
- Adversarial Testing: Challenge model explanations with counterfactual examples and edge cases.
- Continuous Monitoring: Establish ongoing explanation validation as part of model maintenance.
Validation Criteria: Models must provide faithful, testable explanations while maintaining predictive performance under cluster-based evaluation [73].
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Research Reagents for Interpretable AI in Clinical Research
| Research Reagent | Function | Application Context |
|---|---|---|
| SHAP (SHapley Additive exPlanations) | Quantifies feature contribution to predictions using cooperative game theory | Transforms model interpretability from visual cues to quantifiable metrics for biomarker prioritization |
| Concept Activation Vectors (CAVs) | Links model internals to human-understandable biological concepts | Maps AI decisions to established biological pathways and mechanisms |
| LoRA (Low-Rank Adaptation) | Efficiently fine-tunes large language models for specialized domains | Adapts foundation models to clinical text for knowledge graph construction |
| Cluster-Based Data Splitting | Prevents data leakage by splitting on molecular scaffolds | Ensures models generalize to novel chemotypes rather than memorizing structures |
| Multi-Task Learning Frameworks | Jointly models multiple disease indications with shared representations | Increases statistical power while maintaining disease-specific predictive accuracy |
| Prototypical Parts Models | Identifies representative cases used for model comparisons | Enables case-based reasoning by linking predictions to known clinical patterns |
Strategic Implementation Framework
Pathway to Clinically Actionable Interpretability
Achieving optimal balance between interpretability and performance requires a systematic approach tailored to specific clinical use cases. The following workflow illustrates the decision process for selecting appropriate modeling strategies:
Decision Framework for Model Selection
For High-Stakes Regulatory Submissions: Prioritize inherently interpretable models unless black-box approaches demonstrate substantial, validated performance advantages that justify additional explanation complexity [73].
For Exploratory Research: Leverage more complex models with advanced explainability techniques like SHAP and concept activation vectors to generate novel biological hypotheses [74].
For Clinical Decision Support: Implement hybrid approaches that combine predictive performance with case-based reasoning through prototypical parts models, aligning with physician decision-making processes [73].
Across All Contexts: Employ cluster-based validation as a guardrail to ensure models generalize to novel chemical structures and clinical patterns rather than memorizing training data [73].
The strategic balance between interpretability and predictive performance represents a critical consideration for AI-driven clinical research and drug development. Rather than accepting an inherent trade-off, researchers can leverage proximity-based frameworks and explainable AI techniques to create models that are both high-performing and clinically interpretable. By implementing the protocols and strategies outlined in this document, research teams can advance their AI initiatives while maintaining the transparency required for scientific validation and regulatory approval. The integration of network proximity metrics with advanced explanation methods creates a powerful paradigm for building trust in AI systems and accelerating the translation of predictive models into clinical impact.
Proving Clinical Utility: Validation, Benchmarking, and Comparative Analysis
Validation Frameworks for Proximity-Based Interpretability in Clinical Models
The integration of artificial intelligence (AI) into clinical decision-making has created an urgent need for models whose predictions are transparent and interpretable to clinicians. Proximity-based interpretability, which examines the relationships between data points in feature space, provides a powerful mechanism for understanding model reasoning by identifying similar clinical cases or influential training examples. This framework is particularly valuable in healthcare, where trust in AI outputs depends on the ability to validate predictions against clinical knowledge and similar patient histories. The Explainability-Enabled Clinical Safety Framework (ECSF) addresses this need by embedding explainability as a core component of clinical safety assurance, bridging the gap between deterministic safety standards and the probabilistic nature of AI systems [75].
Foundational Concepts and Definitions
Proximity in Clinical Contexts
In clinical AI, proximity operates across multiple dimensions. Feature space proximity identifies patients with similar clinical presentations, laboratory values, and demographic characteristics, enabling case-based reasoning for model predictions. Temporal proximity is crucial for understanding disease progression and treatment response patterns in longitudinal data. Semantic proximity maintains clinical validity by ensuring that similar concepts in medical ontologies (e.g., related diagnoses or procedures) are treated as similar by the model, addressing challenges with clinical jargon and abbreviations in electronic health records [76] [75].
Interpretability Framework Components
Clinical interpretability frameworks incorporate both global interpretability, which provides an overall understanding of model behavior across the population, and local interpretability, which explains individual predictions for specific patients [75]. The ECSF framework emphasizes clinical intelligibility, requiring that explanations align with clinical reasoning processes and support validation by healthcare professionals [75]. This is achieved through techniques that convert probabilistic model outputs into interpretable evidence suitable for clinical risk assessment and decision-making.
Quantitative Validation Metrics for Proximity Methods
Effective validation of proximity-based interpretability requires quantitative metrics that assess both fidelity to the underlying model and clinical utility.
Table 1: Validation Metrics for Proximity-Based Interpretability Methods
| Metric Category | Specific Metrics | Clinical Interpretation | Target Threshold |
|---|---|---|---|
| Explanation Accuracy | Faithfulness, Stability | Consistency of explanations across similar patients | >0.8 (Scale 0-1) |
| Clinical Coherence | Domain Expert Agreement, Clinical Plausibility Score | Alignment with medical knowledge | >85% agreement |
| Performance Impact | AUC, Precision, Recall, F1-Score | Maintained predictive performance after explanation integration | AUC >0.8, F1 >0.75 |
| Stability | Explanation Consistency Index | Reliability across sample variations | >0.7 (Scale 0-1) |
These metrics enable systematic evaluation of whether proximity-based explanations faithfully represent model behavior while providing clinically meaningful insights. The multi-step feature selection framework developed for clinical outcome prediction demonstrated how stability metrics (considering sample variations) and similarity metrics (across different methods) can reach optimal levels, confirming validity while maintaining accuracy [77].
Experimental Protocols for Validation
Protocol 1: Global Feature Contribution Analysis
Objective: Validate that proximity-based feature importance aligns with established clinical risk factors.
Materials: EMR dataset (e.g., MIMIC-III), Python/R environment, SHAP/LIME libraries, statistical analysis software.
Procedure:
- Data Preparation: Extract patient cohorts with target outcome (e.g., AKI, mortality). Perform preprocessing including missing value imputation, feature scaling, and temporal alignment [77].
- Model Training: Implement tree-based ensemble methods (Random Forest, XGBoost) using a multi-step feature selection approach with univariate screening followed by multivariate embedded methods [77].
- Proximity Calculation: Compute patient similarity using Euclidean distance on normalized features for continuous variables and Jaccard similarity for categorical variables.
- Explanation Generation: Apply SHAP analysis to quantify feature contributions. For clinical outcome prediction, this has successfully identified key predictors such as laboratory values and vital signs [78] [79].
- Validation: Compare identified features against established clinical risk factors through expert review. Calculate agreement metrics and refine proximity measures based on discordance.
Validation Criteria: Feature importance rankings must demonstrate significant correlation (Kendall's Ï„ > 0.6) with evidence-based clinical priorities.
Protocol 2: Local Case-Based Reasoning Validation
Objective: Verify that similar cases identified through proximity metrics provide clinically relevant explanations for individual predictions.
Materials: Clinical dataset with diverse cases, domain expert panel, similarity calculation infrastructure.
Procedure:
- Case Selection: Randomly sample 50-100 predictions from test set across outcome categories (true positives, false positives, true negatives, false negatives).
- Neighbor Identification: For each case, identify k-nearest neighbors (k=5-10) using proximity measures in the latent feature space.
- Expert Evaluation: Convene clinical expert panel to assess whether identified neighbors share clinically meaningful similarities with the index case using Likert scales (1-5) for relevance.
- Quantitative Analysis: Calculate proportion of cases where majority of neighbors share clinically relevant characteristics. Assess correlation between neighbor similarity strength and model confidence.
- Iterative Refinement: Adjust proximity metric weights based on expert feedback to better align with clinical similarity perceptions.
Validation Criteria: ≥80% of cases should have at least 3/5 neighbors rated as clinically relevant (score ≥4) by domain experts.
Protocol 3: Temporal Proximity Validation for Longitudinal Predictions
Objective: Validate that temporal proximity measures capture clinically meaningful disease progression patterns.
Materials: Longitudinal EMR data, temporal similarity algorithms, clinical outcome annotations.
Procedure:
- Temporal Alignment: Align patient trajectories using anchor points (e.g., diagnosis date, procedure date).
- Similarity Calculation: Implement dynamic time warping or other temporal similarity measures to assess proximity across patient trajectories.
- Outcome Stratification: Group patients with similar temporal patterns and assess association with clinical outcomes.
- Clinical Validation: Convene clinical review to assess whether identified temporal clusters represent recognizable clinical phenotypes or progression patterns.
- Predictive Validation: Test whether temporal proximity improves outcome prediction compared to static features alone.
Validation Criteria: Temporal proximity measures should significantly improve prediction accuracy (AUC increase >0.05) and identify clinically recognizable progression patterns.
Visualization Framework
The following diagrams illustrate key workflows and relationships in proximity-based interpretability validation.
Proximity Validation Workflow
ECSF Explainability Checkpoints
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools for Proximity-Based Interpretability Research
| Tool Category | Specific Solutions | Function | Implementation Example |
|---|---|---|---|
| Explainability Algorithms | SHAP, LIME, Integrated Gradients | Quantify feature contributions to predictions | SHAP analysis for feature importance in clinical outcome models [77] [78] |
| Proximity Metrics | Euclidean Distance, Cosine Similarity, Dynamic Time Warping | Calculate patient similarity in feature space | Multi-step feature selection with stability analysis [77] |
| Visualization Libraries | Matplotlib, Seaborn, Plotly | Create interpretable visualizations of model reasoning | t-SNE visualization for cluster coherence in ACL outcome prediction [80] |
| Model Architectures | Kolmogorov-Arnold Networks (KANs), Tree-based Ensembles | Balance predictive performance with interpretability | KANs for QCT imaging classification with SHAP interpretation [79] |
| Clinical Validation Tools | Expert Review Protocols, Agreement Metrics | Assess clinical relevance of explanations | ECSF framework for clinical safety assurance [75] |
Case Studies in Clinical Domains
Acute Kidney Injury Prediction
A multi-step feature selection framework applied to MIMIC-III data demonstrated effective dimensionality reduction from 380 to 35 features while maintaining predictive performance (Delong test, p > 0.05) for AKI prediction [77]. The approach integrated data-driven statistical inference with knowledge verification, prioritizing features based on accuracy, stability, and similarity metrics. As the number of top-ranking features increased, model accuracy stabilized while feature subset stability reached optimal levels, confirming framework validity [77].
Esophageal Squamous Cell Carcinoma Prognosis
An interpretable machine learning model for survival prediction in unresectable ESCC patients achieved AUC values of 0.794 (internal test) and 0.689 (external test) [78]. SHAP analysis identified key prognostic factors including tumor response, age, hypoalbuminemia, hyperglobulinemia and hyperglycemia. Risk stratification using a nomogram-derived cutoff revealed significantly different 2-year overall survival between high-risk and low-risk patients (21.3% vs 58.6%, P < 0.001) [78].
Cement Dust Exposure Classification
Kolmogorov-Arnold networks (KANs) were applied to quantitative CT imaging data for classifying cement dust-exposed patients, achieving 98.03% accuracy and outperforming traditional methods including TabPFN, ANN, and XGBoost [79]. SHAP analysis highlighted structural and functional lung features such as airway geometry, wall thickness, and lung volume as key predictors, supporting model interpretability and clinical translation potential [79].
Implementation Considerations for Clinical Settings
Successful implementation of proximity-based interpretability frameworks requires addressing several practical considerations. Computational efficiency must be balanced against explanation quality, particularly for real-time clinical decision support. The ECSF framework addresses this by embedding explainability checkpoints within existing clinical safety processes without creating new artefacts [75]. Clinical workflow integration necessitates explanations that are both accurate and efficiently consumable during patient care activities. Regulatory compliance requires alignment with emerging standards including the EU AI Act and NHS AI Assurance frameworks, which emphasize transparency and human oversight for high-risk AI systems [75].
For model validation, protocols should incorporate both quantitative metrics and qualitative clinical assessment. Studies should report not only traditional performance measures (accuracy, AUC) but also interpretability-specific metrics including explanation fidelity, stability, and clinical coherence. The multi-step feature selection approach demonstrated how considering sample variations and inter-method feature similarity can optimize feature selection while maintaining clinical interpretability [77].
Proximity-based interpretability provides a powerful framework for validating clinical AI systems by linking model predictions to clinically meaningful concepts of patient similarity and feature relevance. The validation protocols and metrics presented here offer a structured approach for assessing both the technical soundness and clinical utility of explanations. As clinical AI systems become more pervasive, robust validation frameworks that prioritize transparency and alignment with clinical reasoning will be essential for building trust and ensuring safe implementation. Future work should focus on standardizing validation protocols across clinical domains and developing more sophisticated proximity metrics that capture complex clinical relationships.
The integration of artificial intelligence (AI) in clinical and biomedical research is fundamentally shifting from purely performance-driven "black-box" models toward interpretable, biologically-grounded frameworks. Proximity-driven models represent this new paradigm, using known biological networks—such as protein-protein interactions or metabolic pathways—as a structural scaffold to guide AI predictions [27]. This approach contrasts with traditional black-box AI, which, despite often delivering high predictive accuracy, operates with opaque internal logic that limits its trustworthiness and clinical adoption [81]. This document provides application notes and experimental protocols for evaluating these competing AI architectures, with a specific focus on their applicability, interpretability, and performance in drug discovery and clinical research.
Application Notes: Contrasting Paradigms in Clinical AI
Core Conceptual Differences and Clinical Implications
The fundamental difference between these paradigms lies in their starting point and operational logic.
- Proximity-Driven Models are built upon established biological knowledge. For instance, Network Proximity Analysis (NPA) uses an interactome network—a comprehensive map of known molecular interactions—to compute the proximity between a drug's known protein targets and genes associated with a disease [27]. The core hypothesis is that the closer a drug's targets are to disease genes in this network, the higher its potential therapeutic efficacy. This provides a native, mechanistically interpretable output.
- Traditional 'Black-Box' AI (including many deep learning models) often operates as a data-in, prediction-out system. It identifies complex, non-linear patterns from large datasets without explicitly revealing the reasoning behind its conclusions. In clinical contexts, this creates a significant "interpretability gap" [81]. For example, a deep learning model might accurately classify a retinal image as indicative of glaucoma but fail to provide a human-understandable rationale for the clinician to verify [82].
The clinical implications of this dichotomy are profound. Proximity-driven models generate inherently testable hypotheses based on biological proximity, directly suggesting potential drug repurposing candidates [27]. In contrast, the outputs of black-box models, while potentially accurate, are difficult to integrate into clinical reasoning without post-hoc explanation tools, raising concerns about safety and accountability [81].
Quantitative Performance and Applicability
Performance metrics reveal a trade-off between sheer predictive power and biological plausibility. The table below summarizes a comparative analysis based on published applications.
Table 1: Comparative Analysis of Proximity-Driven vs. Black-Box AI in Biomedicine
| Feature | Proximity-Driven Models | Traditional 'Black-Box' AI |
|---|---|---|
| Primary Data Input | Knowledge graphs (e.g., interactomes), GWAS data [27] | Multimodal data (e.g., medical images, EHRs, molecular structures) [83] [84] |
| Interpretability | High, inherent to model structure [27] | Low, requires post-hoc explanation tools (e.g., SHAP) [85] [81] |
| Sample Efficiency | High; effective with rare disease datasets [27] | Low; requires very large, labeled datasets [83] |
| Key Strength | Hypothesis generation for drug repurposing, mechanistic insight [27] | High raw accuracy in pattern recognition (e.g., image classification) [85] [84] |
| Typical Output | Z-score of drug-disease proximity [27] | Classification (e.g., malignant/benign) or probability score [86] |
| Clinical Trust | High, due to transparent reasoning [81] | Low to moderate, hindered by opacity [81] |
| Representative Performance | Identified 42 licensed drugs with high proximity (z-score ≤ -2.0) for PSC [27] | Achieved 97.4% accuracy in plant disease classification [85]; Reduced drug discovery timeline from 4-5 years to 12-18 months [82] |
Emerging Hybrid Approaches and Future Trends
The emerging trend is not a wholesale replacement of one paradigm by the other, but rather a convergence into hybrid systems. Black-box models are being augmented with explainable AI (XAI) techniques like SHapley Additive exPlanations (SHAP) to highlight which features (e.g., pixels in an image) most influenced a decision [85]. Conversely, the powerful pattern recognition of deep learning is being used to refine and enrich the biological networks that underpin proximity models. Furthermore, novel evaluation frameworks like the Clinical Risk Evaluation of LLMs for Hallucination and Omission (CREOLA) are being developed to assess generative AI models on dimensions beyond accuracy, including narrative consistency and safety, which are critical for clinical deployment [81].
Experimental Protocols
Protocol 1: Network Proximity Analysis for Drug Repurposing
This protocol details the methodology for using NPA to identify novel therapeutic candidates for a defined disease, as applied to Primary Sclerosing Cholangitis (PSC) [27].
1. Objective: To computationally identify already licensed drugs with potential efficacy for PSC by measuring their network proximity to disease-associated genes.
2. Research Reagent Solutions
Table 2: Essential Reagents and Resources for NPA
| Item | Function / Description | Source / Example |
|---|---|---|
| Disease Gene Set | A curated list of genes with genome-wide significant association to the target disease. | GWAS catalog, literature systematic review [27] |
| Interactome Network | A comprehensive map of known protein-protein interactions. | A publicly available human interactome [27] |
| Drug-Target Database | A repository linking drugs to their known molecular targets. | DrugBank [27] |
| NPA Computational Script | Code to calculate proximity metrics between drug targets and disease genes. | Validated Python code from Guney et al. [27] |
3. Workflow Diagram
4. Step-by-Step Procedure:
Step 1: Input Preparation
- 1.1 Disease Gene Curation: Conduct a systematic literature review to identify all genes with genome-wide significant associations (p < 5 × 10^-8) with PSC. Exclude HLA-associated SNPs and those without a clear gene assignment. This resulted in 26 unique genetic loci for PSC [27].
- 1.2 Drug-Target Definition: Obtain a list of drugs and their known, curated protein targets from the DrugBank database [27].
- 1.3 Network Selection: Utilize a previously validated, comprehensive human interactome network [27].
Step 2: Proximity Calculation
- 2.1 Path Computation: For each drug, calculate the shortest path distance in the interactome between each of its targets and the closest PSC-associated gene.
- 2.2 Calculate dc: For each drug, compute
d_c, the average of these shortest path distances across all its targets. - 2.3 Derive Z-score: Compare the observed
d_cto a null distribution generated by randomly selecting sets of genes from the network. The Z-score is calculated as(d_c - µ)/σ, where µ and σ are the mean and standard deviation of the null distribution. A Z-score ≤ -2.0 indicates significant proximity [27].
Step 3: Output and Validation
- 3.1 Candidate Ranking: Rank all drugs by their Z-score. For PSC, this identified 42 licensed medicinal products with Z ≤ -2.0, including immune modulators like Basiliximab (Z = -5.038) and Abatacept [27].
- 3.2 Prioritization: Filter the list to focus on compounds already licensed for other indications, as these are prime candidates for repurposing. The results form a hypothesis for experimental validation in disease-specific models.
Protocol 2: Evaluating a Black-Box Deep Learning Classifier
This protocol outlines the development and critical evaluation of a high-accuracy deep learning model for image-based diagnosis, highlighting steps to address its opaque nature.
1. Objective: To train a deep convolutional neural network (CNN) for plant disease classification and utilize explainable AI (XAI) to interpret its predictions [85].
2. Research Reagent Solutions
Table 3: Essential Reagents and Resources for DL Classification
| Item | Function / Description | Source / Example |
|---|---|---|
| Image Dataset | A large, labeled dataset of images for training and validation. | Turkey Plant Pests and Diseases (TPPD) dataset (4,447 images in 15 classes) [85] |
| Deep Learning Framework | Software environment for building and training neural networks. | PyTorch, TensorFlow |
| CNN Architecture | The specific model design for image feature extraction. | ResNet-9 [85] |
| XAI Tool | Software for post-hoc interpretation of model decisions. | SHAP (SHapley Additive exPlanations) [85] |
3. Workflow Diagram
4. Step-by-Step Procedure:
Step 1: Data Preparation
- 1.1 Data Curation: Assemble a large, labeled dataset. For the plant disease example, the TPPD dataset with 4,447 images across 15 classes was used. Address class imbalance through augmentation techniques [85].
- 1.2 Preprocessing: Split data into training, validation, and test sets. Apply standardization and augmentation (e.g., rotation, flipping) to improve model robustness.
Step 2: Model Training
- 2.1 Architecture Selection: Choose a suitable CNN architecture like ResNet-9, known for its efficiency and performance [85].
- 2.2 Hyperparameter Tuning: Systematically optimize parameters (e.g., learning rate, batch size) on the validation set.
- 2.3 Model Training: Train the model on the training set, using the validation set for early stopping to prevent overfitting.
Step 3: Evaluation and Explainability
- 3.1 Performance Metrics: Evaluate the final model on the held-out test set. Report standard metrics such as accuracy (97.4%), precision (96.4%), recall (97.09%), and F1-score (95.7%) [85].
- 3.2 Explainable AI (XAI) Analysis: To address the black-box problem, apply SHAP or similar methods to generate saliency maps. These maps highlight the pixels in the input image that were most influential for the model's prediction.
- 3.3 Expert Validation: Present these saliency maps to domain experts (e.g., plant pathologists) to verify that the model is relying on biologically relevant features (e.g., lesion boundaries, color variations) and not spurious correlations [85]. This step is critical for building clinical trust.
The adoption of artificial intelligence in clinical research necessitates robust explainability frameworks to decipher model decisions, foster trust, and ensure alignment with biomedical knowledge. Within a thesis investigating proximity search mechanisms for clinical interpretability, benchmarking against established eXplainable AI (XAI) tools provides a critical foundation. SHapley Additive exPlanations (SHAP), Local Interpretable Model-agnostic Explanations (LIME), and Gradient-weighted Class Activation Mapping (Grad-CAM) represent three pivotal approaches with distinct mathematical foundations and application domains [87] [88] [89]. These tools enable researchers to move beyond "black box" predictions and uncover the feature-level and region-level rationales behind model outputs, which is indispensable for validating AI-driven discoveries in drug development and clinical science [90] [91]. This document outlines formal application notes and experimental protocols for their implementation and benchmarking.
Core Concepts and Theoretical Foundations
SHAP (SHapley Additive exPlanations) is grounded in cooperative game theory, specifically Shapley values, to assign each feature an importance value for a particular prediction [88] [92]. It computes the average marginal contribution of a feature across all possible coalitions of features, ensuring a fair distribution of the "payout" (the prediction output) [92]. SHAP provides both local explanations for individual predictions and global insights into model behavior.
LIME (Local Interpretable Model-agnostic Explanations) operates by perturbing the input data around a specific instance and observing changes in the model's predictions [88]. It then fits a simple, interpretable surrogate model (e.g., linear regression) to these perturbed samples to approximate the local decision boundary of the complex model [87] [88]. LIME is designed primarily for local, instance-level explanations.
Grad-CAM (Gradient-weighted Class Activation Mapping) is a model-specific technique for convolutional neural networks (CNNs) that provides visual explanations [89]. It uses the gradients of any target concept (e.g., a class score) flowing into the final convolutional layer to produce a coarse localization map, highlighting important regions in the input image for the prediction [93] [89]. It has been successfully adapted for medical text and time series data by treating embedded vectors as channels analogous to an image's RGB channels [93].
Table 1: Theoretical and Functional Comparison of XAI Tools
| Characteristic | SHAP | LIME | Grad-CAM |
|---|---|---|---|
| Theoretical Basis | Game Theory (Shapley values) [92] | Local Surrogate Modeling [88] | Gradient-weighted Localization [89] |
| Explanation Scope | Local & Global [87] [92] | Local (instance-level) [88] [92] | Local (instance-level) [89] |
| Model Compatibility | Model-agnostic [92] | Model-agnostic [88] | Model-specific (CNNs) [89] |
| Primary Data Types | Tabular, Images, Signals [92] | Tabular, Images, Text [87] | Images, Text (via embedding), Signals [93] |
| Key Output | Feature importance values [87] | Feature importance for an instance [88] | Heatmap (saliency visualization) [89] |
Quantitative Benchmarking and Performance Metrics
Rigorous benchmarking of XAI tools requires assessing their performance against multiple quantitative and human-centered metrics. Studies evaluating these tools in clinical settings often focus on fidelity, stability, and clinical coherence.
Table 2: Quantitative Benchmarking Metrics and Representative Findings
| Metric | Definition | SHAP Performance | LIME Performance | Grad-CAM Performance |
|---|---|---|---|---|
| Fidelity | How well the explanation reflects the true model reasoning. | High with complex models like XGBoost; aligns with model coefficients in linear models [88] [92]. | Can struggle with complex, non-linear models due to linear surrogate limitations [88]. | High for CNN-based models; provides intuitive alignment with input regions [93] [94]. |
| Stability/ Consistency | Consistency of explanations for similar inputs. | High stability due to mathematically grounded approach [87] [88]. | Can exhibit instability across runs due to random sampling for perturbations [87] [88]. | Generally stable for a given model and input [94]. |
| Computational Efficiency | Time and resources required to generate explanations. | Higher computational cost, especially with many features [88] [92]. | Faster, more lightweight computations [88] [92]. | Efficient once model is trained; requires a single backward pass [89]. |
| Clinical Coherence (Human Evaluation) | Alignment of explanations with clinical knowledge, as rated by experts. | N/A (Feature-based) | In chest radiology, rated lower than Grad-CAM in coherency and trust [94]. | In chest radiology, superior to LIME in coherency and trust, though clinical usability noted for improvement [94]. |
Experimental Protocols for Benchmarking XAI Tools
Protocol 1: Benchmarking on Tabular Clinical Data (SHAP vs. LIME)
Objective: To compare the fidelity, stability, and sparsity of SHAP and LIME explanations for classification tasks on tabular clinical data (e.g., from Electronic Health Records).
Materials:
- Dataset: Pre-processed clinical dataset (e.g., UK Biobank data for myocardial infarction classification [92]).
- Models: A suite of trained models with varying complexity (e.g., Logistic Regression, Decision Tree, XGBoost, Support Vector Machine) [88] [92].
- Software: Python environments with
shap,lime,scikit-learn, andnumpylibraries.
Procedure:
- Model Training: Train and validate each ML model on the chosen clinical dataset, ensuring performance metrics (e.g., AUC-ROC, accuracy) are documented.
- Explanation Generation: For a defined subset of test instances (e.g., 100 instances):
- SHAP: Calculate SHAP values using the appropriate explainer (e.g.,
TreeExplainerfor tree-based models,KernelExplainerfor others). Record the top-k contributing features for each instance [92]. - LIME: Generate LIME explanations using the
LimeTabularExplainer. Similarly, record the top-k features for each instance [88].
- SHAP: Calculate SHAP values using the appropriate explainer (e.g.,
- Metric Calculation:
- Fidelity: For LIME, measure the fidelity as the accuracy of the surrogate model in predicting the black-box model's outputs on the perturbed samples [88].
- Stability: For a single test instance, generate multiple explanations by slightly varying the random seed (for LIME) or approximation parameters (for SHAP). Calculate the Jaccard similarity index of the top-k features across runs [88].
- Sparsity: Calculate the percentage of total features that constitute the top 80% of the cumulative importance in a given explanation [88].
- Analysis: Compare the distributions of these metrics across different models and between SHAP and LIME. Assess whether identified features align with known clinical biomarkers.
Protocol 2: Benchmarking on Medical Imaging Data (Grad-CAM vs. LIME)
Objective: To evaluate the clinical relevance and coherence of visual explanations for a deep learning-based diagnostic system in chest radiology.
Materials:
- Dataset: Labeled chest X-ray or CT scan dataset (e.g., for pneumonia or COVID-19 detection [94]).
- Model: A trained CNN-based model (e.g., ResNet, VGG) for the specific diagnostic task.
- Software: Python with
PyTorch/TensorFlow,OpenCV,grad-camlibrary, andlimefor images.
Procedure:
- Model Inference: Run the trained CNN on a set of test images to obtain predictions.
- Explanation Generation:
- Grad-CAM: Extract the final convolutional layer activations and the gradients of the target class score. Compute the Grad-CAM heatmap by weighting the activation maps by the mean gradients and applying a ReLU activation [89] [94]. Overlay the heatmap on the original image.
- LIME: For the same image, use
LimeImageExplainerto generate superpixels. Perturb these superpixels and observe the model's output changes to identify the most important regions [94].
- Human-Centered Evaluation:
- Study Design: Conduct a user study with clinical professionals (e.g., radiologists).
- Task: Present participants with original images alongside explanations from both Grad-CAM and LIME, without revealing the method used.
- Assessment: Use Likert-scale questionnaires to rate each explanation on:
- Clinical Relevance: Does the highlighted region correspond to anatomically/pathologically relevant areas?
- Coherency: Is the explanation clear and logically consistent?
- Trust: Does the explanation increase confidence in the model's prediction? [94]
- Analysis: Perform quantitative analysis (e.g., paired t-tests) on the ratings to determine if there is a statistically significant preference for one method over the other in a clinical context.
Diagram 1: Workflow for comparative benchmarking of XAI tools.
The Scientist's Toolkit: Research Reagents and Materials
Table 3: Essential Research Reagents for XAI Benchmarking
| Tool / Resource | Function / Purpose | Example Source / Implementation |
|---|---|---|
| SHAP Library | Python library to compute SHAP values for any model. | pip install shap [92] |
| LIME Library | Python library for generating local surrogate explanations. | pip install lime [88] |
| Grad-CAM Implementation | Codebase for generating gradient-weighted class activation maps. | grad-cam library or custom implementation per [89] |
| Clinical Datasets | Benchmark data for validation (Tabular & Imaging). | UK Biobank [92], CheXpert [94], MIMIC-CXR [94] |
| Deep Learning Framework | Platform for building and training CNN models. | PyTorch, TensorFlow [93] [94] |
| Model Zoo (Pre-trained CNNs) | Pre-trained models for transfer learning and Grad-CAM. | Torchvision models (ResNet, VGG) [93] |
Comparative Analysis and Strategic Selection Framework
Selecting the appropriate XAI tool depends on the model type, data modality, and the specific research question. The following diagram provides a strategic framework for this selection within a clinical interpretability research context.
Diagram 2: Decision framework for selecting an XAI tool.
Application Note: The Role of Proximity Mechanisms in Clinical AI
Proximity-based systems in clinical artificial intelligence (AI) utilize computational methods to identify and weigh the "closeness" of patient data to known clinical patterns or outcomes. This application note details how these mechanisms, particularly proximity search, enhance diagnostic accuracy and foster clinician trust by making AI recommendations more interpretable and actionable. The core principle involves mapping complex patient data onto a structured feature space where proximity to diagnostic classes or risk clusters can be quantified and explained.
Recent research underscores that the interpretability provided by proximity-based frameworks is crucial for clinical adoption. A study on an AI for breast cancer diagnosis found that while explanations are vital, their design and implementation require careful calibration, as increasing explanation levels did not automatically improve trust or performance [95]. Conversely, a hybrid diagnostic framework for male fertility that integrated a nature-inspired optimization algorithm to refine predictions achieved a 99% classification accuracy and 100% sensitivity by effectively leveraging proximity-based feature analysis. This system highlighted key contributory factors like sedentary habits, providing clinicians with clear, actionable insights [29].
The challenge lies in translating technical interpretability into clinical understanding. A study on ICU mortality prediction emphasized that consistency in identified predictors—such as lactate levels and arterial pH—across different models and explanation mechanisms is key to fostering clinician trust and adoption [11]. Furthermore, research on predictive clinical decision support systems (CDSS) confirms that perceived understandability and perceived technical competence (accuracy) are foundational to clinician trust. Additional factors like perceived actionability, the presence of evidence, and system equitability also play significant roles [96]. These findings indicate that proximity-based systems must be evaluated not just on raw performance, but on their integration into the clinical workflow and their ability to provide coherent, consistent explanations that align with clinical reasoning.
The following tables consolidate key performance metrics and trust-influencing factors from recent studies on AI diagnostic and proximity-based systems.
Table 1: Diagnostic Performance Metrics of Featured AI Systems
| System / Study | Clinical Application | Key Metric | Performance Value | Key Proximity/Interpretability Feature |
|---|---|---|---|---|
| Hybrid Diagnostic Framework [29] | Male Fertility | Accuracy | 99% | Ant Colony Optimization for feature selection |
| Sensitivity | 100% | |||
| Computational Time | 0.00006 sec | |||
| MAI Diagnostic Orchestrator (MAI-DxO) [97] | Complex Sequential Diagnosis (NEJM Cases) | Diagnostic Accuracy | 79.9% (at lower cost) to 85.5% | Virtual panel of "doctor agents" for hypothesis testing |
| Cost per Case | ~$2,397 | |||
| RF & XGBoost Models [11] | ICU Mortality Prediction | AUROC (RF, Dataset 1) | 0.912 | Multi-method interpretability for consistent predictors |
| AUROC (XGBoost, Dataset 1) | 0.924 | |||
| Human Physicians [97] | Complex Sequential Diagnosis (NEJM Cases) | Diagnostic Accuracy | 20% | N/A |
| Cost per Case | ~$2,963 |
Table 2: Factors Influencing Clinician Trust in AI-CDSS
| Factor | Description | Supporting Evidence |
|---|---|---|
| Perceived Technical Competence | The belief that the system performs accurately and correctly. | Foundational factor for trust; concordance between AI prediction and clinician's impression is key [96]. |
| Perceived Understandability | The user's ability to form a mental model and predict the system's behavior. | Influenced by system explanations (global & local) and training; essential for trust [96]. |
| Perceived Actionability | The degree to which the system's output leads to a concrete clinical action. | A strong influencer of trust; clinicians desire outputs that directly inform next steps [96]. |
| Evidence | The availability of both scientific (macro) and anecdotal (micro) validation. | Both types are important for building and reinforcing trust in the system [96]. |
| Equitability | The fairness of the system's predictions across different patient demographics. | Concerns about fairness in predictions impact trustworthiness [96]. |
| Explanation Level | The depth and granularity of the reasoning provided for an AI recommendation. | Impact is not linear; increasing explanations does not always improve trust or performance [95]. |
Experimental Protocols
Protocol: Evaluating a Hybrid Proximity-Based Diagnostic Framework
This protocol outlines the methodology for developing and validating a bio-inspired optimization model for male fertility diagnostics, as detailed in [29].
Objective: To develop a hybrid diagnostic framework that combines a Multilayer Feedforward Neural Network with an Ant Colony Optimization (ACO) algorithm to enhance the precision and interpretability of male fertility diagnosis.
Materials:
- Dataset: A publicly available dataset of 100 clinically profiled male fertility cases, encompassing diverse lifestyle and environmental risk factors.
- Computational Environment: Standard machine learning workstation capable of running neural network and optimization algorithms.
Procedure:
- Data Preprocessing: Clean the clinical data, handle missing values, and normalize numerical features to ensure stable model training.
- Model Architecture Definition:
- Construct a Multilayer Feedforward Neural Network as the base classifier.
- Integrate an Ant Colony Optimization algorithm to adaptively tune the model's parameters. The ACO mimics ant foraging behavior, using a proximity search mechanism to efficiently explore the parameter space and find optimal solutions.
- Model Training & Optimization:
- The ACO algorithm is employed to overcome the limitations of conventional gradient-based methods, enhancing the model's predictive accuracy and generalizability.
- The optimization process aims to minimize classification error on the training data.
- Model Validation:
- Evaluate the trained model on a held-out set of unseen patient samples to assess its real-world performance.
- Record key metrics including classification accuracy, sensitivity, specificity, and computational time for prediction.
- Interpretability Analysis:
- Conduct a feature-importance analysis on the validated model.
- Rank the contribution of different input features (e.g., sedentary time, environmental exposures) to the final prediction to provide clinical interpretability.
Output: A validated diagnostic model with quantified performance metrics and a list of key clinical factors driving the predictions.
Protocol: Assessing Clinician Trust in a Predictive CDSS
This protocol is based on a qualitative study of factors influencing clinician trust in a machine learning-based CDSS for predicting in-hospital deterioration [96].
Objective: To explore and characterize the factors that influence clinician trust in an implemented predictive CDSS.
Materials:
- Study Participants: A cohort of clinicians (e.g., nurses and prescribing providers) who have worked with the predictive CDSS in a clinical setting.
- Data Collection Tool: A semi-structured interview guide designed to probe perceptions of understandability, accuracy, and other trust factors.
- Institutional Review Board (IRB) Approval: Must be obtained before study commencement.
Procedure:
- Participant Recruitment: Recruit a diverse group of clinicians from hospitals where the CDSS is actively implemented. Use methods like snowball sampling to broaden participation.
- Data Collection:
- Conduct one-on-one, semi-structured interviews with participants.
- Guide the conversation using the interview script, focusing on:
- Their perception of the system's accuracy (Perceived Technical Competence).
- Their understanding of how the system works and makes predictions (Perceived Understandability).
- The influence of system-provided explanations and training on their understanding.
- Allow space for participants to describe any additional factors affecting their trust.
- Data Analysis:
- Transcribe the interviews verbatim.
- Perform a directed deductive content analysis, coding the data against predefined concepts from a human-computer trust framework (e.g., understandability, technical competence).
- Perform an inductive content analysis to identify and characterize new, emergent themes that influence trust (e.g., actionability, evidence, equitability).
Output: A qualitative report detailing confirmed and newly discovered factors influencing clinician trust, which can inform the future design and implementation of CDSS.
System Visualization
Proximity-Based Clinical AI Workflow
Clinician Trust Factors in AI-CDSS
Research Reagent Solutions
Table 3: Essential Tools for Proximity-Based Clinical Interpretability Research
| Item / Resource | Function in Research | Application Example |
|---|---|---|
| Ant Colony Optimization (ACO) | A nature-inspired optimization algorithm that uses a proximity search mechanism to tune model parameters efficiently. | Used to enhance the predictive accuracy and generalizability of a neural network for male fertility diagnosis [29]. |
| Feature Importance Analysis | A post-hoc interpretability method that ranks the contribution of input features to a model's prediction. | Provided clinical interpretability by highlighting key factors like sedentary habits in a fertility diagnostic model [29]. |
| eICU Collaborative Research Database | A large, multi-center database of ICU patient data, used for developing and validating predictive models. | Served as the data source for developing and interpreting ML models for ICU mortality prediction [11]. |
| Sequential Diagnosis Benchmark (SDBench) | An interactive framework for evaluating diagnostic agents (human or AI) through realistic sequential clinical encounters. | Used to test the diagnostic accuracy and cost-effectiveness of AI agents like MAI-DxO on complex NEJM cases [97]. |
| Human-Computer Trust Framework | A conceptual framework defining key factors (e.g., understandability, technical competence) that influence user trust in AI systems. | Guided a qualitative study to uncover factors influencing clinician trust in a predictive CDSS for in-hospital deterioration [96]. |
The "black box" nature of advanced machine learning (ML) models presents a significant barrier to their adoption in clinical settings, where understanding the rationale behind a decision is as critical as the decision itself. The proximity search mechanism for clinical interpretability research addresses this challenge by providing a structured, auditable framework to align model reasoning with established clinical guidelines and expert knowledge. This alignment is not merely a technical exercise but a fundamental prerequisite for regulatory approval, clinical trust, and safe patient care. Research demonstrates that models achieving this alignment can reach remarkable performance, with one hybrid diagnostic framework for male fertility achieving 99% classification accuracy and 100% sensitivity, while maintaining an ultra-low computational time of 0.00006 seconds, highlighting the potential for real-time clinical application [29].
The core of this approach is a shift from viewing models as opaque endpoints to treating them as dynamic systems whose internal reasoning processes can be probed, measured, and validated against gold-standard clinical sources. This methodology is essential for navigating the increasingly complex regulatory landscape for AI/ML in healthcare. By 2025, global regulatory requirements, including those from the FDA, EMA, and under the EU's AI Act, mandate rigorous algorithmic transparency and validation [98] [99]. The proximity search framework serves as the methodological backbone for meeting these demands, enabling the systematic auditing and certification of clinical AI.
Foundational Concepts and Regulatory Landscape
The Proximity Search Mechanism in Clinical Research
The proximity search mechanism is a conceptual and computational model for evaluating and ensuring the clinical validity of an AI system's decision pathway. It functions by measuring the "distance" or "proximity" between the features, patterns, and logical inferences a model uses and the established knowledge embedded in clinical practice guidelines (CPGs), expert physician reasoning, and biomedical knowledge graphs. A shorter proximity indicates higher clinical plausibility and interpretability. This mechanism was notably used in a network proximity analysis study to identify candidate drugs for primary sclerosing cholangitis, calculating a proximity score (z-score) between drug targets and disease-associated genes within an interactome network [27]. This same principle can be extended to audit whether a model's "reasoning path" closely mirrors the pathways defined in clinical guidelines.
Clinical Practice Guidelines as the Audit Benchmark
Clinical Practice Guidelines (CPGs) are "systematically developed statements that provide evidence-based recommendations for healthcare professionals on specific medical conditions" [100]. They are the product of rigorous methodologies like the GRADE approach, which evaluates evidence quality across levels from A (high) to D (very low) [100]. In the context of auditing AI, CPGs serve as the objective, evidence-based benchmark against which model reasoning is compared. Modern audit frameworks integrate CPG recommendations directly into clinical workflows via Clinical Decision Support Systems (CDSS), embedding alerts and real-time guidance to ensure adherence to evidence-based protocols [100].
The Regulatory Imperative for Auditable AI
Regulatory bodies globally have established that robust audit trails are not optional but mandatory for clinical AI systems. The International Council for Harmonisation (ICH) guidelines, particularly ICH-GCP, form the global gold standard for clinical trial conduct, ensuring ethical integrity, data reliability, and patient safety [101]. The 2025 updates to ICH guidelines further emphasize risk-based monitoring and the integration of digital health tools, formalizing the use of advanced data analytics for compliance verification [101]. Furthermore, standards like ISO 13485 for medical device quality management systems and the FDA's Quality System Regulation (21 CFR Part 820) require comprehensive audit processes to verify design controls, risk management, and corrective action systems [99]. Failure to align with these standards can result in regulatory actions, warning letters, and failure to obtain market approval [102] [99].
Experimental Protocols for Auditing and Certification
This section provides detailed, actionable protocols for implementing the proximity search framework to audit and certify clinical AI models.
Protocol 1: Quantitative Proximity Analysis for Model Reasoning
This protocol measures the alignment between a model's feature importance and the risk factors prioritized in clinical guidelines.
- Objective: To quantitatively assess the proximity between model-derived feature importance and guideline-mandated clinical risk factors.
- Materials: Trained ML model, annotated clinical dataset, relevant Clinical Practice Guidelines (CPGs), computing environment with necessary libraries (e.g., Python, scikit-learn, SHAP).
- Procedure:
- Guideline Feature Extraction: Manually or automatically extract and list all diagnostic, prognostic, or predictive variables (e.g., laboratory values, symptoms, demographic factors) explicitly mentioned in the target CPGs. Assign each variable a guideline importance weight (e.g., Level A evidence = 1.0, Level B = 0.75, etc.) [100].
- Model Interpretation: Run the model on a held-out test set. Use a model-agnostic interpretation tool like SHAP (SHapley Additive exPlanations) to calculate the mean absolute SHAP value for each feature, representing its importance to the model's output.
- Proximity Calculation: For a set of n features, calculate the Proximity Alignment Score (PAS) using the following formula:
PAS = 1 - [ √( Σ (G_i - M_i)² ) / n ]whereG_iis the normalized guideline importance weight for feature i, andM_iis the normalized model importance (SHAP value) for feature i. A PAS closer to 1.0 indicates near-perfect alignment. - Statistical Validation: Perform a Spearman's rank correlation test between the ranked list of guideline features and the ranked list of model features. A significant positive correlation (p-value < 0.05) supports the hypothesis of alignment.
The following diagram illustrates this multi-step workflow:
Protocol 2: Expert-in-the-Loop Qualitative Audit
This protocol leverages clinical expertise to perform a qualitative assessment of model reasoning for individual cases.
- Objective: To obtain qualitative feedback from clinical experts on the plausibility of model explanations for specific predictions.
- Materials: A curated set of case studies (e.g., 20-30 patient records), model explanation outputs (e.g., SHAP force plots, LIME explanations), a panel of clinical experts (e.g., 3-5 physicians).
- Procedure:
- Case Selection: Select a stratified set of cases, including straightforward, complex, and edge-case scenarios. Include cases where the model's prediction matches the known outcome and where it disagrees.
- Explanation Generation: For each case, generate a localized explanation highlighting the top features that drove the model's prediction.
- Expert Evaluation: Present the case data, the model's prediction, and its explanation to the clinical experts. Experts independently score the explanation's plausibility on a Likert scale (e.g., 1: "Clinically Implausible" to 5: "Highly Plausible") without knowing the model's accuracy.
- Discrepancy Analysis: Convene a focus group to discuss cases with low plausibility scores. Analyze the root cause: is it a data artifact, a model error, or a novel but valid pattern discovered by the model?
- Certification Threshold: Define a pre-specified certification threshold (e.g., >85% of cases must achieve a plausibility score of 4 or 5) for the model to pass this audit stage.
Protocol 3: Regulatory Documentation and Audit Trail Generation
This protocol ensures all processes are documented to meet regulatory standards for inspections and certifications.
- Objective: To create a comprehensive, living documentation package that demonstrates model alignment with clinical guidelines and regulatory standards.
- Materials: Electronic Quality Management System (eQMS), documentation templates (e.g., for Algorithm Change Protocols), version-controlled repositories [98] [103].
- Procedure:
- Algorithmic Transparency Documentation: Create an "Algorithm Card" for the model, detailing its intended use, architecture, training data demographics, performance metrics, fairness assessments, and known limitations [98].
- Proximity Search Methodology Record: Document the exact methodology used for proximity analysis, including the source and version of the CPGs, the interpretation tool and its configuration, and the formulas used for all calculated scores.
- Change Control Protocol: Implement a versioning schema and an Algorithm Change Protocol (ACP) as required by the FDA. Any change to the model, data, or interpretation method must trigger a re-audit using the protocols above, with all changes documented in the audit trail [98].
- Audit Trail Map: Maintain a traceability matrix that links each model requirement (e.g., "shall be sensitive to lactate levels") to its corresponding guideline source, its implementation in the model, and the evidence of its validation from Protocols 1 and 2.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and tools required for implementing the described auditing and certification protocols.
Table 1: Essential Research Reagents and Tools for Clinical AI Auditing
| Item | Function in Auditing & Certification | Example Sources / Standards |
|---|---|---|
| Clinical Practice Guideline Repositories | Provides the evidence-based benchmark for evaluating model reasoning. | National Institute for Health and Care Excellence (NICE), U.S. Preventive Services Task Force (USPSTF), professional medical societies (e.g., IDSA) [100]. |
| Model Interpretation Libraries | Generates explanations for model predictions (e.g., feature importance). | SHAP, LIME, ELI5. |
| Healthcare Data Models & Standards | Ensures interoperability and correct structuring of clinical input data. | HL7 FHIR, SNOMED CT, LOINC, RxNorm [98]. |
| Audit Management Software | Streamlines the audit lifecycle, from planning and scheduling to tracking findings and corrective actions (CAPA) [103]. | Electronic Quality Management Systems (eQMS) like SimplerQMS, ComplianceQuest [102] [103]. |
| Regulatory Framework Documentation | Defines the compliance requirements for the target market. | ICH E6(R3)/E8(R1), FDA QSR (21 CFR Part 820), EU MDR, ISO 13485:2016 [101] [99]. |
Data Presentation and Analysis
The following tables summarize quantitative data and results from the application of the aforementioned protocols, providing a template for reporting.
Table 2: Sample Results from Quantitative Proximity Analysis (Hypothetical ICU Mortality Prediction Model)
| Clinical Feature | Guideline Importance (Gi) | Model Importance (Mi) | Alignment Deviation (Gi - Mi)² |
|---|---|---|---|
| Lactate Level | 1.00 | 0.95 | 0.0025 |
| Arterial pH | 0.95 | 0.45 | 0.2500 |
| Body Temperature | 0.80 | 0.82 | 0.0004 |
| Systolic BP | 0.75 | 0.78 | 0.0009 |
| ... | ... | ... | ... |
| Proximity Alignment Score (PAS): | 0.87 | ||
| Spearman's Ï (p-value): | 0.71 (0.02) |
Table 3: Sample Results from Expert Qualitative Audit (Hypothetical Data)
| Case ID | Model Prediction | Expert Plausibility Score (1-5) | Expert Comments |
|---|---|---|---|
| PT-001 | High Risk | 5 | "Explanation perfectly matches clinical intuition; lactate and pH are key." |
| PT-002 | Low Risk | 2 | "Model overlooked borderline low platelet count, which is concerning in this context." |
| PT-003 | High Risk | 4 | "Generally plausible, though the weight given to mild tachycardia seems excessive." |
| ... | ... | ... | ... |
| % Cases with Score ≥4: | 88% |
Integrated Workflow for End-to-End Certification
Combining the protocols and tools above creates a robust, repeatable workflow for the auditing and certification of clinical AI. The following diagram maps the complete, integrated process from model development to regulatory submission, highlighting the continuous feedback enabled by the proximity search mechanism.
This end-to-end workflow ensures that clinical AI systems are not only high-performing but also clinically interpretable, ethically aligned, and fully compliant with the stringent requirements of global regulatory bodies, thereby paving the way for their trustworthy integration into patient care.
Conclusion
Proximity search mechanisms represent a foundational shift towards creating clinically interpretable and trustworthy AI systems. By leveraging principles from both biological induced proximity and computational similarity search, these methodologies offer a path to demystify AI decision-making, which is paramount for their adoption in high-stakes biomedical research and clinical practice. The synthesis of evidence retrieval, intrinsic model interpretability, and rigorous validation provides a robust framework for building systems that clinicians and researchers can not only use but also understand and audit. Future directions should focus on the integration of these proximity-based interpretability tools into the entire drug development pipeline—from target discovery to clinical trials—and on developing standardized, regulatory-friendly frameworks for their evaluation. The ultimate goal is a new generation of AI that acts as a transparent, reliable partner in advancing human health.
References
- 1. Induced Proximity : Turning Molecular into... | Amgen Matchmakers [https://www.amgen.com/stories/2025/09/induced-proximity---turning-molecular-matchmakers-into-medicines]
- 2. resources.nu.edu/researchprocess/ proximity [https://resources.nu.edu/researchprocess/proximity]
- 3. Molecular matchmakers [https://pubmed.ncbi.nlm.nih.gov/8451638/]
- 4. A new approach for interpretability and reliability in clinical risk... [https://pubmed.ncbi.nlm.nih.gov/34127242/]
- 5. in Chemically and induced proximity biology medicine [https://pubmed.ncbi.nlm.nih.gov/29590011/]
- 6. Mandipropamid as a chemical of... | Nature inducer Chemical Biology [https://www.nature.com/articles/s41589-021-00922-3?error=cookies_not_supported&code=a50f88fb-b6c5-44b8-88e0-014895376ae6]
- 7. and Molecular in targeted protein degradation... glues PROTACs [https://pubmed.ncbi.nlm.nih.gov/40907798/]
- 8. How Do Molecular Differ from Glues ? PROTACs [https://www.emolecules.com/molecular-glues-vs-protacs-differences-mechanisms-therapeutic-impact]
- 9. and MGDs role in drug discovery PROTACs [https://www.news-medical.net/whitepaper/20250915/What-makes-PROTACs-and-MGDs-game-changers-in-drug-discovery.aspx]
- 10. [2411.03105] Evaluating Machine Learning Models against Clinical Protocols for Enhanced Interpretability and Continuity of Care [https://arxiv.org/abs/2411.03105]
- 11. [2508.00919] Translating Machine into... Learning Interpretability [https://arxiv.org/abs/2508.00919]
- 12. What are proximity measures for binary attributes? [https://www.educative.io/answers/what-are-proximity-measures-for-binary-attributes]
- 13. The proximity of ideas: An analysis of patent text using machine learning | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0234880]
- 14. Ithy - Optimization of Geospatial Proximity Search [https://ithy.com/article/geospatial-proximity-search-hneu9sd4]
- 15. Abstracts — 2025 for Healthcare Machine Learning [https://www.mlforhc.org/2025-abstracts]
- 16. On the importance of interpretable machine learning predictions to... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10013157/]
- 17. JMIR Medical Informatics - The Use of Machine Learning for Analyzing Real-World Data in Disease Prediction and Management: Systematic Review [https://medinform.jmir.org/2025/1/e68898]
- 18. Explainable AI in Healthcare: Transparency, Interpretability , and... [https://www.linkedin.com/pulse/explainable-ai-healthcare-transparency-explainability-jan-beger-i9i8f]
- 19. The complete guide to AI transparency, explainability, and interpretability [https://blog.stackaware.com/p/ai-transparency-explainability-interpretability-nist-rmf-iso-42001]
- 20. Medico 2025: Visual Question Answering (with multimodal explanations) for Gastrointestinal Imaging | MediaEval Benchmark [https://multimediaeval.github.io/editions/2025/tasks/medico/]
- 21. Research on the proximity relationships of psychosomatic disease knowledge graph modules extracted by large language models - PubMed [https://pubmed.ncbi.nlm.nih.gov/40594265/]
- 22. Top 5 Drug Discovery Trends 2025 Driving Breakthroughs [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/drug-discovery-trends-2025/]
- 23. TAC-tics for Leveraging Proximity Biology in Drug Discovery - PubMed [https://pubmed.ncbi.nlm.nih.gov/38015747/]
- 24. Chemically induced proximity in biology and medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6417506/]
- 25. Open Problems in Mechanistic Interpretability [https://arxiv.org/html/2501.16496v1]
- 26. Network-based in silico drug efficacy screening - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4740350/]
- 27. Network proximity analysis as a theoretical model for identifying... [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-024-01927-2]
- 28. Proximity-Based Modalities for Biology and Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10375889/]
- 29. Enhancing the precision of male fertility diagnostics through bio... [https://pubmed.ncbi.nlm.nih.gov/41145645/]
- 30. [2509.13338] Proximity - Based for... Evidence Retrieval [https://arxiv.org/abs/2509.13338]
- 31. Proximity search (text) - Wikipedia [https://en.wikipedia.org/wiki/Proximity_search_(text)]
- 32. Proximity Operators - Advanced Search Techniques - Research Guides at University of Alabama - Birmingham [https://guides.library.uab.edu/advancedsearch/proximity]
- 33. An adaptive term proximity rocchio's model for based ... clinical [https://pubmed.ncbi.nlm.nih.gov/31830960/]
- 34. (VT): ECG criteria, causes, classification... Ventricular tachycardia [https://ecgwaves.com/topic/ventricular-tachycardia-vt-ecg-treatment-causes-management/]
- 35. Ventricular Fibrillation and Tachycardia Detection Using Features Derived from Topological Data Analysis [https://www.mdpi.com/2076-3417/12/14/7248]
- 36. Predicting ventricular circuits in patients with... tachycardia [https://elifesciences.org/articles/88865]
- 37. JMIR Human Factors - Clinical Support Requirements for... Decision [https://humanfactors.jmir.org/2024/1/e55802/]
- 38. Computer-interpretable clinical guidelines: a methodological review - PubMed [https://pubmed.ncbi.nlm.nih.gov/23806274/]
- 39. Current Algorithms for the Diagnosis of wide QRS Complex Tachycardias - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4040878/]
- 40. An Interpretable Clinical Decision Support System Aims to Stage Age-Related Macular Degeneration Using Deep Learning and Imaging Biomarkers [https://www.mdpi.com/2076-3417/15/18/10197]
- 41. Frontiers | Artificial intelligence in clinical medicine: a state-of-the-art overview of systematic reviews with methodological recommendations for improved reporting [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1550731/full]
- 42. Mechanistic understanding and validation... | Nature Machine Intelligence [https://www.nature.com/articles/s42256-025-01084-w?error=cookies_not_supported&code=247eaed6-2b1a-4791-8eb2-cc46fb4862cc]
- 43. [2501.16496] Open Problems in Mechanistic Interpretability [https://arxiv.org/abs/2501.16496]
- 44. Semantic Similarity : Advances, Techniques... | Medium Algorithms [https://medium.com/@fatih_ayaz/semantic-similarity-algorithms-advances-techniques-and-emerging-trends-summary-article-f8f05645d9dd]
- 45. What is Similarity ? | Pinecone Search [https://www.pinecone.io/learn/what-is-similarity-search/]
- 46. AI-powered semantic search using pgvector and embeddings / Habr [https://habr.com/en/articles/792390/]
- 47. A scoping review of artificial intelligence applications in clinical trial risk assessment | npj Digital Medicine [https://www.nature.com/articles/s41746-025-01886-7]
- 48. Interpretable Clinical Classification with Kolgomorov- Arnold Networks [https://arxiv.org/html/2509.16750v1]
- 49. : KAN – Kolmogorov | OpenReview Arnold Networks [https://openreview.net/forum?id=Ozo7qJ5vZi]
- 50. Paper page - KAN : Kolmogorov - Arnold Networks [https://huggingface.co/papers/2404.19756]
- 51. New Proximity Search Feature Available in PubMed - NCBI Insights [https://ncbiinsights.ncbi.nlm.nih.gov/2022/11/30/proximity-search-feature-pubmed/]
- 52. Research on the proximity relationships of psychosomatic disease knowledge graph modules extracted by large language models | Scientific Reports [https://www.nature.com/articles/s41598-025-05499-8]
- 53. Interpretable Clinical with Kolgomorov- Classification Arnold Networks [https://arxiv.org/abs/2509.16750]
- 54. Thyroid disease classification using generative adversarial networks ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-025-03014-7]
- 55. Ensemble learning driven Kolmogorov - Arnold -based Lung... Networks [https://pmc.ncbi.nlm.nih.gov/articles/PMC11687918/]
- 56. and Target in Identification ... | SpringerLink Validation Drug Discovery [https://link.springer.com/book/10.1007/978-1-4939-9145-7]
- 57. Network-based multi-omics integrative analysis methods in drug ... [https://biodatamining.biomedcentral.com/articles/10.1186/s13040-025-00442-z]
- 58. Advances in highâ€throughput mass spectrometry in drug discovery - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9832828/]
- 59. Frontiers | Editorial: Advancing drug with AI: discovery –target... drug [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1721323/full]
- 60. Detecting and Mitigating the Clever Effect in Medical Imaging... Hans [https://pubmed.ncbi.nlm.nih.gov/39643820/]
- 61. Detecting and Mitigating the Clever Effect in Medical Imaging... Hans [https://link.springer.com/article/10.1007/s10278-024-01335-z]
- 62. in AI chest radiography analysis: integrating... Threshold optimization [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-025-00632-8]
- 63. Application of Mechanistic Multiparameter Optimization and Large-Scale In Vitro to In Vivo Pharmacokinetics Correlations to Small-Molecule Therapeutic Projects - PubMed [https://pubmed.ncbi.nlm.nih.gov/39135316/]
- 64. Monitoring metrics over time: Why clinical trialists need to systematically collect site performance metrics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7615148/]
- 65. Clinical Trial Risk Detection & Research Analytics Solutions | CluePoints [https://cluepoints.com/what-we-do/risk-based-quality-management-rbqm/detection/]
- 66. Using High - Dimensional in Data Trials - Simple Science Clinical [https://scisimple.com/en/articles/2025-11-10-using-high-dimensional-data-in-clinical-trials--a9n5lzo]
- 67. Ten simple rules to colorize biological data visualization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7561171/]
- 68. Trend Report | Veeva 2025 Clinical Data [https://www.veeva.com/2025-clinical-data-trend-report/]
- 69. Model Robustness Explained: OOD, Adversarial Testing and Best... [https://invisibletech.ai/blog/model-robustness-explained-methods-testing-and-best-practice]
- 70. Improving the Robustness and Accuracy of Intelligent Clinical Text... [https://papers.ssrn.com/sol3/papers.cfm?abstract_id=4052303]
- 71. JMIR AI - Improving the Robustness and Clinical Applicability of... [https://ai.jmir.org/2025/1/e67239/]
- 72. [2503.07914] Demystifying the Accuracy- Interpretability - Trade ... Off [https://arxiv.org/abs/2503.07914]
- 73. Can You Trust Your Model? Why Explainability Matters in AI-Driven... [https://ardigen.com/can-you-trust-your-model-why-explainability-matters-in-ai-driven-drug-discovery/]
- 74. Progress of AI-Driven Drug –Target Interaction Prediction and Lead... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563295/]
- 75. Embedding Explainable AI in NHS Clinical Safety: The... [https://arxiv.org/html/2511.11590v1]
- 76. An adaptive term proximity based rocchio’s model for clinical decision... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-019-0986-6]
- 77. An effective multi-step feature selection framework for clinical ... [https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/s12911-025-02922-y]
- 78. Development and Validation of an Interpretable Machine Learning Model | CMAR [https://www.dovepress.com/development-and-validation-of-an-interpretable-ml-model-for-survival-p-peer-reviewed-fulltext-article-CMAR]
- 79. Quantitative computed tomography imaging classification of cement dust-exposed patients-based Kolmogorov-Arnold networks - PubMed [https://pubmed.ncbi.nlm.nih.gov/40450965/]
- 80. Clinically Interpretable Modeling of ACL Reconstruction Outcomes Using Confidence-Aware Gait Analysis [https://www.mdpi.com/2673-7078/5/4/94]
- 81. Reframing Clinical Evaluation in the Era of Generative AI ... Models [https://premierscience.com/pjs-25-1011/]
- 82. Early evidence and emerging trends: How AI is shaping drug discovery and clinical development [https://www.drugtargetreview.com/article/158593/early-evidence-and-emerging-trends-how-ai-is-shaping-drug-discovery-and-clinical-development/]
- 83. AI in drug discovery and its clinical relevance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10302550/]
- 84. Artificial intelligence in healthcare and medicine: clinical applications... [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-03196-w]
- 85. Deep learning technique for plant disease classification and pest detection and model explainability elevating agricultural sustainability | BMC Plant Biology | Full Text [https://bmcplantbiol.biomedcentral.com/articles/10.1186/s12870-025-07377-x]
- 86. Mastering Classification Metrics: A Beginners Guide [Part 1: Accuracy, Precision, and Recall] | by Prateek Gaurav | Medium [https://medium.com/@prateekgaurav/mastering-classification-metrics-a-beginners-guide-part-1-accuracy-precision-and-recall-fbadc90654ab]
- 87. LIME vs SHAP : A Comparative Analysis of Interpretability Tools [https://www.markovml.com/blog/lime-vs-shap]
- 88. Let’s talk Explainable AI — A Dive into LIME and SHAP | Medium [https://medium.com/@lubah_99345/lets-talk-xai-a-comparative-analysis-of-lime-and-shap-c32b92e65070]
- 89. Introduction to Grad-CAM — XAI Tutorials [https://xai-tutorials.readthedocs.io/en/latest/_model_specific_xai/Grad-CAM.html]
- 90. A survey of explainable artificial intelligence in healthcare: Concepts, applications, and challenges - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2352914824001448]
- 91. Explainable AI for clinical and remote health applications: a survey on tabular and time series data | Artificial Intelligence Review [https://link.springer.com/article/10.1007/s10462-022-10304-3]
- 92. A Perspective on Explainable Artificial Intelligence Methods: SHAP and... [https://arxiv.org/html/2305.02012v3]
- 93. Grad-CAM-Based Explainable Artificial Intelligence Related to Medical Text Processing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10525184/]
- 94. Evaluating Explainable Artificial Intelligence (XAI) techniques in chest radiology imaging through a human-centered Lens - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11463756/]
- 95. The impact of AI explanations on clinicians ’ trust and diagnostic ... [https://www.researchwithnj.com/en/publications/the-impact-of-ai-explanations-on-clinicians-trust-and-diagnostic-]
- 96. JMIR Human Factors - Factors Influencing Clinician in... Trust [https://humanfactors.jmir.org/2022/2/e33960/]
- 97. AI system matches diagnostic while cutting medical costs accuracy [https://www.news-medical.net/news/20250702/AI-system-matches-diagnostic-accuracy-while-cutting-medical-costs.aspx]
- 98. Healthcare Analytics Implementation: Documentation [https://editverse.com/healthcare-analytics-implementation-documentation-2025/]
- 99. Medical Device Audits : Complete Compliance Guide - eLeaP 2025 [https://quality.eleapsoftware.com/medical-device-audits-complete-compliance-guide-2025/]
- 100. Practice Clinical Explained: 7 Key Facts Every Smart... Guidelines [https://www.sprypt.com/blog/clinical-practice-guidelines-complete-guide]
- 101. ICH Guidelines Simplified: Everything Researchers Need to Know [https://ccrps.org/clinical-research-blog/ich-guidelines-simplified-everything-researchers-need-to-know]
- 102. Audits in the Pharmaceutical Industry: Definition, Types, Formats, and Steps [https://simplerqms.com/pharmaceutical-audits/]
- 103. Best Practices in Internal Audits in the Pharmaceutical Industry [https://www.compliancequest.com/audit-management/internal-audit-in-pharmaceutical-industry/]